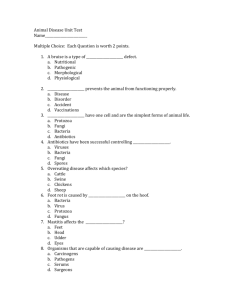
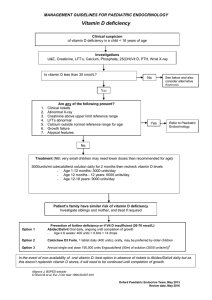
Overview of rickets in children Author: Thomas Carpenter, MD Section Editor: Joseph I Wolfsdorf, MD, BCh Deputy Editor: Alison G Hoppin, MD Contributor Disclosures All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Sep 2023. | This topic last updated: Jul 11, 2023. INTRODUCTION Normal bone growth and mineralization require adequate calcium and phosphate, the two major nutritional elements that constitute the crystalline component of bone. Deficient mineralization can result in rickets and/or osteomalacia. Rickets refers to deficient mineralization at the growth plate, as well as architectural disruption of this structure. Osteomalacia refers to impaired mineralization of the bone matrix. Rickets and osteomalacia usually occur together as long as the growth plates are open; only osteomalacia occurs after the growth plates have fused [1]. (See "Epidemiology and etiology of osteomalacia".) An overview of the pathogenesis, clinical presentation, and the differential diagnosis of rickets is presented here. The etiology and treatment of calcipenic and phosphopenic rickets are discussed separately. (See "Etiology and treatment of calcipenic rickets in children" and "Hereditary hypophosphatemic rickets and tumor-induced osteomalacia".) TYPES OF RICKETS Mineralization defects are classified according to the predominant mineral deficiency: ● Calcipenic rickets is caused by calcium deficiency, which usually is due to insufficient intake of vitamin D or failure to metabolize dietary vitamin D into its active form. In some cases, it is caused by insufficient intake or absorption of calcium in the setting of normal vitamin D levels. Calcipenic rickets may be associated with low serum calcium levels but also occurs in the setting of normocalcemia. ● Phosphopenic rickets is characterized by low serum levels of phosphorus, usually caused by renal phosphate wasting and, less commonly, by nutritional phosphorus deficiency. PATHOGENESIS Growth plate thickness is determined by two opposing processes [1]: ● Chondrocyte proliferation and hypertrophy ● Calcification of growth plate cartilage with subsequent vascular invasion of the growth plate and conversion to primary bone spongiosa Vascular invasion requires mineralization of the growth plate cartilage, which is delayed or prevented by deficiency of calcium or phosphorus [1-3]. In these circumstances, growth plate cartilage accumulates and the growth plate expands. In addition, the chondrocytes of the growth plate become disorganized, losing their columnar orientation [4-6] with characteristic expansion of the hypertrophic zone and impaired mineralization [7]. In the bone tissue below the growth plate (metaphysis), the mineralization defect leads to the accumulation of osteoid [8]. These abnormalities alter the overall geometry of the involved skeletal sites, leading to secondary increases in the diameters of the growth plate and metaphysis. These changes may be regarded as an attempt to compensate for decreased bone strength by increased bone diameter. Nonetheless, bone stability is compromised. If the underlying condition does not improve, a structural deformity, such as bowing, ensues. CLINICAL MANIFESTATIONS Calcipenic and phosphopenic rickets initially manifest at the distal forearm, knee, and costochondral junctions. These are the sites of rapid bone growth, where the demand for calcium and phosphorus accrual is greatest. Skeletal findings — The skeletal findings are similar for calcipenic and phosphopenic rickets. The typical findings of advanced rickets include [9]: ● Delayed closure of the fontanelles ● Parietal and frontal bossing ● Craniotabes (soft skull bones) ● Enlargement of the costochondral junction visible as beading along the anterolateral aspects of the chest (the "rachitic rosary") ( ● image 1) Formation of Harrison sulcus (or groove) at the lower margin of the thorax caused by the inward pull by diaphragmatic attachments of the softened lower ribs ● Widening of the wrist and bowing of the distal radius and ulna ● Progressive lateral bowing of the femur and tibia ( picture 1) The site and type of deformity of the extremities depend upon the age of the child and the weight-bearing patterns in the limbs. Thus, deformities of the forearms and posterior bowing of the distal tibia are more