Pathology Exam 1 Review: Morphogenesis, Pediatric & GI Diseases
advertisement

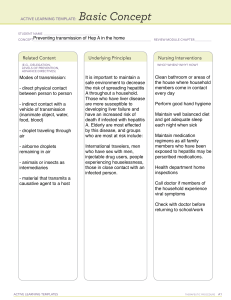
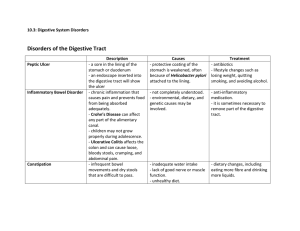
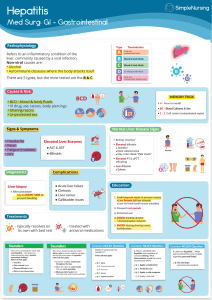
2023 DBCS 324 Review for Exam 1 Pathology M. Beth Miloro, DDS, MPH Assistant Clinical Professor University of Illinois at Chicago Department of OMDS Errors of Morphogenesis Malformations Disruptions Deformations Sequence Malformation syndrome Malformations • Intrinsically abnormal developmental process – Primary errors of morphogenesis – Cause: • Genetic • Environmental • Multifactorial Malformation Causes • Genetic diseases – Down syndrome – Turner/Klinefelter syndrome • Environmental factors – Viruses – rubella – Drugs – • Thalidomide - limb malformations • Alcohol – fetal alcohol syndrome • Smoking - low birth weight, SIDS • Multifactorial - environment + genetic – Cleft palate/lip, neural tube defects Microcephaly and Zika What we don’t know • Causal relation between Zika virus and microcephaly or other adverse pregnancy outcomes • Full spectrum of phenotypes in affected infants • Impact of timing of infection during pregnancy • Impact of severity of maternal infection • Magnitude of the possible risk of microcephaly and other adverse pregnancy outcomes Microcephaly • Microcephaly is the clinical finding of a small head compared with infants of the same sex and age, or gestational age if measured at birth • Head circumference is considered a reliable assessment of the volume of the underlying brain • Head circumference (HC) is also known as occipital-frontal circumference (OFC) • Anencephaly • Failure of the neural tube to close resulting in failure of the brain and skull to form • Spina bifida • Failure of neural tube closure resulting in an opening in the spine • Can occur anywhere along the spine Thalidomide malformation FAS (Fetal Alcohol Syndrome) • Low birth weight • Heart septum defects • #1 cause of acquired mental impairment • Short memory spans, Impulsive behavior Neural tube defects Disruptions • Extrinsic disturbance in morphogenesis • Secondary destruction of an organ or body region that was previously normal in development • Ex: amniotic bands – Rupture of amnion formation of “bands” compress/attach to parts of developing fetus • Environmental cause: – Viral infections, drugs, and radiation Pathogenesis • Timing – Embryonic period: 1st 9 weeks pregnancy • Early – 1st 3 weeks after fertilization • 3rd -9th weeks – very susceptible to teratogens (4-5 weeks organs forming) – Fetal period: 10 weeks – birth • Susceptible to growth retardation/injury to already formed organs • Environment and genetic factors Lymphangioma • Benign tumor of dilated lymph vessels • Present at birth or acquired • Skin and deeper regions of neck, axilla, mediastinum, and retroperitoneum • Increase in size after birth • Pediatric diseases – SIDS – Benign tumors – Malignant tumors • Neuroblastoma • Retinoblastoma • Wilms tumor Malignant Tumors of Childhood “small, round, blue cell tumors” Neuroblastoma • Second most common solid malignancy of childhood after brain tumors • Arise from primordial neural crest cells • Most are sporadic but 1-2% familial • Most arise in the adrenal medulla, others in paravertebral region of abdomen • In situ lesions are 40% more common than overt tumors and most regress! Neuroblastoma • Histopath: – primitive-appearing cells with dark nuclei, poorly defined cells growing in solid sheets – Mitosis – Homer-Wright pseudo-rosettes Neuroblastoma Prognosis • Outlook for children younger than 18 months more favorable than older children • Amplification of the NMYC oncogene (25% of cases has a profound affect - greater the number of copies, the worse the prognosis • Overexpression of telomerase – adverse prognostic factors Retinoblastoma • • • • • Intraocular malignancy 40% mutation in RB1 gene (heritable) Neural in origin Bilateral (familial) or unilateral (sporadic) Familial cases have increased chance of osteosarcoma Retinoblastoma • Clinical: – Present at birth, presents ~ age 2 – Poor vision – Strabismus – Whitish hue to pupil (“cat’s eye reflex”) – Pain and tenderness • Histopath: – Flexner-Wintersteiner rosettes (small round blue cells around a central lumen Retinoblastoma • Prognosis: – High survival rate with treatment – Familial type has increased chance of osteosarcoma Wilm’s Tumor (Nephroblastoma) • Tumor of kidney • 2-5 years of age • Increased risk in 3 syndromes – WAGR (Wilms tumor, aniridia, genital abnormalities, mental retardation) – BWS (Beckwith-Wiedemann syndrome) – enlargement of tongue, kidneys or liver – DDS (Denys-Drash syndrome)- gonadal