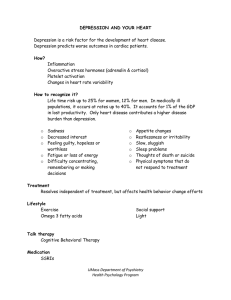
Personalized medicine in psychiatry 1–2 (2017) 11–25 Contents lists available at ScienceDirect Personalized medicine in psychiatry journal homepage: www.elsevier.com/locate/pmip Depression as a systemic disease Jorge Luis Sotelo a,⇑, Charles B. Nemeroff b a b Department of Psychiatry and Behavioral Sciences, Leonard M. Miller School of Medicine, University of Miami, United States Leonard M. Miller School of Medicine, University of Miami, United States a r t i c l e i n f o Article history: Available online 25 November 2016 a b s t r a c t Depression is now conceptualized as a systemic illness because of neurobiological mechanisms that explain how it influences other medical illnesses. Significant research has been conducted to explain the mechanisms by which depression increases the risk of, and complicates, already established medical illness. Biological processes as diverse as inflammation, neuroendocrine regulation, platelet activity, autonomic nervous system activity, and skeletal homeostasis are influenced by depression. In this review we aim to elucidate the mechanisms through which depression affects patients with heart disease, cancer, stroke, diabetes, and osteoporosis. These are conditions in which the interplay between depression and medical illness continues to be investigated. Ó 2016 Elsevier Inc. All rights reserved. Introduction Major depressive disorder is one of the leading causes of disability worldwide [1]. According to the World Health Organization (WHO), it will become the second leading cause of disabilityadjusted life years lost by the year 2020 [2]. Depression is believed to increase the risk, accelerate the progression and portend a poorer treatment response of a variety of medical disorders, including cardiovascular disease [4–6], stroke, cancer, renal disease and diabetes [7]. Processes as diverse as inflammation, neuroendocrine dysregulation, altered platelet activity, alterations in autonomic nervous system activity and decreased bone density may play a role in complicating the prognosis of major depression, especially in the setting of comorbid medical illness (Tables 1 and 2). Depression and heart disease According to the WHO Global Burden of Disease Survey, coronary heart disease and major depressive disorder are currently the two leading causes of disability in developed countries and it is estimated that this will apply to all countries throughout the world by the year 2020 [9,10]. A bidirectional association between depression and heart disease has been established and reviewed [12–20]. Ample evidence suggests that depression is highly prevalent in patients with congestive heart failure (CHF) [21–23], atrial fibrillation (AF) [24], post-myocardial infarction (MI) [20,25], ⇑ Corresponding author. E-mail addresses: jsotelo@med.miami.edu (J.L. Sotelo), cnemeroff@med.miami. edu (C.B. Nemeroff). http://dx.doi.org/10.1016/j.pmip.2016.11.002 2468-1717/Ó 2016 Elsevier Inc. All rights reserved. post-coronary-artery bypass graft surgery (CABG), and that it has an adverse effect on morbidity and mortality in these populations [26–28]. Multiple studies have demonstrated that depression increases the risk of developing cardiovascular disease in healthy individuals. Depression is a significant independent risk factor for coronary artery disease (CAD)-related morbidity and mortality, with an increased adjusted relative risk (RR) of 1.5- to 2-fold [36–42]. In addition, an important study of over 2800 adults without history of heart disease and a mean follow-up of 12.4 years showed that depressed mood and hopelessness were associated with an increased risk of fatal (RR 1.5, 95% CI 1.0–2.3) and nonfatal (RR 1.6, 95% CI 1.1–2.4) ischemic heart disease after adjusting for other risk factors [36]. Major depression was also a predictor of development of CAD (RR 2.12, 95% CI 1.24–3.63, P < 0.01) and MI (RR 2.12, 95% CI 1.11–4.06, P < 0.01) in subjects who were followed for 40 years [39] and the depression-associated risk was independent of traditional risk factors. A review of 13 prospective studies of 40,000 healthy subjects over a mean of 10 years found that depression was a significant independent risk factor for the development of CAD morbidity and mortality with an adjusted RR for major depression showing a 4- to 4.5-fold increase [43]. In another study with a median follow up of 8.5 years, patients with major depression were 2.7 times more likely to die from ischemic heart disease [45]. In addition, data from the Danish Psychiatric Central Research Register showed positive associations between depression and acute MI (incidence rate ratio [IRR] 1.16, 95% CI 1.10–1.22, P < 0.0001), as well as anxiety and acute MI (IRR 1.56, 95% CI 1.35–1.79, P < 0.0001) [46]. Data from the Swedish Twin Registry (over 30,000 twin pairs) revealed that onset of major depression resulted in an increase in the risk of concurrent (HR 2.53, 95% CI 12 J.L. Sotelo, C.B. Nemeroff / Personalized medicine in psychiatry 1–2 (2017) 11–25 Table 1 Pathophysiology of depression. Changes observed in depression ": proinflammatory cytokines ": formation of kynurenine metabolites ": clotting diathesis, annexin V protein binding to platelets, surface expression of P-selectin, activation of platelet fibrinogen receptor integrin a-IIb-b3 complex, platelet-leukocyte aggregates, platelet reactivity to ADP ": subclinical hypothyroidism ": HPA axis activity ;: glucocorticoid receptor sensitivity SNP within vWf gene Early life adversity HPA: Hypothalamic-pituitary-adrenal. SNP: Single-nucleotide polymorphism. vWf: von Willebrand factor. Table 2 Mechanisms through which depression affects medical illness. Illness Pathophysiology Heart disease Coronary artery disease ": CRP, proinflammatory cytokines, inflammatory genes, plasma VEGF, tryptophan/kynurenine ratio, serum b-thromboglobulin, PF4 ;: plasma and saliva cortisol, tryptophan Coronary artery calcification AA phenotype of SNP of BDNF gene Myocardial infarction ": CRP, IL-6 Heart failure ": CRP, IL-2, IL-4, IL-6, IFN-c, TNF-a, MCAP1, MIP-1b ;: IL-10 Atrial fibrillation ": CRP Cancer ": CRP, IL-1, IL-6, IL-8, TNF-a, soluble IL-2 receptor a chain, soluble IL-6 receptor, sTNFR2, activation of NF-jB regulated genes, nocturnal cortisol ;: diurnal cortisol slope SNP of serotonin transporter gene Early life adversity Bone health ": fall risk, salivary cortisol, bone NE, PTH, bone resorption markers, osteocalcin ;: BMD, GHRH, GnRH, 25-hydroxyvitamin D, ionized calcium SSRIs linked to falls, bone loss and fractures Stroke Endothelial dysfunction Fibrinogen dysregulation Exaggerated platelet reactivity Diabetes Inflammation Abnormal glucose metabolism Subclinical hypercortisolism Prolonged hypercortisolemia Blunted diurnal cortisol rhythm Hypocortisolism Impaired glucocorticoid sensitivity Increased catecholamines HPA axis activation ADP: Adenosine diphosphate. BDNF: Brain-derived neurotrophic factor. BMD: Bone mineral density. CRP: C-reactive protein. GHRH: Growth hormone-releasing hormone. GnRH: Gonadotropin-releasing hormone. HPA: hypothalamic-pituitaryadrenal. IFN: interferon. IL: interleukin. MCAP1: monocyte chemoattractant protein 1. MIP: macrophage inflammatory protein. NE: norepinephrine. PF4: platelet factor 4. PTH: parathyroid hormone. SNP: single-nucleotide polymorphism. sTNFR2: soluble tumor necrosis factor receptor 2. TNF: tumor necrosis factor. VEGF: vascular endothelial growth factor. 1.7–3.78, P < 0.001) and ongoing (HR 1.17, 95% CI 1.04–1.31, P = 0.008) CAD [47]. Moreover, a 2013 study of 45 young adults at increased risk of depression showed evidence of altered cardiovascular risk profile even in the absence of depressive symptoms [48]. Depression has been recognized as a negative prognostic factor associated with an increased risk of cardiovascular related morbidity and mortality [43,49,50]. Doering et al. [51] demonstrated that co-morbid anxiety and depression were predictive of all-cause mortality in patients with CAD. A study of 610 patients treated for ischemic heart disease revealed that depression was associated with an increased hazard rate for all-cause mortality (HR 1.96). In addition, depression was associated with time to first hospitalization, total number of hospitalizations, and cumulative length of hospital stay. Depression was also independently associated with an increased risk for 5-year all-cause mortality [52]. Beach et al. [53] demonstrated that higher initial Patient Health Questionnaire-9 (PHQ-9) scores were significantly associated with subsequent rehospitalization at 6 months in patients with acute coronary syndrome, heart failure, or arrhythmia. These scores were also associated with increased risk of composite outcome of cardiac readmission or mortality. The PHQ-9 score was more strongly associated with adverse cardiac outcome than other variables. In addition, a meta-analysis of 30 studies [18] found a pooled RR of coronary heart disease of 1.30 (95% CI, 1.22–1.40) and a pooled RR of MI of 1.30 (95% CI, 1.18–1.44) in patients with depression. The prevalence of depression in patients with heart failure is also increased, as are the morbidity and mortality of that patient population. Approximately 20% of outpatients with heart failure fulfill criteria for major depression and up to 48% experience depressive symptoms [58]. In addition, more than half of patients with heart failure have significant anxiety or depression symptoms [59–61]. In patients with CHF, major depressive disorder is an independent risk factor for reduced quality of life, adverse health outcomes, and elevated risk of mortality [63–68]. Previous studies have documented an association between depression and mortality in outpatients [69–72] and hospitalized patients with heart failure [73,63]. A recent study reported on 1260 patients with heart failure on whom data was collected over 12 months [75]. More than half (52.9%) of the participants had anxiety, 32.5% had depression, and 26.8% had both anxiety and depression. Patients with heart failure with comorbid anxiety and depression were 2.6 times more likely to die compared with those who were neither depressed nor anxious. Increased inflammation has been identified in patients with depression and in patients with heart disease [76–79]. Proinflammatory cytokines play significant roles in the development and clinical progression of CHF [80,81]. Inflammation also plays a central role in the pathogenesis of CAD and is involved in all stages of atherosclerosis. Patients with CAD exhibit higher circulating proin- J.L. Sotelo, C.B. Nemeroff / Personalized medicine in psychiatry 1–2 (2017) 11–25 flammatory cytokines, higher C-reactive protein (CRP) levels, and increased expression of inflammatory genes [82,83]. Elevated CRP levels have been associated with an increased risk of major adverse cardiac events in the 2 years after an acute coronary syndrome event [84]. Proinflammatory cytokines have been shown to be elevated in major depressive disorder and there is a positive association between severity of depressive symptoms and various markers of inflammation [50,85–92]. Increased inflammation induces depressive symptoms by several mechanisms, including effects on the serotonergic system [106,107]. In response to inflammation, tryptophan metabolism shifts towards the formation of kynurenine metabolites [108] with an increased production of 3-hydroxykynurenine and quinolinic acid [109]. Excessive inflammation due to impaired glucocorticoid receptor sensitivity has also been found in patients with major depressive disorder [110,111], in the elderly [112] and in patients at risk for cardiovascular disease [113]. It has been postulated that glucocorticoid resistance may occur as a result of chronic stress and prolonged exposure to inflammatory cytokines [114]. Moreover, a meta-analysis of articles published between 1967 and 2008 showed a positive correlation between inflammatory markers and depression in groups of patients with depression and in community-based cohorts [97]. Chronic inflammatory states might mediate the increased risk of CAD in depression [98–100]. Downregulation of the antiinflammatory cytokine interleukin-10 (IL-10) and upregulation of the proinflammatory cytokines IL-6 and tumor necrosis factor alpha (TNF-a) have been reported in heart failure patients with depressive symptoms [101]. In addition, MI patients have increased plasma IL-6 and CRP concentrations and altered response to the anti-inflammatory properties of glucocorticoids, which independently correlate with depressive symptoms [102]. The Gutenberg Health Study (n = 10,000; ages 35–74) [115] revealed that CRP concentrations were higher in patients with AF (3.6 vs 2.9) and there was an association between the degree of depressive symptoms and AF. Self-reported physical health status and mental health status were lower in patients with AF and were related to depression symptom severity. Evidence suggests that depressive symptoms are related to the recurrence of AF episodes [116] and of complications, such as heart failure and death [24]. Psychological distress may influence hemodynamics, vascular function, autonomic tone, inflammatory activity, and hemostasis [117–119], all of which play a role in the pathogenesis and complications of AF. Nikkheslat et al. [120] reported on CAD patients with (n = 28) and without (n = 55) depression. CAD patients with depression had higher levels of CRP, IL-6 gene expression, and plasma vascular endothelial growth factor (VEGF) and lower plasma and saliva cortisol levels. The CAD depressed group also exhibited a reduction in glucocorticoid receptor expression and sensitivity. Finally, tryptophan levels were significantly lower and tryptophan/kynurenine ratios were increased in patients with depression. In this study, CAD patients with depression had elevated levels of inflammation in the context of HPA axis hypoactivity, glucocorticoid receptor resistance, and increased kynurenine pathway activation. Reduced cortisol bioavailability and decreased expression and sensitivity of glucocorticoid receptors may lead to insufficient glucocorticoid signaling and increased inflammation [120]. Furthermore, Xiong et al. [121] reported on 155 patients (25 nondepressed; 130 depressed) admitted for acute heart failure exacerbations. Major depressive disorder was associated with elevated IL-2, IL-4, IL-6, interferon (IFN)-c, monocyte chemoattractant protein 1, macrophage inflammatory protein 1b, and TNF-a. Platelets may also play a role in the interplay between depression, inflammation and heart disease. They recruit inflammatory cells that contribute to atherosclerosis [122–124]. Platelets also contribute to artery remodeling and atheroma formation by 13 producing growth factors that promote the proliferation of smooth muscle cells in the atheroma [125–128]. Unchecked inflammation can induce recruitment of monocyte progenitor cells [125–127], which can become activated macrophages capable of inducing apoptosis of smooth muscle cells within the arterial wall [129]. Alterations in platelet activation and aggregation in the clotting cascade observed in patients with depression result in an increased clotting diathesis [5]. Patients with major depression also exhibit increased annexin V protein binding to platelets, increased surface expression of P-selectin, and increased activation of the platelet fibrinogen receptor integrin a-IIb-b3 complex, the final common pathway for platelet activation [130,131]. In patients with depression, studies have shown significant increases in platelet activation and circulating platelet-leukocyte aggregates and enhanced platelet reactivity to ADP [132]. Marked elevations of serum bthromboglobulin and