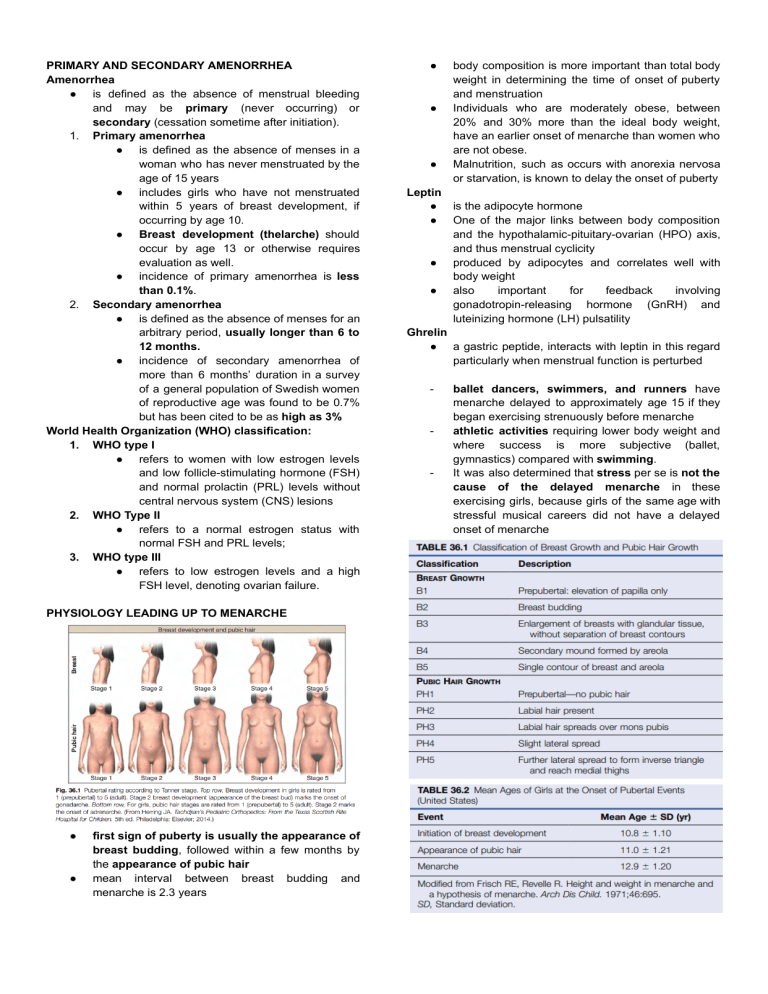
PRIMARY AND SECONDARY AMENORRHEA Amenorrhea ● is defined as the absence of menstrual bleeding and may be primary (never occurring) or secondary (cessation sometime after initiation). 1. Primary amenorrhea ● is defined as the absence of menses in a woman who has never menstruated by the age of 15 years ● includes girls who have not menstruated within 5 years of breast development, if occurring by age 10. ● Breast development (thelarche) should occur by age 13 or otherwise requires evaluation as well. ● incidence of primary amenorrhea is less than 0.1%. 2. Secondary amenorrhea ● is defined as the absence of menses for an arbitrary period, usually longer than 6 to 12 months. ● incidence of secondary amenorrhea of more than 6 months’ duration in a survey of a general population of Swedish women of reproductive age was found to be 0.7% but has been cited to be as high as 3% World Health Organization (WHO) classification: 1. WHO type I ● refers to women with low estrogen levels and low follicle-stimulating hormone (FSH) and normal prolactin (PRL) levels without central nervous system (CNS) lesions 2. WHO Type II ● refers to a normal estrogen status with normal FSH and PRL levels; 3. WHO type III ● refers to low estrogen levels and a high FSH level, denoting ovarian failure. PHYSIOLOGY LEADING UP TO MENARCHE ● ● first sign of puberty is usually the appearance of breast budding, followed within a few months by the appearance of pubic hair mean interval between breast budding and menarche is 2.3 years ● ● ● Leptin ● ● ● ● body composition is more important than total body weight in determining the time of onset of puberty and menstruation Individuals who are moderately obese, between 20% and 30% more than the ideal body weight, have an earlier onset of menarche than women who are not obese. Malnutrition, such as occurs with anorexia nervosa or starvation, is known to delay the onset of puberty is the adipocyte hormone One of the major links between body composition and the hypothalamic-pituitary-ovarian (HPO) axis, and thus menstrual cyclicity produced by adipocytes and correlates well with body weight also important for feedback involving gonadotropin-releasing hormone (GnRH) and luteinizing hormone (LH) pulsatility Ghrelin ● a gastric peptide, interacts with leptin in this regard particularly when menstrual function is perturbed - - - ballet dancers, swimmers, and runners have menarche delayed to approximately age 15 if they began exercising strenuously before menarche athletic activities requiring lower body weight and where success is more subjective (ballet, gymnastics) compared with swimming. It was also determined that stress per se is not the cause of the delayed menarche in these exercising girls, because girls of the same age with stressful musical careers did not have a delayed onset of menarche ● ● ● ● ● ● 1. 2. 3. 4. 5. 6. metabolic features of amenorrheic athletes, who are considered to be in a state of negative energy balance, are fairly characteristic. These include elevated serum FSH and insulinlike growth factor-binding protein 1 (IGFBP-1) and lowered insulin-like growth factor (IGF) levels. Emotional stress can lead to inhibition of the GnRH axis. The mechanism involves an increased secretion of corticotropin releasing hormone (CRH), releasing adrenocorticotropic hormone (ACTH), opioid peptides such as beta-endorphin, and cortisol. CRH itself is known to inhibit GnRH. Before puberty, circulating levels of LH and FSH are low, with an FSH/LH ratio greater than 1 CNS-hypothalamic axis is extremely sensitive to the negative feedback effects of low levels of circulating estrogen. As the critical weight or body composition is approached, the CNS-hypothalamic axis becomes less sensitive to the negative effect of estrogen and GnRH is secreted in greater amounts, causing an increase in LH and, to a lesser extent, FSH levels. This release from the prepubertal “brake” on GnRH secretion is depicted in Fig. 36.4, which also illustrates the integral role of neuropeptides such as kisspeptin The initial endocrinologic change associated with the onset of puberty is the occurrence of episodic pulses of LH during sleep These pulses are absent before the onset of puberty. After menarche, the episodic secretions of LH occur during sleep and while awake. The last endocrinologic event of puberty is activation of the positive gonadotropin response to increasing levels of estradiol (E2), which results in the midcycle gonadotropic surge and ovulation PRIMARY AMENORRHEA Causes Breasts Absent and Uterus Present ● breast development is a biomarker of ovarian estrogen production ○ no breast development and a uterus present = no estrogen production Gonadal Failure (Hypergonadotropic Hypogonadism) ● Failure of gonadal development - most common cause of primary amenorrhea ● Gonadal failure ○ most commonly caused by a chromosomal disorder or deletion of all or part of an X chromosome, ○ chromosomal genetic defect and, rarely, defective CYP-17 leading to 17a-hydroxylase deficiency ● Not inherited ● Pure gonadal dysgenesis ○ 46,XX ○ gonadal development is absent ○ + gene disorder - inherited, can occur in siblings ● cardiovascular or renal anomalies ● shorter stature ○ Turner syndrome - deletion of the entire X chromosome ○ Deletion of the short arm (p) of the X chromosome ○ ● ● ● ● ● ● - - Deletions of only the long arm (q) usually do not affect height Gonadal streak ○ In place of the ovary a band of fibrous tissue When ovarian follicles are absent, synthesis of ovarian steroids and inhibin does not occur. Breast development does not occur because of the low circulating E2 levels. Because the negative hypothalamic-pituitary action of estrogen and inhibin is not present, gonadotropin levels are markedly elevated, with FSH levels being higher than LH. Estrogen is not necessary for müllerian duct development or wolffian duct regression, so the internal and external genitalia are phenotypically female. An occasional individual with mosaicism, an abnormal X chromosome, pure gonadal dysgenesis (46,XX), or even Turner syndrome (45,X) may have a few follicles that develop under endogenous gonadotropin stimulation early in puberty and may synthesize enough estrogen to induce breast development and a few episodes of uterine bleeding, resulting early in premature ovarian failure, usually before age 25. Rarely, ovulation and pregnancy can occur. primary amenorrhea and plasma FSH levels higher than 40 mIU/mL - no functioning ovarian follicles in the gonadal tissue. diagnosis of gonadal failure primary amenorrhea + FSH levels are consistently elevated, without requiring ovarian tissue evaluation. 45,X and Related Abnormalities ● Turner syndrome (45,X) ○ 1 per 2000 to 3000 live births but is much more common in abortuses. ○ primary amenorrhea ○ absent breast development, ○ other somatic abnormalities ■ short stature (< 60 inches in height ■ webbing of the neck ■ short fourth metacarpal ■ cubitus valgus. ○ Cardiac abnormality, renal abnormalities, and hypothyroidism are also more prevalent. ● chromosomal mosaics ○ X/XX - most common ■ with primary amenorrhea ■ normal female external genitalia ○ X/XXX and X/XX/XXX ■ primary amenorrhea ■ generally taller ■ fewer anatomic abnormalities than individuals with a 45,X karyotype ○ ● some of them may have a few gonadal follicles and ~ 20% have sufficient estrogen production to menstruate ○ ovulation may occur Noonan syndrome ○ Isolated phenotypic features of Turner syndrome (without gonadal failure) in males Structurally Abnormal X Chromosome ● 46,XX karyotype but part of one X chromosome is structurally abnormal ● Deletion of long arm (Xq) ○ Normal height ○ No somatic abnormalities ● Deletion of short arm (Xp) ○ Individual is short ● isochromosome of the long arm of X chromosome ● Other X chromosome abnormalities ○ Ring X ○ Minute fragmentation of the X chromosome Pure Gonadal Dysgenesis (46,XX and 46,XY With Gonadal Streaks) ● may have a familial/genetic association (siblings) ● normal stature and phenotype ● absence of secondary sexual characteristics ● primary amenorrhea ● Some have a few ovarian follicles, develop breasts, and may even menstruate spontaneously for a few years a. 46,XY gonadal dysgenesis abnormal testis in utero incomplete forms with some degree of testicular tissue “pure” form as a dysgenetic streak, Swyer syndrome. If a Y chromosome is present or is found as part of a mosaic karyotype, with or without any clinical signs of androgenization, gonadectomy should be performed 17a-Hydroxylase Deficiency with 46,XX Karyotype ● Rare ● primary amenorrhea without breast development ● normal female internal genitalia ● can also occur in genetic males 46,XY ● hypernatremia and hypokalemia ● ● ● ● ● ● Decreased cortisol, elevated ACTH Elevated mineralocorticoids ○ because 17a-hydroxylase is not necessary for the conversion of progester- one to deoxycortisol or corticosterone. excessive sodium retention and potassium excretion, leading to hypertension and hypokalemia Elevated serum progesterone (not converted to cortisol cystic ovaries and viable oocytes. Tx: sex steroid replacement and cortisol administration Genetic Disorders with Hyperandrogenism ● Hyperandrogenism ~ 10% of women with gonadal dysgenesis. ● Most have Y chromosome or a fragment of it. ● Some may only have DNA fragment that contains SRY gene without full Y chromosome ● Those with hypergonadotropic hypogo- nadism and a female phenotype who have any clinical manifestation of hyperandrogenism, such as hirsutism, should have a gonadectomy, even if a Y chromosome is not present, because gonadal neoplasms are common. CNS-Hypothalamic-Pituitary Disorders ● low estrogen levels are caused by an abnormal or absent signal to the ovary resulting in very low circulating gonadotropin levels. ● cause of low gonadotropin production may be morphologic or endocrinologic a. CNS lesions anatomic lesion of hypothalamus/pituitary gonadotropin. Can be congenital or acquired Pituitary adenoma → elevated PRL levels Chromophobe adenomas and craniopharyngiomas → PRL not elevated , rarely cause of primary amenorrhea with low gonadotropin levels Primary amenirrha + gonadotropin +/prolactin - CT scanning or MRI of the hypothalamic pituitary region to r/o cns lesion ⬇️ ⬆️ b. ⬇️ Inadequate GnRH Release (Hypogonadotropic Hypogonadism) gonadotropin w/o lesion Thought to be primary pituitary failure hypothalamic defect with insufficient GnRH synthesis or a CNS neurotransmitter defect, resulting in inadequate GnRH synthesis abnormal kisspeptin anosmia - specific defect of the KAL gene (Xp 22-3) ⬇️ - Females with Kallmann syndrome and related forms of gonadotropic deficiency normal height growth of long bones (greater wingspan-to-height ratio) Men hypogonadism wingspan-to-height ratio altered spatial orientation abilities. Have tendency to be familial/ inherited Majority are sporadic Responds to GnRH administration ⬆️ - ⬆️ c. Isolated Gonadotropin Deficiency (Pituitary Disease) do not respond to GnRH thalassemia major (with iron deposits in the pituitary) or retinitis pigmentosa. prepubertal hypothyroidism, kernicterus, or mumps encephalitis. d. Estrogen resistance mutation in estrogen receptor alpha (ER ∝) does not allow estrogen signaling or a biologic response to estrogen action. endogenous estrogen gonadotropins (to try to provoke an estrogen response) ovaries are cystic Exogenous estrogen does not normally induce changes ⬆️ ⬆️ BREAST ABSENT DEVELOPMENT PRESENT AND UTERUS Androgen resistance X-linked recessive or sexlinked AD disorder “testicular feminization” androgen receptor synthesis or action does not occur absence of an X-chromosome gene responsible for cytoplasmic or nuclear testosterone receptor function XY karyotype w/ normally functioning male gonads that produce normal male levels of testosterone and dihydrotestosterone Lack of receptors in target organs lack of male differentiation of the external and internal genitalia External genitalia remains feminine Wolffian duct development Usually due to testosterone stimulation but fails to take place women with this disorder have no female or male internal genitalia, normal female external genitalia short or absent vagina Pubic hair and axillary hair are absent or scanty as a lack of androgenic receptors breast development is normal or enhanced testosterone is responsible for inhibiting breast proliferation. ➡️ ⬅️ - - Thus with androgen resistance, the absence of androgen action allows even low levels of estrogen to cause unabated breast stimulation Estrogen - normal male range LH is slightly elevated. Testes that are intraabdominal or that occur in the inguinal canal have an increased risk of developing a malignancy (gonadoblastoma or dysgerminoma) → must be removed after age 18 Congenital Absence of the Uterus Uterine Agenesis Uterovaginal Agenesis, Mayer-Rokitansky -Küster-Hauser Syndrome Hox genes are important for uterine development, and mu- tations (e.g., in HOXA13) No pattern of inheritance 2nd most common cause of primary amenorrhea Complete Uterine Agenesis normal ovaries regular cyclic ovulation normal endocrine function normal breast and pubic and axillary hair development shortened or absent vagina Absent uterus On occasion one or both rudimentary horns may have some functioning endometrium. obstructed outflow, cyclic pelvic pain may be encountered. Majority are caused by an isolated developmental defect Vs. androgen resistance: normal pubic hair normal endocrinologically; able to have children (surrogate or gestational carrier) ABSENT BREAST AND UTERINE DEVELOPMENT ● Rare ● male karyotype ● gonadotropin ● testosterone: normal or below-normal female range ⬆️ ● Differential diagnosis: 1. 