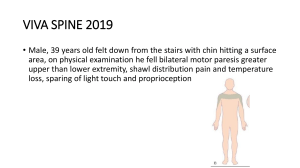
Viva in Medical Physiology Viva in Medical Physiology Second Edition AK Basak PhD Professor and Head Department of Physiology Haldia Institute of Dental Sciences and Research, Haldia, Purba Medinipur, West Bengal, India Formerly Associate Professor and Head Department of Physiology Institute of Dental Sciences , Bareilly, UP, India Associate Professor and Head Department of Physiology Avadh Institute of Dental Sciences, Lucknow, UP, India Asst. Professor in Physiology Universal College of Medical Sciences, Nepal Asst. Professor in Physiology Nepalgunj Medical College, Nepal ® JAYPEE BROTHERS MEDICAL PUBLISHERS (P) LTD St Louis (USA) • Panama City (Panama) • New Delhi • Ahmedabad • Bengaluru Chennai • Hyderabad • Kochi • Kolkata • Lucknow • Mumbai • Nagpur Published by Jitendar P Vij Jaypee Brothers Medical Publishers (P) Ltd Corporate Office 4838/24, Ansari Road, Daryaganj, New Delhi 110 002, India. Phone: +91-11-43574357 Fax: +91-11-43574314 Registered Office B-3, EMCA House, 23/23B Ansari Road, Daryaganj, New Delhi 110 002, India Phones: +91-11-23272143, +91-11-23272703, +91-11-23282021, +91-11-23245672 Rel: +91-11-32558559 Fax: +91-11-23276490, +91-11-23245683 e-mail: jaypee@jaypeebrothers.com Website: www.jaypeebrothers.com Branches • • • • • • • • • 2/B, Akruti Society, Jodhpur Gam Road Satellite Ahmedabad 380 015 Phones: +91-79-26926233, Rel: +91-79-32988717 Fax: +91-79-26927094 e-mail: ahmedabad@jaypeebrothers.com 202 Batavia Chambers, 8 Kumara Krupa Road, Kumara Park East Bengaluru 560 001 Phones: +91-80-22285971, +91-80-22382956, +91-80-22372664 Rel: +91-80-32714073 Fax: +91-80-22281761 e-mail: bangalore@jaypeebrothers.com 282 IIIrd Floor, Khaleel Shirazi Estate, Fountain Plaza, Pantheon Road Chennai 600 008 Phones: +91-44-28193265, +91-44-28194897, Rel: +91-44-32972089 Fax: +91-44-28193231 e-mail: chennai@jaypeebrothers.com 4-2-1067/1-3, 1st Floor, Balaji Building, Ramkote Cross Road Hyderabad 500 095 Phones: +91-40-66610020, +91-40-24758498 Rel:+91-40-32940929 Fax:+91-40-24758499, e-mail: hyderabad@jaypeebrothers.com No. 41/3098, B & B1, Kuruvi Building, St. Vincent Road Kochi 682 018, Kerala Phones: +91-484-4036109, +91-484-2395739, +91-484-2395740 e-mail: kochi@jaypeebrothers.com 1-A Indian Mirror Street, Wellington Square Kolkata 700 013 Phones: +91-33-22651926, +91-33-22276404, +91-33-22276415 Rel: +91-33-32901926 Fax: +91-33-22656075, e-mail: kolkata@jaypeebrothers.com Lekhraj Market III, B-2, Sector-4, Faizabad Road, Indira Nagar Lucknow 226 016 Phones: +91-522-3040553, +91-522-3040554 e-mail: lucknow@jaypeebrothers.com 106 Amit Industrial Estate, 61 Dr SS Rao Road, Near MGM Hospital, Parel Mumbai 400012 Phones: +91-22-24124863, +91-22-24104532, Rel: +91-22-32926896 Fax: +91-22-24160828, e-mail: mumbai@jaypeebrothers.com “KAMALPUSHPA” 38, Reshimbag, Opp. Mohota Science College, Umred Road Nagpur 440 009 (MS) Phone: Rel: +91-712-3245220, Fax: +91-712-2704275 e-mail: nagpur@jaypeebrothers.com North America Office 1745, Pheasant Run Drive, Maryland Heights (Missouri), MO 63043, USA Ph: 001-636-6279734 e-mail: jaypee@jaypeebrothers.com, anjulav@jaypeebrothers.com Central America Office Jaypee-Highlights Medical Publishers Inc. City of Knowledge, Bld. 237, Clayton, Panama City, Panama Ph: 507-317-0160 Viva in Medical Physiology © 2009, Jaypee Brothers Medical Publishers All rights reserved. No part of this publication should be reproduced, stored in a retrieval system, or transmitted in any form or by any means: electronic, mechanical, photocopying, recording, or otherwise, without the prior written permission of the author and the publisher. This book has been published in good faith that the material provided by author is original. Every effort is made to ensure accuracy of material, but the publisher, printer and author will not be held responsible for any inadvertent error(s). In case of any dispute, all legal matters are to be settled under Delhi jurisdiction only. First Edition: 2004 Second Edition: 2009 ISBN 978-81-8448-684-1 Typeset at JPBMP typesetting unit Printed at To my dear son 'Sohom’, my students and well wishers Preface to the Second Edition I must extend my heart-felt gratitude for warm response from my students, readers and colleagues and even my teachers for the 1st edition of this book. I also acknowledge some suggestions from my students and colleagues that led me to bring this 2nd edition of this book. To make this book more beneficial and meaningful from the examination point of view and also to make it self-contained as per the demand of the students, the following aspects are also included in this edition of this book: More number of clinical/applied questions with their answers. Questions with answers for preparing practical (Lab-based) viva examinations. Important values to remember to have a bird's eye view on different physiological norms just before facing the viva voce examinations. I am deeply indebted to Prof BN Koley and Dr (Mrs) J Koley (Calcutta University), Prof NK Mishra and Prof SN Pandeya (Nepalgunj Medical College), Prof V Reghunandanan and Dr (Mrs) R Reghunandanan (Universal College of Medical Sciences), Prof VK Negi (Harsaran Dass Institute of Dental Sciences, Ghaziabad), Prof SK Saxena (Sikkim-Manipal Institute of Medical Sciences), Dr Ashoke Agarwal and Dr Keshav Agarwal (Institute of Dental Sciences, Bareilly, UP), Prof Sekhar Chakraborty and Dr J Samanta (Haldia Institute of Dental Sciences and Research) who always thought very good of mine. The generous help rendered by the faculty members of Haldia Institute of Dental Sciences and Research (especially Dr Soudeep Sau and Dr SR Tripathy) is also warmly acknowledged. I also wish to express my sincere thanks to my wife Dhriti Basak—who has helped me in each and every step of the preparation of this book and also has edited the literary aspect of this book. Finally I also express my sincere gratitude to Shri Jitendar P Vij Chairman and Managing Director, Tarun Duneja, DirectorPublishing and other Staff of M/s Jaypee Brothers Medical Publishers (P) Ltd. for publishing this book. viii VIVA IN MEDICAL PHYSIOLOGY I will be grateful if this book meets the demand of the students. The author is highly regretted for any typographical mistake, human errors, inaccuracies or ambiguities if any in this title. I will be very happy to receive any opinion, feedback and valuable suggestions from the teachers, senior colleagues and students for further improvement of this book. AK Basak Preface to the First Edition While examining the MBBS and BDS students in their viva voce examination, I have felt that even the good students hardly answer the questions very precisely and to the point. Though there are small number of viva books in Physiology with us, these are not sufficient to meet the demand of the students so that they can answer A to Z of viva questions generally asked by the examiners. Moreover, it is never possible to the students to go through any text book while going to face viva-voce examinations. These facts led me to write the book Viva in Medical Physiology . While writing thisbook I have tried my best to include all types of viva questions dealt with basic, brainstorming, applied and clinical. Language of the book has also been kept easily understandable. I hope this book will serve the purpose for not only the BDS students but equally also the MBBS , MSc and BSc (Medical/ Human Physiology), MD (Physiology) students and also other allied health subjects like physiotherapy, nursing, etc. I am highly grateful to my students, colleagues and well wishers of Avadh Institute of Dental Sciences (Lucknow); Universal College of Medical Sciences (Nepal) and also Nepalgunj Medical College (Nepal) for their encouragement and sincere suggestions for writing up of this book. I am also deeply indebted to Prof. B N Koley and Dr (Mrs) J Koley (Calcutta University), Prof NK Mishra and Prof SN Pandeya (Nepalgunj Medical College), Prof V Reghunandanan and Dr (Mrs) R Reghunandanan (Universal College of Medical Sciences), Prof VK Negi (Harsaran Dass Institute of Dental Sciences, Gaziabad), Prof SK Saxena (Sikkim-Manipal Institute of Medical Sciences), Dr Rajuma Baudha (Avadh Institute of Dental Sciences) who always thought very good of mine. I am also highly grateful to my family members who always supported me in my academic pursuit. I am really obliged to my wife, Mrs Dhriti Basak not only for editing the language of this book but also for her sacrifice whose time I usurped during the preparation of this book. Finally I also express my sincere gratitude to Shri Jitendar P Vij, Chairman and Managing Director, Tarun Duneja, Director- x VIVA IN MEDICAL PHYSIOLOGY Publishing and other Staff of M/s Jaypee Brothers Medical Publishers (P) Ltd. for publishing this book. I will be grateful if this book meets the demand of the students. I will be very happy to receive opinions , comments and valuable suggestions from all my senior colleagues, fellow teachers and students so that every aspects of this book can be reviewed in succeeding editions. AK Basak Contents Section I: Theory Viva 1. Basic Concepts ................................................................... 1 2. Blood ................................................................................. 11 3. Cardiovascular System ................................................... 39 4. GI System and Metabolism ............................................ 75 5. Respiratory System ......................................................... 91 6. Nerve Muscle Physiology ............................................ 117 7. Excretory System ........................................................... 135 8. Skin and Body Temperature Regulation ................... 147 9. Central Nervous System .............................................. 152 10. Special Senses ................................................................. 178 11. Endocrinal System ......................................................... 189 12. Reproductive System .................................................... 212 Section II: Practical Viva Part A: Hematology ...................................................... 226 Part B: Human Experiments ........................................ 239 Section III: Appendix Important Values to Remember .................................. 252 BASIC CONCEPTS 1 SECTION I : THEORY VIVA SECTION I: THEORY VIVA 1.1 Basic Concepts 1. What do you mean by unit membrane? Not only the cell membrane but also the nucleus, chloroplast and mitochondria are double membranous, i.e. they are covered by two wall layers each of which, is consisting of protein-lipid-lipid-protein. This type of membrane is known as unit membrane. 1 2. What is fluid mosaic model of cell membrane? As per this model all membranes of different cell organelles along with the plasma membrane are made up of double layer of lipid molecules in which proteins are embedded like the tiles of mosaic floors. This model is first proposed by Singer and Nicholson. 3. Mention the chemical nature of proteins present in plasma membrane with special reference to its functions. Chemically the proteins present on plasma membrane are of two types: i. Lipoproteins—It functions as enzymes and ion channels. ii. Glyco-proteins—It functions as receptor for hormone and neurotransmitters. 4. Classify the proteins as per their location on plasma membrane and mention each of their functions. As per their location proteins are of 3 types: 2 VIVA IN MEDICAL PHYSIOLOGY i. Intrinsic protein—These are located in the inner surface of membrane and serve mainly as enzymes. ii. Extrinsic protein—These are located in the outer surface of membrane and contribute to the cytoskeleton. iii. Transmembrane protein—They extend through the membrane and serve as channel proteins, carriers, pump and receptors. 5. Mention the function of SER and RER. Functions of smooth endoplasmic reticulum (SER) are as follows: • It is the site of steroid synthesis. • It plays important role in skeletal and cardiac muscles. Function of RER: It is the site of protein synthesis. 6. Name at least four lysosymes. These are: Ribonuclease and deoxyribonuclease, phosphatase, collagenase and glycosidase. 7. What are the differences between microfilaments and microtubules? Microtubules are long, hollow structure, 25 mm in diameter whereas microfilaments are solid fibres of 4-6 mm in diameter. 8. Enumerate different types of cell junction and each of their function. On the basis of their functions cell junctions are classified into 3 groups: 1. Occluding junction or Zona occludens or tight junction—Prevents movement of ions and other molecules across the membrane. 2. Anchoring junctions—These are of 3 types: a. Macula adherens or desmosome—which acts as a strong anchor between the cells/tissues is subjected to mechanical stress like epidermis of skin. b. Zonula adherens or belt desmosome. c. Fascia adherens or strip desmosome. SECTION I : THEORY VIVA BASIC CONCEPTS 3 3. Communicating junctions—These are again of 3 types a. Gap junction- allows the speedy movement of Na+, K+, Ca+2, ATP, Sugar, amino acids, vitamins, etc. across the membrane. b. Plasmodesmata. c. Chemical synapse. 9. What are the types of intercellular communication? There are 5 types of intercellular communication process as follows: i. Neural communication: In this process on stimulation the nerve cells release neurotransmitters which act on post synaptic cell to activate or inhibit it. ii. Endocrine communication: In this process the cells (endocrine cells) release hormones which reach target cell via circulating blood and thus communicate with other cells. iii. Paracrine communication: Depending on the requirement sometimes cell produces some substances which diffuse to ECF. While circulating through the ECF these substances control the activity of neighbouring cells. iv. Autocrine communication: Sometimes some cells secrete chemical messengers which bind to receptors on the same cell to modify the activity of that cell. This process is known as autocrine communication. v. Juxtacrine communication: In some situations some cells express multiple growth factors e.g.: trans forming growth factors alpha (TGF α) extracellularly on transmembrane proteins that provide an anchor to the cell. Other cells having TGF α receptors bind to those cells having TGF α on their membrane to communicate each other. 4 VIVA IN MEDICAL PHYSIOLOGY 10. How does lipid and water soluble substances diffuse through cell membrane? Lipid soluble substances diffuse through lipid layer of membrane whereas water soluble substances diffuse through the channels present in cell membrane. 11. What do you mean by voltage gated and ligand gated channels? Give example of each. The ion channels, the gate(s) of which open or close by alteration in membrane potential, is known as voltage gated channels. Examples, Na+ and K+ or Ca++ channels present in cell membrane. Whereas the ion channels, the gate(s) of which open or close in response to binding of channel proteins with some ligand molecules like neurotransmitters, hormone, intra-cellular Ca++, cAMP, G protein, etc. is called as ligand gated channels. Example—Na+ and K+channels present in post-synaptic membrane of synapses. 12. Name the types of bone cells. What is the function of osteoclast cells? There are three types of bone cells—Osteoblast, Osteoclasts and Osteocytes. The osteoclast cells are phagocytic in nature which digest the bone and release their products into ECF. 13. Classify the bones and give the examples of each of them. On the basis of histology: It is of 2 types: i) Compact bone: These are solid, dense and harder (e.g. shaft of long bones) ii) Cancellous (spongy) Bone: It is characterised by bigger marrow spaces and is relatively less hard (e.g. ends of long bones). On the basis of shape: It is of 4 types: iii) Long bones (e.g. femur, humorous) iv) Short bones (e.g. carpals, tarsal, phalanges) v) Flat bones (e.g. scapulae, sternum) vi) Irregular bones (e.g. vertebral, facial bones). SECTION I : THEORY VIVA BASIC CONCEPTS 5 14. What is facilitated diffusion? Give example. It is a carrier mediated transport process in which carrier protein undergoes repetitive spontaneous configurational changes during which the binding site for the substance is alternatively exposed to the ECF and ICF and thereby allow the inward movement of substances inside the cell. Example—transport of glucose into RBC. 15. Name the factors affecting diffusion. The factors are: Gradient, Temperature, Size of the molecule, Solubility and Cross sectional area. 16. Define osmosis. It is the passive flow of solvent, i.e. water across the selectively permeable membrane into a region of higher concentration of solute to which the membrane is impermeable. 17. Define osmotic pressure. The tendency for movement of solvent molecules to a region of greater solute concentration can be prevented by applying pressure to the more concentrated solution. The pressure necessary to prevent this type of solvent migration is called as osmotic pressure. 18. What is osmolarity and osmolality? Osmolarity is the number of osmoles per litre of solution. Whereas osmolality is the number of osmoles per kg of the solvent. 19. What is osmolality of normal human plasma? What is tonicity? Osmolality of normal human plasma is 290 mosm/lit. The osmolality of a solution relative to plasma is called as tonicity. 20. How does hyperosmolality can produce coma? It is by causing cellular dehydration. 6 VIVA IN MEDICAL PHYSIOLOGY 21. What is solvent drag? When water flows into or out of capillaries it carries dissolved particles with it. This force is known as solvent drag. 22. Define active transport process. What are their types? When the transport of substances across the membrane takes place against their chemical or electrical or pressure gradient for which energy is required, this type of transport process is called as active transport process. It is mainly of 2 types as follows: • Primary active transport where energy is required directly. • Secondary active transport in which the required energy is obtained from primary active transport. 23. Name the types of pump required for primary active transport with its site of location. • Na+–K+ pump—Present in cell membrane of all parts of the body. • Ca+2–pump—Present in sarcoplasmic reticulum of muscle cells. • K +–H + pump—Present in the cells of the gastric mucosa and renal tubules. 24. How many types of carrier mediated transport processes are present in body? Name them with examples? These are of three types which are as follows: • Uniport—facilitated diffusion of glucose in renal tubules. • Symport—secondary active transport of glucose in renal tubules coupled with Na+. • Antiport—Na+– Ca++exchanger in muscle cell and also Na+– H+exchanger in renal tubules. 25. Define phagocytosis. It is the process by which the extracellular substances SECTION I : THEORY VIVA BASIC CONCEPTS 7 like bacteria, dead tissue, foreign particles are engulfed and digested by the cells. 26. What is the total amount of water in our body? It is 42 litre in a 60 kg body weight person, i.e. 70 per cent of the body weight. 27. Why total body water is lower in female than male? It is because of presence of relatively greater amount of subcutaneous fat in female body. 28. Name different compartments of ECF. • Plasma—25 per cent • Interstitial fluid—75 per cent • Transcellular fluid—minute amount. 29. Name the method for measuring body fluid volume. It is indicator dilution method. 30. What are the criteria of good indicator used for measuring body fluid volume? These are as follows: • Must be non-toxic. • Must mix evenly throughout the compartments being measured. • It should neither be reabsorbed nor be secreted. • It should not alter the water distribution of the compartment being measured. • It should be relatively easy to measure. 31. From the clinical point of view define acidosis and alkalosis. Decrease blood pH, less than 7.35 is known as acidosis and increase blood pH, more than 7.45 is called alkalosis. 32. What is buffer? What is its chemical nature? Buffer is a substance that has the ability to bind or release H+ ion in solution. Chemically it is a weak acid and its conjugated base. 8 VIVA IN MEDICAL PHYSIOLOGY 33. What is anion gap? There is a difference of sum totals of anions and cations in each compartment which is known as anion gap. Normal anion gap in plasma is 10-15 mosml/ lit which is reduced in metabolic acidosis during diabetic coma. 34. Define oedema. Accumulation of water either in cell interior (intra cellular edema) or within ECF (extra cellular edema) is termed as oedema. 35. What are the mechanisms by which body fluid volume is regulated ? The body fluid volume is kept constant within the normal range by different mechanisms as follows: 1. ADH mechanism 2. By initiation of thirst sensation 3. By renin angiotensin–Aldosterone system 4. Renal body fluid mechanism 5. By controlling secretion of atrial natriuretic peptide (ANP). 36. Define homeostasis. Maintenance of the constant internal environment of the body to enable its normal function is known as homeostasis. 37. What do you mean by internal environment? The ECF surrounding the body cells is called internal environment as the cellular function depends on this particular environmental condition. 38. What is negative feedback mechanism? The homeostatic mechanism in which the final response becomes opposite to that of its initiating stimulus is known as negative feedback mechanism. 39. Define positive feedback mechanism. The homeostatic mechanism in which the final response becomes similar to that of its initiating stimulus is known as positive feedback mechanism. SECTION I : THEORY VIVA BASIC CONCEPTS 9 40. Does the positive feedback is harmful to the body? Not always, in case of parturition, blood clotting and initiation of action potential positive feedback mechanism is operated which is not harmful to the body rather beneficial one. 41. Define action potential. What are its phases? Definition: In response to a stimulus of threshold intensity there is transient change in potential difference across the cell membrane (inside electronegative and outside electropositive) which when reaches to a critical level, produces a electrical signal that can be propagated beyond its site of origin. This transient change of membrane potential which is propagatory in nature is known as Action Potential (AP). The phase of AP are—Resting or polarised phase, depolarisation, repolarisation and hyperpolarisation. 42. What are monophasic and biphasic action potential? Give the example of each of them. The AP initiated in response to the stimulus can be recorded through Cathode Ray Oscilloscope by placing two electrodes in two separate site of the membrane. If one electrode is placed outside the membrane and another is inserted inside the membrane or one electrode is placed externally on the surface of the healthy site of the membrane and another at the damaged/injured/ sectioned site then the recorded action potential will be monophasic. Whereas if both the electrodes are placed at the outside of the membrane the AP is recorded as an upward deflection followed by short isoelectric period and then a downward deflection which is known as biphasic action potentia (Fig.1.1.1A). Monophasic AP is intracellular recording whereas biphasic AP is extracellular recordings.The examples of biphasic AP are: ECG, EEG, EMG 10 VIVA IN MEDICAL PHYSIOLOGY Fig. 1.1.1A: Graphical presentation of biphasic action potential Fig. 1.1.1B: Graphical presentation of compound action potential 43. What is compound action potential? It is the monophasic recording of the action potential from the nerve trunk (mixed nerve) which contains many fibers of varying diameter. As the diameter of the nerves fiber in a mixed nerve varies their conduction rate will also vary. This is why the onset of the peak in different nerve fiber will be different resulting a wavy action potential (Fig. 1.1.1B). BLOOD 11 SECTION I : THEORY VIVA 1.2 Blood 1. What are the formed elements of blood? These are RBC, WBC and platelets. 2. Enumerate the functions of plasma protein. These are: A. Coagulation of blood: Fibrinogen, prothrombin and other coagulation factors help in coagulation of blood. B. Maintenance of colloidal osmotic pressure: The plasma proteins do not pass through the capillary membrane easily during normal state. So it remains in the blood and exerts osmotic pressure. This helps to maintain the exchange of fluid at tissue level. C. Maintenance of viscosity of blood and Blood pressure: It (especially albumin) regulates viscosity of the blood and as resistance of blood flow is directly proportional to viscosity of blood, it also maintains the systemic arterial blood pressure. D. Maintenance of acid base balance: The plasma proteins, particularly albumin, play an important role in maintaining the acid base balance in the blood. This is due to the fact that in physiological pH plasma proteins exist as an ‘ionised’ form and in this form it’s C terminal end (i.e. COO= –) can buffer the change due to the addition of an acid and N terminal end (i.e. –NH3+) can buffer the change that follow addition of an alkali. E. Regulation of ESR : Globulin and fibrinogen increase the rate of rouleaux formation and thus increase ESR. 12 VIVA IN MEDICAL PHYSIOLOGY F. Providing of suspension stability of RBC: During circulation, the RBCs remain suspended uniformly in the blood without rouleaux formation. This property of RBC is known as suspension stability of RBC, which is provided mainly by globulin and fibrinogen. G. Act as a reservoir : Plasma proteins act as a reservoir during the conditions like fasting, starvation, etc. H. Production of trephone: Leukocytes produce trephones from plasma proteins which are required for nourishment of tissue cells in culture. I. Immune function: Globulin produces antibodies and thus provides immunity to the body. J. Transportation: It combines loosely with hormones, metal, drugs, etc. and transports to appropriate site for their release as an active components. K. Fibrinolysis: Intravascular clot (thrombus) is digested by the enzymes of fibrinolytic system present in plasma which saves the body from disastrous effects of thrombus. 3. What are the non-protein substances in blood? These include urea, uric acid, creatine, creatinine, xanthine and hypoxanthine (in traces). 4. Name three clinical conditions when NPN in blood alters. NPN increases in renal insufficiency, adrenal insufficiency and thyrotoxicosis, whereas it decreases in later months of pregnancy. 5. What are non-NPN substances in blood? These are neutral fat, phospholipids, glucose and cholesterol. 6. What is the difference between plasma and serum? Plasma is fluid portion of the blood obtained without clotting while serum is the fluid obtained after clotting. Serum is thus plasma without fibrin. SECTION I : THEORY VIVA BLOOD 13 7. What is the normal concentration of plasma protein? It is 6.4-8.3 gm/100 ml of blood. 8. What is the origin of plasma proteins? • In embryonic stage—Mesenchymal cell • In adult—Albumin and fibrinogen from liver; globulin from reticulo-endothelial cells, lymphocytes. 9. What will happen if plasma protein concentration decreases? a. Less than 2 gm%: results shock and even death. b. To 4 gm%: exhaustion of protein reserves in the body 10. How hypoproteinemia produces edema? Hypoproteinemia→ decrease in capillary oncotic pressure→ decrease in filtration at arterial end→ decrease in absorption of fluid at venous end→ abonormal collection of fluid in interstitial spaces→ edema. 11. What is A/G ratio? It is the ratio of albumin to globulin. Normally it is 1.7:1. 12. Name three conditions when there physiological decrease of albumin. In infancy, newborns and early pregnancy. is a 13. What is the average daily production of plasma proteins? It is about 15 gm/day. 14. Can any of the plasma proteins pass through capillary endothelium? Capillary endothelium normally is impermeable to plasma proteins though in some diseases like glomerulonephritis, nephrotic syndrome, etc. albumin can pass through the capillary membranes. 14 VIVA IN MEDICAL PHYSIOLOGY 15. State the specific gravity of blood, serum and corpuscles. Blood: 1.055–1.060; Serum: 1.028–1.032; Corpuscles: 1.090. 16. Name the main conditions in which blood viscosity rise. It is during acidosis, hypercalcaemia and hyperglycaemia. 17. What is the normal pH of blood? It is 7.3 - 7.4. 18. Name the buffer systems in the body which help to maintain the body pH. It is bicarbonate, phosphate, protein and hemoglobin buffer systems. 19. How is the biconcavity of RBC is maintained? It is maintained by the presence of a contractile layer of a lipoprotein molecule "spectrin" in a fibrillar manner below its cell membrane. 20. What are the advantages of biconcave shape of RBC? These are: • It can withstand considerable changes of osmotic pressure by altering its cell volume and thereby prevent hemolysis. • Allows easy passage of RBC through narrow capillaries by folding itself. • Facilitates quick and optimal exchange of gases in and out of hemoglobin. 21. What are the advantages of having no nucleus, no mitochondria and no ribosome in RBC. It is to accommodate more amount of hemoglobin and also to decrease the use of O2 by its own structure and thereby increases the availability of O2 to the other cells. SECTION I : THEORY VIVA BLOOD 15 22. What are the disadvantages of non-nucleated RBC? • It cannot multiply. • It cannot synthesize necessary enzymes so has less life span. 23. How does RBC survive for 120 days though it has no nucleus, mitochondria and ribosomes? For energy supply RBCs depend on glucose metabolism only, which comes through facilitated diffusion. These glucoses are oxidised by cytoplasmic enzymes already present inside the cells to get the energy for their activity. When these cytoplasmic enzymes are exhausted, i.e. after 120 days, it dies. 24. Which is the principle cation in RBC? It is potassium ion. 25. What is the diameter of normal RBC? It is 6.7-7.7 cµ. 26. Why RBC is stained pink by Leishman’s stain though it has no ribosomes in their cytoplasm? It is because of presence of hemoglobin. 27. Mention the site of RBC formation. • In foetus—bone marrow, spleen, liver and thymus gland. • After birth—red bone marrow of long bones like sternum, vertebrae, etc. 28. Name the mother cell of RBC. Haemocytoblast which gives rise proerythroblast. 29. Why hemoglobin is present within RBC not in plasma? There are several reasons like: • To prevent rise of viscosity of plasma that may lead to increase of blood pressure. • To prevent the increase in osmotic pressure of plasma and thereby prevent the disturbances of fluid exchange mechanism due to rise in osmotic pressure. 16 VIVA • • IN MEDICAL PHYSIOLOGY To prevent breakdown of Hb by tissue macrophage system. To prevent loss of Hb through urine. 30. What is the shape of Hb crystals of human blood? What is its name? Shape is rhombic or trycyclic. It is haemin crystal. 31. What is the site of production of heme of Hb? It is in mitochondria. 32. Mention the average daily production of Hb in the body? It is about 7-8 gms/day. 33. Name the common methods of Hb estimation. These are: Sahli’s haemoglobinometer method, Haldane haemoglobinometer method, Oxy-Hb colorimetric and also Cyano methaemoglobin colorimetric method. 34. Why does Sahli’s method so accurate? • In this method reduced Hb in the blood is not converted into acid haematin, thereby the value obtained is less than the total Hb content in the blood. • This method depends on person’s colour vision. As the colour vision varies from person to person result may also vary. 35. Enumerate main functions of iron. These are: Hb synthesis, RBC development, O2 carriage and tissue oxidation through cytochrome. 36. In which form iron is stored in reticuloendothelial cells? Ferritin and hemosiderin form. 37. Mention the forms of Hb present in human blood. These are: Oxyhaemoglobin, carbaminohaemoglobin, reduced (deoxygenated) Hb, Carboxy-Hb and Methaemoglobin. SECTION I : THEORY VIVA BLOOD 17 38. Mention the varieties of haemoglobin with special reference to difference of each. These are as follows: • Adult Hb (HbA) - Contains 2 α and 2 β globin chain. • Adult Hb (HbA2) - Contains 2 α and 2 δ chain. • Foetal Hb (HbF) - Contains 2 α and 2 γ chain • HbS - Contains 2 α and 2 β chain but in β chain glutamate of 6th position is replaced by a valine residue. 39. Why does Hb level lower in female? This is due to the: • Presence of estrogen which inhibits erythropoietin secretion resulting less RBC formation. • Absence of testicular androgens which stimulate Erythropoietin secretion in male and thereby increases RBC count. 40. Why does Hb level high in the newborn? The newborns are generally in a state of mild hypoxia which in turn stimulates erythropoietin secretion and thereby increases RBC count and thus Hb concentration. 41. What is the fate of hemoglobin? Old and inactive red cells are ingested by the RES and are broken into globin and iron. Globin and iron are reused whereas the porphyrin moiety of iron is converted into biliverdin and thence bilirubin which are excreted into bile and ultimately excreted mostly through the faeces and partly through the urine. 42. Define anaemia. It is a clinical condition characterised by decrease in O2 carrying capacity of blood either due to decreased Hb concentration or decreased RBC count or both. 43. Classify anemia. On the basis of etiological classification it is of following types: 18 VIVA • • • • IN MEDICAL PHYSIOLOGY Hemorrhagic anemia Dietary deficiency anemia like folic acid deficiency and iron deficiency anemia. Anemia due to abnormal hemopoiesis, i.e. aplastic anemia. Hemolytic anemia. 44. What are the signs and symptoms of anemia? • Signs: Paleness of skin and mucous membrane of mouth cavity, etc. spoon-shaped nails and hemorrhages in the retina. In severe cases there may be enlargement of heart and even heart failure. • Symptoms: Breathlessness, fatigue, palpitation, loss of appetite and bowel disturbances. 45. What is the commonest form of anemia in the world? It is iron deficiency anemia. 46. What is the etiology of pernicious anemia? It is due to deficiency of hematinic principle, i.e. lack of castle’s intrinsic factor, resulting failure of absorption of vitamin B12 from diet through ileum. 47. Name the physiological and pathological condition of anemia? Physiological—Pregnancy. Pathological—Thalassemia, spherocytosis, malaria, iron deficiency, etc. 48. What is polycythemia? What is its difference with polycythemia vera? Polycythemia refers to the increase in the number of RBC above normal level. Polycythemia vera is the condition characterised by very high RBC count due to gene abnormalities of hemopoietic cells. 49. Name the physiological and pathological condition of polycythemia. Physiological—Muscular exercise, high altitude, high environmental temperature, etc. Pathological—Cardiac failure, diarrhoea, etc. SECTION I : THEORY VIVA BLOOD 19 50. Which is the most common site for bone marrow biopsy? Body of sternum between 2nd and 3rd ribs. 51. Which type of bone marrow is concerned with hemopoiesis - red or yellow? It is red bone marrow. 52. What are the common indications for bone marrow study? These are – disorders of haemopoietic system, conditions like multiple myeloma, cancer in lung, liver, prostate, breast, etc. 53. What is the normal average ratio of WBC to RBC in human blood? It is 1:700 (WBC:RBC). 54. What is MCV and what is its significance? It is volume of a single RBC in cubic micron. The normal range is 74-94 mm3. It is the basis to diagnose the maturity of the RBC, i.e. whether it is normocytes or microcytes or macrocytes. 55. What is MCH? It is the average amount of Hb in a single RBC in picogram. Normal value is 30 pgm (range:28-32 pgm). 56. What is MCHC? What is its importance? It is the amount of Hb expressed as percentage of the volume of a RBC or it is the Hb concentration in a single RBC. Normal value is 33 per cent (range: 35 ± 3%). MCHC is determined to know whether the RBC is normochromic or hypochromic. 57. Can it be possible to be hyperchromic anaemia? No, as MCHC can never be more than 38% because it cannot hold Hb beyond the saturation point. 58. What will happen a. If iron in heme is present in ferric form 20 VIVA IN MEDICAL PHYSIOLOGY b. If HBF persists during adult life: i. Ferric form of iron will bind O2 tightly resulting no removal of O2 from iron atom and then O2 can not be used by the body. ii. If HBF is present in adult blood there is shifting of O2 dissociation curve to the left because of less affinity of HbF for 2-3-DPG resulting more uptake of O2 in lungs and less release of O2 in tissues. 59. What will happen if folic acid is given to pernicious anemic patient? The administration of folic acid to pernicious anemic patient will improve the blood picture but it can not protect against neuropathy which is due to deficiency of vit-B12. 60. What is the role of iron in the body? These are: synthesis of hemoglobin, myoglobin and cytochromes. 61. What is the blood and bone marrow picture in iron deficiency anemia? The RBCs are microcytic, hypochromic and MCH, MCHC and total RBC count is reduced, whereas the bone marrow shows proliferation of the precursor cells with a larger proportion of the mature forms. Some of the precursor cells may show scanty, polychromatic cytoplasm with a pyknotic necleus, i.e. the cytoplasmic maturity is less than nuclear maturity. 62. What is the blood and bone marrow picture in megaloblastic anemia? The blood picture is characterised by macrocytosis, anisocytosis, poikilocytosis, neutropenia with over matured neutrophils and also thrombocytopenia. Whereas in bone marrow all the RBC precursors show megaloblastic changes that includes: 1. Larger cell with larger nucleus 2. More reticular chromatin 3. Normal hemoglobinisation of cytoplasm. BLOOD 21 SECTION I : THEORY VIVA 63. What is the dietary, active and therapeutic form of folic acid? • Dietary form: polyglutamates • Active form: tetrahydropholate • Therapeutic form: pteroylglutamic acid 64. What are the effects of foliate deficiency? This results defective erythropoiesis resulting megaloblastic anemia. 65. Compare and contrast the folic acid, vit-B12 and iron deficiency anemia. Iron deficiency anemia Folic acid deficiency anemia Vit-B12 deficiency anemia RBC s are microcytic and hypochromic RBC s are macrocytic RBC s are macrocytic Bone marrow shows hyperplasia of red cell precursors Bone marrow shows megaloblastic changes and presence of erythroblasts Bone marrow shows megaloblastic changes and presence of erythroblasts Nuclear maturation of RBC is normal Nuclear maturation of RBC is impaired Nuclear maturation of RBC is impaired. No associated neurological hazzards No associated neurological hazzards Associated neurological hazzards 66. Give characteristics features of (i) iron deficiency anemia (ii) pernicious anemia. i. Characteristics feature of iron deficiency anemia is as follows: • Microcytic hypochromic RBC • MCV, MCH, MCHC and CI decreases • RBC count decreases or remains normal • Normoblastic hyperplasia of bone marrow • Normal WBC and platelet count • Soft, brittle and spoon shaped nail • Angry red tongue and dysphagia • Irritability, loss of concentration, headache, impotence • Early breathlessness, palpitation 22 VIVA IN MEDICAL PHYSIOLOGY ii. Characteristics feature of pernicious anemia is as follows: • Microcytic normochromic RBC • Marked decrease in RBC count and Hb concentration • Lemon yellow coloured skin due to anemic paleness and mild jaundice • MCV, MCH increases and MCHC remains normal • Increase in reticulocyte count • Low grade hemolytic jaundice • Increase in serum iron concentration • Paresthesia, i.e. numbness, tingling, burning sensation ataxia, etc. 67. Define colour index. It is the ratio of Hb to RBC which is normally about 1 (range 0.85-1.15). 68. What is PCV? It is the percentage composition of the cells in the whole blood. 69. What is ESR? How it differs from PCV? ESR is the rate of settling of red cells in a special tube fixed vertically. To determine PCV the tube containing anticoagulant mixed blood is required to be centrifuged whereas in ESR centrifugation is not required. 70. What is importance of ESR? It helps to diagnose broader aspect of some disease though it has got more prognostic value. It helps in assessing the progress of patients treated for chronic diseases like pulmonary tuberculosis and rheumatoid arthritis. 71. What happens if the RBC is kept in hypotonic and hypertonic saline? • In hypotonic solution, water moves inside the RBC cell due to concentration gradient → swelling up of RBC →increase of RBC volume →rupture (hemolysis) of RBC takes place. SECTION I : THEORY VIVA • BLOOD 23 In hypertonic solution, water moves out of the cell → shrinkage of the cell (crenated). 72. What is the clinical significance of doing osmotic fragility test? It is a screening test in various types of hemolytic anemia and also used as a diagnostic purpose in hereditary spherocytosis. 73. Enumerate the variations of osmotic fragility of RBC. Osmotic fragility is decreased during acholuric jaundice and some anemias. Whereas it is increased during hereditary spherocytosis, deficiency of glucose-6phosphate dehydrogenase, cobra bite, etc. 74. At what serum bilirubin level clinical jaundice occurs in adults and infants? • In adult: If serum bilirubin increases beyond 2 mg% it results jaundice • In infants: If serum bilirubin increases beyond 5 mg% it results jaundice 75. Why jaundice is first detected in the eyes? It is because of whiteness of sclera. Sclera has a protein known as elastin which has high affinity to bind bilirubin. So even in low grade of jaundice bilirubin can get bind with sclera. 76. What is the clinical importance of glycosylated hemoglobin? The blood level of glycosylated hemoglobin (HbA1C) reflects the average blood glucose level over the period of preceding 5-8 weeks and thus serves as an index of long-term control of diabetes mellitus. Thus a pateint if becomes careless about controlling his hyperglycemia and takes an insulin injection only before visiting his doctor would have normal blood glucose but his HbA1C will be raised. 24 VIVA IN MEDICAL PHYSIOLOGY 77. Why does stool darken on standing in air? It is due to the conversion of residual urobilinogens (colourless) to coloured urobillins. 78. What is prehepatic jaundice? Why it does result in unconjugated hyperbilirubinemia? When jaundice occurs due to increased formation of bilirubin it is called as prehepatic or hemolytic jaundice. In this case the liver is unable to conjugate the large amounts of bilirubin produced resulting in unconjugated hyperbilirubinemia. 79. What is post hepatic jaundice? Why it does result in conjugated hyperbilirubinemia? If the jaundice occurs due to biliary obstruction it is known as post hepatic jaundice. In this case the conjugated bilirubin produced in the liver regurgitates back into blood instead of flowing out into the duodenum. This is why it results in conjugated hyperbilirubinemia. 80. What is hepatic jaundice? Why it does usually result in conjugated hyperbilirubinemia? The jaundice due to the impairment of all steps of bilirubin metabolism in liver is known as hepatic jaundice. The commenest cause is infective hepatitis. In this case the excretion of bilirubin is worstly affected that results in conjugated hyperbilirubinemia. 81. What are trephones? These are the substances prepared by leucocytes from plasma proteins that help in tissue nutrition. 82. What is the average period for normal development of neutrophils? 12 days. 83. Why the neutrophils are called polymorphs? Because they have multilobed nucleus. 84. Why neutrophils are so named? This is a misnomer because they are not stained by the BLOOD 25 SECTION I : THEORY VIVA neutral stain rather by the mixed (both acidic and basic) stain like Leishman stain. 85. Which stain is generally used to stain the peripheral blood smear? It is Leishman stain. 86. Which is the largest cell in the peripheral blood? It is monocyte (diameter 15-20 µm). 87. What is respiratory burst? Within seconds of stimulation neutrophils sharply increase their oxygen uptake which is known as respiratory burst. 88. What is Cook-Arneth count? What is its significance? Counting of neutrophils on the basis of the number of lobes of their nuclei is called Cook- Arneth count. Clinical significance: It represents the maturity of neutrophils. If shift to the left occurs that indicates the hyperactive bone marrow whereas hypoactive bone marrow is indicated by shift to the right. 89. How do you differentiate between neutrophils, eosinophils and basophils? Parameter Neutrophils Eosinophils Basophils 1. Size of the cell 2. Number of lobes in nucleus 10-14 µm. 10-16 µm 10-14 µm Multilobed Usually bi lobed bi lobed 3. Shape of nucleus Irregular Spectacleshaped Usually ‘S’ shaped 4. Colour of granules in cytoplasm Pinkish Brick red Purple 5. Nature of granules Very fine Coarse Very coarse, making the nucleus obscure Very dense Small in number 6. Number of granules Few 26 VIVA IN MEDICAL PHYSIOLOGY 90. How do you differentiate small and large lymphocyte? Which one is more mature? Parameter Small Lymphocyte Large Lymphocyte 1. Size of the cell Almost equal to the RBC size Almost twice of RBC 2. Amount of cytoplasm Very thin layer of cytoplasm present only in periphery Plenty in compare to small lymphocyte. 3. Shape of nucleus Round Round or oval Small lymphocyte is more mature. 91. How do you differentiate large lymphocyte with monocyte? Parameter Large lymphocyte Monocyte 1. Size Twice of RBC Almost thrice of RBC 2. Shape of nucleus Round or oval Indented or kidney-shaped 3. Position of nucleus Central Eccentric 4. Amount of cytoplasm More than half of the cell. Less than half of the cell 92. What is Schilling index? Arranging and counting of all leucocytes according to their age is known as Schilling index. 93. What are the body’s Ist line of defense and where they are located? It is monocyte macrophage system or RES. They are located in almost all the tissues but in different form, e.g.: • In skin and subcutaneous tissues — Histocytes • Lungs — Alveolar macrophages • Intestine — Lymphoid tissue • Liver and spleen pulp — Kupffer cells. 