Contemporary Psychodynamic Psychotherapy Contemporary Psychodynamic Psychotherapy Evolving Clinical Practice Edited by David Kealy Department of Psychiatry, University of British Columbia, Vancouver, Canada John S. Ogrodniczuk Department of Psychiatry, University of British Columbia, Vancouver, Canada Academic Press is an imprint of Elsevier 125 London Wall, London EC2Y 5AS, United Kingdom 525 B Street, Suite 1650, San Diego, CA 92101, United States 50 Hampshire Street, 5th Floor, Cambridge, MA 02139, United States The Boulevard, Langford Lane, Kidlington, Oxford OX5 1GB, United Kingdom Copyright © 2019 Elsevier Inc. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or any information storage and retrieval system, without permission in writing from the publisher. Details on how to seek permission, further information about the Publisher’s permissions policies and our arrangements with organizations such as the Copyright Clearance Center and the Copyright Licensing Agency, can be found at our website: www.elsevier.com/permissions. This book and the individual contributions contained in it are protected under copyright by the Publisher (other than as may be noted herein). Notices Knowledge and best practice in this field are constantly changing. As new research and experience broaden our understanding, changes in research methods, professional practices, or medical treatment may become necessary. Practitioners and researchers must always rely on their own experience and knowledge in evaluating and using any information, methods, compounds, or experiments described herein. In using such information or methods they should be mindful of their own safety and the safety of others, including parties for whom they have a professional responsibility. To the fullest extent of the law, neither the Publisher nor the authors, contributors, or editors, assume any liability for any injury and/or damage to persons or property as a matter of products liability, negligence or otherwise, or from any use or operation of any methods, products, instructions, or ideas contained in the material herein. British Library Cataloguing-in-Publication Data A catalogue record for this book is available from the British Library Library of Congress Cataloging-in-Publication Data A catalog record for this book is available from the Library of Congress ISBN: 978-0-12-813373-6 For Information on all Academic Press publications visit our website at https://www.elsevier.com/books-and-journals Publisher: Nikki Levy Acquisition Editor: Nikki Levy Editorial Project Manager: Ruby Smith Production Project Manager: Bharatwaj Varatharajan Cover Designer: Mark Rogers Typeset by MPS Limited, Chennai, India List of contributors Dana Atzil-Slonim Psychology Department, Bar-Ilan University, Ramat Gan, Israel Louise Balfour The Ottawa Hospital, University of Ottawa, Ottawa, ON, Canada Jacques P. Barber Derner Institute of Advanced Psychological Study, Adelphi University, New York, NY, United States Anthony Bateman University College London, London, United Kingdom Fredric N. Busch Weill Cornell Medical College, New York, NY, United States Eve Caligor Columbia University College of Physicians and Surgeons, New York, NY, United States Richard A. Chefetz Washington Baltimore Center for Psychoanalysis, Washington, DC, United States; Institute of Contemporary Psychotherapy & Psychoanalysis, Washington, DC, United States John F. Clarkin Weill Cornell Medical College, New York, NY, United States; New York Presbyterian Hospital Cornell Medical Center, White Plains, NY, United States Katherine Crits-Christoph Department of Psychiatry, University of Pennsylvania, PA, United States Paul Crits-Christoph Department of Psychiatry, University of Pennsylvania, PA, United States Celine De Meulemeester Faculty of Psychology and Educational Sciences, University of Leuven, Leuven, Belgium Martin Debbané Developmental Clinical Psychology Research Unit, Faculty of Psychology and Educational Sciences, University of Geneva, Geneva, Switzerland; Research Department of Clinical, Educational and Health Psychology, University College London, London, United Kingdom x List of contributors Guy Diamond Center for Family Intervention Science, College of Nursing and Health Professions, Drexel University, Philadelphia, PA, United States Nel Draijer Private practice Johannes C. Ehrenthal Heidelberg University, Heidelberg, Germany Peter Fonagy Research Department of Clinical, Educational and Health Psychology, University College London, London, United Kingdom Mary Beth Connolly Gibbons Department of Psychiatry, University of Pennsylvania, PA, United States Geoff Goodman Clinical Psychology Doctoral Program, Long Island University, Brookville, NY, United States; Institute for Psychoanalytic Training and Research, NY, United States Charles A. Granoff, MSW Community Services Institute, Springfield and Dorchester, MA, United States Robert J. Gregory Department of Psychiatry and Behavioral Sciences, SUNY Upstate Medical University, Syracuse, NY, United States James Higginbotham Community Services Institute, Springfield and Dorchester, MA, United States Mark J. Hilsenroth Derner School of Psychology, Adelphi University, New York, NY, United States Robert Johansson Department of Psychology, Stockholm University, Stockholm, Sweden; Department of Behavioural Sciences and Learning, Linköping University, Linköping, Sweden David Kealy Department of Psychiatry, University of British Columbia, Vancouver, Canada John R. Keefe Weill Cornell Medical College, University of Pennsylvania, University Park, PA, United States Johannes Kruse Department of Psychosomatics and Psychotherapy, University of Giessen, Giessen, Germany; Department of Psychosomatics and Psychotherapy, University of Marburg, Marburg, Germany List of contributors xi Falk Leichsenring Department of Psychosomatics and Psychotherapy, University of Giessen, Giessen, Germany; Department of Psychosomatics and Psychotherapy, Justus-Liebig-University Giessen, Giessen, Germany Kenneth N. Levy Department of Psychology, Weill Cornell Medical College, Pennsylvania State University, University Park, PA, United States Suzanne Levy Center for Family Intervention Science, College of Nursing and Health Professions, Drexel University, Philadelphia, PA, United States Vittorio Lingiardi Department of Dynamic and Clinical Psychology, Faculty of Medicine and Psychology, Sapienza University of Rome, Rome, Italy Patrick Luyten Faculty of Psychology and Educational Sciences, University of Leuven, Leuven, Belgium; Research Department of Clinical, Educational and Health Psychology, University College London, London, United Kingdom Norka T. Malberg, Psy.D Western New England Psychoanalytic Society, CT, United States; Yale Child Study Center, CT, United States Syreeta Mason Center for Family Intervention Science, College of Nursing and Health Professions, Drexel University, Philadelphia, PA, United States Helga Mattheß University of Worcester, Worcester, United Kingdom Kevin S. McCarthy Chestnut Hill College, Philadelphia, PA, United States; Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, United States Nick Midgley Anna Freud National Centre for Children and Families, University College London, London, United Kingdom Barbara L. Milrod Weill Cornell Medical College, New York, NY, United States; New York Psychoanalytic Institute, New York, NY, United States; Columbia University Center for Psychoanalytic Training and Research, New York, NY, United States Nicola Nardelli Department of Dynamic and Clinical Psychology, Faculty of Medicine and Psychology, Sapienza University of Rome, Rome, Italy Pamela Nathan CASSE Aboriginal Australian Relations Program xii List of contributors John S. Ogrodniczuk Department of Psychiatry, University of British Columbia, Vancouver, Canada Seth R. Pitman Austen Riggs Center, Stockbridge, MA, United States Bent Rosenbaum Institute of Psychology, University of Copenhagen, Denmark; Head of Psychotherapy Research, Psychiatric Center Copenhagen, Clinic of Psychotherapy Frank Sacco Jr, Psy.D. Community Services Institute, Springfield and Dorchester, MA, United States Frank C. Sacco, PhD Community Services Institute, Springfield and Dorchester, MA, United States Björn Salomonsson Department of Women’s and Children’s Health, Karolinska Institutet, Stockholm, Sweden Daniel Smyth Private practice, London, United Kingdom; Sport and Thought, Football as Therapy, London, United Kingdom Christiane Steinert Department of Psychosomatics and Psychotherapy, University of Giessen, Giessen, Germany; Department of Psychology, MSB Medical School Berlin, Berlin, Germany; Department of Psychosomatics and Psychotherapy, Justus-Liebig-University Giessen, Giessen, Germany Giorgio A. Tasca School of Psychology, University of Ottawa, Ottawa, ON, Canada Pratyusha Tummala-Narra Department of Counseling, Developmental and Educational Psychology, Boston College, Chestnut Hill, MA, United States Pauline Van Zon Private practice Wolfgang Wöller Rhein-Klinik, Hospital for Psychosomatic Medicine and Psychotherapy, Bad Honnef, Germany Frank E. Yeomans Weill Cornell Medical College, New York, NY, United States Sigal Zilcha-Mano University of Haifa, Haifa, Israel Introduction Psychodynamic psychotherapy is one of the most widely practiced forms of psychotherapy today, applied in a variety of settings and contexts, across a wide range of patient or client problems, and by members of several mental health disciplines. A great many psychotherapists expressly identify themselves as “psychodynamically oriented,” and countless others incorporate psychodynamic principles and strategies in their work, often blending or integrating psychodynamic understanding and technique with other therapy models. Similarly, many consumers of psychotherapy benefit from psychodynamic approaches without having explicitly sought them out in their quest to obtain help. Seeking relief from suffering, they may happen upon a psychodynamic process through consulting with a therapist at a local outpatient clinic or in an integrative therapy group that blends psychoeducation with examination of interpersonal processes. Many individuals seeking psychotherapy, however, are intent upon engaging in a therapeutic process that allows for a thorough exploration of one’s mind, interpersonal relationships, and broader sociocultural influences in the process of understanding and addressing complex life problems. These consumers have little difficulty regarding an extended, even meandering, exploratory therapy as a legitimate and effective means to alleviate suffering and expand personal capacities. Psychodynamic psychotherapy offers this possibility for those who seek it. Indeed, many psychotherapists themselves choose to obtain psychodynamic therapy for their own personal therapy, whether to address personal challenges or simply for better self-understanding, regardless of the therapeutic approach they offer their clients. Other prospective therapy consumers, however, seek a more direct route to problem resolution. These individuals may want a time-limited, structured approach that can zero in on conflicted motivations, constricted affects, or unsatisfactory attachment patterns underlying their troublesome symptoms. Here again, psychodynamic therapy can deliver, with well-defined, structured models available for a range of mental health problems. These various permutations, among others, add up to a lot of psychodynamic psychotherapy being sought by clients, practiced by clinicians, and—we would argue—delivered to good effect. Despite this widespread proliferation, misconceptions abound regarding psychodynamic psychotherapy as a contemporary treatment. One common misconception is the notion that a psychodynamic approach is old-fashioned, a dusty relic of a bygone era. According to this perception, the theory underlying psychodynamic therapy was long ago supplanted by more modern, scientific understandings of the mind and mental disorder, rendering psychodynamic therapy an antiquated and irrelevant endeavor. Related to this misconception is the claim that psychodynamic psychotherapy has been eclipsed by “evidence-based” treatments that have been xiv Introduction validated by rigorous empirical research, implying that psychodynamic therapy has not been or, worse, that it has been found to be an inferior approach compared to other mental health treatments. Another misconception may even be unwittingly perpetuated by some practitioners within the psychodynamic community: that there is one particular way—steeped in tradition—of doing psychodynamic psychotherapy. This myth is most likely to be transmitted implicitly, through the training and supervision of new clinicians, and may be compounded by new therapists’ anxieties about practicing “the right way.” From our perspective, these various misconceptions could hardly be further from the truth. Psychodynamic psychotherapy today is a diverse and vibrant field. The scientific basis for psychodynamic approaches has become more robust and expansive, with an ongoing accrual of research evidence regarding treatment outcomes and processes—shedding light on how therapy works —across different conditions and populations. Meanwhile, theoretical and practice innovations continue, contributing further conceptual refinements and novel applications. Rather than ossifying, psychodynamic psychotherapy is enjoying a quiet renaissance. When we were considering the development of this volume, our objective was to share some of the evolution and vitality evident in the field of contemporary psychodynamic psychotherapy. We felt that it was about time for a book to bring together a number of recent developments, including research contributions, conceptual developments, research-to-practice translation, and innovations in clinical delivery. This book is thus intended to celebrate the leading edge of psychodynamic psychotherapy today. In one sense, we view the book as a compendium of current knowledge regarding psychodynamic psychotherapy: a snapshot of where the field is today and some of the directions in which it is moving. At the same time, we also hope that this compilation overall conveys a sense of the organic, everdeveloping nature of contemporary psychodynamic science and practice. For the reader who is new to psychodynamic psychotherapy, we hope that the chapters within will reveal how versatile this approach can be. While the chapters are not exhaustive in scope, we have tried to include a variety of problem areas for psychodynamic applications, with different points of technical emphasis conveyed across the chapters. Similarly, for readers who identify with other theoretical traditions but seek to incorporate psychodynamic interventions in their clinical toolkit, the different approaches described in the book offer opportunities for comparison, integration, and further exploration. Our hope for the seasoned psychodynamically oriented reader is a volume that provides an update on research-based models, contemporary practice considerations, and innovative treatment formats. To meet the objectives we had in mind for this book, we sought contributions from people who are actively moving psychodynamic therapy forward and who are communicating their work through academically oriented writings. This work doesn’t always get into the hands of practitioners in a timely manner and often not in one volume. Here, we wanted such contributions to be addressed to clinicians— therapists in real-world practice—in a way that distills key insights, allows for ready translation to clinical work, and stimulates interest in further learning. We asked leading psychodynamic therapy researchers to present key implications of Introduction xv their work, focusing on various mental health problems that often bring people to psychotherapy. To complement this problem-based focus, we invited scholars to discuss psychodynamically informed perspectives regarding clinical work with particular client populations as well as special clinical considerations that reflect the diversity and complexity of contemporary practice. Recognizing that leading edge practices are often not well established in the literature, we also invited contributions from authors whose academic work is nascent, though highly innovative in applying and integrating psychodynamic principles and interventions in novel ways. Thus to further reflect the vitality of contemporary psychodynamic psychotherapy, we sought to bring under one roof the work of scholars and clinicians across a variety of areas and stages of development. Some readers may observe that psychoanalysis is conspicuously underrepresented throughout this book. The relationship between psychodynamic psychotherapy and psychoanalysis is a complicated one, discussion of which would take us too far afield from the objectives of this book. Suffice it to say that psychodynamic psychotherapy and psychoanalysis are not one and the same. Psychoanalysis has left an indelible impression on psychodynamic psychotherapy, and there remains an ongoing exchange between these disciplines that, in our view, strengthens both. Yet psychodynamic psychotherapy has evolved in its own right, and our intention is to showcase the current state of this evolution. While echoes of psychoanalysis may be heard throughout these chapters, psychodynamic psychotherapy is playing the lead role here. The chapters have been loosely organized into five sections. We begin with a section on prominent theoretical developments in contemporary psychodynamic psychotherapy, followed by a section devoted to an overview of the empirical support for psychodynamic constructs, treatments, and therapeutic processes. The third section comprises chapters that describe psychodynamic therapy approaches for various mental health problems. These chapters draw upon the authors’ and others’ empirical research and clinical expertise, often including illustrative case material, to convey a sense of how these disorders can be addressed using psychodynamic therapy. Since the differences and concerns among clients transcend their presenting problem or diagnosis, the fourth section is focused on special populations and critical considerations. These chapters draw attention to some of the nuances that emerge through clients’ diverse needs and experiences and highlight psychodynamic perspectives that can assist the clinician in working effectively with these complexities. The final part of the book contains chapters that outline several novel means of delivering psychodynamic intervention. These contributions provide compelling examples of the ways in which psychodynamic therapy is extending its reach, often through integration with other modes of service. Section 1: conceptual advances Our first chapter gives an overview of prominent theoretical developments, aimed at introducing key features of psychodynamic theory to the novice reader and xvi Introduction providing a sense of conceptual evolution to readers grounded in psychodynamic practice. In the second chapter, Mark Hilsenroth and Seth Pitman focus on the specific issue of understanding and working with patients’ cyclical relational patterns, a hallmark of psychodynamic therapy. This contribution takes the reader through the traditional meta-psychological construct of transference and moves toward a more descriptive and experience-near conceptualization of the processing of insession, here-and-now relational dynamics. Next, Martin Debbané provides an overview of contemporary attachment and mentalization theories. This chapter introduces a mentalization-based conceptualization of psychopathology along with a discussion of the nature of therapeutic change from the perspective of mentalization theory. Section 2: psychodynamic psychotherapy as evidence-based treatment The second section is intended to give the reader a sense of the scientific work being done to support the efficacy of psychodynamic psychotherapy and to further our understanding of how it works and for whom. Owing to the volume of work in these areas, these chapters are necessarily concise, providing summaries and overviews of the current evidence base rather than a detailed examination of each individual study. This section begins with a chapter by Falk Leichsenring and Christiane Steinert that reviews the efficacy of psychodynamic therapy, revealing substantial evidence for the efficacy of psychodynamic therapy in depressive, anxiety, somatoform, eating, substance-related, and personality disorders. This is followed by a review by Kevin McCarthy, Sigal Zilcha-Mano, and Jacques Barber of some of the sophisticated and novel studies regarding interventions in psychodynamic psychotherapy, the therapeutic relationship, and their relation to other phenomena in psychodynamic psychotherapy and its outcomes. The section closes with a chapter by Kenneth Levy, John Keefe, and Johannes Ehrenthal that provides an overview of empirical evidence that supports basic psychodynamic tenets, with consideration of the implications of these concepts for the process of psychotherapy treatment. Section 3: contemporary psychodynamic treatment for specific conditions Major advances in the application of psychodynamic therapy regarding specific clinical disorders are presented in this section. These chapters provide informative overviews of empirically supported psychodynamic models, many with illustrative case examples, for several mental health challenges. The section begins with a chapter in which Mary Beth Connolly Gibbons, Katherine Crits-Christoph, and Paul Introduction xvii Crits-Christoph outline an adaptation of short-term supportive-expressive psychotherapy for the treatment of depression, specifically designed for implementation in community mental health settings. The treatment of anxiety is taken up by Fredric Busch and Barbara Milrod, with a description of Panic-Focused Psychodynamic Psychotherapy. This chapter outlines an extension of the panic-focused psychodynamic psychotherapy model to address a range of DSM-V anxiety disorders, cluster C personality disorders, and posttraumatic stress disorder. In their chapter on mentalization-based treatment, Anthony Bateman and Peter Fonagy expand on a conceptualization of personality disorder that emphasizes the vulnerability to losing the capacity to mentalize. The chapter outlines the use of mentalization-based therapy for patients suffering from borderline and antisocial personality disorders, conditions that are commonly regarded as challenging to treat. Another prominent evidence-based treatment for personality disorder is featured in the chapter by Eve Caligor, John Clarkin, and Frank Yeomans. These authors articulate the use of transference-focused psychotherapy for patients with both borderline and narcissistic personality disorder, the latter of which is often neglected in structured approaches to treating personality disorders. Focusing on the immense challenges of working with patients who suffer from cooccurring substance use and personality disorder, the chapter by Robert Gregory presents a comprehensive treatment model called dynamic deconstructive psychotherapy for use with this patient population. Although there is a rich history of its use with patients who suffer from psychoses, psychodynamic treatment has often been overlooked as an appropriate therapy for such patients. Bent Rosenbaum provides a chapter that challenges this omission by describing the contemporary use and empirical grounding of psychodynamically informed supportive therapy for patients with psychosis. Next, Patrick Luyten, Celine De Meulemeester, and Peter Fonagy describe dynamic interpersonal therapy, a contemporary psychodynamic approach to the understanding and treatment of patients with somatic symptom disorder or functional somatic disorder. Their work is founded on three related biobehavioral systems that are central in current psychodynamic approaches to helping patients with these conditions. The section closes with a contribution from Giorgio Tasca and Louise Balfour describing an approach to psychotherapy for patients with eating disorders that is informed by attachment theory and an interpersonally based psychodynamic model. This chapter invites readers to consider psychodynamic conceptualizations and approaches to treating eating disorders that take into account social and relational contexts and attachment-related states of mind. Section 4: special populations and critical considerations This section extends the practical focus of the preceding section to the application of psychodynamic approaches for client populations with specialized needs as well as critical considerations for generalist clinicians to bear in mind, better equipping them to consider the unique experiences and needs of diverse clients. A trio of chapters xviii Introduction focus on the use of psychodynamic therapies for younger populations (infants, children, and adolescents). Bjorn Salomonsson considers the development of psychodynamic therapy for infants and parents, comparing models on the basis of their conceptual and technical emphases regarding the psychologies of and interactions between infant, parent, and therapist. Geoff Goodman and Nick Midgley provide a review of five different manualized child psychodynamic therapies, presenting the aims and methods of each approach, summarizing their treatment course, and offering empirical evidence in support of their effectiveness. Following along the age trajectory set forth by these two chapters, Dana Atzil-Slonim contributes an overview of adolescent psychodynamic psychotherapy, discussing psychodynamic theories of adolescence and describing psychodynamic practice with adolescent clients. Psychotherapy that ignores issues related to clients’ sexual orientation and/or gender identity is, in addition to lacking effectiveness, likely to perpetuate marginalization of sexual and gender minorities. Many such issues and their implications for psychodynamic therapy are discussed in a chapter by Vittorio Lingiardi and Nicola Nardelli. This contribution offers the clinician a framework for contemplating critical issues in psychodynamic practice with clients who identify as members of sexual and gender minorities. Immigrants and refugees represent another broad group whose social challenges, including trauma and marginalization, need special consideration in psychotherapy. Pratyusha Tummala-Narra provides an overview of key sociocultural factors that may shape the clinical picture in work with immigrant and/or refugee clients. The chapter invites the reader to consider premigration and postmigration contexts, acculturation and related stress, and trauma as well as the implications of these factors for the client’s negotiation of separation and loss and for the dynamics of the therapeutic relationship. The next set of chapters in this section present potential considerations and approaches in psychodynamic work with people who have encountered profoundly traumatic experiences. Richard Chefetz addresses the issue of dissociative processes, often highly salient in the experience of individuals who have suffered severe trauma. This chapter demonstrates the dissociative concealment of the underlying meanings of experience, behavior, and motivation that ultimately shapes the client’s subjective sense of self and organization of mind. Next, Nel Draijer and Pauline Van Zon describe the application of transference-focused psychotherapy to the treatment of former child soldiers suffering from dissociative identity disorder. These authors discuss how this approach can address overwhelming, dissociated negative affects, including their role in controlling and alienating others, in order to help sufferers of severe trauma to find release from internal oppression. The final chapter in this section, contributed by Christiane Steinert, Johannes Kruse, Falk Leichsenring, Helga Mattheß, and Wolfgang Wöller, considers the immense gap between the need for mental health services and the availability of such services in postconflict and refugee crisis settings. The chapter describes a brief, culturally adaptable, manualized intervention that puts special emphasis on the therapeutic relationship, stabilization and emotion regulation, and the strengthening of resources while addressing dissociative states and transference and countertransference reactions in the context of trauma. Introduction xix Section 5: innovative modes of delivery The final section of the book highlights several novel ways of delivering psychodynamically informed intervention beyond the typical configuration of therapist and client meeting in the consulting room. Chapters in this section describe applications that extend the reach of psychodynamic work, offering benefit to clients who otherwise might not access psychodynamically informed intervention as traditionally offered. While the applications profiled in this section are diverse, a common thread of innovation runs through these contributions. While some of these efforts have been well researched, several represent the work of leading clinicians who—fortunately for the contemporary psychodynamic field—have recently begun writing about their work. We hope that the sharing of these accomplishments might inspire clinicians to implement such novel approaches or to consider other ways in which they might develop innovative psychodynamic applications in their own practice. Robert Johansson begins the section with a chapter that describes psychodynamic intervention in the form of guided self-help through the internet. This mode of delivery holds promise for the potential to reach individuals who may not otherwise have access to sophisticated psychological treatment. For others, online delivery may be ideally suited to their preferences and life demands. The next chapter, by Guy Diamond, Syreeta Mason, and Suzanne Levy, provides an overview of a psychodynamically informed, attachment-based family therapy. Aimed at helping distressed adolescents and young adults, this approach seeks to identify and resolve, through direct family-level therapeutic work, family conflicts that contribute to damaged trust between parents and adolescents. Psychodynamic principles are also being applied at the broader community level. The chapter by Pamela Nathan describes such an effort, profiling the work of a notfor-profit, psychoanalytic organization known as Creating A Safe Supportive Environment (CASSE) in central Australia. Guided by key principles of psychodynamic practice and modified for broader application to the community, CASSE forms partnerships and collaborations with Aboriginal organizations and other stakeholders to work toward ameliorating the psychological impact of colonialism and cultural dispossession experienced by Aboriginal communities. Another community-based effort, known as Sport and Thought, is described in the chapter by Daniel Smyth. This chapter outlines an innovative approach to help adolescent boys with behavioral and emotional difficulties through the fusing of psychodynamic principles with football. The Sport and Thought program offers an accessible prevention and early intervention approach for youth who would not engage via traditional therapeutic routes. The next chapter, by Frank Sacco, Jr., James Higginbotham, Charles Granoff, and Frank C. Sacco, also profiles an approach targeting high-risk youth. This contribution describes therapeutic mentoring, a community-based program that extends mentalizing work into community settings with young people who are receiving more traditional psychodynamic therapy. Therapeutic mentoring is delivered as part of a team-based approach whereby the mentor reinforces mentalizing and social adaptation through engagement in xx Introduction community-based activities. Young people are also featured in the final chapter in this section, although the insights shared by Norka Malberg in this contribution extend to various populations receiving intensive medical treatment. This chapter describes psychodynamic group intervention in inpatient medical settings, indicating the benefits—both for patients’ emotional well-being and for their ongoing medical care—of helping patients work through the psychodynamic concerns that often accompany compromised physical health and the need for intensive medical treatment. A final note The field of psychodynamic psychotherapy is continually evolving. While traditionally focused on unconscious elements that underlie various psychological maladies, psychodynamic psychotherapy in contemporary practice has a broad scope that merges attention to complex mental states with consideration of biological, interpersonal, social, and cultural factors. Drawing upon a rich heritage of theorizing about the complexities of human development, interaction, and psychopathology, contemporary psychodynamic psychotherapy represents a viable means of addressing emotional suffering and mental disorder. Moreover, the principles and interventions gathered under the psychodynamic umbrella are aimed not only at the amelioration of particular symptoms, but also toward the encouragement of growth in essential human capacities to love, work, play, and laugh—to live with creativity and meaning. To support these aims, psychodynamic theorists, clinicians, and researchers eschew complacency by contemplating new questions and challenges that further advance the perspectives, applications, and empirical bases of psychodynamic psychotherapy. It is our hope that this book, through consolidating some of the foremost advances in the psychodynamic field, will inform and inspire readers to consider how such developments might help to shape their own contemporary psychodynamic practice. David Kealy and John S. Ogrodniczuk Theoretical evolution in psychodynamic psychotherapy 1 David Kealy and John S. Ogrodniczuk Department of Psychiatry, University of British Columbia, Vancouver, Canada Theory is essential to the practice of psychotherapy. It helps therapists to organize information about their patients and to understand their patients’ difficulties, and it provides a framework for mechanisms of therapeutic action. As Wampold (2010) notes, “there is no therapy without theory” (p. 43). Psychodynamic psychotherapy is founded upon psychoanalytic theory, the elucidation, refinement, and revision of which has arguably preoccupied the field to a greater extent than empirical research or dissemination of formal psychodynamic treatment guidelines. Psychoanalytic theory has changed a lot since its inception more than a century ago; thorough documentation of this would require a book unto itself, if not several volumes. We believe, however, that a basic grasp of the evolution of psychoanalytic theory—at least some major points along the way—can help clinicians in their understanding and practice of contemporary psychodynamic psychotherapy. In this chapter we will discuss some of the key developments in psychoanalytic theory that have contributed to contemporary psychodynamic psychotherapy. Given the breadth and depth of the psychoanalytic theoretical literature, we will paint with broad strokes and focus on theoretical developments that we perceive to be particularly salient to practitioners of psychotherapy therapy today. Our aim is to provide a concise introduction to readers who may be less familiar with psychodynamic psychotherapy and its theoretical foundations while at the same time highlighting some points of convergence and debate that may resonate with more experienced clinicians. In doing so, we will chart a crash course through the evolution of psychoanalytic theory and into its application in the contemporary practice of psychodynamic therapy. What makes a theory—and therapy—psychodynamic? While technical distinctions can be made between psychoanalysis and various psychodynamic psychotherapies, a shared emphasis on unconscious mental processes forms the bedrock of a uniting theoretical foundation. Beyond this foundation, however, the precise nature of core psychodynamic theory has been rather difficult to pin down, partly owing to a proliferation of ideas and schools of thought within psychoanalysis and throughout the numerous psychotherapies informed by psychodynamic concepts. This makes for some difficulty in precisely defining a core psychodynamic theory. Indeed, contemporary psychodynamic practice is more fittingly Contemporary Psychodynamic Psychotherapy. DOI: https://doi.org/10.1016/B978-0-12-813373-6.00001-5 © 2019 Elsevier Inc. All rights reserved. 4 Contemporary Psychodynamic Psychotherapy characterized by a plurality of approaches under a broad psychoanalytic umbrella. Nevertheless, all psychodynamic models conceive of unconscious psychological processes as playing an important role in shaping the ways in which people experience (i.e., make sense of) and act in their world (Gabbard, 2017). Thus psychodynamic theories emphasize a motivated unconscious or, in other words, unconscious motivation. Moreover, the nature of unconscious experience is regarded as highly unique for each individual, knowable largely through inference or introspection or partially glimpsed through dreams and fantasies. Psychodynamic theories also pay careful attention to childhood experiences as influences on the development of unconscious motivational tendencies, representations of self and other, and conflicts between motivational or affective states. Similarly, psychopathology is typically conceptualized as involving unconscious causes—such as excessive conflict or problematic relational representations—playing a significant role in consciously perceived distress or dysfunction. In addition to conceptualizations of the mind and psychopathology, theories of therapeutic technique and change mechanisms distinguish psychodynamic approaches from other psychotherapies. In general, psychodynamic therapies emphasize change occurring by way of increased access to emotional experience and through the development of insight into unconscious motivations, defenses, and interpersonal patterns (Gabbard, 2017). Psychodynamic therapy also emphasizes the therapeutic relationship itself as a vehicle of change, both for highlighting the patient’s emotional and interpersonal patterns and for providing interactional experiences that serve corrective developmental purposes for the patient. Various technical stances and interventions support and facilitate these mechanisms, including the patient’s free association—expressing whatever comes to mind—or at least the patient’s leading the dialogue, the therapist’s observation and clarification of difficult or contradictory thoughts and feelings, and a joint exploration of unconscious meanings and motivations. Exploration, guided by empathic inquiry, is applied not only to the various concerns and issues in the patient’s world, but also to the relational dynamics occurring between therapist and patient. Indeed, perhaps more so than other therapy models, psychodynamic approaches pay close attention to the emotional responses of the patient regarding the therapist—known as transference— and of the therapist regarding the patient—referred to as countertransference. Despite the centrality of such interventions to dynamic psychotherapy, it must be noted that aspects of these elements are increasingly being absorbed by other, nondynamic approaches—often referred to using different jargon—and combined with other techniques by therapists who take an integrative stance toward treatment. Moreover, as a close reading of this book’s chapters will reveal, psychodynamic approaches often differ in their emphasis on particular mechanisms and technical strategies. Indeed, the considerable breadth and depth in the revisions of psychoanalytic theory provide numerous opportunities for divergence in its application to treatment. Our coverage of these developments will be focused on their application to psychotherapy rather than on psychoanalysis per se and will by necessity be exceedingly brief and beyond incomplete. Our succinct account of Freudian theory, for instance, does little justice to the revisions Freud made during his lifetime. Several excellent volumes offer comprehensive treatment of the evolution toward Theoretical evolution in psychodynamic psychotherapy 5 contemporary psychoanalytic theory, including those by Mitchell and Greenberg (1983), Bacal and Newman (1990), Fonagy (2001), and Eagle (2011). Discussion of some of the finer points of convergence and divergence in contemporary theory is also offered by Gabbard and Westen (2003) and Kernberg (2011). From classical theory to ego psychology Freud’s model of the mind—regarded as “classical” psychoanalytic theory—considered the nervous system as a mediator of the buildup and discharge of affect, serving regulatory functions aimed toward the seeking of pleasure and reduction of unpleasure (Freud, 1920/1966). Survival-oriented biological drives (reflecting survival of both the individual and the species), such as hunger or sexual urges, press for discharge and register in the mind as desires or wishes. The constant pressure on the mind for the gratification of these wishes—the discharge of drives—manifests in their expression across various aspects of cognition and behavior. Sexual wishes, for example, may find expression in how one interprets a painting or in the content of an erotic dream (Freud, 1920/1966). These expressions reflect the conflict between internal, instinct-based wishes (emanating from a mental structure labeled the “id”) and the demands and limits imposed by external reality. Freud evolved his theory to suggest that a specific structure of the mind, the ego, serves to inhibit immediate drive gratification in response to reality considerations and to facilitate eventual, appropriate gratification (Freud, 1923). Partial gratification, represented by the various expressions of these wishes in the individual’s mental life, is allowed by the ego in order to prevent excessive buildup of excitation. The ego also attenuates awareness of the instinctual origins of such wishes in order to spare the individual from excessive anxiety associated with their forbidden nature and with the anticipated consequences of their gratification. Freudian theory emphasizes the implications of drive derivatives—particularly sexual and aggressive wishes—being directed toward childhood “objects” (the child’s parents) for gratification. The need to manage potential anxiety associated with childhood instinctual wishes peaks during the so-called oedipal period (roughly 3 5 years old). During this phase, the child’s libidinal wishes directed toward one parent—and aggressive wishes toward the “rival” parent—raise the fear of several detrimental consequences, including the risk of retribution (including bodily damage) from the “rival” parent or the loss of the parental object or that parent’s love. The ego must find a way to discharge the persistent drive derivatives while avoiding a calamitous outcome—as well as to reduce the anxiety that accompanies cognizance of these forbidden desires. Thus the ego seeks to obtain some measure of compromise in which attenuated fulfillment of a wish is achieved as its instinctual basis remains hidden, lest the child become fully aware of its forbidden nature and dangerous consequences. While Freud (1936) focused on repression as a principal mechanism by which the ego renders forbidden wishes unconscious, various ego defenses were subsequently identified as accomplishing the function of repression via an array of means. Thus, defense mechanisms—projection, displacement, reaction formation, 6 Contemporary Psychodynamic Psychotherapy and so on—reduce tension by responding to signal anxiety with the relegation of threatening drive derivatives to an unconscious portion of the mind. This dynamic unconscious is a distinctly psychoanalytic notion of unconscious mental activity, in that the latter comprises not only nonconscious mental automaticity, but also affects and thoughts that are banished from awareness for regulatory purposes. The end result of the pressing of instinctual wishes and their modulation by the ego is a compromise between wish and defense that may manifest either adaptively or maladaptively, with the potential to emerge as a symptom or character trait. Evolving from Freud’s classical theory, ego psychology represents the contributions of analysts who paid closer attention to the functions of the ego, arguing that the ego exerted a substantial influence on behavior and personality beyond its role as mediator of instinct and reality. While ego psychologists expanded the conceptualization of defenses (Freud, 1966), they highlighted additional ways in which the ego regulates the individual’s mental life. Heinz Hartmann, a key figure in ego psychology, suggested that the ego possesses several capacities that are largely independent from drive regulation (Hartmann, 1958). These ego functions—including capacities for reality testing and judgment—serve to perceive, organize, and synthesize aspects of the environment in order to allow the individual to adapt to his or her reality. The expansion of the role of the ego introduced by Hartmann (1958) and others included motivational interests, such as desires for personal and social achievements, that were mainly autonomous from, and sometimes competing with, pressure from drive derivatives (Eagle, 2011). Indeed, Erikson (1959) situated the development of personal identity, facilitated through cultural and environmental experience, within the ego and elaborated a model of psychosocial development throughout the life span that transcended drive theory. The conceptual extensions of ego psychology helped psychoanalytic theory transition from what has been referred to as a one-person psychology, in which endogenous drives are directed at objects (i.e., people as targets whose individual psychologies were deemphasized), toward a two-person psychology whereby the qualities and behaviors of other people are seen as playing a significant role in shaping the individual’s psychic life. To regard this transition as a sharp departure would be misleading; Freud’s own concept of the superego as the structure containing morals and ideals—internalized through relations with parental objects—was itself a step toward a psychology grounded in interpersonal relationships (Ogden, 2002). With regard to psychopathology, classical and ego psychological theory emphasize symptom- and character-based neuroses rooted in repressed conflicts, typically connected to sexual and aggressive wishes from the oedipal period. Such conflicts—more precisely, pathological compromise formations—take the form of phobias, compulsions, inhibitions, and character traits that contribute to suffering, though their origins remain obscured by defenses. A primary goal of treatment is thus to promote insight into the wish-defense compromises underlying the patient’s symptoms and to explicate their origins in the patient’s particular oedipal struggles. Since drive derivatives continue to press for discharge and given the unresolved nature of the patient’s oedipal conflicts, the wishes and the defenses mobilized to contain them will invariably find expression in the patient’s relationship with the Theoretical evolution in psychodynamic psychotherapy 7 therapist. Known as the transference neurosis, this “transference” of the patient’s earlier oedipal situation to the therapy relationship provides an in vivo demonstration of the patient’s unresolved childhood wishes and conflicts. Further evidence obtained through the patient’s free associations and recounting of dreams and memories informs the therapist in gradually making interpretations regarding the patient’s unconscious mental life. Thus the mechanism of therapeutic action rests largely upon the interpretation of wish-defense conflicts and compromises and the resolution of the transference neurosis. To facilitate this, the therapist remains relatively neutral and abstinent so that the intrapsychic origins of the transference are rendered more vivid and so that the patient can—without undue suggestion from the therapist—employ newly acquired insight to relinquish oedipal wishes and strengthen the capacity of the ego to tolerate anxiety and seek adaptive discharge of affect (Eagle, 2011). Interpersonal and object relations theories Although the theoretical extensions of ego psychology paved the way for a twoperson psychoanalysis, other, more radical departures from Freudian classical theory shifted the field toward its contemporary appreciation for real-world interactions between people and their implications for unconscious and conscious mental life. Such developments brought renewed attention to the pathogenic influence of actual traumatic experience—particularly in early parent-child relations—rather than instinct- and fantasy-related conflicts (Freud renounced his original theory of sexual abuse as the origin of hysteria) and introduced a broader and more pluralistic conceptualization of therapeutic action (Greenberg & Mitchell, 1983). Several analysts were inspired to modify or reject aspects of Freudian theory through their observations of more troubled patients, for whom traditional interpretation of oedipal transferences seemed ineffective. Melanie Klein was particularly influential in contributing to what became known as British object relations theory (the term object unfortunately was retained to refer to people toward whom wishes are directed). Klein (1946) retained the classical focus on endogenous drives, emphasizing aggressive wishes and the anxieties they evoke. However, she positioned the oedipal situation much earlier in the infant’s development, portraying infants as seething with oscillations of contentment/deprivation and love/hate. The infant projects these affects onto—fantasying them to reside within—parental objects (whose actual qualities Klein minimized) and thus experiences the mother as either a “good breast” or a “bad breast.” In this way, defense is used very early on by the infant to deal with primitive anxieties related to wishes to possess or destroy the parental object. This primitive cauldron of affect developmentally resolves into an easing of extreme wishes, the capacity for guilt over aggressive urges, and tolerance of coexisting positive and negative affects; psychopathology reflects relative deficiency in such development. While Klein’s theory itself did not radically move psychoanalysis toward relational models, her elaboration of the infant’s defensive 8 Contemporary Psychodynamic Psychotherapy splitting of the psyche to reflect internal objects—aspects of the mind identified with caregivers—influenced subsequent theorists’ work and drew attention to early infancy, and her concept of projective identification was later reformulated as an interactive process that contributes to mental development (Bion, 1962). Fairbairn (1952) presented a more comprehensive object relations theory that rejected the primacy of instinctual drives and founded the development of the personality upon the establishment of loving and responsive relationships with real figures. Fairbairn suggested that ties with caregivers form the basis of the child’s primary motivation, to be preserved at all costs. Rather than seeing ego splitting as a consequence of the fantasized return of endogenous wishes projected onto objects (as in Klein’s theory), Fairbairn regarded the actual behavior of parents as contributing to the child’s need to manage inevitable—and sometimes extreme and overwhelming—frustrations through introjection and splitting. He developed a complex model, the scope of which we are unable to reproduce here, detailing the splitting of the ego into components representing experiences with early caregivers; these internal object relations shape one’s personality throughout life at a level beyond conscious awareness. Fairbairn suggested that when early relationships are fraught with turmoil or trauma, the child maintains a psychological tie with parental objects by “cleansing” them through the internalization of their overstimulating and rejecting aspects (Grotstein, 1993). One mechanism in this process consists of feeling responsible for frustration or maltreatment; the child can then maintain a relationship with a “good” parent by defensively obscuring frustrating aspects of the relationship—at an extreme, feeling convinced that it is the child who is bad and thus undeserving of love. The “bad objects” that reflect dissatisfying early relations continue to haunt the individual with feelings of shame and badness and are brought to bear on subsequent interpersonal relationships. Indeed, while Fairbairn paid particular attention to patients who managed this bleak situation by withdrawal into fantasy, he regarded restriction of intimate relatedness more generally as a hallmark feature of psychopathology rooted in internalized early experience. Winnicott (1965) also highlighted the crucial role of caregivers’ actual qualities and behaviors in the development of personality and psychopathology. Winnicott’s (1965) concept of the holding environment refers to the quality of environmental provision required for the emergence of the child’s sense of being a person. The caregiver’s adequate “holding” of the infant—metaphorically encompassing sensitivity and responsiveness to the child’s needs—is considered the cornerstone element in helping the infant to feel secure, alive, and integrated. A vital aspect of holding is the mother’s or father’s sense of the infant as a subjective self, involving the parents’ prioritization of the infant’s nascent experience of being a person. This process requires the parents’ tolerance of negative features of infant care and “good-enough” management of the inevitable ruptures in the caregiver-infant relationship (Winnicott, 1965). Otherwise, a deficient holding environment composed of repeated faulty parent-child responsiveness impinges on the child’s natural development. Under these conditions the child’s “true self” retreats, and a compliant “false self” evolves to manage the impinging environment (Winnicott, 1956). This false self protects the more authentic core of the personality, though at the expense Theoretical evolution in psychodynamic psychotherapy 9 of feeling fully alive and capable of creativity and intimacy. Moreover, as in Fairbairn’s theory, the origins of early relational frustrations—the foundation of psychopathology—remain defensively obscured from awareness. Thus object relations theories retain the notion of the dynamic unconscious while positing alternative unconscious content and motivation, at least with regard to psychopathology. Rather than forbidden sexual and aggressive wishes, what are regarded as most threatening—and therefore relegated to the unconscious—are the inimical experiences with early caregivers that thwart the optimal growth of one’s personality. In other words, conflict and compromise represent repressed wishes for contact and responsiveness, kept at bay to reduce anxiety over the danger of losing all object ties and to avoid anticipated further rejections. Sullivan’s (1953) interpersonal theory similarly situated personality development within an interactional field. Sullivan observed fundamental “integrating tendencies” that bring people together throughout the life span. An infant’s cry, for example, yields in the mother a corresponding responsiveness tendency (including biophysical changes). Successful coming together in such scenarios produces positive feelings and, over time, integration of one’s sense of personhood in relation to others’ responses. Imbalanced integrating tendencies (i.e., failed responsiveness) lead to disintegrating experiences, a preponderance of which will flood the self with anxiety. Sullivan (1953) regarded anxiety as a universal threat to interpersonal relations, potentially upending integrating tendencies and contagiously suffusing one or both participants with intolerable dysphoria. Repeated anxiety-ridden interactions throughout development leave lasting negative self-concepts known as “bad me” or “not me” experiences. Thus Sullivan’s interpersonal theory is concerned not only with interactions among people, but also with the internal psychological structures that arise from—and are subsequently reinforced or modified by—interpersonal relations. Sullivan observed the use of “security operations” to manage anxiety. These psychological safety features are functionally similar to defense mechanisms, though protective against perceived interactional and self-representational endangerment rather than against drive derivatives. Security operations may become pathological if entrenched as “illusionary me you patterns” (Bacal & Newman, 1990, p. 34) that reflect characterological distortions of the interpersonal field. These departures from classical theory held profound implications for treatment, in that therapeutic action could be seen to arise from a “corrective emotional experience” (Alexander, 1950) provided through the analyst’s direct action or a “new beginning” (Balint, 1968) in the therapeutic relationship that counters previous traumatic experience. Rather than resolving the transference of oedipal wishes, psychotherapy from Fairbairn’s perspective involves the therapist’s acceptance and interpretation of the patient’s imposed object representations onto the therapist. At the same time, the therapist’s provision of actual concern and interest, as a new good object, helps the patient to reduce the perniciousness of internal bad objects and the restriction of real relatedness (Fairbairn, 1952). Winnicott also suggested that the therapist treating a patient with a “false self-disorder” must expect to provide a holding environment that withstands the transference of earlier frustrations, gradually allowing for the patient’s vulnerable, “true self” to emerge in accordance 10 Contemporary Psychodynamic Psychotherapy with the therapist’s steadfast responsiveness to the patient’s sensitivities and needs. The implications for therapeutic action—involving both transferential and real relatedness with the therapist—afforded by object relations and interpersonal theories is highlighted in Harry Guntrip’s succinct synopsis: To find a good parent at the start is the basis of psychic health. In its lack, to find a genuine ‘good object’ in one’s analyst is both a transference experience and a real life experience. In analysis as in real life, all relationships have a subtly dual nature. All through life we take into ourselves both good and bad figures who either strengthen or disturb us, and it is the same in psychoanalytic therapy: it is the meeting and interacting of two real people in all its complex possibilities (Guntrip, 1975, p. 156). Psychologies of the self and the patient’s subjectivity Interestingly, the evolution of psychoanalytic theories toward a focus on faulty early relationships in pathogenesis corresponded with a greater emphasis on conceptualizing the self. Interpersonal and object relations theories placed the seeking of connectedness with others and the experience of being recognized and responded to at the center of motivation and the development of a subjective self. Heinz Kohut, initially formulating a conceptualization of narcissistic personality disorder, articulated a psychoanalytic psychology of the self in which the cohesiveness and strivings of the self—the central organization of subjective experience—are themselves principal sources of motivation. According to Kohut’s self psychology, a healthy and cohesive self is developed through repeated experiences of empathic responses from caregivers (Kohut & Wolf, 1978; Kohut, 1971). Empathic responses from others contribute to a greater sense of cohesion and vitality of the self; such responses are referred to as selfobject experiences. An individual functions as a selfobject to the extent to which his or her “presence or activity evoke and maintain the self and the experience of selfhood” (Wolf, 1988, p. 184). Early childhood (or “archaic”) responses to selfobject needs, such as the need to be mirrored and prized by a parent or the need to merge with an admired parent, are thought to be experienced subjectively as aspects of the self. When such responses on the whole are appropriate, selfobject needs become less urgent and more differentiated as development advances, and their expression changes according to maturational themes. Moreover, while selfobject responses are required throughout the life span, their internalization into the structure of the self reduces the urgency with which other people’s responses are required for self-cohesion. Because selfobject experiences are essential for the self’s robustness and vitality, their absence or chronic frustration pave the way for dysfunction and disorder of the self. Kohut (1971, 1984) wrote extensively on the fragmentation of the self as a painful subjective experience of deficiency, shame, and weakness. Individuals with a fragmentation-prone self may develop maladaptive strategies such as Theoretical evolution in psychodynamic psychotherapy 11 self-aggrandizement, impulsive behavior, and superficial admiration seeking to bolster a fragile self, forestall fragmentation, and compensate for unmet selfobject needs. Indeed, unmet archaic selfobject needs do not merely evaporate and may be vigorously pursued in maladaptive ways that represent significant psychopathology (Kohut & Wolf, 1978). At the same time, such needs—and the sense of deficiency and shame attending them—may be repressed via a range of pathological attitudes and behaviors, further reducing opportunities for more mature self-selfobject relations. The priority in a self psychological treatment is the patient’s experience of the therapist’s sustained empathic responsiveness. Although the therapist interpretively explains the patient’s transference experience of unmet selfobject needs, the therapist’s acceptance of performing a role as a selfobject to the patient is of critical importance. To give an oversimplified example, some patients with archaic selfobject deficiencies may gain little from interpretive interventions when in states of experiencing the therapist as a needed mirroring selfobject, while others may draw self-cohesion through idealized perceptions of the therapist. Indeed, in such instances, interpretations or other behaviors on the part of the therapist could— from the patient’s subjective perspective—disrupt the selfobject experience obtained through the therapeutic relationship and utilized by the patient to restore and strengthen the self. Disruptions in the self-selfobject relationship are of special importance in self psychology. Kohut considered the inevitable ruptures and frustrations in therapy (as paralleled in child development) to be opportunities for “optimal frustration” that contribute—in the context of an overall empathically responsive milieu—to the patient’s gradual internalization of selfobject functions (Gehrie, 2011). In other words, optimal frustration contributes to the eventual strengthening of a fragile or arrested self, though what may be most crucial in such instances is the therapist’s empathic attunement to the patient’s subjective experience of the rupture, privileging this over an attempt to discern the objective “truth” of what occurred (Bacal & Newman, 1990; Eagle, 2011). In this way, the therapist demonstrates an effort to understand the patient’s subjectivity—the experience of which, for the patient, contributes to the building of new self-structure. In other words, the empathic understanding and repair of a therapeutic rupture may be a heightened form of selfobject experience that can be internalized by the patient. Bacal (1998) elaborated other possibilities for selfobject “optimal responsiveness” to occur in therapy, beyond those surrounding frustration experiences. Through placing the subjectivity of the patient—and the legitimacy of the patient’s need to feel understood—at the very center of therapeutic focus, self psychology expands the range of potentially therapeutic responses. Depending on the patient’s experience, optimal responsiveness may thus take various forms: It may entail an inquiring attitude or a quiet noninquiring presence, an echoing confirmation, or a confrontational challenge. Its form will be determined not only by the issues that the patient and the analyst are working on but also by the strength of the patient’s self, and by the patient’s operative level of developmental achievement (Bacal, 1994, p. 27). 12 Contemporary Psychodynamic Psychotherapy In this way, psychotherapy—at least for patients with disorders of the self—is less of an exercise in unearthing relics from the patient’s unconscious and more of a developmental experience in which new modes of functioning are evoked through the therapist’s understanding and responsiveness (Emde, 1990). The contributions of control-mastery theory further emphasize the patient’s subjectivity in determining the therapeutic value of interventions and highlight the patient’s active role in seeking corrective experiences in the therapy relationship. From the control-mastery perspective formulated by Weiss (1993), patients seek to address pathogenic beliefs—grim beliefs that severely constrict the self—in a variety of ways. As in other object relations theories, pathogenic beliefs about the self and others are viewed in control-mastery theory as forming largely in response to (and serving to maintain) dysfunctional early relationships with caregivers. In therapy, patients may actively test these beliefs directly with the therapist; the therapist’s responses to such tests provide an indication of whether the patient can begin to relinquish the beliefs or not. For example, a patient may unconsciously invite the therapist to become overly directive and authoritative, as the patient experienced her parents, to test the belief that the patient is not capable of thinking for herself or entitled to lead the way. The therapist could address this through interpretation but also through refusing to direct the session and by gently encouraging the patient’s self-determination. Conversely, a patient who was traumatized by neglect may experience the therapist’s unobtrusiveness as an attenuated form of neglect—perhaps confirming the patient’s belief that she is uninteresting or undeserving—and might instead benefit from the therapist adopting a more directive stance. Through testing, the patient takes an active approach to seeking corrective experiences from the therapist, who ideally has enough understanding of the patient’s therapeutic needs and goals to “pass” these tests with individually tailored responses. In line with the concept of optimal responsiveness, a variety of potential responses—including interpretations, attitudes, and relational responses—have the potential to disconfirm the patient’s pathogenic beliefs; the therapeutic value of the therapist’s responses lies in their meaning to the individual patient rather than in a priori notions of correct technique (Weiss, 1993). The therapist who fosters therapeutic progress thus does so by consistently responding with the patient’s unique subjectivity in mind. Having one’s mind in mind is an important aspect of mentalizing, conceptualized as the capacity to think about and reflect upon underlying mental states and motivations in both oneself and others (Allen, Fonagy, & Bateman, 2008). Mentalizing, or mentalization, has been a focus of contemporary attachment theory in explaining the development of affect regulation, subjectivity, and interpersonal abilities. Like other object relations theories, attachment theory—initiated by the work of British psychoanalyst John Bowlby—emphasizes the early parent-child bond in providing affect-regulatory functions for the child and as a primary source of learning about the self, others, and interpersonal relatedness. Internal working models of self and others—conceptually similar to internal object relations—are formed through a matrix of attachment interactions, including the child’s use of the attachment figure as a secure base from which to explore and a safe haven to seek comfort Theoretical evolution in psychodynamic psychotherapy 13 from when distressed (Bowlby, 1988). These inner templates typically correspond to identifiable patterns of attachment—attachment styles—characterized by relatively secure or insecure attachment tendencies. In addition to informing psychodynamic therapy, attachment theory is widely embraced and well researched within many branches of psychology (and therefore our brief discussion of attachment is exceedingly cursory); an example of its application to family therapy is provided in Chapter 24. In addition to shaping the individual’s attachment style, early attachment relationships provide a crucible for the development of mentalizing abilities. The capacity to interpret behaviors and attitudes in terms of underlying mental states and to recognize that others’ mental states differ from one’s own is advantageous for both self-regulatory functions and for interactions with others (Fonagy, Gergely, Jurist, & Target, 2002). Whereas secure attachment relationships promote mentalizing through the child’s psychological experiences being consistently reflected and represented by attachment figures, insecure attachments tend to involve faulty or inconsistent attention to the child’s emotional states. Moreover, a traumatized child may become defensively disinclined to mentalize, given the distress that may be evoked in reflecting upon the intentions of an abusive attachment figure. A mentalization framework applied to psychotherapy pays particular attention to limitations in the patient’s capacity to mentalize (Allen et al., 2008). Nonmentalizing modes of functioning are seldom absolute; people shift into and out of them, often in response to perceived threats. Impaired mentalizing tends, however, to be more prominent among patients with personality disorders, for which a specific mentalization-based treatment has been developed. We leave further discussion of mentalizing in psychotherapy to Chapter 3, “Attachment and Mentalization in Contemporary Psychodynamic Psychotherapy”, and of mentalization-based treatment for personality disorders to Chapter 9, “Mentalization-based treatment for borderline and antisocial personality disorder”. Overall, contributions from a contemporary attachment framework have focused attention on mentalizing as both a process and an outcome of psychotherapy (Allen et al., 2008). In other words, while the achievement of more robust mentalizing abilities may be a major goal of psychodynamic therapy, mentalizing in the therapy itself is regarded as a primary mechanism by which this may be achieved. From this perspective, psychodynamic therapy may constitute a kind of skill development, consisting of repeated, consistent efforts to reflect on mental states. Indeed, transference-focused psychotherapy has been found to contribute to improved reflective functioning and attachment status, perhaps owing to its intensive focus on the patterns of relations between patient and therapist (Levy et al., 2006). Based on Kernberg’s (1984) influential object relations model of personality disorder—emphasizing levels of personality functioning and sophistication of defenses—transference-focused psychotherapy involves the therapist’s collaborative inquiry with the patient regarding disavowed experiences of self and other. This process, sometimes turbulent and characterized by strong expressions of affect or enactment, requires the therapist’s careful attention to the patient’s subjectivity, including attention to unconscious aspects that may be projected or split 14 Contemporary Psychodynamic Psychotherapy off and experienced primarily through the therapist’s countertransference responses. Consistent attention to the patient’s shifting emotional and interpersonal experience—while holding the patient’s mind in mind—is thus theorized to result in the patient’s ability to integrate discordant and/or intolerable emotional experiences, reduction of primitive defenses, and enhanced mentalizing. Further description of transference focused therapy is provided in Chapter 10, “Transference-focused psychotherapy for borderline and narcissistic personality disorders”. Contemporary integration The evolution of psychodynamic theory and its application to clinical practice over the past century have provided fertile ground for innovation and integration. Indeed, the developments we have described are in themselves integrative efforts involving shifts of emphasis, conceptual amendments, and the addition of new perspectives. While the most dramatic shift in psychoanalytic theory has been the movement away from the mediation of sexual drive pressure as fundamental to personality and psychopathology toward an emphasis on interpersonal relations in contributing to mental structure, the notion of drives—at least in terms of basic motivations and affects—has hardly been discarded. Rather, a broader array of basic motivations has been recognized and integrated with contemporary psychoanalytic theories of affects, attachment, and self-regulation (Fonagy et al., 2002; Lichtenberg, 1989). Similarly, an earlier emphasis on ego defenses has not been supplanted by relational theories but has been integrated into contemporary recognition of the self’s need to protect against an array of threatening phenomena, such as traumatic memories, painful affects, and intolerable self-states (see Chapter 20: for a discussion of dissociation). The result of such development is a contemporary psychodynamic theory—or a body of multiple, related theories—characterized by the recognition that no one model is comprehensive enough to explain all minds, all psychopathologies, and all therapeutic endeavors. Different points of emphasis across models contribute nuance to common-ground concepts such as transference and countertransference and may be of use to therapists as alternative vantage points from which to view complex clinical phenomena. For example, interaction structures (Jones, 2000), which are unconsciously enacted and often repetitive interactions between patient and therapist, are widely acknowledged as important events for clinical attention. Different conceptual paradigms can help the clinician contemplate the degree to which a particular enactment reflects an activation of primitive affect-tinged internal object relations (Kernberg, 2011), therapist countertransference or miscommunication (Jacobs, 2001), a testing of pathogenic beliefs (Weiss, 1993), or an aspect of the ongoing mutual negotiation of the therapeutic alliance (Safran & Muran, 2000). Many of the major questions with which the field has historically grappled have more or less resolved into an acceptance that different points of view are necessary Theoretical evolution in psychodynamic psychotherapy 15 to encompass the complexity of human experience and the complicated nature of the therapeutic process. For example, rather than debating whether conflict or deficit is central to psychopathology, it is possible to legitimately view both as important considerations in developing a clinical formulation for a given patient. Similarly, the debate over whether therapeutic action rests on the promotion of insight or through corrective properties of the therapeutic relationship has largely been settled with the recognition of multiple pathways to change in psychotherapy (Gabbard & Westen, 2003). Moreover, these mechanisms likely interact in a synergistic manner (Eagle, 2011; Gabbard, 2017). As patients feel safer and understood in the therapy relationship, they may become less defensive and capable of greater self-knowledge. Likewise, developing insight into interpersonal patterns in the therapy relationship may in itself constitute a corrective experience that opens new developmental possibilities. The theoretical undergirding of psychodynamic psychotherapy continues to evolve. One of the most exciting developments in this process of evolution has been the relatively recent testing of psychoanalytic constructs (see Chapter 6: Research support for psychodynamic constructs), psychodynamic models of therapy (see Chapter 4: The efficacy of psychodynamic psychotherapy: an up-to-date review), and mechanisms of action (see Chapter 5: Process Research in psychodynamic psychotherapy: interventions and the therapeutic relationship) through empirical research. Such work will likely continue to refine the ways in which clinicians understand and address the difficulties faced by their patients—and maintain the status of psychodynamic theory and therapy as an organic and progressive field. References Alexander, F. (1950). Analysis of the therapeutic factors in psychoanalytic treatment. Psychoanalytic Quarterly, 19, 482 500. Allen, J. G., Fonagy, P., & Bateman, A. W. (2008). Mentalizing in clinical practice. Arlington, VA: American Psychiatric Publishing. Bacal, H. A. (1994). The selfobject relationship in psychoanalytic treatment. In A. Goldberg (Ed.), Progress in self psychology (Vol. 10, pp. 21 30). Hillsdale, NJ: Analytic Press. Bacal, H. A. (1998). Optimal responsiveness and the therapeutic process. In H. A. Bacal (Ed.), Self psychology and intersubjectivity. Optimal responsiveness: How therapists heal their patients (pp. 3 34). Lanham, MD: Jason Aronson. Bacal, H. A., & Newman, K. M. (1990). Theories of object relations: Bridges to self psychology. New York, NY: Columbia University Press. Balint, M. (1968). The basic fault: Therapeutic aspects of regression. London: Tavistock. Bion, W. R. (1962). Learning from experience. Northvale, NJ: Jason Aronson. Bowlby, J. (1988). A secure base. London, UK: Routledge. Eagle, M. N. (2011). From classical to contemporary psychoanalysis: A critique and integration. New York, NY: Routledge. Emde, R. N. (1990). Mobilizing fundamental modes of development: Empathic availability and therapeutic action. Journal of the American Psychoanalytic Association, 38, 881 913. 16 Contemporary Psychodynamic Psychotherapy Erikson, E. H. (1959). Identity and the life cycle: Selected papers. Oxford, UK: International Universities Press. Fairbairn, W. R. D. (1952). Psychoanalytic studies of the personality. London, UK: Routledge. Fonagy, P. (2001). Attachment theory and psychoanalysis. New York, NY: Other Press. Fonagy, P., Gergely, G., Jurist, E. L., & Target, M. (2002). Affect regulation, mentalization, and the development of the self. New York, NY: Other Press. Freud, A. (1966). The ego and the mechanisms of defense. New York, NY: International Universities Press. Freud, S. (1923). The ego and the id. In J. Strachey (Ed. & Trans.) The standard edition of the complete psychological works of Sigmund Freud (vol. 19, pp. 12 66). London, UK: Hogarth Press. Freud, S. (1920/1966). Introductory lectures on psychoanalysis (J. Strachey, Trans.). New York, NY: W. W. Norton. Gabbard, G. O. (2017). Long-term psychodynamic psychotherapy: A basic text (3rd ed.). Arlington, VA: American Psychiatric Publishing. Gabbard, G. O., & Westen, D. (2003). Rethinking therapeutic action. International Journal of Psychoanalysis, 84, 823 841. Gehrie, M. J. (2011). From archaic narcissism to empathy for the self: The evolution of new capacities in psychoanalysis. Journal of the American Psychoanalytic Association, 59, 331 333. Greenberg, J. R., & Mitchell, S. A. (1983). Object relations in psychoanalytic theory. Cambridge, MA: Harvard University Press. Grotstein, J. S. (1993). A reappraisal of W. R. D. Fairbairn. Bulletin of the Menninger Clinic, 57, 421 449. Guntrip, H. (1975). My experience of analysis with Fairbairn and Winnicott: How complete a result does psycho-analytic therapy achieve. International Review of Psycho-Analysis, 2, 145 156. Hartmann, H. (1958). Ego psychology and the problem of adaptation. New York, NY: International Universities Press. Jacobs, T. J. (2001). On misreading and misleading patients: some reflections on communications, miscommunications and countertransference enactments. International Journal of Psychoanalysis, 82, 653 669. Jones, E. E. (2000). Therapeutic action: A guide to psychoanalytic therapy. Northvale, NJ: Jason Aronson. Kernberg, O. F. (1984). Severe personality disorders: Psychotherapeutic strategies. New Haven, CT: Yale University Press. Kernberg, O. F. (2011). Divergent contemporary trends in psychoanalytic theory. Psychoanalytic Review, 98, 633 664. Klein, M. H. (1946). Notes on some schizoid mechanisms. International Journal of Psychoanalysis, 27, 99 110. Kohut, H. (1971). The analysis of the self. New York, NY: International Universities Press. Kohut, H. (1984). How does analysis cure? Chicago, IL: University of Chicago Press. Kohut, H. A., & Wolf, E. S. (1978). The disorders of the self and their treatment: An outline. International Journal of Psychoanalysis, 59, 413 425. Levy, K. N., Meehan, K. B., Kelly, K. M., Reynoso, J. S., Weber, M., Clarkin, J. F., & Kernberg, O. F. (2006). Change in attachment patterns and reflective function in a randomized control trial of transference focused psychotherapy for borderline personality disorder. Journal of Consulting and Clinical Psychology, 74, 1027 1040. Theoretical evolution in psychodynamic psychotherapy 17 Lichtenberg, J. D. (1989). Psychoanalysis and motivation. Hillsdale, NJ: Analytic Press. Ogden, T. H. (2002). A new reading of the origins of object-relations theory. International Journal of Psychoanalysis, 83, 767 782. Safran, J., & Muran, J. C. (2000). Negotiating the therapeutic alliance: A relational treatment guide. New York, NY: Guilford Press. Sullivan, H. S. (1953). The interpersonal theory of psychiatry. New York, NY: Norton. Wampold, B. E. (2010). The basics of psychotherapy: An introduction to theory and practice. Washington, DC: American Psychological Association. Winnicott, D. W. (1956). On transference. International Journal of Psychoanalysis, 37, 386 388. Winnicott, D. W. (1965). The maturational processes and the facilitating environment: Studies in the theory of emotional development. London, UK: Hogarth Press. Weiss, J. (1993). How psychotherapy works: Process and technique. New York, NY: Guilford. Wolf, E. S. (1988). Treating the self: Elements of clinical self psychology. New York, NY: Guilford Press. Working with cyclical relational patterns in contemporary psychodynamic psychotherapy 2 Mark J. Hilsenroth1 and Seth R. Pitman2 1 Derner School of Psychology, Adelphi University, New York, NY, United States, 2Austen Riggs Center, Stockbridge, MA, United States The active exploration of patients’ cyclical relational patterns is a central focus of psychodynamic psychotherapy. Ideas about the role these patterns play in patients’ lives, within the therapeutic relationship, and in the therapeutic change process have evolved over the years, along with developments in psychodynamic theory and advancing empirical evidence. Today, psychodynamic clinicians can take various approaches to working with cyclical relational patterns, depending on the nature of the patient’s problems, therapist and patient variables, as well as the specific therapeutic approach being employed. Within psychodynamic schools there has been a movement away from the relatively constrained approach of interpreting patients’ transference toward the more descriptive and experience near processing of in-session, here-and-now content. In this chapter we trace the evolution of new and emerging ways of working with patients’ cyclical relational patterns, and we provide relevant evidence as well as clinical applications. Transference and its interpretation The significance of working in the therapeutic relationship was first recognized by Freud (1916) in his development of the concept of transference, an intrapsychic phenomenon based on fantasy wherein patients ascribe to the therapist qualities based on previous relational experiences with important figures from the patient’s past. Freud considered transferences to be haunting specters of the past that were “something analogous [to], but immeasurably more important” than the circumstances of the present (1905/1953, p. 109). Central to Freud’s original conceptualization is the understanding that the patient’s transferential response to the therapist is inherently unrealistic. Therefore he suggested (1917/1963) that “We overcome the transference by pointing out to the patient that his feelings do not arise from the present situation and do not apply to the person of the doctor” (pp. 443 444, emphasis added). While psychodynamic psychotherapy continues to emphasize the importance of transference, to date there is little empirical evidence to support the Contemporary Psychodynamic Psychotherapy. DOI: https://doi.org/10.1016/B978-0-12-813373-6.00002-7 © 2019 Elsevier Inc. All rights reserved. 