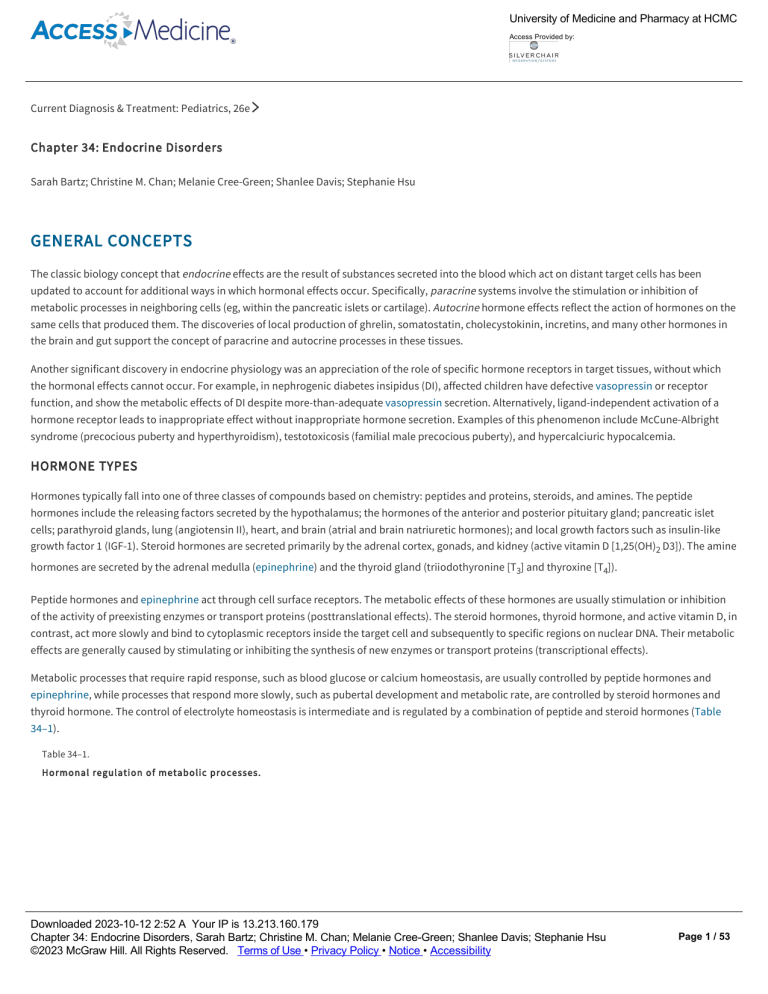
University of Medicine and Pharmacy at HCMC Access Provided by: Current Diagnosis & Treatment: Pediatrics, 26e Chapter 34: Endocrine Disorders Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu GENERAL CONCEPTS The classic biology concept that endocrine effects are the result of substances secreted into the blood which act on distant target cells has been updated to account for additional ways in which hormonal effects occur. Specifically, paracrine systems involve the stimulation or inhibition of metabolic processes in neighboring cells (eg, within the pancreatic islets or cartilage). Autocrine hormone effects reflect the action of hormones on the same cells that produced them. The discoveries of local production of ghrelin, somatostatin, cholecystokinin, incretins, and many other hormones in the brain and gut support the concept of paracrine and autocrine processes in these tissues. Another significant discovery in endocrine physiology was an appreciation of the role of specific hormone receptors in target tissues, without which the hormonal effects cannot occur. For example, in nephrogenic diabetes insipidus (DI), affected children have defective vasopressin or receptor function, and show the metabolic effects of DI despite more­than­adequate vasopressin secretion. Alternatively, ligand­independent activation of a hormone receptor leads to inappropriate effect without inappropriate hormone secretion. Examples of this phenomenon include McCune­Albright syndrome (precocious puberty and hyperthyroidism), testotoxicosis (familial male precocious puberty), and hypercalciuric hypocalcemia. HORMONE TYPES Hormones typically fall into one of three classes of compounds based on chemistry: peptides and proteins, steroids, and amines. The peptide hormones include the releasing factors secreted by the hypothalamus; the hormones of the anterior and posterior pituitary gland; pancreatic islet cells; parathyroid glands, lung (angiotensin II), heart, and brain (atrial and brain natriuretic hormones); and local growth factors such as insulin­like growth factor 1 (IGF­1). Steroid hormones are secreted primarily by the adrenal cortex, gonads, and kidney (active vitamin D [1,25(OH)2 D3]). The amine hormones are secreted by the adrenal medulla (epinephrine) and the thyroid gland (triiodothyronine [T3] and thyroxine [T4]). Peptide hormones and epinephrine act through cell surface receptors. The metabolic effects of these hormones are usually stimulation or inhibition of the activity of preexisting enzymes or transport proteins (posttranslational effects). The steroid hormones, thyroid hormone, and active vitamin D, in contrast, act more slowly and bind to cytoplasmic receptors inside the target cell and subsequently to specific regions on nuclear DNA. Their metabolic effects are generally caused by stimulating or inhibiting the synthesis of new enzymes or transport proteins (transcriptional effects). Metabolic processes that require rapid response, such as blood glucose or calcium homeostasis, are usually controlled by peptide hormones and epinephrine, while processes that respond more slowly, such as pubertal development and metabolic rate, are controlled by steroid hormones and thyroid hormone. The control of electrolyte homeostasis is intermediate and is regulated by a combination of peptide and steroid hormones (Table 34–1). Table 34–1. Hormonal regulation of metabolic processes. Rapid Response, Most Direct Metabolite or Other Parameter Glucose Stimulus Endocrine Gland Hormone Hyperglycemia Pancreatic beta cell Insulin Downloaded IP is 13.213.160.179 Glucose 2023­10­12 2:52 A Your Hypoglycemia Pancreatic alpha cell Glucagon Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility Glucose Hypoglycemia Adrenal medulla Epinephrine Page 1 / 53 thyroid hormone. The control of electrolyte homeostasis is intermediate and is regulated by a combination of peptide and steroid hormones (Table University of Medicine and Pharmacy at HCMC 34–1). Access Provided by: Table 34–1. Hormonal regulation of metabolic processes. Rapid Response, Most Direct Metabolite or Other Stimulus Endocrine Gland Hormone Glucose Hyperglycemia Pancreatic beta cell Insulin Glucose Hypoglycemia Pancreatic alpha cell Glucagon Glucose Hypoglycemia Adrenal medulla Epinephrine Calcium Hypercalcemia Thyroid C cell Calcitonin Calcium Hypocalcemia Parathyroid PTH Sodium/plasma osmolality Hypernatremia/hyperosmolality Hypothalamus with posterior pituitary gland as ADH Parameter reservoir Plasma volume Hypervolemia Heart ANH Abnormality Endocrine Gland Hormone Hyponatremia Kidney Renin (an enzyme) Hyperkalemia Liver and others Angiotensin I Hypovolemia Lung Angiotensin II Adrenal cortex Aldosterone Endocrine Target Tissue Endocrine Gland Intermediate Response, Multiple Intermediaries Metabolite or Other Parameter Sodium/potassium Slow Response, Longer Acting Processes Hypothalamic­Releasing Trophic Hormone (Pituitary Hormone Gland) CRH ACTH Adrenal cortex Cortisol GHRH GH Liver and other tissues IGF­1 GnRH LH Testis Testosterone GnRH FSH/LH Ovary Estradiol/progesterone TRH TSH Thyroid gland T 4 and T3 Hormone ACTH, adrenocorticotropic hormone; ADH, antidiuretic hormone; ANH, atrial natriuretic hormone; CRH, corticotropin­releasing hormone; FSH, follicle­stimulating hormone; GH, growth hormone; GHRH, growth hormone releasing hormone; GnRH, gonadotropin­releasing hormone; IGF­1, insulin­like growth factor 1; LH, luteinizing hormone; PTH, parathyroid hormone; T3, triiodothyronine; T4, thyroxine; TRH, thyrotropin­releasing hormone; TSH, thyroid­stimulating hormone. Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 Page 2 / 53 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility FEEDBACK CONTROL OF HORMONE SECRETION TRH TSH Thyroid gland T 4 and T3 University of Medicine and Pharmacy at HCMC Access Provided by: ACTH, adrenocorticotropic hormone; ADH, antidiuretic hormone; ANH, atrial natriuretic hormone; CRH, corticotropin­releasing hormone; FSH, follicle­stimulating hormone; GH, growth hormone; GHRH, growth hormone releasing hormone; GnRH, gonadotropin­releasing hormone; IGF­1, insulin­like growth factor 1; LH, luteinizing hormone; PTH, parathyroid hormone; T3, triiodothyronine; T4, thyroxine; TRH, thyrotropin­releasing hormone; TSH, thyroid­stimulating hormone. FEEDBACK CONTROL OF HORMONE SECRETION Hormone secretion is regulated by feedback in response to changes in the internal environment. When the metabolic imbalance is corrected, stimulation of the hormone secretion ceases and may even be inhibited. Overcorrection of the imbalance stimulates secretion of counterbalancing hormone or hormones so that homeostasis is maintained within relatively narrow limits. Hypothalamic­pituitary control of hormonal secretion is regulated by feedback. End­organ failure (endocrine gland insufficiency) leads to decreased circulating concentrations of endocrine gland hormones and increased secretion of the respective hypothalamic releasing hormones and pituitary hormones (see Table 34–1; Figure 34–1). If restoration of normal circulating concentration of hormones occurs, feedback inhibition at the pituitary and hypothalamus results in cessation of the previously stimulated secretion of hypothalamic and pituitary hormones and restoration of their circulating concentrations to normal. Figure 34–1. General scheme of the hypothalamus­pituitary­endocrine gland axis. Releasing hormones synthesized in the hypothalamus are secreted into the hypophyseal portal circulation. Trophic hormones are secreted by the pituitary gland in response, and they in turn act on specific endocrine glands to stimulate the secretion of their respective hormones. The endocrine gland hormones exert their respective effects on various target tissues (end organs) and exert a negative feedback (feedback inhibition) on their own secretion by acting at the level of the pituitary and hypothalamus. This system is characteristic of those hormones listed in Table 34–1 (third level). Similarly, if there is autonomous endocrine gland hyperfunction (eg, McCune­Albright syndrome, Graves disease, or adrenal tumor), the specific hypothalamic releasing and pituitary hormones are suppressed (see Figure 34–1). Bethin K, Fuqua JS: General concepts and physiology. In: Kappy MS, Allen DB, Geffner ME (eds): Pediatric Practice­Endocrinology . McGraw Hill; 2010:1–22. Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu DISTURBANCES OF Reserved. GROWTH ©2023 McGraw Hill. All Rights Terms of Use • Privacy Policy • Notice • Accessibility Page 3 / 53 Disturbances of growth and development are the most common problems evaluated by a pediatric endocrinologist. While most cases represent hypothalamic releasing and pituitary hormones are suppressed (see Figure 34–1). University of Medicine and Pharmacy at HCMC Access Provided by: Bethin K, Fuqua JS: General concepts and physiology. In: Kappy MS, Allen DB, Geffner ME (eds): Pediatric Practice­Endocrinology . McGraw Hill; 2010:1–22. DISTURBANCES OF GROWTH Disturbances of growth and development are the most common problems evaluated by a pediatric endocrinologist. While most cases represent normal developmental variants, it is critical to identify abnormal growth patterns. Deviations from the norm can be the first or only manifestation of an endocrine disorder. In evaluation of growth, height velocity is the most critical parameter. Height percentiles represent comparisons to a population and assume typical growth velocity. Therefore, a persistent increase or decrease in height percentiles between age 2 years and the onset of puberty indicates abnormal growth and always warrants evaluation. Similarly, substantial deviations from target (midparental) height may indicate underlying endocrine or skeletal disorders. It is more difficult to distinguish normal from abnormal growth in the first 2 years of life, as infants may have catch­up or catch­down growth during this period. In addition, growth variations during the late childhood and early adolescent years require careful consideration due to the variable timing of the onset of puberty. Appropriate standards must be used to evaluate growth. The National Center for Health Statistics provides standard cross­sectional growth charts for North American children (see Chapter 9) and the World Health Organization (WHO) growth charts use an ethnically more diverse sample. Normal growth standards may vary with country of origin. Growth charts are available for some ethnic groups in North America and for some syndromes with specific growth disturbance such as Turner or Down syndromes. Current treatment practices for patients with Turner and Down syndrome (including the use of growth hormone in Turner syndrome) can cause children to grow differently than reflected in their specific growth charts. TARGET HEIGHT & SKELETAL MATURATION A child’s height potential is determined largely by genetic factors. The target height of a child is calculated from the mean parental height plus 6.5 cm for boys or minus 6.5 cm for girls. This calculation helps identify a child’s genetic growth potential. Most children achieve an adult height within 10 cm of the target height. Another parameter that determines growth potential is skeletal maturation or bone age. Beyond the neonatal period, bone age is evaluated by comparing a radiograph of the child’s left hand and wrist with the standards of Greulich and Pyle. Delayed or advanced bone age is not diagnostic of any specific disease, but the extent of skeletal maturation allows determination of remaining growth potential as a percentage of total height and is used in the predication of adult height. However, it is important to remember that the bone age is a snapshot of a point in time, and bone age delay or advancement can change over time. For example, children with a previously delayed bone age may develop a bone age closer to their chronological age as they approach puberty. SHORT STATURE It is important to distinguish normal variants of growth (familial short stature and constitutional growth delay) from pathologic conditions (Table 34– 2). Pathologic short stature is more likely in children who have a low growth velocity (crossing major height percentiles on the growth curve, < 4 cm/y) or who are significantly short for their family. Children with chronic illness or nutritional deficiencies may have poor linear growth, and this can be associated with inadequate weight gain and low body mass index (BMI). In contrast, endocrine causes of short stature are usually associated with maintenance or increase in BMI percentiles. Subtypes of short stature are discussed next. Table 34–2. Causes of short stature. NORMAL A. Genetic­familial short stature B. Constitutional growth delay PATHOLOGICAL C. Endocrine disturbances 1. Growth hormone (GH) deficiency a. Hereditary b. Idiopathic—with and without associated abnormalities of midline structures of the central nervous system c. Acquired d. Transient (eg, psychosocial short stature) Downloaded 2023­10­12 2:52 Airradiation Your IPofisthe 13.213.160.179 e. Organic—tumor, central nervous system, infection, or trauma Chapter 34:2. Endocrine Disorders, Sarah Bartz; M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu GH resistance/insulin­like growth factor Christine 1 (IGF­1) deficiency ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility 3. Hypothyroidism 4. Excess cortisol—Cushing disease and Cushing syndrome Page 4 / 53 2). Pathologic short stature is more likely in children who have a low growth velocity (crossing major height percentiles on the growth curve, < 4 cm/y) University of Medicine and Pharmacy at HCMC or who are significantly short for their family. Children with chronic illness or nutritional deficiencies may have poor linear growth, and this can be Access Provided by: associated with inadequate weight gain and low body mass index (BMI). In contrast, endocrine causes of short stature are usually associated with maintenance or increase in BMI percentiles. Subtypes of short stature are discussed next. Table 34–2. Causes of short stature. NORMAL A. Genetic­familial short stature B. Constitutional growth delay PATHOLOGICAL C. Endocrine disturbances 1. Growth hormone (GH) deficiency a. Hereditary b. Idiopathic—with and without associated abnormalities of midline structures of the central nervous system c. Acquired d. Transient (eg, psychosocial short stature) e. Organic—tumor, irradiation of the central nervous system, infection, or trauma 2. GH resistance/insulin­like growth factor 1 (IGF­1) deficiency 3. Hypothyroidism 4. Excess cortisol—Cushing disease and Cushing syndrome 5. Diabetes mellitus (poorly controlled) 6. Pseudohypoparathyroidism 7. Rickets D. Intrauterine growth restriction 1. Intrinsic fetal abnormalities—chromosomal disorders 2. Syndromes (eg, Russell­Silver, Noonan, Bloom, de Lange, Cockayne) 3. Congenital infections 4. Placental abnormalities 5. Maternal abnormalities during pregnancy E. Inborn errors of metabolism F. Intrinsic diseases of bone 1. Defects of growth of tubular bones or spine (skeletal dysplasias) 2. Disorganized development of cartilage and fibrous components of the skeleton G. Short stature associated with chromosomal defects 1. Autosomal (eg, Down syndrome, Prader­Willi syndrome) 2. Sex chromosomal (eg, Turner syndrome–XO) H. Chronic systemic diseases, congenital defects, and cancers I. Psychosocial short stature (deprivation dwarfism) 1. Familial Short Stature & Constitutional Growth Delay Children with familial short stature typically have normal birth weight and length. In the first 2 years of life, their linear growth velocity decelerates until they near their genetically determined percentile. Once the target percentile is reached, the child resumes normal linear growth parallel to the growth curve, usually between 2 and 3 years of age. Skeletal maturation and timing of puberty are consistent with chronologic age. The child grows along his/her own growth percentile and the final height is short but appropriate for the family (Figure 34–2). Figure 34–2. Typical pattern of growth in a child with familial short stature. After attaining an appropriate percentile during the first 2 years of life, the child will have normal linear growth parallel to the growth curve. Skeletal maturation and the timing of puberty are consistent with chronologic age. The height percentile the2023­10­12 child has been following and final height is short but appropriate for the family. Downloaded 2:52 A YourisIPmaintained, is 13.213.160.179 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility Page 5 / 53 Figure 34–2. University of Medicine and Pharmacy at HCMC Access Provided by: Typical pattern of growth in a child with familial short stature. After attaining an appropriate percentile during the first 2 years of life, the child will have normal linear growth parallel to the growth curve. Skeletal maturation and the timing of puberty are consistent with chronologic age. The height percentile the child has been following is maintained, and final height is short but appropriate for the family. Children with constitutional growth delay (CGD), sometimes called “late bloomers,” have a growth pattern similar to those with familial short stature with a decline in linear growth velocity between ages 2 and 3 years and then maintenance of a normal growth velocity prior to puberty. The difference is that children with CGD follow a growth percentile that is below what is expected based on parental heights, have a delay in skeletal maturation compared to chronologic age, and exhibit a delay in the onset of puberty. The late puberty often manifests as exaggerated short stature during the typical time of puberty. In these children, growth continues beyond the time the average child stops growing, and final height is appropriate for target height (Figure 34–3). Figure 34–3. Typical pattern of growth in a child with constitutional growth delay. Growth slows during the first 2 years of life, similarly to children with familial short stature. Subsequently the child will have normal linear growth parallel to the growth curve. However, skeletal maturation and the onset of puberty are delayed. Growth continues beyond the time the average child has stopped growing, and final height is appropriate for target height. Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility Page 6 / 53 Figure 34–3. University of Medicine and Pharmacy at HCMC Typical pattern of growth in a child with constitutional growth delay. Growth slows during the first 2 years of life, similarly to children with familial short Access Provided by: stature. Subsequently the child will have normal linear growth parallel to the growth curve. However, skeletal maturation and the onset of puberty are delayed. Growth continues beyond the time the average child has stopped growing, and final height is appropriate for target height. 2. Growth Hormone Deficiency Human growth hormone (GH) is produced by the anterior pituitary gland. Secretion is stimulated by growth hormone­releasing hormone (GHRH) and inhibited by somatostatin. GH is secreted in a pulsatile pattern, and has direct growth­promoting and metabolic effects (Figure 34–4). GH also promotes growth indirectly by stimulating production of insulin­like growth factors, primarily IGF­1. Figure 34–4. The GHRH/GH/IGF­1 system. The effects of growth hormone (GH) on growth are partly due to its direct anabolic effects in the muscle, liver, and bone. In addition, GH stimulates many tissues to produce insulin­like growth factor 1 (IGF­1) locally, which stimulates the growth of the tissue itself (paracrine effect of IGF­1). The action of GH on the liver results in the secretion of IGF­1 (circulating IGF­1), which stimulates growth in other tissues (endocrine effect of IGF­1). The action of growth hormone on the liver also enhances the secretion of IGF­binding protein 3 (IGFBP­3) and acid­labile subunit (ALS), which form a high­molecular­weight complex with IGF­1. The function of this complex is to transport IGF­1 to its target tissues, but the complex also serves as a reservoir and possible inhibitor of IGF­1 action. In various chronic illnesses, the direct metabolic effects of GH are inhibited; the secretion of IGF­1 in response to GH is blunted, and in some cases IGFBP­3 synthesis is enhanced, resulting in marked inhibition in the growth of the child. GHRH, growth hormone­releasing hormone. Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility Page 7 / 53 which form a high­molecular­weight complex with IGF­1. The function of this complex is to transport IGF­1 to its target tissues, but the complex also University of Medicine and Pharmacy at HCMC serves as a reservoir and possible inhibitor of IGF­1 action. In various chronic illnesses, the direct metabolic effects of GH are inhibited; the secretion of Access Provided by: IGF­1 in response to GH is blunted, and in some cases IGFBP­3 synthesis is enhanced, resulting in marked inhibition in the growth of the child. GHRH, growth hormone­releasing hormone. Growth hormone deficiency (GHD) is characterized by decreased growth velocity and delayed skeletal maturation in the absence of other explanations (Figure 34–5). Because GH promotes lipolysis, many GH­deficient children have excess truncal adiposity. GHD may be isolated or coexist with other pituitary hormone deficiencies and may be congenital (septo­optic dysplasia or ectopic posterior pituitary), genetic (GH or GHRH gene mutation), or acquired (craniopharyngioma, germinoma, histiocytosis, or cranial irradiation). Idiopathic GHD is the most common deficiency state with an incidence of about 1:4000 children. Patients have also been described with congenital GH­resistance syndromes. The presentation of GH resistance is similar to that of GHD, but short stature is often severe, with little or no response to GH therapy and may be accompanied by dysmorphic features. Figure 34–5. Typical pattern of growth in a child with acquired growth hormone deficiency (GHD). Children with acquired GHD have an abnormal growth velocity and fail to maintain height percentile during childhood. Other phenotypic features (central adiposity and immaturity of facies) may be present. Children with congenital GHD will cross percentiles during the first 2 years of life, similarly to the pattern seen in familial short stature and constitutional delay, but will fail to attain a steady height percentile subsequently. Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility Page 8 / 53 Typical pattern of growth in a child with acquired growth hormone deficiency (GHD). Children with acquired GHD have an abnormal growth velocity University of Medicine and Pharmacy at HCMC and fail to maintain height percentile during childhood. Other phenotypic features (central adiposity and immaturity of facies) may be present. Access Provided by: Children with congenital GHD will cross percentiles during the first 2 years of life, similarly to the pattern seen in familial short stature and constitutional delay, but will fail to attain a steady height percentile subsequently. Features of infantile GHD include normal birth weight and slightly reduced length, hypoglycemia (if accompanied by adrenal insufficiency), micropenis (if accompanied by gonadotropin deficiency), and conjugated hyperbilirubinemia (if other pituitary hormone deficiencies present). In isolated GHD and hypopituitarism, growth abnormalities may not present until late in infancy or childhood. Laboratory tests to assess GH status may be difficult to interpret because there is significant overlap in GH secretion between normal and GH­deficient children. GH secretion is pulsatile, so random samples for measurement of serum GH are of no value in the diagnosis of GHD outside of the first week of life. Serum concentrations of IGF­1 give reasonable estimations of GH secretion and action in the adequately nourished child (see Figure 34–4) and are often used as a first step in the evaluation for GHD. IGF­binding protein 3 (IGFBP­3) is a less sensitive marker of GH deficiency but may be useful in the underweight child or in children younger than 4 years, since it is less affected by age or nutritional status. Provocative studies using such agents as insulin, arginine, levodopa, clonidine, or glucagon are traditionally done to clarify GH secretion, but are not physiologic and are often poorly reproducible, ultimately limiting their value in the clarification of GH secretion. The diagnosis of GHD is often a compilation of clinical and laboratory evidence and must be approached with care. All patients diagnosed with GHD should have an MRI of the hypothalamus and pituitary gland to evaluate for a tumor prior to starting therapy. 