common in infants, whereas an exaggeration of the normal physiologic bowing of the legs (genu varum) is a characteristic finding in the toddler who has started to walk ( picture 1 and image 2). In the older child, valgus deformities of the legs ("knock-knees") or a windswept deformity (valgus deformity of one leg and varus deformity of the other) may be apparent. The type of deformity depends upon the biomechanical forces acting on the lower extremities at the time when the structural weakness develops. (See "Approach to the child with bow-legs", section on 'Rickets' and "Approach to the child with knockknees", section on 'Other causes'.) Radiographic findings — The changes of rickets are best visualized at the growth plates of rapidly growing bones, where mineral demand is greatest. Thus, in the upper limbs, the distal ulna is the site that best demonstrates the early signs of impaired mineralization ( image 3). In the lower extremities, the metaphyses above and below the knees are the most useful sites. Radiographic signs include: ● Epiphyseal/metaphyseal interface – Early signs of rickets are widening of the epiphyseal plate and loss of definition of the zone of provisional calcification at the epiphyseal/metaphyseal interface ( image 3). As the disease progresses, this region becomes more disorganized, with cupping, splaying, formation of cortical spurs, and stippling. The appearance of the epiphyseal bone centers may be delayed or they may be small, osteopenic, and ill defined [10]. ● Long bones – The shafts of the long bones are osteopenic, and the cortices may become thin. The trabecular pattern is reduced and becomes coarse. Deformities of the shafts of the long bones are often present. ● Looser zones and fractures – In severe rickets, pathologic fractures and Looser zones (also known as Milkman pseudofractures or insufficiency fractures) may be noted [11]. Looser zones represent partial-thickness cortical fractures and are radiographically apparent as narrow radiolucent lines 2 to 5 mm in width, often with sclerotic borders, usually perpendicular to the cortical margin. They are characteristic of severe osteomalacia ( image 4) and are often observed in the femur (at the femoral neck or under the lesser trochanter) or at pubic and ischial rami. The ulna, scapula, clavicle, rib, and metatarsal bones also may develop these lesions and show increased radionuclide uptake ("hot spots") on bone scans [12]. Extraskeletal findings — The extraskeletal manifestations of rickets vary depending upon the primary mineral deficiency. Hypoplasia of the dental enamel is a typical finding of calcipenic rickets, whereas dental abscesses occur more often in heritable forms of phosphopenic rickets. (See "Developmental defects of the teeth", section on 'Enamel defects'.) Calcipenic rickets can affect the musculoskeletal system with decreased muscle tone, leading to delayed achievement of motor milestones [13-15]. Presentation with hypocalcemic seizures occurs most frequently in the first year of life [14]. Transient cardiomyopathy may be evident [16,17]. Children with calcipenic rickets also are particularly prone to acquiring infectious diseases [18,19]. (See "Clinical manifestations of hypocalcemia".) Laboratory findings — Biochemical findings vary depending upon the type of rickets ( ● table 1) [20]: Calcium – The serum calcium concentration may be either decreased or normal in calcipenic rickets, depending on the stage of rickets; serum calcium usually is normal in phosphopenic rickets. ● Phosphorus – Serum phosphorus concentrations usually are low in both calcipenic and phosphopenic rickets. ● Parathyroid hormone (PTH) – The serum concentration of PTH typically is elevated in calcipenic rickets. In contrast, PTH concentrations are usually normal or only modestly elevated in phosphopenic rickets. If phosphorus deficiency is nutritional or not mediated by fibroblast growth factor 23 (FGF23), PTH levels may be in the low-normal range. ● Alkaline phosphatase – Serum alkaline phosphatase activity usually is increased markedly over the age-specific reference range in nutritional rickets (often up to 2000 international units/L), whereas the level is elevated to a lesser extent (400 to 800 international units/L) in the common form of heritable phosphopenic rickets (X-linked hypophosphatemia [XLH]). Alkaline phosphatase participates