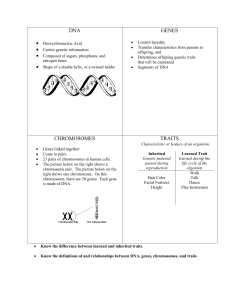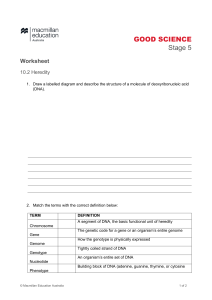
MED-SURG. NURSING GENETICS AND GENOMICS Introduction Genetics is the study of genes and their role in inheritance. Genetics determines the way that certain traits or conditions are passed down from one generation to another. Genomics is the study of all of a person's genes (the genome), including interactions of these genes with each other and with the person's environment. Genomics includes the study of complex diseases such as heart disease, asthma, diabetes mellitus, and cancer, because these diseases are typically caused by a combination of genetic and environmental factors rather than by a single gene. Introduction • A person's genes can have a profound impact on health and disease. • More than 4000 diseases are thought to be related to altered genes. Genomic factors play a role in 9 of the 10 leading causes of death in the United States, including heart disease, cancer, diabetes, stroke, and Alzheimer's disease. • Genornics may help us understand why some people who eat healthy diets and exercise regularly still die at a young age of cancer, whereas some people eat unhealthy diets and never exercise and yet live to an old age. Basic Principles of Genetics • Genes: are the basic units of heredity. • There are more than 22,000 genes in each person's genetic makeup, or genome. • Genes encode (carry the instructions) for proteins that direct the activities of cells and functions of the body. • Genes control how a cell functions, including how quickly it grows, how often it divides, and how long it lives. • To control these functions, genes produce proteins that perform specific tasks and act as messengers for the cell. • Therefore it is essential that each gene have the correct instructions or "code" for making its protein so that the protein can perform the proper function for the cell. • Genes are arranged in a specific linear formation along a chromosome. • Each gene has a specific location on a chromosome, termed a locus. • An allele is one of two or more alternative forms of a gene that occupy corresponding loci on homologous chromosomes (a pair of chromosomes having corresponding deoxyribonucleic acid [DNA] sequences, with one coming from the mother and the other from the father). • Each allele codes for a specific inherited characteristic. • The long, stringy DNA that makes up genes is spooled within chromosomes inside the nucleus of a cell. (Note that a gene would actually be a much longer stretch of DNA than what is shown here.) • When there are two different alleles, the allele that is fully expressed is the dominant allele. • The other allele that lacks the ability to express itself in the presence of a dominant allele is the recessive allele. • Physical traits expressed by an individual are termed the phenotype, and the actual genetic makeup of the individual is termed the genotype. Chromosomes. • Chromosomes are contained in the nucleus of a cell and occur in pairs. • Humans have 23 pairs of chromosomes; 22 of the 23 pairs of chromosomes are homologous and are termed autosomes. • Autosomes are the same in both males and females. • The sex chromosomes make up the twenty-third pair of chromosomes. • A female has two X chromosomes, and a male has one X and one Y chromosome. • One chromosome of each pair is inherited from the mother and one from the father. • One half of each child's chromosomes (and therefore the genetic makeup) comes from his or her father and one half from his or her mother. DNA • Genes are made up of a nucleic acid called deoxyribonucleic acid (DNA). • DNA stores genetic information and encodes the instructions for synthesizing specific proteins needed to maintain life. • DNA also dictates the rate at which proteins are made. • Every somatic cell in a person's body has the same DNA. • The information in DNA is stored as a code made up of four nitrogenous bases: adenine (A), guanine (G), cytosine (C), and thymine (T). • Human DNA consists of about 3 billion bases, and more than 99% of those bases are the same in all people. • The order (or sequence) of these bases determines the information for building and maintaining an organism. • This is similar to the way letters of the alphabet are used to create words and sentences. DNA • DNA bases pair up with each other, A with T and C with G, to form units called base pairs. • Each base is also attached to a sugar molecule and a phosphate molecule. • Together, a base, sugar, and phosphate are called a nucleotide. • Nucleotides are arranged in two long strands that form a spiral called a double helix. • The structure of the double helix is somewhat like a ladder, with the base pairs forming the ladder's rungs and the sugar and phosphate molecules forming the ladder's vertical sidepieces. • DNA can replicate (make copies of itself). Each strand of DNA in the double helix can serve as a pattern for duplicating the sequence of bases. • When cells divide, each new cell must have an exact copy of the DNA that was in the parent (original) cell. • DNA consists of two long, twisted chains made up of nucleotides. • Each nucleotide contains one base, one phosphate molecule (P), and the sugar molecule deoxyribose (S). • The bases in DNA nucleotides are adenine (A), thymine (T), cytosine (C), and guanine (G). RNA • Ribonucleic acid (RNA) is similar to DNA but with some significant differences. • Like DNA, RNA contains the nitrogenous bases adenine, guanine, and