20 Contemporary Psychodynamic Psychotherapy assertion that transference manifestations reflect a highly unrealistic perspective of the therapeutic relationship seen “through a glass, darkly.” In parallel to this issue, more recent psychoanalytic authors have suggested that the transference concept should include additional aspects of the interaction between the therapist and the client that also take into account the contribution of the therapist (Ehrenreich, 1989; Gabbard, 2000; Gill, 1984; Høglend & Gabbard, 2012). While transference research has demonstrated that it can be reliably operationalized and assessed through careful observation, the way in which it plays out in the therapy process and how it reflects and diverges from patients’ problematic, characteristic relational patterns are less straightforward. Researchers have attempted to operationalize the construct of transference from a variety of perspectives and using several working definitions. Gelso, Hill, Mohr, Rochlen, and Zack (1999) distinguished two models of transference measurement within the therapeutic relationship: direct measurement (in which in-session patient reactions and emotions are assessed as explicitly unrealistic to the treatment situation) or indirect measurement (assessing patients’ common relational patterns and affects as they arise in treatment but without inferring the justification of such reactions). One direct measure of transference, The Missouri Identifying Transference Scale (MITS) (Multon, Patton, & Kivlighan, 1996), asks therapists to rate adjectives describing their patients’ extreme and unrealistic emotional or behavioral reactions. Initial validation of the MITS found partial supporting evidence that the client’s self-reported view of his or her mother (but not father) was significantly related to counseloridentified transference reactions. This finding was later replicated by Woodhouse, Schlosser, Crook, Ligiéro, and Gelso (2003), as therapists observed more negative transference reactions in clients who had perceived their maternal care as cold and rejecting. Multon et al.’s (1996) results also suggested some direct linkage between a client’s in-session reactions and his or her negative perceptions of the counselor. When the client perceived his or her therapist to be more controlling and less sociable, the counselor observed more negative transference reactions in the client. Without the addition of independent observer ratings of the therapeutic process, it is difficult to formulate whether these negative transference reactions were based on the clients’ unrealistic misinterpretations of the counselor or their realistic assessment of a counselor’s interactional stance. Overall ratings of negative transference were low, and only counselors’ ratings of positive transference were significantly related to their perceptions of the overall “amount” of transference occurring in a session. If internal distortions of relational interactions (epitomized by the distortion of the patient therapist relationship) are theorized to be at the core of the problems that bring patients to treatment, one would reasonably expect the bulk of transference reactions to be negative, particularly early in the therapeutic encounter. Similarly, a number of authors have used Graff and Luborsky’s (1977) singleitem measurements of positive, negative, and amount of transference as observed by therapist raters. While these ratings have exhibited modest psychometric qualities, converging with Multon and colleagues’ positive and negative transference scales, findings related to the course of transference scores across treatment are inconsistent, with studies suggesting that transference increases throughout Working with cyclical relational patterns in contemporary psychodynamic psychotherapy 21 successful psychoanalytic work (Graff & Luborsky, 1977; Patton & Kivlighan, 1997) but diminishes in the latter part of successful nonanalytic or theoretically heterogeneous treatment (Gelso, Kivlighan, Wine, Jones, & Friedman, 1997). Finally, despite the fact that these transference measurement instruments are explicitly designed to assess unrealistic and extreme relational reactions, they do not evidence consistently significant inverse relationships with client and therapist ratings of genuineness and realism in the therapeutic relationship (Gelso, 2002; Marmarosh et al., 2009). In addition to this attempt to operationalize the concept of transference, psychotherapy researchers have attempted to isolate and examine the impact of transference interpretation as a therapeutic technique. Because a therapeutic interpretation can be conceptualized as the explicit linking of implicit patterns and because transference manifests itself through the intersection of internal states and external experiences, three main transference interpretation “routes” are possible. Interpretations can be made that establish links to past figures (genetic interpretations), current relationships outside of psychotherapy (extratransference interpretations), and/or the patient therapist interaction (transference interpretation) (Høglend & Gabbard, 2012; Malan, 1979; McCullough et al., 2003). In 1999 Bøgwald, Høglend, and Sorbye (1999) first reported on the specific therapeutic technique (STT) scale (Høglend, 1994), a brief and efficient psychotherapy process scale for measuring the frequency of therapist interventions that address the patienttherapist interaction and transference phenomena. Only one aspect of the STT scale relates to genetic transference interpretations as traditionally understood (i.e., therapist attempts to explore interpersonal repetitive patterns with important others and/or parents and link these patterns to transactions between the patient and therapist). The remaining elements focus more exclusively on the patient therapist relationship (e.g., “therapist addresses transactions in the patient therapist relationship,” “therapist actively encourages the patient to explore thoughts and feelings about the therapist, therapy, and/or the patient therapist relationship,” and “therapist encourages the patient to discuss how the therapist might feel or think about the patient”). The conventional clinical wisdom has been that patients with greater psychological resources and more mature relationships will benefit from the depth and complexity of transference interpretation (Gabbard, 2006; Sifneos, 1992). However, several studies have demonstrated that the interactions among patient quality of object relations (QOR), exploration of the treatment relationship (under the purview of transference interpretations as measured by the STT scale; Høglend, 1994), and outcome are mixed and difficult to interpret. For instance two studies have demonstrated that a greater number of transference interpretations have led to negative outcome effects for patients with high QOR (Høglend, 1993; Piper et al., 1991), whereas two studies have found positive or equivalent effects for patients with high QOR (Connolly et al., 1999; Ogrodniczuk, Piper, Joyce, & McCallum, 1999). These studies have discussed this discrepancy in terms of the frequency of transference interpretations, with the former studies having high levels per session (i.e., five to six) and the latter studies utilizing low to moderate levels per session 22 Contemporary Psychodynamic Psychotherapy (i.e., one to four) (Høglend, 1993; Piper, Ogrodniczuk, & Joyce, 2004). Most recently, in an experimental study, patients with high QOR benefited equally from treatments with and without transference interpretations, whereas patients with low QOR benefited more from treatment that included transference interpretations, an effect that was sustained during long-term follow-up (Høglend et al., 2006; Høglend et al., 2008; Høglend, Johansson, Marble, Bøgwald, & Amlo, 2007). As prior empirical studies have traditionally examined the frequency and not necessarily the competence in delivery of transference interpretations, the mixed results described above may suggest that treatments containing higher degrees of transference interpretation could reflect therapists’ attempts to force interpretive elements or inaccurate conceptualizations that simply do not fit the situation. Therapeutic wrong turns, miscues, and case corrections are an inevitable part of treatment, but interpretive work raises a unique hazard: patients who rightfully reject or dismiss inaccurate interpretations may be viewed as “resistant” or “defensive,” leading some therapists to increase their interpretive stance. According to Høglend and Gabbard (2012), “it seems fair to conclude that clinicians should be aware that a high dosage level of transference interpretations (on average four to six or more per session) does not seem to overcome patient resistance and defensiveness and may in fact contribute to a negative therapeutic process” (p. 454). These results are also consistent with emerging data that suggest that an in-session focus on the therapeutic relationship is most effective when the alliance has been found to be high (Ryum, Stiles, Svartberg, & McCullough, 2010; Schut et al., 2005). Based on the evidence reviewed above, transference interpretations are most likely not the only or even the primary mechanism of change in psychodynamic psychotherapy. The effectiveness of transference interpretation as a therapeutic technique is not yet well established and appears to be variable, depending on various clinical and research definitions of this phenomena, patient characteristics such as QOR or insight and the context of the therapeutic relationship (i.e., therapeutic alliance). A contemporary, empirically informed conceptualization of transference phenomena supports the view of the therapeutic relationship as a unique and novel relational experience, influenced by personality styles rooted in developmental history but not simply a distortion based on interactions from the past. Working with cyclical relational patterns in the here-andnow: therapeutic immediacy Discussion of these research findings is not to suggest that patients enter psychotherapy as a relational tabula rasa. Individuals do exhibit characteristic patterns of thinking and relating with others, which can be observable and stable across relational contexts, including psychotherapy. Luborsky (1977; Luborsky & Crits-Christoph, 1998) classified these relational templates as core conflictual relationship themes (CCRTs), composed of three elements: interpersonal wishes, real Working with cyclical relational patterns in contemporary psychodynamic psychotherapy 23 or fantasized responses of others, and responses of self. The CCRT scales show satisfactory internal consistency and can be reliably scored by independent raters. Patients’ common CCRT patterns with significant others in their lives are to some degree related to similar interaction components that emerge with the therapist across psychotherapy interactions (Barber, Foltz, DeRubeis, & Landis, 2002). Contemporary psychodynamic theorists view the therapeutic relationship not only as an important foundation for the therapeutic work, but also as one of the core mechanisms in the change process itself, that is, via exploration of the hereand-now in-session process (Strupp & Binder, 1984). This includes exploring patients’ thoughts and feelings about interactions within the treatment relationship, engaged by the therapist from a dyadic and relational perspective (Cooper, 1987; Safran & Muran, 2000; Wachtel, 1993, 2008) and without directly linking this exploration to a past relationship (as in the more traditional intrapsychic distortion perspective). The difference between these theoretical perspectives—one focused primarily on the here-and-now and one focused on distortions from past relationships—is an important distinction that often muddies the water in research on insession patient therapist interactions. To overcome the definitional ambiguity of these perspectives, Hill et al. (2008) made a distinction between transference interpretations and what she referred to as therapist immediacy (“disclosure within the therapy session of how the therapist is feeling about the client, him or herself in relation to the client, or about the therapeutic relationship”, p. 298 ). She suggested that a focus on the therapeutic relationship can be used to address relationship problems in general, discuss issues of importance specific to the therapeutic relationship, challenge patients to recognize maladaptive patterns, make covert communication in the session more direct, provide the patient with feedback, and provide the patient with a model of how to resolve interpersonal problems. In order to capture the more interactive and dyadic nature of the therapeutic relationship, this definition has recently been broadened to also reflect any clientinitiated disclosures of feelings about the therapist or the client therapist relationship. Kuutmann and Hilsenroth (2012) suggested the revised term therapeutic immediacy, which involves any discussion within the therapy session about the relationship between therapist and patient that occurs in the here-and-now as well as processing what occurs in the here-and-now client therapist relationship. Typical examples of therapeutic immediacy include (1) exploring parallels of how interpersonal and affective themes covered in other relationships during a session might be expressed or occur in the therapeutic relationship; (2) expressing an immediate insession affect or association regarding the therapeutic relationship or treatment process; (3) one member of the therapeutic relationship (client or therapist) being asked to take the perspective (thoughts or feelings) of the other; (4) one or both parties asking to reflect on or process what is happening in the immediate therapeutic interaction or feeling in the room; (5) exploring emotional experiences in the relationship that might have been avoided or gone unrecognized; (6) addressing a rupture event; (7) recognizing adaptive changes in functioning that occur in relation to the therapeutic relationship or treatment process; (8) explicitly supporting, affirming, 24 Contemporary Psychodynamic Psychotherapy and validating engagement, involvement, or greater experiencing in the therapeutic relationship or treatment process; and (9) processing the termination of the therapeutic relationship. Thus therapeutic immediacy seeks to create a corrective emotional-relational experience for the patient by focusing on here-and-now awareness. This approach stands in contrast to the use of transference interpretations in order to help the patient discover and understand the origin of the previous, displaced maladaptive interactional patterns enacted during the session. The benefits of immediacy have been studied by using both quantitative and qualitative methods in three recent case studies of experienced therapists from psychodynamic and interpersonal orientations (Hill et al., 2008; Kasper, Hill, & Kivlighan, 2008; Mayotte-Blum et al., 2012). While the amount of immediacy varied between cases, immediacy was seen across each study as promoting client emotional awareness or insight, helping to resolve problems in the therapeutic relationship, facilitating a correlative relational experience, and providing a model for resolving relationship problems outside therapy. Studies have also suggested that certain patient factors might influence how therapists use immediacy and its effect on treatment. For instance Kuutmann and Hilsenroth (2012) found that higher levels of pretreatment personality pathology and interpersonal problems were positively correlated with a greater focus on the patient therapist relationship early in treatment. This was especially true for patients with a cold/distant interpersonal style and low self-esteem. Moreover, these two patient pretreatment characteristics demonstrated a significant change over the course of therapy, and the amount of change in these specific patient characteristics (cold/distant interpersonal style and low self-esteem) was significantly related to greater early treatment focus on the patient therapist relationship. That is, the pretreatment patient characteristics subsequently related to early session focus on patient therapist interactions later demonstrated change over the course of therapy that was related to the use of more of this same intervention. In addition, the results from this study found that an interaction effect between QOR (i.e., higher levels of object relations) and greater early treatment focus on the patient therapist relationship positively affected subsequent changes in patients’ cold/distant interpersonal problems. The focus on the therapeutic relationship variable used in the study was much broader than the specific focus on transference interpretations and encompassed any in-session discussion of the patient therapist interaction, that is, the nine therapeutic immediacy examples listed earlier, regardless of whether these were interpretive. Finally, research has also focused on the effects of one aspect of therapeutic immediacy: therapist self-disclosure of intrasession or extrasession content. Proponents of therapist self-disclosure sprang from the person-centered tradition as originated by Rogers, who emphasized the importance of the therapist’s modeling openness, strength, and vulnerability in nurturing a trusting and empathic therapeutic relationship. This more open stance stands in contrast to traditional psychoanalytic concerns related the potential negative impact of therapist disclosure on the therapy process, notably cautioned by Freud’s likening of the therapist to a “blank screen” (1912/1958). Therapist self-disclosure has been empirically examined on a number of matrices, including the emotional quality of the disclosure (positive or Working with cyclical relational patterns in contemporary psychodynamic psychotherapy 25 negative content valence), whether the information disclosed reveals similarity or dissimilarity to the client, and whether the disclosure pertains to content occurring during the session (intrasession; e.g., “I feel uncharacteristically tense during our session today”; “I admire how hard you are working at this right now”) or outside of the therapy context (extrasession; e.g., “I’ve been to that place too”; “I know what it’s like to lose someone you love”). Intrasession therapist self-disclosure overlaps with a number of other similar constructs, including (but not limited to) countertransference disclosures (Myers & Hayes, 2006) and therapeutic immediacy. A recent randomized controlled trial studied the impact of therapist selfdisclosure on distress symptoms within a form of brief integrative therapy that included a psychodynamic focus on insight (Ziv-Beiman, Keinan, Livneh, Malone, & Shahar, 2016), using three control conditions. The authors found that integrative psychotherapy augmented by immediate (intrasession) therapist self-disclosure was more successful in reducing psychiatric symptoms among actively symptomatic patients than were no self-disclosure and nonimmediate (extrasession) selfdisclosure conditions. Therapists in the immediate self-disclosure group were also viewed more favorably than those in the nonself-disclosure group. The authors suggested that these findings are in line with previous research indicating that highly distressed patients find greater benefit from a more supportive, reassuring therapist stance, as represented by therapist self-disclosure, and that use of immediacy may help facilitate the resolution of treatment ruptures and contribute to a corrective relational experience (CRE) (Hill et al., 2008; Kasper et al., 2008; Mayotte-Blum et al., 2012). Therapeutic immediacy in relation to treatment ruptures and corrective emotional-relational experiences One area in which a focus on the therapeutic relationship is particularly important is regarding treatment ruptures (Hill et al., 2008; Muran et al., 2009). For instance, an early study in this area by Rhodes, Hill, Thompson, and Elliot (1994) found focus on the therapeutic relationship to be an important factor in the resolution of patient reports of ruptures with the therapist. Therefore identifying and disseminating strategies for solving treatment ruptures are important for improving effectiveness in psychotherapy. Further developing this idea, Safran and Muran (2000) proposed two stage-process models for how to resolve ruptures in the therapeutic alliance, in which a focus on the therapeutic relationship plays a figural role in the eventual resolution of these ruptures. These two models are based on the different rupture subtypes: those representing withdrawal and confrontation. Withdrawal ruptures may occur with overly compliant patients or avoidant patients who have difficulties in expressing their needs in the relationship. Confrontation ruptures are manifested as directly expressed hostility or resentment toward the therapist or the treatment. According to Safran and Muran, the therapist in both withdrawal and confrontation situations easily becomes embedded in the patients’ cyclical relational patterns by responding to the rupture 26 Contemporary Psychodynamic Psychotherapy interactions in a way that reinforces the patients’ feelings and beliefs [expected response of other, or core conflictual relational theme (CCRT), Luborsky, 1984]. To disembed himself or herself from the patient’s enacted cyclical patterns, the therapist needs to direct the patient’s attention to the here-and-now of the therapeutic relationship. Thus a focus on the here-and-now therapeutic relationship is one way to explore the patient’s underlying construal of the interaction and helps the patient to become aware of and, through a corrective emotional-relational experience, change his or her maladaptive interpersonal patterns. In complement to treatment ruptures, Huang, Hill, Strauss, Heyman, and Hussain (2016) found that a majority of patients reported having had a corrective relational experience (CRE) during psychodynamic-interpersonal psychotherapy and that these experiences typically occurred in the context of therapeutic relationships that were seen as primarily positive but not without some difficulties in that process (e.g., reenactments of interpersonal problems). Therapists facilitated CREs by actively identifying patients’ maladaptive interpersonal patterns, both outside of therapy and within the therapeutic relationship, in a manner that conveyed trustworthiness. Corrective relational shifts included the patient understanding himself or herself and the use of therapy in new ways and the patient’s gaining new insight into relational and behavioral patterns. These patients reported that CREs led to a deepening of the therapeutic relationship as well as positive intrapersonal changes, although some patients also reported feeling uncomfortable about changes in their behavioral patterns in particular. We would also note the consistency between several of the interventions described above and the provision of an actively supportive milieu, as well as the rupture-and-repair model of Safran and Muran (2000), involving attachmenttheory-based strategies for decreasing psychological/emotional distance from others. These distance-decreasing attachment strategies include (1) explicitly acknowledging or considering the other’s message, (2) showing an intention or willingness to share information with the other, (3) exploring similarity or shared experience with the other, and (4) expressing positive feeling and support for the other (Hess, 2002). Therefore providing more adaptive (i.e., corrective) emotional-relational experiences with the therapist is an important aspect of psychodynamic psychotherapy, and may be particularly so for patients with a cold/ distant relational style. In sum, consistent with the work of Hess (2002), Hill, Knox and Pinto-Coelho (2018), Hill et al. (2008), Wachtel (1993, 2008), McCullough et al. (2003), and Safran and Muran (2000), we would suggest that the most curative aspect of here-and-now in-session processing of the therapeutic relationship consists in illuminating patients’ familiar patterns of relatedness while simultaneously providing a template for more adaptive attachment strategies and interpersonal functioning. Rather than interpretively linking expressions of these familiar patterns to archaic or genetic associations, this approach to working with cyclical relational patterns highlights and utilizes new opportunities for an examined in vivo emotional-relational interaction in a new relationship, created between the therapist and patient Working with cyclical relational patterns in contemporary psychodynamic psychotherapy 27 Conclusion As reviewed above, prior evidence supporting the effectiveness of transference interpretations is often dependent on patient characteristics. In addition, research evidence increasingly demonstrates that supportive forms of dynamic therapy or dynamic therapies that integrate both supportive and interpretive (i.e., expressive) components have been found to be as highly effective and efficacious in comparison with more interpretive forms of dynamic treatment (Leichsenring, Leweke, Klein, & Steinert, 2015). We believe that a singular interpretive treatment focus and prohibition of supportive techniques represent a false dichotomy of practice that appears inconsistent with the available data on the optimal use of techniques exploring the patient therapist relationship. Consistent with the findings reviewed here, an optimal approach to interpretive work seems to exist at a low to moderate number (one to four) of interventions per session examining the patient therapist relationship and in the context of a strong therapeutic alliance (see Kuutmann & Hilsenroth, 2012; Ryum et al., 2010; Schut et al., 2005). As the therapeutic relationship is often experienced as an intimate, emotionally charged, asymmetrical, and typically nurturant relationship, psychotherapy is likely to activate many attachment-related patterns of thought, feeling, and conflict (Fonagy et al., 1996; Seligman & Csikszentmihalyi, 2000). Rather than viewing the treatment situation as an interpretive stimulus field to be deconstructed, the therapeutic relationship instead offers an active experimental arena in which in vivo examination of patienttherapist relational experiences provides insight into some of the patient’s familiar patterns of close interpersonal relationships. By extension it presents a unique relational training ground to brainstorm and attempt new models of thinking and relating, which may generalize to lasting personal changes (e.g., Blatt, 1990). For instance therapists would explore how interpersonal and affective themes covered during a session might play out in the therapeutic relationship (e.g., “You know we’ve talked a lot about the issue of ____ today, and I wonder how that might play out in here between the two of us?”; “How do you understand that issue in regard to our relationship?”), they would also frequently encourage perspective taking in this relationship and about the therapy, as observed in a mentalizing therapeutic stance (Allen, Fonagy, & Bateman, 2008), (e.g., “How do you imagine I feel after hearing your story?”; “What do you imagine I might be thinking about you?”; “That certainly makes sense, but I wonder if there could be any other reason why I might do that other than just being upset with you?”; “I wonder if you can imagine any other way I might feel?”). Also importantly, clinicians can view the therapeutic relationship as an arena in which more adaptive relating is first practiced and explored rather than as just a place to repeat prior behavior. Therefore adaptive relational changes, no matter how small, need to be underlined and supported (e.g., “I think it’s important to point out that you were just able to express this issue in here with me; what do you think helps to do that in here as opposed to your other relationships?”; “What do you think has changed the most in our relationship that allows you to say that to me now as opposed to in the past?”). Likewise, clinicians 28 Contemporary Psychodynamic Psychotherapy may want to consider affirming, validating, and supporting patients’ involvement or experience in the therapeutic relationship (e.g., “Given your history, it seems only reasonable that you’d be cautious in allowing yourself to become emotionally open with me, a man”; “Recognizing the reasons for that caution, I feel privileged you’re sharing those feelings with me now”). Furthermore, clinicians working from a short-term dynamic therapy framework may want to sustain focus on the therapeutic relationship with follow-up inquiry of patients’ experiences of the in-session process (e.g., “What’s it like to share that out loud, in here with me?”; “What’s it like to hear me say that?”; “How does it feel to tell me about having accomplished this?”). This exploration of in-session affective experience about the therapeutic relationship can also be extended to the clinicians (e.g., “As I listen to the story you just told me, I also feel a deep sense of hopelessness and despair”), as well as observing the “emotional temperature” in the therapeutic space (e.g., “It seems like something has changed in the room during the last few minutes between us; things have become more quiet and it feels like we are more distant from each other than we were earlier”; “As you were speaking about that, it seems like the room has filled with joy and excitement”). A contemporary, empirically informed psychodynamic approach has moved away from the conceptualization of “transference reactions” as distortions of old neurotic conflicts that must be identified, divorced from the person of the clinician, and exorcised from the therapeutic encounter. Instead, the patient therapist interactions that occur during the course of treatment are seen to be rooted in the experiential present and accessible to (even if not always attended by) conscious experience. We would suggest that the time has come to shift away from the outdated and variably defined meta-psychological term transference toward more contemporary articulations of relational schemas and internal working models. As such, we would offer the term therapeutic immediacy as a more experience near alternative to many current clinical uses of the construct transference in the contemporary psychodynamic lexicon. In effect, this may allow psychodynamic researchers and clinicians to communicate more accurately and effectively across various psychotherapy orientations and disciplines. References Allen, J. G., Fonagy, P., & Bateman, A. W. (2008). Mentalizing in clinical practice. Washington, DC: American Psychiatric Publishing. Barber, J. P., Foltz, C., DeRubeis, R. J., & Landis, J. R. (2002). Consistency in interpersonal themes in narratives about relationships. Psychotherapy Research, 12(2), 139 158. Bøgwald, K. P., Høglend, P., & Sorbye, O. (1999). Measurement of transference interpretations. Journal of Psychotherapy Practice and Research, 8, 264 273. Connolly, M., Crits-Christoph, P., Shappell, S., Barber, J., Luborsky, L., & Shaffer, C. (1999). Relation of transference interpretations to outcome in the early sessions of brief supportive-expressive psychotherapy. Psychotherapy Research, 9, 485 495. Working with cyclical relational patterns in contemporary psychodynamic psychotherapy 29 Cooper, A. M. (1987). Changes in psychoanalytic ideas: Transference interpretation. Journal of the American Psychoanalytic Association, 35, 77 98. Ehrenreich, J. H. (1989). Transference: One concept or many? Psychoanalytic Review, 76, 37 65. Fonagy, P., Leigh, T., Steele, M., Steele, H., Kennedy, R., Mattoon, G., & Gerber, A. (1996). The relation of attachment status, psychiatric classification, and response to psychotherapy. Journal of Consulting and Clinical Psychology, 64, 22 31. Freud, S. (1953). Dora: Fragments of an analysis of a case of hysteria. In J. Strachey (Ed. and Trans.), The standard edition of the complete psychological works of Sigmund Freud (Vol. 7, pp. 1 122). London: Hogarth Press. (Original work published 1905). Freud, S. (1958). The dynamics of transference. In J. Strachey (Ed.), The standard edition of the complete psychological works of Sigmund Freud (Vol. 12, pp. 97 108). London, England: Hogarth Press. (Original work published 1912). Freud, S. (1963). Introductory lectures on psycho-analysis: Part III. General theory of the neuroses. In J. Strachey (Ed. and Trans.), The standard edition of the complete psychological works of Sigmund Freud (Vol. 16, pp. 241 463). London: Hogarth Press/ Institute of Psycho-Analysis. (Original work published 1917). Gabbard, G. O. (2000). Psychodynamic psychiatry in clinical practice. Arlington, VA: American Psychiatric Publishing. Gabbard, G. O. (2006). When is transference work useful in dynamic psychotherapy? American Journal of Psychiatry, 163, 1667 1669. Gelso, C. J. (2002). Real relationship: The “something more” of psychotherapy. Journal of Contemporary Psychotherapy, 32, 35 40. Gelso, C. J., Hill, C. E., Mohr, J. J., Rochlen, A. B., & Zack, J. (1999). Describing the face of transference: Psychodynamic therapists’ recollections about transference in cases of successful long-term therapy. Journal of Counseling Psychology, 46, 257 267. Gelso, C. J., Kivlighan, D. M., Wine, B., Jones, A., & Friedman, S. C. (1997). Transference, insight, and the course of time-limited therapy. Journal of Counseling Psychology, 44, 209 217. Gill, M. M. (1984). Psychoanalysis and psychotherapy: A revision. International Review of Psychoanalysis, 11, 161 179. Graff, H., & Luborsky, L. (1977). Long-term trends in transference and resistance: A report on a quantitative-analytic method applied to four psychoanalyses. Journal of the American Psychoanalytic Association, 25, 471 490. Hess, J. A. (2002). Distance regulation in personal relationships: The development of a conceptual model and a test of representational validity. Journal of Social and Personal Relationships, 19, 663 683. Hill, C. E., Knox, S., & Pinto-Coelho, K. G. (2018). Therapist Self-Disclosure and Immediacy: A Qualitative Meta-Analysis. Psychotherapy, 55, 445 460. Hill, C. E., Sim, W., Spangler, P., Stahl, J., Sullivan, C., & Teyber, E. (2008). Therapist immediacy in brief psychotherapy: Case study II. Psychotherapy, 45, 298 315. Høglend, P. (1993). Transference interpretations and long-term change after dynamic psychotherapy of brief to moderate length. American Journal of Psychotherapy, 47, 494 507. Høglend, P. (1994). Manual for process ratings of general skill, supportive interventions and specific techniques. Unpublished manual. Oslo, Norway: Department of Psychiatry, University of Oslo. Høglend, P., Amlo, S., Marble, A., Bogwald, K. P., Sorbye, O., Sjaastad, M. C., & Heyerdahl, O. (2006). Analysis of the patient therapist relationship in dynamic psychotherapy: An experimental study of transference interpretations. American Journal of Psychiatry, 163, 1739 1746. 30 Contemporary Psychodynamic Psychotherapy Høglend, P., Bøgwald, K. P., Amlo, S., Marble, A., Ulberg, R., Sjaastad, M. C., & Johansson, P. (2008). Transference interpretations in dynamic psychotherapy: Do they really yield sustained effects? American Journal of Psychiatry, 165, 763 771. Høglend, P., & Gabbard, G. O. (2012). When is transference work useful in psychodynamic psychotherapy? A review of empirical research. In R. A. Levy, J. S. Ablon, & H. Kächele (Eds.), Psychodynamic psychotherapy research: Evidence-based practice and practice-based evidence (pp. 449 470). Totowa, NJ: Springer. Høglend, P., Johansson, P., Marble, A., Bøgwald, J., & Amlo, S. (2007). Moderators of the effects of transference interpretations in brief dynamic psychotherapy. Psychotherapy Research, 17, 162 174. Huang, T. C. C., Hill, C. E., Strauss, N., Heyman, M., & Hussain, M. (2016). Corrective relational experiences in psychodynamic-interpersonal psychotherapy: Antecedents, types, and consequences. Journal of Counseling Psychology, 63(2), 183. Kasper, L. B., Hill, C. E., & Kivlighan, D. M., Jr. (2008). Therapist immediacy in brief psychotherapy: Case study I. Psychotherapy, 45, 281 297. Kuutmann, K., & Hilsenroth, M. J. (2012). Exploring in-session focus on the patient therapist relationship: Patient characteristics, process, and outcome. Clinical Psychology and Psychotherapy, 19, 187 202. Leichsenring, F., Leweke, F., Klein, S., & Steinert, C. (2015). The empirical status of psychodynamic psychotherapy: An update: Bambi’s alive and kicking. Psychotherapy and Psychosomatics, 84(3), 129 148. Luborsky, L. (1977). Measuring a pervasive psychic structure in psychotherapy: The core conflictual relationship theme. In N. Freedman, & S. Grand (Eds.), Communicative structures and psychic structures (pp. 367 395). New York: Plenum. Luborsky, L., & Crits-Christoph, P. (1998). Understanding transference: The core conflictual relationship theme method. Washington, DC: American Psychological Association. Malan, D. H. (1979). Individual psychotherapy and the science of psychodynamics. London: Butterworths. Marmarosh, C. L., Gelso, C. J., Markin, R. D., Majors, R., Mallery, C., & Choi, J. (2009). The real relationship in psychotherapy: Relationships to adult attachments, working alliance, transference, and therapy outcome. Journal of Counseling Psychology, 56, 337 350. Mayotte-Blum, J., Slavin-Mulford, J., Lehmann, M., Pesale, F., Becker-Matero, N., & Hilsenroth, M. (2012). Therapeutic immediacy across long-term psychodynamic psychotherapy: An evidence-based case study. Journal of Counseling Psychology, 59, 27 40. McCullough, L., Kuhn, N., Andrews, S., Kaplan, A., Wolf, J., & Hurley, C. L. (2003). Treating affect phobia: A manual for short-term dynamic psychotherapy. New York: Guilford Press. Multon, K. D., Patton, M. J., & Kivlighan, D. M., Jr. (1996). Development of the Missouri Identifying Transference Scale. Journal of Counseling Psychology, 43, 243 252. Muran, J. C., Safran, J. D., Gorman, B. S., Samstag, L. W., Eubanks Carter, C., & Winston, A. (2009). The relationship of early alliance ruptures and their resolution to process and outcome in three time-limited psychotherapies for personality disorders. Psychotherapy, 46, 233 248. Ogrodniczuk, J. S., Piper, W. E., Joyce, A. S., & McCallum, M. (1999). Transference interpretations in short-term dynamic psychotherapy. Journal of Nervous and Mental Disease, 187, 571 578. Patton, M. J., & Kivlighan, D. M. (1997). The Missouri Psychoanalytic Counseling Research Project: Relation of changes in counseling process to client outcomes. Journal of Counseling Psychology, 44, 189 208. Working with cyclical relational patterns in contemporary psychodynamic psychotherapy 31 Piper, W. E., Azim, H. F., Joyce, A. S., McCallum, M., Nixon, G. W., & Segal, P. S. (1991). Quality of object relations versus interpersonal functioning as predictors of therapeutic alliance and psychotherapy outcome. Journal of Nervous and Mental Disease, 179, 432 438. Piper, W. E., Ogrodniczuk, J. S., & Joyce, A. (2004). Quality of object relations as a moderator of the relationship between pattern of alliance and outcome in short-term individual psychotherapy. Journal of Personality Assessment, 83, 345 356. Rhodes, R., Hill, C., Thompson, B., & Elliot, R. (1994). Client retrospective recall of resolved and unresolved misunderstanding events. Journal of Counseling Psychology, 41, 473 483. Ryum, T., Stiles, T. C., Svartberg, M., & McCullough, L. (2010). The role of transference work, the therapeutic alliance, and their interaction in reducing interpersonal problems among psychotherapy patients with Cluster C personality disorders. Psychotherapy, 47, 442 453. Safran, J. D., & Muran, J. C. (2000). Negotiating the therapeutic alliance: A relational treatment guide. New York: The Guilford Press. Schut, A. J., Castonguay, L. G., Flanagan, K. M., Yamasaki, A. S., Barber, J. P., Bedics, J. D., & Smith, T. L. (2005). Therapist interpretation, patient-therapist interpersonal process, and outcome in psychodynamic psychotherapy for avoidant personality disorder. Psychotherapy, 42, 494 511. Seligman, M. E., & Csikszentmihalyi, M. (2000). Positive psychology. An introduction. American Psychologist, 55, 5 14. Sifneos, P. (1992). Short-term anxiety-provoking psychotherapy: A treatment manual. New York: Basic Books. Strupp, H. H., & Binder, J. (1984). Psychotherapy in a new key. New York: Basic Books. Wachtel, P. L. (1993). Therapeutic communication. New York: The Guilford Press. Wachtel, P. L. (2008). Relational theory and the practice of psychotherapy. New York: The Guilford Press. Woodhouse, S. S., Schlosser, L. Z., Crook, R. E., Ligiéro, D. P., & Gelso, C. J. (2003). Client attachment to therapist: Relations to transference and client recollections of parental caregiving. Journal of Counseling Psychology, 50, 395 408. Ziv-Beiman, S., Keinan, G., Livneh, E., Malone, P. S., & Shahar, G. (2016). Immediate therapist self-disclosure bolsters the effect of brief integrative psychotherapy on psychiatric symptoms and the perceptions of therapists: A randomized clinical trial. Psychotherapy Research, 27, 1 13. Further reading Flückiger, C., Del Re, A. C., Wampold, B. E., & Horvath, A. O. (2018). The alliance in adultpsychotherapy: A meta-analytic synthesis. Psychotherapy, 55(4), 316 340. Høglend, P., Hersoug, A. G., Bøgwald, K. P., Amlo, S., Marble, A., Sørbye, Ø., . . . CritsChristoph, P. (2011). Effects of transference work in the context of therapeutic alliance and quality of object relations. Journal of Consulting and Clinical Psychology, 79(5), 697. Piper, W. E., McCallum, M., Joyce, A. S., Azim, H. F., & Ogrodniczuk, J. S. (1999). Follow-up findings for interpretive and supportive forms of psychotherapy and patient personality variables. Journal of Consulting and Clinical Psychology, 67(2), 267. Attachment and mentalization in contemporary psychodynamic psychotherapy 3 Martin Debbané1,2 1 Developmental Clinical Psychology Research Unit, Faculty of Psychology and Educational Sciences, University of Geneva, Geneva, Switzerland, 2Research Department of Clinical, Educational and Health Psychology, University College London, London, United Kingdom Attachment theory and mentalization theory resonate on many dimensions, and their concepts yield clinical utility for the practice of psychotherapy. As a cardinal point of contact, both theories lend central importance to the type of learning that takes place within relationships characterized by security and trust. These theories have evolved as forms of applied science linked to a common theoretical ancestor, psychoanalysis, with which they continue to entertain complex and often uneasy familial ties. The feuds between proponents of attachment theory and those of psychoanalysis have been described at length (Fonagy, 2001a), and the field of tension created has been characterized as being entrenched in “bad blood.” The mentalization-based approach was arguably born out of this field of tension in which psychoanalysis and attachment theories confronted each other (Fonagy & Campbell, 2015), a field of conflict that also contained the potential for development and creativity—specifically in the application of these theories to psychodynamic psychotherapy. In terms of positioning, the “in-betweenness” of mentalization theory has taken advantage of a space in which conceptual integration could emerge. Mentalization theory as applied to psychotherapy integrates a diverse set of principles originating from different theories, including psychoanalysis, attachment theory, developmental psychology, and cognitive neuroscience (Bateman & Fonagy, 2004, 2006). In order to contextualize the latest conceptual developments concerning mentalization in psychotherapy, this chapter will attempt to address some of the key questions that arise when we consider points of contact between attachment and mentalization theories. While mentalization is believed to be salient across all psychodynamic approaches to psychotherapy, mentalization-based treatment (MBT) will be referred to throughout the chapter as an exemplar of applied mentalization theory in contemporary psychodynamic practice. First, the concept of mentalizing in the context of psychotherapy will be defined, and its affiliation with attachment theory and its empirical foundations will be retraced. The second section will outline Contemporary Psychodynamic Psychotherapy. DOI: https://doi.org/10.1016/B978-0-12-813373-6.00003-9 © 2019 Elsevier Inc. All rights reserved. 34 Contemporary Psychodynamic Psychotherapy the importance of how these two theories conceptualize the nature of psychopathology and the implicit views they share on the nature of therapeutic change. The final section will consider new developments in mentalization theory, reaching beyond its initial tenets and leaning toward an overall theory of psychotherapeutic communication that sheds new light on how we understand the therapeutic effects of psychodynamic psychotherapy. Conceptual and empirical links between attachment theory and mentalization in dynamic psychotherapy From the perspective of mentalization theory, mentalizing—the suite of psychological processes devoted to thinking about the mental states underlying behaviors in self and others—constitutes a key ingredient driving change in psychotherapy (Bateman & Fonagy, 2006). Thus it was hypothesized that mentalization could be thought of as an active agent inducing therapeutic change in almost all psychotherapeutic models, ranging from psychodynamic to systemic, cognitive behavioral, humanistic, and person-centered approaches (Allen, Fonagy, & Bateman, 2008). As a time-limited psychodynamic therapy model, MBT places particular emphasis on mentalizing as both a process and an outcome of treatment. Moreover, a mentalization perspective, embodied in MBT, proposes a sophisticated developmental framework accounting for the maturational dependency of the child’s mentalizing capacity on the minds of its caregivers. This conceptualization provides key insights into the development of borderline personality disorder (BPD) while proposing a focused therapeutic method as a psychodynamic alternative to the classical psychoanalytic cure, which has often failed to provide therapeutic change in patients with BPD and has sometimes even provoked negative therapeutic reactions (Bateman & Fonagy, 2004). For the purpose of conciseness this chapter will examine the empirical foundation of mentalization in the psychotherapeutic context from three main areas of study: (1) research on attachment; (2) research on reflective functioning (RF); and (3) research on the developmental dynamics linking trauma, attachment insecurity, impairments in mentalization, and the development of BPD. Relying on attachment research using the strange situation procedure (SSP; Ainsworth, Blehar, Waters, & Wall, 1978), mentalization theory emphasizes the dyadic regulation of affect between the infant and its caregiver, which studies employing SSP have depicted so tangibly. Formulating a contemporary account of the Winnicottian transitional space (Winnicott, 1965, 1971) created by the mother infant dyadic communication, the mentalization-based framework stipulates that caregivers foster regulation of affect in children when the caregivers offer contingent, congruent, and marked responses in communicating (mirroring) their understanding of the child’s expressed affect (Fonagy, Gergely, Jurist, & Target, 2002). Indeed, from the perspective of mentalization theory, the parent child communication system provides a matrix upon which much therapeutic communication Attachment and mentalization in contemporary psychodynamic psychotherapy 35 is modeled. While parental contingent mirroring involves adequate and sensitive timing of the parent’s response to the child’s emotional signals, the congruency of the parental response refers to the success the parent encounters when correctly identifying the category of affect dominating the child’s experience. Critical to parental success is the efficient transmission of the parent’s affective understanding through nonverbal and verbal communication with the child. Importantly, the parental response’s degree in marking (marked mirroring) is crucial to establish metacommunication, that is, to convey that the parent is communicating about the child’s emotion and not simply reacting to the child’s affective expression. Marked mirroring focuses the attentional lens of dyadic communication on learning about affect through reflectivity; it organizes the links between the trigger of affective arousal, the affective experience, its meaning for the child, and the consequence of affect on the child’s behavioral expression. The parental response already constitutes a rich and complex repertoire of communication that employs ostensive communication cues, such as eye contact and turn taking, that the child naturally decodes. Similarly, a therapist practicing from a mentalizing standpoint is encouraged to come into contact with the patient’s emotional expression through empathic validation (Bateman, O’Connell, Lorenzini, Gardner, & Fonagy, 2016), that is, through sensitively reflecting what the patient may be affectively experiencing. Through the careful monitoring of the patient’s emotional arousal in session, the therapist employs a spectrum of interventions designed to foster the process of mentalizing. The interventions of the therapist are to be used as an object to be edited, transformed by the patient to sustain the therapeutic process, and fuel further mentalizing. Therefore mentalizing involves at least two individuals implicated in affective regulation through communication about mental states (Luyten, 2014). Research on RF, which attempts to operationalize and measure the psychological processes that are captured by the term mentalization, constitutes the second line of empirical knowledge upon which a mentalizing perspective in psychotherapy is founded. Our understanding of this process in psychotherapy derives from the rich historical definitions of mentalization (Lecours & Bouchard, 1997). The brevity of this chapter unfortunately does not permit adequate tribute to the authors who contributed to this understanding before the birth of MBT—authors such as Pierre Marty and colleagues whose proposed definition of mentalization is still traceable today in Bateman and Fonagy’s MBT model (Debbané, 2016). Discussion of RF (Fonagy, Target, Steele, & Steele, 1998) will occur within the confines of both conceptual and empirical research in MBT, delineating some key milestones and the questions they have raised. It may be argued that research on RF constitutes the cornerstone of a mentalization focus in psychodynamic psychotherapy. Indeed, in the first practical guides outlining the MBT method of psychotherapy (Bateman & Fonagy, 2004, 2006), the patient’s RF (capacity to mentalize self and others) was designated as the main target of treatment. RF is investigated as the process by which thinking about mental states in oneself and others contributes to understanding behaviors in the social domain, especially within interactions involving significant others (Bouchard et al., 2008). 36 Contemporary Psychodynamic Psychotherapy The measurement of RF is drawn from narrative material collected using the adult attachment interview (George, Kaplan, & Main, 1985). The RF scale (Fonagy, Steele, & Steele, 1991; Fonagy et al., 1998) provides the interview with more sensitivity to capture the adult’s awareness of mental states, and their employment of mental state information to understand themselves and others. Importantly, RF in parents is found as a key predictor of the child’s attachment status, linking parental mentalizing skills to the establishment of secure attachment relationships (Fonagy et al., 1991). It further supports the view that situates early attachment relationships as the initial playground in which the child learns about minds (Fonagy & Target, 1996). Research on RF lends support to mentalizing as playing a key developmental role in the establishment of secure attachment, which through a virtuous cycle further promotes the development of mentalizing. Most crucially, one’s capacity to develop reflective thinking depends, in part, on the way significant others have thought about our minds as children: . . . a fundamental need of every infant is to find his own mind, or intentional state, in the mind of the object. In Epilogue, Fonagy et al. (2002, p. 474) In other words, the capacity for RF develops, to a large extent, through the reflective function of caregivers. This is extended to the psychotherapeutic context, in that the therapist’s RF with regard to the patient’s mind is seen as foundational for the patient’s enhancement of mentalizing abilities. For this reason—the idea that mentalizing minds breed mentalizing minds—a focus on RF characterizes the focused approach of MBT in guiding the therapist to identify her or his own moments of loss of mentalizing as a key feature to the psychotherapeutic process. While sensitive to the concepts of transference and countertransference, MBT technique encourages the psychotherapist to attend to process rather than content in the therapeutic exchange and to react swiftly to interrupt nonmentalizing interactions in the heat of the session. Thus MBT explicitly demonstrates how RF as a threedimensional process (therapist RF, patient RF, therapist patient RF) lies at the heart of psychodynamic psychotherapy. From the perspective of mentalization theory a considerable degree of psychopathology—particularly that which pertains to self- and affect-regulation— may be traced to the thwarted development of mentalization. Both cross-sectional and longitudinal studies provide supporting evidence for the view that early trauma induces the establishment of insecure attachment in children, who are more likely to demonstrate developmental delays or impairments in mentalization (Berthelot et al., 2015; Ensink, Berthelot, Begin, Maheux, & Normandin, 2017). Prospective research observes that insecure attachment is linked to impaired mentalizing in adolescents, which itself mediates the association between early insecure attachment and adult development of borderline personality symptomatology (Carlson, Egeland, & Sroufe, 2009). With the advancement of neuroscientific research at the turn of the 21st century, attachment and mentalization researchers have increasingly emphasized the impact Attachment and mentalization in contemporary psychodynamic psychotherapy 37 of trauma on stress regulation mechanisms (Debbané & Nolte, 2019; Nolte, Guiney, Fonagy, Mayes, & Luyten, 2011), that is, the neurobiological underpinnings relating to the HPA axis, together with interacting dopaminergic, oxytonergic, and serotonergic systems (Luyten & Fonagy, 2015; Mayes, 2000). Such an articulation between attachment, stress regulation, and mentalization confers on therapy the role of rejuvenating the regulatory function of mentalizing through assisting its development or strengthening depending on the degree of alteration. The neuroscience of emotion regulation thus further frames contemporary psychodynamic psychotherapy as a practice that increases patients’ capacities to self-regulate. Shared assumptions on psychopathology and change Attachment and mentalization theories have historically participated in the nature/ nurture debate on the origins of psychopathology (Bowlby, 1988; Fonagy, 2001b), formulating critical arguments for the role of early relationships as key factors to mental health. As would be expected from theories that model human development by focusing on the social and emotional growth fostered in close relationships, attachment theory and mentalization theory put heavy emphasis on the impact of childhood experiences in developing psychopathology. The two theories converge in suggesting that their central construct represents a nonspecific risk/resilience factor for mental health (Fonagy, Steele, Steele, Higgitt, & Target, 1994; Mikulincer & Shaver, 2012). They both advance the idea that their central construct, whether mentalizing or attachment, contributes to developing psychopathology or mental health through (1) (dys)regulation of emotions, (2) (de)stabilization of self and other representations, and (3) (in)capability of developing high-quality interpersonal relationship (Fonagy et al., 2002; Mikulincer & Shaver, 2012). At the heart of their therapeutic propositions lies the necessity to primarily regulate arousal in order to positively influence the mental models the patient entertains about both self and others. Consistent with object relations models of therapy (Kernberg, Yeomans, Clarkin, & Levy, 2008), this focus on regulation of arousal is designed to enable psychotherapeutic work on representations or internal working models. Moreover, the linking of attachment and mentalizing as nonspecific factors in psychopathology has contributed to the creative development of psychodynamic psychotherapies for groups of patients who could not necessarily access services in which contemporary psychodynamic psychotherapy was delivered (Bevington, Fuggle, & Fonagy, 2015; Byrne et al., 2018; Debbané et al., 2016; Fuggle et al., 2015; Weijers et al., 2016). One important limitation to the nature of the links between attachment, mentalizing, and psychopathology is that the strength of these associations remains relatively low (Groh, Roisman, van Ijzendoorn, Bakermans-Kranenburg, & Fearon, 2012; Katznelson, 2014). Similarly, no clear causality relationships can be gleaned from the available associative studies (Mikulincer & Shaver, 2012). Furthermore, the 38 Contemporary Psychodynamic Psychotherapy contributions of these concepts to our understanding of psychopathology has been muddled by the overlap they have with other concepts such as empathy, mindfulness, psychological mindedness, object relations, compassion, and the like (ChoiKain & Gunderson, 2008). Currently, while significant progress has been made through the application of attachment and mentalization theories to psychodynamic therapies, the lack of specificity and important overlap between these approaches and others could potentially limit advancement if the “Dodo bird verdict” would represent their ultimate contribution. Recently, significant attention and attempts to understand the overlap between contemporary constructs have been put forward in psychotherapy research, using the term common factors (Wampold, 2015). Most psychotherapists and clinical researchers today will admit to shared transtheoretical elements between different models of psychotherapy, the best known being the so-called therapeutic alliance (Arnow & Steidtmann, 2014). The impact of common factors is commonly found to be double that of the specific techniques linked to specialized psychotherapy models (Wampold, 2015), notwithstanding the significant impact of placebo in psychotherapy (Baskin, Tierney, Minami, & Wampold, 2003). From this perspective, attachment-based or mentalization-based perspectives do not necessarily hold the key to the city of therapeutic change. What is perhaps more troubling to clinicians is being confronted with research suggesting that the largest portion of their therapeutic impact with their patients relies on extratherapeutic factors (Wampold, 2015). These factors have to do with the contextual variables within which any psychotherapy takes place. Few concrete psychodynamic applications addressing these factors have been proposed to date (Asen & Fonagy, 2017). To summarize, attachment and mentalization theories conceptualize their key constructs as central to risk/resilience in the manifestation of psychopathology and propose intervention models that specifically aim to work on mechanisms that will sustain emotion regulation and foster work on self and other representations. This nonspecific approach to psychopathology and therapeutic change is both useful and limited. It is useful in the application of psychodynamic therapy for severe and also hard-to-reach clinical needs, but it may be limited because it does not necessarily address other areas of potential gains in psychotherapy, such as extratherapeutic factors. To account for these limitations, a series of developments in mentalization theory have recently undertaken to reframe the nature of therapeutic communication (Fonagy & Allison, 2014; Fonagy, Luyten, & Allison, 2015), proposing a novel model for thinking about therapeutic effects in psychodynamic psychotherapy. From regulation therapy to learning from experience: beyond the therapeutic relationship Initial formulations of the mentalization perspective on psychotherapy stated that therapeutic change, no matter what therapeutic approach was used, could be linked to each technique’s effect on the patient’s ability to mentalize. Bateman and Attachment and mentalization in contemporary psychodynamic psychotherapy 39 Fonagy (2004, 2006) proposed a unified, transtheoretical perspective of therapeutic gain around the notion of mentalization while suggesting with a hint of impertinence that mentalization-based therapies offered the model to follow to help patients recover and deepen their mentalizing capacity. More recently, these authors have proposed a reformulation of the link between mentalization and therapeutic gain, shifting its conceptual framework from a mentalization-centered approach to an integrative articulation of the specific and general factors of evidenced-based psychotherapeutic approaches (Fonagy & Allison, 2014; Fonagy et al., 2015). This recent evolution introduces three additional notions: epistemic trust, the transmission of cultural knowledge through natural pedagogy, and psychotherapeutic communication systems. As surveyed in the first two sections of this chapter, one of the key characteristics of the attachment relationship is to provide an interpersonal context within which the child (and, in psychotherapy, the patient) can learn to identify and represent mental states specific to self and others and to regulate emotions and to “play” with psychic reality, all of which promote robust social cognition, self-regulation, and resilience (Fonagy et al., 1994; Fonagy & Target, 1996). More recent elaborations on the role of early attachment relationships examine the characteristics of communication within the early attachment relationship, specifically those characteristics that foster the internalization of cultural knowledge (Csibra & Gergely, 2009; Fonagy & Allison, 2014). Fonagy, Luyten, Allison, and Campbell (2017a,b) propose that the context of attachment serves not only to promote the capacity to mentalize, but also to generate a particular type of trust, epistemic trust, opening the way to receptivity and the process of. The key value of internalization processes is to extend beyond the confines of the privileged relationship with a parent (or a therapist) into the interpersonal and social spheres in the child’s (or patient’s) life. Epistemic trust refers to the individual’s propensity to consider new information as trustworthy, relevant to oneself, and generalizable to other contexts. If epistemic trust is essential to the therapeutic effect, how can therapists approach the question of their credibility in the eyes of patients who suffer from personality disorders, which have evolved in environments that are hostile to mental states, conferring on these patients rigid, inflexible, and chronic epistemic vigilance? Mentalization theory approaches this question through the prism of the patient’s subjective experience. A therapist’s only hope to restore a certain degree of epistemic trust is by engaging with the patient’s subjective experience. This commitment and dedication to trying to understand the patient’s subjectivity are likely to lead the patient to reconsider his or her perception of himself or herself and others and the patient’s relationships to others as opportunities to discover useful and satisfying elements to his or her life. To rekindle epistemic trust, the therapist’s primary interest and focus are directed more toward a process that can revive the patient’s ability to learn from his or her experience with the world around the patient (Bion, 1962). To resituate the place of mentalization in the therapeutic effect, Fonagy et al. (2015) hypothesized that mechanisms of therapeutic change are underpinned by three systems of therapeutic communication that, cumulatively, contribute to 40 Contemporary Psychodynamic Psychotherapy therapeutic gains during treatment and beyond. Each of these systems of therapeutic communication is seen as contributing to patients having the experience of their subjectivity being contained and understood. This in turn leads to feelings of confidence that such experiences exist outside the consulting room, thereby extending the effects of psychotherapy to the extratherapeutic domain. Communication System I: Content relevance and the establishment of epistemic trust The first system of therapeutic communication refers to the formulation of mental health and disease proposed and conveyed by a given model of psychotherapy. Thus the generic proposition of a therapy model can potentially yield a subjective impression of being understood by or in the approach in question. Therapeutic orientations each communicate, in an ostensive manner (Csibra & Gergely, 2009), a representation of the functioning of psychological suffering that is sufficiently generic for it to be read by the candidate for therapy. In the experience of this reading, the future patient can feel a kind of congruent and marked mirroring conveyed by the generic message offered by the therapeutic orientation. Through this metacommunication, the encounter with a model is likely to stimulate a hope of change in the future patient or in the patient beginning a therapy. Moreover, such metacommunication informs the patient of the ability and potential effectiveness of the approach to solve a set of psychological problems and suffering. Therefore at the first level of psychotherapeutic communication, each psychotherapy model generates for the future or new patient a subjective feeling of being understood by the explanatory framework in question and a hope of evolving beyond one’s current state. For patients entering psychodynamic psychotherapy, the generic mechanism of contemplating underlying motivations, thoughts, and feelings—conveyed implicitly and explicitly to the patient—provides the initial basis for the establishment or reestablishment of epistemic trust. The patient’s openness to discovery and new knowledge at this level paves the way for the second communication system that specifically targets the capacity to mentalize. Communication System II: The reemergence of robust mentalization Upon initiation of a treatment that proposes ways in which the patient might feel recognized and understood, the second communication system emerges in the specificity of the interactions between patient and therapist. From the standpoint of mentalization theory, the key to therapeutic efficacy is the therapist’s understanding of the subjective experience of the patient. Thus the therapist will more likely communicate about highly relevant content to the patient’s experience of self and others. For the patient, this essential experience of having one’s own subjectivity received, accepted, and understood by the therapist revives the ability to mentalize (Fonagy, 2002). Experiencing a therapy as consistent with one’s current needs, accompanied Attachment and mentalization in contemporary psychodynamic psychotherapy 41 by a person (the therapist) committed to understanding one’s subjective experience, is the essence of the second communication system. This process regenerates mentalizing or, more precisely, the desire to understand others. As the patient increasingly feels understood and represented in the mind of the therapist, the patient may become curious about the therapist’s mind, seeking to understand how it works and in turn how others’ perspectives are mentally generated. This process of mutual and differentiated understanding thus constitutes a therapeutic communication from which mentalizing emerges and is strengthened. Mentalization theory recasts the activities and communications within psychodynamic psychotherapy as primarily facilitating a mentalizing process between therapist and patient, thereby stimulating and enhancing the patient’s compromised RF. This process, however, cannot be limited to the walls of the consulting room. Rather, the mentalizing process engendered in psychodynamic therapy—and explicitly targeted in MBT—is seen as stimulating and sustaining the patient’s epistemic confidence in the world beyond the therapy session. Through the reactivation of epistemic trust, mentalization leads to a central aspect of the third system of communication: that of the desire and capacity to learn from experience (Bion, 1962) in the social world. Communication System III: Reemergence of the ability to learn in the social world beyond the therapeutic relationship In Systems I and II the psychotherapeutic process builds on the sustained experience of the patient’s subjectivity being thought about and reflected upon by the therapist. It is hypothesized that this experience contributes to opening a wider path that could be referred to as an epistemic highway: the possibility of internalizing, on the basis of experience outside the consultation room, new knowledge that is both relevant to oneself and generalizable to the world. The experience of being carefully thought about and understood can potentially break open rigid and inflexible beliefs that keep the patient stuck in complex yet circular inferences (Rudrauf & Debbané, 2018). This experience is theorized to propel the individual beyond the confines of the privileged therapy relationship, making the uncertainty and the unknown of any trajectory of human life tolerable or even desirable. While this evolution is partly driven by the therapeutic process, the patient’s environment is critical in the development and generalization of processes revitalized by psychotherapy. When the patient reengages with social and interpersonal interactions, he or she gains further increased understanding. This new understanding, bolstered by epistemic confidence, regenerates the patient’s agency within these interactions and reinforces a desire to draw from them as sources of knowledge and satisfaction that, until then, were inaccessible. The third system of communication initiates a third virtuous circle: the increased mentalization of the social world, where interpersonal relationships increase the patient’s understanding of the functioning of his or her environment. This in turn sensitizes the patient to complementary sources of support and meaningful relationships that may maintain the patient’s subjectivity in mind, that may engage the 42 Contemporary Psychodynamic Psychotherapy patient in socially constructive ways, and that may afford an increase in suspended time in which vigilance gives way to epistemic trust. In a world characterized by demands, change, and fundamentally unpredictable events, curiosity and openness to experience represent the currencies that critically engage with sources of potential learning. The systems of communication framework proposed by mentalization theory suggests that the reemergence of the ability to learn from one’s experience—fostered through the mentalizing process of communication between therapist and patient— lies at the heart of lasting psychotherapeutic success. Beyond the walls of the consultation room, epistemic trust supports the individual in his or her personal and social development, facilitating new or renewed understanding of how things work naturally in complex interpersonal and social systems. Thus in addition to promoting mentalization within the therapy itself, psychodynamic therapy is seen as helping the patient to increasingly move toward relationships in which he or she can find his or her mind and apprehend new sources of knowledge from interpersonal experiences. Conclusion This chapter surveyed recent developments in attachment and mentalization theories as they pertain to understanding psychopathology and the processes of psychodynamic psychotherapy. In its integrative effort to conceptualize contemporary psychodynamic psychotherapy—and through the formulation of a specific MBT model—mentalization theory emphasizes the regulation of affect, security of therapy relationship, and understanding of subjective experience as central to the therapeutic endeavor. Moreover, a mentalization perspective reframes therapeutic gains within the broader context of socioemotional communication and experience. The systems of communication framework proposed in mentalization theory regards psychotherapy as a means for strengthening self-regulation through clinical practices that facilitate increased learning from experience outside the consultation room. Thus recent conceptual developments point to the importance of understanding how generalization processes infuse the patient’s mind to seek out experiences of learning from one’s environment. In this way, mentalization theory underlines the limitations of the strictly dyadic framework that characterizes most psychotherapy models, considering extratherapeutic factors that require further conceptualization, testing, and innovation in the future of psychodynamic psychotherapy. References Ainsworth, M. D., Blehar, M. C., Waters, E., & Wall, S. (1978). Patterns of attachment: A psychological study of the strange situation. Hillsdale, NJ: Lawrence Erlbaum. Allen, J. G., Fonagy, P., & Bateman, A. W. (2008). Mentalizing in clinical practice. Washington, DC: American Psychiatric Publishing. Attachment and mentalization in contemporary psychodynamic psychotherapy 43 Arnow, B. A., & Steidtmann, D. (2014). Harnessing the potential of the therapeutic alliance. World Psychiatry, 13(3), 238 240. Available from https://doi.org/10.1002/wps.20147. Asen, E., & Fonagy, P. (2017). Mentalizing family violence Part 2: Techniques and interventions. Family Process, 56(1), 22 44. Available from https://doi.org/10.1111/ famp.12276. Baskin, T. W., Tierney, S. C., Minami, T., & Wampold, B. E. (2003). Establishing specificity in psychotherapy: A meta-analysis of structural equivalence of placebo controls. Journal of Consulting and Clinical Psychology, 71(6), 973 979. Available from https://doi.org/ 10.1037/0022-006x.71.6.973. Bateman, A., O’Connell, J., Lorenzini, N., Gardner, T., & Fonagy, P. (2016). A randomised controlled trial of mentalization-based treatment versus structured clinical management for patients with comorbid borderline personality disorder and antisocial personality disorder. BMC Psychiatry, 16, 304. Available from https://doi.org/10.1186/s12888-0161000-9. Bateman, A. W., & Fonagy, P. (2004). Psychotherapy of borderline personality disorder: Mentalisation based treatment. Oxford: Oxford University Press. Bateman, A. W., & Fonagy, P. (2006). Mentalization-based treatment for borderline personality disorder: A practical guide. Oxford: Oxford University Press. Berthelot, N., Ensink, K., Bernazzani, O., Normandin, L., Luyten, P., & Fonagy, P. (2015). Intergenerational transmission of attachment in abused and neglected mothers: The role of trauma-specific reflective functioning. Infant Ment Health Journal, 36(2), 200 212. Available from https://doi.org/10.1002/imhj.21499. Bevington, D., Fuggle, P., & Fonagy, P. (2015). Applying attachment theory to effective practice with hard-to-reach youth: The AMBIT approach. Attachment & Human Development, 17(2), 157 174. Available from https://doi.org/10.1080/14616734.2015.1006385. Bion, W. R. (1962). Learning from experience. London: Heinemann. Bouchard, M. A., Target, M., Lecours, S., Fonagy, P., Tremblay, L. M., Schachter, A., & Stein, H. (2008). Mentalization in adult attachment narratives: Reflective functioning, mental states, and affect elaboration compared. Psychoanalytic Psychology, 25(1), 47 66. Available from https://doi.org/10.1037/0736-9735.25.1.47. Bowlby, J. (1988). A secure base: Clinical applications of attachment theory. London: Routledge. Byrne, G., Sleed, M., Midgley, N., Fearon, P., Mein, C., Bateman, A., & Fonagy, P. (2018). Lighthouse Parenting Programme: Description and pilot evaluation of mentalizationbased treatment to address child maltreatment. Clinical Child Psychology and Psychiatry. Available from https://doi.org/10.1177/1359104518807741. Carlson, E. A., Egeland, B., & Sroufe, L. A. (2009). A prospective investigation of the development of borderline personality symptoms. Development and Psychopathology, 21(4), 1311 1334. Choi-Kain, L. W., & Gunderson, J. G. (2008). Mentalization: Ontogeny, assessment, and application in the treatment of borderline personality disorder. American Journal of Psychiatry, 165(9), 1127 1135. Available from https://doi.org/10.1176/appi.ajp.2008.07081360. Csibra, G., & Gergely, G. (2009). Natural pedagogy. Trends in Cognitive Sciences, 13(4), 148 153. Available from https://doi.org/10.1016/j.tics.2009.01.005. Debbané, M. (2016). Mentaliser. Louvain-la-Neuve: De Boeck Supérieur. Debbané, M., Benmiloud, J., Salaminios, G., Solida-Tozzi, A., Armando, M., Fonagy, P., & Bateman, A. (2016). Mentalization-based treatment in clinical high-risk for psychosis: A rationale and clinical illustration. Journal of Contemporary Psychotherapy, 46(4), 217 225. Available from https://doi.org/10.1007/s10879-016-9337-4. 