17a-hydroxylase deficiency Present testes Female external genitalia 2. 17,20-desmolase deficiency 3. agonadism Aka vanishing testes syndrome no gonads present SECONDARY SEX CHARACTERISTICS (BREATS) PRESENT AND FEMALE INTERNAL GENITALIA (UTERUS) PRESENT second largest category of individuals with primary amenorrhea 25% + hyperprolactinemia and prolactinomas PCOS PRIMARY AMENORRHEA WITH ABSENT ENDOMETRIUM ● Rare ● Normal Endocrine function, uterus, ovaries, and fallopian tubes ● absent endometrium Differential Diagnosis and Management ● If breasts are absent but a uterus is present, the diagnostic evaluation should differentiate between CNS-hypothalamic-pituitary disorders and failure of normal gonadal development. ○ similar phenotypes because of low E2 levels ○ single serum FSH assay can differentiate between these two ● hypergonadotropic hypogonadism (FSH . 40 mIU/mL) ○ peripheral WBCl karyotype to check presence of Y chromosome ○ If present, streak gonads should be excised ○ If absent, it is unnecessary to remove the gonads unless there are signs of hyperandrogenism ● elevated FSH level and an XX karyotype - measure electrolyte and serum progesterone levels to rule out 17a-hydroxylase deficiency ● Women with ovarian failure or hypergonadotropic hypogonadism who wish to become pregnant may undergo egg donation ● Turner syndrome - cardiac evaluation is mandatory before pregnancy because of potential risks such as aortic dissection ● rare individuals without breast development and no internal genitalia should be referred to an endocrine center for the extensive evaluation necessary to establish the diagnosis SECONDARY AMENORRHEA Causes ● amenorrhea w/o galactorrhea, hyperprolactinemia, or hirsutism disorders in the CNS (hypothalamic-pituitary axis), ovary, or uterus. ● uterine cause of secondary amenorrhea - normal endocrine function Uterine Factor ● Intrauterine adhesions (IUAs) or synechiae ● Asherman syndrome ○ can obliterate the endometrial cavity and produce secondary amenorrhea Pregnancy complication, prior instrumentation, or, rarely, endometrial tuberculosis most common cause: endometrial curettage associated with pregnancy (evacuation of a live or dead fetus) diagnostic dilation and curettage (D&C) in a nonpregnant woman severe endometritis or fibrosis after a myomectomy, metroplasty, or cesarean delivery Confirmation of dx - hysterosalpingogram ■ ● ● ● CNS and Hypothalamic Causes ● CNS Structural Abnormalities ○ interfering with GnRH release ○ Hypothalamic lesions: craniopharyngiomas, granulomatous disease (tuberculosis, sarcoidosis), and sequelae of encephalitis. gonadotropins and ○ E2 ○ withdrawal uterine bleeding will not occur after progesterone administration ● Drugs ○ Phenothiazine derivatives, certain antihypertensive agents - amenorrhea without hyperprolactinemia ○ Oral contraceptive steroids ■ acting on the hypothalamus to suppress GnRH ■ directly on the pituitary to suppress FSH and LH ■ inhibit ovulation ○ postpill amenorrhea syndrome ■ hypothalamic pituitary suppression persists for several months after oral contraceptives are discontinued ⬇️ ⬇️ oral contraception–induced suppression should not last longer than 6 months Stress and Exercise ○ Stressful situations, including a sudden change in a normal routine, can produce amenorrhea ○ amenorrheic athletes ran more miles weekly ○ Both stress and exercise can increase brainderived factors that can inhibit GnRH release ( CRH, opioid peptides etc.) Weight Loss ○ malnourished reproductive capacity ○ associated with amenorrhea in women ■ moderately underweight: 15% to 25% less than ideal body weight ■ severely underweight: > 25% of ideal body weight ○ excessive dietary restrictions, malnutrition ○ anorexia nervosa ○ women with amenorrhea associated with simple weight loss have direct and indirect evidence of hypothalamic dysfunction ○ failure of normal GnRH release, with the lack of a pituitary response under extreme conditions. ○ Hypoleptinemia, alterations in ghrelin, and GH and thyroid dysfunction Polycystic Ovary Syndrome ○ prolonged periods of amenorrhea ○ irregularity or oligomenorrhea - more common ○ need not be overweight or obese, or have symptoms and signs of hyperandrogenism ○ elevated serum LH ■ normal in obese ■ Not a diagnostic criterion ○ diagnosis of PCOS may be confirmed by visualizing polycystic ovaries on ultrasound ○ Rotterdam criteria for the diagnosis of PCOS, women may be diagnosed as having PCOS with only the menstrual disturbance (in this case amenorrhea) and polycystic ovaries seen with ultrasound. mens disturbance, UTZ ■ ⬆️ ➕ ● ⬇️ ➖ Functional Hypothalamic Amenorrhea ○ no anatomic abnormalities ○ not on drugs ○ no history of excessive exercise, stress, or large changes in body ○ alteration of hypothalamic GnRH release ○ No cyclic alterations in LH pulsatility ■ no pulses ■ Or persistent pulsatility ○ stress-induced hypothalamic amenorrhea ■ hypnotherapy and cognitive behavior therapy - restore ovarian activity ○ ○ ○ severity of the hypothalamic suppression can be assessed by a sensitive assay for E2 ■ < 30pg/mL significant hypoestrogenism ■ <20 pg/mL - after menopause If endogenous E2 has been sufficient to allow the endometrium to proliferate, then progestogen administration will result in withdrawal bleeding ■ determined by visualizing the endometrial stripe by ultrasound ■ < 4 mm = hypoestrogenism polycystic ovaries on UTZ 25% FHA = ➕ Pituitary Causes (Hypoestrogenic Amenorrhea) ● Neoplasms ○ most pituitary tumors secrete PRL ○ Chromophobe adenomas most common non–PRL-secreting pituitary tumors ○ Basophilic (ACTH-secreting) and acidophilic (GH-secreting) adenomas may not secrete PRL ○ symptoms of acromegaly or Cushing disease ○ ● Nonneoplastic Lesions ○ Pituitary cells - become damaged or necrotic as a result of anoxia, thrombosis, or hemorrhage ○ Sheehan syndrome - pituitary cell destruction caused by hypotensive episode during pregnancy ○ Simmonds disease - unrelated to pregnancy ○ pituitary damage ACTH and TSH ■ LH and FSH. ■ ○ ○ ● ● ● ● ● ● ● Occurs before age 40 ovaries cease to produce sufficient estrogen to stimulate endometrial growth several years before the age of physiologic menopause ○ two types of ovarian pathologic findings ■ generalized sclerosis similar to the findings of a normal postmenopausal ovary ■ 30%, numerous primordial follicles with no progression past the early antrum stage are seen, which looks identical to a normal ovary gonadotropin-resistant ovary syndrome ○ a gonadotropin receptor defect ○ primary amenorrhea ○ but usually sufficient estrogen is produced so that they menstruate for several months or even years autoimmune process with autoimmune diseases ○ Hypoparathyroidism ○ Hashimoto thyroiditis ○ Addison disease. It is recommended that immunologic screening be performed in young women with POI. CBC, comprehensive metabolic panel, TSH and antithyroid antibody levels adrenal antibodies (against 21-hydroxylase) and cortisol levels ACTH stimulation test general screen for adrenal function by obtaining levels of dehydroepiandrosterone sulfate (DHEAS) Diagnostic Evaluation and Management ⬇️ ⬇️ ➡️⬇️ Ovarian Causes (Hypergonadotropic Hypogonadism) estrogen secretion by ● Damaged follicles no endometrial growth ovaries ● follicles are damaged due to ○ infection ○ interference with blood supply ○ depletion of follicles caused by bilateral cystectomies ● amenorrheic after ○ medical treatment of bilateral tubo-ovarian abscess ○ bilateral cystectomy ○ benign ovarian neoplasms ○ hysterectomy ■ during which the vascular supply to the ovaries is compromise (AKA cystic degeneration of the ovaries) ● premature ovarian failure (POF) or premature ovarian insufficiency (POI) ○ premature menopause ➡️ ● ● instrumentation of the endometrial cavity, particularly temporally related to pregnancy, should alert to the possibility of IUA History and PE: ○ ● ● ● ● ● ● ● medications currently being used or if oral contraceptives have been recently discontinued ○ questions regarding diet, weight loss, stress, and strenuous exercise are pertinent ○ history of hot flushes, decreasing breast size, or vaginal dryness CBC, urinalysis, and serum chemistries should be carried out to rule out systemic disease sensitive TSH assay, serum E2, FSH, and PRL should be measured Insulin tolerance test To rule out mosaicism or a dysgenetic gonad, including the possibility of a Y cell line, a karyotype should be obtained in women with POF who are aged 25 years or younger. Women with anovulation, including those with PCOS, who desire conception ○ may be treated with clomiphene citrate or letrozole, which are effective for inducing ovulation. ○ Clomiphene is not successful if the estrogen levels are low woman with more severe hypothalamic-pituitary suppression (low estrogen levels) desires fertility, ○ ovulation can be induced with exogenous gonadotropins or pulsatile GnRH. Young women with POI and those with a chronic hypoestrogenic state are also vulnerable to accelerated atherosclerosis and diabetes and have been found to have increased all-cause mortality. PRECOCIOUS PUBERTY ● sequence of the physiologic events of puberty ○ Begins with breast development ○ subsequent appearance of pubic and axillary hair ○ followed by the period of maximal growth velocity ○ finally, menarche ● Menarche ○ may occur before the appearance of axillary or pubic hair in 10% of normal females ● growth velocity ○ before breast development the is → 6 cm/year ○ Peak height velocity, around age 12 → velocity is around 8 cm/year ○ by the completion of puberty, around age 14, the velocity is down to 1 cm/year, explained by closure of the epiphyses ● Precocious puberty ○ defined as the appearance of any signs of secondary sexual maturation at an early age ○ girls with breast development or pubic hair should be evaluated when these signs occur before age 7 in white girls and age 6 in black girls ○ ○ ○ ○ ● carry out a complete evaluation of precocious puberty at age 8 years associated with a wide range of disorders US incidence: 1 in 10,000 young girls two primary concerns ■ social stigma associated with the child being physically different from her peers ■ diminished ultimate height caused by the premature closure of epiphyseal growth centers Puberty ○ time of accelerated growth, skeletal maturation, and resulting epiphyseal closure. Types of Disorders ● Precocious puberty is subdivided into GnRH dependent (complete, true) and GnRH independent (incomplete, pseudo), and these causes have been subcategorized as feminizing (previously termed isosexual) or virilizing (previously termed heterosexual) Disorders. ● The pathophysiology of precocious puberty is divided into two distinct categories: a normal physiologic process involving GnRH secretion with an integrated hypothalamic-pituitary axis, which occurs at an abnormal time, or an abnormal physiologic process independent of an integrated HPO axis. ● GnRH-dependent precocious puberty involves premature maturation of the HPO axis and includes normal menses, ovulation, and the possibility of pregnancy. GnRH-independent precocious puberty involves premature female sexual maturation, which may lead to estrogen-induced uterine stimulation and bleeding without any normal ovarian follicular activity. ● The majority of girls with precocious puberty (70%) develop a GnRH-dependent process. ● A definitive diagnosis is established more often for pseudoprecocious puberty, which is usually related to an ovarian or adrenal disorder. ● If the secondary sex characteristics are discordant with the genetic and phenotypic gender, the condition is termed heterosexual or virilizing precocious puberty. ● This is premature virilization in a female child and includes development of masculine secondary sexual characteristics. ● The androgens that cause heterosexual (virilizing) precocious puberty usually come from the adrenal gland. Premature Thelarche ● Premature thelarche is defined as isolated unilateral or bilateral breast development as the only sign of secondary sexual maturation. ● It is not accompanied by other associated evidence of pubertal development, such as axillary or pubic hair or changes in vaginal epithelium. ● Estrogen levels are normal (prepubertal) together with estrogen levels in pubertal