94. Which lobed neutrophils are most active? It is three lobed neutrophil (N3). SECTION I : THEORY VIVA BLOOD 27 95. What do you mean by shift to the left and what is its significance? In Arneth count, if N1 + N2 + N3 becomes greater than 80 percent then it is known as shift to left or regenerative shift. It indicates the hyperactive bone marrow. 96. What is shift to the right? What is its significance? In Arneth count, if N4 + N5 + N6 is greater then 20 per cent it is called as shift to right or degenerative shift which indicates the hypoactive bone marrow. 97. Is trilobed eosinophil possible? Yes, 15 percent of eosinophils are trilobed. 98. What are the stages of phagocytosis of WBC? These are as follows: Diapedesis → chemotaxis → opsonisation and then phagocytosis → which causes degranulation → then inflammatory response → finally stops or limits inflammation. 99. Classify the lymphocytes. Histologically—two types: Small and large lymphocytes. Functionally—two types: T-lymphocytes (responsible for cellular immunity) and B-lymphocytes (responsible for humoral immunity). 100. Define neutrophilia and neutropenia. Mention each of their causes. Increase in the number of neutrophils in differential count and absolute count (over 10,000 cumm of blood) is called as neutrophilia. Causes Pathological • Acute pyogenic infection like abscess, tonsilitis, appendicitis, etc. • Burn, acute hemorrhage and hemolysis • Tissue necrosis like myocardial infarction and renal infarction. 28 VIVA IN MEDICAL PHYSIOLOGY Physiological: Muscular exercise, stress, pregnancy, etc. Neutropenia: The clinical condition characterised by the reduction of neutrophil count in both differential and absolute count is called as neutropenia. Causes • Viral infection like typhoid, paratyphoid, AIDS, Kalaazar, etc. • Bone marrow depression. 101. Define eosinophilia and eosinopenia. Mention their causes. Increase of absolute eosinophil count more than 500 cells per cumm of blood is called as eosinophilia whereas the reduction of the absolute count below 50 cumm of blood is known as eosinopenia. Causes of eosinophilia—Allergy, parasitic infection, leukaemia, etc. Causes of eosinopenia—ACTH or glucocorticoid therapy, acute stressful illness and acute pyogenic infection. 102. What is basophilia? When does it occur? Increase of absolute count of basophil more than 100 cumm is known as basophilia. It occurs in viral infection like small-pox, chickenpox and also in chronic myeloid leukaemia. 103. What is monocytosis? Mention the causes of monocytosis and monocytopenia. Increase in the count of monocyte (absolute count >5000/ cumm of blood) is called as monocytosis. Causes of monocytosis—Malaria, Kala-azar, Rheumatoid arthritis, Leukaemias, etc. Causes of monocytopenia—Bone marrow depression. 104. Define lymphocytosis and lymphopenia. When do they occur? High lymphocyte count (absolute count > 5000/cumm of blood) is known as lymphocytosis. It occurs in viral infection like chickenpox, whooping cough, etc., chronic SECTION I : THEORY VIVA BLOOD 29 infection like TB, hepatitis, leukaemia, etc. Whereas low lymphocyte count in peripheral blood is known as lymphocytopenia. It is seen in patients with steroid therapy. 105. What is leukaemoid reaction? Extreme increase of TLC (>50,000/cumm of blood) characterised with elevated level of leucocyte alkaline phosphatase due to severe infection is known as leukaemoid reaction. Its difference with leukaemia is that in case of leukaemia alkaline phosphatase level is reduced whereas here it is increased significantly. 106. What is leucocytosis? Name the physiological and pathological condition causing leucocytosis. Increase in TLC beyond 11000 cells/cumm of blood is called leucocytosis. Physiological condition—Newborn babies, exercise, parturition, etc. Pathological condition—Acute pyogenic infection like boils, abscess, tonsilitis, appendicitis and also MI, burns and malignancies. 107. What is leukopenia? Name the physiological and pathological conditions causing leukopenia. Decrease of the TLC below 4000 cells/cumm of blood is known as leukopenia. Causes Physiological condition — Exposure to extreme cold. Pathological condition — Nonpyogenic infection like typhoid, paratyphoid fever. • Viral infection like influenzae, smallpox and AIDS. • Arsenic and Antimony poisoning, • Vit. B12 and folate deficiency. • Malnutrition and starvation. 108. What is the leukaemia? What is its difference with leukocytosis? Leukaemia is a group of malignant neoplasms resulting 30 VIVA IN MEDICAL PHYSIOLOGY from uncontrolled proliferation of hemopoietic leukocytic stem cells of bone marrow and lymphoid tissue. In this case, TLC becomes much higher than leukocytosis, i.e. 1-3 lac/cumm and number of immature cells are dominant. 109. Mention the functions of platelets. These are to: protect endothelial linning of blood vessels, initiate blood clotting, hasten clot retraction, release histamine and prostaglandin for vasoconstriction. 110. What are the events involved in hemostasis? These are: a. Vasoconstriction b. Formation of temporary hemostatic plug. c. Conversion of temporary hemostatic plug into secondary or definitive hemostatic plug by fibrin. 111. How the primary hemostatic plug is formed? It is represented by the following sequences: Platelets adhesion → platelets activation → platelets aggregation →activation of phospholipase A2 →release of arachidonic acid from membrane phospholipids → release of thromboxane A2 and prostacyclin → this ultimately causes adhesion of more and more platelets and then platelets are aggregated with each other to seal the rupture of blood vessels temporarily. 112. What are the principle causes of hemorrhagic state in the body? These are: a. Defect in the blood vessels due to infection, allergy, etc. b. Defect in platelets (purpura) c. Defect in clotting mechanism. 113. Which coagulation factor is lacking in hemophilia? It is factor VIII or anti-hemophilic globulin. SECTION I : THEORY VIVA BLOOD 31 114. What is clot retraction? What is the role of platelets in clot retraction? After the formation of clot, it starts contracting and after about 30-45 min, a straw coloured fluid, i.e. serum oozes out. This process of contraction of clot and oozing of serum out of clot is called as clot retraction. The platelets contribute directly to clot retraction by releasing the platelet thrombosthenin, actin and myosin which causes strong contraction of the platelet spicules attached to the fibrin. 115. Name some anticoagulants used in hematological study. These are: sodium citrate, potassium oxalate, amonium oxalate, EDTA, etc. 116. Why blood do not clot in the body? This is because of following reasons: • Smoothness of endothelial lining which prevents platelet adhesion. • Negativity of endothelial lining that repels the negatively charged plasma clotting factors. • High blood pressure that increases velocity of blood. • Presence of natural anticoagulants like heparin and protein C in the blood. • Simultaneous activation of fibrinolytic system along with clotting mechanism. This causes lysis of fibrin molecules. 117. What is the mode of action of heparin as an anticoagulant? It inhibits the reaction between thrombin and fibrinogen and also interferes in formation of thromboplastin. 118. What is the importance of vit K in coagulation? Vitamin K serves to maintain the plasma prothrombin level. 32 VIVA IN MEDICAL PHYSIOLOGY 119. What is platelet ratio? It is the ratio of platelets to RBC which is about 1:16 to 18. 120. Which one is the principal plasma protein associated with rate of sedimentation of RBCs.? It is fibrinogen. 121. What are indications of BT and CT? These are: a. Frequent and persistent bleeding from minor injuries. b. Before the minor/ major surgeries. c. In case of family history of bleeding. 122. Which aspects of hemostasis are tested by BT and CT? BT is to test for platelet function whereas CT is to test the abnormalities (if any) in clot formation. That is why in hemophilia BT is normal but CT is prolonged as in hemophilia, temporary hemostatic plug is formed because of normal functioning of platelets but they are washed off by the flowing blood as definitive hemostatic plug, i.e. clott is not formed. 123. Mention the conditions when BT and CT is prolonged. BT is increased during thrombocytopenic purpura, allergic and also senile purpura, infection like typhus, bacterial endocarditis, deficiency of vitamin C, etc. CT is prolonged in hemophilia, afibrinogenemia, vitaminK deficiency, liver disease, etc. 124. What are the physiological and pathological variations of platelet count? Physiological Increase of count—in severe exercise and high altitude Decrease of count—in newborn babies and after menstruation Pathological Increase of count—Severe hemorrhage and removal of spleen. SECTION I : THEORY VIVA BLOOD 33 Decrease of count—Bone marrow depression, acute septic fever, aplastic anaemia, toxemia, autoimmunodestruction of platelets, AIDS, etc. 125. What is the basic difference between intrinsic and extrinsic system of blood clotting? In the intrinsic system, injury to blood cells like platelets, releases phospholipid that activate different clotting factors to induce clotting. Whereas in the extrinsic system injury to blood vessels or nearby tissues releases tissue thromboplastin which induces clotting mechanism by activating different clotting factors by cascade mechanism. 126. What is prothrombin time? What is its significance? Prothrombin time is the test for prothrombin activity and thereby it is a test for testing the extrinsic system of blood coagulation. Normal value of prothrombin time is 11-16 sec and it is increased in liver failure and deficiency of vitamin-K. It is generally used to monitor patients with anticoagulants therapy to adjust its dose. 127. Mention the role of Ca++ in clotting mechanism. Except for the first 2 steps in the intrinsic pathway calcium ions are required for the promotion of all reactions involved in both intrinsic and extrinsic pathway. 128. Why Ca++ deficiency does not produce coagulation defects? Only traces of calcium ions are required for coagulation of blood which are normally available in the body. 129. Why clot does not spread in the injured vessel after blood coagulation? The reasons are: • Removal of some activated clotting factors specially IX, X, and XII from the circulation by antithrombin III secreted by the liver. • Reduction in the supply of clotting factor. • Balancing activity of thromboxane A2 and prostacyclin 34 VIVA IN MEDICAL PHYSIOLOGY that prevent excessive extension of clot and maintaining blood flow around it. 130. How a balance is maintained between the clotting mechanism and fibrinolytic system in the body? Factors that initiate clotting mechanism also stimulate the dissolution of clot (fibrinolysis) by the following mechanism. 131. What is purpura? What are its causes? The purpura is purple coloured petechial hemorrhagic condition with bruises in the skin due to the degradation of Hb over a period of time. The causes are thrombocytopenia, allergy, old age, functional platelet defects, etc. 132. What is the difference between thrombocytopenia and thromboasthenia? Reduction of platelet count below 1.5 lakh/cumm of blood is known as thrombocytopenia whereas impairment of platelet functions due to presence of abnormal platelets are known as thromboasthenia. 133. Name two well known vascular causes of bleeding? Scurvy and Cushing Syndrome. 134. Why does vit-K deficiency cause bleeding tendency? This is due to the facts that Vitamin K deficiency results in low plasma levels of both procoagulants as well as some anticoagulants. These proteins are called vitamin K dependent proteins. SECTION I : THEORY VIVA BLOOD 35 135. Why does blood become incoagulable following violent death? In case of violent death, the blood remains in fluidic and incoagulable in nature due to fibrinolysis resulted due to adrenaline induced rapid release of plasminogen activators from endothelial cells. 136. What is the difference between rouleaux formation and agglutination? Rouleaux formation is simply stacking of RBCs without any hemolysis whereas in agglutination there is antigenantibody reaction on the red cells resulting hemolysis of RBC. 137. Name the cold antibodies present in our body. ABO antibodies are the cold antibodies because they act best at low temperature, i.e. between 5°C-20oC. 138. Name the warm antibodies present in our body? Rh-antibody is the warm antibody because they act best at normal body temperature, i.e. 37°C. 139. What are the indications of blood transfusion? These are blood loss, blood disorders like hemophilia, purpura, blood diseases like leukaemia, severe anaemia, CO poisoning, shock, etc. 140. What do you mean by major and minor crossmatch? What is its clinical significance? In the cross-matching technique, the red cells and the plasma of donor and recepient’s blood are first separated by centrifugation. Then if the donor’s red cells are treated with recepients plasma it is known as major cross-match and if the donor’s plasma is reacted with recepients RBC it is known as minor cross-match. If no agglutination takes place in both the occasions then only the donor’s blood is used to the recepient. 36 VIVA IN MEDICAL PHYSIOLOGY 141. What is Landsteiner’s law? Is it applicable in all types of blood groups? In an individual, if an agglutinogen is present in his RBCs, the corresponding agglutinin will be absent in his plasma and similarly if an agglutinin is present in his plasma, the corresponding agglutinogen will be absent in his RBC. This law is known as Landsteiner’s law. This law is not applicable to other blood group systems as there are no naturally occurring antibodies present in those systems. 142. In ‘O’ blood group no antigens are there, still both antibodies are present in plasma. How these antibodies are formed? Any of the specific blood group antibodies are absent at birth but in childhood while taking some foods like seed and plants or from intestinal bacteria these nonselfantigens are absorbed from GI tract to blood and thereby induces to develop the antibodies against that particular antigen or antigens. 143. Name the various Rh-agglutinogens in Rh-system? These are C,c, D,d, E and e. Of these ‘D’ is clinically important which may be positive or negative, i.e. present in blood or absent respectively. 144. Why ABO incompatibilities rarely produce hemolytic disease of newborn? It is because the alpha and beta antibodies are of IgM type of antibodies having large MW. This is why these can not pass through the placenta to result agglutination of RBCs. 145. Why the stored blood is not suitable for transfusing WBCs and platelets to a recipient? It is because the blood stored for more than 24 hours does not contain active WBCs and platelets. SECTION I : THEORY VIVA 146. BLOOD 37 The term universal donor and universal recipient are no longer valid. Justify In both the cases complications can also be produced due to mismatching of Rh factors and other blood groups. 147. What changes RBCs undergo during cold storage? Cold storage results following changes: • appearance of spherocytic RBC due to net increase in volume of cell . • increase in tendency of hemolysis. 148. At what age after birth a child’s blood group is set in it’s true ABO type? During adolescence i.e. upto 10 years. 149. How hemolytic disease in a newborn can be prevented? It is by removing small quantities of infant’s blood successively from IVC and replacing an equal amount of compatible Rh- blood. 150. What is the management of hemolytic transfusion reactions? In case of hemolytic transfusion reactions transfusion must be stopped immediately and the patient is to be given intravenous injection of rapid acting corticoids. 151. What do you mean by secretors and nonsecretors? The A and B antigens are also present in other tissues like liver, pancreas, kidney, etc. and also in body fluids like saliva, semen, etc. The individuals who have high concentration of these antigens in their body fluids are called secretors and those having low concentration of these antigens in their body fluid are known as nonsecretors. 152. What are human leucocyte antigens (HLA) and what is their importance? HLA are the antigens present on the surface of WBCs. 38 VIVA IN MEDICAL PHYSIOLOGY HLA typing is done before tissue or bone marrow transplant since they are responsible for early rejection of transplant. 153. Name the factors promoting erythropoiesis. These are hypoxia, iron, porphyrin, traces of cupper, cobalt, protein, vitamin-C, thyroxin, hematinic principle, maturation factor, etc. 154. Why spleen is not essential for life? The function of spleen can also be maintained by some other organs and tissues like Kupffer cells in liver, lymph nodes, subcutaneous tissue, osteoclasts, microglia in brain, lymphocytes, thymus gland, etc. This is why it is not essential in life, however in absence of spleen bacterial infections are more common and severe. 155. Why incidences of tumours are more with advancing age? It is because of the gradual declining of cellular immune mechanism. 156. Why we do not make an immunological response of our own body proteins? Body has got the capacity to identify it’s own ‘self’ protein against of which no immunological response is evoked. CARDIOVASCULAR SYSTEM 39 SECTION I : THEORY VIVA 1.3 Cardiovascular System 1. What structural characteristics of cardiac muscle enable its continuous rhythmic contractions? These are: Presence of pacemaker cell that initiates autorhythmicity, presence of special conductive tissue and presence of free branchings between the muscle fibres (syncytium) ensure the quick passage of impluse from pacemaker cell to all parts of heart to initiate continuous rhythmic contractions. 2. Name the special conducting tissues of heart. SA node, AV node, bundle of His and Purkinje fibre. 3. What is cardiac pacemaker? SA node is called as the cardiac pacemaker because it is made up of ‘P’cells which can generate the impulse more rapidly than any of the pacemaker tissue of heart and thereby determine the rate at which the heart beats. 4. What is law of heart muscle? It states that the size of muscle fibers, glycogen content and rate of conduction increases from nodal to Purkinje’s fiber whereas length of systole, duration of refractory period and rhythmicity increases in the reverse direction. 5. What is intercalated disc and what is its importance? At the point of contact of two cardiac muscle fibers, extensive folding of cell membrane occurs which is known as intercalated discs. They provide a strong union 40 VIVA IN MEDICAL PHYSIOLOGY between fibers so that the pull of one contractile unit can be transmitted to the next, thereby helps in increasing force of contraction. 6. What is the role of gap junction in cardiac muscle? Gap junction is present in the intercalated disc of cardiac muscle fibers and helps in rapid transferring of electrical currents, ions, etc. from one cell to another without coming in contact with ECF. Thus they provide low resistance bridge for the rapid spread out of electrical impulse, thereby helps the cardiac muscle to act as syncytium (functional). 7. Name the valves and their location. There are 4 valves—two in between the atria and ventricles known as atrio-ventricular valves (A-V valves) and two are at the opening of the blood vessels arising from the ventricles (semilunar valves). a. A-V valves: These are present in between the atria and ventricles. The valve present in between right atria and right ventricle is known as Tricuspid valve and the valve present in between left atria and left ventricle is known as Bicuspid valve. b. Semilunar valves: There are two semilunar valves namely Pulmonary valve and Aortic valve. The pulmonary valve is present at pulmonary orifice which leads from RV to pulmonary artery and the aortic valve is present at aortic orifice which leads from LV to the aorta. 8. Name the special junctional tissues and their conduction rate. The special junctional tissues and their rate of impulse generating capacity are: Special junctional tissues Impulse generating capacity S A Node A V Node Bundle of His Purkinje’s fiber 75 ± 5 times/min 60 times/min 40 times/min 20 times/min SECTION I : THEORY VIVA CARDIOVASCULAR SYSTEM 41 9. What do you mean by pacemaker potential or diastolic depolarisation? The pacemaker tissue is characterised by unstable RMP due to slow depolarisation resulting from leakage of Na+ from outside to inside through Na+ leak channels. This show leakage of Na+ inside the cell causes increase in electropositively inside the cell which ultimately enables to induce another action potential easily. This slow polarisation in between action potential is known as prepotential or pacemaker potential or diastolic depolarisation. 10. Why SA node is called as cardiac pacemaker? SA node acts as a pacemaker of heart because the rate of impulse generation in normal heart is determined by this node because of its highest rate of impulse generating capacity (75 ± 5 times/min) than other junctional tissues. This is why it is known as cardiac pacemaker. 11. What is ectopic pacemaker? When the pacemaker is other than SA Node (e.g. AV node, etc.) it is called as ectopic pacemaker. 12. What do you mean by nodal and idioventricular rhythm? The AV node takes the charge of generating impulse rhythmically when SA node does not work. In this condition atria and ventricles beat almost simultaneously at the rate of 60 times per min. This rhythm of heart is known as Nodal rhythm. Whereas 2nd Stannius ligature applied over the A-V groove makes the atria to continue beating with it’s own rhythm whereas the ventricle stops beating due to blockade of impulse from atria to ventricles. After sometimes ventricle generates it’s own impulse and starts beating at much slower rate. This rhythm of heart beat in which atria and ventricular beating do not follow any specific pattern is known as idioventricular rhythm. 42 VIVA IN MEDICAL PHYSIOLOGY 13. What is AV delay? What is its significance? When the impluse reaches to AV node, there is a delay of about 0.1 sec to pass the impulse to bundle of His. This time gap is known as AV delay. It allows the atria to contract just ahead of ventricular contraction thereby atria is emptied before ventricular ejection. 14. What is Frank-Starling's law? Within the physiological limit the larger the initial length of muscle fiber (end diastolic fiber length), the greater will be the force of contraction of the heart which is known as Frank-Starling's law of heart. 15. What is the ionic basis of plateau phase of cardiac action potential? Immediately after depolarisation voltage gated Na+ channel's used to close resulting stoppage of entry of Na+ ions and voltage gated K+ channel starts opening resulting exit of K + . These result rapid fall of electropositivity initially known as rapid repolarisation. Afterwards, the rate of repolarisation becomes slower due to prolonged opening of voltage gated Ca+2 channel through which Ca+2 enters inside. Thus the exit of K+ is almost counterbalanced by entry of Ca+2 resulting sustained depolarisation known as plateau phase. 16. Is all or none law applicable in heart? All or none law which states that if a stimulus is applied, whatever may be the strength of stimulus, the cardiac muscle responds maximally or it does not give any response at all. Of course it is applicable only in whole artrial muscle (i.e. atrial syncitium) or in whole ventricular muscle (i.e. ventricular syncitium) not to a single cardiac muscle fiber. 17. Why left ventricular subendocardial region is more prone to myocardial infarction? The blood supply to the cardiac muscle in different areas of heart is not same. On the surface of the cardiac muscle SECTION I : THEORY VIVA CARDIOVASCULAR SYSTEM 43 there are large epicardial arteries supplying more blood to those areas whereas in the subendocardial region blood supply is less because it is supplied by smaller intramuscular arteries and plexus of subendocardial artery the diameter of which are less. This blood supply to the subendocardial plexus is further reduced during systole. Therefore the subendocardial region is more prone to myocardial infarction. Again as the left ventricular thickness is much more than that of right ventricle the occlusion is more severe in left ventricle. For this region LV subendocardial region is more prone to MI. 18. What are the importance of anastomatic channels in heart muscle? In the normal heart there are some collaterals among the smaller arteries which become active under abnormal conditions like myocardial ischemia. They open up within a few seconds after the sudden occlusion of larger artery and become double in number by the end of 2nd or 3rd day and reach to normal by one month. When atherosclerosis causes constriction of coronary arteries slowly over a period of many years, collateral vessels develop restoring normal blood and thus the patient never experiences acute episode of cardiac dysfunction. 19. What is the importance of autoregulation in blood supply in heart muscle? Like some other organs the heart has the capacity to regulate it’s own blood flow up to a certain limit in order to maintain an almost constant blood flow to the cardiac musculature inspite of any alteration of systemic blood flow. This is known as autoregulation of coronary blood supply. 20. What is angina pectoris? Due to myocardial ischemia there is stimulation of nociceptors present in heart muscle resulting pain sensation which is normally referred to upper sternum, 44 VIVA IN MEDICAL PHYSIOLOGY left forearm, left shoulder, neck and side of the face. This clinical condition is known as angina pectoris. 21. Why cardiac muscle cannot be tetanised? It is because of it's long absolute refractory period and thus summation of contractile response is not possible which is essential for tetanisation of heart muscle. 22. What is staircase effect in heart muscle? When the cardiac muscle begins to contract after a brief period of rest (e.g. following vagal stimulation) its initial length of contraction increases before reaching to a plateau. This phenomenon is called as staircase effect or treppe response. 23. What is cardiogram? The record of the mechanical activity of the heart is known as cardiogram. 24. Mention the maximum and minimum pressure in heart during systole and diastole? Chamber Peak pressure in systole Min. pressure in diastole Left ventricle Right ventricle Left atrium Right atrium Aorta 120 mm Hg 25 mm Hg 15 mm Hg 6 mm Hg 120 mm Hg 5-12 mm Hg 2-6 mm Hg 5-8 mm Hg 1-5 mm Hg 80 mm Hg Pulmonary artery 25 mm Hg 5-12 mm Hg 25. Define and give normal values of end diastolic volume, stroke volume and end systolic volume. During ventricular diastole the intraventricular volume is increased which results filling of the ventricles. At the end of diastole the amount of blood filled by the ventricle is known as end diastole volume (EDV). It is about 120130 ml. During ventricular systole intraventricular volume decreases which results increase in pressure thus SECTION I : THEORY VIVA CARDIOVASCULAR SYSTEM 45 ejection of blood out of ventricles. During each systole the amount of blood pumped out by each ventricle is known as stroke volume (SV). Normal value:70 ml/beat. At the end of systole however some amount of blood is remained in each ventricle which is known end systolic volume (ESV). The normal volume: 50-60 ml/ beat. 26. What do you mean by vagal escape? What is its cause? If strong vagal stimulation to heart is continued then after a pause the ventricles resume to beat at a slow rhythm which is called as vagal escape represented by the Figure 1.3.1. Fig. 1.3.1: Demonstration of vagal escape on heart muscle During prolonged vagal stimulation right auricle stops beating and distends due to blood overflow which leads to fall of BP → afferent impulse from carotid sinus to cardiac centers →stimulate ventricles to start its beat. 27. Define apex beat. Apex beat is the impulse or throb which is felt and seen on the chest wall normally in the left 5th intercostal space just medial to left nipple. 28. Name different phases of cardiac cycle. Mention the duration of each phase. Phases of cardiac cycle Duration in sec a) b) c) 0.1 0.7 0.3 Total 0.05 Atrial systole Atrial diastole Ventricular systole i) Isovolumetric contraction Contd... 46 VIVA IN MEDICAL PHYSIOLOGY Contd... Phases of cardiac cycle d) ii) Rapid ejection phase iii) Slow ejection phase Ventricular diastole i) Protodiastole ii) Isovolumetric relaxation iii) Filling phase • Ist rapid filling phase • Slow filling phase • Last rapid filling phase Duration in sec 0.1 0.15 0.5 Total 0.04 0.08 0.38 Total 0.1-0.12 0.18-0.20 0.06-0.10 29. What is protodiastole? Is it part of systole or diastole? Protodiastole is the very brief phase before diastole in which ventricular systole has ceased but relaxation yet to start. It can not be well defined whether the protodiastole is a part of systole or diastole as some workers include it in diastole as muscle contraction is stopped at this phase whereas some others believe that it is a part of systole as muscle relaxation has not yet started. 30. Define cardiac cycle. The sequence of events (mechanical,electrical, etc.) associated with consecutive heart beat is repeated cyclically which is known as cardiac cycle. Normal duration is 0.8 sec if heart rate is 75 beats/min. 31. What are the causes of 1st heart sound? These are: i. Closure and vibrations of AV valves at the beginning of ventricular systole. ii. Vibrations of blood surrounding the AV valves. iii. Vibrations of major blood vessels around the heart. iv. Vibrations of walls of heart. 32. What are the characteristics of 1st heart sound? It is: • Soft, prolonged with low pitch. SECTION I : THEORY VIVA • • CARDIOVASCULAR SYSTEM 47 Duration is 0.12 sec and occurs in peak or downstroke of R wave in ECG and just before onset of ‘c’ wave in jugular pulse tracing. Best heard at apex beat area and is associated with onset of ventricular systole. 33. What is the significance of 1st heart sound? It indicates force of contraction, condition of myocardium and competence of AV valves. 34. What are the causes of 2nd heart sound? These are: Closure and vibration of semilunar valves at the end of ventricular systole. Vibrations of blood surrounding these valves. Vibrations of walls of aorta and pulmonary artery. Vibrations of the wall of ventricles to a little extent. 35. What are the characteristics of 2nd heart sound? It is: • Sharp, short and high pitched. • Duration is 0.08 sec and follows T wave in ECG and coincides with ‘v’ wave in jugular venous pulse tracing. • Best heard at 2nd right costal cartilage for aortic component and 2nd intercostal space at left sternal border for pulmonary component. • Associated with onset of ventricular diastole. 36. What is the significance of 2nd heart sound? It indicates the competence of semilunar valves. 37. When and how 3rd heart sound is produced? 3rd heart sound is produced during the first 1/3 of ventricular diastole. It occurs due to the vibrations set up by the rushing of the blood during the rapid filling phase of ventricular diastole. 48 VIVA IN MEDICAL PHYSIOLOGY 38. Differentiate 1st and 2nd heart sound. 1st heart sound i. It is prolonged, lowpitched and soft. ii. Coincides with carotid pulse iii. Coincides with R wave of ECG iv. Best heard over the mitral area v. Time interval between 1st and 2nd is shorter 2nd heart sound It is sharper, abrupt, clear and high pitched Does not coincide May precede, coincide or follow the T wave of ECG. Best heard over aortic and pulmonary area. Time interval beween 2nd and next 1st is comparatively longer. 39. What is murmur? It is the sound produced by turbulence produced in the blood by a forward flow through a stenosed (narrowed) valve or back flow (regurgitation) through a deformed or incompetent valve. 40. How do you classify murmur? It will be classified on the basis of their relationship with main heart sounds like presystolic, systolic, diastolic and also to and fro murmurs. 41. What are the maximum and minimum pressure in heart? • Maximum pressure in left ventricle is above 120 mm Hg. • Max pressure in right ventricle is above 25 mm Hg. • Minimum pressure in left ventricle is 80 mm Hg. • Minimum pressure in right ventricle is few mm Hg. 42. What is the normal heart rate? What are the factors affecting heart rate (HR)? Normal value of HR is 72 beat/min with the normal range is 60-90 beat/min. The factors are: age, sex, body temperature, hypoxia, emotion, exercise, etc. and drugs like epinephrine and norepinephrine. SECTION I : THEORY VIVA CARDIOVASCULAR SYSTEM 49 43. Why HR is slightly higher in females than males? It is because of two reasons: • Lower systemic BP • More resting sympathetic tone. 44. What is Cushing reflex? It is represented by following sequential events: Increased intracranial pressure → decreases blood supply to medullary hypoxia and hypercapnia → stimulation of medulary vasomotor center →increase of systemic BP →stimulation of baroreceptors →stimulation of vagus nerve →decrease of HR and respiration. This reflex mechanism by which increased intracranial pressure results bradycardia is known as Cushing reflex. 45. What do you mean by sinus arrhythmia? Heart rate increases with inspiration and decreases during expiration. This phenomenon is known as sinus arrhythmia. 46. State Mary’s law. If the other conditions remain constant then the HR is inversely related with systemic BP. 47. Define cardiac output, stroke volume and cardiac index. Cardiac output: The amount of blood pumped out by each ventricle per min is called as cardiac output. The normal value is 5 lit/min/ventricle. Stroke volume: The amount of blood pumped out by each ventricle in each beat is known as stroke volume. Normal value is 70 ml/beat/ventricle. Cardiac index: It is the cardiac output per square meter of body surface area. The normal value is 3.2 L/m2/min. 48. What do you mean by extrinsic and intrinsic autoregulation of cardiac output? If cardiac output is controlled by controlling only heart rate (as CO = HR × SV) it is known as extrinsic autoregulation of cardiac output whereas if it is regulated 50 VIVA IN MEDICAL PHYSIOLOGY by regulating only stroke volume, it is known as intrinsic autoregulation. 49. What is the difference between heterometric and homometric regulation of cardiac output? To control cardiac output when ventricular contraction is regulated by controlling initial length of the muscle fibre, i.e. EDFL, then it is called as heterometric regulation which is independent of cardiac nerves. Whereas when cardiac nerves regulate the myocardial contractility to control the cardiac output, it is known as homometric regulation of cardiac output. 50. What is Frank-Starling’s law of heart? What is its relation with venous return? It states that within the physiological limit, the force of ventricular contraction is directly proportional to the initial length of muscle fibres (EDFL). If venous return is increased the EDFL of the ventricular muscle is also increased resulting more force of ventricular contraction thereby more cardiac output. 51. What do you mean by Vis A Tergo and Vis A Fronte in relation to cardiac pump? Vis A Tergo is the force which drives the blood forward from behind, e.g. the contraction of the heart drives the blood in forward direction, whereas Vis A Fronte is the force acting from front that attracts blood in the veins towards the heart, e.g. ventricular systolic and diastolic suction pressure. 52. Enumerate the factors affecting venous return. The factors are: Thoracic or respiratory pump, cardiac pump, muscle pump, total blood volume and increased sympathetic activities on veins. 53. Name two methods by which cardiac output is measured. These are: • Direct Fick method and • Indirect dye dilution method. SECTION I : THEORY VIVA CARDIOVASCULAR SYSTEM 51 54. Enumerate Fick’s principle. It states that the amount of a substance taken up by an organ or by whole body per unit time is equal to the arterial level of that substances minus the venous level (i.e. A-V difference) times the blood flow, i.e. amount of substance taken/min = A-V difference of the substance × blood flow/ min. 55. What are the disadvantages of Fick’s method? These are: • As it is the invasive method the subject is exposed to all risk of hemorrhage, infection, etc. • As the subject is conscious of the whole technique cardiac output may be higher than normal. 56. Which dye is generally used in Dye dilution method and why? It is generally Evans blue or radio-active isotopes. Criteria for selection are as follows: • These stay in the circulation during the test. • These are not harmful and not toxic. • Do not alter the hemodynamics of blood flow. • Concentration of these substances can be easily measured. • Excreted totally and neither reabsorbed nor secreted by the body. 57. What is Ballistocardiogram? It is a record of the to and fro movements of the body in the headward to footward direction when the subject lies on a suitably suspended table. This is the another method of measuring cardiac output though it is now absolute. 58. What is Bundle of KENT? In the individuals with WPW syndrome, there is one additional nodal connecting tissue in between atria and ventricles besides AV node which conducts the impulse more rapidly than AV node. This additional conducting pathway is known as Bundle of KENT. 52 VIVA IN MEDICAL PHYSIOLOGY 59. Define blood pressure (BP). It is the lateral pressure exerted by the moving column of blood on the wall of blood vessels during its flow. 60. Define systolic, diastolic, mean and pulse pressure with each of their normal average values. Systolic pressure (SP): It is the maximum pressure exerted during systole of the heart. Normal value = 120 mm Hg (Normal range:110-140 mm Hg). Diastolic pressure (DP): It is the minimum pressure during diastole of the heart. Normal value = 80 mm Hg (Normal range: 60-90 mm Hg). Pulse pressure (PP): Pulse pressure is the difference between systolic and diastolic pressure. Normal value = 40 mm Hg. Mean pressure: It is average pressure during each cardiac cycle. Normal value = 93.3 mm Hg. 61. Enumerate the significance of SP, DP, PP and MP. • Systolic pressure indicates the extent of work done by the heart and also the force with which the heart is working. It also indicates the degree of pressure the arterial wall have to withstand. • Diastolic pressure is the measure of the total peripheral resistance and it indicates the constant load against which heart has to work. • Pulse pressure determines the pulse volume. Whereas mean pressure indicates the perfusion pressure head which causes the flow of blood through the arteries, arterioles, capillaries, veins and venules. 62. Why does systolic pressure increase after meal? After meal pressure over heart increases due to distended abdomen which in turn increases heart rate and also there is a release of epinephrine which also increases systolic blood pressure. SECTION I : THEORY VIVA CARDIOVASCULAR SYSTEM 53 63. What do you mean by baroreceptors? Where are they located? Baroreceptors are the pressure receptors stimulated in response to change of pressure around them. These are located in the wall of blood vessels (e.g. arterial baroreceptor–present in carotid sinus, aortic arch, root of right subclavian artery, junction of thyroid artery with common carotid artery, also pulmonary trunk) and also in the walls of the heart (e.g. atrio-caval receptors, atrial receptors). 64. What do you mean by buffer nerves? Why they are so called? Carotid sinus nerve originated from carotid sinus and aortic nerve arised from arch of aorta are collectively known as buffer nerves as they prevent any change in systemic BP and thus help the BP to keep normal. 65. What is Bainbridge reflex? Rapid injection of blood or saline in anesthetised animals produces a rise in heart rate if the initial heart rate is low. This is called as Bainbridge reflex. 66. Name different chemoreceptors responsible for BP regulation. What are their stimulants? These are carotid bodies and aortic bodies. They get stimulated by hypoxia, hypercapnia, asphyxia and also acidemia. 67. Sudden standing increases diastolic BP—explain how? On standing there is peripheral pooling of blood in lower parts of body →lowering of venous return to the heart →decrease cardiac output → thereby decrease systolic BP → leads to decrease baroreceptor discharge → thereby increases sympathetic activity →results increase of the total peripheral resistance due to vasoconstriction →ultimately leads to increase of diastolic pressure. 54 VIVA IN MEDICAL PHYSIOLOGY 68. If mean BP is decreased to 60 mm Hg then what compensatory mechanism will operate to bring it normal? Both baroreceptor mechanism (which operates in between 60-200 mm Hg mean blood pressure) and chemoreceptor mechanism which operates between 40100 mm Hg of mean BP. 69. If BP is decreased to 40 mm Hg then which compensatory mechanism will start into action? Both chemoreceptor mechanism and CNS ischemic response. 70. If mean BP is increased to 140 mm Hg then what compensatory mechanism will be operated? Only baroreceptor mechanism. 71. What do you mean by stress relaxation and reverse stress relaxation mechanism in relation to BP regulation? Rise in arterial BP due to intravenous transfusion of blood increases perfusion pressure in blood storage organs that causes relaxation of blood vessels, thereby decreases venous return and thereby decreases cardiac output. This leads to decrease BP to normal level. This mechanism is known as stress relaxation. The opposite phenomenon is known as reverse stress relaxation mechanism which is as follows: Prolonged bleeding causes decreases of BP →thereby decreases perfusion pressure → leads to vasoconstriction of blood storage organs → results increase of venous return and thus increases cardiac output →which in turn increases BP to normal level. 72. What is hypertension? What do you mean by systolic hypertension and white coat hypertension? Chronic elevation of blood pressure beyond 140/90 is generally labelled as hypertension. In advanced age, due to loss of elasticity of blood vessels, stretching of the wall SECTION I : THEORY VIVA CARDIOVASCULAR SYSTEM 55 of blood vessels decreases which results in increasement of pressure during systole with normal diastolic pressure. This condition is known as systolic hypertension which is characterised by high pulse pressure. Some hypertensive patients because of nervousness, have higher BP in the clinician’s chamber than during their normal day time activity. This condition is known as white coat hypertension. 73. What do you mean by malignant hypertension? In some patients the blood pressure especially the diastolic pressure is increased to very high level (>120 mm Hg) within a short period. This condition is known as malignant hypertension. 74. Which pressure is considered better to judge the hypertension–SP or DP? Justify your answer. Clinically diastolic pressure is more useful to characterise the state of hypertension because diastolic pressure is comparatively constant and does not fluctuate like SP in response to day to day activity. 75. What do you mean by labile hypertension? In early stages of essential hypertension, systolic BP fluctuates. This is why it is referred as labile hypertension. 76. What is hypotension? Chronic low BP specially the diastolic pressure below 60 mm Hg is called as hypotension. 77. What do you mean by postural hypotension? In some hypotensive patients, sudden standing causes further fall of systemic BP that may result dizziness, dimness of vision and even fainting. This is known as postural hypotension. 78. What is the difference between pulse pressure and pressure pulse? Pulse pressure is the difference of systolic and diastolic pressure whereas the pressure pulse or pulse is the wave transmitted to the arteries like radial arteries due to 56 VIVA IN MEDICAL PHYSIOLOGY stretching and relaxation of wall of aorta in response to ventricular ejection of blood and ventricular filling respectively during cardiac cycle. 79. What is the purpose of doing exercise tolerance test? It is for determining the efficiency of the heart as a pumping organ. 80. What is cardiac reserve? It is the difference between the basal cardiac output of an individual and the maximum cardiac output that can be achieved in that person. It is also expressed as cardiac reserve percent. 81. By observing HR can you predict the intensity of exercise or work done by a person? Yes, - If HR is <100 ; it will be light exercise. - If HR is 100-125 ; it will be moderate exercise. - If HR is 126-150 ; it will be heavy exercise. - If HR is >150 ; it will be severe exercise. 82. Where do you find physiological bradycardia? It is seen in athelets, during sleep and meditation. 83. What is apex-pulse deficit? Normally the pulse rate and heart rate are identical but in some cases like extra-systoles and atrial fibrillations, some of the heart beats are too weak to be felt at the radial artery resulting missing of that particular pulse. This causes higher heart rate than pulse rate. This condition is known as apex-pulse deficit or pulse deficit. 84. Name the waves of normal arterial pulse tracing. What are their physiological basis? In the normal arterial pulse recording, there are one steep upstroke called anacrotic limb and one rather slow down stroke called catacrotic limb. The end of anacrotic limb and beginning of catacrotic limb is designated as percussion wave (p). In the catacrotic limb there is also a negative wave called dicrotic notch (n) followed by a SECTION I : THEORY VIVA CARDIOVASCULAR SYSTEM 57 positive wave called dicrotic wave. Besides this, sometimes after the peak of the tracing there is another small wave called tidal wave (t). The waves are represented by Figure 1.3.2. Fig. 1.3.2: Normal arterial pulse tracing a. Percussion wave: It is due to expansion of the artery for ventricular ejection during ventricular systole. b. Catacrotic limb: It is due to normalisation of artery due to slow passing of blood towards periphery. c. Dicrotic notch: It is due to backflow of the blood from aorta towards heart due to pressure difference during ventricular diastole. d. Dicrotic wave: It is due to increase pressure again in the aorta due to prevention of back flow of blood towards heart by closure of aortic valve. 85. Can you indicate the systolic and diastolic phases of the ventricle on the arterial pulse tracing? Yes, the maximum ejection phase lasts from the start of the upstroke to peak of ‘p’ wave while the reduced ejection phase lasts from peak of ‘p’ wave to peak of dicrotic notch. The rest time period represents diastole. 