in the mineralization of bone and growth plate cartilage and is an excellent marker of disease activity [21]. ● Vitamin D – Serum concentrations of 25-hydroxyvitamin D (25OHD) reflect the amount of vitamin D stored in the body and, consequently, are low in vitamin D deficiency. (See 'Calcipenic rickets' below.) In calcipenic rickets, serum concentrations of 1,25-dihydroxyvitamin D (1,25[OH]2D) can be low, normal, or increased and thus are not the ideal primary laboratory indicators of the type of rickets present. However, in some forms of phosphopenic rickets (those mediated by excess FGF23, such as XLH and tumor-induced osteomalacia [TIO]), serum concentrations of 1,25(OH)2D may be low or inappropriately normal (in view of the ambient hypophosphatemia, which would normally increase production of 1,25(OH)2D). In other forms of phosphopenic rickets (those not mediated by excess FGF23, such as hereditary hypophosphatemic rickets with hypercalciuria [HHRH]), the serum concentration of 1,25(OH)2D may be elevated. (See "Hereditary hypophosphatemic rickets and tumor-induced osteomalacia".) EVALUATION The evaluation of a child with clinical signs of rickets should include a dietary history, with particular attention to calcium and vitamin D intake, along with a medication history and a history of sun exposure. Radiographic evaluation of a child with rickets should include, at a minimum, plain films of the wrist and hand or knees to evaluate the growth plates at rapidly growing sites. (See 'Radiographic findings' above.) Initial classification — Serum parathyroid hormone (PTH), alkaline phosphatase, inorganic phosphorus, and calcium concentrations are used to determine the initial classification of rickets ( algorithm 1). Rickets is an unlikely diagnosis if all of these values are normal. Serum creatinine and liver enzymes should be measured to screen for renal and liver disease, respectively. (See 'Rickets associated with chronic kidney disease' below and 'Disorders that mimic rickets' below.) ● Calcipenic rickets – If the serum PTH is considerably elevated and phosphorus concentration is normal or low, then a provisional diagnosis of calcipenic rickets can be made. Serum calcium may be normal in calcipenic rickets or may be low in advanced disease. The diagnosis is confirmed if appropriate healing is observed on a radiograph during the course of therapy. (See 'Calcipenic rickets' below.) ● Phosphopenic rickets – If the serum PTH is normal or only mildly elevated and the phosphorus concentration is low, then phosphopenic rickets should be suspected. Demonstration of renal phosphate wasting will identify most forms of phosphopenic rickets, but in cases of inadequate supply of dietary phosphorus (albeit an uncommon event), enhanced renal conservation of phosphate should be evident. (See 'Phosphopenic rickets' below.) Further evaluation — The causes of rickets include conditions that lead to hypocalcemia and/or hypophosphatemia as a result of decreased intake, malabsorption, and/or increased excretion of calcium, phosphate, or vitamin D( table 2). To determine the optimal treatment, the common nutritional causes of rickets must be distinguished from the forms caused by a gastrointestinal or renal disease or an inherited disorder. Calcipenic rickets — If the serum PTH is considerably elevated and phosphorus concentration is low, then a provisional diagnosis of calcipenic rickets can be made. Most cases of acquired rickets are calcipenic. Calcipenic rickets can be further divided into the following disorders, which can be distinguished by measuring serum levels of 25-hydroxyvitamin D (25OHD) and, in rare cases, 1,25-dihydroxyvitamin D (1,25[OH]2D) ( algorithm 2 and ● table 1): Low serum 25OHD • Nutritional rickets – Calcipenic rickets is usually caused by dietary deficiency of vitamin D. Occasionally, nutritional rickets is caused by deficiency of dietary calcium or a mixed deficiency of both vitamin D and calcium. 