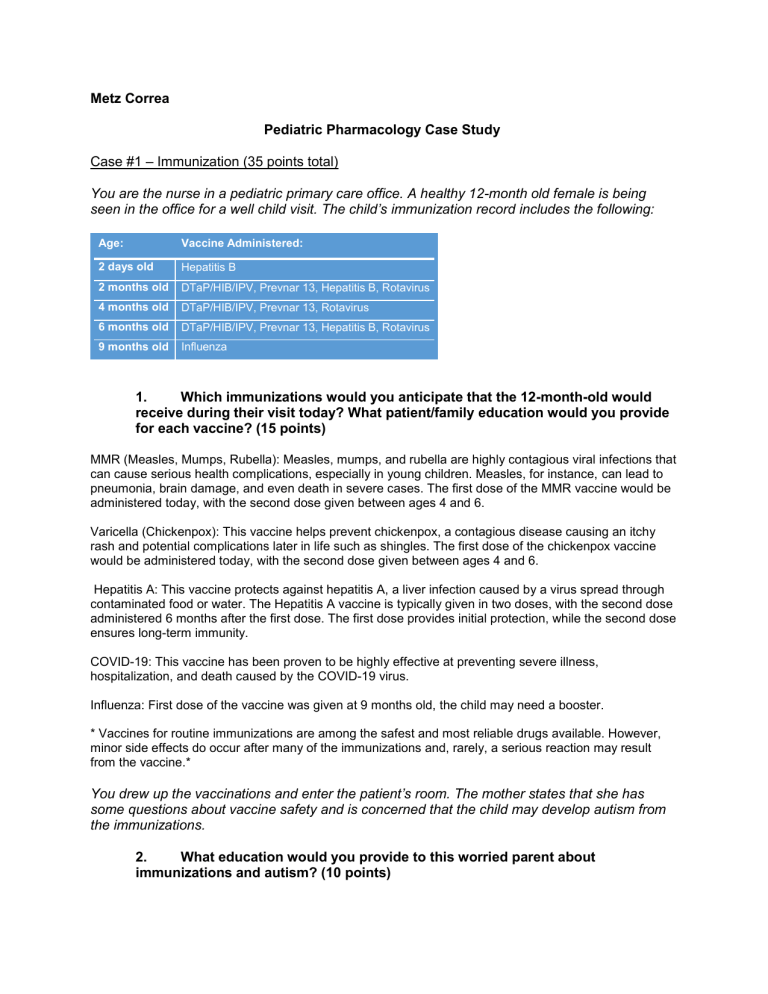
Metz Correa Pediatric Pharmacology Case Study Case #1 – Immunization (35 points total) You are the nurse in a pediatric primary care office. A healthy 12-month old female is being seen in the office for a well child visit. The child’s immunization record includes the following: Age: Vaccine Administered: 2 days old Hepatitis B 2 months old DTaP/HIB/IPV, Prevnar 13, Hepatitis B, Rotavirus 4 months old DTaP/HIB/IPV, Prevnar 13, Rotavirus 6 months old DTaP/HIB/IPV, Prevnar 13, Hepatitis B, Rotavirus 9 months old Influenza 1. Which immunizations would you anticipate that the 12-month-old would receive during their visit today? What patient/family education would you provide for each vaccine? (15 points) MMR (Measles, Mumps, Rubella): Measles, mumps, and rubella are highly contagious viral infections that can cause serious health complications, especially in young children. Measles, for instance, can lead to pneumonia, brain damage, and even death in severe cases. The first dose of the MMR vaccine would be administered today, with the second dose given between ages 4 and 6. Varicella (Chickenpox): This vaccine helps prevent chickenpox, a contagious disease causing an itchy rash and potential complications later in life such as shingles. The first dose of the chickenpox vaccine would be administered today, with the second dose given between ages 4 and 6. Hepatitis A: This vaccine protects against hepatitis A, a liver infection caused by a virus spread through contaminated food or water. The Hepatitis A vaccine is typically given in two doses, with the second dose administered 6 months after the first dose. The first dose provides initial protection, while the second dose ensures long-term immunity. COVID-19: This vaccine has been proven to be highly effective at preventing severe illness, hospitalization, and death caused by the COVID-19 virus. Influenza: First dose of the vaccine was given at 9 months old, the child may need a booster. * Vaccines for routine immunizations are among the safest and most reliable drugs available. However, minor side effects do occur after many of the immunizations and, rarely, a serious reaction may result from the vaccine.* You drew up the vaccinations and enter the patient’s room. The mother states that she has some questions about vaccine safety and is concerned that the child may develop autism from the immunizations. 2. What education would you provide to this worried parent about immunizations and autism? (10 points) Many studies studies have found no credible link between vaccines and autism. Extensive research hasn't found any evidence supporting a correlation between autism and vaccines. All vaccines undergo rigorous testing for safety and efficacy before approval by the CDC for public. The benefits associated with these vaccines far outweigh the extremely low risk of adverse reactions. The mother of the patient appreciates the education that you provided and would like for her child to receive all of the ordered vaccines today. 3. How would you administer each vaccine (which site) and via which route? (10 points) If the child is receiving all 5 vaccines at this visit, they will all be IM injections (except MMR & Varicella which are subcutaneous - 11/27). Each vaccination will be in a separate syringe and in a different location. However, all injections will be given in the child’s left or right Vastus Lateralis. Because there will be 5 vaccinations, another nurse and myself would administer the vaccines together. One nurse would inject two of the five in the right thigh while the other injects the remaining three vaccinations into the left thigh. Case #2 – Exercise induced asthma (35 points total) You are the nurse taking care of a twelve-year old male who has recently been diagnosed with exercise induced bronchospasm. He is on the soccer team and has games/practices three days a week. He has been prescribed a ProAir HFA inhaler. 