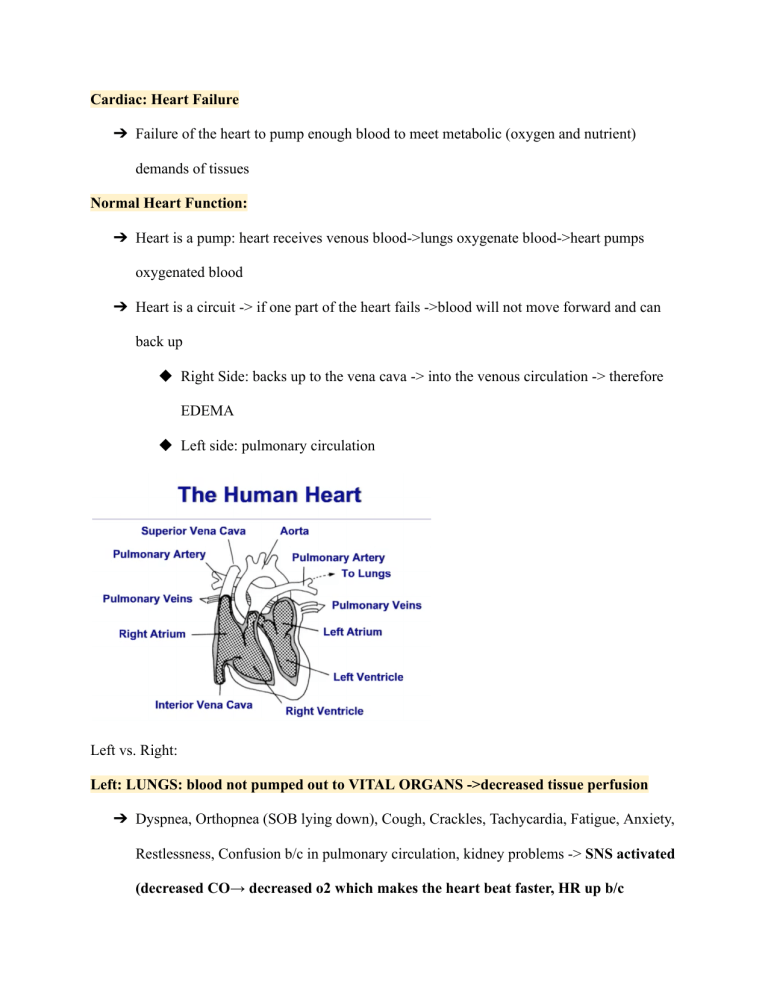
Cardiac: Heart Failure ➔ Failure of the heart to pump enough blood to meet metabolic (oxygen and nutrient) demands of tissues Normal Heart Function: ➔ Heart is a pump: heart receives venous blood->lungs oxygenate blood->heart pumps oxygenated blood ➔ Heart is a circuit -> if one part of the heart fails ->blood will not move forward and can back up ◆ Right Side: backs up to the vena cava -> into the venous circulation -> therefore EDEMA ◆ Left side: pulmonary circulation Left vs. Right: Left: LUNGS: blood not pumped out to VITAL ORGANS ->decreased tissue perfusion ➔ Dyspnea, Orthopnea (SOB lying down), Cough, Crackles, Tachycardia, Fatigue, Anxiety, Restlessness, Confusion b/c in pulmonary circulation, kidney problems -> SNS activated (decreased CO→ decreased o2 which makes the heart beat faster, HR up b/c peripheral blood vessels constrict → distole shortens, ventricles don’t fill well therefore decreased stroke volume then decreased CO AGAIN Right: extremities -> most common cause is left sided HF Blood backs up into the pulmonary system then into right ventricle → stretched b/c too much blood volume → w/ right HF blood is not pumped forward into the pulmonary circulation or into left heart -> goes into VENOUS CIRCULATION therefore congestion of vital organs esp liver (fluid moves from the blood into the interstitial space causing EDEMA) ➔ Jugular vein distention (JVD). ➔ Dependent edema, especially lower extremities and progressing up the body eventually up to the abdomen. ➔ Hepatomegaly. ➔ Right upper quadrant tenderness. ➔ Increasing hepatic dysfunction. ➔ Ascites, anorexia, nausea, weight gain, weakness, respiratory distress, abdominal pain. ➔ Altered liver function and liver function tests. ➔ Gastrointestinal distress. Treatment: ➔ Oxygen (O2). ➔ Digoxin. ➔ Diuretics. ➔ Vasodilators. ➔ Potassium supplements. ➔ Low-sodium diet. ➔ Bed rest ->elevate HOB. (Diuretics, which reduce preload by decreasing total blood volume and circulatory congestion. ACE inhibitors, which dilate blood vessels and decrease systemic vascular resistance, thus reducing the workload of the heart. Vasodilators may be given to the client who cannot tolerate ACE inhibitors. Digoxin, which may help strengthen myocardial contractility. Beta-adrenergic blockers, which may prevent cardiac remodeling (left ventricular dilation and hypertrophy). It is necessary to alternate periods of rest with periods of activity. A sodium-restricted diet is essential.) Physiology: ➔ The heart is a muscle, and its basic function is to pump blood. ➔ Heart failure results from a variety of cardiovascular diseases, but can also lead to some common heart abnormalities that result in decreased contraction (systole) and/or decreased filling (diastole). Pathophysiology: ➔ There are two types of heart failure: ◆ Diastolic heart failure: an alteration in ventricular filling, which