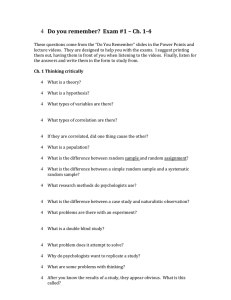
Hypnotic Drugs and Their Effectiveness All-night EEG Studies of Insomniac Subjects Anthony Kales, MD; Clyde Allen, MA; Martin and Joyce D. Kales, MD, Los Angeles T HE results of previous studies with normal subjects in our laboratory suggested that 1,000 mg of chloral hydrate (Noctec) and 30 mg of flurazepam (Dalmane) were effective in enhancing sleep: chloral hydrate appeared to induce sleep while flurazepam induced and maintained sleep.1 The aim of the present study was to further evaluate the effectiveness of 1,000 mg of chloral hydrate and 30 mg of flurazepam by using insomniac subjects and a twoweek drug administration period as part of a 22-night protocol. This contrasted with our previous use of normal subjects and a three-night drug administration period as part of an eight-night schedule. The use of insomniac subjects provides a clear-cut way in which to study the effectiveness of sleep medications. The two-week drug administration period provides not only a more rigorous evaluation of whether drugs produce sleep stage alterations, but also allows for the determination of the length of the effectiveness of the drugs. In order to compare the effectiveness of drugs which do not significantly alter REM sleep (1,000 mg of chloral hydrate and 30 mg of flurazepam) with one which does produce marked alterations in this sleep phase,2 500 mg of glutethimide (Doriden) was also administered using the 22-night protocol. Methods Insomniac subjects for this experiment were obtained through two general sources: (1) a pool of subjects obtained for other studies in our lab and (2) through public advertisements for individuals with moderate to severe insom¬ nia. Potential subjects from either source were screened carefully to eliminate those who were Accepted for publication April 13, 1970. From the departments of psychiatry (Dr. A. Kales, Mr. Allen, and Mr. Scharf), psychology (Mr. Allen), and anatomy (Dr. J. Kales), Sleep Research and Treatment Facility, and the Brain Research Institute (Dr. A. Kales), UCLA School of Medicine, Los Angeles. Reprint requests to UCLA Sleep Research and Treatment Facility, 760 Westwood Plaza, Los Angeles 90024 (Dr, A, Kales). B. Scharf: not in good general health, used medications of any type, appeared to have severe psychopathological disturbances, or did not, by history, seem to have significant insomnia. In these studies we chose primarily those individuals who had moderate to severe difficulty falling asleep—that is, required more than one hour at least four times per week. Design of Study.—Flurazepam was studied initially, using four insomniac subjects. Subse¬ quently chloral hydrate and glutethimide were studied in four additional subjects who under¬ took the 22 nights of experimental study on two separate occasions. An interval of four weeks separated these two series of 22 nights. During the drug administration period of the first 22-night study, two of the subjects re¬ ceived 500 mg of glutethimide while the other two subjects received 1,000 mg of chloral hy¬ drate. In the second series of 22 nights, each subject received the alternate drug. Thus, each drug was evaluated with each subject for a 22-night series. The experimental protocol for each of these three 22-night series was as follows: Nights 1-4 Protocol Substance Placebo Administration Baseline in laboratory 5-7 Active 8-15 Active 16-18 Active drug laboratory 19-22 Placebo Withdrawal in drug drug Taken in laboratory Taken in home Taken in laboratory The first laboratory night in each series allowed for adaptation and readaptation, was re¬ spectively. Throughout every study, the subjects were instructed not to nap, significantly vary their level of physical activity, or use any drugs. During the flurazepam study, one of the sub¬ jects indicated that he had been intermittently taking glutethimide on his own, thereby com¬ plicating our results. For this reason, data re¬ ported for flurazepam are for three subjects. On laboratory nights, the subjects were allowed to sleep for 8V2 hours and were continuously monitored to obtain an all-night electroenceph¬ alogram (EEG), electromyograrri (EMG), and Downloaded From: http://archpsyc.jamanetwork.com/ by a University of Otago Library User on 11/21/2016 electrooculogram (EOG). In the laboratory, the placebo or active drug was given at lights out. For the home trials, the subjects were instruct¬ ed to take the capsule specified for that night at bedtime and to set the alarm clock for 8% hours from the time they went to bed. By these measures, we attempted to prevent any signif¬ icant excess or limitation of sleep while at home. Subjects were asked each morning to briefly assess whether their sleep the previous night had been better, worse, or "average" compared to their accustomed pattern prior to the study. In each study, the placebo and drug were administered on a double-blind basis. In addi¬ tion, each subject's all-night sleep recordings were scored independently of knowledge of the experimental conditions.3 The parameters mea¬ sured included those related to sleep induction (sleep latency) and sleep maintenance (wake time after sleep onset and total number of awakenings). Other parameters measured relat¬ ed to possible sleep pattern alterations and included quantifications of each sleep stage, the interval between sleep onset and first REM period (REM latency), and the total number of REM periods. Results Sleep Induction and Maintenance.—Ta¬ ble 1 compares the three hypnotic drugs in terms of their effects on sleep induction and maintenance. One Thousand Milligrams of Chloral Hy¬ drate.—On the first three nights of chloral hydrate administration (nights 5 to 7) the mean values for sleep latency showed a sig¬ nificant decrease as compared to baseline nights 2 to 4 (31.3 vs 52.5 minutes). By nights 16 to 18, sleep latency had returned to baseline levels while on withdrawal nights 19 to 22, sleep latency was slightly increased above baseline values. In regard to wake time after sleep onset and the number of awakenings, there was no change as a function of initial drug administration (nights 5 to 7). With continued administra¬ tion, however, a decrease resulted in both parameters on drug nights 16 to 18. This effect was also noted through withdrawal nights 19 to 22. While taking the drug at home (nights 8 to 15), subjects reported that sleep effectiveness was diminishing rap¬ idly, and this was associated with their com¬ plaint that falling asleep was becoming pro¬ gressively more difficult. Five Hundred Milligrams of Glutethi¬ mide,—With glutethimide administration on nights 5 to 7, the mean values for sleep latency showed a significant decrease as compared to baseline nights 2 to 4 (38.0 vs 76.2 minutes). While taking the drug at home (nights 8 to 15) subjective evaluations indicated that effectiveness had diminished quickly, and on laboratory nights 16 to 18 sleep latency was actually observed to be slightly above baseline values. On withdraw¬ al nights 19 to 22, sleep latency decreased slightly to below the baseline level. In re¬ gard to wake time after sleep onset and number of awakenings, there was a slight increase in both parameters on drug nights 5 to 7. By drug nights 16 to 18, both values had returned to baseline. Following with¬ drawal (nights 19 to 22), wake time after sleep onset again increased above baseline; the number of awakenings after sleep onset showed, however, no further change. This meant that although subjects were awaken¬ ing no more often than they were while taking the drug, they were staying awake longer. Thirty Milligrams of Flurazepam.—On both sets of drug nights, 5 to 7 and 16 to 18, there was a significant decrease in sleep latency, wake time after sleep onset, and number of awakenings as compared to base¬ line nights 2 to 4. In addition, all three parameters remained moderately decreased on withdrawal nights 19 to 22. The subject reports indicated that sleep effectiveness had continued throughout drug nights 8 to 15; they felt they were falling asleep and staying asleep better than was their accustomed prac¬ tice prior to entering the study. Sleep Stage Alterations.—One Thousand Milligrams of Chloral Hydrate.