cytosine, but lacks the nitrogenous base thymine and instead contains uracil. • RNA is single stranded and contains ribose instead of deoxyribose sugar. • RNA transfers the genetic information obtained from DNA to the proper location for protein synthesis. Protein Synthesis • Protein synthesis, or the making of proteins, occurs in two steps: transcription and translation. • Transcription is the process by which messenger RNA (mRNA) is synthesized from single-stranded DNA. • The mRNA becomes attached to a ribosome, where translation occurs. • At this point another specialized type of RNA, transfer RNA (tRNA), arranges the amino acids in the correct sequence to assemble the protein. • Once the protein is completed, it is released from the ribosome and is able to perform its specific function in the cell. Mitosis & Meiosis • Mitosis is a type of cell division that results in the formation of genetically identical daughter cells. • Before cell division, the chromosomes duplicate, and each new cell (called daughter cells) receives an exact replica of the chromosomes from the original cell (called the parent cell). • Meiosis occurs only in sexual reproductive cells. • In meiosis the number of chromosomes is reduced, resulting in half of the usual number of chromosomes. • Therefore oocytes and sperm contain only a single copy of each chromosome, whereas all other body cells contain duplicates of each chromosome. Genetic Mutations • A mutation is any change in the usual DNA sequence. • Subtle variations in DNA are called polymorphisms (meaning many forms). • Many of these gene polymorphisms account for slight variations among people such as hair and eye color. • However, some gene variations may result in disease or an increased risk for disease. • These gene variations or changes are referred to as mutations. • A genetic mutation is like a spelling error in a gene's sequence. • For example, in people with sickle cell disease, a substitution of a single base (adenine is replaced by thymine) in a single gene (~-globin gene) causes the disease. • Mutations range in size from a single DNA base (building block) to a large segment of a chromosome. • In sickle cell disease a single gene mutation leads to mutant (incorrect) protein. • The substitution of valine (VAL) for glutamic acid on the globin chain of hemoglobin produces abnormal hemoglobin, hemoglobin S (Hb S). • In response to low 02 levels, the erythrocytes with Hb S stiffen and elongate, taking on a sickle shape. Types of Mutations Genetic mutations occur in two ways. These inherited from a parent (germline mutation) or acquired (somatic mutation) during a person's lifetime. Germline mutations: These mutations are present in the oocyte and sperm cells. This type of mutation is present throughout a person's life in virtually every cell in the body. Acquired (somatic) mutations occur in the DNA of a cell at some time during a person's life. An acquired mutation is passed on to all cells that develop from that single cell. These mutations in somatic cells cannot be passed on to the next generation. Acquired mutations can occur if a mistake is made as DNA replicates during cell division or environmental factors alter the DNA. Mistakes such as deletions, insertions, or duplication of DNA material can occur during replication. In addition to cell division, DNA damage can also occur from environmental factors such as, ultraviolet (UV) radiation can cause DNA damage, leading to skin cancer, toxins in cigarettes can lead to lung cancer. Many chemotherapy drugs used to treat cancer target the DNA of cancer cells and healthy cells, in the process, these drugs increase a person's risk of developing secondary cancers. Cells have built-in mechanisms that catch and repair most of the changes that occur during DNA replication or from environmental damage. However, as we age, our DNA repair does not work as effectively and we accumulate changes in our DNA. Inheritance Patterns Genetic disorders can be categorized into autosomal dominant, autosomal recessive, or X-linked (sex-linked) recessive disorders. If the mutant gene is located on an autosome, the genetic disorder is called autosomal. If the mutant gene is on the X chromosome, the genetic disorder is called Xlinked. Examples of family pedigrees showing inheritance of (A) autosomal dominant, (B) autosomal recessive, and (C) X-linked recessive disorders. Autosomal Disorders Autosomal dominant disorders are caused by a mutation of a single gene pair (heterozygous) on a chromosome. A dominant allele prevails over a normal allele. Autosomal dominant disorders show variable expression. Variable expression means that disease because the normal allele predominates. However, this person is a carrier. Autosomal Recessive Disorders: are caused by mutations of two gene pairs (homozygous) on a chromosome. A person who inherits one copy of the recessive allele does not develop the disease because the normal allele predominates. (However, this person is a Affected individuals may have unaffected parents who are heterozygous for trait. Children of two heterozygous parents have 25% chance of being affected and 50% chance of being carriers. Frequently there is a no family history of disease X-linked Disorders X-linked recessive disorders are caused by a mutation on the X chromosome. Usually only men are affected by this disorder because women who carry the mutated gene on one X chromosome have another X chromosome to compensate for