dysgenesis and renal abnormalities • Presents as abdominal mass, abdominal pain • Very good prognosis Wilms Tumor (Nephroblastoma) • Histopath – triphasic – blastemal (small blue cells), epithelial (abortive tubules),stromal (fibrous) anaplastic areas – More anaplastic areas, worse prognosis GI Pathology Outline • Esophagus • Stomach • Intestine • Liver • Hepatitis • Alcoholic liver disease • Hemochromatosis • Wilson disease • Carcinoma Viral Hepatitis • Caused by Hepatitis A, B, or C viruses • Some cases asymptomatic • Some cases symptomatic: • Acute (jaundice) • Chronic (may lead to cirrhosis and liver failure) • Fulminant (liver failure) Hepatitis A Hepatitis B Hepatitis C Transmission Fecal-oral Parenteral Parenteral Chronic Hepatitis None 5% >85% Fulminant hepatitis 0.1% 0.1-1.0% Rare Carcinoma No Yes Yes Other stuff 50% of people > 50 are + Vaccine effective New drugs are promising Bottom line Benign, selflimited disease Most recover; small % die Nasty! Almost 10% die Chronic viral hepatitis: ground-glass hepatocytes Jaundice • Yellow skin, eyes due to elevated bilirubin • Conjugated hyperbilirubinemia • liver excretion (hepatitis) • bile flow (tumor blocking bile duct) • Unconjugated hyperbilirubinemia • production (hemolytic anemia) • uptake (hepatitis) Bilirubin metabolism and elimination Laboratory Tests Serum aspartate aminotransferase (AST) Hepatocyte integrity Serum alanine aminotransferase (ALT) Serum bilirubin (total and direct) Biliary function Serum alkaline phosphatase Serum albumin Hepatocyte function Prothrombin time Cirrhosis • Fibrotic, nodular liver • Causes: alcoholism, hepatitis • Leads to portal hypertension and liver failure • Increased risk of liver carcinoma Portal Hypertension • Decreased blood flow through liver • Biggest cause: cirrhosis • Symptoms • ascites • venous shunts (esophageal varices, hemorrhoids) • congestive splenomegaly • hepatic encephalopathy Consequences of portal hypertension Liver Failure • End point of severe liver disease • Causes: fulminant hepatitis, cirrhosis, drug overdose • Symptoms: jaundice, edema, bleeding, hyperammonemia • Multiple organ-system failure • Hepatic encephalopathy • Hepatorenal syndrome Oral Manifestations of Liver Injury • Hematomas, gingival bleeding • Jaundiced mucosa • Glossitis (in alcoholic hepatitis) • Reduced healing after surgery Alcoholic Liver Disease • 100,000 -200,000 deaths/year • Effects on liver: steatosis, hepatitis, cirrhosis • How much do you need to drink? • Short-term ingestion of 8 beers/day reversible steatosis • Long-term ingestion of 5 beers/day severe injury • Beer and binge drinking are risky Alcoholic liver disease Alcoholic hepatitis: inflammation and Mallory bodies Hereditary hemochromatosis • Autosomal recessive disease: body iron • Cause: mutations in hemochromatosis gene (regulates iron absorption) • Cirrhosis, skin pigmentation, liver carcinoma • Early detection and treatment (phlebotomy, iron chelators) = normal life expectancy Wilson Disease • Autosomal recessive disease: body copper • Cause: mutation in gene regulating copper excretion • Symptoms: acute and chronic liver disease, neuropsychiatric manifestations, KayserFleisher rings in cornea • Treatment: copper chelation therapy Hepatocellular Carcinoma • Strongly associated with hepatitis B and C, chronic liver disease, and aflatoxins • Rapid increase in liver size, worsening ascites, fever and pain • alpha fetoprotein level • Median survival 7 months (death from bleeding, liver failure, cachexia) Metastatic Carcinoma • Most common malignancy in the liver • Usually multiple lesions • Most common primaries: colon, lung, breast, pancreas, stomach. Cholelithiasis • Common! (10% of adults in US) • Cholesterol stones: Female, Fat, Fertile, Forty • Pigment (bilirubin) stones: Asian countries, hemolytic anemia and biliary infections • Symptoms: None, or excruciating pain • Complications: cholecystitis, empyema, perforation, fistula, obstruction, pancreatitis Acute Pancreatitis • Acute inflammation and reversible destruction • • • • of pancreas Symptoms: abdominal pain radiating to back Main causes: alcoholism, gallstones Labs: elevated serum amylase and lipase Prognosis: Most recover, but 5% die in first week Chronic Pancreatitis • Longstanding, irreversible pancreatic destruction • Most are alcohol related, some idiopathic • Symptoms: silent, or bouts of jaundice and pain • Prognosis: poor (50% mortality over 20 years) Pancreatic Carcinoma • 4th leading cause of cancer death in US • Biggest risk factor: smoking • Highly invasive • Silent until late (especially tail); then pain, jaundice • Very high mortality: 5ys <5%