3. Small for Gestational Age/Intrauterine Growth Restriction Small­for­gestational­age (SGA) infants have a birth weight and/or length below the 3rd percentile for the population’s birth weight–gestational age relationship. SGA infants include constitutionally small infants and infants with intrauterine growth restriction (IUGR). Many children with mild SGA/IUGR and no intrinsic fetal abnormalities exhibit catch­up growth during the first 3 years, but 15%–20% remain short throughout life. Catch­up growth may also be inadequate in preterm SGA/IUGR infants with poor postnatal nutrition. Children who do not show catch­up growth may have Downloaded A aYour IPheight is 13.213.160.179 normal growth2023­10­12 velocity but2:52 follow lower percentile than expected for the family. In contrast to children with constitutional growth delay, those Page 9 / 53 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu with SGA/IUGR have skeletal maturation that corresponds to chronologic age or is only mildly delayed. GH therapy for SGA/IUGR children with growth ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility delay is approved by the U.S. Food and Drug Administration (FDA) and appears to increase growth velocity and final adult height. 3. Small for Gestational Age/Intrauterine Growth Restriction University of Medicine and Pharmacy at HCMC Access Provided by: Small­for­gestational­age (SGA) infants have a birth weight and/or length below the 3rd percentile for the population’s birth weight–gestational age relationship. SGA infants include constitutionally small infants and infants with intrauterine growth restriction (IUGR). Many children with mild SGA/IUGR and no intrinsic fetal abnormalities exhibit catch­up growth during the first 3 years, but 15%–20% remain short throughout life. Catch­up growth may also be inadequate in preterm SGA/IUGR infants with poor postnatal nutrition. Children who do not show catch­up growth may have normal growth velocity but follow a lower height percentile than expected for the family. In contrast to children with constitutional growth delay, those with SGA/IUGR have skeletal maturation that corresponds to chronologic age or is only mildly delayed. GH therapy for SGA/IUGR children with growth delay is approved by the U.S. Food and Drug Administration (FDA) and appears to increase growth velocity and final adult height. 4. Disproportionate Short Stature There are more than 200 sporadic and genetic skeletal dysplasias that may cause disproportionate short stature. Measurements of arm span and upper­to­lower body segment ratio are helpful in determining whether a child has normal body proportions. If disproportionate short stature is found, a skeletal survey may be useful to detect specific radiographic features characteristic of some disorders. The effect of GH on most of these rare disorders is unknown. 5. Short Stature Associated With Syndromes Short stature is associated with many genetic syndromes, including Turner, Down, Noonan, and Prader­Willi. Girls with Turner syndrome often have recognizable features such as micrognathia, webbed neck, low posterior hairline, edema of hands and feet, multiple pigmented nevi, and an increased carrying angle. However, short stature can be the only clinically obvious manifestation of Turner syndrome. Consequently, any girl with unexplained short stature for family warrants a chromosomal evaluation. Although girls with Turner syndrome are not usually GH­deficient, GH therapy can improve final height by an average of 6 cm. Duration of GH therapy is a significant predictor of long­term height gain; consequently, it is important that Turner syndrome be diagnosed early and GH started as soon as possible if the family desires to maximize height. GH is approved for treatment of growth failure in Prader­Willi syndrome–associated GHD. GH improves growth, body composition, and physical activity. A few deaths have been reported in children with Prader­Willi Syndrome receiving GH. These deaths occurred in very obese children, children with respiratory impairments, or possibly unidentified respiratory infections. The role of GH in these deaths is unknown, but it is recommended that all patients with Prader­Willi syndrome be evaluated for upper airway obstruction and sleep apnea prior to starting GH therapy. Children with Down syndrome should be evaluated for GHD only if their linear growth is abnormal compared with the Down syndrome growth chart. Given their increased malignancy risk, some families may be wary of adding GH therapy. 6. Psychosocial Short Stature (Psychosocial Dwarfism) Psychosocial short stature refers to growth impairment associated with emotional deprivation. Undernutrition probably contributes to growth slowing in some of these children. Other symptoms include unusual eating and drinking habits, bowel and bladder incontinence, social withdrawal, and delayed speech. GH secretion in children with psychosocial short stature is diminished, but GH therapy is usually not beneficial. A change in the psychological environment at home usually results in improved growth and improvement of GH secretion, personality, and eating behaviors. Clinical Evaluation Laboratory investigation should be guided by the history and physical examination, including history of chronic illness and medications, birth weight and height, pattern of growth since birth, familial growth patterns, pubertal stage, dysmorphic features, body segment proportion, and psychological health. In a child with poor weight gain as the primary disturbance, a nutritional assessment is indicated. The following laboratory tests may be useful as guided by history and clinical judgment: (1) radiograph of left hand and wrist for bone age; (2) karyotype (girls) and/or Noonan syndrome testing; (3) thyroid function tests: thyroxine (T4) and thyroid­stimulating hormone (TSH); (4) IGF­1 and/or IGFBP­3 in children younger than 4 years or in malnourished individuals; (5) complete blood count (to detect chronic anemia or leukocyte markers of infection); (6) erythrocyte sedimentation rate (often elevated in collagen­vascular disease, cancer, chronic infection, and inflammatory bowel disease); (7) urinalysis, blood urea nitrogen, and serum creatinine (occult renal disease); (8) serum electrolytes, calcium, and phosphorus (renal tubular disease and metabolic bone disease); (9) stool examination for fat, or measurement of serum tissue transglutaminase (malabsorption or celiac disease). Growth Hormone Therapy GH therapy is approved by the FDA in children with GHD; growth restriction associated with chronic renal failure; Turner, Prader­Willi, and Noonan syndromes; children born small for gestational age (SGA) who fail to demonstrate catch­up growth by age 2; and short stature homeobox­containing (SHOX) gene mutations. GH2:52 therapy has IP also approved for children with idiopathic short stature whose current height is more than 2.25 standard Downloaded 2023­10­12 A Your is been 13.213.160.179 Page 10 / 53 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie deviations below the normal range for age. With GH treatment, final height may be 5–7 cm taller in this population. TheHsu role of GH for idiopathic short ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility stature is still unclear, especially due to the expense, long duration of treatment, and unclear psychological consequences. Side effects of recombinant GH are uncommon but include intracranial hypertension and slipped capital femoral epiphysis. With early diagnosis and treatment, children with GH examination for fat, or measurement of serum tissue transglutaminase (malabsorption or celiac disease). Growth Hormone Therapy University of Medicine and Pharmacy at HCMC Access Provided by: GH therapy is approved by the FDA in children with GHD; growth restriction associated with chronic renal failure; Turner, Prader­Willi, and Noonan syndromes; children born small for gestational age (SGA) who fail to demonstrate catch­up growth by age 2; and short stature homeobox­containing (SHOX) gene mutations. GH therapy has also been approved for children with idiopathic short stature whose current height is more than 2.25 standard deviations below the normal range for age. With GH treatment, final height may be 5–7 cm taller in this population. The role of GH for idiopathic short stature is still unclear, especially due to the expense, long duration of treatment, and unclear psychological consequences. Side effects of recombinant GH are uncommon but include intracranial hypertension and slipped capital femoral epiphysis. With early diagnosis and treatment, children with GH deficiency reach normal or near­normal adult height. Recombinant IGF­1 injections may be used to treat children with GH resistance or IGF­1 deficiency, but improvements in growth may not be as substantial as seen with GH therapy for GH deficiency. Currently, the recommended schedule for GH therapy is subcutaneous recombinant GH given subcutaneously 6 or 7 days per week with total weekly dose of 0.15–0.47 mg/kg. Altzoglou KS et al: Isolated growth hormone deficiency (GHD) in childhood and adolescence: recent advances. Endocr Rev 2014;35:376–432 [PubMed: 24450934] . Cohen LE: Idiopathic short stature: a clinical review. JAMA 2014;311:1787–1796 [PubMed: 24794372] . Loche S et al: Growth hormone treatment in non­growth hormone­deficiency children. Ann Pediatr Endocrinol Metab 2014;19:1–7 [PubMed: 24926456] . Rogol AD, Hayden GF: Etiologies and early diagnosis of short stature and growth failure in children and adolescents. J Pediatr 2014 May;164(5 Suppl):S1–14.e6 [PubMed: 24731744] . TALL STATURE Although growth disturbances are usually associated with short stature, potentially serious pathologic conditions may also be associated with tall stature and excessive growth (Table 34–3). Excessive GH secretion is rare, particularly in children, and generally associated with a functioning pituitary adenoma. GH excess leads to gigantism if the epiphyses are open and to acromegaly if the epiphyses are closed. The diagnosis is confirmed by finding elevated random GH and IGF­1 levels and failure of GH suppression during an oral glucose tolerance test. Precocious puberty can also cause tall stature for age or rapid growth but would be associated with early signs of puberty and an advanced bone age. Obese youth are also often tall for age, but they do not achieve a taller final height. Table 34–3. Causes of tall stature. A. Constitutional (familial) B. Endocrine causes 1. Growth hormone excess (pituitary gigantism) 2. Precocious puberty 3. Hypogonadism C. Nonendocrine causes 1. Klinefelter syndrome 2. XYY males 3. Marfan syndrome 4. Cerebral gigantism (Sotos syndrome) 5. Homocystinuria Davies JH, Cheetham T: Investigation and management of tall stature. Arch Dis Child 2014;99:772–777 [PubMed: 24833789] . Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility DISORDERS OF THE POSTERIOR PITUITARY GLAND Page 11 / 53 5. Homocystinuria University of Medicine and Pharmacy at HCMC Access Provided by: Davies JH, Cheetham T: Investigation and management of tall stature. Arch Dis Child 2014;99:772–777 [PubMed: 24833789] . DISORDERS OF THE POSTERIOR PITUITARY GLAND The posterior pituitary (neurohypophysis) is an extension of the ventral hypothalamus. Its two principal hormones—oxytocin and arginine vasopressin —are synthesized in the supraoptic and paraventricular nuclei of the ventral hypothalamus. These peptide hormones are packaged in granules with specific neurophysins and transported via the axons to their storage site in the posterior pituitary. Vasopressin is essential for water balance; it acts primarily on the kidney to promote reabsorption of water from urine. Oxytocin is most active during parturition and breast feeding and is not discussed further here. ARGININE VASOPRESSIN (ANTIDIURETIC HORMONE) PHYSIOLOGY Vasopressin release is controlled primarily by serum osmolality and intravascular volume. Release is stimulated by minor increases in plasma osmolality (detected by osmoreceptors in the anterolateral hypothalamus) and large decreases in intravascular volume (detected by baroreceptors in the cardiac atria). Disorders of vasopressin release and action include: (1) central diabetes insipidus (DI), (2) nephrogenic DI (see Chapter 24), and (3) the syndrome of inappropriate secretion of antidiuretic hormone (SIADH). CENTRAL DIABETES INSIPIDUS ESSENTIALS OF DIAGNOSIS & TYPICAL FEATURES Polydipsia, polyuria (> 2 L/m2/day), nocturia, dehydration, and hypernatremia. Inability to concentrate urine after fluid restriction (urine specific gravity < 1.010; urine osmolality < 300 mOsm/kg). Plasma osmolality 300 > mOsm/kg with urine osmolality < 600 mOsm/kg. Low plasma vasopressin with antidiuretic response to exogenous vasopressin. General Considerations Central DI is an inability to synthesize and release vasopressin. Without vasopressin, the kidneys cannot concentrate urine, causing excessive urinary water loss. Genetic causes of central DI are rare and include mutations in the vasopressin gene and the WFS1 gene that causes DI, diabetes mellitus, optic atrophy, and deafness (Wolfram or DIDMOAD syndrome). The most common causes of pediatric central DI are midline defects (septo­optic dysplasia, holoprosencephaly); trauma (surgery, injury); infiltrative/neoplastic disease (tumors such as craniopharyngioma, germinoma, Langerhans cell histiocytosis, sarcoidosis); infectious (meningitis); and idiopathic. Traumatic DI often has three phases. Initially, transient DI is caused by edema in the hypothalamus or pituitary area. In 2–5 days, unregulated release of vasopressin from dying neurons causes the SIADH. Finally, permanent DI occurs if a sufficient number of vasopressin neurons are destroyed. Clinical Findings Onset of DI is characterized by polyuria, nocturia, enuresis, and intense thirst, usually with a preference for cold water. Hypernatremia, hyperosmolality, and dehydration occur if insufficient fluid intake does not keep up with urinary losses. In infants, symptoms may also include failure to thrive, vomiting, constipation, and unexplained fevers. Some infants may present with severe dehydration, circulatory collapse, and seizures. Vasopressin deficiency may be masked in patients with panhypopituitarism due to the impaired excretion of free water associated with adrenocorticotropic hormone (ACTH) insufficiency; treatment with glucocorticoids may unmask DI in these patients. Diabetes insipidus is confirmed when serum hyperosmolality is associated with urine hypo­osmolarity. If the history indicates that the child can go through the night comfortably without drinking, outpatient testing is appropriate. Oral fluid intake is prohibited after midnight. Osmolality, sodium, and specific gravity of the first obtained. If symptoms suggest child cannot safely go through night without drinking or if outpatient Downloaded 2023­10­12 2:52morning A Your void IP isare 13.213.160.179 12 / 53 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M.be Chan; Cree­Green; Shanlee Davis; testing results are unclear, the water deprivation test should doneMelanie in the hospital. See “Essentials” box forStephanie diagnosticHsu criteria. Children Page with central ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility DI should have an MRI of the head with contrast to look for tumors or infiltrative processes. Primary polydipsia must be distinguished from DI. Children with primary polydipsia tend to have lower serum sodium levels and usually can to thrive, vomiting, constipation, and unexplained fevers. Some infants may present with severe dehydration, circulatory collapse, and seizures. Vasopressin deficiency may be masked in patients with panhypopituitarism due to the impaired excretion of free water associated with University of Medicine and Pharmacy at HCMC adrenocorticotropic hormone (ACTH) insufficiency; treatment with glucocorticoids may unmask DI in these patients. Access Provided by: Diabetes insipidus is confirmed when serum hyperosmolality is associated with urine hypo­osmolarity. If the history indicates that the child can go through the night comfortably without drinking, outpatient testing is appropriate. Oral fluid intake is prohibited after midnight. Osmolality, sodium, and specific gravity of the first morning void are obtained. If symptoms suggest child cannot safely go through night without drinking or if outpatient testing results are unclear, the water deprivation test should be done in the hospital. See “Essentials” box for diagnostic criteria. Children with central DI should have an MRI of the head with contrast to look for tumors or infiltrative processes. Primary polydipsia must be distinguished from DI. Children with primary polydipsia tend to have lower serum sodium levels and usually can concentrate their urine with overnight fluid deprivation. Some may have secondary nephrogenic DI due to dilution of the renal medullary interstitium and decreased renal concentrating ability, but this resolves with restriction of fluid intake. Treatment Central DI is treated with oral or intranasal desmopressin acetate (DDAVP). The aim of therapy is to provide antidiuresis that allows uninterrupted sleep. Breakthrough urination should occur before the next dose. It is important to note that postsurgical DI can be associated with disruption of thirst mechanism, and for these patients, a prescribed volume of fluid intake may be necessary. Children hospitalized with acute­onset DI can be managed with intravenous or subcutaneous vasopressin. Due to the amount of antidiuresis, electrolytes should be closely monitored to avoid water intoxication. Infants with DI should not be treated with DDAVP, since their primary source of nutrition is through liquid calories and this combination can result in water intoxication. For this reason, infants are treated with extra free water to maintain normal hydration. A formula with a low renal solute load and thiazide diuretic may be helpful in infants with central DI. Di Iorgi N et al: Diabetes insipidus—diagnosis and management. Horm Res Paediatr 2012;77:69 [PubMed: 22433947] . Rivkees SA et al: The management of central diabetes insipidus in infancy: desmopressin, low renal solute load formula, thiazide diuretics. J Pediatr Endocrinol Metab 2007;20:459 [PubMed: 17550208] . Wise­Faberowski L et al: Perioperative management of diabetes insipidus in children. J Neurosurg Anesthesiol 2004;16:14 [PubMed: 14676564] . THYROID GLAND FETAL DEVELOPMENT OF THE THYROID As early as the 10th week of gestation, the fetal thyroid synthesizes thyroid hormone, which appears in the fetal serum by the 11th week of gestation and progressively increases throughout gestation. The fetal pituitary­thyroid axis functions largely independently of the maternal pituitary­thyroid axis because maternal TSH cannot cross the placenta. However, maternal thyroid hormone can cross the placenta in limited amounts. At birth, there is a TSH surge peaking at about 70 mU/L within 30 minutes. Thyroid hormone levels increase rapidly during the first days of life in response to this TSH surge. The TSH level decreases to childhood levels within a few weeks. This physiologic neonatal TSH surge can produce a false­ positive newborn screen for hypothyroidism (ie, high TSH) if the blood sample for the screen is collected on the first day of life. PHYSIOLOGY Hypothalamic thyrotropin­releasing hormone (TRH) stimulates the anterior pituitary gland to release TSH. In turn, TSH stimulates the thyroid gland to take up iodine and synthesize and release T4 and T3. This process is regulated by negative feedback involving the hypothalamus, pituitary, and thyroid (see Figure 34–1). T4 is the predominant thyroid hormone secreted by the thyroid gland. Most circulating T3 and T4 are bound to thyroxine­binding globulin (TBG), albumin, and prealbumin. Less than 1% of thyroid hormone exists in the free form. T4 is deiodinated in the tissues to T3, which binds to nuclear thyroid hormone receptors in the cytoplasm and translocates to the nucleus, exerting its biologic effects by modifying gene expression. Causes of low T4 are hypothyroidism (central or primary), prematurity, malnutrition and severe illness, and following therapy with T3. Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 Page 13 / 53 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu Total is also low in All situations that decrease TBG, of such deficiency, or renal failure and in patients receiving glucocorticoids ©2023T4McGraw Hill. Rights Reserved. Terms Useas• familial PrivacyTBG Policy • Notice cirrhosis, • Accessibility or androgens. Since these effects primarily involve TBG, TSH and free T4 (FT4) levels remain in the normal range. Conversely, total T3 and T4 levels may (see Figure 34–1). University of Medicine and Pharmacy at HCMC T4 is the predominant thyroid hormone secreted by the thyroid gland. Most circulating T3 and T4 are bound to thyroxine­binding globulin (TBG), Access Provided by: albumin, and prealbumin. Less than 1% of thyroid hormone exists in the free form. T4 is deiodinated in the tissues to T3, which binds to nuclear thyroid hormone receptors in the cytoplasm and translocates to the nucleus, exerting its biologic effects by modifying gene expression. Causes of low T4 are hypothyroidism (central or primary), prematurity, malnutrition and severe illness, and following therapy with T3. Total T4 is also low in situations that decrease TBG, such as familial TBG deficiency, cirrhosis, or renal failure and in patients receiving glucocorticoids or androgens. Since these effects primarily involve TBG, TSH and free T4 (FT4) levels remain in the normal range. Conversely, total T3 and T4 levels may be elevated in conditions associated with increased TBG levels (congenital TBG excess, pregnancy, estrogen therapy) and increased thyroid hormone binding to transport proteins. Again, patients are clinically euthyroid in this circumstance. A T3 resin uptake (T3RU) can help differentiate between binding protein problems and true hypo­ or hyperthyroidism. HYPOTHYROIDISM (CONGENITAL & ACQUIRED) ESSENTIALS OF DIAGNOSIS & TYPICAL FEATURES Growth impairment, decreased physical activity, weight gain, constipation, dry skin, cold intolerance, and delayed puberty. Untreated congenital hypothyroidism: thick tongue, large fontanels, poor muscle tone, hoarseness, umbilical hernia, jaundice, and intellectual impairment. T4, FT4, and T3 resin uptake are low; TSH levels are elevated in primary hypothyroidism. General Considerations Thyroid hormone deficiency may be congenital or acquired (Table 34–4). It can be due to defects in the thyroid gland (primary hypothyroidism) or in the hypothalamus or pituitary (central hypothyroidism). Table 34–4. Causes of hypothyroidism. A. Congenital 1. Aplasia, hypoplasia, or maldescent of thyroid 2. Inborn errors of thyroid hormone synthesis, secretion, or recycling 3. Maternal antibody­mediated (inhibit TSH binding to receptor) 4. TSH receptor defect 5. Thyroid hormone receptor defect 6. In utero exposures a. Radioiodine therapy b. Goitrogens (propylthiouracil, methimazole) c. Iodine excess 7. Iodide deficiency B. Acquired (juvenile hypothyroidism) 1. Autoimmune (lymphocytic) thyroiditis 2. Thyroidectomy or radioiodine therapy 3. Irradiation to the thyroid 4. Thyrotropin deficiency 5. TRH deficiency due to hypothalamic injury or disease 6. Medications a. Iodides 1. Excess (eg, amiodarone) 2. Deficiency b. Lithium Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 c. Cobalt Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu 7. Large hemangiomas ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility 8. Idiopathic Page 14 / 53 General Considerations University of Medicine and Pharmacy at HCMC Access Provided by: Thyroid hormone deficiency may be congenital or acquired (Table 34–4). It can be due to defects in the thyroid gland (primary hypothyroidism) or in the hypothalamus or pituitary (central hypothyroidism). Table 34–4. Causes of hypothyroidism. A. Congenital 1. Aplasia, hypoplasia, or maldescent of thyroid 2. Inborn errors of thyroid hormone synthesis, secretion, or recycling 3. Maternal antibody­mediated (inhibit TSH binding to receptor) 4. TSH receptor defect 5. Thyroid hormone receptor defect 6. In utero exposures a. Radioiodine therapy b. Goitrogens (propylthiouracil, methimazole) c. Iodine excess 7. Iodide deficiency B. Acquired (juvenile hypothyroidism) 1. Autoimmune (lymphocytic) thyroiditis 2. Thyroidectomy or radioiodine therapy 3. Irradiation to the thyroid 4. Thyrotropin deficiency 5. TRH deficiency due to hypothalamic injury or disease 6. Medications a. Iodides 1. Excess (eg, amiodarone) 2. Deficiency b. Lithium c. Cobalt 7. Large hemangiomas 8. Idiopathic T 3, triiodothyronine; T4, thyroxine; TRH, thyrotropin­releasing hormone; TSH, thyroid­stimulating hormone. Congenital hypothyroidism occurs in about 1:3000–1:4000 infants. Untreated, it causes severe neurocognitive impairment. Most cases are sporadic resulting from hypoplasia or aplasia of the thyroid gland or failure of the gland to migrate to its normal anatomic location (eg, lingual or sublingual thyroid gland). Other causes are listed in Table 34–4. In severe maternal iodine deficiency, both the fetus and the mother are T4­deficient, with irreversible brain damage to the fetus. Acquired hypothyroidism, particularly if goiter is present, is usually a result of chronic lymphocytic (Hashimoto) thyroiditis. Clinical Findings A. Symptoms and Signs Even when the thyroid gland is completely absent, most newborns with congenital hypothyroidism appear normal. However, because congenital hypothyroidism is associated with intellectual impairment, thyroid testing is included in the newborn screen and treatment must be initiated as early as possible. Jaundice associated with an unconjugated hyperbilirubinemia may be present in newborns with congenital hypothyroidism. Features of juvenile hypothyroidism include poor linear growth; delayed bone age and delayed dental eruption; skin changes (dry, thick, scaly, coarse, pale, cool, or sallow); hair changes (dry, coarse, or brittle) and hair loss; lateral thinning of the eyebrows; neurological findings (hypotonia and a slow relaxation component of deep tendon reflexes); physical and mental sluggishness; nonpitting myxedema; constipation; cold temperature intolerance; bradycardia; delayed puberty; and occasional pseudopuberty (secondary to weak FSH activity of marked elevated TSH levels). Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 Page 15 / 53 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie HsuThyroid enlargement In hypothyroidism resulting from enzymatic defects or chronic lymphocytic thyroiditis, the thyroid gland may be enlarged. in ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility children is usually symmetrical, and the gland is moderately firm and not nodular. In chronic lymphocytic thyroiditis, however, the thyroid frequently has a cobblestone surface (see the following text). as possible. Jaundice associated with an unconjugated hyperbilirubinemia may be present in newborns with congenital hypothyroidism. University of Medicine and Pharmacy at HCMC Provided by: changes (dry, thick, scaly, coarse, Features of juvenile hypothyroidism include poor linear growth; delayed bone age and delayed dental Access eruption; skin pale, cool, or sallow); hair changes (dry, coarse, or brittle) and hair loss; lateral thinning of the eyebrows; neurological findings (hypotonia and a slow relaxation component of deep tendon reflexes); physical and mental sluggishness; nonpitting myxedema; constipation; cold temperature intolerance; bradycardia; delayed puberty; and occasional pseudopuberty (secondary to weak FSH activity of marked elevated TSH levels). In hypothyroidism resulting from enzymatic defects or chronic lymphocytic thyroiditis, the thyroid gland may be enlarged. Thyroid enlargement in children is usually symmetrical, and the gland is moderately firm and not nodular. In chronic lymphocytic thyroiditis, however, the thyroid frequently has a cobblestone surface (see the following text). B. Laboratory Findings In primary hypothyroidism, the total T4 and FT4 may be normal or decreased and the serum TSH is elevated. Circulating autoantibodies to thyroid peroxidase and/or thyroglobulin may be present. In central hypothyroidism, the TSH is usually inappropriately normal in the face of a low total T4 and FT4. Other pituitary deficiencies may be present, as central hypothyroidism may be associated with congenital or acquired disorders of the hypothalamus or pituitary gland. C. Imaging Thyroid imaging, while helpful in establishing the cause of congenital hypothyroidism, does not affect the treatment plan and is not necessary. Bone age is delayed. Cardiomegaly is common. Long­standing primary hypothyroidism may be associated with thyrotrophic hyperplasia characterized by an enlarged sella or pituitary gland. D. Screening Programs for Neonatal Hypothyroidism All newborns should be screened for congenital hypothyroidism shortly after birth. Depending on the state, the newborn screen measures either the total T4 or TSH level. Abnormal newborn screening results should be confirmed immediately with a venous T4 and TSH level. Treatment should be started as soon as possible. Initiation of treatment in the first month of life and good medication adherence during infancy usually results in a normal neurocognitive outcome. Treatment Synthetic T4 or levothyroxine (75–100 mcg/m2/day) is the drug of choice for hypothyroidism. In neonates with congenital hypothyroidism, the recommended initial dose is 10–15 mcg/kg/day. Serum total T4 or FT4 concentrations are used to monitor the adequacy of initial therapy because the high neonatal TSH may not normalize for weeks. Subsequently, T4 and TSH are monitored in combination. Kaplowitz, P: Neonatal thyroid disease: testing and management. Pediatr Clin North Am 2019;66(2):343–352 [PubMed: 30819341] . Léger J et al: European Society for Paediatric Endocrinology consensus guidelines on screening, diagnosis, and management of congenital hypothyroidism. J Clin Endocrinol Metab 2014;99(2):363–384 [PubMed: 24446653] . van der Sluijs Veer L et al: Evaluation of cognitive and motor development in toddlers with congenital hypothyroidism diagnosed by neonatal screening. J Dev Behav Pediatr 2012;33:633–640 [PubMed: 23027136] . THYROIDITIS 1. Chronic Lymphocytic Thyroiditis (Chronic Autoimmune Thyroiditis, Hashimoto Thyroiditis) ESSENTIALS OF DIAGNOSIS & TYPICAL FEATURES Firm, freely movable, nontender, diffusely enlarged thyroid gland. Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu function often normal but may be elevated or decreased the stage of the disease. ©2023Thyroid McGraw Hill. AllisRights Reserved. Terms of Use • Privacy Policydepending • Notice •on Accessibility Page 16 / 53 THYROIDITIS University of Medicine and Pharmacy at HCMC Access Provided by: 1. Chronic Lymphocytic Thyroiditis (Chronic Autoimmune Thyroiditis, Hashimoto Thyroiditis) ESSENTIALS OF DIAGNOSIS & TYPICAL FEATURES Firm, freely movable, nontender, diffusely enlarged thyroid gland. Thyroid function is often normal but may be elevated or decreased depending on the stage of the disease. General Considerations Chronic lymphocytic thyroiditis is the most common cause of goiter and acquired hypothyroidism in childhood. It is more common in girls, and the incidence peaks during puberty. The disease is caused by an autoimmune attack on the thyroid. Increased risk of thyroid autoimmunity (and other endocrine autoimmune disorders) is associated with certain histocompatibility alleles. The following conditions are associated with increased risk for autoimmune (Hashimoto) thyroiditis: Down syndrome, Turner syndrome, celiac disease, vitiligo, alopecia, and type 1 diabetes. Clinical Findings A. Symptoms and Signs The thyroid is characteristically enlarged, firm, freely movable, nontender, and symmetrical. It may be nodular. Onset is usually insidious. Occasionally, patients note a sensation of tracheal compression or fullness, hoarseness, and dysphagia. No local signs of inflammation or systemic infection are present. Most patients are euthyroid. Some patients are symptomatically hypothyroid, and few patients are symptomatically hyperthyroid. A detailed family history may reveal the presence of multiple autoimmune diseases in family members. Individuals at a high risk based on a chromosomal disorder or other autoimmune disease benefit from careful monitoring of growth and development, routine screening (in the case of Down syndrome, Turner syndrome, type 1 diabetes, and celiac disease), and a low threshold for measurement of thyroid function. B. Laboratory Findings Laboratory findings vary. Serum concentrations of TSH, T4, and FT4 are usually normal. Some patients are hypothyroid with an elevated TSH and low thyroid hormone levels. A few patients are hyperthyroid early in the disease course (aka Hashitoxicosis) with a suppressed TSH and elevated thyroid hormone levels. Thyroid antibodies (antithyroglobulin, antithyroid peroxidase) are frequently elevated. C. Imaging Routine thyroid ultrasound is not indicated unless a focal nodule or mass is palpated. Thyroid uptake scan adds little to the diagnosis. Surgical or needle biopsy is diagnostic but seldom necessary. Treatment There is controversy about the need to treat chronic lymphocytic thyroiditis with normal thyroid function. Full replacement doses of thyroid hormone may decrease the size of the thyroid, but may also result in hyperthyroidism. Hypothyroidism commonly develops over time. Consequently, patients require lifelong surveillance. Children with documented hypothyroidism should receive thyroid hormone replacement. 2. Acute (Suppurative) Thyroiditis Acute thyroiditis is rare. The most common causes are group A streptococci, pneumococci, Staphylococcus aureus, and anaerobes. Thyroid abscesses may form and are often left sided due to pyriform sinus fistula. The patient presents with fever and an enlarged and tender thyroid gland with associated erythema, hoarseness, and dysphagia. Thyroid function tests are typically normal. Patients have a leukocytosis, “left shift,” and elevated erythrocyte sedimentation rate. Antibiotic therapy is required. 3. Subacute (Nonsuppurative) Thyroiditis Subacute thyroiditis (de Quervain thyroiditis) is rare. It is thought to be caused by viral infection with mumps, influenza, echovirus, coxsackievirus, Downloaded 2023­10­12 2:52 A Presenting Your IP is 13.213.160.179 Epstein­Barr virus, or adenovirus. features are similar to acute thyroiditis—fever, malaise, sore throat, dysphagia, and thyroid pain. The Page 17 / 53 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu thyroid is firm and enlarged. Sedimentation rate is elevated. In contrast to acute thyroiditis, the onset is generally insidious and serum thyroid ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility hormone concentrations may be elevated. associated erythema, hoarseness, and dysphagia. Thyroid function tests are typically normal. Patients have a leukocytosis, “left shift,” and elevated University of Medicine and Pharmacy at HCMC erythrocyte sedimentation rate. Antibiotic therapy is required. Access Provided by: 3. Subacute (Nonsuppurative) Thyroiditis Subacute thyroiditis (de Quervain thyroiditis) is rare. It is thought to be caused by viral infection with mumps, influenza, echovirus, coxsackievirus, Epstein­Barr virus, or adenovirus. Presenting features are similar to acute thyroiditis—fever, malaise, sore throat, dysphagia, and thyroid pain. The thyroid is firm and enlarged. Sedimentation rate is elevated. In contrast to acute thyroiditis, the onset is generally insidious and serum thyroid hormone concentrations may be elevated. HYPERTHYROIDISM ESSENTIALS OF DIAGNOSIS & TYPICAL FEATURES Palpitations, nervousness, hyperactivity, excessive appetite, tremor, weight loss, fatigue, and heat intolerance. Goiter, tachycardia, exophthalmos, systolic hypertension, widened pulse pressure, weakness, and moist, warm skin. TSH is suppressed. Thyroid hormone levels (T4, FT4, T3) and T3 resin uptake (T3RU) are elevated. General Considerations In children, most cases of hyperthyroidism are due to Graves disease, caused by antibodies directed at the TSH receptor that stimulate thyroid hormone production. Other causes include thyroiditis (acute, subacute, or chronic); autonomous functioning thyroid nodules; tumors producing TSH; McCune­Albright syndrome; exogenous thyroid hormone excess; and acute iodine exposure. Clinical Findings A. Symptoms and Signs Hyperthyroidism is more common in females than males. In children, it most frequently occurs during adolescence. The course of hyperthyroidism may be cyclic, with spontaneous remissions and exacerbations. Symptoms include poor concentration, hyperactivity, fatigue, emotional lability, personality disturbance/unmasking of underlying psychosis, insomnia, weight loss (despite increased appetite), palpitations, heat intolerance, increased perspiration, increased stool frequency, polyuria, and irregular menses. Signs include tachycardia, systolic hypertension, increased pulse pressure, tremor, proximal muscle weakness, and moist, warm skin. Accelerated growth and development may occur. Thyroid storm is a rare condition characterized by fever, cardiac failure, emesis, and delirium that can result in coma or death. Most cases of Graves disease are associated with a diffuse firm goiter. A thyroid bruit and thrill may be present. Many cases are associated with exophthalmos. B. Laboratory Findings TSH is suppressed. T4, FT4, T3, and free T3 (FT3) are elevated except in rare cases in which only the serum T3 is elevated (T3 thyrotoxicosis). The presence of thyroid­stimulating immunoglobulin (TSI) or thyroid eye disease confirms the diagnosis of Graves disease. TSH receptor­binding antibodies (TRAb) are usually elevated. C. Imaging Radioactive iodine uptake by the thyroid is increased in Graves disease, whereas in subacute and chronic thyroiditis it is decreased. An autonomous hyperfunctioning nodule takes up iodine and appears as a “hot nodule” while the surrounding tissue has decreased iodine uptake. In children with hyperthyroidism, bone age may be advanced. In infants, accelerated skeletal maturation may be associated with premature fusion of the cranial sutures. Long­standing hyperthyroidism causes osteoporosis. Treatment A. General Measures Strenuous physical activity should be avoided in untreated severe hyperthyroidism due to concern for cardiovascular instability. Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 B. Medical Treatment Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility 1 . β­Adrenergic blocking agents Page 18 / 53 These are adjuncts to therapy. They can rapidly ameliorate symptoms and are indicated in severe disease with tachycardia and hypertension. β ­ Treatment A. General Measures University of Medicine and Pharmacy at HCMC Access Provided by: Strenuous physical activity should be avoided in untreated severe hyperthyroidism due to concern for cardiovascular instability. B. Medical Treatment 1 . β­Adrenergic blocking agents These are adjuncts to therapy. They can rapidly ameliorate symptoms and are indicated in severe disease with tachycardia and hypertension. β1­ Specific agents such as atenolol are preferred because they are more cardioselective. Propranolol also decreases conversion of T4 to active T3, so is preferred in severe cases/thyrotoxicosis. 2. Antithyroid agents (m e t h i m a z o l e) Antithyroid agents are frequently used in the initial treatment of childhood hyperthyroidism. These drugs interfere with thyroid hormone synthesis, and usually take a few weeks to produce a clinical response. Adequate control is usually achieved within a few months. If medical therapy is unsuccessful, more definitive therapy, such as thyroidectomy or radioiodine ablation should be considered. Propylthiouracil (PTU) is rarely utilized because of reports of severe hepatotoxicity. A. INITIAL DOSAGE Methimazole is initiated at a dose of 10–60 mg/day (0.5–1 mg/kg/day) given once a day. Initial dosing is continued until FT4 or T4 have normalized and signs and symptoms have subsided. B. MAINTENANCE The optimal dose of antithyroid agent for maintenance treatment remains unclear. Recent studies suggest that 10–15 mg/day of methimazole provides adequate long­term control in most patients with a minimum of side effects. Treatment usually continues for 2 years with the goal of inducing remission. If thyroid hormone levels are well controlled at that point, a trial off medication could be considered. C. TOXICITY If vasculitis, arthralgia, arthritis, granulocytopenia, or hepatitis occur, the drug must be discontinued. Urticarial rash can sometimes be treated symptomatically. 3. Iodide Large doses of iodide usually produce a rapid but short­lived blockade of thyroid hormone synthesis and release. This approach is recommended only for acute management of severely thyrotoxic patients or in preparation for thyroidectomy. C. Radioactive Iodine Therapy Radioactive iodine ablation of the thyroid is usually reserved for children with Graves disease who do not respond to antithyroid agents, develop adverse effects from the antithyroid agents, fail to achieve remission after several years of medical therapy, or have poor medication adherence. Antithyroid agents should be discontinued 4–7 days prior to radioiodine treatment to allow radioiodine uptake by the thyroid. 131I is administered orally, concentrating in the thyroid and resulting in decreased thyroid activity. In the first 2 weeks following radioiodine treatment, hyperthyroidism may worsen as thyroid tissue is destroyed and thyroid hormone is released and temporary therapy with a β­adrenergic antagonist or methimazole may be necessary. In most cases, hypothyroidism develops and thyroid hormone replacement is needed. Long­term follow­up studies have not shown any increased incidence of thyroid cancer, leukemia, infertility, or birth defects when ablative doses of 131I were used. D. Surgical Treatment Subtotal and total thyroidectomies may also be considered in children with Graves disease. Surgery is indicated for extremely large goiters, goiters with a suspicious nodule, very young or pregnant patients, or patients refusing radioiodine ablation. Before surgery, a β­adrenergic blocking agent is given to treat symptoms, and antithyroid agents are given for several weeks to minimize the surgical risks associated with hyperthyroidism. Iodide (eg, Lugol solution, one drop every 8 hours, or saturated solution of potassium iodide, one to two drops three times per day) can be given for 1–2 weeks prior to surgery to reduce thyroid vascularity and inhibit release of thyroid hormone. Surgical complications include hypocalcemia due to hypoparathyroidism and recurrent laryngeal nerve damage. An experienced thyroid surgeon is crucial to good surgical outcome. After thyroidectomy, patients become hypothyroid and need thyroid hormone replacement. Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu Course & Prognosis ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility Page 19 / 53 Partial remissions and exacerbations may continue for several years. Treatment with an antithyroid agent results in prolonged remissions in one­third with a suspicious nodule, very young or pregnant patients, or patients refusing radioiodine ablation. Before surgery, a β­adrenergic blocking agent is University of Medicine and Pharmacy at HCMC given to treat symptoms, and antithyroid agents are given for several weeks to minimize the surgical risks associated with hyperthyroidism. Iodide (eg, Access Provided Lugol solution, one drop every 8 hours, or saturated solution of potassium iodide, one to two drops three times perby:day) can be given for 1–2 weeks prior to surgery to reduce thyroid vascularity and inhibit release of thyroid hormone. Surgical complications include hypocalcemia due to hypoparathyroidism and recurrent laryngeal nerve damage. An experienced thyroid surgeon is crucial to good surgical outcome. After thyroidectomy, patients become hypothyroid and need thyroid hormone replacement. Course & Prognosis Partial remissions and exacerbations may continue for several years. Treatment with an antithyroid agent results in prolonged remissions in one­third to two­thirds of children. Bauer AJ: Approach to the pediatric patient with Graves’ disease: when is definitive therapy warranted? J Clin Endocrinol Metab 2011;96:580–588 [PubMed: 21378220] . Rivkees SA: Pediatric Graves’ disease: management in the post­propylthiouracil. Era Int J Pediatrc Endocrinol 2014;2014(1):10 [PubMed: 25089127] . Yuan L, Yang J: Radioiodine treatment in pediatric Graves’ disease and thyroid carcinoma. J Pediatr Endocrinol Metab 2011;24:877–883 [PubMed: 22308835] . Neonatal Graves Disease Transient congenital hyperthyroidism (neonatal Graves disease) occurs in about 1% of infants born to mothers with Graves disease. It occurs when maternal TSH receptor antibodies cross the placenta and stimulate excess thyroid hormone production in the fetus and newborn. Neonatal Graves disease can be associated with irritability, intrauterine growth restriction (IUGR), poor weight gain, flushing, jaundice, hepatosplenomegaly, and thrombocytopenia. Severe cases may result in cardiac failure and death. Hyperthyroidism may develop several days after birth. In high­risk neonates, TSH receptor antibody (TRAb) level should be obtained at birth and free T4 and TSH obtained day of life 3–5. Immediate management should focus on the cardiac manifestations. Temporary treatment may be necessary with iodide, antithyroid agents, β­adrenergic antagonists, or corticosteroids. Hyperthyroidism gradually resolves over 1–3 months as maternal antibodies decline. As TRAbs may still be present in the serum of previously hyperthyroid mothers after thyroidectomy or radioablation, neonatal Graves disease should be considered in all infants of mothers with a history of hyperthyroidism. Léger J, Carel JC: Hyperthyroidism in childhood: causes, when, and how to treat. J Clin Res Pediatr Endocrinol 2013;5(Suppl 1):50–56 [PubMed: 23154161] . Lewis KA et al: Neonatal Graves disease associated with severe metabolic abnormalities. Pediatrics 2011;128(1):e232–e236 [PubMed: 21646263] . van der Kaay et al: Management of neonates born to mothers with Graves’ disease. Pediatrics 2016;137(4):e20151878 [PubMed: 26980880] . THYROID CANCER Thyroid cancer is rare in childhood. Children usually present with a thyroid nodule or an asymptomatic asymmetrical neck mass. Dysphagia and hoarseness are unusual symptoms. Thyroid function tests are usually normal. A “cold” nodule is often seen on a technetium or radioiodine uptake scan of the thyroid. Fine­needle aspiration biopsy of the nodule assists in the diagnosis. The most common thyroid cancer is papillary thyroid cancer, a well­differentiated cancer arising from the thyroid follicular cell. Follicular thyroid cancer is another type of differentiated thyroid cancer. Children with thyroid cancer are more likely than adults to have metastases to the cervical lymph nodes and lungs. Despite its aggressive presentation, children with differentiated thyroid cancer have an excellent prognosis, with a 20­year survival rate greater than 95%. Treatment consists of total thyroidectomy and removal of involved lymph nodes, usually followed by radioiodine ablation to destroy residual thyroid remnant and metastatic tissue left behind after surgery. Thyroid hormone replacement is started to suppress TSH stimulation of residual thyroid tissue and to treat the hypothyroidism that results from surgical removal of the thyroid gland. Since thyroid cancer in Downloaded 2023­10­12 A recurrence Your IP is rate, 13.213.160.179 children is associated with2:52 a high long­term follow­up is required. Page 20 / 53 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu ©2023 McGraw All Rights Reserved. of Use • Privacy • Notice • Accessibility Medullary thyroidHill. cancer, anaplastic cancer,Terms and lymphoma are less Policy common thyroid malignancies. Medullary thyroid cancer arises from the thyroid C cells, which secrete calcitonin, and it is associated with elevated serum calcitonin levels. In children, medullary thyroid cancer is usually familial due to an inherited mutation in the RET proto­oncogene as for example in multiple endocrine neoplasia (MEN) type 2. In affect families, all members should The most common thyroid cancer is papillary thyroid cancer, a well­differentiated cancer arising from the thyroid follicular cell. Follicular thyroid University Medicine and Pharmacy at HCMC cancer is another type of differentiated thyroid cancer. Children with thyroid cancer are more likely than adults to of have metastases to the cervical by: lymph nodes and lungs. Despite its aggressive presentation, children with differentiated thyroid cancerAccess haveProvided an excellent prognosis, with a 20­year survival rate greater than 95%. Treatment consists of total thyroidectomy and removal of involved lymph nodes, usually followed by radioiodine ablation to destroy residual thyroid remnant and metastatic tissue left behind after surgery. Thyroid hormone replacement is started to suppress TSH stimulation of residual thyroid tissue and to treat the hypothyroidism that results from surgical removal of the thyroid gland. Since thyroid cancer in children is associated with a high recurrence rate, long­term follow­up is required. Medullary thyroid cancer, anaplastic cancer, and lymphoma are less common thyroid malignancies. Medullary thyroid cancer arises from the thyroid C cells, which secrete calcitonin, and it is associated with