—With chloral hydrate administration (5 to 7 and 17 and 18) and withdrawal (19 to 22) nights there were only slight changes in the total nightly amount of REM sleep (Table 2). (Night 16 was not included in the aver¬ ages for the second set of drug nights since we have found that subjects show readaption to the laboratory consisting of a de¬ crease in REM sleep.4 This readaption phenomenon occurred with each of the three groups of subjects when they returned to the laboratory on night 16.) On the first set of drug nights, the percentage and absolute amount of REM sleep was similar to base¬ line levels. On the second set of drug nights, REM sleep was slightly decreased compared to baseline levels. Following drug withdraw- Downloaded From: http://archpsyc.jamanetwork.com/ by a University of Otago Library User on 11/21/2016 Table 1.—Effectiveness of Medications on Sleep Induction and Maintenance Drug Baseline Withdrawal (Nights 2-4) (Nights 5-7) (Nights 16-18) (Nights 19-22) Wake time after sleep onset Total No. of wakes Total sleep time 52.5 21.4 9.2 437.8 85.6 31.3 23.6 9.1 455.4 89.3 48.3 12.2 5.7 449.4 88.1 61.2 8.8 5.7 440.0 86.2 Total No. of wakes 36.2 14.3 4.1 459.2 90.0 13.9* 5.0 2.7 491.7 96.4 18.8 5.3 2.4 485.2 95.1 25.4 10.4 3.2 470.4 92.2 76.2 13.7 6.8 421.9 82.7 38.0 19.7 10.9 452.4 88.7 88.3 14.3 6.8 407.4 79.8 62.9 and Dose Chloral Drug Hydrate (1,000 mg) Sleep latency Percent sleep time Flurazepam (30 mg) Sleep latency Wake time after sleep onset Total sleep time Percent sleep time Glutethimide (500 mg) Sleep latency Wake time after sleep onset Total No. of wakes Total sleep time Percent sleep time * P<0.05. (All comparisons related means.) are with baseline nights 2 to 4. The statistic used was Table 2.—Effect of 1,000 mg of Chloral Hydrate (No. the Student's f-test for = Sleep Parameters REM 22.6 on Sleep (99.4) Percent sleep stages REM sleep No. of REM latency* periods Nights 19-22 Parameters* 22.5 20.8 (102.4) (94.9) 24.4 (107.6) 7.0 7.0 6.0 6.2 60.4 61.3 62.1 59.8 7.9 3.2 6.8 5.7 3.2 3.5 116.7 129.3 3.7 3.7 Mean REM Minutes First one-third Middle one-third Last one-third Total Withdrawal Nights 17-18 Nights 5-7 cor¬ 4) Drug Baseline Nights 2-4 Effects 23.3 6.5 423.9 83.1 by Thirds 138.3 3.3 of Night 11.7 5.6 5.3 30.1 40.6 29.1 57.6 99.4 56.2 102.4 94.9 60.5 6.3 3.3 107.0 3.7 12.2 34.1 61.3 107.6 * Numbers in parentheses represent the absolute values in minutes of REM sleep. REM sleep latency is also expressed in minutes. al, both the percentage and absolute amount al, but none of these changes was statistical¬ of REM sleep were slightly increased above ly significant. baseline. Five Hundred Milligrams of Glutethi¬ When REM sleep was evaluated by com¬ mide.—On drug nights 5 to 7 there was a paring absolute amounts in each third of the marked decrease in both the percentage and night to corresponding baseline values, the the absolute amount of REM sleep (Table slight suppression on nights 17 and 18 and 3). This decrease was maintained through slight increase on nights 19 to 22 were both the next set of drug nights (17 and 18). found to occur in the first two thirds of Following drug withdrawal (nights 19 to those respective nights. 22), there was a marked increase above Chloral hydrate administration and with¬ baseline levels in both the percentage and drawal did not produce any changes in other absolute amount of REM sleep. When drug sleep stages or the total number of REM nights (5 to 7 and 17 and 18) were further periods. REM sleep latency was slightly evaluated by examining each third of the increased on both sets of drug nights and night, it was noted that the majority of slightly decreased following drug withdraw- REM suppression had occurred in the first Downloaded From: http://archpsyc.jamanetwork.com/ by a University of Otago Library User on 11/21/2016 Table 3.—Effect of 500 mg of Glutethimide Sleep REM Effects 21.3 = 4) Drug Baseline Nights 2-4 Parameters (No. Withdrawal Nights on Sleep (88.0) 5-7 Nights 17-18 Nights 19-22 18.3 27.0t (114.0) Parameters* 14.4t (65.5) 6.0 (73.8) 8.7 5.5 6.1 66.3 66.4 56.5 6.6 6.0 7.3 6.3 3.9 4.1 3.2 REM sleep latency* 130.5 138.4 101.4 179.2 No. of REM periods 3.3 3.3 4.1 3.3 Mean REM Minutes by Thirds of Night First one-third 6.9 6.5 18.0 4.2 Middle one-third 22.0 33.6 33.5 16.4 47.6 Last one-third 62.4 44.9 88.0 114.0 Total 65.5 73.8 * Numbers in parentheses represent the absolute values in minutes of REM sleep. REM sleep latency is also expressed in minutes. 