platelet factor 4 (PF4) have also been shown in elderly patients with depression and CAD compared with elderly nondepressed patients with CAD and in healthy young controls [133]. Overt and subclinical hypothyroidism are associated with an increased risk of cardiovascular disease and related mortality [155]. In depressed patients, considerable evidence suggests an increased prevalence of subclinical hypothyroidism [156,157]. Many patients with depression also exhibit hypothalamicpituitaryadrenal (HPA) axis hyperactivity [158]. Increased cortisol levels are also associated with an increased risk of cardiovascular mortality. In the CHIANTI study, urinary cortisol levels predicted cardiovascular mortality risk, with participants in the highest tertile of urinary cortisol levels exhibiting a fivefold increase in risk of cardiovascular death [159]. In a cohort of 382 patients hospitalized due to depression, dexamethasone nonsuppression of cortisol secretion and elevated baseline cortisol levels both predicted mortality from cardiovascular disease [160]. Another study revealed that cortisol awakening response is negatively correlated with HRV [161]. One single-nucleotide polymorphism (SNP), rs216873, located within the von Willebrand factor gene has been associated with severe depression based on Beck Depression Inventory score [162]. von Willebrand factor recruits platelets to damaged endothelium during the pathogenesis of atherosclerosis [163]. Other SNPs associated with inflammation, endothelial function, and platelet aggregation have also been identified as suggestive of an association with depression [164]. Twin studies have suggested that depression, elevations in plasma lipids, and HRV may share genetic mechanisms [165,166]. A study of patients with CAD revealed that the AA phenotype of the Val66Met SNP of the brain-derived neurotrophic factor (BDNF) gene predisposed to CAD and CAD with depression in women [167]. Adverse events in early life, including childhood trauma, are associated with an increased susceptibility to both depression and cardiovascular disease [168]. A retrospective analysis of over 17,000 adults revealed a dose-response relationship between adverse childhood experiences and ischemic heart disease [168]. This is of importance because childhood maltreatment is associated with a number of biological alterations that are similar to depression and increase the risk for medical disorders. These include inflammation and altered autonomic nervous system activity [169]. Such events lead to modification of the superstructure of the chromatin through methylation, thus altering ultra-conserved nongenic regions of the genome and the accessibility of certain genetic regions to transcriptional enzymes and microRNAs. These molecular events might directly affect genes important for susceptibility to cardiovascular disease or could trigger additional molecular events that further modify the superstructure of the chromatin and consequently increase susceptibility to cardiovascular disease. Early life trauma may therefore be the mechanism through which some individuals develop heart disease. 14 J.L. Sotelo, C.B. Nemeroff / Personalized medicine in psychiatry 1–2 (2017) 11–25 Finally, one study of 454 healthy individuals assessed for depression over 10 years revealed that persistent depression was associated with a two-fold increase in the risk of both detectable and severe coronary artery calcification [170]. A study of 314 patients, ages 19–79, who presented with chest pain showed that each 1 point increase in the Beck Depression Inventory score was associated with a 5–6% increase in abnormal coronary angiographic findings or definitive CAD [171]. Other studies have found associations between depression severity and intima-media thickness of the carotid bulb [172] and impaired endothelial function [173]. Depression and cancer Prevalence rates for depression in patients with cancer range from 1.5% to 50%, with median point prevalence rates between 15% and 29% [174–178]. A study by Linden [179] and a review by Ng [180] in over 9000 patients calculated prevalence rates of 10.8 and 12.9%, respectively. One large-scale prospective study found that cancer diagnosis and treatment resulted in a four-fold increase in depression occurrence during the first two years after diagnosis [181]. It leads to a poorer quality of life and compromises patient outcomes, resulting in higher mortality rates [182–185]. A meta-analysis revealed that depression increases mortality rates in cancer patients by up to 39% and even patients with few depressive symptoms may be at a 25% increased risk [186]. In a recent study of patients with a mixture of different cancer types, the most frequent initial psychiatric diagnoses were minor depression (17.6%), major depressive disorder (15.8%), and adjustment disorder (15.8%) [187]. Cancer patients without psychiatric morbidity in this study had a survival benefit of 2.24 months. After adjusting for demographics and cancer stage, psychiatric comorbidity remained associated with poorer survival (HR 4.13, 95% CI 1.32– 12.92). Depression may, in part, adversely affect medical outcomes in these patients by resulting in an increase in length of hospitalizations, diminishing quality of life, a reduction in the ability to care for oneself, and a decrease in adherence with treatments [174,188–190]. In breast cancer, the prevalence of clinical depression is between 10 and 30% within the first five years after diagnosis [192] and it is associated with increased mortality [183]. Hung et al. [194] found an increased risk for mood disorders in older women and women with comorbid conditions in over 26,000 women with breast cancer. A recent study of over 44,000 women with breast cancer followed from 1998 to 2011 [195] found that in the first year after diagnosis, the rate ratio for a hospital contact for depression was 1.70 (95% CI, 1.41–2.05) and that for use of antidepressant was 3.09 (95% CI, 2.95–3.22). These ratios were significantly increased after 3 and 8 years, respectively. A threefold increased risk for first use of antidepressant was found close to diagnosis, decreasing to a 20% significantly increased risk 8 years after diagnosis. Comorbidity, node-positive disease, older age, basic and vocational educational levels and living alone were associated with use of antidepressants. However, there was no association between type of surgery or adjuvant treatment and risk for depression. Four other studies on factors associated with breast cancer-related depression in populations ranging from 190 to 1933 women also found no associations with type of surgery [196–198], or chemotherapy [196,197,199]. Associations between increasing age, comorbid disease, and use of antidepressants were also found in a study of over 8000 women treated with radiotherapy [200]. In men with prostate cancer, longitudinal studies [201–207] have shown increased rates of anxiety, depression, cardiovascular events, and suicide that may result from uncertainties regarding treatment, cancer control, erectile dysfunction, or urinary incontinence following treatment. Depression symptoms are more common in older patients with prostate cancer, though younger patients are more likely to report increased levels of psychological distress [208]. Prasad et al. reported on 41,275 men diagnosed with prostate cancer between 2004 and 2007, 4.6% of whom (1894) also had a diagnosis of depressive disorder in the 2 years before cancer diagnosis [209]. Men with depressive disorders were more likely to have high-risk disease. In this study a pre-existing diagnosis of depressive disorder was independently associated with treatment choice and outcomes of localized prostate cancer. Men with prostate cancer and a recent diagnosis of depression were less likely to undergo definitive treatment and experienced worse overall survival. Depressed men with intermediate and high-risk prostate cancer were less likely to choose definitive therapy. Men with depression were also more likely to receive androgen deprivation therapy (ADT) alone as treatment, which increases psychological distress and worsens quality of life in this patient population; [210] but its use does not appear to worsen depressive symptoms in men with prostate cancer and depression [211]. Men with a diagnosis of depression had a significantly higher number of doctor visits in the 2 years before prostate cancer diagnosis but were also more likely to present with aggressive disease. Intervention and improvement in symptoms is associated with improved survival in patients with metastatic cancer [191,213]. As was highlighted above, proinflammatory cytokines may be involved in depression in healthy and medically ill individuals, including cancer patients [214–216,177]. The cytokine hypothesis of depression suggests that behavioral changes in cancer patients may be caused by proinflammatory cytokines, which influence neuroendocrine pathways, resulting in depression and other comorbidities [217,90,218–221]. This hypothesis is supported by studies showing a correlation between serum levels of proinflammatory cytokines and depressive symptoms in pancreatic and ovarian cancer patients [90,222]. Epidemiological studies have shown that chronic inflammation predisposes to various types of cancer. Inflammation has actually been linked to 15–20% of all deaths from cancer worldwide [223] and is associated with recurrence of cancer [224]. In addition, recent studies suggest that blocking the effect of proinflammatory cytokines reduces symptoms of depression (especially fatigue) in cancer patients [227]. Tumor cells and cells in the tumor environment produce high levels of IL-6 [228–231]. IL-6 promotes angiogenesis [228], invasion and attachment [230], and generation of tumor-associated macrophages [232]. Elevations of IL-6 are also associated with decreased time to recurrence and shorter survival time in ovarian cancer patients [233–235]. An association has also been found between IL-6 levels and vegetative signs and symptoms of depression, disability, and fatigue in patients with ovarian cancer [238]. In one study of women undergoing radiation treatment of breast cancer, soluble IL-6 receptor levels were significantly elevated in patients with severe versus mild depression [239]. Fatigue during radiation treatment has also been associated with increased levels of inflammatory markers [240,241]. NF-kB has also been implicated in cancer development and treatment resistance [242,243]. Fatigued breast cancer survivors demonstrate increased activation of NF-kB-regulated genes [244]. In addition, chemotherapy has been associated with NF-kB activation in breast cancer tissue and peripheral blood [227,245]. Prior chemotherapy was associated with significantly higher depression scores, increased expression of NF-kB regulated gene transcripts, and increased levels of IL-6 and soluble TNF receptor 2 (sTNFR2) in women undergoing breast cancer radiation treatment [246]. Moreover, IL-1 and IL-6 concentrations significantly correlate with fatigue in patients with cancer treated with radiation or chemotherapy [247,248]. J.L. Sotelo, C.B. Nemeroff / Personalized medicine in psychiatry 1–2 (2017) 11–25 In patients with breast, ovarian, cervical cancer and lymphoma, dysregulated patterns of cortisol secretion have been observed [249–252]. Elevated nocturnal cortisol and blunted diurnal cortisol slope has been observed in ovarian cancer patients prior to surgery [238,253]. Disruption of cortisol rhythms resulting in flattening of the cortisol slope has been associated with shortened survival time in patients with breast cancer [254]. In animal models, altered glucocorticoid receptor expression secondary to elevated cortisol has been recognized as a likely mechanism in the initiation of ovarian cancer [255], the failure of cancer cells to undergo apoptosis [256–258], the development of chemotherapy resistance [259] and accelerated tumor growth [260]. In addition, cortisol dysregulation has been associated with poor performance status [261], fatigue [262], and depression [250] in cancer patients. Abnormal cortisol rhythms have also been linked with symptoms of depression in patients with ovarian cancer [238,253]. Genetic factors may also play a role in determining vulnerability to depression in patients with cancer. The rs12150214 SNP of the SLC6A4 serotonin transporter gene has been associated with severity of depression symptoms as assessed with the Beck Depression Inventory and elevated IL-6 levels in some populations [263]. This polymorphism has also been associated with poor overall survival and decreased disease specific survival in patients with colorectal cancer [264]. Patients with the C allele were at 57% increased risk of death than their counterparts. This study suggests that emotional or physiological stress (inflammation) and their associated mechanisms can be modified by the availability of the serotonin transporter protein, either by environmental factors or variations in the SLC6A4 gene. Individuals with a history of childhood abuse or neglect are at increased risk for psychological distress when confronted with new traumatic experiences, including a diagnosis of breast cancer [265]. Childhood trauma may alter neurocircuitry during a time when the brain is vulnerable to environmental stressors [266– 268]. As noted above, childhood abuse has been associated with elevated markers of inflammation including CRP, IL-6, and TNF-a, in adults. These biomarkers have been correlated with fatigue and depression in breast cancer patients [246,244,268]. A cancer diagnosis may trigger women with a history of childhood abuse to experience higher levels of intrusive cancer-related thoughts, images, emotions, and dreams during and after cancer treatment [265]. A study of breast cancer patients confirmed that childhood abuse predicted poorer quality of life, as well as severe fatigue, depression, and stress during and after cancer therapy [270]. In addition, two cross-sectional studies of breast cancer survivors found that patients with childhood trauma reported reduced quality of life and greater fatigue and psychological distress following cancer treatment [271,272]. Han et al. studied 20 women 18– 75 years of age with stage 0-IIIA breast cancer treated with breast-conserving surgery followed by radiation therapy [273]. Patients with a history of childhood trauma exhibited significantly greater fatigue. In addition, 50% of patients with childhood trauma (vs 8% of patients without) had symptoms of moderate to severe depression at some point during the study. Radiotherapy did not significantly account for the fatigue, depression, or perceived stress in patients with or without childhood trauma. However, significant positive associations between severity of trauma on the Childhood Trauma Questionnaire (CTQ) and depression scores were found. CTQ symptom severity was the most significant predictor of perceived stress after controlling for covariates. In patients with childhood trauma significant positive correlations were also found between fatigue scores and CRP and perceived stress scores and CRP and IL-6. Childhood trauma patients exhibited alterations in gene transcripts related to inflammatory signaling, including IL22, IL-17, and C-C chemokine receptor 5 signaling in macrophages and T lymphocytes. They also exhibited an over-representation of 15 genes regulated by the NF-kB family transcription factor, RelA (p65 subunit of NF-kB). This study confirmed that childhood abuse was common in breast cancer patients and that it was associated with inflammation-mediated fatigue and depression scores before, during, and after radiotherapy. Another study of