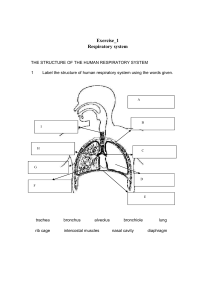
1 Respiratory Insufficiency Research Paper Gregory Go Stanbridge University PHIL 2010: Critical Reasoning and Ethics Professor Allison Lyon December 10, 2023 2 Respiratory Insufficiency Research Paper Introduction Gasping for each breath can mark a dire health crisis: respiratory insufficiency. When lungs fail to gather ample oxygen, both mind and body suffer—oxygen fuels them. We inhale air; our lungs purge carbon dioxide—a cellular byproduct. Life hinges on this exchange. Blood must carry oxygen from our lungs to nourish organs and tissues. Carbon dioxide overload can harm these vital parts, starving or delaying the delivery of life-giving oxygen. Without warning, breathing may halt abruptly—an acute event sparked by ailments like pneumonia or trauma such as opioid overdose and stroke; perhaps a spinal cord mishap plays its part too. A gradual onset exists: chronic respiratory failure, it's known as. Telltale signs may include breathlessness—as if starved for air—fatigue hitting hard, exercise becoming a challenge (once routine), overpowering sleepiness creeps in (van Goor et al., 2022). To confirm such failure, doctors assess blood for gas levels: How fast does one breathe? Are breaths shallow? They measure lung exertion too while considering lung function test outcomes. Treatments may demand added oxygen—through nasal tubes or even ventilators—if severity calls for it. With myriad causes yet ample treatments researched thoroughly, respiratory insufficiency stands out as prime material—for study and expanded understanding. Background Respiratory insufficiency can be seen as the impairment of respiratory gas exchange between the ambient air and circulating blood. Check arterial blood gases for all those gravely ill or with signs of lung fail. A must: chest x-rays. Echocardiography—often not routine, yet it can prove handy at times. PFTs might offer insight; while an ECG is vital to rule out heart issues 3 causing lung woes, and it might spot bad rhythms due to low oxygen or high acid in the blood. Some debate the value of right-heart cath tests.The main risk being organ failure due to lack of air (hypoxemia). Once hypoxemia is addressed, stabilize breathing and blood flow, we must hunt down and fix what caused the lung fail. Treatments will hinge on why the lungs failed first off. Respiratory failure strikes when the lungs fail at one or both tasks: adding oxygen to and taking carbon dioxide out of the blood. Medics split this condition into hypoxemic or hypercapnic types (Murat Kaynar, 2021). Type I, known as hypoxemic respiratory failure, happens with an arterial oxygen level (PaO2) below 60 mm Hg but normal or low CO2 pressure (PaCO2). Most lung diseases that happen fast—like fluid buildup or alveoli collapse—can lead to this kind. Fluid in the heart's sac, infection in the lungs, and bleeding within them serve as prime examples. Type II—or hypercapnic respiratory failure—shows a PaCO2 above 50 mm Hg. Patients breathing plain air often have low oxygen levels too. Bicarbonate levels, which play an important part in this process, tend to fluctuate in relation to the duration that one's carbon dioxide levels have been elevated. This type may stem from overdose, muscle nerve issues, odd chest walls, or severe airway problems—for instance asthma or COPD. One can also describe these failures as acute or chronic; acute cases are lifethreatening with quick changes in blood gases and body acid balance while chronic ones are less obvious without immediate danger signs. Acute hypercapnic failures take place within minutes to hours leading to pH values under 7.3; renal adjustments don't have time to kick in fully for bicarbonate increase. Yet over days—and sometimes more—the body adjusts and ups its bicarbonate thus not greatly dropping pH levels. Telling apart between long-term low oxygen failures versus sudden ones just by looking at blood gases is tricky indeed! Signs like increased red cell count—or heart strain due to lung disease—hint at persistent issues. 4 Fallacies, Myths, Emotions, and Biases Often associated with any illness are the false claims associated with the illness to either reflect relaxation or despair. Some of these include “respiratory insufficiency is rare”, “only smokers develop respiratory insufficiency”, “people with respiratory insufficiency cannot exercise”, “shortness of breath is the only symptom of respiratory insufficiency”, and “a healthy diet cannot help with respiratory insufficiency” (Newman, 2021). Contrary to these popular beliefs, there is proof in numbers and research, evidencing that these claims are wrong. While some of the notions put forth included the uncommonness of respiratory insufficiency, the idea that only smokers develop such a condition, the inability of those with respiratory insufficiency to exercise, shortness of breath being solely symptomatic, and diet having no impact, Newman in 2021 has challenged several of these preconceived notions. Contrary to these popular beliefs, there is proof in numbers and research, evidencing that these claims are wrong. According to the World Health Organization, respiratory insufficiency caused over 4 million deaths in 2019, making it the third leading cause of death worldwide (Newman, 2021). While tobacco smoking remains a primary cause of respiratory deficiencies, other environmental factors such as air pollution, occupational hazards, infections, and particular asthma types also notably endanger lung health. Approximately "10–20% of COPD patients never smoked" and can develop it due to "secondhand smoke exposure, genetic predisposition, or substantial exposure to air pollution” (Newman, 2021). A healthy diet can help respiratory insufficiency patients. Healthier diets rich in fruits and fish, likely owing to their fiber and omega-3 content respectively, have been found by studies exploring links between dietary patterns and COPD to correlate with a decreased prevalence and risk of the disease, whereas less nutritious eating habits devoid of such protective associations fail to share these benefits. 