girls, those with precocious puberty and adults ● Breast hyperplasia is a normal physiologic phenomenon in the neonatal period and may persist until the child is up to 6 months of age. ● Premature thelarche usually occurs in two waves: within the first 2 years, and between ages 6 and 8. ● ● Premature Pubarche or Adrenarche ● Premature pubarche is early isolated development of pubic hair without other signs of secondary sexual maturation. ● Premature adrenarche is isolated early development of axillary hair. ● Neither of these conditions is progressive, and the girls do not have clitoral hypertrophy; however, it is important to differentiate premature pubarche from the virilization produced by congenital adrenal hyperplasia. ● Similar to premature thelarche, the child should have periodic follow-up visits to confirm that the condition is not progressive. ● Many cases of premature adrenarche evolve into PCOS. ● Measurements of testosterone and 17-hydroxyprogesterone should also be carried out to rule out other conditions. Central Precocious Puberty (GnRH Dependent) Idiopathic ● Idiopathic development is responsible for approximately 80% of the cases of GnRH-dependent precocious puberty. ● Some of these children are simply at the earliest limits of the normal distribution of the biologic curve. ● A high incidence of abnormal EEGs in children with idiopathic precocious puberty has raised the question of potential CNS disease. ● These girls have no genital abnormality except for early development. ● Occasionally, follicular cysts of the ovary may form secondary to increased pituitary gonadotropin levels. ● In these cases the cysts are the result, not the cause, of precocious puberty. ● LH responses suggesting GnRH dependency are more than 5 mIU/mL. CNS Lesions ● A wide range of inflammatory, degenerative, neoplastic, or congenital defects that involve the CNS may produce GnRH-dependent precocious puberty. ● This occurs in up to 20% of cases and warrants a careful evaluation by imaging. ● Usually, symptoms of a neurologic disease, especially headaches and visual disturbances, precede the manifestations of precocious puberty. Primary Hypothyroidism ● Hypothyroidism is usually associated with delayed pubertal development; however, in rare cases, untreated hypothyroidism results in GnRH-dependent precocious puberty. ● The hypothyroidism associated with precocious puberty is caused by primary thyroid insufficiency, usually Hashimoto thyroiditis, and not by a deficiency in pituitary TSH. ● The pathophysiology of this syndrome is a result of the diminished negative feedback of thyroxine, resulting in an increased production of TSH, which may be accompanied by an increase in production of gonadotropins. Interestingly, hypothyroidism is the only cause of precocious puberty in which the bone age is retarded. This syndrome is usually observed in girls between the ages of 6 and 8 years. Peripheral (GnRH-Independent) Precocious Puberty ● The most common cause of pseudo- or feminizing precocious puberty is an estrogen-secreting ovarian cyst or large functioning follicle. ● Granulosa cell tumors are the most common type of solid ovarian tumor resulting in precocious puberty. ● Adrenocortical neoplasms may produce isosexual (feminizing) or heterosexual (virilizing) precocious puberty. ● The relationship between congenital adrenal hyperplasia and puberty depends on the time of initial diagnosis and therapy. ● In this category, apart from adrenal imaging, measurements of steroids to rule out the various forms of adrenal hyperplasia caused by enzymatic deficiencies (e.g., 21- or 11b-hydroxylase or 3 b-ol dehydrogenase) should be carried out. ● McCune-Albright syndrome (MAS) is a rare condition caused by a mutation in the G3 protein leading to activation of adenylate cyclase. ● Iatrogenic or factitious precocious puberty results when a young girl has used hormone cream or ingested adult medications such as oral estrogen or birth control pills. Diagnostic Evaluation ● The diagnostic workup of a young child with precocious puberty begins with a meticulous history and physical examination. ● The primary emphasis should be to rule out life-threatening neoplasms of the ovary, adrenal gland, or CNS. ● The secondary emphasis is to delineate the speed of the maturation process because this is crucial in making decisions concerning therapy. ● The height of the girl and exact stage of pubertal development, including Tanner stage, should be recorded. ● Acceleration of growth is one of the earliest clinical features of precocious puberty. ● Thus bone age should be determined by hand-wrist films and compared with standards for a patient’s age. ● Diseases of the CNS are suggested by symptoms such as headaches, seizures, trauma to the head, and encephalitis. ● Hypothalamic hamartomas can be categorized based on the tumor topology on MRI. ● Serum levels of LH, PRL, TSH, E2, testosterone, DHEAS, HCG, androstenedione, 17-hydroxyprogesterone, triiodothyronine (T3), and thyroxine (T4) may be of value in establishing the differential diagnosis. ● A GnRH agonist stimulation test is diagnostic in differentiating incomplete from true precocious puberty as described previously, but it does not specifically identify children with CNS lesions. Treatment ● The treatment of precocious puberty depends on the cause, extent, and progression of precocious signs and whether the cause may be removed operatively. ● The goals of therapy are to reduce gonadotropin secretion and reduce or counteract the peripheral actions of the sex steroids, decrease the growth rate to normal, and slow skeletal maturation to allow development of maximal adult height. ● The present drug of choice for GnRH-dependent precocious puberty is one of the potent GnRH agonists, which have been studied extensively. ● Although 3-month regimens are available, therapy usually begins with a once-per-month preparation at a dose of 0.3 mg/kg of leuprolide or its equivalent. ● Leuprolide acetate can be administered at doses of 7.5 mg, 11.25 mg, and 15 mg; the larger dose can be used if there is evidence for pubertal progression despite treatment. ● Treatment usually continues until around age 11. ● McCune-Albright syndrome is caused by an activating mutation of a G protein that is coupled with gonadotropin receptors, resulting in the ovaries being stimulated autonomously. ● Girls may be treated with aromatase inhibitors (anastrozole, letrozole), which prevent the conversion to biologically active estrogens. ● Unfortunately this treatment has had limited success, as has the use of tamoxifen. ● The child with precocious puberty and her family need intensive counseling. ● The child will have the psychosocial and behavioral maturation of children of her chronologic age, not the age reflected by her physical appearance. ● She may be exposed to ridicule by her peers and to sexual exploitation. ● Thus the child needs extensive sex education and help in anticipating and confronting various social experiences. CHAPTER 37 HYPERPROLACTINEMIA: Evaluation and Management Prolactin is a polypeptide hormone containing 198 amino acids and with a molecular weight of 22 kDa. ● It circulates in 2 different molecular sizes: ○ Monomeric form- small (MW of 22 kDa) ■ Biologically active; approx. 80% of the hormone is secreted in this form. ○ Polymeric form - big (MW of 50 kDa) ■ Big PRL is presumed to be a dimer ○ Larger polymeric form - big big (MW of >100 kDa) ■ Big-big PRL may present an aggregation of monomeric molecules. ■ Also contain added sugar moieties (glycosylation) – decreases biologic activity. ● PRL is synthesized and stored in the pituitary gland in chromophobe cells called lactotrophs. ○ Encoded by its gene (10kb) on chromosome 6 ○ Main function: to stimulate the growth of mammary glands tissue and to produce and secrete milk into the alveoli; thus it has mammogenic and lactogenic functions. ○ TRH or thyroid-releasing is the principal stimulating factor. ○ Dopamine (Prolactin inhibiting factor or PIF) is the major inhibiting factor. ○ Estrogen also improves PRL secretion by enhancing the effects of TRH and inhibiting the effects of dopamine ○ A potential direct effect may also be mediated by galanin. ○ D2 is the principal receptor with which dopamine interacts ■ Also the target for various dopamine agonists used in the treatment of hyperprolactinemia. ○ Normal measurable amounts in adult women: serum PRL of approx. 8 ng/ml ○ Specific receptors: present in the plasma membrane of mammary cells and in many other tissues. Physiology ● PRL synthesis and release from the lactotrophs are controlled by central nervous system neurotransmitters – which act on the pituitary via the hypothalamus. ● Inhibition is the major mechanism because pituitary stalk section results in increased PRL secretion. ● There are specific dopamine receptors on the lactotrophs, and dopamine inhibits PRL synthesis and release in pituitary cell cultures. ● ● ● ● ● ● ● ● Serotonin and thyrotropin-releasing factors stimulate PRL release of prolactin. TRF stimulates PRL release only minimally unless infused Serotonin ○ is a PRF or is responsible for secretion of PRL ○ It also controls the rise of PRL levels during sleep. PRL is secreted episodically and serum levels fluctuate throughout the day and throughout the menstrual cycle, with peak levels occurring at midcycle. Although changes in PRL levels are not as marked as the pulsatile episodes of luteinizing hormone (LH), estrogen stimulates PRL production and release. ○ At puberty: Estrogen increases PRL levels increase in girls ○ After menopause: there is a slight decline in PRL During pregnancy: ○ As estrogen levels increase, there is a concomitant hypertrophy and hyperplasia of the lactotrophs. ○ The maternal increase in PRL levels occurs soon after implantation, concomitant with the increase in circulating estrogen. ○ Circulating levels of PRL steadily increase throughout pregnancy, reaching approximately 200 ng/mL in the third trimester ■ the rise is directly related to the increase in circulating levels of estrogen ■ however, there is a wide range of values of PRL in pregnancy, and values as high as 400 ng/mL can be found in normal pregnancy ○ Lactation does not occur during pregnancy despite elevated PRL levels because estrogen inhibits the action of PRL on the breast by blocking the PRL’s interactions with its receptor. ○ 1 or 2 days after delivery of the placenta: ■ estrogen and PRL levels decline rapidly and lactation is initiated ○ 2 to 3 weeks: PRL levels reach basal levels in non nursing women ○ Basal levels of circulating PRL decline to the nonpregnant range: ■ Approximately 6 months after parturition in nursing women, ■ after each act of suckling – PRL levels increase markedly and stimulate milk production for the next feeding PRL levels also increase by: ○ Nipple and breast stimulation ○ ○ Trauma to the chest wall Other physiologic stimuli such as exercise, sleep and stress ○ After ingestion of the midday meal ● PRL fluctuate throughout the day ○ Maximal levels occur during the night while asleep ○ Smaller increase occurring in the early afternoon ● Normal PRL levels in nonpregnant women is usually 20-25 ng/ml ○ Greater than 20-25 ng/ml is a condition called hyperprolactinemia. ● Stress is the most common cause of slightly elevated PRL levels ● Hyperprolactinemia can produce disorders of gonadotropin sex steroid function, resulting in menstrual cycle derangement such as: ○ oligomenorrhea and amenorrhea ○ anovulation ○ inappropriate lactation or galactorrhea ● The mechanism whereby elevated PRL levels interfere with gonadotropin release appears to be related to abnormal gonadotropin-releasing hormone (GnRH) release. ● Women with hyperprolactinemia have abnormalities in the frequency and amplitude of LH pulsations, with a normal or increased gonadotropin response after GnRH infusion. ● Abnormality of GnRH cyclicity thus inhibits gonadotropin release but not its synthesis. ○ The reason for this abnormal secretion of GnRH is an inhibitory effect of dopamine and opioid peptides at the level of the hypothalamus. ○ In addition, elevated PRL levels have been shown to interfere with the positive estrogen effect on midcycle LH release. ○ It has also been shown that elevated levels of PRL directly inhibit basal and gonadotropin stimulated ovarian secretion of estradiol and progesterone ● Should measure prolactin levels in all women with galactorrhea, oligomenorrhea and amenorrhea not explained by another reason such as ovarian failure. Special cases in the Measurement of Prolactin: Hook Effect and Macroprolactin ● Hook Effect: ○ Because of possible aggregation of molecular forms of PRL when levels are high, if a tumor (adenoma) is suspected and values of PRL are only mildly elevated, the test should be repeated in a diluted sample. ○ Explained by high endogenous levels of PRL binding up all the assay antibodies, leaving an inadequate quantity for the assay. ○ Dilute the sample before assay