2 to are with baseline P<0.05. (All comparisons 4. The statistic used was the Student's f-test for cor¬ nights related means.) Percent sleep stages 62.0 Table 4.—Effect of 30 mg of Flurazepam (No. Nights 5-7 Nights REM Effects 18.2 on REM sleep latency* No. of REM periods First one-third Middle one-third Last one-third Total Nights 17-18 Withdrawal 19-22 Nights Sleep Parameters* (84.0) Percent sleep stages 3) Drug Baseline 2-4 Sleep Parameters = 3.0 64.0 7.5 7.3 104.1 3.7 Mean REM Minutes 15.4 32.3 36.3 84.0 18.9 18.3 19.6 (93.0) (88.5) (91.7) 3.6 64.3 9.1 4.1 95.0 4.0 by Thirds of Night 11.4 30.9 50.7 93.0 2.2 6.6 76.3 3.0 69.9 0.2 3.9 0.0 126.5 3.6 117.3 3.5 7.3 18.9 28.5 44.3 26.5 54.7 88.5 91.7 Numbers in parentheses represent the absolute values in minutes of REM sleep. REM sleep expressed in minutes. * latency is also two thirds of the night. Following drug percentage of REM sleep was similar to withdrawal, increases in REM sleep were baseline levels while the absolute amount found in the first and last thirds. Glutethimide administration further re¬ sulted in an increase in REM latency on the first set of drug nights, while withdrawal of the drug produced a decrease. The shifts in REM sleep were accompanied primarily by a reciprocal change in stage 2 sleep. Thirty Milligrams of Flurazepam.—The administration of flurazepam (nights 5 to 7 and 17 and 18) and its withdrawal (19 to 22) resulted in only slight changes in the total nightly amount of REM sleep (Table 4). On the first set of drug nights, the was increased due to an increase in total sleep time. On the second set of drug nights, both the percentage and absolute REM val¬ essentially the same as baseline. Following drug withdrawal, both the per¬ centage and absolute amounts of REM sleep were slightly increased above baseline. When REM sleep was evaluated by com¬ paring absolute amounts in each third of the night to corresponding baseline values, REM sleep was increased in the last third of both sets of drug nights and the withdrawal nights. In addition, on the second set of ues were Downloaded From: http://archpsyc.jamanetwork.com/ by a University of Otago Library User on 11/21/2016 drug nights, REM sleep was decreased in the first two thirds. There were no significant changes be¬ tween conditions in REM latency or in the total number of REM periods. Flurazepam administration produced a marked, progres¬ sive decrease in stage 4 sleep which was maintained through the withdrawal nights (19 to 22). The percentage of stage 3 sleep increased slightly on the first set of drug nights and decreased considerably on the second set of drug nights, and this decrease was maintained following drug withdrawal. On the second set of drug nights and the withdrawal nights, the decreases in stages 3 sleep stage alterations with chloral hydrate corresponds to our findings in short-term studies with normal sleepers.1 The degree of REM suppression and rebound produced with glutethimide administration and with¬ drawal, respectively, was also similar to changes attributed to this drug in our shortterm study.2 In addition, it should be noted that the level of withdrawal REM rebound in insomniacs following our two-week drugadministration was only slightly greater than the REM rebound seen in our eightnight study in normal subjects. This sug¬ gests that there is probably a point at which increased REM suppression will not pro¬ and 4 sleep were accompanied primarily by duce increased rebound, and further studies into the implications of this phenomenon a reciprocal change in stage 2 sleep. are indicated. Comment It has been assumed that when REM Drug Effectiveness.