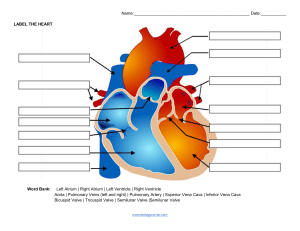
Czarina Beatriz SG. Lim BSN 3 REVIEW OF CARDIOVASCULAR ANATOMY AND PHYSIOLOGY DEFINE/DESCRIBE THE FOLLOWING TERMS ● Atria - The upper two chambers of the heart that receive blood returning from the body and lungs. ● Diastole - The phase of ventricular relaxation leading to ventricular filling. ● Endocardium - The inner layer of the heart composed of endothelial tissues, lining the heart and valves. ● Epicardium - The outer layer of the heart. ● Myocardium - The heart's muscular layer responsible for pumping. ● Pericardium - The thin, fibrous sac enveloping the heart with two layers. ● Systole - The phase of ventricular contraction leading to blood ejection into the pulmonary artery and aorta. ● Ventricles - The lower, thick-walled chambers of the heart pumping blood out forcefully. ● Afterload - Resistance to blood ejection from the ventricle. ● Cardiac output - The volume of blood pumped by each ventricle per minute. ● Depolarization - Electrical activation of a cell caused by sodium influx and potassium exit. ● Ejection fraction - The percentage of end-diastolic blood volume ejected from the ventricle with each heartbeat. ● Preload - The stretch of cardiac muscle fibers at the end of diastole. ● Repolarization - Cell return to resting state, involving potassium reentry and sodium exit. ● Stroke volume - The blood volume ejected from one ventricle per heartbeat. DEFINE AND DESCRIBE THE FOLLOWING VALVES: ● Aortic valve - It is a semilunar valve located between the left ventricle and the aorta. It is composed of three leaflets, which are shaped like half-moons. Czarina Beatriz SG. Lim BSN 3 ● Mitral valve - It is the atrioventricular valve located between the left atrium and left ventricle which prevents the blood from leaking back into the left atrium during ejection (systole). ● Pulmonary valve - It is one of the two semilunar valves, and the valve between the right ventricle and the pulmonary artery. ● Tricuspid valve - It is one of the valves that separates the atria from the ventricles. It is also composed of three cups or leaflets, separating the right atrium from the right ventricle. DEFINE AND DESCRIBE THE FOLLOWING PARTS OF THE HEART THAT FUNCTIONS IN THE CONDUCTION PATHWAY ● The Bundle of His - also referred to as the atrioventricular bundle, represents the initial segment of the AV node that traverses the fibrous trigone and extends into the membranous part of the interventricular septum. In a normally functioning heart, the AV bundle permits only the forward movement of action potentials, disallowing the backward transmission of impulses. Additionally, it receives supply from the interventricular branches of the coronary artery. ● The SA Node - known as the sinoatrial node, serves as the heart's primary pacemaker and is situated in the connective tissue between the superior vena cava and the right atrium. Employing the internodal pathways, it generates 60 to 100 impulses per minute under normal conditions, with the rate potentially changing based on the body's metabolic response. These impulses induce electrical stimulation, leading to the subsequent contraction of the atria. ● The AV Node - functioning as the secondary pacemaker, is positioned in the right atrial wall near the tricuspid valve. This structure acts as a bridge between the electrical systems of the atria and ventricles, imparting electrical impedance from the atria and serving as an intrinsic pacemaker in the absence of other pacemaker activity. ● Purkinje fibers - also known as endocardiac branches, are distributed throughout the subendocardiac layer. They transmit impulses at a rate six times faster than ventricular muscles and 150 times faster than AV nodal fibers, attributed to the abundance of gap junctions they contain compared to AV nodal cells and the surrounding myocytes. Describe the following properties of the heart in terms of its conduction system function: ● Automaticity - The heart's ability to contract without direct nervous system stimulation. Czarina Beatriz SG. Lim BSN 3 ● Excitability - The capacity of a cardiac cell to generate an action potential in response to depolarization. ● Conductivity - The ability of muscle cells to transmit electrical impulses from cell to cell. ● Refractoriness - Tissue response to the introduction of premature stimuli. Heart sounds are produced by the closure of the atrioventricular valves. Describe the following: ● S1 (lub) - It is easily discernible