Adrenergic Pharmacology: Agonists, Receptors, and Mechanisms
advertisement

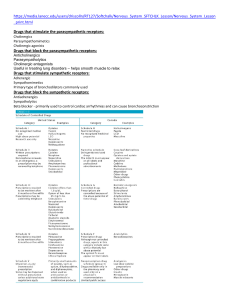
Adrenergic pharmacology Catecholamine Synthesis, Storage, and Release • Reuptake of catecholamine into the neuronal cytoplasm is mediated by a selective catecholamine transporter ( norepinephrine transporter, or NET) that is also known as Uptake 1. Approximately 90% of the released norepinephrine is taken up by this process (recycled); the remainder is either metabolized locally or diffuses into the blood. thus, limiting the postsynaptic response and allowing neurons to recycle the transmitter for subsequent release. • Catecholamine metabolism involves the two enzymes MAO and catechol-O-methyltransferase (COMT). Adrenergic receptors (adrenoceptors) • α receptors(α1, α2) epinephrine = norepinephrine >> isoproterenol • β-Adrenoceptors (β1, β2, and β3) • is isoproterenol > epinephrine > norepinephrine • β1 receptors have approximately equal affinities for epinephrine and norepinephrine, whereas β2 receptors have a higher affinity for epinephrine than for norepinephrine. Distribution of adrenergic receptors Adrenergic agonists can be classified according to mechanism of action into: • Direct-acting agonists • Indirect-acting agonists cocaine and amphetamine • Mixed-action agonists Ephedrine and pseudoephedrine DIRECT-ACTING ADRENERGIC AGONISTS Epinephrine Cardiovascular: • ↑ heart rate and ↑ contractility → cardiac output→ ↑ systolic blood pressure. This effect is mainly caused by Β1 activation in the heart • Epinephrine constricts arterioles in the skin, mucous membranes, and viscera (α effects), and it dilates vessels going to the liver and skeletal muscle (β2 effects). Consequently, total peripheral resistance(PVR) may actually fall, explaining the fall in diastolic pressure that is seen with epinephrine injection. Therefore, the cumulative effect is an increase in systolic blood pressure, coupled with a slight • decrease in diastolic pressure due to ß2 receptor–mediated vasodilation in the skeletal muscle vascular bed DIRECT-ACTING ADRENERGIC AGONISTS Epinephrine • Respiratory: Epinephrine causes powerful bronchodilation by acting directly on bronchial smooth muscle (ß2 action). It also inhibits the release of allergy mediators such as histamine from mast cells. • Hyperglycemia: Epinephrine has a significant hyperglycemic effect because of increased glycogenolysis in the liver (ß2 effect), increased release of glucagon (ß2 effect), and a decreased release of insulin (α2 effect). • Lipolysis: Epinephrine initiates lipolysis through agonist activity on the ß receptors of adipose tissue. • Epinephrine activates β1 receptors on the kidney to cause renin release. Renin is an enzyme involved in the production of angiotensin II, a potent vasoconstrictor. DIRECT-ACTING ADRENERGIC AGONISTS Epinephrine • Therapeutic uses: A. Anaphylactic shock: Epinephrine is the drug of choice for the treatment of type I hypersensitivity reactions (including anaphylaxis) in response to allergens. B. Cardiac arrest: Epinephrine may be used to restore cardiac rhythm in patients with cardiac arrest. C. Local anesthesia: Local anesthetic solutions may contain low concentrations (for example, 1:100,000 parts) of epinephrine. Epinephrine greatly increases the duration of local anesthesia by producing vasoconstriction at the site of injection. Epinephrine also reduces systemic absorption of the local anesthetic and promotes local hemostasis. • Adverse effects: DIRECT-ACTING ADRENERGIC AGONISTS Epinephrine • Epinephrine can produce adverse CNS effects that include anxiety, fear, tension, headache, and tremor. • It can trigger cardiac arrhythmias, particularly if the patient is receiving digoxin. • Epinephrine can also induce pulmonary edema due to increased afterload caused by vasoconstrictive properties of the drug. • Patients with hyperthyroidism may have an increased production of adrenergic receptors in the vasculature, leading to an enhanced response to epinephrine, and the dose must be reduced in these individuals. • Epinephrine increases the release of endogenous stores of glucose. In diabetic patients, dosages of insulin may have to be increased. • Nonselective ß-blockers prevent vasodilatory effects of epinephrine on ß2 receptors, leaving a receptor stimulation unopposed. This may lead to increased peripheral resistance and increased blood pressure. DIRECT-ACTING ADRENERGIC AGONISTS Epinephrine Question for you : can epinephrine be used in the treatment of asthma? • Norepinephrine DIRECT-ACTING ADRENERGIC AGONISTS Norepinephrine • is an agonist at both α1 and α2 receptors. Norepinephrine also activates ß1 receptors with similar potency as epinephrine, but has relatively little effect on ß2 receptors. Consequently, norepinephrine increases peripheral resistance and both diastolic and systolic blood pressure. • Compensatory baroreflex activation : • Norepinephrine increases blood pressure, and this stimulates the baroreceptors, inducing a rise in vagal activity. The increased vagal activity produces a reflex bradycardia, which is sufficient to counteract the local actions of norepinephrine on the heart, although the reflex compensation does not affect the positive inotropic effects of the drug DIRECT-ACTING ADRENERGIC AGONISTS