86. What is dicrotic pulse? There are two palpable waves- one in systole and another in diastole in congestive cardiomyopathy patients where stroke volume is low. This type of pulse is known as dicrotic pulse. 87. What is plateau pulse? During some pathological conditions like aortic stenosis the pulse wave rises slowly, followed by delayed and 58 VIVA IN MEDICAL PHYSIOLOGY sustained peak and then the pulse faded slowly. Such type of pulse is known as plateau pulse as represented by Figure 1.3.3 Fig. 1.3.3: Abnormal arterial pulse tracing (plateau pulse) 88. What is anacrotic pulse? Slow rising and slow fall of pulse wave due to prolonged ventricular ejection as occurs in aortic stenosis is known as anacrotic pulse. 89. What do you mean by pulsus alterans and paradoxus? Pulsus alterans is alternative weak and strong beating of pulse whereas the phenomenon when pulse disappears or becomes feeble during inspiration and becomes maximum during expiration is known as pulsus paradoxus. 90. What is water hammer pulse? In some conditions like aortic regurgitation there is sharp and steep rise followed by sleep fall of pulse which is known as water hammer pulse. 91. How does jugular venous pulse record give the idea about right atrial pressure? Jugular vein is connected directly with right atrium and as there is no valve at the junction of superior vena cava and right atrium, any change of right atrial pressure is directly transmitted to the jugular vein. That is why jugular venous pressure record gives the idea about right atrial pressure. 92. Name the waves of jugular venous pulse and the causes of their onset. The waves and their causes are as follows: SECTION I : THEORY VIVA • • • • • CARDIOVASCULAR SYSTEM 59 ‘a’ wave – It is due to increase in pressure within atrium due to atrial systole. ‘c’ wave – It is due to increased pressure within atrium due to bulging of the tricuspid valve into the right atrium during isovolumic ventricular contractile phase. ‘v’ wave – It is due to the rise in atrial pressure due to atrial filling before the tricuspid valve opens during diastole. X descends-It is due to fall of intra-atrial pressure due to descend of the tricuspid valves. Y descends-It is due to the fall of intra-atrial pressure due to the opening of tricuspid valves to result ventricular filling. 93. Define ECG. It is the record of electrical activities of heart by electrocardiograph during different periods of cardiac cycle. 94. Enumerate the clinical significance of ECG. Any abnormalities of the heart like ischemic heart disease, myocardial infraction, extrasystole, heart block, ventricular fibrillation and flutter, sinus arrhythmias, etc. are detected by the ECG record of the person. 95. What does ‘P’ wave represent? What does it signify? ‘P’ wave represents the atrial depolarisation. Any abnormalities of the ‘P’ wave means abnormality in the atria like larger ‘P’ wave denotes the atrial hypertrophy. 96. What do QRST and QRS represent? What is the duration of ventricular complex? QRST represents ventricular complex, i.e. ventricular depolarisation and ventricular repolarisation. Normal duration is 0.48 sec. QRS complex represents ventricular depolarisation only. 97. What do Q and RS waves indicate? ‘Q’ wave indicates the ventricular septal activity whereas 60 VIVA IN MEDICAL PHYSIOLOGY ‘RS’ wave indicates the excitation of ventricle proper with duration of 0.08-0.1 sec. 98. What is the significance of T wave? It is due to repolarisation of ventricles and its normal duration is 0.27 sec. It indicates the functional activity of base of the heart. Clinically it signifies the myocardial damage in case of any abnormality in T wave. 99. What does PR interval represent? What is its significance? It represents atrial depolarisation and conduction through bundle of His. Normal duration is 0.13-0.16 sec. It is the interval from beginning of P wave to the beginning of Q or R wave. Prolonged PR interval signifies the conduction block. 100. What is TP interval and what is its significance? It is the period from the end of T wave to the beginning of P wave of next cardiac cycle. It represents the diastole or polarised state of whole heart. Normal duration is 0.2 sec at a HR of 75/min. 101. What is QT interval and what does it represent? It is the interval from the beginning of Q wave to the end of T wave (Normal duration 0.40-0.43 sec). It represents ventricular events. 102. What is ST interval? What does it represent? End of S wave to the end of T wave is known as ST interval. The normal duration of which is 0.32 sec. It represents ventricular repolarisation only. 103. What is ST segment? What is its significance? Following the QRS there is a long isoelectric period which extends from the end of S wave to the beginning of T wave called as ST segment. Any change of the position of ST segment from the isoelectric line indicates the functional abnormalities of the heart. Deviation of ST segment more than 2 mm up from the isoelectric line is called elevated ST segment which is the clinical feature SECTION I : THEORY VIVA CARDIOVASCULAR SYSTEM 61 of MI. Similarly deviation of the same more than 2 mm downward from the isoelectric line is called as depressed ST segment as seen in angina pectoris. 104. Define lead. The electrocardiographic connections, i.e. wires along with the electrodes to record ECG is known as lead. 105. Classify leads. Leads are classified as unipolar and bipolar leads which are again divided as follows: • Unipolar lead • Unipolar augmented limb lead – aVR – aVL – aVF • Chest lead (V1-V6) • Bipolar lead – Standard limb lead—I – Standard limb lead—II – Standard limb lead—III 106. Why unipolar lead is so called? In this type of leads, one electrode becomes inactive (indifferent electrode) whereas other one is active (exploring electrode). That is why it is known as unipolar lead. 107. What do you mean by rule of thumb? It is the general observation in the ECG record obtained from chest leads as follows: a. As we pass across the chest leads (V1- V6) ‘R’ wave increases gradually in size and ‘S’ wave becomes smaller gradually. In lead V3 both are equal. b. R wave in V6 and S wave in V1 represent left ventricular activity whereas R wave in V1 and S wave in V6 represent right ventricular activity. 108. What is augmented limb lead? Why is it so called? Augmented limb leads are unipolar type limb leads with slight modification in the recording technique where one 62 VIVA IN MEDICAL PHYSIOLOGY electrode (active) is connected to the positive terminal of ECG machine and other two are connected through electrical resistant to the negative terminal of the ECG machine. It is so called because the magnitude of different waves become larger by 50 per cent than the same obtained from standard limb leads without any change of its normal pattern. These are classified as aVR, aVL and aVF. 109. What do unipolar chest leads represent? V1 and V2 are associated with right atrial and ventricular activity respectively whereas V4, V5 and V6 represent left ventricular activity. V3 is regarded as transitional zone. 110. What do you mean by dextocardiogram? In case of damage of left branch of bundle of His, the impulse travels through right branch to the right ventricle resulting predominant activity of right ventricle. Such a record is called as dextocardiogram. 111. What is levocardiogram? When right branch of bundle of His is damaged there is predominance of left ventricular activity. This type of record is called as levocardiogram. 112. What do you mean by Einthoven’s triangle? The equilateral triangle obtained by connecting the right arm, left arm and right leg, by means of electrical wires with current source as the heart at its centre is known as Einthoven’s triangle. 113. What is Einthoven’s law? It states that if the electrical potentials of any two of the three bipolar leads are known at any given instant, the 3rd one can be determined mathematically from the 1st two by simply summing the 1st two by considering the positive and negative signs of the different leads. 114. What is J point? What is its significance? J point is the end point of S wave and beginning of ST segment where there is no electrical activity of the heart SECTION I : THEORY VIVA CARDIOVASCULAR SYSTEM 63 exists. Normally the J point locates on the isoelectric line. Upward or downward deviation of this point indicates the heart diseases like MI and cardiac ischemia. 115. What is vector? It is an arrow that points the direction of the electrical potential generated by the current flow with the arrowhead in the positive direction. 116. Mention the characteristics of vector. These are: a. Direction of current flow is represented by the arrowhead and b. Length of the arrow is drawn proportionate to the voltage of the potential. 117. What do you mean by vector cardiogram? Vector of current flow through the heart changes rapidly as the impulse spreads through the heart muscle. These changes are: a. The vector increases and decreases in length because of the increasing and decreasing voltage of the vector. b. It also changes direction accordingly with the changes in the average direction of the electrical potential of the heart. The record that shows these changes in the vectors at different times during the cardiac cycle is called as vector cardiogram. 118. What do you mean by electrical axis of the heart or cardiac vector? Since the standard limb leads I, II, III are records of the potential difference between two points, therefore, deflection in each lead at any point indicates the magnitude and direction in the axis of the electromotive force generated in the heart. This is called as electrical axis of the heart. 64 VIVA IN MEDICAL PHYSIOLOGY 119. What do you know about U wave in ECG? It is rarely seen as a small positive round wave after the T wave. It is due to slow repolarisation of papillary muscles. It is more commonly seen in children. 120. What do you mean by left and right axis deviation? From the ECG record how can you assess whether any person is having left or right axis deviation? If the normal direction of mean QRS vector falls in between –30° to +30°, it is called as left axis deviation which represents the horizontal position of heart. Similarly, if it falls in between +75° to +110°, it is known as right axis deviation which also represents vertical position of heart. Clinically axis deviations are made by finding the amplitude of R wave in the bipolar leads as follows: a. If R wave is the tallest in lead II, it is normal electrical axis of heart (+59°). b. If R wave is the tallest in lead I, it is left axis deviation. c. If R wave is the tallest in lead III it is called as right axis deviation. 121. What are the physiological left or right axis deviation? What is the clinical significance of electrical axis of heart? Physiological left axis deviation is seen: a. During expiration b. When a person lies down c. If the person is stocky and fatty. Physiological right axis deviation is seen: d. During inspiration e. When a person stands up f. Normally in tall and lanky people. Clinical significance: Hypertrophy of any ventricles and bundle branch block is indicated from the electrical axis of heart. In patients with hypertrophy of left ventricle and left bundle branch block, left axis deviation is seen whereas in hypertrophy of right ventricles and right bundle branch block patients, right axis deviation takes place. SECTION I : THEORY VIVA CARDIOVASCULAR SYSTEM 65 122. What is the difference between 1st degree and 2nd degree heart block? When all atrial impulses reach the ventricles therefore atrial rate: ventricular rate becomes 1:1 but PR interval becomes longer than 0.2 sec, it is called as 1st degree incomplete heart block. Whereas when all atrial impulses are not conducted to the ventricles producing atrial and ventricular contraction at a rate of either 2:1 or 3:1 ratio with gradual lengthening of PR interval till one ventricular beat is missed, this type of heart block is known as 2nd degree incomplete heart block. 123. What do you mean by Wenckebach phenomenon? In case of 2nd degree heart block, there is a gradual increase of PR interval untill one ventricular beat is missed.This is known as Wenckebach phenomenon. 124. What is 3rd degree heart block? What do you mean by idioventricular rhythm? Complete blockade of conduction of impulse from atria to ventricle is known as third degree or complete heart block. In the case of complete heart block, ventricle starts beating at its own rate, i.e. 45 beats/min which is independent to SAN. This rhythmic ventricular contraction is known as idioventricular rhythm. 125. What is the difference between flutter and fibrillation? Flutter Fibrillation 1. This is due to spreading of regular circus movement of impulse through the heart. This is due to spreading of irregular circus movement in many areas of the heart. 2. In this case there is a coordinated contraction of heart takes place. There is an incoordinated contraction of heart 3. Heart rates are within 200 to 300 beats/min. Heart rates are more than 300 beats/min. 66 VIVA IN MEDICAL PHYSIOLOGY 126. What are the clinical findings of ECG during MI? a. Elevation of ST segments in the leads overlying the area of infarct and b. Depression of ST segment in the reciprocal leads. 127. What do you mean by Stokes-Adams syndrome? In case of complete heart block, there is some delay before ventricles start beating at their own rate. During this period the systemic blood pressure falls to a very low level and blood supply to brain becomes inadequate. If ventricles do not beat for more than few seconds it causes dizziness and fainting called as Stokes-Adams syndrome. 128. What are the ECG changes during bundle branch block? What changes take place in heart sound production during its bundle branch block? The ECG changes are as follows: • Prolonged QRS complex (>0.12 sec) • Abnormal ST segment and T wave. • The second heart sound is splited. 129. What do you mean by extra-systole? The spontaneous heart beat produced by the irritable focus within heart under some abnormal condition is known as extra-systole. 130. What types of ECG changes take place in atrial flutter and atrial fibrillation? In case of atrial flutter following changes are seen: a. Shortening of all time intervals, e.g. PR, TP intervals b. Merger of T wave with P wave of next cardiac cycle c. 2nd degree type (2:1) of heart block. In case of atrial fibrillation following changes are seen: d. Absence of P wave. e. Appearance of fibrillation (f) waves f. Absence of T wave g. Irregular QRS complex. SECTION I : THEORY VIVA CARDIOVASCULAR SYSTEM 67 131. How does the ECG record changes with time after MI? • Within few hours after MI: Elevation of ST segment. • After some days of MI: Elevation of ST segment along with inversion of T wave. • After several weeks of MI: ST segments return to normal but inversion of T wave is still present along with appearance of Q wave. • After months and years of MI: T wave becomes normal and Q wave becomes deep. 132. What do you mean by mean circulatory filling pressure and mean systemic filling pressure? If the heart beat is stopped, the flow of blood every where in the circulation ceases after few seconds resulting equal pressure within the whole circulation which is known as mean circulatory filling pressure. Whereas the mean systemic filling pressure is the pressure measured everywhere in the systemic circulation after blood flow is stopped by the clamping of the large blood vessels at the heart. Normally the amount of both are almost equal. 133. Name different types of blood vessels in vascular system with examples of each. These are as follows: a. Distensible (Windkessel) vessels—aorta, pulmonary artery and their large branches. b. Resistance vessels—arterioles, meta-arterioles c. Exchange vessels—capillaries d. Capacitance vessels—venules and venous compartments e. Shunt vessels—AV anastomoses. 134. Blood flow to the different body organs can be so effectively regulated by only small chages in the caliber of the arteries. How is it possible? As resistance to blood flow is inversely proportional to the 4th power of the radius (r) of arterioles,the small 68 VIVA IN MEDICAL PHYSIOLOGY changes of radius can cause greater changes of resistance to blood flow and thereby flow to the different body organ. 135. What do you mean by critical closing pressure? Extravascular tissues exert a small but definite pressure on vessels and when the intra-luminal pressure falls below this extra-vascular pressure the vessel collapses. The pressure at which the flow ceases is called as critical closing pressure. 136. State the law of Laplace. What is its functional significance? It states that the distending pressure (P) in a distensible hollow object is equal at equilibrium to the tension in the wall (T) divided by two principal radii of curvature of object (R1 and R2), i.e. P = T (1/R1+1/R2). Significance: (i) smaller the radius of the blood vessels lesser the tension in the wall necessary to balance the distending pressure. This is why (i) thin and delicate capillaries are less prone to rupture, (ii) dilated heart has to do more work than normal heart. 137. What is axon reflex? In response to a firm stroke in the skin the afferent impulses are relayed to the endings near cutaneous arterioles down the branches of sensory nerve to result cutaneous arteriolar dilatation. This neural pathway which does not involve CNS is known as axon reflex. 138. What do you mean by cold blue skin and warm red skin? Cold blue skin is the skin in which the arterioles are constricted and the capillaries are dilated whereas in warm red skin both arterioles and capillaries are dilated. 139. What is tripple response? A firm and strong stroke on the skin by a blunt object evokes a series of responses which are (i) Red reaction SECTION I : THEORY VIVA CARDIOVASCULAR SYSTEM 69 (ii) Flare and (iii) Wheal. These responses to the injury are collectively known as tripple response. 140. What is the physiological basis of red reaction, flare and wheal? Red reaction: It is due to the dilatation of precapillary sphincter due to release of histamine and/or bradykinin like vasodilator substances. Flare: It is due to dilatation of arterioles, terminal arterioles and precapillary sphincter which causes increase in blood flow and thereby irregular erythematous area surrounding the red line. Wheal: It is due to increased capillary permeability and rise of capillary pressure which ultimately causes local diffuse swelling at and near the site. 141. What is white reaction? When a pointed object is drawn lightly over the skin the stroke line becomes pale due to draining out of blood from the capillaries and small vein due to contraction of precapillary sphincters. 142. What is the average total peripheral resistance of rest? It is 1 PRU. 143. On what factors the peripheral resistance does depend. It depends on the elasticity of vessel wall, diameter of arterioles (inversly), viscosity and velocity of blood directly. 144. Define Poiseuille’s law. It states that resistances to blood flow in a blood vessel proportionately varies with length of blood vessels and viscosity of blood and inversely with 4th power of radius of lumen of vessels. 70 VIVA IN MEDICAL PHYSIOLOGY 145. What is circulation time? Give the value of total circulation time. It is time taken by blood to flow from one site to any other specific site. Normal total circulation time is 12-16 sec. 146. Coronary blood flow fluctuates with each phases of cardiac cycle, explain. During systole the coronary blood flow is reduced because of compression of coronary vessels due to contraction of cardiac muscle whereas during diastole as cardiac muscle relaxes, there is distention of coronary vessels to its original diameter and thus blood flow through it to heart muscle is increased. 147. Why does the subendocardial portion of left ventricle is more prone for MI? It is for two reasons as follows: a. No blood flows to this portion during systole because of poor blood supply in this region and also compression of blood vessels during systole. b. Anaerobic respiration goes on in inner layer which increases further under stress. 148. What is the normal time taken for coronary circulation? It is about 8 sec. 149. What are the factors on which coronary blood flow depends? These are mainly lumen of coronary vessels, mean aortic pressure and also by cardiac output, HR, body temperature, CO2 concentration in blood and cardiac sympathetic stimulation. 150. What is normal pulmonary blood flow rate? It is about 3-5 lit/min. 151. What is the normal blood flow rate in liver? It is about 1500 ml/min. SECTION I : THEORY VIVA CARDIOVASCULAR SYSTEM 71 152. What is the normal coronary blood flow? It is about 225 ml/min. 153. Give the normal value of cerebral blood flow. It is approx. 750 ml/min. 154. Define shock. Classify it. Shock is a syndrome characterised by low cardiac output which is inadequate to maintain normal tissue perfusion. It is of 4 types—hypovolemic, vasogenic, cardiogenic and obstructive shock. 155. What do you mean by cold shock? When the amount of fluid in the vascular system is inadequate to fill it, resulting in decrease in circulatory blood volume it is known as hypovolemic or cold shock. 156. What is warm shock? When the diameter of capacitance vessels is increased by vasodilatation, there is a decrease of cardiac output inspite of normal blood volume. This type of shock is vasogenic shock and in this type of shock as skin becomes warm it is also called as warm shock. 157. What is congested shock? The cardiogenic shock causes congestion of lungs, viscera and that is why it is called as congested shock. 158. What is Bezold-Jarish reflex? The Ventricular receptors are sensitive to chemicals or partial occlusion of aorta or coronary artery which are responsible for profound bradycardia, hypotension and apnoea. This response is known as ‘Coronary chemo reflex’ or Bezold Jarish reflex which is clinically associated with Myocardial infarction or vaso-vagal syncope. 159. What is sinus arrhythmia? During inspiration HR is increased and during expiration HR is reduced. This phenomenon is called as sinus arrhythmia. 72 VIVA IN MEDICAL PHYSIOLOGY 160. What is bradycardia? Where can you see the physiological bradycardia? Decrease of heart rate below 60 beat/min is known as bradycardia which is physiologically seen in following conditions. • Athelets • Males • Emotional stimuli like shock, grief, depression, etc. • During expiration. 161. What do you mean by laminar and turbulent flow? How does turbulence produce? a) Laminar or stream line flow: It is fixed layer wise i.e. each layer of blood remains at the same distance from the wall blood vessels flowing through a long vessel and the velocity of blood is maximum in the core of the blood vessels and minimum in it’s periphery or surface. This type of steady rate of blood flow is known as laminar blood flow. b) Turbulent blood flow: When the blood flows crosswise in the vessels by forming whorls in the blood is called as eddy current. This type of blood flow is known as turbulent blood flow. It is produced by obstruction of vessels or when it takes sharp U turn. 162. What are the signs and symptoms of Shock? Different signs and symptoms manifested during shock are as follows: • Reduction in arterial blood pressure. • Reflex tachycardia and reduced stroke volume. • Decrease in pulse pressure and appearance of thready pulse. • Reduction in velocity of blood flow producing stagnant hypoxia and cyanosis. • Pale and cold skin due to reflex vasoconstriction. • Decreased urinary output due to reduced renal blood flow and GFR. SECTION I : THEORY VIVA • • • • • CARDIOVASCULAR SYSTEM 73 Fainting due to reduced blood flow to the brain tissue. Feeling of intense thirst if the patient is conscious. Rapid and shallow breathing. Metabolic acidosis due to excessive production of lactic acid by myocardium. Death due to cerebral or cardiac failure. 163. What are the symptoms of left ventricular failure? These are: a. Difficulty in breathing on exertion. b. Dyspnoeic attack at night. c. Dyspnoea in supine position. 164. What are signs and symptoms of right ventricular failure? These are: a. Engorgement of right atrium b. Increased venous pressure c. Swelling of liver d. Peritoneal and pleural effusion. e. Cyanosis and dyspnoea. f. Edema. 165. What are the common causes of left ventricular failure? These are: essential hypertension, coronary insufficiency, myocardial fibrosis and mitral valve incompetence. 166. What are the salient features of left ventricular failure? These are: a. Decrease in cardiac output with vasoconstriction of peripheral vessels b. Pulmonary edema, dyspnoea and anoxia (cardiac asthma) 167. How do you differentiate left and right cardiac failure broadly on the basis of edema? In left heart failure, pulmonary edema is seen whereas in right heart failure, edema is systemic in nature. 74 VIVA IN MEDICAL PHYSIOLOGY 168. Enumerate some of the effects of severe hemorrhage. These are decreased blood volume, state of shock, increased heart rate, decreased systolic BP, vasoconstriction, hemo-dilution, rapid and shallow breathing, blurred vision, fainting, etc. GI SYSTEM AND METABOLISM 75 SECTION I : THEORY VIVA 1.4 Gl System and Metabolism 1. Name the different layers in cross-section of GIT. These are—serous layer, longitudinal and circular smooth muscular layer, submucous layer and mucous layer. 2. Enumerate the intrinsic innervation of GIT. Intrinsic innervation is divided into two types as follows: a. Myenteric or Auerbach’s plexus—present between longitudinal and circular muscle layer. It is mainly motor in function. b. Submucous or Meissner’s plexus—lies between submucous and inner circular muscle layer. It is mainly sensory in function. 3. Define villi. Mucosal surface of duodenum and small intestine shows finger like projections to provide greater surface area for absorption. These finger like projections are called as villi. 4. What is glycocalyx? What is its function? On the luminal surface, the brush border of GI tract is lined by an amorphous layer called glycocalyx. It has a protective function. 5. What is crypts of Lieberkühn? What are the component cells of it? Between the villi of intestines there are some simple tubular glands lined by low columnar epithelium. These are known as crypts of Lieberkühn. It contains: 76 VIVA IN MEDICAL PHYSIOLOGY a. Goblet cells—secrete mucous. b. Argentaffin cells—Secrete secretin and 5 HT. c. Paneth cells—Along with epithelial cells these secrete enzymes responsible for digestion. 6. What are Brunner’s glands? What is its function? In duodenum, there are some special submucosal glands which are tortuous, long and resemble gastric pyloric glands. These submucosal glands are known as Brunner’s glands. In response to fatty food and secretin, it produces a large volume of thick alkaline mucosa responsible for protection of duodenal mucosa from gastric acid. 7. What is Peyer’s patch? The aggregated lymphatic follicles seen in ileum are known as Peyer’s patch. 8. What is taenia coli? The longitudinal smooth muscle layer is not equally distributed throughout the gut wall but is collected into 3 distinct bands in large intestine. These bands are called taenia coli. 9. Name the salivary glands. What are the constituent cells of each gland? There are 3 pairs of salivary glands named: a) Parotid gland—constitutes serous cells only. b) Submandibular gland—contains both serous and mucous cells though serous cells are more in number. c) Sublingual gland—constitutes mainly mucous and partly serous cells. 10. What are the actions of parasympathetic and sympathetic nerve stimulation on salivary gland? Parasympathetics are secretomotor in function and sympathetic fibers are vasoconstrictor. 11. What is ptyalin? State its functions. Ptyalin is a digestive enzyme present in saliva secreted by serous cells of salivary gland. When activated it converts unboiled starch to maltose. SECTION I : THEORY VIVA GI SYSTEM AND METABOLISM 77 12. What is mucin? What are its functions? It is secretory product of mucous cells of salivary gland. It has following functions: a. It lubricates the food b. It protects oral mucosa. c. It aids speech by facilitating the movements of lips and tongue. 13. Is salivation a secretory or an excretory process? It is a secretory process. 14. What do you mean by primary and secondary salivary secretions? The acinar cells of salivary glands secrete K+and HCO3¯ and also Cl¯ along with sufficient water into the acinal lumen making the secretion isotonic. This secretion is known as primary secretion. When these acinar cell secretions pass through salivary duct the salivary duct cells actively absorb K+ and an accompanying anion making the previous secretion hypotonic. These final secretory products are known as secondary salivary secretion. 15. What is xerostomia? What is due to? The suppression of salivary secretion is known as xerostomia or aptyalism. It is due to: a. Anxiety, fear, fever and dehydration. b. Obstruction of salivary duct due to calculus. 16. What is Sialorrhoea? The state of hypersecretion of saliva is known as sialorrhoea seen in pregnancy, parkinsonism, schizophrenia, etc. 17. What are the different muscles of mastication? These are masseter, temporalis, internal and external pterygoid and buccinator. 18. What are the role of teeth in mastication? Different teeth helps in mastication for example: • Incisors provide strong cutting action. 78 VIVA IN MEDICAL PHYSIOLOGY • • Canines helps in tearing action. Premolars and molars have grinding action. 19. How saliva prevents the formation of dental carries? It decreases the risk of buccal infection and dental caries and thus maintain oral hygiene by: • Continuous secretion of saliva that washes away food debris and pathogenic bacteria. • The enzymes lysozyme and thiocyanate kill some bacteria like Staphylococcus, Streptococcus and Brucella. • The protein antibodies which destroy bacteria including the bacteria causing dental carries. 20. What are different stages of deglutition? These are oral stage, pharyngeal stage and oesophageal stage. 21. What is deglutition apnoea? During pharyngeal stage of deglutition process once the deglutition reflex is initiated there is a elevation of larynx along with hyoid bone and also approximation of vocal cords. This event ultimately causes stoppage of breathing known as deglutition apnoea. 22. Where is the deglutition centre located? It is in medulla oblongata. 23. What is dysphagia? It is the difficulty in swallowing. 24. What do you mean by aerophagia? What is its cause? Aerophagia is a state of increase intake of air through mouth. It occurs in nervous individuals whose upper esophageal sphincter tone is low. So air is unavoidably swallowed in the process of eating and drinking. 25. What is Achalasia cardia? What is its relation with dysphagia? It is the state of failure of lower esophageal sphincter to SECTION I : THEORY VIVA GI SYSTEM AND METABOLISM 79 relax (due to excessive tone of LES) completely during swallowing → Leads distension of esophagus which is clinically known as Achalasia or megaesophagus. As it causes in difficulty in exit of food to stomach during swallowing it results dysphagia. 26. What do you mean by Gastroesophagial reflux? Why it is associated with heart burn? Any abnormality in closing the LES due to incompetence of LES causes efflux of acid pepsin mixed chyme from stomach to the oesophagus, which is known as gastro oesophageal reflux. In this situation the acid pepsin mixed chyme enters the esophagus the wall of which is not resistant enough to that of stomach wall → leads ulceration of oesophageal mucosa →results epigastic burning sensation (clinically known as ‘Heart burn). 27. Name different gastric glands and their secretions. There are three types of gastric glands as follows: • Main gastric gland: It is found in mucosa of body and fundus of stomach. It contains 3 cells: a. Parietal (oxyntic) cell—secretes HCl and intrinsic factor. b. Chief or peptic cell—secretes pepsinogen. c. Surface epithelial cell—secretes visible mucous. • Cardiac tubular gland: It secretes soluble mucous • Pyloric or antral gland contains: i. Surface epithelial cells—secrete soluble mucous. ii. G cells—secrete gastrin. 28. What do you mean by APUD cells? Some specialised cells present in brain and also in GIT are capable of amine precursor uptake and decarboxylation, which are known as APUD cells. G cells, S cells present in GIT are the examples of APUD cells. 29. Mention the factors increasing gastrin release. They are as follows: a) Luminal factors: These are the products of protein digestion and distension of pyrolic antrum. 80 VIVA IN MEDICAL PHYSIOLOGY b) Neural factors: Vagal stimulation c) Blood-borne factors like calcium, epinephrine, etc. 30. What do you mean by post-prandial alkaline tide? When gastric acid secretion is increased after meal, sufficient amount of H+ is secreted to raise HCO3¯ concentration in the gastric venous blood which contributes a greater amount of HCO3¯to the systemic circulation and pH of systemic blood increases. This condition is known as post-prandial alkaline tide. 31. Name the phases of gastric secretion. These are cephalic phase, gastric phase and intestinal phase. 32. What do you mean by appetite juice? In response to psychic stimuli by taste, sight, smell of food there is a reflex stimulation of vagus nerve which in turn increases gastric secretion known as appetite juice. 33. What do you mean by Pavlov’s pouch (Fig. 1.4.1)? What is its significance? In an experiment, Pavlov surgically separated a small portion of stomach with intact nerve and blood supply from the main body of stomach to prevent the entry of food into that small separated sac like structure. This is known as Pavlov’s pouch as represented by Figure 1.4.2A. In this type of experimentation on dog, stimulation of vagus nerve causes a flow of gastric juice rich in HCl and pepsin from the both part (main body and Pavlov’s pouch) of stomach but it can be collected in a pure form from (without mixing with food) Pavlov’s pouch only. This proves that vagus has secretomotor function on stomach. 34. What do you mean by Sham feeding? In another experiment, the esophagus is divided in the neck region of a dog and two ends are brought separately to the surface and satured in position. In this case, animal can eat for hours without satisfying its appetite as the SECTION I : THEORY VIVA GI SYSTEM AND METABOLISM 81 Fig. 1.4.1: Pavlov’s pouch swallowed food never reach to the stomach but falls out through the neck opening. This type of feeding is known as Sham feeding as represented by Figure 1.4.2. Figs 1.4.2A and B: Sham feeding. (A) represents the opening of the divided oesophagus and (B) is the body of stomach with fistula 35. What is receptive relaxation? When food enters into the stomach, it relaxes by a reflex process to accommodate food further. This reflex relaxation of stomach is called as receptive relaxation. 36. What do you mean by gastric (antral) pumps? The peristaltic wave provides a pumping action in the antral or pyloric region of the stomach which results 82 VIVA IN MEDICAL PHYSIOLOGY gastric emptying. This pumping action is called as antral or pyloric or gastric pumps. 37. What is enterogastric reflex? The products of protein digestion and acid in duodenum reflexly decrease gastric emptying. This neurally mediated reflex is known as enterogastric reflex. 38. How does the gastric emptying associate with type of food ingested? It depends on the basis of type of food as follows: • Carbohydrate rich food—results rapid gastric emptying. • Protein rich food—results slow gastric emptying. • Fat rich food—results slowest gastric emptying. 39. What do you mean by hunger contraction? What is its significance? In empty condition ordinarily there is no peristaltic wave but at intervals of one or two hours a powerful peristaltic wave develops in the antral region which ultimately reaches the end of the ileum. As these contractions are associated with pangs of hunger it is known as hunger contraction. This results the driving out of remnant food from stomach to small intestine. 40. Name different gastric function tests. These are: • Histamine test • Fractional test meal • Augmented histamine test • Barium meal X-ray • Endoscopy and biopsy. 41. What is achlorhydria? Why it is often associated with pernicious anaemia? The complete failure of gastric acid secretion due to atrophy or degeneration of gastric mucosa is known as achlorhydria. SECTION I : THEORY VIVA GI SYSTEM AND METABOLISM 83 HCl and intrinsic factors are secreted by same cell of gastric mucosa and intrinsic factor is responsible for vit B12 absorption from food which in turn increases RBC formation. Due to atrophy or degeneration of gastric mucosa, intrinsic factor is also not secreted. So the achlorhydria is thus associated with pernicious anemia. 42. What is dumping syndrome? A condition characterised by development of weakness, dizziness and sweating after meal is known as dumping syndrome. 43. Define peptic ulcer. What are its causes? Peptic ulcer is referred as the breakdown of the mucosal epithelium of the stomach and of duodenum. Causes are: • H. pylori infection • Use of NSAID • Zollinger-Ellison syndrome • Increase in gastric secretion • Mental and physical stress. 44. What is false and true achlorhydria? Sometimes the stomach secretes acid but it is not detected as it gets neutralised by the test meal. This is called as false achlorhydria. Whereas true achlorhydria is the condition when stomach does not secrete any acid at all. 45. Define vomiting. What is the vomiting center. Vomiting is an act of expulsion of gastric contents by regurgitation through the esophagus and oral cavity. The vomiting centre is the chemosensitive trigger zone (CTZ) located in or near the area postremas on medullary surface. 46. Which portion of pancreas subserves the exocrine function? It is compound alveolar tissues containing secretory acini and duct cells. 84 VIVA IN MEDICAL PHYSIOLOGY 47. Which hormones are responsible for pancreatic secretion? What are their roles? Generally two hormones—secretin and cholecystokininpancreozymin (CCK-PZ). Secretin increases the alkaline watery pancreatic juice secretion whereas CCK-PZ increases pancreatic secretion rich in enzyme. 48. Mention the substances synthesised by liver. These are: i. Plasma proteins ii. Clotting factors like fibrinogen, prothrombin, factor V, VII, IX, and X iii. Enzymes like SGOT, SGPT and alkaline phosphatase iv. Urea v. Cholesterol. 49. What is bile? Differentiate between liver and gallbladder bile. Bile is the secretory product of hepatic cells that helps in digestion and absorption of fatty foods specially. Parameter Liver bile Gallbladder bile Colour Consistency Water Bile salts Bile pigments Light golden yellow Like water 97% Less (120-180 mg%) Less Almost black Thicker 89% More (5 to 6 times) More pH 7.3-7.7 7.0-7.2 50. What do you mean by primary and secondary bile acids? The cholic acid and chenodeoxycholic acid produced in liver from cholesterol are known as primary bile acids. When these are exposed to colon they are converted to deoxycholic acid and lithocholic acid by colonic bacteria which are known as secondary bile acids. SECTION I : THEORY VIVA GI SYSTEM AND METABOLISM 85 51. Define bile salts. Give examples. Sodium and potassium salts of bile acids are known as bile salts. These are Na+/K+- glycocholate or taurocholate. 52. What do you mean by enterohepatic circulation? Of the total bile salts entering into the duodenum 90-95 percent are reabsorbed actively from the terminal ileum in the portal vein and return to the liver to be excreted again. This cyclical passage of bile salts from liver to intestine and then back to liver is known as enterohepatic circulation. 53. Name the different bile pigments and their origin. Bilirubin and biliverdin. They are formed from globin portion of hemoglobin after the destruction of old RBCs by RE cells. 1gm Hb produces 40 mg of bilirubin. 54. What do you mean by cholerectic and cholago-gues? • Cholerectic are substances which increase biliary secretion from the liver, e.g. bile salts and bile acids. • Cholagogues are the substances that cause contraction of gallbladder, e.g. fatty acids, Ca++, etc. 55. What is cholelithiasis? What are the types of gallstone? Presence of stones in the gallbladder or bile ducts is called as cholelithiasis. Gallstones are of two types: a. Cholesterol stones—These are radioluscent. b. Pigment stone (Calcium bilirubinate)—These are radioopaque. 56. Give normal value of A:G ratio. In which condition it is reversed? Normal value is 1.7:1. It is reversed in hepatic insufficiency. 57. Mention some liver function tests. i. Galactose tolerance test ii. Estimation of SGOT, SGPT and alkaline phosphatase 86 VIVA IN MEDICAL PHYSIOLOGY iii. Estimation of total bilirubin iv. Hippuric acid excretion test v. Ultrasound scan and CT scan. 58. What is Jaundice? It is the clinical condition characterised by yellowish pigmentation of the skin, mucous membrane and deeper tissues due to presence of more than 2 mg% serum bilirubin. 59. Mention the differences between hemolytic and obstructive jaundice. Parameters Hemolytic jaundice Obstructive jaundice Cause Excessive breakdown of RBC High (unconjugated) Normal Obstruction of bile ducts. Normal Present Normal Absent Absent Present Increases Excessive yellow Normal Indirect positive Absent Clay coloured Increased Direct positive Normal Mildly impaired Serum bilirubin Serum alkaline phosphatase A: G ratio Hemorrhagic tendency Urinary bilirubin Urinary urobilinogen Faecal colour Faecal fat Van Den Bergh test Liver function test High (conjugated) High 60. What do you mean by succus entericus? The secretion of the crypts of Lieberkühn in the small intestine is known as intestinal juices or succus entericus. 61. What do you mean by intestinal adaptation? What is due to? Removal of short segment of small intestine (jejunum or ileum) leads to compensatory hypertrophy and hyperplasia of the remaining mucosa with gradual return of normal absorption. This is known as intestinal adaptation. It is due to: SECTION I : THEORY VIVA • • GI SYSTEM AND METABOLISM 87 Direct effect of nutrients in the intestinal lumen on the mucosa. GI hormonal influence on the intestinal mucosa. 62. Enumerate in brief the movements of small intestine. In small intestine, two types of contractions are seen as follows: a) Rhythmic segmental contraction—by this movement food is segmented and mixed together with digestive juices. b) Peristalsis—it propels the intestinal contents towards the ileo-caecal valve. 63. What is ‘law of the gut’? The peristaltic movement once initiated in response to food is bidirectional but it normally dies out rapidly in oral direction while continuing towards aboral direction for considerable distance. This property is known as polarity of the intestine or ’law of the gut’ 64. What is peristaltic rush? Why does pain sensation associates with peristaltic rush? Localised mechanical obstruction of small intestine initiates very tense peristaltic waves called peristaltic rush which causes severe cramping pain. This pain is due to: • Compression of blood vessels in its wall producing local ischemia. • Stimulate visceral afferent nerve fibers to cause sweating, hypotension and severe vomiting. 65. What is gastro-ileal reflex? When food leaves the stomach the caecum relaxes and passage of chyme through the ileo-caecal valve increases.This is called as gastroileal reflex. 66. What is mass peristalsis? These are the simultaneous contractions of the smooth muscle occurring at the same time over a large portion of the colon. 88 VIVA IN MEDICAL PHYSIOLOGY 67. What is gastrocolic reflex? Distension of the stomach by the food initiates contractions of the rectum resulting a frequent desire to defecate. This reflex is called as gastrocolic reflex. 68. What is diarrhoea? Why does it may result even death? Increase frequency of passage of stools is called as diarrhoea. In severe cases, it may even cause death because of shock, i.e. cardiovascular collapse resulted due to loss of large amount of electrolytes like Na+, K+ and water. 69. Name two colonic bacteria. Give its two functions. These are Escherichia coli and Enterobactor. Its useful functions are as follows: i. It synthesises vit K, B complex and folic acid. ii. It helps in metabolism of bile pigments. 70. What are the digestive enzymes present in gastric juice? These are pepsinogen, lipase and renin. 71. Enumerate the function of pepsin, HCl and renin: • Pepsin—It converts protein into peptones and proteases by the help of HCl • HCl• It kills the bacteria present in food. • It hydrolyses food and helps in digestion. • It activates pepsinogen to form pepsin. • It also helps in iron and Ca2+ absorption. • Renin—It curdles the milk and converts caseinogen into calcium paracaseinate. 72. What are the functions of villikinins and cholecystokinin? Villikinin secreted by duodenal mucosa helps to stimulate villi movements whereas CCK liberated by duodenal mucosa stimulates contraction of gallbladder. SECTION I : THEORY VIVA GI SYSTEM AND METABOLISM 89 73. What are the digestive enzymes of pancreatic juice? Mention their function. These are trypsinogen, chymotrypsinogen, amylase and lipase. • Trypsinogen—Once activated by enterokinase it activates chymotrypsinogen to chymotrypsin. • Chymotrypsinogen—Once activated it converts peptones into dipeptide stage. • Amylase—It converts starch into maltose. • Lipase—It converts fat into fatty acids and glycerols. 74. Name the various enzymes present in succus entericus. Mention each of their function. These are erepsin, nuclease, nucleotidase, arginase, sucrase, maltase and lactase. • Erepsin—It converts simple peptides into amino acids. • Nuclease (Nucleosidase and nucleotidase)—These are responsible for digestion of nucleoproteins. • Arginase—It converts arginine to urea and ornithine. • Sucrase—Splits sucrose into fructose and glucose. • Maltase—Converts maltose to 2 molecules of glucose. • Lactase—Lactase converts lactose to glucose and galactose. 75. What is steatorrhoea? Inflammation of pancreatic acinar cell due to any cause destroys the acinar and ductular cell resulting deficient secretion of pancreatic juice. This condition results low digestion of fatty food due to absence of activation of lipase →increased fat or oil in the stool which is known as steatorrhoea. 