elevated serum calcitonin levels. In children, medullary thyroid cancer is usually familial due to an inherited mutation in the RET proto­oncogene as for example in multiple endocrine neoplasia (MEN) type 2. In affect families, all members should be screened for the mutation, and those identified with the mutation should be treated with prophylactic thyroidectomy in early childhood. Chan et al: Pediatric thyroid cancer. Adv Pediatr 2017;64(1):171–190 [PubMed: 28688588] . Francis GL et al: Management guidelines for children with thyroid nodules and differentiated thyroid cancer. Thyroid 2015;25(7):716–759 [PubMed: 25900731] . Waguespack SG et al: Management of medullary thyroid carcinoma and MEN2 syndromes in childhood. Nat Rev Endocrinol 2011;23(7):596–607 [PubMed: 21862994] . Wells SA Jr et al: Revised American Thyroid Association guidelines for the management of medullary thyroid carcinoma. Thyroid 2015;25(6):567–610 [PubMed: 25810047] . DISORDERS OF CALCIUM & PHOSPHORUS METABOLISM Calcium plays an important role in virtually every cell. It is necessary for muscle function, neurotransmission, adenosine triphosphate (ATP) metabolism, and many other roles. Serum calcium concentration is tightly regulated by the coordinated actions of the parathyroid glands, kidney, liver, and small intestine. Low serum calcium concentrations, detected by calcium­sensing receptors on the surface of parathyroid cells, stimulate parathyroid hormone (PTH) release. PTH in turn promotes release of calcium and phosphorus from the bone, reabsorption of calcium from the renal tubule, excretion of phosphorus in the urine, and conversion of vitamin D from it’s inactive to active form. The first step in production of this active form of vitamin D, 1,25 dihydroxy vitamin D (calcitriol), occurs in the liver where dietary vitamin D is hydroxylated to 25­hydroxy vitamin D. The final step in formation of calcitriol is 1α­hydroxylation, which takes place in the kidney under control of PTH. Calcitriol then increases absorption of calcium from the intestines. The net effect of PTH secretion is to increase serum calcium and decrease serum phosphate. HYPOCALCEMIC DISORDERS A normal serum calcium concentration varies with age. It is approximately 8.8–10.2 mg/dL in children and young adults. Preterm infants may be as low as 7 mg/dL. Fifty to sixty percent of calcium in the serum is protein­bound and metabolically inactive. Thus, measurement of ionized serum calcium, the metabolically active form, is helpful if serum proteins are low or in conditions such as acidosis that cause abnormal calcium binding to protein. ESSENTIALS OF DIAGNOSIS & TYPICAL FEATURES Tetany with facial and extremity numbness, tingling, cramps, spontaneous muscle contractures, carpopedal spasm, positive Trousseau and Chvostek signs, loss of consciousness, and convulsions. Diarrhea, prolongation of electrical systole (QT interval), and laryngospasm. In hypoparathyroidism or pseudohypoparathyroidism (PHP): defective nails and teeth, cataracts, and ectopic calcification in the subcutaneous tissues and basal ganglia. General Considerations Hypocalcemia results from an imbalance of calcium absorption, excretion, and distribution. It may be associated with rickets in patient’s whose Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 epiphyses34: have not yet fused. Causes of hypocalcemia include the following: Page 21 / 53 Chapter Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility Nutritional calcium deficiency tissues and basal ganglia. University of Medicine and Pharmacy at HCMC Access Provided by: General Considerations Hypocalcemia results from an imbalance of calcium absorption, excretion, and distribution. It may be associated with rickets in patient’s whose epiphyses have not yet fused. Causes of hypocalcemia include the following: Nutritional calcium deficiency Hypoparathyroidism Vitamin D deficiency Hyperphosphatemia (eg, rhabdomyolysis, tumor lysis syndrome, etc) Activating mutation of calcium­sensing receptor (hypercalciuric hypocalcemia) Hypomagnesemia Hypoalbuminemia (eg, nephrotic syndrome) Drugs (eg, diuretics, chemotherapy, transfusion products) Rickets is a disorder that result from decreased bone mineralization due to deficiencies of calcium and/or phosphate. It is characterized by genu varum, prominent costochondral junctions (rachitic rosary), enlarged wrists, frontal bossing, craniotabes, and delayed closure of the fontanelles. Vitamin D deficiency, caused by lack of sunlight exposure or dietary deficiency, is the most common cause of rickets. High rates of occult vitamin D deficiency formed the basis for the 2008 recommendation by the American Academy of Pediatrics that breast­fed infants receive vitamin D supplementation of at least 400 IU/day. Another form, familial hypophosphatemic rickets, is due to abnormal renal phosphate loss related to abnormal fibroblast growth factor 23 (FGF23) regulation. Causes and features of the forms of rickets are outlined in Table 34–5. Table 34–5. Hypocalcemia associated with rickets. Initial Biochemical Findings Condition Pathogenesis Disease Clinical States/Inheritance Features Serum Serum Calcium Phosphorus Vitamin D­ Deficient dietary May cluster in families Characteristic Normal Low or deficiency rickets vitamin D, vitamin D due to shared risk skeletal changes until late normal malabsorption; factors appear early, in course other risk factors poor growth, include dark skin symptomatic and lack of sunlight hypocalcemia is a exposure late finding Serum Alkaline Other Phosphatase Elevated Elevated PTH levels, low 25­OH vitamin D Vitamin D 1α­ Mutation in 1­ Autosomal recessive Skeletal changes hydroxylase hydroxylase inheritance of rickets, Low Low or Elevated deficiency enzyme required for symptomatic 1,25­OH synthesis of fully hypocalcemia vitamin D normal Elevated PTH, low active 1,25­OH vitamin D Vitamin D Mutation in 1,25­OH Autosomal recessive Severe skeletal resistance vitamin D receptor inheritance changes of Low Low or Elevated normal rickets, total Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 alopecia, Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu symptomatic ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility hypocalcemia Elevated PTH, elevated 1,25­OH Page 22 / 53 vitamin D Vitamin D deficiency, caused by lack of sunlight exposure or dietary deficiency, is the most common cause of rickets. High rates of occult vitamin D University of Medicine and Pharmacy at HCMC deficiency formed the basis for the 2008 recommendation by the American Academy of Pediatrics that breast­fed infants receive vitamin D Access Provided by: supplementation of at least 400 IU/day. Another form, familial hypophosphatemic rickets, is due to abnormal renal phosphate loss related to abnormal fibroblast growth factor 23 (FGF23) regulation. Causes and features of the forms of rickets are outlined in Table 34–5. Table 34–5. Hypocalcemia associated with rickets. Initial Biochemical Findings Condition Pathogenesis Disease Clinical States/Inheritance Features Serum Serum Calcium Phosphorus Vitamin D­ Deficient dietary May cluster in families Characteristic Normal Low or deficiency rickets vitamin D, vitamin D due to shared risk skeletal changes until late normal malabsorption; factors appear early, in course other risk factors poor growth, include dark skin symptomatic and lack of sunlight hypocalcemia is a exposure late finding Serum Alkaline Other Phosphatase Elevated Elevated PTH levels, low 25­OH vitamin D Vitamin D 1α­ Mutation in 1­ Autosomal recessive Skeletal changes hydroxylase hydroxylase inheritance of rickets, Low Low or Elevated deficiency enzyme required for symptomatic 1,25­OH synthesis of fully hypocalcemia vitamin D normal Elevated PTH, low active 1,25­OH vitamin D Vitamin D Mutation in 1,25­OH Autosomal recessive Severe skeletal resistance vitamin D receptor inheritance changes of Low Low or Elevated normal Elevated PTH, rickets, total elevated alopecia, 1,25­OH symptomatic vitamin D hypocalcemia Hypophosphatemic Excessive loss of X­linked dominant Skeletal changes Normal rickets phosphate in the due to PHEX primarily in the or low Very low Usually high Normal urine activation or lower extremities initially, Decreased autosomal dominant —genu varum or abnormally fibroblast growth due to FGF23 valgus, short high factor 23 (FGF23) mutations stature urinary PTH levels activity phosphate excretion Deficient PTH secretion may be due to deficient parathyroid tissue (DiGeorge syndrome), autoimmunity, or sometimes, magnesium deficiency. Decreased PTH action may be due to magnesium deficiency, vitamin D deficiency, or defects in the PTH receptor (eg, pseudohypoparathyroidism). Occasionally, PTH deficiency is idiopathic. Table 34–6 summarizes the clinical and laboratory characteristics of disorders of PTH secretion and action. Table 34–6. Hypocalcemia associated with disorders of parathyroid hormone secretion or action. Initial Biochemical Findingsa Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 Condition Pathogenesis Inheritance Pattern Clinical Features Serum Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Stephanie Hsu Serum Davis; Serum Alkaline ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility Calcium Phosphorus Phosphatase Page 23 / 53 Serum PTH Table 34–6. University of Medicine and Pharmacy at HCMC Hypocalcemia associated with disorders of parathyroid hormone secretion or action. Access Provided by: Initial Biochemical Findingsa Condition Pathogenesis Acquired isolated Trauma, surgical hypoparathyroidism destruction, iron Inheritance Pattern None known Clinical Features Symptoms of Serum Serum Calcium Phosphorus Low High Serum Alkaline Phosphatase Normal or low hypocalcemia Serum PTH Low, low 1,25­OH overload, vitamin isolated D autoimmune destruction Familial Isolated Mutations in Autosomal recessive Symptoms of hypoparathyroidism GCMB, PTH gene, (GCMB, PTH gene) or hypocalcemia preproPTH gene Autosomal dominant vitamin (preproPTH gene) D DiGeorge syndrome APS type 1 Low High Normal or low Low, low 1,25­OH Deletion in Majority represent new Symptoms of chromosome 22 mutations hypocalcemia, 1,25­OH cardiac anomalies, vitamin immune disorder D Autoimmune Autosomal recessive destruction Mucocutaneous Low Low High High Normal or low Normal or low Low, low Low, low candidiasis, Addison 1,25­OH disease; potential for vitamin autoimmune D destruction in other endocrine glands PHP type IA Mutation in Autosomal dominant AHO phenotype, Low or Elevated or Variable Very stimulatory G short stature, normal normal protein; variable low 1,25­ resistance to PTH hypocalcemia, may OH action have resistance to vitamin other hormones D elevated, using G protein signaling PPHP Mutation in Autosomal dominant— AHO phenotype, stimulatory G frequently found biochemical protein within same families parameters are with PHP type IA normal Transient neonatal Deficiency in PTH Sporadic—associated Onset of symptoms hypoparathyroidism secretion or with birth asphyxia, of hypocalcemia —early action infants of diabetic within 2 wk of birth Normal Normal Normal Normal Low Normal or Normal or low Normal low or low, low 1,25­ mothers, or maternal OH hyperparathyroidism vitamin D Transient neonatal Deficiency in PTH Sporadic—associated Onset of symptoms Low Normal or Normal or low Downloaded 2023­10­12 2:52 A Your hypoparathyroidism secretion or IP is 13.213.160.179 with infant formulas of hypocalcemia low Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu —late onset action that have a high after 2 wk of age ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility phosphate content Normal or low, Page 24 / 53 low 1,25­ OH vitamin —early action infants of diabetic within 2 wk of birth low 1,25­ mothers, or maternal University of Medicine and Pharmacy OH at HCMC hyperparathyroidism Access Provided by: vitamin D Transient neonatal Deficiency in PTH Sporadic—associated Onset of symptoms hypoparathyroidism secretion or with infant formulas of hypocalcemia —late onset action that have a high after 2 wk of age Low Normal or Normal or low low Normal or low, low 1,25­ phosphate content OH vitamin D Familial Gain of hypercalciuric functional Autosomal dominant Symptoms of hypocalcemia, family Low High Normal or low 1,25­OH hypocalcemia mutation of history vitamin calcium­sensing Low, low D receptor AHO, Albright hereditary osteodystrophy; APS, autoimmune polyglandular syndrome; PHP, pseudohypoparathyroidism; PPHP, pseudo­ pseudohypoparathyroidism; PTH, parathyroid hormone. aUrinary calcium excretion (calcium­creatinine ratio) is low in all but familial hypercalciuric hypocalcemia. Autoimmune parathyroid destruction with subsequent hypoparathyroidism may be isolated, or associated with other autoimmune disorders in the APECED (autoimmune polyendocrinopathy­candidiasis­ectodermal dystrophy, or APS­1) syndrome. Hypoparathyroidism may also be secondary to manipulation of the blood supply of the parathyroid glands or removal of the parathyroid glands during thyroidectomy. Autosomal dominant hypocalcemia, also called familial hypercalciuric hypocalcemia, is associated with a gain­of­function mutation in the calcium­sensing receptor, which causes a low serum PTH despite hypocalcemia, and excessive urinary loss of calcium. A family history of hypocalcemia may be the clue that differentiates this condition from other causes of hypocalcemia. Transient neonatal hypoparathyroidism is caused both by a relative deficiency of PTH secretion and PTH action (see Table 34–6). The late form of transient neonatal hypoparathyroidism (after 2 weeks of age) occurs in infants receiving high­phosphate formulas (whole cow’s milk is a well­known example) due to intestinal calcium­phosphate binding, resulting in decreased absorption of intestinal calcium. Clinical Findings A. Symptoms and Signs Prolonged hypocalcemia from any cause is associated with tetany, photophobia, blepharospasm, and diarrhea. Symptoms of tetany include numbness, muscle cramps, twitching of the extremities, carpopedal spasm, and laryngospasm. Tapping the face in front of the ear causes facial spasms (Chvostek sign), and inflation of a sphygmomanometer above systolic blood pressure causes a carpal spasm (Trousseau’s sign). Some patients with hypocalcemia exhibit bizarre behavior, irritability, loss of consciousness, and convulsions. Electrocardiogram may demonstrate prolonged QTc. Headache, vomiting, increased intracranial pressure, and papilledema may occur. In early infancy, respiratory distress may be a presenting finding. B. Laboratory Findings Tables 34–5 and 34–6 outline the specific laboratory findings in various causes of hypocalcemia (Shaw, 2015). It is important to obtain the samples at the time of hypocalcemia. Critical diagnostic samples typically include serum calcium, phosphate, magnesium, intact parathyroid hormone, 25­ hydroxyvitamin D, 1,25­dihydroxyvitamin D. Measurement of urinary excretion of calcium (calcium­creatinine ratio) can also assist in the diagnosis of calcium disorders. C. Imaging Soft tissue and basal ganglia calcification may occur in idiopathic hypoparathyroidism and PHP. Various skeletal changes are associated with rickets, including cupped and irregular long bone metaphyses. Torsional deformities can result in genu varum (bowleg). Accentuation of the costochondral junction gives the rachitic rosary appearance seen on the chest wall. Downloaded Differential 2023­10­12 Diagnosis 2:52 A Your IP is 13.213.160.179 Page 25 / 53 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility Tables 34–5 and 34–6 outline the features of disorders associated with hypocalcemia. In individuals with hypoalbuminemia, the total serum calcium may be low and yet the functional serum ionized calcium is normal. Ionized calcium is the test of choice for hypocalcemia in patients with low serum C. Imaging University of Medicine and Pharmacy at HCMC Soft tissue and basal ganglia calcification may occur in idiopathic hypoparathyroidism and PHP. Various skeletal changes are associated with rickets, Access Provided by: including cupped and irregular long bone metaphyses. Torsional deformities can result in genu varum (bowleg). Accentuation of the costochondral junction gives the rachitic rosary appearance seen on the chest wall. Differential Diagnosis Tables 34–5 and 34–6 outline the features of disorders associated with hypocalcemia. In individuals with hypoalbuminemia, the total serum calcium may be low and yet the functional serum ionized calcium is normal. Ionized calcium is the test of choice for hypocalcemia in patients with low serum albumin. Treatment A. Acute or Severe Tetany Symptomatic patients are treated acutely by administration of a 10% calcium gluconate infusion at a dose of 1–2 mL/kg (9 mg of elemental calcium/mL) over 5–10 minutes. Calcium gluconate is preferred over calcium chloride since it is less likely to cause tissue necrosis if extravasated. Intravenous calcium infusions should not exceed 50 mg/min because of possible cardiac arrhythmia. Cardiac monitoring should be performed during calcium infusion. Rise in serum calcium is limited to about 2–3 hours after an intravenous calcium bolus infusion, therefore the bolus will need to be followed by oral or continuous calcium infusions if hypocalcemia persists. Given these risks and limitations of intravenous calcium, it is recommended to transition to oral calcium supplementation as soon as patient is no longer symptomatic. B. Maintenance Management of Hypoparathyroidism or Chronic Hypocalcemia The objective of treatment is to maintain the serum calcium and phosphate at near­normal levels without excess urinary calcium excretion. 1. Diet Calcium supplementation should start at a dose of 50–75 mg/kg/day of elemental calcium divided in three to four doses. Supplemental calcium can often be discontinued in patients with rickets after vitamin D therapy has stabilized. 2. Vitamin D supplementation Ergocalciferol (vitamin D2) and cholecalciferol (vitamin D3) are the most commonly used oral vitamin D preparations. Cholecalciferol is slightly more active than ergocalciferol. Calcitriol (1,25­dihydroxy vitamin D3) supplementation is only recommended for impaired metabolism of dietary vitamin D to 25­OH vitamin D as seen in hepatic dysfunction, impaired metabolism to its active end product, 1,25­dihydroxy vitamin D, or impaired PTH function. Selection and dosage of vitamin D supplements varies with the underlying condition and the response to therapy. 3. Monitoring Dosage of calcium and vitamin D must be tailored for each patient. Monitoring serum calcium, urine calcium, and serum alkaline phosphatase levels at 1­ to 3­month intervals is necessary to ensure adequate therapy and to prevent hypercalcemia, hypercalciuria/nephrocalcinosis and vitamin D toxicity. The major goals of monitoring in vitamin D deficiency are to ensure: (1) maintenance of serum calcium and phosphorus concentrations within normal ranges, (2) normalization of alkaline phosphatase activity for age, (3) regression of skeletal changes, and (4) maintenance of an age­appropriate urine calcium­creatinine ratio. The urine calcium­creatinine ratio should be less than 0.8 in newborns, 0.3–0.6 in children, and less than 0.2 in adolescents (when using creatinine and calcium measured in mg/dL). Monitoring goals are somewhat different in hypophosphatemic rickets. Serum calcium and alkaline phosphatase, and urinary calcium to creatinine ratio should be maintained within normal limits. Monitoring of serum PTH is necessary to ensure that secondary hyperparathyroidism does not develop from excessive phosphate treatment or inadequate calcitriol replacement. PSEUDOHYPOPARATHYROIDISM (RESISTANCE TO PARATHYROID HORMONE ACTION) In pseudohypoparathyroidism (PHP), PTH production is adequate, but target organs (renal tubule, bone, or both) fail to respond because of receptor resistance. Resistance to PTH action is due to a heterozygous inactivating mutation in the stimulatory G protein subunit associated with the PTH receptor, which leads to impaired signaling. Resistance to other G protein­dependent hormones, such as TSH, GHRH, and follicle­stimulating hormone (FSH)/luteinizing hormone2:52 (LH),Amay also Downloaded 2023­10­12 Your IPbe is present. 13.213.160.179 Page 26 / 53 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu There severalHill. types PHP with variable Terms biochemical phenotypic (see Table 34–6). Biochemical abnormalities in PHP (hypocalcemia ©2023are McGraw AllofRights Reserved. of Useand • Privacy Policyfeatures • Notice • Accessibility and hyperphosphatemia) are similar to those seen in hypoparathyroidism, but the PTH levels are elevated. PHP may be accompanied by a characteristic phenotype known as Albright hereditary osteodystrophy (AHO), which includes short stature; round, full facies; irregularly shortened PSEUDOHYPOPARATHYROIDISM (RESISTANCE TO PARATHYROID HORMONE ACTION) University of Medicine and Pharmacy at HCMC Access Provided by: In pseudohypoparathyroidism (PHP), PTH production is adequate, but target organs (renal tubule, bone, or both) fail to respond because of receptor resistance. Resistance to PTH action is due to a heterozygous inactivating mutation in the stimulatory G protein subunit associated with the PTH receptor, which leads to impaired signaling. Resistance to other G protein­dependent hormones, such as TSH, GHRH, and follicle­stimulating hormone (FSH)/luteinizing hormone (LH), may also be present. There are several types of PHP with variable biochemical and phenotypic features (see Table 34–6). Biochemical abnormalities in PHP (hypocalcemia and hyperphosphatemia) are similar to those seen in hypoparathyroidism, but the PTH levels are elevated. PHP may be accompanied by a characteristic phenotype known as Albright hereditary osteodystrophy (AHO), which includes short stature; round, full facies; irregularly shortened fourth metacarpal; a short, thick­set body; delayed and defective dentition; and mild intellectual disability. Corneal and lenticular opacities and ectopic calcification of the basal ganglia and subcutaneous tissues (osteoma cutis) may occur with or without abnormal serum calcium levels. Treatment includes calcium and calcitriol supplementation. Clarke B et al: Epidemiology and diagnosis of hypoparathyroidism. J Clin Endocrinol Metab 2016 Jun;101(6):2284–2299 [PubMed: 26943720] . Elder CJ, Bishop NJ: Rickets [Review]. Lancet 2014;383:1665–1676 [PubMed: 24412049] . Shaw N: A practical approach to hypocalcaemia in children [Review]. Endocr Dev 2015;28:84–100 [PubMed: 26138837] . HYPERCALCEMIC STATES Hypercalcemia is defined as a serum calcium concentration greater than 11 mg/dL. Severe hypercalcemia is a concentration greater than 13.5 mg/dL. ESSENTIALS OF DIAGNOSIS & TYPICAL FEATURES Abdominal pain, polyuria, polydipsia, hypertension, nephrocalcinosis, failure to thrive, renal stones, intractable peptic ulcer, constipation, uremia, and pancreatitis. Bone pain or pathologic fractures, subperiosteal bone resorption, renal parenchymal calcification or stones, and osteitis fibrosa cystica. Impaired concentration, altered mental status, mood swings, and coma. General Considerations Hypercalcemia is less common in children than in adults and etiology varies by age. Table 34–7 summarizes the differential diagnosis of childhood hypercalcemia. Table 34–7. Hypercalcemic states. A. Primary hyperparathyroidism 1. Parathyroid hyperplasia 2. Parathyroid adenoma 3. Familial, including MEN types 1 and 2 4. Ectopic PTH secretion 5. Maternal hypoparathyroidism B. Other hypercalcemic states resulting from increased intestinal or renal absorption of calcium 1. Hypervitaminosis D (including idiopathic hypercalcemia of infancy) 2. Familial hypocalciuric hypercalcemia 3. Lithium therapy Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 4. Sarcoidosis Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu 5. Phosphate depletion ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility 6. Aluminum intoxication 7. Subcutaneous fat necrosis (due to vitamin D activation) Page 27 / 53 General Considerations University of Medicine and Pharmacy at HCMC Access Provided by: Hypercalcemia is less common in children than in adults and etiology varies by age. Table 34–7 summarizes the differential diagnosis of childhood hypercalcemia. Table 34–7. Hypercalcemic states. A. Primary hyperparathyroidism 1. Parathyroid hyperplasia 2. Parathyroid adenoma 3. Familial, including MEN types 1 and 2 4. Ectopic PTH secretion 5. Maternal hypoparathyroidism B. Other hypercalcemic states resulting from increased intestinal or renal absorption of calcium 1. Hypervitaminosis D (including idiopathic hypercalcemia of infancy) 2. Familial hypocalciuric hypercalcemia 3. Lithium therapy 4. Sarcoidosis 5. Phosphate depletion 6. Aluminum intoxication 7. Subcutaneous fat necrosis (due to vitamin D activation) 8. Premature infant on human milk or standard formula C. Other hypercalcemic states 1. Hyperthyroidism 2. Immobilization 3. Lithium and Thiazides 4. Vitamin A intoxication 5. Adrenal insufficiency 6. Hypophosphatasia 7. Genetic syndromes a. William syndrome b. IMAGe syndrome c. Blue diaper syndrome d. Jansen metaphyseal chondrodysplasia 8. Malignant neoplasms a. Ectopic PTH secretion or PTH­related protein (PTHRP) b. Prostaglandin­secreting tumors c. Tumors metastatic to bone d. Myeloma MEN, multiple endocrine neoplasia; PTH, parathyroid hormone. Hyperparathyroidism is rare in childhood and may be primary or secondary. The most common cause of primary hyperparathyroidism is due to a single parathyroid adenoma. Familial hyperparathyroidism may be an isolated disease, or it may be associated with MEN type 1, or rarely type 2A. Hypercalcemia of malignancy is associated with solid and hematologic malignancies and is due either to local destruction of bone by tumor or to ectopic secretion of PTH­related protein (PTHrP). When ectopic PTHrP is present, calcium is elevated, serum PTH is suppressed, and serum PTHrP is elevated. Chronic renal disease with impaired phosphate excretion is the most common cause of secondary hyperparathyroidism. Clinical Findings A. Symptoms and Signs 1. Due to hypercalcemia Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 Chapter 34: Endocrine Disorders, Sarah Bartz; weakness; Christine M. Chan;mood Melanie Cree­Green; Shanlee Davis; Stephanie Hsuabdominal pain,Page 28 / 53 Manifestations include hypotonicity and muscle apathy, swings, and bizarre behavior; nausea, vomiting, ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility constipation, and weight loss; hyperextensibility of joints; and hypertension, cardiac irregularities, bradycardia, and shortening of the QT interval. Coma rarely occurs. Calcium deposits occur in the cornea or conjunctiva (band keratopathy) and are detected by slit­lamp examination. Intractable elevated. Chronic renal disease with impaired phosphate excretion is the most common cause of secondary hyperparathyroidism. University of Medicine and Pharmacy at HCMC Clinical Findings Access Provided by: A. Symptoms and Signs 1. Due to hypercalcemia Manifestations include hypotonicity and muscle weakness; apathy, mood swings, and bizarre behavior; nausea, vomiting, abdominal pain, constipation, and weight loss; hyperextensibility of joints; and hypertension, cardiac irregularities, bradycardia, and shortening of the QT interval. Coma rarely occurs. Calcium deposits occur in the cornea or conjunctiva (band keratopathy) and are detected by slit­lamp examination. Intractable peptic ulcer and pancreatitis occur in adults but rarely in children. 