breast cancer patients over a 9-month period [270] found that a history of childhood adversity was associated with increased fatigue, depression, and perceived stress before and during treatment [270]. Depression and anxiety occur in approximately 30–40% of patients with colorectal cancer [275,276]. High levels of proinflammatory cytokines in these patients suggest that cytokines also play a role in the etiology and pathophysiology of depression and anxiety [277]. In a study of 20 adults recently diagnosed with colorectal cancer, a combination of severe anxiety and depression symptoms was found in 65% of colorectal cancer patients. These patients had 3.2- to 4.4-fold higher concentrations of the proinflammatory cytokines IL-1b, IL-6, IL-8, and TNF-a. Anxiety, depression, and combined anxiety and depression were positively correlated with IL-1, IL-6, IL-8, and TNF-a. In advanced colorectal cancer patients, increased serum levels of the soluble portion of the IL-2 receptor a chain have been previously shown to correlate with depression symptoms, suggesting that tumor-induced immune activation contributes to depression [278]. Treatment of cancer may also predispose patients to depression. There is a possible link between invasive surgical procedures and higher levels of IL-6 and CRP [279,280]. In depressed patients who underwent abdominal procedures, increased serum IL-6 concentrations correlated with depression severity scores [281]. However, these postsurgical mood changes and proinflammatory alterations have not been replicated in other studies [282–284]. In contrast, cortisol and IL-6 levels decreased significantly over the course of 1 year following surgery to treat ovarian cancer in another study, and these changes were observed by 6 months post-surgery. The decrease in IL-6 levels was associated with decreased fatigue and vegetative signs of depression, and decreased nocturnal cortisol concentration was significantly associated with decreased disability and fatigue [285]. Chemotherapy is associated with increased proinflammatory cytokine levels, which may be associated with fatigue and sleep disturbance [268,286–288]. Fatigue, depression, and stress are commonly reported side effects of radiotherapy [241,246,289,290]. Breast cancer patients who develop fatigue and depression undergoing radiotherapy have been found to have elevated proinflammatory markers, including CRP, IL-6, IL-1 receptor antagonist, soluble NFj B DNA binding [239–241,246,290]. Depression and bone health Depression has been linked to low bone mass [352] and there is evidence that depression may lead to bone health deterioration and increased fracture risk in adults [353–357] and that it could even affect peak bone mass in children and adolescents [358]. Low bone mineral density (BMD) is prevalent even at early stages of major depression [356,360]. After adjusting for osteoporosis risk factors, BMD is negatively associated with depressive symptoms in older patients [361]. This association has been observed in a variety of patient populations [351,355,356,361–367,362]. In men, bone mass is generally lower in those with depression compared to those who are not depressed [368–371]. Danielson et al. [372] measured the BMD of 207 motherdaughter pairs and found that the daughters of mothers with a low BMD or who had suffered osteoporotic fractures also had lower BMD. Two studies of postmenopausal women [367,373] and one study of men [371] demonstrated a positive association between depressive symptoms and a decrease in BMD. Two 16 J.L. Sotelo, C.B. Nemeroff / Personalized medicine in psychiatry 1–2 (2017) 11–25 [374,375] longitudinal studies reported that depression symptoms were associated with a decrease in BMD at the total hip. One of these studies [374] found that the number of depressive symptoms correlated with rates of bone loss. In the other study [375], depressive symptoms in men were associated with lower BMD with and without adjustment for medication use. Cizza et al. performed a meta-analysis concluding that depression is associated with loss of bone mass leading to osteoporosis [376]. Yirmiya and Bab [377] evaluated data from 23 projects and found a significant association between depression and lower bone density. A review of studies between 1994 and 2007 found a possible association between depression and osteoporosis [378]. In another metaanalysis, Wu et al. showed a pooled lower BMD at the spine and hip for depressed subjects compared to non-depressed controls [357]. A study assessing determinants of osteoporotic fractures suggests that depression can be considered a predisposing factor with clinical significance and magnitude of impact similar to other established risk factors [379]. Data summarized in the American Geriatrics Society guidelines suggest that depression confers a higher mean relative risk for falls (2.2) than cognitive impairment (1.8) or age 80 years and older (1.7) [381]. The MOBILIZE Boston Study showed that the association of depressive symptoms with fall risk in older adults is mediated in part by chronic pain [382]. A bidirectional relationship of depression with falls proposes the mechanism of excessive fear of falling, which, through impairment of gait and balance, mediated through cognitive, sensory, and motor pathways, leads to further increase in fall risk [383]. The Multiple Outcomes of Raloxifene Evaluation (MORE) study showed an increased prevalence of depression among patients with osteoporosis, especially in postmenopausal women with vertebral fractures. The number of fractures resulted in a proportionately more severe score on the Geriatric Depression Scale [373]. In a prospective study of older Mexican-American women, higher levels of depression predicted self-reported fractures [385]. In a prospective population-based study of Norwegian women aged 50 or older, those with the highest level of distress were at greater risk for hip fracture [386]. In a large cohort of subjects aged 25–74 followed for 22 years, depression predicted hip fractures after adjusting for age, gender, race, BMI, smoking, alcohol, and physical activity [354]. Middle aged women with depression had a 40% increase for non-vertebral fractures compared to women without depression after adjusting for their increased likelihood of falling [387]. In a longitudinal cohort study in Norway, both pre- and post-menopausal women with mental distress had increased fracture risk [388]. Hypercortisolemia has been hypothesized to be an important causative factor for the observed bone deficits in depression. Depression is associated with a sustained and protracted activation of the stress system and thereby leads to excessive activity of the HPA and sympathoadrenal axes [363,391,392] with increased corticotropin-releasing hormone (CRH) production [362]. A few studies have observed increased plasma cortisol [393,394] or increased UFC [391] though no differences were found in other studies [393,356,395–397,360]. Salivary cortisol following a public speech task was higher in 9 depressed postmenopausal women compared to 10 non-depressed postmenopausal women [398]. Depressed women also had significantly lower total lumbar and femur BMD, demonstrating a negative relationship between poststress salivary cortisol and BMD. Depression also results in suppression of the gonadal and somatotrophic axes with decreased production of growth hormone-releasing hormone (GHRH) and gonadotropin-releasing hormone (GnRH), which suppresses the secretion of GH and gonadal steroids, respectively. CRH also stimulates catecholamine release, inducing IL-6 production. The hyperactivity of the HPA and sympathoadrenal axes, together with the suppression of the somatotrophic and gonadal axes, results in decreased bone formation [399]. Depression’s association with excessive adrenergic activity results in an increase in bone norepinephrine levels accompanied by restrained bone formation resulting from reduced osteoblast number and skeletal deficiency. This mechanism suggests a role for the sympathetic nervous system in the skeletal effects of depression [400]. Treatment with SSRIs may also interfere with 5-HT uptake by bone [401,402]. It has been suggested that there is a dual effect of 5-HT on bone metabolism with anabolic action from the brain-derived substance and catabolic action from the gut-produced circulating 5-HT [403], and this could determine the basis for understanding the effects of SSRIs on bone health. Leptin may play a role in the skeletal complications seen in patients with depression. In animal models, leptin resulted in bone loss by centrally inhibiting bone formation via activation of the sympathetic nervous system [410]. In depressed subjects, reports of serum leptin levels have been conflicting [368,393,411–413]. Evidence indicates that leptin acts centrally, through its receptor in serotonin-producing neurons of the raphe nuclei, decreasing the expression of tryptophan hydroxylase 2, the gene encoding the initial enzyme for serotonin biosynthesis [363,407]. Thus leptin regulation of bone metabolism and bone mass may be mediated through its inhibition of nuclear serotonin synthesis [414]. Other data on leptin suggest that it plays an anabolic role in bone formation and its administration increases insulin-like growth factor 1, osteocalcin, osteoprotegerin and receptor activator of NFƙB ligand (RANKL) [415]. There are multiple reports of reduced vitamin D concentrations in depressed patients [418–425]. Low levels of 25-OH vitamin D could lead to both depression and lower BMD [420]. Women with depression had slightly higher PTH levels and had lower 25-OH vitamin D and ionized calcium levels compared to controls [356]. Vitamin D receptors are present in several human brain areas involved in neuroendocrine and autonomic functions [424], potentially supporting a direct role of vitamin D in modulating mood and behavior in depression. Vitamin D deficiency and concurrent hyperparathyroidism are known predisposing factors for osteoporosis [425]. No association of depression and PTH has been shown in some [422,426,427] but not all studies [365]. However, very recent reviews associate primary hyperparathyroidism with depression and link parathyroidectomy with symptom alleviation [428]. Since PTH receptors have been found in hypothalamic, limbic, and sensory brain regions that potentially exert an influence on the neuroendocrine system [429], chronically elevated PTH levels may have a direct effect on the nervous system, thus affecting mood. On the other hand, an increase in bone remodeling, independent of vitamin D deficiency, may induce calcium release and inhibition of parathyroid hormone secretion in patients with depressive disorders [430]. Low bone mass in patients treated with antidepressants has been reported since the 1990s [363]. The Women’s Health Initiative Observational Study [431] reported that antidepressant use was associated with more fractures at the spine and other sites, even in the absence of changes in BMD. SSRIs have collectively been associated with osteoporosis and fractures [363,432,433]. In the Study of Osteoporotic Fractures, elderly women treated with SSRIs experienced greater bone loss at the hip, likely due to a class-specific effect because no increase was observed in patients treated with TCAs [434]. SSRIs have been linked to falls, bone loss, and fractures [435,436,383,437]. A recent meta-analysis implicated the use of SSRIs with a twofold increase in fracture risk with a dose-response relationship for SSRIs and an effect linked to the affinity of each SSRI for the serotonin transporter. Compared to non-SSRI users, SSRIs increase the relative risk of fracture by 72 % [436]. Use of SSRIs was associated with a 2.25-fold increase in J.L. Sotelo, C.B. Nemeroff / Personalized medicine in psychiatry 1–2 (2017) 11–25 fracture risk in a large cohort study conducted in Rotterdam [438]. Serotonin transporters and receptors have been identified on osteoblasts [439] suggesting a direct effect on bone mass. In addition, use of SSRIs and TCAs might induce fractures by increasing risk of falls, especially in the elderly, possibly through arrhythmias or postural hypotension [440]. A recent study of middle-aged women initiating antidepressants did not find a significant decrease in BMD in new users of SSRIs or TCAs [375]. Bone turnover markers (BTM) are products released during bone matrix synthesis or degradation. In some studies, depressed patients show increased urinary levels of bone resorption markers [360,377] and serum osteocalcin, PTH and C-terminal telopeptide (CTX) [430]. This probably reflects increased bone remodeling. In a recent study, bone turnover markers, PTH and Receptor for Nuclear Factor B Ligand were significantly higher in depressed patients compared to controls, while serum levels of 25hydroxyvitamin D and osteoprotegerin were significantly lower [366]. Two prospective studies have examined the relationship between BTMs and antidepressant use. In the first study treatment with escitalopram was associated with a significant decrease in the bone resorption marker beta-CTX but only in participants whose depression improved [450]. The second study, involving older men and women, found that treatment with venlafaxine was associated with significantly increased levels of the bone resorption marker only in participants whose depression did not remit [451]. Furthermore, the bone formation marker did not change in the overall group but it significantly decreased in individuals genetically defined as having high transcription of the serotonin transporter and low transcription of the serotonin 1B receptor, a receptor known to be involved in bone formation [452]. These preliminary results suggest that antidepressant treatment leading to remission of depression may have a positive effect on bone homeostasis, whereas unsuccessful antidepressant treatment may have no or deleterious effects on bone resorption. Lifestyle factors play a relatively small role in inducing bone loss in subjects with depression. Studies report no differences in dietary calcium intake [356,453,374,434,369] or calcium supplementation [387,362] in subjects with depression compared to controls. Smoking has been correlated with bone loss but most studies found no differences between depressed and non-depressed subjects [373,356,395,396,374,434,370,365,361,454]. Alcohol intake is also an established risk factor for osteoporosis and yet was found to be either similar in subjects with depression and controls [356,369–371,355,455], or significantly lower in subjects with depression [354,387,361]. A systematic review of the English literature from 1990 to 2006 reported inconsistent or insufficient evidence to conclude that any of those factors are associated with BMD [456]. Depression and stroke Nearly one third of stroke survivors develop depression [292]. Conversely, depression has been linked to various risk factors for stroke [293–296]. Prior studies have found that depression and dementia are individually associated with increased risk of stroke [296–306]. There is evidence suggesting that depressive symptoms or diagnoses consistently predict elevated risk of stroke onset [298–300]. Recent meta-analyses examining the effects of depression and depressive symptoms on stroke risk estimated an adjusted HR of 1.45 (95% CI 1.29–1.63) and an overall adjusted HR of 1.34 (95% CI 1.17–1.54). Depressive phenotypes have been linked with various physiological risk factors for stroke that develop slowly over time, such as hypertension, atherosclerosis [293,307], dysregulation of the autonomic nervous system [294] and increased inflam- 17 matory responses [295,296]. Alternatively, depression may influence