occurs as the result of continued increased workload on the heart. ◆ Systolic heart failure: an alteration in ventricular contraction, which means that less blood is ejected from the ventricle. Who’s at RISK?? Decreased Cardiac Output: ➔ Increased blood volume: preload: the amount of blood left in the ventricle at the end of diastole so that amount of blood that does not get expelled: ◆ If amount of volume gets to the point where the myocardium is stretched and had ineffective pumping ->less blood will be ejected with each contraction (ex. preganacy , valvylar disease) ➔ Arterial pressure (has to pump at a higher pressure) -> afterload: the resistance against which the heart must pump -> hypertension and vasoactives cause vasoconstriction and increase resistance to the heart ->stretches and will fail ➔ Contractility : decrease in contractility in the heart: decreases effective pumping -> cardiomyopathy, post MI, CHD Diagnostic Tests: ➔ BNP → elevated blood levels of B-type natriuretic peptides: elevated with HF; the more severe the heart failure ➔ Chest x-ray: show fluid build up in alveoli ➔ MUGA scan: show decreased ejection fraction ◆ Measures amount of bloof ejectedw/ each contraction of the ventricle ➔ Echocardiogram: assess the contractility of the heart ➔ Kidney and Liver Function: BUN and creatinine may be elevated if renal perfusion is decreased (kidney fed off the aorta -> left sided HF will impact kidney function; righ sided HF impacted w/ fluid backed up into kidneys causing injury) ◆ Liver may demonstrate engorgment w/ right-side HF ➔ Cardiac Cath: placement of catheter into the heart openings → evaluate the function of the valves; measures the strength of the contraction, thickness of myocardium, presence of CAD ➔ Continuous EKG monitor is always applied: HR may increase in the beginning and decrease to compensate for the decreased CO then decrease with limited O2 Preload: If there is an excess of blood in the heart, the force of contraction is decreased. If blood volume or preload is decreased, the heart contracts more efficiently, there DIURETICS. ➔ Increases UO, decreases blood volume -> DECREASES PRELOAD ◆ Taken in morning → MONITOR POTASSIUM LEVELS Afterload: The heart does not have to work as hard if we decrease the resistance in the arteries, decreasing the pressure or resistance of afterload. ANGIOTENSIN decrease systemic vascular resistance in the ARTERIES (beta-blockers decrease afterload) ➔ Heart able to pump more efficiently against less resistance ➔ CAN INCREASE POTASSIUM LEVELS -> MONITOR WEIGHT GAIN (3-5lbs in a week → INDICATION TO HF-> contact PCP) Blood flow: from superior and inferior vena cava (brings back waste products) → right atrium -> right ventricle ->out pulmonary arteries ->lungs (waste product eliminated) -> out pulmonary veins ->brings blood back to heart and into left atrium -> left ventricle ->out to body via aorta