when PRL levels are unexpectedly low. ● Opposite occurrence when PRL is found to be elevated in a woman who is normal clinically. ○ This is due to clumping of glycosylated PRL with immunoglobulin ○ Can be corrected by gel electrophoresis or by adding polyethylene glycol to the serum GALACTORRHEA ● Is defined as the nonpuerperal secretion of watery or milky fluid from the breast that contains neither pus nor blood ● The fluid may appear spontaneously or after palpation ○ Palpate the breast , moving from the periphery toward the nipple in an attempt to express any secretion. ● Diagnosis: can be confirmed by observing multiple fat droplets in the fluid under low power magnification ● Incidence of galactorrhea in women with hyperprolactinemia is ranging from 30% to 80% CAUSES OF HYPERPROLACTINEMIA Pathologic causes: ● Prolactinoma ● Acromegaly ● Cushing disease ● Hypothalamic disease ● Various pharmacologic agents ● Hypothyroidism ● Chronic renal disease ● Any chronic type of breast nerve stimulation such as may occur with: ○ thoracic operation ○ herpes zoster infection ○ Chest trauma ● One of the most common causes of galactorrhea and hyperprolactinemia is the ingestion of pharmacologic agents particularly: ○ Tranquilizers ■ Phenothiazines and diazepam can produce hyperprolactinemia by depleting the hypothalamic circulation of dopamine or by blocking its binding sites — decreasing dopamine action. ○ Narcotics ○ Antihypertensive agents ■ reserpine depletes catecholamines ■ ● ● ● ● ● ● ● methyldopa blocks the conversion of tyrosine to dihydroxyphenylalanine (dopa) Tricyclic antidepressants block dopamine uptake Drugs that block the hypothalamic dopamine receptor include: ○ Propranolol ○ Haloperidol ○ Phentolamine ○ Cyproheptadine Ingestion of oral contraceptive steroids can also mildly increase the levels of PRL, with a greater incidence of hyperprolactinemia occurring with older, higher-estrogen formulations. Galactorrhea does not usually occur during oral contraceptive ingestion because the exogenous estrogen blocks the binding of PRL to its receptors Primary hypothyroidism can also produce hyperprolactinemia and galactorrhea ○ Reason: because of decreased negative feedback of thyroxine on the hypothalamic-pituitary axis ○ The resulting increase in TRH stimulates PRL secretion and TSH secretion from the pituitary ○ Approx. 3% to 5% of individuals with hyperprolactinemia have hypothyroidism. ○ TSH is the most sensitive indicator of hypothyroidism and should be measured in all individuals with hyperprolactinemia. Hyperprolactinemia can occur in those with abnormal renal disease resulting from decreased metabolic clearance and increased production rate. Mild hyperprolactinemia (30 to 40 ng/mL) may occur in women with polycystic ovary syndrome (PCOS). ○ occurs in up to 30% of women and may be related to the chronic state of unopposed estrogen stimulation . CENTRAL NERVOUS SYSTEM DISORDERS Hypothalamic Causes ● Diseases of the hypothalamus that produce alterations in the normal portal circulation of dopamine can result in hyperprolactinemia. ● These include: ○ ○ Craniopharyngioma - most common infiltration of the hypothalamus by sarcoidosis, histiocytosis, leukemia, or carcinoma ● These tumors arise from remnants of Rathke’s pouch along the pituitary stalk. ● Grossly they can be cystic, solid, or mixed, and calcification is usually visible on a radiograph. ● They are most often diagnosed during the second and third decades of life and usually result in impairment of secretion of several pituitary hormones Pituitary Causes ● Various types of pituitary tumors, lactotroph hyperplasia, and the empty sella syndrome can be associated with hyperprolactinemia. ● As many as 80% of all pituitary adenomas secrete PRL. ● The most common pituitary tumor associated with hyperprolactinemia is the prolactinoma, arbitrarily defined as a: ○ microadenoma if its diameter is less than 1 cm ○ macroadenoma if it is larger ● Hyperprolactinemia has been reported to occur in approximately: ○ 25% of those with acromegaly and 10% of those with Cushing disease, indicating that these pituitary adenomas, which mainly secrete growth hormone (GH) and adrenocorticotropic hormone (ACTH), often also secrete PRL. ● Hyperplasia of lactotroph occurs in approx. 8% of pituitary glands examined at autopsy ● Individuals with hyperplasia of the lactotrophs cannot be distinguished from those having a microadenoma by any clinical, laboratory, or radiologic method. ● The diagnosis can be made only at the time of surgical exploration of the pituitary gland. ● Functional hyperprolactinemia is the term used for the clinical diagnosis of cases of elevated PRL levels without imaging evidence of an adenoma. ● Primary empty sella syndrome ○ Another cause of hyperprolactinemia ○ a clinical situation in which an intrasellar extension of the subarachnoid space results in compression of the pituitary gland and an enlarged sella turcica. ○ It results from a congenital or acquired (by radiation or surgery) defect in the sella diaphragm that allows the subarachnoid membrane to herniate into the sella turcica ○ It is usually associated with normal pituitary function, except for hyperprolactinemia, although some with primary empty sella syndrome have a coexistent prolactinoma ○ Serum PRL levels is < 10 ng/ml ○ Some women with this syndrome have normal PRL levels, with or without galactorrhea. PROLACTINEMIA ● PRL was found in approximately 50% of the glands, indicating that more than 10% of those in the general population have an undiagnosed prolactinoma. ● Overall, approximately 50% of women with hyperprolactinemia have a prolactinoma. ● The incidence is higher when the PRL levels exceed 100 ng/mL, and almost all individuals with PRL levels greater than 200 ng/mL have a prolactinoma. ● There is an approximate positive correlation between the size of the adenoma and the PRL level. ● Significant elevations in PRL affect menstrual function and may lead to hypoestrogenism DIAGNOSTIC TEST Imaging Studies ● Recommended diagnostic techniques: ○ Computed tomography (CT) scan with intravenous contrast ■ Beneficial for bony structural abnormalities ○ Magnetic resonance imaging (MRI) with gadolinium enhancement ■ Provides better soft tissue definition, without radiation ■ Provides 1-mm resolution and thus should be able to detect all microadenomas ■ It is the recommended imaging study to obtain Recommended Evaluation ● PRL levels be measured in all women with: ○ Galactorrhea ○ Oligomenorrhea ○ Amenorrhea who do not have an elevated FSH level ● PRL is also often measured in the workup of infertility ● If the PRL level is elevated, a TSH assay should be performed to rule out the presence of primary hypothyroidism ● If the TSH level is elevated, T3 and T4 should be measured to rule out the rare possibility of a TSH-secreting pituitary adenoma ● ● ● ● If the TSH level is elevated and hypothyroidism is present, appropriate thyroid replacement should begin and the PRL level will usually return to normal If the TSH level is normal and the woman has a normal PRL level with galactorrhea, no further tests are necessary if she has regular menses If PRL levels are persistently elevated (typically .40 ng/mL) and the TSH level is normal, an MRI (preferably) or CT scan should be obtained to detect a microadenoma or macroadenoma ○ Macroadenomas are uncommon and rarely present with a PRL level less than 100 ng/mL ○ If the PRL level is more than 100 ng/mL or the woman complains of headaches or visual changes, the likelihood of a tumor extending beyond the sella turcica is increased ○ Microadenomas are a common cause of hyperprolactinemia and remain stable in most cases Routine visual field testing and measurements of ACTH, GH,and thyroid function are not necessary unless warranted clinically TREATMENT Expectant treatment ● Women with radiologic evidence of a microadenoma or functional hyperprolactinemia who do not wish to conceive may be followed without treatment by measuring PRL levels once annually ● If estrogen is deficient, low estrogen levels in combination with hyperprolactinemia have been shown to be associated with the early onset of osteoporosis ○ Thus exogenous estrogen should be administered. ● Hormonal therapy, as is used for postmenopausal women, or oral contraceptives may be used ● Those with hyperprolactinemia, with or without microadenomas, who have adequate estrogen levels and who do not wish to conceive should be treated with periodic progestogen withdrawal ○ Medroxyprogesterone acetate, 5 to 10 mg/day for 10 days each month or ○ With combination oral contraceptives to prevent endometrial hyperplasia ● ● ● ● ● Directlystimulates dopamine-2 receptors and, as a dopamine receptor agonist, it inhibits PRL secretion in vitro and in vivo After ingestion, bromocriptine is rapidly absorbed, with blood levels reaching a peak 1 to 3 hours later Serum PRL levels remain depressed for approximately 14 hours after ingestion of a single dose, after which time the drug is not detectable in the circulation ○ Therefore the drug is usually given at least twice daily, with initial therapy being started at half of the 2.5-mg tablet to minimize side effects The most common side effects are orthostatic hypotension, with an incidence of 15%, which can produce fainting and dizziness as well as nausea and vomiting ○ To minimize these symptoms, the initial dose should be taken in bed and with food at night Less common adverse symptoms include headache, nasal congestion, fatigue, constipation, and diarrhea CABERGOLINE ● Cabergoline is a long-acting dopamine receptor agonist is currently preferred over bromocriptine for primary therapy because of greater efficacy and fewer side effects ● This agent directly inhibits pituitary lactotrophs, thereby decreasing PRL secretion ○ It is given orally in doses of 0.25 to 1 mg twice weekly ○ The initial dose is half a 0.5-mg tablet twice a week ○ Peak plasma levels occur in 2 to 3 hours, and the drug has a half-life of 65 hours. ● The effectiveness of cabergoline was greater than that of bromocriptine ● A potential concern with cabergoline is the development of cardiac valvular lesions; however, this has only been observed with large doses, as used for Parkinson disease, and has not been reported with lower doses Medical treatment of prolactinomas ● The initial treatment for women with macroadenomas, as well as for those women with hyperprolactinemia who are anovulatory and wish to conceive, should be the administration of a dopamine receptor agonist. Cabergoline and bromocriptine have been used successfully BROMOCRIPTINE ● Semisynthetic ergot alkaloid, developed in 1967 to inhibit PRL secretion Operative Approaches for Prolactinoma ● ● Transsphenoidal microsurgical resection of prolactinoma has been widely used for therapy Numerous reports of large series of individuals treated by this technique have been published ● ● Radiation Therapy for Macroadenomas ● External radiation with cobalt, proton beam, or heavy particle therapy and brachytherapy with yttrium-90 rods implanted in the pituitary have all been used to treat macroadenomas but are not the primary mode of treatment ● The current method of choice is probably the gamma knife and linear accelerator ○ Results have been inconsistent, and damage to normal pituitary tissue may occur, leading to abnormal anterior pituitary function and diabetes insipidus ○ Damage to the optic nerves may also occur, which led to the more precise technique of the gamma knife ● Radiation therapy should be used only as adjunctive management after incomplete operative removal of large tumors Pregnancy and Treatment of Prolactinomas ● Many women with hyperprolactinemia, with or without adenomas, wish to become pregnant ● A small percentage of these women conceive spontaneously, but most require treatment to induce ovulation ● With microprolactinomas, less than 1% had changes in visual fields, radiologic evidence of tumor enlargement, or neurologic signs ● 2.7% of women with a microadenoma became symptomatic, and 22.9% of women with a macroadenoma were symptomatic ● Women with a microadenoma do not require treatment during pregnancy, whereas women with macroadenoma only require treatment if they become symptomatic ● Testing of visual fields every 3 months should be carried out in all women with a macroadenoma ● Routine measurements of PRL during pregnancy have been controversial because of the wide range of values in pregnancy; however, it has been suggested that if PRL exceeds 400 ng/mL, this level should prompt visual field testing in women with an adenoma ● Although cabergoline is the dopamine agonist of choice for hyperprolactinemia, bromocriptine is used in pregnancy because there is a greater experience with bromocriptine, whereas there is no evidence of an adverse effect with cabergoline *** Women with Hyperprolactinoma who do not wish to conceive ● For women who do not wish to conceive and for whom galactorrhea is not a problem, no therapy is