44 Contemporary Psychodynamic Psychotherapy Debbané, M., & Nolte, T. (2019). Contemporary neuroscientific research. Handbook of mentalizing in mental health practice (2nd ed., pp. 23 40). Washington, DC: American Psychiatric Association Publishing. Ensink, K., Berthelot, N., Begin, M., Maheux, J., & Normandin, L. (2017). Dissociation mediates the relationship between sexual abuse and child psychological difficulties. Child Abuse & Neglect, 69, 116 124. Available from https://doi.org/10.1016/j. chiabu.2017.04.017. Fonagy, P. (2001a). Attachment theory and psychoanalysis. New York: Other Press. Fonagy, P. (2001b). The human genome and the representational world: The role of early mother-infant interaction in creating an interpersonal interpretive mechanism. Bulletin of the Menninger Clinic, 65(3), 427 448. Fonagy, P. (2002). The internal working model or the interpersonal interpretative function. Journal of Infant, Child, and Adolescent Psychotherapy, 2(4), 27 28. Available from https://doi.org/10.1080/15289168.2002.10486417. Fonagy, P., & Allison, E. (2014). The role of mentalizing and epistemic trust in the therapeutic relationship. Psychotherapy, 51(3), 372 380. Available from https://doi.org/10.1037/ a0036505. Fonagy, P., & Campbell, C. (2015). Bad blood revisited: Attachment and psychoanalysis. British Journal of Psychotherapy, 31(2), 229 250. Available from https://doi.org/ 10.1111/bjp.12150. Fonagy, P., Gergely, G., Jurist, E. L., & Target, M. (2002). Affect regulation, mentalization, and the development of the self. New York: Other Press. Fonagy, P., Luyten, P., & Allison, E. (2015). Epistemic petrification and the restoration of epistemic trust: A new conceptualization of borderline personality disorder and its psychosocial treatment. Journal of Personality Disorders, 29(5), 575 609. Available from https://doi.org/10.1521/pedi.2015.29.5.575. Fonagy, P., Luyten, P., Allison, E., & Campbell, C. (2017a). What we have changed our minds about: Part 1. Borderline personality disorder as a limitation of resilience. Borderline Personality Disorder and Emotion Dysregulation, 4, 11. Available from https://doi.org/10.1186/s40479-017-0061-9. Fonagy, P., Luyten, P., Allison, E., & Campbell, C. (2017b). What we have changed our minds about: Part 2. Borderline personality disorder, epistemic trust and the developmental significance of social communication. Borderline Personality Disorder and Emotion Dysregulation, 4, 9. Available from https://doi.org/10.1186/ s40479-017-0062-8. Fonagy, P., Steele, H., & Steele, M. (1991). Maternal representations of attachment during pregnancy predict the organization of infant-mother attachment at one year of age. Child Development, 62(5), 891 905. Available from https://doi.org/10.1111/j.14678624.1991.tb01578.x. Fonagy, P., Steele, M., Steele, H., Higgitt, A., & Target, M. (1994). The Emanuel Miller Memorial Lecture 1992. The theory and practice of resilience. Journal of Child Psychology and Psychiatry, 35(2), 231 257. Available from https://doi.org/10.1111/ j.1469-7610.1994.tb01160.x. Fonagy, P., & Target, M. (1996). Playing with reality: I. Theory of mind and the normal development of psychic reality. International Journal of Psychoanalysis, 77(Pt 2), 217 233. Fonagy, P., Target, M., Steele, H., & Steele, M. (1998). Reflective-Functioning manual version 5 for application to adult attachment interviews. https://mentalizacion.com.ar/ images/notas/Reflective%20Functioning%20Manual.pdf. Attachment and mentalization in contemporary psychodynamic psychotherapy 45 Fuggle, P., Bevington, D., Cracknell, L., Hanley, J., Hare, S., Lincoln, J., . . . Zlotowitz, S. (2015). The Adolescent Mentalization-based Integrative Treatment (AMBIT) approach to outcome evaluation and manualization: Adopting a learning organization approach. Clinical Child Psychology and Psychiatry, 20(3), 419 435. Available from https://doi. org/10.1177/1359104514521640. George, C., Kaplan, N., & Main, M. (1985). Adult attachment interview. Berkeley: University of California. Groh, A. M., Roisman, G. I., van Ijzendoorn, M. H., Bakermans-Kranenburg, M. J., & Fearon, R. P. (2012). The significance of insecure and disorganized attachment for children’s internalizing symptoms: A meta-analytic study. Child Development, 83(2), 591 610. Available from https://doi.org/10.1111/j.1467-8624.2011.01711.x. Katznelson, H. (2014). Reflective functioning: A review. Clinical Psychology Review, 34(2), 107 117. Available from https://doi.org/10.1016/j.cpr.2013.12.003. Kernberg, O. F., Yeomans, F. E., Clarkin, J. F., & Levy, K. N. (2008). Transference focused psychotherapy: Overview and update. International Journal of Psychoanalysis, 89(3), 601 620. Available from https://doi.org/10.1111/j.1745-8315.2008.00046.x. Lecours, S., & Bouchard, M. A. (1997). Dimensions of mentalisation: Outlining levels of psychic transformation. International Journal of Psychoanalysis, 78, 855 875. Luyten, P. (2014). A new take on the treatment of Borderline Personality Disorder: Are we witnessing the end or merely the beginning of the great psychotherapy debate? In Paper presented at the 3th International Congress on Borderline Personality Disorder and Allied Disorders, Rome, Italy. Luyten, P., & Fonagy, P. (2015). The neurobiology of mentalizing. Personality Disorders, 6 (4), 366 379. Available from https://doi.org/10.1037/per0000117. Mayes, L. C. (2000). A developmental perspective on the regulation of arousal states. Seminars in Perinatology, 24(4), 267 279. Available from https://doi.org/10.1053/ sper.2000.9121. Mikulincer, M., & Shaver, P. R. (2012). An attachment perspective on psychopathology. World Psychiatry, 11(1), 11 15. Nolte, T., Guiney, J., Fonagy, P., Mayes, L. C., & Luyten, P. (2011). Interpersonal stress regulation and the development of anxiety disorders: An attachment-based developmental framework. Frontiers in Behavioral Neuroscience, 5, 55. Available from https://doi.org/ 10.3389/fnbeh.2011.00055. Rudrauf, D., & Debbané, M. (2018). Building a cybernetic model of psychopathology: Beyond the metaphor. Psychological Inquiry, 29(3), 156 164. Available from https:// doi.org/10.1080/1047840X.2018.1513685. Wampold, B. E. (2015). How important are the common factors in psychotherapy? An update. World Psychiatry, 14(3), 270 277. Available from https://doi.org/10.1002/ wps.20238. Weijers, J., Ten Kate, C., Eurelings-Bontekoe, E., Viechtbauer, W., Rampaart, R., Bateman, A., & Selten, J. P. (2016). Mentalization-based treatment for psychotic disorder: protocol of a randomized controlled trial. BMC Psychiatry, 16, 191. Available from https://doi.org/ 10.1186/s12888-016-0902-x. Winnicott, D. W. (1965). The maturational processes and the facilitating environment. New York: International Universities Press. Winnicott, D. W. (1971). Playing and reality. London: Tavistock. The efficacy of psychodynamic psychotherapy: an up-to-date review 4 Falk Leichsenring1 and Christiane Steinert1,2 1 Department of Psychosomatics and Psychotherapy, Justus-Liebig-University Giessen, Giessen, Germany, 2Department of Psychology, MSB Medical School Berlin, Berlin, Germany Mental disorders represent a significant public health concern, owing to their prevalence, associated impairment, and economic impact (Wittchen et al., 2011). Psychotherapy is the first-line treatment option for most of these disorders. Various forms of psychotherapy are available, such as cognitive-behavioral therapy (CBT), interpersonal therapy, and psychodynamic therapy. Although psychodynamic therapy is frequently used in clinical practice (Cook, Biyanova, Elhai, Schnurr, & Coyne, 2010; Norcross, Hedges, & Castle, 2002), early reviews reported limited evidence for its use with specific mental disorders (Connolly Gibbons, CritsChristoph, & Hearon, 2008; DeRubeis & Crits-Christoph, 1998; Task Force on Promotion and Dissemination of Psychological Procedures, 1995). For this reason, the Task Force on Promotion and Dissemination of Psychological Procedures concluded in 1995 that “it is critical that more efficacy evidence on the outcome of psychodynamic therapies for specific disorders be obtained if this clinically verified treatment is to survive in today’s market” (Task Force on Promotion and Dissemination of Psychological Procedures, 1995, p. 2). Meanwhile, the empirical status of psychodynamic therapy has improved considerably. For most of the common mental disorders, randomized controlled trials (RCTs) are available, providing evidence for the efficacy of psychodynamic therapy (Abbass et al., 2014; Fonagy, 2015; Leichsenring, Leweke, Klein, & Steinert, 2015; Leichsenring, Luyten, et al., 2015; Shedler, 2010). Evidence-based medicine and empirically supported treatments Several proposals have been made to grade the available evidence of both medical and psychotherapeutic treatments (Canadian Task Force on the Periodic Health Examination, 1979; Chambless & Hollon, 1998; Clarke & Oxman, 2003; Cook, Guyatt, Laupacis, Sacket, & Goldberg, 1995). Apart from other differences, Contemporary Psychodynamic Psychotherapy. DOI: https://doi.org/10.1016/B978-0-12-813373-6.00004-0 © 2019 Elsevier Inc. All rights reserved. 50 Contemporary Psychodynamic Psychotherapy all available proposals regard RCTs as the gold standard for the demonstration that a treatment is effective. The most stringent test of efficacy is achieved by comparison with rival treatments, thus controlling for specific and unspecific therapeutic factors (Chambless & Hollon, 1998). For psychotherapy, the most rigorous criteria for efficacy were proposed by Chambless and Hollon (1998). For a designation of efficacious, there must be at least two RCTs, controlled single-case experiments, or equivalent time sampling designs carried out in independent research settings in which the respective treatment is superior to no treatment, placebo, or alternative treatments or equivalent to an already established treatment, with sufficient power to detect moderate differences. In addition, the use of a treatment manual or logical equivalent is required, as are reliable and valid procedures to assess diagnosis and outcome and appropriate data analysis. If there is conflicting evidence, the preponderance of the data must support the treatment’s efficacy. For a designation of possibly efficacious, one RCT (with a sample size of three or more in the case of single-case experiments) suffices in the absence of conflicting evidence. A treatment can be considered efficacious and specific if it has been shown to be superior to placebo or to an alternative bona fide treatment in at least two independent research settings (Chambless & Hollon, 1998)1. The RCT methodology is viewed as the gold standard, but it has both strengths and certain weaknesses (Seshia & Young, 2013). For example, a randomized controlled efficacy study maximizes the internal validity of a study, that is, the observed effects can be causally related to the applied treatments, at the possible expense of external validity, that is, generalizability to real-world conditions of clinical practice. In contrast, effectiveness studies investigate the effects of an intervention in routine clinical care and therefore have high external validity but at the possible expense of internal validity. Thus efficacy and effectiveness studies address different research questions. For treatments that have been evaluated in RCTs, benchmarking studies are needed to investigate their effectiveness in reallife conditions (Leichsenring, 2004). Because of their gold standard status, however, we will include only RCTs in this review. Definition of psychodynamic psychotherapy Psychodynamic therapy is an umbrella concept for treatments that operate on an interpretive-supportive continuum (Luborsky, 1984). Through interpretive interventions, insight into wishes, affects, object relations, or defense mechanisms is enhanced. Supportive interventions include fostering a therapeutic alliance, setting goals, or strengthening psychosocial capacities such as reality testing or impulse control (Luborsky, 1984). The use of more supportive or more interpretive (insightenhancing) interventions is tailored to the patient’s needs (Luborsky, 1984). A range of manualized psychodynamic therapies applying the above-mentioned 1 We would like to thank Dr. Chambless for some clarifications with regard to the criteria. The efficacy of psychodynamic psychotherapy: an up-to-date review 51 principles exists (Leichsenring, Leweke, et al., 2015; Leichsenring, Luyten, et al., 2015). These therapies vary in the extent to which they focus more on supportive or expressive elements. The empirical status of psychodynamic therapy Several meta-analyses have provided evidence for the efficacy of psychodynamic therapy. The Cochrane report by Abbass et al. (2014) showed that psychodynamic therapy is superior to control conditions in common mental disorders. The most recent meta-analysis showed that psychodynamic therapy is as efficacious as treatments with established efficacy, including CBT (Steinert, Munder, Rabung, Hoyer, & Leichsenring, 2017). This meta-analysis applied the logic of equivalence testing and controlled for research allegiance on the level of both individual studies and the meta-analysis itself (Steinert, Munder, et al., 2017). Furthermore, efficacy of the comparator in the respective disorder was ensured, that is, RCTs demonstrating its efficacy were required. Results were not affected by diagnostic group. For this chapter we have updated previous reviews on the efficacy of psychodynamic psychotherapy for specific mental disorders (Abbass et al., 2014; Fonagy, 2015; Leichsenring, Leweke, et al., 2015; Leichsenring, Luyten, et al., 2015). In most RCTs, short- to medium-term psychodynamic therapy, encompassing 8 40 sessions, was studied (Table 4.1). Several studies also included long-term psychodynamic therapy (LTPP) with a duration between 12 and 36 months. Depressive disorders In several RCTs, psychodynamic therapy was superior to waiting list control conditions or alternative treatments with regard to improving depression (Table 4.1) (Ajilchi, Nejati, Town, Wilson, & Abbass, 2016; Knekt et al., 2008; Maina, Forner, & Bogetto, 2005; Thompson, Gallagher, & Breckenridge, 1987). In addition, psychodynamic therapy was superior to treatment as usual in treatmentresistant depression (Town, Abbass, Stride, & Bernier, 2017) and in specific groups of depressed patients: patients with maternal depression (Cooper, Murray, Wilson, & Romaniuk, 2003) and patients with breast cancer (Beutel et al., 2014). Internet-guided psychodynamic self-help was reported to be superior to internetdelivered structured support (Johansson et al., 2013, 2012). Furthermore, in major depressive disorder, psychodynamic therapy combined with pharmacotherapy was found to be superior to pharmacotherapy alone or combined with supportive therapy (Burnand, Andreoli, Kolatte, Venturini, & Rosset, 2002; de Jonghe, Kool, van Aalst, Dekker, & Peen, 2001; Maina, Rosso, Crespi, & Bogetto, 2007). A small pilot study reported large effect sizes in favor of psychodynamic therapy compared to treatment as usual, but the study was not sufficiently powered for a superiority trial, and the differences did not achieve statistical significance (Connolly Gibbons et al., 2012). 52 Contemporary Psychodynamic Psychotherapy Table 4.1 Randomized controlled studies of manual-guided psychodynamic psychotherapy in specific mental disorders. Study N (psychodynamic therapy) Comparison group Duration of psychodynamic therapy 15 sessions (mean) 20 sessions, 16 weeks Major depressive disorder Ajilchi et al. (2016) 16 Waiting list: N 5 16 Barber et al. (2012) 51 Barkham et al. (1996) Connolly Gibbons et al. (2012) Driessen et al. (2013) Connolly et al. (2016) Cooper et al. (2003) 18 21 Pharmacotherapy: N 5 55Placebo: N 5 50 CBT: N 5 18 TAU: N 5 19 de Jonghe et al. (2004) 106 Johansson et al. (2012) 46 Salminen et al. (2008) Shapiro et al. (1994) Thompson et al. (1987) and GallagherThompson et al. (1990) Town et al. (2017) 26 58 24 8 vs 16 sessions 12 sessions 30 CBT: N 5 164 CBT: N 5 119 CBT: N 5 43 Counseling: N 5 48 TAU: N 5 52 Psychodynamic therapy plus pharmacotherapy: N 5 85 Structured support: N 5 46 Fluoxetine: N 5 25 CBT: N 5 59 BT: N 5 25 CBT: N 5 27 Waiting list: N 5 19 TAU: N 5 30 30 CBT: N 5 36 16 20 sessions 10 Supportive therapy: N 5 10 Waiting list: N 5 10 15 30 sessions, M 5 19.6 177 118 50 16 sessions 16 sessions 10 sessions 16 sessions 10 weeks 16 sessions 8 vs 16 sessions 16 20 sessions 20 Depressed caregivers Gallagher-Thompson and Steffen (1994) Dysthymic disorder Maina et al. (2005) Depressive disorders in patients with breast cancer Beutel et al. (2013) 78 TAU: N 5 79 Up to 25 sessions (Continued) The efficacy of psychodynamic psychotherapy: an up-to-date review 53 Table 4.1 (Continued) Study N (psychodynamic therapy) Comparison group Duration of psychodynamic therapy Psychodynamic therapy combined with pharmacotherapy for major depressive disorder Burnand et al. (2002) 35 de Jonghe et al. (2001) 72 Maina et al. (2007) 18 Comipramine: N 5 39 Pharmacotherapy: N 5 57 Brief supportive therapy combined with pharmacotherapy: N 5 17 10 weeks 16 sessions 15 30 sessions Mixed samples of patients with depressive and/or anxiety disorders Bressi et al. (2010) 30 TAU: N 5 30 Johansson et al. (2013)a 50 Knekt et al. (2008)a STPP: 101 LTPP: 128 Supportive interventions: N 5 50 Solution-focused therapy (SFT): N 5 97 40 sessions, 1 year 10 weeks LTPP: 232 sessions STPP: 18.5 sessions SFT: 9.8 sessions Complicated grief 27 Waiting list: N 5 27 12 sessions 53 Supportive therapy: N 5 54 12 sessions Bögels et al. (2014) 22 36 sessions Knijnik et al. (2004) 15 Leichsenring, Salzer, Beutel et al. (2013) and Leichsenring et al. (2014) 207 CBT: N 5 27 Waiting list: N 5 27 Credible placebo control group: N 5 15 Cognitive therapy: N 5 209 Waiting list: N 5 79 McCallum and Piper (1990) Piper et al. (2001) Social anxiety disorder 12 sessions 30 sessions (Continued) 54 Contemporary Psychodynamic Psychotherapy Table 4.1 (Continued) Study N (psychodynamic therapy) Comparison group Duration of psychodynamic therapy Psychodynamic therapy combined with pharmacotherapy for social anxiety disorder Knijnik et al. (2008, 2009) 29 Pharmacotherapy: N 5 29 12 sessions 28 CBT: N 5 29 30 sessions 27 ICBT: N 5 27 Waiting list: N 5 27 8 weeks Milrod et al. (2007) 26 24 sessions Beutel et al. (2013) Milrod et al. (2015) 36 80 Applied relaxation: N 5 23 CBT: N 5 18 CBT: 81, Applied relaxation: 39 Generalized anxiety disorder Leichsenring, Salzer, et al. (2009) Andersson et al. (2012) Panic disorder 24 sessions 19 24 sessions Psychodynamic therapy combined with pharmacotherapy for panic disorder Wiborg and Dahl (1996) 20 Pharmacotherapy alone (N 5 20) 15 sessions Psychodynamic therapy combined with pharmacotherapy for obsessivecompulsive disorder Maina et al. (2010) 27 Pharmacotherapy: N 5 30 10 16 sessions Desensitization: N 5 31 Hypnotherapy: N 5 29 Waiting list: 23 Waiting list: N 5 33 18.8 sessions Paroxetine: N 5 43 TAU: N 5 86 Medical treatment: N 5 25 8 sessions Posttraumatic stress disorder Brom et al. (1989) 29 Steinert et al. (2016, 2017) 53 5 sessions Somatoform disorders Creed et al. (2003) 59 Faramarzi et al. (2013) 24 16 sessions (Continued) The efficacy of psychodynamic psychotherapy: an up-to-date review 55 Table 4.1 (Continued) Study N (psychodynamic therapy) Comparison group Duration of psychodynamic therapy Guthrie et al. (1991) 50 8 sessions Hamilton et al. (2000) 37 Guthrie et al. (1993) 50 Monsen and Monsen (2000) Sattel et al. (2012) 20 Supportive listening: N 5 46 Supportive therapy: N 5 36 Supportive listening: N 5 46 TAU/no therapy: N 5 20 Enhanced medical care: N 5 104 107 7 sessions 8 sessions 33 sessions 12 sessions Bulimia nervosa CBT: N 5 11 Cognitive therapy: N 5 17 Nutritional counseling: N 5 10 CBT: N 5 25 CBT: N 5 36 19 46 sessions 48 Group CBT: N 5 47 Waiting list: N 5 40 16 sessions Dare et al. (2001) 21 M 5 24.9 sessions Zipfel et al. (2013) 80 Cognitive-analytic therapy: N 5 22 Family therapy: N 5 22 Routine treatment: N 5 19 Enhanced CBT (E-CBT): N 5 80 Optimized TAU (O-TAU): N 5 82 Fairburn et al. (1986) Bachar et al. (1999) 11 17 Garner et al. (1993) Poulsen et al. (2014) 25 34 19 sessions PP: 73 sessions CBT: 20 sessions Binge eating disorder Tasca et al. (2006) Anorexia nervosa Psychodynamic therapy: 39.9 sessions E-CBT: 44.8 sessions O-TAU: 50.8 sessions (Continued) 56 Contemporary Psychodynamic Psychotherapy Table 4.1 (Continued) N (psychodynamic therapy) Comparison group Duration of psychodynamic therapy Woody et al. (1983, 1990) 31 12 sessions Woody, Luborsky, McLellan, and O’Brien (1995) 57 Drug counseling (DC): N 5 35 CBT 1 DC: N 5 34 DC: N 5 27 Study Opiate addiction 26 sessions Cocaine dependence Crits-Christoph et al. (1999, 2001) 124 CBT 1 group DC: N 5 97 Individual DC: N 5 92, Individual DC 1 group DC: N 5 96 Up to 36 individual and 24 group sessions, 4 months Borderline personality disorder Bateman and Fonagy (1999, 2001) Bateman and Fonagy (2009) 19 TAU: N 5 19 18 months 71 18 months Clarkin et al. (2007) and Levy et al. (2006) 30 Doering et al. (2010) 43 Giesen-Bloo et al. (2006) 42 Structured clinical management: N 5 63 Dialecticalbehavioral therapy: N 5 30 Supportive psychodynamic therapy: N 5 30 Treatment by experienced community therapists: N 5 29 CBT: N 5 44 Gregory et al. (2008) 15 TAU: N 5 15 12 months 1 year 3 years with sessions twice a week 24.9 sessions (mean) (Continued) The efficacy of psychodynamic psychotherapy: an up-to-date review 57 Table 4.1 (Continued) Study N (psychodynamic therapy) Comparison group Duration of psychodynamic therapy Brief relational therapy: N 5 33 CBT: N 5 29 CBT: N 5 25 30 sessions CBT: N 5 21 Waiting list: N 5 18 20 sessions Minimal contact, N 5 13 Brief supportive psychotherapy, N 5 24 Communitydelivered psychodynamic therapy, N 5 76 Brief adaptive psychotherapy, N 5 30; Waiting list, N 5 26 27.7 sessions (mean) 40 sessions 55 TAU: N 5 55 8 sessions 30 Behavioral marital therapy: N 5 29 Waiting list: N 5 20 Up to 25 sessions Cluster C personality disorders Muran et al. (2005) 22 Svartberg et al. (2004) 25 40 sessions Avoidant personality disorder Emmelkamp et al. (2006) 23 Heterogeneous personality disorders Abbass et al. (2008) 14 Hellerstein et al. (1998) 25 Vinnars et al. (2005) 80 Winston et al. (1994) 25 40 sessions 40 weeks, M 5 40.3 sessions High utilizers of psychiatric services Guthrie et al. (1999) Marital distress Snyder and Wills (1989) and Snyder et al. (1991) BT, Behavior therapy; CBT, cognitive-behavioral therapy; DC, drug counseling; ICBT, internet cognitive-behavioral therapy; LTPP, long-term psychodynamic therapy; SFT, solution-focused therapy; STPP, Short-term psychodynamic therapy; TAU, treatment as usual. a The outcome was evaluated separately for depressive and anxiety disorders; only results of STPP was included in this review as for LTTP no manuals were used. 58 Contemporary Psychodynamic Psychotherapy With regard to comparisons with established treatments such as CBT or pharmacotherapy, three studies were sufficiently powered to test for equivalence or noninferiority (Connolly Gibbons et al., 2016; de Jonghe et al., 2004; Driessen et al., 2013). No statistically significant differences in outcome were found in these RCTs. However, the first study did not apply the two one-sided test procedure but instead used the traditional two-sided test (de Jonghe et al., 2004); the other RCT tested for noninferiority (Driessen et al., 2013). In this RCT, noninferiority of psychodynamic therapy compared with CBT was not shown for remission rates (21% vs 24%) but was shown for continuous measures of depression posttreatment (Driessen et al., 2013); the difference in remission rates (21% vs 24%) is minimal from a clinical perspective. In the third study, psychodynamic therapy proved to be noninferior to CBT (Connolly Gibbons et al., 2016). In addition, several RCTs have reported no differences in outcome between psychodynamic therapy and treatments with established efficacy, but these were not sufficiently powered to demonstrate equivalence if a criterion of at least 70 patients per group, as previously suggested (Leichsenring, Luyten, et al., 2015), is applied (Barber, Barrett, Gallop, Rynn, & Rickels, 2012; Barkham, 1996; GallagherThompson & Steffen, 1994; Salminen et al., 2008; Shapiro et al., 1994). Meta-analyses of even relatively few studies achieve a higher statistical power than individual studies; thus it is of note that several meta-analyses found individual psychodynamic therapy to be efficacious for depressive disorders with no differences compared to other bona fide treatments (Abbass & Driessen, 2010; Cuijpers, van Straten, Andersson, & van Oppen, 2008; Driessen et al., 2010). Complicated grief The efficacy of psychodynamic therapy for complicated grief was demonstrated in two RCTs (McCallum & Piper, 1990; Piper, McCallum, Joyce, & Ogrodniczuk, 2001). In these studies, psychodynamic therapy was superior to a waiting list condition or a supportive treatment. Anxiety disorders Several RCTs have provided evidence for the efficacy of psychodynamic therapy in the treatment of anxiety disorders (Table 4.1). For panic disorder, psychodynamic therapy was superior to applied relaxation (Milrod et al., 2007). In a recent RCT by Milrod et al. (2015) comparing psychodynamic therapy, CBT, and applied relaxation for panic disorder, a significant site-by-treatment interaction was found, with CBT being superior in one site. When overall response rates were taken into account, no significant differences between CBT and psychodynamic therapy were found (63% vs 59%; 46% for applied relaxation). In another The efficacy of psychodynamic psychotherapy: an up-to-date review 59 RCT comparison of psychodynamic therapy and CBT for panic disorder, no significant differences in remission rates were found, but the study was not sufficiently powered to show equivalence (Beutel et al., 2013). For social anxiety disorder, psychodynamic therapy was superior to a credible placebo or as efficacious as CBT (Bögels, Wijts, Oort, & Sallaerts, 2014; Knijnik, Kapczinski, Chachamovich, Margis, & Eizirik, 2004), and a recent RCT found psychodynamic therapy to be superior to a waiting list condition and to be as efficacious as CBT in all outcomes, including social anxiety, general psychopathology, and defense mechanisms (Bögels et al., 2014). In the latter study, which the authors reported to be sufficiently powered to detect medium differences (Bögels et al., 2014, p. 370), success rates were above 50% and were found to be stable at the 3- and 12-month follow-ups. In a large multicenter RCT, both psychodynamic therapy and CBT were superior to a waiting list condition (Leichsenring, Salzer, et al., 2013); no differences between psychodynamic therapy and CBT were found with regard to response rates and reduction of depression. CBT was superior with regard to remission rates, self-reported social anxiety and interpersonal problems, yet these differences were small and below the threshold defined a priori as clinically meaningful (Leichsenring, Salzer, et al., 2013). Furthermore, no differences were found with regard to long-term effects on any outcome measure 6, 12, and 24 months after the end of therapy (Leichsenring et al., 2014). Although originally designed as a superiority study to detect small differences in outcome, this study was sufficiently powered to test for equivalence if the criteria proposed above are applied. A review of social anxiety disorder was recently provided by Leichsenring and Leweke (2017). For generalized anxiety disorder an RCT reported no significant differences between psychodynamic therapy and CBT in the primary outcome measure (Hamilton Anxiety Rating Scale), but the study was not sufficiently powered for an equivalence trial (Leichsenring et al., 2009). For secondary measures (e.g., worry, depression), CBT achieved significantly better outcomes (Leichsenring et al., 2009; Salzer, Winkelbach, Leweke, Leibing, & Leichsenring, 2011). Treatment effects were stable 12 months after the end of therapy (Salzer et al., 2011). In another RCT, internet-guided psychodynamic self-help proved to be superior to a waiting list control condition for generalized anxiety disorder (Andersson et al., 2012). No differences compared to internet-guided CBT were reported, but this study was not sufficiently powered to demonstrate equivalence (Table 4.1). For a mixed sample including the various categories of anxiety disorders, short-term psychodynamic therapy was superior to LTPP (and as efficacious as solution-focused therapy) with regard to recovery at 7-month follow-up (Knekt et al., 2008). In a mixed sample of patients with depressive and/or anxiety disorders, psychodynamic therapy was superior to treatment as usual (pharmacotherapy) (Bressi, Porcellana, Marinaccio, Nocito, & Magri, 2010). The combination of psychodynamic therapy plus pharmacotherapy was shown to be superior to pharmacotherapy alone in the treatment of both social anxiety disorder (Knijnik et al., 2008, 2009) and panic disorder (Wiborg & Dahl, 1996). For panic disorder, psychodynamic therapy combined with pharmacotherapy was superior to 60 Contemporary Psychodynamic Psychotherapy pharmacotherapy alone with regard to rates of remission and relapse prevention (Wiborg & Dahl, 1996). In a recent meta-analysis, psychodynamic therapy was superior to inactive control conditions in anxiety disorders (Keefe, McCarthy, Dinger, Zilcha-Mano, & Barber, 2014); no differences were found between psychodynamic therapy and other bona fide treatments (Keefe et al., 2014). For this meta-analysis the authors reported that large and medium effect sizes between psychodynamic therapy and alternative active treatments at termination would be detected with a power of about 1.00 regardless of the degree of heterogeneity (Keefe et al., 2014). Posttraumatic stress disorder For posttraumatic stress disorder (PTSD) an RCT (Brom, Kleber, & Defares, 1989) found no statistically significant differences in outcome between psychodynamic therapy, hypnotherapy, or CBT. However, this study was not sufficiently powered to show equivalence (Table 4.1). Psychodynamic therapy was superior to a waiting list condition in two of three measures and achieved the largest within-group effect sizes at follow-up. In a recent RCT carried out in Cambodia (Steinert et al., 2016; Steinert, Bumke, et al., 2017), resource-oriented psychodynamic therapy proved to be efficacious compared to a waiting list condition. Somatoform disorders or somatic symptom disorder There is a substantial body of evidence for the efficacy of psychodynamic therapy in somatoform disorders, now referred to as somatic symptom disorder in DSM 5 (Table 4.1). Evidence from RCTs is available for irritable bowel syndrome (Creed et al., 2003; Guthrie, Creed, Dawson, & Tomenson, 1991; Guthrie, Creed, Dawson, & Tomenson, 1993), functional dyspepsia (Faramarzi et al., 2013; Hamilton et al., 2000), and somatoform pain disorder (Monsen & Monsen, 2000; Sattel et al., 2012). In each of these RCTs, psychodynamic therapy was found to be superior to treatment as usual or supportive therapy. A meta-analysis found psychodynamic therapy to be efficacious in patients with somatic disorders (Abbass, Kisely, & Kroenke, 2009). Eating disorders For bulimia nervosa, one study found that psychodynamic therapy was superior to cognitive therapy and nutritional counseling (Bachar, Latzer, Kreitler, & Berry, 1999). Two other studies found no difference between psychodynamic therapy and CBT with regard to the primary outcome measure (bulimic episodes, vomiting) (Fairburn, Kirk, O’Connor, & Cooper, 1986; Garner et al., 1993); but again, these The efficacy of psychodynamic psychotherapy: an up-to-date review 61 studies were not sufficiently powered to demonstrate equivalence (Table 4.1). Differences in favor of CBT were found in secondary measures (Fairburn et al., 1986; Garner et al., 1993). In a recent RCT, CBT was found to be superior to psychodynamic therapy (Poulsen et al., 2014). The study was controversial because the psychodynamic therapy was manualized but not symptom focused, potentially disadvantaging the psychodynamic treatment (Poulsen & Lunn, 2014; Tasca, Hilsenroth, & Thompson-Brenner, 2014). Two studies provide evidence for psychodynamic therapy in anorexia nervosa (Dare, Eisler, Russel, Treasure, & Dodge, 2001; Zipfel et al., 2013). One RCT compared manual-guided psychodynamic therapy, enhanced CBT, and optimized treatment as usual in the treatment of anorexia nervosa (Zipfel et al., 2013). At the end of treatment, significant improvements were found in all treatments, with no differences in the primary outcome measure (body mass index). At 12-month follow-up, however, psychodynamic therapy was significantly superior to optimized treatment as usual on rates of recovery, whereas enhanced CBT was not (Zipfel et al., 2013). Recovery rates were 35% for psychodynamic therapy, 19% for enhanced CBT, and 13% for optimized treatment as usual. This study was sufficiently powered to show equivalence (Table 4.1). For binge-eating disorder, psychodynamic therapy was found to be superior to a waiting list condition and to be as efficacious as CBT (Tasca et al., 2006). Two of the studies were not sufficiently powered to demonstrate equivalence to active treatments (Table 4.1) (Dare et al., 2001; Tasca et al., 2006). For the comparison with routine treatment (Dare et al., 2001) and a waiting list condition (Tasca et al., 2006), these studies were apparently sufficiently powered to show superiority. Personality disorders Cluster C personality disorders Evidence for the use of psychodynamic therapy for cluster C personality disorders was reported by two RCTs with no differences in outcome relative to CBT (Muran, Safran, Samstag, & Winston, 2005; Svartberg, Stiles, & Seltzer, 2004). These studies were not sufficiently powered to demonstrate equivalence (Table 4.1). Another RCT reported CBT as more effective than a waiting list control condition and psychodynamic therapy in the treatment of avoidant personality disorder (Emmelkamp et al., 2006). The study has attracted controversies because of possible biases (Emmelkamp, 2007; Leichsenring & Leibing, 2007), for example, whether a disorder-specific, manual-guided, bona fide version of psychodynamic therapy was used (Emmelkamp, 2007; Leichsenring & Leibing, 2007). Cluster B personality disorders Several RCTs show that borderline personality disorder can be successfully treated with psychodynamic therapy (Bateman et al., 1999; Bateman & Fonagy, 2009; 62 Contemporary Psychodynamic Psychotherapy Clarkin, Levy, Lenzenweger, & Kernberg, 2007; Doering et al., 2010; Gregory et al., 2008; Levy et al., 2006) In their initial RCT, Bateman and Fonagy (1999) found psychodynamic therapy (mentalization-based therapy, MBT) to be superior to typical treatment. In a subsequent RCT, MBT was found to be superior to a manual-guided structured clinical management (Bateman & Fonagy, 2009). MBT was superior with regard to self-reported and clinically significant problems, including suicide attempts and hospitalization. Clarkin et al. (2007) compared two types of psychodynamic therapy (transference focused therapy, TFP, and supportive psychodynamic therapy, SPT) to dialectical-behavioral therapy (DBT). No differences were found between the three treatments across several outcome measures, but TFP was superior to DBT with regard to improvements in reflective functioning and attachment (Levy et al., 2006). Only TFP and SPT were associated with improvements in anger and impulsivity, and only TFP was associated with change in irritability and verbal and direct assault (Clarkin et al., 2007). TFP demonstrated significant improvements in 10 of 12 outcome measures, DBT in 5 of 12 measures, and SPT in 6 of 12 measures (Clarkin et al., 2007). The efficacy of TFP was corroborated by another RCT showing that TFP was superior to treatment by experienced community therapists (Doering et al., 2010). Gregory et al. (2008) reported psychodynamic therapy (deconstructive therapy) to be superior to a treatment as usual condition for borderline personality disorder patients with cooccurring alcohol use disorder. Another RCT compared psychodynamic therapy (TFP) with schemafocused therapy (Giesen-Bloo et al., 2006). The authors reported statistically and clinically significant improvements for both treatments. However, schema-focused therapy was found to be superior to TFP in several outcome measures. Furthermore, a significantly higher dropout was reported for TFP. Several concerns have been raised about this study, most prominently regarding the treatment integrity of TFP (Giesen-Bloo & Arntz, 2007; Yeomans, 2007). The two studies comparing psychodynamic therapy to another active treatment were both insufficiently powered to show equivalence, but both of them reported superiority of psychodynamic therapy or the comparison condition at least in some measures (Giesen-Bloo et al., 2006; Levy et al., 2006). Heterogeneous samples of patients with personality disorders In two RCTs, psychodynamic therapy was superior to waiting list or minimal contact conditions in samples with heterogeneous personality disorders (Abbass, Sheldon, Gyra, & Kalpin, 2008; Winston et al., 1994). Another RCT found no differences in outcome between psychodynamic therapy and brief supportive therapy (Hellerstein et al., 1998). However, two of these studies (Hellerstein et al., 1998; Winston et al., 1994) were not sufficiently powered to detect possible differences between psychodynamic therapy and the comparator treatments. In a sufficiently powered study, manual-guided psychodynamic therapy was as effective as community-delivered psychodynamic therapy (Vinnars, Barber, Noren, Gallop, & Weinryb, 2005). Several meta-analyses found psychodynamic therapy to be efficacious in the treatment of personality disorders (Barber, Muran, McCarthy, & Keefe, 2013; Town, Abbass, & Hardy, 2011). The efficacy of psychodynamic psychotherapy: an up-to-date review 63 Substance-related disorders For opiate dependence, two RCTs provided evidence for the efficacy of psychodynamic therapy in several outcomes, including days worked, drug use, illegal income, depression, and general psychiatric symptoms (Woody et al., 1983; Woody et al., 1995). In one of these RCTs (Woody et al., 1983), both psychodynamic therapy and CBT were superior to drug counseling (standard treatment). No differences were found between psychodynamic therapy and CBT, but the studies were not sufficiently powered to test for equivalence. In the second study (Woody et al., 1995), psychodynamic therapy was superior to drug counseling. Thus psychodynamic therapy proved to be efficacious in opiate addiction. In contrast, both psychodynamic therapy and CBT were reported to be inferior to individual drug counseling for cocaine dependence (Crits-Christoph et al., 1999, 2001). Obsessive-compulsive disorder In the only RCT of psychodynamic therapy for obsessive-compulsive disorder, psychodynamic therapy combined with pharmacotherapy was not superior to pharmacotherapy alone (Maina, Rosso, Rigardetto, Chiado Piat, & Bogetto, 2010). High utilizers of psychiatric services Psychodynamic therapy was superior to a treatment as usual condition in high utilizers of psychiatric services (Guthrie et al., 1999). The sample primarily included patients with depressive and anxiety disorders. Relationship distress: marital therapy No significant differences were found between a psychodynamic therapy and a behavioral couple therapy with regard to individual and relationship functioning (Snyder & Wills, 1989). Both treatments were superior in this regard to a waiting list control group. Effects were maintained at 6-month follow-up. At 4-year followup, significantly more couples in the behavioral condition than in psychodynamic therapy had divorced (38% vs 3%) (Snyder, Wills, & Grady-Fletcher, 1991). The study was sufficiently powered for showing superiority but not equivalence. Long-term psychodynamic therapy for complex mental disorders In several meta-analyses, LTPP—defined as involving at least 50 sessions or lasting for at least 1 year—was shown to be superior to shorter or less intensive forms of 64 Contemporary Psychodynamic Psychotherapy treatment in patients with complex mental disorders, defined as chronic mental disorders, personality disorders, or multiple comorbid disorders (Leichsenring, Abbass, et al., 2013; Leichsenring & Rabung, 2008, 2011b). Superiority was found for improvements in target problems, general psychiatric symptoms, personality, and social functioning. These results are consistent with data on dose-effect relations, which suggest that for many patients with chronic mental disorders or personality disorders, short-term psychotherapy is not sufficient (Howard, Kopta, Krause, & Orlinsky, 1994). For these patients, long-term treatments seem to be more effective. The results of this meta-analysis were controversially discussed, for example, with regard to statistical analysis and the included comparison conditions (Bhar et al., 2010). Several responses have addressed these concerns (Leichsenring, Abbass, et al., 2013; Leichsenring & Rabung, 2011a,b). The results of the previous metaanalysis were corroborated if, for example, only active comparison conditions were included, studies previously not included were considered, or between-group effect sizes were analyzed (Leichsenring, Abbass, et al., 2013; Leichsenring & Rabung, 2011b). Thus in complex mental disorders, LTPP again proved to be superior to shorter or less intensive treatments. Analogously, we expect other forms of longterm psychotherapy to be superior to shorter forms of these treatments in treating complex mental disorders. DBT or schema-focused therapy for borderline personality disorders, for example, are also long-term treatments (Clarkin et al., 2007; Giesen-Bloo et al., 2006). Discussion Psychodynamic therapy is frequently used in clinical practice (Norcross & Rogan, 2013). Efficacy research, however, has been neglected in psychodynamic therapy for a long time. There remain concerns among some psychodynamic therapists and researchers about applying the methodology of RCTs to psychodynamic therapy (Westen, Novotny, & Thompson-Brenner, 2004). While it is true, for example, that studying unconscious conflicts or processes poses a unique challenge to research on psychodynamic therapy, the outcome of psychodynamic therapy in the form of observable manifestations of improvement may be studied. With regard to the problem of treatment manualization, the available RCTs using treatment manuals show that the complex interpersonal process of psychodynamic therapy can be manualized (Table 4.1), but treatment manuals should not be mistaken as cookbooks. Current manuals allow for a wide range of flexibility in therapist behavior (Leichsenring & Salzer, 2014; Leichsenring & Schauenburg, 2014; Leichsenring & Steinert, 2017b). Even LTPP may be manual-guided, as shown by the RCTs by Bateman and Fonagy (2009), Clarkin et al. (2007), and Vinnars et al. (2005) Furthermore, the methodological quality of studies of psychodynamic therapy was shown to be comparable to those of CBT (Gerber et al., 2011; Thoma et al., 2012), demonstrating that the methodology of RCTs may be as adequately applied to psychodynamic therapy as to CBT. The efficacy of psychodynamic psychotherapy: an up-to-date review 65 In recent years, efficacy research on psychodynamic therapy has caught up, and evidence is beginning to accumulate (Abbass et al., 2014; Barber et al., 2013; Steinert, Munder, et al., 2017). According to the results presented in this review, there is substantial evidence for the efficacy of psychodynamic therapy in depressive, anxiety, somatoform, eating, substance-related, and personality disorders. This is consistent with a recent Cochrane Report that found psychodynamic therapy to be efficacious in common mental disorders (Abbass et al., 2014). Effects of psychodynamic therapy were found to be stable or even increased in follow-up assessments (Abbass et al., 2009, 2014; Leichsenring & Rabung, 2008). Although there is a growing body of evidence for the efficacy of psychodynamic therapy, there are also some limitations. Only a few studies exist that are sufficiently powered to show equivalence to an alternative treatment (Leichsenring, Luyten, et al., 2015). However, this is true for CBT as well (Cuijpers, 2016). With regard to the comparison of psychodynamic therapy and CBT, no substantial differences in efficacy were found in the studies that were sufficiently powered for testing equivalence (Crits-Christoph et al., 1999; Driessen et al., 2013; Leichsenring, Luyten, et al., 2015; Leichsenring et al., 2014; Zipfel et al., 2013). Equivalence of psychodynamic therapy to treatments established in efficacy was recently explicitly tested and demonstrated (Steinert, Munder, et al., 2017). If future research confirms that there are no substantial differences in outcome between the different forms of bona fide psychotherapy in common mental disorders, the next question becomes which patients benefit more from which kind of therapy, such as is addressed by Piper et al. (2001). In the RCTs included here, various methods of psychodynamic therapy were used (Table 4.1). However, from an empirical perspective, it is not clear how “different” the various approaches really are. For the treatment of anxiety disorders and depressive disorders, the various approaches were shown to be consistent with each other and to overlap to a high degree (Leichsenring & Salzer, 2014; Leichsenring & Schauenburg, 2014; Leichsenring, & Steinert, 2018). Thus developing unified or transdiagnostic protocols for the psychodynamic treatment of major mental disorders is possible and may be an important target for future research and practice. Nevertheless, open questions remain requiring further research on psychodynamic therapy. For specific mental disorders, further RCTs are required. This applies, for instance, to obsessive-compulsive disorder and PTSD. For PTSD, only two RCTs exist (Brom et al., 1989; Steinert, Bumke, et al., 2017). Further, more adequately powered equivalence trials are needed. In future studies of psychodynamic therapy, not only measures of symptoms or DSM criteria should be applied, but also measures more specific to psychodynamic therapy. Future studies should also examine whether there are specific gains achieved only by psychodynamic therapy; this is known as the question of “added value.” Such an added value was demonstrated, for example, by Levy et al. (2006) comparing psychodynamic therapy to DBT with regard to improvements in reflective functioning and attachment. Research should address the mechanisms of change not only of psychodynamic 66 Contemporary Psychodynamic Psychotherapy therapy, but also of other bona fide treatments beyond brand names of treatment. This is important to further improve the treatments. Last but not least, more attention needs to be devoted to the question of what works for whom with regard to patient characteristics beyond the diagnosis. At present, no method of psychotherapy may claim to be the gold standard (Leichsenring & Steinert, 2017a). Monocultures have rarely proved to be successful. A plurality of (evidence-based) therapies is to be welcomed, both in treatment and research. Only plurality allows for bridging the gaps between the different approaches and for learning from each other to further improve the treatment of patients with mental disorders (Roy-Byrne, 2017). References Abbass, A., & Driessen, E. (2010). The efficacy of short-term psychodynamic psychotherapy for depression: A summary of recent findings. Acta Psychiatrica Scandinavica, 121, 398 399. Abbass, A., Sheldon, A., Gyra, J., & Kalpin, A. (2008). Intensive short-term dynamic psychotherapy for DSM-IV personality disorders: A randomized controlled trial. Journal of Nervous and Mental Disease, 196(3), 211 216. Available from https://doi.org/10.1097/ NMD.0b013e3181662ff0. Abbass, A. A., Kisely, S., & Kroenke, K. (2009). Short-term psychodynamic psychotherapy for somatic disorders. Systematic review and meta-analysis of clinical trials. Psychotherapy and Psychosomatics, 78, 265 274. Abbass, A. A., Kisely, S. R., Town, J. M., Leichsenring, F., Driessen, E., De Maat, S., . . . Crowe, E. (2014). Short-term psychodynamic psychotherapies for common mental disorders. Cochrane Database of Systematic Reviews, 1(7), CD004687. Available from https://doi.org/10.1002/14651858.CD004687.pub4. Ajilchi, B., Nejati, V., Town, J. M., Wilson, R., & Abbass, A. (2016). Effects of intensive short-term dynamic psychotherapy on depressive symptoms and executive functioning in major depression. Journal of Nervous and Mental Disease, 204(7), 500 505. Available from https://doi.org/10.1097/NMD.0000000000000518. Andersson, G., Paxling, B., Roch-Norlund, P., Östman, G., Norgren, A., Almlöv, J., . . . Silverberg, F. (2012). Internet-based psychodynamic versus cognitive behavioral guided self-help for generalized anxiety disorder: A randomized controlled trial. Psychotherapy and Psychosomatics, 81, 344 355. Bachar, E., Latzer, Y., Kreitler, S., & Berry, E. M. (1999). Empirical comparison of two psychological therapies: Self psychology and cognitive orientation in the treatment of anorexia and bulimia. Journal of Psychotherapy Practice and Research, 8, 115 128. Barber, J., Barrett, M., Gallop, R., Rynn, M., & Rickels, K. (2012). Short-term dynamic psychotherapy versus pharmacotherapy for major depressive disorder: A randomized, placebo-controlled trial. Journal of Clinical Psychiatry, 73, 66 73. Barber, J. P., Muran, J. C., McCarthy, K. S., & Keefe, R. J. (2013). Research on psychodynamic therapies. In M. J. Lambert (Ed.), Bergin and Garfield’s handbook of psychotherapy and behavior change (6th ed., pp. 443 494). New York, NY: Wiley. Barkham, M., Rees, A., Shapiro, D. A., Stiles, W. B., Agnew, R. M., Halstead, J., . . . Harrington, V. (1996). Outcomes of time-limited psychotherapy in applied settings: Replication of the second Sheffield psychotherapy project. Journal of Consulting and Clinical Psychology, 64, 1079 1085. The efficacy of psychodynamic psychotherapy: an up-to-date review 67 Bateman, A., & Fonagy, P. (1999). The effectiveness of partial hospitalization in the treatment of borderline personality disorder: A randomized controlled trial. American Journal of Psychiatry, 156, 1563 1569. Bateman, A., & Fonagy, P. (2001). Treatment of borderline personality disorder with psychoanalytically oriented partial hospitalization: An 18-month follow-up. American Journal of Psychiatry, 158, 36 42. Bateman, A., & Fonagy, P. (2009). Randomized controlled trial of outpatient mentalizationbased treatment versus structured clinical management for borderline personality disorder. American Journal of Psychiatry, 166, 1355 1364. Beutel, M. E., Scheurich, V., Knebel, A., Michal, M., Wiltink, J., Graf-Morgenstern, M., . . . Subic-Wrana, C. (2013). Implementing panic-focused psychodynamic psychotherapy into clinical practice. (Randomized Controlled Trial) Canadian Journal of Psychiatry, 58(6), 326 334. Beutel, M. E., Weissflog, G., Leuteritz, K., Wiltink, J., Haselbacher, A., Ruckes, C., . . . Brähler, E. (2014). Efficacy of short-term psychodynamic psychotherapy (STPP) with depressed breast cancer patients: Results of a randomized controlled multicenter trial. Annals of Oncology, 25 (2), 378 384. Available from https://doi.org/10.1093/annonc/mdt526. Bhar, S. S., Thombs, B. D., Pignotti, M., Bassel, M., Jewett, L., Coyne, J. C., & Beck, A. T. (2010). Is longer-term psychodynamic psychotherapy more effective than shorter-term therapies? Review and critique of the evidence. Psychotherapy and Psychosomatics, 79, 208 216. Bögels, S. M., Wijts, P., Oort, F. J., & Sallaerts, S. J. (2014). Psychodynamic psychotherapy versus cognitive behavior therapy for social anxiety disorder: An efficacy and partial effectiveness trial. Depression and Anxiety, 31(5), 363 373. Available from https://doi. org/10.1002/da.22246. Bressi, C., Porcellana, M., Marinaccio, P. M., Nocito, E. P., & Magri, L. (2010). Short-term psychodynamic psychotherapy versus treatment as usual for depressive and anxiety disorders: A randomized clinical trial of efficacy. Journal of Nervous and Mental Disease, 198(9), 647 652. Brom, D., Kleber, R. J., & Defares, P. B. (1989). Brief psychotherapy for posttraumatic stress disorders. Journal of Consutling and Clinical Psychology, 57, 607 612. Burnand, Y., Andreoli, A., Kolatte, E., Venturini, A., & Rosset, N. (2002). Psychodynamic psychotherapy and clomipramine in the treatment of major depression. Psychiatric Services, 53, 585 590. Canadian Task Force on the Periodic Health Examination. (1979). The periodic health examination. Canadian Medical Association Journal, 121, 1193 1254. Chambless, D. L., & Hollon, S. D. (1998). Defining empirically supported therapies. Journal of Consulting and Clinical Psychology, 66, 7 18. Clarke, M., & Oxman, A.D. (2003). Cochrane Reviewers’ Handbook 4.1.6 (updated January 2003) (Vol. Issue 1). Oxford: Update Software. Updated quarterly. Clarkin, J. F., Levy, K. N., Lenzenweger, M. F., & Kernberg, O. F. (2007). Evaluating three treatments for borderline personality disorder: A multiwave study. American Journal of Psychiatry, 164(6), 922 928. Connolly Gibbons, M. B., Crits-Christoph, P., & Hearon, B. (2008). The empirical status of psychodynamic therapies. Annual Review of Clinical Psychology, 4, 93 108. Connolly Gibbons, M. B., Gallop, R., Thompson, D., Luther, D., Crits-Christoph, K., Jacobs, J., . . . Crits-Christoph, P. (2016). Comparative effectiveness of cognitive therapy and dynamic psychotherapy for major depressive disorder in a community mental health setting: A randomized clinical noninferiority trial. JAMA Psychiatry, 73(9), 904 911. Available from https://doi.org/10.1001/jamapsychiatry.2016.1720. 68 Contemporary Psychodynamic Psychotherapy Connolly Gibbons, M. B., Thompson, S. M., Scott, K., Schauble, L. A., Mooney, T., Thompson, D., . . . Crits-Christoph, P. (2012). Supportive-expressive dynamic psychotherapy in the community mental health system: A pilot effectiveness trial for the treatment of depression. Psychotherapy, 49, 303 316. Cook, D. J., Guyatt, G. H., Laupacis, A., Sacket, D. L., & Goldberg, R. J. (1995). Clinical recommendations using levels of evidence for antithrombotic agents. Chest, 108(4 Suppl.), 227S 230S. Cook, J. M., Biyanova, T., Elhai, J., Schnurr, P. P., & Coyne, J. C. (2010). What do psychotherapists really do in practice? An internet study of over 2.000 practitioners. Psychotherapy, 47, 260 267. Cooper, P. J., Murray, L., Wilson, A., & Romaniuk, H. (2003). Controlled trial of the shortand long-term effect of psychological treatment of post-partum depression. I. Impact on maternal mood. British Journal of Psychiatry, 182, 412 419. Creed, F., Fernandes, L., Guthrie, E., Palmer, S., Ratcliffe, J., Read, N., . . . North of England IBS Research Group. (2003). The cost-effectiveness of psychotherapy and paroxetine for severe irritable bowel syndrome. Gastroenterology, 124, 303 317. Crits-Christoph, P., Siqueland, L., Blaine, J., Frank, A., Luborsky, L., Onken, L. S., . . . Beck, A. T. (1999). Psychosocial treatments for cocaine dependence: National Institute on Drug Abuse Collaborative Cocaine Treatment Study. Archives of General Psychiatry, 56, 493 502. Crits-Christoph, P., Siqueland, L., McCalmont, E., Weiss, R. D., Gastfriend, D. R., Frank, A., . . . Thase, M. E. (2001). Impact of psychosocial treatments on associated problems of cocaine-dependent patients. Journal of Consulting and Clinical Psychology, 69, 825 830. Cuijpers, P. (2016). Are all psychotherapies equally effective in the treatment of adult depression? The lack of statistical power of comparative outcome studies. Evidence-Based Mental Health, 19(2), 39 42. Available from https://doi.org/10.1136/eb-2016-102341. Cuijpers, P., van Straten, A., Andersson, G., & van Oppen, P. (2008). Psychotherapy for depression in adults: A meta-analysis of comparative outcome studies. Journal of Consulting and Clinical Psychology, 76, 909 922. Dare, C., Eisler., Russel, G., Treasure, J., & Dodge, L. (2001). Psychological therapies for adults with anorexia nervosa: Randomised controlled trial of out-patient treatments. British Journal of Psychiatry, 178, 216 221. de Jonghe, F., Hendricksen, M., van Aalst, G., Kool, S., Peen, V., Van, R., . . . Dekker, J. (2004). Psychotherapy alone and combined with pharmacotherapy in the treatment of depression. British Journal of Psychiatry, 185, 37 45. de Jonghe, F., Kool, S., van Aalst, G., Dekker, J., & Peen, J. (2001). Combining psychotherapy and antidepressants in the treatment of depression. Journal of Affective Disorders, 64, 217 229. DeRubeis, R. J., & Crits-Christoph, P. (1998). Empirically supported individual and group psychological treatments for adult mental disorders. Journal of Consulting and Clinical Psychology, 66, 37 52. Doering, S., Horz, S., Rentrop, M., Fischer-Kern, M., Schuster, P., Benecke, C., . . . Buchheim, P. (2010). Transference-focused psychotherapy v. treatment by community psychotherapists for borderline personality disorder: Randomised controlled trial. British Journal of Psychiatry, 196, 389 395. Driessen, E., Cuipers, P., deMaat, S. C. M., Abbass, A., deJonghe, F., & Dekker, J. J. M. (2010). The effiacy of short-term psychodynamic psychotherapy for depression: A metaanalysis. Clinical Psychology Review, 30, 25 36. The efficacy of psychodynamic psychotherapy: an up-to-date review 69 Driessen, E., Van, H. L., Don, F. J., Peen, J., Kool, S., Westra, D., . . . Dekker, J. J. (2013). The efficacy of cognitive-behavioural therapy and psychodynamic therapy in the outpatient treatment of major depression: A randomized clinical trial. American Journal of Psychiatry, 170, 1041 1050. Emmelkamp, P. (2007). Author’s reply. British Journal of Psychiatry, 190, 80 81. Emmelkamp, P., Benner, A., Kuipers, A., Feiertag, G., Koster, H. C., & van Appelddorn, F. J. (2006). Comparison of brief dynamic and cognitive-behavioral therapies in avoidant personality disorder. British Journal of Psychiatry, 189, 60 64. Fairburn, C., Kirk, J., O’Connor, M., & Cooper, P. J. (1986). A comparison of two psychological treatments for bulimia nervosa. Behaviour Research and Therapy, 24, 629 643. Faramarzi, M., Azadfallah, P., Book, H. E., Tabatabaei, K. R., Taheri, H., & Shokri-shirvani, J. (2013). A randomized controlled trial of brief psychoanalytic psychotherapy in patients with functional dyspepsia. Asian Journal of Psychiatry, 6, 228 234. Fonagy, P. (2015). The effectiveness of psychodynamic psychotherapies: An update. World Psychiatry, 14(2), 137 150. Available from https://doi.org/10.1002/wps.20235. Gallagher-Thompson, D., Hanley-Peterson, P., & Thompson, L. W. (1990). Maintenance of gains versus relapse following brief psychotherapy for depression. J Consult Clin Psychology, 58, 371 374. Gallagher-Thompson, D. E., & Steffen, A. M. (1994). Comparative effects of cognitivebehavioral and brief psychodynamic psychotherapies for depressed family caregivers. Journal of Consulting and Clinical Psychology, 62, 543 549. Garner, D. M., Rockert, W., Davis, R., Garner, M. V., Olmsted, M. P., & Eagle, M. (1993). Comparison of cognitive-behavioral and supportive-expressive therapy for bulimia nervosa. American Journal of Psychiatry, 150, 37 46. Gerber, A. J., Kocsis, J. H., Milrod, B. L., Roose, S. P., Barber, J. P., Thase, M. E., . . . Leon, A. C. (2011). A quality-based review of randomized controlled trials of psychodynamic psychotherapy. American Journal of Psychiatry, 168, 19 28. Giesen-Bloo, J., & Arntz, A. (2007). Questions concerning the randomized trial of schemafocused therapy vs transference-focused psychotherapy Reply. Archives of General Psychiatry, 64, 610 611. Giesen-Bloo, J., van Dyck, R., Spinhoven, P., van Tilburg, W., Dirksen, C., van Asselt, T., . . . Arntz, A. (2006). Outpatient psychotherapy for borderline personality disorder: Randomized trial of schema-focused therapy vs transference-focused psychotherapy. Archives of General Psychiatry, 63, 649 658. Gregory, R. J., Chlebowski, S., Kang, D., Remen, A. L., Soderberg, M. G., Stepkovitch, J., & Virk, S. (2008). A controlled trial of psychodynamic psychotherapy for co-occurring borderline personality disorder and alcohol use disorder. Psychotherapy, 45, 28 41. Guthrie, E., Creed, F., Dawson, D., & Tomenson, B. (1991). A controlled trial of psychological treatment for the irritable bowel syndrome. Gastroenetrology, 100, 450 457. Guthrie, E., Creed, F., Dawson, D., & Tomenson, B. (1993). A randomised controlled trial of psychotherapy in patients with refractory irritable bowel syndrome. British Journal of Psychiatry, 163, 315 321. Guthrie, E., Moorey, J., Margison, F., Barker, H., Palmer, S., McGrath, G., . . . Creed, F. (1999). Cost-effectiveness of brief psychodynamic-interpersonal therapy in high utilizers of psychiatric services. Archives of General Psychiatry, 56, 519 526. Hamilton, J., Guthrie, E., Creed, F., Thompson, D., Tomenson, B., Bennett, R., . . . Liston, R. (2000). A randomized controlled trial of psychotherapy in patients with chronic functional dyspepsia. Gastroenterology, 119, 661 669. 70 Contemporary Psychodynamic Psychotherapy Hellerstein, D. J., Rosenthal, R. N., Pinsker, H., Samstag, L. W., Muran, J. C., & Winston, A. (1998). A randomized prospective study comparing supportive and dynamic therapies. Outcome and alliance. Journal of Psychotherapy Practice and Research, 7, 261 271. Howard, K. I., Kopta, S. M., Krause, M. S., & Orlinsky, D. E. (1994). The dose-effect relationship in psychotherapy. American Psychologist, 41, 159 164. Johansson, R., Björklund, M., Hornborg, C., Karlsson, S., Hesser, H., Ljotsson, B., . . . Andersson, G. (2013). Affect-focused psychodynamic psychotherapy for depression and anxiety through the internet: A randomized controlled trial. PeerJ, 102, 1 22. Johansson, R., Ekbladh, S., Hebert, A., Lindström, M., Möller, S., Petitt, E., . . . Andersson, G. (2012). Psychodynamic guided self-help for adult depression through the internet: A randomised controlled trial. PLoS One, 7(5), e38021. Keefe, J. R., McCarthy, K. S., Dinger, U., Zilcha-Mano, S., & Barber, J. P. (2014). A metaanalytic review of psychodynamic therapies for anxiety disorders. Clinical Psychology Review, 34(4), 309 323. Available from https://doi.org/10.1016/j.cpr.2014.03.004. Knekt, P., Lindfors, O., Harkanen, T., Valikoski, M., Virtala, E., Laaksonen, M. A., . . . Helsinki Psychotherapy Study Group. (2008). Randomized trial on the effectiveness of long-and short-term psychodynamic psychotherapy and solution-focused therapy on psychiatric symptoms during a 3-year follow-up. Psychological Medicine, 38, 689 703. Knijnik, D. Z., Blanco, C., Salum, G. A., Moraes, C. U., Mombach, C., Almeida, E., . . . Eizirik, C. L. (2008). A pilot study of clonazepam versus psychodynamic group therapy plus clonazepam in the treatment of generalized social anxiety disorder. European Psychiatry, 23, 567 574. Knijnik, D. Z., Kapczinski, F., Chachamovich, E., Margis, R., & Eizirik, C. L. (2004). Psychodynamic group treatment for generalized social phobia. Revista Brasileira de Psiquiatria, 26, 77 781. Knijnik, D. Z., Salum, G. A. J., Blanco, C., Moraes, C., Hauck, S., Mombach, C. K., . . . Eizirik, C. L. (2009). Defense style changes with the addition of psychodynamic group therapy to clonazepam in social anxiety disorder. Journal of Nervous and Mental Disease, 197, 547 551. Leichsenring, F. (2004). Randomized controlled versus naturalistic studies: A new research agenda. Bulletin of the Menninger Clinic, 68(2), 137 151. Available from https://doi. org/10.1521/bumc.68.2.137.35952. Leichsenring, F., Abbass, A., Luyten, P., Hilsenroth, P., & Rabung, S. (2013). The emerging evidence for long-term psychodynamic therapy. Psychodynamic Psychiatry, 41, 361 384. Leichsenring, F., & Leibing, E. (2007). Fair play, please! Letter to the editor. British Journal of Psychiatry, 190, 80. Leichsenring, F., & Leweke, F. (2017). Social anxiety disorder. New England Journal of Medicine, 376(23), 2255 2264. Available from https://doi.org/10.1056/ NEJMcp1614701. Leichsenring, F., Leweke, F., Klein, S., & Steinert, C. (2015). The empirical status of psychodynamic psychotherapy An update: Bambi’s alive and kicking. (Review) Psychotherapy and Psychosomatics, 84(3), 129 148. Available from https://doi.org/ 10.1159/000376584. Leichsenring, F., Luyten, P., Hilsenroth, M. J., Abbass, A., Barber, J. P., Keefe, J. R., . . . Steiner, C. (2015). Psychodynamic therapy meets evidence-based medicine: A systematic review using updated criteria. (Review) Lancet Psychiatry, 2(7), 648 660. Available from https://doi.org/10.1016/S2215-0366(15)00155-8. The efficacy of psychodynamic psychotherapy: an up-to-date review 71 Leichsenring, F., & Rabung, S. (2008). Effectiveness of long-term psychodynamic psychotherapy: A meta-analysis. (Meta-Analysis) JAMA, 300(13), 1551 1565. Available from https://doi.org/10.1001/jama.300.13.1551. Leichsenring, F., & Rabung, S. (2011a). Double standards in psychotherapy research. Psychotherapy and Psychosomatics, 80, 48 51. Leichsenring, F., & Rabung, S. (2011b). Long-term psychodynamic psychotherapy in complex mental disorders: Update of a meta-analysis. (Meta-Analysis Review) British Journal of Psychiatry, 199(1), 15 22. Available from https://doi.org/10.1192/bjp.bp.110.082776. Leichsenring, F., & Salzer, S. (2014). A unified protocol for the transdiagnostic psychodynamic treatment of anxiety disorders: An evidence-based approach. Psychotherapy (Chicago, III), 51(2), 224 245. Available from https://doi.org/10.1037/a0033815. Leichsenring, F., Salzer, S., Beutel, M. E., Herpertz, S., Hiller, W., Hoyer, J., . . . Leibing, E. (2013). Psychodynamic therapy and cognitive-behavioral therapy in social anxiety disorder: A multicenter randomized controlled trial. American Journal of Psychiatry, 170, 759 767. Leichsenring, F., Salzer, S., Beutel, M. E., Herpertz, S., Hiller, W., Hoyer, J., . . . Leibing, E. (2014). Long-term outcome of psychodynamic therapy and cognitive-behavioral therapy in social anxiety disorder. American Journal of Psychiatry, 171(10), 1074 1082. Available from https://doi.org/10.1176/appi.ajp.2014.13111514. Leichsenring, F., Salzer, S., Jaeger, U., Kachele, H., Kreische, R., Leweke, F., . . . Leibing, E. (2009). Short-term psychodynamic psychotherapy and cognitive-behavioral therapy in generalized anxiety disorder: A randomized, controlled trial. American Journal of Psychiatry, 166(8), 875 881. Available from https://doi.org/10.1176/appi.ajp.2009.09030441. Leichsenring, F., & Schauenburg, H. (2014). Empirically supported methods of short-term psychodynamic therapy in depression Towards an evidence-based unified protocol. (Review) Journal of Affective Disorders, 169C, 128 143. Available from https://doi. org/10.1016/j.jad.2014.08.007. Leichsenring, F., & Steinert, C. (2017a). Is cognitive behavioral therapy the gold standard for psychotherapy?: The need for plurality in treatment and research. JAMA, 318(14), 1323 1324. Available from https://doi.org/10.1001/jama.2017.13737. Leichsenring, F., & Steinert, C. (2017b). Short-term psychodynamic therapy for obsessivecompulsive disorder: A manual-guided approach to treating the “inhibited rebel. Bulletin of the Menninger Clinic, 81(4), 341 389. Available from https://doi.org/10.1521/ bumc_2017_81_07. Leichsenring, F., & Steinert, C. (2018). Towards an evidence-based unified psychodynamic protocol for emotional disorders. Journal of Affective Disorders, 232, 400 416. Levy, K. N., Meehan, K. B., Kelly, K. M., Reynoso, J. S., Weber, M., Clarkin, J. F., & Kernberg, O. F. (2006). Change in attachment patterns and reflective function in a randomized control trial of transference-focused psychotherapy for borderline personality disorder. Journal of Consulting and Clinical Psychology, 74, 1027 1040. Luborsky, L. (1984). Principles of psychoanalytic psychotherapy. Manual for supportiveexpressive treatment. New York: Basic Books. Maina, G., Forner, F., & Bogetto, F. (2005). Randomized controlled trial comparing brief dynamic and supportive therapy with waiting list condition in minor depressive disorders. Psychotherapy and Psychosomatics, 74, 3 50. Maina, G., Rosso, G., Crespi, C., & Bogetto, F. (2007). Combined brief dynamic therapy and pharmacotherapy in the treatment of major depressive disorder: A pilot study. Psychotherapy and Psychosomatics, 76, 298 305. 72 Contemporary Psychodynamic Psychotherapy Maina, G., Rosso, G., Rigardetto, S., Chiado Piat, S., & Bogetto, F. (2010). No effect of adding brief dynamic therapy to pharmacotherapy in the treatment of obsessive-compulsive disorder with concurrent major depression. (Randomized Controlled Trial) Psychotherapy and Psychosomatics, 79(5), 295 302. Available from https://doi.org/ 10.1159/000318296. McCallum, M., & Piper, W. E. (1990). A controlled study of effectiveness and patient suitablility for short-term group psychotherapy. International Journal of Group Psychotherapy, 40, 431 452. Milrod, B., Chambless, D. L., Gallop, R., Busch, F. N., Schwalberg, M., McCarthy, K. S., . . . Barber, J. P. (2015). Psychotherapies for panic disorder: A tale of two sites. Journal of Clinical Psychiatry, 77(7), 927 935. Available from https://doi.org/10.4088/ JCP.14m09507. Milrod, B., Leon, A. C., Busch, F., Rudden, M., Schwalberg, M., Clarkin, J., . . . Shear, M. K. (2007). A randomized controlled clinical trial of psychoanalytic psychotherapy for panic disorder. American Journal of Psychiatry, 164(2), 265 272. Available from https://doi.org/10.1176/ajp.2007.164.2.265. Monsen, K., & Monsen, T. J. (2000). Chronic pain and psychodynamic body therapy. Psychotherapy, 37, 257 269. Muran, J. C., Safran, J. D., Samstag, L. W., & Winston, A. (2005). Evaluating an alliancefocused treatment for personality disorders. Psychotherapy, 42, 532 545. Norcross, J. C., Hedges, M., & Castle, P. H. (2002). Psychologists conducting psychotherapy in 2001: A study of the division 29 membership. Psychotherapy: Theory, Research, Practice, Training, 39, 97 102. Norcross, J. C., & Rogan, J. D. (2013). Psychologists conducting psychotherapy in 2012: Current practices and historical trends among division 29 members. Psychotherapy, 50 (4), 490 495. Available from https://doi.org/10.1037/a0033512. Piper, W. E., McCallum, M., Joyce, A. S., & Ogrodniczuk, J. (2001). Patient personality and time-limited group psychotherapy for complicated grief. International Journal of Group Psychotherapy, 51, 525 552. Poulsen, S., & Lunn, S. (2014). Response to Tasca et al. American Journal of Psychiatry, 171(5), 584. Poulsen, S., Lunn, S., Daniel, S. I., Folke, S., Mathiesen, B. B., Katznelson, H., & Fairburn, C. G. (2014). A randomized controlled trial of psychoanalytic psychotherapy or cognitive-behavioral therapy for bulimia nervosa. American Journal of Psychiatry, 171 (1), 109 116. Available from https://doi.org/10.1176/appi.ajp.2013.12121511. Roy-Byrne, P. (2017). Transdiagnostic cognitive-behavioral therapy and the return of the repressed. JAMA Psychiatry, 74(9), 867 868. Available from https://doi.org/10.1001/ jamapsychiatry.2017.1982. Salminen, J. K., Karlsson, H., Hietala, J., Kajander, J., Aalto, S., Markkula, J., . . . Toikka, T. (2008). Short-term psychodynamic psychotherapy and fluoxetine in major depressive disorder: A randomized comparative study. Psychotherapy and Psychosomatics, 77, 351 357. Salzer, S., Winkelbach, C., Leweke, F., Leibing, E., & Leichsenring, F. (2011). Long-term effects of short-term psychodynamic psychotherapy and cognitive-behavioral therapy in generalized anxiety disorder: 12-Month follow-up. Canadian Journal of Psychiatry, 56, 503 508. Sattel, H., Lahmann, C., Gündel, H., Guthrie, E., Kruse, J., Noll-Hussong, M., . . . Henningsen, P. (2012). Brief psychodynamic interpersonal psychotherapy for patients with multisomatoform disorder: randomised controlled trial. British Journal of Psychiatry, 200, 60 67. The efficacy of psychodynamic psychotherapy: an up-to-date review 73 Seshia, S. S., & Young, G. B. (2013). The evidence-based medicine paradigm: Where are we 20 years later? Part 1. (Review) Canadian Journal of Neurological Sciences, 40(4), 465 474. Shapiro, D. A., Barkham, M., Rees, A., Hardy, G. E., Reynolds, S., & Startup, M. (1994). Effects of treatment duration and severity of depression on the effectiveness of cognitive-behavioral and psychodynamic-interpersonal psychotherapy. Journal of Consulting and Clinical Psychology, 62, 522 534. Shedler, J. (2010). The efficacy of psychodynamic psychotherapy. American Psychologist, 65, 98 109. Snyder, D. K., & Wills, R. M. (1989). Behavioral vs. insight-oriented marital therapy: Effects on individual and interspousal functioning. Journal of Consulting and Clinical Psychology, 57, 39 46. Snyder, D. K., Wills, R. M., & Grady-Fletcher, A. (1991). Long-term effectiveness of behavioral versus insight-oriented marital therapy: A 4-year follow-up study. Journal of Consulting and Clinical Psychology, 59(1), 138 141. Steinert, C., Bumke, P. J., Hollekamp, R. L., Larisch, A., Leichsenring, F., Matthess, H., . . . Kruse, J. (2016). Treating post-traumatic stress disorder by resource activation in Cambodia. (Letter) World Psychiatry, 15(2), 183 185. Available from https://doi.org/ 10.1002/wps.20303. Steinert, C., Bumke, P. J., Hollekamp, R. L., Larisch, A., Leichsenring, F., Matthess, H., . . . Kruse, J. (2017). Resource activation for treating post-traumatic stress disorder, comorbid symptoms and impaired functioning: A randomized controlled trial in Cambodia. Psychological Medicine, 47(3), 553 564. Available from https://doi.org/ 10.1017/S0033291716002592. Steinert, C., Munder, T., Rabung, S., Hoyer, J., & Leichsenring, F. (2017). Psychodynamic therapy: As efficacious as other empirically supported treatments? A meta-analysis testing equivalence of outcomes. American Journal of Psychiatry, 174(10), 943 953. Available from https://doi.org/10.1176/appi.ajp.2017.17010057. Svartberg, M., Stiles, T. C., & Seltzer, M. H. (2004). Randomized, controlled trial of the effectiveness of short-term dynamic psychotherapy and cognitive therapy for cluster C personality disorders. American Journal of Psychiatry, 161, 810 817. Tasca, G., Hilsenroth, M., & Thompson-Brenner, H. (2014). Psychoanalytic psychotherapy or cognitive-behavioral therapy for bulimia nervosa: Considering these findings in context. (Letter to editor) American Journal of Psychiatry, 17(5), 583 584. Tasca, G. A., Ritchie, K., Conrad, G., Balfour, L., Gayrton, J., Lybanon, V., & Bissada, H. (2006). Attachment scales predict outcome in a randomized clinical trial of group psychotherapy for binge eating disorder: An aptitude by treatment interaction. Psychotherapy Research, 16, 106 121. Task force on promotion and dissemination of psychological procedures. (1995). Training and Dissemination of empirically-validated psychological treatments. Report and recommendations. The Clinical Psychology, 48, 3 23. Thoma, N. C., McKay, D., Gerber, A. J., Milrod, B. L., Edwards, A. R., & Kocsis, J. H. (2012). A quality-based review of randomized controlled trials of cognitive-behavioral therapy for depression: An assessment and metaregression. American Journal of Psychiatry, 169, 22 30. Thompson, L. W., Gallagher, D., & Breckenridge, J. S. (1987). Comparative effectiveness of psychotherapies for depressed elders. Journal of Consulting and Clinical Psychology, 55, 385 390. Town, J. M., Abbass, A., & Hardy, G. (2011). Short-term psychodynamic psychotherapy for personality disorders: A critical review of randomized controlled trials. (Meta-Analysis Review) Journal of Personality Disorders, 25(6), 723 740. Available from https://doi. org/10.1521/pedi.2011.25.6.723. 74 Contemporary Psychodynamic Psychotherapy Town, J. M., Abbass, A., Stride, C., & Bernier, D. (2017). A randomised controlled trial of intensive short-term dynamic psychotherapy for treatment resistant depression: The Halifax depression study. Journal of Affective Disorders, 214, 15 25. Available from https://doi.org/10.1016/j.jad.2017.02.035. Vinnars, B., Barber, J. P., Noren, K., Gallop, R., & Weinryb, R. M. (2005). Manualized supportive-expressive psychotherapy versus nonmanualized community-delivered psychodynamic therapy for patients with personality disorders: Bridging efficacy and effectiveness. American Journal of Psychiatry, 162(10), 1933 1940. Westen, D., Novotny, C. M., & Thompson-Brenner, H. (2004). The empirical status of empirically supported psychotherapies: Assumptions, findings, and reporting in controlled clinical trials. Psychological Bulletin, 130, 631 663. Wiborg, I. M., & Dahl, A. A. (1996). Does brief dynamic psychotherapy reduce the relapse rate of panic disorder? Archives of General Psychiatry, 53, 689 694. Winston, A., Laikin, M., Pollack, J., Samstag, L. W., McCullough, L., & Muran, J. C. (1994). Short-term psychotherapy of personality disorders. American Journal of Psychiatry, 151, 190 194. Wittchen, H., Jacobi, F., Rehm, J., Gustavsson, A., Svensson, M., Jönsson, B., . . . Steinhausen, H. C. (2011). The size and burden of mental disorders and other disorders of the brain in Europe 2010. Neuropsychopharmacology, 21, 655 679. Woody, G., Luborsky, L., McLellan, A. T., & O’ Brien, C. P. (1990). Corrections and revised analyses for psychotherapy in methadone maintenance patients. Archives of General Psychiatry, 47, 788 789. Woody, G., Luborsky, L., McLellan, A. T., & O’Brien, C. P. (1995). Psychotherapy in community methadone programs: A validation study. American Journal of Psychiatry, 152, 1302 1308. Woody, G., Luborsky, L., McLellan, A. T., O’ Brien, C. P., Beck, A. T., Blaine, J., . . . Hole, A. (1983). Psychotherapy for opiate addicts: Does it help? Archives of General Psychiatry, 40, 639 645. Yeomans, F. (2007). Questions concerning the randomized trial of schema-focused therapy vs transference-focused psychotherapy. Archives of General Psychiatry, 64, 610 611. Zipfel, S., Wild, B., Groß, G., Friederich, H.-C., Teufel, M., Schellberg, D., . . . ANTOP study group. (2013). Focal psychodynamic therapy, cognitive behaviour therapy, and optimised treatment as usual in outpatients with anorexia nervosa (ANTOP study): Randomised controlled trial. Lancet, 383, 127 137. Process research in psychodynamic psychotherapy: interventions and the therapeutic relationship 5 Kevin S. McCarthy1,2, Sigal Zilcha-Mano3 and Jacques P. Barber4 1 Chestnut Hill College, Philadelphia, PA, United States, 2Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, United States, 3University of Haifa, Haifa, Israel, 4Derner Institute of Advanced Psychological Study, Adelphi University, New York, NY, United States Contemporary psychodynamic psychotherapy (PDT) benefits from an abundant and verdant literature describing the therapy process, that is, what happens inside of the treatment. In this chapter we present some of the sophisticated, novel process research investigations of PDT that have occurred. While illuminating, these thoughtful inquiries also underscore the complexities of the therapy process and the challenges in studying the inner workings of therapy. Indeed, with its 120-year history, we know that PDT is effective (Abbass et al., 2014; Barber, Muran, McCarthy, & Keefe, 2013; Chapter 4: The efficacy of psychodynamic psychotherapy: an up-to-date review, in this volume), but knowing precisely what PDT therapists do in treatment to help their patients achieve benefits remains an elusive goal, although one that seems more attainable as process research becomes more sophisticated and nuanced. Since mediators of change in PDT such as insight into conflict, relationship representations, unconscious defenses, and affect tolerance are well reviewed in this book (Chapters 2, 3, and 6) and elsewhere (Barber et al., 2013), our focus in this chapter will be on PDT interventions and the therapeutic relationship. PDT interventions Interventions in PDT can be conceptualized as existing on a supportive-expressive/ interpretive continuum (Piper, Joyce, McCallum, Azim, & Ogrodniczuk, 2002; Summers & Barber, 2010). Supportive interventions are often characterized as nondirective or generic helping skills. However, in a psychodynamic sense, these techniques can hardly be regarded as nondirective or generic but instead are selectively targeted to meet the needs of the patient based on a comprehensive formulation of the patient’s individual conflicts and deficits. For example, a PDT therapist might work to instill hope in a patient adjusting to a recent loss but remain neutral Contemporary Psychodynamic Psychotherapy. DOI: https://doi.org/10.1016/B978-0-12-813373-6.00005-2 © 2019 Elsevier Inc. All rights reserved. 