Bacterial Comparison: Helicobacter, Campylobacter, Salmonella
advertisement

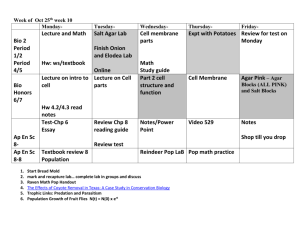
Helicobacter Campylobacter vibro Salmonella shape -ve curved bacilli -ve curved bacilli (seagul) -ve comma shaped bacilli -ve rods Motility Motile by multipolar flagella Motile by sigle polar flagellum Motile (darting motility) Motile Shigella -ve rods Brucella -ve coccobacilli Cl. Perfringens Cl.botulinum +ve rods +ve rods Motile Non Capsule Non Capsulated Non Spore Non Subterminal spore Sporulated worldwide &associated with MOI ® chronic superficial gastritis. ® gastric or duodenal ulcers ingestion of contaminated water, milk or undercooked foods. Commonest cause of enterocolitis in children Contaminated water or food Contaminated food Contaminated food Pathogenesis ® gastric carcinoma. ® Spiral shape For motility ® C. jejuni has LPS within this mucous layer. with endotoxin activity. ® Urease activity Which ® Cytopathic generate ammonium lons extracellular toxins that buffer gastric acidity ® Enterotoxin. ® microaerobic :For survival ® small infecting dose Is within the mucous gel required to cause illness ® Attachment to epithelial cells By as few as 800 bacteria fimbria, adhesion ® illness gradually occur after 2 – 4 days ® Penetrates the mucus layer covering intestinal mucosa by secretion of neuraminidase and proteases and adhere to the mucosal cell by fimbriae and outer proteins where they subsequently produce enterotoxin which causes extensive diarhia → dehydration, hypokalemia, metabolic acidosis and anuria typhi and paratyphi penetrate intestinal epithelium → multiply in mesenteric lymph nodes → pass to blood stream → septcemia (1st week) → shed into gallbladder and goes to lumen of intestine s.typhimurium s.enteritis: invade enteric epithelium ( no systemic infection) → cause diarrhea and fever Shigatoxin exotoxin inhibit protein synthesis and has enterotoxic, neurotoxic properties multiply in large intestine → penetrate epith cell → multiply intracellular → tissue destruction → dysentry (stool with blood & mucous & pus) + ANVAC D ® Handiling infected animals ® contaminated milk (Zoonosis) ® no human to human infection enter the gut → reticuloendothelial system → multiply in macrophage cells causing granuloma → release from granulomas cause bacteraemia and fever Reheated meat dishes containing spores or enterotoxin Multiply producing toxins: ® toxins form spores make Ca influx → cause cell death and intestinal damage → fluid & electrolite loss → cause diarrhea and abdominal colic -Direct ingestion of toxins -Wounds grow in necrotic tissus -In infant due to honey contaminated with spore ® active cholinergic nerves inhibitor -preventing release of acetylcholine cause blurred vision and inability to swallow and difficulty in speaking and paralysis of respiratory muscles and death incupation period cause ANVAC D + fever. ® Large infectious dose 10*8 to 10*10 Culture characters Sample Hoste defense Gastric acidity & antitoxin IGA Gastric biopsy Stool Microaerobic Microaerobc Capnophilic 5-10% Thermophilic 42 ® Grow on nonselective Media media, as chocolate agar ® antibiotic containing selective media:as Skirrow's medium and incubate for 2- 5 days. ® Skirrow's medium: containing vancomycin, polymyxin and trimethoprim is a selective medium used for their isolation from stools. Mucus flecks from rice water stools. Highly aerobic Alkaline PH ® ordinary media TCBS medium (thiosulphate citrate bile sucrose), ® they give yellow colonies as they ferment sucrose ® 1st week: Blood ® 2nd week: Stool, serum ® 3rd week: Urine, serum stool which contains mucus and blood. O2 :facultative anaerobic Co2 0,03% temp: 37 ph 7.4 ® ordinary media : grow ® enrichment : selenite ,Tetrathionate ® selective : SS (XLD) ® Indicator : macconkey → pale = non lactose fermenter Blood, biopsy of lymph node, spleen, liver and bone marrow. Co2: 5 - 10% tem :37 ph 7,4 O2 aerobic ® Need to be obtained early in disease ® Blood agar and trypticase soya agar are media of choice ® no hemolysis on blood agar Identification 1 -film stain ® Campy blood agar: is a selective medium Colonies can be identified by Gram & giemsa & acridine orange & H&E stain. ® Examined by dark-field or phase contrast micrascopy for darting motility. ® By Gram staining to detect morphology ® Gram stain to show morphology ® Dark field microscope show motility Gram stain to show morphology Gram staining is not useful to show the organisms in Clinical specimens as they are intracellular Fecal samples are the best specimens for detecting toxin in food, Food, feces, serum or vomitus Stool O2 obligate anaerobe CO2 0.03% Temp. 37°C PH 7.4 ® egg yolk-glucose agar or serum agar ® Ordinary media: grow ® Blood agar ® Robrtson cooked meat medium ® Ordinary media: grow ® Blood agar: haemolysis ® Robrtson cooked meat medium 2 -BR • urease • • oxidase • catalase positive • (3+ve). • Detection of H.pylori antigen in the stool ferments MGLS with production of acid only positive cholera-red reaction oxidase +ve Agglutination with V. cholera O group 1 polyvalent antiserum ® Ferement : glucose, mannite, maltose with acid & gas production Lactose is not fermented ® H2S produced From ‘thiosulfate’ ® O antibody appears early and disappears early ® H antibodies appears late and disappears late. Serology ®So we can determine the onset of infection by interpreting the titre of both O and H antibodies -If the O titre is higher than the H titre this means early infection others - If the H titre is higher than the O titre this means late infection • Rapid urase test • PCR • Rapid detection • Urea breth test • Culture confirmation • Typing of C jejuni PCR for PCR → Detect cholera toxin gene strains treatment Triple chemotherapy • PPI • Antibiotics(clarithromycin & • ® Replacement therapy for fluid loss amoxicillin & metronidazole ® No value for antibiotics Bithmuth component but broad spectrum one may be used to reduce output of viable organisms ® ferments MGLS produces gases & acid s ® S. dyenteriae → glucose ,indole ® S. flexneri → glucose,mannite, indole ® S. boydi → glucose, mannite ,indole ® S. sonnei → glucose,mannite ,late fermentation for lactose ----------------- ® stormy clot in litmus milk ® brucella agglutination test - slide or tube agglutination test - detect serum antibodies against brucella (diagnostic Tire :160 or rising) ® ELISA to differentiate between specific IgM and IgG