76. What are the main sources of energy in man? They are of two types: • High energy phosphate—like ATP, ADP, creatinine phosphate, acetylphosphate. • Low energy phosphate—like glucose-1–phosphate, glucose-6-phosphate, etc. 90 VIVA IN MEDICAL PHYSIOLOGY 77. Define calorie and joule. A calorie is the amount of heat required to raise the temperature of 1 kg of water from 15°C to 16°C. This large calorie is equivalent to 1000 small calories. Joule is defined as the energy expressed when one kilogram of substance moved through one meter by 1 newton, i.e. a force which accelerate 1kg by 1m/sec2. 78. • • • What is the potential energy of various foods? 1 gm of carbohydrate evolves 4.1 cal heat. 1 gm of protein evolves 4.1 cal of heat. 1 gm of fat evolves 9.3 cal of heat. 79. Define BMR. How does it express? BMR is the amount of heat produced in the body in a given time in complete physical and mental resting state at 20°C room temperature. It is expressed as calories/ sqm body surface area/hour. Normal value is 40 cal/sqm/ hr. 80. Name some conditions when BMR varies. • Increase of BMR: • Physiological conditions—muscular activity, cold weather, food intake, tension, etc. • Pathological conditions—hyperthyroidism, fever, anaemia, etc. • Decrease of BMR: • Physiological condition—Starvation, undernutrition • Pathological condition—hypothyroidism, adrenal cortex deficiency, hypothermia, etc. 81. What is the main source of energy of following tissue/organ? • Skeletal muscle glucose. • Cardiac muscle lactic acid. • Brain blood glucose. RESPIRATORY SYSTEM 91 SECTION I : THEORY VIVA 1.5 Respiratory System 1. What do you mean by external and internal respiration? The absorption of O2 and removal of CO2 from the body through lungs is known as external respiration. Whereas the utilisation of O2 and production of CO2 by the cells at the cellular level is known as internal respiration. 2. What do you mean by conducting zone and respiratory zone? The portion of the respiratory tract (i.e. upto 16th generation as per Weibel's lung model) where no exchange of gases takes place is known as conduction zone whereas the portion of respiratory tract (i.e. beyond 16th generation) where gaseous exchange takes place is known as respiratory zone which includes respiratory bronchioles, alveolar ducts and the alveoli. 3. What is partial pressure? What are the partial pressure of following gases? The pressure exerted by any one gas in a mixture of gases is called its partial pressure. The partial pressure of different gases are as follows: O2—20.98 per cent; CO2—0.03 per cent, N2—78.06 per cent. 4. If the percentage of O2 in inspired air is 20.98 per cent then what will be the PO2 at sea level? PO2 = per cent of gas/100 × total atmospheric pressure = 20.98/100 × 760 mm Hg (at sea level) = 159.5 mm Hg. 92 VIVA IN MEDICAL PHYSIOLOGY 5. What is Dalton's law? It states that total pressure exerted by a mixture of gases is equal to the sum of the partial pressures of all the gases present within it. 6. What is Henry's law? It states that if temperature is kept constant, amount of gas dissolved in any solution is directly proportional to the partial pressure of that gas. 7. What do you mean by 'Pump Handle' movement and 'Bucket Handle' movement in relation to respiration? During inspiration the upper ribs, i.e. 2nd to 6th ribs move upward to assume more horizontal position to increase anteroposterior diameter of the chest. This type of movement of upper ribs is called as 'Pump Handle movement'. On the other hand during inspiration the lower ribs (i.e. 7th to 10th) swing outward and upward to increase the transverse diameter of the chest like a bucket handle and therefore is known as 'Bucket Handle" movement. 8. Give the normal value of intrapulmonary or intraalveolar pressure. It is about 760 mm Hg. 9. Why intra-alveolar pressure is equal to that of atmospheric pressure? How is it affected during inspiration and expiration? It is equal to the atmospheric pressure as during quiet breathing, at the end of expiration and at the end of inspiration, no air is going in and out of the lungs. During inspiration it decreases 3 mm Hg below its normal value, i.e. 757 mm Hg and during expiration it increases 3 mm Hg above its normal value, i.e. 763 mm Hg. SECTION I : THEORY VIVA RESPIRATORY SYSTEM 93 10. What is Valsalva manoeuvre and Muller's manoeuvre? Forced expiration against a closed glottis may produce positive intrapulmonary pressure of > 100 mm Hg above the atmospheric value. This voluntary act is known as Valsalva manoeuvre. Forced inspiration against closed glottis can reduce the intrapulmonary pressure to < 80 mm Hg below the atmospheric value. This voluntary act to reduce the intrapulmonary pressure is known as Muller's manoeuvre. 11. What is intrapleural pressure? How does it varry during inspiration and expiration? Why normally it is negative? It is the pressure within the pleural cavity around the lungs. Normal value is -2.5 mm Hg. During inspiration it decreases further to -7.5 mm Hg and during expiration it increases to 2.5 mm Hg. It is normally negative because of following factors: i. The lung tries to collapse because of its elasticity (elastic recoil) and surface tension in the alveoli. ii. The chest wall always tries to expand. Therefore the two pleural layers become subjected to a force that tries to separate them resulting a suction pressure or negative pressure. 12. Name the muscles of inspiration and expiration. a) Muscles during normal breathing: i. Diaphragm ii. External intercostal muscles. b) Muscles during forceful breathing: • Inspiratory muscles : Along with the muscles described above there are other muscles termed as accessory inspiratory muscles responsible for forceful inspiration. These are: • Sternocleidomastoid - lifts the sternum upward. • Serratus anterior - lifts many ribs. • Scalene - lifts 1st two ribs. 94 VIVA IN MEDICAL PHYSIOLOGY • Expiratory muscles: • Internal intercostal muscles • Abdominal muscles: These include abdominal recti, transverse abdominis, internal oblique. 13. Why the 'Wheeze' sound is heard during expiration but not in inspiration of an asthma patient? During inspiration the intrapleural and mediastinal negativity rises and as a result the bronchial diameter increases. Reverse occurs during expiration. Therefore resistance to airflow is normally low in inspiration and high in expiration. This is why in bronchial asthma inspiration may not be difficult but expiration becomes difficult. This explains why the "Whezze" in bronchial asthma is heard during expiration but not in inspiration. 14. Define and give the normal value of TV, IRV, ERV and EV. • Tidal volume (TV): It is the amount of air breathed in or out of lungs during quiet respiration. Normal value is 500-800 ml. • Inspiratory reserve volume (IRV): It is the maximum amount of air that can be inspired from the end inspiratory position by forceful and maximal activity. Its normal value is 2000-3200 ml. • Expiratory reserve volume (ERV): It is the maximum amount of air that can be expired by maximum forcible effort from the end of normal expiratory position. Normally its value is 750-1000 ml. • Residual volume (RV): It is the volume of air which remains in lungs even after forceful expiration. Normal value =1200 ml. 15. Define and give the normal value of IC, FRC and TLC. • Inspiratory capacity (IC): It is the maximum amount of air that can be inspired from the end expiratory position. Normal value: 2500-3700 ml. SECTION I : THEORY VIVA • • RESPIRATORY SYSTEM 95 Functional residual capacity (FRC): It is the amount of air contained in the lungs at end expiratory position. Normal value is 2500 ml. Total lung capacity: It is the volume of air retained by the lungs after a maximal inspiration. Normal value is 6 lits. 16. Define vital capacity. What is its importance? It is the maximum volume of air which can be expired by forceful effort after a maximal inspiration. It provides useful information about the strength of respiratory muscles and also provides useful information about other aspects of pulmonary function through FEV1. 17. In which posture VC is highest and why? In standing posture it is the highest as in standing position diaphragm descends down increases intrathoracic volume increases intra-alveolar volume increases inspiration. 18. Why does VC decrease during pregnancy? During pregnancy diaphragm is pushed up by the growing foetus resulting decrease of intra-thoracic volume and thereby decrease of capacity to inspire air and there by VC is decreased. 19. Name two methods for measuring FRC. It is nitrogen wash out method and helium dilution method. 20. What is the significance of FRC? These are: • It maintains the RV constant. • It acts as a buffer and allows continuous exchange of gases to occur even during expiration, thereby prevents sudden changes in partial pressure of gases in the blood. 21. What are the factors affecting FRC? These are: Old age, emphysema, bronchial asthma, atelectasis. 96 VIVA IN MEDICAL PHYSIOLOGY 22. Define timed vital capacity. The maximum volume of air which can be breathed out as forcibly and rapidly as possible after deepest inspiration is known as vital capacity. If this VC is recorded in relation to time, it is known as timed vital capacity. 23. What is the significance of FEV1 or Ist second of timed vital capacity? It helps to distinguish between restrictive and obstructive lung diseases. In restrictive lung diseases like kyphoscoliosis and ankylosing spondylitis vital capacity decreases but FEV 1 remains normal whereas in obstructive diseases like emphysema and bronchial asthma vital capacity remains normal but FEV 1 decreases. 24. What is pulmonary ventilation? It is the amount of air breathed in or out in one minute. It is computed as TV × RR/min where RR represents respiratory rate. 25. What is maximum breathing capacity? It is the largest amount of air that can be breathed in or out in one minute by maximum voluntary efforts. It is computed as VC × RR/ min = 100 L/min. 26. Define pulmonary reserve or breathing reserve. It is the maximum amount of air above the pulmonary ventilation which can be breathed in and out in each minute. It can be computed as MVV-PV (PV represents pulmonary ventilation). 27. What is the dyspnoeic index? What value marks the presence of dyspnoea? When the pulmonary reserve is expressed as percentage of MVV it is known as pulmonary reserve or dyspnoeic index (DI). It is computed as (MVV-PV) × 100/ MVV; normal value is > 60-70 per cent. If this value becomes less than 60 per cent then dyspnoea may be present. SECTION I : THEORY VIVA RESPIRATORY SYSTEM 97 28. What do you mean by lung surfactant? What do you mean by hyalin membrane disease? Lung surfactant is a mixture of protein-lipid complexes made up of mainly dipalmitoyl phosphatyl choline, secreted by type II alveolar epithelial cells, which reduces the surface tension of the fluid linning of the alveoli. Due to deficiency of surfactant in this disease the surface tension in the lungs of these newborn babies is very high making the expansion of the lungs very difficult. This may cause the death of that infant due to pulmonary insufficiency. This disease is known as respiratory distress syndrome or hyalin membrane disease. 29. State Hook's law in relation to lung. Length is directly proportional to force within a physiological limit. 30. Define lung compliance. What is 'hysteresis' curve of lung compliance? The change of lung volume per unit change in airway pressure is called as lung compliance. In compliance curve, at identical intrapleural pressure, the volume of lung is less in inspiratory phase than in the expiratory phase. This different pressure volume relationship curve during inspiration and expiration is known as 'hysteresis 'curve as represented by Figure 1.5.1. Fig. 1.5.1: Compliance curve of lungs 98 VIVA IN MEDICAL PHYSIOLOGY 31. What is specific compliance? What is its advantage to use? The compliance when expressed as a function of FRC is known as specific compliance. In individuals with one lung only, lung compliance is approximately half of the normal even if the normal distensibility of normal lung is present. Similarly in children compliance is lower than normal though the distensibility of lung remains normal. This fallacy is removed with specific compliance since FRC is proportionately reduced and specific compliance remains essentially constant. 32. Why bronchial asthma is regarded as a disease of expiratory obstruction? During inspiration the thorax expands resulting fall of intrathoracic pressure and thereby the pressure around smaller bronchioles falls. This facilitates to expand the bronchiole and thus air can flow inward but during expiration intrathoracic pressure increases resulting compression of smaller bronchioles and thus difficulty of outward air flow takes place. 33. What is peak expiratory flow rate? What is its significance? It is the maximum flow rate during a single, forceful expiration. It is valuable when measured serially to establish the pattern of airway obstructive disease and to monitor its responses in treatments especially in asthma. 34. What do you mean by alveolar ventilation? It is the amount of air comes in and out of the lung alveoli/ min. It is computed as follows: Alveolar ventilation = (TV – dead space air) × RR/min = (500 – 150) × 14/min = 5 Lit/min. SECTION I : THEORY VIVA RESPIRATORY SYSTEM 99 35. What do you mean by dead space air? Compare between anatomical and physiological dead space air? The amount of air in the respiratory system which does not take part in the gaseous exchange process is known as dead space air. Anatomical dead space is the amount of air present in the conducting zone of the respiratory system where exchange of gases does not take place. Its total amount is approx. 150 ml. The physiological dead space or total dead space includes the anatomical dead space and the amount of the air in the alveoli specially apical portion of lungs which does not take part in gaseous exchange (alveolar dead space) process because of poor blood supply. 36. What is ventilation-perfusion ratio? It is the ratio of alveolar ventilation to pulmonary blood flow. Normal value is 0.8. 37. What do you mean by diffusion capacity of lungs? It is the amount of a gas that crosses the alveolar capillary membrane per minute per mm Hg difference in partial pressure of gas on the two sides of the membrane. Its normal value is 20-30 ml/min/ mm Hg at rest. 38. Enumerate the factors affecting diffusion capacity. These are: i. Total surface area of the alveolar capillary membrane—This is directly related with diffusion capacity. ii. Thickness of the membrane—Inversely related. iii. Diffusion constant—Inversely related and depends on. a. Solubility of gases—directly related with diffusion constant. b. Molecular weight of the gases—inversely related. 100 VIVA IN MEDICAL PHYSIOLOGY 39. In case of damage of alveolar capillary membrane diffusion capacity decreases and thus diffusion of both O2 and CO2 should decrease. But practically the persons suffer from lack of O2 only without any sign and symptom of CO2 excess, why? It is because the diffusion capacity of CO2 is 20 times more than diffusion capacity of O2 and thus inspite of damage of respiratory membrane a significant amount of CO2 produced by the body diffuse to alveoli and thus no symptoms of CO2 excess is found in the body. 40. What is O2 dissociation curve? What is its normal shape? The plot of percentage of O2 saturation of hemoglobin against the partial pressure of O2 gives a sigmoid-shaped curve which is known as O2 dissociation curve as represented by Figure 1.5.2. 41. Why this curve is sigmoid? A Hb molecule contains 4 atoms of Fe++each of which combines with O2 in varried affinity. The combination of 1st heme in the hemoglobin molecule with O2 increases the affinity of the 2nd heme for O2 and oxygenation of 2nd heme increases the affinity of the 3rd and so on. This shifting of affinity of Hb for O2 produces sigmoid shape. Fig. 1.5.2: Oxygen-hemoglobin dissociation curve SECTION I : THEORY VIVA RESPIRATORY SYSTEM 101 42. What is the significance of the sigmoid shape of O2 dissociation curve? 1. O2 dissociation curve has the plateau above 60 mm Hg. This flat upper part indicates that even if the PO2 increases from 60 mm Hg to 300 mm Hg. The O2 content of the blood will not vary significantly. Similarly the effect of O2 lack on the body will not be manifested until the PO2 goes down below 60 mm Hg. 2. The steep slope of the curve indicates that the slight decrease of PO2 will cause greater release of O2 from hemoglobin. 43. What do you mean by shift to the right? Name some situations when this takes place. When the affinity of hemoglobin with O2 decreases, it favours the release of O2 to the tissues or unloading of O2 by the tissues. This is known as shift to the right. Causes: • Fall of blood pH due to either increased CO2 or presence of any acid, i.e. acidemia. • Increase in body temperature. • Increase in 2-3 DPG concentration in blood. 44. What do you mean by shift to left? What may be its causes? When the affinity of hemoglobin to combine with O2 increases, there is less release of O2 in the tissues whereas oxygenation in the lungs increases. This is known as shift to left. Causes: • Rise in blood pH or alkalemia. • Decrease in body temperature. • Increase in carbon monoxide in blood. • Presence of foetal hemoglobin. • Increase myoglobin concentration and decrease 2-3 DPG concentration in blood. 102 VIVA IN MEDICAL PHYSIOLOGY 45. What is Bohr's effect? Loading of CO2 to blood causes unloading of O2. This phenomenon seen at tissue level is known as Bohr's effect. 46. What do you mean by P50? What is its significance? It means the PO2 at which the hemoglobin is half saturated with O2. Its normal value is 26 mm Hg at PCO2 40 mm Hg, pH 7.4 and temperature 37°C. It serves as a convenient index of hemoglobin affinity for O2. Higher is the P50, lower is the affinity of hemoglobin for O2. 47. What are the vehicles of O2 transport and which one is ideal and why? Vehicles are - plasma and water of RBC and in combination with of which Hb is ideal vehicle as other two are not sufficient to meet the tissue demand of O2. 48. What is the O2 content in arterial and venous blood? Arterial blood-19 ml%; venous blood - 14 ml%. 49. What is the partial pressure of O2 in arterial and venous blood? Arterial blood - 100 mm Hg; Venous blood- 40 mm Hg. 50. In which form O2 is carried from lungs to tissues and in what amount? • In dissolved form in plasma and RBC- 0.3 ml % • In oxyhemoglobin form - 18.7 ml % 51. What do you mean by O2 carrying capacity of blood? It is the O2 carrying capacity of the total hemoglobin of blood. If the Hb content of a person is 16 gm% then his O2 carrying capacity will be 16 × 1.34 ml (each gram Hb carry 1.34 ml O2), i.e. 21 ml per decilitre of blood. 52. What is the difference between O2 content and O2 capacity? The O2 content refers to the amount of O2 actually present in a given sample of blood where as O2 capacity refers SECTION I : THEORY VIVA RESPIRATORY SYSTEM 103 to the total amount of O2 that can be carried by blood when the hemoglobin is fully saturated with O2. 53. What is coefficient of utilisation? The percent of blood that gives up its O2 as it passes through the tissue capillaries is called as the coefficient of utilisation. At rest it is about 25 per cent and during heavy exercise it increases upto 75 per cent. 54. In which form CO2 transported in blood? Mainly in 3 forms: 1. In dissolved form in plasma and RBC- 0.3 ml% 2. As bicarbonate form of Na+ and K+ - 3 ml% 3. As carbamino compound form - 0.7 ml% 55. What is the CO2 content and partial pressure of CO2 in arterial and venous blood? CO2 content PCO2 Arterial blood-48 ml% 40 mm Hg Venous blood-52 ml% 46 mm Hg. 56. In which form the venous CO2 is mostly found? In bicarbonate form. 57. What are the effects of CO2 addition to blood? It causes increase in plasma bicarbonate ion, decrease in plasma chlorides and increase in RBC chlorides. 58. What do you mean by maximum venous point and arterial point? In deoxygenated blood with maximum PCO2, 60-67 mm Hg, CO2 content is 65 ml% called as the maximum venous point as represented by Figure 1.5.3. In oxygenated blood at PCO2 40 mm Hg, CO2 content is 48 ml% called as the arterial point as represented by Figure 1.5.3. 59. What do you mean by physiological CO2 dissociation curve? If we join maximum 'venous point' and 'arterial point' which corresponds to extreme CO 2 level in the body respectively, it will roughly reflect changes between PCO2 104 VIVA IN MEDICAL PHYSIOLOGY and CO2 content in the blood and called the physiological CO2 dissociation as represented by curve C of Figure 1.5.3. Fig. 1. 5.3: CO2 dissociation curve in whole blood 60. What are the factors affecting CO2 dissociation curve? These are: • Increase in body temperature shifts the curve to the left, i.e. at increased body temperature larger amount of CO2 can be taken by the blood at a given PCO2. • Decrease in PO2 shifts the curve to the left and there by helps in loading of CO2 in blood. 61. What is a Haldane effect? Loading of O2 to blood favours the unloading of CO2. This phenomenon seen at the lung level is known as Haldane effect. SECTION I : THEORY VIVA RESPIRATORY SYSTEM 105 62. What is chloride shift? At the tissue level when CO2 enters into RBC of venous blood there is formation of bicarbonate ion which quickly diffuses out of RBC. This causes entry of one molecule of Cl– from plasma to RBC to maintain the electrical neutrality within RBC. This phenomenon is known as chloride shift. 63. Why Cl– content of RBC in venous blood is more than in arterial blood? Because of chloride shift, i.e. entry of Cl– from plasma to RBC at tissue level. 64. Why the size of RBC in venous blood is comparatively more than in arterial blood? Because of entry of CO2 in RBC at tissue level there is addition of osmotically active substances, i.e. HCO3 ion or Cl– in the RBC. This results absorption of water by the RBCs and thus RBC becomes swollen. This also results increase hematocrit value of venous blood (3% more than arterial blood). 65. Name the respiratory centers? It is of two types: • Medullary respiratory center: located in the ventrolateral medulla overlying the olivary nucleus. It constitutes of 2 centres (neurons): • Inspiratory neurons—causes inspiration • Expiratory neurons—causes expiration. • Pontine respiration center : it constitutes of 2 centers as follows: • Apneustic centre: Located in lower pons and activates inspiratory neuron or centers of medulla and thereby favours inspiration. • Pneumotaxic centre: Located in upper pons and contains both inspiratory and expiratory neurons and thereby active in both phases of respiration. It also inhibits the neurons of lower pons, i.e. apneustic center and thus prevents apneusis. 106 VIVA IN MEDICAL PHYSIOLOGY 66. What do you mean by 'inspiratory ramp'? The DRG neurons normally discharge the repetitive bursts of action potentials which is weak in the beginning and increases steadily for about 2 seconds followed by abrupt cessation of the impulse generation for next 3 secs. This type of signal is known as Ramp signal or Inspiratory ramp. Because of this signal inspiration starts slowly and then reaches peak gradually followed by abrupt turning off of inspiration resulting quiet expiration. 67. What is apneusis? How it can be resulted? It is the arrest of respiration in inspiratory phase. It can be experimentally resulted by transection in mid pons along with sectioning of vagus nerves. 68. State the neural path for voluntary control of respiration. Pathway for such voluntary control of respiration like voluntary hyperventilation, breath holding, etc. is mediated through corticospinal pathway by passing the medullary respiratory centers. 69. What is Hering-Breuer reflex? During inspiration the lungs alveoli distend causing stimulation of stretch receptors present at the walls of alveoli. This results in transmission of afferent impulses through vagus nerve to inhibit the inspiratory center and thereby stops inspiration. This reflex is known as HeringBreuer reflex which is active in case of forceful breathing of human beings. 70. What are J receptors? Which factors act as their stimulant? Hyperventilation of lungs stimulate unmyelinated vagal afferent nerve endings located in alveolar wall, juxtaposition to alveolar capillaries are called juxtapulmonary capillary receptor or J receptors. Stimulants are–hyperinflation of lungs, pulmonary congestion, pulmonary edema, inhalation of strong irritants. SECTION I : THEORY VIVA RESPIRATORY SYSTEM 107 71. What is 'J' reflex? When 'J' receptors are stimulated they inhibit spinal stretch reflex and thus limit the power of contraction of skeletal muscles including respiratory muscles. This reflex is known as J reflex. 72. What do you mean by adrenaline apnoea? Injection of adrenaline in high doses increases systemic blood pressure which in turn inhibits the respiration called adrenaline apnoea. 73. Name the chemoreceptors responsible for regulation of respiration. These are of 3 types: • Peripheral chemoreceptors, e.g. aortic bodies and carotid bodies. • Central chemoreceptors-present in ventral surface of medulla. • Pulmonary and myocardial chemoreceptors. 74. What are the chemical stimulants which regulate the respiration? These are: • Decrease of PO2 • Increase of PCO2 • Increase of H+ concentration or decrease of pH. 75. Out of these above mentioned stimulants which one is potent? It is the increase of PCO2. 76. Which stimulant is the only direct stimulant for central chemoreceptor? It is H+ concentration. 77. If both the inspiratory and expiratory centers are equally and simultaneously stimulated action of which will be dominant? Inspiratory center. 108 VIVA IN MEDICAL PHYSIOLOGY 78. What is pulmonary chemoreflex? Injection of veratridine or nicotine like alkaloid substances into pulmonary capillaries stimulate chemoreceptors present in pulmonary vessels producing bradycardia, hypotension and apnoea followed by tachycardia. This response is called pulmonary chemoreflex. 79. What do you mean by CO2 narcosis? The accumulation of CO2 in the body depresses the CNS, including respiratory centers and also produces headache, confusion, dizziness, apnoea and eventually coma. This ill effect of excess CO2 in the body is referred as CO2 narcosis. 80. Define dyspnoea. What is dyspnoeic point? It is defined as the breathing in which the person becomes conscious of shortness of his breath and thereby breathing becomes unpleasant and discomfort. The level of pulmonary ventilation, when increased to a certain level, results initiation of uncomfortable breathing or dyspnoea is knwon as, dyspnoeic point. It is generally 4-5 times increase of normal pulmonary ventilation. 81. What is apnoea? What are its causes? Apnoea is the temporary inhibition or stoppage of breathing. The causes are–deglutition, after hyperventilation, Bezold-Jarish reflex, Hering-Breuer reflex and also during sleep. 82. What is sleep apnoea? What do you mean by sudden infant death syndrome (SIDS)? In few individuals, sometimes respiration becomes inhibited or depressed with periods of apnoea during sleep. This condition is known as sleep apnoea. A form of sleep apnoea, more commonly seen in premature infants where apnoea occurs during sleep, is called as SIDS. 83. Why cardiac failure patients are preferred to sit down than lying position? It is because in lying position pulmonary congestion is SECTION I : THEORY VIVA RESPIRATORY SYSTEM 109 increased and thereby decreases vital capacity which in turn may aggravate the dyspnoeic condition (orthopnoea). 84. What do you mean by breaking point? What is due to? If breathing is stopped voluntarily, a time will come when the breathing can no longer be stopped forcibly. This point where breathing starts automatically is known as breaking point. It is due to increased arteriolar PCO2, decreased arterial PO2. 85. Define asphyxia. Inproper airation of blood due to O2 lack and CO2 excess in blood is known as asphyxia. 86. What is the difference between fresh water and sea water drowning? In fresh water drowning as the hypotonic water enters in the lungs alveoli there is continuous diffusion of water from lung alveoli to capillary blood resulting hemodilution. This inturn results swelling of RBC and ultimately hemolysis. In case of sea water drowning the hypertonic fluid enters in the lungs alveoli that initiate continuous diffusion of water from capillary blood to alveoli resulting hemoconcentration. This inturn results shrinkage of RBC and no hemolysis but decrease in blood volume. 87. Define periodic breathing. Classify it. Periodic breathing is the repeated sequence of apnoea followed by respiration. It is of 2 types: Cheyne stokes breathing and Biot's breathing. 88. What is Cheyne-Stokes breathing? Name the conditions when this type of breathing occur? The repeated sequence of gradual onset of apnoea followed by gradual restoration of respiration is called as Cheyne-Stokes breathing as represented by Figure 1.5.4. 110 VIVA IN MEDICAL PHYSIOLOGY Fig. 1.5.4: Cheyne-Stokes breathing pattern It is seen during following conditions: Physiological: Voluntary hyperventilation, high altitude, and sometimes during sleep. Pathological: Left heart failure, uremia and brain damage. 89. Define Biot's breathing. In which condition it is seen? The periodic breathing in which there are 3-4 cycles of normal respiration followed by abrupt onset of apnoea and again abrupt onset of respiration is known as Biot's breathing.It is seen in some pathological conditions like meningitis and medullary disease. 90. What do you mean by eupnoea and hyperapnoea? Eupnoea means the normal rate and amplitude of respiration whereas hyperapnoea means the increased rate and amplitude in breathing. 91. What is hypercapnoea and hypocapnoea? Hypercapnoea is the excess of CO2 in the body fluid whereas hypocapnoea is the decreased of CO2 in the body fluid. 92. What is tachypnoea and bradypnoea? Tachypnoea is rapid breathing where as bradypnoea is the decreased rate of breathing. 93. Enumerate the types of apnoea. Types of apnoea are: • Voluntary apnoea, SECTION I : THEORY VIVA • • • • • • RESPIRATORY SYSTEM 111 Vagal apnoea, Anoea vera (due to change in blood pressure), Acapnic apnoea (due to complete lack of CO2), Deglutition apnoea, Sleep apnoea, Adrenaline apnoea. 94. What are the causes of asphyxia? These are–CO2 excess, O2 lack and change in blood pH. 95. What are the various stages of asphyxia? These are hyperapnoea, respiratory convulsions and stage of exhaustion. 96. What are the various factors causing respiratory insufficiency? These are–alveolar hyperventilation, decrease in pulmonary diffusion capacity and decrease in O2 transport. 97. What is hypoxia? Enumerate its type. Hypoxia is the condition characterised by the lack of O2 in the tissue. It is of 4 types—hypoxic, anaemic, stagnant and histotoxic hypoxia. 98. Define hypoxic hypoxia. What are its causes? The condition characterised by a low arterial PO2 keeping O2 carrying capacity of blood and rate of blood flow normal or elevated is known as hypoxic hypoxia. Causes: • Low PO2 in inspiratory air • Reduced pulmonary ventilation • Decrease in gaseous exchange through alveolar capillary membrane. 99. Define anemic hypoxia. What are its causes? Hypoxia in which arterial PO2 is normal but the amount of Hb available to carry O2 is reduced, is known as anemic hypoxia. Causes: Anaemia, hemorrhage, formation of carboxy hemoglobin or methaemoglobin. 112 VIVA IN MEDICAL PHYSIOLOGY 100. Define stagnant hypoxia. What are its causes? The hypoxic condition in which the blood flow to the tissues is reduced inspite of normal arterial PO 2 and Hb concentration is known as stagnant hypoxia. Causes: Circulatory failure, heart failure, hemorrhage, etc. 101. Define histotoxic hypoxia. Hypoxia in which the amount of O2 delivered to the tissues is adequate but the tissues cannot utilise the supplied O2 because of the action of toxic agent within it, is called histotoxic hypoxia. 102. What do you mean by O2 poisoning. Inhalation of O2 in high O2 pressure that occurs when O2 is breathed at a very high alveolar oxygen pressure like in Caisson may result seizures followed by coma in most people. The other symptoms include nausea, muscle twitching, dizziness, disturbances of vision, irritability, etc. This phenomenon is called as O2 poisoning. 103. In case of severe pulmonary failure, O2 therapy may cause death, why? In case of severe pulmonary failure, there is both hypoxia and hypercapnoea present. In this situation whatever respiration is there that is due to hypoxic stimulation of peripheral chemoreceptors. O2 therapy in this stage can cause inhibition of respiration resulting further depression of respiration centers by severe hypoxia and hypercapnoea. This may cause death. 104. Define cyanosis. What are its common sites? Cyanosis is the bluish colouration of skin and/or mucosa membrane due to presence of at least 5 gm of reduced hemoglobin per 100 ml of blood in the capillaries. Its common sites are: • Mucous membrane of undersurface of tongue. • Lips • Ear lobes SECTION I : THEORY VIVA • • RESPIRATORY SYSTEM 113 Nailbeds Tip of the nose. 105. In which type of hypoxia cyanosis cannot take place and why? • In anemic and histotoxic anemia, cyanosis is absent. • In case of anemic hypoxia, the amount of Hb becomes too low and thus enough reduced Hb to produce blue colour is lacking. • In case of histotoxic hypoxia, O2 is not taken up by the tissues and thereby there is minimum chance to produce reduced Hb in greater amount to produce cyanosis. 106. Compare the central and peripheral cyanosis? Central cyanosis Peripheral cyanosis 1. It is due to hypoxic hypoxia. It is due to stagnant hypoxia. 2. Extremities become warmer due to increase blood flow to the tissue and hypertension which reflexly produce vasodilatation. Extremities become cooler due to decrease tissue blood flow and hypotension. 107. What do you mean by Caissons disease? It is the condition caused by sudden release of pressure if Caisson under water is suddenly brought out. This results the abdominal pain, disturbance of vital center in CNS and even sudden collapse of a person present within the Caisson. 108. What do you mean by N2 narcosis? If the body is exposed to high atmospheric pressure, because of high N2 pressure larger amount of N2 will enter into lungs and thereby in body fluids ultimately causing euphoria, impairement of mental function and symptoms of alcoholic intoxication. These effects of N2 in higher pressure is called N2 narcosis. 114 VIVA IN MEDICAL PHYSIOLOGY 109. How does effect of N2 narcosis can be avoided? By adopting two methods: • By using O2 helium mixture instead of N2 - O2 mixture in Caisson. • By gradual release of pressure from the Caisson. 110. What is high pressure nervous syndrome (HPNS)? At high atmospheric pressure O2 helium mixture used in Caisson can produce tremor, drowsiness, depression of activity in EEG. This condition is known as HPNS. 111. Name different lung function tests. These are: • Measurement of FRC • Measurement of dead space • Measurement of VC and FEV1 • Measurement of lung volume and capacities • Measurement of PO 2 and PCO 2 in inspiratory, expiratory and alveolar air. 112. What is acute mountain sickness? In some instances, the compensatory mechanism to high altitude breaks down and gives rise to serious symptoms known as Monge's disease or acute mountain sickness characterised by: • Considerable increase of red cell mass and PCV. • High pulmonary arterial pressure. • Right heart failure in some cases. 113. What is chronic mountain sickness? It is the disease occurring in case of failure of long-term acclimatization process to the residents of high altitude. The signs and symptoms are: • Extreme polycythemia • Increase in viscosity of blood that results fall of blood flow • Increase in BP • Cyanosis, fatigue, exercise intolerance • Pulmonary oedema. SECTION I : THEORY VIVA RESPIRATORY SYSTEM 115 114. What are the acclimatization to the natives of high landers? The acclimatization that occurs in the residents who are residing in the high altitude permanently for generations after generations, are as follows: • Short body stature and large sized chest that results high ratio of ventilatory capacity to body mass. • Hypertrophy of right heart. • Polycythemia • Shifting of O2 dissociation curve to right • Increase in size of carotid bodies. 115. What are the aims of artificial respiration? These are: • Avoiding asphyxia to brain • Oxygenation of body tissue • Ventilation of lung • Stimulation of spontaneous breathing. 116. What are the indications of artificial respiration? Artificial respiration is given to the subject in case of following conditions: a) Acute respiratory failure due to: • Overdose of anesthetic agent • CO poisoning • Drowning • Electric shock • Hanging • Intake of narcotic drugs • Resuscitation of new born b) Chronic respiratory failure due to: • Diphtheria • Poliomyelitis • Ascending paralysis 117. What do you mean by CPR? If the respiration fails along with stoppage of heart beat this procedure is followed till the person is not hospitalised for proper treatment. The procedures are: 116 VIVA IN MEDICAL PHYSIOLOGY • • • • Cleaning of the airways Mouth to mouth breathing at the rate of 16-18/min External cardiac massage by pressing lower border of sternum by 4-5 cm at the rate of 80-90 times/min. After every 15 cardiac massage two mouth to mouth (15:2) breathing (if two subjects are present. After every 5 cardiac massage 1 mouth to mouth (5:1) breathing (if one subject is available). 118. What do you mean by Kussmaul breathing? During some clinical conditions like diabetic coma there is rapid and deep breathing eliminating CO 2 and bicarbonate. This type of rapid and shallow breathing is known as Kussmaul breathing. NERVE MUSCLE PHYSIOLOGY 117 SECTION I : THEORY VIVA 1.6 Nerve Muscle Physiology 1. Why nerve cells do not divide? It is because of absence of centriole. 2. What is the structural and functional unit of nerves? Enumerate its components. The structural and functional unit of nerve is neuron. It consists of cell body or soma, axon, dendron and dendrites. 3. Classify the neuron. The neurons can be classified by 3 different approaches as follows: A. Depending on the function: On the basis of it's function neuron is classified as: a) Motor neurons: These carry the motor impulses from CNS to the peripheral effector organs. This is why it is also known as efferent nerves. The motor neurons have long axons and short dendrites. b) Sensory neurons: These carry the sensory impulses from peripheral organs or tissues to the CNS and is also known as afferent nerves. These neurons have a short axon and long dendrites. B. Depending on the polarity : As per this it is divided into 3 types - Unipolar, Bipolar and Multipolar neurons. a) Unipolar: In this type of neuron both the processes of neuron i.e. axon and dendrite originate from one pole or site of cell body. This type of nerve cell is present only in embryonic stage in human. 118 VIVA IN MEDICAL PHYSIOLOGY b) Bipolar: In this type of neuron axon and dendron arise from two different pole. c) Multipolar: This has many poles, i.e. one of the poles gives rise to the axon and all the other give rise dendrites. C. Depending on the length of axon: On the basis of the length of axon neurons are of two types - Golgi type-I and Golgi type -II. a) Golgi type I neurons: In this type of neurons the axons are long and the cell body is present in CNS and their axons reach the remote peripheral organs. b) Golgi type- II neurons: These neurons have short axons and are present in cerebral cortex, spinal cord, etc. 4. What is 'nodes of Ranvier'? What are the functions of myelin sheath? The axon of neuron is surrounded by a protein-lipid complex called myelin sheath except at its endings and also at periodic constrictions about 1 mm apart. This part of axons where there are no myelin sheath present, is called 'nodes of Ranvier'. Functions of myelin sheath: • Prevents cross-stimulation of adjacent axons due to its high insulating property. • Facilitates rapid conduction of nerve impulse. • Protects and provides the nutrition to the axoplasm. 5. Compare the myelinated and unmyelinated nerves. Myelinated Unmyelinated 1. Presence of myelin sheath. Absence of myelin sheath. 2. Location - in all preganglionic fibers of ANS and somatic nerve fibers more than 1µm diameter. Location - in all post-ganglionic fibers and somatic nerve fibers of <1µm in diameter. 3. Conduction rate through it is fast. It is rather slow. SECTION I : THEORY VIVA NERVE MUSCLE PHYSIOLOGY 119 6. Name different types of glial cell. These are the supporting cells in nervous system and mainly are of 3 types. • Microglia—These are phagocytic cells that enter the CNS from meninges and blood vessels. • Astrocytes—These are found throughout the brain joining to the blood vessels and investing synaptic structures, neuronal bodies, neuronal processes. It helps in support, transport, inflammatory reaction and also helps in forming blood-brain barriers. • Oligodendroglia—These are the cells that form myelin around axon within CNS. 7. What is nerve growth factor? Mention their function. Nerve growth factors are protein in nature present in salivary glands, plasma and in many different tissues, necessary for the growth and maintenance of sympathetic neurons. Function: Helps in growth and maintenance of sympathetic neurons and also some sensory neurons and cholinergic neurons in brain. 8. Enumerate the heat production in nerve fiber. Heat is evolved by the nerves during its activation in 3 phases as follows: • Resting heat—It is the amount of heat produced while nerve is inactive. • Initial heat: — Immediately after muscular activity is started, heat is produced by the working muscle which is dependent on anaerobic changes in the muscle. This heat is named as initial heat. — It occurs during action potential. — It is anaerobic and coincides with the spike potential. — It is due to breakdown of ATP and creatine phosphate (CP) 120 VIVA IN MEDICAL PHYSIOLOGY • Delayed or recovery heat: — Delayed heat is the heat liberated during relaxation process of a muscle — It is aerobic and 30 times of the initial heat. — Here, energy is used for resynthesis of ATP and CP. 9. What do you mean by accommodation in relation to neuron? Which nerves have less power of accommodation-sensory or motor? If a nerve is submitted to the passage of a constant strength of current, the site of the nerve under stimulation shows decrease of excitability after sometime. This property of fiber is known as accommodation. Sensory nerve has less power of accommodation. 10. What do you mean by saltatory conduction? In case of myelinated nerves, the wave of depolarisation jumps from one node of Ranvier to the next as myelin sheath is impermeable to ions. This is responsible for rapid transmission of nerve impulse. This type of jumping of depolarisation from node to node is called as saltatory conduction. 11. What do you mean by orthodromic and antidromic conduction? When an action potential is initiated in the middle of an axon or neuron, it can be conducted in either direction but the impulses normally pass in one direction, i.e. from receptor or synaptic junction of a neuron to the synaptic knob of that particular neuron down the axon. Such conduction is called as orthodromic conduction. Conduction in opposite direction is called as antidromic conduction seen in sensory nerve supplying the blood vessels. 12. Which one is the best form of artificial stimulus for the nerve fiber and why? It is the electrical stimulus as: SECTION I : THEORY VIVA • • • NERVE MUSCLE PHYSIOLOGY 121 Its intensity and frequency can be precisely controlled. It can be applied to a specific site. It does not cause any injury. 13. What is the thermal range for nerve fibers activity? It varies, though the normal range is 0°C to 50°C. 14. What do you mean by normal coefficient of nerve impulse? It means that within physiological range the velocity of nerve impulse is doubled with every 10°C rise of temperature. 15. What do you mean by nerve impulse? Nerve impulse is the state of electronegativity by depolarisation at point of stimulation of nerve fiber and its propagation throughout its length. 16. What do you men by All or None law? Is it applicable in nerve bundle or muscle mass? If a nerve fiber is stimulated by a stimulus it will be excited (depolarised) maximally or not at all. This relationship between the stimulus and response is known as All or None Law. It is applicable only in a single nerve fiber or single muscle fiber not in a nerve bundle or muscle mass. 17. What is the relation of thickness of nerve fiber with the velocity of nerve impulse? It is directly related, i.e. the more the thickness of the nerve, the more is its velocity of conduction rate. 18. Why does temporary paralysis is seen after sitting cross leged for long periods? It is due to the loss of conduction in motor, touch and pressure fibers due to prolonged pressure on a nerve. In this case pain sensation remains unaltered. 19. What is the Bell and Megendie's classification of nerve fiber? It is based on the direction of impulse. On this basis it is of two types: 122 VIVA IN MEDICAL PHYSIOLOGY • • Afferent fibers that carry impulse from periphery to center. Efferent fibers that carry impulse from centre to periphery. 20. What are the Erlanger and Gasser classification of nerve fibers? As per this classification it is divided into mainly 3 groups: • A fibers which are further subdivided into α, β , γ and δ. • B fibers • C fibers. 21. What do you mean by 1st degree and 5th degree injury of nerve fiber? • First degree injury is the temporary impairment of nerve function due to ischaemia caused by direct pressure to a nerve for a limited time. • Fifth degree injury means the complete transection of nerve fiber. 22. What is chromatolysis? After the sectioning of nerve fibers the Nissl's granules of cell body of a nerve disintegrates and loose their staining reaction, thereby cell becomes colourless. This event is known as chromatolysis. 23. Define neuromuscular junction. The junction between the motor nerve and skeletal muscle fiber is called neuromuscular junction. 