necessary unless estrogen levels are low ● Thus to prevent osteoporosis in this clinical situation, estrogen-progestogen hormone ● replacement or oral contraceptives should be given, regardless of whether an adenoma is present Long-term evaluation of all women with hyperprolactinemia should be carried out Unless a macroadenoma is present, measurement of PRL levels once a year is advisable Repeat imaging studies are unnecessary unless symptoms of headaches or visual disturbances occur or PRL levels increase substantially CHAPTER 38: Androgen Excess in Women ● ● ● ● ● ● ● ● ● ● Androgen excess in women ○ elevated androgen levels in blood ○ skin manifestations (acne, hirsutism, and scalp hair loss or alopecia) ○ but many women exhibit only skin manifestations without demonstrable findings in blood→ due to lack of sensitivity of current clinical laboratory assays Merely having elevated androgens in blood (hyperandrogenemia), per se, should not be the target of any treatment. The pilosebaceous unit (PSU) is composed of a sebaceous component and pilary component from which the hair shaft arises. ○ Abnormalities of the sebaceous component → acne ○ abnormalities of the pilary unit → excessive growth (hirsutism) or excessive shedding (alopecia) 2 types of hair: ○ vellus hair- soft, fine, and unpigmented ○ terminal hair-coarse, thick, pigmented, and undergoes cyclic changes Androgen is necessary to produce development of terminal hair ○ duration of the anagen phase is directly related to the levels of circulating androgen and determines the length of hair, which varies in different parts of the body ○ For facial hair it is approximately 4 months Activity level of the enzyme 5-alpha-reductase (5a-reductase) most directly influences the degree of androgenic effect on hair growth. With elevated levels of circulating androgen or increased activity of 5a-reductase, terminal hair appears where normally only vellus hair is present. With these alterations, the length of the anagen phase is prolonged and the hair becomes thicker. Hirsutism: ○ In the milder forms, hair is found only on the upper lip and chin ○ with increasing severity it appears on the cheeks, chest (intermammary), abdomen (superior to the umbilicus), inner aspects of the thighs, lower back, and intergluteal areas. The severity of the hirsutism can be roughly quantified by a modified scoring system of Ferriman and Gallwey ○ A score greater than 7 or 8 → only pertains to the Caucasian or African American population ○ Greater than 3→ In Asian women ● ● ● ● ● ● ● ● ● ● Hypertrichosis→ Increased hair growth only on the extremities or in isolated areas Virilization is a relatively uncommon clinical finding and its presence is usually associated with markedly elevated levels of circulating testosterone (2 ng/mL). ○ Signs of virilization usually occur over a relatively short period ○ These signs are caused by the masculinizing and defeminizing (antiestrogenic) actions of testosterone and include: ■ temporal balding ■ clitoral hypertrophy ■ decreased breast size ■ dryness of the vagina ■ increased muscle mass Women with virilization are almost always amenorrheic. Suspect androgen-secreting neoplasms → who develops signs of virilization, particularly if the onset is rapid PHYSIOLOGY OF ANDROGENS IN WOMEN ● Androgen production: from glandular tissues, (ovaries and adrenals) and from non glandular (peripheral) tissues ● Major androgen produced by the ovaries is testosterone and that of the adrenal glands is dehydroepiandrosterone sulfate (DHEAS). ○ Measurement of the amount of these two steroids in the circulation provides clinically relevant information regarding the presence and source of increased androgen production. ● Conversion of androstenedione and dehydroepiandrosterone (DHEA) to testosterone occurs in peripheral tissues ● ● ● ● ● The ovaries secrete only approximately 0.1 mg of testosterone/ day, mainly from the thecal and stroma cells. Other androgens secreted by the ovary are androstenedione (1 to 2 mg/day) and DHEA (,1 mg/day) The adrenal glands, in addition to secreting large quantities of DHEAS (6 to 24 mg/day), secrete approximately the same daily amount of androstenedione (1 mg/day) as the ovaries and less than 1 mg of DHEA/day. The normal adrenal gland secretes little testosterone Androstenedione and DHEA do not have strong androgenic activity but are peripherally converted at a slow rate to the biologically active androgen, testosterone. Approximately two-thirds (0.22 mg) of the daily testosterone produced in a woman originates from the ovaries ○ Thus increased circulating levels of testosterone usually indicate abnormal ovarian androgen production. For practical purposes, circulatory levels of DHEAS reflect an adrenal source of production, and in women more than 95% is adrenal derived ○ Although DHEAS serves as a good marker of adrenal hyperandrogenism, several guidelines for the evaluation of androgen excess in women omit this measurement, because DHEAS itself is a “weak” androgen and may not contribute much to the overall androgenicity. ○ Nevertheless it is our perspective that the measurement of DHEAS gives a more complete picture of androgen production. Occasionally, in women who have increased production of ovarian DHEA ,such as some with polycystic ovary syndrome (PCOS), the elevated levels of DHEAS might have an ovarian component because DHEA may be converted to DHEAS in the circulation. Another specific marker of adrenal androgen production, used for research purposes, is 11bhydroxyandrostenedione, because the adrenal primarily has the ability to 11-hydroxylate androstenedione, whereas the ovary has a limited ability to do so. Most testosterone in the circulation (85%) is tightly bound to sex hormone–binding globulin (SHBG) and is believed to be biologically inactive. An additional 10% to 15% is loosely bound to albumin, with only approximately 1% to 2% not bound to any protein (free testosterone) ○ Serum testosterone can be measured as the total amount, the amount that is believed to be biologically active (unbound, or non-SHBG bound), and as the free form. To exert a biologic effect, testosterone is metabolized peripherally in target tissues to the more potent androgen 5adihydrotestosterone (DHT) by the enzyme 5a-reductase ● ● ● ● ● ● After further 3-keto reduction, DHT is converted to another metabolite, 5a-androstane-3a,17b-diol (3a-diol). 3a-Diol is conjugated to the sulfate or glucuronide. The glucuronide, 5a-androstane-3a,17b-diol glucuronide (3a-diol-G), is a stable, irreversible product of intracellular 5a-reductase activity and reflects this activity in blood Even with normal circulatory levels of androgen, increased 5a-reductase activity in the PSU results in increased androgenic activity, producing hirsutism Measurements of 5a-reductase activity in skin biopsies have found that the level of activity correlated well with the degree of hirsutism present 3a-diol-G levels can be directly measured in serum ○ the most accurate indicator of the degree of peripheral androgen metabolism in women, as long as the level of glandular production (testosterone) is appreciated. ● ● If testosterone and DHEAS are normal but there is significant hirsutism, then measuring 3a-diol-G may not be necessary and one may merely assume a peripheral source of androgen excess CAUSES OF ANDROGEN EXCESS ● administration of androgenic medication. ○ Testosterone ○ 19-norprogestogen ○ Danazol ● abnormal gonadal development ○ external sexual ambiguity or primary amenorrhea ○ androgen excess ○ Y chromosome ● during pregnancy - increased ovarian testosterone production. ○ luteoma of pregnancy→ unilateral or bilateral solid ovarian enlargement ○ hyperreactio luteinalis→ bilateral cystic ovarian enlargement ○ After pregnancy is completed, the excessive ovarian androgenic production resolves spontaneously and the androgenic signs regress “Idiopathic” hirsutism and PCOS are the most common disorders, together making up more than 90% of cases. ○ PCOS is the most common disorder Idiopathic Hirsutism (Peripheral Disorder of Androgen Metabolism) - - - - Idiopathic hirsutism is diagnosed when there are signs of hirsut-ism and regular menstrual cycles in conjunction with normal circulating levels of androgens (both testosterone and DHEAS). Because this type of disorder is often present in certain families and ethnicities, it has also been called familial, or constitutional, hirsutism. Because neither ovarian nor adrenal androgen production is increased, the cause of the androgen excess has been called idiopathic hirsutism the cause of hirsutism is largely the result of increased 5- reductase activity TX: Antiandrogens that block peripheral testosterone action or interfere with 5-RA Polycystic Ovary Syndrome most common disorder diagnosed in women presenting with symptoms and signs of androgen excess. women who are anovulatory and have irregular periods as well as hyperandrogenism, as determined by signs such as hirsutism or elevated blood levels of androgens, testosterone, or DHEAS. most important feature of PCOS is that it is a hyperandrogenic disorder Functional or Idiopathic Hyperandrogenism - Eu- ropean clinicians; it is considered to occur in up to 15% of women presenting with hirsutism Stromal Hyperthecosis Stromal hyperthecosis is an uncommon benign ovarian disor- der in which the ovaries are typically bilaterally enlarged to ap- proximately 5 to 7 cm in diameter. Like PCOS, this disorder has a gradual onset and is initially as- sociated with anovulation or amenorrhea and hirsutism; however, unlike PCOS, with increasing age the ovaries se- crete steadily increasing amounts of testosterone. Androgen-Producing Tumors Tumors are rare, occurring less than 1% of the time in women presenting with hyperandrogenism, but they represent the most important reason for evaluating women with androgen excess. Ovarian Neoplasms Androgen-producing ovarian tumors usually produce rapidly progressive signs of virilization. the tumor is almost always (85% of the time) palpable during bimanual examination markedly elevated levels of testosterone (more than 2.5 times the upper limits of the normal range), with normal levels of DHEAS, usually facilitate the diagnosis. Adrenal Tumors Almost all the androgen-producing adrenal tumors are adenomas or carcinomas that generate large amounts of the C19 steroids normally produced by the adrenal gland—DHEAS, DHEA, and androstenedione. computed tomography (CT) scan or magnetic resonance imaging (MRI) of the adrenal to confirm the diagnosis Late or Adult-Onset 21-Hydroxylase Deficiency Congenital adrenal hyperplasia (CAH) is an inherited disorder caused by an enzymatic defect (usually 21-hydroxylase [21-OHase] or, less often, 11-hydroxylase), resulting in de- creased cortisol biosynthesis. As a consequence, adrenocortico- tropic hormone (ACTH) secretion increases and adrenal cortisol precursors produced proximal to the enzymatic block accumu- late. The steroids involved are mainly to 17-hydroxyprogesterone and androstenedione, and androstenedione in turn is converted to testosterone, which produces signs of androgen excess Both classic CAH and LOCAH are transmitted in an autosomal recessive manner at the CYP21A2 locus in proximity to the HLA-B locus Molecular genotyping is primarily used for prenatal testing when there is a known severe mutation to determine the risk of having a severely affected child. Corticosteroid treatment is normally reserved for patients wishing to conceive to restore ovulatory function Cushing Syndrome Excessive adrenal production of glucocorticoids caused by in- creased ACTH secretion (Cushing - - disease) or adrenal tumors produces the signs and symptoms of Cushing syndrome. Cushing syndrome can be easily excluded by performing an overnight dexamethasone suppression test Late-night salivary cortisol is now consid- ered to be the most accurate method and is the primary method of choice. THE DIAGNOSTIC APPROACH FOR WOMEN WITH ANDROGEN EXCESS Women with androgen excess present with acne, hirsutism, or alo- pecia, and some women have more than one of these three complaints Measurements of total testosterone, free (unbound) testoster- one, or the free androgen index have all been advocated to assist in the diagnosis of androgen excess. the laboratory workup should include an accurate measure of testosterone (unbound testosterone or the free androgen index [testosterone/SHBG is optional]), DHEAS, and 17-hydroxypro- gesterone when LOCAH is suspected ● Masculinizing ovarian or adrenal tumors are associated with rapidly progressive signs of hirsutism and virilization. ● Serum testosterone levels higher than 2 ng/mL, with normal DHEAS levels, indicate the probable presence of an ovarian tumor. ● The diagnosis can be confirmed by bimanual pelvic examination and ultrasonography, CT, or MRI. ● Women with a rapid progression of virilization and DHEAS levels greater than 8 mg/mL most likely have an androgen-producing adrenal adenoma; CT or MRI