stroke risk via short-term biological processes or stroke triggers, such as cerebrovascular reactivity or AF [308]. Triggers can spur stroke regardless of a person’s underlying vascular pathology [309] and may include infection [310] or AF [311,116]. Acute infection, for example, can increase platelet reactivity and platelet-leukocyte interactions, increasing platelet aggregation [309]. Damage can also be incurred by indirect effects of depression on health behaviors, whereby depressed individuals are more likely to engage in deleterious behavior such as smoking and physical inactivity [311]. A recent study found that persistent depression is associated with twice the risk of stroke in adults over 50 [312]. Researchers interviewed 16,178 initially stroke free participants over the age of 50 in the Health and Retirement Study every 2 years from 1998 to 2010. Subjects with persistent depressive symptoms at two consecutive interviews had twice the risk of having a first stroke in the two years after assessment compared with participants with low depressive symptoms (adjusted HR of 2.14, 95% CI 1.69–2.71). This increased risk was observed in all subgroups analyzed, with a slightly higher risk in women (adjusted HR 2.59) than in men (adjusted HR 1.96). Risk of stroke was also increased in those who had experienced depression at some point but whose symptoms had remitted (HR1.66, 95% CI 1.22–2.26). The risk of stroke in this study remained elevated even if depressive symptoms had resolved, suggesting a long-term effect of depression. A recent retrospective-cohort study examined 7031 individuals older than 50 years who participated in the Health and Retirement Study [314]. After adjusting for demographic characteristics, cognitive impairment without dementia alone (OR 1.39, 95% CI 1.13– 1.71) and co-occurring depression and cognitive impairment without dementia (OR 1.76, 95% CI 1.33–2.32) remained associated with increased odds of ischemic stroke, whereas dementia alone and co-occurring depression and dementia were no longer significantly associated with odds of ischemic stroke. These associations persisted after adjusting for medical comorbidities and health-risk behaviors. This data identified cognitively impaired women as a subgroup that may be at elevated risk, a finding consistent with prior work [315]. The results of this study confirmed previous findings that individuals with co-occurring depression and cognitive impairment are a uniquely at risk population for a wide range of adverse outcomes, including cognitive decline, institutionalization and mortality [316,317]. Co-occurring depression and cognitive impairment may be associated with increased risk of ischemic stroke through several mechanisms. A biologically plausible mediator is endothelial dysfunction and impaired regulation of coagulation pathways. Mild cognitive impairment and depression have been associated with fibrinogen dysregulation and exaggerated platelet reactivity [130,318], both of which could predispose to vascular pathology and ischemic stroke [319]. Prior work has established that depression in older adults with medical illnesses is frequently chronic [323] and rates of depression among HRS participants have been found to be fairly stable over time [324]. Depression and diabetes The prevalence of depression is increased in patients with diabetes. Anderson et al. [326] performed a meta-analysis that included studies of patients with type 1 and 2 diabetes. The overall odds of depression were twice as high for patients with diabetes compared to non-diabetic controls (OR = 2.0, 95% CI 1.8–2.2). Pouwer et al. [327] found that the prevalence of depressive affect was 25% and 30% for men and women, respectively, in type 1 dia- 18 J.L. Sotelo, C.B. Nemeroff / Personalized medicine in psychiatry 1–2 (2017) 11–25 betes, when using the Center for Epidemiologic Studies Depression Scale (CES-D) questionnaire. The prevalence of a major depressive disorder was 8% when using the WHO Composite International Diagnostic Interview (CIDI). In this study, depression was associated with the presence of proliferative retinopathy and suboptimal glycemic control. In a large cross-sectional study that included more than 200,000 adults, individuals with diabetes had an increased risk of an episode of depressive symptoms (adjusted OR 2.36, 95% CI 1.91–2.92). Comparable associations were found in South American, Asian, and European countries [328]. Substantial evidence supports the hypothesis that depression is a risk factor for the onset and exacerbation of diabetes [335,336]. Thirty-three articles published between 1991 and 2012 involving over 2 million participants were reviewed in a recent metaanalysis [338]. This meta-analysis found that depression is associated with an increased risk for developing diabetes mellitus with a pooled relative risk of 1.41 (95% CI, 1.25–1.59). Four similar metaanalyses also conducted recently [330,339–341] found such an association with relative risk for type 2 diabetes mellitus of 1.25 (95% CI, 1.02–1.48) [339], 1.37 (95% CI, 1.14–1.63) [341], 1.60 (95% CI, 1.37–1.88) [340] and 1.38 (95% CI, 1.23–1.55) [330]. Comorbid diabetes and depression has been associated with poorly controlled diabetes. Although there is a modest association between depression and poorly controlled diabetes, there is a stronger association between depressive symptoms and diabetes complications including retinopathy, sexual dysfunction, and nephropathy. Given the negative impact of depression upon diabetes, several investigators have also documented that patients with depression and diabetes suffer premature mortality [332]. Multiple biological mechanisms may contribute to the relationship between depression and diabetes. These include activation of inflammatory processes and the hypothalamic-pituitaryadrenal (HPA) axis as well as abnormalities in glucose metabolism [333]. Depression and mental stress is associated with subclinical hypercortisolism, blunted diurnal cortisol rhythm, or hypocortisolism with impaired glucocorticoid sensitivity, and increased catecholamines and inflammation secondary to hypothalamicpituitaryadrenal (HPA) axis activation [334]. Low-grade systemic inflammation has been associated with the development of type 2 diabetes [342]. Prolonged hypercortisolemia is associated with visceral adiposity, insulin resistance, dyslipidemia, and hypertension. It can also worsen atherosclerosis by increasing vessel fragility, changes in lipids and catecholamines, which increase heart rate and contribute to increased risk for thrombus formation through increased platelet aggregation. Adipose tissue and damaged vessels then release pro-inflammatory cytokines, which can induce anhedonia, anorexia, sleep changes, and decreased social interaction. All these biological pathways are activated in major depression and are associated with insulin resistance. It has been suggested that the key to metabolic syndrome, insulin resistance, and the development of type 2 diabetes is hypothalamic hyperactivity and excessive sympathetic drive [343]. HPA axis hyperactivity has been posited as a contributing factor to increasing abdominal obesity and stress has been hypothesized to cause a more central distribution of fat, which in turn can give rise to diabetes [344]. Serum BDNF concentrations are decreased in patients with depression [346,347]. BDNF is also strongly associated with type 2 diabetes and obesity because it modulates the secretion and activities of insulin, leptin, ghrelin, neurotransmitters, neuropeptides, and proinflammatory cytokines associated with energy homeostasis [348]. In addition, animal studies have also shown that BDNF has important effects on the regulation of eating behavior, suggesting that BDNF may also play a role in the development of obesity and type 2 diabetes in humans [349]. Finally, the development of diabetes in people with depression may be related to behaviors observed in depression (such as inactivity, poor diet, weight gain, poor medication adherence) [337,350] or to the medications used to treat it, rather than to the depression itself. Conclusions Depression is common in the general population. Depression may be conceptualized as a systemic illness because of the several biological mechanisms by which it can affect general health. A bidirectional relationship between depression and some of the medical disorders examined above has already been established through an emerging literature reporting on the medical complications of depression. Enhanced inflammation, HPA axis hyperactivity, disrupted arterial wall repair, oxidative damage, decreased heart rate variability, and sympathetic nervous system dysregulation are some of the findings that account for the extent to which depression can increase susceptibility to, and complicate the prognosis of, other medical conditions. Heart disease, cancer, stroke, diabetes, and osteoporosis are also common medical conditions afflicting an increasingly aging population and the prevalence of depression in patients with these disorders is greater than that which is observed in the general population. Patients with these conditions who exhibit depressive symptoms are at greater risk for morbidity and mortality than their nondepressed counterparts. Indeed depression has been identified as an independent risk factor for some of these conditions. Therefore, it is imperative that depressive symptoms be treated aggressively in patients with chronic medical conditions because their resolution may be accompanied by general symptomatic improvement and an important decrease in complications and mortality risk. The effects of childhood trauma in patients with general medical conditions need to be studied in greater detail. Not only are early adverse experiences associated with an increased risk for depression and anxiety syndromes later in life, they may also predispose patients to poorer medical outcomes through similar mechanisms, such as increased inflammation and HPA axis hyperactivity. Depressed patients are also more likely to exhibit limited adherence to treatment recommendations, such as lifestyle modifications (abstinence from tobacco, alcohol, and recreational drugs; exercise; dietary changes), clinic appointments, and appropriate medication compliance. Our review does not support a greater role to these factors than the biological mechanisms described. This review highlights the bidirectional mechanisms by which depression and medical illness may affect each other. A recent meta-analysis of randomized clinical trials (10 publications reporting on 14 trials and over 6200 participants) reviewed the effect of anti-inflammatory treatments on depression [472]. Antiinflammatory treatments, in particular the selective cyclooxygenase 2 inhibitor celexoxib, reduced depressive symptoms compared with placebo. Biomarkers cannot yet reliably be used to determine which patients may benefit from a specific treatment or which treatments should be used in a particular patient. However, our understanding of depression has evolved from the days of the monoaminergic hypothesis of the illness, paving the way for new antidepressant treatments that could target the biological mechanisms of disease outlined in this review. Such treatments could hypothetically treat the symptoms of depression and improve medical outcomes in patients with chronic medical illness, as well. Future research focusing on the interplay between depression and medical illness should further elucidate the underlying pathophysiology responsible for increased morbidity and mortality in J.L. Sotelo, C.B. Nemeroff / Personalized medicine in psychiatry 1–2 (2017) 11–25 depressed and medically compromised individuals. Interventions that target the biological alterations observed in depressed patients could theoretically improve the course of illness in those individuals. References [1] Üstün TB, Ayuso-Mateos JL, Chatterji S, Mathers C, Murray CJ. Global burden of depressive disorders in the year 2000. Br J Psychiatry 2004;184:386–92. [2] Moesgaard IK, Voss T, Salomon J, Murray CJL. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study. Lancet 2013;2015:1–58. [4] Lippi G, Montagnana M, Favalor EJ, Franchini M. Mental depression and cardiovascular disease: a multifaceted, bidirectional association. Semin Thromb Hemost 2009;35:325–36. [5] Musselman DL, Cowles MK, McDonald W, Nemeroff CB. In: Fuster V, O’Rourke RA, Walsh RA, Poole-Wilson P, editors. Hurst’s The Heart. New York: McGrawHill; 2008. p. 2169–87. [6] Kahn FM, Kulaksizoglu B, Cilingiroglu M. Depression and coronary heart disease. Curr Atheroscler Rep 2010;12:105–9. [7] Cowles M, Nemeroff CB, Pariente C. In: Pariente C, Nesse RM, Nutt D, Wolpert L, editors. Understanding depression: a translational approach. Oxford University Press; 2009. p. 7–16. [9] Blazer DG, Kaplan BH. Controversies in community-based psychiatric epidemiology: let the data speak for themselves. Arch Gen Psychiatry 2000;57:227–8. [10] Licinio J, Yildiz B, Wong ML. Depression and cardiovascular disease: cooccurrence of shared genetic substrates? Mol Psychiatry 2002;7:1031–2. [12] Musselman DL, Evans DL, Nemeroff CB. The relationship of depression to cardiovascular disease: epidemiology, biology, and treatment. Arch Gen Psychiatry 1998;55:580–92. [13] Mavrides N, Nemeroff CB. Treatment of depression in cardiovascular disease. Depress Anxiety 2013;30:328–41. [14] Nemeroff CB, Goldschmidt-Clermont PJ. Heartache and heartbreak—the link between depression and cardiovascular disease. Nat Rev Cardiol 2012;9:526–39. [15] Seligman F, Nemeroff CB. The interface of depression and cardiovascular disease: therapeutic implications. Ann N Y Acad Sci 2015;1345:25–35. [16] Rudisch B, Nemeroff CB. Epidemiology of comorbid coronary artery disease and depression. Biol Psychiatry 2003;54:227–40. [17] Carney RM, Freedland KE, Steinmeyer B, Rubin EH, Mann DL, Rich MW. Cardiac risk markers and response to depression treatment in patients with coronary heart disease. Psychosom Med 2015. http://dx.doi.org/10.1097/ PSY.0000000000000245. [18] Gan Y, Gong Y, Tong X, Sun H, Cong Y, Dong X, et al. Depression and the risk of coronary heart disease: a meta-analysis of prospective cohort studies. BMC Psychiatry 2014;14:371. [19] Meyer T, Hussein S, Lange HW, Herrmann-Lingen C. Transient impact of baseline depression on mortality in patients with stable coronary heart disease during long-term follow-up. Clin Res Cardiol 2014;103:389–95. [20] Frasure-Smith N, Lespérance F, Talajic M. Depression following myocardial infarction: impact on 6-month survival. JAMA 1993;270:1819–25. [21] May HT, Horne BD, Carlquist JF, Sheng X, Joy E, Catinella AP. Depression after coronary artery disease is associated with heart failure. J Am Coll Cardiol 2009;53:1440–7. [22] Kato N, Kinugawa K, Yao A, Hatano M, Shiga T, Kazuma K. Relationship of depressive symptoms with hospitalization and death in Japanese patients with heart failure. J Cardiac Fail 2009;15:912–9. [23] Lesman Leegte I, Veldhuisen DJ, Hillege HL, Moser D, Sanderman R, Jaarsma T. Depressive symptoms and outcomes in patients with heart failure: data from the COACH study. Eur J Heart Fail 2009;11:1202–7. [24] Frasure-Smith N, Lespérance F, Habra M, Talajic M, Khairy P, Dorian P, et al. Elevated depression symptoms predict long-term cardiovascular mortality in patients with atrial fibrillation and heart failure. Circulation 2009;120:134–40. [25] Glassman AH, Bigger Jr JT, Gaffney M. Psychiatric characteristics associated with long-term mortality among 361 patients having an acute coronary syndrome and major depression: seven-year follow-up of SADHART participants. Arch Gen Psychiatry 2009;66:1022–9. [26] Tully PJ, Baker RA, Turnbull D, Winefield H. The role of depression and anxiety symptoms in hospital readmissions after cardiac surgery. J Behav Med 2008;31:281–90. [27] Dao TK, Chu D, Springer J, Gopaldas RR, Menefee DS, Anderson T, et al. Clinical depression, posttraumatic stress disorder, and comorbid depression and posttraumatic stress disorder as risk factors for in-hospital mortality after coronary artery bypass grafting surgery. J Thorac Cardiovasc Surg 2010;140:606–10. [28] Kendel F, Gelbrich G, Wirtz M, Lehmkuhl E, Knoll N, Hetzer R, et al. Predictive relationship between depression and physical functioning after coronary surgery. Arch Intern Med 2010;170:1717–21. [36] Anda R, Williamson D, Jones D, Macera C, Eaker E, Glassman A, et al. Depressed affect, hopelessness, and the risk of ischemic heart disease in a cohort of US adults. Epidemiology 1993;4:285–94. 