2. Due to Increased calcium and phosphate excretion Loss of renal concentration causes polyuria, polydipsia, and calcium phosphate deposition in renal parenchyma or as urinary calculi resulting in progressive renal damage. 3. Due to changes in the skeleton Initial findings include bone pain, osteitis fibrosa cystica, subperiosteal bone absorption in the distal clavicles and phalanges, absence of lamina dura around the teeth, spontaneous fractures, and moth­eaten appearance of the skull on radiographs. Later, there is generalized demineralization. B. Imaging Bone changes may be subtle in children. Technetium sestamibi scintigraphy is preferred over conventional procedures (ultrasound, computed tomography, and MRI) for localizing parathyroid tumors. Treatment A. Symptomatic Initial management is vigorous hydration with normal saline to rehydrate the patient, dilute serum calcium concentration, and to promote urinary calcium excretion. Loop diuretic can increase urinary calcium excretion but may exacerbate intravascular volume contraction so should be used with caution. If response is inadequate, glucocorticoids or calcitonin may be used. Bisphosphonates, standard agents for the management of acute hypercalcemia in adults, are being used more often in refractory pediatric hypercalcemia. B. Chronic Treatment options vary with the underlying cause. Resection of parathyroid adenoma or subtotal removal of hyperplastic parathyroid glands is the preferred treatment. Postoperatively, hypocalcemia due to the rapid remineralization of chronically calcium­deprived bones may occur (hungry bone syndrome). A diet high in calcium and vitamin D is recommended immediately postoperatively and is continued until serum calcium concentrations are normal and stable. Treatment of secondary hyperparathyroidism from chronic renal disease is primarily directed at controlling serum phosphorus levels with phosphate binders and pharmacologic doses of calcitriol are used to suppress PTH secretion. Long­term therapy for hypercalcemia of malignancy is the treatment of the underlying disorder. FAMILIAL HYPOCALCIURIC HYPERCALCEMIA (FAMILIAL BENIGN HYPERCALCEMIA) Familial hypocalciuric hypercalcemia is characterized by slightly elevated serum calcium, low urine calcium, and normal (or slightly elevated) PTH. In most cases, the genetic defect is an inactivating mutation in the membrane­bound calcium­sensing receptor expressed on parathyroid and renal tubule cells. It is inherited as an autosomal dominant trait with high penetrance. There is a low rate of new mutations. Most patients are asymptomatic, and treatment is unnecessary. However, a severe form of symptomatic neonatal hyperparathyroidism may occur in infants homozygous for the receptor mutation. HYPERVITAMINOSIS D Vitamin D intoxication is almost always the result of ingestion of excessive amounts of vitamin D. Signs and symptoms of vitamin D­induced hypercalcemia are the same as those in other hypercalcemic conditions. Treatment depends on the severity of hypercalcemia and initial treatment is similar to other hypercalcemic states. However, due to the storage of vitamin D in the adipose tissue, several months of a low­calcium, low­vitamin D diet may also 2023­10­12 be required. 2:52 A Your IP is 13.213.160.179 Downloaded Page 29 / 53 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility WILLIAMS SYNDROME Williams syndrome is an uncommon disorder of infancy characterized by elfin­appearing facies and hypercalcemia in infancy. Other features include HYPERVITAMINOSIS D University of Medicine and Pharmacy at HCMC Access Provided by: Vitamin D intoxication is almost always the result of ingestion of excessive amounts of vitamin D. Signs and symptoms of vitamin D­induced hypercalcemia are the same as those in other hypercalcemic conditions. Treatment depends on the severity of hypercalcemia and initial treatment is similar to other hypercalcemic states. However, due to the storage of vitamin D in the adipose tissue, several months of a low­calcium, low­vitamin D diet may also be required. WILLIAMS SYNDROME Williams syndrome is an uncommon disorder of infancy characterized by elfin­appearing facies and hypercalcemia in infancy. Other features include failure to thrive, mental and motor impairment, cardiovascular abnormalities (primarily supravalvular aortic stenosis), irritability, purposeless movements, constipation, hypotonia, polyuria, polydipsia, and hypertension. A gregarious and affectionate personality is often seen in children with the syndrome. Hypercalcemia may not appear until several months after birth. Treatment consists of restriction of dietary calcium and vitamin D (Calcilo formula) and, in severe cases, moderate doses of glucocorticoids or even bisphosphonates. A defect in the metabolism of, or increased responsiveness to, vitamin D is postulated as the cause of Williams syndrome. The risk of hypercalcemia generally resolves by age 4. IMMOBILIZATION HYPERCALCEMIA Abrupt immobilization, particularly in a rapidly growing adolescent, may cause hypercalcemia and hypercalciuria. Abnormalities often appear 1–3 weeks after immobilization. The mechanism is not fully understood but is thought to result from increased osteoclastic activity and reduced osteoblastic activity. Medical or dietary intervention may be required in severe cases. HYPOPHOSPHATASIA Hypophosphatasia is a rare autosomal recessive condition characterized by deficiency of alkaline phosphatase activity in serum, bone, and tissues, resulting from mutations in the gene for tissue­nonspecific isozyme of alkaline phosphatase (TNSALP). Enzyme deficiency leads to poor skeletal mineralization with clinical and radiographic features similar to rickets. Severity ranges from severe skeletal deformity and perinatal death to milder skeletal findings (including craniosynostosis), reduced bone mineral density, and motor delays. Serum calcium levels may be elevated. The diagnosis of hypophosphatasia is made by demonstrating elevated urinary phosphoethanolamine associated with low serum alkaline phosphatase. Enzyme­ replacement therapy has recently been approved and shows promise for improved prognosis. Belcher R et al: Characterization of hyperparathyroidism in youth and adolescents: a literature review. Int J Pediatr Otorhinolaryngol 2013 Mar;77(3):318–322 [PubMed: 23313432] . Stokes V et al: Hypercalcemic disorders in children. J Bone Miner Res 2017 Nov;32(11):2157–2170 [PubMed: 28914984] . GONADS (OVARIES & TESTES) DEVELOPMENT Sex development is a complex process beginning with the differentiation of the bipotential gonad into either a testis or ovary. In an infant with a Y chromosome, expression of the transcription factor SRY initiates a cascade of gene expression that directs the formation of testes. Without expression of SRY, ovaries develop; however, a 46,XX complement of chromosomes, in addition to several unique genes, is necessary for the development of normal ovaries. Secretion of testosterone and antimüllerian hormone (AMH) by the testes results in the development of male internal ducts (epididymis, seminal vesicle, and vas deferens) and regression of the müllerian ducts, which are the precursors of the female internal genital structures (fallopian tubes, uterus, and vagina) (Figure 34–6). Figure 34–6. Differentiation of internal reproductive ducts. (Reproduced with permission from Kronenberg H: Williams Textbook of Endocrinology, 11th ed. Philadelphia, PA: Saunders/Elsevier; 2008.) Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility Page 30 / 53 Figure 34–6. University of Medicine and Pharmacy at HCMC Access Provided by: Differentiation of internal reproductive ducts. (Reproduced with permission from Kronenberg H: Williams Textbook of Endocrinology, 11th ed. Philadelphia, PA: Saunders/Elsevier; 2008.) The external genitalia develop from sexually indifferent structures called the genital tubercle, the urethral folds, and the labioscrotal swellings (Figure 34–7). Development of typical male external genitalia depends on an adequate circulating concentration of testosterone and its metabolite dihydrotestosterone (DHT). Sexual differentiation of the external genitalia is completed at about 12 weeks of gestation. Figure 34–7. Differentiation of external genitalia ducts. (Adapted with permission from Spaulding MH: The development of the external genitalia in the human embryo. Contrib Embryol 1921;13:69–88.) Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility Page 31 / 53 Figure 34–7. University of Medicine and Pharmacy at HCMC Access Provided by: Differentiation of external genitalia ducts. (Adapted with permission from Spaulding MH: The development of the external genitalia in the human embryo. Contrib Embryol 1921;13:69–88.) DISORDERS OF SEXUAL DEVELOPMENT Disorders of sex development (DSD) can arise from alterations in three main processes: gonadal differentiation, steroidogenesis, or androgen action. Many DSDs will be evident in the newborn period, but some will not manifest until later with abnormal pubertal development. In disorders of gonadal differentiation, the testes or ovaries do not develop normally, which results in either ambiguous genitalia or sex reversal. As an example, individuals with 46,XY complete gonadal dysgenesis do not develop normal gonadal tissue (ie, have streak gonads), and this results in typical female internal and external reproductive structures. XY partial gonadal dysgenesis is associated with incomplete testes development and usually results in a phenotype of ambiguous genitalia. Mutations in genes important for gonadal differentiation have been demonstrated in many patients with both complete and partial gonadal dysgenesis. Mixed gonadal dysgenesis is usually due to presence of both 45,XO and 46,XY cell lines in the same individual. There is typically a testis on one side and a streak gonad on the contralateral side. Ovotesticular DSD occurs when there is both ovarian and testicular tissue. Steroidogenesis refers to steroid hormone biosynthesis and depends on the function of multiple enzymes (Figure 34–8). Enzymatic defects in this pathway can result in decreased or absent testosterone synthesis and in affected XY individuals, there will be reduced or lack of androgen effects resulting in ambiguous genitalia. Since the gonad and adrenal gland share common enzymes of steroid hormone production, some of the enzymatic defects associated with male undervirilization may also affect production of cortisol and aldosterone, leading to cortisol deficiency and salt wasting. Deficiency of 21­hydroxylase, an enzyme in the cortisol and aldosterone pathways, leads to overproduction of adrenal androgens and the most common form of congenital adrenal hyperplasia. In the classic salt­losing form of this disorder, 46,XX infants present with genital ambiguity due to the excess of adrenal androgen production, but have normal uterus and ovaries. Figure 34–8. Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 Page 32 / 53 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu The corticosteroid hormone synthetic pathway. Theofpathways illustrated present in differing amounts in the steroid­producing tissues: adrenal ©2023 McGraw Hill. All Rights Reserved. Terms Use • Privacy Policyare • Notice • Accessibility glands, ovaries, and testes. In the adrenal glands, mineralocorticoids from the zona glomerulosa, glucocorticoids from the zona fasciculata, and androgens (and estrogens) from the zona reticularis are produced. The major adrenal androgen is androstenedione, because the activity of 17­ defects associated with male undervirilization may also affect production of cortisol and aldosterone, leading to cortisol deficiency and salt wasting. University of Medicine andand Pharmacy at HCMC Deficiency of 21­hydroxylase, an enzyme in the cortisol and aldosterone pathways, leads to overproduction of adrenal androgens the most Access Provided by: common form of congenital adrenal hyperplasia. In the classic salt­losing form of this disorder, 46,XX infants present with genital ambiguity due to the excess of adrenal androgen production, but have normal uterus and ovaries. Figure 34–8. The corticosteroid hormone synthetic pathway. The pathways illustrated are present in differing amounts in the steroid­producing tissues: adrenal glands, ovaries, and testes. In the adrenal glands, mineralocorticoids from the zona glomerulosa, glucocorticoids from the zona fasciculata, and androgens (and estrogens) from the zona reticularis are produced. The major adrenal androgen is androstenedione, because the activity of 17­ ketoreductase is relatively low. The adrenal gland does secrete some testosterone and estrogen, however. The pathways leading to the synthesis of mineralocorticoids and glucocorticoids are not present to any significant degree in the gonads; however, the testes and ovaries each produce both androgens and estrogens. Further metabolism of testosterone to dihydrotestosterone occurs in target tissues of the action of the enzyme 5α­ reductase. DHEA, dehydroepiandrosterone. Disorders of androgen action include the diagnosis of androgen insensitivity syndrome (AIS) which is caused by an inactivating mutation in the androgen receptor gene located on the proximal long arm of the X chromosome. In complete AIS (CAIS), there is no androgen action; thus, 46,XY affected individuals have normal appearing female external genitalia with a short vagina, absent müllerian structures and absence or rudimentary wolffian structures. Gonads are located either intra­abdominally or in the inguinal canal. Many of these individuals present when surgery for an inguinal hernia reveals a testis in the hernia sack. With partial AIS (PAIS), the degree of virilization and ambiguity depends on the degree of abnormality in androgen binding. Evaluation On physical examination, dysmorphic features and other congenital anomalies should be noted. The genital examination should include measuring the width and length of the stretched phallus and noting the position of the urethral meatus as well as degree of labioscrotal fusion. The normal stretched penile length (SPL) is greater than 2.0 cm in term male infants. The labioscrotal and inguinal regions should be palpated for presence of gonads. Since ovaries and streak gonads do not typically descend, the presence of a palpable gonad is suggestive of a 46,XY or 45X/46,XY karyotype. In all these infants, laboratory studies should be done within the first 24 hours of life and include a FISH for SRY/X­centromere, chromosomal analysis or microarray, electrolytes, LH, FSH, testosterone, and 17­hydroxyprogesterone. Additional laboratory evaluation is usually based on these results. A pelvic ultrasound can be helpful to evaluate for the presence of a uterus; however, ultrasound findings can be unreliable so should be done in an institution which has expertise in pediatric imaging. Many times, laparoscopic examination is necessary to delineate internal structures. It is important that gender assignment be avoided until expert evaluation by a multidisciplinary team is performed. Ideally this team includes pediatric specialists from endocrinology, urology, gynecology, genetics, psychology, and nursing. The team should develop a plan for diagnosis, gender assignment, and treatment options before making any recommendations. Open communications with the parents is essential and their participation in decision­ making encouraged. Arboleda VA, Sandberg DE, Vilain E: DSDs: genetics, underlying pathologies and psychosocial differentiation. Nat Rev Endocrinol 2014:10(10):603–615 [PubMed: 25091731] . Lambert SM, Vilain EJ, Kolon TF: A practical approach to ambiguous genitalia in the newborn period. Urol Clin N Am 2010;37(2):195–205 Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 [PubMed:34: 20569798] . Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu Page 33 / 53 Chapter Endocrine ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility Ostrer H: Disorders of sex development (DSDs): an update. J Clin Endocrinol Metab 2014;99:1503–1509 [PubMed: 24758178] . making encouraged. University of Medicine and Pharmacy at HCMC Access Provided by: Arboleda VA, Sandberg DE, Vilain E: DSDs: genetics, underlying pathologies and psychosocial differentiation. Nat Rev Endocrinol 2014:10(10):603–615 [PubMed: 25091731] . Lambert SM, Vilain EJ, Kolon TF: A practical approach to ambiguous genitalia in the newborn period. Urol Clin N Am 2010;37(2):195–205 [PubMed: 20569798] . Ostrer H: Disorders of sex development (DSDs): an update. J Clin Endocrinol Metab 2014;99:1503–1509 [PubMed: 24758178] . ABNORMALITIES IN FEMALE PUBERTAL DEVELOPMENT & OVARIAN FUNCTION 1. Precocious Puberty in Girls Precocious puberty is defined as pubertal development occurring below the age limit set for normal onset of puberty. Puberty is considered precocious in girls if the onset of secondary sexual characteristics occurs before age 8 years in Caucasian girls and 7 years for African­American and Hispanic girls. Precocious puberty is more common in girls than in boys. Many girls showing signs of puberty between 6 and 8 years of age have a benign, slowly progressing form that requires no intervention. The age of pubertal onset may be advanced by obesity. Central (gonadotropin­releasing hormone [GnRH]­dependent) precocious puberty (CPP) involves activation of the hypothalamic GnRH pulse generator, an increase in gonadotropin secretion, and a resultant increase in production of sex steroids (Table 34–8). The sequence of hormonal and physical events in central precocious puberty is identical to that of normal puberty. Central precocious puberty in girls is generally idiopathic but may be secondary to a central nervous system (CNS) abnormality that disrupts the prepubertal restraint on the GnRH pulse generator. Such CNS abnormalities include, but are not limited to, hypothalamic hamartomas, CNS tumors, cranial irradiation, hydrocephalus, and trauma. Peripheral precocious puberty (GnRH­independent) occurs independent of gonadotropin secretion. In girls, peripheral precocious puberty can be caused by ovarian or adrenal tumors, ovarian cysts, late­onset congenital adrenal hyperplasia, McCune­Albright syndrome, or exposure to exogenous estrogen. Table 34–8. Causes of precocious pubertal development. A. Central (GnRH­dependent) precocious puberty 1. Idiopathic 2. Central nervous system abnormalities a. Acquired—abscess, chemotherapy, radiation, surgical trauma b. Congenital—arachnoid cyst, hydrocephalus, hypothalamic hamartoma, septo­optic dysplasia, suprasellar cyst c. Tumors—astrocytoma, craniopharyngioma, glioma B. Peripheral (GnRH­independent) precocious puberty 1. Congenital adrenal hyperplasia 2. Adrenal tumors 3. McCune­Albright syndrome 4. Familial male­limited gonadotropin independent precocious puberty 5. Gonadal tumors 6. Exogenous estrogen—oral (contraceptive pills) or topical 7. Ovarian cysts (females) 8. HCG­secreting tumors (eg, hepatoblastomas, choriocarcinomas) (males) GnRH, gonadotropin­releasing hormone; HCG, human chorionic gonadotropin. Clinical Findings A. Symptoms and Signs Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 Female CPP usually starts with breast development, followed by pubic hair growth and menarche. However, the order may vary and girls younger than Page 34 / 53 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu 5©2023 years may not have pubic hair development. Girls with ovarian cysts or tumors generally have signs of estrogen excess such as breast development, McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility vaginal discharge and possibly vaginal bleeding. Adrenal tumors and CAH produce signs of androgen excess which include pubic hair, axillary hair, acne, and increased body odor. Children with precocious puberty usually have accelerated growth and skeletal maturation, and may temporarily be GnRH, gonadotropin­releasing hormone; HCG, human chorionic gonadotropin. University of Medicine and Pharmacy at HCMC Clinical Findings Access Provided by: A. Symptoms and Signs Female CPP usually starts with breast development, followed by pubic hair growth and menarche. However, the order may vary and girls younger than 5 years may not have pubic hair development. Girls with ovarian cysts or tumors generally have signs of estrogen excess such as breast development, vaginal discharge and possibly vaginal bleeding. Adrenal tumors and CAH produce signs of androgen excess which include pubic hair, axillary hair, acne, and increased body odor. Children with precocious puberty usually have accelerated growth and skeletal maturation, and may temporarily be tall for age. However, because skeletal maturation advances at a more rapid rate than linear growth, final adult stature may be compromised. B. Laboratory Findings If the bone age is advanced, further laboratory evaluation is warranted. In CPP, random FSH and LH concentrations may confirm the diagnosis. However, in early central puberty, gonadotropins are secreted overnight and may drop to prepubertal levels during the daytime. If random gonadotropins are in prepubertal range but clinical suspicion remains high for CPP, a GnRH stimulation test is needed with a pubertal LH response indicative of CPP. In peripheral precocious puberty, the LH response to GnRH stimulation is suppressed by the autonomously secreted gonadal steroids (see Figure 34–1). In girls with an ovarian cyst or tumor, estradiol levels will be markedly elevated. In girls who present with pubic and/or axillary hair but no breast development, androgen levels (testosterone, androstenedione, dehydroepiandrosterone sulfate) and 17­ hydroxyprogesterone should be measured. C. Imaging One of the first steps in evaluating a child with early pubertal development is obtaining a radiograph of the left hand and wrist to determine skeletal maturity (bone age). When a diagnosis of central precocious puberty is made, an MRI of the brain should be done to evaluate for CNS lesions. In girls whose laboratory tests suggest peripheral precocious puberty, an imaging of the ovaries and/or adrenal gland may be indicated. Treatment Girls with CPP can be treated with GnRH analogues that downregulate pituitary GnRH receptors and thus decrease gonadotropin secretion. Currently, the two most common GnRH analogues used are (1) leuprolide, which is given as an intramuscular injection at 1, 3, or 6 month intervals or (2) histrelin subdermal implant, which is replaced annually. With treatment, physical changes of puberty regress or cease to progress and linear growth slows to a prepubertal rate. Projected final heights often increase as a result of slowing of skeletal maturation. After stopping therapy, pubertal progression resumes, and ovulation and pregnancy have been documented. Treatment of peripheral precocious puberty is dependent on the underlying cause. In a girl with an ovarian cyst, intervention is generally not necessary, as the cyst usually regresses spontaneously. Serial ultrasounds are recommended to document this regression. Surgical resection and possibly chemotherapy are indicated for the rare adrenal or ovarian tumor. Regardless of the cause of precocious puberty or the medical therapy selected, attention to the psychological needs of the patient and family is essential. 