—The results of this suppressant hypnotics are administered at a study showed that 30 mg of flurazepam was single clinical dose, the total REM time effective in insomniac subjects both in in¬ returns to baseline after a few consecutive ducing and maintaining sleep throughout nights of drug administration. Although this the two-week administration period and for has been the case with many hypnotic drugs several withdrawal nights as well. Both 1,- we have studied in our laboratory, we first 000 mg of chloral hydrate and 500 mg of noted an exception in our short-term glu¬ glutethimide significantly decreased sleep la¬ tethimide evaluation where REM suppres¬ tency on the first set of drug nights (5 to 7). sion remained consistent through three The effectiveness of these drugs, however, nights of drug administration.2 The current appeared to diminish rapidly when the sub¬ series of experiments indicates that even jects went home and continued drug admin¬ after two weeks of glutethimide administra¬ istration (8 to 15). This could not have been tion, the REM suppression effected by this due simply to the fact of sleeping at home drug remains consistently below baseline. since, with both drugs, sleep latency was at This demonstrates that the REM suppres¬ baseline levels upon return to the laboratory sion produced by a single clinical dose of a on drug nights 16 to 18. Neither chloral hypnotic drug can persist long after the first hydrate nor glutethimide appeared to im¬ night or two of drug administration. Simi¬ sleep maintenance consistently larly, we reported that the long term use of prove throughout the drug-administration period either of two hypnotic drugs, in multiple although it should be noted that difficulty in clinical doses (1,000 mg of glutethimide and staying asleep was not the primary com¬ 300 mg of pentobarbital) resulted in a per¬ sistent marked suppression of REM sleep.5 plaint in these subjects. Following withdrawal of flurazepam, Both this and the current studies clearly there remained a carry-over effect in terms demonstrate that one cannot make the gen¬ of sleep induction and sleep maintenance eralization that REM suppression with hyp¬ through several withdrawal nights. This in notic drugs does not persist beyond the ini¬ itself probably facilitates a smooth transi¬ tial few nights of drug administration. tion through the withdrawal process and is The marked decrease in stage 4 sleep an advantage. However, this also raises the produced by glutethimide in normal possibility that, as with any hypnotic drug, sleepers2 was not apparent in the current there may be a carry-over effect of the drug study where only a minimal decrease was into the daytime following its use at night. noted. The marked decrease to absent stage The possibility of the drug carry-over 4 sleep with flurazepam administration was affecting daytime levels of performance similar to that seen in normal subjects. In should be evaluated in future studies with contrast to REM sleep rebound following withdrawal of REM suppressant drugs, no all hypnotic drugs. Sleep Stage Alterations.—The minimal rebound in stage 4 sleep was noted following Downloaded From: http://archpsyc.jamanetwork.com/ by a University of Otago Library User on 11/21/2016 withdrawal of flurazepam. Flurazepam pro¬ any claims can be made concerning its use duced only minimal changes in REM sleep as a hypnotic, either in terms of sleep efficacy in this study whereas it resulted in slight or a lack of REM sleep alterations. The present study with 1,000 mg of chlor¬ REM suppression in normal subjects.1 In neither study was there a REM rebound al hydrate indicates that its effectiveness in inducing sleep is limited to several nights. If following withdrawal of flurazepam. a patient presents only a mild transient number of are altera¬ There a sleep stage tions in these studies which merit future insomnia either chloral hydrate or fluraze¬ investigation. While the change in REM pam could be used. Since, however, our in¬ sleep distribution by thirds of the night by vestigations with 30 mg of flurazepam show flurazepam may suggest an initial suppres¬ that it effectively induces and maintains sion and a later rebound within a given drug sleep for at least two weeks, it would be the night, it should also be noted that the base¬ more ideal drug if the insomnia were more line distribution of REM sleep in the flura¬ severe or extended. While