25OHD levels are typically low, but they may be normal if calcium deficiency is the primary nutritional deficiency. (See "Etiology and treatment of calcipenic rickets in children", section on 'Nutritional rickets'.) • Genetic disorders – 25-hydroxylase deficiency ( MIM #600081) is caused by variants in CYP2R1, the gene encoding the enzyme that converts vitamin D to the major circulating vitamin D metabolite, 25OHD, thus limiting the biosynthesis of 25OHD [22]. Activating variants in the enzyme that enhances clearance of 25OHD ( CYP3A4, MIM #619073) can also cause early-onset rickets [23]. These disorders are exceedingly rare and may be suspected when pharmacologic doses of vitamin D used in the treatment of nutritional rickets do not result in appropriate correction of the serum level of 25OHD. The differential diagnosis includes poor compliance with medication or fat malabsorption. (See "Etiology and treatment of calcipenic rickets in children", section on 'Genetic disorders'.) • Secondary defects in vitamin D metabolism or absorption of calcium or vitamin D – This can occur in extremely severe liver disease or in intestinal disorders such as celiac disease. The circulating 25OHD level may be low or normal, depending on whether the calcium malabsorption is mediated by vitamin D deficiency or another process. ● Normal serum 25OHD • 1-alpha-hydroxylase deficiency – 1-alpha-hydroxylase deficiency ( MIM #264700) is a rare disorder caused by variants in CYP27B1, which encodes the vitamin D 1-alpha-hydroxylase enzyme that converts 25OHD into the active metabolite 1,25(OH)2D. Serum levels of 25OHD are normal, and 1,25(OH)2D levels are low. This was previously known as vitamin D-dependent rickets type I or pseudovitamin D deficiency. • Hereditary resistance to vitamin D – Previously referred to as vitamin D-dependent rickets type II, hereditary resistance to vitamin D ( MIM #277440) is a rare form of calcipenic rickets usually caused by variants in the gene that encodes the vitamin D receptor ( VDR), leading to vitamin D resistance. 25OHD levels are normal, and 1,25(OH)2D levels are usually high or very high. The diagnosis and management of each of these disorders are discussed in a separate topic review. (See "Etiology and treatment of calcipenic rickets in children".) For children with a provisional diagnosis of calcipenic rickets who do not heal appropriately during the course of therapy, an alternate diagnosis should be considered. Phosphopenic rickets — Phosphopenic rickets is characterized by low serum phosphorus concentration; PTH concentrations are usually normal, although levels may be slightly elevated (and, rarely, even higher) at the time of presentation of X-linked hypophosphatemia (XLH) ( table 1). Phosphopenic rickets in children and adolescents is almost always caused by renal phosphate wasting, which may be isolated or part of a generalized renal tubular disorder. Occasionally, it is caused by nutritional phosphate deficiency. The causes are outlined below. The steps in the evaluation are: ● Tubular reabsorption of phosphorus (TRP) and TmP/GFR – Perform a fasting urine collection (usually for two hours) and obtain a blood sample during the course of the urine collection with measurement of phosphorus and creatinine concentrations in both the blood and the urine samples. These values are then used to calculate the TRP, expressed as a percentage of filtrate, and maximal renal tubular threshold for phosphate, expressed per glomerular filtration rate (TmP/GFR). The finding of very low TmP/GFR confirms renal phosphate wasting. In contrast, very high TRP and TmP/GFR indicate renal conservation of phosphate, implicating compromised dietary supply or intestinal absorption. ● Other urine studies – If renal phosphate wasting is present, perform a routine urinalysis to determine pH and glucose, and an assessment of urinary calcium excretion. For screening purposes, we usually obtain a random spot urine specimen for calcium and creatinine and determine the ratio. It should be kept in mind that normative values differ when using SI units as compared with conventional (mass) units, even though a ratio is employed. A more precise evaluation in the older child can be performed by obtaining these measurements in a 24-hour urine collection. If renal loss of multiple solutes is suspected, obtain urinary amino acids to assess for renal Fanconi syndrome. ● Serum 1,25(OH)2D – If renal phosphate wasting is present, measurement of serum 1,25(OH)2D may help to distinguish the causes that are mediated by fibroblast growth factor 23 (FGF23) from those that are not. This evaluation will help to distinguish among the causes of phosphopenic rickets, as outlined below ( ● algorithm 3): Renal phosphate wasting (low TRP and TmP/GFR) • Renal tubular disorders – Renal tubular disorders such as Fanconi syndrome can cause rickets due to renal loss of phosphate. Fanconi syndrome is characterized by hypophosphatemia due to phosphaturia, variably accompanied by renal glucosuria (glucosuria with a normal plasma glucose concentration), aminoaciduria, tubular proteinuria, and/or proximal renal tubular acidosis. (See "Etiology and clinical manifestations of renal tubular acidosis in infants and children", section on 'Fanconi syndrome'.) • FGF23-mediated disorders (normal or low serum 1,25[OH]2D and urinary calcium excretion) – Many forms of renal phosphate wasting are mediated by an excess of FGF23, which acts on the kidney to induce renal phosphate wasting: - XLH – XLH ( MIM #307800) is the most common cause of isolated renal phosphate loss, caused by variants in the PHEX gene. Renal phosphate wasting is apparent beginning shortly after birth, but the disorder is generally recognized clinically when the child begins to walk, causing bowing of the legs. (See "Hereditary hypophosphatemic rickets and tumor-induced osteomalacia", section on 'X-linked hypophosphatemia'.) Less common autosomal dominant and autosomal recessive forms of hypophosphatemic rickets also exist. (See "Hereditary hypophosphatemic rickets and tumor-induced osteomalacia", section on 'Autosomal dominant hypophosphatemia' and "Hereditary hypophosphatemic rickets and tumor-induced osteomalacia", section on 'Autosomal recessive hypophosphatemic rickets'.) - Tumor-induced osteomalacia (TIO) – TIO also causes isolated phosphate loss. It is an acquired disorder caused by a tumor, which usually, but not always, is benign. These tumors express FGF23 and, in some cases, other phosphaturic factors. The treatment of choice is complete removal of the tumor, which will remove the source of FGF23, thereby curing the disorder. However, other measures may be required if the tumor is not localized or is unable to be resected completely. TIO may present in late childhood and adolescence but is more commonly seen in adults. (See "Hereditary hypophosphatemic rickets and tumor-induced osteomalacia", section on 'Tumor-induced osteomalacia'.) - Other causes of excess FGF23 production – Phenotypes of FGF23mediated renal phosphate loss and rachitic bone disease may be observed in other conditions, which generally occur in sporadic fashion. These disorders include cutaneous skeletal hypophosphatemia syndrome, also known as epidermal nevus syndrome [24], and fibrous dysplasia of bone, as occurs in McCuneAlbright syndrome [25]. • Not FGF23-mediated (increased serum 1,25[OH]2D and urinary calcium excretion): - Hereditary hypophosphatemic rickets with hypercalciuria (HHRH) – HHRH ( MIM #241530) is an autosomal recessive disease and is another rare cause of phosphopenic rickets. This disorder is distinguished from the FGF23-mediated forms of hypophosphatemic rickets by an elevated serum 1,25(OH)2D concentration and increased urinary calcium excretion. Because the treatment for this disorder is distinct, it is important to evaluate for HHRH in every patient with phosphopenic rickets before initiating therapy by measuring serum 1,25(OH)2D and urinary calcium excretion. The disorder is due to loss of function variants in NPT2C (encoded by SLC34A3), a sodium-phosphate transporter expressed in renal tubules. Variable renal phenotypes can be observed in heterozygotes. (See "Hereditary hypophosphatemic rickets and tumor-induced osteomalacia", section on 'Hypophosphatemic rickets with hypercalciuria'.) ● No renal phosphate wasting (high TRP and TmP/GFR) • Nutritional phosphate deficiency – Occasionally, hypophosphatemic rickets is caused by nutritional phosphate deficiency, which is characterized by very high TRP and TmP/GFR, indicating renal conservation of phosphate. This may occur in premature infants who receive breast milk as their sole source of nutrition and reflects the relatively low phosphate content of breast milk. It was also reported in several case series of young children with complex disease who were fed Neocate brand formula (an elemental formula designed for children with multiple food allergies), suggesting a problem with phosphate bioavailability compared with standard formulas [26-28]. Reformulated products designed to avoid this complication were subsequently introduced to alleviate this problem. H2-receptor blocking agents have