the mutation. However, women who carry the mutated gene can transmit it to their offspring. It is possible for women to have X-linked recessive disorders, and this can occur when an affected male mates with an unaffected female carrier. This points to the importance of testing the carrier status of the female partner of affected males. X-linked dominant disorders do exist, but they are rare Multifactorial Inherited Conditions Multifactorial inherited conditions are caused by a combination of genetic and environmental factors. These disorders run in families but do not show the same inherited characteristics as the single gene mutation conditions. Multifactorial conditions include diabetes mellitus, obesity, hypertension, cancer, and coronary artery disease. Family pedigrees showing three generations: A. Family pedigree suggestive of an autosomal dominant disorder. B. Family pedigree suggestive of an autosomal recessive disorder. C. Family pedigree suggestive of an X-linked recessive disorder. A. Genetic disorders can be caused by a mutation in a single gene (e.g., sickle cell disease, cystic fibrosis, hemophilia]. B. Most genetic disorders are multifactorial genetic disorders caused by a combination of mutations in multiple genes, often interacting with environmental factors. Examples include cancer, diabetes mellitus, obesity, and hypertension. Genetic Disorders A genetic disorder is caused in whole or in part by an alteration in the DNA sequence. As discussed in the section on genetic mutations, genetic disorders can be inherited (person born with altered genetic code) or they can be acquired (e.g., replication errors, damage to DNA from toxins). Genetic disorders can be caused by: i. ii. a mutation in one gene (single gene disorder); mutations in multiple genes (multifactorial inheritance disorder), which are often related to environmental factors; or iii. damage to chromosomes (changes in the number or structure of chromosomes). Classification of Genetic Disorders Single Gene Disorders. Some genetic disorders result from a single gene mutation. Examples of these diseases include cystic fibrosis, sickle cell disease, and polycystic kidney disease. The pattern of inheritance for single gene disorders can be autosomal dominant, autosomal recessive, or X-linked. Single gene disorders are relatively rare compared with more commonly occurring multifactorial genetic disorders such as diabetes mellitus and heart disease. Multifactorial Genetic Disorders. Multifactorial genetic disorders are complex diseases that result from small inherited variations in genes, often acting together with environmental factors Classification of Genetic Disorders Heart disease, diabetes, and most cancers are examples of such disorders. Although many common diseases are usually caused by inheritance of mutations in multiple genes, such diseases can also be caused by rare hereditary mutations in a single gene. In these cases, genetic mutations that cause or strongly predispose a person to these diseases run in a family. These mutations can significantly increase each family member's risk of developing the disease. One example is breast cancer, in which inheritance of a mutated BRCA1 or BRCA2 gene confers significant risk of developing the disease. Epigenetics: Environmental factors can alter the way our genes are expressed (i.e., which genes are "switched" on or off). Epigenetics is the study of the chemical modification of specific genes or geneassociated proteins of an organism. Epigenetic modifications can define how the information in genes is expressed and used by cells. Genetic and environmental factors interact to influence a person's predisposition to different diseases. The expression of genes can be affected both positively and negatively by environmental factors, such as exercise, diet, chemicals, toxins, or smoking. Identical twins, who have the same genetic makeup, do not always develop the same diseases or at the same rate. Twins share the same genes but their environments become more different as they age. This unique aspect of twins makes them an excellent model for understanding how genes and the environment contribute to certain traits, especially complex behaviors and diseases Chromosome Disorders. Chromosome disorders are caused by structural changes within chromosomes or by an excess or deficiency of the genes that are located on chromosomes. For example, Down syndrome is caused by an extra copy of chromosome 21 (called trisomy 21 ), so there are three copies of this chromosome instead of two. In Down syndrome there is no individual abnormal gene on the chromosome. Chronic myelocytic leukemia can be caused by a chromosomal translocation, in which portions of two chromosomes (chromosomes 9 and 22) are exchanged. This translocation is called the Philadelphia chromosome. Genetic Testing Genetic testing includes any procedure done to analyze chromosomes, genes, or any gene product that can determine whether a mutation or predisposition to a condition exists. A person's blood, skin, hair, or saliva can be used to obtain samples for genetic testing; tissues and cells obtained prenatally. Most tests assess single genes and are used to diagnose genetic disorders such as cystic fibrosis or Duchenne muscular dystrophy. Some genetic tests look at rare inherited mutations of otherwise protective genes, such as BRCAl and BRCA2, which are responsible for some types of hereditary breast and ovarian cancers. The results of