Norepinephrine • Therapeutic uses: Norepinephrine is used to treat shock (for example, septic shock), because it increases vascular resistance and, therefore, increases blood pressure. It has no other clinically significant uses. • Pharmacokinetics: Norepinephrine is given IV for rapid onset of action. The duration of action is 1 to 2 minutes, following the end of the infusion. It is rapidly metabolized by MAO and COMT, and inactive metabolites are excreted in the urine. • Adverse effects: These are similar to epinephrine. In addition, norepinephrine is a potent vasoconstrictor and may cause blanching and sloughing of skin along an injected vein. • Question for you : can Norepinephrine be used in the treatment of asthma? DIRECT-ACTING ADRENERGIC AGONISTS Isoproterenol (isoprenaline) ) • Isoproterenol (isoprenaline) • It is a very potent ß-receptor agonist and has little effect on a receptors. The drug has positive chronotropic and inotropic actions; because isoproterenol activates ß receptors almost exclusively with insignificant effect on α receptors, it is a potent vasodilator. These actions lead to a marked increase in cardiac output associated with a fall in diastolic and mean arterial pressure and a slight increase in systolic pressure DIRECT-ACTING ADRENERGIC AGONISTS Dopamine • Dopamine • Dopamine is the immediate precursor of norepinephrine. Dopamine can activate a- and ß-adrenergic receptors. At higher doses, it causes vasoconstriction by activating α1 receptors, whereas at lower doses, it stimulates ß1 cardiac receptors. In addition, D1 and D2 dopaminergic receptors, different from the a- and ß-adrenergic receptors, occur in the peripheral mesenteric and renal vascular beds, where binding of dopamine produces vasodilation. • Therapeutic uses: • Dopamine can be used for cardiogenic and septic shock and is given by continuous infusion. It raises blood pressure by stimulating the ß1 receptors on the heart to increase cardiac output and α1 receptors on blood vessels to increase total peripheral resistance. • It enhances perfusion to the kidney and splanchnic areas, as described above. Increased blood flow to the kidney enhances the glomerular filtration rate and causes diuresis. By contrast, norepinephrine can diminish blood supply to the kidney and may reduce renal function. • Salbutamol, metaproterenol, and terbutaline DIRECT-ACTING ADRENERGIC AGONISTS • they are short-acting β2 agonists (SABAs) used primarily as bronchodilators and administered by a metered-dose inhaler . Salbutamol is the SABA of choice for the management of acute asthma symptoms. • terbutaline is used as a uterine relaxant to suppress premature labor, and use for this indication should not exceed 72 hours. • One of the most common side effects of these agents is tremor, but patients tend to develop tolerance to this effect. Other side effects include restlessness, apprehension, and anxiety. When these drugs are administered orally, they may cause tachycardia or arrhythmia (due to β1 receptor activation), especially in patients with underlying cardiac disease. • Salmeterol, formoterol, and indacaterol • They are long-acting ß2 selective agonists (LABAs) used for the management of respiratory disorders such as asthma and chronic obstructive pulmonary disease • INDIRECT-ACTING SYMPATHOMIMETICS INDIRECTACTING ADRENERGIC AGONISTS • Indirect-acting sympathomimetics can have one of two different mechanisms . First, they may enter the sympathetic nerve ending and displace stored catecholamine transmitter. Such drugs have been called amphetamine-like or “displacers.” Second, they may inhibit the reuptake of released transmitter by interfering with the action of the norepinephrine transporter, NET. • Amphetamine and amphetamine like • Amphetamine it displaces endogenous catecholamines from storage vesicles (similar to tyramine). It can enter the CNS, where it has marked stimulant effects on mood and alertness and a depressant effect on appetite. Amphetamine’s actions are mediated through the release of norepinephrine and, to some extent, dopamine. • Amphetamine can cause psychological and physiologic dependence as well as tolerance. Amphetamine may cause paranoia and hallucinations. Methamphetamine (“crystal meth”) is a major drug of abuse • Tyramine • Tyramine is a dietary amine that is ordinarily metabolized by MAO in the gastrointestinal tract and liver. In patients taking MAO inhibitors tyramine is absorbed in the gut, transported through the blood, and taken up by sympathetic neurons, where it is transported into synaptic vesicles by VMAT. Uptake of tyramine by the synaptic vesicles causes displacement o vesicular norepinephrine and nonvesicular release of norepinephrine from the nerve terminal via reversal of NET. • Catecholamine Reuptake Inhibitors • Tricyclic Antidepressant, Cocaine, by inhibiting NET MIXED-ACTING ADRENERGIC AGONISTS • Ephedrine and pseudoephedrine are mixedaction adrenergic agents. They not only enhance release of stored norepinephrine from nerve endings but also directly stimulate both a and ß receptors. Ephedrine and pseudoephedrine are not catecholamines and are poor substrates for COMT and MAO. Therefore, these drugs have a long duration of action. Oral pseudoephedrine is primarily used to treat nasal and sinus congestion