studies involving two-week drug zepam subjects was not normal. The amount of REM sleep in the last third for the administration are adequate in most cases baseline nights for these subjects was much for judging the effectiveness and sleep-alter¬ lower than that usually seen, and may be a ing characteristics of a drug, they do not tell reflection of their insomnia. We have subse¬ us about the effects of the drug when taken quently evaluated flurazepam in eight addi¬ over a longer interval, especially on a longtional insomniac subjects. In this study the term basis. In this regard, long-term studies drug only minimally to slightly supressed of hypnotic drugs are necessary to demon¬ REM sleep, without REM rebound follow¬ strate if extended use produces sleep stage ing withdrawal, produced a marked decrease alterations not found in shorter term in stage 4 sleep, and was quite effective both studies. Additionally, it would be possible to in inducing and in maintaining sleep. Fur¬ determine by such long-term investigations ther, no suppression or rebound within ac¬ whether the effectiveness of a hypnotic drug tual drug nights were noted in this study, so is maintained. In choosing a hypnotic drug, the general we have concluded that the changes in the current study were related to a redistribu¬ physician can now rely on data which is tion of sleep following drug administration. considerably more objective and quantified We are now in the process of evaluating than was the information previously avail¬ whether the drug affects phasic aspects of able through the traditional methods of clin¬ REM sleep, ie, the number and frequency of ical observation. The evaluation of a hyp¬ the eye movements themselves. notic drug should include the following Future studies should evaluate whether considerations: (1) does the drug effectively long-term use of either chloral hydrate or induce or maintain sleep, and if so for how flurazepam produces a significant REM sup¬ long; (2) does the drug produce sleep stage pression or REM rebound following with¬ alterations, particularly REM sleep rebound drawal. In the current study, a REM re¬ following withdrawal; (3) if the subject is bound was noted following withdrawal of awakened during the period of drug action, each drug but this was less than the 10% does the drug significantly affect perfor¬ criterion we arbitrarily feel is significant.1 mance, and (4) are mood and performance Clinical Implications.—The differential significantly affected the next day following hypnotic effectiveness of 30 mg of fluraze¬ drug use? We have extensively evaluated the pam and 1,000 mg of chloral hydrate indi¬ first two aspects, while studies are currently cates that drugs can selectively induce sleep, in progress relating to the latter two areas. maintain sleep, or induce and maintain Technical Considerations and Interpreta¬ sleep while only minimally affecting REM tion of Data.—The sleep laboratory pro¬ sleep. We feel that any hypnotic drug which vides an excellent means for objectively and in short-term studies appears to be effective rigorously evaluating whether or not a drug and does not significantly suppress REM alters sleep patterns, and, in addition, par¬ sleep must also be studied, using insomniac ticularly with hypnotic drugs, a means of subjects and a longer term protocol, before objectively determining their effectiveness. Downloaded From: http://archpsyc.jamanetwork.com/ by a University of Otago Library User on 11/21/2016 In a previous publication,6 we emphasized that the validity of such sleep laboratory studies depends on the particular methodol¬ ogy used. In order to allow for proper adap¬ tation (or readaptation if necessary), and to determine initial and cumulative drug effects as well as withdrawal changes, we have recommended recording consecutive baseline, drug, and withdrawal nights, in¬ cluding at least several nights of drug ad¬ ministration. We also recommended that all sleep stages be scored, different drug doses studied, and special protocols and appropri¬ ate patients used when studying drug effectiveness. In addition to the methodology of the sleep-laboratory—drug