these tests are used in diagnosing an illness or risk for a disorder and provide the basis for appropriate treatments. Other genetic tests identify people at high risk for conditions that may be preventable, e.g., monitoring for and removing polyps or the entire colon in those inheriting a gene for familial adenomatous polyposis (FAP) have saved many lives. Genetic Testing Cont… Genetic testing of individuals may raise ethical and social issues. However, the Genetic Information Nondiscrimination Act (GINA) protects people from discrimination by employers and health insurance companies. If an individual has genetic testing, it may uncover information that may also affect a family member who was not tested. These individuals are frequently not a part of the decision making process to undergo testing. Similarly, if a whole family is tested, the results may indicate that the biologic relationship is not what the family believed it to be. Some tests are used to help guide HCPs' recommendations for treatment in consultation with the patient (e.g., BRCA testing). Interpreting Genetic Test Results The results of genetic tests are not always straightforward, which often makes them challenging to interpret and explain. When interpreting test results, HCPs need to consider a person's medical history and family history and the type of genetic test that was done. A positive test result means that the laboratory found a change in a particular gene, chromosome, or protein that was being tested. Depending on the purpose of the test, this result may confirm a diagnosis (e.g., Huntington's disease), indicate that a person is a carrier of a particular genetic mutation (e.g., cystic fibrosis), identify an increased risk of developing a disease (e.g., breast cancer), or suggest a need for further testing. Interpreting Genetic Test Results Cont… • A positive result of a predictive or presymptomatic genetic test usually cannot establish the absolute risk of developing a disorder, cannot predict the course or severity of a condition. • In some situations, it is difficult to interpret a positive result because some people who have the genetic mutation being tested never develop the disease. • For example, having the apolipoprotein E-4 (Apo E-4) allele increases the risk of developing Alzheimer's disease. • However, many people who test positive for Apo E-4 never develop Alzheimer's disease. • A negative test result means that the laboratory did not find an altered form of the gene, chromosome, or protein under consideration. • This result can indicate that a person is not affected by a particular disorder, is not a carrier of a specific genetic mutation, or does not have an increased risk of developing a certain disease. • However, it is possible that the test missed a disease-causing genetic alteration, since many tests cannot detect all the genetic changes that cause a particular disorder. • Further testing may be required to confirm a negative result. Use of Genetic Tests Genetic Technology DNA Fingerprinting: begins by extracting DNA from the cells in a sample of blood, saliva, semen, or other appropriate fluid or tissue. Polymerase chain reaction (PCR) is a quick, easy method to provide unlimited copies of a DNA or RNA sequence using only a small amount of sample. PCR involves the artificial replication of a DNA or RNA sequence. The DNA or RNA strands can be separated to form new templates that are used for replication. PCR is an essential technique to finding mutations in genes. It is also used extensively in forensic medicine to identify DNA of criminal suspects by using samples from blood, hair, saliva, and semen. PCR has also been used in paternity testing and finding evidence to free wrongly incarcerated prisoners. PCR can also be used as a confirmatory test in HIV testing. This is especially important when an infant of a mother who is HIV-antibody positive also tests HIV positive. In this situation, it is not known whether the antibodies from the infant's blood are from the baby or the mother. PCR techniques can be used on the baby’s lymphocytes to determine whether the baby is infected with HIY. Genetic Technology Cont… DNA Microarray (DNA Chip). Although all of a person's somatic cells contain identical genetic material, the same genes are not active in every cell. Studying which genes are active and which are inactive in different cell types helps to understand i. ii. how these cells function normally and how they are affected when various genes do not perform properly. Gene expression profiling uses a technology called DNA microrrays (DNA chips). This technology is used to measure the expression levels of large numbers of genes simultaneously or to genotype multiple regions of a genome. The chips are laid out by robots that can position DNA fragments so precisely that more than 20,000 of them can fit on one microscope slide. Then fluorescent-tagged molecules are washed over the DNA fragments. Some molecules (with green fluorescent tags) bind to their complementary sequence. These molecules can be identified because they glow under fluorescent light when scanned using automated equipment. Complete patterns of gene activity can be captured with this technology. Pharmacogenomics & Pharmacogenetics Patients vary widely in their response to drugs. Although the reasons for this are complex, genetic factors may account for a large percentage of patient variability in response to individual drugs. Pharmacogenomics is