also been associated with a similar problem. Rickets associated with chronic kidney disease — Renal dysfunction is an important cause of bone disease (renal osteodystrophy), which can include rickets. In children with suspected rickets, renal function should be evaluated by measuring serum creatinine. Bone disease occurs in children with renal insufficiency for many reasons, including reduced formation of 1,25(OH)2D, metabolic acidosis, administration of aluminum, and secondary hyperparathyroidism. (See "Pediatric chronic kidney disease-mineral and bone disorder (CKD-MBD)".) DISORDERS THAT MIMIC RICKETS A variety of conditions cause signs or symptoms that resemble rickets: Skeletal abnormalities or bowing ● Skeletal dysplasias – Skeletal dysplasia (eg, achondroplasia, pseudoachondroplasia, metaphyseal chondrodysplasia) is another cause of bilateral, symmetric bowed legs. The radiographic features can be similar to those of rickets. However, serum inorganic phosphorus and parathyroid hormone (PTH) concentrations usually are normal in children with skeletal dysplasia. (See "Approach to the child with bow-legs", section on 'Skeletal dysplasia' and "Skeletal dysplasias: Approach to evaluation".) ● Blount disease – Blount disease is a pathologic varus deformity of the knee that results from disruption of normal cartilage growth at the medial aspect of the proximal tibial physis. It can be distinguished from rickets by distinct radiographic findings and normal serum biochemistry values. (See "Approach to the child with bow-legs", section on 'Blount disease'.) Laboratory abnormalities ● Liver disease – Elevations of serum alkaline phosphatase activity is seen in rickets but also can be caused by liver disease. The possibility of liver disease can be further evaluated by measuring liver enzymes (serum alanine aminotransferase [ALT], aspartate aminotransferase [AST], and gamma-glutamyl transpeptidase [GGT]). (See "Approach to the patient with abnormal liver biochemical and function tests", section on 'Elevated alkaline phosphatase'.) ● Transient hyperphosphatasemia – Children with isolated elevations of serum alkaline phosphatase but normal liver enzymes and no radiographic evidence of rickets may have transient hyperphosphatasemia of infancy and early childhood. This is usually a benign condition that arises after a minor infectious illness and spontaneously remits over a several-month period. (See "Transient hyperphosphatasemia of infancy and early childhood".) ● Primary hypoparathyroidism – Primary hypoparathyroidism causes marked hypocalcemia but is usually not associated with rickets. This observation suggests that low serum phosphorus and/or PTH itself may play roles in mediating the growth plate lesion. (See "Etiology of hypocalcemia in infants and children", section on 'Hypocalcemia with low PTH (hypoparathyroidism)'.) ● Hypophosphatasia – Hypophosphatasia is a rare genetic disorder of alkaline phosphatase activity [29]. Like rickets, it is characterized by bone demineralization. In contrast to rickets, serum alkaline phosphatase activity is very low. Childhood forms are characterized by premature loss of primary teeth. (See "Epidemiology and etiology of osteomalacia", section on 'Hypophosphatasia' and "Periodontal disease in children: Associated systemic conditions", section on 'Hypophosphatasia'.) ● Other – Occasionally, patients, usually infants, may present with hypocalcemia, elevated phosphorus and PTH levels, and normal 25hydroxyvitamin D (25OHD) concentrations. This combination of findings is consistent with: • Pseudohypoparathyroidism. (See "Etiology of hypocalcemia in infants and children", section on 'End-organ resistance to PTH (pseudohypoparathyroidism)'.) • Dietary calcium deficiency (severe). (See "Etiology and treatment of calcipenic rickets in children", section on 'Calcium deficiency'.) • Longstanding vitamin D deficiency with a recent dosing of vitamin D. In this case, the hyperphosphatemia has been attributed to transient resistance to PTH. (See "Etiology and treatment of calcipenic rickets in children", section on 'Vitamin D deficiency'.) SOCIETY GUIDELINE LINKS Links to society and government-sponsored guidelines from selected countries and regions around the world are provided separately. (See "Society guideline links: Vitamin D deficiency" and "Society guideline links: Pediatric bone health".) SUMMARY