76 Contemporary Psychodynamic Psychotherapy with a patient who is ambivalent about change. Four categories of supportive interventions are reinforcing strengths (e.g., gratifying the patient’s needs, supporting adaptive defenses), reducing vulnerabilities (e.g., undermining maladaptive defenses), changing behaviors and environments, and ego lending (e.g., relying on the therapist as an auxiliary problem solver) (Piper et al., 2002). Expressive techniques uncover or facilitate the patient’s awareness of interpersonal patterns that the patient may be repeating, via exploration of interpersonal themes and affect (questioning or selectively attending), confrontation (asking a patient to resolve two or more discrepant pieces of information or experiences), clarification (making an experience explicit to the patient), and interpretation (connecting between different experiences in the patient’s life). Recently, the development of various instruments has made it possible to assess therapist technique use in a session from multiple theoretical orientations simultaneously. In proportion to all interventions in a session, modal studies suggest that supportive and expressive techniques are used in PDT about 25% and 15% of the time, respectively [range for supportive: 15% (McCarthy & Barber, 2009) to 81% (Hersoug, Bøgwald, & Høglend, 2005); range for expressive: 11% (Trijsburg et al., 2002) to 96% (Hilsenroth, Blagys, Ackerman, Bonge, & Blais, 2005)]. Investigations of psychoanalysis are rarer and show frequencies of 18% 60% supportive and 18% 23% expressive interventions (McCarthy & Barber, 2009; Roy, Perry, Luborsky, & Banon, 2009; Tschuschke et al., 2015). By way of comparison, 18% and 10% of techniques in cognitive-behavioral sessions have been classified as supportive and interpretive, respectively, in modal studies [range for supportive: 15% (McCarthy & Barber, 2009) to 50% (Barber, Krakauer, Calvo, Badgio, & Faude, 1997); range for expressive: ,1% (Banon et al., 2013) to 31% (Barber, Morse, Krakauer, Chittams, & Crits-Christoph, 1997)]. Relations of technique to outcome Greater levels of supportive interventions have not been shown to be consistently related to outcome (Barber, Crits-Christoph, & Luborsky, 1996; Hersoug et al., 2005; Milbrath et al., 1999; Ogrodniczuk & Piper, 1999), but this does not necessarily imply that supportive techniques are unhelpful. As was described above, supportive techniques often comprise the largest share of interventions in PDT and other treatments, reflecting their importance across various models of PDT. Supportive interventions can strengthen the therapeutic alliance (Ogrodniczuk & Piper, 1999) and make the emotionally challenging work of therapy possible. Supportive interventions also may be used frequently with patients who are least likely to show symptom improvement (Piper et al., 2002). Well-conducted supportive psychotherapy is often equivalent to other efficacious manualized treatments (Clarkin, Levy, Lenzenweger, & Kernberg, 2007; Piper et al., 2002). The relationship between supportive techniques and outcome needs greater empirical exploration to contextualize their effective use. Expressive interventions also show mixed associations with outcome, including positive, null, and negative relationships (Barber et al., 2013; Høglend, 2014; McCarthy, Keefe, & Barber, 2016). The negative correlations observed between Process research in psychodynamic psychotherapy: interventions and the therapeutic relationship 77 expressive interventions, specifically interpretation, and symptom outcomes are not ignorable and beg for an explanation (Høglend, 2014), leading dynamic theorists and researchers to wonder how PDT can be effective when its definitive technique may be correlated with poorer outcomes for some patients. Variability in the technique-outcome relation A number of factors ought to be considered in trying to make sense of the variability in associations observed between technique use in PDT and treatment outcome. Interpretive techniques may be more likely to show positive results with mechanisms and outcomes that are more central to PDT, such as insight, defenses, affect tolerance, and relationships, rather than with symptoms (Barber et al., 2013; Høglend, 2014; Perry & Bond, 2017; Town, Hardy, McCullough, & Stride, 2012). Whereas much process-outcome research is focused on symptom-related outcomes, therapeutic success in PDT is often much broader and more complex than symptom amelioration. Specific expressive techniques may have different relationships with symptom improvement. Affective and interpersonal exploration may share positive associations with symptom improvement (Diener, Hilsenroth, & Weinberger, 2007; SlavinMulford, Hilsenroth, Weinberger, & Gold, 2011), as may confrontation (Town et al., 2012) and immediacy, a focus on the here-and-now relationship between patient and therapist (Hill et al., 2014; Kuutman & Hilsenroth, 2012). These interventions work to uncover unconscious feelings and conflict but leave it to the patient to decide how much and when to reveal. Other more direct expressive techniques such as interpretation may be experienced by the patient as exposing or emotionally activating and so, when delivered with greater frequency, may lead to greater discomfort and disorientation. Certain types of patients may respond especially well to expressive interventions, whereas others may not. There is some converging evidence that individuals with a distant or controlling interpersonal style might do especially well in PDT compared to other patients (Barber et al. 1997; Dinger, Strack, Leichsenring, & Schauenburg, 2007; Dinger, Zilcha-Mano, McCarthy, Barrett, & Barber, 2013; Kuutman & Hilsenroth, 2012), as PDT’s emphasis on relationships and affect may especially benefit patients for whom these are not strengths. The level of psychological adjustment with which a patient enters PDT may affect the therapy process and outcome. Mature defenses at intake may predict better outcome but may also draw less frequent use of interpretive technique from the therapist (Perry & Bond, 2017). Individuals with poorer quality of object relations (a less differentiated or accurate cognitive-affective schema for relationships) may be less able to build a therapeutic relationship but may respond better to a more expressive treatment (Høglend, 2014). Finally, a finding that minority-status males were more likely to benefit from PDT than from medication (Barber, Barrett, Gallop, Rynn, & Rickels, 2012) invites speculation about the restorative nature of PDT interventions for individuals exposed to manifold oppression and stigmatization and the opportunity to discuss important relationships. Moderators of treatment process are a promising but 78 Contemporary Psychodynamic Psychotherapy difficult area of study, as individuals are rarely randomized in studies on these important characteristics, and large samples are required to test interaction effects. It is probable that a complex temporal sequence exists among expressive techniques, PDT mechanisms, and symptom and behavior change. Interpretation certainly influences PDT mechanisms but, at the same time, may be disruptive to functioning in the short term. Explicitly pointing out uncomfortable elements in the therapy relationship or calling attention to shameful or unacceptance experiences that the patient would rather avoid is likely to manifest in negative therapy process (Milbrath et al., 1999; Petraglia, Bhatia, de Roten, Despland, & Drapeau, 2015; Schut et al., 2005) or emotional arousal (Town et al., 2012). At the same time the mechanisms initiated by these therapeutic encounters may promote improvements in symptoms and functioning later on (Barber et al., 2013). For example, an interpretation of how the patient is mistreating the therapist in a session may be upsetting for the patient to hear. However, knowing this information (and progressively working through this conflict) allows the patient to change this behavioral pattern. The effects of PDT may actually unfold over time even after termination (a “sleeper” effect), as it is often shown that the effect size of PDT increases during the follow-up period (Abbass et al., 2014). Termination of therapy may represent a critical period for the techniqueoutcome association in PDT because it recapitulates the problems many patients have in ending relationships (Joyce, Piper, Ogrodniczuk, & Klein, 2007). Patients may show a localized spike in symptoms in this period as they work toward resolving these difficulties. Therapists may intervene more during termination or in preparation for it (Nof, Leibovich, & Zilcha-Mano, 2017). Both of these potential phenomena may artefactually induce a correlation between techniques and higher symptom levels at the end of treatment, which while statistically valid may not be clinically meaningful. Termination is difficult to study, as many endings are premature, unilateral, or unpredicted. Additionally, to model the trajectory of change, multiple assessments are needed before and after the end of treatment. Successfully managing negative process moments, especially those originating from particular intervention use, may necessitate greater competence on the part of the therapist. Competence is the skill with which the therapist intervenes and has been linked to outcome (Barber et al., 2013; Killingmo, Varvin, & Strømme, 2014). Competence is not simply the application of PDT technique. The timing of when a therapist delivers an intervention is one dimension of competence, similar to the concept of responsiveness, or matching the moment-to-moment needs of the patient (Kramer & Stiles, 2015). Coregulating and making use of the affects that emerge in both the patient and the therapist in response to interventions may require experience and sensitivity (Dahl et al., 2016; Fisher, Atzil-Slonim, BarKalifa, Rafaeli, & Peri, 2016; Milbrath et al., 1999; Nissen-Lie et al., 2017; Town, Salvadori, Falkenström, Bradley, & Hardy, 2017), as the therapist must have sufficient self-awareness and interpersonal skills to manage the interaction productively. Monitoring and cultivating the alliance and pairing interventions accordingly may also represent the proficiency of the therapist (Owen & Hilsenroth, 2011; Petraglia et al., 2015; Ryum, Stiles, Svartberg, & McCullough, 2010) in Process research in psychodynamic psychotherapy: interventions and the therapeutic relationship 79 helping the patient take advantage of expressive interventions. Flexibility of technique use may be an aspect of timing, and two novel approaches approximate therapist flexibility. First, testing a curvilinear relation between expressive technique use and outcome can show that a moderate level of intervention (neither too much nor too little—a “Goldilocks” effect) is associated with symptom improvement (McCarthy et al. 2016; Ogrodniczuk & Piper, 1999). Second, estimating therapist flexibility as the variability of PDT intervention use within a case (i.e., a therapist employs differing amounts of techniques at different times in a treatment) and between cases (i.e., a therapist gives more technique to certain patients than to others) can also predict better outcomes (Barber, 2009; Owen & Hilsenroth, 2014). Accuracy of interpretive interventions, or how closely they match the patient’s formulation, may also be important for outcome (Andrusyna, Luborsky, Pham, & Tang, 2006; Crits-Christoph, Cooper, & Luborsky, 1988; Stigler, de Roten, Drapeau, & Despland, 2007). A recent study of therapists in practice found that when therapists predicted their ideal interventions from a patient’s formulation and actually performed those interventions, 3 months later their patients reported better outcomes (Castonguay et al., 2017). Examination of aspects of competence such as flexibility and accuracy suggests that PDT may require a certain artfulness in the therapist to best facilitate success. Therapeutic relationship The therapeutic alliance is a concept that originated in the analytic literature and has evolved over time (Zilcha-Mano, 2017). The most common definition of the therapeutic alliance consists of the agreement on the work of therapy and the quality of the relationship between therapist and patient. The therapeutic alliance measured early in treatment (around the third session) is one of the most robust predictors of improvement later on in treatment (Horvath, Del Re, Flückinger, & Symonds, 2011). However, this correlation does not tell us whether the alliance is itself directly related to outcome, is a necessary vehicle or medium for change (but not sufficient in itself), facilitates intervention uptake, or is a by-product of being helped (DeRubeis, Brotman, & Gibbons, 2005). More recently, research on the development of the therapeutic relationship over time and its interaction with other process factors has brought us closer to disentangling its relationship to outcome, especially with new models of thinking about the alliance. The therapeutic alliance exists even before treatment starts as part of the patient’s expectations regarding the helpfulness of the therapist (Barber et al., 2014) or the initial contact with professionals during an assessment evaluation (Hilsenroth, Peters, & Ackerman, 2004). Zilcha-Mano, McCarthy, Dinger, and Barber (2014) demonstrated that pretreatment representations of others explained up to half the variance in alliance scores taken before patients met their providers. Other patient interpersonal factors also have been shown to contribute to alliance during the treatment, including attachment style (Bernecker, Levy, & Ellison, 2014), relationship functioning 80 Contemporary Psychodynamic Psychotherapy (Barber, Foltz, DeRubeis, & Landis, 2002; Beretta et al., 2007), and interpersonal problems (Dinger, Strack, Sachsse, & Schauenburg, 2009; Hersoug, Høglend, Havik, von der Lippe, & Monsen, 2009). Therapist interpersonal patterns influence the development of the alliance (Dinger et al., 2009; Nissen-Lie, Monsen, & Rønnestad, 2010), and therapists’ views and attitudes about the relationship affect how their patients experience the alliance (Kivlighan, Marmarosh, & Hilsenroth, 2014; Zilcha-Mano et al., 2015, 2016). Certain PDT therapists seem better able than others to form good-quality relationships that benefit their patients (Dinger, Strack, Leichsenring, Wilmers, & Schauenburg, 2008), although there is good evidence that alliance fostering can be increased with training, even among experienced therapists (Crits-Christoph et al., 2006). When patients and therapists share similar perceptions of the quality of their relationship (i.e., their alliance scores are similar to one another), outcomes are better for the patients (Marmarosh & Kivlighan, 2012). The mutual influence of PDT and other theoretical orientations on one another in training and practice is changing how therapists relate to their patients. Integration of psychoeducational techniques early in treatment, namely, helping the client understand the treatment and define goals, affords a good alliance (Goldman, Hilsenroth, Owen, & Gold, 2013). There may also be unique processes for alliance development in different therapies. One study showed that in PDT the affective bond was related to symptom improvement when affect was engaged, whereas in CBT avoiding emotional arousal was associated with an increased bond and reduced symptoms (Ulvenes et al., 2012). Further understanding of the multiple pathways to an alliance is increasingly important as practitioners from all orientations begin to appreciate and utilize the vitality of the therapeutic relationship. More and more research is examining alliance development over time. Different trajectories of alliance have been reported (Dinger et al., 2008; Kivlighan & Shaughnessy, 2000; Kramer, Roten, Beretta, Michel, & Despland, 2008; Stiles et al., 2004). How these trajectories are associated with outcome is still not entirely clear, but high stable alliances across treatment and improving alliances are often predictors of good outcome. The alliance is often unstable across treatment, and methods to examine multiple alliance measurements within an individual (e.g., aggregation, Crits-Christoph, Gibbons, Hamilton, Ring-Kurtz, & Gallop, 2011; disaggregation, Falkenström, Granström, & Holmqvist, 2013; Zilcha-Mano et al., 2015) will often produce a more accurate estimate of the alliance that is better predictive of outcome. Such methods and findings are a reminder that alliance is not static and should be tracked in treatment. Alliance ruptures Alliance ruptures and their resolution are another research area arising out of studying the alliance in PDT treatment (Eubanks, Muran, & Safran, 2018). Ruptures are no longer conceptualized as setbacks in the therapy but are seen as events that occur commonly in psychotherapy and are markers for important therapeutic work (Eubanks et al., 2018). Interpersonal problems often bring patients to therapy and Process research in psychodynamic psychotherapy: interventions and the therapeutic relationship 81 inevitably are experienced in-session with the therapist (Barber et al., 2002; Beretta et al., 2007). Ruptures and their resolution provide an opportunity to understand these patterns and work toward developing more adaptive ways of relating to others. Research suggests that noticing and disengaging a rupture and permitting a patient to express and get vulnerable needs met (Eubanks et al., 2018) may lead to better outcomes in psychotherapy. Therapist immediacy may be related to detecting and managing the resolution (Hill et al., 2014), whereas interventions connecting the rupture to interpersonal patterns may need to come after resolution to be effective (Gerostathos, de Roten, Berney, Despland, & Ambresin, 2014). A type of PDT involving attention to the alliance and alliance ruptures is associated with less dropout and comparatively better outcomes when the patient did not do well in a previous treatment (Safran, Muran, Samstag, & Winston, 2005). Furthermore, a meta-analysis showed modest symptom improvement following rupture and repair sequences (Eubanks et al., 2018). New models of the alliance Informed by relational theory and time-series design research, Zilcha-Mano (2017) proposed a trait-state model of alliance: The ability of patients to form a relationship based on their interpersonal history and motivations may be considered a trait, whereas the development of the relationship during treatment reflects the statelike nature of the alliance and may serve as a curative factor in therapy. In this model, the characteristic tendency of a patient to form positive relationships (i.e., high trait-level alliance) enables the therapy to proceed more quickly on average because the patient is more trusting, emotionally available, and accepting of the therapist’s attempts to help. The state of the relationship between the patient and therapist changes, develops, and even deteriorates during the therapy itself in response to therapist behaviors and the therapy process. Often, ongoing negotiation of the alliance is critical to the patient either because (1) the patient lacks helping relationships and so the establishment of such a relationship with the therapist is transformative or (2) the interpersonal problems for which a patient enters treatment find their way into the therapy relationship (Barber et al., 2002; Beretta et al., 2007) and, with the therapist’s observation and assistance, a new solution to these problems is arrived at. State-related changes (e.g., improvement in the alliance) may lead to changes in the patient’s trait-level alliance-building ability, which facilitates better and more satisfying relationships. Intricate studies of within-patient (state) and between-patient (trait) levels of alliance in PDT over time provide evidence validating these potential pathways of relationship change (Crits-Christoph et al., 2011; Falkenström et al., 2013; Zilcha-Mano et al., 2015). Contemporary PDT thinking and practice privilege the personal involvement or therapeutic presence of the therapist as opposed to detachment or objectivity. Reflecting this trend, Gelso (2014) has proposed an additional element of the alliance: the real relationship, or the authenticity of the therapist in the relationship. 82 Contemporary Psychodynamic Psychotherapy Here, the therapist is not just a blank screen for patients’ projections or an instrument to detect patients’ problems but an actual contributor and cocreator of the relationship who brings genuine parts of himself or herself to therapy. This authentic presence can be measured and shown to predict symptom change over and above the contribution of other factors (Gelso, 2014). Conclusions Inescapably, the cleverest empirical work can represent only some small portion of the richness and depth of PDT. Nevertheless, research concerning therapist interventions and the therapy relationship can reciprocally inform the practice of PDT. Therapy process research has helped to (1) validate the complexity of PDT processes that clinicians report; (2) chronicle the use of supportive, expressive, and other techniques and the fluctuating character of the alliance over time; (3) identify some of the temporal and contextual factors that facilitate the helpfulness of PDT; and (4) inform our understanding of the curative strength of the developing therapeutic relationship and well-applied PDT interventions. Further research using time-series, task-analysis, multiple observations over treatment, and qualitative inquiry is needed to uncover of the nuances of PDT processes in order to understand better the workings of PDT. The effect of psychotherapy integration is essential to consider, especially as PDT explicitly and implicitly accommodates other technical approaches. Indeed, many of the studies included in our review involved some element of integrative therapy. Furthermore, as PDT concepts such as alliance ruptures and exploration of interpersonal patterns permeate other approaches (e.g., Castonguay et al., 2004), greater understanding of how these concepts work will pay large dividends. Finally, the appreciation of culture is another element that PDT and its holistic appraisal of the person is well positioned to enhance, especially the concepts of multiple intersecting identities and recognition of conflict of needs within and among individuals (Tummala-Narra, 2016; see Chapter 19: Working with immigrants and refugees in psychodynamic psychotherapy, in this volume). Cultural factors in therapy are necessarily complex and difficult to study. However, just as the intricacy of PDT processes has given rise to new and emerging models of study, these same approaches may be able to bring out and describe the complex situations of a pluralistic encounter. References Abbass, A. A., Kisely, S. R., Town, J. M., Leichsenring, F., Driessen, E., De Maat, S., . . . Crowe, E. (2014). Short-term psychodynamic psychotherapies for common mental disorders. Cochrane Database of Systematic Reviews, 1(7), CD00468. Available from https://doi.org/10.1002/14651858.CD004687.pub4. Process research in psychodynamic psychotherapy: interventions and the therapeutic relationship 83 Andrusyna, T. P., Luborsky, L., Pham, T., & Tang, T. Z. (2006). The mechanisms of sudden gains in supportive expressive therapy for depression. Psychotherapy Research, 16(5), 526 536. Available from https://doi.org/10.1080/10503300600591379. Banon, E., Perry, J. C., Semeniuk, T., Bond, M., De Roten, Y., Hersoug, A. G., & Despland, J.-N. (2013). Therapist interventions using the Psychodynamic Interventions Rating Scale (PIRS) in dynamic therapy, psychoanalysis, and CBT. Psychotherapy Research, 23(2), 121 136. Available from https://doi.org/10.1080/10503307.2012.745955. Barber, J. P. (2009). Toward a working through of some core conflicts in psychotherapy research. Psychotherapy Research, 19(1), 1 12. Available from https://doi.org/10.1080/ 10503300802609680. Barber, J. P., Barrett, M. S., Gallop, R., Rynn, M. A., & Rickels, K. (2012). Short-term dynamic psychotherapy versus pharmacotherapy for major depressive disorder: A randomized, placebo-controlled trial. The Journal of Clinical Psychiatry, 73(1), 66 73. Available from https://doi.org/10.4088/JCP.11m06831. Barber, J. P., & Crits-Christoph, P. (1996). Development of a therapist adherence/competence rating scale for supportive-expressive dynamic psychotherapy: A preliminary report. Psychotherapy Research, 6(2), 81 94. Available from https://doi.org/10.1080/ 10503309612331331608. Barber, J. P., Foltz, C., DeRubeis, R. J., & Landis, J. R. (2002). Consistency of interpersonal themes in narratives about relationships. Psychotherapy Research, 12, 139 158. Available from https://doi.org/10.1093/ptr/12.2.139. Barber, J. P., Krakauer, I., Calvo, N., Badgio, P. C., & Faude, J. (1997). Measuring adherence and competence of dynamic therapists in the treatment of cocaine dependence. Journal of Psychotherapy Practice and Research, 6, 12 24. Available from https://doi.org/ 10.1080/10503309612331331608. Barber, J. P., Morse, J. Q., Krakauer, I. D., Chittams, J., & Crits-Christoph, K. (1997). Change in obsessive-compulsive and avoidant personality disorders following timelimited supportive-expressive therapy. Psychotherapy: Theory, Research, Practice, Training, 34(2), 133. Available from https://doi.org/10.1037/h0087774. Barber, J. P., Muran, J. C., McCarthy, K. S., & Keefe, R. J. (2013). Research on psychodynamic therapies. In M. J. Lambert (Ed.), Handbook of psychotherapy and behavior change (6th ed, pp. 443 494). New York, NY: Wiley. Barber, J. P., Zilcha-Mano, S., Gallop, R., Barrett, M., McCarthy, K. S., & Dinger, U. (2014). The associations among improvement and alliance expectations, alliance during treatment, and treatment outcome for major depressive disorder. Psychotherapy Research, 24, 257 268. Available from https://doi.org/10.1080/10503307.2013.871080. Beretta, V., Despland, J.-N., Drapeau, M., Michel, L., Kramer, U., Stigler, M., & de Roten, Y. (2007). Are relationship patterns with significant others reenacted with the therapist?: A study of early transference reactions. Journal of Nervous & Mental Disease, 195(5), 443 450. Available from https://doi.org/10.1097/01.nmd.0000253766.35132.30. Bernecker, S. L., Levy, K. N., & Ellison, W. D. (2014). A meta-analysis of the relation between patient adult attachment style and the working alliance. Psychotherapy Research, 24(1), 12 24. Available from https://doi.org/10.1080/10503307.2013.809561. Castonguay, L. G., Janis, R. A., Youn, S. J., Xiao, H., McAleavey, A. A., Boswell, J. F., . . . Wiley, M. O. (2017). Clinician’s prediction and recall of therapeutic interventions: Practice research network study. Counselling Psychology Quarterly, 30(3), 308 322. Available from https://doi.org/10.1080/09515070.2017.1334628. Castonguay, L. G., Schut, A. J., Aikens, D. E., Constantino, M. J., Laurenceau, J. P., Bologh, L., & Burns, D. D. (2004). Integrative cognitive therapy for depression: A preliminary 84 Contemporary Psychodynamic Psychotherapy investigation. Journal of Psychotherapy Integration, 14(1), 4 20. Available from https:// doi.org/10.1037/1053-0479.14.1.4. Clarkin, J. F., Levy, K. N., Lenzenweger, M. F., & Kernberg, O. F. (2007). Evaluating three treatments for borderline personality disorder: A multiwave study. American Journal of Psychiatry, 164, 922 928. Available from https://doi.org/10.1176/ajp.2007.164.6.922. Crits-Christoph, P., Cooper, A., & Luborsky, L. (1988). The accuracy of therapists’ interpretations and the outcome of dynamic psychotherapy. Journal of Consulting and Clinical Psychology, 56(4), 490 495. Available from https://doi.org/10.1037/0022-006X.56.4.490. Crits-Christoph, P., Gibbons, M. B. C., Crits-Christoph, K., Narducci, J., Schamberger, M., & Gallop, R. (2006). Can therapists be trained to improve their alliances? A preliminary study of alliance-fostering psychotherapy. Psychotherapy Research, 16, 268 281. Available from https://doi.org/10.1080/10503300500268557. Crits-Christoph, P., Gibbons, M. B. C., Hamilton, J., Ring-Kurtz, S., & Gallop, R. (2011). The dependability of alliance assessments: The alliance outcome correlation is larger than you might think. Journal of Consulting and Clinical Psychology, 79, 267 278. Available from https://doi.org/10.1037/a0023668. Dahl, H.-S. J., Høglend, P., Ulberg, R., Amlo, S., Gabbard, G. O., Perry, J. C., & CritsChristoph, P. (2016). Does therapists’ disengaged feelings influence the effect of transference work? A study on countertransference. Clinical Psychology and Psychotherapy. Available from https://doi.org/10.1002/cpp2015. DeRubeis, R. J., Brotman, M. A., & Gibbons, C. J. (2005). A conceptual and methodological analysis of the nonspecifics argument. Clinical Psychology: Science and Practice, 12, 174 183. Available from https://doi.org/10.1093/clinpsy.bpi022. Diener, M. J., Hilsenroth, M. J., & Weinberger, J. (2007). Therapist affect focus and patient outcomes in psychodynamic psychotherapy: A meta-analysis. American Journal of Psychiatry, 164, 936 941. Dinger, U., Strack, M., Leichsenring, F., & Schauenburg, H. (2007). Influences of patients’ and therapists’ interpersonal problems and therapeutic alliance on outcome in psychotherapy. Psychotherapy Research, 17(2), 148 159. Available from https://doi.org/ 10.1080/10503300600865393. Dinger, U., Strack, M., Leichsenring, F., Wilmers, F., & Schauenburg, H. (2008). Therapist effects on outcome and alliance in inpatient psychotherapy. Journal of Clinical Psychology, 64, 344 354. Available from https://doi.org/10.1002/jclp.20443. Dinger, U., Strack, M., Sachsse, T., & Schauenburg, H. (2009). Therapists’ attachment, patients’ interpersonal problems and alliance development over time in inpatient psychotherapy. Psychotherapy: Theory, Research, Practice, Training, 46(3), 277 290. Available from https://doi.org/10.1037/a0016913. Dinger, U., Zilcha-Mano, S., McCarthy, K. S., Barrett, M. S., & Barber, J. P. (2013). Interpersonal problems as predictors of alliance, symptomatic improvement and premature termination in treatment of depression. Journal of Affective Disorders, 151(2), 800 803. Available from https://doi.org/10.1016/j.jad.2013.07.003. Eubanks, C. F., Muran, J. C., & Safran, J. D. (2018). Alliance rupture repair: A meta-analysis. Psychotherapy, 55(4), 508 519. Available from http://dx.doi.org/10.1037/pst0000185. Falkenström, F., Granström, F., & Holmqvist, R. (2013). Therapeutic alliance predicts symptomatic improvement session by session. Journal of Counseling Psychology, 60, 317 328. Available from https://doi.org/10.1037/a0032258. Fisher, H., Atzil-Slonim, D., Bar-Kalifa, E., Rafaeli, E., & Peri, T. (2016). Emotional experience and alliance contribute to therapeutic change in psychodynamic therapy. Psychotherapy, 53, 105 116. Available from https://doi.org/10.1037/pst0000041. Process research in psychodynamic psychotherapy: interventions and the therapeutic relationship 85 Gelso, C. (2014). A tripartite model of the therapeutic relationship: Theory, research, and practice. Psychotherapy Research, 24(2), 117 131. Available from https://doi.org/ 10.1080/10503307.2013.845920. Gerostathos, A., de Roten, Y., Berney, S., Despland, J.-N., & Ambresin, G. (2014). How does addressing patients’ defenses help to repair alliance ruptures in psychodynamic psychotherapy? An exploratory study. Journal of Nervous and Mental Disease, 202(5), 419 424. Available from https://doi.org/10.1097/NMD0000000000000112. Goldman, R. E., Hilsenroth, M. J., Owen, J. J., & Gold, J. R. (2013). Psychotherapy integration and alliance: Use of cognitive-behavioral techniques within a short-term psychodynamic treatment model. Journal of Psychotherapy Integration, 23(4), 373 385. Available from https://doi.org/10.1037/a0034363. Hersoug, A. G., Bøgwald, K.-P., & Høglend, P. (2005). Changes of defensive functioning: Does interpretation contribute to change? Clinical Psychology and Psychotherapy, 12, 288 296. Available from https://doi.org/10.1002/cpp.444. Hersoug, A. G., Høglend, P., Havik, O. E., von der Lippe, A., & Monsen, J. T. (2009). Pretreatment patient characterisitics related to the level and development of working alliance in long-term psychotherapy. Psychotherapy Research, 19(2), 172 180. Available from https://doi.org/10.1080/10503300802657374. Hill, C. E., Gelso, C. J., Chui, H., Spangler, P. T., Hummel, A., Huang, T., . . . Miles, J. R. (2014). To be or not to be immediate with clients: The use and perceived effects of immediacy in psychodynamic/interpersonal psychotherapy. Psychotherapy Research, 24, 299 315. Available from https://doi.org/10.1080/10503307.2013.812262. Hilsenroth, M. J., Blagys, M. D., Ackerman, S. J., Bonge, D. R., & Blais, M. A. (2005). Measuring psychodynamic-interpersonal and cognitive-behavioral techniques: Development of the Comparative Psychotherapy Process Scale. Psychotherapy: Theory, Research, Practice, Training, 42(3), 340 356. Hilsenroth, M. J., Peters, E. J., & Ackerman, S. J. (2004). The development of therapeutic alliance during psychological assessment: Patient and therapist perspectives across treatment. Journal of Personality Assessment, 83, 332 344. Available from https://doi.org/ 10.1207/s15327752jpa8303_14. Horvath, A. O., Del Re, A. C., Flückinger, C., & Symonds, D. (2011). Alliance in individual psychotherapy. Psychotherapy: Theory, Research, & Practice, 48, 9 16. Available from https://doi.org/10.1037/a0022186. Høglend, P. (2014). Exploration of the patient-therapist relationship in psychotherapy. American Journal of Psychiatry, 171(10), 1056 1066. Joyce, A. S., Piper, W. E., Ogrodniczuk, J. S., & Klein, R. H. (2007). Termination in psychotherapy: A psychodynamic model of processes and outcomes. Washington, DC: American Psychological Association. Killingmo, B., Varvin, S., & Strømme, H. (2014). What can we expect from trainee therapists? A study of acquisition of competence in dynamic psychotherapy. Scandinavian Psychoanalytic Review, 37(1), 24 35. Available from https://doi.org/10.1080/ 01062301.2014.903029. Kivlighan, D. M., Jr., Marmarosh, C. L., & Hilsenroth, M. J. (2014). Client and therapist therapeutic alliance, session evaluation, and client reliable change: A moderated actorpartner interdependence model. Journal of Counseling Psychology, 61, 15 23. Available from https://doi.org/10.1037/a0034939. Kivlighan, D. M., & Shaughnessy, P. (2000). Patterns of working alliance development: A typology of client’s working alliance ratings. Journal of Counseling Psychology, 47, 362 371. 86 Contemporary Psychodynamic Psychotherapy Kramer, U., Roten, Y. D., Beretta, V., Michel, L., & Despland, J. N. (2008). Patient’s and therapist’s views of early alliance building in dynamic psychotherapy: Patterns and relation to outcome. Journal of Counseling Psychology, 55(1), 89 95. Available from https://doi.org/10.1080/10503300902956742. Kramer, U., & Stiles, W. B. (2015). The responsiveness problem in psychotherapy: A review of proposed solutions. Clinical Psychology: Science and Practice, 22, 277 295. Available from https://doi.org/10.1111/cpsp.12107. Kuutman, K., & Hilsenroth, M. J. (2012). Exploring in-session focus on the patient-therapist relationship: Patient characteristics, process, and outcome. Clinical Psychology and Psychotherapy, 19, 187 202. Available from https://doi.org/10.10002/cpp.743. Marmarosh, C. L., & Kivlighan, D. M., Jr. (2012). Relationships among client and counselor agreement about the working alliance, session evaluations, and change in client symptoms using response surface analysis. Journal of Counseling Psychology, 59(3), 352 367. Available from https://doi.org/10.1037/a0028907. McCarthy, K. S., & Barber, J. P. (2009). The multitheoretical list of therapeutic interventions (MULTI): Initial report. Psychotherapy Research, 19, 96 113. Available from https:// doi.org/10.1080/10503300802524343. McCarthy, K. S., Keefe, J. R., & Barber, J. P. (2016). Goldilocks on the couch: Moderate levels of psychodynamic and process-experiential technique predict outcome in psychodynamic therapy. Psychotherapy Research, 26(3), 307 317. Available from https://doi. org/10.1080/10503307.2014.973921. Milbrath, C., Bond, M., Cooper, S., Znoj, H. J., Horowitz, M. J., & Perry, J. C. (1999). Sequential consequences of therapists’ interventions. Journal of Psychotherapy Practice and Research, 8(1), 40 54. Nissen-Lie, H. A., Monsen, J. T., & Rønnestad, M. H. (2010). Therapist predictors of early patient-rated working alliance: A multilevel approach. Psychotherapy Research, 20(6), 627 646. Available from https://doi.org/10.1080/10503307.2010.497633. Nissen-Lie, H. A., Rønnestad, M. H., Høglend, P. A., Havik, O. E., Solbakken, O. A., Stiles, T. C., & Monsen, J. T. (2017). Love yourself as a person, doubt yourself as a therapist? Clinical Psychology and Psychotherapy, 24, 48 60. Available from https:// doi.org/10.1002/cpp.1977. Nof, A., Leibovich, L., & Zilcha-Mano, S. (2017). Supportive expressive interventions in working through treatment termination. Psychotherapy, 54(1), 29 36. Available from https://doi.org/10.1037/pst0000094. Ogrodniczuk, J. S., & Piper, W. E. (1999). Use of transference interpretations in dynamically oriented individual psychotherapy for patients with personality disorders. Journal of Personality Disorders, 13(4), 297 311. Available from https://doi.org/10.1521/pedi.1999.13.4.297. Owen, J., & Hilsenroth, M. J. (2011). Interaction between alliance and technique in predicting patient outcome during psychodynamic psychotherapy. Journal of Nervous & Mental Disease, 199(6), 384 389. Available from https://doi.org/10.1097/NMD.0b013e31821cd28a. Owen, J., & Hilsenroth, M. J. (2014). Treatment adherence: The importance of therapist flexibility in relation to therapy outcomes. Journal of Counseling Psychology, 61(2), 280 288. Available from https://doi.org/10.1037/a0035753. Perry, J. C., & Bond, M. (2017). Addressing Defenses in Psychotherapy to Improve Adaptation. Psychoanalytic Inquiry, 37(3), 153 166. Available from https://doi.org/ 10.1080/07351690.2017.1285185. Petraglia, J., Bhatia, M., de Roten, Y., Despland, J.-N., & Drapeau, M. (2015). An empirical investigation of defense interpretation depth, defensive functioning, and alliance strength in psychodynamic psychotherapy. American Journal of Psychotherapy, 69(1), 2015. Process research in psychodynamic psychotherapy: interventions and the therapeutic relationship 87 Piper, W. E., Joyce, A. S., McCallum, M., Azim, H. F., & Ogrodniczuk, J. S. (2002). Interpretive and supportive psychotherapies: Matching therapy and patient personality. Washington, DC: American Psychological Association. Roy, C. A., Perry, C. J., Luborsky, L., & Banon, E. (2009). Changes in defensive functioning in completed psychoanalyses: The Penn psychoanalytic treatment collection. Journal of the American Psychoanalytic Association, 57(2), 399 415. Available from https://doi. org/10.1177/0003065109333357. Ryum, T., Stiles, T. C., Svartberg, M., & McCullough, L. (2010). The role of transference work, the therapeutic alliance, and their interaction in reducing interpersonal problems among psychotherapy patients with cluster C personality disorders. Psychotherapy: Theory, Research, Practice, Training, 47(4), 442 453. Available from https://doi.org/ 10.1037/a0021183. Safran, J. D., Muran, J. C., Samstag, L. W., & Winston, A. (2005). Evaluating alliancefocused intervention for potential treatment failures: A feasibility study and descriptive analysis. Psychotherapy: Theory, Research, Practice, Training, 42, 512 531. Available from https://doi.org/10.1037/0033-3204.42.4.512. Schut, A. J., Castonguay, L. G., Flanagan, K. M., Yamasaki, A. S., Barber, J. P., Bedics, J. D., & Smith, T. L. (2005). Therapist interpretation, patient-therapist interpersonal process, and outcome in psychodynamic psychotherapy, for avoidant personality disorder. Psychotherapy: Theory, Research, Practice, Training, 42(4), 494 511. Available from https://doi.org/10.1037/0033-3204.42.4.494. Slavin-Mulford, J., Hilsenroth, M., Weinberger, J., & Gold, J. (2011). Therapeutic interventions related to outcome in psychodynamic psychotherapy for anxiety disorder patients. Journal of Nervous and Mental Disease, 199(4), 214 221. Available from https://doi. org/10.1097/NMD.0b013e3182125d60. Stigler, M., de Roten, Y., Drapeau, M., & Despland, J. N. (2007). Process research in psychodynamic psychotherapy: A combined measure of accuracy and conflictuality of interpretations. Swiss Archives of Neurology and Psychiatry, 58, 225 232. Stiles, W. B., Glick, M. J., Osatuke, K., Hardy, G. E., Shapiro, D. A., Agnew-Davies, R., & Barkham, M. (2004). Patterns of alliance development and the rupture-repair hypothesis: Are productive relationships U-shaped or V-shaped? Journal of Counseling Psychology, 51, 81 92. Available from https://doi.org/10.1037/0022-0167.51.1.81. Summers, R. F., & Barber, J. P. (2010). Psychodynamic therapy: A guide to evidence-based practice. New York, NY: Guilford. Town, J. M., Hardy, G. E., McCullough, L., & Stride, C. (2012). Patient affect experiencing following therapist interventions in short-term dynamic psychotherapy. Psychotherapy Research, 22(2), 208 219. Available from https://doi.org/10.1080/10503307.2011.637243. Town, J. M., Salvadori, A., Falkenström, F., Bradley, S., & Hardy, G. (2017). Is affect experiencing therapeutic in major depressive disorder? Examining associations between affect experiencing and changes to the alliance and outcome in intensive short-term dynamic psychotherapy. Psychotherapy, 54(2), 148 158. Available from https://doi.org/ 10.1037/pst0000108. Trijsburg, R. W., Frederiks, G. C. F. J., Gorlee, M., Klouwer, E., den Hollander, A. M., & Duivenvoorden, H. J. (2002). Development of the Comprehensive Psychotherapeutic Interventions Rating Scale (CPIRS). Psychotherapy Research, 12(3), 287 317. Available from https://doi.org/10.1093/ptr/12.3.287. Tschuschke, V., Crameri, A., Koehler, M., Berglar, J., Muth, K., Staczan, P., & KoemedaLutz, M. (2015). The role of therapists’ treatment adherence, professional experience, therapeutic alliance, and clients’ severity of psychological problems: Prediction of 88 Contemporary Psychodynamic Psychotherapy treatment outcome in eight different psychotherapy approaches. Preliminary results of a naturalistic study. Psychotherapy Research, 25, 420 434. Available from https://doi. org/10.1080/10503307.2014.896055. Tummala-Narra, P. (2016). Psychoanalytic theory and cultural competence in psychotherapy. Washington, DC: American Psychological Association. Ulvenes, P. G., Berggraf, L., Hoffart, A., Stiles, T. C., Svartberg, M., McCullough, L., & Wampold, B. E. (2012). Different processes for different therapies: Therapist actions, therapeutic bond, and outcome. Psychotherapy, 49(3), 291 302. Available from https:// doi.org/10.1037/a0027895. Zilcha-Mano, S. (2017). Is the alliance really therapeutic? Revisiting this question in light of recent methodological advances. American Psychologist, 72(4), 311. Available from https://doi.org/10.1037/a0040435. Zilcha-Mano, S., McCarthy, K. S., Dinger, U., & Barber, J. P. (2014). To what extent is alliance affected by transference? An empirical exploration. Psychotherapy: Theory, Research, & Practice, 51, 424 433. Available from https://doi.org/10.1037/a0039373. Zilcha-Mano, S., Muran, J. C., Hungr, C., Eubanks, C. F., Safran, J. D., & Winston, A. (2016). The relationship between alliance and outcome: Analysis of a two-person perspective on alliance and session outcome. Journal of Consulting and Clinical Psychology, 84, 484 496. Available from https://doi.org/10.1037/ccp0000058. Zilcha-Mano, S., Solomonov, N., Chui, H., McCarthy, K. S., Barrett, M. S., & Barber, J. P. (2015). Therapist-reported alliance: Is it really a predictor of outcome? Journal of Counseling Psychology, 62, 568 578. Available from https://doi.org/10.1037/ cou0000106. Research support for psychodynamic constructs 6 Kenneth N. Levy1, John R. Keefe2 and Johannes C. Ehrenthal3 1 Department of Psychology, Weill Cornell Medical College, Pennsylvania State University, University Park, PA, United States, 2Weill Cornell Medical College, University of Pennsylvania, University Park, PA, United States, 3Heidelberg University, Heidelberg, Germany Beginning with Freud, psychoanalytic theory has provided a number of clinically rich and useful concepts that illuminate our understanding of normative processes of the self and interpersonal relationships and of the development and treatment of psychopathology. Central to psychodynamics has been a focus on unconscious processes, subjective experience, and defensive processes, among others constructs. Contrary to common misconceptions, there is a great deal of empirical support for psychodynamic concepts, which we will survey in this chapter. Basic tenets and concepts There are a number of basic tenets and concepts that are central to psychodynamic theory. These include the idea that some mental processes, such as motives, desires, and memories, are not available to awareness or conscious introspection. This idea is often referred to as unconscious mental functioning or unconscious processing. Unconscious mental processes have evolved from a conceptual proposition based on clinical observations to a field of study in psychodynamic research (Westen, 1998) and have been integrated in research within social psychology (Dijksterhuis & Strick, 2016) and neurosciences (Soon, Brass, Heinze, & Haynes, 2008). While attention to unconscious mental life remains central to psychoanalytic or psychodynamic psychotherapy, much of our experience is available and accessible for introspection, reflection, and conscious decision making. As Wachtel (2005) has noted, consciousness is better conceptualized as a matter of degree of accessibility and articulation than as a discrete division between conscious and unconscious. Another tenet of the psychodynamic approach is that while some mental processes happen to be outside of our awareness, people are also motivated to push threatening thoughts or feelings from awareness. This process is the idea of defense or defense mechanism. This concept of defense is generally supported in the empirical literature examining narratives of adults, psychophysiological data, and neuroscience data and is generally well accepted (Cramer, 2000). A third tenet central of Contemporary Psychodynamic Psychotherapy. DOI: https://doi.org/10.1016/B978-0-12-813373-6.00006-4 © 2019 Elsevier Inc. All rights reserved. 90 Contemporary Psychodynamic Psychotherapy psychodynamic theory is that of a developmental perspective wherein childhood relationships with caregivers are seen as playing a role in shaping current relationships. This is not to imply a linear relationship or a critical period between early experience and later development. Psychodynamic theory, consistent with a developmental psychopathology perspective, is probabilistic rather than deterministic. From this perspective, childhood experiences, in concert with genetic (what Freud called constitutional) factors, are considered with regard to their influence on one’s internal experience of oneself as well as one’s overt behavior. A fourth tenet of a psychodynamic perspective emphasizes the importance of subjective experience or individual or personal meaning of events. Psychodynamic theorists and clinicians are interested in the patient’s phenomenological experience, that is, how the patient experiences himself or herself, important others, and the world in general. This differs from the schema concepts of the cognitive-behavioral tradition in that from a psychodynamic perspective, these schemas are seen as having both explicit, conscious aspects and implicit, unconscious aspects, with the latter including both implicit parts (i.e., simply beyond awareness) and parts that are kept out of awareness for defensive purposes. The psychodynamic model also posits that individuals may use one set of representations—inner templates of self and others—to defend against other intolerable representations. Finally, there is greater attention to the emotional aspects of these schemas and to the structural aspects of representations, that is, the degree of differentiation and hierarchical integration of representations (see Blatt, Auerbach, & Levy, 1997). Evidence from developmental, clinical, and neurological sciences provides validation for these basic premises (for a review, see Westen, 1999). In addition to the ideas of unconscious processes, defense mechanisms, a developmental perspective, and subjectivity, the concept of transference (and the related concept of countertransference) is central to psychodynamic clinical approaches. Although other concepts have been stressed within psychoanalysis at various times, such as the Oedipus complex or psychosexual stages, we would contend that these concepts are not as central to contemporary psychodynamic models as they were in the past. In this chapter we will review evidence for key psychodynamic concepts, with a focus on classic and recent research, in order to develop a big-picture perspective. Specifically, we will focus on the unconscious and defense mechanisms, transference, insight, and mentalizing and on some implications of these concepts for the psychotherapy process. Although the developmental perspective is central to a psychodynamic approach, we will not focus on it in this chapter because it is no longer unique or specific to psychodynamics. However, we will address some aspects of attachment theory, where relevant, and we refer interested readers to the literature of attachment theory as empirical support for this aspect of psychodynamics (see Levy et al., 2015). Defensive processes Psychodynamic conceptualizations of defensive processes have evolved considerably since first being proposed by Freud. Quite simply, a defense mechanism is a Research support for psychodynamic constructs 91 process by which one pushes threatening thoughts or feelings from awareness. Freud developed drive theory, in which defense was not just seen as a repression but described as the compromise formation between two competing ideas: on the one hand, a wish, a desire, or a want (impulse) and, on the other hand, a prohibition against the wish, desire, or want. This created an inner conflict and resulted in a compromise formation involving defensive thoughts, feelings, or behaviors. Typically, one or both sides of the conflict were partially or fully out of awareness. Dreams, forgetting, parapraxes (Freudian slips), and neurotic symptoms were all seen as compromise formations or the result of defensive processes. Often, the wish or desire was sexual or aggressive and seen as deriving from an internal drive. In the service of compromise formation, defensive solutions can range from being relatively healthy and mature (reality based) to being very unhealthy, immature, and even underlying psychotic symptoms. More recent conceptualizations emphasize the general regulatory function of defensive operations in light of unpleasant emotions, perceptions, and cognitions. These operations follow a developmental trajectory from less mature mechanisms to more nuanced strategies (Cramer, 2015), helping the individual to remain functional in a complex world by focusing on some information while fading out other information. Defenses, however, can become restricting and dysfunctional under conditions of high levels of internal conflict or low levels of personality integration. From a clinical perspective, defense mechanisms help the therapist to observe the psychodynamics or “mind in motion.” While initially seen as predominantly intrapsychic, defensive functioning mayinfiltrate interpersonal relations as well (Westerman, 2018). Given the considerable amount of empirical research on defensive functioning, we will highlight exemplary studies and discuss some of the findings. Hierarchy of defenses The most commonly employed conceptualization of defense proposes a hierarchy of defenses, ranging in severity from mature to neurotic to immature or borderline defenses (Perry & Bond, 2005; Vaillant, Bond, & Vaillant, 1986). Mature defenses, to a degree, recognize the meanings associated with potentially threatening mental contents; an example would be consciously deciding to not deal with distressing interpersonal news until a different point in the day (i.e., suppression). Neurotic defenses attempt to prevent conflicted mental contents from reaching full conscious awareness through avoidance (e.g., intellectualization), misattribution (e.g., displacement, projection), or blocking (e.g., isolation of affect, repression) of threatening mental contents. Immature or borderline defenses entail substantial distortions that affect representations of the self and others and/or external reality to attenuate anxiety (e.g., devaluation) or to express parts of a conflict in an exaggerated, pathological form (e.g., acting out). Overall, levels of self- and observer-reported defensive functioning correlate with degree of psychosocial functioning, both crosssectionally and longitudinally (Bond, 2004). While individuals with low levels of personality functioning or integration share a considerable amount of immature defenses, there are some specific characteristic patterns of defense that allow blind 92 Contemporary Psychodynamic Psychotherapy observers to differentiate specific personality disorders (Perry, Presniak, & Olson, 2013) as well as symptom disorders (Bloch, Shear, Markowitz, Leon, & Perry, 1993; Busch, Shear, Cooper, Shapiro, & Leon, 1995). In addition, efforts have been made to link social psychological and other experimental findings as indicating the workings of defensive processes (Baumeister, Dale, & Sommer, 1998). A classic study in this vein examined penile response to erotic images (Adams, Wright, & Lohr, 1996), which in men is typically strongly linked to self-reported arousal (Chivers, Seto, Lalumiere, Laan, & Grimbos, 2010). The study specifically recruited ostensibly heterosexual men who self-reported being very or not at all homophobic and presented to them both heterosexual and homosexual erotic images. Interestingly, among the high-homophobia group, around half of subjects experienced penile engorgement in response to homosexual images, while this was not observed among the low-homophobia men. The authors interpreted this as evidence that homophobia was sometimes the result of the defense of reaction formation, such that strongly antihomosexual attitudes developed in response to or to prevent awareness of conflicted homosexual desires. A recent study using a gaze fixation rather than penile response paradigm conceptually replicated this finding, reporting greater incidence of gaze fixation toward homosexual erotic images among homophobic heterosexually identified men compared to less homophobic men (Cheval et al., 2016). In another study that has been cited to support evidence for projection, subjects who had been classified as high repressors (Weinberger, Schwartz, & Davidson, 1979) were more likely than other individuals to perceive in the ambiguous behavior of others traits they deemed bad, particularly traits that acquaintances indicated that the subjects had but that the subjects themselves did not report to experimenters (Newman, Duff, & Baumeister, 1997). However, on the whole the experimental literature supporting specific dynamic conceptualizations of defense is underdeveloped. One such experiment purported not to find evidence for the defense of displacement, observing that more narcissistic individuals who were insulted by a confederate did not show evidence of increased aggression toward a third party, while they did express more anger toward the insulting confederate (Bushman & Baumeister, 1998). This experimental operationalization of displacement is arguably misspecified, as displacement theoretically requires that an individual be conflicted about a feeling toward an object, whereas the average individual (never mind a narcissistic person retaliating against narcissistic injury) is possibly not conflicted about feeling angry toward an insulting individual with whom one has no prior relationship. Another explanation would be that while specific defense mechanisms are highly relevant as sometimes very subtle indicators for detecting and understanding central motivational topics (i.e., wishes and fears) of patients in the clinical situation, their stability and statistical impact on experimental tasks may be rather small. Broader approaches appear to produce more robust findings. For example, attachment theory provides a dynamically informed model for intrapsychic and interpersonal regulation, which includes the strategies of hyperactivation and deactivation. Attachment Research support for psychodynamic constructs 93 theory proposes a basic need or motive to relate that leads to the development of internal representations of the self and significant others in interaction. Depending on early interactions with primary caregivers, secure, and insecure mental representations with regard to attachment develop in early childhood and stay comparably stable across the life span (Fraley, 2002; Simpson, Collins, Tran, & Haydon, 2007). Related to these mental representations are regulatory styles of hyperactivation and deactivation of attachment-related perception, emotions, cognitions, and behavior (Mikulincer, Shaver, & Pereg, 2003). Bowlby (1980) described the mechanisms behind these styles as “unconscious defensive exclusion” employed by children to help them deal with adverse and neglecting caregivers (i.e., by keeping disturbing aspects of care out of awareness). He proposed two central defensive regulatory mechanisms that keep painful thoughts or wishes out of conscious experience: deactivation (i.e., shutting down of attachment-related emotions and cognitions) and cognitive disconnection (i.e., separation of attachment-related event and one’s emotional reaction to it and being preoccupied with one’s own internal state instead of its cause). Attachment-related defenses in adults are activated to regulate distress resulting from rejection, loneliness, or fear. In classical psychodynamic terms, there is a motive (the need to attach), which results in situational wishes (to relate to possible attachment figures), which are defended against owing to the developmentally acquired expectation that these needs will not be adequately met. Attachment-related avoidance, which is accompanied by the habitual use of deactivation as a primary regulatory strategy, has in particular been the subject of several experimental studies. Attachment avoidance was found to be related to a better ability to suppress attachment-related cognitions, less encoding of attachment-related information, and lower levels of sympathetic arousal as measured by skin conductance under conditions of normal functioning, stressing the adaptive nature of defensive strategies (Fraley & Shaver, 1997; Fraley, Garner, & Shaver, 2000). However, cognitive or attachment-related emotional loads make these potentially positive effects disappear (Gillath, Giesbrecht, & Shaver, 2009; Mikulincer, Dolev, & Shaver, 2004), suggesting the fragility of inflexibility in regulatory strategies. At the same time it is relevant to consider the outcome criterion being studied. For example, there are main effects of attachment avoidance on the perception, recognition, and reaction to especially negative emotions in others (Dan & Raz, 2012; Dewitte, 2011; Suslow, Dannlowski, Arolt, & Ohrmann, 2010) but also a retrospective overestimation of negative emotions in romantic partners (Overall, Fletcher, Simpson, & Fillo, 2015). Nonsituational variables also have an impact on attachment-related reaction; for example, interactions between adverse childhood experiences and attachment insecurity may affect psychobiological reactivity and recovery (Ehrenthal, Levy, Scott, & Granger, 2018). To sum up, attachment theory may provide a model of studying defensive processes while at the same time pointing out the difficulties of such research. Comprehensive psychodynamic research programs focused on understanding the operations of particular defenses or defensive regulatory styles would be invaluable for disentangling basic and applied aspects of regulatory defensive processes. 94 Contemporary Psychodynamic Psychotherapy Defense change in psychotherapy If generally agreed-upon features of defense are valid—that defenses act unconsciously to prevent awareness of conflicted mental contents, both preventing the working through of conflict and underlying symptoms and dysfunctions in themselves—it should be expected that improvements in defensive functioning would be a unique signature of longitudinal treatment success. Perhaps the most rigorous examination of change in defense to date, defensive functioning of patients in a mixed sample (predominantly personality disordered; n 5 21) receiving long-term psychodynamic therapy was rated near the beginning of therapy, midtreatment (approximately 6 months), and after 2.5 years rated by blind observers using the Defense Mechanisms Rating Scales (Perry & Bond, 2012). Patients who experienced greater improvement in observer-rated defensive functioning from the beginning of treatment to 2.5 years evidenced superior improvements in symptoms (r 5 0.58) and psychosocial functioning (r 5 0.60) over the next 2.5 years of follow-up, controlling for their intake severity in symptomatology and psychosocial functioning. Improvements in defensive functioning reflected diminished use of defenses theorized to be less mature and adaptive (e.g., projective identification; d 5 20.67) as well as increases in the use of adaptive defenses (e.g., humor; d 5 0.80) (Perry & Bond, 2012). Several other studies have also found correlations between contemporaneous improvements in defensive functioning and symptomatic remission or functional improvements in binge-eating disorder (Hill et al., 2015), cluster C personality disorder (Johansen, Krebs, Svartberg, Stiles, & Holen, 2011), depression (Kramer, de Roten, Perry, & Despland, 2013), adjustment disorder (Kramer, Despland, Michel, Drapeau, & de Roten, 2010), and samples with a mix of mood, anxiety, and personality disorders (Bond & Perry, 2004; Lindfors, Knekt, Heinonen, Harkanen, & Virtala, 2015). Across investigations of change in defense mechanisms, it is typically reported that the use of mature defense mechanisms and immature defenses generally shifts the most during treatment (Perry & Bond, 2017). In addition, a change in these defense bands—but not neurotic or high-borderline defenses—is often found to correlate with symptomatic and functioning improvements (Schauenburg, Willenborg, Sammet, & Ehrenthal, 2007). This might lead to a conclusion that defensive functioning changes through a combination of including more mature defenses in the defensive repertoire while simultaneously cutting down on the use of the most distorting defenses. However, these group-level findings may belie substantive clinical heterogeneity in defense style and change between individuals, thereby inviting consideration of whether changes in defenses that are specific to the individual’s characteristic use are particularly predictive of improvements in therapy. For example, an individual with borderline personality traits whose defense use indicates a high focus on affect and action over meaning making (e.g., acting out) may especially benefit from using relatively more obsessional, affect-dampening defenses (e.g., intellectualization, isolation of affect). However, further research is needed, which takes into account dynamic and static aspects of defenses and how they relate to other aspects of functioning such as emotion regulation Research support for psychodynamic constructs 95 (Aldao, Nolen-Hoeksema, & Schweizer, 2010) or ego functioning (for an international perspective, see Ehrenthal & Benecke, 2019). Transference Generally, transference is considered to be a tendency in which representational aspects of important and formative relationships (such as with parents and siblings) can be both consciously experienced and/or unconsciously ascribed to other relationships (Levy, 2009). Similar to defensive functioning, transference has a normative side that is closely related to the economy of social cognition but may significantly distort the perception of others. Experimental studies of transference In discussing experimental support for transference, it is helpful to distinguish between what can be termed general transference and dynamic transference. General transference refers to the degree to which relational schemata developed from past experiences of important relationships are activated to influence perceptions, goals, and behaviors toward other people in the current relational environment. There is ample evidence supporting the existence of general patterns of transference in day-to-day life (Przybylinski & Andersen, 2012). A typical experimental paradigm for examining general transference entails two steps, the second taking place at least a week after the first and ostensibly entailing a different study. In the first step, subjects are asked to generate several positive and negative descriptions of at least two significant life figures. In the second step, these same subjects are presented with an individual (either through verbal description or in the form of a confederate) whose traits match those of significant life figures provided in the first step, often to a shallow or minor degree. The alternative condition in such studies typically pairs a subject with individuals matched to other subjects’ significant others. Common findings in this literature generally demonstrate that people often “fill in the blanks” of presented individuals with superficial similarity to significant life figures so as to resemble those life figures, while they do not attribute these traits to individuals without such similarity (Przybylinski & Andersen, 2012). By contrast, a specifically dynamic understanding of transference incorporates ways in which other motivated, conflicted, or defensive components of the selfinteract with relational schemata to produce a manifestation of transference. For example, an individual who has an unusually negative reaction toward someone who resembles a beloved parent, because the individual is conflicted about becoming too intimate with someone they might really like (e.g., the parent and, by extension, the acquaintance), might be said to be exhibiting dynamic transference. Much of the current empirical evidence for dynamic transference comes from research examining the ways in which attachment styles predict different patterns 96 Contemporary Psychodynamic Psychotherapy of expressing transference. Securely attached individuals who are undergoing transference induction concerning a parental figure report a relative increase in positive mood compared to more anxiously or avoidantly attached individuals (Andersen, Bartz, Berenson, & Keczkemethy, 2006). In comparison, more anxiously attached individuals experience a unique increase in anxiety under transference induction, while avoidantly attached individuals express motivation to avoid an individual who reminds them of a past positive life figure. Thus attachment styles interact with mental representations activated by transference to drive mood and motivational states, such as concern about whether the other might be accessible to them (anxious) or a desire to avoid emotional contact with a potentially desirable other (avoidant). In another attachment study involving transferential processes, individuals were asked to generate lists of traits they believe describe their actual self and traits that they “are most glad [they] don’t possess and [they] don’t want to have” and then were invited to one of three allegedly unrelated experiments (Mikulincer & Horesh, 1999). Across experiments, subjects with more anxious attachment styles were more likely to regard novel others as having traits that the subjects described for themselves, had an easier time correctly remembering novel others as having those selftraits, and exhibited memory biases toward recalling novel others as having been described with those traits even if they were not originally described that way (Mikulincer & Horesh, 1999). Strikingly, subjects with more avoidant attachment showed the opposite pattern, in which traits that were regarded as undesirable for the self were those projected onto novel others. These results suggest that more anxiously attached patients tend toward transference patterns in which they experience others as like them, whereas avoidantly attached patients are more likely to experience a transference in which others resemble what they dislike about themselves. Other studies have examined the degree to which factors such as past relational history and current mood state affect transference manifestations. In one study, individuals underwent transference induction concerning a loved significant figure toward whom the individual felt chronically relationally dissatisfied (Berk & Andersen, 2008). In the transference induction condition only, the degree to which these individuals felt hostility toward the new other predicted their behavioral persistence on a task designed to solicit liking from this new person. The authors interpreted this to indicate a conflict played out in the transference, by which individuals were frustrated with dissatisfying others but also were reciprocally motivated to (finally) acquire the others’ attention and liking. Another study hypothesized that dysphoric college students, relative to other college students, when transference-induced regarding a loved past other, would experience transference patterns commensurate with expectations of disappointment and rejection (Miranda, Andersen, & Edwards, 2013). These dysphoric students undergoing transference induction concerning a loved significant figure showed increases in state depressed mood and offered more rejected selfdescriptions as compared to induction regarding a disliked significant figure. Therapeutic focus on the transference A transference interpretation is a tactful comment that clarifies and links the patient’s experience of others outside of therapy with that of the therapist in therapy Research support for psychodynamic constructs 97 and with the patient’s experience of past relationships with caregivers (Levy, 2009). A predominant clinical hypothesis among psychodynamic clinicians and researchers is that, for patients with highly dysfunctional object relations and more severe personality pathology, transference interpretations may be too destabilizing or that such patients do not have enough capacity to work with such interpretations in a productive manner. A contrasting clinical hypothesis would be that patients with poor object relations and personality pathology may particularly benefit from the use of transference interpretations. An integrative view would be that transference interpretations may be especially helpful for individuals with low levels of personality functioning (including deficits in their ability to understand others) if the interventions are adapted to what such patients can tolerate. Recently, three trials of psychodynamic therapies were structured to focus predominantly on the therapeutic relationship and transference. The First Experimental Study of Transference compared psychodynamic therapy for a mixed disorder population, randomizing patients to receive or not receive transference interpretations (Høglend et al., 2008). In the subsample of patients with poor personality functioning (predominantly cluster C personality disorders), therapy without transference interpretations was less effective at improving patients’ insights into their conflicts and patterns of defense (see later), leading to worse improvements in psychosocial functioning compared to therapy with consistent use of transference interpretations (Hoglend et al., 2008; Høglend, Dahl, Hersoug, Lorentzen, & Perry, 2011; Johansson et al., 2010). Consistent with the integrative view stated above, for individuals with lower levels of personality functioning, transference interpretations were especially helpful if the therapists acted from a “parental” stance, whereas the converse was true for individuals with higher levels of personality functioning (Dahl et al., 2014). Among samples of patients with borderline personality disorder (BPD), transference-focused psychotherapy (TFP) has been compared to dialectical-behavioral therapy, dynamic-supportive therapy, and treatment by community experts (Clarkin, Levy, Lenzenweger, & Kernberg, 2007; Doering et al., 2010). In both trials, TFP was also shown to uniquely promote patient improvements in mentalization and attachment security (Buchheim, Horz, Rentrop, Doering, & Fischer-Kern, 2012; Fischer-Kern et al., 2015; Levy et al., 2006), which is consistent with a view that transference interpretation may be uniquely helpful in this population specifically for fostering intrapsychic integration. Chapter 3, Attachment and mentalization in contemporary psychodynamic psychotherapy, provides a more comprehensive consideration of transference and cyclical relational patterns in the context of psychotherapy. Psychodynamic psychotherapy processes Insight Insight refers to the degree to which an individual richly understands his or her own internal conflicts, defensive functioning, and maladaptive relationship patterns (Ulberg, Amlo, Dahl, & Høglend, 2017). Psychodynamic conceptions of insight 98 Contemporary Psychodynamic Psychotherapy incorporate both cognitive/intellectual and emotional levels of self-understanding. Higher-insight individuals who habitually find themselves in problematic romantic relationships not only can describe how and why they find themselves instantiating this pattern, but also have experienced the affects associated with these conflicts and have learned to recognize and tolerate them. Across multiple studies of psychodynamic psychotherapy it has been found that patients who attain greater observer-rated insight over the course of treatment have superior long-term outcomes, even statistically controlling for their prior symptomatic improvements during treatment (see the review in Ulberg et al., 2017). Conversely, patients whose insight does not improve tend to have less stable gains from therapy and do not make further positive changes across follow-up. This pattern is consistent with the perspective that gains in insight represent a unique, positive psychological change that is capturing something meaningfully different from acute symptom relief. Providing some support for this perspective, a recent metaanalysis of 22 studies (involving 1112 individuals) found a moderate effect of insight on treatment outcome (r 5 .31; 95% CI 5 .22 .40), that is, it found that insight across a variety of conditions is indeed an important treatment factor in psychotherapy (Jennissen, Huber, Ehrenthal, Schauenburg, & Dinger, 2018). The authors state that the meta-analysis was underpowered to reliably detect moderator effects, indicating that further research is needed to determine whether insight is especially related to outcome in insight-oriented treatments or is broadly applicable to different types of treatments. Mentalizing/Reflective Functioning Historically, there has been a schism between psychodynamic treatments and behavioral and cognitive-behavioral treatments in terms of focus on symptoms versus a focus on what psychodynamic scholars call structural change. By structural change, dynamic scholars mean change in the structure or organization of one’s mind; what was unconscious is now conscious, what was undifferentiated is now differentiated, and what was unintegrated is now integrated. In psychodynamic psychotherapy, structural change was seen as the Holy Grail of improvement, and symptom change was relegated to secondary importance. In contrast, CognitiveBehavioral Therapy (CBT) and especially behavioral treatments privileged symptom change. While psychodynamic therapy has over time paid increasing attention to symptom change, most dynamic treatments still focus on structural change and often consider structural change to be the mechanism by which symptom reduction occurs. Levy et al. (2006) examined structural change, defined as change in attachment and mentalizing/reflective function (RF), in the context of a randomized controlled trial for BPD. Patients receiving TFP exhibited superior improvements in RF as compared to patients who received dialectical-behavioral therapy (DBT) or manualized dynamic-supportive therapy (d vs DBT 5 0.56, d vs supportive 5 0.85). In fact, RF did not reliably change in either of the two comparison treatments. Research support for psychodynamic constructs 99 Importantly, and increasing our confidence in the findings, they were replicated in another randomized trial for BPD: Patients who were randomized to TFP exhibited significantly greater improvements in RF as compared to patients in an enhanced treatment as usual condition with expert community providers (d 5 0.45), among whom RF did reliably not increase (Fischer-Kern et al., 2015). Intriguingly, patients who improved their RF capacities also tended to develop healthier personality organizations (r 5 0.31), bespeaking an increasing capacity to stably maintain a complex image of themselves and of others by integrating different types of representations. Psychodynamic neuroscience Evidence is mounting that psychodynamic therapy encourages neurobiological changes that are commensurate with, yet unique from, those produced by cognitivebehavioral therapies (Abbass, Nowoweiski, Bernier, Tarzwell, & Beutel, 2014; Roffman, Gerber, & Glick, 2012). Neurobiological changes during psychodynamic treatments have been observed in major depressive disorder (MDD), panic disorder, BPD, and somatoform disorder (Abbass et al., 2014; Perez et al., 2016; Roffman et al., 2014; Wiswede et al., 2014). These neurobiological changes are typically found to correlate with the degree of symptomatic improvements patients experienced in therapy. By contrast, psychodynamic theory has not strongly informed the probes and tasks that patients undergo in neurobiological studies, even in most examinations of psychodynamic therapies. For example, in neuroimaging investigations of MDD, patients often perform basic neurocognitive exercises, such as n-back working memory tasks, Go/NoGo response inhibition and signal detection tasks, classifying generic faces as reflecting broad emotional categories (e.g., happy, sad), or reading generic positively, negatively, or neutrally valenced sentences (Muller et al., 2017). These studies generally assume that a basic neurocognitive function instantiated in particular brain regions is commonly dysregulated among individuals with MDD, building on research identifying cognitive deficits and differences in MDD patients, such as attentional bias toward negatively valenced stimuli (Warren, Pringle, & Harmer, 2015). Strikingly, a recent large-scale meta-analysis of functional magnetic resonance imaging studies comparing blood oxygen level dependent (BOLD) activation in various scanner tasks among MDD patients as compared to control subjects (Muller et al., 2017) found no replicated areas of hyperactivated or hypoactivated brain regions consistent across different experiments. Patients with depression comprise a heterogeneous group with multiple etiologies for their depressed state (Fisher & Boswell, 2016) that may not reflect common neural substrates for shared symptomatology. It is possible that these types of neuroimaging tasks do not capture more nuanced or idiosyncratic interpersonal or intrapersonal processes that give rise to and maintain a depressed state. Psychodynamically informed, personalized 100 Contemporary Psychodynamic Psychotherapy neuroimaging probes could potentially produce more informative, replicable, and clinically interesting results. A novel psychodynamic approach to neuroimaging in depression attempted to develop personalized psychodynamic-interpersonal stimuli for patients, under the hypothesis that these stimuli would activate mental representations of their idiosyncratic dynamics (Kessler et al., 2011). To organize the construction of these stimuli, experienced clinicians conducted a structured clinical interview using the Operationalized Psychodynamic Diagnosis system (OPD Task Force, 2008). Individualized stimuli of sentences describing a subject’s most typical interpersonal pattern were generated on the basis of coding of the subject’s interviews by independent judges. For example, one subject was assigned the following personalized experimental stimulus set: “You wish to be accepted by others,” “Therefore you do a lot for them,” “That is often too close for them, so they retreat,” “Then you feel empty and lonesome.” Stimulus sets were generated for both depressed and psychiatrically healthy subjects, and patterns of whole-brain BOLD activation were compared for both viewing of the individual stimuli and a control condition consisting of a stressful narrative about navigating traffic. As compared to controls, patients evidenced patterns of activation suggesting especially heightened limbic (e.g., amygdala) and subcortical (e.g., basal ganglia) hyperactivity when viewing their individualized stimulus compared to the control narrative. The authors interpreted this to indicate that the depressed patients may have increased emotional involvement with and affective activation from situations reflecting their interpersonal conflicts. Interestingly, a follow-up study was performed on these same patients and control participants after the patients had received 8 months of psychodynamic therapy, which focused on the intrapsychic conflicts and dysfunctional interpersonal patterns derived from the OPD that were used to generate their personalized experimental stimuli (Wiswede et al., 2014). After treatment, patients no longer evidenced hyperactivity of limbic and subcortical structures in response to reading about their problematic interpersonal patterns, which could be a neurobiological signal of working through these conflicts. Another trial of 15 months of psychodynamic therapy for recurrent MDD also used personalized stimuli as neuroimaging probes, this time developed from attachment-relevant narratives generated by the Adult Attachment Projective picture set (Buchheim et al., 2012). Similarly, limbic normalization compared to control subjects was observed before and after treatment. Unique to this study, normalization of task-generated activity was observed in the subgenual cingulate (specifically implicated in treatment-resistant depression) and the medial prefrontal cortex (implicated in voluntary emotional regulation), which correlated with degree of symptom improvement. A more rigorous control condition for these types of investigations would be to have subjects also view another subject’s personalized stimuli. This would help to determine whether observed differences in activity constitute altered responses to interpersonal narratives generally or specifically interpersonal narratives reflecting problematic patterns that define the individual’s own life. Research support for psychodynamic constructs 101 Conclusion There is strong, accumulating evidence from attachment theory, experimental psychology research, including neuroscience, and psychotherapy research that supports the validity and clinical usefulness of several constructs (defensive processes, transference and countertransference, insight, and mentalizing) that underlie psychodynamic psychotherapy. For instance the concept of transference is consistent with what is known about schemas and pattern matching, implicit memory processes, and other concepts from cognitive and neurological sciences. There is also interesting preliminary evidence that transference is not just a cognitive-information bias or process but that it is also a dynamic process related to attachment and defensive processes. The psychodynamic model of mind is a generative research framework. Future experimental and clinical work on psychodynamic psychological mechanisms may not only help to elucidate the processes of psychotherapy and change, but also provide unique hypotheses and data with which to richly describe and predict human cognition and behavior. References Abbass, A. A., Nowoweiski, S. J., Bernier, D., Tarzwell, R., & Beutel, M. E. (2014). Review of psychodynamic psychotherapy neuroimaging studies. Psychotherapy and Psychosomatics, 83, 142 147. Available from https://doi.org/10.1159/000358841. Adams, H. E., Wright, L. W., Jr., & Lohr, B. A. (1996). Is homophobia associated with homosexual arousal? Journal of Abnormal Psychology, 105, 440 445. Aldao, A., Nolen-Hoeksema, S., & Schweizer, S. (2010). Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review, 30, 217 237. Available from https://doi.org/10.1016/j.cpr.2009.11.004. Andersen, S. M., Bartz, J., Berenson, K., & Keczkemethy, C. (2006). Triggering the attachment system: Evoking emotions through implicitly activating a parental representation. New York, NY: New York University. Baumeister, R. F., Dale, K., & Sommer, K. L. (1998). Freudian defense mechanisms and empirical findings in modern social psychology: Reaction formation, projection, displacement, undoing, isolation, sublimation, and denial. Journal of Personality, 66, 1081 1124. Available from https://doi.org/10.1111/1467-6494.00043. Berk, M. S., & Andersen, S. M. (2008). The sting of lack of affection: Chronic goal dissatisfaction in transference. Self and Identity, 7, 393 412. Available from https://doi.org/ 10.1080/15298860701800092. Blatt, S. J., Auerbach, J. S., & Levy, K. N. (1997). Mental representations in personality development, psychopathology, and the therapeutic process. Review of General Psychology, 1(4), 351 374. Available from https://doi.org/10.1037/1089-2680.1.4.351. Bloch, A. L., Shear, M. K., Markowitz, J. C., Leon, A. C., & Perry, J. C. (1993). An empirical study of defense mechanisms in dysthymia. American Journal of Psychiatry, 150, 1194 1198. Available from https://doi.org/10.1176/ajp.150.8.1194. 