19 [37] Barefoot JC, Scroll M. Symptoms of depression, acute myocardial infarction, and total mortality in a community sample. Circulation 1996;93:1776–80. [38] Schulz R, Beach SR, Ives DG, Martire LM, Ariyo AA, Kop WJ. Association between depression and mortality in older adults: the Cardiovascular Health Study. Arch Intern Med 2000;160:1761–8. [39] Ford DE, Mead LA, Chang PP, Cooper-Patrick L, Wang NY, Klag MJ. Depression is a risk factor for coronary artery disease in men: the precursors study. Arch Intern Med 1998;158:1422–6. [40] Ferketich AK, Schwartzbaum JA, Frid DJ, Moeschberger ML. Depression as an antecedent to heart disease among women and men in the NHANES I study. Arch Intern Med 2000;160:1261–8. [41] Ariyo AA, Haan M, Tangen CM, Rutledge JC, Cushman M, Dobs A, et al. Depressive symptoms and risks of coronary heart disease and mortality in elderly Americans. Circulation 2000;102:1773–9. [42] Aromaa A, Raitasalo R, Reunanen A, Impivaara O, Heliovaara M, Knekt P, et al. Depression and cardiovascular diseases. Acta Psychiatr Scand 1994;89 (s377):77–82. [43] Jiang W, Krishnan RR, O’Connor CM. Depression and heart disease: evidence of a link, and its therapeutic implications. CNS Drugs 2002;16:111–27. [45] Surtees PG, Wainwright NW, Luben RN, Wareham NJ, Bingham SA, Khaw KT. Depression and ischemic heart disease mortality: evidence from the EPICNorfolk United Kingdom prospective cohort study. Am J Psychiatry 2008;165:515–23. [46] Jakobsen AH, Foldager L, Parker G, Munk-Jorgensen P. Quantifying links between acute myocardial infarction and depression, anxiety and schizophrenia using a care register database. J Affect Disord 2008;109:177–81. [47] Kendler K, Gardner CO, Fiske A, Gatz M. Major depression and coronary artery disease in the Swedish Twin Registry: phenotypic, genetic, and environmental sources of comorbidity. Arch Gen Psychiatry 2009;66:857–63. [48] Mannie ZN, Williams C, Diesch J, Steptoe A, Leeson P, Cowen PJ. Cardiovascular and metabolic risk profile in young people at familial risk of depression. Br J Psychiatry 2013;203:18–23. [49] Meijer A, Conradi HJ, Bos EH, Thombs BD, van Melle JP, de Jonge P. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis of 25 years of research. Gen Hosp Psychiatry 2011;33:203–16. [50] Miller GE, Stetler CA, Carney RM, Freedland KE, Banks WA. Clinical depression and inflammatory risk markers for coronary heart disease. Am J Cardiol 2002;90:1279–83. [51] Doering LV, Moser DK, Riegel B, McKinley S, Davidson P, Baker H, et al. Persistent comorbid symptoms of depression and anxiety predict mortality in heart disease. Int J Cardiol 2010;145:188–92. [52] Versteeg H, Hoogwegt MT, Hansen TB, Pedersen SS, Zwuisler A-D, Thygesen LC. Depression, not anxiety, is independently associated with 5-year hospitalizations and mortality in patients with ischemic heart disease. J Psychosom Res 2013;75:518–25. [53] Beach SR, Januzzi JL, Mastromauro CA, Healy BC, Beale EE, Celano CM, et al. Patient Health Questionnaire-9 score and adverse cardiac outcomes in patients hospitalized for acute cardiac disease. J Psychosom Res 2013;75:409–13. [58] Gottlieb SS, Khatta M, Friedmann E, Einbinder L, Katzen S, Baker B, et al. The influence of age, gender, and race on the prevalence of depression in heart failure patients. J Am Coll Cardiol 2004;43:1542–9. [59] Konstam V, Moser DK, De Jong MJ. Depression and anxiety in heart failure. J Card Fail 2005;11:455–63. [60] Moser DK, Dracup K, Evangelista LS, Zambroski CH, Lennie TA, Chung ML, et al. Comparison of prevalence of symptoms of depression, anxiety, and hostility in elderly patients with heart failure, myocardial infarction, and a coronary artery bypass graft. Heart Lung J Acute Crit Care 2010;39:378–85. [61] Denollet J, Brutsaert DL. Personality, disease severity, and the risk of longterm cardiac events in patients with a decreased ejection fraction after myocardial infarction. Circulation 1998;97:167–73. [63] Jiang W, Alexander J, Christopher E, Kuchibhatla M, Gaulden LH, Cuffe MS, et al. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch Intern Med 2001;161:1849–56. [64] Rumsfeld JS, Havranek E, Masoudi FA, Peterson ED, Jones P, Tooley JF, et al. Cardiovascular Outcomes Research Consortium. Depressive symptoms are the strongest predictors of short-term declines in health status in patients with heart failure. J Am Coll Cardiol 2003;42:1811–7. [65] Rozzini R, Sabatini T, Frisoni GB, Trabucchi M. Depression and major outcomes in older patients with heart failure. Arch Intern Med 2002;162:362–4. [66] Penninx BW, Beekman AT, Honig A, Deeg DJ, Schoevers RA, van Eijk JT, et al. Depression and cardiac mortality: results from a community-based longitudinal study. Arch Gen Psychiatry 2001;58:221–7. [67] Vaccarino V, Kasl SV, Abramson J, Krumholz HM. Depressive symptoms and risk of functional decline and death in patients with heart failure. J Am Coll Cardiol 2001;38:199–205. [68] Angermann CE, Gelbrich G, Störk S, Fallgatter A, Deckert J, Faller H, et al. MOOD-HF investigators: rationale and design of a randomized, controlled, multicenter trial investigating the effects of selective serotonin re-uptake inhibition on morbidity, mortality, and mood n depressed heart failure patients (MOOD-HF). Eur J Heart Fail 2007;9:1212–22. 20 J.L. Sotelo, C.B. Nemeroff / Personalized medicine in psychiatry 1–2 (2017) 11–25 [69] Murberg TA, Bru E. Social relationships and mortality in patients with congestive heart failure. J Psychosom Res 2001;5:521–7. [70] Murberg TA, Bru E, Aarsland T, Svebak S. Functional status and depression among men and women with congestive heart failure. Int J Psychiatry Med 1998;28:273–91. [71] Murberg TA, Bru E, Svebak S, Tveterås R, Aarsland T. Depressed mood and subjective health symptoms as predictors of mortality in patients with congestive heart failure: a two-years follow-up study. Int J Psychiatry Med 1999;29:311–26. [72] Faris R, Purcell H, Henein MY, Coats AJS. Clinical depression is common and significantly associated with reduced survival in patients with non-ischaemic heart failure. Eur J Heart Fail 2002;4:541–51. [73] Jiang W, Kuchibhatla M, Cuffe MS, Christopher EJ, Alexander JD, Clary GL, et al. Prognostic value of anxiety and depression in patients with chronic heart failure. Circulation 2004;110:3452–6. [75] Alhurani AS, Dekker RL, Abed MA, Khalil A, Al Zaghal MH, Lee KS, et al. The association of co-morbid symptoms of depression and anxiety with all-cause mortality and cardiac rehospitalization in patients with heart failure. Psychosomatics 2015;56:371–80. [76] Halaris A. Inflammation, heart disease, and depression. Curr Psychiatry Rep 2013;15:1–9. [77] Kop WJ, Gottdiener JS. The role of immune system parameters in the relationship between depression and coronary artery disease. Psychosom Med 2005;67:S37–41. [78] Maes M, Ruckoanich P, Chang YS, Mahnonda N, Berk M. Multiple aberrations in shared inflammatory and oxidative & nitrosative stress (IO&NS) pathways explain the co-association of depression and cardiovascular disorder (CVD), and the increased risk for CVD and due mortality in depressed patients. Prog Neuropsychopharmacol Biol Psychiatry 2011;35:769–83. [79] McCaffery JM, Frasure-Smith N, Dube M-P, Theroux P, Rouleau GA, Dan Q, et al. Common genetic vulnerability to depressive symptoms and coronary artery disease: a review and development of candidate genes related to inflammation and serotonin. Psychosom Med 2006;68:187–200. [80] Givertz MM, Colucci WS. New targets for heart-failure therapy: endothelin, inflammatory cytokines, and oxidative stress. Lancet 1998;352:I34–138. [81] Seta Y, Shan K, Bozkurt B, Oral H, Mann DL. Basic mechanisms in heart failure: the cytokine hypothesis. J Card Fail 1996;2:243–9. [82] Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. NEJM 2005;352:1685–95. [83] Libby P. Inflammation and cardiovascular disease mechanisms. Am J Clin Nutr 2006;83:456S–60S. [84] Frasure-Smith N, Lespérance F, Irwin MR, Sauvé C, Lespérance J, Théroux P. Depression, C-reactive protein and two-year major adverse cardiac events in men after acute coronary syndromes. Biol Psychiatry 2007;62:302–8. [85] Suarez EC. C-reactive protein is associated with psychological risk factors of cardiovascular disease in apparently health adults. Psychosom Med 2004;66:684–91. [86] Suarez EC, Krishnan RR, Lewis JG. The relation of severity of depressive symptoms to monocyte-associated proinflammatory cytokines and chemokines in apparently healthy men. Psychosom Med 2003;65:362–8. [87] Kop WJ, Gottdiener JS, Tangen CM, Fried LP, McBurnie MA, Walston J, et al. Inflammation and coagulation factors in persons >65 years of age with symptoms of depression but without evidence of myocardial ischemia. Am J Cardiol 2002;89:419–24. [88] Dentino AN, Pieper CF, Rao MK, Currie MS, Harris T, Blazer DG, et al. Association of interleukin-6 and other biologic variables with depression in older people living in the community. J Am Geriatr Soc 1999;47:6–11. [89] Miller AH, Maletic V, Raison CL. Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression. Biol Psychiatry 2009;65:732–41. [90] Musselman DL, Miller AH, Porter MR, Manatunga A, Gao F, Penna S, et al. Higher than normal plasma interleukin-6 concentrations in cancer patients with depression: preliminary findings. Am J Psychiatry 2001;158:1252–7. [91] Lindqvist D, Janelidze S, Hagell P, Erhardt S, Samuelsson M, Minthon L, et al. Interleukin-6 is elevated in the cerebrospinal fluid of suicide attempters and related to symptom severity. Biol Psychiatry 2009;66:287–92. [92] Davidson KW, Schwartz JE, Kirkland SA, Mostofsky E, Fink D, Guernsey D, et al. Relation of inflammation to depression and incident coronary heart disease (from the Canadian Nova Scotia Health Survey [NSHS95] Prospective Population Study). Am J Cardiol 2009;103:755–61. [97] Howren MB, Lamkin DM, Suls J. Associations of depression with C-reactive protein, IL-1, and IL-6: a meta analysis. Psychosom Med 2009;71:171–86. [98] Currier MB, Nemeroff CB. Inflammation and mood disorders: proinflammatory cytokines and the pathogenesis of depression. AntiInflammatory Antiallergy Agents Med Chem 2010;9:212–20. [99] Raison CL, Cowles MK, Miller AH. In: Schatzberg AF, Nemeroff CB, editors. Textbook of psychopharmacology. Washington, DC: American Psychiatric Publishing; 2009. p. 201–20. [100] Raedler TJ. Inflammatory mechanisms in major depressive disorder. Curr Opin Psychiatry 2011;24:519–25. [101] Parissis JT, Adamopoulos S, Rigas A, Kostakis G, Karatzas D, Venetsanou K, et al. Comparison of circulating proinflammatory cytokines and soluble apoptosis mediators in patients with chronic heart failure with versus without symptoms of depression. Am J Cardiol 2004;94:1326–8. [102] Pizzi C, Manzoli L, Mancini S, Costa GM. Analysis of potential predictors of depression among coronary heart disease risk factors including heart rate variability, markers of inflammation, and endothelial function. Eur Heart J 2008;29:1110–7. [106] Dantzer R, O’Connor JC, Lawson MA, Kelley KW. Inflammation-associated depression: from serotonin to kynurenine. Psychoneuroendocrinology 2011;36:426–36. [107] Wichers MC, Maes M. The role of indoleamine 2,3-dioxygenase (IDO) in the pathophysiology of interpheron-alpha-induced depression. J Psychiatry Neurosci 2004;29:11–7. [108] Lapin IP, Oxenkrug GF. Intensification of the central serotoninergic processes as a possible determinant of the thymoleptic effect. Lancet 1969;1:132–6. [109] Myint AM, Kim YK. Cytokine-serotonin interaction through IDO: a neurodegeneration hypothesis of depression. Med Hypotheses 2003;61:519–25. [110] Pace TW, Hu F, Miller AH. Cytokine-effects on glucocorticoid receptor function: relevance to glucocorticoid resistance and the pathophysiology and treatment of major depression. Brain Behav Immun 2007;21:9–19. [111] Stewart JC, Rand KL, Muldoon MF, Kamarck TW. A prospective evaluation of the directionality of the depression-inflammation relationship. Brain Behav Immun 2009;23:936–44. [112] Rohleder N, Kudielka BM, Hellhammer DH, Wolf JM, Kirschbaum C. Age and sex steroid-related changes in glucocorticoid sensitivity of proinflammatory cytokine production after psychosocial stress. J Neuroimmunol 2002;126:69–77. [113] Carvalho LA, Urbanova L, Hamer M, Hackett RA, Lazzarino AI, Steptoe A. Blunted glucocorticoid and mineralocorticoid sensitivity to stress in people with diabetes. Psychoneuroendocrinology 2015;51:209–18. [114] Miller AH, Pariante CM, Pearce BD. Effects of cytokines on glucocorticoid receptor expression and function. Glucocorticoid resistance and relevance to depression. Adv Exp Med Biol 1999;461:107–16. [115] Schnabel RB, Michal M, Wilde S, Wiltink J, Wild PS, Sinning CR, et al. Depression in atrial fibrillation in the general population. PLoS One 2013;8 (12):e79109. [116] Lange HW, Herrmann-Lingen C. Depressive symptoms predict recurrence of atrial fibrillation after cardioversion. J Psychosom Res 2007;63:509–13. [117] Jones A, Steeden JA, Pruessner JC, Deanfield JE, Taylor AM, Muthurangu V. Detailed assessment of the hemodynamic response to psychosocial stress using real-time MRI. J Magn Reson Imaging 2011;33:448–54. [118] Carney RM, Freedland KE, Veith RC, Cryer PE, Skala JA, Lynch T, et al. Major depression, heart rate, and plasma norepinephrine in patients with coronary heart disease. Biol Psychiatry 1999;45:458–63. [119] Whooley MA, de Jonge P, Vittinghoff E, Otte C, Moos R, Carney RMA, et al. Depressive symptoms, health behaviors, and risk of cardiovascular events in patients with coronary heart disease. JAMA 2008;300:2379–88. [120] Nikkheslat N, Zunszain PA, Horowitz MA, Barbosa IG, Parker JA, Myint AM, et al. Insufficient glucocorticoid signaling and elevated inflammation in coronary heart disease patients with comorbid depression. Brain Behav Immun 2015;48:8–18. [121] Xiong GL, Prybol K, Boyle SH, Hall R, Streilein RD, Steffens DC, et al. Inflammation markers and major depressive disorder in patients with chronic heart failure: results from the sertraline against depression and heart disease in chronic heart failure study. Psychosom Med 2015;77:808–15. [122] Goldschmidt-Clermont PJ. Loss of bone marrow-derived vascular progenitor cells leads to inflammation and atherosclerosis. Am Heart J 2003;146: S5–S12. [123] Goldschmidt-Clermont PJ, Peterson ED. On the memory of a chronic illness. Sci Aging Knowledge Environ 2003;45:8. [124] Asahara T, Murohara T, Sullivan A, Silver M, van der Zee R, Li T, et al. Isolation of putative progenitor endothelial cells for angiogenesis. Science 1997;275:964–6. [125] Ross R. Atherosclerosis – an inflammatory disease. NEJM 1999;340:115–26. [126] Lusis AJ. Atherosclerosis. Nature 2000;407:233–41. [127] Libby P. Inflammation in atherosclerosis. Nature 2002;420:868–74. [128] Goldschmidt-Clermont PJ, Seo DM, Wang L, Beecham GW, Liu ZJ, VazquezPadron RI, et al. Inflammation, stem cells and atherosclerosis