can confirm the diagnosis. ● Values suggestive of an androgen-secreting tumor are lower in a postmenopausal woman; values of testosterone greater than 0.9 ng/mL (90 ng/dL) and DHEAS levels greater than 4 ug/mL are significant. ● The diagnosis of ovarian stromal hyperthecosis should be suspected for women with these signs and testosterone levels greater than 1.5 ng/mL. ● The diagnosis of LOHD is established by measurement of 17-hydroxyprogesterone, either by testing of an early morning serum sample or after ACTH stimulation. TREATMENT OF ANDROGEN EXCESS ● The most successful disorder to treat is acne followed by hirsutism and finally alopecia. Specific Disorders Ovarian and Adrenal Tumors ● Tumors are best identified by high-grade imaging techniques. ● Suppression and stimulation tests have not been beneficial because many tumors are LH responsive and androgens are suppressed somewhat with OCs and gonadotropin-releasing hormone (GnRH) agonists. ● Almost all Sertoli-Leydig cell tumors are unilateral. ● ● ● ● ● ● ● If the woman has not completed her family and these tumors are well differentiated and confined to one ovary, the tumors may be treated by unilateral salpingo-oophorectomy. hilus cell tumors ○ occur after menopause ○ treated by bilateral salpingo-oophorectomy and total abdominal hysterectomy. Adrenal adenomas and carcinomas should also be treated by operative removal. Adrenal carcinomas often have metastasized to the liver by the time the androgenic signs have developed. Despite chemotherapy, the prognosis is poor after metastases have occurred. Stromal hyperthecosis is also best treated by bilateral salpingo-oophorectomy in older women. After removal of the ovaries of women with stromal hyperthecosis or any of the androgen-producing tumors, the acne and oiliness of the skin disappear, breast size increases, and clitoral size decreases. The excess central hair becomes finer and grows less rapidly but does not disappear. Electrolysis or laser treatment can remove the body hair more effectively once the source of PSU stimulation has been removed. Late-Onset 21-Hydroxylase Deficiency (Congenital Adrenal Hyperplasia) ● The androgen excess and menstrual irregularity can be treated as in women with PCOS, usually with an OC ● if women wish to conceive, it is preferable to use glucocorticoids such as hydrocortisone (15 to 20 mg), prednisone (5 to 7.5 mg), or dexamethasone (0.5 to 0.75 mg) in divided doses. ● Doses as low as 2.5 mg of prednisone or 0.25 mg dexamethasone may be used initially. ● The aim of treatment is to suppress androstenedione and bring 17-hydroxyprogesterone and progesterone levels into the normal range. Ovulation usually resumes rapidly. Polycystic Ovary Syndrome ● lifestyle measures and weight loss will assist in the treatment of hyperandrogenism in PCOS Treatment of Skin Manifestations of Androgen Excess: Hirsutism ● Although ovarian or adrenal androgen excess increases the likelihood of complaints, enhancement of these effects because of increased 5a-RA largely explains the abnormalities. ● Thus a successful strategy usually requires an antiandrogen added to suppression therapy, usually with an OC. ● Although it is reasonable to begin with monotherapy (OC), particularly if the disorder is relatively mild, in women with more significant complaints and findings, an antiandrogen can be used initially ● ● It is important to use antiandrogens in conjunction with an OC because of the concerns of exposure during pregnancy. In women who have “idiopathic” hirsutism and very mild and localized complaints, it is also reasonable not to use medical therapy and to use hair removal alone, as described later. Oral Contraceptives ● usually prescribed orally, but the effect would be similar with transdermal or vaginal preparations ● suppress ovarian androgens by inhibiting LH stimulation of the ovary. ● decrease adrenal androgens (DHEAS) by about 30% and inhibit 5a-RA. ● The potency of ethinyl estradiol in OCs increases SHBG, which results in lower free or unbound testosterone. ● it would seem logical to use a less androgenic progestogen (norgestimate, desogestrel, drospirenone) than more androgenic ones (levonorgestrel) ● The increased risk with the less androgenic OCs is relatively small, and the absolute risk of thrombosis in young women is also rare and less than that of normal pregnancy. It is important, however, to use lower-dose estrogen products (20 mg). ● obesity is an additional risk for thrombosis, and thus lifestyle management is important, particularly in women with PCOS. Antiandrogens ● Peripheral androgen blockade with antiandrogens is dose related. ● Receptor blockade with spironolactone and flutamide and a specific 5a-2 inhibitor, finasteride, are the agents most commonly used. ● Cyproterone acetate (2 mg), which is a progestogen, is most often used in combination with ethinyl estradiol as an OC ● Drospirenone in the doses used in contraceptives (3 mg) does not have appreciable antiandrogenic activity and is estimated to have an equivalent effect of 10 mg of spironolactone. ● Spironolactone ○ treatment of choice for women with idiopathic hirsutism, as well as many with PCOS ○ an androgen receptor blocker ○ decreases ovarian testosterone production and inhibits 5a-RA. ○ 200 mg/day of spironolactone is more effective than 100 mg/day ○ With the higher dose of spironolactone, liver function test results and plasma electrolyte levels are usually unchanged, and side effects occur infrequently, except for irregular uterine bleeding. ○ The latter can be controlled with concomitant use of OCs. ○ Electrolytes and blood pressure should be monitored for the first few weeks of ● ● ● therapy to ensure that hypotension and hyperkalemia do not occur. Flutamide ○ pure androgen blocker that has shown efficacy in the treatment of hirsutism. ○ There is a dose-response relationship (250 to 750 mg/day), and even lower doses have some efficacy; ○ the major concern is hepatic toxicity Finasteride ○ a 5a-reductase inhibitor (5 mg/day) ○ an effective treatment for hirsutism ○ 5 mg has similar efficacy as 100 mg of spironolactone ○ specific 5a-2 inhibitor (there are two isoenzymes for 5a reductase: 1 and 2) ○ hirsutism is likely a combination of both types 1 and 2 ○ second-line treatment when there are side effects or problems with using spironolactone. Dutasteride ○ an inhibitor of enzyme types 1 and 2 ○ clinically available for use in men. Other Agents for Treatment ● GnRH agonist with estrogen or an OC add-back ○ For severe cases ○ expensive and cannot be used for long-term therapy. ○ It has been used in women with high levels of circulating androgens. ● Ketoconazole ○ blocks adrenal and gonadal steroidogenesis by inhibiting cytochrome P450–dependent enzyme path- ways, ○ 200 mg, twice daily - to treat hyperandrogenism associated with PCOS and idiopathic hirsutism. ○ decreases hair growth and acne ○ but major side effects and complications (including hepatitis) occur in most women so treated. ● Glucocorticoids ○ treatment of androgen excess ○ Because of its potential for serious side effects, glucocorticoids are not recommended for treating androgen excess but may be considered as an adjunct to ovulation induction in some women. ● Insulin sensitizers ○ have been proposed as agents to treat androgen excess and have been used in women with PCOS. ● Eflornithine cream 13.9% ○ topical treatment for facial hirsutism. ○ inhibitor of ornithine decarboxylase, which is an enzyme necessary for the growth and development of the hair follicle. Follow-up for Treatment of Hirsutism ● ● Because of the length of the hair growth cycle, responses to treatment should not be expected to occur within the first 3 months of therapy, and it usually takes about 6 months to see a response. Remaining excess hair can be removed by electrolysis or laser techniques. Treatment should be continued for 3 years and then stopped to determine whether hirsutism recurs. If so, therapy can be reinitiated. Hair Removal Techniques ● can be used as a primary treatment for mild isolated hirsutism or should be initiated after adequate suppressive therapy to remove unwanted hair once the growth rate has been inhibited by therapy. ● Electrolysis uses electrical energy through a wire electrode. Destruction of hair follicles results in its permanent removal. ● Photoepilation uses lasers that apply heat to pigmented hair follicles. ● Four types of lasers: Nd:YAG, diode, alexandrite, and ruby, and a meta-analysis suggested superiority of the diode laser. ● Long wavelength, long pulse duration lasers such as the Nd:YAG or diode are recommended for pigmented darker hair. ● For women with light or blond hair, electrolysis is recommended. Acne Vulgaris ● Acne vulgaris is a manifestation of androgen excess, although it need not be, and particularly in adolescents it merely reflects the physiologic responses of the PSU to the changing hormonal status and alterations in the bacteriologic flora. ● androgens stimulate sebum production, and high doses of estrogen can inhibit it. ● Among hyperandrogenic disorders, acne vulgaris is the disorder that is most successfully treated. ● Among women who present with acne, 52% can be found to have androgen excess, with increases in unbound testosterone being the most frequently encountered ● An enhancement of 5a- reductase, mostly type 1, is a large part of the androgen abnormalities in acne ● Treatment is usually with combination OCs, which is at least as effective as chronic antibiotic therapy. ● Among OCs, less androgenic progestogens have been preferred. ● The estrogen component of the contraceptive pill inhibits sebum production, although it usually does not require increasing ethynyl estradiol greater than the 35-mg dose. ● Although most antiandrogenic agents are effective (Fig. 38.12), OCs and pure antiandrogens are superior to finasteride. ● If OCs alone are not completely successful, as with hirsutism, the addition of antiandrogens are beneficial. Alopecia: Female Pattern Hair Loss ● Previously called androgenic alopecia ● ● ● ● ● ● ● ● ● This may or may not be associated with androgen excess. Hair loss is usually on the frontal scalp and vertex, with relative sparing of the occipital scalp. Androgen excess, perhaps estrogen abnormalities, and genetics play into the cause. With androgen excess, exaggerated 5a-RA has been implicated in women with alopecia Antiandrogen therapy is the mainstay of treatment. In women, spironolactone and flutamide (to be used with caution) have efficacy; however, finasteride, which is used widely in men, may not be effective in women Minoxidil is also used to stimulate hair growth. combination of minoxidil with an antiandrogen is the most effective treatment for FPHL genetic manipulations and stem cell therapy may prove to be beneficial. POLYCYSTIC SYNDROME ● ● ● ● ● ● ● ● ● ● ● Phenotype C ○ Hyperandrogenism and polycystic ovaries in ovulatory women Phenotype D ○ irregular cycles and polycystic ovaries in the absence of documented hyperandrogenism Androgen Excess and Polycystic Ovary Syndrome (AEPCOS) Society definition: ○ hyperandrogenism as a key feature ○ recognizes that women with PCOS can have polycystic ovaries on US or menstrual irregularity (anovulation) OVARIAN most common endocrine disorder in reproductive-age women first described in 1935 by Stein and Leventhal as a syndrome consisting of amenorrhea, hirsutism, and obesity in association with enlarged polycystic ovaries NIH definition: diagnosis does not require findings on ultrasound (US) of characteristic polycystic ovaries Classic features: ○ signs of elevated androgens ■ hirsutism, oligomenorrhea or amenorrhea ○ present in as many as 15% to 20% of reproductive-age women diagnosis is usually made after the exclusion of other causes of irregular cycles and elevated androgens Rotterdam Criteria (ESHRE/ASRM): ○ Menstrual irregularity ○ symptoms of findings of hyperandrogenism ○ polycystic ovaries on US ○ 2 out of three = PCOS Phenotype A ○ classic phenotype ○ includes all 3 criteria with US findings of polycystic ovaries Phenotype B ○ denotes women with the NIH definition when there are no US findings ● ● Diagnosis of PCOS is made on a clinical basis laboratory measurements can be supportive but are not necessary OVARIAN MORPHOLOGY ● US findings of polycystic ovaries: ○ classic definition required 12 or more peripherally oriented cystic structures (2-9 mm) in one sonographic plane, and typically the finding in one ovary is sufficient ○ the total follicle count in each ovary that is most diagnostic ○ Ovarian volume: 10 mL or more is diagnostic ○ Follicle number per ovary (FNPO) should be 19-20 or 22 ○ Anti-mullerian hormone (AMH) >4.7 ng/mL - surrogate marker of FNPO for the diagnosis of PCO; not diagnostic as US; levels vary ● Polycystic-appearing ovaries (PAO), polycystic ovarian morphology (PCOM) or simply PCO ○ 10-25% of the normal reproductive-age population (no S/Sx of PCOS) may have polycystic ovaries found on US. DIAGNOSIS