5 Exercise is actually recommended for respiratory insufficiency patients and can "increase their breathing capacity and improve their daily symptoms" according to doctors, though it may be difficult without proper guidance (Newman, 2021). Case Study Gunter Schleicher, Warren Lowman, and Guy Richards conducted a study on a patient with asthma and Covid-19, documenting the patient’s treatment plan associated with his respiratory insufficencies. Patient care was impacted in several ways throughout this case study: Asthma marked the patient for a tough fight against severe Covid-19 infection; hospital admission soon followed his deteriorating health. The case study warns, "Long-term corticosteroid users like asthmatics...might fail to rally an effective immune defense and thus are vulnerable to harsh impacts from a Covid-19 attack. Following his admittance, no progress came from antiviral meds alone. Over 5 days, "His condition plunged further downhill despite these drugs," says the case study (Schelicher et al., 2020). Markers in his blood also climbed sharply— proof that usual methods fell short. Soon after, he faced hyperinflammatory syndrome—CRS and ARDS—to signal grave danger. The study paints a grim picture: this state brings worsening ARDS, organ failures (MODS), blood clotting woes, heart inflammation—and often death. Doctors turned to corticosteroids (methylprednisolone) plus tocilizumab for treatment as they saw signs of hyperinflammation setting in. Relief was quick; within one day's time, he showed clear gains in health markers and symptoms eased enough so mechanical breath support wasn't needed. To conclude and summarize the case study, initial high-risk due to asthma was noted by the case study; typical remedies lacked effect; the disease advanced fiercely but tackling the 6 hyperinflammatory phase with specific drugs brought swift improvement—a win for patient care and healing. Evidence-Based Practice In order to provide the highest quality evidence-based patient care, it is imperative that one incorporates the most recently validated research that is directly applicable to the precise type of care being administered. Looking into the article regarding evidence-based practice for patients with respiratory insufficiency, a deep analysis will be conducted on Ervin and her colleague’s research. The evidence they provided conducted a systematic review of other review studies and guidelines to identify evidence-based practices that are recommended for treating patients receiving invasive mechanical ventilation for acute respiratory failure or acute respiratory distress syndrome (ARDS). It identified 20 evidence-based practices supported by over 117 individual studies involving more than 30,000 patients (Ervin et al.,2020). These practices covered the full continuum of care - from intubation and initiating mechanical ventilation, to preventing complications during ventilation, to safely removing ventilation. Some of the key evidence-based practices included using “low tidal volumes for lung-protective ventilation, conditional recommendations for higher positive end-expiratory pressure and prone positioning for moderate-severe ARDS, protocols to minimize sedation and delirium, early mobility, and ventilator liberation protocols” (Ervin et al., 2020). Their research categorized the 20 evidence-based practices into the three phases of care: 6 related to intubation and escalating care, 10 for preventing complications, and 4 for safely removing ventilation. It noted that optimizing the whole continuum is important rather than 7 focusing on individual parts. In summary, Ervin was able to identify and organize the current best practices for invasive ventilation based on various guidelines and reviews, to help clinicians provide optimal care across the full process for patients with respiratory failure or ARDS. Improved survival rates and quality of life after critical respiratory illness will lead to better long-term outcomes for these patients. Conclusion From the background of respiratory insufficiency to fallacies associated with the illness paired with evidence-based practice, studies and research can conclude that the illness can be severe or mild, varying from each individual case. Along with the condition of the illness comes the treatments that are currently valid within the medical community. With ongoing research, new treatments may emerge that can better manage symptoms and improve quality of life for those living with the condition. There is hope that future research will lead to more effective treatments leading to better patient outcomes and a decreased amount in population mortality rates because of respiratory insufficiency. 8 References Ervin, J. N., Rentes, V. C., Dibble, E. R., Sjoding, M. W., Iwashyna, T. J., Hough, C. L., Ng Gong, M., & Sales, A. E. (2020). Evidence-Based Practices for Acute Respiratory Failure and Acute Respiratory Distress Syndrome: A Systematic Review of Reviews. Chest, 158(6), 2381–2393. https://doi.org/10.1016/j.chest.2020.06.080 Murat Kaynar, A. (2021). Respiratory Failure. Medscape. https://emedicine.medscape.com/article/167981-overview?form=fpf Newman, T. (2021). 11 myths about COPD. Medical News Today. https://www.medicalnewstoday.com/articles/medical-myths-all-about-copd Schleicher, G. K., Lowman, W., & Richards, G. A. (2020). Case Study: A Patient with Asthma, Covid-19 Pneumonia and Cytokine Release Syndrome Treated with Corticosteroids and Tocilizumab. Wits Journal of Clinical Medicine, 2(SI), 47–52. https://doi.org/10.18772/26180197.2020.v2nSIa9 van Goor, H. M. R., Vernooij, L. M., Breteler, M. J. M., Kalkman, C. J., Kaasjager, K. A. H., & van Loon, K. (2022). Association of Continuously Measured Vital Signs With Respiratory Insufficiency in Hospitalized COVID-19 Patients: Retrospective Cohort Study. Interactive journal of medical research, 11(2), e40289. https://doi.org/10.2196/40289