102 Contemporary Psychodynamic Psychotherapy Bond, M. (2004). Empirical studies of defense style: Relationships with psychopathology and change. Harvard Review of Psychiatry, 12, 263 278. Available from https://doi.org/ 10.1080/10673220490886167. Bond, M., & Perry, J. C. (2004). Long-term changes in defense styles with psychodynamic psychotherapy for depressive, anxiety, and personality disorders. American Journal of Psychiatry, 161, 1665 1671. Available from https://doi.org/10.1176/appi. ajp.161.9.1665. Buchheim, A., Horz, S., Rentrop, M., Doering, S., & Fischer-Kern, M. (2012). Attachment status before and after one year of transference focused psychotherapy (TFP) versus therapy as usual (TAU) in patients with borderline personality disorder. Paper presented at the 2nd International Congress on Borderline Personality Disorders and Allied Disorders, Amsterdam, The Netherlands. Buchheim, A., Viviani, R., Kessler, H., Kächele, H., Cierpka, M., Roth, G., . . . Taubner, S. (2012). Changes in prefrontal-limbic function in major depression after 15 months of long-term psychotherapy. PLoS One, 7, e33745. Available from https://doi.org/10.1371/ journal.pone.0033745. Busch, F. N., Shear, M. K., Cooper, A. M., Shapiro, T., & Leon, A. C. (1995). An empirical study of defense mechanisms in panic disorder. The Journal of Nervous Mental Diseases, 183, 299 303. Bushman, B. J., & Baumeister, R. F. (1998). Threatened egotism, narcissism, self-esteem, and direct and displaced aggression: Does self-love or self-hate lead to violence?. Journal of Personality Social Psychology, 75, 219 229. Cheval, B., Radel, R., Grob, E., Ghisletta, P., Bianchi-Demicheli, F., & Chanal, J. (2016). Homophobia: An impulsive attraction to the same sex? Evidence from eye-tracking data in a picture-viewing task. The Journal of Sexual Medicine, 13, 825 834. Available from https://doi.org/10.1016/j.jsxm.2016.02.165. Chivers, M. L., Seto, M. C., Lalumiere, M. L., Laan, E., & Grimbos, T. (2010). Agreement of self-reported and genital measures of sexual arousal in men and women: A metaanalysis. Archives of Sexual Behavior, 39, 5 56. Available from https://doi.org/ 10.1007/s10508-009-9556-9. Clarkin, J. F., Levy, K. N., Lenzenweger, M. F., & Kernberg, O. F. (2007). Evaluating three treatments for borderline personality disorder: A multiwave study. American Journal of Psychiatry, 164, 922 928. Available from https://doi.org/10.1176/ajp.2007.164.6.922. Cramer, P. (2000). Defense mechanisms in psychology today: Further processes for adaptation. American Psychologist, 55(6), 637 646. Available from https://doi.org/10.1037/ 0003-066X.55.6.637. Cramer, P. (2015). Defense Mechanisms: 40 years of empirical research. Journal of Personality Assessment, 97, 114 122. Available from https://doi.org/10.1080/00223891.2014.947997. Dahl, H.-S. J., Røssberg, J. I., Crits-Christoph, P., Gabbard, G. O., Hersoug, A. G., Perry, J. C., . . . Høglend, P. A. (2014). Long-term effects of analysis of the patient therapist relationship in the context of patients’ personality pathology and therapists’ parental feelings. Journal of Consulting Clinical Psychology, 82, 460 471. Available from https://doi.org/10.1037/a0036410. Dan, O., & Raz, S. (2012). Adult attachment and emotional processing biases: An EventRelated Potentials (ERPs) study. Biological Psychology, 91, 212 220. Available from https://doi.org/10.1016/j.biopsycho.2012.06.003. Dewitte, M. (2011). Adult attachment and attentional inhibition of interpersonal stimuli. Cognition and Emotion, 25, 612 625. Available from https://doi.org/10.1080/ 02699931.2010.508683. Research support for psychodynamic constructs 103 Doering, S., Horz, S., Rentrop, M., Fischer-Kern, M., Schuster, P., Benecke, C., . . . Buchheim, P. (2010). Transference-focused psychotherapy v. treatment by community psychotherapists for borderline personality disorder: Randomised controlled trial. British Journal of Psychiatry, 196, 389 395. Available from https://doi.org/10.1192/bjp. bp.109.070177. Ehrenthal, J. C., Levy, K. N., Scott, L. N., & Granger, D. A. (2018). Attachment-related regulatory processes moderate the impact of adverse childhood experiences on stress reaction in borderline personality disorder. Journal of Personality Disorders, 32, 93 114. Available from https://doi.org/10.1521/pedi.2018.32.supp.93. Fischer-Kern, M., Doering, S., Taubner, S., Horz, S., Zimmermann, J., Rentrop, M., . . . Buchheim, A. (2015). Transference-focused psychotherapy for borderline personality disorder: Change in reflective function. British Journal of Psychiatry. Available from https://doi.org/10.1192/bjp.bp.113.143842. Fisher, A. J., & Boswell, J. F. (2016). Enhancing the personalization of psychotherapy with dynamic assessment and modeling. Assessment, 23, 496 506. Available from https:// doi.org/10.1177/1073191116638735. Fraley, R. C. (2002). Attachment stability from infancy to adulthood: Meta-analysis and dynamic modeling of developmental mechanisms. Personality and Social Psychology Review, 6, 123 151. Available from https://doi.org/10.1207/S15327957PSPR0602_03. Fraley, R. C., Garner, J. P., & Shaver, P. R. (2000). Adult attachment and the defensive regulation of attention and memory: Examining the role of preemptive and postemptive defensive processes. Journal of Personality and Social Psychology, 79, 816 826. Available from https://doi.org/10.1037/0022-3514.79.5.816. Fraley, R. C., & Shaver, P. R. (1997). Adult attachment and the suppression of unwanted thoughts. Journal of Personality and Social Psychology, 73, 1080 1091. Gillath, O., Giesbrecht, B., & Shaver, P. R. (2009). Attachment, attention, and cognitive control: Attachment style and performance on general attention tasks. Journal of Experimental Social Psychology, 45, 647 654. Available from https://doi.org/10.1016/j. jesp.2009.02.011. Hill, R., Tasca, G. A., Presniak, M., Francis, K., Palardy, M., Grenon, R., . . . Bissada, H. (2015). Changes in defense mechanism functioning during group therapy for bingeeating disorder. Psychiatry, 78, 75 88. Available from https://doi.org/10.1080/ 00332747.2015.1015897. Hoglend, P., Bogwald, K. P., Amlo, S., Marble, A., Ulberg, R., Sjaastad, M. C., . . . Johansson, P. (2008). Transference interpretations in dynamic psychotherapy: Do they really yield sustained effects? American Journal of Psychiatry, 165, 763 771. Available from https://doi.org/10.1176/appi.ajp.2008.07061028. Høglend, P., Dahl, H. S., Hersoug, A. G., Lorentzen, S., & Perry, J. C. (2011). Long-term effects of transference interpretation in dynamic psychotherapy of personality disorders. European Psychiatry, 26, 419 424. Available from https://doi.org/10.1016/j. eurpsy.2010.05.006. Jennissen, S., Huber, J., Ehrenthal, J. C., Schauenburg, H., & Dinger, U. (2018). Association between insight and outcome of psychotherapy: Systematic review and meta-analysis. American Journal of Psychiatry, 175(10), 961 969. Available from https://doi.org/ 10.1176/appi.ajp.2018.17080847. Johansen, P.-Ø., Krebs, T. S., Svartberg, M., Stiles, T. C., & Holen, A. (2011). Change in defense mechanisms during short-term dynamic and cognitive therapy in patients with cluster C personality disorders. The Journal of Nervous Mental Disorder, 199, 712 715. Available from https://doi.org/10.1097/NMD.0b013e318229d6a7. 104 Contemporary Psychodynamic Psychotherapy Kessler, H., Taubner, S., Buchheim, A., Münte, T. F., Stasch, M., Kächele, H., . . . Wiswede, D. (2011). Individualized and clinically derived stimuli activate limbic structures in depression: An fMRI study. PLOS One, 6, e15712. Available from https://doi.org/ 10.1371/journal.pone.0015712. Kramer, U., Despland, J.-N., Michel, L., Drapeau, M., & de Roten, Y. (2010). Change in defense mechanisms and coping over the course of short-term dynamic psychotherapy for adjustment disorder. Journal of Clinical Psychology, 66, 1232 1241. Available from https://doi.org/10.1002/jclp.20719. Kramer, U., de Roten, Y., Perry, J. C., & Despland, J. N. (2013). Change in defense mechanisms and coping patterns during the course of 2-year-long psychotherapy and psychoanalysis for recurrent depression: A pilot study of a randomized controlled trial. The Journal of Nervous Mental Disorder, 201, 614 620. Available from https://doi.org/ 10.1097/NMD.0b013e3182982982. Levy, K. N. (2009). Psychodynamic and psychoanalytic psychotherapies. In D. Richard, & S. Huprich (Eds.), Clinical psychology assessment, treatment, and research (pp. 181 214). Burlington, MA: Elsevier Academic Press. Levy, K. N., Meehan, K. B., Kelly, K. M., Reynoso, J. S., Weber, M., Clarkin, J. F., & Kernberg, O. F. (2006). Change in attachment patterns and reflective function in a randomized control trial of transference-focused psychotherapy for borderline personality disorder. Journal of Consult Clinical Psychology, 74, 1027 1040. Available from https://doi.org/10.1037/0022-006X.74.6.1027. Lindfors, O., Knekt, P., Heinonen, E., Harkanen, T., & Virtala, E. (2015). The effectiveness of short- and long-term psychotherapy on personality functioning during a 5-year follow-up. Journal of Affective Disorders, 173, 31 38. Available from https://doi.org/ 10.1016/j.jad.2014.10.039. Mikulincer, M., Dolev, T., & Shaver, P. R. (2004). Attachment-related strategies during thought suppression: Ironic rebounds and vulnerable self-representations. Journal of Personality and Social Psychology, 87, 940 956. Available from https://doi.org/ 10.1037/0022-3514.87.6.940. Mikulincer, M., & Horesh, N. (1999). Adult attachment style and the perception of others: The role of projective mechanisms. Journal of Personality and Social Psychology, 76, 1022 1034. Mikulincer, M., Shaver, P. R., & Pereg, D. (2003). Attachment theory and affect regulation: The dynamics, development, and cognitive consequences of attachment-related strategies. Motivation and Emotion, 27, 77 102. Available from https://doi.org/10.1023/ a:1024515519160. Miranda, R., Andersen, S. M., & Edwards, T. (2013). The relational self and pre-existing depression: Implicit activation of significant-other representations exacerbates dysphoria and evokes rejection in the working self-concept. Self and Identity, 12, 39 57. Available from https://doi.org/10.1080/15298868.2011.636504. Muller, V. I., Cieslik, E. C., Serbanescu, I., Laird, A. R., Fox, P. T., & Eickhoff, S. B. (2017). Altered brain activity in unipolar depression revisited: Meta-analyses of neuroimaging studies. JAMA Psychiatry, 74, 47 55. Available from https://doi.org/10.1001/ jamapsychiatry.2016.2783. Newman, L. S., Duff, K. J., & Baumeister, R. F. (1997). A new look at defensive projection: Thought suppression, accessibility, and biased person perception. Journal of Personality and Social Psychology, 72, 980 1001. Task Force, O. P. D. (Ed.), (2008). Operationalized psychodynamic diagnosis OPD-2: Manual of diagnosis and treatment planning. Cambridge, MA: Hogrefe & Huber. Research support for psychodynamic constructs 105 Overall, N. C., Fletcher, G. J. O., Simpson, J. A., & Fillo, J. (2015). Attachment insecurity, biased perceptions of romantic partners’ negative emotions, and hostile relationship behavior. Journal of Personality and Social Psychology, 108, 730 749. Available from https://doi.org/10.1037/a0038987. Perez, D. L., Vago, D. R., Pan, H., Root, J., Tuescher, O., Fuchs, B. H., . . . Stern, E. (2016). Frontolimbic neural circuit changes in emotional processing and inhibitory control associated with clinical improvement following transference-focused psychotherapy in borderline personality disorder. Psychiatry Clinical Neurosciences, 70, 51 61. Available from https://doi.org/10.1111/pcn.12357. Perry, J. C., & Bond, M. (2012). Change in defense mechanisms during long-term dynamic psychotherapy and five-year outcome. American Journal of Psychiatry, 169, 916 925. Available from https://doi.org/10.1176/appi.ajp.2012.11091403. Perry, J. C., & Bond, M. (2017). Addressing defenses in psychotherapy to improve adaptation. Psychoanalytic Inquiry, 37, 153 166. Available from https://doi.org/10.1080/ 07351690.2017.1285185. Perry, J. C., & Bond, M. (2005). Defensive functioning [in personality disorders]. In J. Oldham, A. E. Skodol, & D. Bender (Eds.), The American Psychiatric Publishing Textbook of Personality Disorders (pp. 589 609). Washington, DC: American Psychiatric Press. Perry, J. C., Presniak, M. D., & Olson, T. R. (2013). Defense mechanisms in schizotypal, borderline, antisocial, and narcissistic personality disorders. Psychiatry, 76, 32 52. Available from https://doi.org/10.1521/psyc.2013.76.1.32. Przybylinski, E., & Andersen, S. M. (2012). Making interpersonal meaning: Significant others in mind in transference. Social and Personality Psychology Compass, 6, 746 759. Available from https://doi.org/10.1111/j.1751-9004.2012.00460.x. Roffman, J. L., Gerber, A. J., & Glick, D. M. (2012). Neural models of psychodynamic concepts and treatments: Implications for psychodynamic psychotherapy. In R. A. Levy, J. S. Ablon, & H. Kächele (Eds.), Psychodynamic psychotherapy research: Evidencebased practice and practice-based evidence (pp. 193 218). New York, NY: Humana. Roffman, J. L., Witte, J. M., Tanner, A. S., Ghaznavi, S., Abernethy, R. S., Crain, L. D., . . . Fava, M. (2014). Neural predictors of successful brief psychodynamic psychotherapy for persistent depression. Psychotherapy and Psychosomatics, 83, 364 370. Available from https://doi.org/10.1159/000364906. Schauenburg, H., Willenborg, V., Sammet, I., & Ehrenthal, J. C. (2007). Self-reported defence mechanisms as an outcome measure in psychotherapy: A study on the German version of the Defence Style Questionnaire DSQ 40. Psychology and Psychotherapy, 80, 355 366. Available from https://doi.org/10.1348/147608306x146068. Simpson, J. A., Collins, W. A., Tran, S., & Haydon, K. C. (2007). Attachment and the experience and expression of emotions in romantic relationships: A developmental perspective. Journal of Personality and Social Psychology, 92, 355 367. Available from https://doi.org/10.1037/0022-3514.92.2.355. Suslow, T., Dannlowski, U., Arolt, V., & Ohrmann, P. (2010). Adult attachment avoidance and automatic affective response to sad facial expressions. Australian Journal of Psychology, 62, 181 187. Available from https://doi.org/10.1080/00049530903567203. Ulberg, R., Amlo, S., Dahl, H.-S. J., & Høglend, P. (2017). Does insight mediate treatment and enhance outcome? Psychoanalytic Inquiry, 37, 140 152. Available from https://doi. org/10.1080/07351690.2017.1285184. Vaillant, G. E., Bond, M., & Vaillant, C. O. (1986). An empirically validated hierarchy of defense mechanisms. Archives of General Psychiatry, 43, 786 794. 106 Contemporary Psychodynamic Psychotherapy Warren, M. B., Pringle, A., & Harmer, C. J. (2015). A neurocognitive model for understanding treatment action in depression. Philosophical Transactions of the Royal Society B: Biological Sciences, 370(1677). Available from https://doi.org/10.1098/rstb.2014.0213. Weinberger, D. A., Schwartz, G. E., & Davidson, R. J. (1979). Low-anxious, high-anxious, and repressive coping styles: Psychometric patterns and behavioral and physiological responses to stress. Journal of Abnormal Psychology, 88, 369 380. Westen, D. (1998). The scientific legacy of Sigmund Freud: Toward a psychodynamically informed psychological science. Psychological Bulletin, 124(3), 333 371. Available from https://doi.org/10.1037/0033-2909.124.3.333. Westen, D. (1999). The scientific status of unconscious processes: Is freud really dead? Journal of the American Psychoanalytic Association, 47(4), 1061 1106. Available from https://doi.org/10.1177/000306519904700404. Westerman, M.A. (2018). Interpersonal defense theory: An integration of philosophical considerations, psychoanalytic concepts, and perspectives on interpersonal processes that provides a guide for a wide range of therapeutic interventions. Journal of Psychotherapy Integration. 28(3), 310-328. doi:10.1037/int0000106 Wiswede, D., Taubner, S., Buchheim, A., Münte, T. F., Stasch, M., Cierpka, M., . . . Kessler, H. (2014). Tracking functional brain changes in patients with depression under psychodynamic psychotherapy using individualized stimuli. PLoS One, 9, e109037. Available from https://doi.org/10.1371/journal.pone.0109037. Further reading Buchheim, A., Horz-Sagstetter, S., Doering, S., Rentrop, M., Schuster, P., Buchheim, P., . . . Fischer-Kern, M. (2017). Change of unresolved attachment in borderline personality disorder: RCT study of transference-focused psychotherapy. Psychotherapy Psychosomatics, 86(5), 314 316. Available from https://doi.org/10.1159/000460257. Psychodynamic psychotherapy for depression in community mental health settings 7 Mary Beth Connolly Gibbons, Katherine Crits-Christoph and Paul Crits-Christoph Department of Psychiatry, University of Pennsylvania, PA, United States Short-term supportive expressive (SE) dynamic psychotherapy has evolved over time to address what we have learned from psychotherapy process research and to meet the demands of therapists, consumers, and stakeholders in real-world community settings. Community SE builds on the supportive and relationship-focused techniques first described by Luborsky (1984) and elaborated further by Book (1997). Details of applying SE specifically to patients with depressive disorders were first delineated by Luborsky et al. (1995). Since these publications, we have had substantial experience training therapists in community mental health settings in SE psychotherapy and evaluating the effectiveness of short-term SE for consumers of services in the community (Connolly Gibbons et al. 2012, 2014, 2016). This chapter is intended to be an adjunct to these previous publications, extending and adapting the SE model to the treatment of depression in community mental health settings. Adapting SE for the community Short-term community SE has demonstrated effectiveness both in a pilot trial of community SE versus treatment as usual for depression (Connolly Gibbons et al., 2012) and in a comparative effectiveness trial of short-term dynamic therapy versus cognitive therapy for major depressive disorder in the community mental health setting (Connolly Gibbons et al., 2014, 2016). This community adaptation of SE for depression was developed specifically to meet the needs of patients and therapists working in community outpatient settings. Addressing patient needs Patients with depression who seek services at community mental health centers are at high risk of early attrition from services. Patients often present to such centers with multiple psychosocial stressors, including loss of jobs, deaths of loved ones, unstable housing situations, fear of losing child custody, and medical healthcare burdens. Our goal was to adapt SE for use in the community so that consumers Contemporary Psychodynamic Psychotherapy. DOI: https://doi.org/10.1016/B978-0-12-813373-6.00007-6 © 2019 Elsevier Inc. All rights reserved. 110 Contemporary Psychodynamic Psychotherapy could work on relationship problems in a short-term treatment that also flexibly addressed the frequent psychosocial stressors that can interfere with treatment. Addressing therapist needs Our work with therapists in community mental health systems revealed that a successful treatment for major depressive disorder would need to include interventions directly targeting the many psychosocial stressors that their patients face. It was clear that therapists had little direction in how to integrate patients’ educational needs into the therapeutic process. Some therapists are very skilled at helping patients access the resources the patients need to deal with these life circumstances, but many therapists also told us that this work took up most of the therapy. Our goal was to ensure that our intervention for depression could help motivate consumers to stay in psychotherapy by including a strong socialization component to teach patients how psychotherapy could be helpful as well as an educational component to help patients acquire the necessary resources they need to deal with life stressors, while still focusing the intervention on the alleviation of depressive symptoms. Our hope was that by addressing these issues as integral to a successful psychotherapy in the community, we would decrease the high rate of attrition that plagues community mental health centers. The community adaptation of SE consists of five important components: alliance building, relationship focus, cultural sensitivity, education, and treatment socialization. The techniques central to each component are detailed below. Alliance-building component The alliance-building component of community SE builds on the techniques outlined in the alliance-fostering psychotherapy manual developed by Crits-Christoph et al. (2006). Alliance-fostering psychotherapy was designed to provide therapists with techniques that could be used to improve the collaborative working relationship with their patients. The techniques were intended to complement any therapeutic modality but were originally examined in the context of short-term, relationship-focused psychotherapy for depression. The therapist works with the patient to establish explicit treatment goals early in treatment and reviews these goals regularly throughout the treatment. Agreement on the tasks of therapy is fostered through an explicit socialization of the patient during the first two sessions of treatment. The therapist and patient openly discuss the tasks of each participant in the therapeutic process. For example, the patient’s role is to discuss his or her feelings and whatever is on the patient’s mind. It is important that the patient not censor his or her thoughts, even if it means disagreeing with or even being angry with the therapist. The therapist’s role is to listen and provide a safe and understanding response to help the patient better understand his or her feelings and relationships. To build the therapeutic relationship, the therapist reviews these tasks regularly throughout the treatment to make sure the patient feels comfortable with the Psychodynamic psychotherapy for depression in community mental health settings 111 treatment progress. In addition, the therapist patient bond is fostered through a number of techniques, including (1) regular examination of the patient’s motivation for treatment, (2) regular monitoring of the patient’s involvement in the therapeutic process, (3) maintenance of an empathic stance indicated by the use of “we” in discussions of therapy tasks and goals, (4) use of a conversational style, (5) repeated acknowledgment that the patient is being heard, (6) use of facial expressions to exhibit interest and respect, (7) regularly noting any positive change accomplished by the patient, and (8) frequent use of reflective clarifications. In addition, the therapist monitors ruptures to the bond, as evidenced by verbal and nonverbal distancing by the patient. In cases of alliance rupture the therapist helps the patient to express his or her feelings and provides an accepting climate for such discussion. Even though therapists working in the community may already attend somewhat to developing a positive working relationship with the patient, the addition of alliancefostering techniques helps the therapist to more frequently and consistently use interventions designed to enhance the working relationship. Providing empathy and support is critical to engaging the patient in the therapeutic process. As the patient’s depression begins to lessen and the alliance strengthens, goals will shift to the relationship focus of SE. Reviewing agreement on tasks and goals and coping with ongoing depression are critical to the adaptation of SE for treating depression in the community. Relationship-focused component Like standard SE therapy, community SE focuses on helping patients explore the wish and response patterns that characterize their current relationships. The main techniques to help patients explore their maladaptive relationship patterns are drawn from the Core Conflictual Relationship Theme (CCRT) method described by Luborsky (1984; see also Book, 1997). The CCRT model postulates that all interpersonal interactions are driven by three components: the patient’s wishes or needs involving the other person, the patient’s stereotypic way of perceiving the reaction of the other person toward the patient, and the stereotypic way the patient reacts to the other person. CCRT patterns are thought to develop across the life span in reaction to life events, early relationships with caregivers, peer relationships, early romantic relationships, and any other relationship experiences that influence the patient’s views of other and the self. In community SE the therapist helps the patient explore multiple aspects of the patient’s wish response pattern. Identifying wishes and responses in current relationship stories The first task for the therapist in formulating the patient’s interpersonal wish and response patterns is to get the patient to tell specific stories of discreet interactions the patient has had recently with the important people in his or her world. Patients often speak in generalities: “He always does this” or “She’ll often just ignore me.” Part of developing a rich formulation of the patient’s patterns is dependent on getting multiple 112 Contemporary Psychodynamic Psychotherapy stories in which the patient describes clearly what the other person actually did and how the patient responded. By eliciting full descriptions of specific interactions, the therapist can get ideas about response patterns that might be problematic, which the patient may not even recognize. It is important to encourage the patient to describe in detail how he or she actually responded to the other person. Patients most often refer generally to how they felt (e.g., “It made me so angry”) but rarely explain in detail how they actually responded. The therapist should express a lot of sympathy for how the patient felt and should provide an accepting environment to help the patient explore his or her own response. The therapist should use questions and clarifications to understand the patient’s interpersonal wishes or needs that were driving the specific interaction. Rarely does the patient explain what it is he or she wanted from the other person without being asked. When asked what they wanted from the other person, patients will initially state a very concrete wish such as “I just wanted him to take out the trash” or a wish that addresses only part of their true wish, such as “I just wanted him to leave me alone.” It is the therapist’s job to explore with the patient the more complex layers of the wish through clarification of what the patient provides and interpretation of the deeper wish that the therapist sees in the story. Recognizing the pattern of wishes and responses across interpersonal interactions Multiple discrete stories are needed in order to develop a full understanding of the relationship pattern that is interfering with the patient’s current relationships. As the therapist starts to see the wish and response patterns that are repeated across the stories, the therapist should use statements to point out to the patient how the wishes and responses across stories are similar. It is important that the patient recognize that the wishes and responses are forming a pattern before the patient can fully understand why he or she needs to change the pattern. In community SE the goal is to make the wish and response pattern explicit for the patient in the early stages of treatment. Initially, the therapist helps to point out specific wishes and responses in specific stories, and in collaboration, the therapist and patient move toward identifying the pattern, using language that the patient can understand. Often, the patient comes up with a shorthand reference to the pattern. In one case, the therapist repeatedly made statements to the patient highlighting how the patient really wanted respect from other people, how she often saw people as putting her down, and how she responded by putting the other person down. The patient on her own came to refer to her pattern as “my devaluing thing.” This is a helpful part of the process of the patient coming to own his or her pattern. Recognizing the historical origins of the interpersonal pattern In community SE we use the CCRT method primarily to help the patient identify and understand the relationship patterns that contribute to current problems. Although past relationships are seen as formative, exploration of past relationships is restricted to helping the patient understand the origins of the pattern once it has been identified in current relationships. Many patients feel shame about their Psychodynamic psychotherapy for depression in community mental health settings 113 patterns. For example, a patient who has the stereotypic response of exploding with anger may feel that there is something wrong with him or her and may wonder, “Why do I keep doing this?” Once the patient and therapist have identified the recurrence of a problematic response pattern in the patient’s current relationships, it is helpful to ask where the patient thinks he or she learned to respond like this. By exploring some past relationship experiences, the therapist can often help to normalize the patient’s stereotypic response and reduce shame. The therapist can point out to the patient how the anger response may have been expected and can be easily understood in the context of the past experiences. The current maladaptive response of self is described to the patient not as something that the patient is doing wrong but as a response style that made sense in past experiences but is not working for the patient in current interpersonal interactions. With this insight, it is not unusual for the patient to review and modify his or her response as the patient feels more accepting and less shameful about it. Exploring the patient’s role in maintenance of a maladaptive interpersonal pattern Once the patient comes to recognize a specific interpersonal pattern that keeps repeating itself across relationships, the patient needs to work toward understanding his or her own role in the maintenance of the pattern, which can help to maintain motivation for making changes. Patients may have learned to expect others to treat them badly and have learned a maladaptive response style to defend themselves. For instance when a patient learns that other people are going to hurt him, he may learn to protect himself by keeping at a distance from others. This pattern may be helpful for a child who needs to protect himself but becomes very maladaptive when, as an adult, he misperceives others as intending to hurt him when in reality they do not have that intention. Maybe there is a kernel of truth to the perception that another significant person does not have the patient’s best interest at heart, but the patient is expecting the other person to be hurtful and so misperceives even small, insignificant behaviors on the other’s part as intending to hurt. Alternatively, the patient may accurately perceive the behaviors of another person when the patient is behaving in some way, usually unconsciously, to elicit this behavior. This sometimes occurs when a patient has competing wishes. Perhaps the patient is aware of wanting respect from another person but also very much wants to be taken care of. If the patient perceives the other person as putting the patient down, the patient may stand up to the other person and tell the person off to prove that the patient deserves respect. The problem is that this behavior may put distance in the relationship and may result in the other person not wanting to take care of the patient. By asserting independence and pushing the other person away, the patient is setting the other person up for not taking care of the patient. Once the patient recognizes what he or she is doing to perpetuate the problem and understands that this behavior is not “crazy” but rather is something that makes sense in the context of the patient’s past experiences, then the patient and therapist can together explore and practice new, more adaptive response patterns. 114 Contemporary Psychodynamic Psychotherapy Integrating the relationship focused component with the other components of community SE Community SE is designed to be implemented flexibly, using the various components as needed across the treatment. Efforts should be made to use every opportunity to explore the relationship implications of anything the patient is talking about. For example, a patient might be in need of medical care and may need an educational intervention to help manage a serious medical problem. While using the techniques of the educational component (described below) to help the patient attain and implement the important steps to get medical attention, the therapist can also see the attempts to get medical help as examples of relationship interactions. The therapist can unpack interactions with medical personnel just as with any other significant relationships. Through integration of the techniques, the therapist can implement necessary educational techniques while still making progress unpacking the maladaptive interpersonal pattern. Cultural sensitivity component We have worked to operationalize the concepts of cultural sensitivity into specific therapeutic techniques that can be used to enhance short-term relationship-focused psychotherapy (White, Connolly Gibbons, & Schamberger, 2006). Building on guidelines for delivering more culturally sensitive treatment (American Psychological Association, 2003), we describe more specifically how to apply these general guidelines within the community SE framework. The following sections outline how community SE can be expanded to include culturally competent interventions. Increased awareness of the therapist’s biases about ethnic minority patients We believe that therapists can best begin to explore their beliefs and biases about minority patients within a supervisory relationship or within peer supervision. In supervision sessions the therapist can explore the following questions with the supervisor: What is my previous experience with members of this specific ethnic minority? What are my assumptions about the values and lifestyle of members of this ethnic minority? What biases do I have about this ethnic group and how do these biases affect my expectations of this patient? Acquisition of knowledge and understanding of the patient’s culture The primary source for gaining knowledge about the patient’s cultural background should be the patient. This joint exploration of the patient’s background by the therapist and patient can be an alliance-building experience and can help to ensure that Psychodynamic psychotherapy for depression in community mental health settings 115 the therapist learns about the patient’s culture from the patient’s perspective. In the community SE model, in each component of therapeutic work, including socialization to treatment, setting goals and tasks, exploring relationship episodes, and developing the core relationship pattern, the therapist is encouraged not only to show an interest in understanding the patient’s unique cultural background, but also to inquire of the patient how the cultural values and norms should be integrated and considered in the work. For example, the therapist and patient may work together to understand the patient’s need for respect and autonomy. The therapist should explore with the patient how the patient’s culture views autonomy, how people from the patient’s cultural background might respond to efforts to assert autonomy, and how individuals the patient respects in his or her culture have achieved respect. The cultural arena is one area in which collaborative work not only builds the alliance, but also is critical for supporting positive and lasting change. Acknowledgment and exploration of cultural differences between therapist and patient Throughout the entire psychotherapeutic process, it is important that the therapist pay attention to references made by the patient to cultural values or beliefs. Such references signal to the therapist an opportunity to acknowledge differences and explore these cultural experiences. The therapist should acknowledge the existence of differences and express a desire to understand the patient’s experience. Educationally oriented component Our work in community mental health systems also informed our focus on education within the psychotherapeutic framework. Many patients come to therapy needing medical, legal, and social services. Patients often describe to their therapists early in treatment legal problems they are experiencing, including problems with child custody. Other common problems presented to the therapist include loss of employment, potential loss of housing, and medical problems in needs of immediate attention. Many patients lack the appropriate information to acquire the necessary services and have many factors in their lives that act as barriers to receiving the services they need to maintain a stable existence. Therapists in community mental health systems are presented with a constant conflict between using the precious few psychotherapeutic sessions to help patients attain the resources they need to stabilize their families, employment, housing, and medical issues and using these sessions to implement therapeutic techniques that can relieve depression. Although the crises that bring patients to therapy are often in need of immediate attention and the therapist knows that the patient needs valuable information to avoid further personal crises, the therapist also knows that the patient’s depression in many ways inhibits the patient from solving many of these problems independently. In community SE psychotherapy the therapist is instructed to help the patient attain the information needed to avoid further life crisis while still maintaining a 116 Contemporary Psychodynamic Psychotherapy focus on the treatment of depressive symptoms. Unlike many of the empirically based psychotherapies developed outside of the community mental health setting, community SE psychotherapy acknowledges that these legal, medical, and family crises are real and need immediate attention. During the early sessions of psychotherapy the therapist should listen for life circumstances that require immediate attention in order to stabilize the individual’s life. The therapist’s task is to explore these problems in order to evaluate whether the event is serious enough to interfere with the stability of the patient’s life and thus interfere with the patient remaining in therapy. The therapist should try to unravel whether there are any necessary actions the patient should take to handle these situations and should assess whether the patient has the information and skills necessary to cope with the situation. Sometimes the best the therapist can do is help the patient target the depression, with the hopes that decreased depression can help the patient cope with the life stressors. The therapist’s task then is to use empathy and alliance-building techniques to support the patient when the patient is describing the life situations, evaluate and use educational techniques when they can be useful to help stabilize the patient, and then return to relationship-focused techniques to target the depression. Integrating the educational component with the alliance-building and relationship-focused components This focus on educating the patient regarding resources necessary to stabilize his or her life is integrated into the community SE model by providing an opportunity for the therapist to build a strong supportive therapeutic alliance with the patient and by providing an opportunity for the therapist to gather information about relationship problems that are contributing to these life circumstances. By focusing on the patient’s current important life issues, the therapist gives the message that he or she understands the importance of these issues to the patient. Without considering these important life issues, the therapist could unknowingly communicate to the patient that the therapist is out of touch with the bigger picture. Patients may be less motivated to continue in a psychotherapy that focuses exclusively on their depressive symptoms and ignores other very real issues. By starting off the treatment helping the patient to stabilize his or her life circumstances, the therapist sets up a strong, dependable therapeutic bond that can serve as the basis for doing the difficult work of uncovering the long-standing relationship problems that contribute to these life circumstances. While exploring medical, legal and social resource needs, the therapist, in addition to ensuring that the patient attains valuable information, should also attempt to understand the role of relationship patterns in these life issues. This is an excellent opportunity early in treatment to identify the important individuals in the patient’s life who are connected to these life problems. The therapist can use this exploration to gather information on what the patient wants from other important people in his or her life, how these other people are responding to the patient, and how the patient may be responding in a maladaptive way to contribute to these life circumstances. Psychodynamic psychotherapy for depression in community mental health settings 117 Socialization-focused component Many models of psychotherapy recommend socializing the patient to psychotherapy. However, very few details of how to socialize the patient are provided in existing treatment manuals, and very little attention is paid to training therapists to socialize their patients to treatment. Our work with therapists in community mental health centers highlighted how often therapists move ahead with the therapeutic process knowing that the patient is not really on board. Patients seeking treatment in community mental health centers often have chaotic lives, and although they seek services while in a particular crisis, they often have little motivation to stay engaged in psychotherapy once the initial crisis has passed. Patients often have misperceptions about exactly what psychotherapy can provide them and can feel disillusioned with a therapy that does not seem to be going anywhere. Without a sufficient understanding of how psychotherapy can help, patients often believe that psychotherapy can’t possibly change their circumstances and are then not motivated to continue. By spelling out specifically how psychotherapy can help and discussing what to expect, the therapist can help to motivate the patient to give psychotherapy a try. We have also found that patients can sometimes see psychotherapy as acute crisis management and don’t understand that they are expected to attend regularly. It is important for the therapist to explicitly review expected attendance with the patient and explore why it is useful to attend every week. For community SE we have made the socialization process a main component of the intervention rather than a simple item to mention in the first session. Our philosophy is that it is not worth moving ahead with the treatment model simply hoping that the patient will see the importance of the intervention. Rather, therapists are trained to focus on helping patients understand what therapy is all about, teaching patients how the therapy can help them, and motivating the patient to give it a try. Therapists should begin the socialization in the first session and make it an important focus throughout treatment, whenever the therapy is not progressing or when there are signs that the patient is not committed or motivated to continue psychotherapy. Our socialization to psychotherapy builds on the socialization component outlined by Book (1997) as part of time-limited dynamic psychotherapy. We have taken the socialization described by Book (1997) and extended it to include wording and information important in a community setting. The important elements of socialization to community SE include an introduction to the therapy model, specifying the time limit, presenting the relationship focus, educating the patient about how the patient’s learned relationship patterns contribute to his or her symptoms, explaining the focused goal, and detailing the therapist’s and patient’s tasks. The socialization is designed to be a collaborative discussion between the therapist and the patient. Rather than delivering a simple speech and then moving on, therapists should cover each of the elements of the socialization, inviting the patient to discuss what he or she thinks, ask questions, raise concerns, and explore conflicting motivations. Sometimes the therapist needs to refer back to the elements of the socialization throughout the therapy, for 118 Contemporary Psychodynamic Psychotherapy example, when patients slide back into a long discussion of their medical stressors. The therapist, while being very supportive of the burdens that the patient carries, should also resocialize the patient to what the therapist can offer. Dealing with lateness or nonattendance Lateness and nonattendance are common in community mental health settings. Some therapists see this so frequently that they come to view it as an inevitable part of treatment in the community. We believe that patients can be and should be encouraged to commit to their treatment. In community SE psychotherapy the therapist first uses the socialization component to set up the treatment ground rules with patients. The therapist specifically lays out the agreed-upon time for meeting and the necessity for the patient to attend every week. The therapist might use educational techniques to help some patients review how to get childcare and transportation needs met so that they can attend the psychotherapy sessions. Once the ground rules have been set, the therapist should return to the review every time the patient is late or misses a session. Even the first time a patient misses a session, the therapist should review why the patient missed the session. The therapist should be very empathic about the circumstances but should also review just how important it is for the patient to attend the sessions regularly. Denial, resistance, or poor motivation Denial, resistance, and poor motivation are also common in community mental health settings. In fact many therapists encounter these phenomena so often that they come to expect them and sometimes simply move on with the treatment, even when the patient is not on board, hoping that the patient’s motivation will improve as treatment progresses. Since attrition from treatment is so high, the goal of community SE psychotherapy is to help motivate the patient from the start and to explore any problems with motivation as they appear and as often as they appear. The therapist can use alliance-fostering techniques (e.g., reviewing treatment goals) to check in with the patient about how treatment is going on a regular basis and can review parts of the socialization interview to help get the patient back on track. Strategies for dealing with crises When a patient begins a session by describing a life crisis, the therapist should first use alliance-building techniques to support the patient and find out what happen. If the crisis occurs in the early stage of treatment, the therapist might then use some educational techniques to identify problems that need to be addressed immediately and to help the patient identify and implement solutions. This is in the service of providing baseline stability to solidify the alliance and the patient’s commitment to treatment. However, if the crisis occurs later in therapy when the alliance is strong, the therapist should ask the patient what the emotional meaning of the crisis is and whether there are people that the patient now feels he or she can go to for problem solving and support. Of course, this does not mean that the therapist isn’t Psychodynamic psychotherapy for depression in community mental health settings 119 compassionate and empathetic about the crisis, but it is important to help the patient draw on the relational work to see that he or she has the ego strength and interpersonal skills to find a solution. If the patient’s relational patterns are influencing how he or she might cope with the crisis, the therapeutic work should focus on exploring alternatives, given the insight the patient has gained thus far. For instance a patient may begin a session with a crisis, such as having been thrown out of his or her home. After providing much empathy while gathering the important details of the event, the therapist should turn to the relationship issues involved. Even if the current crisis seems quite different from the relationship issues that were previously discussed in treatment, every new event should be seen as an opportunity to broaden understanding of the relationship pattern. The therapist should ask himself or herself whether the patient’s stereotypic way of perceiving others and stereotypic way of responding to others might have contributed to the crisis or might interfere with resolution of the crisis. The therapist should try to gather specific information regarding what the patient wanted from the other people involved, how the patient saw the other people as responding to the patient, and how the patient in turn responded to the other people. The danger of the therapist being drawn into giving advice is well understood in dynamic psychotherapy, but for community SE, the danger is being drawn away from important therapeutic work in the limited shortterm framework. Termination of treatment The reality in community settings is that most psychotherapies end prematurely. With community SE we recommend utilizing the treatment as a time-limited intervention from the start. The time limits can be useful for motivating both the therapist and the patient. Since many patients seeking treatment in these settings have doubts about whether psychotherapy can really help with the enormous hurdles they face, the therapist should work with the patient to set realistic short-term goals and then motivate the patient to commit to the therapy by pointing out that it may be worth a try to commit for the short term. This time limit can often be reassuring for the patient and can help to increase the patient’s commitment to treatment. The time limits can be set firmly by agreeing to a specific number of sessions or, more flexibly, by an agreement to reevaluate treatment goals after a specific number of sessions. Either way, it is important for the therapist to regularly review these time limits with the patient. The goal is to use alliance-building techniques to maintain a focus on the agreed-upon goals and to use relationship-focused techniques to explore reactions to the termination with the therapist. Exploration of the patient’s reaction to termination can deepen the exploration of current relationship patterns. Reemergence of symptoms near the end of treatment can be expected, as patients tend to feel anxious about losing the therapeutic relationship. The therapist can use this reemergence of symptoms to deepen the patient’s understanding of the relationship conflict, and often these symptoms will lessen. 120 Contemporary Psychodynamic Psychotherapy In summary, community SE includes techniques developed in collaboration with community stakeholders to meet the needs of patients and therapists working together in community settings. This approach includes a focus on alliance building, interpersonal relationships, cultural sensitivity, education, and socialization. By including techniques to enhance the therapeutic alliance, address cultural differences, and socialize patients, this model attempts to engage patients in the therapeutic process so that relationship-focused strategies can be used to help patients explore the maladaptive relationship patterns that lead to symptoms. References American Psychological Association. (2003). Guidelines on multicultural education, training, research, practice, and organizational change for psychologists. American Psychologist, 58, 377 422. Book, H. E. (1997). How to practice brief psychodynamic psychotherapy. Washington, DC: American Psychological Association. Connolly Gibbons, M. B., Gallop, R., Thompson, D., Luther, D., Crits-Christoph, K., Jacobs, J., . . . Crits-Christoph, P. (2016). Comparative effectiveness of cognitive and dynamic therapies for major depressive disorder in a community mental health setting: A randomized clinical non-inferiority trial. JAMA Psychiatry, 73(9), 904 912. Available from https://doi.org/10.1001/jamapsychiatry.2016.1720. Connolly Gibbons, M. B., Mack, R., Lee, J., Gallop, R., Thompson, D., Burock, D., & CritsChristoph, P. (2014). Comparative effectiveness of cognitive and dynamic therapies for major depressive disorder in a community mental health setting: Study protocol for a randomized non-inferiority trial. BMC Psychology, 2, 47. Available from https://doi.org/ 10.1186/s40359-014-0047-y. Connolly Gibbons, M. B., Thompson, S. M., Scott, K., Schauble, L. A., Heintz, L. E., Thompson, D., . . . Crits-Christoph, P. (2012). Supportive-expressive dynamic psychotherapy in the community mental health system: A pilot effectiveness trial for the treatment of depression. Psychotherapy, 49(3), 303 316. Crits-Christoph, P., Connolly Gibbons, M. B., Crits-Christoph, K., Narducci, J., Schamberger, M., & Gallop, R. (2006). Can therapists be trained to improve their alliances? A pilot study of alliance-fostering therapy. Psychotherapy Research, 13, 268 281. Luborsky, L. (1984). Principles of psychoanalytic psychotherapy: A manual for supportiveexpressive treatment. New York: Basic Books. Luborsky, L., Mark, D., Hole, A. V., Popp, C., Goldsmith, B., & Cacciola, J. (1995). Supportive-Expressive dynamic psychotherapy of depression: A time-limited version. In J. P. Barber, & P. Crits-Christoph (Eds.), Dynamic therapies for psychiatric disorders (Axis I). New York: Basic Books. White, T. M., Connolly Gibbons, M. B., & Schamberger, M. (2006). Cultural sensitivity and supportive expressive psychotherapy: An integrative approach to treatment. American Journal of Psychotherapy, 60, 299 316. Panic-focused psychodynamic psychotherapy extended range 8 Fredric N. Busch1 and Barbara L. Milrod1,2,3 1 Weill Cornell Medical College, New York, NY, United States, 2New York Psychoanalytic Institute, New York, NY, United States, 3Columbia University Center for Psychoanalytic Training and Research, New York, NY, United States Introduction Panic-focused psychodynamic psychotherapy (PFPP) was developed to elaborate core psychodynamic conflicts and meanings of symptoms associated with panic disorder and agoraphobia and to modify more open-ended psychodynamic approaches to focus on panic symptoms (Busch, Milrod, Singer, & Aronson, 2012). This treatment has been extended (Panic-focused psychodynamic psychotherapy extended range; PFPP-XR) to address a range of DSM 5 (American Psychiatric Association, 2013) anxiety disorders, cluster C personality disorders, and posttraumatic stress disorder (PTSD), with the identification of dynamisms that appear prominently in these various disorders (Busch et al., 2012). PFPP has been subjected to efficacy testing in randomized controlled trials as a 12-week, 24-session psychotherapy and has demonstrated efficacy for treatment of panic disorder with and without agoraphobia (Milrod et al., 2007; Subic-Wrana, Knebel, & Beutel, 2010). It has also been studied in comparison to cognitive-behavioral therapy and applied relaxation training (Milrod et al., 2016) and meets evidence-based medicine criteria. A psychodynamic formulation for panic and anxiety disorders Busch, Cooper, Klerman, Shapiro, and Shear (1991), Shear, Cooper, Klerman, Busch, and Shapiro (1993), and Milrod, Busch, Cooper, and Shapiro (1997) articulated a series of dynamic psychological constellations underlying panic disorder. According to this psychodynamic formulation, a combination of genetically based vulnerabilities and significant developmental experiences contributes to psychological vulnerabilities to panic disorder onset and persistence as well as a range of anxiety disorders. Children in these circumstances feel particularly threatened by separation and develop a sense of fearful dependency on caregivers, who are experienced as (and often are in some ways) unreliable or rejecting. Normal efforts to develop autonomy create anxiety and conflict because of their link to separation Contemporary Psychodynamic Psychotherapy. DOI: https://doi.org/10.1016/B978-0-12-813373-6.00008-8 © 2019 Elsevier Inc. All rights reserved. 122 Contemporary Psychodynamic Psychotherapy and symbolic loss of primary attachment figures. Such strivings may well have constituted high-anxiety situations for parents in childhood because of their own separation and attachment dysregulations. The children become frightened and guilty about angry feelings and fantasies, fearing that they will disrupt or damage relationships with caregivers or parents. Defense mechanisms such as denial, reaction formation, and undoing are triggered in an unconscious effort to reduce the threat from angry feelings and fantasies and to ensure a greater sense of safety in core attachment relationships (Busch, Shear, Cooper, Shapiro, & Leon, 1995), but the potential conscious emergence of these seemingly disruptive fantasies causes persistent anxiety and guilt. In addition, mentalization, that is, the capacity to conceive of behaviors as deriving from mental states (Fonagy & Target, 1997), is disrupted in these anxious patients by avoidance of feelings and frightening experiences with caretakers. The lack of capacity to mentalize interferes with the ability to identify relevant feelings and thoughts occurring in intense attachment relationships, often contributing to conflicts being expressed in somatic form. In adulthood, perceived attachment threats cause regression and a surge of anger, anxiety, and guilt, along with a shutdown of mentalization capacity that cannot be readily identified or managed, leading ultimately to panic. The resulting panic attacks can function as punishment for angry fantasies, as a defense against anger through presenting the self as weak and damaged (often a calming fantasy for these patients), and as a plea for more regressive, childlike care from core attachment figures via appealing for help. Patients with other DSM 5 anxiety disorders have dynamic constellations that overlap in varying degrees with those typically found in patients with panic disorder. Patients with anxiety disorders are prone to viewing themselves as inadequate and ineffective, believing that another person is essential for their safety or even survival. These self-representations are triggered by fears of greater autonomy or of angry feelings, which are often perceived as threats to close attachment relationships. In addition, specific conflicts can be more characteristically prominent among patients with individual DSM 5 anxiety disorders. For example, patients with social phobia often struggle with an underlying sense of inadequacy that triggers compensatory grandiose fantasies and exhibitionistic wishes. Grandiose and exhibitionistic fantasies can create conflict and guilt and can lead to feelings of disappointment and excessive self-criticism in actual social situations, fueling anxiety. In generalized anxiety disorder, patients are often fearful of the conscious emergence of conflicted feelings and fantasies and maintain a constant state of vigilance in an effort to prevent fantasized dangers that could arise if they were to relax. Worries about finances and somatic concerns can also function as defenses against unacceptable feelings and fantasies. Chronic worrying and hypervigilance can also emerge from insecure, frightening, or unstable early relationships. Children may develop chronic fears that their close attachments with others can be easily disrupted by their own feelings and fantasies or by the fragility of others. The PFPPXR manual describes specific dynamics of various anxiety disorders in greater depths along with approaches to these disorders (Busch et al., 2012). Panic-focused psychodynamic psychotherapy extended range 123 Description of panic-focused psychodynamic psychotherapy extended range PFPP-XR differs from more open-ended psychodynamic psychotherapeutic approaches, focusing on the feelings, circumstances, and meanings of panic attacks, severe anxiety states, and phobic avoidance (Busch et al., 2012; Milrod et al., 1997). This information is used to identify and develop a psychodynamic formulation pertaining to the individual patient’s anxiety symptoms. Sessions initially are open-ended with the therapist exploring the themes that the patient brings up. However, anxiety symptoms and their impact are focused on consistently throughout the treatment. If the patient does not discuss his or her anxiety symptoms or related dynamics in the course of the session, the therapist eventually turns the patient’s attention to them. Seemingly unrelated emergent themes are consistently linked to anxiety symptoms and their underlying dynamics, including their emergence in the transference. This time-limited treatment requires a more rapid development of a formulation surrounding the underlying meanings of panic and anxiety than typically occurs in more traditional, open-ended psychodynamic psychotherapy. PFPP-XR is divided into three phases, although elements of each phase can occur throughout the treatment. In the first phase the therapeutic focus is on episodes of panic or severe anxiety; exploring the patient’s circumstances, feelings, and thoughts surrounding symptoms; and beginning to identify underlying fantasies and meanings of symptoms. The therapist works with the patient to demonstrate that symptoms have powerful emotional meanings and context rather than coming out of the blue; this work serves to improve reflective functioning. The patient’s developmental history is explored as it pertains to anxiety, and the therapist begins to discuss this overarching psychological context in terms of its potential relevance to symptoms. The therapist develops and presents a preliminary psychodynamic formulation about the meaning and dynamics of the patient’s anxiety or panic during this phase, usually within the first few sessions, typically involving themes and conflicts surrounding separation, anger, sexuality, and guilty self-punishment. This formulation provides a framework for further therapeutic work and will be added to and modified over the course of treatment. In the middle phase of therapy the therapist helps the patient to identify additional fantasies, conflicts, and developmental experiences and their relevance to prominent anxiety symptoms. The intensification of the transference during this phase allows the therapist to highlight core conflicts as they emerge in the relationship with the therapist. The goals are to reduce anxiety vulnerability with improved identification of anxiety precipitants, meanings, and conflicted feelings and fantasies; better tolerance of the patient’s own anger; and an enhanced ability to reflect on emotions and their meaning (reflective function) (Fonagy & Target, 1997). In the termination phase the therapist explores the patient’s mixed feelings about ending the therapy. If the patient has not addressed termination upon entering the final third of treatment, the therapist will raise the issue at that point. Conflicts and 124 Contemporary Psychodynamic Psychotherapy fears surrounding attachment and separation can be further explored as they emerge in the context of the upcoming separation from the therapist. These fears and conflicts can be articulated and can be understood and better tolerated in the context of the relationship with the therapist. Active focus on termination increases the patient’s capacity to manage separation, anger, guilt, and associated fantasies in ways that improve reflective functioning, which may be protective against reoccurrence of anxiety after therapy ends. Studies of panic-focused psychodynamic psychotherapy In an open clinical trial conducted at Weill Cornell Medical College, 21 patients with primary DSM 4 (American Psychiatric Association, 1994) panic disorder with or without agoraphobia were treated with twice weekly, 24-session PFPP (Milrod et al., 2000, 2001). At the end of treatment, 16 of 21 patients showed remission of panic and agoraphobia, defined by multisite panic disorder study criteria (Barlow, Gorman, Shear, & Woods, 2000). Depression remitted in patients with comorbid major depression (N 5 8). Patients demonstrated substantial improvements in symptoms and psychosocial function [within-group effect size (ES) 5 2.08 in the primary outcome measure, the Panic Disorder Severity Scale (PDSS); Shear et al., 1997], which persisted at 6-month follow-up. Milrod et al. (2007) studied 49 patients with primary DSM 4 panic disorder with or without agoraphobia, diagnosed with the Anxiety Disorders Interview Schedule (Brown, DiNardo, & Barlow, 1995), who were randomized to either PFPP or applied relaxation therapy (ART) (Cerny et al., 1984). For patients receiving medication (18%) the dose and type of medication were kept constant. Patients were excluded if they were in another psychotherapy, and those entering the study could not engage in nonstudy psychotherapy during the treatment. Patients with severe agoraphobia, comorbid major depression, and personality disorder comorbidities were included, whereas patients with psychosis, bipolar disorder, and substance abuse (6 months remission necessary) were excluded. PFPP and ART were conducted twice weekly in 24 sessions. ART consisted of a three-session cognitive explanation about panic disorder (Cerny et al., 1984), progressive muscle relaxation techniques, and in vivo exposure to anxiety-inducing situations. Adherence ratings were assessed on three sessions from each treatment and indicated high adherence in both treatments. The ART group contained a higher proportion of men (47% vs 15%; two-tailed Fisher’s exact text, P 5 0.03), but otherwise, treatment groups were matched on demographic and clinical variables. No significant between-group differences were found with symptoms of anxiety and depression, as measured by the Hamilton Depression Rating Scale (Hamilton, 1960; P 5 0.07) and the Hamilton Anxiety Rating Scale (Hamilton, 1959; P 5 0.58). With response defined as a 40% decrease in the total PDSS score from baseline (Barlow et al., 2000), PFPP demonstrated a significantly higher response rate than ART (73% vs 39%; P 5 0.016). Subjects in Panic-focused psychodynamic psychotherapy extended range 125 the PFPP condition experienced significantly greater improvement in panic symptoms, as assessed by the PDSS (P 5 0.002), and psychosocial function, as measured by the Sheehan Disability Scale (Sheehan, 1983; P 5 0.014). PFPP was well tolerated, with a 7% (2 of 26 subjects) dropout rate. PFPP was the first psychoanalytic treatment to demonstrate efficacy for treatment of an axis I anxiety disorder (DSM 4 panic disorder and agoraphobia). In a pilot study utilizing data from the controlled trial described above, Rudden, Milrod, Target, Ackerman, and Graf (2006) studied reflective function and panicspecific reflective functioning (PSRF). PSRF was developed as a measure of the extent to which patients are aware of the link between panic and anxiety symptoms and underlying emotional content. Patients treated with PFPP demonstrated a significant improvement in PSRF from baseline to posttreatment, but those treated with ART did not. However, in this pilot study, which was underpowered, the degree of change in panic severity on the PDSS did not correlate with the degree of change in the PSRF, nor was the design appropriate to assess mechanisms. Milrod et al. (2016) conducted a randomized controlled trial of 201 patients with primary DSM 4 panic disorder with or without agoraphobia at two sites (Weill Cornell Medical College and the University of Pennsylvania) comparing PFPP, cognitive-behavioral therapy (CBT), and ART. Patients were included if they had had more than one panic attack per week in the preceding month as assessed by the ADIS IV Lifetime Version (Brown et al., 1995). Patients with active substance dependence, history of bipolar disorder or psychosis, acute suicidality, or organic mental syndrome were excluded. Patients on medication were included if doses had been stable for at least 2 months. The medication was monitored throughout the course of treatment, and ongoing psychotherapy was prohibited. Patients received 19 24 sessions over 16 weeks, lasting 45 50 minutes. CBT followed the protocol of panic control therapy (Craske, Barlow, & Meadows, 2000), modified by Chambless and Schwalberg to match the number of sessions in this study. This treatment contains (1) psychoeducation about anxiety and panic disorder; (2) identification and correction of maladaptive thoughts about anxiety and panic; (3) training in slow, diaphragmatic breathing; and (4) exposure to bodily sensations designed to mimic those of anxiety and panic (interoceptive exposure). ART was more active, with a more rigorous in vivo exposure protocol than in the Milrod et al. (2007) trial, and PFPP was employed as per the treatment described in this chapter. Response was defined as 40% reduction from the baseline PDSS score (Shear et al., 1997), the primary outcome measure. Adherence ratings were assessed by modality-specific rating scales by trained raters. Patients were found to have high comorbidity, including 80% with moderate to severe agoraphobia, 73% with more than one comorbid axis I disorder, 68% with at least one additional anxiety disorder, and 48% with axis II comorbidity on the SCID-II (First, Spitzer, Gibbon, Williams, & Benjamin, 1994). Relative to the Cornell sample, the Penn patients were found to have higher baseline severity of panic disorder on the PDSS, had less education, were younger, and were less racially and ethnically diverse. There were significant site by treatment differences in the effects of psychotherapies. Cornell patients improved at similar rates across 126 Contemporary Psychodynamic Psychotherapy all three treatments, whereas Penn patients improved significantly faster in ART and CBT than in PFPP. At treatment termination, Cornell patients responded better to PFPP and CBT compared to ART, whereas Penn patients did not show a differential response across treatments. Overall response rates across both sites were 46% for ART, 63% for CBT, and 59% for PFPP. Dropout rates were significantly higher for ART, which did not vary by site, and patients who were most symptomatic dropped out of ART significantly more (69% in ART, 26% in PFPP, 24% in CBT, P 5 0.013). Medication use, which was sevenfold higher at the Penn site, did not account for all of the differences in treatment effect. The underperformance of PFPP at Penn might reflect its novelty for the psychodynamic therapists there or might reflect the influence of other process factors. PFPP-XR case example Mr. A was a 40-year-old man who directed a division of computer programmers at a tech company, was in his second marriage, and had a 5-year-old daughter from his first marriage. He had his most recent panic attack 2 days before his 40th birthday, 6 weeks before he entered treatment. He was diagnosed with panic disorder with agoraphobia, social phobia, and generalized anxiety disorder on the ADIS-IVL (Brown et al., 1995) and was randomized to a 24-session, 12-week treatment with PFPP as part of the psychotherapies for panic disorder study. Phase I In starting the treatment, the therapist explored the circumstances and feelings surrounding panic onset while attending to the meaning of symptoms. Mr. A reported that he had recently found his work extremely stressful. He acknowledged wanting to be the perfect boss and had struggled with expectations from the company that he reprimand or fire several of his employees. The necessity of doing so had increased because of financial cutbacks in his division, which he attributed to competition from other companies and poor management of his own company. He had hoped to turn around some of these problems when he had become head of his division, but it had not gone as he had expected. He felt responsible and guilty about his inability to fix the problems even as he acknowledged that he had a limited ability to control the situation. He denied being angry at the company managers, despite blaming them for many of the difficulties in his job. On the day of his panic attack, he had to fire someone and had a surge of guilt, feeling that he had let the employee down. He described it as the most stressful day in his life. When he experienced the onset of numbness and paresthesias in his arms and legs along with twitching and severe anxiety, he thought he was having a stroke and went to the emergency department, where he was medically cleared and told that he was likely having a panic attack. Mr. A’s first panic attack had occurred 4 years before, when he was at his prior job, which was also very stressful. He was getting divorced after finding out that Panic-focused psychodynamic psychotherapy extended range 127 his then-wife was involved in an affair with a man whom she eventually married. Mr. A reported that an additional stress in the period between his past and recent panic episodes had been tensions with his ex-wife regarding custody and financial arrangements for their daughter. His ex-wife recurrently threatened to prevent Mr. A’s visits with his daughter, sometimes refusing to let the child go. On one of these occasions, about 2 years previously, his ex-wife called the police after a particularly severe argument. Mr. A was arrested and charged with assault, although he denied that this had occurred. He was eventually cleared of all charges but had to go through a lengthy trial that led to the loss of his prior job. Since that time, he had remained very tense and wary when seeing his ex-wife, although their conflicts about visits had not been as severe. In addition to his struggles at work and with his ex-wife, Mr. A reported that he was grappling with long-standing demands from his mother that he pay more attention to her. In this context the therapist explored the patient’s developmental history in greater depth. Mr. A reported that his early environment was repeatedly disrupted. His parents did not believe that the metropolitan area that he was growing up in was safe, so they sent him to live with his grandparents in a Caribbean country from ages 4 to 8. He returned to live with his parents but felt lost and confused in his third-grade class in school. He then was sent to live with an aunt and uncle in another metropolitan area for 2 years, where his academic work improved. His parents divorced when he was 14, and he was sent to military school from 8th to 11th grade. When he was back home, he felt pressure to take care of his mother, who remained embittered about her divorce, which was precipitated in part by his father having an affair. Mr. A felt that he had become his mother’s counselor and needed to be the man of the family. He believed that he had to hold in his own thoughts and feelings to protect her. Related problems occurred when his mother, a nurse, took care of an older man who was verbally abusive to her. Mr. A and his mother moved into a room in the man’s house for a period. Mr. A was exposed to the verbal abuse but was not allowed to respond. He reported that he had learned early on as part of his culture that he was supposed to respect authority and not complain. Mr. A was able to fairly readily link his panic attacks to issues related to his mother. His mother criticized his ex-wife for not having his mother more involved in their lives and was now very critical of Mr. A for trying to set limits on her involvement with his new wife. It emerged that Mr. A believed that his mother was self-centered and maintained a victim stance. She had had an accident 10 years previously in which her leg was injured, and she had successfully pursued a legal case. However, he believed that afterward, his mother made little effort to improve her situation, remaining homebound, complaining about her fate, and making demands on Mr. A to spend time with her. During the fifth session, the therapist offered a preliminary formulation to Mr. A regarding his panic attacks and generalized anxiety. The therapist suggested that Mr. A’s wish to please others and need for perfection had developed in the context of efforts to appease his parents after he felt abandoned as a child when sent to live with relatives. The need to be perfect, however, placed undue pressure on him, 128 Contemporary Psychodynamic Psychotherapy particularly in the context of the problems in his current life, including the demands of his job, mother, and ex-wife. Complicating his abandonment fears, Mr. A struggled with angry feelings toward the managers at work, his mother, and his ex-wife, but he typically denied being angry, believing that such feelings did not show respect for others. The therapist suggested that Mr. A was very frightened of his anger and that his panic attacks stemmed from fears of his anger and being abandoned. Mr. A reported that his father was demanding and that contact with him was limited. An English teacher, Mr. A’s father was very frustrated with his son’s difficulties in spelling and writing. Mr. A recalled a terrifying incident in which his father chased him around a table when he was 8 years old when he misspelled a word. His father grabbed him, opened the door, and was going to throw him out when his mother intervened. He had had a rapprochement with his father in his early 20s after his father attended a therapy course recommended by Mr. A. Mr. A described his first wife as “feisty” and as having said that she was frustrated that he would not make more efforts to defend himself. Marital stresses were created by struggles for control with his mother, who demanded his time and attention. His ex-wife was angry that he did not set better limits with his mother. Mr. A stated that he was attracted to women who had overcome adversity. His second wife, whom he had married 2 years previously, had lost her mother and was estranged from her father. He described her as very “up front” and said the relationship was going well. Mr. A worked to set limits with his mother, but he believed that his mother recurrently attempted to punish him for this by being withholding and critical, triggering intense guilt. On Mother’s Day, his mother had adopted an “oh don’t bother with me” attitude when Mr. A said that he did not have time to take her out to a restaurant, behavior that he experienced as guilt inducing, passive aggressive, and manipulative. He felt that he was disappointing her by not spending more time with her. Phase II In phase II the therapist further explored the dynamics surrounding Mr. A’s panic and difficulties with relationships. Mr. A described how at some point, he learned that the best way to be liked was to be “perfect,” including being the perfect son and perfect boss, always nice to others. He made efforts to please people, with the idea that then they would like him. In this context, the therapist and Mr. A recognized that his need to discipline people at work and set boundaries with his mother created intense anxiety. Mr. A talked about his ongoing struggles at work, and the therapist focused on what Mr. A was experiencing. He felt pressured by his bosses to do things he did not agree with, which he described as “dog eat dog.” The manager who had made Mr. A head of his division left the company, and the new leader did not have the same ethics. Mr. A blamed himself for the problems in his division, and the therapist pointed out that he had been placed in a very difficult position. Panic-focused psychodynamic psychotherapy extended range 129 The most difficult interactions with employees occurred when Mr. A had to critique, reprimand, or increase pressure on them. He felt that he was hurting others rather than supporting them, which made him feel guilty. The therapist noted that others were disappointing him and perhaps he was angry, but Mr. A said that he was very slow to get angry. During the exchanges with employees, his stomach was tight, as if he were waiting for someone to punch him. The therapist remarked on how Mr. A felt as though he was punching others and wondered perhaps whether his bodily experience represented a punishment. Mr. A described how he had decided not to tell his mother he was marrying his second wife, as he felt that she would be too critical and controlling. When he did tell her, she did not speak to him for several weeks. He described how difficult it was to disappoint her. The therapist suggested that he felt abandoned when he was sent away three times and believed that if he had been a better or perfect child, this would not have happened. The link between abandonment and not doing what was expected of him was explored in session 10 when Mr. A brought up another memory. At age 7, his mother served him a bowl of cereal and told him to eat it. When he did not, she left the house and locked the door behind her. He panicked, took a chair, and smashed through a window. He tried to climb out and began getting cuts from the glass. His mother, who was waiting outside, had to extricate him. Even now, Mr. A felt guilt and shame in recalling this incident. The therapist suggested that this acute sense of shame and terror was likely related to his panic. His panic attacks rapidly diminished as he increasingly understood that his symptoms represented the feelings of anger and guilt and fears of abandonment by others that he could not tolerate. A recurrence of panic that followed a visit to his mother was addressed in session 13. Mr. A’s mother had criticized him for not visiting her more often, which left him feeling undermined and guilty. In addition, the next day he had to fire an employee whom he thought of as being very much like his mother. The employee was complimentary toward him but bad-mouthed him behind his back. Mr. A was able to acknowledge some anger at his mother and the employee. The therapist noted that Mr. A’s anger likely contributed to his anxiety and guilt. The therapist continued to explore Mr. A’s unacknowledged anger in several contexts. These feelings had to be repressed in the attempt to be perfect and pleasing to others, to avoid being abandoned. Mr. A noted that one situation in which he had learned to suppress his anger was when his mother took care of the elderly man when Mr. A was in high school. He was angry at the man for his abusive behavior but, at his mother’s request, did not express the anger. He felt in part that it was a racial issue because black people (such as Mr. A and his mother), in his mother’s view, needed to submit to white men (such as the elderly man). However, Mr. A felt less troubled by racial issues at the time of his treatment. He also felt guilty because he believed that his mother had stayed at this job to afford sending him to college. Understanding his inhibitions and guilt helped him to acknowledge his frustration with his mother, employees, and his bosses. 