2. Benign Variants of Precocious Puberty Benign premature thelarche (breast development) occurs most commonly in girls younger than 2 years of age. Girls present with isolated breast development without other signs of puberty such as linear growth acceleration and pubic hair development. The breast development is typically present since birth and often waxes and wanes in size. It may be unilateral or bilateral. Treatment is parental reassurance regarding the self­limited nature of the condition. Observation of the child every few months is indicated. Onset of thelarche after age 36 months or in association with other signs of puberty requires evaluation. Benign premature adrenarche (adrenal maturation) is manifested by early development of pubic hair, axillary hair, acne, and/or body odor. Benign premature adrenarche is characterized by normal linear growth and no or minimal bone age advancement. Laboratory tests (see earlier discussion) will differentiate benign premature adrenarche from late­onset CAH and adrenal tumors. It is recognized that approximately 15% of girls with benign premature adrenarche will go on to develop polycystic ovary syndrome. Fuqua J: Treatment and outcomes of precocious puberty: an update. J Clin Endocrinol Metab 2013;98(6):2198–2207 [PubMed: 23515450] . Latronico AC et al: Causes, diagnosis, and treatment of central precocious puberty. Lancet Diabetes Endocrinol 2016;4(3):265–274 Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 [PubMed:34: 26852255] . Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu Chapter Endocrine ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility Utriainen P et al: Premature adrenarche—a common condition with variable presentation. Horm Res Paediatr 2015;83(4):221–231 [PubMed: 25676474] . Page 35 / 53 premature adrenarche will go on to develop polycystic ovary syndrome. University of Medicine and Pharmacy at HCMC Access Provided by: Fuqua J: Treatment and outcomes of precocious puberty: an update. J Clin Endocrinol Metab 2013;98(6):2198–2207 [PubMed: 23515450] . Latronico AC et al: Causes, diagnosis, and treatment of central precocious puberty. Lancet Diabetes Endocrinol 2016;4(3):265–274 [PubMed: 26852255] . Utriainen P et al: Premature adrenarche—a common condition with variable presentation. Horm Res Paediatr 2015;83(4):221–231 [PubMed: 25676474] . 3. Delayed Puberty Delayed puberty in girls should be evaluated if there are no pubertal signs by age 13 years or menarche by 16 years. Primary amenorrhea refers to the absence of menarche, and secondary amenorrhea refers to the absence of menses for at least 6 months after regular menses have been established. The most common cause of delayed puberty is constitutional growth delay (Table 34–9). This growth pattern, characterized by short stature, normal growth velocity, and a delay in skeletal maturation, is described in detail earlier in this chapter. The timing of puberty in children with constitutional growth delay is commensurate to the bone age, not the chronologic age. Girls may also have delayed puberty from any condition that delays growth and skeletal maturation, such as hypothyroidism and GHD. Table 34–9. Causes of delayed puberty or amenorrhea. A. Constitutional growth delay B. Hypogonadism 1. Primary ovarian insufficiency a. Gonadal dysgenesis (Turner syndrome, true gonadal dysgenesis) b. Premature ovarian failure 1. Autoimmune disease 2. Surgery, radiation, chemotherapy c. Galactosemia 2. Central hypogonadism a. Hypothalamic or pituitary tumor, infection, irradiation b. Congenital hypopituitarism c. Kallmann syndrome (hypogonadism plus anosmia) d. Hyperprolactinemia, Cushing’s syndrome, hypothyroidism e. Functional (chronic illness, undernutrition, exercise, hyperprolactinemia) C. Anatomic 1. Müllerian agenesis (Mayer­Rokitansky­Küster­Hauser syndrome) 2. Complete androgen resistance Primary hypogonadism in girls refers to a primary abnormality of the ovaries. The most common diagnosis in this category is Turner syndrome, in which the lack of or an abnormal second X chromosome leads to early loss of oocytes and accelerated stromal fibrosis. Other types of primary ovarian insufficiency include 46,XY gonadal dysgenesis and 46,XX gonadal dysgenesis, galactosemia, autoimmune ovarian failure, radiation, and chemotherapy. Premutation carriers for fragile X syndrome are also at increased risk of premature ovarian failure. Central hypogonadism refers to a hypothalamic or pituitary deficiency of GnRH or FSH/LH, respectively. Central hypogonadism can be functional (reversible), caused by stress, undernutrition, prolactinemia, excessive exercise, or chronic illness. Permanent central hypogonadism is typically associated with conditions that cause multiple pituitary hormone deficiencies, such as congenital hypopituitarism, CNS tumors, or cranial irradiation. Isolated gonadotropin deficiency is rare but may occur in Kallmann syndrome, which is also characterized by hyposmia or anosmia. There are many genes that have been implicated in both isolated gonadotropin deficiency and Kallmann syndrome. In either primary or central hypogonadism, signs of adrenarche are generally still present. Downloaded 2023­10­12 2:52 Aamenorrhea Your IP is 13.213.160.179 Delayed menarche or secondary may result from primary ovarian failure or central hypogonadism, or may be the consequence of Page 36 / 53 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu hyperandrogenism, anatomic obstruction precluding menstrual outflow, or Müllerian agenesis. ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility Clinical Evaluation (reversible), caused by stress, undernutrition, prolactinemia, excessive exercise, or chronic illness. Permanent central hypogonadism is typically associated with conditions that cause multiple pituitary hormone deficiencies, such as congenital hypopituitarism, tumors, orPharmacy cranial irradiation. University of CNS Medicine and at HCMC Isolated gonadotropin deficiency is rare but may occur in Kallmann syndrome, which is also characterized byProvided hyposmia or anosmia. There are many Access by: genes that have been implicated in both isolated gonadotropin deficiency and Kallmann syndrome. In either primary or central hypogonadism, signs of adrenarche are generally still present. Delayed menarche or secondary amenorrhea may result from primary ovarian failure or central hypogonadism, or may be the consequence of hyperandrogenism, anatomic obstruction precluding menstrual outflow, or Müllerian agenesis. Clinical Evaluation The history should ascertain whether and when puberty commenced, level of exercise, nutritional intake, stressors, sense of smell, symptoms of chronic illness, and family history of delayed puberty. Past growth records should be assessed to determine if height and weight velocity have been appropriate. Physical examination includes body proportions, breast and genital development, and stigmata of Turner syndrome. Pelvic examination or pelvic ultrasonography should be considered, especially in girls with primary amenorrhea. A bone age radiograph should be obtained. If the bone age is lower than that consistent with pubertal onset (< 12 years in girls), evaluations should focus on finding the cause of the bone age delay. If short stature and normal growth velocity are present, constitutional growth delay is likely. If growth rate is abnormal, evaluation for causes of growth delay is warranted. Measurement of FSH and LH may not be helpful in the setting of delayed bone age since prepubertal levels are normally low. If the patient has attained a bone age of more than 12 years and there are minimal or no signs of puberty on physical examination, FSH and LH levels will distinguish between primary ovarian failure (elevated FSH/LH) and central hypogonadism (low FSH/LH). If gonadotropins are elevated, a karyotype should be performed to evaluate for Turner syndrome. Central hypogonadism is characterized by low gonadotropin levels, and evaluation is geared toward determining if the hypogonadism is functional or permanent. Laboratory tests should be directed toward identifying chronic disease and hyperprolactinemia. Cranial MRI may be helpful. In girls with adequate breast development and amenorrhea, a progesterone challenge may be helpful to determine if sufficient estrogen is being produced and to evaluate for anatomical defects. Girls who are producing estrogen typically have a withdrawal bleed after 5–10 days of oral progesterone, whereas those who are estrogen­deficient or have an anatomical defect have little or no bleeding. The most common cause of amenorrhea in girls with sufficient estrogen is polycystic ovary syndrome. Girls who are estrogen­deficient should be evaluated similarly to those who have delayed puberty. Treatment Replacement therapy in hypogonadal girls begins with estrogen alone at the lowest available dosage. Oral preparations such as estradiol or topical estrogen patches are used. Estrogen doses are gradually increased every 6 months, and, then 18–24 months later, progesterone is added either cyclically or continuously. Eventually, the patient may change over to an estrogen­progestin combined pill or patch if desired. Progesterone therapy is needed to counteract the effects of estrogen on the uterus, as unopposed estrogen promotes endometrial hyperplasia. Estrogen replacement will also stimulate growth rates but close growth plates and is also necessary to promote bone mineralization and prevent osteoporosis. Nelson LM: Clinical practice: primary ovarian insufficiency. N Engl J Med 2009;360:606 [PubMed: 19196677] . Silvereira LF, Latronico AC: Approach to the patient with hypogonadotropic hypogonadism. J Clin Endocrinol Metab 2013;98:1781–1788 [PubMed: 23650335] . Villanueva C, Argente J: Pathology or normal variant: what constitutes a delay in puberty? Horm Res Paediatr 2014;82:213–221 [PubMed: 25011467] . 4. Secondary Amenorrhea See discussion of amenorrhea in Chapter 4. POLYCYSTIC OVARY SYNDROME Downloaded 2:52 A Your IP is 13.213.160.179 ESSENTIALS 2023­10­12 OF DIAGNOSIS & TYPICAL FEATURES Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu ©2023Oligomenorrhea McGraw Hill. AllorRights Reserved. Terms or of laboratory Use • Privacy Policy • Notice • Accessibility amenorrhea and clinical signs of hyperandrogenism. Diagnosis of exclusion and other causes of menstrual dysfunction or elevated androgens need to be ruled out. Page 37 / 53 See discussion of amenorrhea in Chapter 4. University of Medicine and Pharmacy at HCMC Access Provided by: POLYCYSTIC OVARY SYNDROME ESSENTIALS OF DIAGNOSIS & TYPICAL FEATURES Oligomenorrhea or amenorrhea and clinical or laboratory signs of hyperandrogenism. Diagnosis of exclusion and other causes of menstrual dysfunction or elevated androgens need to be ruled out. Increased risk of many comorbidities including type 2 diabetes, fatty liver disease, hypertension, depression, and obstructive sleep apnea. 1. General Considerations Polycystic ovary syndrome (PCOS) is one of the most common menstrual disorders in women, estimated to affect 10%–15% of all reproductive age women. The underlying pathology of PCOS is not well understood. Many girls with PCOS will have a history of early adrenarche. The diagnosis cannot formally be made until at least 1 year post­menarche or with primary amenorrhea, due to the normal duration of time required for girls to establish regular menstrual cycles. Many girls with PCOS are obese, which contributes to an increased prevalence of the disease, but PCOS is also present in girls without obesity. Adolescents with PCOS typically present for cosmetic concerns such as cystic acne or menstrual irregularities. However, PCOS is associated with many comorbidities and it is important to provide comprehensive screening and care. 2. Clinical Findings PCOS should be considered in adolescents who have (1) menstrual abnormalities including: (a) oligomenorrhea of less than 8 menses a year 2 years following menarche, (b) severe oligomenorrhea: more than 90 days between cycle at least a year post­menarche, (c) primary amenorrhea greater than or equal to 15 years, or (d) primary amenorrhea greater than or equal to 2 years after breast development; and (2) clinical signs and symptoms of hyperandrogenism such as hirsutism, cystic acne, androgenic alopecia, and/or biochemical hyperandrogenism. PCOS is a diagnosis of exclusion and other causes of irregular menses should be excluded. These include primary ovarian failure, prolactinoma, thyroid dysfunction, hypothalamic hypogonadotropic hypogonadism, as seen in those who are underweight or with extreme obesity, ovarian tumor or pituitary mass. Causes of hyperandrogenism such as adrenal tumors, ovarian tumors, or congenital adrenal hyperplasia should be ruled out with laboratory testing. The physical examination should be comprehensive and assess for severity of acne, hirsutism as scored by the Ferriman­Gallwey scale, alopecia, acanthosis nigricans, skin tags, pilonidal cysts, hidradenitis, thyroid size, airway and tonsil size, liver size, peripheral edema, striea size, and color and clitoral enlargement. Ovarian ultrasound is not recommended for the diagnosis of PCOS until 8 years post­menarche due to the large variability of normal ovaries in adolescent girls. Uterine ultrasound can be used to determine structural abnormalities causing amenorrhea, thickness of the endometrium in cases of failure to initiate a menstrual bleed following a short course of medroxyprogesterone or to monitor for large cysts causing ovarian pain. Once a diagnosis of PCOS is established, girls also need to be screened for associated co­morbidities. Adolescents with PCOS have an increased risk of developing insulin resistance and type 2 diabetes, and a 75­g 2­hour oral glucose tolerance should be performed, or alternatively a hemoglobin A1C test at diagnosis and then every 1–2 years. Fasting lipids should be measured at diagnosis and then per American Academy of Pediatrics guidelines. Up to 50% of obese girls with PCOS have nonalcoholic fatty liver disease, and transaminases should be checked at diagnosis, and liver size assessed by examination. The risk of hypertension is increased, and blood pressure should be checked at every appointment with an appropriate sized cuff. If symptoms of obstructive sleep apnea are present, overnight polysomnography should be performed. All girls should be screened for anxiety and depression on a routine basis. 3. Treatment The treatment for PCOS should be comprehensive, personalized for each individual, and ideally delivered via a coordinated multidisciplinary approach. All girls, even those of normal weight are encouraged to maintain a healthy lifestyle, with moderate to vigorous activity 3–5 days a week and a healthy diet. To induce weight loss, diets may need to be very low calorie (1200–1500 kcal/day) and exercise may need to be daily. Monophasic combined oral contraceptives, with 30–35 mcg of estradiol and a third­ or fourth­generation nonandrogenic progestin are used to regulate menses, decrease acne, hirsutism, and alopecia. Other methods of delivery including combined estradiol and progesterone patches or vaginal rings can also be used, although they are less reliable for contraception in individuals greater than 200 pounds. Long­acting implantable and uterine progestins can be utilized to prevent endometrial hyperplasia, although due to the risk of weight gain, multiple doses of injectable progesterone should be avoided. Cyclic oral progesterone, at a dose of 10 mg daily for 10 days can be utilized to initiate menses every 3 months in those that do not desire to take oral Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 contraceptives. Metformin, at a dose of 1000 mg twice a dayM. can be used to treat insulin resistance and hyperglycemia Page 38 / 53 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine Chan; Melanie Cree­Green; Shanlee Davis; Stephanieand Hsucan induce modest ©2023 McGrawinHill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • at Accessibility improvements menstrual regularity. The extended­release form can be prescribed 2000 mg once a day in those with gastric intolerance to the regular formulation. Typical acne treatments should be used, and for hirsutism treatments include spironolactone up to 200 mg a day, eflornithine cream, electrolysis, and laser hair treatment. Topical minoxidil can reduce androgenic alopecia, and alpha­hydroxy acid lotion can be used for a healthy diet. To induce weight loss, diets may need to be very low calorie (1200–1500 kcal/day) and exercise may need to be daily. Monophasic University of Medicine and at HCMC combined oral contraceptives, with 30–35 mcg of estradiol and a third­ or fourth­generation nonandrogenic progestin are used to Pharmacy regulate menses, Access Provided by: decrease acne, hirsutism, and alopecia. Other methods of delivery including combined estradiol and progesterone patches or vaginal rings can also be used, although they are less reliable for contraception in individuals greater than 200 pounds. Long­acting implantable and uterine progestins can be utilized to prevent endometrial hyperplasia, although due to the risk of weight gain, multiple doses of injectable progesterone should be avoided. Cyclic oral progesterone, at a dose of 10 mg daily for 10 days can be utilized to initiate menses every 3 months in those that do not desire to take oral contraceptives. Metformin, at a dose of 1000 mg twice a day can be used to treat insulin resistance and hyperglycemia and can induce modest improvements in menstrual regularity. The extended­release form can be prescribed at 2000 mg once a day in those with gastric intolerance to the regular formulation. Typical acne treatments should be used, and for hirsutism treatments include spironolactone up to 200 mg a day, eflornithine cream, electrolysis, and laser hair treatment. Topical minoxidil can reduce androgenic alopecia, and alpha­hydroxy acid lotion can be used for acanthosis. Standard therapies for obstructive sleep apnea, hyperlipidemia, hypertension, and psychological disturbances should be utilized as needed. The use of weight loss medications such as topiramate, phentermine, or glucagon like receptor­1 agonist should be considered in older obese adolescents in conjunction with lifestyle therapies. Patients should be seen every 3–6 months, pending the complexity of their medical needs. Legro RS et al: Diagnosis and treatment of polycystic ovary syndrome: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 2013;98:4565–4592 [PubMed: 24151290] . Teede HJ et al: Recommendations from the international evidence­based guideline for the assessment and management of polycystic ovary syndrome. Hum Reprod 2018;33:1602–1618 [PubMed: 30052961] . Witchel SF et al: The diagnosis of polycystic ovary syndrome during adolescence. Horm Res Paediatr 2015;83:376–389 [PubMed: 25833060] . ABNORMALITIES IN MALE PUBERTAL DEVELOPMENT & TESTICULAR FUNCTION 1. Precocious Puberty in Boys Puberty is considered precocious in boys if secondary sexual characteristics appear before age 9 years, and like in girls, can be central (gonadotropin­ dependent) or peripheral (gonadotropin­independent). While the frequency of central precocious puberty is much lower in boys than girls, boys are much more likely to have an associated CNS abnormality (see Table 34–8) and require medical evaluation. In addition, several types of gonadotropin­ independent (peripheral) precocious puberty occur in boys (see Table 34–8). Clinical Findings A. Symptoms and Signs Appearance of pubic hair is the most common presenting sign of puberty in boys, followed by enlargement of the phallus, scrotal maturation, axillary hair, voice deepening, and increased growth velocity. Testicular size differentiates central precocity, in which the testes enlarge (> 2 cm in the longitudinal axis or > 4 mL using Prader beads), from gonadotropin­independent causes, in which the testes usually remain much smaller than expected for the degree of virilization. Tumors of the testis are associated with either asymmetrical or unilateral testicular enlargement. B. Laboratory Findings Testosterone concentrations are usually elevated in precocious puberty. Basal high­sensitivity serum LH and FSH concentrations will be in the pubertal range in boys with central precocious puberty, but suppressed in peripheral precocity. GnRH­analogue (leuprolide) stimulation testing can also distinguish central from gonadotropin­independent puberty, but is often not needed in boys because increased testicular volume is usually a reliable physical sign of central puberty. In boys with peripheral precocious puberty caused by congenital adrenal hyperplasia (CAH), plasma adrenal androgens and 17­hydroxyprogesterone will be elevated. Serum β­HCG concentrations signify the presence of an HCG­producing tumor (eg, CNS dysgerminoma or hepatoma) in boys who present with precocious puberty and testicular enlargement but suppressed gonadotropins. Genetic testing may be helpful in diagnosing CAH or familial male precocious puberty (due to mutations in the LH receptor). C. Imaging A radiograph of the left hand to assess epiphyseal maturation (bone age) is useful in evaluating precocious puberty. In all boys with central precocious Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 puberty, brain MRI should be obtained to evaluate for a CNS If testing suggestsShanlee peripheral precocious puberty studies 39 /are 53 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M.abnormality. Chan; Melanie Cree­Green; Davis; Stephanie Hsu and laboratoryPage not consistent with imaging may be useful to detect adrenal, testicular tumors. ©2023 McGraw Hill.CAH, All Rights Reserved. Terms of Usehepatic, • Privacy Policy and • Notice • Accessibility Treatment dysgerminoma or hepatoma) in boys who present with precocious puberty and testicular enlargement but suppressed gonadotropins. Genetic testing University of Medicine and Pharmacy at HCMC may be helpful in diagnosing CAH or familial male precocious puberty (due to mutations in the LH receptor). Access Provided by: C. Imaging A radiograph of the left hand to assess epiphyseal maturation (bone age) is useful in evaluating precocious puberty. In all boys with central precocious puberty, brain MRI should be obtained to evaluate for a CNS abnormality. If testing suggests peripheral precocious puberty and laboratory studies are not consistent with CAH, imaging may be useful to detect hepatic, adrenal, and testicular tumors. Treatment Treatment of central precocious puberty in boys entails treatment of the underlying cause and the use of GnRH analogues. Boys with McCune­Albright syndrome or familial male precocious puberty are treated with agents that block steroid synthesis (eg, ketoconazole) or with a combination of antiandrogens (eg, spironolactone) and aromatase inhibitors (eg, anastrozole or letrozole) that block the conversion of testosterone to estrogen. 