the study of genomic variation associated with drug responses. Pharmacogenomics examines the entire genome and allows for the identification of variations in multiple genes affecting the drug response. Pharmacogenetics is the study of genetic variability of drug responses related to variations in single genes. Pharmacogenetic and pharmacogenomic studies can potentially lead to drugs that can be tailor-made or adapted to each person's particular genetic makeup. Examples of Pharmacogenomics Application in Drug Therapy Gene Therapy • Gene therapy is an experimental technique that uses genes to treat or prevent disease, this approach is use in treating potentially lethal and disabling diseases that are caused by single gene deficiencies. • Approaches to gene therapy include the following: Replacing a mutated gene that causes disease with a healthy copy of the gene Inactivating, or "knocking out;' a mutated gene that is functioning improperly Introducing a new gene into the body to help fight a disease • A carrier molecule called a vector is usually used to deliver the therapeutic gene to the patient's target cells. • Currently, the most common vector is a virus that has been genetically altered to carry normal human DNA. • The vector can be injected or given IV directly into specific tissue. • The vector unloads its genetic material containing the therapeutic human gene into the target cell. • If the treatment is successful, the new gene will make a functional protein and restore the target cell to a normal state. A diagram of gene therapy is depicted in • Although gene therapy is a promising treatment option for a number of diseases (including inherited disorders, some types of cancer, and certain viral infections), the technique remains risky and is still under study to make sure that it will be safe and effective. • Gene therapy is currently only being tested for the treatment of diseases that have no other cure. Stem Cell Therapy Stem cells are the subject of much discussion because they may offer treatment for many diseases. The use of stem cells may allow for the regeneration of lost tissue and restoration of function in various diseases. Stem cells are unspecialized cells in the body that have the ability to i. ii. remain in their unspecialized state and divide or differentiate and develop into specialized cells such as a brain cell or a muscle cell. In some body organs such as the gastrointestinal (GI) tract and bone marrow, stern cells divide to repair and replace damaged or old tissues. In other organs such as the pancreas and the heart, stem cells divide only under special conditions. Stem cells can be divided into two types: embryonic and adult. Embryonic stem cells come from the embryo at a very early stage in development (4 to 5 days old) and have the ability to become any one of the hundreds of types of cells in the human body. These stem cells can be stimulated to differentiate into any type of tissue (e.g., skin, liver, kidney, blood) found in an adult human. Adult stem cells are undifferentiated cells that are found in small numbers in many adult organs and tissues, including brain, bone marrow, peripheral blood, blood vessels, skeletal muscle, skin, teeth, heart, GI tract, liver, ovarian epithelium, and testes. They are thought to reside in a specific area of each tissue called a stem cell niche. Adult stern cells are more limited than embryonic stem cells in their potential (e.g., stem cells from liver may only develop into more liver cells). The primary roles of adult stem cells in the body are to maintain and repair tissues in which they are found. They are usually thought of as multipotent cells, giving rise to a closely related family of cells within the tissue. For example, skin stern cells produce new skin cells. Hematopoietic stern cells found within the bone marrow are capable of forming all of the various blood cells. These cells are prolific by design and are already being used for bone marrow transplants. Medical researchers are investigating the use of stem cells to repair or replace damaged body tissues, similar to whole organ transplants. Currently not enough donated organs are available to meet the demand for transplants. • In organ transplants, when tissues from a donor are placed into a patient’s body, the patient's immune system may react and reject the donated tissue as "foreign." • However, using stern cells presents less risk of this immune rejection, and the therapy may be more successful. • In addition, stern cells could be directed to differentiate into specific cell types. • They would then become a renewable source of replacement cells and tissues to treat conditions such as Alzheimer's disease, spinal cord injury, stroke, burns, heart disease, diabetes, osteoarthritis, and rheumatoid arthritis. • It may become possible to generate healthy heart muscle cells in the laboratory and then transplant those cells into patients with chronic heart disease. • Whether these cells can generate heart muscle cells or stimulate the growth of new blood vessels is under investigation. Nursing Management: Genetics and Genomics By understanding the profound influence that genetics has on health and illness, you can assist the patient and family in making critical decisions related to genetic issues, such as genetic testing. You also would have to collaborate with the health care team to involve a genetic nurse or a genetic counselor. A genetic nurse is a licensed professional