24. What are palisades? What are their importance? In the neuromuscular junction, underneath the nerve endings, the muscle membrane of motor end plate is thrown into folds called palisades. It increases the surface area on which neurotransmitters can act. 25. What is end plate potential (EPP)? In response to binding with neurotransmitter, e.g. ACh on post-synaptic membrane, the post-synaptic membrane SECTION I : THEORY VIVA NERVE MUSCLE PHYSIOLOGY 123 undergoes depolarisation due to Na+ influx. This wave of depolarisation below the threshold level is called as end plate potential which is not propagatory in nature. 26. What is MEPP? Differentiate EPP and AP. During rest there is very small potential changes (upto 0.5 mv) can be recorded from the motor end plate even if there is no impulse. This is known as MEPP. EPP AP 1. Non-propagatory in nature 2. It does not obey all or none law Propagatory in nature Obeys all or none law 3. It can be summated Cannot be summated. 27. What is giant end plate potential (GEPP)? In experimental animals, inhibition of MEPP results in production of GEPP due to release of more quantity of ACh. This results more depolarisation of motor end plate though not sufficient to produce action potential. 28. What is myasthenia gravis? What are its common sites? Myasthenia gravis is characterised by rapid onset of fatigue with marked generalised weakness of muscles due to damage of nicotinic ACh receptors by circulating antibodies on the post-synaptic membrane of neuromuscular junction. Common site is extraocular muscle, facial muscle, swallowing and mastication muscle. 29. What is Lambert-Eaton syndrome? It is also characterised by the weakness of muscle caused by the antibodies against Ca++ channels in the nerve ending at the neruomuscular junction. This decreases Ca++ influx to the synaptic knob and thereby decreases ACh release to the synaptic cleft. 30. Classify and compare different types of muscle. Muscle is of 3 types—skeletal, cardiac and smooth. 124 VIVA IN MEDICAL PHYSIOLOGY Parameters Skeletal Cardiac Smooth 1. Location Attached to the bone In heart In hollow viscera like GIT, blood vessels. 2. Structure Presence of Presence of well-Lack cross well-developed developed cross-striations. cross-striations striations 3. Control Non-syncytial Functionally syncytial Can be both. Single unitfunctional syncytial, Multiunit- non syncytial Voluntary Involuntary Involuntary 31. What is due to the cross-striation in the skeletal muscles? It is due to the difference in the refractive index of various parts of muscle fiber. Dark band is due to the highly refractile material (myosin) and light band is due to the lower refractile material (actine, tropomyosin and troponin). 32. What is the contractile unit of muscle? Define it. Sarcomere is the contractile unit. The area of the muscle fiber in between two adjacent Z lines is called as sarcomere. 33. Enumerate thick and thin filaments? Thick filaments are myosin each of which is comprised of a short compact head known as heavy meromyosin (HMM) and a long tail called light meromyosin (LMM).Thin filaments are comprised of: • Actin: Which are of two types-G actin (globular) and F actin (fibrous) • Tropomyosin • Troponin: Which are of again 3 types-troponin I, troponin T and troponin C. SECTION I : THEORY VIVA NERVE MUSCLE PHYSIOLOGY 125 34. What is the contractile machinery of muscle? What is the main function of myosin? Actin and myosin are the contractile machinery. Main function of myosin-it has ATPase activity and thereby converts ATP to ADP with formation of initial energy needed for muscle contraction. 35. What do you mean by sarcotubular system? What is triad? It is the specialised system within the muscle fiber responsible for conduction of electrical impulse from sarcolemma to the interior of muscle fiber. It is made-up of two structures. • Transverse tubular system—extension of sarcolemma into muscle fibers at A-I junction. • Longitudinal sarcoplasmic reticulum—sac like structure of dialated sarcoplasmic reticulum (SR) known as terminal cisternae. There is a close proximity of the terminal cisternae and the T system. Transverse tubules with two adjacent terminal cisternae in opposite site is called as triad. 36. What do you mean by E-C coupling? The process by which depolarisation of the muscle fiber initiates contraction of muscle is called as E-C coupling. 37. What changes take place in sarcomere during active muscle contraction? During contraction A band remains unchanged in length whereas H and I bands are shortened. 38. What is contractile component of muscle? Contractile component represents the elasticity of thick and thin filaments and is of two types: • Series elastic component (SEC)—example: tendon • Parallel elastic component (PEC)—example: connective tissue and sheath. 126 VIVA IN MEDICAL PHYSIOLOGY 39. What do you mean by optimum and equilibrium length of muscle? Optimum length is the length of the muscle in which it develops maximum active tension. Equilibrium length is the length of the relaxed muscle cut free from its bony attachments. 40. What do you mean by isotonic and isometric contraction? During muscular contraction when the length of the muscle remains same and no external work is done then that type of contraction is known as isometric contraction whereas the muscle contraction in which length of the muscle changes while tension remains constant is called as isotonic contraction. 41. How does muscle length remain same during isometric contraction? By two ways: • All the muscle fibers in a group of muscle do not contract at the same time. Some contract, others are kept in relaxed thereby shortening of some fibers are compensated by relaxation of others. • Any shortening in muscle length gets compensated by stretching of the SEC, i.e. tendon therefore, length remains same. 42. Why does no external work is done in isometric contraction? As distance through which weight is moved is almost zero and as work done is equal to force timed distance, therefore the external work done is also zero. 43. What do you mean by freeload and after load? In which condition work done is greater? • After loaded contraction is the contraction of muscle in which the load acts on the muscle only after it starts to contract. In a free loaded contraction, the load acts on the muscle before it starts to contract. SECTION I : THEORY VIVA • NERVE MUSCLE PHYSIOLOGY 127 Freeloaded muscles do more work than an afterloaded muscle upto a physiological limit. It is due to the increase of initial length of muscle fiber due to stretching of muscle by the load in rest. 44. Define motor unit. What do you mean by recruitment of motor unit? Each single motor neuron and all the muscle fibers supplied by each single motor neuron is called as motor unit. Recruitment of motor unit: When an excitatory nerve is stimulated with a stimulus of constant strength for a long time, there is a progressive increase in the reflex response. This is due to the progressive increase in the number of motor neurons activated. This phenomenon is known as recruitment of motor unit. It is similar to the effect of temporal summation. 45. What is size principle? Fast or white muscles are innervated by fast conducting, i.e. myelinated motor neurons. Whereas slow or red muscles are innervated by slow conducting, i.e. unmyelinated motor neurons. This is known as size principle. 46. Contrast between fast and slow muscles? White (fast) muscles Red (slow) muscles Muscle fibers are large in diameter. Moderate in diameter. Contain high amount of glycogen and ATPase (That is why pale or white). Moderate glycogen level with low ATPase activity. Innervated by large and myelinated nerves. Innervated by small and slow, i.e. unmyelinated fibers. These are specialised for fine Respond slowly and adapted for skill movements, e.g. extraocular. long, slow and posture maintaining muscles and muscles in hand. contractions. Easily fatigued. Resistant to fatigue. 128 VIVA IN MEDICAL PHYSIOLOGY 47. Define a simple muscle twitch. What are duration of a muscle twitch in fast and slow muscle fibers? A single and brief electrical shock of adequate intensity applied to the motor nerve gives a single action potential which in turn causes a brief contraction followed by relaxation of muscle. This response is called as 'A simple muscle twitch'. • Duration of a twitch in fastest muscle is 7.5 msec. • Duration of a twitch in slowest muscle is 100 msec. 48. What do you mean by make and break stimulus? In neuromuscular preparation, galvanic current causes stimulation both at make and break point. At make, stimulus starts from cathode and is called as cathodal or make stimulus whereas at break, stimulus starts from anode and is called as anodal or break stimulus. 49. State Bois Regmond's law? It states that it is only at make or break a nerve can be stimulated. 50. What do you mean by ascending and descending current? In nerve muscle preparation, if anode lies close to muscle and direction of current is away from it, it is called as ascending current whereas if cathode is nearer to the muscle and direction of current is towards muscle it is known as descending current. 51. What is electrotonus? It is the altered physiological state around the electrode point in a nerve fiber due to constant current. 52. What is meant by the terms 'tension' and 'load'? Tension is the force exerted by a contracting muscle on an object and load is the force exerted by the weight of an object on a contracting muscle. Thus in true sense tension and load are opposing forces. SECTION I : THEORY VIVA NERVE MUSCLE PHYSIOLOGY 129 53. Define minimal and maximal stimulus. Minimal stimulus is the amount of weakest current that can produce a muscle contraction whereas the maximal stimulus is the current which produces the strongest contraction of a muscle which is capable of by a single stimulus. 54. What is rheobase and chronaxie? Rheobase is the weakest intensity of constant current in volts capable of exciting the muscle. It is about 0.2-0.3 volts. Chronaxie is the minimum duration required to contract (exite) the muscle by the intensity of current strength of twice of rheobase. 55. What is latent period? It is the time taken to contract the muscle in response to its stimulation and is denoted from point of stimulation to beginning of contraction. 56. What is true latent period? If the muscle is directly stimulated and if an optical recording system is employed to exclude the inertia of the mechanical lever then the latent period is much reduced. The latent period still present in that condition is known as true latent period. 57. Define refractory period. In which muscle it is maximum? It is a short period of ineffectivity or unresponsiveness of second stimulus applied at a very short interval after the 1st stimulus. Cardiac muscle has the largest refractory period. 58. Define fatigue. Which one is the seat of fatigue? Fatigue is defined as progressive and temporary loss of excitability in a muscle due to its continuous stimulation. In nerve muscle preparation, seat of fatigue is in neuromuscular junction where as in whole body it is in nerve cell or even in CNS. 130 VIVA IN MEDICAL PHYSIOLOGY 59. If two successive stimulus is applied to motor nerve in a nerve muscle preparation the effect of 2nd stimulus becomes greater. What is this property known as? What is due to? It is known as beneficial effect which is due to the following reasons: • Increase in temperature. • Accumulation of metabolites. • Decrease in viscosity of muscle. 60. What do you mean by treppe response or staircase phenomenon? What is its cause? When a series of maximal stimuli are applied to nerve muscle preparation in such a way so that successive stimuli falls during the relaxation phases of the previous stimulus, the tension developed during each twitch increases gradually and successively till a uniform tension per contraction is reached. This successive increase of tension of each twitch is called as treppe response or staircase phenomenon. It is due to increase availability of Ca2+ for binding troponin C. 61. What do you mean by Tetanus? What is complete and incomplete tetanus? When a series of repetitive stimuli are applied in muscle at a rate high enough to cause summation of contraction so that there is continuous contraction with no ralaxation at all, that state is termed as tetanus. In such a tetanic contraction when there is no relaxation between stimuli it is called as complete tetanus as represented by Figure 1.6.1 (in left panel) whereas when there are periods of incomplete relaxation between the summated stimuli it is known as incomplete tetanus as represented by Figure 1.6.1 (in right panel) SECTION I : THEORY VIVA NERVE MUSCLE PHYSIOLOGY 131 Fig. 1.6.1: Genesis of tetanus 62. What is rigor mortis? After death the muscle fibers develop a state of extreme rigidity due to complete depletion of ATP and phosphocreatine. This state of rigidity of the muscle after death is called rigor mortis. 63. How do you record temperature changes in the muscles? By using an instrument named thermopile. 64. Define steady state? When body can maintain a steady rate of O2 usage to keep the lactic acid produced by muscular activity constant by balancing its rate of formation and removal, this state is called as steady state. 65. What is O2 debt? After a period of severe muscular exercise the amount of O2 consumed is enormously more than the amount of O2 consumed under resting condition. This extra amount of oxygen which is utilised for reversal of some metabolic process is known as O2 debt. The metabolic processes are: • Resynthesis of glucose from lactic acid accumulated, • Resynthesis of ATP and creatine phosphate. 132 VIVA IN MEDICAL PHYSIOLOGY • Restoration of amount of O 2 dissociated from hemoglobin and myoglobin. 66. What do you mean by muscular fasciculation? It is a spontaneous contraction of motor units which is visible through the skin as fine ripping movement in the relaxed muscles. 67. What is second wind? During exercise after an initial dysponea there is again adjustment in respiration and circulation and the subject is said to have got second wind. 68. What is electromyography? It is the procedure to obtain the record of muscular activity by using electromyograph and helpful to diagnose neuromuscular disorder like myasthenia gravis, myotonias, etc. 69. What are the morphological features of cardiac muscle? These are as follows: • Presence of intercalated disc which is extensive folding of cell membrane at the point of contact of two muscle fibers. It provides strong union between fibers. • Presence of gap junction which provides rapidity of conduction of impulse. • Presence of functional syncytium. • Highly vascular, well-developed sarcotubular reticulum with plenty cytoplasm, mitochondria and rich in glycogen. 70. What is the difference between sarcotubular system of heart and skeletal muscle? In both the muscles, it is well developed but in the cardiac muscle 'T' system penetrates the sarcomere at Z Line and therefore there is only one triad per sarcomere but in skeletal muscle there are 2 triads per sarcomere as T system penetrates at A-I junction and as 2 A-I junctions are present in each sarcomere. SECTION I : THEORY VIVA NERVE MUSCLE PHYSIOLOGY 133 71. Why does atrial and ventricular muscle fibers do not have pre-potentials? It is because of K+ permeability is constant in those muscles during diastole. 72. What is calcium rigor? Increase Ca ++ concentration in ECF, increases myocardial contractility with marked increase in serum Ca++, that relaxes heart less in diastole and finally stops in systole. This condition of heart is known as calcium rigor. 73. Differentiate between pre-load and after-load. Pre-load 1. This is the load which acts on the muscle before it begins to contract. After-load This is the load which acts on the muscle after it begins to contract. 2. It results isometric contraction. It causes isotonic contraction. 3. In vivo it is the degree to which It is the resistance against which the the myocardium is stretched ventricles pump the blood. before it contracts. 74. Why does cardiac muscle do not have fatigue? Why it can't be tetanised? It does not have fatigue as the refractory period is too long and during this period replenishment of energy takes place and thereby no exhaustion of energy. It can't be tetanised as absolute refractory period is too long and hence summation of contractile response is not possible. 75. What do you mean by plasticity of muscle? The length tension relationship of muscle is called as plasticity of muscle. 76. What is excitatory junctional potential (EJP)? In smooth muscles in which adrenergic discharge is 134 VIVA IN MEDICAL PHYSIOLOGY excitatory, stimulation of the adrenergic nerve produces discrete partial depolarisation that resembles small end plate potential. These potential changes are called as EJP. 77. What is the source of energy in a smooth muscle? These are mainly fatty acids, acetoacetic acid and glucose in lesser extent. 78. What are the types of a smooth muscle fibers? Where are they located? It is of two types: Single unit and multi-unit. • Single unit: (Named as they function as functional syncytial fashion)–Present in GIT, uretors, bronchi, uterus, urinary bladder. • Multi-unit: (Non-syncytial)-Iris, cilliary muscles of eye, pilomotor muscle of skin and muscles of blood vessels. 79. What is muscle tone? The living skeletal muscles are always in the state of partial sustained contraction. This is known as muscle tone. EXCRETORY SYSTEM 135 SECTION I : THEORY VIVA 1.7 Excretory System 1. What is the anatomical and physiological unit of kidney? It is nephron. 2. Which kidney is not palpable normally? When it becomes palpable? Left kidney is not usually palpable. It becomes palpable when it is enlarged or low in position. 3. Classify and differentiate between types of nephron. It is of two types: cortical and juxtamedullary: Parameters 1. Amount Cortical nephron Juxtamedullary nephron 85% 15% 2. Size of glomerulus Small Large 3. Site of glomerulus In outer cortex Junction of cortex and medulla (Inner cortex) 4. Size of Henle's loop Small Long 5. Vascular supply Through peritubular capillaries Through vasa recti and peritubular capillaries 6. Rate of filtration 7. Function Slow Fast. Reabsorption and concentration of urine secretion 4. Enumerate the components of nephron. It consists of: 136 VIVA IN MEDICAL PHYSIOLOGY 1. Renal corpuscle—Which is made up of two structuresBowman's capsule and glomerulus 2. Renal tubule—It is a long tube containing different segments named as proximal convoluted tubule (PCT), Henle's loop, distal convoluted tubule (DCT), collecting tubule (CT) and collecting duct. 5. Mention the non-excretory functions of kidney. 1. Homeostatic function: It maintains the constancy of the internal environment, i.e. ECF by regulating body fluid volume, body fluid composition via conserving and excreting water and solutes and pH of the body fluid. 2. Endocrine function: It secretes different hormones or hormone like substances in different condition e.g.: Renin secretion, Erythropoietin secretion, Mudullipin secretion (which is secreted from renal papilla and acts in opposite to renin - angiotensin mechanism to regulate arterial BP) and conversion of Cholecalciferol (Vit D3) to 1-25 Dihydroxy cholecalciferol which helps in regulation of Ca2+ concentration in body fluids. 3. Metabolic function: In unusual condition like prolonged starvation, chronic respiratory acidosis kidney synthesises and releases glucose from noncarbohydrate source by gluconeogenesis. 6. What is the rate of blood flow through the kidney? It is 1200-1300 ml/ min. 7. What peculiarities of renal circulation help the kidney to work even in chronic renal disease? It is because of presence of Ludwig shunt. 8. What is the rate of glomerular filtrate formation? It is 125 ml/min and 180 L/day. 9. What is filtration fraction? What does it represent? It is the ratio of glomerular filtration rate and plasma flow rate, i.e. FF = GFR/PFR = 130/700 = 0.18 It is a measure of filtering efficiency of glomerulus. SECTION I : THEORY VIVA EXCRETORY SYSTEM 137 10. Name the factors affecting GFR along with its relationship. These are as follows: • Glomerular capillary hydrostatic pressure—directly related with GFR. • Glomerular capillary oncotic pressure—inversely related with GFR. • Bowman's capsular hydrostatic pressure—directly related. • Bowman's capsular oncotic pressure—inversely related. • Permeability of glomeruler capillary—directly. • Surface area—irectly related with GFR. 11. What are the factors affecting renal blood flow? • Exercise: Exercise decreases the RBF by increasing the sympathetic activity which results vasoconstriction in renal bed, i.e. Exercise →increase in sympathetic activity →increase in release of NE/Angiotensin- II→ vasoconstriction in afferent arteriole → decrease in RBF. • Posture: In sudden change of posture from supine to standing the RBF falls due to: Change of posture from supine to standing → decrease in BP → reflex increase of sympathetic activity → vasoconstriction → decrease in RBF. • High protein diet: It increases RBF by increasing the glomerular capillary pressure. • BP: Increase in renal arterial BP →reflex reduction in sympathetic tone → renal arteriolar dilatation → increase in RBF • Neurohumoral substances: – Norepinephrine, Angiotensin- II → decrease in RBF – Prostaglandins, ACh →increase in RBF 138 VIVA IN MEDICAL PHYSIOLOGY 12. Enumerate the factors affecting GFR. The factors affecting the GFR are: • Bowman's capsular hydrostatic pressure (PB) • Glomerular capillary hydrostatic pressure (PG): It is further determined by (i) Arterial pressure (ii) Renal blood flow (iii) Afferent arteriolar resistance and (iv) Efferent arteriolar resistance. • Glomerular capillary oncotic pressure (πG) • Bowman's capsular oncotic pressure (πB) • Filtration coefficient (Kf): It is further determined by permeability of the glomerular capillary membrane and surface area and thus both these factors determine GFR by influencing Kf. 13. Which method of renal function tests is most preferred clinically? What are its advantages? Creatinine clearence test. It is a simple method as no intravenous infusion is required. 14. What do you mean by filtered load and excretory load? The amount of a substance that appears in urine/unit time is called as excretory load whereas the amount of solute transported across the glomerular membranes per unit time is called as filtered load or tubular load. It is calculated as filtered load = blood glucose level × GFR/100. 15. What do you mean by high threshold, low threshold and no threshold substances? Some of the contents of glomerular filtrate like glucose, Na + , K + , water, Ca ++ , etc. are reabsorbed almost completely. These are known as 'high threshold substances' whereas some contents like urea, uric acid, phosphates are reabsorbed to some extent only and are known as 'low threshold' and the substances like creatinine and sulphates are not reabsorbed at all which are called as no 'threshold substances'. SECTION I : THEORY VIVA EXCRETORY SYSTEM 139 16. What is transport maximum (Tm) limited mechanism? According to this, substances like glucose, certain amino acids are completely reabsorbed under certain concentration beyond which those are excreted in the urine. 17. What is gradient time limited mechanism? If the substances are allowed to stay more in the renal tubles, there is more reabsorption of that substances by the renal tubules. This kind of mechanism of reabsorption of substances like Na+ is known as gradient time limited mechanism. 18. What is obligatory reabsorption? When the reabsorption of substances are not controlled or concerned with regulating levels of substances in the body, it is known as obligatory reabsorption. Eighty per cent of NaCl and water reabsorption is obligatory in nature. 19. What is facultative reabsorption? When reabsorption of substances take places according to the need of the body and is regulated by some regulatory substances in the body, it is called as facultative reabsorption. 20% of NaCl and water reabsorption through DCT and CT is through ADH and therefore, it is an example of facultative reabsorption. 20. What is Tm limited mechanism? Give the Tm value of glucose, amino acid, creatinine, PAH and plasma protein. For substances that are actively reabsorbed or secreted by the renal tubules, there is a maximum rate at which they are reabsorbed or secreted. This maximum rate of transport is known as transport maxima or Tm. 140 VIVA IN MEDICAL PHYSIOLOGY Tm value for some substances Substances Tm value Tm of actively reabsorbed substances: Glucose 320 mg/min Amino acids 1.5 mg/min Plasma proteins 30 mg/min PO4= 0.1 mg/min SO4= 0.06 mg/min Tm of actively secreted substances: Creatinine 16 mg/min PAH 80 mg/min 21. Name the substances reabsorbed by renal tubules along with the site of reabsorption. Substances Site of reabsorption %age of reabsorption Na+ (98%) PCT DCT CT 80 % 15 % 2-3 % K+ PCT DCT & CT 90 % 10 % Cl– PCT Henle's loop 70-85 % 15-30 % HCO3– PCT DCT& CT 85-90 % 10-15 % Glucose Water PCT PCT DCT & CT 100 % 70-85 % 15-30 % 22. What do you mean by tubular maxima for glucose (TmG)? Critical level at which filtered load of glucose exceeds the capacity of reabsorption system through renal tubules is called as tubular maximum for glucose. 23. What is renal threshold for glucose? It is the plasma level of glucose at which glucose first SECTION I : THEORY VIVA EXCRETORY SYSTEM 141 appears in the urine in more than the normal minute amount. Its value is 180 mg%. 24. If TmG is 320 mg/min still why does glucose appears in the urine when the plasma glucose level is 180 mg% at which the tubular load is 225 mg/min? This is because all tubules within the kidney are not capable of absorption of same (equal) amount of glucose. Some tubules have much lower TmG than others. In these tubules some glucose remain unabsorbed even at a lower plasma glucose level and thus is excreted in urine. This phenomenon is known as 'Splay'. 25. What is the chief function of juxtamedullary and cortical nephrons? Juxtamedullary nephrons are mainly responsible for water reabsorption through counter current system and cortical nephrons are mainly responsible for Na+ reabsorption. 26. Enumerate JGA along with its function. The JGA is a combination of specialised tubular and vascular cells located at the vascular pole where the afferent and efferent arterioles enter and leave the glomerulus. It is composed of 3 types of cells: • Juxtaglomerular or JG cells—Present in afferent arteriolar wall mainly and also in efferent arteriolar wall, where these enter and leave glomerulus. These cells are responsible for synthesis, storage and release of enzyme renin and also hormone erythropoietin. • Mucula densa cells—These are present in distal tubule part and they function as chemoreceptor and are stimulated by decrease NaCl concentration in tubular fluid passing through DCT. • Mesangial cells or lacis cells—These are supporting cells found between capillary loops. They also play a role in the regulation of glomerular filtration because of its contractile property. 142 VIVA IN MEDICAL PHYSIOLOGY 27. What do you mean by tubuloglomerular feedback? In response to change of NaCl concentration in distal tubular fluid (Decrease NaCl concentration) there is stimulation of macula densa cells which in turn stimulates JG cells to release renin. This renin by series of events ultimately controls GFR. This mechanism is known as tubulo-glomerular feedback mechanism. 28. What is filtration coefficient? It is the function of the capillary surface area and the membrane permeability (i.e. surface area × membrane permeability). This determines the GFR in some pathological condition. 29. Define uniport, co-transport and antiport with suitable example. • Uniport: This is the mechanism by which the carrier protein present in the cell membrane causes transportation of a single molecule in one direction only. – Example: facilitated diffusion of glucose. • Co-transport or symport: The mechanism by which the carrier proteins present in the cell membrane transports two particles together in same direction is called as symport or co-transport. – Example: secondary active transport of glucose. • Antiport or counter transport: The mechanism by which the carrier proteins of the cell membrane transports two or more molecules in opposite direction is known as antiport or counter transport. – Example: Na +- K+ pump operated in the cell membrane. 30. What is normal blood urea level? It is 15-40 mg%. 31. What is normal urea clearance level? If urine excretion is 2 ml or more per minutes then the amount of urea excreted in urine is known as maximum SECTION I : THEORY VIVA EXCRETORY SYSTEM 143 clearance which is 72 ml/min, whereas if urine excretion is less than 2 ml/min then the amount of urea excreted in urine is known as standard clearance which is 24 ml/min. 32. What is normal insulin and creatinine clearance? It is 120-130 and 80-110 ml/min respectively. 33. What are the salient features of a substances used for measuring GFR? Name some of them. It has to be following features: • It should be freely filtered. • It should be neither reabsorbed nor secreted and nor metabolised. • It should not be toxic. • It should not alter the hemodynamics. Such substances are- inulin, creatinine, mannitol, sorbitol, radio-iodine, etc. 34. What is the average daily urea formation in the body? In human it is 25-30 gm/day. 35. What are the main symptoms of uraemia? These are drowsiness, headache, muscular twitching and weakness, vomiting, metabolic acidosis, hypertension, anaemia and cardiac arrhythmias. 36. Which is the major source of ammonia formation by the kidney? It is glutamate. 37. What do you use to determine GFR and RBF? Inulin for GFR and PAH for RBF. 38. At what stage does chronic renal failure occur? When normal function of kidney falls to 25 per cent or below than its normal function or loss of 75 per cent or more nephrons take place then chronic renal failure occurs. 39. How does dilute or concentrated urine is formed? It is by counter current system. 144 VIVA IN MEDICAL PHYSIOLOGY 40. What are the components of countercurrent system and the parts of the kidney associated with it? The components are: • Counter current multiplier system—Henlee's loop, medullary interstitium and collecting duct of kidney are associated with this system. • Counter current exchanger system—Vasa recta and medullary interstitium are associated with this system. 41. What do you mean by metabolic acidosis and alkalosis? Metabolic acidosis is defined as the fall of blood pH below the normal range due to excess CO2 produced in the body whereas metabolic alkalosis is referred to as the rise of blood pH above the normal value due to deficient formation of CO2 by the body. 42. What is the physiological and anatomical capacity of urinary bladder? • Anatomical—700 to 800 ml. • Physiological—250 to 450 ml. 43. What do you mean by cystometrogram? On the basis of which law it is plotted? Cystometrogram is the plot of intravesicular pressure against the volume of fluid in the urinary bladder as represented by Figure 1.7.1. It manifests Laplace's law. Fig. 1.7.1: Cystometrogram SECTION I : THEORY VIVA EXCRETORY SYSTEM 145 44. What is micturition waves? What is due to? In cystometrogram, superimposed on the tonic pressure changes during filling of urinary bladder, there are periodic acute rise in the pressure called micturition waves which lasts from few seconds to more than a minute. It is due to stretch reflex initiated by stretch receptors present in the urinary bladder and proximal urethra. 45. What is micturition reflex? When the pressure within urinary bladder is increased above 100 cm of H2O, a nervous reflex is initiated to void the urine or desire to urinate. This reflex is called as micturition reflex. 46. What is residual urine and retention of urine? In all types of urinary bladder dysfunction, bladder contracts but contractions are insufficient to empty the bladder completely, therefore some amount of urine is left in the urinary bladder called residual urine. During spinal shock, activity in detrusor muscle remains suspended for long period but activity in sphincter tone returns early. In this case then bladder responds purely and passively to distension with urine like an elastic bag resulting retention of urine. 47. What do you mean by retention with overflow? During spinal shock as a result of retention of urine, bladder becomes increasingly overstretched and sphincters are finally forced to open resulting escape of small amount of urine at frequent intervals. This is known as retention with overflow or passive incontinence or overflow incontinence. 48. What do you mean by 'Automatic bladder', 'Isolated bladder' and 'Spastic neurogenic bladder'? • In case of tabes dorsalis patients there may be failure of micturition at regular intervals causing accumulation of urine in urinary bladder resulting either precipitation of involuntary automatic evacuation of bladder or 146 VIVA IN MEDICAL PHYSIOLOGY • • dribbling of urine. In this situation bladder is known as automatic bladder. In case of denervation of both afferent and efferent nerves, the urinary bladder becomes flaccid and distended called as isolated or decentralised bladder. Repeated infection of urinary bladder causes hypertrophy of urinary bladder and micturition reflex becomes hyperactive resulting contraction of bladder at irregular intervals even along with small amounts of urine called as spastic (contracted) neurogenic bladder. SECTION I : THEORY VIVA SKIN AND BODY TEMPERATURE REGULATION 147 1.8 Skin and Body Temperature Regulation 1. Name the functions of skin. Skin has varried functions. The important functions are: Protection,Regulation of body temperature,Excretion, Synthetic function, Receptive function, Secretory function, Absorptive function, Water balance and Storage function (the dermis of the skin and subcutaneous tissue can store fats, water, salts and glucose). 2. Classify the sweat gland and differentiate it. Sweat glands are of two types: Eccrine and apocrine. Parameter Eccrine Apocrine i. Location Found in all over the body Found in axilla, mons pubis, scrotum, nipple, etc. ii. Type of secretion Clear, watery and thin Milky, opalescent and having characteristic smell on decomposition. iii. Stimulus Increase of body temperature Stress and sexual stimulation. 3. What do you mean by homiothermic and poikiothermic? Give examples of each. • The animals capable of maintaining constant body temperature inspite of wide variations in environmental temperature are known as homiothermic (warm blooded) animals, e.g. man, mammals, birds. 148 VIVA IN MEDICAL PHYSIOLOGY • Whereas the animals showing variation of body temperature in accordance with environmental temperature are called as poikiothermic or cold blooded animals e.g. reptiles, fish, amphibians, etc. 4. What is the normal body temperature in man? What do you mean by comfortable or neutral zone temperature? Normal BT of man is 98.4°F or 37°C. Comfort zone: It is the ambient temperature at which there is no active heat gain or heat loss mechanism operated by the body. It is 27 ± 2°C. 5. What is the normal skin and oral temperature? • Normal oral temperature: 36.3 -37.1°C (97°F - 98.8°F) • Normal skin temperature: 29.5°C-33.9°C (85°F-93°F) 6. What is basal temperature? Give the value of core temperature. What are the site for recording core temperature? Basal temperature is the body temperature recorded under complete physical and mental rest which is recorded generally in morning after awaking. Core temperature is 0.5°C to 1°C more than oral temperature, i.e. its value is 37.5°C to 38°C in an average. Site of recording of core temperature includes rectum, vagina, esophagus and tympanic membrane. 7. What will be the effect on body if core temperature is changed in following ways? • If it is decreased to 26°C or less—It will lead to death of that person due to cardiac failure. • If it is increased to 43.5°C or more—It will lead to death due to heat stroke. • If it is increased to 41°C for prolonged period—There will be irreversible brain damage. SECTION I : THEORY VIVA SKIN AND BODY TEMPERATURE REGULATION 149 8. Why regulation of body temperature is required? It has following reasons: • Speed of chemical reaction in the tissues varies with temperature. • Enzyme system of our body has got narrow range of optimum temperature at which it functions properly. Thus the normal body function depends on a relatively constant body temperature. 9. What is the average daily sweat secretion? It is about 1 lit/day. 10. What are the main functions of sweat? It helps to regulate body temperature, maintains water electrolyte and acid-base balance, helps to excrete some excretory products and also keeps the skin moist. 11. What do you mean by thermal sweating, nonthermal sweating, emotional sweating? • Thermal sweating: It occurs in response to rise of environmental or body temperature and mediated by eccrine sweat glands. • Non-thermal sweating: When sweating is stimulated by increased epinephrine level in the blood this type of sweating is called as non-thermal sweating. It is mainly mediated through apocrine type of gland. • Emotional sweating: This is the type of sweating which takes place during emotion controlled by premotor area of cerebral cortex. 12. How thermal sweating is controlled? It is by hypothalamus. 13. Name the main tissues where heat is produced in most. It is in liver and muscle. 14. Name the heat gain mechanisms. These are: shivering, increase in TSH and adrenaline secretion, continuous indirect vasoconstriction. 150 VIVA IN MEDICAL PHYSIOLOGY 15. What are the heat loss mechanisms? These are: by radiation from the body to cooler object, by conduction and convection to surroundings, by evaporation through sweating, by excreta in urine and faeces. 16. Name the main calorigenic hormones in the body. It is adrenaline and thyroxin. 17. How much is the approximate daily heat loss through various channels? Through skin-2200 cal.; through lungs-150 cal; through warming of air and food-100 cal; through urine and faeces-50 cal.; total = 2500 cal. 18. What is the role of brown fat in BT regulation? Brown fat which plays a role in BT regulation mainly in infants, is present between the scapula, at the nape of neck, along the great vessels in the thorax and abdomen. These fat cells contain mumerous mitochondria and thereby by increasing fatty acid oxidation it produces heat. 19. What do you mean by insensible perspiration?What is its role in BT regulation? Insensible perspiration is the passage of water by continuous diffusion through the epidermis which cannot be seen or felt. Its amount is 50 ml/hr. It helps in loosing the heat from the body by 30 Kcal/ hour. 20. Why one feels hotter in a humid day? In a humid weather, the heat loss by evaporation becomes difficult as rate of evaporation depends on relative humidity. As humidity is high, the rate of evaporation becomes low and thereby heat loss becomes less. 21. Name the heat gain and heat loss centre. Heat loss centre is posterior hypothalamus whereas heat gain center is anterior hypothalamus. SECTION I : THEORY VIVA SKIN AND BODY TEMPERATURE REGULATION 151 22. Can a person be made poikiothermic? Yes, Lesion in posterior hypothalamus causes body termperature to fall towards environmental temperature as both hot and cold regulating mechanisms are destroyed as anterior hypothalamic fiber passes via the posterior hypothalamus. 23. What is critical temperature? It is defined as the temperature at which a naked body needs the help of accessory chemical reactions to maintain the BT. 24. What is pyrexia and hyperpyrexia? Pyrexia is the state of the body when BT ranges from 37.2°C to 40.5°C (99°F to 105°F) where as hyperpyrexia is the state when BT rises above 40.5°C or 105°F. 25. What is hypothermia and deep hypothermia? Hypothermia is a state of body when BT falls to 30°C32°C whereas deep hypothermia is a state when BT falls below 25°C. 26. What do you mean by heat stroke, heat cramp and heat exhaustion? • Heat stroke: It is caused due to high environmental temperature, i.e. more than 41°C resulting impairment of body temperature regulating mechanism. • Heat exhaustion: It is caused by excessive sweating in response to heat which results loss of water, sodium chloride through sweat and thereby reduction of blood volume. • Heat cramps: Sometimes in people working in hot weather the muscles become hyperexcitable due to excessive loss of Na+ and Cl¯ from the body due to excessive sweating. This condition is called as heat cramps. 152 VIVA VOCE IN PHYSIOLOGY 1.9 Central Nervous System 1. What are neuroglia and its function? Neuroglia are the supporting cells in the nervous system of which star-shaped cells are called as astrocytes and cells with few processes are called as oligodendroglia and very small sized cells are termed as microglia. The main function of neuroglia is to provide support and protection of nervous tissues. In addition, they supply some nutrition to the nerve cells, neutralise the toxins and function as the RE system. 2. Classify motor neurons. It is of two types: i. α neurons: Innervate large skeletal muscle. ii. γ neurons: Innervate special skeletal small muscle fibers called intrafusal fibers. 3. What is synapse? A synapse is the junction between two neurons for the passage of the nerve impulse. 4. What do you mean by presynaptic, subsynaptic and postsynaptic membranes? Presynaptic: It is the membrane of neuron in close approximation with the membrane of postsynaptic cell in a synapse. Subsynaptic: Surface of the cell membrane involved in the synapse is called as the subsynaptic membrane. CENTRAL NERVOUS SYSTEM 153 SECTION I : THEORY VIVA Postsynaptic: The remainder of the motor neuron cell membrane is called as the postsynaptic membrane. 5. Distinguish between electrical and chemical synapses. Chemical Electrical 1. Impulse is transmitted from pre Impulse is transmitted through gap to post-synaptic site through junction. release of neurotransmitter i.e. chemical mediators. 2. Most of synapses are chemical Present only in specific synaptic type junction of brain. 3. Presence of synaptic cleft Cleft is replaced by low resistance bridges 4. Synaptic delay is present Absent 5. Sensitive to O2 lack Insensitive to O2 lack. 6. What is EPSP and IPSP? In response to binding of neurotransmitter on the receptor present in postsynaptic membrane there is opening of ligand gated Na+ channels. This results inward diffusion of Na+ causing alternation of membrane potential towards electro-positive.This non-propagative electrical potential which ultimately initiates action potential is called as excitatory postsynaptic potential or EPSP. Whereas when inhibitory neurotransmitters bind on the PSM there is opening of ligand gated K+ or Cl– channels resulting hyperpolarisation of PSM. This is known as IPSP. 7. Differentiate between EPSP and AP. EPSP AP 1. Stimulus intensity to generate EPSP has no threshold Has threshold level 2. Does not obey all or none law 3. Absence of refractory period Obeys all or none law Present 4. Summation can occur Never possible 5. Non-propagatory Propagatory. 154 VIVA VOCE IN PHYSIOLOGY 8. What are the properties of generator potential? The properties of GP are: (i) It is non-propagatory in nature (ii) It is monophasic (iii) It does not obey all or none law. 9. What do you mean by spatial and temporal summation? • Simultaneous stimulation of two afferent nerves by a stimulus of subthreshold intensity can evoke action potential in motor neuron. This property is known as spatial summation. • Whereas if subminimal stimuli are repeated at short intervals in a single nerve, reflex action can also be evoked which is known as temporal summation. 10. What is the fractionation phenomenon? Direct stimulation of motor nerve results more response than reflex response or in other words the tension developed reflexly is always a fraction of response that is produced by direct motor nerve stimulation. This is known as fractionation phenomenon. 11. What is after-discharge? Continuation of discharge of impulses from motor neuron even after withdrawal of stimulation from sensory side is called as after-discharge. 12. What do you mean by law of forward conduction? Synapse permits the conduction of impulse from presynaptic to postsynaptic neuron only, i.e. unidirectionally. This property is known as law of forward conduction.1 13. What is occlusion and subliminal fringe? When two afferent nerves to a skeletal muscle are simultaneously stimulated, it is sometimes seen that, the tension developed by the muscle under observation is less than the sum of the tension developed by each SECTION I : THEORY VIVA CENTRAL NERVOUS SYSTEM 155 afferent nerve stimulated separately due to the overlapping of afferent fibres in their central distribution. This property is known as occlusion. The opposite phenomenon is called as subliminal fringe. 14. What is synaptic plasticity? Synaptic transmission can be increased or decreased on the basis of past experience. This property is known as synaptic plasticity. 15. Why receptors are called as biotransducers? Receptor has got the capability to convert any form of energy (stimulus, i.e. touch, pressure, pain, temperature, etc.) to electrical energy (action potential). That is why it is known as biotransducer. 16. What do you mean by proprioceptive impulse? Which receptors are responsible for this? The impulses which are concerned with the activity of the body itself with regard to position and movements of different parts of the body are known as proprioceptive or kinaesthetic impulses. Receptors are muscle spindle, joint receptors, Golgi tendon organ and vestibular receptors. 17. Name the receptors responsible for following sensations—touch, pressure, hot, cold and pain. • Touch—Markel’s disc or Meissner’s corpuscle • Pressure—Pacinian corpuscle • Hot—Ruffini’s end organs • Cold—Krause’s end bulb • Pain—Free nerve endings. 18. Classify the receptors. Receptors are generally classified into two types: 1. Exteroceptors—This gives response to stimuli arising from outside the body. These are further subdivided into 3 groups: • Cutaneous—These are mechanoreceptors present in the skin and are of 4 types as per the nature of stimulus. 