130 Contemporary Psychodynamic Psychotherapy Phase III termination Because Mr. A had not raised the issue of upcoming termination, the therapist reminded him of the approaching end of treatment at session 16, as they entered the last phase. At first, Mr. A denied that this was of concern to him, as his panic remained diminished and he believed that he had a much better understanding of the factors contributing to it. However, over the next few sessions he recognized that he was having some anxiety about treatment ending and about whether he would be okay afterward. He asked for clarification of the policy on booster sessions. The therapist explored with him potential abandonment concerns, given his history of being repeatedly “sent away” as a child. He was able to recognize this link and that now, in contrast to when he was a child, he had a clear understanding of the basis for ending treatment and ways to reconnect should he need to. Like many patients, he was more reluctant to acknowledge anger toward the therapist but did acknowledge frustration that treatment had to end, as he found it very valuable. As Mr. A left therapy, his panic remained resolved, as did his generalized anxiety disorder, and he recognized an ongoing need to be alert to abandonment fears and angry feelings. His limit setting with his mother had improved significantly, with diminished guilt. Conclusion PFPP has demonstrated efficacy in the treatment of panic disorder with or without agoraphobia. The approach has been expanded to treat a broader range of anxiety disorders in a revised treatment manual (PFPP-XR). Further research is necessary to determine the impact of PFPP-XR on other anxiety disorders, cluster C personality disorders, and PTSD to help identify which patients respond better to this approach in comparison with medications and CBT. In addition, further studies will be necessary to determine what treatment or combination of treatments works best for which patients over the long term. Additional efforts to identify effective components and mediators of treatment are necessary, including further exploration of the role of reflective functioning, consistency of focus on panic and anxiety symptoms and dynamics, and/or the value of addressing specific dynamics. Dr. Milrod’s work was supported in part through a Fund in the New York Community Trust established by DeWitt Wallace and a grant through the Weill Cornell Clinical Translational Science Center Grant/Protocol Number: UL1 TR000457. References American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: American Psychiatric Press. American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Press. Panic-focused psychodynamic psychotherapy extended range 131 Barlow, D. H., Gorman, J. M., Shear, M. K., & Woods, S. W. (2000). Cognitive-behavioral therapy, imipramine, or their combination for panic disorder. JAMA, 283, 2529 2536. Brown, T. A., DiNardo, P., & Barlow, D. H. (1995). Anxiety disorders interview schedule for DSM-IV: Lifetime Version (ADISIV-L). New York: Graywinds. Busch, F., Cooper, A. M., Klerman, G. L., Shapiro, T., & Shear, M. K. (1991). Neurophysiological, cognitive-behavioral and psychoanalytic approaches to panic disorder: Toward an integration. Psychoanalytic Inquiry, 11, 316 332. Busch, F., Milrod, B. L., Singer, M., & Aronson, A. (2012). Panic-focused psychodynamic psychotherapy, EXtended Range. New York: Routledge. Busch, F., Shear, M. K., Cooper, A. M., Shapiro, T., & Leon, A. (1995). An empirical study of defense mechanisms in panic disorder. Journal of Nervous and Mental Disease, 183, 299 303. Cerny, J.A., Vermilyea, B.B., Barlow, D.H., et al. (1984) Anxiety treatment project relaxation treatment manual. Unpublished manuscript. Craske, M. G., Barlow, D. H., & Meadows, E. (2000). Master your own anxiety and panic: Therapist guide for anxiety, panic, and agoraphobia (MAP-3). San Antonio, TX: Graywind/Psychological Corporation. First, M. B., Spitzer, R. L., Gibbon, M., Williams, J. B. W., & Benjamin, L. (1994). Structured clinical interview for DSM-IV Axis II personality disorders (SCID-II), Version 2.0. New York: Biometrics Research Department, New York State Psychiatric Institute. Fonagy, P., & Target, M. (1997). Attachment and reflective function: Their role in selforganization. Development and Psychopathology, 62, 880 893. Hamilton, M. (1959). The assessment of anxiety states by rating. British Journal of Medical Psychology, 32, 50 55. Hamilton, M. (1960). A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry, 23, 56 62. Milrod, B., Busch, F., Cooper, A., & Shapiro, T. (1997). Manual of panic-focused psychodynamic psychotherapy. Washington, DC: American Psychiatric Press. Milrod, B., Busch, F., Leon, A. C., Aronson, A., Roiphe, J., Rudden, M., . . . Shear, M. K. (2001). A pilot open trial of brief psychodynamic psychotherapy for panic disorder. Journal of Psychotherapy Practice and Research, 10(4), 239 245. Milrod, B., Busch, F., Leon, A. C., Shapiro, T., Aronson, A., Roiphe, J., . . . Shear, M. K. (2000). An open trial of psychodynamic psychotherapy for panic disorder: A pilot study. American Journal of Psychiatry, 157, 1878 1880. Milrod, B., Chambless, D. L., Gallop, R., Busch, F. N., Schwalberg, M., McCarthy, K. S., . . . Barber, J. P. (2016). Psychotherapies for panic disorder: A tale of two sites. Journal of Clinical Psychiatry, 77, 927 935. Milrod, B., Leon, A. C., Busch, F. N., Rudden, M., Schwalberg, M., Clarkin, J., . . . Shear, M. K. (2007). A randomized controlled clinical trial of psychoanalytic psychotherapy for panic disorder. American Journal of Psychiatry, 164, 265 272. Rudden, M., Milrod, B., Target, M., Ackerman, S., & Graf, E. (2006). Reflective functioning in panic disorder patients: A pilot study. Journal of the American Psychoanalytic Association, 54, 1339 1343. Shear, M. K., Brown, T. A., Barlow, D. H., Money, R., Sholomskas, D. E., Woods, S. W., . . . Papp, L. A. (1997). Multicenter collaborative Panic Disorder Severity Scale. American Journal of Psychiatry, 154, 1571 1575. Shear, M. K., Cooper, A. M., Klerman, G. L., Busch, F. N., & Shapiro, T. (1993). A psychodynamic model of panic disorder. American Journal of Psychiatry, 150, 859 866. 132 Contemporary Psychodynamic Psychotherapy Sheehan, D. V. (1983). The Sheehan disability scales. The anxiety disease (p. 151) New York: Scribner. Subic-Wrana, C., Knebel, A., Beutel, M. E. (2010). The Mainz PFPP study: A RCT comparing a psychodynamic and a cognitive behavioral short-term psychotherapy for panic disorder. Panel presentation at Society for Psychotherapy Research, Asilomar, CA. Further reading Craske, M. G., & Barlow, D. H. (1988). Cognitive-behavioral treatment of panic. In A. J. Frances, & R. E. Hales (Eds.), Review of psychiatry. Washington, DC: American Psychiatric Press. Mentalization-based treatment for borderline and antisocial personality disorder 9 Anthony Bateman1 and Peter Fonagy2 1 University College London, London, United Kingdom, 2Research Department of Clinical, Educational and Health Psychology, University College London, London, United Kingdom Mentalizing is the ability to understand actions of other people and oneself according to underlying mental states, that is, through recognizing thoughts, feelings, wishes, and desires as being intentional. It is a very human capability that underpins everyday interactions (Allen, Bleiberg, & Haslam-Hopwood, 2003; Fonagy, Gergely, Jurist, & Target, 2002). Trying to understand other people’s behavior in terms of mental states contrasts with understanding others’ and one’s own actions through their consequences in the physical world: we are what we do. For instance, I see someone drop something, so he or she meant to do so. Similarly, I did something, so I must have wanted to do it. Mentalizing is not an entirely stable, consistent, or one-dimensional process. People are not all able to mentalize to the same extent. Many of us have strengths or weaknesses in particular aspects of mentalizing, and most people are more likely to struggle to mentalize in moments of stress or anxiety. We can all act according to mistaken beliefs about others’ mental states, leading to everyday misunderstandings, difficulties, and social faux pas. In addition, problems in mentalizing are the common factor in many psychiatric disorders (Bateman & Fonagy, 2012), particularly personality disorders. The multidimensional nature of mentalizing Mentalizing is not an all-or-nothing phenomenon. It ranges from full and effective mentalizing through ineffective mentalizing to nonmentalizing. In daily life, people’s ability to mentalize fluctuates, and people with personality disorders may show excellent mentalizing at times. The mentalizing model of borderline personality disorder (BPD) and antisocial personality disorder (ASPD) is not a deficit model. It is a model of vulnerability to imbalance and instability in mentalizing. It provides a comprehensive account of the phenomenology and origins of BPD and ASPD from a developmental perspective and informs clinicians how to target in treatment the mentalizing vulnerability that is hypothesized to be at the core of the disorders (Fonagy & Bateman, 2007, 2008). People with BPD show greater Contemporary Psychodynamic Psychotherapy. DOI: https://doi.org/10.1016/B978-0-12-813373-6.00009-X © 2019 Elsevier Inc. All rights reserved. 134 Contemporary Psychodynamic Psychotherapy propensity than others to lose mentalizing in interpersonal interactions and in a wider range of situations, they experience nonmentalizing for longer periods, and they find it more difficult to regain mentalizing once it has been lost. People with ASPD show similar mentalizing instability but also demonstrate a persistent imbalance of mentalizing in cognitive affective process, with cognitive mentalizing of both self and other dominating affective mentalizing. Neurobiology of mentalizing Neuroscience has identified four distinct components to mentalizing (Luyten & Fonagy, 2015), which are organized into dimensions that are helpful for therapists to identify in the clinical practice of mentalization-based treatment (MBT). These dimensions are automatic versus controlled mentalizing; mentalizing the self versus others; mentalizing with regard to internal versus external features; and cognitive versus affective mentalizing. These are not dimensions in the normal understanding of the term. They link on the basis of joint function. To mentalize effectively requires an individual not only to be able to maintain a balance across the dimensions of mentalizing, but also to apply the dimensions appropriately according to context. Consistent favoring of one or other side (or pole) of a dimension leads to distorted understanding of the mental states of oneself or others, which can be associated with profound social and emotional difficulties (Fonagy, Luyten, & Bateman, 2015). Commonly, one or more of the dimensions is relatively neglected at one end, and consequently, the opposite pole comes to dominate social cognition. For example, overly emotional thinking emerges in the absence of cognitive mentalizing. Clinically, the patient seems to be dominated by affective process and emotionally driven decision making, yet the problem can be due to the loss of cognitive processing systems. As another example, if the patient’s subjective experience of selfstates is reduced, the influence of others dominates and the patient becomes vulnerable to exploitation. From this perspective, different types of psychopathology can be distinguished on the basis of different combinations of impairments on the four dimensions. In other words, personality disorders (and, to some extent, other psychiatric disorders) can be understood according to their characteristic mentalizing profiles. Automatic versus controlled mentalizing The most fundamental dimension to mentalizing is the spectrum between automatic (or implicit) and controlled (or explicit) mentalizing. Controlled mentalizing reflects a serial and relatively slow process, which is typically verbal and demands reflection, attention, awareness, intention, and effort. The balancing pole of this dimension—automatic mentalizing—involves much faster processing, tends to be reflexive, and requires little or no attention, awareness, intention, or effort. Mentalization-based treatment for borderline and antisocial personality disorder 135 Mentalizing the self versus others This mentalizing dimension involves the capacity to mentalize one’s own state— the self (including one’s own physical experiences)—and/or the state of others. The two are closely connected, and an imbalance signals vulnerability in mentalizing others and/or the self. People with mentalizing difficulties are likely to preferentially focus on one end of the spectrum. Individuals with BPD tend to be highly sensitive to others and vulnerable to others’ states of mind; individuals with ASPD show sudden switches from being more other-directed to defending the self from disorganizing shame. Internal versus external mentalizing Mentalizing involves making inferences on the basis of the external indicators of a person’s mental states (e.g., facial expressions, tone of voice, body posture) or working out someone’s internal experience from what one knows about the other person and the situation and feeling state the other person is in. People with BPD and ASPD focus more on external than internal indicators. Cognitive versus affective mentalizing Cognitive mentalizing involves the ability to name, recognize, and reason about mental states (in oneself and others), whereas affective mentalizing involves the ability to experience and understand associated feelings, again, in oneself or others. Both need to be integrated for any genuine experience of empathy or true sense of self-coherence. Dimensional mentalizing profile characteristic of BPD and ASPD Individuals with BPD and ASPD easily find themselves switching to persistent automatic mentalizing. Stress and arousal, especially in an attachment context, bring automatic mentalizing to the fore and disengage the neural systems that are associated with controlled mentalizing. Under these conditions, interactions become nonquestioning precisely when they need to be more controlled and contextualized. Thinking becomes impulsive; the individual makes assumptions about others’ thoughts and feelings that are not reflected upon or tested. Logic is intuitive, unreasoned, and nonverbal. As a consequence, patients may be overly distrustful (paranoid) or, in BPD, sometimes overly trustful (naive). Patients with BPD may show excessive concern about their own internal state; that is, they hypermentalize in relation to the self without having an awareness of how others perceive them. In contrast, patients with ASPD tend to avoid selfscrutiny and hypermentalize about others. Failure to balance self-perception with 136 Contemporary Psychodynamic Psychotherapy sincere curiosity about how one is perceived by others (people with ASPD do not care how others perceive them) can lead to exaggeration of the self-image in either a positive (more common in ASPD) or a negative (more common in BPD) direction. A balanced, adaptive form of self-mentalizing conditioned by the social context is absent. Patients with BPD and ASPD pay more attention to external indicators of mental states, and their initial ideas, arising from automatic mentalizing, go unchecked by controlled, reflective mentalizing. For example, if the clinician looks out of the window, to the patient this means that the clinician is not taking the patient seriously. A focus on external features, in the absence of reflective mentalizing, renders an individual highly vulnerable in social contexts, as it generates interpersonal hypersensitivity and hypervigilance. The reemergence of nonmentalizing modes in BPD and ASPD While the dimensions of mentalizing can reflect anomalies in terms of mechanisms, the clinician experiences the outcomes of these malfunctions as nonmentalizing modes. These are grouped into three typical modes of subjectivity: psychic equivalence mode, teleological mode, and pretend mode (Fonagy & Bateman, 2008). The nonmentalizing modes are important for the clinician to recognize and understand, as they tend to emerge in the consulting room and reflect core aspects of the patient’s experience. It is important to address them because they cause considerable interpersonal difficulties and result in destructive behaviors. In general terms, nonmentalizing modes fluctuate in BPD and are more persistent in ASPD. Newbury-Helps, Feigenbaum, and Fonagy (2017) found a range of mentalizing problems in people with ASPD, which were more pronounced in offenders than in nonoffenders. Psychic equivalence mode In the psychic equivalence mode, thoughts and feelings become “too real” to a point at which it is extremely difficult for the patient to entertain possible alternative perspectives. What thought is experienced as being real and true, leading to concreteness of thought; that is, thoughts are treated as facts. Patients with BPD and ASPD who are in this mode describe an overriding sense of certainty about their beliefs; for example, “the therapist does not like me” or “I am a wicked person.” These thoughts and beliefs cannot be argued with. Teleological mode In the teleological mode, states of mind are recognized and believed only if their outcomes are physically observable. Hence, the individual can recognize the Mentalization-based treatment for borderline and antisocial personality disorder 137 existence and potential importance of states of mind, but this recognition is limited to physical indicators. For example, affection is perceived to be real only if it is accompanied by a touch or caress. A patient with BPD, describing a recent incident in which her partner failed to respond to a text message, may say that her partner’s nonresponse to the message “means that he does not love me.” In ASPD, teleological function is often engrained in how others’ motives are understood (you are what you do); for instance, someone who does not step aside in the street has malevolent intent with determination to dominate and challenge. The teleological mode is apparent in patients who are imbalanced toward the external pole of the internal external mentalizing dimension. They are heavily biased toward understanding how people (and they themselves) behave and what their intentions may be in terms of what they actually do. Pretend mode In the pretend mode, thoughts and feelings become severed from reality. Taken to an extreme, this may lead to feelings of derealization and dissociation. Patients in pretend mode can discuss experiences without contextualizing them in any kind of physical or material reality, as if they were creating a pretend world. The patient may hypermentalize or pseudomentalize, a state in which the patient is overly focused on internal self-states and may say much about states of mind but with little true meaning or connection to reality. In ASPD the focus on self-states may, paradoxically, be about others’ motives, with self-serving justification of violent or threatening behavior, for example. Attempting psychotherapy with patients who are in this mode can lead to lengthy but inconsequential discussions of internal experience that have no link to genuine experience and will achieve no change. In summary, imbalances within the dimensions of mentalizing predictably generate the nonmentalizing modes. Psychic equivalence is inevitable if emotion (affect) dominates cognition. Teleological mode follows from an exclusive focus on external features to the neglect of the internal. Pretend mode thinking and hypermentalizing are unavoidable if reflective, explicit, controlled mentalizing is not well established. Attachment It is a central tenet of the mentalization-based approach that a sense of self and the capacity to mentalize both develop in the context of attachment relationships (Fonagy & Luyten, 2018). In patients with BPD and ASPD there is a common history of early (in particular emotional) neglect, a disrupted early social environment, and abusive or even brutalized family relationships. These may contribute to undermining the ability of some individuals to develop full mentalizing capacities. Subsequent adversity or trauma may disrupt mentalizing further, in part as an adaptive maneuver on the part of the individual to limit exposure to a dehumanizing 138 Contemporary Psychodynamic Psychotherapy psychosocial environment and in part because the high level of arousal generated by attachment hyperactivation and disorganized attachment strategies serve to disrupt less well-practiced and less robustly established higher cognitive capacities. In addition, genetic influences may be expressed through the mediation of mentalizing. In summary, the mentalizing model points to a final common developmental pathway that a range of biological, family, and broader social contextual influences may take to generate the range of difficulties that are normally considered under the term personality disorder (Fonagy et al., 2015). Epistemic trust The most recent theoretical developments in our thinking about mentalizing and therapeutic change have important implications for how we approach our clinical practice. This new thinking involves the theory of epistemic trust. In short, this theory emphasizes the social and emotional significance of the trust we place in the information about the social world that we receive from another person—that is, the extent and ways in which we are able to consider social knowledge as genuine and personally relevant to us. The development of epistemic trust goes hand in hand with attachment processes, with the bond of secure attachment opening up trust in others to facilitate learning from them, whereas the interaction in insecure and disorganized attachment reduces this capacity. Our view is that in BPD and ASPD this process has been compromised. For further discussion of this view, see Fonagy, Luyten, and Allison (2015). The evidence base for MBT from outcome research Research has been integrated with MBT from its inception. Randomized controlled trials (RCTs) have tested the effectiveness of MBT in BPD, ASPD, eating disorders, and self-harming adolescents with borderline features. In an early RCT of MBT for BPD in a partial hospital setting in the United Kingdom (Bateman & Fonagy, 1999, 2001), an 18-month program was associated with significant and enduring improvements in self-destructive behavior, mood states, and interpersonal functioning, and reduction in service use. Treatment for BPD showed considerable cost savings after treatment (Bateman & Fonagy, 2003), and an 8-year follow-up found that patients who had received MBT remained better than the control group, who had received treatment as usual (TAU) (Bateman & Fonagy, 2008). Two well-controlled single-blind randomized trials of outpatient MBT have been conducted in the United Kingdom, with adults with BPD (Bateman & Fonagy, 2009) and adolescents presenting to clinical services with self-harm, the vast majority of whom met BPD criteria (Rossouw & Fonagy, 2012). In the latter trial the participants received a form of MBT designed for adolescents (MBT-A). In both trials Mentalization-based treatment for borderline and antisocial personality disorder 139 MBT proved superior to TAU in reducing self-harm (including suicidality) and depression. Improvement was mediated by improved levels of mentalizing, reduced attachment avoidance, and reduction in features of BPD. Three more recent studies provided further support for MBT in patients with BPD. An RCT in Denmark investigated the efficacy of MBT versus a less intensive, manualized supportive group therapy, both delivered in combination with psychoeducation and medication, for patients diagnosed with BPD (Jørgensen et al., 2013). In another study in Denmark (Petersen et al., 2010) a cohort of patients treated with partial hospitalization followed by MBT group therapy showed significant improvements after 2 years on a range of measures, with further improvement at 2-year follow-up. A naturalistic study by Bales et al. (2012) in the Netherlands showed moderate to large effect sizes at the end of treatment and, when the authors used a matched control design, found that MBT had larger effect sizes than other specialized psychotherapeutic treatments (Bales et al., 2015). Another naturalistic trial in the Netherlands studied the feasibility and effectiveness of inpatient MBT-A in 11 female adolescents aged 14 18 years with borderline symptoms (Laurenssen et al., 2014). Results showed significant decreases in symptoms and improvements in personality functioning and quality of life 12 months after the start of treatment. Better outcomes for people with ASPD receiving MBT compared with TAU have led to a definitive multicenter trial in the United Kingdom (Bateman, O’Connell, Lorenzini, Gardner, & Fonagy, 2016). Finally, an RCT comparing MBT with specialist supportive clinical management in the treatment of adults with eating disorders and impulsive BPD traits has been reported in the United Kingdom (Robinson et al., 2016). Both interventions achieved reductions in eating disorder symptoms, but MBT was associated with greater reductions in shape concern and weight concern. The clinical approach in mentalization-based treatment MBT is operationalized as combined individual and group therapy, although it is now often delivered in one mode alone. The evidence-based program for BPD was organized as weekly individual and group therapy for a period of 18 months. MBT for ASPD consists of weekly group therapy, with an individual session at the request of the clinician or patient a maximum of once a month, for a period of 1 year. MBT requires the clinician to develop a treatment frame and milieu that facilitate epistemic trust. To do so, the clinician focuses on contingent and marked mentalizing of the patient’s internal states, because feeling mentalized is the most potent ostensive cue. The patient’s interpersonal processes and current life events form the content of this process. Initially, MBT takes a directive and informative approach (Bateman & Fonagy, 2016). MBT requires the clinician and patient to do the following: 1. Collaboratively develop a formulation early in the assessment process (see later, in the section “Collaborative process and formulation”). 140 Contemporary Psychodynamic Psychotherapy 2. Identify mentalizing vulnerabilities in terms of dimensional rigidity and nonmentalizing modes, using examples that are personal to the patient. Pathways to the loss of mentalizing are identified and established as vulnerability points to be monitored carefully. 3. Discuss the diagnosis in terms of the patient’s symptoms and history. The diagnosis is less important than agreeing on a lens through which the variability of symptoms can be understood. 4. Map attachment patterns and how they play out in current relationships. The identification of attachment strategies is essential if the patient and clinician are to recognize their deployment during treatment and in the patient’s interpersonal interactions. 5. Engage the patient in an introductory phase that combines psychoeducation with some interpersonal process. The MBT-Introductory group (Bateman & Fonagy, 2016) offers the patient and clinician a shared framework for understanding BPD and the whole process of therapy. 6. Establish a developmental narrative of problems. The patient’s background and context support a compassionate view of the problems. 7. Jointly agree on goals that are relevant to the patient so that therapy is about what is important to the patient. To this end, MBT for ASPD asks the patient and clinician to work together, identifying the patient’s current and hoped-for values, to ensure that the patient does not experience therapy as imposition of the therapist’s, or an establishment, value system. In essence, we suggest that the explanations and suggestions and the process of developing a value-driven clinical agreement in the initial phase of therapy are ostensive cues that signal to the patient the relevance to them of the information that is being conveyed. These serve to trigger in the patient a feeling of being personally recognized by the clinician in the therapeutic situation. MBT is structured, organized around the development of an attachment relationship with the patient, offers a careful focus on the patient’s internal mental processes as they are experienced moment by moment, and emphasizes the therapeutic alliance, with the active repair of ruptures in the relationship between patient and clinician. Principles The clinician follows a number of principles that are framed to increase mentalizing and to prevent iatrogenic reduction of mentalizing. These are listed in Box 9.1 and discussed in detail in Bateman and Fonagy (2016). Collaborative process and formulation The formulation is predominantly a collaborative clinical agreement. It is written by the clinician and shared with the patient, and is regularly revised as new understandings develop. It is important that the patient recognizes himself or herself within the formulation. It is written from a positive perspective with the patient’s strengths emphasized. It includes information from some of the domains identified below, expressed in terms of developmental vulnerabilities (e.g., “It is Mentalization-based treatment for borderline and antisocial personality disorder 141 Box 9.1 MBT principles 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. Primary aim is to increase the patient’s capacity to mentalize self and others. Manage the patient’s arousal levels. Focus on the patient’s mind and not on his or her behaviors. Monitor the patient’s capacity to mentalize, and use interventions that are consistent with the patient’s level of mentalizing. Identify imbalances in the poles of mentalizing, and intervene to regain balance. Seek out moments of mentalizing vulnerability leading to behaviors (e.g., selfharm, violence). Address current events and immediate states of mind. Consider marking and contingency in all interventions. Use a stepwise intervention process, starting with empathic validation, moving on to exploration, clarification, and challenge, through affect identification and affect focus, to mentalizing the clinician patient relationship itself. The clinician must maintain or regain his or her own mentalizing at all times. Do not: a. Meet nonmentalizing in the patient with high-level mentalizing in the clinician. b. Elaborate on the patient’s nonmentalizing. understandable with all these experiences that you have become sensitive and have problems with relationships, managing your emotions, and controlling your actions”). G G G G G Risk factors, such as suicidal or violent behavior or threats to engagement with and continuity of therapy Attachment patterns, which are often insecure anxious-avoidant/anxious-preoccupied in BPD and with marked disorganization in ASPD when strategies are activated Self-identity, that is, how the patient sees himself or herself and others. In BPD the patient may show identity confusion; in ASPD the self-states may be held in pretend mode with no connection to reality; for example, a narcissistic and grandiose self is given priority, and any threat to this is treated with dismissal Mentalizing strengths and nonmentalizing vulnerabilities, such as the mentalizing and nonmentalizing loops (see later) Immediate short-term goals in therapy, placed in relation to goals in the outside world. Identification of nonmentalizing process The MBT clinician becomes sensitive to the vicissitudes of nonmentalizing process. The three primary nonmentalizing modes discussed earlier are not mutually exclusive; in fact, they are more likely to interweave than to manifest themselves in pure form. MBT techniques target the nonmentalizing modes to help the patient manage them better while, at the same time, exploring what triggered them when they arise. Addressing nonmentalizing modes is partly embedded in the general clinical stance and partly requires specific intervention. 142 Contemporary Psychodynamic Psychotherapy Interventions for nonmentalizing modes In psychic equivalence the patient’s mind is fixed, with no capacity to recognize alternative perspectives. This means that complex statements involving interpretation or even cognitive appraisal of the validity of the patient’s belief will be outside the patient’s comprehension. Such interventions need a higher level of mentalizing if they are to be understood by the patient. Fundamentally, the patient has to be able to think about his or her current state and appraise it if such interventions are to be useful. The MBT clinician may initially probe psychic equivalence belief and question the certainty of the patient’s understanding, but arguing with psychic equivalence is contraindicated. Instead, the clinician tries to stimulate mentalizing in a linked area of mental function. If, for instance, the topic is about the patient’s partner and the rigidity of the patient’s belief is about not being loved, it is better to make a detour, for example, to ask the patient to review how his or her relationship with the partner was a few weeks ago. If this allows some reflection, the current relationship can be explored from that standpoint. The clinician engages in a similar process when the patient’s mental processes are infused with teleological process. Working with the pretend mode is somewhat different. The clinician is more likely to unwittingly join in with pretend mode—by entering into exploration of thoughts and feelings that have no grounding in reality—but must avoid doing this. More specifically, the clinician should begin to challenge pretend mode, gently at first and then more insistently. Not-knowing stance The not-knowing stance requires the MBT clinician to work authentically from the perspective of equality and collaboration, as the clinician can never know what is really going on in his or her own or others’ mind states. The clinician has knowledge and is expert in many ways but has to respect the opacity of mental states. Both patient and clinician have to accept that experience of mental states is impressionistic. The clinician has to accept the validity of the patient’s experience even if the clinician does not understand it. The clinician does not have to understand the patient or to make sense of the seemingly incomprehensible. This means that the clinician should never be worried if he or she does not understand what the patient is talking about. If the clinician does not know what the patient is talking about, the clinician does not try to piece it together, but says, “You know, I am having a real problem here. I can’t follow this, I can’t put it together. Can we try again?” Not-knowing is a key therapeutic attitude to enhance curiosity about mental process and experience. Curiosity is modeled by the clinician through reflecting on his or her own mind states without judgment and with empathic acceptance of experience. Mentalizing poles The MBT clinician becomes attuned to indicators of nonmentalizing in the dialog, such as the overuse of absolutes or simplistic, overdetermined explanations and the Mentalization-based treatment for borderline and antisocial personality disorder 143 mental rigidity that arises when mentalizing becomes stuck at one of the poles of mentalizing. If, for example, the patient is highly other externally focused and is watching the clinician’s movements carefully, the clinician directs the dialogue toward an internal state (of either self or other) to find out whether this instills more reflection. A clinician turned around and spoke to his patient with ASPD as they walked down the corridor to the consulting room. As they sat down, the patient stated coercively that the clinician was not to turn around to look at the patient or to speak to him as they walked down the corridor. The clinician asked what his backward glance had done to the patient—an intervention to focus the patient on the “self internal”, to balance his “other external” focus. The patient kept the focus on the clinician (other), so the clinician accepted the patient’s “other external” focus by saying that he had turned around simply as a social gesture and was not aware of any wish to cause offense. Having done this, the clinician again tried to rebalance some of the focus of mentalizing by asking the patient to describe what he had experienced from the backward glance. The same principle of intervention applies if a patient is excessively cognitive. The MBT clinician balances this by harnessing the use of affective experience while accepting that it may be important to be fixed at the cognitive pole at certain times, for example, when solving a practical problem. This move to the affective pole can be difficult without becoming formulaic, for example, by continually asking someone how he or she feels. This is irritating for patients, who may not know how they feel, and it is often a barren intervention in terms of stimulating further mentalizing. For the MBT clinician the important factor is the quality of mentalizing—that is, whether it has become fixed and rigid—rather than whether the mental processing is either cognitive or affective. MBT recommends that the clinician increases interpersonal affectivity when the patient is fixed in a cognitive rational process with limited flexibility and, conversely, increases cognitive processing when the patient is trapped in affective dysregulation. To move from the cognitive pole, the clinician increasingly uses relational interventions in the dialogue; to move the other way, the clinician reduces the relational component and increasingly becomes more practical or rational. The aim of these interventions is to make a mentalizing process more flexible, more responsive to context, and increasingly implicit. Mentalizing and nonmentalizing loops The clinician identifies common nonmentalizing “loops” with the patient. These are common interpersonal interactions that lead to diminished mentalizing by the patient, often in a particular form—psychic equivalence, for example—which results in painful internal states in the self (e.g., shame), which in turn leads to control of the other person, coercive behavior, or violence. It is in these loops, underpinned by the dimensions of mentalizing, that mentalizing differences between 144 Contemporary Psychodynamic Psychotherapy BPD and ASPD are apparent to the clinician. People with BPD commonly show excessive affective mentalizing with low levels of cognitive mentalizing, so they become sensitive to others while having a lowered sense of self. Clinical intervention is focused on helping the patient manage emotional dysregulation through developing more robust mentalizing and increasing cognitive control of emotions, along with better self other differentiation. In ASPD, higher cognitive mentalizing of self and other is likely to be apparent, sometimes combined with exploitation or control of others. This is often linked to a lack of affective empathy for others. Clinically, the task is therefore to increase the patient’s affective mentalizing of self and the affective component of empathy for others. MBT suggests a focus on identifying this nonmentalizing loop and increasing a more mentalizing loop—of understanding one’s own emotions, recognizing the other person’s feelings, and then empathizing with the other’s experience to the extent that interpersonal behavior becomes more constructive. The aim is that the patient becomes constrained by his or her effect on others so that, for example, the patient cares if he or she makes someone upset or frightened. This is done in group therapy, in which patients are initially asked to identify their own and each other’s emotions and underlying mental states. Trajectory of sessions Finally, MBT not only has an overall structure to the treatment program (described in detail by Bateman & Fonagy, 2016), but also suggests a trajectory for each session. In each session there is a recommended stepwise move from a supportive position toward a more relational subjective experiential process. The MBT clinician is required, as a general principle, to start from an empathic and supportive position before moving toward a more relational focus. The clinician first needs to find out the subjective truth of the patient’s experience and to demonstrate that he or she has understood it from the patient’s perspective. Only then can the clinician “sit alongside the patient” so that the clinician and patient start looking at the patient’s story and subjective experience from a shared vantage point. As soon as the clinician senses that he or she and the patient have a shared affective platform, a process of exploration and elaboration takes place with the clarification of mental states. Clarification requires a reconstruction of events but with an emphasis on the changing mental states that were experienced during the events, a tracing of process over time, and a recognition that decisions may in the end be capricious and yet of value. The judicious use of challenge is also recommended in MBT. Challenge is a very important intervention, particularly, as mentioned earlier, when the patient is in pretend mode. There are a number of indicators for challenge. First, it should be considered specifically when a patient is interminably in a nonmentalizing mode. This may be particularly the case if the patient is in prolonged pretend mode, when the patient is in danger of believing his or her own narrative without question or Mentalization-based treatment for borderline and antisocial personality disorder 145 reflection. Challenge as an intervention in MBT has certain defined characteristics. It is nearly always outside the current therapy dialogue, so it “comes from left field.” The aim is for the patient to be surprised and suddenly derailed from pretend mode. Once the clinician and patient are able to maintain a mentalizing interaction, MBT suggests an increasing focus on affect and the interpersonal domain. This has the effect of increasing emotional intensity; if mentalizing is maintained under these conditions, the MBT clinician can then move to mentalizing the relationship. The purpose of this move is to recreate the core sensitivity of the patient with BPD in the session. People with BPD are highly sensitive to interpersonal process; arousal in the interpersonal domain triggers much of the emotional dysregulation that is characteristic of BPD, which in turn disrupts mental processing further. MBT for BPD focuses on this area of sensitivity to generate more robust mentalizing around interpersonal processing, that is, relational mentalizing. The aim of mentalizing the relationship is to increase the affective interpersonal experience with the patient while maintaining mentalizing, as this is the core of the interpersonal difficulty for people with BPD. If the patient says something striking in the context of the patient clinician relationship that is of significance in the patient’s external relationships, the first task for the clinician is to validate the patient’s experience. Where is the accuracy in how the patient sees the clinician; in what way was the clinician like that? A patient with BPD told her clinician that he was too modest. To validate this experience, the clinician asked the patient what he does that is “too” modest. The patient explained that the clinician does not stand up for himself at times and seems to accept her criticisms too readily, particularly when she knows she is being difficult and irritable. The clinician and patient together identified a recent example of this, and the clinician accepted his role in the patient’s experience. Importantly, he did not question it as a distortion; it was a valid experience, contributed to by the clinician’s attitude. Next, the clinician had to identify what it was like for the patient to be working with a clinician who is too modest—what did it matter that she has a clinician who she saw as too modest? It shouldn’t really matter, but it did seem to matter to her. It turned out that the patient had seen a video on the internet of the clinician speaking at a conference and experienced him as so modest that she felt that he could not stand up for himself in the face of professional criticism. This experience had led her to self-harm, indicating how serious the issue was for her. The MBT clinician now has to explore this sensitive area to try to get to an alternative perspective or, at least, a more complex understanding of what has happened. What actually had happened in this scenario was that the patient felt that if the clinician could not be proud of his achievements, it reduced her own achievements in life to futile meaningless events, because she saw them as being minimal compared with those of the clinician. She experienced this in psychic equivalence, so her experience of her achievements as utterly useless meant that she was useless and 146 Contemporary Psychodynamic Psychotherapy meaningless, and her life was nothing. This is an alternative perspective in MBT. Mentalizing the relationship is not an interpretation in the sense of insight; it is an attempt within the relationship to generate meaningful complexity about what has happened by engaging in a slowly unfolding relational process. At all times, the clinician monitors the reaction of the patient to the alternative perspective. Mentalizing the relationship in MBT must be approached with caution. Side effects stimulated by the clinician are common. For example, the patient’s experience is seen by the clinician as a distortion and the patient is alienated; the process becomes a jointly elaborated pretend mode in which both patient and clinician believe that they are working at depth when they are, in fact, engaged in clever cognitive work but both lose contact with reality. MBT is explicit about managing and working with components of mentalizing the counterrelationship (or the countertransference). Mentalizing the counterrelationship—essentially, using the feelings evoked in the clinician by exchanges with the patient—requires self-awareness on the part of the clinician. Some clinicians default to a state of self-reference whereby they consider most of what they experience in therapy as being relevant to the patient. This default mode needs to be resisted, and clinicians need to be mindful of the fact that their own mental states might unduly color their understanding of the patient’s mental states and that they might tend to equate these mental states without adequate foundation. The clinician therefore has to “quarantine” his or her feelings. How the clinician “quarantines” informs the MBT technical approach to countertransference, which is defined as those experiences, both affective and cognitive, that the clinician has in sessions and thinks might further develop an understanding of mental processes. Feelings in the clinician are not considered initially as a result of projective processes, and the clinician must identify these experiences clearly as his or her own; that is, they are “marked.” The purpose of expressing the counterrelationship is to explore the dyadic interaction in more detail, to explore how mind states affect mind states. As an example, a patient who is intimidating in attitude will evoke a sense of wariness or fear in the clinician, and exploring this interaction in its immediacy will be important if the patient is to modify his or her relationships. Summary MBT is rooted in a theoretical framework derived from neuroscience and attachment research. The focus of the intervention is on increasing the stability of mentalizing processes in patients with BPD and ASPD whose difficulties arise from vulnerability to losing mentalizing, particularly in relationships. Treatment is structured according to a research-based protocol and organized around identification of the triggers of episodes of nonmentalizing. A relational process is used to promote the ability of patients to maintain their affect and mentalizing within intimate relationships and during stressful interactions. Mentalization-based treatment for borderline and antisocial personality disorder 147 References Allen, J. G., Bleiberg, E., & Haslam-Hopwood, T. (2003). Understanding mentalizing: Mentalizing as a compass for treatment. Houston, TX: The Menninger Clinic. Available from http://www.menningerclinic.com/education/clinical-resources/mentalizing. Bales, D., van Beek, N., Smits, M., Willemsen, S., Busschbach, J. J., Verheul, R., & Andrea, H. (2012). Treatment outcome of 18-month, day hospital mentalization-based treatment (MBT) in patients with severe borderline personality disorder in the Netherlands. Journal of Personality Disorders, 26, 568 582. Available from https://doi.org/10.1521/ pedi.2012.26.4.568. Bales, D. L., Timman, R., Andrea, H., Busschbach, J. J., Verheul, R., & Kamphuis, J. H. (2015). Effectiveness of day hospital mentalization-based treatment for patients with severe borderline personality disorder: A matched control study. Clinical Psychology & Psychotherapy, 22, 409 417. Available from https://doi.org/10.1002/cpp.1914. Bateman, A., & Fonagy, P. (1999). Effectiveness of partial hospitalization in the treatment of borderline personality disorder: A randomized controlled trial. American Journal of Psychiatry, 156, 1563 1569. Available from https://doi.org/10.1176/ajp.156.10.1563. Bateman, A., & Fonagy, P. (2001). Treatment of borderline personality disorder with psychoanalytically oriented partial hospitalization: An 18-month follow-up. American Journal of Psychiatry, 158, 36 42. Available from https://doi.org/10.1176/appi.ajp.158.1.36. Bateman, A., & Fonagy, P. (2003). Health service utilization costs for borderline personality disorder patients treated with psychoanalytically oriented partial hospitalization versus general psychiatric care. American Journal of Psychiatry, 160, 169 171. Available from https://doi.org/10.1176/appi.ajp.160.1.169. Bateman, A., & Fonagy, P. (2008). 8-year follow-up of patients treated for borderline personality disorder: Mentalization-based treatment versus treatment as usual. American Journal of Psychiatry, 165, 631 638. Available from https://doi.org/10.1176/appi. ajp.2007.07040636. Bateman, A., & Fonagy, P. (2009). Randomized controlled trial of outpatient mentalizationbased treatment versus structured clinical management for borderline personality disorder. American Journal of Psychiatry, 166, 1355 1364. Available from https://doi.org/ 10.1176/appi.ajp.2009.09040539. Bateman, A., O’Connell, J., Lorenzini, N., Gardner, T., & Fonagy, P. (2016). A randomised controlled trial of mentalization-based treatment versus structured clinical management for patients with comorbid borderline personality disorder and antisocial personality disorder. BMC Psychiatry, 16, 304. Available from https://doi.org/10.1186/s12888-0161000-9. Bateman, A. W., & Fonagy, P. (2016). Mentalization-based treatment for personality disorders: A practical guide. Oxford, UK: Oxford University Press. Bateman, A. W., & Fonagy, P. (Eds.), (2012). Handbook of mentalizing in mental health practice. Washington, DC: American Psychiatric Publishing. Fonagy, P., & Bateman, A. (2008). The development of borderline personality disorder—A mentalizing model. Journal of Personality Disorders, 22, 4 21. Available from https:// doi.org/10.1521/pedi.2008.22.1.4. Fonagy, P., & Bateman, A. W. (2007). Mentalizing and borderline personality disorder. Journal of Mental Health, 16, 83 101. Available from https://doi.org/10.1080/ 09638230601182045. 148 Contemporary Psychodynamic Psychotherapy Fonagy, P., Gergely, G., Jurist, E., & Target, M. (2002). Affect regulation, mentalization, and the development of the self. New York, NY: Other Press. Fonagy, P., & Luyten, P. (2018). Attachment, mentalization, and the self. In W.J. Livesley & R. Larstone (Eds.), Handbook of personality disorders: Theory, research, and treatment (2nd ed., pp. 123 140). New York, NY: Guilford Press. Fonagy, P., Luyten, P., & Allison, E. (2015). Epistemic petrification and the restoration of epistemic trust: A new conceptualization of borderline personality disorder and its psychosocial treatment. Journal of Personality Disorders, 29, 575 609. Available from https://doi.org/10.1521/pedi.2015.29.5.575. Fonagy, P., Luyten, P., & Bateman, A. (2015). Translation: Mentalizing as treatment target in borderline personality disorder. Personality Disorders: Theory, Research, and Treatment, 6, 380 392. Available from https://doi.org/10.1037/per0000113. Jørgensen, C. R., Freund, C., Boye, R., Jordet, H., Andersen, D., & Kjolbye, M. (2013). Outcome of mentalization-based and supportive psychotherapy in patients with borderline personality disorder: A randomized trial. Acta Psychiatrica Scandinavica, 127, 305 317. Available from https://doi.org/10.1111/j.1600-0447.2012.01923.x. Laurenssen, E. M., Hutsebaut, J., Feenstra, D. J., Bales, D. L., Noom, M. J., Busschbach, J. J. V., . . . Luyten, P. (2014). Feasibility of mentalization-based treatment for adolescents with borderline symptoms: A pilot study. Psychotherapy, 51, 159 166. Available from https://doi.org/10.1037/a0033513. Luyten, P., & Fonagy, P. (2015). The neurobiology of mentalizing. Personality Disorders: Theory, Research, and Treatment, 6, 366 379. Available from https://doi.org/10.1037/ per0000117. Newbury-Helps, J., Feigenbaum, J., & Fonagy, P. (2017). Offenders with antisocial personality disorder display more impairments in mentalizing. Journal of Personality Disorders, 31, 232 255. Available from https://doi.org/10.1521/pedi_2016_30_246. Petersen, B., Toft, J., Christensen, N. B., Foldager, L., Munk-Jorgensen, P., Windfeld, M., . . . Valbak, K. (2010). A 2-year follow-up of mentalization-oriented group therapy following day hospital treatment for patients with personality disorders. Personality and Mental Health, 4, 294 301. Available from https://doi.org/10.1002/Pmh.140. Robinson, P., Hellier, J., Barrett, B., Barzdaitiene, D., Bateman, A., Bogaardt, A., . . . Fonagy, P. (2016). The NOURISHED randomised controlled trial comparing mentalisation-based treatment for eating disorders (MBT-ED) with specialist supportive clinical management (SSCM-ED) for patients with eating disorders and symptoms of borderline personality disorder. Trials, 17, 549. Available from https://doi.org/10.1186/ s13063-016-1606-8. Rossouw, T. I., & Fonagy, P. (2012). Mentalization-based treatment for self-harm in adolescents: A randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry, 51, 1304 1313. Available from https://doi.org/10.1016/j. jaac.2012.09.018. Transference-focused psychotherapy for borderline and narcissistic personality disorders 10 Eve Caligor1, John F. Clarkin2,3 and Frank E. Yeomans3 1 Columbia University College of Physicians and Surgeons, New York, NY, United States, 2 New York Presbyterian Hospital Cornell Medical Center, White Plains, NY, United States, 3Weill Cornell Medical College, New York, NY, United States Introduction Transference-focused psychotherapy (TFP) (Yeomans, Clarkin, & Kernberg, 2015) is a long-term, theory-driven, psychodynamic treatment for severe personality disorders. The goals of TFP are improved self and interpersonal functioning in conjunction with symptom relief and resolution of maladaptive behaviors. TFP is empirically supported for treatment of borderline personality disorder (BPD), and the treatment principles, tactics, and techniques of TFP have been extended and successfully applied to patients with narcissistic personality disorder (NPD) (Diamond, Yeomans, Stern, & Kernberg, in press) as well as to those with higherlevel or subsyndromal personality pathology (Caligor, Kernberg, & Clarkin, 2007). Because TFP is focused on pathology in self and other functioning, pathology that is central to the entire spectrum of personality disorders (Sharp et al., 2015), this treatment model has recently been further articulated as a comprehensive psychodynamic approach for patients with personality pathology across the range of severity, with modifications introduced to tailor treatment to each individual patient and phase of illness (Caligor Kernberg, Clarkin, & Yeomans, 2018). In this chapter, we focus on the treatment of patients with BPD and NPD, which often cooccur in clinical samples (Diamond et al., 2014). The TFP treatment model begins with careful diagnostic assessment and case formulation. Before treatment begins, the treatment frame is established in the form of a verbal treatment contract. The therapy makes use of the structure provided by the treatment contract, in conjunction with careful attention to the patient’s day-today functioning, to support psychodynamic exploration in patients with severe personality disorders. The clinical focus is on the present. The therapist attends closely to the patient’s moment-to-moment experience and behavior in therapy sessions, with special attention to disturbed interpersonal behaviors, both in relation to the therapist and in the patient’s current relationships. Contemporary Psychodynamic Psychotherapy. DOI: https://doi.org/10.1016/B978-0-12-813373-6.00010-6 © 2019 Elsevier Inc. All rights reserved. 150 Contemporary Psychodynamic Psychotherapy Description of treatment model and clinical approach Frame of reference and model of pathology TFP is based in psychodynamic object relations theory as developed by Kernberg (Kernberg and Caligor, 2005). The model focuses on the role of affectively charged mental representations of self and other, referred to as internal object relations, in organizing subjective experience and interpersonal relationships. An internal object relation is composed of an image of the self in interaction with an image of another person, with the relationship linked to an affect state. These self-other representation dyads appear, either explicitly or implicitly, in therapy exchanges as they organize patients’ descriptions of relationship patterns with others and patients’ moment-to-moment experiences in relation to the therapist. In the TFP model, the nature of self and interpersonal functioning is anchored in the construct of identity. Normal identity formation corresponds with a core sense of self that is stable, coherent, realistic, and continuous across time; a corresponding stable and rich experience of significant others; and affective experience that is complex and well modulated. A coherent and integrated conception of self and others contributes to relationships that involve empathy and mutual dependence, as well as the ability to mentalize, that is, to understand self and others in terms of intentions, motivations, and emotions. In contrast, severe personality disorders are characterized by pathology of identity formation in which affectively charged, extreme, caricature like, and largely negative experiences of self and other are mutually dissociated and fail to coalesce to organize a core complex sense of self. In this setting, the experience of self is unstable, discontinuous, distorted, and poorly contextualized, with a corresponding experience of significant others, and affects are poorly integrated and poorly modulated. The objective of TFP is to promote identity consolidation, corresponding with the integration of dissociated, affectively charged experiences of self and other and associated internal object relations to form a continuous and stable sense of self in relation to a similarly stable and coherent experience of significant others. Model of change In the TFP model, the predominance of highly charged negative affect states is seen as driving the activation of splitting-based defenses and related dissociative processes. In particular, negative affects and associated representations of self and others are dissociated from positive affective experience and representations. These dynamics are seen to interfere with integrative processes and identity consolidation while introducing instability into interpersonal relations. Given the centrality of negative affect in the TFP model of pathogenesis, the treatment model posits a central role for affect activation, followed by affect containment, in the clinical process (Caligor, Diamond, Yeomans, & Kernberg, 2009; Levy et al., 2006). The TFP treatment frame and the technically neutral stance assumed by the TFP therapist support the emergence of affectively charged object relations in the Transference-focused psychotherapy for borderline and narcissistic personality disorders 151 treatment, where they can be safely contained within the structure of the treatment setting and the therapeutic relationship. These affectively charged perceptions of self and other, which may be expressed in the patient’s interactions with the therapist and/or descriptions of current interpersonal relationships, are a focus of clinical attention in the therapy. For example, a therapist may call attention to a patient’s conviction that the therapist dislikes the patient and wants to get rid of him or her; at another time, the therapist may put into words this same patient’s experience of being very special to the therapist. As affectively charged perceptions of self in relation to others are identified and explored, affects are contained, and extreme and distorted, paranoid and idealized perceptions of self and other are contextualized in relation to one another. The interpretive process, described and illustrated below, organizes these developments and guides clinical interventions so as to promote affect containment, self-awareness, reflection on internal states, and mentalization—capacities that foster integrative processes. Over time, as affects are tempered and extreme perceptions of self and others are gradually modified, dissociated experiences of self and others coalesce, leading to identity consolidation. Principal intervention strategies and techniques Treatment contract Treatment begins with negotiation of a verbal treatment contract. The treatment contract defines the treatment frame and the respective roles and responsibilities of patient and therapist. Patient responsibilities include coming to scheduled sessions on time and speaking as freely as possible about what is on the patient’s mind. Therapist responsibilities include attending closely to the patient’s verbal and nonverbal communications and making comments, when appropriate, to assist the patient’s understanding of himself or herself and others. Because patients with severe personality disorders may not be involved in meaningful work, the contracting process includes discussion about the need to be engaged in some form of work or studies. In addition to these general aspects of contracting, individualized elements are introduced on the basis of the patient’s clinical presentation and prior treatment history. Elements that are frequently introduced involve procedures for handling emergencies and self-destructive behavior within the framework of the treatment and management of behaviors that have interrupted prior treatments, such as inconsistent attendance, excessive or disruptive phone calls or texting, and failure to leave sessions at the end of the hour. In sum, in TFP the treatment contract represents the necessary conditions for treatment, providing a secure and consistent setting in which the patient’s interpersonal relationships, interactions with the therapist, and internal object relations can be explored. Treatment does not begin until the treatment contract has been established. Once the therapy has begun, important aspects of the patient’s personality often come into focus around his or her response to the contract. 152 Contemporary Psychodynamic Psychotherapy Technical neutrality Once the treatment contract has been negotiated and accepted by patient and therapist, the therapist adopts the basic stance of the TFP therapist, described in terms of therapeutic neutrality or technical neutrality. The TFP therapist’s ability to diagnose and explore the dominant, active object relations at each point in the treatment is dependent upon the therapist’s positioning himself or herself as a neutral observer in relation to the patient’s conflicts. Rather than joining with any one side of the patient’s conflict, the therapist attempts to observe all of the conflicting forces within the patient, including those that the patient neglects or rejects; the neutral therapist assesses the entire clinical field. The technically neutral therapist allies himself or herself with that part of the patient that has a capacity for selfobservation, with the aim of fostering the patient’s capacity to observe himself or herself and reflect upon his or her behavior and internal conflicts, replacing reflex action with reflective self-observation. We emphasize that the TFP therapist’s neutral stance defines the therapist’s position in relation to the patient’s conflicts as distinct from the therapist’s attitude toward the patient as a person. In his or her attitude toward the patient, the therapist is anything but neutral. Rather, the TFP therapist conveys interest and curiosity in understanding the patient’s experience and an expectation that the patient can change in ways that will lead to a more productive and satisfying life. Interpretive process In TFP, clinical intervention is organized in relation to the interpretive process, which focuses on exploring the patient’s current relationships, with both the therapist and significant others, and on the patient’s current functioning in his or her daily life. The process of interpretation is carried out repeatedly over time and throughout the course of treatment, titrated to the rise and fall of the patient’s affective state and serving a variety of functions at different clinical moments and phases of treatment. Through the process of interpretation the patient’s self and object representations are identified and labeled by the therapist and traced as they contribute to the patient’s experience of interpersonal relationships. The overall objective of the interpretive process is to expand the patient’s ability to observe himself or herself, to reflect on his or her internal experience and external behavior, and to put momentary perceptions of self and others associated with intense affective states into the larger context of a complex relationship. This selfreflective capacity enhances the patient’s ability to pursue study and work and to maintain satisfying relations with others. The interpretive process can be conceptualized in terms of four levels of intervention, with each sequential level preparing the patient to make use of subsequent levels (Caligor et al., 2009). In concert, the four levels of intervention constitute a complex process, involving much repetition and moving to and fro, played out somewhat differently with each patient. The first level of intervention entails defining the dominant object relations, the implicit perceptions that the patient has of himself or herself in relationship to Transference-focused psychotherapy for borderline and narcissistic personality disorders 153 others, including the therapist. The therapist begins by putting words to the patient’s dominant affective experience in session, described in terms of an internal object relation or relationship pattern. In the treatment of BPD patients the dominant object relation often takes the form of a victim in the hands of a persecutor. In the treatment of NPD patients the dominant object relation is often composed of someone superior and devaluing in relation to someone inferior, dismissed, and inept. With both BPD and NPD patients the dominant affect is most commonly negative, colored by hostility. Regardless of the specific features of the dominant object relation, the TFP therapist begins by attempting to clarify the view of self and other organizing the patient’s experience in the session. This process often leads to the activation of the dominant object relations in relation to the therapist, whose task it is to help the patient put his or her experience into words. In this process, the therapist approaches the material through the patient’s subjectivity without calling into question the patient’s experience. Done well, identifying and putting words to the dominant object relationship of patient to therapist or significant other can provide affective containment and promote self-observation on the part of the patient while communicating the therapist’s empathy and wish to understand. The next level of interpretation entails observing and identifying role reversals within the object relations dyads that are active in the session. In this process, the therapist tactfully helps the patient to attend to aspects of the patient’s behavior and experience (typically aggressive) that have been dissociated, denied, and seen in the other. For example, at the same time that the patient may perceive himself or herself as a victim in the hands of a victimizing therapist, the patient may angrily criticize the therapist; that is, the therapist becomes the victim of verbal attack at the hands of the patient. Or, as commonly occurs in treating patients with NPD, at the same time that the patient experiences the therapist as inattentive and uninterested, the patient uses the therapist as a sounding board, ignoring or interrupting whenever the therapist attempts to speak. Often, the patient is very aware of one configuration, for example, feeling like a victim in the hands of others or dismissed by an uninterested and inattentive therapist, but is not consciously aware of the relationship with roles reversed. For example, the first patient is not aware of victimizing the other, and the second patient is not aware of being dismissing and inattentive toward the therapist. By pointing out role reversals, the therapist introduces a new and different perspective, inviting the patient to go beyond his or her immediate, in-the-moment experience to attend to aspects of his or her behavior and experience that have been dissociated and denied. This process promotes self-awareness along with the patient’s capacity to step outside of immediate, affectively charged experiences to entertain alternative perspectives. Individuals with NPD often have particular difficulty developing this capacity and may remain locked in a one-sided, rigid, and static view of the therapeutic interaction for extended periods of time (Diamond, Yeomans, & Levy, 2011). The third level of interpretation entails making connections between contradictory (typically idealized and persecutory) experiences of self in relation to other that have been defensively dissociated across time. Here, the therapist invites the patient to observe and reflect on the polarized and contradictory nature of the 154 Contemporary Psychodynamic Psychotherapy patient’s experience, for example, that today the therapist is heartless and the patient is neglected and enraged, while only last session the therapist was infinitely caring and the patient was basking in the therapist’s love (a common contradiction in treating patients with BPD), or today the therapist is useless, totally ineffective, an exploitative charlatan, while last session the therapist was a powerful genius, admired and feared (a common contradiction in treating patients with NPD). This level of intervention begins by pointing out the instability of the patient’s experience, a process that invites reflection and curiosity on the part of the patient about the relationship between his or her internal experience and external reality. Appreciation of the shifting and contradictory quality of the patient’s experience ultimately helps the patient appreciate that experience is subjective, internal, and constructed, in contrast to concrete; the patient has the opportunity to observe and reflect upon how his or her mind works and how it influences the patient’s behavior and relationships, fostering a capacity for mentalization. The fourth level in the interpretive process moves to the level of symbolic meanings and unconscious motivations as the therapist offers hypotheses about how to understand the polarized and unstable quality of the patient’s experience. For example, the therapist might suggest that the patient with BPD maintains maladaptive, contradictory, and polarized (idealized and persecutory) views of the therapist or significant others out of a wish to preserve the possibility of finding a perfect caretaker or that the patient with NPD clings to a devalued view of the therapist because if the therapist were effective and able to help, it would constitute a humiliating confirmation of the patient’s inferiority. It is this final step in the interpretive process that corresponds with conventional psychodynamic and psychoanalytic notions of interpretation, focusing on conveying understanding of unconscious meanings and motivations. However, in TFP, it is emphasized that in the treatment of severe personality disorders, exploration of unconscious meanings is the final step in a complex process and is introduced only after earlier interventions have helped the patient become aware of, troubled by, able to reflect upon, and curious about the dissociated nature of his or her experience. Process of treatment There are discernible stages in the TFP treatment of severe personality disorders. Treatment is preceded by careful diagnostic assessment focusing on presenting symptoms and difficulties, overall functioning in work, interpersonal and intimate relations, and personal interests and use of leisure time. Conventional evaluation of symptoms and personality functioning is complemented by assessment of level of personality organization, reflecting the severity of personality pathology across the domains of identity, object relations, defenses, moral functioning, and aggression. After completing the assessment, the therapist shares his or her diagnostic impression and discusses treatment options with the patient. If patient and therapist agree upon a course of TFP, the next step is negotiation of a verbal treatment contract. Contracting sets the stage for the early treatment phase, in which challenges to the treatment frame, threats of premature dropout, Transference-focused psychotherapy for borderline and narcissistic personality disorders 155 and patient criticism of the therapy are common. It is in this phase that serious and potentially lethal behaviors are most common in the treatment of patients with BPD, while either scathing devaluation of the therapist or a dismissive, neglectful attitude that fails to register the therapist as an individual is common in the treatment of patients with NPD. The structure of the treatment frame, consistent focus on destructive acting out, and utilization of limit setting as needed ultimately lead to attenuation of out-of-session self-destructive behavior, making it possible to shift clinical attention to understanding the underlying conflictual object relations that drive these behaviors, which typically now become focused in the treatment and, in particular, in the therapeutic relationship. A sign of progress in TFP is when the patient’s daily life is operating without disruptive acting out while the patient’s dysfunctional representations of self and other are manifested in a conflicted relationship with the therapist, where they can be actively examined. The usual progression of change in TFP is a reduction in problem behaviors followed by the patient’s growing recognition of aggressive affects that can be owned rather than projected onto others. Gradually, there is modification in the representations of self and others; idealized and persecutory object relations become less extreme and affectively charged and begin to transiently coalesce. These changes are reflected in the quality of the therapeutic relationship and track with growing productive involvement in work and relationships in the patient’s daily life. In our clinical experience, enhanced capacity for intimate relationships is often the last domain to develop. Supporting evidence A principle-driven TFP treatment manual was first described in 1999 (Clarkin, Yeomans, & Kernberg, 1999) based on observing videotaped treatments of senior clinicians treating BPD patients and then extracting principles of intervention. Completion of the TFP treatment manual and early feasibility pilot studies (Clarkin et al., 2001) were followed by an RCT comparing TFP with dialectical behavioral therapy (DBT) and with a dynamically oriented supportive treatment (Clarkin, Levy, Lenzenweger, & Kernberg, 2007). BPD patients (N 5 90) were randomly assigned to treatment delivered by therapists trained in the respective treatments, with blind raters and reliably measured outcome variables. All three treatments showed significant change across multiple domains after 1 year of treatment. Both TFP and DBT were associated with improvement in suicidality. Only TFP was significantly associated with improvement in impulsivity, irritability, verbal assault, and direct assault. Patients receiving TFP improved significantly in narrative coherence on the Adult Attachment Interview, unlike patients receiving the other treatments. Reflective functioning (RF), the capacity to understand the behavior of oneself and others in terms of intentional mental states such as thoughts, feelings, and beliefs, also increased significantly in patients receiving TFP. There was no significant change in RF with the other treatments. 