AND RECOMMENDATIONS ● Definition – Rickets refers to the disorganized expansion and deficient mineralization of growth plate cartilage. Osteomalacia refers to impaired mineralization of bone and, in children, typically accompanies rickets. (See 'Introduction' above.) ● Classification – Rickets is classified according to the predominant mineral deficiency. Phosphopenic rickets usually is caused by renal phosphate wasting. Serum calcium levels are often, but not always, decreased in calcipenic rickets. (See 'Types of rickets' above.) • Calcipenic rickets usually is caused by dietary deficiency of vitamin D and/or calcium; this is the most common cause of rickets worldwide. Rarely, it is caused by genetic defects in vitamin D metabolism or action leading to vitamin D resistance. (See 'Calcipenic rickets' above.) • Phosphopenic rickets in children and adolescents is almost always caused by renal phosphate wasting, which is usually an isolated phenomenon but may be part of a generalized tubular disorder such as Fanconi syndrome. Rarely, it may result from inadequate dietary phosphorus or intestinal malabsorption. Renal phosphate wasting syndromes can be fibroblast growth factor 23 (FGF23)-mediated or occur independent of FGF23 excess. (See 'Phosphopenic rickets' above.) ● Skeletal findings – The skeletal findings are similar for calcipenic and phosphopenic rickets and may include delayed closure of the fontanelles, parietal and frontal bossing, enlargement of the costochondral junction ("rachitic rosary"), widening of the wrist, and lateral bowing of the femur and tibia (bow legs) ( picture 1). (See 'Skeletal findings' above.) ● Radiographic findings – Radiographic findings of rickets include expansion of the growth plate and loss of definition of the zone of provisional calcification at the epiphyseal/metaphyseal interface, progressing to disorganization of the growth plate with cupping, splaying, and formation of cortical spurs ( image 3). The changes are best seen in the distal ulna and the metaphyses above and below the knee. (See 'Radiographic findings' above.) ● Laboratory findings – Serum alkaline phosphatase activity is elevated in both types of rickets and is a good marker of disease severity in children. Other biochemical findings may include hypocalcemia and hypophosphatemia, but the pattern varies depending on the type and severity of the rickets ( table 1). Serum concentration of parathyroid hormone (PTH) typically is quite elevated in calcipenic rickets but not in phosphopenic rickets. (See 'Laboratory findings' above.) ● Identifying the cause – Measurements of serum PTH and inorganic phosphorus serve to distinguish calcipenic from phosphopenic rickets ( algorithm 1). (See 'Initial classification' above.) • Calcipenic rickets – For children with calcipenic rickets, measurements of serum 25-hydroxyvitamin D (25OHD) help to distinguish rickets caused by vitamin D deficiency (the most common form) from other causes of calcipenic rickets ( algorithm 2). (See 'Calcipenic rickets' above and "Etiology and treatment of calcipenic rickets in children".) • Phosphopenic rickets – For children with phosphopenic rickets, an assessment of renal excretion of phosphate should be performed (as tubular reabsorption of phosphorus [TRP] or maximal renal tubular threshold for phosphate, expressed per glomerular filtration rate [TmP/GFR]) ( algorithm 3). - Low TRP or TmP/GFR suggests renal phosphate wasting. Causes of renal phosphate wasting should be investigated with assessment of serum 1,25-dihydroxyvitamin D (1,25[OH]2D), a routine urinalysis to determine pH and glucose, and an assessment of urinary calcium excretion. - High TRP or TmP/GFR indicates renal conservation of phosphate and is consistent with nutritional phosphate deprivation. This may be due to insufficient phosphate content or decreased bioavailability in formula products and other nutritional supplements. (See 'Phosphopenic rickets' above and "Hereditary hypophosphatemic rickets and tumor-induced osteomalacia".) REFERENCES 1. Pitt MJ. Rickets and osteomalacia are still around. Radiol Clin North Am 1991; 29:97. 2. Shapiro IM, Boyde A. Mineralization of normal and rachitic chick growth cartilage: vascular canals, cartilage calcification and osteogenesis. Scanning Microsc 1987; 1:599. 