156 VIVA VOCE IN PHYSIOLOGY • Touch receptors—like Meissner’s corpuscle and Merkel’s disc. • Pressure receptors—like Pacinian corpuscle. • Thermo receptors—like Krause’s end bulb for cold and Ruffini’s end organ or warm temperature. • Pain receptors—like free nerve endings. • Chemoreceptors—These give response to chemical stimuli. Examples: Taste buds for taste sensation and olfactory cells for smell sensation. • Telereceptors—These are stimulated in response to the stimuli arising away from the body like Hair cells of Organ of Corti for hearing and rods and cones in retina for vision. 2. Interoceptors—These give response to stimuli arising within the body. These are of two types: • Viscero receptors—present in viscera and are stimulated either-by stretch (stretch receptor) or pressure (baroreceptor), or chemicals (chemoreceptor) or osmolarity of body fluid (osmo receptors). • Proprioceptors: These are stimulated in response to the change in position of different body parts. These include receptor in labyrinth apparatus and muscle spindle, golgi tendon, pacinian corpuscle, etc. in muscle, ligament, joint, tendon, etc. 19. What do you mean by law of adequate stimulus? Each type of receptor gives maximum response to a particular or specific stimulus. However it can give incomplete response to other type of stimulus provided the intensity of stimulus is higher. For example, warm water stimulates Ruffini’s receptor at lower intensity of stimulus producing a specific response though it also stimulates the free nerve endings of pain at high intensity of stimulus and this response is incomplete. This property of the receptor is known as Law of Adequate Stimulus or Specificity of Response. SECTION I : THEORY VIVA CENTRAL NERVOUS SYSTEM 157 20. What is Weber Fechner law? The frequency of action potential in a sensory nerve is directly proportional to the magnitude of generator potential which inturn is directly proportional to the intensity of stimulus. This relationship betwen intensity of stimulus, magnitude of GP and frequency of AP in the afferent nerve is known as Weber Fechner law. 21. What do you mean by tonic and phasic type of receptors? • Tonic receptors are poor, slow and incompletely adapting receptors, i.e. they can be stimulated continuously for many hours even if the intensity of stimulus remains absolutely constant over many days, e.g. muscle spindle, pain receptor, baro and chemoreceptor for BP. • Phasic receptors are rapidly adapting receptors and transmit signals only when the stimulus strength is changed and thus the generator potential in them is short and decays rapidly, e.g. touch, olfactory, pressure receptors. 22. What is Muller’s doctrine of specific nerve energy? Sensation produced by impulses generated in a receptor depends on the specific part of brain, i.e. the specific pathways for specific sensation are separated from nerve organ to cerebral cortex. This is known as Muller’s law. 23. What do you mean by law of projection? What is phantom limb? No matter where a particular sensory pathways is stimulated along its course to the cortex, the conscious sensation produced is referred to the location of the receptor. This principle is called as law of projection. A limb that has been lost by accident or amputation, the patient usually experiences intolerable pain and proprioceptive sensations in the absent limb and is called as phantom limb. 158 VIVA VOCE IN PHYSIOLOGY 24. What do you mean by law of intensity discrimination? The brain interpretes different intensities of sensations by variating the frequency of AP generated by receptor and/or by variating the number of receptors activated or both. This is known as law of intensity discrimination. 25. How it is possible to tell whether the pain is mild or mederate or severe? The information about the intensity of stimulus is perceived by the sensory cortex through two mechanisms as follows: • By variating the frequency of the action potential generated by the given receptor in response to a stimulus. • By altering the number of receptors involvement to transmit the impulse i.e. the more the strength of stimulus, the more the number of receptors activated (Recruitment of sensory units). This property explains how it is possible to tell whether the pain is mild, moderate or severe; touch is crude or fine. 26. Name the reflexes which are of mainly clinical importance. Tendon reflex and pupillary light reflex. 27. Enumerate the characteristics of a reflex arch. Excitibility, summation, delay, refractory period, fatigue, facilitation, irradiation, fractionation, subliminal fringe, occlusion, etc. 28. What is positive Babinski’s sign? If plantar side of foot is scratched it normally causes dorsiflexion of toes. In lesion of pyramidal tract, the response is extension along with fanning of toes. This is termed as postive Babinski’s sign which is also normally seen in infants. SECTION I : THEORY VIVA CENTRAL NERVOUS SYSTEM 159 29. Name the components of reflex arch. Receptor, afferent nerve, centre, efferent nerve and effector. 30. What is Bell–Magendie law? In the spinal cord, the dorsal roots are sensory in nature whereas the ventral roots are motor. This principle is known as Bell-Magendie law. 31. Classify reflex with example depending on number of synapse. • Monosynaptic, e.g. bicep, tricep and knee jerk. • Polysynaptic, e.g. withdrawal reflex, pupilary reflex. 32. Differentiate intrafusal and extrafusal fibers? Each muscle spindle contains 2-12 muscle fibers enclosed in a connective tissue capsule called as the intrafusal fibers whereas the regular contractile units of muscle are extrafusal muscle fibers. 33. What are nuclear bag and nuclear chain fibers? Intrafusal muscle fibers are of two types. In one type many nuclei are present in a centrally dilated area called as nuclear bag fiber whereas in other type a single line of nuclei are present lying in a chain and fibers are shorter and thinner than 1st type which are known as nuclear chain fibers. 34. What do you mean by static and dynamic response in relation to stretch reflex? The nerve endings in the nuclear bag fibers discharge most rapidly when the muscle is being stretched and less rapidly during sustained (continual) stretch. This is called as dynamic response. Whereas the afferent nerve endings in the nuclear chain fibers discharge at an increased rate throughout the period of sustained stretch only called as static response. 160 VIVA VOCE IN PHYSIOLOGY 35. What do you mean α−γ linkage? For the maintenance of muscle tone, the impulses from the γ motor neuron causes contraction of end portion of intrafusal fibers resulting stretching of muscle spindle. This leads to the discharge of impulses from the primary sensory nerve endings. These impulses stimulate the a motor neurons of spinal cord which in turn send impulses to extra-fusal fibers and cause contraction of extrafusal muscle. This is known as α−γ linkage. 36. What is reciprocal inhibition? When a stretch reflex is induced, activity of afferent fibers from muscle spindle excites the motor neurons supplying the muscle from which the impulses come and inhibits those supplying its antagonist muscle. This phenomenon is called as reciprocal inhibition. 37. What is inverse stretch reflex? If muscle spindle is stretched by noxious stimulus (strong, intense stretching) instead of contraction of the muscle there will be relaxation of the concerned muscle. This type of reflex is called as inverse stretch reflex. 38. Compare monosynaptic and polysynaptic reflex. Parameter Monosynaptic Polysynaptic 1. No of synapse Only one Many 2. Latent period Shorter Comparatively longer 3. Important feature Do not have phenomenon of after-discharge Present 4. Example Stretch reflex Withdrawal and superficial reflex. 39. What are the effects of sectioning of posterior nerve root? There is loss of all forms of sensations, muscle tone, superficial and deep reflexes and visual sensibility. SECTION I : THEORY VIVA CENTRAL NERVOUS SYSTEM 161 40. What are the effects of section of anterior nerve root? These are—complete paralysis of muscle with loss of voluntary and sensory movements, loss of reflexes and vasomotor paralysis with muscle atrophy, sympathetic system paralysis. 41. What is the cause of spinal shock? Immediately after the spinal transection there is a state of depression for some short period called as spinal shock. It is due to release phenomenon which is set up owing to cessation of impulses from higher levels, which normally produce facilitating effect. 42. What are the symptoms of spinal shock? • Many reflexes are lost causing flaccidity of limb muscle. • Muscle tone is completely lost. • BP is lowered. • Retention of urine in bladder. • Penis is flaccid and erection is impossible. 43. What do you mean by paraplegia and quadriplegia? In case of complete spinal transection, if both the lower limbs get paralysed the condition is called as paraplegia and if all 4 limbs are paralysed it is called as quadriplegia. 44. What are the effects of complete spinal transection in man? The effects are divided in 3 stages: • Stage of shock—Immediately there is loss of all movements and sensation below the level of lesion. BP becomes low and rectal and urinary bladder sphincters are contracted. • Stage of reflex activity—After 2-3 weeks some reflex activity is regained that results the movement of locomotion to some extent though walking without support is impossible, BP becomes normal, sphincters become less tonic allowing passing of urine and stool. There is also preponderance of flexor muscles over extensors so that there is semiflexion of lower limbs. 162 VIVA VOCE IN PHYSIOLOGY • Stage of failure of reflex activity—Reflexes disappear again and muscles are wasted if the patients of spinal transection suffer from general infection or toxaemia. 45. What do you mean by hemisection of spinal cord? What is Brown-Sequard syndrome? Lesion of one lateral half of spinal cord is known as hemisection. Brown-Sequard syndrome states that—below the level of lesion in spinal cord on the same side there is extensive loss of motor activity but little sensory loss, whereas on the opposite side there is extensive sensory loss but little motor loss. 46. What do you mean by decerebrate preparation? Decerebrate preparation means sectioning at midbrain level so that body function is controlled by spinal cord, medulla, pons and cerebellum without having any influences from midbrain and structure above the midbrain. 47. What are the symptoms of decerebrated animals? • High arterial pressure with intact cardiac and respiratory reflexes. • Respiration continues and swallowing and vomiting can take place. • Temperature regulation and righting reflexes are lost. • Extensor reflexes are exaggerated resulting rigidity of limbs called as decerebrate rigidity. 48. What is decorticate preparation? Removal of entire cerebral cortex is known as decorticate preparation. 49. What is syringomyelia? This is a condition involving the gray matter around the central canal of spinal cord in which excessive growth of neuroglial tissue occurs with cavity formation. It first affects the posterior horn of lower cervical and upper CENTRAL NERVOUS SYSTEM 163 SECTION I : THEORY VIVA thoracic regions. There is sensory loss with muscular weakness and if progressed there is also loss of pain sensation with trophic ulcers, injuries and vasomotor disturbances. 50. What is dissociated anaesthesia? In case of syringomyelia there is loss of pain and temperature sensation whereas sense of touch is unaffected. This conditon is known as dissociated anaesthesia. 51. What is tabes dorsalis? Degenaration of dorsal (sensory) roots specially in dorsal column and fibers which carry pain sensation is known as tabes dorsalis. Usually it is caused by syphilis. 52. Which sensations are carried by these nerves? Fasciculus gracilis and Fasciculus cuneatus Fine touch, tactile localisation, kinesthetic movements, vibration, deep pressure. Lateral spinothalamic Pain and temperature. Ventral spinothalamic Crude touch. 53. Differentiate superficial and deep pain. Parameter Superficial Deep Location Skin and subcutaneous tissue Muscles and holow viscera Nature Sharp and well localised Dull and poorly localised Function Leads to reflex withdrawal movements, increase in HR, BP and respiration. Produces faintness, nausea, vomiting, sweating, fall in BP. 164 VIVA VOCE IN PHYSIOLOGY 54. Distinguish between Aδ δ and C fibers. Aδ fibers C fibers 1. Small myelinated, 2-5 µm diameter, 12-30 mm/sec. conduction velocity. Nonmyelinated, 0.4-1.2 µm diametar with conduction volocity 0.5-2 mm/sec 2. Less in number Relatively more 3. Conduct impulse only to noxious stimulus. In response to thermal and mechanical stimulus. 4. Sensitive to electrical stimulus. Less sensitivity 5. Most sensitive to pressure Most sensitive to local anaesthetics and chemical factors. 55. What do you mean by fast and slow pain? Fast pain is due to activation of Aδ nerve fibers and are bright, sharp and well localised where as slow pain is due to activation of C group of nerve fibers and causes a dull, intense, diffuse and unpleasant feeling of pain. 56. What is Lewis-P factor? Muscle activity releases group of substances like K+, adenine nucleotides, lactic acid, PG, etc. which produces pain and are collectively termed as Lewis-P factor. 57. What is referred pain? The sensation of pain if experienced at the site of other than the injured or diseased part is known as referred pain, e.g. • During heart attack pain is often experienced in the inner aspect of left arm and left shoulder instead of heart. • Stone in gallbladder referred to the tip of the shoulder. • Pain in testicles due to stone in the uretor. 58. Which sensations are carried by Dorsal Column Medial Lemniscus system? This system carries the sensation like fine touch, two point discrimination, vibration sense, sense of position. SECTION I : THEORY VIVA CENTRAL NERVOUS SYSTEM 165 59. Which sensations are carried by anterolateral pathway? This system carries crude touch, temperature and pain sensation. 60. Enumerate the types of lemniscus. It is of 4 types: • Spinal lemniscus: Formed by STT in medulla oblangata. • Lateral lemniscus: Formed by fibers carrying sensations of hearing from cochlear nuclei to inferior colliculus and medial geniculate body. • Medial lemniscus: Formed by fibers arising from N. gracilis and N. cuneatus of medula. • Trigeminal Lemniscus: Formed by fibers from sensory nuclei of trigeminal nerve which carries general sensation from head, neck, eyeball, face, mouth, ears. 61. Name the sensory tracts (ascending tracts) passing through dorsal white column of spinal cord. Tracts in dorsal (Posterior) white column • Fasciculus Gracilis (Tract of Goll) • Fasciculus cuneatus (Tract of Burdach). 62. Name the sensory tracts passing through lateral white column of spinal cord. Tracts in lateral white column. • Lateral spinothalamic tract—carries pain and temperature sensation • Ventral spinocerebellar tract—carries sub conscious kinaesthetic impulses • Dorsal spinocerebellar tract—carries nonsensory impulse, i.e. subconscious kinesthetic sensation. • Spinotectal tract—for spinovisual reflex • Spinoreticular tract—for consciousness • Spinoolivary tract—proprioceptive impulse. 63. Name the sensory tracts passing through ventral white column of spinal cord. Tracts in ventral white column: 166 VIVA VOCE IN PHYSIOLOGY Ventral spinothalamic tract—carries crude touch sensation. 64. What is Dermatomal rule? Pain is usually referred to a structure that develops from the same segment during the embryonic development. This principle is known as dermatomal rule. 65. What do you mean by upper motor neurons and lower motor neurons? The pyramidal cells and there tracts constitute the upper motor neurons whereas the spinal and cranial motor neurons which directly innervate the muscles are collectively called as lower motor neurons. 66. Why pyramidal tracts are so named? For two reasons as follows: • They are originated from pyramidal cells of cerebral cortex. • They pass through medulla in the form of pyramid. 67. What do you mean by hemiplegia? The condition characterised by the weakness or paralysis on the opposite site of the body due to injury to the pyramidal tracts in the brain (common lesion site is internal capsule) is known as hemiplegia. 68. What are the main differences between upper and lower motor neuron lesion? LMNL UMNL a. Single individual muscle is affected Group of muscles are affected. b. Flaccid type of muscle paralysis due to hypotonia Spastic type of muscle paralysis due to hypertonia c. Disuse atropy of muscle takes place Not severe Contd... SECTION I : THEORY VIVA CENTRAL NERVOUS SYSTEM 167 Contd... d. All reflexes are absent as motor pathway is damaged. Deep reflexes are hyperactive due increased γ motor activity and some superficial reflexes like abdominal, cremastric reflexes are lost. e. Babinski’s sign is negative It is positive. 69. What are hypertonia, hypotonia, spasticity and rigidity? What are their causes? • Hypertonia: It is a state of increase muscle tone in the body. It occurs in lesion of UMN and extrapyramidal lesions. • Hypotonia: It is a state of decrease tone of muscle. It is due to lesion of lower motor neuron (corticospinal) and cerebellar lesions. • Spasticity: It is the state of hypertonia resulting from lesion of corticospinal system. • Rigidity: It is the state of rigidity results from basal ganglion disease and is also called as extrapyramidal rigidity. 70. What do you mean by epicretic and protopathic sensations? Epicretic: • Mild or light sensations like fine touch, tactile localisation, tactile discrimination temperature range of 25-40oC, etc. are known as epicretic sensation. • These sensations are perceived accurately. Protopathic sensations: • Crude sensations like pressure, pain and temperature range above 40oC and below 25oC. 71. Which part of spinal cord contains cell body of nerve fiber and which part contains axons of nerve fiber? Gray matter contains cell bodies and white matter contains axons of nerve fiber. 168 VIVA VOCE IN PHYSIOLOGY 72. What do you mean by Charcot’s joint? Swollen painless knee joint in Tabes dorsalis patient is known as Charcot’s joint. 73. Name the descending tracts and give an account of each of their function. Descending tracts of the spinal cord are formed by motor fibers originating from brain. These are of 2 types: A. Pyramidal tracts—Directly from motor cortex to spinal motor neurons B. Extrapyramidal tracts—From motor cortex to spinal motor neurons via subcortical nuclei. A. Pyramidal tracts: Examples: (i) Corticospinal tract—Motor fibers of cerebral cortex to ventral horn cell of spinal cord constitute corticospinal tract. It is of again 2 types: • Lateral corticospinal or crossed/indirect pyramidal tract • Anterior corticospinal or uncrossed/direct pyramidal tract. (ii) Corticobulbar tract—Motor fiber's originating from cerebral cortex, when terminate in brainstem structure is known as corticobulbar tract. B. Extrapyramidal tracts: • Rubrospinal tract • Reticulospinal tract • Vestibulospinal tract • Tectospinal tract • Olivospinal tract. 74. What are the chemical transmitters at autonomic nervous systems? • In both sympathetic and parasympathetic preganglionic neurons, neurotransmitter is ACh. • In sympathetic post-ganglionic neurons, neurotransmitter is norepinephrine. SECTION I : THEORY VIVA • CENTRAL NERVOUS SYSTEM 169 In parasympathetic post-ganglionic neurons neurotransmitter is ACh mainly. 75. What are the main levels of integration for following functions? Control of spinal reflex—spinal cord. Regulation of heart rate, respiration rate and antigravity reflexes—medulla Regulation of righting reflex—midbrain Regulation of locomotor reflex—midbrain and thalamus. Emotional function—hypothalamus and limbic system. Initiation of voluntary movements, memory, emotion, conditioned reflex—cerebral cortex. 76. What do you mean by righting reflex? It is a chain of reaction following one another in an orderly sequence to maintain normal standing position and keep the head upright. 77. What is decerebrate rigidity and what is its relation to γ rigidity? Transection of the midbrain in between superior and inferior colliculi in animals results increased muscle tone in extensor group of muscles called decerebrate rigidity. This type of rigidity occurs due to increase of γ motor discharge because of withdrawal of inhibitory extrapyramidal discharge. Besides this, there is also facilitatory discharge from descending facilitatory reticular projection to γ motor neuron. This is why this type of rigidity is called as γ rigidity. 78. What do you mean by reticular formation? It is those parts of the brainstem (medulla, pons and mid-brain) which are characterised by an interlacing network of fiber bundles. It is composed of more than 50 nuclear masses which together constitute the reticular formation. 170 VIVA VOCE IN PHYSIOLOGY 79. Why reticular formation is absolutely essential for life? The reasons are as follows: • Some RF neurons act as an integration center of some important physiological function, e.g. cardiovascular and respiratory function, swallowing, etc. • It receives and integrates information from all regions in the CNS. 80. How does cerebellum is connected with brainstem? By means of 3 peduncles as follows: • To the medulla by inferior cerebellar peduncle. • To the pons by middle cerebellar peduncle. • To the midbrain by superior cerebellar penduncle. 81. What do you mean by climbing fiber and mossy fiber? Both are the afferent fibers of cerebellar cortex. Climbing fibers originate from cells in inferior olivary nucleus and establish one to one connection with Purkinje cells to excite it. It also gives some collaterals to Golgi cells to excite it whereas, mossy fibers are axon of spinocerebellar vestibulo-cerebellar, reticulo-cortico-ponto-cerebellar tracts and connected with many granule cells in a series of moss-like glomeruli. 82. Give a account of nerve fibers present in white matter of cerebral cortex. White matter consists of mainly myelinated fibers arising from the cells of gray matter and coming from other areas of CNS. There are 3 types of fibers forming white matter: • Association fiber—Connects the neurons of different parts of cerebrum of same side. • Commissural fiber—Connects corresponding areas of cerebral hemsiphere of two sides, e.g: Corpus callosum. • Projection fiber—Connects cerebral cortex with brainstem structures and spinal cord. SECTION I : THEORY VIVA CENTRAL NERVOUS SYSTEM 171 83. What do you mean by Frontal lobe syndrome? Injury or ablation of frontal lobe results frontal lobe syndrome which has following symptoms: • Lack of concentration and lack of fixing attention. • Person loses the ability to solve problem • Lack of initiation and difficulty in planning. • Emotional instability • Loss of moral and social sense • Loss of recent memory • Hyperphagia, slight tremor, etc. 84. What do you mean by adiadochokinesis? Due to cerebellar lesion, patient is unable to carry out alternate and opposite movements rapidly. This is known as adiadochokinesis. 85. What are the voluntary disturbances of cerebellar lesion? • Asthenia, i.e. feeble movement. • Ataxia, i.e. inco-ordination of movement. • Asynergia, i.e. lack of co-ordination between protogonists, antagonists and synergists muscle. • Dysmetria, i.e.the movement is poorly carried out in direction, range and force. • Intention tremor • Drunken gait • Slow and lalling (like a baby) speech. 86. What is Charcot’s triad? It is a syndrome characterised by nystagmus, intention tremor and lalling speech due to disturbances of cerebellar connection with brainstem which generaly occurs during disseminated sclerosis. 87. Name two cerebellar function tests. These are finger nose test, walking along a straight line, testing of muscle tone. 88. What is metathalamus and epithalamus? Medial and lateral geniculate bodies are collectively known 172 VIVA VOCE IN PHYSIOLOGY as metathalamus and the part of thalamus which is connected with olfactory system like pineal body and Hebenular complex is called as epithalamus. 89. What are the main waves of EEG and their characteristic features? Mainly four waves α, β, θ and δ. • α wave: Moderate frequency with high amplitude obtained in inattentive brain or drowsiness or light sleep with closed eyes only. • β wave: High frequency with low amplitude wave obtained during mental activity or arousal state. • θ wave: Low frequency and low amplitude wave generally obtained in children of below 5 years old. • δ wave: Low frequency with high amplitude (voltage) wave commonly occurs in early childhood during waking hours and mainly adults during deep sleep. 90. What is Kluver Bucy Syndrome? It is due to bilateral destruction of temporal lobe (in animal) along with amygdaloid nucleus and uncus (in human) which is charecterised by-Speech disturbances (Aphasia), Auditory disturbances, Disturbances in smell and taste, Dreamy state and Visual hallucination. 91. What is Papez circuit? What is it’s importance? Prefrontal lobe forms a closed circuit connecting with thalamus, hypothalmus and hippocampus called as Papez circuit which is responsible for resting EEG, genesis and control of emotion and memory. 92. What is Thalamic syndrome? What do you mean by thalamic phantom limb? Thalamic lesion leads Thalamic syndrome. Causes: Mostly due to blockade of one of the arteries supplying thalamus. Symptoms/Features: • Thalamic pain—spontaneous and often excessive pain on opposite side of the body which may be aroused by simply light touch or by cold. SECTION I : THEORY VIVA • • • • • • CENTRAL NERVOUS SYSTEM 173 Loss of all sensations. Asteriognosis—inability to recognise a known object by handling with closed eyes. Ataxia—in co-ordination of voluntary movement due to loss of kinesthetic sensation. Thalamic phantom limb—inability to locate the position of limb with closed eyes Thalamic hand—in some patients the contralateral hand is held in an abnormal posture, i.e. moderate flexion at wrist joint with hyperextension of all fingers. Abnormal involuntary motor movements like: – Chorea, i.e. quick jerky movements – Intention tremor – Athetosis, i.e. slow writhing and twisting movements 93. Give an account of hyperkinetic syndrome of basal ganglia. Hyperkinetic syndrome may be due to: • Lesion of Caudate N and Putamen: It is characterised by purposeless involuntary jerky movements which do not follow definite pattern known as Chorea. • Lesion of Globus Pallidus: It is characterised by slow confluent writhing or worm like movement called Atheosis. 94. What is parkinsonism? Lesion of Substantia Nigra results Parkinsonism. Cause: Decrease secretion of dopamine which results abnormal excitation of basal ganglia. Physiological basis: Dopamine secreted in caudate nucleus and putamen by substantia nigra is inhibitory. Therefore, destruction of substantia nigra causes withdrawal of inhibition of these structures which in turn become overactive and cause continuous output of excitatory signal to the corticospinal motor system. 174 VIVA VOCE IN PHYSIOLOGY Features: • Lead pipe or Cogwheel rigidity—due to increase in muscle tone. • Static tremors—Tremor at rest and disappears during voluntary activity due to oscillatory continuous discharge of pyramidal system by a closed circuit through basal ganglia. • Akinesis—It is difficulty in initiation or starting movement due to rigidity of the muscles so the automatic associated movements do not occur resulting: • Mask like face (no facial expression) • Statue like posture. • Festinant Gait—The person walks with short quick steps with the body bent forwards as if the person is trying to prevent himself from falling. 95. Differentiate REM and NREM sleep. Slow wave sleep or orthodox or Non rapid eye movement (NREM) sleep: • It occupies 70% of sleep period. • Lasts for every 70-90 min and interrupted by 10-20 mins of REM sleep. • Produced by absence of desynchronising activity via RAS. • EEG shows slow, synchronised theta and delta waves. Rapid eye movement (REM) or paradoxical or fast wave or dream sleep: • Rapid to and fro movement of eye ball occurs. • HR and respiratory rate becomes irregular. • Occasional muscle twitch can take place. • Difficult to wake an individual if he is in this phase of sleep. • Dreams are more vivid. • Shows fast desynchronised waves. 96. Enumerate the site of memory storage. It is randomly stored in the brain. However important sites SECTION I : THEORY VIVA CENTRAL NERVOUS SYSTEM 175 are-Hippocampus of limbic system and Wernick’s area of cerebral cortex. 97. What do you mean by amnesia, retrograde amnesia and anterograde amnesia? • Amnesia : It is defined as the inability to recall the memories of recent events. • Retrograde amnesia : It is inability to recall memories from the distant past. • Anterograde amnesia : It is the inability of the person to establish new long-term memories of those types of information that are basis of intelligence. It occurs due to lesion in hippocampus. 98. What is pure motor apnasia? Loss of articular speech without mental confusion is pure motor apnasia. 99. What is pure word blindness? Inability to recognise meaning of written or printed words is known as pure word blindness. In this case patient is unable to read. 100. What is agrolphia? It is the inability to write. 101. What is pure word deafness? It is failure to recognise spoken speech with no other defect of speech or intelligence. 102. What is dysarthria? Speech disturbance due to defects in excitomotor areas in cortex, pyramidal tract, cranial nuclei, etc. is known as dysarthria. 103. What is Wernicke’s area, Dejerine area and sensory speech center? • Wernicke’s area is auditory speech center located in the region at the posterior end of the superior temporal gyrus in the dominant hemisphere and is concerned with comprehension, i.e. interpretation and understanding of auditory information. 176 VIVA VOCE IN PHYSIOLOGY • Dejerine area is visual speech center located in the angular gyrus behind Wernicke’s area. These two areas are collectively known as Sensory speech area. 104. What are the motor speech areas? It includes Broca’s area (area 44) and Exner’s area (motor writing center). Broca’s area is located in the inferior frontal gyrus in the region of the anterior and ascending rami of the lateral sulcus in the dominant hemisphere whereas Exner’s area is located in the middle frontal gyrus in the dominant hemisphere. 105. Enumerate the origin of sympathetic and parasympathetic nervous system? Origin of sympathetic: Lateral gray horn of thoracic and lumber (T1- L2) segments of spinal cord. Origin of parasympathetic: Cranio-sacral • Cranial: - Oculomotor (IIIrd nerve) from midbrain (Tectum) level. - Facial (VII nerve), glossopharyngeal (IX nerve) and vagus (Xth nerve) from bulbar level of brain. • Sacral: 2nd to 4th sacral segments of spinal cord. 106. Enumerate the spinal and cranial nerves. i. ii. iii. iv. v. Spinal nerves Cranial nerves 8 pairs of cervical (C8) 12 pairs of thoracic (T12) 5 pairs of lumbar (L5) 5 pairs of sacral (S5) 1 pair of coccygeal (Cg1) i. ii. iii. iv. v. vi. vii. viii. ix. x. xi. xii. Olfactory (Afferent) Optic (Afferent) Oculomotor (mixed) Trochlear (mixed) Trigeminal (mixed) Abducens (mixed) Facial (mixed) Vestibulo-cochlear (Afferent) Glossopharyngeal (mixed) Vagus (mixed) Spinal Accessory (efferent) Hypoglossal (efferent) SECTION I : THEORY VIVA CENTRAL NERVOUS SYSTEM 177 107. What is BBB? What are its importance? The entry of some substances from the blood to the brain ECF is restricted due to barrier offered by the walls of the capillaries supplying the brain. This barrier is known as Blood-Brain Barrier (BBB). 108. How can you collect CSF? If required CSF can be collected by lumbar puncture technique. In this technique a needle is inserted in between 3rd and 4th lumbar spinous processes into the subarachnoid space within the vertebral canal and CSF is sucked-outside. In this process there is no risk of damaging the spinal cord as it ends at the level of first lumbar vertebra. 109. What is the average volume and pressure of CSF? Volume—100-110 ml Pressure—100-110 mm of water. 110. What is normal glucose level in CSF? 50-70 mg%. 111. What is the normal cerebral blood flow? 750 ml/min. 178 VIVA IN MEDICAL PHYSIOLOGY 1.10 Special Senses 1. Name the layers of the eyes? • Sclera (outer fibrous protective layer). • Choroid (middle vascular layer). • Retina (inner nervous layer). 2. Colour of the eye is colour of what structure of eye? What is the function of the pigment present in it? It is iris and pigmented layer of iris absorbs the extra amount of light. 3. What is blind spot and yellow spot? The small area of retina where optic nerve leaves the eye is called as optic disc. It does not contain any light sensitive photoreceptor and that is why vision is not possible over this area. This spot is called as blind spot. At the posterior pole of the eye there is yellowish pigmented spot which marks the location of fovea centralis where rods are not present, only cones are densely packed. This spot is called as yellow spot or macula lutea which is also the point of greatest visual acuity. 4. Name the refractive media of the eye? They are cornea, aqueous humour, lens, vitreous humour. 5. What is the function of iris in the eye? It restricts the peripheral light rays and also prevents spherical abberations. It also controls the intensity of light falling on the eye. SECTION I : THEORY VIVA SPECIAL SENSES 179 6. What are the functions of lacrimal gland secretion? These are: It lubricates the conjunctiva, its lysozymes have bacteriocidal action, helps to remove the foreign body from the eye through overflow. 7. How is aqueous humour formed? It is formed by ciliary body and anterior surface of iris by dialysis of crystaloids. 8. What are the functions of aqueous humour? • It maintains normal intraocular pressure required for normal refraction. • It provides nutritions to the cornea and lens. 9. What is the function of vitreous humour and where does it present? • It prevents the walls of eyeball from collapse. • It also maintains intraocular pressure. It is present in the interior of the eyeball between the lens and the retina. 10. Where does aqueous humour present? It is present in the anterior and posterior chamber of the eye. 11. What is the physiological and clinical importance of Canal of Schlemm? Aqueous humour once formed from the ciliary process passes from the posterior chamber then via pupil enters into anterior chamber which then passes into the intrascleral venous plexus through canal of Schlemm, thereby this canal helps to drainage the aqueous humour continuously secreting from cilliary body. Blockade of the canal of Schlemm leads to increase intraocular pressure above 80 mm Hg resulting pain and degeneration of blood vessels of retina and choroid. This condition is known as glaucoma. 180 VIVA IN MEDICAL PHYSIOLOGY 12. Define the term anopia, homonymous hemianopia, heteronymous hemianopia, scotoma. • Anopia—It is the complete loss of visual field in an eye (Fig. 1.10.1A) • Hemianopia—Refers to the blindness of half of the visual field (Fig. 1.10.1B) • Homonymous hemianopia—It refers to the loss of field of vision of same halves in two eyes (Fig. 1.10.1B) • Heteronymous hemianopia—When different halves of field of vision in two eye are lost (Fig. 1.10.1C). Figs 1.10.1A to C: Types of hemianopia • Scotoma—Loss of vision in an eye which is confined to the center of the visual field. SECTION I : THEORY VIVA SPECIAL SENSES 181 13. What type of anopia you will see in case of lesion of following structure? a. Optic nerve—complete anopia b. Optic chiasma—heteronymous hemianopia c. Optic tract—homonymous hemianopia d. Lateral geniculate body—homonymous hemianopia e. Occipital cortex—quadrantanopia f. Area 18/19—visual agnosia. 14. What is Wernicke pupillary reflex? In case of partial damage of light reflex fibers, when light is focused on the blind part of retina light reflex is lost and if light is focused on the sound retinal part light reflex persists. This reflex is known as Wernicke pupillary reflex. 15. What do you mean by macular sparing? In case of occipital cortex lesion, oftenly there is a loss of peripheral vision with normal and complete macular vision called as macular sparing. 16. Define visual acuity. It is the shortest distance by which two lines can be separated by the eyes. It is expressed in visual angle. 17. What do you mean by direct and indirect reflex? Focusing of light in one eye leads to constriction of the pupil of that particular eye which is known as direct light reflex and the same event also results constriction of pupil of other eye which is known as indirect or consensual light reflex. 18. Define accommodation. It is the ability of the eye to focus an object at varying distances by changing the curvature of anterior surface of the lens. 19. What is accommodation reflex or near response? When an individual looks at near object to focus the image of an object properly, three events take place— contraction of ciliary muscles, constrictions of pupils and 182 VIVA IN MEDICAL PHYSIOLOGY convergence of visual axis. This reflex is known as accommodation reflex. 20. What is the range of accommodation? • Near point is 9-10 cm at age of 10 years. • Far point is 6 meter from the eye. 21. What is the amplitude of accommodation? It is 14 diopters. 22. What is Argyll Robertson pupil and reverse Argyll Robertson pupil? In case of lesion in aqueduct and superior colliculi, there is a loss of light reflex keeping the convergence accommodation reflex intact. This type of pupil is referred to as Argyll Robertson pupil. Where as due to the lesion in frontal lobe (bilaterally) or damage of its descending fibers to III nerve nucleus pupillary constriction in response to light is present but accommodation is lost. This is known as reverse Argyll Robertson pupil. 23. What do you mean by spherical and chromatic aberration? • Spherical aberration is due to difference in refractive indices of central and peripheral parts of the lens and usually reduced with the help of iris. • Chromatic aberration is due to different wave lengths of coloured rays. 24. What is presbyopia? Decreased ability of the eye to accommodate due to aging is called as presbyopia. 25. What is cataract? UV irradiation results agglutination of iris protein and its coagulation in the presence of Ca+2 making the lens hard, opaque and swollen which is called as cataract. 26. What is emmetropia? It is the normal refractory function of the eyes. SECTION I : THEORY VIVA SPECIAL SENSES 183 27. What is aetropia? It is the deviation from normal refractory state of the eyes. 28. What is myopia, hypermetropia and astigmatism? How these are corrected? • Myopia—It is the condition in which distant objects are not seen clearly as parallel rays of light from distant objects are focused in front of retina either due to increase length of eye ball or increase refractory power of lens. It can be corrected by concave lens. • Hypermetropia—It is the condition in which near objects are not seen clearly as parallel light rays from objects are focused behind the retina due to shortening of eyeball or diminishing of refractive power of lens. It is corrected with the help of convex lens. • Astigmatism—It is an error of vision in which the light rays are not brought to a point focus on the retina resulting blurring of vision. It is corrected with cylindrical lens placed in such a way so that the refraction from all the meridians become equal. 29. What is photopic, scotopic and mesopic vision? • Photopic—It is daylight vision due to cone receptor. • Scotopic—It is dim light vision and a function of rods. • Mesopic—It is a full moon night vision where reading becomes difficult. 30. What do you mean by transition zone? Between 0.01 to 1.0 mÅ function of cones overlap with rods. This zone is called as transition zone. 31. What do you mean by Purkinje shift or Purkinje phenomenon? The shifting of sensitivity of eye in response to change of light intensity from photopic to scotopic vision is known as Purkinje shift. It is seen normally towards the evening. 184 VIVA IN MEDICAL PHYSIOLOGY 32. What is dark adaptation? When an individual passes from a bright light to dark his vision first gets poor but then gradually improves. This is the function of rods in which rhodopsin is regenerated in dark. This phenomenon is known as dark adaptation. 33. What is nyclopia? In severe vit. A deficiency the function of rods is disturbed and so the process of dark adaptation is practically absent. This condition is characterised as nyclopia or night blindness. 34. What is colour blindness? How they can be diagnosed? It is the inability to differentiate the colours. It can be diagnosed by using Edridge Green and Red lantern and with Ishihara chart. 35. What do you mean by monochromats, dichromats and trichromats? • Monochromats—Individuals with only one cone system present. • Dichromats—Individuals with only two cone system present thus they have either protanopia (red blindness) or deuterapanopia (Green blindness) or tritanopia (Blue blindness). • Trichromats—Individuals with normal colour vision or they have all the Red, Green, and Blue coloured cone system but one may be weak is called trichromats. 36. What is red-green blindness? If either red or green or both of these cones are missing from the retina in a person, that person can’t distinguish red colour from green colour. This condition is known as red-green blindness. 37. What is meant by Deuteranomaly, Protanomaly and Tritanomaly? • Weakness of green colour is deuteranomaly. • Weakness of red colour is protanomaly. • Weakness of blue colour is tritanomaly. SECTION I : THEORY VIVA SPECIAL SENSES 185 38. What is glaucoma? Any obstruction of the outflow of aqueous humor results increased intraocular pressure which is known as glaucoma. 39. What is electro-olfactogram? When an odorous molecule gets absorb in the olfactory mucosa a monophasic negative potential is recorded which lasts for 4-6 secs. This recorded electrical changes is known as electro-olfactogram. 40. What is the function of tympanic membrane? • It acts as a pressure receiver. • It acts as a resonator and starts vibrating freely when the sound waves strike. • It helps in impedance matching device. 41. What are the components of impedance matching devices in ear? How impedance is matched? Tympanic membrane, ear ossicles and oval window are components of impedance matching device. The impedance is matched by following mechanism: • The high ratio of surface area of tympanic membrane to oval window increases pressure 17 times. • The lever system of ear ossicles also increases the sound intensity by 1.2–1.3 times. 42. What is Eustachian tube and what is its importance? It connects the middle ear cavity with the pharynx. Normally its pharyngeal opening is closed but opens during act of swallowing, chewing or yawning and thereby helps the air to enter into middle ear. Therefore it serves to equalise the pressure on the two sides of tympanic membrane when atmospheric pressure changes. 43. Why does there is pain in ear and even loss of hearing in sore throat? Due to infection during sore throat there is an inflammation occurs in pharynx causing closure of pharyngo-tympanic tube. Thus middle ear cavity becomes a closed cavity 186 VIVA IN MEDICAL PHYSIOLOGY due to inability to open eustachian tube. When the air within the middle ear gets absorbed, its pressure decreases resulting inward bulging of tympanic membrane that causes pain sensation and in severe cases there may be rupture of tympanic membrane resulting loss of hearing. 44. Name the muscles present in middle ear? What are their functions? • Tensor tympani—attached to the neck of malleus. • Stapedius—attached to the neck of stapes. In response to loud sounds, these muscles contract reflexly → decrease the amplitude of vibration of TM in response to loud sound →cause less pressure change in cochlear fluid → Protect the internal ear from being damaged. This protective mechanism is called as acaustic reflex or tympanic reflex. 45. Name different structures in internal ear. Vestibule or Saccule, Cochlea and Semicircular canal. 46. Name different cavities in cochlea and the respective type of fluids. • Scala vestibuli—Contains perilymph. • Scala media—Contains endolymph. • Scala tympani—Contains perilymph. 47. What is helicotrema? Scala tympani and scala vestibuli communicate at the apex by a small opening called as helicotrema. 48. What is the range of sound frequencies audible to the human ear? 20-20,000 cycles per second. 49. Which part of cochlea is affected by low frequency and which part is affected by high frequency of sound? Apex of the cochlea is affected by low frequency and base of the cochlea is affected by high frequency sound. SECTION I : THEORY VIVA SPECIAL SENSES 187 50. What is cortico-lymphatic, and endo-cochlear potential? • An electrical potential of about 180 mv exists all the time between endolymph and perilymph with positivity inside the scala media and negativity outside. This is called as endocochlear potential which is generated by the continual transport of K+ ions into scala media by the stria vascularis. • The potential difference between supporting cells or haircells and perilymph during resting condition is known as corticolymphatic potential. 51. What are the types of deafness and their causes? • Conductive deafness: Causes-accumulation of ear wax perforation of tympanic membrane (otitis media inflammation of middle ear), otosclerosis, (rigidity of ear ossicles). • Nerve deafness: Causes-damage of hair cells in response to loud sound, injury to VIII nerve, tumour of VIII nerve, vascular damage in medulla, degeneration of VIII nerve due to streptomycin injection or during measles, meningitis. 52. What is tinnitus? It is a ringing sensation in the ears by irritative stimulation of either the internal ear or the auditory nerve. 53. Name the receptor for smell sensation. Olfactory neuroepithelium. 54. What is anosmia? It is the complete loss of smell sensation. 55. Man is macrosomotic or microsmotic? Microsmotic as their smell sensation is not well developed like that of dog or rabbit. 56. Where are the taste buds lie? • On the surface of fungiform papillae. • In the grooves of foliate papillae. • At vallate papillae present at back of tongue. 188 VIVA IN MEDICAL PHYSIOLOGY 57. What are the types of sensation and what is due to? • Sour—Due to presence of H+ in the substance. • Salt—Due to the presence of Na+. • Bitter—Due to presence of many chemicals like quinine, nicotine, caffeine, etc. • Sweet—Due to organic compounds. 