156 Contemporary Psychodynamic Psychotherapy In a second RCT (Doering et al., 2010), conducted at two sites in Europe (Munich, Germany, and Vienna, Austria), female patients with BPD (N 5 104) were randomized to 1 year of either TFP or treatment by community therapists experienced in the treatment of BPD. The outcome in the TFP group was significantly superior with regard to the number of DSM 4 BPD criteria at the end of treatment; improvement in psychosocial functioning; and reduction in suicide attempts, number and duration of in-patient treatments during the 1 year of treatment, and number of premature dropouts (38.5% vs. 67.3%). In addition, patients in TFP showed superior improvement relative to the comparison group in positive change in personality organization and functioning. A more recent study explored the impact of 1 year of TFP at the level of neural functioning in patients with BPD (Perez et al., 2015). The study employed an emotional linguistic Go/NoGo task to investigate the processing of negative stimuli by female patients with BPD prior to and after 1 year of treatment. Measures of psychological functioning at multiple points during the 1 year of treatment were combined with assessment of neurocognitive functioning before and after treatment. Patients (N 5 10) exhibited significant change over the course of 1 year, including a reduction in affective lability, a reduction in interpersonal sensitivity, and a reduction in paranoia. In a comparison of pretreatment and posttreatment fMRI scans, BPD patients manifested relative increased activation in cognitive control regions (right anterior-dorsal ACC, dorsal-lateral PFC and FPC). Relative activation decreases were found in left ventrolateral PFC and hippocampus. The investigators concluded that TFP may mediate clinical symptom improvement, in part, by improving cognitive emotional control via increased engagement of dorsal ACC, posterior-medial OFC, frontopolar, and dlPFC activity. These effects may be mediated by top-down frontal control over limbic emotional reactivity and semantic memory-processing systems. This is consistent with the clinical hypothesis that the mechanism of change for BPD in TFP in part involves increased affect regulation achieved through the ability of the patient to put momentary affect arousal, especially in social interactions, into a more benign and broader context (Levy et al., 2006). Clinical illustration of TFP for BPD and NPD Basic strategies of transference-focused psychotherapy The TFP therapist’s basic strategy is to identify the object relations organizing the patient’s experience in the moment. As the dominant object relations are identified, interventions are guided by an understanding of the TFP interpretive process. A 28-year-old woman diagnosed with BPD with prominent narcissistic features presented with problems with interpersonal and intimate relationships. Borderline features included affective instability, stormy and unstable interpersonal relationships, anger outbursts, intermittent dissociative states, feelings of emptiness, and an identity disturbance. Narcissistic features included covert grandiosity, failure of Transference-focused psychotherapy for borderline and narcissistic personality disorders 157 empathy, entitlement, and chronic feelings of envy. The patient has been in TFP for 6 months. Patient: So, Bill [the patient’s boyfriend] and I had another fight last night. He is so withholding and selfish . . . I can’t stand him. He used to be so caring, but now he only thinks of himself. I’m so frustrated . . . just disgusted with him. And now I’m upset because he’s not speaking to me. [The therapist asks for clarification.] Therapist: Hmm. Can you tell me more about what happened last night? Patient: He didn’t get home until 10:00. He knows I hate that. It’s always the same thing. And then we get into a fight. And then I get so upset . . . I can’t sleep. [The patient’s communications remain vague, superficial, and self-referential. The therapist further pursues clarification.] Therapist: Can you take me through what happened so that I can get a clear understanding of what led up to the fight? Patient: Well, I was upset because he texted me to say he had to work late— again! So there I was, waiting and waiting, texting and texting. And then he stopped responding to my texts. I was so upset. He knew how upset I was, I told him, how could he stop responding? Therapist: It’s hard to be waiting, and then when he stops responding, it makes you feel even worse. [The therapist has put the patient’s experience in the dominant object relation into words while communicating empathy.] Patient: Yes, exactly. It’s always the same thing. Maybe I should just give up on having a relationship. [Pause] Patient: And then it turned out he didn’t get home until after 10:00! By then I was just so upset about everything. But I thought we could talk it out. I told him I just needed him to give me a hug and tell me I had a right to be angry and upset. I told him if he would do that, I would feel better, and then I could listen to his side, but not before. But he wouldn’t do it! He just got angry at me and stormed out. All I wanted was a hug! He’s so selfish. Therapist: You needed to feel that he was listening to you . . . to feel he heard you. Patient: [Calming down] Yes. [Thus far the therapist has clarified the patient’s experience and put it into words, in the process communicating empathy and the ability to understand. These interventions have also provided some degree of affect containment, and the patient seems more reflective. The therapist infers the patient may be in a sufficiently reflective state to respond favorably to an invitation to entertain an alternative perspective.] Therapist: I get it. It’s upsetting and frustrating to be put in that position, waiting for someone who doesn’t hear you, who doesn’t seem to care about how you are feeling. At the same time, I’m trying to imagine how Bill felt. Patient: What are you saying? Therapist: Well, I guess I’m thinking about this familiar pattern between you and Bill . . . I’m wondering if in a funny way the two of you kind of end up in the same boat. 158 Contemporary Psychodynamic Psychotherapy [Pause] Patient: What do you mean? Therapist: Well, at the same time that you experienced Bill as selfish, refusing to listen and not caring about your needs, I wonder if he might experience you in the same way. For example, when you refuse to discuss things with him until he hugs you, even though he might not have felt like hugging you, or says you are right to be angry, when he might feel otherwise. What are your thoughts about what I am suggesting? In response to this and similar interventions made over time, the patient became increasingly able to get beyond a rigidly held view of herself as the frustrated and disappointed victim of someone withholding and refusing to meet her needs while becoming more aware of her own frustrating and withholding behavior. Several weeks later Therapist: We’ve been talking a lot about how you often experience other people as frustrating you, not giving you what you need. It sounds like this is something that happens a lot, pretty much in all your important relationships. Patient: Yeah, the more we talk about it, the more I see how I always end up in that place, frustrated, disappointed, and angry. I must choose the wrong people. Therapist: Perhaps. But it always starts out feeling promising. Like with Bill in the beginning. Patient: True. But then I see their true colors. Therapist: Well, maybe. But I’m struck by how unstable your image of the other person seems to be, how it can shift, kind of dramatically—like with Bill, in the beginning seeming like someone who could take care of you, which made you feel happy and hopeful, then changing to someone who is selfish and uncaring, and you feel frustrated and angry. Patient: It does shift, like you say. Therapist: It’s like it’s black or white, all or nothing—as if in your mind the other person is either perfectly caring or they become totally selfish—there’s no in between. And when they frustrate you or let you down, it’s like the positive, caring relationship you had evaporates. Patient: That is what happens. Every time. It’s awful. You’re the only person who never disappoints me or lets me down. [The therapist has called the patient’s attention to the rigidly polarized and dissociated quality of her experience. The patient’s response to the intervention is somewhat concrete. The therapist decides to focus on the transference.] Therapist: Well, I’ve been thinking about that, how you never talk about feeling frustrated or disappointed with me. Patient: What about it? That’s how I feel. Therapist: It kinds of reminds me of how things were with Bill in the beginning. You felt that way. Patient: But now I am always angry at him. Transference-focused psychotherapy for borderline and narcissistic personality disorders 159 Therapist: Yes, exactly. It makes me wonder if out of your awareness, you’re working hard to keep our relationship free of conflict, almost perfect, to make sure you don’t end up once again disappointed and frustrated. Then you would lose me too, and that would feel terrible. [The therapist has offered an interpretation, suggesting that the patient may feel the need to keep her relationship with the therapist in an idealized state for fear that any frustration in relation to the therapist might lead her to lose the feeling of positive connection and care she experiences in the transference.] The special challenge of narcissistic transferences While the basic strategies of TFP for BPD and NPD are the same, there are predictable differences in the clinical process with the two groups of patients, particularly in relation to the object relations activated in the early phases of treatment. Patients with BPD frequently present with a central dyad of a hurt or abandoned self in relation to a persecutory or rejecting other. These object relations are typically quickly joined by a variety of other polarized dyads (e.g., loving, hating, dependent, fearful). In contrast, patients with NPD generally present initially with a central dyad of a grandiose self in relation to a devalued other and an apparently stable organization around that central dyad. This organization is typically expressed in the NPD patient’s attitude toward and interactions with the therapist. These “narcissistic transferences” are often concretely experienced, persistent, and difficult to address. Interventions, such as those illustrated earlier, that mirror the patient’s dominant experience without calling it into question can be helpful insofar as they avoid confronting the patient’s grandiosity early in treatment at a time when recognizing that the therapist has perspectives that go beyond what the patient is already aware of may be experienced as a humiliation or a threat by the patient. The therapist’s capacity to empathize with the NPD patient’s experience without challenging it is dependent on the therapist’s ability to contain the often negative feelings stimulated in therapists by the NPD patient’s devaluation. During the first several months of her therapy, the patient above had spoken virtually nonstop and unreflectively about whatever was on her mind in the moment. Her discourse was unfocused, undirected, and superficial. When the therapist attempted to intervene, the patient became irritated. She consistently ignored, devalued, or distorted anything the therapist said. Patient: I got to work on time, but then one of the elevators was out of service, so I had to wait. Other than that, I had a good day at the office. There’s a lot going on. A fair amount of work. And I’m redecorating my apartment. My boss is out of town but calls in all the time. I’m going to a concert tonight. Bill is going to meet me there. I like the band. Therapist: [Attempting to organize and deepen the patient’s monologue] Sounds like you’re making an effort to balance the demands of your job and your life outside work. [Patient rolls her eyes but otherwise ignores the therapist’s comments, returning to her monologue.] 160 Contemporary Psychodynamic Psychotherapy Therapist: You rolled your eyes in response to my comment. Patient: I didn’t notice. It doesn’t mean anything if I did. What did you say? Therapist: You sound annoyed. Patient: I am annoyed. You aren’t listening to me. [Patient returns to monologue.] Therapist: It strikes me that what is happening here is similar to what happens with Bill, I mean your feeling that I don’t listen. Patient: You are an idiot! You are nothing like Bill. And you keep interrupting me. [The therapist recognizes that her intervention was premature. She shifts gears, focusing on the patient’s experience in the moment.] Therapist: I can see how frustrating it is to have a therapist who insists on interrupting and seems not to understand that what you need it to be heard. [Patient relaxes a bit, is silent.] Therapist: What are your thoughts? [Interventions of this kind, focusing on the first level of interpretation, can help the patient with narcissistic pathology develop a capacity to observe and ultimately reflect on his or her role in the ideal self devalued therapist dyad. Over time, this patient became able to make use of the second level of interpretation as she came to appreciate how she actively devalued the therapist while anticipating that the therapist would at any moment devalue her.] Concluding comments TFP is a theory-driven, psychodynamic treatment for severe personality disorders focused specifically on the structural organization of self-functioning and related functioning with others (American Psychiatric Association, 2013). The duration of treatment depends on the level of severity of self and other functioning. TFP is empirically supported for treatment of BPD, and the principles of the treatment are being expanded to address NPD (Diamond et al., in press) and the range of self and other functioning across the personality disorders (Caligor et al., 2018). TFP is based in object relations theory, and the clinical focus is on identifying and exploring the affectively charged perceptions of self and other that are activated, moment to moment, in each session. TFP uses a structured approach articulated in the treatment contract to attain a level of behavioral control needed to successfully pursue exploratory psychotherapy with patients with severe personality disorders. Putative mechanisms of change focus on fostering top-down, cortical control of highly charged affect states activated in the treatment. References American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author. Transference-focused psychotherapy for borderline and narcissistic personality disorders 161 Caligor, E., Diamond, D., Yeomans, F. E., & Kernberg, O. F. (2009). The interpretive process in the psychoanalytic psychotherapy of borderline personality disorder. Journal of the American Psychoanalytic Association, 57, 271 301. Caligor, E., Kernberg, O. F., & Clarkin, J. F. (2007). Handbook of dynamic psychotherapy for higher level personality pathology. Washington, DC: American Psychiatric Publishing. Caligor, E., Kernberg, O.F., Clarkin J.F., & Yeomans, F.E. (2018). Psychodynamic therapy for personality pathology: Treating self and interpersonal functioning. Washington, DC: American Psychiatric Publishing. Clarkin, J. F., Foelsch, P. A., Levy, K. N., Hull, J. W., Delaney, J. C., & Kernberg, O. F. (2001). The development of a psychodynamic treatment for patients with borderline personality disorder: A preliminary study of behavioral change. Journal of Personality Disorders, 15, 487 495. Clarkin, J. F., Levy, K. N., Lenzenweger, M. F., & Kernberg, O. F. (2007). Evaluating three treatments for borderline personality disorder: A multiwave study. American Journal of Psychiatry, 164, 922 928. Clarkin, J. F., Yeomans, F. E., & Kernberg, O. F. (1999). Psychotherapy for borderline personality. New York: Wiley. Diamond, D., Levy, K. N., Clarkin, J. F., Fischer-Kern, M., Cain, N. M., Doering, S., . . . Buchheim, A. (2014). Attachment and mentalization in female patients with comorbid narcissistic and borderline personality disorder. Personality Disorder: Theory, Research, and Treatment, 5, 428 433. Diamond, D., Yeomans, F. E., & Levy, K. N. (2011). Psychodynamic psychotherapy for narcissistic personality disorder. In K. Campbell, & Miller (Eds.), The handbook of narcissism and narcissistic personality disorder: Theoretical approaches, empirical findings, and treatment. New York: Wiley. Diamond, D., Yeomans, F.E., Stern, B. & Kernberg, O.F. (in press). A clinical guide for treating narcissistic disorders: A transference focused psychotherapy. New York: Guilford Press. Doering, S., Horz, S., Rentrop, M., Fischer-Kern, M., Schuster, P., Benecke, C., . . . Buchheim, P. (2010). Transference-focused psychotherapy v. treatment by community psychotherapists for borderline personality disorder: Randomized controlled trial. British Journal of Psychiatry, 196, 389 395. Kernberg, O. F., & Caligor, E. (2005). A psychoanalytic theory of personality disorders. In M. Lenzenweger, & J. F. Clarkin (Eds.), Major theories of personality disorder (2nd ed., pp. 114 156). New York: Guilford Press. Levy, K. N., Meehan, K., Kelly, K., Reynoso, J., Weber, M., Clarkin, J. F., & Kernberg, O. F. (2006). Change in attachment patterns and reflective function in a randomized control trial of transference-focused psychotherapy for borderline personality disorder. Journal of Consulting and Clinical Psychology, 74, 1027 1040. Perez, D., Vago, D., Pan, H., Root, J., Tuescher, O., Fuchs, B., . . . Stern, E. (2015). Frontolimbic neural circuit changes in emotional processing and inhibitory control associated with clinical improvement following transference-focused psychotherapy in borderline personality disorder. Psychiatry and Clinical Neurosciences, 70, 51 61. Sharp, C., Wright, A., Fowler, J., Frueh, B., Allen, J., Oldham, J., & Clark, L. (2015). The structure of personality pathology: Both general (‘g’) and specific (‘s’) factors? Journal of Abnormal Psychology, 24, 387 398. Yeomans, F., Clarkin, J. F., & Kernberg, O. F. (2015). Transference-focused psychotherapy for borderline personality disorder: A clinician’s guide. Washington, DC: American Psychiatric Publishing. Dynamic deconstructive psychotherapy for substance use disorders co-occurring with personality disorders 11 Robert J. Gregory Department of Psychiatry and Behavioral Sciences, SUNY Upstate Medical University, Syracuse, NY, United States Conventional wisdom regarding substance use disorders often emphasizes the biomedical model, that is, understanding substance use disorders as resulting from a genetic predisposition kindled by the direct effects of chemical substances on the brain’s neural reward circuitry. Certainly, it is important to acknowledge the effects of external chemicals on human motivation, that is, how the chemicals can induce physical dependence through tolerance and withdrawal, as well as how they can activate the opioid and dopamine reward systems in the brain and downregulate the receptors of those same neurotransmitters, leading to increasing drug craving and dysphoria. The biomedical model usefully explains why laboratory animals will repeatedly inject themselves with certain chemicals to the point of death. This model has more difficulty explaining why addictive behavior may occur with drugs that do not induce physical dependence, such as some hallucinogens, or with nonchemical activities, such as gambling. Alternatively or adjunctively, a behavioral model for understanding substance use disorders has been proposed. In this model, chemicals and activities that are highly pleasurable are understood to be highly reinforcing of addictive behaviors. Behaviors that are reinforced tend to increase in frequency and, over time, can be difficult to extinguish. The behavioral model helps us to understand how pleasurable activities can become as addictive as certain chemicals. It also helps us to understand how environmental cues that remind us of the reinforcer, that is, are conditioned with it, can trigger cravings (think of Pavlov’s dogs). The behavioral model does not take into account mental processes, the unconscious, relationships, identity, or emotions. It has difficulty explaining why addictive behavior can persist despite strong negative consequences that should counteract the reinforcing effects of the chemical or pleasurable activity. It also cannot explain the profound personal and interpersonal aspects of addictive illness (e.g., why therapists may dread treating individuals who struggle with substance use disorders and use pejorative labels?). The present chapter aims to present a contemporary psychodynamic understanding of addiction, especially its personal and interpersonal aspects. It will also Contemporary Psychodynamic Psychotherapy. DOI: https://doi.org/10.1016/B978-0-12-813373-6.00011-8 © 2019 Elsevier Inc. All rights reserved. 164 Contemporary Psychodynamic Psychotherapy introduce dynamic deconstructive psychotherapy (DDP) (Gregory & Remen, 2008), a psychotherapy model that uses this psychodynamic understanding to effectively treat individuals suffering from addictive illness, especially those cooccurring with personality disorders. Emotion processing There is evidence that the etiology of substance use disorders varies in different groups of individuals. For example, individuals with trauma histories tend to use substances in response to negative emotions and stressful situations, whereas those without trauma histories tend to use substances in response to environmental cues (Waldrop, Back, Verduin, & Brady, 2007). An interpretation of these findings is that the latter group of individuals may have a biological drive for certain substances, which is induced through continued use of the substance and is triggered by environmental cues. However, individuals with a history of trauma may use substances to self-medicate their distress, employing their addiction as a coping mechanism. An overlapping group of individuals, that is, those with personality disorders, may also turn to substances as a coping mechanism. Up to two thirds of individuals with borderline personality disorder (BPD) have cooccurring substance use disorders (Zanarini, Frankenburg, Hennen, Reich, & Silk, 2004). Tragesser, Trull, Sher, & Park (2008) demonstrated that among individuals with cluster B personality disorders, drinking alcohol serves in part to cope with negative emotions. In order to understand why substances can provide important soothing functions for individuals with personality disorders, it is helpful to look at the neuroscience of emotion processing. Normal and adaptive processing of emotions involves activation of neural pathways through the prefrontal cortex, enabling identification of emotions, accurate appraisal of experiences, and selection of appropriate responses (Ochsner et al., 2004). However, studies examining emotion processing of individuals with personality disorders, especially BPD, indicate that the prefrontal areas are relatively deactivated when the individual is presented with an emotional stimulus, such as viewing upsetting photographs (New, Perez-Rodriguez, & Ripoll, 2012). When individuals are unable to use their prefrontal areas to identify their emotions and appraise their experiences, certain subcortical areas of the brain become hyperactivated in response to an emotional stimulus, especially the amygdala, which mediates anxiety and arousal, and the ventral striatum, which mediates impulsive pleasure seeking. Such individuals therefore become anxious and hyperaroused when presented with an emotional stimulus, such as rejection. They then seek impulsive pleasurable activities, such as binge eating, shopping, sex, or substance use, since these activities dampen their arousal through a negative feedback loop from the ventral striatum to the amygdala. Thus engagement in impulsive pleasurable activities serves as a primitive coping mechanism to manage the anxiety and hyperarousal that are characteristic of this population’s response to emotional stress. Dynamic deconstructive psychotherapy for substance 165 The treatment implication of this model is for therapists to find ways to strengthen the higher level neural pathways for emotion processing. A remarkable and well-replicated neuroscience finding is that when healthy individuals simply try to identify emotions in response to a stimulus, activity in the amygdala and physiological arousal decrease (Lieberman et al., 2007). Helping patients to identify specific emotions can help to reroute emotion processing from the subcortical regions to the prefrontal cortex, therefore decreasing anxiety and arousal, and decreasing the need to use substances or other impulsive pleasurable activities to self-soothe. The analogy in physical medicine is the treatment of stroke. After the first few hours the only effective treatments are physical therapy and occupational therapy. Through these treatments, patients can sometimes achieve complete or nearcomplete restoration of functioning. The reason that these treatments are effective is that they reroute neural processing from dead nerve cells to alternative neural pathways through repeated practice. There is an old adage: Neurons that fire together wire together. As these motor neuron pathways become strengthened through continued practice, neuromuscular functioning is restored. Similarly, an important mechanism of psychotherapy is to rewire the brain through strengthening of higher level neural pathways for emotion processing (see the subsection “Association” under the section “Summary of the dynamic deconstructive psychotherapy treatment model”). The denial system and relationships In addition to self-soothing, another important function of substance use among individuals with personality disorders is that they substances can serve as a substitute for relationships. Patients sometimes tell me that giving up smoking was like saying goodbye to their best friend. Thus soothing and comforting aspects of addiction have an interpersonal aspect. This may not be surprising, given that the attachment system and the drug reward system are mediated through the same brain region, that is, the ventral striatum, and through the same receptor system, that is, µ opioid receptors (Moles, Kieffer, & D’Amato, 2004). In other words, the brain’s reward system cannot tell the difference between a hug and a drug. The advantage of having a drug as your best friend is that a drug is a friend who will never hurt you or betray you; it is a relationship in which you are in control—or at least that is the fantasy; the denial system maintains an illusion of control. Mark Twain is said to have quipped, “Cigarettes are the easiest things to quit in the world! I’ve quit hundreds of times!” Individuals struggling with substance use disorders will use similar language, but not get the humor of the statement. The phenomenon of splitting is also part of the denial system. In splitting, individuals with substance use disorders hold in consciousness either idealized or devalued attributions regarding their substance use but not both at the same time. For example, they may describe their substance use as “a nasty habit that does me no good.” Conversely, they may describe the wonderful effects of the substance but 166 Contemporary Psychodynamic Psychotherapy split off from consciousness its negative consequences. For example, they may describe their substance use as “the only thing that helps me to relax and be myself. I don’t see any problem with it.” This tendency against psychological integration of the positive and negative aspects of substance use makes it difficult for addicted individuals to think effectively about their relationship with the substance and to gain perspective on their addictive behavior. A treatment implication is for the therapist to help patients to acknowledge both positive and negative aspects of their substance use and to hold the opposing perspectives in their consciousness at the same time. It is sometimes helpful to think of addiction as a type of transitional object, since it has many of the same features, as expounded by Winnicott (1953). Addictions, such as those to alcohol and drugs, have soothing and comforting qualities; they enable separation from real relationships, provide an illusion of omnipotent control, and bridge the boundary between internal and external reality. The denial system, with its illusion of control, accounts for why the CAGE questionnaire is such an effective screen for alcoholism. The C of the CAGE asks, “Have you ever tried to cut down on your drinking?” Often, the alcoholic will proudly provide an affirmative response, since he or she has “quit hundreds of times.” The denial system also accounts for why Step 1 of Alcoholics Anonymous (AA) is so helpful and also so difficult (Johnson, 1993). Step 1 is to “admit that I am powerless over my drinking behavior.” This step challenges the very core of the denial system, that is, the illusion of control. Finally, the denial system, including both the fantasy of control and splitting, accounts for why a motivational interviewing approach can be helpful. In motivational interviewing, the therapist respects the autonomous decision-making of the patient, thereby enabling the patient to maintain a sense of control while bringing together the split attributions involved in the addictive behavior. An important treatment implication is for the therapist to be sensitive to the patient’s sense of vulnerability in close relationships and fear of control. It is therefore especially important in this patient population to respect the patient’s autonomy. Technically, this includes avoiding asking intrusive questions, letting patients set the agenda for the session, and avoiding giving advice or instruction. It is also important to be very receptive to criticism or disagreement, providing many opportunities for patients to verbalize their ambivalence about treatment, abstinence, and/ or the patient therapist relationship. The more the ambivalence is verbalized, the less it will be acted out. Respect for autonomy does not imply that the therapist cannot provide information about substances and the potentially harmful effects of their use, but the therapist does so in the role of a consultant, letting the patient decide what to do with the information, and respecting the patient’s right and ability to choose what is in his or her own best interests. For example, a therapist might state, “It’s possible that much of your anxiety and periods of depression are due to heavy alcohol use. I am not saying that you should give up the drinking behavior, but I am sharing this so that you can be fully informed when deciding whether the positive benefits that you derive from drinking outweigh the downside risks.” Dynamic deconstructive psychotherapy for substance 167 Another clinical implication of the denial system is the importance for the therapist to check in regularly with addicted patients about any recent relapses of substance misuse and to explore these incidents. A common mistake of therapists is to ignore the addiction and instead to focus exclusively on stressors and relationships, both past and present, providing support, advice, and interpretation of these. The results of this mistake are not immediately apparent. At first, everything seems to be going well; the patient seems engaged in treatment and the therapist is feeling useful. The only difficulty is that the patient’s presenting symptoms of depression or anxiety are not getting better and actually seem to be gradually getting worse. It is eventually revealed that the addictive behavior has worsened over time, culminating in a medical, financial, legal, or family crisis. The therapist ends up feeling foolish, as though he or she has been duped and betrayed, and vows never again to treat addicted patients with psychodynamic therapy. This commonly occurring anecdote can be understood as the therapist unconsciously participating in the patient’s denial system, minimizing the central importance of the addiction, and mutually avoiding speaking of it. As the therapy progresses toward exploration of sensitive material, the patient increasingly fears and resents the therapist’s intrusive questions, advice, and interpretations. To maintain the relationship, even while distancing himself or herself from it, the patient turns increasingly to addictive behaviors, often using the substances before sessions. Relational dynamics of shame (or why do we dread patients with substance use disorders?) The denial system is driven not only by a fear of loss of control, but also by shame. Therapists will be unable to effectively manage patients’ addictions unless they recognize the profound and often unconscious sense of shame underlying all addictive behavior. Shame can be difficult to recognize in addicted patients, since they can often appear grandiose. One way to understand this is to think of severely addicted patients as having a narcissistic self-structure characterized by a grandiose self that is conscious while their shameful and shaming internal objects are split off and projected onto others, repressed, or defended against through blame and externalization of agency (Kernberg, 1975). For example, such individuals may blame losing their job on having an unreasonable boss rather than on repeatedly showing up late or intoxicated to work. Spouses are another frequent target of externalization; for example, the patient may say, “I wouldn’t need to drink if my wife weren’t on my case all the time!” The combination of bragging about accomplishments while blaming others for negative consequences of the patient’s addictions engenders scornful, judgmental, and pejorative countertransference reactions among friends, families, and providers who interact with patients who have substance use disorders. A natural countertransference impulse is for the therapist to give the patient a reality check and say something like “I notice you are blaming everyone else for your problems. Until 168 Contemporary Psychodynamic Psychotherapy you start taking responsibility for the consequences of your addictive behavior, you are not going to get very far in recovery.” What the therapist is not understanding is that the patient’s grandiosity and externalization are intrapsychic defenses against shame, and therefore any intervention that induces further shame will be unsuccessful. Instead of breaking through the grandiosity, such an intervention will only cause the patient to become more defensive, either reacting with hostility, demanding of the therapist, “Just who do you think you are to judge me?,” or detaching from the therapist and seeking a safer, more soothing relationship with a substance. A patient once confided to me, “Every time my doctor tells me to quit drinking, I get a strong urge to drink and head for the nearest bar after the visit.” As discussed earlier, a fantasy of control is an important component of the denial system. This fantasy protects against the feelings of shame, concern, and helplessness that are engendered through an inability to control the addiction, despite repeated negative consequences. Individuals with substance use disorders are remarkably adept at unconsciously transferring these feelings and reactions onto friends, family, and providers by using projective identification. Family members typically try to control the addictive behaviors through hiding substances in the home or through threats, for example, “I’m going to leave you unless you stop drinking.” The family members have incorporated the afflicted individual’s fantasy that the addictive behavior can be controlled through willpower. A major focus of Al-Anon is to help families to realize that they are unable to control their family member’s addiction. By way of the patient’s projective identification, therapists may also incorporate the fantasy of control and will often manifest the fantasy through suggestions that their patients cut down on their use of addictive substances. As part of this fantasy, therapists believe that they can control the addiction through the power of providing insight, education, and suggestions. For example, a therapist might state, “Your excessive drinking is causing you to feel sick and feel even worse about yourself, which is causing you even more stress. If you cut down on your drinking and exercise regularly, you will feel healthier, less stressed, and will have more energy.” The patient might accept this insight and suggestion with gratitude, because the patient shares the fantasy of control with the therapist. But as the urges become uncontrollable and the behavior spins out of control again, the patients attempt to hide their addictive behavior and its severity from both themselves and their therapists. After weeks or months, the therapist finds out that the addictive behavior has worsened and then feels duped, angry, and helpless. After many such episodes, the therapist begins to feel hopeless about ever being able to be helpful to the addicted patient or to other individuals suffering from addictions and will try to avoid treating this patient population in the future. They will tell prospective patients, “First get your substance misuse under control. Then we can start the therapy.” One treatment implication of shame dynamics is to support patients’ self-esteem even when they are grandiose, to avoid control struggles, and to keep the conflict within the patient. Self-esteem can be supported by labeling the substance use disorder as an illness that is largely outside the patient’s control. The therapist can reinforce this message by reminding patients of Step 1 of AA, that is, admitting Dynamic deconstructive psychotherapy for substance 169 powerlessness over the addiction. If substance misuse is outside the patients’ control, the patient no longer needs to feel ashamed about it. Although these patients cannot control their substance misuse, they can control and accept responsibility for getting into treatment and staying in treatment. That’s a powerful message for individuals struggling with addictions. Self-esteem can also be supported through mirroring. Mirroring is a paradoxical technique developed by Kohut (1995) for the treatment of narcissistic personality disorder. Kohut described mirroring as “the gleam in the mother’s eye, which mirrors the child’s exhibitionistic display” (p. 116). Thus the therapist acts as a mirror to the grandiosity, reflecting it back to the patient instead of challenging it. For example, when a patient begins to brag about the many textbooks he or she has read and how much more psychology he or she knows than the therapist, the countertransference impulse is for the therapist to provide a reality check and ask, “So what graduate school in psychology did you attend?” This is a shaming response that only ends up strengthening the patient’s grandiosity in order to defend against shame. Instead, a mirroring response would be to state, “Wow! You are well read and know a lot about psychology.” In my experience, the stronger the countertransference impulse toward a reality check, the more effective a mirroring response will be. Often, the results can be immediate and dramatic as the patient begins to identify and acknowledge shame about substance misuse and to take responsibility for his or her actions. Another treatment implication of shame dynamics is to avoid control struggles and to keep the conflict within the patient, that is, to change the conflict from an interpersonal phenomenon to an intrapsychic phenomenon. This can be very difficult to achieve, since addicted patients will attempt to engage the therapist in a control struggle in order to maintain the denial system and avoid an intrapsychic conflict. A good general rule is that if therapists find themselves in a control struggle with their patients, they are likely involved in an enactment, and the session is heading in the wrong direction. I am reminded of a severely addicted patient who presented to me stating, “Doc, you got to do something about my drinking. It’s killing me!” My countertransference emotion was hopelessness, given the severity of his addiction and repeated unsuccessful attempts at rehabilitation. Nevertheless, I proceeded to run through a list of treatment options and facilities, stating, “Just because prior attempts at rehab were unsuccessful doesn’t mean that future ones will be too. Usually it takes more than one attempt at rehab before a lasting recovery can be achieved.” The patient responded, “But I don’t want to quit drinking!” So there we were, only 2 minutes into the interview and already in a control struggle. The patient was attempting to transfer his concerns about drinking onto me through projective identification. Fortunately, in this instance I was able to recognize the defense and respond therapeutically, stating, “But that is the question, isn’t it? What do you want? When you entered the room, you asked me to help you with your drinking, but now you’re not so sure you want to quit. Your drinking must do some very good things for you if you are still wanting to continue using it despite the many negative consequences you have sustained. If you would like, we can explore together the good and bad aspects of drinking so that you can weigh these 170 Contemporary Psychodynamic Psychotherapy together and decide what you’d like to do. I’m in no position to judge what is best for you. Only you can decide that.” Through this intervention, I was able to avoid the control struggle that the patient was unconsciously attempting to create and instead put the conflict about whether or not the patient should drink back onto the patient, where it could be resolved. Dynamic deconstructive psychotherapy DDP is a treatment that takes into account the emotion processing, denial system, and shame dynamics of addiction as outlined above and presents an organized, systematic approach (Gregory & Remen, 2008). It incorporates findings from neuroscience research and object relations theory, especially emphasizing the ideas of Winnicott, Kernberg, and Kohut. The overarching treatment philosophy is deconstructive in orientation. Derrida defined deconstruction as “openness to the other” (Derrida, 2004, p. 155). This philosophy suggests a deferral of assured meaning and an openness to different perspectives. DDP therapists try not to make authoritative interpretations about the meaning behind their patients’ actions or how patients should best live their lives. Instead, therapists work toward facilitating the development of a complex and integrated self through creating a safe space for patients to put their experiences into words, to explore new perspectives on their experiences, and to risk authenticity in their relationship with the therapist. DDP was originally developed for treatment-resistant BPD, especially for cases complicated by cooccurring substance use disorders, but has since been used with many different disorders, especially those involving impulsive behaviors and suicide risk. Both process and outcome researches have been performed on DDP, as summarized below. Empirical research on DDP Empirical research supporting the effectiveness of DDP is based primarily on two clinical trials. The first was a 12-month randomized controlled trial for individuals suffering from cooccurring alcohol use disorders and BPD (Gregory et al., 2008), with a 30-month naturalistic follow-up (Gregory, Delucia-Deranja, & Mogle, 2010). Participants in the study were severely ill; almost half (43%) met criteria for antisocial personality disorder, and 83% met criteria for other substance use disorders. Because of ethical concerns, participants in the control group were not assigned to just a minimalist treatment but were instead referred to the best alternative treatment available in the community, depending on availability and the participant’s willingness to engage in such treatment. The control treatments, labeled optimized community care (OCC), included drug and alcohol rehabilitation facilities, dialectical behavior therapy (DBT), case management, pharmacotherapy, and therapists of an eclectic orientation specializing in the treatment of BPD. When both individual and group contacts were added together, the OCC participants actually received Dynamic deconstructive psychotherapy for substance 171 greater treatment intensity than those receiving DDP. DDP was carried out primarily by psychiatry residents, who had received 3 6 months of weekly training and supervision prior to treating study participants. By the end of the 12-month trial, individuals who had received DDP achieved significantly greater reductions in symptoms of BPD, depression, and heavy drinking than those who had received OCC. These differences were even greater at 30-month follow-up. Clinical response rates for BPD were 90% for individuals receiving 12 months of DDP, as compared to only 40% for those receiving OCC. Moreover, illicit drug use markedly decreased during treatment with DDP, completely remitting by 12 months and sustained at 30-month follow-up. Those receiving OCC, however, steadily increased their use of illicit drugs throughout treatment and follow-up. The second clinical trial was a quasirandomized observational study examining 12-month outcomes of patients treated at a medical university BPD specialty clinic by therapists who were expert in DDP or DBT (Gregory & Sachdeva, 2016). All patients met criteria for BPD, and most had a cooccurring alcohol or drug use disorder. Three treatment modalities were compared: DDP, comprehensive DBT (individual and group components), and a control treatment of weekly eclectic individual psychotherapy with or without DBT skills group. The outcomes of this study were remarkably consistent with those of the prior trial. Patients who received DDP were significantly more likely to achieve reductions in symptoms of BPD and depression than the control recipients; 90% of those receiving 12 months of DDP achieved a clinical response, compared to 40% of those receiving the control treatment. Patients receiving DBT had an intermediate response rate of 67%. In the intent-to-treat analysis, patients receiving DDP had significantly greater reductions in BPD symptoms, depression, and self-harm than those receiving DBT and experienced greater improvement in social and occupational functioning. Other research on DDP has focused on mechanisms of change. When video recordings of DDP sessions were rated by observers who were blinded to outcome, therapist adherence to the DDP treatment model was found to correlate strongly with outcome (r 5 0.64), suggesting that DDP works primarily through specific mechanisms rather than through common factors, such as therapist warmth and attentiveness (Goldman & Gregory, 2009). After an independent review of the evidence supporting its effectiveness by a US federal agency, the Substance Abuse and Mental Health Services Administration, DDP was included in the National Registry of Evidence-Based Programs and Practices (www.nrepp.samhsa.gov). Summary of the DDP treatment model In a nutshell, the overall aim of DDP is to help individuals to connect to themselves and to others. In other words, DDP creates a safe space to help individuals to identify, acknowledge, and bear their interpersonal experiences and emotional pain, instead of using avoidance maneuvers, and to take the risk of relating to others in more authentic ways, beginning with the patient therapist relationship. DDP involves weekly individual therapy sessions, each lasting 45 50 minutes. It is 172 Contemporary Psychodynamic Psychotherapy time-limited treatment (12 months), with the end date set at the beginning of treatment. There are four stages of treatment and recovery, each with a specific task and underlying thematic question; successful negotiation of each stage is important for a lasting recovery (Gregory, 2004). In negotiating each stage, DDP employs three basic sets of techniques: association, attribution, and alterity. Association Association techniques aim to help patients link their experiences to their symbolic verbal capacity. Most commonly, this involves helping patients to put their recent emotionally laden social interactions into words, but can also involve exploration of creative activities, such as dreams, artwork, or poetry. As explained in the “Emotion processing” section, individuals with addictions and personality disorders commonly have an extraordinarily difficult time verbalizing specific interpersonal interactions and their emotional responses. They may be very glib when it comes to speaking generally about their experiences with other people, but when the therapist asks them to share specific instances, to put the events in sequence, and to label their emotional responses, they struggle to find the words to describe their experiences. Within DDP, symptoms of anxiety and arousal are viewed and framed as evidence of unprocessed underlying emotions, such as anger or shame, which patients are not able to identify, acknowledge, and bear. The therapist helps patients to recognize, verbalize, and tolerate such painful emotions. Through remediating emotion-processing pathways, association techniques help with the symptoms that are caused by subcortical activation and prefrontal deactivation. For patients who are well engaged in treatment, anxiety markedly improves within 2 3 months of beginning treatment. As the levels of anxiety and arousal settle down, craving for substances also diminishes. And as patients become better able to identify their emotions, they develop a greater sense of self and a more stable identity. DDP has been found to be an effective treatment for dissociative identity disorder (Chlebowski & Gregory, 2012), with association techniques being particularly helpful (Goldman & Gregory, 2010). Attribution Whereas association techniques help patients to verbalize their interpersonal experiences, attribution techniques address how patients make meaning of those experiences. Attributions of individuals with addictions, as well as those with borderline or narcissistic traits, tend to be rigid and polarized, a phenomenon that has been referred to as splitting (see section “Denial system and relationships”). Two kinds of splitting have been noted in the literature. Most commonly, splitting refers to attributions of value in which self and other (or substances) become either idealized or devalued, with little in between. The second form of splitting is one of agency rather than value. I am using the term agency to refer to the agent of change, that is, the person responsible for the consequences. Patients may sometimes see themselves as an innocent victim of others’ actions, bearing no responsibility for their Dynamic deconstructive psychotherapy for substance 173 present circumstances; the opposite may also occur, when patients see themselves as the perpetrator and the cause of all their troubles. One way in which DDP aims to deconstruct this rigid and polarized attribution system is by asking about opposite or alternative meanings within interpersonal narratives and then helping patients hold both sides of the split in their consciousness at the same time. For example, when patients are explaining how soothing and helpful cannabis is for them (idealization of the drug), the therapist might bring in the other side by asking, “In addition to its helpful aspects, do you also have concerns about your use of cannabis?” As another example, when patients are complaining about how others are criticizing their drinking (having a self-attribution as victim), the therapist might point out, “But I can guess who is your harshest critic,” and the patient usually responds by saying, “Me” (now having shifted into a self-attribution as perpetrator). Alterity Splitting involves more than a polarized attribution system. It also encompasses an intersubjective matrix in which therapists’ “buttons are pushed” by patients’ projective identifications, which can lead to therapists responding to patients in ways that reinforce the patient’s polarized attributions. For example, therapists may feel compelled to make shaming remarks to their addicted patients, which end up reinforcing patients’ devalued attributions of themselves (see section “Relational dynamics of shame”). The term alterity refers to otherness, that is, an outside and more objective perspective. Alterity techniques break through the patient’s self-reinforcing and polarized attribution system and open up new possibilities for relatedness within the patient therapist relationship (Gregory, 2005). Techniques within this category are experiential and relational in nature, involving deconstructive aspects of the patient therapist relationship in the here-andnow. Patients with severe personality pathology, including those having substance use disorders, are unable to find space for themselves in relationships. They tend to believe that in order to maintain relationships, they must conform totally to the other person’s values, motives, and opinions. Their expectation is that to do otherwise will inevitably result in being rejected and ejected from the relationship. The patients thus act as chameleons, making themselves invisible in relationships. They may also experience difficulty differentiating their own values, motives, and opinions from those of individuals with whom they are in relationship, a phenomenon that Kernberg has labeled identity diffusion (Kernberg, 1975, p. 165). When disagreement or resentment builds up within the patient toward others, it either is quelled through the use of substances; is turned against the self in the form of depression, cutting, and suicide ideation; or spills over into hostility. Alterity techniques provide a sense of safety within the patient therapist relationship by balancing caring and respect with maintenance of clear boundaries, roles, and expectations. Alterity techniques also provide space for patients to feel close to the therapist, while also being authentic, a phenomenon that can be called individuated relatedness. In order to facilitate individuated relatedness, the therapist 174 Contemporary Psychodynamic Psychotherapy attempts to be a soothing and warm presence while supporting autonomous decision-making, withholding judgment regarding the patient’s decisions (either positive or negative), and encouraging the patient to voice criticism of and disagreement with the therapist. For example, when patients are complaining about other people judging them for their use of substances, an Alterity technique is to ask the patient, “Do you ever feel that way here?” Even if the answer is no, the intervention is still therapeutic, since it gives patients the message that they do not have to play the “good patient” in their relationship with the therapist; they have space to be themselves. The question also deconstructs the patient’s expectation that the therapist will be harsh and judgmental and thus opens up new possibilities for relationships, strengthening the patient’s sense of trust. In process research, the use of alterity techniques has been found to be strongly correlated with improvement in social functioning (Goldman & Gregory, 2010). Conclusion As can be understood from the above summary of DDP, this treatment model can be considered as having both unique and common elements with other psychoanalytically oriented therapies, differing more in emphasis than in absolutes. The overall treatment philosophy of DDP is less authoritative and interpretative than most psychodynamic therapies, leaving it to the patient to be the final arbitrator of meaning and direction. There is a strong emphasis on helping patients to identify their emotions while recounting the details of specific social interactions, to create complex meanings to their experiences, to mourn their own and others’ limitations, and to experience a novel and deconstructive relationship with their therapist as important components of the healing process. Each of the three sets of techniques, that is, association, attribution, and alterity, helps to treat different aspects of the psychopathology and dynamic underpinnings of addiction and personality disorders, synergizing to build selfawareness and integration toward a long-lasting recovery. An updated version of the DDP treatment manual is available (at no cost) at www.upstate.edu/ddp. Other training materials are also available on the website, including video-recorded lectures and an interactive web-based training module. References Chlebowski, S. M., & Gregory, R. J. (2012). Three cases of dissociative identity disorder and co-occurring borderline personality disorder treated with dynamic deconstructive psychotherapy. American Journal of Psychotherapy, 66, 165 180. Derrida, J. (2004). Deconstruction and the other. In R. Kearney (Ed.), Debates in continental philosophy (pp. 139 156). New York: Fordham University Press. Goldman, G. A., & Gregory, R. J. (2009). Preliminary relationships between adherence and outcome in dynamic deconstructive psychotherapy. Psychotherapy: Theory, Research, Practice, Training, 46, 480 485. Dynamic deconstructive psychotherapy for substance 175 Goldman, G. A., & Gregory, R. J. (2010). Relationships between techniques and outcomes for borderline personality disorder. American Journal of Psychotherapy, 64, 359 371. Gregory, R. J. (2004). Thematic stages of recovery in the treatment of borderline personality disorder. American Journal of Psychotherapy, 58, 335 348. Gregory, R. J. (2005). The deconstructive experience. American Journal of Psychotherapy, 59, 295 305. Gregory, R. J., Chlebowski, S., Kang, D., Remen, A. L., Soderberg, M. G., Stepkovitch, J., & Virk, S. (2008). A controlled trial of psychodynamic psychotherapy for co-occurring borderline personality disorder and alcohol use disorder. Psychotherapy: Theory, Research, Practice, Training, 45, 28 41. Gregory, R. J., Delucia-Deranja, E., & Mogle, J. A. (2010). Dynamic deconstructive psychotherapy versus optimized community care for borderline personality disorder cooccurring with alcohol use disorders: 30-month follow-up. Journal of Nervous and Mental Disease, 198, 292 298. Gregory, R. J., & Remen, A. L. (2008). A manual-based psychodynamic therapy for treatment-resistant borderline personality disorder. Psychotherapy: Theory, Research, Practice, Training, 45(1), 15 27. Gregory, R. J., & Sachdeva, S. (2016). Naturalistic outcomes of evidence-based therapies for borderline personality disorder at a medical university clinic. American Journal of Psychotherapy, 70, 167 184. Johnson, B. (1993). A developmental model of addictions, and its relationship to the twelve step program of Alcoholics Anonymous. Journal of Substance Abuse Treatment, 10, 23 34. Kernberg, O. F. (1975). Borderline conditions and pathological narcissism. New York: Jason Aronson. Kohut, H. (1995). The analysis of the self. Monograph series of the psychoanalytic study of the child, No. 4. Madison, CT: International Universities Press. Lieberman, M. D., Eisenberger, N. I., Crockett, M. J., Tom, S. M., Pfeifer, J. H., & Way, B. M. (2007). Putting feelings into words: Affect labeling disrupts amygdala activity in response to affective stimuli. Psychological Science, 18, 421 428. Moles, A., Kieffer, B. L., & D’Amato, F. R. (2004). Deficit in attachment behavior in mice lacking the µ-opioid receptor gene. Science, 304, 1983 1986. New, A. S., Perez-Rodriguez, M., & Ripoll, L. H. (2012). Neuroimaging and borderline personality disorder. Psychiatric Annals, 42, 65 71. Ochsner, K. N., Knierim, K., Ludlow, D. H., Hanelin, J., Ramachandran, T., Glover, G., & Mackey, S. (2004). Reflecting upon feelings: An fMRI study of neural systems supporting the attribution of emotion to self and other. Journal of Cognitive Neuroscience, 16, 1746 1772. Tragesser, S. L., Trull, T. J., Sher, K. J., & Park, A. (2008). Drinking motives as mediators in the relation between personality disorder symptoms and alcohol use disorder. Journal of Personality Disorders, 22, 525 537. Waldrop, A. E., Back, S. E., Verduin, M. L., & Brady, K. T. (2007). Triggers for cocaine and alcohol use in the presence and absence of posttraumatic stress disorder. Addictive Behaviors, 32, 634 639. Winnicott, D. W. (1953). Transitional objects and transitional phenomena; a study of the first not-me possession. International Journal of Psycho-Analysis, 34, 89 97. Zanarini, M. C., Frankenburg, F. R., Hennen, J., Reich, D. B., & Silk, K. R. (2004). Axis I comorbidity in patients with borderline personality disorder: 6-year follow-up and prediction of time to remission. American Journal of Psychiatry, 161, 2108 2114. Psychosis and individual psychodynamic psychotherapy 12 Bent Rosenbaum1,2 1 Institute of Psychology, University of Copenhagen, Denmark, 2Head of Psychotherapy Research, Psychiatric Center Copenhagen, Clinic of Psychotherapy More than 100 years after the publication of the first cases of psychoanalytic psychotherapy of patients with psychosis (Bertschinger & Allen, 1916; Bjerre, 1912; Waelder, 1925), no uniform treatment method has achieved the status of being considered the psychodynamic treatment of choice for individuals with psychosis. Such uniformity may, however, not have been expected, since psychoanalytic psychotherapy is directed at the person as a whole—an emphasis on the unique history, subjectivity, and psychological complexity of each individual. In the period from World War I to the decade after World War II, investigations of psychotherapy of psychosis (mainly schizophrenia) were presented as case descriptions and as retrospective studies of small groups without any follow-up after termination of therapy (Beck, 1952; Federn, 1953; Sechehaye, 1950). From the 1960s a number of systematized comparative studies were carried through, and some of them demonstrated a positive effect by adding individual psychotherapy to treatment as usual (Frank & Gunderson, 1990; Karon & VandenBos, 1981; Sjöström, 1985). Most of the published case studies after World War II were long-term therapies with chronic psychosis patients; however, successful short-term cases also surfaced (Beck, 1952; Donelly, 1966). A multitude of guidelines appeared, most of them of great value to therapists, who could apply an array of recommendations from experts to their own patients (e.g., Arieti, 1974; Federn, 1953; Fromm-Reichmann, 1959; Gunderson & Mosher, 1975; Searles, 1965), but these guidelines were never systematized and tested in empirical trials. Thus the generalizability of such recommendations was neither confirmed nor disconfirmed, particularly with respect to the spectrum of psychosis and varying pathogenic courses. The term psychodynamic psychotherapy of psychosis was conceived of as referring to a broad, inclusive, and integrative form of modified psychoanalytic psychotherapy, forming the background to the comparative studies of psychotherapy of schizophrenia (Summers & Rosenbaum, 2013) or studies in which intervention effect size could be calculated (Gottdiener & Haslam, 2002). In the 1990s devaluing reviews of psychodynamic psychotherapy for psychosis appeared in major psychiatric journals (e.g., Lehman & Steinwachs, 1998). Thereafter, only one prospective comparative study has been published (Harder, Koester, Valbak, & Rosenbaum, 2014; Rosenbaum, Harder, & Knudsen, 2012), which happened to demonstrate advantages of adding individual psychodynamic psychotherapy to treatment as usual. Contemporary Psychodynamic Psychotherapy. DOI: https://doi.org/10.1016/B978-0-12-813373-6.00012-X © 2019 Elsevier Inc. All rights reserved. 178 Contemporary Psychodynamic Psychotherapy One common denominator of the psychodynamic approach is the view of psychosis as states of mind resulting from psychic development and based in a mindbrain dialectic, which is supported by four decades of mother infant observation studies (Stern, 1985, 1994) and developmental research addressing symbolic integration and psychic stability (Harder & Rosenbaum, 2015). The development of psychosis encompasses several unconscious structural preconditions. This includes disturbed ego functions, which refers to withdrawal of interest and the psychic (drive) investment in the painfully perceived world, often characterized by experiences of trauma (de Masi, 2009; Kirshner, 2015; Read, Bruce, Moskowitz, & Connolly, 2001; Read & Ross, 2003), ego fragmentation, and blurred ego boundaries (Frosch, 1983; Robbins, 1993). These disturbances may lead to narcissistic isolation and incoherent thinking without stable goals and perspectives. Lack of capacity for repression is another precondition, implying an inability to protect the psychic apparatus from perceptions from outside and sensations, thoughts, and emotions from inside. The outcome of this lack of repression may be a mind overwhelmed by strong anxiety, rage, desperation, and hyperreflectivity (Sass, 2014). A third precondition is disturbed symbol formation, which includes difficulties in distinguishing what is universal or general from what is special or particular and in forming illusions temporarily. Furthermore, there are difficulties in understanding that something may have a meaning both for “me” and for “you” and that its meaning may not be exactly the same for the two of us. Related to this are challenges in understanding that “I” and “you” are both separated and closely linked subjects, in understanding that the content of the communication has to be validated consensually, and in considering the mind of the other and the minds of the collective. A final precondition concerns disturbed attachment patterns, especially dismissiveavoidant and disorganized attachment. Severe forms of disorganized attachment have been hypothesized to be involved in several areas of disturbed development related to psychosis, such as disturbed affect regulation, difficulties with interpersonal relationships, fragmentation of self-experience, and serious impairments in mentalization or metacognition, as well as the specific psychotic symptoms of delusions and hallucinations (Harder & Rosenbaum, 2015) These phenomena should always be in the mind of the therapist. They constitute the theoretical basis on which the (hopefully) creative part of the therapist’s experience will form the preferred technique with words and nonverbal attitudes that suit the specific moment of the intervention. It is also the transformation from theoretical thinking to uttered and nonuttered signifiers that may distinguish routine and inspired interventions—be they clarifications, confrontations, or interpretations. Description of treatment approach Supportive psychodynamic psychotherapy (SPP) for psychosis is founded upon several core principles, which include the following: 1. A stable, yet flexible frame 2. The therapist’s attention to countertransference Psychosis and individual psychodynamic psychotherapy 179 3. Clarification of the patient’s subjective experience, emotions, and interpersonal world, including efforts to give psychotic symptoms an understandable context in internal and external object relationships 4. Clear communication and attention to divergent perspectives 5. A supportive attitude on the part of the therapist, with an emphasis on clarifying and understanding interventions and including in-the-moment psychodynamic psychoeducation on the human condition in general (communication, habits, daily cultural life experiences, etc.) The frame and setting of individual psychodynamic psychotherapy is defined by (1) its stability and regularity, (2) the therapist’s capacity for empathy and longterm interest in the other person’s psychic growth, and (3) the therapist’s capacity for containing misunderstandings, aggression, and hopelessness with integrity, responsiveness, and creativity. Moreover, in relation to the latter point, the frame is supported by the therapist’s capacity to clarify the dynamics of the interpersonal relations in the therapeutic sessions (transference, broadly speaking) and outside the therapy without creating an atmosphere of polarization. The setting should not be too rigid, especially during times of psychotic crisis. Length of sessions will vary; some sessions will contain a more conversational atmosphere (but without irrelevant statements from the therapist’s side), while in other sessions the therapist may be more silent, letting the patient take the lead. In some sessions the patient cannot sit still and has to move around in the room, and the therapist has to find ways to explore the reasons for this and at the same time has to calm the patient down. Altogether, the therapist’s attitude must vary according to the condition of the patient. With facial expression, gestures, voice, attitude of informality, and general demeanor, the therapist must do whatever is in his or her power to remove the fear that is automatically aroused by the fact that a human being (the therapist) wants to establish contact with a person in psychosis. Some therapists also suggest that it may be an advantage to see significant members of the family if the patient permits it. Such meetings could take the form of the psychotherapeutically oriented need-adapted treatment (Alanen, Räkköläinen, Laakso, Rasimus, & Kaljonen, 1986) in which all participants may have a chance to openly state their feelings and opinions on the situation here-and-now and intermediary conclusions may be reached in the presence and with confirmation of the patient. The risk of countertransference reactions is greater in treating persons in psychotic states of mind than in treatment with persons with neurotic and borderline states of mind (although the latter category of patients often creates great countertransference problems influencing the therapy). Fromm-Reichmann (1959, p. 215) formulates the issues along these lines: “Severe anxiety, withdrawn loneliness, aggressive hatred and lack of improvement of the psychotic patient may be contagious to therapists.” The disturbed symbol formation of the patient (see above) makes it difficult for the therapist to make proper use of his or her countertransference feelings. First, they usually appear too late in the therapist’s consciousness to be handled properly (starting as pure unconscious phenomena); second, the ways of transforming one’s countertransference confusion, anger, and anxiety are inhibited by the patient’s communication difficulties. 180 Contemporary Psychodynamic Psychotherapy During the entire course of therapy a supportive psychodynamic attitude should be embedded in the style of the therapist. The following are some principles: 1. The patient’s enunciations—regardless of their “normality” or “pathology”—are conceived as subjective truths that shall be clarified and explored rather than corrected. 2. Even though there is always more to the patient’s problem than what is obvious, commonsensical, and capable of being simply unlearned, the content of the therapy should be focused and with references as clear as possible to the issues talked about in the dialogue. The therapist is aware of the polysemous and associative nature of language but is at the same time aware that polysemy and too many associations may be confusing to the patient. 3. The therapist must help the patient to make sense of and better understand his or her feelings, attitudes, and subjective intentions in concrete interpersonal relationships. Often, clarifying step by step in the interactions may be helpful in understanding the interpersonal dynamics (e.g., what goes on and what may have been avoided), while at other times, the step-by-step method may lead to too much information and be undigestible at that time. 4. Diverging viewpoints between patient and therapist should never develop into entrenched positions, offensive defensive fixations, or any other forms of polarization. 5. An ongoing task of the therapist is to structure the meeting with the patient to ensure that the patient feels listened to. This in turn may, by means of increasing internal safety, help the patient to start listening to not only the therapist’s viewpoints, but also to the patient’s own. 6. The aim of securing structure is to counterbalance dissolution and breakdown and counterbalance the patient’s negative and self-denigrating attitude. 7. Finally, the therapist’s attitude should encompass—when necessary and in order to contain the patient’s painful state of mind—the use of modified psychoanalytic techniques such as clarifications, affirmations, and suggestions; maximizing adaptive strategies and encouraging patient activities; and helping the patient to understand how psychotic mechanisms work psychologically in the individual and in specific interactions with others and how other people might be expected to react (with commonsense reactions). This kind of intervention may be labeled in-the-moment psychodynamic psychoeducation. The initial sessions The main objectives of the initial phase are to forge a constructive working relationship with the patient, to develop a sense of the patient’s history with both its traumatic and helpful events, and to situate the patient’s symptoms in the context of his or her subjective experience and social functioning. It is important in the first meeting to persuade the patient that the therapist is interested in understanding the patient as a human being and as a person with a history that can be meaningfully connected with the patient’s present painful situation. Could you tell me about yourself in such a way that I can get a picture of you as the person you are? I am interested in hearing what you feel is characteristic for the way you see and think about yourself and the problems in your life as they relate to the course of your life. Psychosis and individual psychodynamic psychotherapy 181 In a collaborative atmosphere the therapist and patient develop a narrative biography of the patient’s life, including its normal and pathological aspects, according to the ideas of developmental psychopathology (Cicchetti & Cohen, 2006). This includes hypotheses about the dynamics of the patient’s current interpersonal problems, associated pathological grieving processes (e.g., loss of friends, loss of daily functions, loss of safety), and defensive experiences due to anxiety. Useful questions could include the following: What do you find to be your most important problems? Where do you think your problems stem from? What situation(s) might worsen your problems or symptoms, and what may ease them? Who or what do you think could help to solve the problems? Tell me what, in your opinion, led to this situation in which you conclude that you need help from other persons, professionals that you do not know. Did you feel it was you who came to this conclusion or did you feel that others’ conclusions were imposed on you? Drawing a life-line with major significant events (objectively) described on the one side (i.e., what happened seen from a third-person perspective) and (subjectively) described on the other side of the line (e.g., “This memory—how do you think you experienced it when it happened and how do you experience it today? What does it mean for you in your daily life?”). These objectively and subjectively described events may function as guidelines for the understanding of the internal object relations that structure and color the patient’s understanding of what happens in his or her daily life and in the transference. Symptoms should also be investigated and understood in the context of the patient’s developmental trajectory. When exploring hallucinations of voices, for instance, the therapist might ask questions such as the following: When did the voices start speaking to you? What did they say? Was their message meaningful to you? What happened in your life when the voices started? Do you find any connections between those life events and the message of the voices? Were the voices hostile from the beginning or did they begin their intrusion with kind messages—maybe even useful for you? What was happening in your life when the voices grew more hostile and persecuting? Such questions are not meant to correct the patient’s hallucinatory modes of perceiving the world. Rather, they are necessary clarifications in order to understand the dynamics of the hallucinations (as potentially reflecting the dynamics of internal and external object relations). These clarifications are intended not only to inform the imagination of the therapist, but also to slowly promote the patient’s understanding of how the hallucinations are psychic phenomena embedded in previously inscribed experiences of a more or less traumatic kind. Thus the aim of such an investigation differs from that of an ordinary psychiatric diagnostic interview. It is important in the initial sessions to give the patient a feeling that the therapist also has an eye for and is genuinely interested in creative aspects of life (e.g., 182 Contemporary Psychodynamic Psychotherapy music, dance, painting, sport, theater, film, literature) as well as the human emotional repertoire consisting of sadness, isolation, aggression, suicidal impulses, and other self-destructive and violent thoughts and acts. The therapist would want to plant a seed in the patient’s mind that the therapist is prepared to help the patient avoid self-destructive aspects being carried out, even though they may be felt as meaningful for the patient at the time when these aspects were dominating daily life. It is equally important that the therapist, together with the patient, clarify the possibilities for—and the obstacles against—the creation of a therapeutic alliance with some degree of stability. Different openings can be used by the therapist, for example, with questions like the following: What can lead you to not attend our scheduled meetings? Are there topics that you in this moment feel will cause so much aversion in you that they may be a reason for you to stay away from being helped by psychotherapy? What can I do to help you overcoming negative feelings about coming to the sessions? Of course, it is countertherapeutic to ask all these questions in one intervening statement. When the therapist has posed a question that he or she believes is of importance, the answers should be explored, the depth of exploration depending on the patient’s state of mind and the therapist’s skills. The initial phase thus involves the development of a creative way of working that involves the therapist’s responsiveness to the patient’s state of mind, such as becoming more exploratory if the patient can tolerate this. Such explorations depend on the therapist’s experience, expertise, and intuition. Different metaphors may be employed as working tools to make the patient feel safe enough to begin a journey, bringing hope into the patient’s mental life. Agreement and disagreement about what is said in the communication, what the words mean, and what the statements are used for are key elements during the first phase of the therapy. In this phase the therapist always has to look for opportunities to join with, rather than confront, the patient. Disagreement, particularly in the early stages of treatment, tends to have relationship-ending connotations and often leads to premature cessation of treatment (Robbins, 1993). Confrontations, therefore, belong more to the middle phase of the therapy. The middle phase As the phase of treatment involving more focused work on symptoms, conflicts, and self-understanding, the middle phase of psychodynamic psychotherapy with individuals with psychosis may be particularly difficult. Finding directions in the open ocean, where neither the shores of departure nor the shores of arrival can be seen and located, is an immense challenge—for both therapists and patients. One major task is to relieve the patient of the experiences of imminent crisis by advising and guiding the patient in a concrete way as to how he or she should tackle, and Psychosis and individual psychodynamic psychotherapy 183 not allow himself or herself to be governed by, the symptoms. Mastery of symptoms means being able to keep them at a distance, which implies an understanding of their function in interpersonal scenarios in which the symptoms are reinforced or attenuated. It is recommended that the therapist always clarify and analyze the symptoms within the interpersonal context (including the transference). However, timing is essential. Sometimes patients do not want to understand their symptoms within a social context. As the result of traumatic and deficient attachment experiences, resulting in feelings of not being emotionally understood, patients might just want to regard their symptoms as something foreign and painful that they should get rid of as soon as possible and as something that they do not want to talk about. This paradox of wanting to get rid of their symptoms but not knowing how to do it and, at the same time, not feeling that the therapist is trustworthy creates situations that often challenge therapists and lead to deadlocks. In such phases or moments it may be more important to downplay the exploration of psychotic experiences and anxiety-provoking conflicts and instead focus on securing the patient’s feeling of safety as much as possible in order to achieve better resocialization. Countertransference feelings become centrally important in these moments of therapy. All in all, even in situations in which major psychotic symptoms are dominating, the therapist needs to trust that development of the self can provide the patient with qualities that go beyond the effect of medication. Therapists need to trust in the existence of some normally functioning aspects to the patient’s personality (Bion, 1957; Freud, 1940; Lotterman, 2015; Summers & Martindale, 2013) and support these more sane parts in a consistent and straightforward manner. The therapist’s aim is to help the patient to expand the sane attitudes and thoughts and diminish the psychotic functioning. A brief vignette may illustrate: A patient came to the session in a severe, hallucinated state of mind in which she walked around in the consultation room, restless and anxious and without making any eye contact. She came to the session saying (in Danish), “I feel blue,” “They step on me,” “They eat me,” “They walk away and walk on me.” The therapist listened in a calming way, saying softly, “It sounds awful. I will help you and protect you. In this room, you can feel safe.” After half an hour, the patient calmed down and sat in the chair, and the therapist asked the patient to tell what had happened to her. She told (although in fragments) how she had been driving her car (which was a small Morris Mascott) behind a huge truck. Suddenly, a fantasy overwhelmed her that the truck contained the bodies of hundreds dead pigs that fell out of the truck and buried her. She managed to park her car near the therapist’s consultation room but had to walk a few hundred meters. Walking on the street, she saw a man carrying a big, black plastic bag, and she immediately believed that this bag contained her two children chopped into small pieces. After this terrifying experience, she looked at the street sign and felt chaos inside herself and as if the world had broken down. In further exploration by the therapist of the event, it appeared that the name on the street sign she had seen had been perceived in a fragmented way. The sentences she had uttered all stemmed from the name of the street, and the patient was to a certain extent calmed down further by that information. The therapist did not in this session go further in his understanding of 184 Contemporary Psychodynamic Psychotherapy the event, and he intentionally avoided following up with an interpretative association connecting the patient’s sentences to the fear the patient had shown in a previous session about the raising of her children, whom she often felt concretely invaded her body. The vignette illustrates how it often may be important for the therapist to manage feelings associated with functioning primarily in a basic affect regulation capacity and to monitor the extent and depth of the interpretation that could be offered. (I am here tacitly assuming that the therapist always has at least some possible interpretations in mind when listening to sentences or narratives of the patient.) Understanding symptoms in the light of primitive defense mechanisms and implementing one’s understanding in subsequent interventions are challenging for the psychotherapist. Nevertheless, an important intervention that may reestablish equilibrium in phases of turmoil is letting the patient feel that defense mechanisms are there to protect and help the patient in the concrete situation. Patients may then recognize that their defensive attitudes have an adaptive and psychologically valuable function in preserving the integrity of the self. Later in the middle phase of the therapy, the therapist may convey to the patient that other attitudes, even giving up some defense patterns, will be a possibility in the future. The timing for these changes should be chosen with care and should be promoted without raising unnecessary anxiety and confusion. The positive and negative sides of defense mechanisms are something that the patient will slowly become aware of in the middle phase of therapy. This may go hand in hand with the therapist helping the patient to mobilize the healthy aspects of the patient’s personality. That includes helping the patient define his or her reality in different situations of social communications, enhancing perspectives for the patient’s life, and gradually supporting available mature defense mechanisms. In short, changes in the patient’s interpersonal attitudes—more openness, more trust, more personal ideas for a social future—are signs from the patient to the therapist that the time is ripe for talking about defense mechanisms in a more nuanced way. As was stated above, confrontations belong more to the middle phase than to the first phase. Confrontation addresses something the patient does not want to accept, or it identifies the patient’s avoidance or minimization (Gabbard, 2014). The