IN ADOLESCENCE ● Rotterdam criteria should not be used ○ because all the 3 criteria for the diagnosis are in a state of flux and change during adolescents, including the evolution and disappearance of polycystic ovaries ● PCOS should not be diagnosed unless all three criteria are firmly in place and at a minimum of 3 years postmenarche ● For the ovarian US criterion, because abdominal US is the mainstay, ovarian volumes of 10 mL or greater should be the criterion used MENSTRUAL IRREGULARITY ● includes oligomenorrhea (cycles longer than 35 days) and a menstrual frequency of every few months and frank amenorrhea (longer than 6 months missed). ● been reported that menstrual irregularity is the best correlate of insulin resistance in women with PCOS ANDROGEN EXCESS (HYPERANDROGENISM) ● cardinal feature of women with PCOS ● may be difficult to diagnose ● production of androgens in excess may emanate from the ovary, the adrenal gland, or the periphery ● symptoms of androgen excess, particularly of hirsutism, are sufficient for the inclusion of this parameter in the diagnosis of PCOS ● blood measurements of testosterone may not always be accurate and often are normal in women with symptoms ● androgen excess has been implicated in contributing to abnormalities in LH secretion, weight gain and adipose deposition and the metabolic derangements of PCOS ● 11-oxygenated androgens (derived from the adrenal) - quantitatively the most abundant androgens in women with PCOS ● Adipose tissues also secrete androgen - seems to contribute to lipid abnormalities and insulin resistance in women with PCOS CHARACTERISTIC ENDOCRINE FINDINGS ● abnormal gonadotropin secretion caused by increased gonadotropin-releasing hormone (GnRH) pulse amplitude or increased pituitary sensitivity to GnRH ○ result in tonically elevated LH levels in ~⅔ of the women ● After a bolus of GnRH, there is usually an exaggerated response of LH but not of FSH ● typically the women with PCOS who are more obese will be found to have normal LH levels ● women with PCOS who are thin often have elevated levels ● high tonic levels of LH (“inappropriate gonadotropin secretion) ○ due to elevated androgen & unbound estradiol or hypothalamic/pituitary ● ● ● ● ● ● ● ● ● ● functional abnormalities related to neurotransmitters such as dopamine FSH levels in women with PCOS are normal or low An elevated LH level or an elevated LH/FSH ratio is neither specific for nor required for the diagnosis of PCOS ○ These measurements should not be used as diagnostic tools ↑ amount of non–SHBG-bound estradiol is caused by a ↓ in SHBG levels, which is brought about by the ↑ levels of androgens and obesity, with ↑ insulin levels present in many of these women Estrone is also ↑ because of ↑ peripheral (adipose) conversion of androgen tonically ↑ levels of biologically active estradiol may stimulate ↑ GnRH pulsatility and produce tonically↑ LH levels and anovulation Relative hyperestrogenism ○ lowered SHBG level increases the biologically active fractions of androgens in the circulation ○ elevated levels of estrone and non–SHBG-bound estradiol often unopposed by progesterone because of anovulation ○ increases the risk of endometrial hyperplasia ■ enhanced further in some women with PCOS who seem to have progesterone resistance ○ progesterone does not work as well in downregulating the actions of estrogen on the endometrium Androgens from a variety of sources are elevated in women with PCOS ○ Serum testosterone levels usually 0.55-1.2 ng/mL ○ androstenedione levels usually 3-5 ng/mL almost all women with PCOS have elevated levels of circulating androgens, the presence or absence of hirsutism depends on whether those androgens are converted peripherally by 5-alpha-reductase to the more potent androgen dihydrotestosterone (DHT) reflected by increased circulating levels of 3-alpha-androstanediol glucuronide (3a-diol-G) Women with PCOS who are not hirsute have elevated circulatory levels of testosterone, DHEAS, or both, but not 3a-diol-G ~20-30% of women with PCOS also have mildly elevated levels of prolactin (20 to 35 ng/mL) ○ related to the ↑ pulsatility of GnRH, as a result of a relative dopamine deficiency or tonic stimulation from unopposed estrogen INSULIN RESISTANCE ● Insulin and insulin-like growth factor 1 (IGF-1) enhance ovarian androgen production by potentiating the stimulatory action of LH on ovarian androstenedione and testosterone secretion. ● High levels of insulin bind to the receptor for IGF-1 (significant homology of the IGF-1 receptor with the insulin receptor) ● ● ● ● ● ● ● ● ● ● ● Granulosa cells also produce IGF-1 and IGF-binding proteins (IGFBPs) → result in paracrine control and enhancement of LH stimulation and production of androgens by the theca cells in women with PCOS IGFBP levels are lower in women with PCOS, increases bioavailable IGF-1, increases stimulation of the theca cells in combination with LH to produce higher levels of androgen production elevated insulin levels (as well as androgen) ○ stimulate adipocyte production of adipokines (adipocytokines), ■ interfere with the metabolism and breakdown of adipose tissue ■ further enhance IR IR in PCOS ○ primarily characterized by an insulin resistance in peripheral tissues, manifest primarily in muscle and adipose and minimally at the level of ovary or adrenal reflects these events with the less efficient serine phosphorylation (rather than tyrosine phosphorylation) ■ resulting in less efficient insulin action (metabolic effect) ■ but with no effects on the production of androgens (intact mitogenic effect) ■ Androgen enhances this effect, intensifying interaction The proximate cause of IR in PCOS is unknown; ○ not caused by insulin receptor defects but by signaling abnormalities ○ genetic factors contribute to these findings. Most women with PCOS will be found to have euglycemia with peripheral IR In more severe cases ○ evidence of beta cell (secretory) dysfunction, which increases the risk of type 2 diabetes. . The negative effects of obesity and PCOS on insulin resistance are additive. Although clinicians may assume most women with PCOS have some degree of IR, particularly those who are older and who are overweight or obese ○ it is recommended that testing should be directed at ruling out diabetes and glucose intolerance, rather than diagnosing IR Fasting glucose levels are a poor predictor of diabetes in PCOS. A convenient way to assess glucose status is the measurement of the level of hemoglobin A1C. ○ Values greater than 5.8% suggest prediabetes ○ Values greater than 6% suggest frank diabetes ● ● ● Various techniques have been used to diagnose IR in women with PCOS ○ it can be argued that women who are overweight or obese with PCOS have IR, and it is not necessary to confirm it. ○ methods include fairly complicated but more accurate measures used only in a research setting: ■ clamp test ■ intravenous frequent sampling glucose tolerance test ■ Insulin tolerance test. Using fasting glucose and insulin measurements and calculating the quantitative insulin sensitivity check index (QUICKI) or homeostasis model assessment of insulin resistance (HOMA-IR) ○ have been useful and correlate well with the more invasive technique ■ It may not be necessary to compute these parameters and clinicians should assume that women who are overweight or obese with PCOS are insulin resistant ■ an oral glucose tolerance test should be carried out to rule out impaired glucose tolerance or diabetes, which cannot be assumed or discounted. If fasting blood is obtained to detect IR, HOMA or QUICKI are the most valuable parameters ANTIMÜLLERIAN HORMONE IN PCOS ● Müllerian-inhibiting substance (MIS) or AMH ○ a glycoprotein produced by the granulosa cells of preantral follicles. ● Because of the larger number of preantral follicles in PCOS, the MIS or AMH level is significantly elevated in women with PCOS. ● Physiologically, AMH attenuates a sensitivity of FSH in stimulating granulosa cells ○ levels are higher in clomiphene-resistant women and in those who are chronically anovulatory compared with those with more regular cycles, even as they age ● AMH levels have also been positively correlated with LH levels. ● AMH is involved in the pathophysiology of anovulation in PCOS, ○ some of the hereditary nature of women with PCOS. ○ higher levels of AMH in amniotic fluid program the fetus in utero to have higher LH and androgens and dysregulate the hypothalamic-pituitary-ovarian axis, resulting in the development of PCOS ● Because AMH correlates with the number of ovarian preantral follicles, ○ AMH may be used as a blood test to substitute for US findings of a polycystic ovary. ○ cutoff value of 4.7 ng/mL with values greater than this being consistent with PCOS ■ degree of overlap in values of AMH between PCOS and normal women precludes its routine use ■ milder phenotypes such as C and D have lower levels of AMH PATHOPHYSIOLOGIC CONSIDERATIONS ● genetic predisposition to PCOS ○ several genes are involved ■ are susceptibility genes that predispose the women affected to develop PCOS. ● A review by Kosova and Urbanek ○ pointed out the many difficulties in finding a direct genetic linkage, which are related to the nature of the disorder, its heterogeneity, and the large sample size required to find meaningful associations ○ multiple family studies of sisters, brothers, and daughters of affected women all showing some traits associated with aspects of PCOS. ● Environmental factors are clearly involved ○ in which PCOS is not always concordant on a genetic basis ● Maternal exposure to androgen (monkey model) ○ to contribute to the development of PCOS ○ Tata and colleagues ■ where the pregnancy environment, related to AMH may also be implicated. ● Genome-wide association studies in Han Chinese and European families ○ susceptibility genes with some consistency ○ loci at 2p16.3, 2p21, and 9q 33.3 ○ LH/human chorionic gonadotropin (HCG) receptor ■ a thyroid adenoma locus, ○ DENND1A, potentially affecting function of the endoplasmic reticulum. ● It has been long established that a vicious cycle propagates the disorder in PCOS, regardless of how it begins (Strauss, 2009) ○ ● ● ● ● ● ● ● ● ● ● dopamine deficiency in the hypothalamus ■ might give rise to the exaggerated LH responses in PCOS ○ It has been observed that morphologically identifiable polycystic ovaries are seen in children ○ adolescent, ovarian morphology has been shown to be variable and can change from being polycystic to normal and viceversa. ■ This occurrence predicts puberty and other normal endocrinologic events, suggesting a central role for altered PCOM in the disorder. Not all women with isolated polycystic ovaries have PCOS An ovary is polycystic in up to 20% of girls (Bridges and colleagues) ○ ovary transitions early in life from normal to polycystic appearing (PAO). ○ This influence occurs in a specific way by genetic factors or environmental factors, or it is induced by other endocrine disturbances (Lobo, 1996). PAO ○ normal menses ○ normal androgen levels ○ normal ovulatory function and parity ○ if subjected to various susceptibility factors (likely genetic) or environmental or other challenges or insults, with varying degrees of severity ○ may develop a full-blown syndrome (PCOS) ○ if full-blown, exhibits the full extent of hyperandrogenism and anovulation, with the most extreme form of this menstrual disturbance being amenorrhea ■ the type A or B phenotype according to Rotterdam criteria In this spectrum of disorders, the androgen disturbances may also be near normal. Menstrual disturbance may be mild. requires that normal homeostatic factors may be able to ward off stressors or insults in some women who can go through life without PCOS but have PAO, which does not change morphologically. a woman’s homeostatic mechanisms may at any time, early or later in reproductive life, allow symptoms of PCOS to emerge with varying degrees of severity. Two of the major insults: ○ weight gain ○ psychological stress typical teenager born with PAO may develop PCOS fairly quickly PCOS picture may only develop later in life in some women, even after having children, with weight gain Consequences of Polycystic Ovary Syndrome ● ● The importance of diagnosing PCOS is that there are known long-term consequences of the diagnosis warranting lifelong surveillance: ○ metabolic and cardiovascular risks ○ risk of certain cancers with aging. With aging, concerns for cardiovascular disease (become more prominent): ○ Hypertension ○ Metabolic syndrome ○ Diabetes ○ Cancer (endometrial and ovarian) WEIGHT GAIN/OBESITY AND METABOLIC SYNDROME ● Weight gain as women age ○ major predictor of abnormal metabolic findings ○ emergence of cardiovascular (CV) disease risks ○ all the symptoms of PCOS are worse with increasing body weight. ● The prevalence of obesity varies widely in different countries. ○ It is lowest in countries such as China and Japan (10%) ○ highest in the United States and some other Western countries (70%) ● There