and serves as a reference point for the entire cardiac cycle. It is also known as the "first heart sound" and commonly referred to as the "lub" sound, tends to be most pronounced at the apical area. ● S2 (dub) - The pulmonic component of S2 is softer and is best heard over the pulmonic area. It is also identified as the "second heart sound" or the "dub" sound, comprises the aortic component, which is loudest over the aortic and pulmonic regions. ● S3 (DUB) - The rhythmic sequence "Lub-dub-DUB" is employed to replicate the abnormal sound of a beating heart when an S3 is present. It manifests early in diastole during the rapid ventricular filling phase as blood moves from the atrium into a non-compliant ventricle. It follows immediately after S2. ● S4 (LUB) - occurs late in diastole, just before the emergence of S1, during atrial contraction as blood forcefully enters a noncompliant ventricle. This resistance to blood flow is a consequence of ventricular hypertrophy, which may arise from conditions such as hypertension, CAD, cardiomyopathies, aortic stenosis, and various other ailments. The mnemonic "LUB lub-dub" is used to mimic this gallop sound. S4, originating in the left ventricle, is examined using the bell of the stethoscope over the apical area with the patient in the left lateral position. ● Gallops - are discernible during tachycardia, where all four sounds, such as "LUB lub-dub DUB," amalgamate into a prominent sound. ● Friction rubs - It produces a harsh, grating sound detectable in both systole and diastole. The sound results from the abrasion of inflamed pericardial surfaces due to pericarditis. Given the potential confusion with murmurs, it is essential to carefully identify and differentiate the sound from murmurs that may be present in both systole and diastole. These are characterized and consequently described by several characteristics such as the following: ● Localization - Identifying the precise location of a murmur aids in determining the specific structures responsible for producing abnormal sounds. Czarina Beatriz SG. Lim BSN 3 ● Timing - Described in relation to its occurrence within the cardiac cycle, such as systole or diastole. Further differentiation involves pinpointing the exact phase of systole or diastole during which the murmur is audible. ● Intensity - Murmurs are evaluated using a grading system to characterize their loudness. Grade 1: Extremely faint, challenging for inexperienced clinicians to detect. Grade 2: Quiet but easily discernible by experienced clinicians. Grade 3: Moderately loud. Grade 4: Loud, potentially associated with a thrill. Grade 5: Very loud, audible even with the stethoscope slightly off the chest, often associated with a thrill. Grade 6: Extremely loud, detectable with the stethoscope off the chest, and typically associated with a thrill. ● Pitch - Describing the frequency of the sound as high, medium, or low-pitched. High-pitched murmurs are best heard with the stethoscope's diaphragm, while low-pitched sounds are detected using the bell, lightly placed on the chest wall. ● Quality - Depicting the sound that the murmur resembles, with variations such as rumbling, blowing, whistling, harsh, or musical. For instance, murmurs resulting from mitral or tricuspid regurgitation may exhibit a blowing quality, whereas mitral stenosis produces a rumbling sound. ● Radiation - Referring to the spread of the murmur from its point of maximum intensity to other areas in the upper chest. The examiner determines the presence of radiation by carefully listening to adjacent areas of the heart where the murmur is most pronounced. If radiation is detected, the precise location is detailed. TRACE THE FOLLOWING BY SHOWING IT IN THE FORM OF A FLOWCHART) ● Pulmonary circulation ● Systemic circulation Czarina Beatriz SG. Lim BSN 3 References: Crawford, P. T., Arbor, T. C., & Bordoni, B. (2022, September 8). Anatomy, Thorax, Aortic Valve. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK559384/#:~:text=It%20is%20between%20the% 20left,connected%20to%20the%20heart%20wall. Heart Valves, Anatomy and Function | ColumbiaDoctors - New York. (2018, March 21). ColumbiaDoctors. https://www.columbiadoctors.org/treatments-conditions/heart-valves-anatomy-and-functi on Hinkle, J. L., & Cheever, K. H. (n.d.). Brunner & Suddarth’s Textbook of Medical-surgical Nursing. LWW. Mitral Valve Function. (2015). Mitral Valve Repair Center. https://www.mitralvalverepair.org/mitral-valve-function