58. What do you mean by ageusia? It is the absence of taste sensation. ENDOCRINAL SYSTEM 189 SECTION I : THEORY VIVA 1.11 Endocrinal System 1. Define endocrine gland. It is a ductless gland which secretes the chemical substances known as hormones directly into blood. 2. Define hormone. These are secretory products of ductless glands released directly into the circulation in small amounts in response to specific stimulus and produce response to the target cell/organ. 3. What are the differences between hormone and vitamins? Parameters Hormone Vitamin 1. Nutritive role Not present Present 2. Incorporation as a structural No moiety in another molecule Yes 4. Classify the hormones citing examples of each. Hormones are classified into 3 major classes: • Steroids—Like adrenocortical hormones, sex hormones and vit-D3 • Proteins and polypeptides—Like anterior and posterior pituitary hormones, hypothalamic hormones, parathyroid hormones, calcitonin, insulin, glucagon, gastrin, secretin and angiotensin. • Amino acid derivatives—Epinephrine, norepinephrine, thyroxine. 190 VIVA IN MEDICAL PHYSIOLOGY 5. Name the hormones secreted by following organs. • Hypothalamus—Releasing hormones, like GnRH, TRH, CRH, etc. • Ant. pituitary—TSH, ACTH, GH, FSH, LH, prolactin. • Post. pituitary—ADH and oxytocin. • Thyroid—thyroxin, Tri-iodothyronine and thyrocalcitonin • Parathyroid—Parathormone (PTH). • Adrenal cortex—Cortisol, corticosterone, aldosterone, androgens, estrogens and progesterone. • Adrenal medulla—Adrenaline and noradrenaline. • Testis—Testosterone. • Ovary—Estrogen and progesterone. • Placenta—HCG, estrogen, progesterone, HPL. • GIT—Gastrin, secretin, motilin, substance-P, cholecystokinin. • Kidney—Erythropoietin, Vit-D3, medullipin. • Heart—ANF (Atrial natriuretic factor). 6. What do you mean by long loop feedback, short loop feedback and ultrashort loop feedback? • When peripheral gland hormones or substances from tissue metabolism exert negative feedback control on both the hypothalamus and anterior pituitary hormones, it is known as long loop feedback mechanism. • When anterior pituitary hormones exert the negative feedback control over the synthesis and release of hypothalamic releasing hormones, it is known as short loop feedback mechanism. • When hypothalamic releasing hormones after its secretion inhibit their further own synthesis and release it is known as ultrashort loop. 7. What do you mean by hypothalamo–hypophyseal portal vessels and hypothalamo-hypophyseal fiber tract? • The glandular part of pituitary gland has vascular connections with hypothalamus through a set of portal SECTION I : THEORY VIVA • ENDOCRINAL SYSTEM 191 vessels through which hypothalamic releasing hormones enter into adenohypophysis to regulate their secretion. These portal blood vessels are known as hypothalamo-hypophyseal portal tract. Whereas the neurohypophysis is connected with hypothalamus by hypothalamo-hypophyseal fiber tracts from supraoptic and paraventricular nuclei of anterior hypothalamus. These tracts are known as hypothalamo-hypophyseal fiber tract through which those above mentioned nuclei pass the oxytocin and vasopressin into posterior pituitary gland for storage. 8. How do you classify anterior pituitary gland cells histologically. 9. Differentiate somatotropin, somatostatin and somatomedins. Somatotropin is the growth hormone (GH) secreted by somatotroph cells of anterior pituitary. Somatostatin is the growth hormone inhibiting hormone released from hypothalamus and also found in nerve endings of brain, cells of antrum of stomach and in cells of pancreatic islets of Langerhans. Somatomedins are growth factors, synthesised and released from liver (mainly), kidneys, muscle, etc. in response to growth hormones and play role on skeletal growth mainly. 192 VIVA IN MEDICAL PHYSIOLOGY 10. What is the normal plasma level of growth hormones? • 4 mµg/ml in adult • 7 mµg/ ml in children. 11. Why the GH is known as protein sparer? It decreases protein and amino acid catabolism by increasing fat catabolism. This is why it is known as “protein sparer”. 12. Why the growth stops after adolescence? At the time of adolescence there is fusion between shaft and each end of epiphysis and thus GH can not promote the increase of growth of long bone at epiphyseal end plate. This results no growth of long bones after adolescence. 13. Lactating mother has less risk to be pregnant –Why? During and after pregnancy high PRL level in blood inhibits LH secretion → unovulation → No further pregnancy as long as high PRL level is maintained. 14. What is gigantism due to? It is due to overproduction of GH during adolescence, i.e. before fusion of epiphyseal plate and is characterised by excessive growth of long bone. 15. What is the cause of acromegaly? It is usually due to tumour of acidophilic cell of anterior pituitary with hyperactivity of growth hormone in adults, i.e. after epiphyseal closure. 16. What are the effects of acromegaly and its physiological basis? Following are the characteristics of acromegaly: • Acromegalic facies, i.e. broad and thick nose, thick skin, prominent brow and coarsening of facial features. These are due to proliferation of connective tissue that leads to edema and also enlargement of frontal, mastoid, ethmoid and maxillary sinuses (for promiment brow). SECTION I : THEORY VIVA • • • ENDOCRINAL SYSTEM 193 Kyphosis—Due to periosteal growth of vertebrae causes bowing of spine. Acral parts—periosteal growth of metacarpals and metatarsals. Hypertrophy of body soft tissue like heart (cardiomegaly), liver (hepatomegaly), etc. 17. What is dwarfism due to? It is due to hypofunction of GH secreting anterior pituitary glandular cells. 18. What is Laurence Moon Biddle syndrome? It has following characteristics: • Physical and mental retardation in growth • Subnormal intelligence. • Infantile gonads. • Obesity with polydactylism • Retinitis pigmentosa All these are due to hypofunction of pituitary gland as a result of tumour of chromophobe cells or lesions in hypothalamus in the young. 19. What is Simmond’s disease? It is due to panhypopituitarism in adults due to degeneration of the whole anterior pituitary gland resulting loss of weight, general emaciation, anaemia, low BMR, low body temperature, atrophy of gonads, etc. 20. What do you know about MSH? Melanocyte stimulating hormone is secreted by intermediate lobe of pituitary gland and is responsible for melanin formation, i.e. pigmentation of skin in human. 21. Name the nuclei secreting ADH and Oxytocin? • Supraoptic nuclei – ADH • Paraventricular nuclei – Oxytocin. 22. What is Neurophysin I and II? Neurophysin I is a carrier protein that helps to transport oxytocin from hypothalamus to posterior lobe of pituitary 194 VIVA IN MEDICAL PHYSIOLOGY gland for storage, through hypothalamo–hypophyseal fiber tract. Neurophysin II is also a carrier protein for the intraneuronal transport of ADH from hypothalamus to posterior pituitary. 23. What do you mean by syndrome of inappropriate ADH secretion (SIADH)? It is due to excessive or inappropriate secretion of ADH resulting— • Increase of blood volume and ECF volume. • Hypernatremia and Hypernatriurea. • Shift of water to ICF that results water intoxication called overhydration or dilution syndrome. 24. What is the normal concentration of iodine in blood? It is 0.5–1 µg%. 25. What is the normal level of protein bound iodide (PBI) in blood? It is 4-8 µg%. 26. What is the normal blood thyroxin level? It is 9 µg%. 27. What is the plasma level of T3 and T4 hormone? • T3- 0.1 µg m% • T4 - 3-8 µg m%. 28. How TSH increases the thyroid hormone secretion? TSH increases the thyroid hormone secretion by following ways: • Increased proteolysis of thyroglobulin → increase release of thyroid hormones. • Increasing activity of Iodide pump • Increasing iodination and coupling reaction • Increasing size and secretory activity of thyroid cells. • Increasing number of thyroid cells. 29. What do you mean by thyroglobulin? It is a glycoprotein synthesised in the thyroid cells and secreted into the colloid in lumen of thyroid follicle. SECTION I : THEORY VIVA ENDOCRINAL SYSTEM 195 30. What should be the daily intake of I2. Average 500 µgm. 31. Which one is the most active thyroid hormone T3 or T4? It is T3 or triiodothyronine. T4 acts as a prohormone, i.e. precursor of T3. 32. What are the main functions of thyroid hormone? These are: • To accelerate the metabolic activity with heat production. • To promote growth. • To ensure normal development of CNS. 33. How is thyroid secretion controlled? It is controlled by several mechanism as follows: • By blood level of free T4 and T3 through hypothalamichypophyseal axis (negative feedback) • Iodine level in blood (autoregulation) • Environmental temperature • Adrenaline and gonadal hormones. 34. What are the causes and effect of hypothyroidism? Causes: • Failure of normal development of thyroid gland. • Formation of autoantibody against thyroglobulin. • Deficiency of iodine. • Surgical removal of thyroid gland. Effect: Cretinism in children and myxoedema in adults. 35. What are the causes of hyperthyroidism? These are: • Excessive secretion of thyroid hormones. • Presence of long acting thyroid stimulator (LATS) substances in blood. 36. What are the signs and symptoms of hyperthyroidism? These are: • Exophthalmos expression of patient. 196 VIVA IN MEDICAL PHYSIOLOGY • • • • • • High BMR. Rapid pulse and heart rate. Increase in cardiac output. Nervous irritability. Involuntary tremors of hand muscles. Creatinuria and glucosuria. 37. What do you mean by autoregulation of thyroid? Iodine content in diet regulates the thyroid hormone production in the body, i.e. excessive ingestion of iodine decreases I2 transport to follicular cells whereas I2 deficiency leads to the enlargement of thyroid glands. Thus normal thyroid hormone secretion is maintained within the physiological limit without altering the TSH secretion. This intrinsic control system of thyroid hormone secretion is known as autoregulation. 38. What is myxoedema, idiot child and myxoedema madness? • In hypothyroidism because of decreased catabolism, there is deposition of mucopolysaccharides like hyaluronic acid and chondroitin sulphate under the skin and subcutaneous tissue which then exert osmotic pressure that causes retention of water and NaCl. This ultimately leads to dry, coarse and puffy appearance of skin (non-pitting oedema) called myxoedema. • Deficiency of T4 after birth upto 2 years in child results under development of brain producing mental retardation of child. This is known as idiot child. • The same cause, i.e. T4 deficiency during adulthood results loss of all intellectual function, memory and also slow speech and mental and physical lethergy. These lead to madness or psychosis known as myxoedema madness. 39. What are the common clinical conditions of hyperthyroidism? Exophthalmic goitre and nodular goitre. ENDOCRINAL SYSTEM 197 SECTION I : THEORY VIVA 40. What do you understand by exophthalmos? It is a characteristic protrusion of the eyeballs from the orbit seen in patient suffering from exophthalmic goitre. 41. How do you classify goitre? 42. What is the cause of simple goitre (endemic goitre)? It is iodine deficiency. 43. What do you suggest to prevent simple goitre in endemic goitre areas? It is advised to add potassium or sodium iodide in common salt in 1:100000 ratio. This ensures daily intake of 200 µg of iodine to prevent occurrence of simple goitre. 44. What is LATS? These are thyroid stimulating immunoglobulins that bind with the receptors on thyroid cell plasma membrane and displace TSH from its binding sites. Then via cAMP it acts to cause prolonged action on thyroid gland to increase formation and release of thyroid hormones and also increase growth of thyroid gland. These ultimately result enlargement and hyperplasia of thyroid gland. 45. What is the normal daily requirement of Ca++ and P and what is their normal blood level? Substance Daily requirement Blood level Ca++ P 0.8 –1 gm 1-1.4 gm 9-11 mg% 2.5 –4 mg% 198 VIVA IN MEDICAL PHYSIOLOGY 46. Name the hormones regulate Ca++ metabolism and their source. • Vitamin D—Diet mainly and also skin by UV radiation. • PTH—Chief cells of parathyroid gland. • Calcitonin—Parafollicular cells (C-cells) of thyroid gland. 47. What are the main actions of PTH? Its action is mediated through mainly 3 organs as follows: • In bone: PTH increases the reabsorption of ionised Ca++ from bone thus raising serum Ca++ ion by enhancing both osteolytic and osteoclastic activity. • In kidney: • It decreases reabsorption of phosphate from PCT and DCT of kidney and decreases serum phosphate level. • It also increases Ca++ reabsorption in DCT, thereby increase of serum Ca++ concentration. • It also promotes the conversion of 25 HCC to 1, 25 DHCC in the kidney. • It increases urinary excretion of Na+, K+ and HCO3¯ and decreases excretion of NH4+, H+. • On GIT: It increases Ca++ and PO4= reabsorption through GIT from food. 48. What are the main actions of calcitonin? Like PTH calcitonin also affects on bone, kidney and GIT but in opposite direction, i.e. lower plasma Ca++ level. • On bone: • Decreases bone resorption process by inhibiting osteoclastic activity. • Increases osteoblastic, i.e. bone formation activity by stimulating synthesis and release of alkaline phosphatase from the osteoblast. • On kidney: • Decreases renal formation of 1-25 DHCC that decreases plasma calcium level. • Increases Ca++, Na+, PO4= excretion in urine. SECTION I : THEORY VIVA • ENDOCRINAL SYSTEM 199 On GIT: • Inhibits Ca++ absorption through intestine. • Increases intestinal secretion of water and electrolytes. 49. Are the parathyroid glands essential for life? Justify your answer. Yes, as their removal will cause the decrease of plasma Ca++ level in a greater extent thereby there will be spasm of laryngeal muscles, thoracic muscles and diaphragm resulting asphyxia and ultimately death. 50. What are the main signs and symptoms of hypoparathyroidism? Hypocalcaemia, hyperphosphataemia, increase in blood pH, neuromuscular hyperirritability causing tetany. 51. What are the common signs present in tetany? Explain each of them. • Trousseau’s sign or carpopedal spasm—It is manifested in the upper limb as flexion at the wrist and thumb with hyper-extension of remaining fingers called obsteric hand/accoucheur’s hand or carpopedal spasm. If this is demonstrated by occluding the blood supply to a limb through sphygmomanometer cuff, it is known as Trousseau’s sign. • Chvostek’s sign—If skin in front of the ear is tapped, there is contraction or spasm of facial muscle. • Erb’s sign—It is depicted by the enhanced motor excitibility of galvanic current. 52. What is laryngeal stridor? Due to hypoparathyroidism sometimes the laryngeal muscle becomes spasmatic resulting airways obstruction and thereby asphyxia and can also result death. This is known as laryngeal stridor. 53. What are the main characteristics of hyperthyroidism? These are as follows: • Weakness, loss of muscle tone, thirst, polyuria, nousea, vomiting, constipation, etc. 200 VIVA IN MEDICAL PHYSIOLOGY • • • • • • Kidney stones (Nephrocalcinosis) Demineralization of bones resulting fragile and spontaneous fracture in bone with multiple bone cysts called osteitis fibrosa cystica. Increase in serum Ca++ upto 22 mg%. Decrease in serum PO4= below 2.5 mg% Increase in serum alkaline phosphatase. Hypercalciuria. 54. Why decreased ionised Ca++ causes neuromuscular hyperexcitibility? Decrease plasma Ca ++ causes increase in Na + permeability and thereby increase in excitability of the tissue. 55. What do you mean by Osteomalacia, Osteoporosis and Osteosclerosis? Osteomalacia is the adult ricket characterised by: • Decrease in mineral in bone/unit of bone matrix • Generally limited to females usually after multiple pregnancy and lactation Causes: • Dietary deficiency of vit D • Malabsorption of Vit -D • Chronic renal failure • Inadequate exposure to sun Characteristic features: • Bone pain and tenderness • Fracture may occur • Proximal myopathy. • Deformed bone with bowing legs • Retarded growth • Thickening of wrists and ankle. ] ] ] In children Osteoporosis: It is the clinical condition charecterised by; • Increase in all constituents of bone due to increase in bone resorption and decrease in bone formation. SECTION I : THEORY VIVA ENDOCRINAL SYSTEM 201 • Causes - Postmenopausal women (due to low oestrogen level resulted from increase in sensitivity of PTH to bone) - Hyperparathyroidism - Hyperthyroidism - Calcium deficiency Osteosclerosis: Increased calcified bone in patient with metastatic tumour, lead poisoning and hypothyroidism. 56. Name the layers of adrenal cortex and the hormones secreting from them. • Zona glomerulosa—Secretes mineralocorticoids (Aldosterone). • Zona fasciculata—Secretes glucocorticoids. • Zona reticularis—Secretes androgen. However in human zona fasciculata and zona reticularis act as a single functional unit synthesising mainly cortisol (glucocorticoids) and androgens. 57. Are the adrenal cortex essential for life? Justify your answer. Yes, as adrenal cortical hormones are essential to maintain normal metabolic process of cells and also to control the water and electrolyte balance which are very much necessary for normal functioning of cells. 58. Which of the layer of adrenal cortex is/are unaffected by absence of ACTH? Zona glomerulosa. 59. What are the steroids produced in the body? • Glucocorticoids—Cortisol, corticosterone, cortisone, etc. • Mineralocorticoids—Aldosterone and deoxycortisone. • Sex steroids—Androgen, estrogen and progesterone. 202 VIVA IN MEDICAL PHYSIOLOGY 60. What is the normal daily secretion and normal plasma level of cortisol and aldosterone? Hormones Daily secretion Normal plasma level Cortisol 12-50 mg/day 6-26 µg% Aldosterone 150 µg 0.03 µg% 61. In which forms cortisol is transported through blood? • 75% is by binding protein called transcortin. • 15% is by binding albumin. • 10% is free form. 62. What is the advantage of steroid binding to specific protein? Inhibition or inactivation of steroid by liver is favoured. 63. What are the chief functions of glucocorticoids? These are as follows: • Counteracts the symptoms produced due to stress. • Concerned with metabolic process of carbohydrate and also protein, fat in an antagonistic manner to that of insulin. • Depression of function of lymphoid tissue, decrease of eosinophil count, depressed tissue reactions. 64. What is the common synergistic and antagonistic action between insulin and hydrocortisone? • Synergistic—Augmentation of glycogenolytic action. • Antagonistic—Lipotropic action and promotion of glucose utilisation. 65. What do you mean by primary aldosteronism (Conn’s syndrome)? It is due to aldosterone oversecretion mainly due to adenoma in adrenal cortex which ultimately results: • Sodium retention and K+ depletion. • Alkalosis—that causes muscular weakness and tetany. SECTION I : THEORY VIVA • • ENDOCRINAL SYSTEM 203 Hypertension and congestive heart failure without edema. Polyuria and polydypsia. 66. What is secondary aldosteronism? When aldosterone secretion is increased not due to adrenal cortical change but due to other factors like severe hemorrhage, diarrhoea, dehydration, sweating, nephrosis, congestive heart failure it is known as secondary aldosteronism. 67. What is the glucose fever? The patient with adrenal cortex insufficiency if suffers from circulatory collapse, glucose infusion may cause high fever known as glucose fever. 68. What do you mean by addisonian or adrenal crisis? This is an acute form of adrenal cortex insufficiency which occurs after removal of adrenal cortex or withdrawal of therapeutically administered glucocorticoids or the patients with reduced basal secretion of cortisol and exposed to a sudden stress or infection. 69. In Cushing Syndrome why the pateint appears a moon like face and buffalo like hump? In Cushing syndrome there is increased secretion of glucocorticoids which promote deposition of fat in unusual sites on the body to result moon like face and buffalo hump. 70. What is Conn’s syndrome? Primary aldosteronism or Conn’s syndrome is the clinical condition due to excess aldosterone secretion due to tumor or hyperplasia of Z. Glomelulosa of adrenal cortex which is characterised by: (i) Muscular weakness (due to prolonged hypokalemia) (ii) Hypokalemic nephropathy (iii) Increase in plasma Na+, 204 VIVA IN MEDICAL PHYSIOLOGY (iv) Increase in plasma aldosterone level without oedema due to aldosterone escape (v) Increase in urinary aldosterone level (vi) Decrease in plasma K+ (vii) Decrease in plasma renin (viii) Albuninuria 71. What is General Adaptation Syndrome? What is it’s role in combating stress? The general manifestation of stress are called the general adaptation syndrome which is contributed by sympathoadrenal medullary system in which adrenal medullary hormones contribute to the Fight or Flight response by following ways: • Allows more light to enter into eyes by relaxing acomodation and producing pupillary dilatation. • Provides better perfusion of vital organs and muscles. • Shortens the bleeding time (if wounded). • Reinforcing the alert and arousal state by decreasing the threshold in reticular formation. • Increasing glycogenolysis in liver and lipolysis in adipose tissue to increase energy supply. 72. What is general adaptive syndrome? General manifestation of stress is called general adaptive syndrome. It occurs in 3 stages: • Stage of alarm—No adaptation takes place. • Stage of resistance—Optimum adaptation occurs due to the interaction of adrenal cortex and adrenal medulla. • Stage of exhaustion—Due to continued stress. 73. What is Addison’s disease? It is a state of chronic adrenal insufficiency when the gland is incapable of producing glucocorticoid hormones particularly under stress. This results in severe shock, low blood pressure, high K+ level in serum, dehydration and pigmentation, muscular weakness, mental confusion, etc. SECTION I : THEORY VIVA ENDOCRINAL SYSTEM 205 74. Describe the adrenogenital syndrome? This is due to tumor of adrenal cortex which causes excessive secretion of sex steroids therefore the male children get precocious development of sex organs with early onset of puberty, sex desire and secondary sex characteristics. Prepubertal and adult females develop male secondary sex characters known as adrenal virilism. The characteristic features include deepening of the voice, amenorrhoea, enlargement of clitoris, masculine types of muscle growth. 75. What is the cause of Cushing syndrome? It is due to oversecretion of cortisol which is due to bilateral adrenal hyperplasia or adrenal tumour. 76. What are the main signs and symptoms of Cushing syndrome? These are: • Retardation of growth in childhood • Moon like face. • Hirsutism or increase in facial hair. • Thin extremities, penduler abdomen and buffalo hump due to centripetal distribution of fat. • Muscular weakness, edema, polyuria, nocturia, osteoporosis, etc. 77. What is the main secretory product of adrenal medulla? It is adrenaline. 78. What are the basic differences of norepinephrine (NE) and epinephrine (EP) in relation to their function? NE is mainly secreted by sympathetic nerves and are mainly responsible for regulation of vascular tone, blood flow and BP whereas EP is mainly secreted by adrenal medulla which has predominant action on metabolism. 206 VIVA IN MEDICAL PHYSIOLOGY 79. What are the main functions of adrenaline? These are as follows: • Increase in systolic BP, HR, force of contraction, cardiac output and conductivity. • Dilatation of coronary blood vessels. • Relaxation of smooth muscles with constriction of sphincters. • Vasoconstriction with excessive sweating of skin. • Dilatation of pupils. • Relaxation of bronchial musculature. • Calorigenic action on metabolism. 80. What is phaeochromocytoma? What are its characteristic features? It is chromaffin cell tumour (benign) of adrenal medulla with oversecretion of noradrenaline and also epinephrine. Characteristic features: • Sustained systemic hypertension. • Headache, sweating, severe palpitation, weakness, anxiety, extreme cold sensation. • Nervous manifestations like tremor, giddiness. • Increased body temperature, hyperglycemia, glycosuria and increased BMR. 81. What are the hormones that regulate blood glucose level? Which one is the most important? Insulin, glucagon, epinephrine, hydrocortisone, ACTH, growth hormone and thyroxin, out of which insulin is most important. 82. Name the cells of islets of Langerhans and their secretory products. α cells—Glucagon β cells—Insulin δ cells—Somatostatin (GHIH) and gastrin. 83. Name the hormones which are antagonistic to the insulin? GH, thyrotrophic hormone, ACTH and glucagon. SECTION I : THEORY VIVA ENDOCRINAL SYSTEM 207 84. What are the main functions of glucagon? Why it is called as ‘hormone of energy release’? Glucagon is glycogenolytic, gluconeogenic, lipolytic and ketogenic hormone. Thus it favours the breakdown of stored nutrients. This is why it is known as hormone of energy release. 85. What is the average daily requirements of insulin? It ranges from 30-50 units/day. 86. What do you mean by labile and stable pool of insulin? Labile pool are the total storage amount of insulin in pancreas. Injection of glucose first initiates the release of 2% of labile pool of insulin and this response is known as primary response. Stable pool are the newly synthesised insulin that is released during 2nd stage after injection of carbohydrate. 87. Mention the main function of insulin. It is glycogenic, antigluconeogenic, antilipolytic, antiketotic. Thus it favours the storage of absorbed nutrients and that is why it is known as hormone of energy storage. 88. Name different varieties of insulin used for therapeutic purpose. Soluble insulin, globin zinc insulin, protamin zinc insulin, etc. 89. Define hyperglycemia and glycosuria. Increase in blood glucose level beyond normal range, i.e. increase in fasting blood glucose level beyond 100 mg% is termed as hyperglycemia and when it exceeds the renal threshold (>180 mg%) then glucose is excreted through urine. This condition is called as glycosuria. 208 VIVA IN MEDICAL PHYSIOLOGY 90. What is the normal blood glucose level in fasting condition? It is 60-95 mg%. 91. Define hypoglycaemia. What are the effects of hypoglycaemia? Fall of blood sugar level below 40 mg% is termed as hypoglycaemia. The characteristic features are: Mental confusion, giddiness, visual disturbances, syncope, coma, convulsions. 92. Define diabetes mellitus. It is a pathological condition characterised by hyperglycaemia and also glycosuria in extreme cases usually due to deficient insulin secretion or its inactivation. 93. Why in diabetic ketotic patient K+ should also be administered along with insulin? If diabetic ketotic patient is treated with insulin, it develops severe hypokalaemia which may be fatal. To overcome this severe hypokalaemia, K+ is also administered. 94. What are the predisposing factors of diabetes mellitus (DM)? These are: Heridity, age (more common in old age), obesity. 95. What are the signs and symptoms of diabetes mellitus? These are: Hyperglycemia, glycosuria, polyuria, dehydration, polydypsia, polyphagia. 96. What do you mean by ‘Starvation in the midst of Plenty’? In case of DM there is hyperglycemia. One of the important causes of this is the decreased utilisation of glucose by the cells. As a result there is intracellular glucose deficiency inspite of plenty of extracellular glucose. This situation is called as starvation in the midst of plenty. SECTION I : THEORY VIVA ENDOCRINAL SYSTEM 209 97. What do you mean by hyperosmolar coma? Diabetic coma resulted from renal failure, cerebral ischemia and severe dehydration produces hyperosmolarity by causing water to flow out of cells and ultimately coma known as hyperosmolar coma. 98. What are the different types of DM? Two types: • Juvenile type: – Usually severe – Insulin dependent – Occurs in children and young adults. – Accompanied by loss of weight • Adult type: – Usually mild – Occurs in middle-aged person – Non-insulin dependent – Person becomes obese. 99. What do you understand by glucose tolerance test (GTT)? It is a common clinical laboratory method to investigate the cases of diabetes mellitus and certain other conditions. The patient is kept on about 300 gm carbohydrate diet daily for 3 days. Fasting sample is collected in the morning after which the patient is administered glucose by oral route (1 gm/kg of b.w). The blood and urine samples are collected ½, 1, 1 ½ and 2 hours interval. The blood glucose values are estimated and urine is tested for presence of glucose. The values of glucose are plotted in a graph paper to obtain a characteristic graph. 100. What are types of GTT graph curves? Three types: • Normal curve, • Lag curve and • Diabetic curve. The lag curve is seen in early diabetic patients. 210 VIVA IN MEDICAL PHYSIOLOGY 101. Differentiate between hypoglycemic coma? hyperglycemic and Parameter Hyperglycemic coma Hypoglycemic coma 1. Cause Due to increase in blood glucose level (>400 mg%) Due to fall of blood glucose level (< 40 mg%) and more severe. 2. Rate of onset Slow Rapid 3. Signs and symptoms (i) Breathing Deep and rapid breathing Laboured breathing called air hunger or Kussmaul breathing. (ii) Sweating Absent Usually marked. (iii) Hydration Marked dehydration Normal (iv) Urine exam. Marked glycosuria and ketonuria Not specific. 102. What are the hormones secreted by thymus gland and mention their function. Two hormones: • Thymosin—Secreted by reticuloendothelial tissue in thymus and stimulates lymphopoiesis both within the thymus and peripheral lymphoid tissue. • Thymopoietin or thymin—Inhibits ACh release at motor nerve endings in myasthenia gravis. 103. Where does pineal gland present? It lies between the superior colliculi, i.e. roof of 3rd ventricle at the posterior end of corpus callosum. 104. What are the analogous organ of pineal in relation to its function? Adrenal medulla, post-pituitary and JG cells. All of these secrete hormone in direct response to nervous activity like pineal gland which secretes hormone melatonin in response to sympathetic nerve activity. SECTION I : THEORY VIVA ENDOCRINAL SYSTEM 211 105. What are the functions of pineal glands? It is not certain in case of human but it is predicted that it has got some role in: • Regulation of onset of puberty—It secretes gonadotrophin inhibiting peptide which may delay onset of puberty, though its role in human is not confirmed. • Pigmentation of skin by secreting a hormone known as melatonin in response to darkness. 106. What are local hormones? Give examples. The hormones which act at the sites of their synthesis and release are called as local hormones like ACh, histamin, PG, angiotensin, plasma kinins, etc. 107. What is physiologic GUT factor? Why oral glucose administration is more effective than intravenous glucose administration? Gastric inhibitory peptide (GIP) in very small concentration can increase insulin secretion. That is why it is known as physiologic gut factor. This is the reason also why oral glucose administration is highly effective as glucose in GIT can secrete GIP which can increase the insulin secretion separately. On the other hand if glucose is administered intravenously there is no question to its presence in GIT, there by no GIP secretion, so no additional insulin secretion. 108. What is APUD cells ? GIT contains some cells which can take up amine precursors and decarboxoylate them to convert it as amines. Therefore these cells are known as Amino precursor Uptake and Decarboxylation (APUD) cells. Similar types of cell are also present in brain normally and also in some cases of lung cancer. G cell is one type of APUD cells. 212 VIVA IN MEDICAL PHYSIOLOGY 1.12 Reproductive System 1. What is the name of the premitive germ cells? Female premitive germ cell—Oogonia Male premitive germ cell—Spermatogonia. 2. Which chromosome determines the type of sex? What is H-Y antigen? Y sex chromosome determines the type of sex. The testis determining gene product is known as H-Y antigen. 3. What do you mean by SRY chromosome? The gene present in the tip of the short arm of the human Y chromosome causes differentiation of indifferent or bipotential gonad to embryonic testis in the 7th–8th weeks after gestation. The region of the Y chromosome that contains the testis determining gene is called as SRY chromosome. 4. What is sex chromatin or Barr body? Soon after cell division has started during embryonic development one of the two X chromosomes of the somatic cell in normal female becomes functionally inactive. The inactive X chromosome is known as sexchromatin or Barr body. 5. What is the name of sex chromatin in male? It is known as F body. 6. To identify sex genotype certain cells are used for the cytological test. What are these cells? These are: The epithelial cells of epidermal spinous layer, SECTION I : THEORY VIVA REPRODUCTIVE SYSTEM 213 buccal mucosa epithelial cells, vaginal epithelial cell, leucocytes. 7. Name the abnormalities of sexual differentiation due to non-disjunction of sex chromosome? These are superfemale (44X XX), Klinefelter’s syndrome (44XXY), Turner’s syndrome (44X0). 8. What are the phenotypic features of Klinefelter’s syndrome? Characteristic features: • Genetic sex is female • Chromosomal configuration 44XXY • Atrophied testis (Gonadal sex) • Phenotypic features: • Male like appearance with feminine stigma • Bilateral Gynaecomastia • Sterile and impotent • Low or normal plasma testosterone level • High serum LH but normal FSH level • Small penis, testis, seminal vesicles, etc. • Secondary sex characters present 9. Name the abnormality of sexual differentiation due to nondisjunction of autosome. It is Down’s syndrome or mongolism. 10. What do you mean by male pseudohermaphroditism? If the female internal genital organs develop in genital male due to less secretion of androgen by defective testis, it is known as pseudohermaphroditism. 11. What is spermiogenesis? It is the sequence of developmental events by which spermatids are transformed into mature sperm without having any further division. The major features of this transformation include: • Formation of an acrosome • Development of flagellum 214 VIVA IN MEDICAL PHYSIOLOGY • • • Condensation of the chromatid accompanied by changes in the shape and size of the nucleus. Loss of excess cytoplasm Synthesis of numerous proteins unique to the spermatozoa. 12. Name the phases of spermiogenesis. These are: Golgi phase, Cap phase, Acrosomal phase and Maturation phase. 13. Define puberty. What is the onset period of puberty in male and female? Puberty is the period when the endocrine and gametogenic functions of the gonad have first developed to the point where the reproduction is possible. For female onset period is between 8-13 years, for male it is 9-14 years of age. 14. What do you mean by Euspermia, Oligospermia and Azoospermia? • When sperm count is more than 20 millions/ml it is known as euspermia. • When sperm count is in between 5-20 million/ml it is known as oligospermia. • When the sperm count is < 5 millions/ml it is known as azoospermia. 15. Before puberty the hypothalamus is more sensitive to the inhibitory effects of gonadal steroids and keeps the release of hypothalamic GnRH under check. At puberty this sensitivity decreases which is responsible for initiation of puberty—How? The exact mechanism by which the sensitivity of hypothalamus to this negative feedback effect of gonadal steroid decreases is not known yet, but it is assumed that before puberty pineal gland secretes melatonin which inhibits hypothalamus to release GnRH. With the advancement of age the pineal gland becomes calcified thereby no melatonin secretion. This results withdrawal of its inhibitory effect on hypothalamus. So the SECTION I : THEORY VIVA REPRODUCTIVE SYSTEM 215 hypothalamus now starts secreting more GnRH to initiate puberty. 16. What is adrenarch? At the time of puberty there is an increase in secretion of adrenal androgens without any change in the secretion of cortisol or ACTH. The onset of this increased adrenal secretion is called as adrenarch. 17. What do you mean by Eunuchoidism and primary amenorrhoea? In some individuals puberty is delayed even though the gonads are present and other endocrine functions are normal. This clinical condition in male is called as eunuchoidism and in females it is known as primary amenorrhoea. 18. What is precocious puberty? Early development of secondary sexual characteristics is called as precocious puberty. 19. Enumerate the function of FSH and LH in both male and female. • FSH on female: Responsible for early growth of ovarian follicles. • FSH on male: Maintains the spermatogenic epithelium. • LH on female: • Responsible for final maturation of ovarian follicles. • Responsible for ovulation and initial formation of corpus luteum. • Responsible for progesterone secretion. • LH on male: Stimulates Leydig cell to release testosterone. 20. What is blood testis barrier? What is its function? In between the Sertoli cells and other cells linning the seminiferous tubular wall there are tight junctions which prevent the free movement of substances acrosss it. This is known as blood testis barrier. Its functions are: 216 VIVA IN MEDICAL PHYSIOLOGY • • Helps in maintaining the composition of the fluid in the lumen of seminiferous tubule. It helps to prevent entry of sperm into blood and also protects the sperm from blood-borne noxious agents. 21. Which is the primary store house of spermatozoa? Where from it get’s energy during storage there? It is in epididymis. Epididymal secretion contains high concentration of glycerophosphoryl choline which is the potential source of energy. 22. Where does spermatozoa first become mature? In epididymis when they are exposed to O2. 23. Which one is secondary store house of spermatozoa? Even after vasectomy why contraceptive methods are suggested to be used for 2-3 months? Secondary store house is vas deferens. It is because after vasectomy viable spermatozoa are stored in the ampula for 2-3 months and thus may be released and may cause fertilisation. To prevent it, contraceptive methods are used for initial 2-3 months after vasectomy. 24. What is the importance of fructose present in semen? Spermatozoa have very little cytoplasm and therefore use fructose as their metabolic fuel. 25. What is the maximum duration of fertilising capacity of sperm? It is 24-48 hours after the entry in female genital tract though motility persists for 48-60 hours. 26. What do you mean by capacitation and acrosomal reaction? When the spermatozoa are first expelled in, they are unable to perform fertilisation of the ovum due to the presence of some inhibitory factors within the semen. However, on coming contact with the fluids of female gential tract multiple changes occur that ultimately SECTION I : THEORY VIVA REPRODUCTIVE SYSTEM 217 activate the sperm for the fertilisation. These collective changes are called as capacitation of the spermatozoa. When the sperms come in contact with zona pellucida of ovum there is a release of stored enzymes from acrosome of the sperm like hyaluronidase and proteolytic enzymes that facilitates the penetration of the sperm through the zona pellucida. This reaction is known as acrosomal reaction. 27. What is the source of testosterone? It is: • Mainly Leydig cells of testis. • Partly by the zona reticularis layer of adrenal cortex. 28. What is inhibin? In response to increased FSH secretion by pituitary gland sertoli cells release one testicular factor which inhibits further FSH secretion by negative feedback mechanism. This testicular factor is known as inhibin. 29. What do you mean by cryptorchidism? What is its effect on testis? Incomplete descending of one or both testes in newborn, i.e. testis remains in the abdominal cavity or inguinal canal without descending to scrotum is called as cryptorchidism. Due to the high temperature in abdominal cavity the sertoli cells are degenerated thereby spermatogenesis fail to occur resulting sterility. 30. What are the effects of castration before puberty? These are as follows: • Absence of characteristic changes at puberty. • Secondary sex organs do not develop fully. • General musculature remains poor. • Voice remains boyish type. • Individual remains sterile and impotent. 31. What are the effects of castration after puberty? These are as follows: • The individual becomes sterile but sex urge is retained. 218 VIVA IN MEDICAL PHYSIOLOGY • • Seminal gland and prostates become atrophied. There is general muscular asthenia. 32. Name the ovarian hormones with each of their source and daily secretion. Estrogens: • Source: Theca interna cells of graffian follicles. • Secretion: 35-300 µg in different stage of menstrual cycle. Progesterons: • Source: Corpus luteum. • Secretion: 0.9 ng /ml in follicular phase and increases 20 times in luteal phase. Relaxin: • Source: Corpus luteum. 33. What are the functions of relaxin? It facilitates child birth by causing: • Relaxation of the symphysis pubis and other pelvic joints. • Initiation of uterine contractility. • Softening of the cervix. 34. What are the different phases of menstrual cycle and what is its cause? There are 4 phases: • Menstrual phase: It is due to withdrawal of progesterone secretion. • Proliferative phase: It is due to estrogen secretion. • Ovulatory phase: It is due to LH surge. • Secretory or luteal phase: It is due to increase in secretion of progesterone. 35. What is estrogen surge, FSH surge and LH surge? • In the preovulatory phase of menstrual cycle rise of FSH concentration increases the serum concentration of estradiol to reach a peak at 12-13 days (in case of 28 days cycle), called oestrogen surge (Fig. 1.12.1A). SECTION I : THEORY VIVA • • REPRODUCTIVE SYSTEM 219 Within 24 hours of oestrogen surge, the increased level of oestrogen augments the responsiveness of the pituitary to GnRH which induces a burst of LH secretion. This peak rise of LH in serum is known as LH surge (Fig. 1.12.1B). At the same time when LH peak occurs serum concentration of FSH also increases suddenly to a peak level called FSH surge (Fig. 1.12.1C). Figs 1.12.1A to C: Hormonal level during ovarian cycle 220 VIVA IN MEDICAL PHYSIOLOGY 36. What do you mean by withdrawal bleeding? If no fertilisation takes place, corpus luteum regresses by the process known as luteolysis resulting sharp fall of estrogen and progesterone secretion. This inturn causes spasm in spiral arteries and thereby ischemia of superficial layer of endometrium. This ultimately leads the shedding of superficial layer of endometrium and thereby release of blood and mucous through vagina known as withdrawal bleeding. 37. What is corpus luteum and corpus albican? • After ovulation capillaries from the theca interna rapidly invade dividing granulosa cells layer and the clotted blood is replaced by yellowish, lipid rich luteal cells known as corpus luteum. • If fertilisation do not occur the corpus luteum regresses and eventually forms corpus albicans. 38. What is the lifespan of corpus luteum? What is its function? If fertilisation does not occur it servives for upto 14 days but if fertilisation occur then it survives upto 3-4 months. Its function is to synthesise and release progesterone. 39. What do you mean by CL of Pregnancy and CL of fertilisation? If the ovum is not fertilized the corpus Luteum (CL) persists for about 14 days which secretes progesterone to initiate endometrial growth required for implantation of zygote. These CL are small and known as corpus luteum of menstruation. Whereas, if the ovum is fertilized and pregnancy results CL persists for 3-4 months and maintains the growth of endometrium. At this stage CL size is longer and known as corpus luteum of pregnancy. After 3-4 months it degenerates and it’s function is taken over by the placenta. 40. What are the various natural forms of oestrogen? These are oestradiol, oestrone and oestriol. SECTION I : THEORY VIVA REPRODUCTIVE SYSTEM 221 41. What are the main synthetic forms of estrogen and progesterone? • Oestrogen—Diethylstilbestrol and hexosterol. • Progesterone—Pregninolone. 42. What is ovulation? When does it occur? Ovulation is the release of ovum from ovary at fairly fixed interval of menstrual cycle. Its appropriate timing is not fixed. In case of regular cycle of 28 days it is generaly the 14th day when ovulation takes place. However, if the cycle is irregular and it is say 24 days or 34 days then the ovulation will occurs at 10th and 20th day of cycle respectively. 43. What is the physiological basis of BBT as indicator of ovulation? At the time of ovulation body temperature rises by 0.3 to 0.5°C than the temperature at preovulatory phase. This increase in temperature is due to the increase of progesterone level in blood which is thermogenic. 44. What is menopause? What is its cause? Menopause is the period of life when menstruation naturally stops permanently. This is due to the exhaustion of the graffian follicles in the ovary which in turn produces egg or ovum. 45. What are the signs and symptoms of menopause? At the onset of menopause initially the menstrual cycle becomes irregular and finally ceases altogether. There is a fall in oestrogen level that causes atrophy of external genitalia, uterus, breasts with decline in sexual urge. Some other symptoms are hot flushes, profuse sweating, transitory emotional disturbances, giddiness, etc. 46. What do you mean by safe period? Just before ovulation, i.e. 2 days before ovulation (as sperm can survive maximum of 2 days in female genital tract) and 2 days after ovulation (as ovum released are functionally active up to 24-48 hrs after ovulation) there 222 VIVA IN MEDICAL PHYSIOLOGY is a minimum chance to conceive. That is why beyond this period, menstrual cycle is safe in relation to conception and is known as safe period though nowadays it is believed that there is no real safe period specially in irregular menstrual cycle. 47. Name the contraceptive measures in male. These are as follows: • Use of condom • Coitus interruptus • Vasectomy • Use of spermatogenesis inhibiting drugs. 48. Name the contraceptive measures in female. These are as follows: • Use of diaphragm • Use of spermicidal jellies and cream • Coitus during safe period • Tubectomy • Intrauterine device • Use of contraceptive pills. 