2. Delayed Puberty Boys should be evaluated for delayed puberty if they have no secondary sexual characteristics by 14 years of age or if more than 5 years have elapsed since the first signs of puberty without completion of genital growth. By far the most common cause of delayed puberty in boys is constitutional growth delay, a normal variant of growth described in detail earlier in this chapter. True hypogonadism in boys may be primary or central. Primary hypogonadism refers to testicular insufficiency and may be due to anorchia; Klinefelter syndrome (47,XXY) or other sex chromosome anomalies; enzymatic defects in testosterone synthesis; or inflammation or destruction of the testes following infection (eg, mumps), autoimmune disorders, radiation, trauma, or tumor. Central hypogonadism refers to deficiencies in pituitary and/or hypothalamic function and may be isolated (gonadotropin deficiency only) or accompany multiple pituitary hormone deficiencies. The etiologies of central hypogonadism in boys are the same as girls (see Table 34–9). Clinical Evaluation The history should focus on when puberty signs started, history of genitourinary malformations that would be concerning for insufficient intrauterine testosterone, growth pattern, symptoms of chronic illness, sense of smell, and family history of delayed puberty. Physical examination should include growth parameters, pubertal stage, and testicular location, size, and consistency. Testes less than 2 cm in length, or less than 4 mL using Prader beads, are prepubertal; symmetric testes more than 2.5 cm or more than 4 mL typically indicate onset of central puberty. A radiograph of the left hand and wrist to assess bone age should be the first step in evaluating delayed puberty. If bone age is delayed relative to chronological age and growth velocity is normal for a prepubertal boy, constitutional growth delay is the most likely diagnosis. Laboratory evaluation may include measurement of LH and FSH levels (if bone age is > 12 years) with elevated gonadotropins indicating primary hypogonadism or testicular failure. Low gonadotropins are not specific but may suggest the possibility of central hypogonadism and warrant further evaluation to assess for pituitary hormone deficiencies, chronic disease, undernutrition, hyperprolactinemia, or CNS abnormalities. Inhibin B, a hormone made by Sertoli cells in the testes, may help differentiate between constitutional delay (normal concentrations) and idiopathic hypogonadotropic hypogonadism (lower concentrations), although there can be significant overlap in levels in these conditions. Treatment Boys with delayed puberty who are troubled by their stature and/or prepubertal appearance may be offered a 4­ to 6­month course of low­dose depot testosterone (50–100 mg/mo given intramuscularly) to promote virilization and possibly “jump­start” their endogenous development. In adolescent boys with permanent hypogonadism, testosterone treatment will need to be gradually increased over 3–4 years to adult dosing. Topical testosterone gel applied daily is an alternative to injections but often is too potent in commercially available concentrations to use in early puberty. Other formulations of testosterone are not widely used in adolescents. 3. Cryptorchidism Cryptorchidism (undescended testis) affects 2%–4% of full­term male newborns and up to 30% of premature infants. Cryptorchidism can occur in an isolated fashion or associated with other findings. Often the cause is unknown, however abnormalities in the hypothalamic­pituitary­gonadal axis, intrinsic testicular development defects, and androgen biosynthesis or receptor defects can result in cryptorchidism. Infertility and testicular malignancy are major risks of untreated cryptorchidism. Histologic changes occur as early as age 6 months in children with undescended 2023­10­12 testes. Fertility is impaired byisapproximately 33% and 66% after unilateral and bilateral cryptorchidism, respectively. The cancer risk for Downloaded 2:52 A Your IP 13.213.160.179 Pageonly 40 / 53 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Cree­Green; Shanlee Davis;ofStephanie Hsu adults after cryptorchidism in childhood is reported to be 5–10Chan; timesMelanie greater than normal. After 6 months age, spontaneous descent occurs ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility very rarely. Consequently, intervention is typically considered after this time. Clinical Findings 3. Cryptorchidism University of Medicine and Pharmacy at HCMC Cryptorchidism (undescended testis) affects 2%–4% of full­term male newborns and up to 30% of premature infants. Cryptorchidism can occur in an Access Provided by: isolated fashion or associated with other findings. Often the cause is unknown, however abnormalities in the hypothalamic­pituitary­gonadal axis, intrinsic testicular development defects, and androgen biosynthesis or receptor defects can result in cryptorchidism. Infertility and testicular malignancy are major risks of untreated cryptorchidism. Histologic changes occur as early as age 6 months in children with undescended testes. Fertility is impaired by approximately 33% and 66% after unilateral and bilateral cryptorchidism, respectively. The cancer risk for adults after cryptorchidism in childhood is reported to be 5–10 times greater than normal. After 6 months of age, spontaneous descent occurs only very rarely. Consequently, intervention is typically considered after this time. Clinical Findings Examination should focus on whether testes can be palpated in the scrotum or inguinal canal, appearance of the genitalia, and any midline defects. To prevent retraction of the testis during examination, two hands are required. One hand milks the testes from the deep inguinal ring to the scrotum. The second hand lies over the scrotum to hold the testis. Examination in the squatting position for older children or in a warm bath can be helpful. Ultrasonography, CT, and MRI may detect testes in the inguinal region, but these studies are not completely reliable and are usually not indicated. During the mini­puberty period of infancy between 1 and 4 months of age, measurement of LH, FSH, and testosterone can assess the HPG axis. After this time, inhibin B and/or an HCG stimulation test can be done to confirm the presence or absence of functional testes. Differential Diagnosis Various differences/disorders of sex development can present with cryptorchidism. A karyotype can identify a virilized 46,XX individual (CAH), mixed gonadal dysgenesis (45,X/46,XY), and 47,XXY/Klinefelter syndrome, all of which can be associated with unilateral or bilateral cryptorchidism. The diagnosis of bilateral cryptorchidism in an apparently normal male newborn should never be made until the possibility that the child is a fully virilized female with potentially fatal salt­losing CAH has been considered. Treatment Surgical orchidopexy should be performed if descent has not occurred by 6–12 months of age. The recommended timing of surgical intervention is based on the assumption that early surgery will allow normal germ cell development and decrease the risk for future infertility and cancer. However, in some cases, a primary abnormality of the testis may be responsible for both the lack of descent and future risks. Therapy with HCG 250–1000 IU twice weekly for 5 weeks has been used to induce descent of the testis but has a low success rate. 4. Gynecomastia Gynecomastia is a common, self­limited condition that occurs in up to 75% of normal pubertal boys. Adolescent gynecomastia typically resolves within 2 years but may not completely resolve if the degree of gynecomastia is extreme (> 2 cm of tissue). Gynecomastia is more common in obese boys, possibly due to adipose aromatization of testosterone to estrogen. Gynecomastia may also occur in untreated male hypogonadism and as a side effect of some medications. Medical therapy using antiestrogens and/or aromatase inhibitors may be beneficial if initiated early when there is active stimulation of the mammary glands, but given most pubertal gynecomastia will self­resolve, pharmacologic management is rarely pursued. Surgical intervention should be considered for prolonged and/or severe cases (see Chapter 4). Hutson JM, Thorup J: Evaluation and management of the infant with cryptorchidism. Curr Opin Pediatr 2015 Aug;27(4):520–524 [PubMed: 26087417] . Latronico AC et al: Causes, diagnosis, and treatment of central precocious puberty. Lancet Diabetes Endocrinol 2016 Mar;4(3):265–274. [PubMed: 26852255] . Wei C, Crowne EC: Recent advances in the understanding and management of delayed puberty. Arch Dis Child 2016 May;101(5):481–488 [PubMed: 26353794] . ADRENAL CORTEX The adult adrenal cortex consists of three zones responsible for synthesis of distinct steroids from the precursor, cholesterol (see Figure 34–8): Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 Outermost zona glomerulosa—mineralocorticoids (primarily aldosterone). Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu ©2023 McGraw All Rights Reserved. Terms of Usecortisol). • Privacy Policy • Notice • Accessibility Middle zonaHill. fasciculata—glucocorticoids (primarily Innermost zona reticularis—androgens. Page 41 / 53 University of Medicine and Pharmacy at HCMC ADRENAL CORTEX Access Provided by: The adult adrenal cortex consists of three zones responsible for synthesis of distinct steroids from the precursor, cholesterol (see Figure 34–8): Outermost zona glomerulosa—mineralocorticoids (primarily aldosterone). Middle zona fasciculata—glucocorticoids (primarily cortisol). Innermost zona reticularis—androgens. The predominant regulator of mineralocorticoid production and secretion is the volume­ and sodium­sensitive renin­angiotensin­aldosterone system. Mineralocorticoids promote sodium retention and stimulate potassium excretion in the distal renal tubule. Glucocorticoid production is under the control of pituitary adrenocorticotropic hormone (ACTH; see Figure 34–1 and Table 34–1), which is in turn regulated by hypothalamic corticotropin­releasing hormone (CRH). ACTH concentration is greatest during the early morning hours with a smaller peak in the late afternoon and a nadir at night. The pattern of serum cortisol concentration follows this pattern with a lag of a few hours. In the absence of cortisol feedback, there is dramatic CRH and ACTH hypersecretion. Glucocorticoids are critical for gene expression in a many cell types. Glucocorticoids also help maintain blood pressure by promoting peripheral vascular tone and sodium and water retention. In excess, glucocorticoids are both catabolic and antianabolic; they promote the release of amino acids from muscle and increase gluconeogenesis while decreasing incorporation of amino acids into muscle protein. They also antagonize insulin activity and facilitate lipolysis. At the onset of puberty, production of androgens (dehydroepiandrosterone and androstenedione) increases and is an important contributor to pubertal development in both sexes. The adrenal gland is the major source of androgen in females. ADRENOCORTICAL INSUFFICIENCY Adrenal insufficiency may be primary—due to disorders of the adrenal gland itself, or central/secondary—due to disorders of CRH and/or ACTH secretion. Primary adrenal insufficiency impairs the production of all adrenal steroids, whereas secondary adrenal insufficiency should not affect production of mineralocorticoids or androgens as these are not regulated by ACTH. The causes of primary and secondary adrenal insufficiency are listed in Table 34–10. Table 34–10. Causes of adrenal insufficiency. A. Primary adrenal insufficiency a. Congenital adrenal hyperplasia (enzyme defect) b. Addison disease (autoimmune) c. Hemorrhage (Waterhouse­Friderichsen syndrome) d. Tumor, calcification, or infection in the gland e. X­linked adrenal hypoplasia congenita (DAX1 mutation or deletion) f. Adrenoleukodystrophy B. Secondary adrenal insufficiency a. Congenital hypopituitarism secondary to transcription factor mutations or structural defects of the hypothalamus or pituitary; sometimes associated with other midline defects or optic nerve hypoplasia sequence b. Congenital absence of transcription factors c. Intracranial tumor d. Surgery or radiation of the hypothalamus or pituitary gland Clinical Findings A. Symptoms and Signs Downloaded 2023­10­12 1. Acute form (adrenal crisis) 2:52 A Your IP is 13.213.160.179 Page 42 / 53 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility Nausea, vomiting, abdominal pain; dehydration; fever (sometimes followed by hypothermia); weakness; hypoglycemia; hypotension and circulatory collapse; and confusion and coma. Hyponatremia and hyperkalemia are seen in primary adrenal insufficiency. Acute illness, surgery, trauma, or University of Medicine and Pharmacy at HCMC Clinical Findings Access Provided by: A. Symptoms and Signs 1. Acute form (adrenal crisis) Nausea, vomiting, abdominal pain; dehydration; fever (sometimes followed by hypothermia); weakness; hypoglycemia; hypotension and circulatory collapse; and confusion and coma. Hyponatremia and hyperkalemia are seen in primary adrenal insufficiency. Acute illness, surgery, trauma, or hyperthermia may precipitate an adrenal crisis in patients with adrenal insufficiency. 2. Chronic form Fatigue, hypotension, weakness, weight loss or failure to gain weight, vomiting and dehydration, and recurrent hypoglycemia. In primary adrenal insufficiency, salt craving and hyponatremia and/or hyperkalemia can be seen, as well as hyperpigmentation, particularly over pressure points, scars, and mucous membranes. B. Laboratory Findings 1. Baseline Labs: Serum ACTH and renin are elevated in primary adrenal but are not helpful in diagnosing central adrenal insufficiency. Serum morning fasting cortisol < 3 mcg/dL is highly suggestive of adrenal insufficiency, whereas >10 mcg/dL is reassuring against adrenal insufficiency. Hypoglycemia is a nonspecific finding that can be seen in both primary and central adrenal insufficiency Hyponatremia, hyperkalemia, and increased urinary sodium in primary adrenal insufficiency. Urinary free cortisol is low in both primary and central adrenal insufficiency, but this is not widely used in the diagnosis. 2. ACTH (c o s y n t r o p i n) s t i m u l a t i o n t e s t Intravenous cosyntropin should stimulate functional adrenal glands to produce cortisol that can be measured in plasma within 1 hour. If primary adrenal insufficiency is suspected, a high­dose (250 mcg) of cosyntropin should be given, whereas a low­dose (1–5 mcg) of cosyntropin is used to evaluate for central adrenal insufficiency. Cortisol less than 18 mcg/dL 30 and 60 minutes after either high or low dose intravenous cosyntropin is consistent with adrenal insufficiency. 3. Glucagon stimulation test Glucagon 0.05 mg/kg or 1 mg given subcutaneously or intravenously should stimulate functional adrenal glands secondary to counter­regulatory mechanisms. Cortisol less than 10 mcg/dL at 120 and 150 minutes is consistent with adrenal insufficiency. Differential Diagnosis Acute adrenal insufficiency must be differentiated from sepsis, diabetic coma, CNS disturbances, dehydration, and acute poisoning. In the neonatal period, adrenal insufficiency may be clinically indistinguishable from respiratory distress, intracranial hemorrhage, or sepsis. Chronic adrenocortical insufficiency must be differentiated from anorexia nervosa, depression, neuromuscular disorders, salt­losing nephropathy, malignancy, and chronic debilitating infections. Treatment A. Acute Insufficiency (Adrenal Crisis) 1. Hydrocortisone sodium succinate Hydrocortisone sodium succinate (50 mg/m2 intravenously over 2–5 minutes or intramuscularly) is given initially followed by 12.5 mg/m2 IV or oral every 4–6 hours until 24 hours after stabilization and resolution of the acute illness. Patients with known adrenal insufficiency should have Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 intramuscular hydrocortisone 50 or 100 mg for home use in the case of an emergency or inability to tolerate enteral stress dosing. Page 43 / 53 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility 2. Fluids and electrolytes A. Acute Insufficiency (Adrenal Crisis) 1. Hydrocortisone sodium succinate University of Medicine and Pharmacy at HCMC Access Provided by: Hydrocortisone sodium succinate (50 mg/m2 intravenously over 2–5 minutes or intramuscularly) is given initially followed by 12.5 mg/m2 IV or oral every 4–6 hours until 24 hours after stabilization and resolution of the acute illness. Patients with known adrenal insufficiency should have intramuscular hydrocortisone 50 or 100 mg for home use in the case of an emergency or inability to tolerate enteral stress dosing. 2. Fluids and electrolytes In primary adrenal insufficiency, 5%–10% glucose in normal saline, 10–20 mL/kg intravenously, is given over the first hour and repeated if necessary to reestablish vascular volume. Normal saline is continued thereafter at 1.5–2 times maintenance fluid requirements until volume and electrolytes have normalized. In central adrenal insufficiency, routine fluid management is generally adequate after initial restoration of vascular volume and institution of cortisol replacement. 3. Fludrocortisone Stress doses of hydrocortisone provide adequate mineralocorticoid activity in the acute setting. When oral intake is tolerated, fludrocortisone should be started for primary adrenal insufficiency. B. Maintenance Therapy 1. Glucocorticoids A maintenance dosage of 6–10 mg/m2/day of hydrocortisone (or equivalent) is given orally in two or three divided doses. To prevent acute adrenal crises, the dose of hydrocortisone is increased to 30–50 mg/m2/day during intercurrent illnesses or other times of stress (fever, trauma, surgery, or systemic illness) should also be increased during significant diarrhea due to reduced absorption. Families should be encouraged to give stress doses of hydrocortisone if they have concerns, as brief exposure to stress doses of hydrocortisone will not have adverse effects. Rarely, families become overly anxious and give stress doses frequently. This should be avoided as it can contribute to obesity, linear growth impairment, and other Cushingoid features. 2. Mineralocorticoids In primary adrenal insufficiency, oral fludrocortisone 0.05–0.15 mg daily as a single dose or in two divided doses is given. Periodic monitoring of blood pressure is recommended to avoid overdosing. Children should be given ready access to table salt. In infants, supplementation of breast milk or formula with 3–5 mEq Na+/kg/day is generally required until table foods are introduced. Course & Prognosis If adrenal crisis is not recognized and promptly treated with pharmacologic glucocorticoids, the course of acute adrenal insufficiency is rapid and death may occur within a few hours, particularly in infants. If treated appropriately, the prognosis of adrenal insufficiency is good; however, spontaneous recovery is unlikely unless the etiology was transient (eg, exogenous glucocorticoid exposure). Regular care with an endocrinologist is required to evaluate management and adjust dosing to ensure adequate replacement while avoiding overdosing that could lead to impaired growth, hypertension, and Cushingoid features. Kirkgoz T, Guran T: Primary adrenal insufficiency in children: diagnosis and management. Best Pract Res Clin Endocrinol Metab 2018 Aug;32(4):397– 424 [PubMed: 30086866] . Patti G et al: Central adrenal insufficiency in children and adolescents. Best Pract Res Clin Endocrinol Metab 2018 Aug;32(4):425–444 [PubMed: 30086867] . CONGENITAL ADRENAL HYPERPLASIAS ESSENTIALS OF DIAGNOSIS & TYPICAL FEATURES Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 Page 44 / 53 Primary adrenal insufficiency. Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility Genital virilization in females, with labial fusion, urogenital sinus, enlargement of the clitoris, or other evidence of androgen action in the most common form. [PubMed: 30086867] . University of Medicine and Pharmacy at HCMC Access Provided by: CONGENITAL ADRENAL HYPERPLASIAS ESSENTIALS OF DIAGNOSIS & TYPICAL FEATURES Primary adrenal insufficiency. Genital virilization in females, with labial fusion, urogenital sinus, enlargement of the clitoris, or other evidence of androgen action in the most common form. Increased linear growth and advanced skeletal maturation. Elevation of plasma 17­hydroxyprogesterone concentrations in the most common form; may be associated with hyponatremia, hyperkalemia, and metabolic acidosis if mineralocorticoid deficiency included. General Considerations Autosomal recessive mutations in the enzymes of adrenal steroidogenesis cause impaired cortisol biosynthesis with increased ACTH secretion. ACTH excess subsequently results in adrenal hyperplasia with increased production of adrenal hormone precursors that are metabolized through the unblocked androgen pathway. Increased pigmentation, especially of the scrotum, labia majora, and nipples, is common due to excessive ACTH secretion. CAH is most commonly (> 90% of patients) the result of homozygous or compound heterozygous mutations in the cytochrome P­450 C21 (CYP21A2) gene causing 21­hydroxylase deficiency (see Figure 34–8). The defective gene is present in 1:250–1:100 people and the worldwide incidence of the disorder is 1:15,000, with increased incidence in certain ethnic groups. In its severe form, excess adrenal androgen production starting in the first trimester of fetal development causes virilization of the female fetus and life­threatening hypovolemic, hyponatremic shock (adrenal crisis) in the newborn if untreated. There are other enzyme defects that less commonly result in CAH. The clinical syndromes associated with these defects are shown in Figure 34–8 and Table 34–11. Table 34–11. Clinical and laboratory findings in adrenal enzyme defects resulting in congenital adrenal hyperplasia. Enzyme Deficiencya StAR protein Elevated Plasma Plasma Metabolite Androgens – ↓↓↓ Aldosterone Hypertension ↓↓↓ – Salt wasting + External Genitalia Males: ambiguous Females: normal 3β­Hydroxysteroid 17­OH pregnenolone dehydrogenase (DHEA) ↑ (DHEA) ↓↓↓ – + Males: ambiguous Females: possibly virilized 17α­Hydroxylase/17–20 Progesterone ↓↓ (↑ DOC) + – lyase Males: ambiguous Females: normal, absent puberty 21­Hydroxylasea 17­OHP ↑↑ ↓↓ – + Males: normal Females: virilized 11β­Hydroxylase 11­Deoxycortisol, DOC ↑↑ (↑ DOC) + – Males: normal Females: virilized P450 oxidoreductase 17­OHP (mild elevation) ↓↓ Normal or mildly + – elevated Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 DHEA, dehydroepiandrosterone; DOC,Sarah deoxycorticosterone; 17­OHP, 17­hydroxyprogestrone. Chapter 34: Endocrine Disorders, Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility Males: ambiguous Females: ambiguous Page 45 / 53 aChildren with “simple virilizing (non–salt­wasting)” forms of 21­hydroxylase deficiency congenital adrenal hyperplasia (CAH) may have normal aldosterone production and serum electrolytes, but some children have normal aldosterone production and serum electrolytes at the expense of elevated plasma renin activity of the disorder is 1:15,000, with increased incidence in certain ethnic groups. In its severe form, excess adrenal androgen production starting in the University of Medicine and Pharmacy at HCMC first trimester of fetal development causes virilization of the female fetus and life­threatening hypovolemic, hyponatremic shock (adrenal crisis) in the Access Provided by: newborn if untreated. There are other enzyme defects that less commonly result in CAH. The clinical syndromes associated with these defects are shown in Figure 34–8 and Table 34–11. Table 34–11. Clinical and laboratory findings in adrenal enzyme defects resulting in congenital adrenal hyperplasia. Enzyme Deficiencya StAR protein Elevated Plasma Plasma Metabolite Androgens – ↓↓↓ Aldosterone Hypertension ↓↓↓ – Salt wasting + External Genitalia Males: ambiguous Females: normal 3β­Hydroxysteroid 17­OH pregnenolone dehydrogenase (DHEA) ↑ (DHEA) ↓↓↓ – + Males: ambiguous Females: possibly virilized 17α­Hydroxylase/17–20 Progesterone ↓↓ (↑ DOC) + – lyase Males: ambiguous Females: normal, absent puberty 21­Hydroxylasea 17­OHP ↑↑ ↓↓ – + Males: normal Females: virilized 11β­Hydroxylase 11­Deoxycortisol, DOC ↑↑ (↑ DOC) + – Males: normal Females: virilized P450 oxidoreductase 17­OHP (mild elevation) ↓↓ Normal or mildly elevated + – Males: ambiguous Females: ambiguous DHEA, dehydroepiandrosterone; DOC, deoxycorticosterone; 17­OHP, 17­hydroxyprogestrone. aChildren with “simple virilizing (non–salt­wasting)” forms of 21­hydroxylase deficiency congenital adrenal hyperplasia (CAH) may have normal aldosterone production and serum electrolytes, but some children have normal aldosterone production and serum electrolytes at the expense of elevated plasma renin activity and are, by definition, compensated salt­wasters. These children usually receive mineralocorticoid as well as glucocorticoid treatment. Children with 21­hydroxylase deficiency CAH should therefore have documented normal plasma renin activity in addition to normal serum electrolytes before they are considered non–salt­ wasters. Prenatal diagnosis is now possible and newborn screening by measurement of serum 17­hydroxyprogesterone (17­OHP) is established in all 50 US states and many countries worldwide. Clinical Findings in 21­Hydroxylase Deficiency A. Symptoms and Signs 1. Classic CAH in females Abnormality of the external genitalia varies from mild enlargement of the clitoris to complete fusion of the labioscrotal folds forming an empty scrotum, a penile urethra, a penile shaft, and clitoral enlargement sufficient to form a normal­sized glans (see Figure 34–7). Signs of adrenal insufficiency (salt loss) typically appear 5–14 days after birth. Without adequate treatment, virilization progresses with accelerated growth, pubic hair, acne, voice deepening, and advanced skeletal maturation with premature epiphyseal fusion resulting in a compromised adult height. Central precocious puberty may occur if treatment is not initiated before the bone age is significantly advanced. Other signs of primary adrenal insufficiency, including hyperpigmentation and adrenal crises, can also occur. 