is increased abdominal and visceral fat in women with PCOS ○ correlated to IR and metabolic dysfunction (Lord, 2006). ● lifestyle management has to be a priority for women with PCOS and must be maintained lifelong. ● Metabolic syndrome ○ largely driven by obesity ○ leads to diabetes and CV disease (CVD) ○ has a prevalence during the reproductive years ● The prevalence of metabolic syndrome in the United States is approximately 60% in young (20 to 39 years) obese women with PCOS (Apridonidze, 2005). ● The diagnosis is made using Adult Treatment Panel III criteria (three of five of the following: ○ waist circumference .88 cm ○ high-density lipoprotein ,50 mg/dL ○ triglycerides .150 mg/dL ○ blood pressure .130/85 mm Hg ○ fasting blood sugar .110 mg/dL ● prevalence of metabolic syndrome in PCOS is still increased but is much lower (5% to 9%) ● constellation of risk factors that make up metabolic syndrome place women with PCOS ○ at increased risk for CVD and diabetes, ○ but there is nothing specific of more significance regarding metabolic syndrome in PCOS. DIABETES ● Type 2 diabetes mellitus is more prevalent (two to three times higher) in women with PCOS of reproductive age (Legro, 1999). ○ ● ● ● ● driven by IR, worsened by: ■ overweight status ■ menstrual irregularity it is extremely important to screen for diabetes in the overweight population with PCOS ○ best done with an oral glucose tolerance test Lack of precision in the screening for diabetes with hemoglobin A1c measurements ○ precluded the recommendation of using hemoglobin A1c as a screening tool ○ proven to be useful in the follow-up of women as they are being treated. Diet and exercise remain the mainstays of treatment Metformin has a significant role to play. ○ In at-risk women ○ glucose intolerance ○ prediabetes ○ often used with doses of 1500 mg/day ○ Doses are often higher in the presence of diabetes QUALITY-OF-LIFE ISSUES It is generally stated that there is poor quality of life among women with PCOS, most likely related to: ➔ burden of being overweight, ➔ having irregular cycles and decreased fertility, ➔ and having skin concerns (acne and hirsutism) ➔ although not all women have the same number or degree of these symptoms ● ● ● ● Depression - factor which may play a major role in women with PCOS seeking care and being compliant with diet, lifestyle, and various treatments - fourfold increase among women with PCOS Anxiety disorder is also prevalent, with a two- to threefold increase Strong argument has been made for screening women with PCOS for anxiety and depression Interventions such as weight loss, are able to improve quality of life CARDIOVASCULAR CONCERNS ➔ Women with PCOS have characteristic lipid and lipoprotein abnormalities ➔ ➔ ➔ ➔ ➔ ➔ Abnormal lipoprotein particles are also present = increase CV risk Women with the milder phenotypes diagnosed using the Rotterdam criteria have fewer CV risk factors. There are no definitive data on whether PCOS increased CV mortality Although multiple risk factors are present (IR, lipids, adipocytokines, inflammatory markers, surrogate markers of atherosclerosis on imaging) retrospective analyses have shown no increase in mortality, except among women with diabetes 2018 reassessment - unless a woman with PCOS has “classic” features of PCOS and has diabetes and obesity, there is no evidence for increased CV morbidity and mortality in women with PCOS Because of the large constellation of risk factors and lack of adverse outcome data, it could be hypothesized that there may be some inherent protective factors in PCOS CANCERS IN POLYCYSTIC OVARY SYNDROME ➔ There is an age-specific onset for some of the consequences of PCOS ➔ Risk for all cancers increases with aging, but endometrial cancer can begin at a younger age because of long-term anovulation and unopposed estrogen stimulation of the endometrium ➔ Breast cancer does not seem to be increased in women with PCOS, both endometrial and ovarian cancer are increased ➔ data for these are negatively affected by the heterogeneity of the patient population and their retrospective nature and most pertain to women diagnosed with classic PCOS ➔ It is likely that women with milder phenotypes may have little or no increased risk ➔ Endometrial cancer is increased at least two- to threefold, even when controlling for weight (due to unopposed estrogen, and possible defect in progesterone signaling in the endometrium among cancer patients ➔ Data are less strong for ovarian cancer, but the risk is thought to be about 2.5 times increased level of risk can be brought down to a normal rate with the use of oral contraceptives (OCs) ➔ Decreased risk of these cancers with the use of OCs for about 5 years is well known and translates into a good strategy for normalizing cancer risk in women with PCOS - because many women normally would be treated with OCs in any event for other symptoms ➔ Metformin ◆ used for women with PCOS ◆ has inhibitory effects on various cancers ◆ data are strongest for endometrial and breast cancer ➔ ➔ ➔ three main categories of complaint: ◆ androgen excess and symptoms of hyperandrogenism; ◆ irregular bleeding (dysfunctional uterine bleeding) and risks of endometrial disease as a result of unopposed estrogen stimulation from anovulation; ◆ fertility concerns and subfertility mostly because of anovulation Common complaint is weight gain or the inability to lose weight - related to IR and metabolic concerns Regardless of complaints, lifestyle management is an extremely important component of any treatment regimen Androgen excess ➔ acne, hirsutism, and alopecia ➔ occurs in the majority of women with PCOS, but not in all women ➔ symptoms are sufficiently mild ➔ treatment involves the use of an OC, with or without an antiandrogen OVARIAN AGING: POLYCYSTIC OVARY SYNDROME AND MENOPAUSE ➔ With aging, ovaries decrease in size and androgen levels decrease as women - true for those with PCOS as well ➔ Some juncture in time, the phenotype of PCOS may change or disappear ➔ As women with PCOS age, their menstrual cycles, if irregular when younger, become more regular and ovulatory - because of a decrease in the total follicular cohort and subsequently lower levels of AMH ➔ By the fourth decade nearly half of the women had evidence of ovulatory function, and in 8% the diagnosis of PCOS could no longer be made ➔ There may be preserved fertility in women with PCOS as they age - confirmed in one retrospective study in an in vitro fertilization (IVF) model, in which the live birth rate was higher at an older age compared with women with tubal disease ➔ As women enter menopause (despite lowered androgen levels) hirsutism may still be prevalent ➔ There is a persistence of the metabolic issues that existed at an earlier age requiring continued vigilance in managing and following these women ISOLATED POLYCYSTIC OVARIES ➔ Women with normal ovulatory function and PAO or PCOM have a subtle form of ovarian hyperandrogenism when stimulated with gonadotropins or HCG ➔ (+) subtle changes in insulin sensitivity and altered lipoproteins - considered as a risk factor for developing the consequences of PCOS TREATMENT OF POLYCYSTIC OVARY SYNDROME ➔ should be directed at the specific complaint Irregular bleeding ➔ Treatment should be directed at supplying the missing progesterone in anovulatory women ➔ Potentially can lead to endometrial hyperplasia or cancer if not treated. ➔ Women who are overweight and older are a higher-risk group, and endometrial biopsy may be indicated ➔ Most have menstrual irregularity who have IR and are more likely to have metabolic dysfunction ➔ Oral contraceptives (OCs) ◆ most logical and effective treatment, particularly because they reduce the risk of endometrial cancer ◆ may also be indicated for treatment of symptoms of androgen excess ➔ Progestogen therapy ◆ can be used for other women; ◆ may be used at 2- to 3-month intervals to shed the endometrium in chronically anovulatory women ◆ medroxyprogesterone acetate (5 to 10 mg) or norethindrone acetate (2.5 to 10 mg) may be used in this setting ➔ More complicated cases of menometrorrhagia are treated, as would other patients. Fertility concerns and subfertility ➔ Treatment is predominantly a result of anovulation ➔ women with the ovulatory phenotype C may have subtle ovulatory disturbances ➔ Some women have endometrial defects in progesterone and insulin signaling ➔ Before treatment with ovulation induction - rule out other fertility factors, specifically male factors by obtaining a semen analysis TREATMENT OF SUBFERTILITY IN POLYCYSTIC OVARY SYNDROME Before ovulation induction: normalize overt abnormalities in glucose tolerance encourage weight loss for overweight women ➔ Ovulation induction may be accomplished by a variety of agents, including: ➔ ➔ ➔ metformin, clomiphene, letrozole, gonadotropins, and pulsatile GnRH, as well as ovarian diathermy or drilling Adjunctive measures include use of: dexamethasone, dopamine agonists, thiazolidinediones, and various combinations -today these agents are rarely used IVF (stimulated or unstimulated) may be indicated in difficult-to-manage cases or if other in fertility factors are present Although metformin had been used as a first-line treatment for infertility - clomiphene is superior to metformin for first-line therapy IVF ● ● ● ● for women who fail to conceive with ovulation induction over six cycles those with other infertility factors only caveat to IVF treatment in women with PCOS is the higher-than-normal risk of OHSS (always in mind: significant dose adjustments in the treatment regimen, and using antagonist cycles, possibly metformin (when indicated), and the GnRH agonist trigger) frozen embryos transfer has been shown to be more successful than fresh embryo transfers because of an exaggerated endometrial response to medications used during IVF Metformin: ➔ if overweight or with obesity to achieve better metabolic control before pregnancy ➔ if with more casual approach to their fertility (metformin takes longer to become effective and may not induce ovulation in some women) ➔ even if it cannot induce ovulation - continued use may be beneficial when combined with clomiphene or gonadotropins ➔ improvement in oocyte quality has been suggested, but the effect has not been proved ➔ decrease the risk of ovarian hyperstimulation syndrome (OHSS) in women with PCOS undergoing IVF Clomiphene ● Mainstay for ovulation induction ● Most pregnancies occur within the first few cycles ● reasonable to use, with or without metformin, as an initial approach, after obtaining a semen analysis, but not for more than three or four ovulatory cycles before a more comprehensive workup is undertaken Letrozole ● 2.5 to 5 mg/day, 5 days ● efficacious as an alternative to clomiphene ● suited for women who have side effects with clomiphene ● randomized head-to head comparison: letrozole was found to be superior - confirmed in a Cochrane review ● cost analysis: letrozole to be more cost effective establishing its place as first-line treatment for women with PCOS Low-dose gonadotropin therapy ● highly effective as a second-line treatment ● for failure with oral agents ● for patient who may have transitory low estrogen status ● no evidence that any one gonadotropin preparation is better than another Pulsatile GnRH therapy ● rarely used, primarily because its use is cumbersome and less effective in PCOS compared with its use for hypothalamic amenorrhea Ovarian drilling (diathermy) ● a reasonable second-line therapy ● particularly in clomiphene failures and when gonadotropin therapy has proved difficult ● resulted in similar pregnancy rates (against standard gonadotropin therapy) but with a lower rate of multiple pregnancies ● rarely carried out - in part because of cost concerns METABOLIC AND WEIGHT CONCERNS ➔ ➔ ➔ Key management strategy = altering lifestyle variables Exercise regimens - when coordinated with a group of similar women, have been shown to be beneficial This approach should be part of all therapies for PCOS - acknowledging that some women with PCOS who are thin or normal weight probably already have a healthy lifestyle Metabolic syndrome (MBS) ➔ Driven largely by weight ➔ Usually treated by a combination of diet and metformin ➔ Six- to 12-month therapy = reduce weight by 5% to 7%, as well as to reduce insulin resistance and improve metabolic parameters Bariatric surgery ➔ Used in women with PCOS and obesity ➔ Most of the symptoms of PCOS were found to disappear after surgery ➔ Carries risks and should not be considered as first-line therapy. Antiandrogens (specifically flutamide) ● may also be efficacious for reducing body weight and visceral fat in women with PCOS ● combination of drospirenone and 17a-ethinylestradiol (EE2) with flutamide and metformin also has been used successfully in adolescents - this multidrug regimen has not been tested in an adult population Improvement of lifestyle variables (weight reduction and fitness) - should be the mainstay of all treatments