49. What are the disadvantages of contraceptive pills? These are as follows: • High risk of thrombo-embolic phenomenon • Increase of systemic BP • Precipitation of diabetes mellitus. 50. What is the physiological basis of pregnancy diagnostic tests? It is based on the presence of hCG in urine which can be detected as early as 14 days after conception, i.e. 10-14 days after the 1st missed period. 51. What is the average duration of human pregnancy? It is 280 days or 40 weeks when calculated from the 1st day of last menstrual period. SECTION I : THEORY VIVA REPRODUCTIVE SYSTEM 223 52. Name some pregnancy diagnostic tests besides immunochemical tests? These are Ascheim Zondek test, Friendman’s test, Kupperman’s test, Hogben’s test, etc. 53. Explain Ascheim Zondek test? 54. In this test 2 ml urine of a subject is injected subcutaneously in female non-pregnant mice for 3 days. On the 5th day if there is hemorrhagic spot or corpora lutea present in ovaries it is considered as positive for pregnancy. 55. What do you mean by double Bohr’s effect? In the feto-placental unit while flowing though the placenta the PCO2 of fetal blood decreases due to pressure gradient. This shifts O2 - Hb dissociation curve to left to cause increase loading of O2 by the fetal blood. Whereas PCO2 of maternal blood increases as it picks up the CO 2 from fetal blood. This shifts O 2 –Hb dissociation curve to right and causes increased of unloading of O2. This event is known as double Bohr’s effect. 56. What is amniotic fluid? What is its function? Amniotic fluid is a clear fluid which is collected in the amniotic cavity and surrounds the foetus. Its functions are as follows: • To provide the foetus with fluid to drink • To keep the foetus at an even temperature • To protect the foetus from injury • To provide a medium for foetal movement. 57. What do you mean by lactogenesis and galactopoiesis? Initiation of milk secretion is known as lactogenesis whereas maintenance of milk secretion is called as galactopoiesis. 224 VIVA IN MEDICAL PHYSIOLOGY 58. What is Colostrum? It is a deep yellow coloured protein and salt enriched fluid secreted by the breast during first 3 days after childbirth. 59. Lactating mother does not generally become pregnant—Why? During lactation cyclic ovarian function ceases in lactating mother due to the inhibition of hypothalamic GnRH release by reflex initiated in response to suckling of nipple. 60. What is meant by transition and mature milk? The milk secreted during the first few weeks after parturition is known as transition milk. Whereas the milk appears at the end of the 1st month is called as mature milk. 61. Name the proteins in human milk. It is caseinogen and lacto albumin. 62. What do you mean by ash in relation to milk? It is the minerals present in milk which are Ca2+, K+, Na+ phosphorus and Cl– in traces. 63. What are the differences between human’s milk and cow’s milk? Human’s milk 1. 2. Cow’s milk It contains less protein, less It contains more protein, more salts salts and more carbohydrates and less carbohydrates. Caseinogen is present more Comparatively in less amount. in amount. 3. It contains less fatty acids. It contains more fatty acids. 64. When does heart beat begins in foetus? It begins by 4th week of pregnancy. 65. When does GIT develop in the foetus? It starts to develop by 4th month and by 7th month it grows almost upto normal stage. SECTION I : THEORY VIVA REPRODUCTIVE SYSTEM 225 66. When do the kidney develops in the foetus? These develop mostly by 3rd trimester of pregnancy but normal functioning becomes complete only few months before birth. 226 VIVA IN MEDICAL PHYSIOLOGY SECTION II: PRACTICAL VIVA Part A Hematology 1. Which blood is generally used in hematological practical–Capillary blood or Venous blood? Capillary blood. 2. What is the difference between capillary blood and venous blood? Capillary blood is obtained from punctured capillaries, smallest arterioles or venules by a skin puncture usually over a finger or ear lobe or the heel of the foot (in infants) and shows lower cell counts, lower hemoglobin concentration and PCV values as some tissue fluid always dilute the blood, whereas the venous blood is obtained from a superficial vein by venopuncture which shows comparatively higher cell counts, higher Hb percentage and PCV values as it is not contaminated with tissue fluid. 3. Why the capillary blood is called peripheral blood? Capillary blood is called as peripheral blood as it comes from the peripheral blood vessels like venules or smallest arterioles or capillaries in contrast to venous blood. 4. Why the thumb or little finger is not pricked for collecting blood? It is because the underlying palmer fascia from these digits extends up to the forearm. So in case of any infection at the site of injury, there is a chance of the infection to spread up to the forearm. SECTION II: PRACTICAL VIVA HEMATOLOGY 227 5. In case of infants where from you will collect the capillary blood? It is from either big toe or heel as the fingers are too small. 6. What measures will you take to prevent the spreading of hepatitis infection following pricking of finger? The needle used to prick the finger should be heated over flame. 7. Why should the pricked finger not to be squeezed? Squeezing the finger results coming out the tissue fluid that dilutes the capillary blood and thus giving lower values. 8. What are the features of ideal blood film? These are: i. It should be tongue shaped, uniformly thick, neither too thick nor too thin and should occupy the middle 2/3rd of the slide. ii. Microscopically all the cells should be separate without any overcrowding and rouleaux formation. 9. What is the composition of Leishman stain? What are the function of each constituent and why the stain should be acetone free? The composition and function of each constituents is: A. Leishman powder: 0.15 gm i. Eosin: An acidic dye stains basic part of cell e.g.; cytoplasm ii. Methylene blue: A basic dye stains acid part of cell e.g. nucleus B. Methyl alcohol (Acetone free): 100 ml (as a fixative and solvent) Acetone free methyl alcohol is used because the acetone being a strong lipid solvent can even destroys the cell by lysing the cell membrane. 228 VIVA IN MEDICAL PHYSIOLOGY 10. Why buffer solution is used instead of distilled water in Leishman’s staining? The pH of buffer solution is adjusted at 6.8 and at this particular pH the ionization of stain is optimum, so the stain particles can easily penetrate the cell to stain it. 11. Why is Leishman’s stain diluted after 1-2 mins? During the initial 1-2 mins staining does not take place, as the stain particles cannot enter the cell as long as they are not ionized by addition of water. During this period the absolute alcohol of Leishman’s stain serves two functions: • Fixes the blood cells on the glass by precipitating the plasma proteins, which act as glue. • Preserves the normal shape and chemistry of cells. 12. Can tap water be used for diluting the stain after fixation? It should not be used as methylene blue of Leishman’s stain may be unable to stain the cells because of improper pH. 13. Name any other stain that can be used to stain the blood film. Geimsa’s stain. 14. What do you mean by ‘Vital Staining’? It is the special staining method to stain the living cells. 15. Why is cedar wood oil required to use Oil immersion lens? It is because the refractive index of this oil is similar to that of glass avoiding the refraction of the light. Otherwise the image will be faint and blurred. 16. Which part of the blood film should be avoided for counting the cells? “Head’ and extreme “Tail” part of the slide as the cells present in these area are few in number and also distorted. SECTION II: PRACTICAL VIVA HEMATOLOGY 229 17. How do you differentiate between RBC pipette and WBC pipette? Parameter RBC pipette WBC pipette Upper gradation 101 11 Diameter of bulb More Less Colour of mouthpiece Red White Colour of bead in the bulb Red White 18. What are the functions of the bulb in a diluting pipette? It helps the blood to be diluted and also to be mixed with the diluting fluid. 19. What are the functions of the bead present inside the bulb of the diluting pipette? It: 1. Helps to mix the blood with the diluting fluid. 2. Helps to identify the pipette by just glancing it. 3. Gives an idea whether the pipette is wet or dry. If it is dry the bead rolls freely inside the bulb. 20. Why it is important to discard the first two drops of diluted blood from the pipette before charging the counting chamber? The stem of the pipette contains only the cell free diluent which is to be discarded before charging the chamber; otherwise the count will be low and thus erroneous. 21. Why any small excess of blood drawn into the pipette should not be removed by a piece of cotton? If the cotton is used to remove the excess blood drawn in the pipette then it will absorb only the fluid not the cells. This will result in higher RBC/WBC count than the actual value. 230 VIVA IN MEDICAL PHYSIOLOGY 22. How will you clean the pipette in case of clotting of the blood inside the stem of the pipette? It is to be kept in strong nitric acid or alkali or H2O2 for 24 hrs and then washed in the running tap water. A flexible suitably thick metal wire is now inserted to clean the capillary bore, finally rinse with alcohol or ether to dry it. 23. How will you clean the pipette? It is by sucking up and blowing out distilled water several times followed by sucking up and blowing out acetone for drying it. 24. How will you clean the chamber and cover slip? It is by washing it first with soap and water and then with alcohol. 25. Can these pipettes be used for any other purpose? The RBC pipette can be used for counting platelets, WBCs (when their count is very high as in leukaemia) and also for counting the spermatozoa in the semen. 26. What are the dimensions of WBC and RBC squares? • Each smallest square for RBC counting: (i) Area: 1/20 mm × 1/20 mm = 1/400 mm2 (ii) Volume: 1/400 mm2 × 1/10 = 1/4000 mm3 • Each smallest square for WBC counting: (i) Area: 1/4 mm × 1/4 mm =1/16 mm2 (ii) Volume: 1/16 mm2 × 1/10 mm = 1/160 mm3 27. What are the features of an ideally charged chamber? These are: • No flowing of blood into the trenches • No air bubbles 28. When blood is taken to the mark 0.5 and the diluting fluid to mark 101, why is the dilution 1 in 200 and not 1 in 202? The dilution of the blood occurs not in its stem but in the bulb of the pipette, the volume of which is 101-1 =100. SECTION II: PRACTICAL VIVA HEMATOLOGY 231 Hence half volume in hundred gives a dilution of 1 in 200. 29. If Haem’s fluid is not available can you use any other? 0.9 gm% normal saline can be used but the cells have to be counted within an hour after filling the pipette, even though the red cells likely to form rouleaux. 30. How do you differentiate red cells from dust particles? The red cells are appeared in round discs of uniform size and light pink in colour whereas the dust particles are angular with varying size and colours. 31. What is the composition of Turk’s fluid? What is the function of each constituents? The composition and function of each constituents is; a. Glacial acetic acid : 1.5 ml (hemolyses the red cells) b. Gentian violet: 1.5 ml (stains the nuclei of WBCs) c. Distilled water: up to 100 ml (as a solvent). 32. Name any other accurate method to do RBC count? Use of electronic cell counter. 33. Why is it necessary to follow the rules of counting? It is to avoid the error of missing some cells and counting other more than once. 34. What is the fate of leucocytes in this experiment? The leucocytes in this experiment are as much diluted that its number are considered very negligible to consider because: • The low count of WBC in comparison to RBC. • Dilution of the WBC by 100 times. Occasionally leucocyte may be seen but its concentration is very less (1 WBC for every 600-700 RBCs, i.e. one WBC in 80 squares). So even if it is counted along with the RBCs the RBC count will not vary too much (i.e. 10,000/cmm of blood). 232 VIVA IN MEDICAL PHYSIOLOGY 35. What do you mean by the term ‘Glacial’? Why it should be glacial acetic acid in Turx's fluid? Glacial means pure. Only the pure form of acetic acid can give the refractivity around the WBCs that helps the WBC to be differentiated from the dust particles (which are opaque). 36. What is the fate of the RBCs in this experiment (Total count of leukocytes)? RBCs are hemolysed by the glacial acetic acid otherwise it would not be possible to count the WBCs. 37. Can any other agent be used to hemolyse the RBCs? No, any strong agent will also lyse the WBCs and any weak agent will take long time to lyse them completely. 38. What is the difference between DLC and absolute leucocyte count? In DLC the percentages of different leucocytes are determined whereas in absolute count the actual number of different leucocytes per cu mm of blood are calculated. 39. How does the DLC of a child differ from that of adult? In adults the granulocytes (mostly neutrophil) predominate whereas in children the lymphocytes predominate. 40. Can you get rough idea of TLC by doing DLC? Yes, if the cells appear more frequently amongst the RBCs the TLC will be high and vice versa. 41. Enumerate the sources of error in hemocytometry? These are: 1. Pipette error, i.e inaccuracy in calibration and in measurement. 2. Field error, i.e unequal distribution of cells over the counting chamber due to: a. Over-charging or under-charging of the chamber. b. Presence of grease or oil on slides or cover slip. SECTION II: PRACTICAL VIVA HEMATOLOGY 233 3. Personal error, i.e. wrong counting of cells. 4. Stastical error: It is inversely proportional to the square root of the number counted. 42. Can you use oxalate mixture in Westergren method and citrate solution in Wintrobe’s method? No, the anticoagulants used for each method can not be interchanged as both the methods are standardized with the specific anticoagulant. 43. What are the advantages and disadvantages of Wintrobe’s and Westergren method? Wintrobe’s method: a. Advantage: Same sample of oxalated blood can be used for ESR first and then after one hour for PCV by centrifuging it. b. Disadvantage: The method is less sensitive as the column of blood is not high. Westergren method: a. Advantage: The method is more sensitive as the column of blood is high. b. Disadvantage: Citrate solution used in this case dilutes the red cells and thus tends to raise the ESR, however as the fibrinogens and globulins of plasma are also diluted there is also tendency of lowering the ESR. 44. Why ESR reading taken after one hour? This is because more than 95-98 % of RBCs settle down by the end of this time and after that the rate of sedimentation of RBCs do not affect the ESR significantly. 45. Why the normal values of ESR are more in Wintrobe’s method than that of Westergren method? It is because of: • Effect of atmospheric pressure over the blood column as the tube is kept open in it’s top. • Nature of powdered mixture of oxalate solution used as an anticoagulant. 234 VIVA IN MEDICAL PHYSIOLOGY 46. What is the importance of determining hematocrit? It is simple but more accurate test for determining the presence of anemia or polycythemia. It is also used for determining various absolute corpuscular values. 47. Which cells make up the buffy layer? How thick it is? When it’s thickness increases? The buffy layer consists of packed leucocytes and platelets. It is 1 mm thick. It’s thickness increases in severe leucocytosis, leukaemia and thrombocytosis. 48. What is the difference between PCV of arterial blood and venous blood? What is the reason behind this difference? The PCV of venous blood is higher than that of arterial blood. It is because in the venous blood the RBCs gain an extra weight due to the entry of water within it resulted due to chloride shift. 49. Why colour index is not an appropriate index of hemoglobin content of RBC? It is because of wide range of normal value of RBC. 50. Which absolute corpuscular value is most useful? It is MCHC because: • It expresses the actual Hb concentration in RBCs only, not in whole blood. • It does not consider the RBC count for it’s calculation. 51. Is it possible to know the sex of a person from the blood film? Yes, in the blood film of females of the Barr body, i.e chromatin of the sex chromosome is seen in some neutrophils. 52. What are the features of a senile neutrophil? These are less motile and least effective. These cells commonly break up during the spreading of the blood film. SECTION II: PRACTICAL VIVA HEMATOLOGY 235 53. Which stage of Neutophil is most effective? 3-lobed neutrophil is the most motile and functionally most effective in killing the bacteria. 54. Why Cook –Arneth count is not used as a routine investigating tool? This is because: a. During some physiological conditions neutrophils used to enter the circulation from various storage pools, whereas during some other conditions there is shifting of neutrophils to the storage pools, resulting shift to the left or right. This normal phenomenon may give the false indication about the status of bone marrow if we totally depend on this investigating tool. b. Besides this the better method like bone marrow biopsy are now available for assessing bone marrow function. 55. What are the indications of doing reticulocytes count? It is to assess the red cell forming and releasing activity of the bone marrow. 56. How does a reticulocyte differs from the RBC? The reticulocytes are comparatively larger than RBCs and also contain dots, strands and filaments of bluish stained material. 57. Why does the ABO incompatibility rarely produce hemolytic disease on the newborn? This is because the anti-A and Anti-B antibodies are IgM type of immunoglobins that do not cross the placenta because of their large MW and thus there is no chance of antigen antibody reaction. 58. What do you mean by Zone phenomenon? For agglutination to occur the concentration of antigen and antibody has to be same, otherwise there will no antigen antibody reaction. This is termed as Zone phenomenon. 236 VIVA IN MEDICAL PHYSIOLOGY 59. What are the earliest effects of a mismatched transfusion? These are: Severe pain anywhere in the body, sense of suffocation, feeling of tightness in chest, shivering and even fever. 60. Which blood substitutes may be used to restore blood volume if suitable donor is not available? Crystalloid solution (glucose saline) and colloid solutions like human albumin, dextrose with NaCl, etc. 61. Why does calcium deficiency not cause a bleeding disorder though it is essential in blood coagulation? It is because the calcium required for the blood clotting is in minute quantities. 62. What is athrombocytopenic purpura and thromboasthenic purpura? Purpura with normal platelet count is called as athrombocytopenic purpura and purpura with normal count but abnormal circulating platelets is called as thromboasthenic purpura. 63. What do you mean by fragility and hemolysis? Fragility means the susceptibility of red cells to being broken down by osmotic or mechanical stresses. Whereas the hemolysis means the breaking down of red cells resulting release of hemoglobin into the surrounding fluid. 64. What is the effect of 5% glucose, 10% glucose, urine and urea solution of any strength on red cells? • 5% glucose: It is isotonic with blood, so no change in size and shape of RBC. • 10% glucose: It is hypertonic, so there is shrinkage of red cells due to exo-osmosis. • Urine: Urine is hypotonic so the red cells will swell up due to entry of some water. • Urea solution: Hemolysis of red cells due to entry of urea followed by water into the red cells. SECTION II: PRACTICAL VIVA HEMATOLOGY 237 65. Can strong acids or alkalis be used instead of HCl to measure haemoglobin? No. the strong acids will oxidize the hemoglobins and the strong alkalis will cause disruption of Hb. So in both the cases there will no formation of acid hematin. 66. What happens if more or less amount of N/10 HCl is taken instead of required amount? If less amount of acid is taken all the hemoglobin will not be converted to acid hematin resulting a low value. Besides this there may be clot formation due to improper mixing of blood with acid. On the other hand if more than the required amount of acid is taken the final colour developed in case of severe anemia would be much lighter than the standard. 67. Why it is necessary to convert hemoglobin in acid hematin? If hemoglobin is not converted into acid hematin then the colour of oxy-hemoglobin, which has a wide spectrum of colours, cannot be standarized. 68. Can tap water be used for diluting and colour matching? No, as the salt present in the tap water may cause turbidity which will interfere with colour matching. 69. Can N/10 HCl be used for diluting and colour matching? Yes. 70. While matching the colour why it is important to lift the stirrer above the solution but not take it out? If the stirrer is kept in the solution it will lighten the colour and thus matching will occur earlier resulting low value. On the other hand if it is taken out every time during the colour matching, some solution will go out of the tube and thus again giving a low value. 238 VIVA IN MEDICAL PHYSIOLOGY 71. Classify the severity of anemia as per the Hb concentration? Depending on the Hb level the anemia may be graded as: • Mild : Hb 10-2 gm% • Moderate : Hb 5-8 gm% • Severe : Hb below 5 gm% Part B Human Experiments 1. What are the general procedures of clinical examination? These are: Inspection, Percussion, Palpation and Auscultation. 2. What is the normal shape of the chest? It is elliptical. 3. What is the pulse respiration ratio? It is 1: 4. 4. What type of respiratory movement is seen in childhood, male and females? • In male: Abdominal • In female: Thoracic • In children: Abdominal. 5. Why a person cannot commit a suicide by holding his/her breath? It is because of the breaking point, i.e. the point when a breath has to be taken automatically due to the strong ventilatory drive even if that person looses consciousness. 6. What is the normal range of breath holding time (BHT)? What are the factors affecting BHT? Normal BHT is 40 sec to 1 min, however the world record of BHT is 5 min 13 sec. • The factors that increase the BHT are: Yoga training, 240 VIVA IN MEDICAL PHYSIOLOGY • motivation and breathing pure O 2 before holding breaths, etc. The factors decreasing the BHT are: Diseases like chronic bronchitis, emphysema, etc. 7. What do you mean by breath holding attacks? In some infants and young children (below 3 years) there are sudden and brief breath holding attacks in which the child starts crying, and becomes stiff and blue, and also looses consciousness. There may be even convulsions. This type of attack is generally precipitated by emotional distress, e.g.; pain, anxiety, fright, frustration, etc. 8. Name the precautions that must be observed during spirometric recordings? These are: • The subject should be well awared about the procedure that he/she has to do. • There should be no leakage of air anywhere from the mouthpiece to the gas bell. • The indicator must be brought to zero reading before each determination. 9. Name the types of breathing. Where is it seen? It is of 3 types. • Thoracic: It is generally seen in adult female. • Abdominal: It is generally seen in adult males and children. • Thoracoabdominal: It is generally seen in pregnant women and also in all peoples after exercise. 10. What do you mean by 'Vocal fremitus'? What is its importance? The detection of vibrations transmitted to the hands (placed over chest) from the larynx through bronchi, lungs and chest wall during the act of phonation is called as vocal fremitus. Vocal fremitus gives the idea about the presence of any blockade, fluid or air in the respiratory passage and also SECTION II: PRACTICAL VIVA HUMAN EXPERIMENTS 241 in pleural cavity. Thus it gives the idea about the status of respiratory system. It is decreased due to any blockade in respiratory passage or dampened by fluid or air in the pleural cavity. It is increased due to consolidation of lungs during pneumonia, etc. 11. Name the types of breathing sound with explanation. • Vesicular sound: These are produced by passage of air in and out of alveoli in the normal lung tissue. These are heard both during inspiration and expiration without having any pause in between. However, the sound during inspiration is intense and rustling in character and of low pitch and its duration is alomost twice of expiratory sound’s duration. • Bronchial sound: These are produced by the passage of air through the trachea and large bronchi. These are also heard during both inspiration and expiration without any silent gap. In this case, the inspiratory sound is harsh and expiratory sound is more intense and of higher pitch. 12. What do you mean by vesicular breath sounds, Bronchial breath sounds and Tracheal breath sounds? By placing the stethoscope over the surface of chest, we can listen some breathing sounds which are basically two types: vesicular and Bronchial breath sounds. • The vesicular breath sounds are produced by the passage of air in and out of alveoli in the normal lung tissue. The features of this type of sounds are: Are heard all over the healthy chest surface but most typically over axillary and infrascapular regions. Are heard both during inspiration and expiration. Inspiratory sound is of low pitch, intense and rustling in character. There is no clear cut pause between inspiration and beginning of expiration. 242 VIVA IN MEDICAL PHYSIOLOGY • • The duration of inspiratory sound is at least twice of expiratory sound. The bronchial breath sounds are produced by the passage of air through the trachea and large bronchi. The features of this type of sounds are: Are heard normally over the trachea. Are heard both during inspiration and expiration and are clear, blowing or hollow in character. The inspiratory and expiratory sounds have the same character though the inspiratory sound is harsh and becomes inaudible just before the end of inspiration. Expiratory sound is of high pitch, more harsh and audible throughout the expiration. There is silent gap between end of inspiration and beginning of expiration. The bronchial breath sounds that heard over the trachea is known as Tracheal breath sounds, though the tracheal sounds are much harsher and louder. 13. What is Peurile breathing? In children (and also during exercise) the breath sounds are normally harsher which is termed as peurile breathing. 14. Why the cuff should be placed at the level of the heart while the BP reading is being taken? The pressure in any vessel below heart level is increased and that in any vessel above the heart level is decreased by the effect of gravity. 15. Name the sound on which basis the BP is measured. It is Korotkoff’s sound. 16. Is Korotkoff sound produced in normal vessel? Justify your answer. No, as the blood flow in the vessels are laminar type. When the blood flow through it is converted into turbulent type then only this sound is produced. SECTION II: PRACTICAL VIVA HUMAN EXPERIMENTS 243 17. Which phase of Korotkoff’s sound indicates diastolic pressure? Which one is true diastolic pressure? The last stage or the disappearance of the sound for the 1st time is considered as diastolic pressure. True diastolic pressure is in between the muffling phase of sound and disappearance of sound and close to disappearance of sound for the 1st time, i.e. 2-4 mm Hg higher than the phase where sound 1st disappears. 18. What do you know by auscultatory gap? In some hypertensive patients, there is a silent gap in between the series of Korotkoff sounds. As the mercury column is lowered, a few faint sounds are heard which soon disappear and again reappear at a much lower pressure head. This brief interruption in the sounds is called as auscultatory gap. 19. Why palpatory method is to be adopted before doing auscultatory method? It is for two purposes as follows: • In case of hypertensive patient, there may be auscultatory gap. In this situation, if the mercury column is raised to this gap phases only, one may miss the 1st appearance of sounds which indicates the actual systolic pressure and thus a false low systolic pressure is being recorded. To avoid this palpatory method should be adopted before auscultatory method. • Without having any gross idea of systolic pressure of a person if auscultatory method is adopted then the pressure around the cuff has to be increased in a greater extent (say 150-200 mm Hg) but the person’s real systolic pressure may be much lower (Say 120 mm Hg). In this situation, this extra increase of pressure may cause stress to that subject and thereby false systolic pressure might be recorded. 244 VIVA IN MEDICAL PHYSIOLOGY 20. What is pulse? How can you record it? It is a wave transmitted along the arteries during each heart beat generated by the pressure differences during cardiac cycle. It can be recorded by Dudgeon’s sphygmograph. 21. How does the blood pressure recorded in the femoral artery differs from that in brachial artery? In the normal person (standing posture) the femoral arterial pressure is more than the brachial arterial pressure. This is because that the pressure recorded from brachial or subclavian artery represents the side or lateral pressure as those arteries originate as the side arms from the wall of aorta, whereas the pressure recorded from femoral artery represents the end pressure as the femoral arteries are the direct extensions of the aorta. 22. Why is it important to record the heart rate (pulse rate) while studying the effect of exercise on blood pressure? It is because the effect of exercise on blood pressure varies with the intensity of exercise and heart rate gives us indications about the intensity of exercise. 23. What are the effects of muscular exercise on blood pressure? The effects of muscular exercise on blood pressure depend on whether the muscle contractions are primarily isometric or isotonic. a. In isometric exercise: • The heart rate rises largely due to decreased vagal tone and also due to sympathetic stimulation by psychic stimuli. • Rise of both the systolic and diastolic pressure. • Reduction of blood flow through the contracting muscles due to compression of blood vessels. SECTION II: PRACTICAL VIVA HUMAN EXPERIMENTS 245 b. In isotonic exercise: • Quick rise in heart rate and stroke volume due to generalized sympathetic stimulation. • Increase in cardiac output and systolic pressure. • Net fall in total peripheral resistance. • Diastolic pressure may remain same or may fall or even increase a little. 24. Name some other cardiac efficiency test? It is Treadmill test (TMT). 25. What do you mean by cardiac pulsation and apex beat? Any pulsation in the precordium which is normally due to the forward systolic thrust of the apex of the left ventricle is called as cardiac impulse or cardiac pulsation. Whereas the apex beat is the lowest and outermost point of definite cardiac pulsation which is usually located in the 5th intercostal space 8-10 cm (about 3.5-4 inches) from the mid-sternal line. 26. Is the apex beat visible always in normal person? No, the apex beat may not be always visible in some normal persons because: • It may be located behind the rib. • Thick chest wall due to fat or muscle. • The breast may be pendulous • The emphysematous lung may cover part of the heart. 27. Palpate the apex beat. What is the significance of palpating apex beat? Apex beat is palpated by placing the flat part of the hand over the heart keeping the base of the palm over the base of the heart and the fingers pointing towards the apex. Once the cardiac pulsation is felt the ulnar border of the hand and then the tip of the index finger is used to locate and confirm the point of the apex beat. Significance of the apex beat: The change of the normal position, the force and the nature of the apex beat can give the idea about the status of the heart, e.g.: 246 VIVA IN MEDICAL PHYSIOLOGY • • • • Enlargement of the heart due to hypertrophy or dilatation may shift of the normal position of the apex beat. Pulling and pushing of the mediastinum due to lung disease may shift the position of the apex beat. Diffuse, sustained and more forceful thrust indicates left ventricular hypertrophy or hyperkinetic circulation. A ‘tapping’ or ‘slapping’ apex beat may be seen in mitral stenosis. 28. Which kidney is not generally palpable? It is left kidney. 29. When are the deep reflexes exaggerated? Deep reflexes are exaggerated during: i. Upper motor neuron lesions above the anterior horn cells. ii. Nervousness and anxiety. iii. Hyper excitability of the nervous system as in hyperthyroidism and tetanus. 30. What is reinforcement of reflexes and when it is required? Occasionally the elicitation of deep reflexes like knee jerk is very difficult. In this situation reinforcement is employed by asking the subject to perform some strong muscular efforts like clenching the teeth, etc. while the examiner strikes the patellar tendon. In this situation, reflex is elicited and evident. 31. What is steriognosis? What is the center of it? Ability to recognize a known object by handling with closed eyes is known as steriognosis. The center of steriognosis is sensory association areas of cerebral cortex. 32. What is the most remarkable feature of cerebellar lesions? Clinically can you diagnose the cerebellar lesion? Intention tremor is the most remarkable feature. The cerebellar lesion can be diagnosed by the tests are: SECTION II: PRACTICAL VIVA HUMAN EXPERIMENTS 247 finger nose test, rebound phenomenon test, adiadochokinesis, Heel-knee test. 33. What is Rhomberg’s sign? For what test it is adopted? If a subject is asked to stand with the feet as close together as possible and then asked to close his eyes, in this situation he starts to sway from side to side as soon as he closes his eyes. This test is known as Rhomberg sign positive. It is tested to determine the loss of position sense or sensory ataxia where it is positive. In case of cerebellar ataxia, the patient is unsteady on his feet irrespective of whether the eyes are open or closed. 34. What is Echoencephalograph? It is an instrument used to detect midline displacement caused by space occupying intracranial lesions. 35. Name the reflexes which are of mainly clinical importance. Tendon reflex and pupillary light reflex. 36. What is positive Babinski’s sign? If plantar side of foot is scratched it normally causes dorsiflexion of toes. In lesion of pyramidal tract, the response is extension along with fanning of toes. This is termed as Positive Babinski’s sign which is also normally seen in infants. 37. Name the condition in which the earliest sensory loss is the loss of pain and temperature? Tabes dorsalis. 38. What happens to the muscle tone and tendon reflexes in lower motor neuron paralysis? Muscle tone becomes hypotonic and tendon reflexes become absent. 248 VIVA IN MEDICAL PHYSIOLOGY 39. Which muscle is tested by asking the subject to wrinkle the skin on his forehead? It is oblicularis occuli. 40. Why irritants should not be used while testing for smell sensation? It is because the irritants may produce abnormal stimulation of receptors in the respiratory tract resulting coughing. 41. Define visual field. The area visualized by each of the eye on the screen when the gaze is fixed at an object is called as visual field. 42. What do you mean by binocular vision? What is its importance? The central parts of the visual fields of two eyes coincide, therefore anything in this position of the field is seen with both the eyes called binocular vision. It plays an important role in appreciation of perception of depth and proportion of objects. 43. How do you distinguish between a convex and concave lens without touching them? Keep the lens close to the page of a book and the image of the writing of the book is to be seen through it. If the letters appear enlarged it is a convex lens and if letters appear diminished in size it is a concave lens. 44. Which part of the retina are not tested by perimetry? It is the macular region, which contains the fovea centralis, which is the region of most acute vision. 45. Name any other method of determining the field of vision? It is Confrontation test, which is a rough test to compare a person’s visual fields with the examiner’s own. SECTION II: PRACTICAL VIVA HUMAN EXPERIMENTS 249 46. What is the intensity of the sound of ordinary conversation? It is 50-60 db at 6-8 feet. 47. At which intensity of sound there may be cochlear damage? It is more than 1014 times which is equal to 140 db approximately. 48. What does a vision 6/60 mean? It means subject’s visual acuity is normal, i.e. he /she can be able to read the top letter from the distance of 6 meter. 49. How a decreased visual acuity can be corrected? The decrease in visual acuity can be corrected by using proper lens, e.g.: The myopic vision can be corrected by using concave lens and the hypermetric vision can be corrected by using convex lens. 50. Name the different types of refractive errors. • Physiological: – Spherical aberration – Chromatic aberration – Diffraction • Pathological: – Myopia – Hypermetropia – Astigmatism 51. Is there any role of rods in colour vision? No, there is no role of rods in colour vision. 52. Whichone of the three tests is commonly used for testing colour blindness? It is Ishihara’s chart. 53. For what kind of jobs the proper perception of colours is essential? • Drivers of air, sea, road transport vehicles 250 VIVA IN MEDICAL PHYSIOLOGY • • Workers in textile industries Workers in painting industries. 54. What is the difference between colour anomaly and colour anopia? Anomaly refers to the colour weakness and anopia refers to the colour blindness. 55. Name the unit of sound. Define bel. Decibel is the unit of sound. Bel is the logarithm of the ratio of the power of the sound to the intensity of the reference sound, i.e. Bel = log x Intensity of a given sound/Intensity of a reference (Standard) sound. 56. What are the different tests for hearing? Rinne's test, Weber' test, Schwabach test. 57. What do you mean by Rinne’s test positive? Air conduction if is more than bone conduction it is known as Rinne’s test positive which is considered as normal ear function. 58. Why the sound is heard louder in a ear with conduction deafness, when Weber’s test is performed? It is because of absence of masking effect of noise in the diseased ear. 59. What do you mean by infrasonic, ultrasonic and supersonic sounds? The infrasonic refers to the frequencies of sound below 20 Hz. Ultrasonic refers to the sound frequencies above 20,000 Hz which can not be perceived by the human beings. Whereas the term supersonic refers to the object that can travel at a speed faster than that of sound. 60. Which frequency of sound is most sensitive to human ear? It is 1000-3000 Hz. SECTION II: PRACTICAL VIVA HUMAN EXPERIMENTS 251 61. What are the limitations of tuning fork tests of hearing? • It cannot give quantitative estimation of acuity of hearing. • While testing of bone conduction in one ear is done the subject will also listen the sound in the other ear as the bone conducted vibrations reach all parts of the skull irrespective of site of the head where the tuning fork is placed. This creates confusion to the subject regarding the involvement of one ear or both the ears. 62. What is audiometry? It is the only reliable method to define the nature and degree of hearing loss if any in a patient in which selected pure tones of 125-8000 Hz can be fed into each ear separately and the subjects electrical response is recorded. SECTION III: APPENDIX IMPORTANT VALUES TO REMEMBER I. Blood 1. Hemoglobin • At birth: 22-24 gm% (Avg-22 gm%) • In adults - Male: 13.5-18 gm% (Avg-15.5 gm%) - Female: 11-16 gm% (Avg-14 gm%) 2. RBC count • At birth: 6-7 million/cumm of blood • In adults - Male : 5-6 million/cumm of blood - Female : 4.5-5.5 million/cumm of blood 3. WBC count (Total) • At birth : 20000/cumm of blood • In adults: 4000-11000/cumm of blood 4. WBC count (Differential) • Neutrophil : 50-70% • Eosinophil : 1-4% • Basophil : < 1% • Lymphocyte : 20-40% • Monocyte : 2-8% 5. WBC count (Absolute) • Neutrophil : 3000-6000/cumm of blood • Eosinophil : 150-300/cumm of blood • Basophil : 10-100/cumm of blood • Lymphocyte : 1500-2700/cumm of blood • Monocyte : 300-600/cumm of blood 6. Reticulocyte count: 24000-84000/cumm of blood 7. Platelet count : 2-5 lacs/cumm of blood SECTION III : APPENDIX IMPORTANT VALUES TO REMEMBER 253 8. ESR • Westergren - Male : 3- 5 mm in 1st hour - Female : 5-7 mm in 1st hour • Wintrobe’s - Male : 0-10 mm in 1st hour - Female : 0-20 mm in 1st hour 9. RBC indices • PCV (Hct): - Male : 40-50% - Female : 36-47% • MCV : 78-94 µm3 • MCH : 27-32 pg • MCHC : 30-38% • CI : 0.85-1.15 10. Fragility of red cells • Hemolysis begins : 0.5% NaCl • Hemolysis completes : 0.36% NaCl 11. Bleeding time • Duke’s method : 2-5 min • Ivy’s method : 3-9 min 12. Coagulation time • Capillary blood (Capillary glass tube method): 3-8 min • Venous blood (Lee and White method) : 5-15 min 13. Prothrombin time : 14-18 sec 14. Total blood volume : 5-6 L 15. Specific gravity • Of blood : 1.048-1.066 • Of RBC : 1.092-1.095 • Of plasma : 1.026-1.035 16. Frequency distribution of blood group in INDIA • A blood group : 21% • B blood group : 39% • AB blood group : 9% • O blood group : 31% • Rh positive : 95% • Rh negative : 5% 254 VIVA IN MEDICAL PHYSIOLOGY II. Plasma/Serum 1. Plasma volume • Male: 39 ml/ kgbw • Female: 40 ml/kgbw 2. Osmolality: • Plasma: 285-295 mosm/kg of serum water • ECF: 3000 mosm/L • ICF : 300 mosm/L 3. NPN Substances: 20-30 mg/dl 4. Proteins (Total): 5.5-8 gm/dl • Albumin: 3.5-5 gm/dl • Globulin: 2-3.5 gm/dl • Fibrinogen: 0.2-0.5 gm/dl 5. Amino acids: 6-8 gm/dl 6. Total lipid: 450-1000 mg/dl 7. Cholesterol:120-220 mg/dl 8. Fatty acids: 160-270 mg/dl 9. Triglycerides: 25-150 mg/dl 10. Glucose • Fasting: 80-110 mg/dl • Post-prandial - Normal: 140 mg/dl - Diabetic :> 200 mg/dl 11. Sodium: 135-145 mEq/L 12. Potassium: 3.5-5 mEq/L 13. Chloride: 95-108 mEq/L 14. Bicarbonate: 26-28 mmol/L 15. Calcium : 2.12- 2.62 mEq/l : 8.5-10.5 mg/dl 16. Magnesium: 2-3 mg/dl : 1.5-2.0 mEq/L 17. Phosphate : 2.5-4.5 mg/dl 18. Amylase : 13-53 nmol/L : 60-180 Somogyi unit/dl 19. SGOT: 100-300 μmol/L 20. SGPT: 50-430 μmol/L 21. Alkaline phosphatase: 0.4-1.5 μmol/L SECTION III : APPENDIX IMPORTANT VALUES TO REMEMBER 255 22. Bilirubin • Total (Indirect): Up to 1 mg/dl • Conjugated (direct): Up to 0.4 mg/dl 23. Creatinin: 0.6-1.5 mg/dl 24. Urea: 20-40 mg/dl 25. Uric acid • Male: 3.6-8.5 mg/dl • Female: 2.3-6.6 mg/dl 26. Protein bound iodide: 3.5-8 μg/dl 27. Thyroid binding globulin: 7-17 mg/L 28. Thyroxin: 70-140 nmol/L 29. Tri-iodothyronine: 1.2-3.0 nmol/L III. Cardiovascular System 1. Pressure inside the heart (in mm Hg) • Right Atrium: 0-8 • Right ventricle (Systolic): 15-30 • Right ventricle (Diastolic): 0-8 • Left ventricle (Systolic/Aortic): >150 • Left ventricle (End diastolic): 3-12 • Pulmonary artery (Systolic): 15-30 • Pulmonary artery (End diastolic): 3-12 • Pulmonary capillary: 8 2. Capillary pressure (systemic) Arterial end: 32 mm Hg Venous end: 12 mm Hg Mean: 20 mm Hg 3. Heart rate (resting) • In adult: 60-90 beat/min In infant: 120-140 beat/min 4. Arterial BP (Resting) Systolic: 110-140 mm Hg Diastolic: 60-90 mm Hg Mean: 100 mm Hg 5. Cardiac output: 5-6lit/min 6. Cardiac Index: 2.5-3.6 lit/min/m2 BSA 7. Stroke volume index: 40 ml/sq.m /beat 256 VIVA IN MEDICAL PHYSIOLOGY 8. 9. 10. 11. 12. 13. 14. Stroke volume: 70-90 ml End systolic volume: 50 ml End diastolic volume: 130 ml Coronary blood flow: 225 ml/min Cerebral blood flow: 750 ml/min Renal blood flow: 1300 ml/min Circulation time: Arm to tongue (saccharin): 14.2 ± 2.4 sec Arm to lung (ether): 4-8 sec Arm to foot (radiosodium): 15-105 sec. IV. Respiratory System 1. Inspired air (Atmospheric air) Gas Percentage Partial pressure (mmHg) O2 20.96 160 CO2 0.04 0.15 N2 79 600 2. Alveolar air O2 13.2 101 CO2 5.3 40 N2 75.3 572 Water 6.2 47 3. Expired air O2 15.5 116.5 CO2 3.6 27.5 N2 74 569 Water 6.2 47 4. Arterial blood O2 19.3 100 CO2 48 40 5. Venous blood O2 14.1 40 CO2 52 46 6. Respiratory rate: 12-18 breaths/min 7. Respiratory quotient: 0.8 8. O2 consumption at rest: 250 ml/min SECTION III : APPENDIX IMPORTANT VALUES TO REMEMBER 257 9. O2 diffusion capacity In male : 27-42 ml/min/mmHg In female : 28-30 ml/min/mmHg 10. Tidal volume: 500-800 ml 11. Inspiratory reserve volume: 2000-3300 ml 12. Expiratory reserve volume: 1100 ml 13. Residual volume: 1200 ml 14. Inspiratory capacity: 3500 ml 15. Expiratory capacity: 1600 ml 16. Functional residual capacity: 2200 ml 17. Vital capacity In male : 4500-5500 ml In female : 3500-4500 ml 18. Total lung capacity: 5700 ml 19. Pulmonary ventilation (RMV): 6-7 lit/min 20. Alveolar ventilation: 4.9 lit/min 21. Maximum voluntary ventilation: • In male : 150-170 lit/min • In female : 80-100 lit/min 22. FEV1: 75-85% 23. Doesponic index: 60-70 % 24. Respiratory dead space volume: 150 ml 25. Lung compliance: • Lungs alone : 220 ml/cm of water • Lungs and Thorax : 130 ml/cm of water 26. O2 transported through plasma: 0.3 ml/100 ml of blood/ 100 mmHg PO2 27. O2 carrying capacity of blood: 20 ml of O2 28. CO2 transport Through plasma: 0.3 ml/100 ml of blood (7%) • Through bicarbonate: 3 ml/100 ml of blood (70%) • Through carbamino compound: 0.7 ml/100 ml of blood (0.7%) V. Excretory System 1. No. of nephron/Kidney: 1 million 2. GFR : 125 ml/min (180 L/day) 258 VIVA IN MEDICAL PHYSIOLOGY 3. Renal fraction: 12-30% 4. TmG of glucose: In male: 300-450 mg/min In female: 250-350 mg/min 5. Inulin clearence: In male: 124 ± 25.8 ml/min In female: 119 ± 12.8 ml/min 6. Creatinine clearence: 91-130 ml/min 7. PAH clearence (Renal plasma flow): In male: 560 ± 630 ml/min In female: 490 ± 700 ml/min 8. Urea clearence: Maximal clearence : 60-90 ml/min Standard clearence : 40-65 ml/min VI. Reproductive System 1. Volume of semen: 3.1 ml 2. Fructose content of semen: 40-400 mg /dl 3. Duration of spermatogenesis: approx. 74 days 4. Testosterone production: 10 mg/day 5. Duration of menstrual cycle: 28 ± 4 days 6. Duration of menstrual blood flow: 3-5 days 7. Menstrual blood loss: 10-55 ml 8. Menarche: 9-16 years 9. Menopause: 45-50 years 10. Gestational period: 280 days VII. Cerebrospinal fluid: 1. Volume : 100-150 ml 2. Pressure: • In Newborn: 30-80 mm of water • In adult : 70-200 mm of water 3. Glucose content: 40-80 mg /dl 4. Rate of formation of CSF: 500-800 ml/day