genetics. Curr Opin Mol Ther 2010;12:712–23. [129] Seshiah PN, Kereiakes DJ, Vasudevan SS, Lopes N, Su BY, Flavahan NA, et al. Activated monocytes induce smooth muscle cell death role of macrophage colony-stimulating factor and cell contact. Circulation 2002;105:174–80. [130] Musselman DL, Tomer A, Manatunga AK, Knight BT. Exaggerated platelet reactivity in major depression. Am J Psychiatry 1996;153:1313. [131] Musselman DL, Marzec UM, Manatunga A, Penna S, Reemsnyder A, Knight BT, et al. Platelet reactivity in depressed patients treated with paroxetine: preliminary findings. Arch Gen Psychiatry 2000;57:875–82. [132] Morel-Kopp MC, McLean L, Chen Q, Tofler GH, Tennant C, Maddison V, et al. The association of depression with platelet activation: evidence for a treatment effect. J Thromb Haemost 2009;7:573–81. [133] Laghrissi-Thode F, Wagner WR, Pollock BG, Johnson PC, Finkel MS. Elevated platelet factor 4 and beta-thromboglobulin plasma levels in depressed patients with ischemic heart disease. Biol Psychiatry 1997;42:290–5. [155] Rondondi N et al. Subclinical hypothyroidism and the risk of coronary heart disease and mortality. JAMA 2010;304:1365–74. [156] Nemeroff CB, Simon JS, Haggerty Jr JJ, Evans DL. Antithyroid antibodies in depressed patients. Am J Psychiatry 1985;142:840–3. J.L. Sotelo, C.B. Nemeroff / Personalized medicine in psychiatry 1–2 (2017) 11–25 [157] Gillespie CF, Garlow SJ, Schatzberg AF, Nemeroff CB. In: Schatzberg A, Nemeroff CB, editors. Textbook of psychopharmacology. Washington, DC: American Psychiatric Publishing; 2009. p. 903–44. [158] Gutman DA, Nemeroff CB. In: Squire LR, editor. Encyclopedia of neuroscience. Oxford, England: Elsevier; 2009. p. 355–66. [159] Vogelzangs N et al. Urinary cortisol and six-year risk of all-cause and cardiovascular mortality. J Clin Endocrinol Metab 2010;95:4959–64. [160] Jokinen J, Nordstrom P. HPA axis hyperactivity and cardiovascular mortality in mood disorder inpatients. J Affect Disord 2009;116:88–92. [161] Stalder T, Evans P, Hucklebridge F, Clow A. Associations between the cortisol awakening response and heart rate variability. Psychoneuroendocrinology 2011;36:454–62. [162] Lopez-Leon S et al. Shared genetic factors in the co-occurrence of symptoms of depression and cardiovascular risk factors. J Afect Disord 2010;122:247–52. [163] Yarnell J et al. Association of European population levels of thrombotic and inflammatory factors with risk of coronary heart disease: the MONICA Optional Haemostasis Study. Eur Heart J 2005;26:332–42. [164] McCaffery JM et al. Genetic predictors of depressive symptoms in cardiac patients. Am J Med Genet B Neuropsychiatr Genet 2009;150B:381–8. [165] Su S et al. Common genes contribute to depressive symptoms and heart rate variability: the Twins Heart Study. Twin Res Hum Genet 2010;13:1–9. [166] Vaccarino V et al. Depressive symptoms and heart rate variability: evidence for a shared genetic substrate in a study of twins. Psychosom Med 2008;70:628–36. [167] Bozzini S et al. Coronary artery disease and depression: possible role of brainderived neurotrophic factor and serotonin transporter gene polymorphisms. Intl J Mol Med 2009;24:813–8. [168] Dong M, Giles WH, Felitti VJ, et al. Insights into causal pathways for ischemic heart disease: adverse childhood experiences study. Circulation 2004;110:1761–6. [169] Danese A, Pariante CM, Caspi A, Taylor A, Poulton R. Childhood maltreatment predicts adult inflammation in a life-course study. Proc Natl Acad Sci 2007;104(4):1319–24. [170] Hamer M, Kivimaki M, Lahiri A, Marmot MG, Steptoe A. Persistent cognitive depressive symptoms are associated with coronary artery calcification. Atherosclerosis 2010;210:209–13. [171] Vural M, Satiroglu O, Akbas B, Goksel I, Karabay O. Coronary artery disease in association with depression or anxiety among patients undergoing angiography to investigate chest pain. Tex Heart Inst J 2009;36:17–23. [172] Kabir AA et al. Association between depression and intima-media thickness of carotid bulb in asymptomatic young adults. Am J Med 2009;122. 1151.e11151.e8. [173] Paranthaman R et al. Vascular function in older adults with depressive disorder. Biol Psychiatry 2010;68:133–9. [174] Fann JR, Thomas-Rich AM, Katon WJ, Cowley D, Pepping M, McGregor BA, Gralow J. Major depression after breast cancer: a review of epidemiology and treatment. Gen Hosp Psychiatry 2008;30:112–26. [175] Massie MJ. Prevalence of depression in patients with cancer. J Natl Cancer Inst Monogr 2004;32:57–71. [176] Miller AH, Ancoli-Israel S, Bower JE, Capuron L, et al. Neuroendocrineimmune mechanisms of behavioral comorbidities in patients with cancer. J Clin Oncol 2008;26:971–82. [177] Raison CL, Miller AH. Depression in cancer: new developments regarding diagnosis and treatment. Biol Psychiatry 2003;54:283–94. [178] Rooney AG, McNamara S, Mackinnon M, Fraser M, Rampling R, Carson A, et al. Frequency, clinical associations, and longitudinal course of major depressive disorder in adults with cerebral glioma. J Clin Oncol 2011;29:4307–12. [179] Linden W, Vodermaier A, Mackenzie R, Greig D. Anxiety and depression after cancer diagnosis: prevalence rates by cancer type, gender, and age. J Affect Disord 2012;141:343–51. [180] Ng CG, Boks MP, Zainal NZ, Wit NJ. The prevalence and pharmacotherapy of depression in cancer patients. J Affect Disord 2011;131:1–7. [181] Polsky D, Doshi JA, Marcus S, Oslin D, Rothbard A, Thomas N, et al. Long-term risk for depressive symptoms after a medical diagnosis. Arch Intern Med 2005;165:1260–6. [182] Colleoni M, Mandala M, Peruzzotti G, Robertson C, Bredart A, Goldhirsch A. Depression and degree of acceptance of adjuvant cytotoxic drugs. Lancet 2000;356:1326–7. [183] Pinquart M, Duberstein PR. Depression and cancer mortality: a metaanalysis. Psychol Med 2010;40:1797–810. [184] Stommel M, Given BA, Given CW. Depression and functional status as predictors of death among cancer patients. Cancer 2002;94:2719–27. [185] Ariaratnam S, Devi A, Kaur G, Sinniah D, Suleiman A, Thambu M, et al. Psychiatric morbidity and survival in newly diagnosed treatment naive cancer patients – a study from Malaysia. Biomed Res 2008;19:113–6. [186] Satin JR, Linden W, Phillips MJ. Depression as a predictor of disease progression and mortality in cancer patients. Cancer 2009;115:5349–61. [187] Chan CMH, Ahmad W, Azman W, MD Yusof M, Ho GF, Krupat E. Effects of depression and anxiety on mortality in a mixed cancer group: a longitudinal approach using standardised diagnostic interviews. Psycho-Oncology 2014;24:718–25. [188] Koenig HG, Shelp F, Goli V, Cohen HJ, Blazer DG. Survival and health care utilization in elderly medical inpatients with major depression. J Am Geriatr Soc 1989;37:599–606. 21 [189] Pelletier G, Verhoef MJ, Khatri N, Hagen N. Quality of life in brain tumor patients: the relative contributions of depression, fatigue, emotional distress, and existential issues. J Neurooncol 2002;57:41–9. [190] Stoudemire A, Thompson TL. Medication noncompliance: systematic approaches to evaluation and intervention. Gen Hosp Psychiatry 1983;5:233–9. [191] Giese-Davis J, Collie K, Rancourt KM, Neri E, Kraemer HC, Spiegel D. Decrease in depression symptoms is associated with longer survival in patients with metastatic breast cancer: a secondary analysis. J Clin Oncol 2011;29:413–20. [192] Mitchell AJ, Chan M, Bhatti H, Halton M, Grassi L, Johansen C, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol 2011;12:160–74. [194] Hung YP, Liu CJ, Tsai CF, Hung MH, Tzeng CH, Liu CY, et al. Incidence and risk of mood disorders in patients with breast cancers in Taiwan: a nationwide population-based study. Psycho-Oncology 2013;22:2227–34. [195] Suppli NP, Johansen C, Christensen J, Kessing LV, Kroman N, Dalton SO. Increased risk for depression after breast cancer: a nationwide populationbased cohort study of associated factors in Denmark, 1998–2011. J Clin Oncol 2014;32:3831–9. [196] Kim SH, Son BH, Hwang SY, Han W, Yang JH, Lee S, et al. Fatigue and depression in disease-free breast cancer survivors: prevalence, correlates, and association with quality of life. J Pain Symptom Manage 2008;35:644–55. [197] Chen X, Zheng Y, Zheng W, Gu K, Chen Z, Lu W, et al. Prevalence of depression and its related factors among Chinese women with breast cancer. Acta Oncol 2009;48:1128–36. [198] Metcalfe KA, Semple J, Quan ML, Vadaparampil ST, Holloway C, Brown M, et al. Changes in psychosocial functioning 1 year after mastectomy alone, delayed breast reconstruction, or immediate breast reconstruction. Ann Surg Oncol 2012;19:233–41. [199] Ganz PA, Kwan L, Stanton AL, Bower JE, Belin TR. Physical and psychosocial recovery in the year after primary treatment of breast cancer. J Clin Oncol 2011;29:1101–9. [200] Azzone V, Frank RG, Pakes JR, Earle CC, Hassett MJ. Behavioral health services for women who have breast cancer. J Clin Oncol 2009;27:706–12. [201] Steginga SK, Occhipinti S, Gardiner RF, Yaxley J, Heathcote P. Prospective study of men’s psychological and decision-related adjustment after treatment for localized prostate cancer. Urology 2004;63:751–6. [202] Potosky AL, Legler J, Albertsen PC, Stanford JL, Gilliland FD, Hamilton AS, et al. Health outcomes after prostatectomy or radiotherapy for prostate cancer: results from the Prostate Cancer Outcomes Study. J Natl Cancer Inst 2000;92:1582–92. [203] Litwin MS, Lubeck DP, Spitalny GM, Henning JM, Carroll PR. Mental health in men treated for early stage prostate carcinoma. Cancer 2002;95:54–60. [204] Litwin MS, Melmed GY, Nakazon T. Life after radical prostatectomy: a longitudinal study. J Urol 2001;166:587–92. [205] Bill-Axelson A, Garmo H, Lambe M, Bratt O, Adolfsson J, Nyberg U, et al. Suicide risk in men with prostate-specific antigen–detected early prostate cancer: a nationwide population-based cohort study from PCBaSe Sweden. Eur Urol 2010;57:390–5. [206] Fang F, Fall K, Mittleman MA, Sparén P, Ye W, Adami HO, et al. Suicide and cardiovascular death after a cancer diagnosis. N Engl J Med 2012;366:1310–8. [207] Roth AJ, Kornblith AB, Batel-Copel L, Peabody E, Scher HI, Holland JC. Rapid screening for psychologic distress in men with prostate carcinoma. Cancer 1998;82:1904–8. [208] Nelson CJ, Weinberger MI, Balk E, Holland J, Breitbart W, Roth AJ. The chronology of distress, anxiety, and depression in older prostate cancer patients. Oncologist 2009;14:891–9. [209] Prasad SM, Eggener SE, Lipsitz SR, Irwin MR, Ganz PA, Hu JC. Effect of depression on diagnosis, treatment, and mortality of men with clinically localized prostate cancer. J Clin Oncol 2014;32:2471–8. [210] Herr HW, O’Sullivan ME. Quality of life of asymptomatic men with nonmetastatic prostate cancer on androgen deprivation therapy. J Urol 2000;163:1743–6. [211] Timilshina N, Breunis H, Alibhai S. Impact of androgen deprivation therapy on depressive symptoms in men with nonmetastatic prostate cancer. Cancer 2012;118:1940–5. [213] Li M, Fitzgerald P, Rodin G. Evidence-based treatment of depression in patients with cancer. J Clin Oncol 2012;30:1187–96. [214] Dantzer R, O’Connor JC, Freund GG, Johnson RW, Kelley KW. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci 2008;9:46–56. [215] Capuron L, Dantzer R. Cytokines and depression: the need for a new paradigm. Brain Behav Immun 2003;17:119–24. [216] Kiecolt-Glaser JK, Glaser R. Depression and immune function: central pathways to morbidity and mortality. J Psychosom Res 2002;53:873–6. [217] Wedding U, Koch A, Röhrig B, Pientka L, Sauer H, Höffken K, et al. Depression and functional impairment independently contribute to decreased quality of life in cancer patients prior to chemotherapy. Acta Oncol 2008;47:56–62. [218] Felger JC, Lotrich FE. Inflammatory cytokines in depression: neurobiological mechanisms and therapeutic implications. Neuroscience 2013;246:199–229. [219] Illman J, Corringham R, Robinson Jr D, Davis HM, Rossi JF, Cella D, et al. Are inflammatory cytokines the common link between cancer-associated cachexia and depression? J Support Oncol 2005;3:37–50. 22 J.L. Sotelo, C.B. Nemeroff / Personalized medicine in psychiatry 1–2 (2017) 11–25 [220] Rich T, Innominato PF, Boerner J, Mormont MC, Iacobelli S, Baron B, et al. Elevated serum cytokines correlated with altered behavior, serum cortisol rhythm, and dampened 24-hour rest-activity patterns in patients with metastatic colorectal cancer. Clin Cancer Res 2005;11:1757–64. [221] Seruga B, Zhang H, Bernstein LJ, Tannock IF. Cytokines and their relationship to the symptoms and outcome of cancer. Nat Rev Cancer 2008;8:887–99. [222] Späth-Schwalbe E, Hansen K, Schmidt F, Schrezenmeier H, Marshall L, Burger K, et al. Acute effects of recombinant human interleukin-6 on endocrine and central nervous sleep functions in healthy men 1. J Clin Endocrinol Metab 1998;83:1573–9. [223] Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature 2008;454:436–44. [224] Cole SW. Chronic inflammation and breast cancer recurrence. J Clin Oncol 2009;27:3418–9. [227] Monk JP, Phillips G, Waite R, Kuhn J, Schaaf LJ, Otterson GA, et al. Assessment of tumor necrosis factor alpha blockade as an intervention to improve tolerability of dose-intensive chemotherapy in cancer patients. J Clin Oncol 2006;24:1852–9. [228] Nilsson MB, Langley RR, Fidler IJ. Interleukin-6, secreted by human ovarian carcinoma cells, is a potent proangiogenic cytokine. Cancer Res 2005;65:10794–800. [229] Offner FA, Obris P, Stadlmann S, Feichtinger H, Klingler P, Herold M, et al. IL-6 secretion by human peritoneal mesothelial and ovarian cancer cells. Cytokine 1995;7:542–7. [230] Obata NH, Tamakoshi K, Shibata K, Kikkawa F, Tomoda Y. Effects of interleukin-6 on in vitro cell attachment, migration and invasion of human ovarian carcinoma. Anticancer Res 1996;17:337–42. [231] Watson JM, Sensintaffar JL, Berek JS, Martínez-Maza O. Constitutive production of interleukin 6 by ovarian cancer cell lines and by primary ovarian tumor cultures. Cancer Res 1990;50:6959–65. [232] Jeannin P, Duluc D, Delneste Y. IL-6 and leukemia-inhibitory factor are involved in the generation of tumor-associated macrophage: regulation by IFN-c. Immunotherapy 2011;3:23–6. [233] Lane D, Matte I, Rancourt C, Piché A. Prognostic significance of IL-6 and IL-8 ascites levels in ovarian cancer patients. BMC Cancer 2011;11:210. [234] Plante M, Rubin SC, Wong GY, Federici MG, Finstad CL, Gastl GA. Interleukin-6 level in serum and ascites as a prognostic factor in patients with epithelial ovarian cancer. Cancer 1994;73:1882–8. [235] Scambia G, Testa U, Panici PB, Foti E, Martucci R, Gadducci A, et al. Prognostic significance of interleukin 6 serum levels in patients with ovarian cancer. Br J Cancer 1995;71:354. [238] Lutgendorf SK, Weinrib AZ, Penedo F, Russell D, DeGeest K, Costanzo ES, et al. Interleukin-6, cortisol, and depressive symptoms in ovarian cancer patients. J Clin Oncol 2008;26:4820–7. [239] Courtier N, Gambling T, Enright S, Barrett-Lee P, Abraham J, Mason MD. Psychological and immunological characteristics of fatigued women undergoing radiotherapy for early-stage breast cancer. Support Care Cancer 2013;21:173–81. [240] Bower JE, Ganz PA, Tao ML, Hu W, Belin TR, Sepah S, et al. Inflammatory biomarkers and fatigue during radiation therapy for breast and prostate cancer. Clin Cancer Res 2009;15:5534–40. [241] Wratten C, Kilmurray J, Nash S, Seldon M, Hamilton CS, O’Brien PC, et al. Fatigue during breast radiotherapy and its relationship to biological factors. Int J Radiat Oncol Biol Physi 2004;59:160–7. [242] DiDonato JA, Mercurio F, Karin M. NF-jB and the link between inflammation and cancer. Immunol Rev 2012;246:379–400. [243] Braunstein S, Formenti SC, Schneider RJ. Acquisition of stable inducible upregulation of nuclear factor-jB by tumor necrosis factor exposure confers increased radiation