3. Hunter WL, Arsenault AL, Hodsman AB. Rearrangement of the metaphyseal vasculature of the rat growth plate in rickets and rachitic reversal: a model of vascular arrest and angiogenesis renewed. Anat Rec 1991; 229:453. 4. Lacey DL, Huffer WE. Studies on the pathogenesis of avian rickets. I. Changes in epiphyseal and metaphyseal vessels in hypocalcemic and hypophosphatemic rickets. Am J Pathol 1982; 109:288. 5. Huffer WE, Lacey DL. Studies on the pathogenesis of avian rickets II. Necrosis of perforating epiphyseal vessels during recovery from rickets in chicks caused by vitamin D3 deficiency. Am J Pathol 1982; 109:302. 6. Takechi M, Itakura C. Ultrastructural studies of the epiphyseal plate of chicks fed a vitamin D-deficient and low-calcium diet. J Comp Pathol 1995; 113:101. 7. Sabbagh Y, Carpenter TO, Demay MB. Hypophosphatemia leads to rickets by impairing caspase-mediated apoptosis of hypertrophic chondrocytes. Proc Natl Acad Sci U S A 2005; 102:9637. 8. Rauch F. The rachitic bone. Endocr Dev 2003; 6:69. 9. Misra M, Pacaud D, Petryk A, et al. Vitamin D deficiency in children and its management: review of current knowledge and recommendations. Pediatrics 2008; 122:398. 10. Oestreich AE. The acrophysis: a unifying concept for understanding enchondral bone growth and its disorders. II. Abnormal growth. Skeletal Radiol 2004; 33:119. 11. Chapman T, Sugar N, Done S, et al. Fractures in infants and toddlers with rickets. Pediatr Radiol 2010; 40:1184. 12. Kim S, Park CH, Chung YS. Hypophosphatemic osteomalacia demonstrated by Tc-99m MDP bone scan: a case report. Clin Nucl Med 2000; 25:337. 13. Carvalho NF, Kenney RD, Carrington PH, Hall DE. Severe nutritional deficiencies in toddlers resulting from health food milk alternatives. Pediatrics 2001; 107:E46. 14. Robinson PD, Högler W, Craig ME, et al. The re-emerging burden of rickets: a decade of experience from Sydney. Arch Dis Child 2006; 91:564. 15. Prasad C, Cummings E. Rickets presenting as gross motor delay in twin girls. CMAJ 2018; 190:E565. 16. Yilmaz O, Olgun H, Ciftel M, et al. Dilated cardiomyopathy secondary to rickets-related hypocalcaemia: eight case reports and a review of the literature. Cardiol Young 2015; 25:261. 17. Yazici MU, Kesici S, Demirbilek H, et al. Reversible Dilated Cardiomyopathy Due to Combination of Vitamin D-Deficient Rickets and Primary Hypomagnesemia in an 11-Month-Old Infant. J Pediatr Intensive Care 2018; 7:46. 18. Muhe L, Lulseged S, Mason KE, Simoes EA. Case-control study of the role of nutritional rickets in the risk of developing pneumonia in Ethiopian children. Lancet 1997; 349:1801. 19. Najada AS, Habashneh MS, Khader M. The frequency of nutritional rickets among hospitalized infants and its relation to respiratory diseases. J Trop Pediatr 2004; 50:364. 20. Baroncelli GI, Bertelloni S, Ceccarelli C, et al. Bone turnover in children with vitamin D deficiency rickets before and during treatment. Acta Paediatr 2000; 89:513. 21. Whyte MP. Physiological role of alkaline phosphatase explored in hypophosphatasia. Ann N Y Acad Sci 2010; 1192:190. 22. Thacher TD, Fischer PR, Singh RJ, et al. CYP2R1 Mutations Impair Generation of 25-hydroxyvitamin D and Cause an Atypical Form of Vitamin D Deficiency. J Clin Endocrinol Metab 2015; 100:E1005. 23. Roizen JD, Li D, O'Lear L, et al. CYP3A4 mutation causes vitamin Ddependent rickets type 3. J Clin Invest 2018; 128:1913. 24. Lim YH, Ovejero D, Derrick KM, et al. Cutaneous skeletal hypophosphatemia syndrome (CSHS) is a multilineage somatic mosaic RASopathy. J Am Acad Dermatol 2016; 75:420. 25. Riminucci M, Collins MT, Fedarko NS, et al. FGF-23 in fibrous dysplasia of bone and its relationship to renal phosphate wasting. J Clin Invest 2003; 112:683. 26. Gonzalez Ballesteros LF, Ma NS, Gordon RJ, et al. Unexpected widespread hypophosphatemia and bone disease associated with elemental formula use in infants and children. Bone 2017; 97:287. 27. Uday S, Sakka S, Davies JH, et al. Elemental formula associated hypophosphataemic rickets. Clin Nutr 2019; 38:2246. 28. Creo AL, Epp LM, Buchholtz JA, Tebben PJ. Prevalence of Metabolic Bone Disease in Tube-Fed Children Receiving Elemental Formula. Horm Res Paediatr 2018; 90:291. 29. Mohn A, De Leonibus C, de Giorgis T, et al. Hypophosphatasia in a child with widened anterior fontanelle: lessons learned from late diagnosis and incorrect treatment. Acta Paediatr 2011; 100:e43. Topic 5856 Version 30.0 © 2023 UpToDate, Inc. All rights reserved.