4. What dose of ProAir would you expect to be ordered and with what directions? Why would we also want to make sure that a spacer has been ordered? (10 points) Dosage: The recommended dosage for a child in this situation is usually 2 puffs (90 mcg per puff) of ProAir inhaler taken 15-30 minutes before exercise. Directions: The directions will include using the inhaler before each soccer practice or game, being that exercise triggers the bronchospasm. The child should inhale the medication as prescribed by the doctor, ensuring proper technique: shake the inhaler exhale completely inhale deeply while pressing the canister Spacer: A spacer should be prescribed along with the inhaler. A spacer is a device that attaches to the inhaler. It helps by coordinating the inhalation and the release of the medication. Using a spacer with an inhaler is very beneficial for children. It will help optimize the delivery of the medication into the airways, especially if the child might have difficulty using the inhaler correctly without it. 5. Describe step-by-step how you would teach the twelve-year-old to administer their ProAir inhaler with a spacer. (10 points) 1. Explain the purpose of the spacer: it helps the medicine reach the lungs more effectively. Demonstrate the spacer and inhaler to the child, explaining that they work together to deliver the medication. 2. Preparing the Inhaler and Spacer: remove the cap from the ProAir inhaler and shake it well. Insert the inhaler's mouthpiece into the spacer. 3. Priming the Inhaler: if it's a new inhaler or hasn't been used for a while, prime it usually by spraying a couple of test sprays into the air. 4. Using the Spacer with Inhaler: have the child stand or sit comfortably, holding the spacer in a horizontal position. Instruct them to take a slow, deep breath and then exhale completely. Have them seal their lips around the mouthpiece of the spacer. Press down on the inhaler canister once to release one puff of medication into the spacer. Have the child breathe in slowly and deeply through their mouth, filling their lungs. Encourage them to hold their breath for about 5-10 seconds or as long as comfortable. Then instruct them to exhale slowly through their mouth. 5. Waiting Period: wait for about 30-60 seconds between puffs if a second puff is needed. Repeat the process if instructed to take more than one puff. 6. Rinsing and Cleaning: remind them to rinse their mouth with water and spit it out to prevent potential side effects like oral thrush. 7. Practice and teach back: allow the child to practice using the spacer with the inhaler while you provide guidance and feedback. Ask them to verbalize the steps for you while completing the task of using their inhaler. The twelve-year-old has a question for you. He doesn’t understand why he doesn’t need to take his new medication everyday. He informs you that his older brother has an inhaler and uses it everyday for asthma. 