studies, we feel that the interpretation of these data, especially in promotional material for various drugs, is another area which should be carefully considered.6 We do not know the spécifie significance of the presence or absence of a given sleep stage. Thus, it would be incor¬ rect to state that REM sleep, stage 4 sleep, etc, are "necessary" unless these claims were clearly substantiated with new data. The important correlate of sleep stage al¬ most terations so far noted relates to the rebound in REM sleep following hypnotic drug with¬ drawal, which may be associated with unde¬ sirable clinical changes including increased dreaming, unpleasant dreams and night¬ mares, and insomnia. We recommend, there¬ fore, that the labeling and advertisements for REM suppressant hypnotic drugs in¬ clude a discussion of the possible clinical changes consequent to withdrawal of the suppressant. Flurazepam (30 mg) was found to be effective both in inducing and in maintain¬ ing sleep over the entire two-week drug adnfinistration period. Chloral hydrate (1, 000 mg) and glutethimide (500 mg) signif¬ icantly decreased sleep latency on the first set of three laboratory drug nights, but this effectiveness appeared to diminish rapidly within several days while the subjects slept at home. This lack of effectiveness was con¬ firmed when the subjects returned to the laboratory. Chloral hydrate and flurazepam produced only minimal changes in REM sleep. Glu¬ tethimide produced a marked REM sup¬ pression which persisted throughout the two weeks of drug administration. Following withdrawal, there was a marked REM re¬ bound. Flurazepam administration resulted in a gradual progressive decrease in stage 4 sleep which was maintained through the withdrawal nights. These all night electrophysiological studies demonstrate that the sleep labora¬ tory allows an accurate and objective deter¬ mination of a drug's effectiveness in induc¬ ing and maintaining sleep, the duration of its effectiveness, and the type of sleep in¬ duced. This contrasts with traditional studies evaluating drug effectiveness where precise measurements of sleep or waking cannot be made. This study was supported in part by NINDB Grant MB-02808, NIMH Training Grant 5 - 6415, and Anatomical Sciences Training Grant 5T01 00616. Computing assistance was obtained from the Health Sciences Computing Facility, UCLA, and sponsored by NIH Grant FR-3. References Summary Three drugs, chloral hydrate (1,000 mg), flurazepam (30 mg), and glutethimide (500 mg), were evaluated in the sleep laboratory with insomniac subjects to determine their effectiveness in inducing and maintaining sleep. A schedule of 22 consecutive nights was used in each separate drug evaluation. The first four nights were placebo-labora¬ tory nights and allowed for adapting to the laboratory and obtaining baseline measure¬ ments. This was followed by two weeks of drug administration which consisted of three laboratory, eight home, and another three laboratory nights. This was in turn followed by four placebo-laboratory nights which al¬ lowed for evaluating withdrawal changes. 1. Kales A, Kales J, Scharf MB, et al: Hypnotics and altered sleep-dream patterns: II. All-night EEG studies of chloral hydrate, flurazepam, and methaqualone. Arch Gen Psychiat, 23:211-218, 1970. 2. Kales A, Preston TA, Tan TL, et al: Hypnotics and altered sleep-dream patterns: I. All-night EEG studies of glutethimide, methyprylon, and pentobarbital. Arch Gen Psychiat, 23:219-225, 1970. 3. Rechtschaffen A, Kales A (eds): A Manual of Standardized Terminology, Techniques, and Scoring System for Sleep Stages of Human Subjects, Public Health Service Publication No. 204. US Government Printing Office, 1968. 4. Scharf M, Kales J, Kales A: Repeated adaptation and "first night" effects of the sleep laboratory. Psychophysiology 6:263, 1969. 5. Kales A, Preston T, Tal TL, et al: Effects of chronic hypnotic use. Psychophysiology 6:259, 1969. 6. Kales A, Kales JD: Sleep laboratory evaluation of psychoactive drugs. Pharmacol Physicians, to be published. Downloaded From: http://archpsyc.jamanetwork.com/ by a University of Otago Library User on 11/21/2016