resistance without increased transformation in breast cancer cells. Mol Cancer Res 2008;6:78–88. [244] Bower JE, Ganz PA, Irwin MR, Arevalo JM, Cole SW. Fatigue and gene expression in human leukocytes: increased NF-jB and decreased glucocorticoid signaling in breast cancer survivors with persistent fatigue. Brain Behav Immun 2011;25:147–50. [245] Hernández-Vargas H, Rodríguez-Pinilla SM, Julián-Tendero M, SánchezRovira P, Cuevas C, Anton A, et al. Gene expression profiling of breast cancer cells in response to gemcitabine: NF-jB pathway activation as a potential mechanism of resistance. Breast Cancer Res Treat 2007;102:157–72. [246] Torres MA, Pace TW, Liu T, Felger JC, Mister D, Doho GH, et al. Predictors of depression in breast cancer patients treated with radiation: role of prior chemotherapy and nuclear factor kappa B. Cancer 2013;119:1951–9. [247] Bower JE, Ganz PA, Aziz N, Fahey JL. Fatigue and proinflammatory cytokine activity in breast cancer survivors. Psychosom Med 2002;64:604–11. [248] Greenberg DB, Gray JL, Mannix CM, Eisenthal S, Carey M. Treatment-related fatigue and serum interleukin-1 levels in patients during external beam irradiation for prostate cancer. J Pain Symptom Manage 1993;8:196–200. [249] Abercrombie HC, Giese-Davis J, Sephton S, Epel ES, Turner-Cobb JM, Spiegel D. Flattened cortisol rhythms in metastatic breast cancer patients. Psychoneuroendocrinology 2004;2004(29):1082–92. [250] Jehn CF, Kühnhardt D, Bartholomae A, Pfeiffer S, Schmid P, Flath B. Association of IL-6, hypothalamus–pituitary–adrenal axis function, and depression in patients with cancer. Integr Cancer Ther 2010;2010(9):270–5. [251] Mormont MC, Levi F. Circadian-system alterations during cancer processes: a review. Int J Cancer 1997;70:241–7. [252] Palesh O, Zeitzer JM, Conrad A, Giese-Davis J, Mustian KM, Popek V, et al. Vagal regulation, cortisol, and sleep disruption in women with metastatic breast cancer. J Clin Sleep Med JCSM 2008;4:441. [253] Weinrib AZ, Sephton SE, DeGeest K, Penedo F, Bender D, Zimmerman B, et al. Diurnal cortisol dysregulation, functional disability, and depression in women with ovarian cancer. Cancer 2010;116:4410–9. [254] Sephton SE, Sapolsky RM, Kraemer HC, Spiegel D. Diurnal cortisol rhythm as a predictor of breast cancer survival. J Natl Cancer Inst 2000;92:994–1000. [255] Rae MT, Hillier SG. Steroid signalling in the ovarian surface epithelium. Trends Endocrinol Metab 2005;16:327–33. [256] Melhem A, Yamada SD, Fleming GF, Delgado B, Brickley DR, Wu W, et al. Administration of glucocorticoids to ovarian cancer patients is associated with expression of the anti-apoptotic genes SGK1 and MKP1/DUSP1 in ovarian tissues. Clin Cancer Res 2009;15:3196–204. [257] Pan D, Kocherginsky M, Conzen SD. Activation of the glucocorticoid receptor is associated with poor prognosis in estrogen receptor-negative breast cancer. Cancer Res 2011;71:6360–70. [258] Schlossmacher G, Stevens A, White A. Glucocorticoid receptor-mediated apoptosis: mechanisms of resistance in cancer cells. J Endocrinol 2011;211:17–25. [259] Pang D, Kocherginsky M, Krausz T, Kim SY, Conzen S. Dexamethasone decreases xenograft response to Paclitaxel through inhibition of tumor cell apoptosis. Cancer Biol Ther 2006;5:933–40. [260] Filipski E, Lévi F. Circadian disruption in experimental cancer processes. Integr Cancer Ther 2009;8:298–302. [261] Touitou Y, Bogdan A, Levi F, Benavides M, Auzeby A. Disruption of the circadian patterns of serum cortisol in breast and ovarian cancer patients: relationships with tumour marker antigens. Br J Cancer 1996;74:1248. [262] Bower JE, Ganz PA, Dickerson SS, Petersen L, Aziz N, Fahey JL. Diurnal cortisol rhythm and fatigue in breast cancer survivors. Psychoneuroendocrinology 2005;30:92–100. [263] Su S, Zhao J, Bremner JD, Miller AH, Tang W, Bouzyk M, et al. Serotonin transporter gene, depressive symptoms, and interleukin-6. Circ Cardiovasc Genet 2009;2:614–20. [264] Savas S, Hyde A, Stuckless SN, Parfrey P, Younghusband HB, Green R. Serotonin transporter gene (SLC6A4) variations are associated with poor survival in colorectal cancer patients. PLOS One 2012;7:e38953. [265] Goldsmith RE, Jandorf L, Valdimarsdottir H, Amend KL, Stoudt BG, Rini C, et al. Traumatic stress symptoms and breast cancer: the role of childhood abuse. Child Abuse Negl 2010;34(6):465–70. [266] Danese A, McEwen BS. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol Behav 2012;106(1):29–39. [267] Heim C, Shugart M, Craighead WE, Nemeroff CB. Neurobiological and psychiatric consequences of child abuse and neglect. Dev Psychobiol 2010;52(7):671–90. [268] Liu L, Mills PJ, Rissling M, Fiorentino L, Natarajan L, Dimsdale JE, et al. Fatigue and sleep quality are associated with changes in inflammatory markers in breast cancer patients undergoing chemotherapy. Brain Behav Immun 2012;26(5):706–13. [270] Janusek LW, Tell D, Albuquerque K, Mathews HL. Childhood adversity increases vulnerability for behavioral symptoms and immune dysregulation in women with breast cancer. Brain Behav Immun 2013;30:S149–62. [271] Fagundes CP, Lindgren ME, Shapiro CL, Kiecolt-Glaser JK. Child maltreatment and breast cancer survivors: social support makes a difference for quality of life, fatigue and cancer stress. Eur J Cancer 2012;48(5):728–36. [272] Bower JE, Crosswell AD, Slavich GM. Childhood adversity and cumulative life stress risk factors for cancer-related fatigue. Clin Psychol Sci 2014;2 (1):108–15. [273] Han TJ, Felger JC, Lee A, Mister D, Miller AH, Torres MA. Association of childhood trauma with fatigue, depression, stress, and inflammation in breast cancer patients undergoing radiotherapy. Psycho-Oncology 2015. [275] Tsunoda A, Nakao K, Hiratsuka K, Yasuda N, Shibusawa M, Kusano M. Anxiety, depression and quality of life in colorectal cancer patients. Int J Clin Oncol 2005;10(6):411–7. [276] Medeiros M, Oshima CTF, Forones NM. Depression and anxiety in colorectal cancer patients. J Gastrointestinal Cancer 2010;41(3):179–84. [277] Szkaradkiewicz A, Marciniak R, Chudzicka-Strugała I, Wasilewska A, Drews M, Majewski P, et al. Proinflammatory cytokines and IL-10 in inflammatory bowel disease and colorectal cancer patients. Archivum immunologiae et therapiae experimentalis 2009;57(4):291–4. [278] Allen-Mersh TG, Glover C, Fordy C, Henderson DC, Davies M. Relation between depression and circulating immune products in patients with advanced colorectal cancer. J R Soc Med 1998;91(8):408–13. [279] Jakeways MSR, Mitchell V, Hashim IA, Chadwick SJD, Shenkin A, Green CJ, et al. Metabolic and inflammatory responses after open or laparoscopic cholecystectomy. Br J Surg 1994;81(1):127–31. [280] Kristiansson M, Saraste L, Soop M, Sundqvist KG, Thörne A. Diminished interleukin-6 and C-reactive protein responses to laparoscopic versus open cholecystectomy. Acta Anaesthesiol Scand 1999;43(2):146–52. [281] Kudoh A, Katagai H, Takazawa T. Plasma inflammatory cytokine response to surgical trauma in chronic depressed patients. Cytokine 2001;13 (2):104–8. [282] Padova F, Pozzi C, Tondre MJ, Tritapepe R. Selective and early increase of IL-1 inhibitors, IL-6 and cortisol after elective surgery. Clin Exp Immunol 1991;85 (1):137–42. J.L. Sotelo, C.B. Nemeroff / Personalized medicine in psychiatry 1–2 (2017) 11–25 [283] Fallowfield LJ. Psychosocial adjustment after treatment for early breast cancer. Oncology (Williston Park NY) 1990;4(4):89–97. [284] Kruimel JW, Pesman GJ, Sweep CGJ, Van der Vliet JA, Liem T, Jansen JBMJ, et al. Depression of plasma levels of cytokines and ex-vivo cytokine production in relation to the activity of the pituitary–adrenal axis, in patients undergoing major vascular surgery. Cytokine 1999;11(5):382–8. [285] Schrepf A, Clevenger L, Christensen D, DeGeest K, Bender D, Ahmed A, et al. Cortisol and inflammatory processes in ovarian cancer patients following primary treatment: Relationships with depression, fatigue, and disability. Brain Behav Immun 2013;30:S126–34. [286] Mills PJ, Ancoli-Israel S, Parker B, Natarajan L, Hong S, Jain S, et al. Predictors of inflammation in response to anthracycline-based chemotherapy for breast cancer. Brain Behav Immun 2008;22(1):98–104. [287] Mills PJ, Dimsdale JE. Sleep apnea: a model for studying cytokines, sleep, and sleep disruption. Brain Behav Immun 2004;18(4):298–303. [288] Wang XS, Shi Q, Williams LA, Mao L, Cleeland CS, Komaki RR, et al. Inflammatory cytokines are associated with the development of symptom burden in patients with NSCLC undergoing concurrent chemoradiation therapy. Brain Behav Immun 2010;24(6):968–74. [289] Stone PC, Minton O. Cancer-related fatigue. Eur J Cancer 2008;44 (8):1097–104. [290] Geinitz H, Zimmermann FB, Stoll P, Thamm R, Kaffenberger W, Ansorg K, et al. Fatigue, serum cytokine levels, and blood cell counts during radiotherapy of patients with breast cancer. Int J Radiat Oncol Biol Phys 2001;51(3):691–8. [292] Ayerbe Luis et al. Natural history, predictors and outcomes of depression after stroke: systematic review and meta-analysis. Br J Psychiatry 2013;202 (1):14–21. [293] Nabi Hermann et al. Trajectories of depressive episodes and hypertension over 24 years the whitehall ii prospective cohort study. Hypertension 2011;57(4):710–6. [294] Kop, Willem J, et al. Autonomic nervous system dysfunction and inflammation contribute to the increased cardiovascular mortality risk associated with depression. Psychosom Med 2010;72(7):626. [295] Empana JP et al. Contributions of depressive mood and circulating inflammatory markers to coronary heart disease in healthy European men the prospective epidemiological study of myocardial infarction (PRIME). Circulation 2005;111(18):2299–305. [296] Arbelaez Jose J et al. Depressive symptoms, inflammation, and ischemic stroke in older adults: a prospective analysis in the cardiovascular health study. J Am Geriatr Soc 2007;55(11):1825–30. [297] Glymour MM et al. Depressive symptoms predict incident stroke independently of memory impairments. Neurology 2010;75(23):2063–70. [298] Pan A, Sun Q, Okereke OI, Rexrode KM, Hu FB. Depression and risk of stroke morbidity and mortality: a meta-analysis and systematic review. JAMA 2011;306(11):1241–9. [299] Pan A, Okereke OI, Sun Q, Logroscino G, Manson JE, Willett WC, et al. Depression and incident stroke in women. Stroke 2011;42(10):2770–5. [300] Dong JY, Zhzng YH, Tong J, Qin LQ. Depression and risk of stroke: a metaanalysis of prospective studies. Stroke 2012;43(1):32–7. [301] Li CT, Bai YM, Tu PC, Lee YC, Huang YL, Chen TJ, et al. Major depressive disorder and stroke risks: a 9-year follow-up population-based, matched cohort study. PLOS One 2012;7(10):e46818. [302] Seifert Christian L et al. Depressive symptoms and the risk of ischemic stroke in the elderly-influence of age and sex. PLOS One 2012:e50803. [303] Tolppanen Anna-Maija et al. Incidence of stroke in people with Alzheimer disease A national register-based approach. Neurology 2013;80(4):353–8. [304] Chi Nai-Fang et al. Alzheimer disease and risk of stroke A population-based cohort study. Neurology 2013;80(8):705–11. [305] Imfeld Patrick et al. Risk of incident stroke in patients with Alzheimer disease or vascular dementia. Neurology 2013:10–1212. [306] Jackson Caroline A, Mishra Gita D. Depression and risk of stroke in midaged women: a prospective longitudinal study. Stroke 2013;44(6):1555–60. [307] Joynt Karen E, Whellan David J, O’Connor Christopher M. Depression and cardiovascular disease: mechanisms of interaction. Biol. Psychiatry 2003;54 (3):248–61. [308] Neu Peter et al. Cerebrovascular reactivity in major depression: a pilot study. Psychosom Med 2004;66(1):6–8. [309] Elkind Mitchell SV. Why now? Moving from stroke risk factors to stroke triggers. Curr Opin Neurol 2007;20(1):51–7. [310] Falagas ME et al. Psychosocial factors and susceptibility to or outcome of acute respiratory tract infections. Int J Tuberc Lung Dis 2010;14(2):141–8. [311] Sher Yelizaveta, Lolak Sermsak, Maldonado José R. The impact of depression in heart disease. Curr Psychiatry Rep 2010;12(3):255–64. [312] Gilsanz Paola et al. Changes in depressive symptoms and incidence of first stroke among middle-aged and older US adults. J Am Heart Assoc 2015;4(5): e001923. [314] Davydow DS, Levine DA, Zivin K, Katon WJ, Langa KM. The association of depression, cognitive impairment without dementia, and dementia with risk of ischemic stroke: a cohort study. Psychosom Med 2015;77(2):200–8. [315] Tsadok Meytal Avgil et al. Sex differences in stroke risk among older patients with recently diagnosed atrial fibrillation. Jama 2012;307(18):1952–8. [316] Rosenberg Paul B et al. The association of neuropsychiatric symptoms in MCI with incident dementia and Alzheimer disease. Am J Geriatr Psychiatry 2013;21(7):685–95. 23 [317] Okura Toru et al. Neuropsychiatric symptoms and the risk of institutionalization and death: the aging, demographics, and memory study. J Am Geriatr Soc 2011;59(3):473–81. [318] Song Fei et al. Plasma protein profiling of Mild Cognitive Impairment and Alzheimer’s disease using iTRAQ quantitative proteomics. Proteome Sci 2014;12(5). [319] Fitzgerald Desmond J. Vascular biology of thrombosis: the role of platelet– vessel wall adhesion. Neurology 2001;57(suppl 2):S1–4. [323] Katon Wayne J et al. The pathways study: a randomized trial of collaborative care in patients with diabetes and depression. Arch Gen Psychiatry 2004;61 (10):1042–9. [324] Zivin Kara et al. Trends in depressive symptom burden among older adults in the United States from 1998 to 2008. J Gen Intern Med 2013;28(12):1611–9. [326] Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes a meta-analysis. Diabetes Care 2001;24(6):1069–78. [327] Pouwer F, Geelhoed-Duijvestijn PHLM, Tack CJ, Bazelmans E, Beekman AJ, Heine RJ, et al. Prevalence of comorbid depression is high in out-patients with Type 1 or Type 2 diabetes mellitus. Results from three out-patient clinics in the Netherlands. Diabet Med 2010;27(2):217–24. [328] Mommersteeg PMC, Herr R, Pouwer F, Holt RIG, Loerbroks A. The association between diabetes and an episode of depressive symptoms in the 2002 World Health Survey: an analysis of 231,797 individuals from 47 countries. Diabet Med 2013;30(6):e208–14. [330] Rotella Francesco, Mannucci Edoardo. Depression as a risk factor for diabetes: a meta-analysis of longitudinal studies. J Clin Psychiatry 2013;74(1):31–7. [332] Katon WJ, Rutter C, Simon G, Lin EH, Ludman E, Ciechanowski P, et al. The association of comorbid depression with mortality in patients with type 2 diabetes. Diabetes Care 2005;28(11):2668–72. [333] Okamura F, Tashiro A, Utumi A, Imai T, Suchi T, Tamura D, et al. Insulin resistance in patients with depression and its changes during the clinical course of depression: minimal model analysis. Metabolism 2000;49 (10):1255–60. [334] Champaneri S, Wand GS, Malhotra SS, Casagrande SS, Golden SH. Biological basis of depression in adults with diabetes. Curr Diabetes Rep 2010;10 (6):396–405. [335] Talbot Frances, Nouwen Arie. A review of the relationship between depression and diabetes in adults: is there a link? Diabetes Care 2000;23 (10):1556–62. [336] Carnethon, Mercedes R, et al. Symptoms of depression as a risk factor for incident diabetes: findings from the National Health and Nutrition Examination Epidemiologic Follow-up Study, 1971–1992. Am J Epidemiol 2003;158(5):416–23. [337] Lin Elizabeth HB. Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care 2004;27 (9):2154–60. [338] Yu M, Zhang X, Lu F, Fang L. Depression and risk for diabetes: a meta-analysis. Can J Diabetes 2015. [339] Cosgrove Martin P, Sargeant Lincoln A, Griffin Simon J. Does depression increase the risk of developing type 2 diabetes? Occup Med 2008;58(1):7–14. [340] Mezuk, Briana, et al. Depression and type 2 diabetes over the lifespan a metaanalysis. Diabetes Care 2008;31(12):2383–90. [341] Knol MJ et al. Depression as a risk factor for the onset of type 2 diabetes mellitus. A meta-analysis. Diabetologia 2006;49(5):837–45. [342] Duncan, Bruce B, et al. Low-grade systemic inflammation and the development of type 2 diabetes the atherosclerosis risk in communities study. Diabetes 2003;52(7):1799–805. [343] Björntorp P. Abdominal obesity and the development of noninsulindependent diabetes mellitus. Diabetes/Metab Rev 1988;4(6):615–22. [344] Björntorp P. Visceral fat accumulation: the missing link between psychosocial factors and cardiovascular disease? J Intern Med 1991;230 (3):195–201. [346] Karege Félicien et al. Low brain-derived neurotrophic factor (BDNF) levels in serum of depressed patients probably results from lowered platelet BDNF release unrelated to platelet reactivity. Biol Psychiatry 2005;57(9):1068–72. [347] Gervasoni Nicola et al. Partial normalization of serum brain-derived neurotrophic factor in remitted patients after a major depressive episode. Neuropsychobiology 2005;51(4):234–8. [348] Rao Allam Appa et al. Bioinformatics analysis of functional protein sequences reveals a role for brain-derived neurotrophic factor in obesity and type 2 diabetes mellitus. Med Hypotheses 2008;70(2):424–9. [349] Fujinami A, Ohta K, Obayashi H, Fukui M, Hasegawa G, Nakamura N, Ohta M. Serum brain-derived neurotrophic factor in patients with type 2 diabetes mellitus: relationship to glucose metabolism and biomarkers of insulin resistance. Clin Biochem 2008;41(10):812–7. [350] Engum Anne. The role of depression and anxiety in onset of diabetes in a large population-based study. J Psychosom Res 2007;62(1):31–8. [351] Schweiger U et al. Low lumbar bone mineral density in patients with major depression. Am J Psychiatry 1994;151:1691–3. [352] Cizza G. Major depressive disorder is a risk factor for low bone mass, central obesity, and other medical conditions. Dialogues Clin Neurosci 2011;13:73–87. [353] Whooley MA, Simon GE. Primary care: managing depression in medical outpatients. NEJM 2000;343:1942–50. [354] Mussolino ME. Depression and hip fracture risk: the NHANES I epidemiologic follow-up study. Public Health Rep 2005;120:71–5. 24 J.L. Sotelo, C.B. Nemeroff / Personalized medicine in psychiatry 1–2 (2017) 11–25 [355] Jacka FN et al. Depression and bone mineral density in a community sample of perimenopausal women: Geelong Osteoporosis Study. Menopause 2005;12:88–91. [356] Eskandari F et al. Low bone mass in premenopausal women with depression. Arch Intern Med 2007;167:2329–36. [357] Wu Q et al. Depresion and low bone mineral density: a meta-analysis of epidemiologic studies. Osteoporos Int 2009;20:1309–20. [358] Weller EB et al. Impact of depression and its treatment on the bones of growing children. Curr Psychiatry Rep 2007;9:94–8. [360] Yazici KM et al. Bone mineral density in premenopausal women with major depressive disorder. Psychiatry Res 2003;117:271–5. [361] Robbins J et al. The association of bone mineral density and depression in an older population. J Am Geriatr Soc 2001;49:732–6. [362] Michelson D et al. Bone mineral density in women with depression. NEJM 1996;335:1176–81. [363] Cizza et al. Depression: a major unrecognized risk factor for osteoporosis? Trends Endocrine Metab 2001;12:198–203. [364] Halbreich U et al. Decreased bone mineral density in medicated psychiatric patients. Psychosom Med 1995;57:485–91. [365] Dorn LD et al. Association of depressive symptoms and anxiety with bone mass and density in ever-smoking and never-smoking adolescent girls. Arch Pediatric Adoles Med 2008;162:1181–8. [366] Atteritano M et al. Bone mineral density, quantitative ultrasound parameters and bone metabolism in postmenopausal women with depression. Intern Emerge Med 2011. XXXX. [367] Erez HB et al. The relationship of depression, anxiety and stress with low bone mineral density in postmenopausal women. Arch Osteoporos 2012;7:247–55. [368] Esel E et al. Effects of antidepressant treatment and of gender on serum leptin in patients with major depression. Prog Neuropsychopharmacol Biol Psychiatry 2005;29:565–70. [369] Mussolino ME et al. Depression and bone mineral density in young adults: results from NHANES III. Psychosom Med 2004;66:533–7. [370] Whooley MA et al. Depressive symptoms and bone mineral density in older men. J Geriatr Psychiatry Neurol 2004;17:88–92. [371] Wong SY et al. Depression and bone mineral density: is there a relationship in elderly Asian men? Results from Mr. Os (Hong Kong). Osteoporos Int 2005;16:610–5. [372] Danielson, Michelle E, et al. Familial resemblance of bone mineral density (BMD) and calcaneal ultrasound attenuation: the BMD in mothers and daughters study. J Bone Miner Res 1999;14(1):102–10. [373] Silverman SL et al. Prevalence of depressive symptoms in postmenopausal women with low bone mineral density and/or prevalent vertebral fracture: results from the Multiple Outcomes of Raloxifene Evaluation (MORE) study. J Rheumatol 2007;34:140–4. [374] Diem SJ et al. Depressive symptoms and rates of bone loss at the hip in older women. J Am Geriatr Soc 2007;55:824–31. [375] Diem SJ et al. Depression symptoms and rates of bone loss at the hip in older men. Osteoporos Int 2013;24:111–9. [376] Cizza G et al. Depression and osteoporosis: a research synthesis with metaanalysis. Hormone Metabol Res 2010;42:467–82. [377] Yirmiya R, Bab I. Major depression is a risk factor for low bone mineral density: a meta-analysis. Biol Psychiatry 2009;66:423–32. [378] Williams LJ et al. Depression and bone metabolism: a review. Psychother Psychosom 2009;78:16–25. [379] Lapi F, Simonetti M, Michieli R, Pasqua A, Brandi ML, Frediani B, et al. Assessing 5-year incidence rates and determinants of osteoporotic fractures in primary care. Bone 2012;50(1):85–90. [381] Kamholz B et al. Depression after hip fracture. J Am Geriatr Soc 2007;55:126–7. [382] Eggermont, Laura HP, et al. Depressive symptoms, chronic pain, and falls in older community-dwelling adults: the MOBILIZE Boston Study. J Am Geriatr Soc 2012;60(2):230–7. [383] Iaboni A, Flint AJ. The complex interplay of depression and falls in older adults: a clinical review. Am J Geriatr Psychiatry 2013;21:484–92. [385] Tolea MI et al. Depressive symptoms as a risk factor for osteoporosis and fractures in older Mexican-American women. Osteoporos Int 2007;18:315–22. [386] Forsen L et al. Mental distress and risk of hip fracture. Do broken hearts lead to broken bones? J Epidemiol Community Health 1999;53:343–7. [387] Whooley MA et al. Depression, falls, and risk of fracture in older women. Study of Osteoporotic Fractures Research Group. Arch Intern Med 1999;159:484–90. [388] Sogaard AJ et al. Long-term mental distress, bone mineral density and nonvertebral fractures. The Tromso Study. Osteoporos Int 2005;16:887–97. [391] Amsterdam JD, Hooper MB. Bone density measurement in major depression. Prog Neuropsychopharmacol Biol Psychiatry 1998;22:267–77. [392] Warden SJ, Robling AG, Haney EM, Turner CH, Bliziotes MM. The emerging role of serotonin (5-hydroxytryptamine) in the skeleton and its mediation of the skeletal effects of low-density lipoprotein receptor-related protein 5 (LRP5). Bone 2010;46(1):4–12. [393] Kahl KG et al. Bone mineral density, bone turnover, and osteoprotegerin in depressed women with and without borderline personality disorder. Psychosom Med 2006;68:669–74. [394] Altindag O et al. Relation of cortisol levels and bone mineral density among premenopausal women with major depression. Int J Clin Pract 2007;61:416–20. [395] Kavuncu Vural et al. Bone metabolism and bone mineral density in premenopausal women with mild depression. Yonsei Med J 2002;43 (1):101–8. [396] Petronijević Milan et al. Low bone mineral density and high bone metabolism turnover in premenopausal women with unipolar depression. Bone 2008;42 (3):582–90. [397] Yazici Aylin Ertekin et al. Bone mineral density in premenopausal women with major depression. Joint Bone Spine 2005;72(6):540–3. [398] Furlan PM et al. The role of stress-induced cortisol in the relationship between depression and decreased bone mineral density. Biol Psychiatry 2005;57:911–7. [399] Ilias Ioannis et al. Depression and osteoporosis in men: association or casual link? HORMONES-ATHENS 2006;5(1):9. [400] Yirmiya R et al. Depression induces bone loss through stimulation of the sympathetic nervous system. Proc Natl Acad Sci USA 2006;103:16876–81. [401] Palfai TP, Cheng DM, Samet JH, Kraemer KL, Roberts MS, Saitz R. Depressive symptoms and subsequent alcohol use and problems: a prospective study of medical inpatients with unhealthy alcohol use. J Stud Alcohol Drugs 2007;68 (5):673–80. [402] Warden SJ, Hassett SM, Bond JL, Rydberg J, Grogg JD, Hilles EL, Turner CH. Psychotropic drugs have contrasting skeletal effects that are independent of their effects on physical activity levels. Bone 2010;46(4):985–92. [403] Ducy Patricia, Karsenty Gerard. The two faces of serotonin in bone biology. J Cell Biol 2010;191(1):7–13. [407] Karsenty G, Ferron M. The contribution of bone to whole-organism physiology. Nature 2012;481(7381):314–20. [410] Takeda S. Central control of bone remodeling. J Neuroendocrinol 2008;20:802–7. [411] Kahl KG. Bone mineral density, Markers of bone turnover, and cytokines in young women with borderline personality disorder with and without comorbid major depressive disorder. Am J Psychiatry 2005;162:168–74. [412] Kraus Thomas et al. Low leptin levels but Norma body mass indices in patients with depression or schizophrenia. Neuroendocrinology 2001;73 (4):243–7. [413] Antonijevic IA et al. Elevated nocturnal profiles of serum leptin in patients with depression. J Psychiatr Res 1998;32(6):403–10. [414] Yadav VK, Oury F, Suda N, Liu ZW, Gao XB, Confavreux C, et al. Leptin regulation of bone mass, appetite and energy expenditure relies on its ability to inhibit serotonin synthesis in the brainstem. Cell 2009;138(5):976. [415] Gimble JM. Leptin’s balancing act between bone and fat. J Bone Miner Res 2011;26(8):1694–7. [418] Black LJ, Jacoby P, Allen KL, Trapp GS, Hart PH, Byrne SM, et al. Low vitamin D levels are associated with symptoms of depression in young adult males. Aust N Z J Psychiatry 2014;48:464–71. [419] Lapid MI, Cha SS, Takahashi PY. Vitamin D and depression in geriatric primary care patients. Clin Interv Aging 2013;8:509–14. http://dx.doi.org/10.2147/ CIA.S42838. Epub 2013 May 3. [420] Anglin RE et al. Vitamin D deficiency and depression in adults: Systematic review and meta-analysis. Br J Psychiatry 2013;202:100–7. [421] Ganji V, Milone C, Cody MM, McCarty F, Wang YT. Serum vitamin D concentrations are related to depression in young adult US population: the Third National Health and Nutrition Examination Survey. Int Arch Med 2010;11(3):29. http://dx.doi.org/10.1186/1755-7682-3-29. [422] Lee DM, Tajar A, O’Neill TW, O’Connor DB, Bartfai G, Boonen S, et al. Pendleton N; EMAS study group. Lower vitamin D levels are associated with depression among community-dwelling European men. J Psychopharmacol 2011 Oct;25(10):1320–8. http://dx.doi.org/10.1177/0269881110379287. Epub 2010 Sep 7. [423] Berk M, Sanders KM, Pasco JA, Jacka FN, Williams LJ, Hayles AL, et al. Vitamin D deficiency may play a role in depression. Med Hypotheses 2007;69:1316–9. [424] Eyles DW et al. Distribution of the vitamin D receptor and 1 alphahydroxylase in human brain. J Chem Neuroanat 2005;29:21–30. [425] Pérez-López FR. Vitamin D and its implications for musculoskeletal health in women: an update. Maturitas 2007;58(2):117–37. [426] Jorde R, Sneve M, Figenschau Y, Svartberg J, Waterloo K. Effects of vitamin D supplementation on symptoms of depression in overweight and obese subjects: randomized double blind trial. J Intern Med 2008;264(6):599–609. [427] Zhao G, Ford ES, Li C, Balluz LS. No associations between serum concentrations of 25-hydroxyvitamin D and parathyroid hormone and depression among US adults. Br J Nutr 2010;104(11):1696–702. [428] Walker MD, Rubin M, Silverberg SJ. Nontraditional manifestations of primary hyperparathyroidism. J Clin Densitom 2013;16(1):40–7. [429] Dobolyi A, Dimitrov E, Palkovits M, Usdin TB. The neuroendocrine functions of the parathyroid hormone 2 receptor. Front Endocrinol 2012;3. [430] Herran A et al. Increased bone remodeling in first-episode major depressive disorder. Psychosom Med 2000;62:779–82. [431] Spangler L et al. Depressive symptoms, bone loss, and fractures in postmenopausal women. J Gen Intern Med 2008;23:567–74. [432] Hebert C, McKean M, Dantz B. Osteoporosis in depression: Which patients are at risk? Curr Psychiatry 2010;9(4):9. J.L. Sotelo, C.B. Nemeroff / Personalized medicine in psychiatry 1–2 (2017) 11–25 [433] Rizzoli R, Cooper C, Reginster JY, Abrahamsen B, Adachi JD, Brandi ML, et al. Antidepressant medications and osteoporosis. Bone 2012;51(3):606–13. [434] Diem SJ et al. Use of antidepressants and rates of bone loss in older women: The Study of Osteoporotic Fractures. Arch Intern Med 2007;167:1240–5. [435] Rabenda V et al. Relationship between use of antidepressants and risk of fractures: a meta-analysis. Osteoporos Int 2013;24:121–37. [436] Wu Q et al. Selective serotonin reuptake inhibitor treatment and risk of fractures: a meta-analysis of cohort and case-control studies. Osteoporos Int 2012;23:365–75. [437] Schwan S, Hallberg P. SSRIs, bone mineral density, and risk of fractures – a review. Eur Neuropsychopharmacol 2009;19:683–92. [438] Ziere Gijsbertus et al. Selective serotonin reuptake inhibiting antidepressants are associated with an increased risk of nonvertebral fractures. J Clini Psychopharmacol 2008;28(4):411–7. [439] Bliziotes MM et al. Neurotransmitter action in osteoblasts: expression of a functional system for serotonin receptor activation and reuptake. Bone 2001;29:477–86. [440] Pacher Pal et al. Serotonin reuptake inhibitors fluoxetine and citalopram relax intestinal smooth muscle. Can J Physiol Pharmacol 2001;79(7):580–4. [450] Aydin H, Mutlu N, Akbas NB. Treatment of a major depressive episode suppresses markers of bone turnover in premenopausal women. J Psychiatr Res 2011;45:1316–20. [451] Shea ML, Garfield LD, Teitelbaum S, Civitelli R, Mulsnat BH, Reynolds 3rd CF, et al. Serotonin-norepinephrine reuptake inhibitor therapy in late life [452] [453] [454] [455] [456] [472] 25 depression is associated with increased marker of bone resorption. Osteoporos Int 2013;24:1741–9. Garfield LD, Muller DJ, Kennedy JL, Mulsant BH, Reynolds 3rd CF, Teitelbaum SL, et al. Genetic variation in the serotonin transporter and HTR1B receptor predicts reduced bone formation during serotonin reuptake inhibitor treatment in adults. World J Biol Psychiatry 2014;15:404–10. Konstantynowicz J, Kadziela-Olech H, Kaczmarski M, Zebaze RM, IulianoBurns S, Piotrowska-Jastrzebska J, et al. Depression in anorexia nervosa: a risk factor for osteoporosis. J Clin Endocrinol Metab 2005;90(9):5382–5. Schweiger U, Weber B, Deuschle M, Heuser I. Lumbar bone mineral density in patients with major depression: evidence of increased bone loss at follow-up. Am J Psychiatry 2000;157:118–20. Niti M, Ng TP, Kua EH, Ho RC, Tan CH. Depression and chronic medical illnesses in Asian older adults: the role of subjective health and functional status. Int J Geriatr Psychiatry 2007;22(11):1087–94. Waugh EJ, Lam MA, Hawker GA, McGowan J, Papaioannou A, Cheung AM, et al. Risk factors for low bone mass in healthy 40–60 year old women: a systematic review of the literature. Osteoporos Int 2009;20(1):1–21. Köhler O, Benros ME, Nordentoft M, Farkouh ME, Iyengar RL, Mors O, et al. Effect of anti-inflammatory treatment on depression, depressive symptoms, and adverse effects: a systematic review and meta-analysis of randomized clinical trials. JAMA Psychiatry 2014;71(12):1381–91.