6. Describe the pathophysiology of exercise induced bronchospasm and compare it to asthma. Also explain the difference between a short acting beta2 adrenergic agonist and asthma control medication. (15 points) Pathophysiology: During exercise, rapid breathing can cause the airways to become dry and lose warmth, leading to irritation. Cool, dry air can cause the airways to contract and become narrower, limiting airflow in and out of the lungs. In susceptible individuals, this irritation triggers the release of inflammatory mediators, resulting in temporary constriction of the smooth muscles around the airways. Exercise induced bronchospasm is triggered by exercise, it is a response to physical exertion. Asthma can occur even without exercise, is a chronic condition with inflammation and airway hypersensitivity. Difference between short acting beta2 adrenergic agonist and asthma control medication: Short-Acting Beta2 Adrenergic Agonists (SABA): Medications like albuterol (e.g., ProAir, Ventolin) are SABAs. They work rapidly by relaxing the smooth muscles around the airways, allowing them to open quickly. These are rescue inhalers used to relieve acute symptoms of bronchospasm in both EIB and asthma attacks. Asthma Control Medications: These medications, including inhaled corticosteroids, long acting beta2 agonists (LABAs), leukotriene modifiers, and others, are used regularly to control and manage asthma symptoms by reducing inflammation, preventing airway constriction, and minimizing the frequency and severity of asthma attacks. They are taken daily to maintain better control and prevent exacerbations rather than providing immediate relief during an attack. While SABAs provide quick relief during acute episodes, asthma control medications are aimed at managing underlying inflammation and providing long-term control of asthma symptoms, reducing the need for rescue medication. Both types of medication play essential roles in managing asthma effectively. Case #3 – Over the Counter medication (30 points total) You are the triage nurse in a busy pediatric practice. You are on the phone with the parent of a 4-month-old infant and 3-year-old child. The parent reports that both of her children have just developed a mild cough and fever. After you provide nursing triage, you determine that the children are well enough to be observed at home and do not need an appointment to be seen at this time. The mother wants to know how to treat symptoms and what over the counter medications she can use to help treat her children’s symptoms. 7. What home care advice would you provide to this parent? What over the counter products would you suggest she use for each child and why? Provide care advice/OTC suggestions for the 4-month old and 3-year-old separately. (15 points for each child) For the 4-Month-Old Infant: Make sure the baby gets plenty of rest and stays hydrated with breastfeeding or formula. Monitor wet/dirty diapers. Use a humidifier in the room to help alleviate congestion. Elevate the baby's head slightly while sleeping to aid breathing (elevate the crib mattress from underneath, avoid putting blankets or pillows in the crib). Constantly check on their temperature and observe for any changes in behavior or breathing difficulties. Over-the-Counter (OTC) Suggestions: Acetaminophen: Use acetaminophen if the baby has a fever. Dosage should be based on weight and age, following the instructions provided on the package. Saline Nasal Drops: Use saline drops to help relieve nasal congestion. A few drops in each nostril can help loosen mucus and facilitate easier breathing. Suctioning the mucus will also provide relief. For the 3-Year-Old Child: Encourage rest and adequate fluid intake with water, juice (not too much due to sugar intake), or popsicles. Use a cool-mist humidifier in their room to ease congestion. Encourage the child to blow their nose gently to clear any mucus that is blocking their airway. Over-the-Counter (OTC) Suggestions: Acetaminophen: Use acetaminophen if the child has a fever. Dosage should be based on weight and age, following the instructions provided on the package.