nurse with special education and training in genetics. Nurses with GCN after their names are baccalaureate-prepared licensed registered nurses who have received specialty credentialing as a Genetic Clinical Nurse (GCN). Nurses with APNG after their names are licensed registered nurses with a master's degree who have received specialty credentialing as an Advanced Practice Nurse in Genetics (APNG). As a basic professional nurse, you should be an advocate for patients and families by facilitating access to genetics resources. In addition, you must provide or reinforce accurate information pertaining to genetics or a genetic disease or concern. This information should be tailored to the patient based on culture, religion, knowledge level, literacy, and preferred language. You can identify and assess inheritance patterns and explain them to the patient and family through the use of family pedigrees and Punnett Squares. Maintain the patient's confidentiality and respect the patient’s values and beliefs because genetic information may have major health and social implications. • Genetic testing may raise many psychologic and emotional issues. • Knowledge of carrier status of a genetic disorder may influence a person's decisions for a career, marriage, and childbearing. • It may also affect significant others in grappling with serious life and health care issues. • For example, how should a wife deal with a husband who has tested positive for Huntington’s disease and shows early signs of cognitive impairment but does not yet show any other neurologic manifestations of the disease? Should their children be tested for the disease? • A 43-year-old woman who has a family history of breast cancer and is now diagnosed with breast cancer wants to know if she and her two teenage daughters should have BRCA testing. • What do you tell her? • Furthermore, there are ethical concerns. • Who should know the results of a genetic test? Who should protect the privacy of individuals' test results and prevent individuals from possible discrimination? Genetic information should not be misused to label individuals or particular ethnic groups. close attention must be paid to better understand the psychosocial needs of individuals and societal responses and health care policy related to genetic testing. People may be reluctant to share or disclose information about family history or genetic test results. They fear they are vulnerable to discrimination based on their DNA. Inform your patients about the Genetic Information Nondiscrimination Act (GINA), which protects them from discrimination by employers and health care insurance companies. Nursing Assessment: Family History Family history is one of the strongest influences on a person’s risk of developing genetic-related disorders such as heart disease, stroke, diabetes, or cancer. Even though a person cannot change his or her genetic makeup, knowing the family history can help in the prevention or early diagnosis and treatment of a disorder. For example, it is important to monitor cholesterol levels in a person with a family history of familial hypercholesterolemia. The key features of a family history that may increase a person's risk for genetic-related diseases are • Disease in more than one close relative Disease that does not usually affect a certain gender (e.g., breast cancer in a male) Diseases that occur at an earlier age than expected (e.g., myocardial infarction before age 35) Certain combinations of diseases within a family (e.g., breast and ovarian cancer, heart disease and diabetes) Nursing Assessment: Family History Cont… If a family has one or more of these features, the family history may hold important clues about a person's risk for a genetic disease. People with a family history of disease may have the most to gain from lifestyle changes and screening tests. People cannot change their genes, but they can change unhealthy behaviors (e.g., smoking, poor eating habits). They can also get screening tests to detect diseases and disease risk factors (e.g., elevated cholesterol, hypertension) that can be treated. Genetic Risk Alert boxes in the assessment chapters in this book highlight a patient's risks related to genetic diseases and disorders. Use the information in these boxes when obtaining a nursing history. Nursing Assessment: Family History Cont… Family health history is a written or graphic record of the diseases and health conditions present in one's family. A useful family health history shows three generations of a person's biologic relatives, the age of diagnosis of a disease, and the age and cause of death of deceased family members. A family health history is a useful tool for understanding health risks and preventing disease in individuals and their close relatives. Talk with your own family members about your family’s health history. Record this information and update it periodically so that you and your family members will have organized and accurate information ready to share with your HCP. Family health history information may help HCPs determine which tests and screenings are recommended to help you and your family know your health risk. To help individuals collect and organize their family history information, the Centers for Disease Control and Prevention (CDC) has collaborated with the U.S. Surgeon General and other federal agencies to develop a Web-based tool called My Family Health Portrait (https://familyhistory. hhs.gov/fhh-web/home.action).