2. Classic CAH in males Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 Page 46 / 53 Chapter Endocrine Disorders, Sarah Christine M. with Chan; Melanie crisis Cree­Green; Shanlee Davis; The male34: infant usually appears normal atBartz; birth and presents salt­losing in the first weeks of life ifStephanie treatment Hsu is not initiated. Like females, ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility progressive virilization and skeletal maturation occurs in the setting of inadequate treatment, sometimes leading to central precocious puberty. Testicular adrenal rest tumors develop in many males with CAH. These are often benign and asymptomatic but can result in impaired spermatogenesis insufficiency (salt loss) typically appear 5–14 days after birth. Without adequate treatment, virilization progresses with accelerated growth, pubic hair, University of Medicine Pharmacy acne, voice deepening, and advanced skeletal maturation with premature epiphyseal fusion resulting in a compromised adult and height. Central at HCMC Access Provided by: precocious puberty may occur if treatment is not initiated before the bone age is significantly advanced. Other signs of primary adrenal insufficiency, including hyperpigmentation and adrenal crises, can also occur. 2. Classic CAH in males The male infant usually appears normal at birth and presents with salt­losing crisis in the first weeks of life if treatment is not initiated. Like females, progressive virilization and skeletal maturation occurs in the setting of inadequate treatment, sometimes leading to central precocious puberty. Testicular adrenal rest tumors develop in many males with CAH. These are often benign and asymptomatic but can result in impaired spermatogenesis and hypogonadism. Like in females, all other symptoms of primary adrenal insufficiency can occur. In some rare enzyme defects, ambiguous genitalia may be present due to impaired androgen production (see Table 34–11). 3. Nonclassic CAH With mild 21­hydroxylase deficiency, affected individuals have a normal phenotype at birth but develop virilization during later childhood, adolescence, or early adulthood. This is included among the causes of gonadotropin­independent precocious puberty, hirsutism, and/or oligomenorrhea. Nonclassic CAH typically does not present with adrenal crisis. B. Laboratory Findings 1. Blood Hormonal studies are essential for accurate diagnosis. Findings characteristic of the enzyme deficiencies are shown in Table 34–11. 2. Genetic studies Rapid assessment of sex chromosomes should be obtained in any newborn with ambiguous genitalia since 21­hydroxylase deficiency is the most common cause of ambiguity in females. C. Imaging Imaging is generally not required to make the diagnosis of CAH. Ultrasonography, CT scanning, and MRI may be useful in defining pelvic anatomy or to exclude an adrenal tumor. Treatment A. Medical Treatment Mineralocorticoid replacement sustains normal electrolyte homeostasis, but excessive mineralocorticoids cause hypertension and hypokalemia. 1. Glucocorticoids Supraphysiologic doses of hydrocortisone are often needed to suppress androgen excess in classic CAH. Maintenance doses of hydrocortisone 10–15 mg/m2/day in three divided doses with dosages adjusted to maintain normal growth rate and skeletal maturation. Serum 17­hydroxyprogesterone and androgens are usually measured to monitor therapy, however the normalization of these lab values often results in overtreatment. The goal is to use the smallest dose of glucocorticoid that will prevent adrenal crisis and virilization while allowing normal of growth and development. Excessive glucocorticoids cause the undesirable side effects of Cushing syndrome. Nonclassic CAH may also benefit from glucocorticoid treatment if symptomatic; if not symptomatic treatment may not be needed. 2. Mineralocorticoids In classic CAH, fludrocortisone, 0.05–0.15 mg/day, is given orally once a day or in two divided doses. Periodic monitoring of blood pressure, electrolytes and plasma renin activity are recommended to avoid overdosing. Salt supplements are often needed for infants. Nonclassic CAH does not require mineralocorticoid treatment. B. Surgical Treatment While early surgery for virilized females was routinely advised in the past, guidelines have evolved in recent years. A multidisciplinary team Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 consultation including urology and/or gynecology should be as soonCree­Green; as possible to inform Davis; sharedStephanie decision­making, Page 47 / 53 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M.arranged Chan; Melanie Shanlee Hsu including surgical options.McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility ©2023 Course & Prognosis electrolytes and plasma renin activity are recommended to avoid overdosing. Salt supplements are often needed for infants. Nonclassic CAH does not University of Medicine and Pharmacy at HCMC require mineralocorticoid treatment. Access Provided by: B. Surgical Treatment While early surgery for virilized females was routinely advised in the past, guidelines have evolved in recent years. A multidisciplinary team consultation including urology and/or gynecology should be arranged as soon as possible to inform shared decision­making, including surgical options. Course & Prognosis The goal of treatment is to prevent adrenal crises and permit normal growth, development, and sexual maturation. If not adequately controlled, CAH results in sexual precocity and masculinization throughout childhood. If treatment is delayed or inadequate, androgens convert to estrogen resulting in rapid skeletal maturation, and true central precocious puberty may occur. Such children often exhibit tall stature and increased growth velocity in childhood, but their adult height is impaired due to premature epiphyseal fusion. Patient education stressing lifelong therapy is important to ensure adherence. Ongoing psychological evaluation and support is a critical component of care. Speiser PW et al: Congenital adrenal hyperplasia due to steroid 21­hydroxylase deficiency: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 2018;103(11):4043–4088 [PubMed: 30272171] . ADRENOCORTICAL HYPERFUNCTION ESSENTIALS OF DIAGNOSIS & TYPICAL FEATURES Truncal adiposity, thin extremities, moon facies, muscle wasting, weakness, plethora, easy bruising, purple striae, decreased growth rate, and delayed skeletal maturation. Hypertension, osteoporosis, and glycosuria. Elevated 24­hour urinary free cortisol, elevated midnight salivary cortisol, failed low­dose dexamethasone suppression test. General Considerations Cushing syndrome may result from excessive autonomous secretion of adrenal steroids (adrenal adenoma or carcinoma), excess pituitary ACTH secretion (Cushing disease), ectopic ACTH or CRH secretion, or chronic exposure to exogenous glucocorticoids (iatrogenic). In children younger than 12 years, Cushing syndrome is usually iatrogenic. It is less commonly due to adrenal tumor, adrenal hyperplasia, pituitary adenoma, or extra­pituitary ACTH­producing tumor. Clinical Findings A. Symptoms and Signs 1. Excess glucocorticoid Adiposity, most marked on the face, neck, and trunk—a fat pad (buffalo hump) in the interscapular area is characteristic but not diagnostic; fatigue; plethoric facies; purplish striae; easy bruising; osteoporosis and back pain; hypertension and glucose intolerance; proximal muscle wasting and weakness; and impairment of growth and skeletal maturation. 2. Excess mineralocorticoid Hypokalemia and mild hypernatremia, increased blood volume, edema, and hypertension. 3. Excess androgen Hirsutism, acne, virilization, and menstrual irregularities. Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu B. Diagnosis of Cushing ©2023 McGraw Hill. AllSyndrome Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility 1. Salivary cortisol Page 48 / 53 Hypokalemia and mild hypernatremia, increased blood volume, edema, and hypertension. University of Medicine and Pharmacy at HCMC Access Provided by: 3. Excess androgen Hirsutism, acne, virilization, and menstrual irregularities. B. Diagnosis of Cushing Syndrome 1. Salivary cortisol Elevated salivary cortisol obtained at midnight is a noninvasive and a specific and sensitive test for hypercortisolism. 2. 24­hour urinary­free cortisol excretion Elevated 24­hour urinary­free cortisol/creatinine suggests Cushing Syndrome. 3. Low­dose (15 mcg/kg) dexamethasone s u p p r e s s i o n t e s t Dexamethasone (15mcg/kg, max 1 mg) is given at midnight followed by measurement of fasting plasma cortisol and ACTH at 8 AM the following morning. Failure to suppress cortisol less than 1.8 ug/dL suggests Cushing syndrome. C. Establishing the Cause of Cushing Syndrome 1. ACTH concentration Decreased ACTH values (< 5 pg/mL) suggest an adrenal cause. Intermediate ACTH values (5–29 pg/mL) are indeterminant and warrant further investigation. Elevated ACTH values (> 29 pg/mL) suggest an ACTH­dependent (pituitary or ectopic) cause. 2. High­dose (8 mg) dexamethasone t e s t i n g High­dose dexamethasone testing may help to determine ACTH­dependent Cushing syndrome from ACTH­independent Cushing syndrome. D. Imaging Pituitary imaging may demonstrate a pituitary adenoma. Adrenal imaging by CT scan may demonstrate adenoma or bilateral hyperplasia. MRI and nuclear medicine studies of the adrenals may be useful in complex cases. Differential Diagnosis Children with exogenous obesity accompanied by striae and hypertension are often suspected of having Cushing syndrome. However, children with Cushing syndrome have a poor growth velocity, relatively short stature, and delayed skeletal maturation, while those with exogenous obesity usually have a normal or slightly increased growth velocity, normal to tall stature, and advanced skeletal maturation. The color of the striae (purplish in Cushing syndrome, pink in obesity) and the distribution of the obesity may assist in differentiation. The urinary­free cortisol excretion may be mildly elevated in obesity, but midnight salivary cortisol is normal and cortisol secretion is suppressed by low­dose dexamethasone suppression test. Treatment In cases of primary adrenal hyperfunction due to tumor, surgical removal is indicated. Glucocorticoids should be administered parenterally in pharmacologic doses during and after surgery until the patient is stable. Supplemental oral glucocorticoids, potassium, salt, and mineralocorticoids may be necessary until the suppressed contralateral adrenal gland recovers, sometimes over a period of several months. Similarly, pituitary adenomas and ectopic sources of ACTH or CRH are generally treated surgically. Recurrent adenomas may respond to irradiation. Lodish et al: Cushing’s syndrome in pediatrics. Endocrinol Metab Clin North Am 2018 Jun;47(2):451–462 [PubMed: 29754644] . PRIMARY HYPERALDOSTERONISM Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 Primary hyperaldosteronism may be caused by an adrenal M. adenoma adrenal hyperplasia.Shanlee It is characterized by paresthesias, tetany, weakness, Page 49 / 53 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine Chan; or Melanie Cree­Green; Davis; Stephanie Hsu ©2023 Hill. All Rights Reserved. Terms ofhypernatremia, Use • Privacy Policy • Notice • Accessibility periodicMcGraw paralysis; nocturnal enuresis; hypokalemia, metabolic alkalosis; hypertension; glucose intolerance; elevated plasma and urinary aldosterone; and suppressed plasma renin activity. Primary hyperaldosteronism is rare in pediatrics, but can occur due to an adrenal tumor or autosomal dominant genetic causes. Imaging and genetic testing are warranted to evaluate the etiology and determine appropriate surgical or medical University of Medicine and Pharmacy at HCMC Lodish et al: Cushing’s syndrome in pediatrics. Endocrinol Metab Clin North Am 2018 Jun;47(2):451–462 Access Provided by: [PubMed: 29754644] . PRIMARY HYPERALDOSTERONISM Primary hyperaldosteronism may be caused by an adrenal adenoma or adrenal hyperplasia. It is characterized by paresthesias, tetany, weakness, periodic paralysis; nocturnal enuresis; hypokalemia, hypernatremia, metabolic alkalosis; hypertension; glucose intolerance; elevated plasma and urinary aldosterone; and suppressed plasma renin activity. Primary hyperaldosteronism is rare in pediatrics, but can occur due to an adrenal tumor or autosomal dominant genetic causes. Imaging and genetic testing are warranted to evaluate the etiology and determine appropriate surgical or medical management. Funder JW et al: The management of primary aldosteronism: case detection, diagnosis, and treatment: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 2016 May;101(5):1889–1916 [PubMed: 26934393] . USES OF GLUCOCORTICOIDS & ADRENOCORTICOTROPIC HORMONE IN TREATMENT OF NONENDOCRINE DISEASES Glucocorticoids are used for their anti­inflammatory and immunosuppressive properties in a variety of conditions. Pharmacologic doses are necessary to achieve these effects, and side effects are common. Numerous synthetic preparations possessing variable ratios of glucocorticoid to mineralocorticoid activity are available (Table 34–12). Table 34–12. Potency equivalents for adrenocorticosteroids. Potency/mg Compared With Cortisol Potency/mg Compared With Cortisol (Glucocorticoid Effect) (Sodium­Retaining Effect) Cortef 1 1 Cortisone Cortone Acetate 0.8 1 Prednisone Meticorten, others 4–5 0.8 Methylprednisolone Medrol, Meprolone 5–6 Minimal Triamcinolone Aristocort, Kenalog 5–6 Minimal Adrenocorticosteroid Trade Names Glucocorticoids Hydrocortisone (cortisol) Kenacort, Atolone Dexamethasone Decadron, others 25–40 Minimal Betamethasone Celestone 25 Minimal Florinef 15–20 300–400 Mineralocorticoid Fludrocortisone When prolonged use of supraphysiologic doses of glucocorticoids is necessary, clinical manifestations of Cushing syndrome are common. Side effects may occur with the use of synthetic exogenous agents by any route, including inhalation and topical administration, or with the use of ACTH. Using the lowest effective dose and/or alternate­day therapy reduce the incidence and severity of some of the side effects (Table 34–13). Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 Table 34–13. Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu Side effects ofHill. glucocorticoid use. ©2023 McGraw All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility Page 50 / 53 Fludrocortisone Florinef 15–20 300–400 University of Medicine and Pharmacy at HCMC Access Provided by: When prolonged use of supraphysiologic doses of glucocorticoids is necessary, clinical manifestations of Cushing syndrome are common. Side effects may occur with the use of synthetic exogenous agents by any route, including inhalation and topical administration, or with the use of ACTH. Using the lowest effective dose and/or alternate­day therapy reduce the incidence and severity of some of the side effects (Table 34–13). Table 34–13. Side effects of glucocorticoid use. A. Endocrine and metabolic effects 1. Hyperglycemia and glycosuria (chemical diabetes) 2. Cushing syndrome 3. Persistent suppression of pituitary­adrenal responsiveness to stress with resultant hypoadrenocorticism B. Effects on electrolytes and minerals 1. Marked retention of sodium and water, producing edema, increased blood volume, and hypertension (more common in endogenous hyperadrenal states) 2. Potassium loss with symptoms of hypokalemia 3. Hypocalcemia, tetany C. Effects on protein metabolism and skeletal maturation 1. Negative nitrogen balance, with loss of body protein and bone protein, resulting in osteoporosis, pathologic fractures, and aseptic bone necrosis 2. Suppression of growth, retarded skeletal maturation 3. Muscular weakness and wasting 4. Osteoporosis 5. Avascular necrosis D. Effects on the gastrointestinal tract 1. Excessive appetite and intake of food 2. Activation or production of peptic ulcer 3. Gastrointestinal bleeding from ulceration or from unknown cause (particularly in children with hepatic disease) 4. Fatty liver with embolism, pancreatitis, nodular panniculitis E. Lowering of resistance to infectious agents; silent infection; decreased inflammatory reaction 1. Susceptibility to bacterial, viral, fungal, and parasitic infections 2. Activation of tuberculosis; false­negative tuberculin reaction 3. Reactivation and poor containment of herpesviruses F. Neuropsychiatric effects 1. Euphoria, excitability, psychotic behavior, and status epilepticus with electroencephalographic changes 2. Increased intracranial pressure with pseudotumor cerebri syndrome G. Hematologic and vascular effects 1. Bleeding into the skin as a result of increased capillary fragility 2. Thrombosis, thrombophlebitis, cerebral hemorrhage H. Miscellaneous effects 1. Myocarditis, pleuritis, and arteritis following abrupt cessation of therapy 2. Cardiomegaly 3. Nephrosclerosis, proteinuria 4. Acne (in older children), hirsutism, amenorrhea, irregular menses 5. Posterior subcapsular cataracts; glaucoma Tapering of Pharmacologic Doses of Steroids Prolonged use of pharmacologic doses of glucocorticoids causes suppression of ACTH secretion and consequent adrenal atrophy; the abrupt discontinuation of glucocorticoids may result in adrenal insufficiency. ACTH secretion generally does not restart until the administered steroid has been given in subphysiologic doses (< 6 mg/m2/day orally) for several weeks. Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 If pharmacologic glucocorticoid therapy has been given for less than ~2 weeks, the drug can be discontinued abruptly because adrenal suppression Page 51 / 53 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu will be short­lived. However, it isReserved. advisable toTerms educate the patient and family• Notice about the signs and symptoms of adrenal insufficiency in case problems ©2023 McGraw Hill. All Rights of Use • Privacy Policy • Accessibility arise. Tapering of Pharmacologic Doses of Steroids University of Medicine and Pharmacy at HCMC Access Providedadrenal by: Prolonged use of pharmacologic doses of glucocorticoids causes suppression of ACTH secretion and consequent atrophy; the abrupt discontinuation of glucocorticoids may result in adrenal insufficiency. ACTH secretion generally does not restart until the administered steroid has been given in subphysiologic doses (< 6 mg/m2/day orally) for several weeks. If pharmacologic glucocorticoid therapy has been given for less than ~2 weeks, the drug can be discontinued abruptly because adrenal suppression will be short­lived. However, it is advisable to educate the patient and family about the signs and symptoms of adrenal insufficiency in case problems arise. In longer treatment durations, stress dose precautions should be provided when therapeutic dosing decreases below ~30 mg/m2/day hydrocortisone equivalents. Although it is not unsafe from an adrenal insufficiency perspective to rapidly decrease glucocorticoid dosing to the physiologic range (8– 10 mg/m2/day hydrocortisone or equivalent) without tapering, some patients may experience a steroid withdrawal syndrome, characterized by malaise, insomnia, fatigue, and loss of appetite. These symptoms may necessitate a two­ or three­step decrease in dose to the physiologic range. Endogenous adrenal function will not resume until glucocorticoid dosing is below physiologic dosing and can take months to fully recover (highly correlated with the duration of suppression). There is no evidence to support any particular regimen of glucocorticoid tapering. Stress dose precautions need to be continued until endogenous adrenal recovery has been documented. After basal physiologic adrenal function returns, the adrenal reserve or capacity to respond to stress and infection can be estimated by the low­dose ACTH stimulation test (see above for details on cosyntropin stimulation testing). Even if the results of testing are normal, careful monitoring and the use of stress doses of glucocorticoids should be considered during severe illnesses and surgery. Wildi­Runge S et al: A search for variables predicting cortisol response to low­dose corticotropin stimulation following supraphysiological doses of glucocorticoids. J Pediatr 2013 Aug;163(2):484–488 [PubMed: 23414662] . ADRENAL MEDULLA PHEOCHROMOCYTOMA Pheochromocytoma and paragangliomas are uncommon tumors, but up to 20% of reported cases occur in pediatric patients. These neuroendocrine tumors can be located wherever chromaffin tissue (adrenal medulla, sympathetic ganglia, or carotid body) is present; if arising in the adrenal gland it is referred to as a pheochromocytoma whereas extra­adrenal locations are called paragangliomas. Pheochromocytoma may be multiple, recurrent, and sometimes malignant. Genetic testing is indicated in pediatric cases including neurofibromatosis 1, MEN 2, and von Hippel­Lindau syndromes, as well as mutations of the succinate dehydrogenase genes. The symptoms of pheochromocytoma are caused by excessive secretion of catecholamines (epinephrine and/or norepinephrine) that can be episodic: headache; sweating; palpitations, tachycardia, hypertension with postural hypotension); anxiety; tremor; dizziness; weakness; nausea, vomiting, diarrhea, weight loss; dilated pupils, blurred vision; abdominal and precordial pain. However, 10%–15% of patients with pheochromocytomas are asymptomatic. Unrecognized and untreated, pheochromocytoma can lead to fatal cardiovascular complications and stroke. Biochemical testing is indicated for individuals with symptoms of catecholamine excess, adrenal masses incidentally found on imaging that was being done for unrelated reasons, and known genetic mutations associated with pheochromocytoma. Plasma free metanephrines are the most sensitive and specific test; a level three times the normal range is strongly suggestive of hormonally active tumor, while normal range values exclude pheochromocytoma with high accuracy. Intermediate values require additional testing as medications and collection techniques can lead to false elevations. Plasma chromogranin A can also be measured to aid in the diagnosis of pheochromocytoma. After biochemical tests confirm catecholamine excess, MRI is used to localize the tumor and functional imaging is used to assess for extension and metastases. Surgical removal is the mainstay of treatment; however, massive release of catecholamines intraoperatively occurs if pre­treatment with alpha­ followed by beta­blockade is inadequate. Intraoperative blood pressures can fluctuate and continuous monitoring with short­acting medications is essential. Postoperatively, hypotension, hypertension, and/or hypoglycemia can occur, thus requiring intensive care monitoring. Long­term prognosis following uncomplicated surgical resection of an isolated pheochromocytoma is generally good for nonmetastatic disease; however, there is a risk of recurrence that requires ongoing surveillance. Jain A et al: Pheochromocytoma and paraganglioma—an update on diagnosis, evaluation, and management. Pediatr Nephrol 2020;35:481–594 [PubMed: 30603807] Waguespack SG et al: A current review of the etiology, diagnosis, and treatment of pediatric pheochromocytoma and paraganglioma. J Clin Endocrinol Metab 2010;95(5):2023–2037 Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 Page 52 / 53 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu [PubMed: 20215394] . ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility ongoing surveillance. University of Medicine and Pharmacy at HCMC Access Provided by: Jain A et al: Pheochromocytoma and paraganglioma—an update on diagnosis, evaluation, and management. Pediatr Nephrol 2020;35:481–594 [PubMed: 30603807] Waguespack SG et al: A current review of the etiology, diagnosis, and treatment of pediatric pheochromocytoma and paraganglioma. J Clin Endocrinol Metab 2010;95(5):2023–2037 [PubMed: 20215394] . Downloaded 2023­10­12 2:52 A Your IP is 13.213.160.179 Chapter 34: Endocrine Disorders, Sarah Bartz; Christine M. Chan; Melanie Cree­Green; Shanlee Davis; Stephanie Hsu ©2023 McGraw Hill. All Rights Reserved. Terms of Use • Privacy Policy • Notice • Accessibility Page 53 / 53