latter is of importance in the psychotherapy of psychosis. By showing what the patient avoids or how the patient goes against his or her own decisions made in previous sessions, confrontations usually open and/or underlie disagreements between patient’s and therapist’s points of view on particular situations and their underlying dynamics, for example, by saying to a patient, “By not attending the funeral of your father, you may submit to the dominance of your fear rather than go against it and pursue your feelings of progress that you have obtained through your hard work in our therapy. You have several times uttered that the gazes from your family members shall not bother you anymore, and we have together explored the reasons behind this, so why go against your own promises?” Psychosis and individual psychodynamic psychotherapy 185 Sometimes when the therapist intervenes with statements that are intended to support and help the patient, the patient may experience the therapist’s words as confusing and objectionable. The patient may even respond with anger toward the therapist for imposing on the patient statements that seem meaningless or feel harmful. Such situations demand that the therapist acknowledge that his or her words have caused an undesired state of mind in the patient, even though the words were uttered with the intention to help. SPP for psychosis follows the analytic principle of free association in that the patient’s associations are seen as paving the road for the themes and topics to be worked on in the session. In contrast to traditional psychoanalytic therapy, however, it is the therapist who structures the sessions in SPP. Thus the therapist assumes the responsibility for drawing into the sessions the disturbed dynamics that were revealed in the assessment and first phase of therapy. Further, it is the therapist’s responsibility to decide in the sessions how far and to what degree the problems can be worked through. Therapist statements such as “What we have talked about just now is of utmost importance, and I think we have come as far as we can today” may sometimes be uttered even in the middle of the session if the therapist feels that the patient has started repeating himself or herself or has become more anxious. Of course, seeking consensus about this structuring intervention is important, as is the therapist’s ability to create continuity: “Before we talked about this important topic, you introduced another topic that we should attend to . . ..” Again, the therapist’s sensitivity and listening capacity are at stake: Intervening at the right moment, with the right words, and with the appropriate, calming prosody, body movement, and facial mimicry is sine qua non in the psychotherapy with patients in psychotic states of mind. Termination phase The termination phase of SPP involves a review and synthesis of the work accomplished during the treatment. Three to six months before ending therapy, the therapist should summarize what has been worked with in the treatment thus far. Differentiating and synthesizing the many elements of a long-lasting therapy are difficult for a person who is still influenced by the transference and reminiscences of psychotic experiences. Therefore the therapist may help in contrasting memories of the patient’s general appearance and mental condition from the beginning of therapy with how the patient appears now after his or her psychic development. Trajectories of the patient’s positive development should be emphasized. After the patient’s responses to this, the therapist may add that there are remaining problems that the patient may still have to deal with, think about, and encounter in different forms also after termination. Therapist and patient must allow for time to talk about how the patient might be able to handle remaining symptoms, considering which strategies may be used and why and what precautions might be taken and why. 186 Contemporary Psychodynamic Psychotherapy The therapist should also give the patient the possibility of commenting on the therapist’s style and ways of being helpful and nonhelpful, ways of listening, and so on. The patient who has stayed in therapy to its end will obviously be hesitant to criticize the therapist. With a sense of warmth the therapist may highlight some blunders that may have affected the patient and as a result of which the therapist has learned something from the patient. I believe that the person who has lived through psychosis and stayed in therapy will experience the separation-individuation process as overwhelming and insupportable. The reasons for this are many. First, the states of schizophrenic psychosis reflect a life in symbiotic states of mind in which the function of the symbolic order fails to overwrite the imaginary order (Fink, 1997, pp. 87 90). The person’s thoughts and senses are caught in a projection of his or her inner world in which they mirror and identify themselves in persecutory and confusional ways (projective identification). The ways out of this symbiotic prison—or claustrum as Meltzer (1994) calls it—toward separation-individuation imply increasing functioning of volitional self-direction, volitional direction of thought and attention (Shapiro, 2000), and the dominance of the capacity of the autobiographical self to engage in the functions of the extended consciousness (Damasio, 1999).1 The work of separation-individuation can be helped immensely when future social circumstances in the patient’s life are drawn to the field of attention: finding work places with a good leadership, going into an educational course that is considered attractive, becoming part of circles with boyfriends and girlfriends who have normal-life social encounters, finding supportive spouses, experiencing positive changes in one’s own family, and so on. Empirical evidence for supportive psychodynamic psychotherapy: the Danish Schizophrenia Project Despite past pessimistic attitudes toward psychodynamic psychotherapy for psychosis, many clinicians and researchers have remained cognizant of the inconclusive empirical status of this issue. Efforts to explore the role of psychodynamic therapy for psychosis have thus persisted. One such effort is the Danish Schizophrenia Project (DNS-II) (Rosenbaum et al., 2012), which compared psychodynamic psychotherapy for psychosis with standard treatment in patients with a first-episode schizophrenia spectrum disorder. The study was designed as a prospective, 1 Damasio (1999, p. 230) nicely summarizes these functions: the abilities to create helpful artifacts, consider the mind of the other, sense the minds of the collective, suffer with pain rather than just feeling pain and reacting to it, sense the possibility of death in the self and in the other, value life, construct a sense of good and of evil distinct from pleasure and pain, take into account the interests of the other and of the collective, sense beauty as opposed to just feeling pleasure, sense a discord of feelings and later a discord of abstract ideas, which is the source of the sense of truth. These functions of the extended consciousness seem to parallel the functions of the lacanian symbolic order (Fink, 1997), the prominence of which may be a measure of the phase of termination. Psychosis and individual psychodynamic psychotherapy 187 comparative, longitudinal, multisite investigation of nonselected, consecutively referred patients. Patients were treated either with SPP—a manualized form of individual psychodynamic treatment—in addition to treatment as usual or with treatment as usual alone (TaU). No preselection of patients to either of these modalities took place; the only selective factor was the home addresses of the patients. Both groups contained university/nonuniversity departments and rural/urban departments. Symptoms and functional outcomes were measured by using the Positive and Negative Syndrome Scale (PANSS) and the Global Assessment of Functioning (GAF) scale. The study included 269 admitted patients, ages 18 35 years, of whom 79% remained in the study after 2 years. The psychotherapy group (119 patients) improved significantly on measures of both PANSS and GAF scores, with large effect sizes at 2-year follow-up after inclusion. Furthermore, improvement on GAFfunction (P 5 .000) and GAFsymptom (P 5 .010) significantly favored SPP in combination with TaU over TaU alone. These differential effects remained; however, they were not sustained to a significant degree at 5-year follow-up (Harder et al. 2014). This is consistent with the findings of other comparative, 5-year follow-up investigations. While these findings indicate promise for SPP for psychosis, they provoke important questions for further inquiry: Is 2 years of active intervention too little? Are some patients helped considerably with only 2 years and others not at all, and thus, by assuming homogeneity of the group, do we lose a possible insight into the differentiated effects of the psychotherapy intervention? Summary Given the serious nature of psychosis, the field needs as many potentially helpful interventions as possible. Psychosis attacks not only the functioning of thinking, feeling, and reasoning, but also, even more so, the person’s conception of self. In the psychodynamic approach, the collaboration of therapist and patient mainly work with the person’s conception, understanding, and feelings for the patient’s self as it appears in the transference, the intersubjective relation (internal object relationship), interpersonal relation (the socially communicating self), and the development of the self toward greater dominance of symbolic integration. In spite of limitations the DNS-II study speaks in favor of including psychodynamic psychotherapy in the treatment for patients with schizophrenic first-episode psychoses. The study also contradicts the repeated cliché about overall harmful effects of psychodynamic psychotherapy. As to scientific methodology, in the end we must ask ourselves what kind of measures we will use to evaluate a good therapy. What are the features of clinical improvement, and might this not necessarily correspond with improvement in the patient’s personal life? Moreover, we should continue to determine the main contributors to these life changes—what combination of therapist abilities, situation with family and/or friends, and/or other stable social conditions? The psychodynamic 188 Contemporary Psychodynamic Psychotherapy approach also questions whether we should ignore the significance of life years from age 0 to 16 years for personality development that antecedes psychosis and the implications for the development of psychosis. These kinds of questions favor an individual and holistic approach, such as a psychodynamic approach that links past, present, and future into subjectively understandable narratives for the patient. In some European countries (Denmark, Norway, Germany), year-long courses in psychosis psychotherapy already exist, and initiatives are being taken to establish more empirical evidence for psychodynamic approaches that may help patients with psychosis in all its different phases and phenomenological appearances. References Alanen, Y. O., Räkköläinen, V., Laakso, J., Rasimus, R., & Kaljonen, A. (1986). Towards need-specifik treatment of schizophrenic psychoses. Heidelberg: Springer Verlag. Arieti, S. (1974). Interpretation of schizophrenia (2nd ed.). New York: Basic Books. Beck, A. T. (1952). Successful outpatient psychotherapy of a chronic schizophrenic with a delusion based on borrowed guilt. Psychiatry, 15, 305 312. Bertschinger, H., & Allen, C. L. (1916). Processes of recovery in schizophrenics. Psychoanalytic Review, 3(2), 176 188. Bion, W. R. (1957). Differentiation of the psychotic from the non-psychotic personalities. International Journal of Psychoanalysis, 38, 266 275. Bjerre, P. (1912). In Sondernabdruck aus dem Jahrbuch für Psychoanalytische undPsychopathologische Forschungen (Ed.), Zur Radikalbehandlung der chronischen Paranoia (Vol. 3). Leipzig: Franz Deuticke. Cicchetti, D., & Cohen, J. D. (Eds.), (2006). Developmental psychopathology (2nd ed.). New York: Wiley & Sons. Damasio, A. (1999). The feeling of what happens. London: Heinemann. de Masi, F. (2009). Vulnerability to psychosis: A psychoanalytic study of the nature and therapy of the psychotic state. London: Karnac. Donelly, J. (1966). Short-term therapy in schizophrenia. In G. L. Usdin (Ed.), Psychoneurosis and schizophrenia (pp. 141 154). Philadelphia: J.P. Lippincott Co, Ch. 12. Federn, P. (1953). On the treatment of psychosis. In P. Federn (Ed.), Ego psychology and psychosis (pp. 117 282). London: Imago Publ, Part II. Fink, B. (1997). A clinical introduction to Lacanian psychoanalysis. Cambridge, MA: Harvard University Press. Frank, A. F., & Gunderson, J. G. (1990). The role of the therapeutic alliance in the treatment of schizophrenia: Relationship to course and outcome. Archives of General Psychiatry, 47, 228 236. Freud, S. (1940). An outline of psychoanalysis. Standard Edition of the Complete Psychological Works of Sigmund Freud, 14(23), 141 207. Fromm-Reichmann, F. (1959). On schizophrenia. In F. Fromm-Reichmann (Ed.), Psychoanalysis and psychotherapy (pp. 117 276). Chicago: University of Chicago Press, Chap. III. Frosch, J. (1983). The psychotic process. New York: International Universities Press. Psychosis and individual psychodynamic psychotherapy 189 Gabbard, G. O. (2014). Psychodynamic psychiatry in clinical practice (5th ed.). Washington, DC: American Psychiatric Publishing. Gottdiener, W. H., & Haslam, N. (2002). The benefits of individual psychotherapy for people diagnosed with schizophrenia: A meta-analytic review. Ethical Human Sciences and Services, 4(3), 163 187. Gunderson, J. G., & Mosher, L. R. (Eds.), (1975). Psychotherapy of schizophrenia. New York: Jason Aronson. Harder, S., Koester, A., Valbak, K., & Rosenbaum, B. (2014). Five-year follow-up of supportive psychodynamic psychotherapy in first-episode psychosis: Long-term outcome in social functioning. Psychiatry: Interpersonal and Biological Processes, 77(2), 155 168. Harder, S., & Rosenbaum, B. (2015). Psychosis. In P. Luyten, et al. (Eds.), Handbook of psychodynamic approaches to psychopathology (pp. 259 286). New York: Guilford Press. Karon, B. P., & VandenBos, G. R. (1981). Psychotherapy of schizophrenia: The treatment of choice. Northvale, NJ: Jason Aronson. Kirshner, L. (2015). Trauma and psychosis: A review and framework for psychoanalytic understanding. International Forum for Psychoanalysis, 24(4), 216 224. Lehman, A. F., & Steinwachs, D. M. (1998). Translating research into practice: The schizophrenia patient outcomes research team (PORT) treatment recommendations. Schizophrenia Bulletin, 24, 1 10. Lotterman, A. (2015). Psychotherapy for people diagnosed with schizophrenia. London: Routledge. Read, J., Bruce, D. P., Moskowitz, A., & Connolly, J. (2001). The contribution of early traumatic events to schizophrenia in some patients: A traumagenic neurodevelopmental model. Psychiatry, 64(4), 319 345. Read, J., & Ross, C. A. (2003). Psychological trauma and psychosis. Journal of the American Academy of Psychoanalytic Dynamic Psychiatry, 31(1), 247 268. Robbins, M. (1993). Experiences of schizophrenia: An integration of the personal, scientific and therapeutic. New York: Guilford Press. Rosenbaum, B., Harder, S., Knudsen, P., Køster, A., Lajer, M., Lindhardt, A., . . . Winther, G. (2012). Supportive psychodynamic psychotherapy versus treatment as usual for first episode psychosis: Two-year outcome. Psychiatry: Interpersonal and Biological Processes, 75, 331 341. Sass, L. (2014). Self-disturbance and schizophrenia: Structure, specificity, pathogenesis. Schizophrenia Research, 152, 5 11. Searles, H. F. (1965). Collected papers on schizophrenia and related subjects. New York: International Universities Press. Sechehaye, M. (1950). Journal d’une schizophre`ne. Paris: Presses universitaires de France. Shapiro, D. (2000). Dynamics of character. New York: Basic Books. Sjöström, R. (1985). Effects of psychotherapy in schizophrenia: A retrospective study. Acta Psychiatrica Scandinavica, 71, 513 522. Stern, D. (1985). The interpersonal world of the infant. New York: Basic Books. Stern, D. (1994). One way to build a clinical relevant baby. Infant Mental Health Journal, 15 (1), 9 25. Summers, A., & Martindale, B. (2013). Using psychodynamic principles in formulation in everyday practice. Advances in Psychiatric Treatment, 19, 203 211. Summers, A., & Rosenbaum, B. (2013). Psychodynamic psychotherapy for psychosis: empirical evidence. In J. Read, et al. (Eds.), Models of Madness (2nd ed., pp. 336 344). London: Routledge. Waelder, R. (1925). The psychoses: Their mechanisms and accessibility to influence. International Journal of Psychoanalysis, 6, 254 281. Psychodynamic therapy in patients with somatic symptom disorder 13 Patrick Luyten1,2, Celine De Meulemeester1 and Peter Fonagy2 1 Faculty of Psychology and Educational Sciences, University of Leuven, Leuven, Belgium, 2 Research Department of Clinical, Educational and Health Psychology, University College London, London, United Kingdom People with persisting somatic complaints comprise a large subset of patients across the different tiers of healthcare. A recent meta-analysis based on 32 studies in 24 countries (total N 5 70,085 patients) estimated that up to 50% of patients in primary care present with at least one somatic complaint that cannot be readily explained by medical causes, with approximately 30% of patients fulfilling criteria for somatic symptom disorder (Haller, Cramer, Lauche, & Dobos, 2015). In tertiary care, up to 9% of patients present with more than one type of somatic symptom disorder (Bass & May, 2002). There is a wide variety of functional somatic symptoms affecting the different body systems. Almost every medical specialty has defined syndromes in which patients present with a particular set of symptoms (see Table 13.1) (Wessely & White, 2004). Evidence is amassing that functional somatic disorders (FSDs) are part of a spectrum of functional somatic syndromes with common genetic, pathophysiological, and psychological mechanisms. Studies have suggested high levels of comorbidity and familial coaggregation among the syndromes (Aggarwal, McBeth, Zakrzewska, Lunt, & Macfarlane, 2006). Furthermore, their high comorbidity with depression and anxiety and similarities in terms of stress response have led to the assumption that they are part of a spectrum of affective disorders (Hudson et al., 2003). This chapter first provides a contemporary attachment perspective to understanding patients with FSDs and empirical evidence supporting this perspective. Next, it discusses how this understanding can be translated into a systematic treatment approach. We provide a clinical example of the systematic treatment approach and end with a discussion of future areas for research and clinical practice. Contemporary Psychodynamic Psychotherapy. DOI: https://doi.org/10.1016/B978-0-12-813373-6.00013-1 © 2019 Elsevier Inc. All rights reserved. 192 Contemporary Psychodynamic Psychotherapy Table 13.1 Examples of functional somatic symptoms in different medical specialties. Type of functional somatic symptoms Medical specialty Chronic fatigue syndrome Fibromyalgia, chronic widespread pain, back pain Irritable bowel syndrome, dyspepsia Chronic pelvic pain Noncardiac chest pain, functional palpitations Hyperventilation syndrome Tension headache, migraine, functional neurological disorder, conversion disorder, somatosensory disorder Urethral syndrome, interstitial cystitis Dermatitis, inflammatory dermatosis Laryngospasm, pharyngospasm, temporomandibular syndrome, bruxism Multiple chemical sensitivity Internal medicine Rheumatology Gastroenterology Gynecology Cardiology Respiratory medicine Neurology Urology Dermatology Otolaryngology Allergy/immunology An attachment and mentalizing approach to FSDs Assessment and heterogeneity of FSDs Patients with FSDs are very heterogeneous in terms of the role of both psychological and biological factors in their symptoms. Hence, any generalization about the role of biological and psychological factors in these patients is clinically unproductive. We have learned to refrain from trying to provide such answers, which are always based on group research. Indeed, in any given case it is often quite difficult, if not impossible, to gauge the respective role of these factors, particularly as the clinician’s knowledge of the patient and his or her condition is typically very limited at the start of any treatment. As treatment progresses, the picture typically becomes clearer, and then this question may be—and typically is—revisited. In this respect, it is always wise to make sure the patient has undergone thorough medical screening. Similarly, for most patients a detailed psychological assessment is indicated, focusing on possible problems related to attachment issues; (embodied) mentalizing, that is, the capacity to reflect on their own (embodied) self and others; and epistemic trust, the capacity to trust others as a source of knowledge, including the knowledge that the clinician offers concerning the patient’s own presenting problems. This assessment determines to a large extent the therapeutic options for the patient and the subsequent focus of treatment. Attachment and emotion regulation in FSDs Impairments in stress and emotion regulation, typically resulting from complex interactions among biological and environmental factors, are a key feature in FSDs (Tak & Rosmalen, 2010). Many FSD patients have experienced chronic Psychodynamic therapy in patients with somatic symptom disorder 193 overburdening of the stress system as a result of physical and/or psychological stress and conflict, leading to a state of allostatic load (McEwen, 2007) that disrupts the dynamic equilibrium (allostasis) typical of the stress regulation system and neurobiological systems associated with the stress response. These systems mainly include the immune and pain-regulating systems and associated biomediators. Physical and psychological stressors are often closely intertwined, as is demonstrated by the finding that many patients with FSDs show a pattern of overactivity, which chronically overburdens the stress system (Luyten, Van Houdenhove, Lemma, Target, & Fonagy, 2013; Van Houdenhove & Luyten, 2008). The emergence of pain and fatigue-related complaints leads to additional stress and conflict, not least because these patients often encounter invalidating responses from others. This leads in turn to the patients experiencing feelings of inferiority and being a failure. A vicious cycle ensues, characterized by increasing emotional distress and conflict; the individual begins to function in a constant state of fight-or-flight. This is why any understanding of the origins of FSDs that does not take into consideration the roles and function of the attachment system is, in our view, problematic. The attachment system is a biobehavioral system that is activated in response to distress and thus plays a key role in restoring allostasis, the dynamic equilibrium that characterizes biological functioning (McEwen, 2007). In normative development, activation of the attachment system leads the individual to seek proximity to attachment figures. When attachment figures are available and responsive, this typically leads to effective downregulation of distress (see Fig. 13.1). This experience is gradually generalized, leading to feelings of agency and efficacy in the face of adversity based on the underlying belief that others will be there to provide support, care, and validation in times of need. Normative stress regulation thus always involves a process of coregulation in relation to attachment figures (Diamond, Stovall-McClough, Clarkin, & Levy, 2003; Sbarra & Hazan, 2008). The neurobiology of the process of coregulation is increasingly understood; it mainly involves the mesocorticolimbic dopaminergic reward system, which underlies the attachment system. This system is responsible not (A) Downregulation of distress via the normally functioning attachment system (B) Hyperactivation of the attachment system in the context of FSD Distress/ fear Distress/ fear Exposure to threat – Activation of attachment – Adverse emotional experience Activation of attachment Downregulation of emotions Proximity seeking Proximity seeking Figure 13.1 The relationship between the attachment and stress regulation systems. 194 Contemporary Psychodynamic Psychotherapy only for the rewarding nature of attachment relationships, but also for the downregulation of neuroendocrine stress regulation systems, including the hypothalamic-pituitary-adrenal axis and the sympathetic nervous system (Luyten & Fonagy, 2018). Persistent somatic complaints make the normative downregulation of distress effectively impossible, as there simply is no (or very little) relief possible from these conditions. This typically leads to a breakdown of the normative stress regulation process, even in individuals who were securely attached before the onset of their complaints. The patient is forced to shift to the use of so-called secondary attachment strategies, that is, affect regulation strategies that are used when the primary or normative stress regulation strategy fails (Mikulincer & Shaver, 2007). There are two main secondary attachment strategies. The first involves hyperactivation of the attachment system. This involves anxious efforts to find understanding, support, and relief and is expressed in increasingly demanding, clinging, and claiming behavior (Waller & Scheidt, 2006). The second involves deactivation of the attachment system; attachment needs are denied, and the patient resorts to a stance emphasizing autonomy, independence, and strength (Cassidy & Kobak, 1988; Mikulincer & Shaver, 2007). This strategy is often expressed in high levels of self-critical perfectionism, persistence, overactivity, and all-or-nothing behavior (Luyten et al., 2011). Although secondary attachment strategies may bring some temporary relief, they are associated with high interpersonal and metabolic costs. Becoming increasingly demanding characteristically leads to frustration with and often rejection by others, confirming the patient’s fear that others will abandon or reject him or her. This self-fulfilling prophecy may have a disastrous impact both on the patient’s intimate relationships and on relationships with health professionals. As a result, allostatic load further increases, which further increases these patients’ tendency to cling on to others in an attempt to find support, relief, and understanding from them (Maunder & Hunter, 2008). Hyperactivation of the attachment system ensues. Presenting oneself as completely self-reliant and invulnerable, as is typical of patients who excessively use attachment-deactivating strategies, increasingly leads to feelings of isolation and loneliness (Mikulincer & Shaver, 2007). Suppressing emotional distress leads to increasing allostatic load, which may lead to a complete “biopsychosocial crash” of the stress system as a result of the “wear and tear” caused by chronic stress. At this point, attachment-deactivating strategies typically fail, and the patient becomes highly anxious, needy, and/or depressed (Mikulincer, Dolev, & Shaver, 2004). It is important to recognize that for many FSD patients, attachment issues are not necessarily present before the onset of their condition but may emerge as a consequence of the persistent somatic complaints and continuing allostatic load, leading to the breakdown of the normative coregulation of stress and overreliance on the secondary attachment strategies outlined above (see Fig. 13.2). Of course, some patients do have a history of disrupted attachment before the onset of their complaints. Studies in animals and humans have demonstrated an association between early adversity and vulnerability to stress-related symptoms. For patients Psychodynamic therapy in patients with somatic symptom disorder Predisposing factors Environmental 195 Biological Stress and allostatic load Precipitating factors Secondary attachment strategies Mentalizing impairments Perpetuating factors Perpetuating behaviors Figure 13.2 Contemporary psychodynamic understanding of individuals with functional somatic disorders. who fall into this subgroup, existing attachment issues may be aggravated by the experience of FSD. This has important implications for the treatment of these patients (Luyten, Mayes, Target, & Fonagy, 2012; Luyten & Van Houdenhove, 2013). Mentalizing in FSDs Disruptions in stress regulation and the excessive use of secondary attachment strategies typically lead to a serious disruption in the capacity for mentalizing, that is, the capacity to interpret the self and others in terms of intentional mental states (feelings, wishes, desires, goals, etc.) and, in particular, in the capacity for embodied mentalizing. Embodied mentalizing refers to the ability to interpret the body as the seat of emotional life and as being intrinsically part of one’s own self-definition and self-image. Chronic somatic complaints typically impair and distort this capacity; somatic symptoms are often experienced as an “attack” from within on the patient’s capacity to reflect. Patients with chronic illness have been described as 196 Contemporary Psychodynamic Psychotherapy experiencing their illness as an “internal object” that is constantly threatening them and that needs to be negotiated with and soothed (Schattner, Shahar, & Abu-Shakra, 2008). In regard to the reflective capacities of FSD patients, earlier formulations of FSD have focused on alexithymia, that is, a general lack of emotional awareness and the inability to describe emotional states. However, only a subset of FSD patients (15% 22%) were found to have clinical levels of alexithymia (Pedrosa Gil, Scheidt, Hoeger, & Nickel, 2008; Pedrosa Gil, Weigl, et al., 2008; Waller & Scheidt, 2006). Alexithymia is not specific to FSD but is also found in other disorders, and it reflects the effects of childhood trauma more generally; only a subset of patients with FSD have such a history. Moreover, evidence suggests that, rather than exhibiting a global deficit in emotional awareness, patients with FSDs have more specific difficulties in embodied mentalizing. For instance, many of these patients are unable to link their emotional states to their own body. They are also less accurate in describing their own physical sensations (Bogaerts et al., 2010). Furthermore, patients with FSDs tend to have negative beliefs about expressing their own emotions (Hambrook et al., 2011). FSD patients’ impairments in mentalizing typically are evident as an oscillation between excessive mentalizing (hypermentalizing), expressed in apparently highly sophisticated narratives about mental states that lack any grounding in subjective experience, and hypomentalizing, that is, the almost complete denial of the importance of inner mental states. In the face of pervasive and persistent somatic complaints, three so-called nonmentalizing modes that are characteristic of earlier developmental stages may reemerge, perpetuating the patient’s symptoms and relationship difficulties (see Box 13.1). Epistemic distrust and FSDs FSD patients are often considered to be difficult to treat (Fischhoff & Wessely, 2003), but this notion is neither accurate nor helpful. In addition to being overwhelmed by the continuing distress of their somatic symptoms, FSD patients are often confronted with disbelief and skepticism from others. Furthermore, health professionals often use unhelpful diagnostic labels and obsolete models of FSDs, offer pessimistic prognoses, and frequently underestimate patients’ need for validation. As a result, many FSD patients feel severely misunderstood, invalidated, and bitter (Blom et al., 2012). The concept of epistemic trust is helpful in this context. Epistemic trust is, in essence, the capacity to trust others as a reliable source of knowledge about the world (including one’s condition) and to see others as being able to convey knowledge that is personally relevant and that can be generalized. This capacity first develops in the context of early attachment relationships and is dependent upon the quality of those relationships. Epistemic distrust is particularly prevalent among individuals with dismissive and disorganized attachment styles, as are commonly Psychodynamic therapy in patients with somatic symptom disorder 197 Box 13.1 Three nonmentalizing modes in patients with functional somatic disorders Psychic equivalence mode G G G Patients equate inner (mental) states with outer reality; the internal has the same power as the external. Intolerance of alternative perspectives, leading to concrete understanding. Managed in therapy by the therapist avoiding being drawn into nonmentalizing discourse. The therapist validates the patient’s thoughts and feelings but suggests alternative perspectives. Teleological mode G G G Extreme exterior focus. Patients cannot accept anything other than an obvious, observable change or action as a true indicator of one’s intentions. Managed in therapy by validation, then switching focus to how this makes the patient feel and how these feelings are connected with current (interpersonal) problems. Pretend mode G G G Ideas form no bridge between inner and outer reality; the patient’s thoughts and feelings are decoupled from the external world. In extreme, may manifest as dissociation of thought (hypermentalizing or pseudomentalizing). Managed in therapy by interrupting nonmentalizing processes and “rewinding” to when the patient was still mentalizing. found in patients with FSDs (Waller & Scheidt, 2006). Individuals who have severe difficulties with epistemic trust may oscillate between being overtrustful of others and being extremely distrustful, so-called epistemic hypervigilance. The individual is constantly on his or her guard, questioning the motives underlying others’ advice and opinions. Problems with epistemic trust can make it difficult for patients to accept help from others, including health professionals, and may possibly lead to such professionals’ attempts to help the patient causing iatrogenic effects (Luyten & Abbass, 2013). Unsurprisingly, the relationships of these patients with health professionals are often turbulent, characterized, for instance, by cycles of idealization and devaluation. The patient may start out by clinging to a health professional as the patient’s “last resort,” soon followed by disappointment and reproach when the symptoms persist, which, in turn, often induces rejection by the health professional. Although many patients with FSD may have premorbid problems with epistemic trust, repeated experiences of invalidation (e.g., “There is nothing wrong with you, it’s all in your mind”) may further erode epistemic trust. 198 Contemporary Psychodynamic Psychotherapy Treatment approach A variety of psychodynamic treatment approaches for patients with FSDs have been developed and empirically validated over the past decades (Abbass, 2015; Guthrie & Moghavemi, 2013; Koelen et al., 2014; Luyten, van Houdenhove, Lemma, Target, & Fonagy, 2012; Sattel et al., 2012). These approaches include brief and longer-term individual outpatient treatments and both brief and longerterm more extensive, often multidisciplinary, multicomponent, psychodynamically oriented treatment programs for the most severely affected patients. There is also emerging evidence that psychodynamic treatments for patients influence the neurobiological circuits that are thought to be centrally involved in FSDs, such as the stress, reward, and mentalizing systems (Abbass, Nowoweiski, Bernier, Tarzwell, & Beutel, 2014). Consistent with our theoretical approach outlined above, our own treatment approach, dynamic interpersonal therapy for FSD (DIT-FSD), focuses on the core features of patients with FSD: their overreliance on secondary attachment strategies, problems with (embodied) mentalizing, and difficulties with epistemic trust. DIT-FSD is based on the general principles of dynamic interpersonal therapy (DIT), a manualized, integrative psychodynamic treatment approach (Lemma, Target, & Fonagy, 2010) that has been empirically validated in both controlled trials (Fonagy et al., 2018; Lemma, Target, & Fonagy, 2011) and routine clinical practice (Department of Health, 2012). Because of its integrative nature, DIT-FSD has much in common with other contemporary psychodynamic treatment approaches for patients with FSDs. DIT has two key foci in treatment. On the one hand, there is a constant focus on fostering the process of mentalizing. On the other hand, there is a focus on the content of the patient’s dynamics, through the joint formulation between the therapist and patient of what is termed an interpersonal affective focus (IPAF)—a recurring and often unconscious pattern of relating to the self and others that is a factor in the onset and perpetuation of complaints. The focus on the process of mentalizing and on current rather than past problems—particularly in the early phases of treatment and in more severely affected patients—is deliberate, because reflecting on connections between presenting symptoms and interpersonal issues (particularly those that happened in the past, as in the case of complex trauma) typically exceeds patients’ mentalizing capacities. Of course, the patient’s past is discussed in DIT, but primarily in relation to its influence on current presenting and interpersonal problems and only once the patient has developed the necessary mentalizing skills to reflect on such connections. DIT can be offered in a 16-session format, although some patients need considerably fewer sessions, or, for more severely affected patients, there is a 28-session format. Here, we will describe the core phases and principles of the 16-session format, which consists of three phases. The first phase (Sessions 1 4) typically involves engagement of the patient and formulation of a treatment focus (the IPAF). Engaging the patient in treatment is the first focus of the initial phase. As was mentioned earlier, many of these patients Psychodynamic therapy in patients with somatic symptom disorder 199 resist psychological explanations for their condition and have a history of negative experiences with health professionals. Many (although not all) patients with FSD therefore present with severe epistemic distrust. The only way for the therapist to counter these feelings is by strong and empathic validation of the patient’s feelings of invalidation, in combination with recognizing the reality of their suffering. In addition, many of these patients’ core anxieties are mobilized by the start of therapy, including anxieties related to their attachment history. Strong expectations of being rejected, abandoned, or criticized are typically activated, because any therapeutic relationship activates the attachment system and thus “old” templates concerning these issues. Explicit discussion and exploration of these issues, and of what might “go wrong” in relation to the therapist and therapy more generally, may prevent early dropout and other avoidance behaviors. In DIT-FSD there is always a focus on the potential for therapeutic interventions to become iatrogenic; premature interpretations or even more general but equally premature attempts to convey a particular model of illness to these patients may lead dropout or difficult and stormy transference countertransference issues (e.g., idealization denigration cycles, regressive dependency, sadomasochistic transferences) (Luyten & Abbass, 2013). It is preferable to try to arrive, through consensus rather than conflict, at a common (implicit or explicit) illness theory that recognizes the patient’s subjective experience and the complexity of FSDs. In DIT-FSD this is partly achieved by the therapist and patient jointly deciding on an IPAF during the first four sessions. Formulating the IPAF with the patient is the second core focus of the initial phase of DIT-FSD. An IPAF refers to a recurrent cognitive affective relational or attachment pattern that is associated with the onset and perpetuation of the patient’s symptoms. The IPAF consists of four elements: a specific, often nonconscious, representation of the self; the same for others; affects linking the two; and the defensive function of this constellation. The defensive function refers to the fact that the IPAF, like an attachment strategy, is seen as an adaptive strategy that is used with the aim of finding a balance in life, however distorted this may be. For example, the self in patients with FSDs is often depicted as caring and concerned for others (i.e., “compulsive caregiving”), while others are experienced as aloof, indifferent, and uncaring. Feelings of sadness, helplessness, and hopelessness are often associated with this self other pattern. However, the frustration and aggression that these patients harbor against others, because others have never cared for the patients in the way they care for others, is defended against. The IPAF is formulated on the basis of the interpersonal narratives of the patient and material that emerges in the here-and-now of the therapeutic session. Hence the formulation of a clear and explicit focus for treatment in collaboration with the patient, based on material that emerges in the session (rather than based on what therapist believes and suggests is “wrong” with the patient), plays an important role in countering epistemic distrust and fosters mentalizing. Indeed, the formulation of the IPAF empowers the patient to begin to recognize this pattern himself or herself in the patient’s daily life between sessions. This recognition typically marks the beginning of the second phase. 200 Contemporary Psychodynamic Psychotherapy The second phase of DIT (Sessions 5 12) consists of working through the IPAF and consolidating therapeutic progress. These aims are achieved by a joint process whereby the patient is helped to recognize his or her typical interpersonal attachment pattern in daily life, with a focus on the patient’s capacity to reflect on the impact of this pattern on the embodied self, others, and self-in-relation-to-others. The patient becomes increasingly able to recognize this pattern and understand its developmental origins and its advantages and disadvantages (i.e., the emotional cost). This is achieved by the therapist accepting and validating the patient’s pattern as understandable given the context and subsequently pointing out the emotional and physical costs associated with this pattern. For instance patients who primarily rely on attachment-deactivating strategies, because of the unavailability of their attachment figures, have learned to adopt a stance marked by compulsive autonomy: They have to be able to face any challenge or obstacle on their own and cannot ask for help or express distress. They often function in a hyperrationalized mode and consider their own body as a largely disembodied “machine.” A major focus in the treatment of these patients is to foster embodied mentalizing so that, for instance, they can begin to realize that feeling “tense” or “nervous” may actually mean that they feel sad and angry because they think that no one really cares for them or cares what it is they are trying to achieve. This entails identifying bodily states as reflecting emotions (affect recognition) and realizing that a presumably undifferentiated bodily state (e.g., “I feel tense”) may actually involve several emotional states that are linked to each other and with the IPAF (e.g., “I actually felt very sad and rejected when she said that, and then I started to feel really angry, but also ashamed and guilty, so I did not mention it to her, and simply carried on”). Increasingly, the patients begin to realize the high personal, interpersonal, and (often) metabolic costs of their repetitive pattern of relating to themselves and others. This is the driving force behind the motivation to change. In DIT the therapist actively encourages and supports change. In the middle phase the therapist uses the full spectrum of psychodynamic interventions: (1) supportive interventions (reassurance, support, and empathy); (2) interventions that foster mentalizing; (3) expressive interventions such as interpretation, which include a limited focus on the transference relationship when appropriate (e.g., when the link between what happens in the therapeutic relationship and the IPAF is so obvious that it needs only little interpretative effort to clarify this link) or when needed (e.g., when the transference relationship becomes overly negative); and (4) directive techniques (e.g., encouraging the patient to change the way in which he or she interacts with others). The final phase (Sessions 13 16) focuses on empowering the patient to continue the process of therapeutic change on his or her own. This is initiated by sharing a draft “goodbye” letter written by the therapist. This letter provides an overview of (1) the presenting problems, (2) the IPAF, (3) what has been achieved in terms of change, and (4) what has not yet been achieved. This letter frequently provokes very strong emotional reactions in the patient. In our experience, the extent to which the IPAF is reactivated in response to this letter and the extent to which the patient realizes this are good indicators of the nature of therapeutic change. Psychodynamic therapy in patients with somatic symptom disorder 201 Hence the final sessions typically focus on empowering the patient to continue the process that has started during therapy. This is particularly important in the context of treating patients with FSD, many of whom have a long history of somatic, psychological, and/or relational problems. Clinical illustration Michelle was referred to me (PL) because of a general state of exhaustion after years of struggling with various somatic complaints, including fatigue, headache, back pain, and neurological symptoms with no clear biological cause (e.g., numbness in her fingers, vision difficulties). Michelle is in her forties and has worked as a nurse in a large university hospital for more than 10 years. She is married and has two daughters. Although she finds her husband generally supportive of her and feels that her relationship with her daughters is generally good, she mentions in the first session that she has always had the feeling that, deep down, her husband and children do not really love her. When asked why she has this feeling, she says that they must think of her as someone who has never accomplished anything significant in life, that she is basically a “grey mouse” who cannot compete with other women who have accomplished much more in life. “Other women,” she says, “can do it all: They have children, they have a career, they have hobbies. I’m nothing basically, I get home tired, try my best to take care of my husband and children, but they never show any appreciation.” Michelle says that she has never had any psychological problems but was rather shy and timid as a child. She describes her parents as “good parents . . . they gave me everything I needed.” When asked to provide an example of her “good parents,” another picture emerges. She says that although her parents did their best, she never had the feeling that they encouraged her to achieve anything important in life or supported her in her life ambitions. They always treated her as a “little shy girl” and were happy that she finally managed to get a job as a nurse and started a family soon after she graduated. According to Michelle, however, she fell in love with “the first decent man I could get hold of. I needed someone, always have, and I wanted to have children as soon as possible, and would do things differently as a mom.” Now, however, she feels increasingly distant from her husband and children, as if they push her away: “They seem to have their own life. Where am I in all this?” She has very few friends and has the same feeling in relation to them, as if they all have their own lives and are not interested in her. This makes her feel sad, helpless, and as if she is alone in the world. Her somatic problems began when she started working again soon after the birth of her second daughter. She had long and varying shifts at work and increasingly began to feel exhausted. She developed severe back pain and other somatic symptoms (e.g., numbness in her fingers), and one evening, when she was looking at the computer screen at work in the hospital, the text on the screen became blurred—something she has repeatedly experienced since. 202 Contemporary Psychodynamic Psychotherapy When she was asked what was happening in her life and relationship at that time, her expression suddenly changed. Up until that point, she had spoken in a timid, fatigued, and depressed manner (almost like a shy little girl); now her voice lifted, she leaned toward me, arms outstretched, and in a desperate yet forceful tone said that the feeling of being left alone, of being unimportant, became very strong around that time. Her husband became less and less interested in her, her daughters seemed to be doing fine without her (e.g., in day care), and even her patients seemed not to need her any more. While caring for patients had been a major source of fulfillment for her up to that point, she increasingly had the feeling that her patients disliked her and preferred other nurses (an example of psychic equivalence). She exclaimed, “How is this possible? Why does everyone reject me?” As soon as she had said this, she almost physically collapsed and started crying, saying, “I feel so tired, I feel so alone.” This was the first time she ever had the feeling that her physical symptoms might be connected to what was going on in her life. This is a crucial feature of DIT-FSD, as it opens up the so-called epistemic superhighway that characterizes epistemic trust. This connection is not suggested by anyone else; it is the patient who experiences the connection in the here-andnow of the session, which leads to increasing curiosity about what else might surface in treatment and what else there might be in the therapist’s mind. In the third session we jointly arrived at the IPAF as a focus for the treatment. Michelle’s self-representation involved extremely negative views of the self as worthless, “a grey mouse,” and even the feeling that she was “nothing.” Others were seen as uninterested in her, not supportive, and unavailable. This made her feel alone, sad, abandoned, helpless, and fatigued, a proto-emotion that covered up all other emotions (see below), particularly the frustration and anger that she felt toward her husband, her children, her parents, her colleagues, and even her patients for “not being there for her.” These feelings, however, were strongly defended against by a feeling of helplessness, fatigue, emotion, often even physical paralysis, and guilt. While initially she responded to these feelings with a hyperactivation of the attachment system and (in teleological mode) hoped that caring for others would lead to those others providing her with love and support, this strategy began to fail as her pattern of compulsive caregiving increasingly strained her physical and emotional capacities. A “biopsychosocial crash” ensued, and one evening she fainted at work and was taken to the emergency room and subsequently referred to specialist psychiatric treatment. During the second phase of treatment, Michelle gradually came to recognize how this pattern of compulsive caregiving had completely controlled her life. She realized how, desperate for love, support, and recognition, she had been continuously focused on “being there for someone else; it became almost an obsession, I had to take care of others, I could not let go any longer.” She increasingly began to realize in the sessions and between sessions how this pattern was related to her physical complaints: “Once you start paying attention to it, you suddenly realize how exhausting it is to always want to take care of others, to constantly think what others will think of you.” She also began to notice how angry this made her and Psychodynamic therapy in patients with somatic symptom disorder 203 how her sadness and anger made her feel exhausted. Hence as her capacity for (embodied) mentalizing improved, she also became aware of the high physical and emotional costs of her lifelong pattern. This was a major turning point in the treatment, as she started wondering how she should do things differently. We started thinking together about first taking small steps, as this stable pattern was most likely not going to change overnight. Michelle’s relationship with her husband and children began to change dramatically; instead of being focused on what she thought they needed, she became very interested in how they had felt. She was astonished by the fact that they had been extremely worried about her all the time and how afraid they had been that they might lose her, particularly when she had fainted at the hospital. For the first time she had the feeling that her husband and children truly loved her. At work she asked for a transfer to a physically and emotionally less demanding unit, and slowly, as her mood lifted, her somatic problems also began to improve, particularly when she began to realize how much anger there always had been in her. When I handed Michelle the goodbye letter in Session 13, she was extremely nervous. She began sweating and almost fainted when she started to read the letter. As a result, it took her a long time to read the letter, and although she agreed with almost everything in it, she added, quite ashamed, “But I am still nothing.” Hence there was a strong reactivation of the IPAF in response to the goodbye letter, which she quickly realized when I suggested this possibility to her. However, for much of the session her mentalizing capacities fluctuated strongly, and she was torn between her “old” self-representation of being unworthy (and her belief that I was uninterested in her) and her “new” stronger image of herself. In the next session we were able to look back at this reactivation of her “old” pattern and to link it to the many challenges that still lay ahead. Indeed, if this old pattern was so readily reactivated in treatment, it could also be easily reactivated outside the consulting room. The remainder of the sessions therefore focused on consolidating changes and further supporting her in finding new ways of thinking and feeling about herself and others with regard to what had happened in the past and what was happening in the present and may happen in the future. By this time her somatic symptoms had almost completely disappeared. Conclusions This chapter has presented a broad, evidence-based psychodynamic approach to the conceptualization and treatment of patients with persistent somatic complaints. This approach helps us to understand the connections between the patient’s presenting problems, his or her subjective responses to these problems, and his or her developmental history. These formulations have clear implications for the treatment of these patients regardless of the specific treatment approach used. We have argued for the importance of recognizing these patients’ impairments in attachment, 204 Contemporary Psychodynamic Psychotherapy mentalizing, and epistemic trust, as these problems may make it more difficult to establish a therapeutic alliance and create the potential for iatrogenic treatment effects. Health professionals, in particular psychodynamic therapists, should be keenly aware of these dynamics and should distinguish the patient’s premorbid vulnerability from his or her response to persistent somatic complaints. References Abbass, A. (2015). Reaching through resistance: Advanced psychotherapy techniques. Kansas City, MO: Seven Leaves Press. Abbass, A. A., Nowoweiski, S. J., Bernier, D., Tarzwell, R., & Beutel, M. E. (2014). Review of psychodynamic psychotherapy neuroimaging studies. Psychotherapy and Psychosomatics, 83, 142 147. Available from https://doi.org/10.1159/000358841. Aggarwal, V. R., McBeth, J., Zakrzewska, J. M., Lunt, M., & Macfarlane, G. J. (2006). The epidemiology of chronic syndromes that are frequently unexplained: Do they have common associated factors? International Journal of Epidemiology, 35, 468 476. Available from https://doi.org/10.1093/ije/dyi265. Bass, C., & May, S. (2002). Chronic multiple functional somatic symptoms. British Medical Journal, 325, 323 326. Available from https://doi.org/10.1136/bmj.325.7359.323. Blom, D., Thomaes, S., Kool, M. B., van Middendorp, H., Lumley, M. A., Bijlsma, J. W., & Geenen, R. (2012). A combination of illness invalidation from the work environment and helplessness is associated with embitterment in patients with FM. Rheumatology (Oxford), 51, 347 353. Available from https://doi.org/10.1093/rheumatology/ker342. Bogaerts, K., Van Eylen, L., Li, W., Bresseleers, J., Van Diest, I., De Peuter, S., . . . den Bergh, O. (2010). Distorted symptom perception in patients with medically unexplained symptoms. Journal of Abnormal Psychology, 119, 226 234. Available from https://doi.org/10.1037/a0017780. Cassidy, J., & Kobak, R. R. (1988). Avoidance and its relation to other defensive processes. In J. Belsky, & T. Nezworski (Eds.), Clinical implications of attachment (pp. 300 323). London, UK: Routledge. Department of Health. (2012). IAPT three-year report. The first million patients. London, UK: Department of Health. Available from http://webarchive.nationalarchives.gov.uk/ 20160302155226/http://www.iapt.nhs.uk/silo/files/iapt-3-year-report.pdf. Diamond, D., Stovall-McClough, C., Clarkin, J. F., & Levy, K. N. (2003). Patient-therapist attachment in the treatment of borderline personality disorder. Bulletin of the Menninger Clinic, 67, 227 259. Available from https://doi.org/10.1521/bumc.67.3.227.23433. Fischhoff, B., & Wessely, S. (2003). Managing patients with inexplicable health problems. British Medical Journal, 326, 595 597. Available from https://doi.org/10.1136/ bmj.326.7389.595. Fonagy, P., Lemma, A., Target, M., O’Keeffe, S., Constantinou, M., Ventura Wurman, T., Pilling, S. (2018). Dynamic interpersonal therapy for moderate to severe depression: A pilot randomized controlled and feasibility trial. Manuscript in review. Guthrie, E., & Moghavemi, A. (2013). Psychodynamic-interpersonal therapy: An overview of the treatment approach and evidence base. Psychodynamic Psychiatry, 41, 619 635. Available from https://doi.org/10.1521/pdps.2013.41.4.619. Psychodynamic therapy in patients with somatic symptom disorder 205 Haller, H., Cramer, H., Lauche, R., & Dobos, G. (2015). Somatoform disorders and medically unexplained symptoms in primary care. Deutsches A¨rzteblatt International, 112, 279 287. Available from https://doi.org/10.3238/arztebl.2015.0279. Hambrook, D., Oldershaw, A., Rimes, K., Schmidt, U., Tchanturia, K., Treasure, J., . . . Chalder, T. (2011). Emotional expression, self-silencing, and distress tolerance in anorexia nervosa and chronic fatigue syndrome. British Journal of Clinical Psychology, 50, 310 325. Available from https://doi.org/10.1348/014466510X519215. Hudson, J. I., Mangweth, B., Pope, H. G., Jr., De Col, C., Hausmann, A., Gutweniger, S., . . . Tsuang, M. T. (2003). Family study of affective spectrum disorder. Archives of General Psychiatry, 60, 170 177. Available from https://doi.org/10.1001/archpsyc.60.2.170. Koelen, J. A., Houtveen, J. H., Abbass, A., Luyten, P., Eurelings-Bontekoe, E. H., Van Broeckhuysen-Kloth, S. A., . . . Geenen, R. (2014). Effectiveness of psychotherapy for severe somatoform disorder: Meta-analysis. British Journal of Psychiatry, 204, 12 19. Available from https://doi.org/10.1192/bjp.bp.112.121830. Lemma, A., Target, M., & Fonagy, P. (2010). The development of a brief psychodynamic protocol for depression: Dynamic interpersonal therapy (DIT). Psychoanalytic Psychotherapy, 24, 329 346. Available from https://doi.org/10.1080/02668734. 2010.513547. Lemma, A., Target, M., & Fonagy, P. (2011). The development of a brief psychodynamic intervention (dynamic interpersonal therapy) and its application to depression: A pilot study. Psychiatry: Interpersonal and Biological Processes, 74, 41 48. Available from https://doi.org/10.1521/psyc.2011.74.1.41. Luyten, P., & Abbass, A. (2013). What is the evidence for specific factors in the psychotherapeutic treatment of fibromyalgia? Comment on ‘Is brief psychodynamic psychotherapy in primary fibromyalgia syndrome with concurrent depression an effective treatment? A randomized controlled trial’. General Hospital Psychiatry, 35, 675 676. Available from https://doi.org/10.1016/j.genhosppsych.2013.07.007. Luyten, P., & Fonagy, P. (2018). The stress-reward-mentalizing model of depression: An integrative developmental cascade approach to child and adolescent depressive disorder based on the Research Domain Criteria (RDoC) approach. Clinical Psychology Review, 64, 87 98. Available from https://doi.org/10.1016/j.cpr.2017.09.008. Luyten, P., & Van Houdenhove, B. (2013). Common and specific factors in the psychotherapeutic treatment of patients suffering from chronic fatigue and pain disorders. Journal of Psychotherapy Integration, 23, 14 27. Available from https://doi.org/10.1037/ a0030269. Luyten, P., Kempke, S., Van Wambeke, P., Claes, S., Blatt, S. J., & Van Houdenhove, B. (2011). Self-critical perfectionism, stress generation, and stress sensitivity in patients with chronic fatigue syndrome: Relationship with severity of depression. Psychiatry: Interpersonal and Biological Processes, 74, 21 30. Available from https://doi.org/ 10.1521/psyc.2011.74.1.21. Luyten, P., Mayes, L. C., Target, M., & Fonagy, P. (2012). Developmental research. In G. O. Gabbard, B. Litowitz, & P. Williams (Eds.), Textbook of psychoanalysis (2nd ed., pp. 423 442). Washington, DC: American Psychiatric Press. Luyten, P., van Houdenhove, B., Lemma, A., Target, M., & Fonagy, P. (2012). A mentalization-based approach to the understanding and treatment of functional somatic disorders. Psychoanalytic Psychotherapy, 26, 121 140. Available from https://doi.org/ 10.1080/02668734.2012.678061. 206 Contemporary Psychodynamic Psychotherapy Luyten, P., van Houdenhove, B., Lemma, A., Target, M., & Fonagy, P. (2013). Vulnerability for functional somatic disorders: A contemporary psychodynamic approach. Journal of Psychotherapy Integration, 23, 250 262. Available from https://doi.org/10.1037/ a0032360. Maunder, R. G., & Hunter, J. J. (2008). Attachment relationships as determinants of physical health. Journal of the American Academy of Psychoanalysis and Dynamic Psychiatry, 36, 11 32. Available from https://doi.org/10.1521/jaap.2008.36.1.11. McEwen, B. S. (2007). Physiology and neurobiology of stress and adaptation: Central role of the brain. Physiological Reviews, 87, 873 904. Available from https://doi.org/10.1152/ physrev.00041.2006. Mikulincer, M., & Shaver, P. R. (2007). Attachment in adulthood: Structure, dynamics and change. New York, NY: Guilford Press. Mikulincer, M., Dolev, T., & Shaver, P. R. (2004). Attachment-related strategies during thought suppression: Ironic rebounds and vulnerable self-representations. Journal of Personality and Social Psychology, 87, 940 956. Available from https://doi.org/ 10.1037/0022-3514.87.6.940. Pedrosa Gil, F., Scheidt, C. E., Hoeger, D., & Nickel, M. (2008). Relationship between attachment style, parental bonding and alexithymia in adults with somatoform disorders. International Journal of Psychiatry in Medicine, 38, 437 451. Available from https:// doi.org/10.2190/PM.38.4.d. Pedrosa Gil, F., Weigl, M., Wessels, T., Irnich, D., Baumuller, E., & Winkelmann, A. (2008). Parental bonding and alexithymia in adults with fibromyalgia. Psychosomatics, 49, 115 122. Available from https://doi.org/10.1176/appi.psy.49.2.115. Sattel, H., Lahmann, C., Gundel, H., Guthrie, E., Kruse, J., Noll-Hussong, M., . . . Henningsen, P. (2012). Brief psychodynamic interpersonal psychotherapy for patients with multisomatoform disorder: Randomised controlled trial. British Journal of Psychiatry, 200, 60 67. Available from https://doi.org/10.1192/bjp.bp.111.093526. Sbarra, D. A., & Hazan, C. (2008). Coregulation, dysregulation, self-regulation: An integrative analysis and empirical agenda for understanding adult attachment, separation, loss, and recovery. Personality and Social Psychology Review, 12, 141 167. Available from https://doi.org/10.1177/1088868308315702. Schattner, E., Shahar, G., & Abu-Shakra, M. (2008). I used to dream of lupus as some sort of creature’: Chronic illness as an internal object. American Journal of Orthopsychiatry, 78, 466 472. Available from https://doi.org/10.1037/a0014392. Tak, L. M., & Rosmalen, J. G. M. (2010). Dysfunction of stress responsive systems as a risk factor for functional somatic syndromes. Journal of Psychosomatic Research, 68, 461 468. Available from https://doi.org/10.1016/j.jpsychores.2009.12.004. Van Houdenhove, B., & Luyten, P. (2008). Customizing treatment of chronic fatigue syndrome and fibromyalgia: The role of perpetuating factors. Psychosomatics, 49, 470 477. Available from https://doi.org/10.1176/appi.psy.49.6.470. Waller, E., & Scheidt, C. E. (2006). Somatoform disorders as disorders of affect regulation: A development perspective. International Review of Psychiatry, 18, 13 24. Available from https://doi.org/10.1080/09540260500466774. Wessely, S., & White, P. D. (2004). There is only one functional somatic syndrome. British Journal of Psychiatry, 185, 95 96. Available from https://doi.org/10.1192/bjp.185.2.95. Psychodynamic treatment of eating disorders: an attachment-informed approach 14 Giorgio A. Tasca1 and Louise Balfour2 1 School of Psychology, University of Ottawa, Ottawa, ON, Canada, 2The Ottawa Hospital, University of Ottawa, Ottawa, ON, Canada Eating disorders are characterized by disturbances in eating or eating-related behavior that significantly impair an individual’s functioning (American Psychiatric Association, 2013). Anorexia nervosa (AN), bulimia nervosa (BN), and bingeeating disorder (BED) are among the most common eating disorder diagnoses included in the Diagnostic and Statistical Manual for Mental Disorder, Version 5 (DSM 5) (American Psychiatric Association, 2013). Key diagnostic criteria of AN include extreme weight loss, an intense fear of gaining weight, and self-critical thoughts with regard to body shape. In the United States the lifetime prevalence rate of AN is approximately 0.9% among females and 0.3% among males (Treasure, Claudino, & Zucker, 2010). Although AN has the lowest prevalence rate of all the eating disorder diagnoses, it has the highest mortality rates, ranging from 1.2% to 12.82% (American Psychiatric Association, 2013). Diagnostic criteria of BN include episodes of binge-eating (i.e., overeating with a subjective sense of loss of control) followed by compensatory behaviors (e.g., abusing laxatives, self-induced vomiting, excessive exercise). According to the National Comorbidity Survey Replication (Hudson, Hiripi, Pope, & Kessler, 2007), the lifetime prevalence rates of BN are 0.9 1.5% among females and 0.1 0.5% among males. BED has higher incidence, with a lifetime prevalence of 3.5% among women and 2% among men in the United States (Hudson et al., 2007). Key diagnostic criteria of BED include recurrent episodes of binge-eating accompanied by distress but no compensatory behaviors (American Psychiatric Association, 2013). While overweight is not required for a diagnosis, many patients with BED are overweight or obese as a result of binge-eating with no compensatory behaviors. Individuals who experience eating disorder symptoms of clinical severity but do not meet diagnostic criteria for AN, BN, or BED are currently diagnosed with other specified feeding and eating disorder or unspecified feeding and eating disorder (American Psychiatric Association, 2013). Individuals with an eating disorder often experience comorbidities with other psychiatric disorders (National Collaborating Centre for Mental Health, 2004), including depressive symptoms, bipolar symptoms, problems with substance abuse, and anxiety symptoms (American Psychiatric Association, 2013). The National Comorbidity Contemporary Psychodynamic Psychotherapy. DOI: https://doi.org/10.1016/B978-0-12-813373-6.00014-3 © 2019 Elsevier Inc. All rights reserved. 208 Contemporary Psychodynamic Psychotherapy Survey Replication (Hudson et al., 2007) found that 56.2% of respondents with AN, 94.5% with BN, and 78.9% with BED (according to DSM 4 diagnostic criteria) met full criteria for another DSM 4 disorder. Many treatment-seeking individuals with eating disorders reported a history of traumatic experiences (Tasca et al., 2013) and medical complications related to their symptoms (Mitchell & Crow, 2006). Currently, the most prevalent theoretical conceptualization of eating disorders is based on a cognitive-behavioral therapy (CBT) model (Fairburn, 2008) in which eating disorder symptoms are maintained by an overevaluation of weight and shape, eating concerns related to binge-eating, and dietary restriction. The prevalence of this model in clinical and research writings on eating disorders exists despite the likelihood that clinicians treating patients with eating disorders often integrate psychodynamic theory and practice into their everyday clinical work (Tobin, Banker, Weisberg, & Bowers, 2007). This integration of psychodynamic theory and practice may be partly due to modest outcomes for the more prevalent treatment approaches for eating disorders (Westen, Novotny, & Thompson-Brenner, 2004) and to the fact that time-limited treatments do not easily accommodate patients with complex comorbidities. Also, the CBT model does not speak to fundamental therapeutic relationship aspects, such as countertransference, that challenge clinicians who treat patients with eating disorders (Satir et al., 2009). Further, current CBT-based models often do not take into account an etiological perspective, remain largely descriptive, and typically do not integrate the impact of traumatic experiences into their conceptualizations. As a result, clinicians who wish to develop a personalized developmental narrative and conceptualization of a patient and his or her problems may find the prevailing models quite limiting. Nevertheless, the CBT model has received some empirical support from studies using cross-sectional transdiagnostic samples in which cognitive and behavioral factors predicted eating disorder symptoms (Tasca and Lampard, 2012). However, only about 50% of patients with eating disorders tend to recover (Grenon et al., 2017; Thompson-Brenner, Glass, & Westen, 2003), and outcomes are substantially poorer for AN, in that only about 25% of patients recover (e.g., Zipfel et al., 2014). Perhaps in response to this, the CBT model was enhanced (CBT-E; Fairburn, 2008) by including additional factors to accommodate patients with an eating disorder for whom interpersonal problems, affect dysregulation, clinical perfectionism, and low selfesteem might also maintain their symptoms. Although these factors were meant to apply to only some with eating disorders, an empirical study demonstrated that in fact these additional maintenance factors operated transdiagnostically to predict eating disorder symptoms in a treatment-seeking sample (Tasca, Presniak, et al., 2011). Another promising model for understanding eating disorder symptoms is the interpersonal model, which was initially developed as part of interpersonal therapy (IPT) for BED (Wilfley et al., 1993). In this model, interpersonal problems lead to negative affect, which in turn leads to greater binge eating. The interpersonal model also has received empirical support as a model that might explain the maintenance of eating disorder symptoms transdiagnostically (Ivanova, Tasca, Proulx, & Bissada, 2015). Fundamental aspects of the CBT-E and interpersonal models of eating disorders (interpersonal problems and affect dysregulation) reflect key elements of psychodynamic theories. Psychodynamic treatment of eating disorders: an attachment-informed approach 209 Psychodynamic models Despite the potential utility of early psychodynamic models for eating disorders, these models failed to achieve wide acceptance and use. For example, Hilde Bruch (1988) was prominent in writing about AN as a disorder associated with difficulties with separation-individuation. Similarly, Masterson (1995) wrote about hostile and supportive maternal introjects in response to separation or passive compliance, respectively. Concurrently, earlier drive theory models viewed bulimic symptoms as displaced, unsublimated aggressive drives (e.g., Schwartz, 1988), and bulimic symptoms have also been described as symbolic expressions of impulses (e.g., Lunn & Poulsen, 2012). Self psychology theorists understand eating disorder pathology as attempts to restore a cohesive or vital self that is lacking in mood regulation and self-soothing functions (Goodsitt, 1997). We believe that these earlier models tended to describe eating disorder development and psychopathology using experience-distant concepts that did not fully account for relational aspects of the disorder. We contend that there is a need for a contemporary psychodynamic model that takes into account social and cultural factors as well as biological pressures in conceptualizing eating disorders and their treatment (see Tasca & Balfour, 2014). Generally, more contemporary psychodynamic models place greater emphasis on social and cultural context and on the primacy of relational factors and attachments rather than drives (Fonagy, 2001). Nevertheless, there remains a dearth of writing and research on eating disorders from such contemporary psychodynamic perspectives. The current primacy of cognitive and behavioral models means that little or no emphasis has been placed on psychological development or on internal mental states. These models are primarily concerned with pressures that impinge on the individual, such as maintenance factors that are primarily cognitive in nature, sociocultural factors related to the dieting and fashion industries, and biological factors such as set point for body weight. Although these various factors are certainly important, they do not address developmental and relational issues that confer vulnerabilities to their pressures experienced by the individual. As a result, most currently defined evidence-based treatment approaches (Yager et al., 2012) pay limited attention to affect regulation, interpersonal stressors, defense mechanisms, the impact of mental states, and the role of attachment. An attachment theory framework Attachment theory was developed from the work of John Bowlby (1988), who noticed predictable patterns with which children responded to separations and reunions with parents. He argued that an infant’s attachment behaviors (e.g., reaching, crying, crawling) are geared toward gaining proximity with the caregiver and a sense of security. Such a sense of security within infants allows them to safely explore their environment, which facilitates learning and psychological growth. Repeated interactions with a caregiver have a profound impact on the development 210 Contemporary Psychodynamic Psychotherapy of internal working models of attachment for an infant, and these internal working models, in large part, define later acquired qualities of affect regulation, expectations of others, self-concept, and interpersonal styles (Bowlby, 1988). The work by Mary Ainsworth (Ainsworth & Bell, 1970), a collaborator of Bowlby’s, involved using the Strange Situation research paradigm to systematically study children’s separation and reunion behaviors in a controlled setting. This research led her to codify attachment behaviors such that some children were classified as secure and others as insecure; and children who were insecure were further described as anxious-avoidant or anxious-ambivalent. Some years later, Mary Main, who also worked with Ainsworth, developed an interview, for adults, the Adult Attachment Interview (AAI; Main, Goldwyn, & Hesse, 2002), in which participants answer questions related to early attachment experiences with parents. The nature and quality of the adult’s narrative with respect to attachment can be coded reliably as secure, dismissing (avoidant), or preoccupied (anxious). These categories represent prominent organized mental states in the adult when the attachment system is activated (i.e., during times of stress, need for security, and threat). Securely attached adults expect caring from others, are able to adaptively regulate their emotions, and are able to give support and love easily to important others. Dismissing or avoidantly attached individuals tend to maladaptively downregulate their emotions so that they have trouble experiencing and expressing emotions, they do not expect others to be there for them in time of need, and they tend to dismiss the importance of relationships. Preoccupied or anxiously attached individuals maladaptively upregulate their affect so that they are easily overwhelmed or preoccupied with emotions that they repeatedly access. They may be needy in relationships and highly concerned about relationship loss, and they are not easily soothed by the caring of others. Attachment theory has become one of the most important clinical frameworks of the last half-century largely because of its explanatory power, its research base, and its wide-ranging implications for clinical practice (Bowlby, 1988; Fonagy, 2001). Attachment categorizations are remarkably stable across the life span, with 70% of individuals remaining securely or insecurely attached from adolescence to adulthood (Waters, Merrick, Treboux, Crowell, & Albersheim, 2000). Most shifts in attachment categorization occur as the result of changes in life circumstances. Positive circumstances (e.g., romantic relationship, mentoring, psychotherapy) may lead an individual who is insecurely attached to become securely attached. Negative circumstances (e.g., trauma, neglect, loss) may lead an individual who is securely attached to become insecurely attached (Pinquart, Feußner, & Ahnert, 2013). An attachment-informed psychodynamic model In our model of eating disorders we reconceptualized Malan’s triangle of conflict (Malan, 1979) within an attachment theory framework. Whereas Malan’s model was largely based on a drive theory conceptualization, we reworked the model to be consistent with a contemporary emphasis on relational factors and renamed the Psychodynamic treatment of eating disorders: an attachment-informed approach 211 Anxiety and negative affect Defenses and ED symptoms Attachment needs for security/adaptive feelings Figure 14.1 Triangle of adaptation for eating disorders (ED). model the Triangle of Adaptation (Fig. 14.1; Tasca, Mikail, & Hewitt, 2005). The main or primary motivating factor in the model has to do with attachment security or insecurity. In particular, attachment insecurity is associated with or leads to anxiety and/or negative affect. For example, someone whose internal working models of attachment are primarily avoidant may dismiss relationships and neglect their own emotions but, nevertheless, may experience a high level of anxiety when social demands are placed on them. Their defense mechanisms may include downregulating emotions by disavowal, obsessive compulsive, and other internalizing defenses. For someone with an eating disorder this may be aided by severe food restriction, which further constrains one’s experiences, cognitions, and feelings. On the other hand, someone whose internal working models of attachment are primarily preoccupied in nature may easily experience overwhelming anxiety or negative affect because of their ongoing concerns about losing relationships. Their defense mechanisms might include more externalizing defenses and acting out. This hyperactivation of emotions and disrupted relationship patterns may in part account for dysregulated eating, binge-eating and purging behaviors, and comorbid problems such as with substance abuse. Attachment and the self The Triangle of Adaptation shown in Fig. 14.1 also provides a useful metaphor for the sense of self. That is, the totality of the experience of attachment security or insecurity, the problematic affective experiences that are generated from attachment internal working models, and the defense mechanisms and relational patterns that ensue are in many ways functions of the self. Northoff (2015) argued that the self is 212 Contemporary Psychodynamic Psychotherapy an integrative structure that organizes and coordinates different functions (affective, cognitive, sensorimotor, and vegetative) with regard to interoceptive and exteroceptive stimuli from one’s body and the environment. The self is also temporal in that the experience of the self extends across time, giving one a sense of coherence and stability in one’s experience of internal states and external events. Northoff (2015) also argued that some individuals with eating disorders maintain an attitude of objectification toward their body, that is, as if it did not pertain to their selves. Both dismissing/avoidant and preoccupied/anxious individuals with an eating disorder may engage in a hyperfocus on the body, which is largely experienced as foreign. Individuals with eating disorders may thus experience an incoherent sense of self, related with their struggle to integrate bodily sensations and affect (Amianto, Northoff, Abbate Daga, Fassino, & Tasca, 2016). From a developmental perspective, self-definition is theorized to originate in the bodily self of the infant (Winnicott, 1964). Progressively, the body and the self differentiate through two dialectical developmental lines of attachment and self-definition that occurs within the context of the relationship between an individual and his or her attachment figures (Blatt & Blass, 1990). A key integrative point in this development is the establishment of a cohesive identity in late adolescence or early adulthood (Erikson, 1963). Bruch (1988) argued that the identity of someone with an eating disorder is interrupted, contributing to the individual’s difficulty considering his or her future and integrating his or her past into a coherent narrative (for a fuller description, see Amianto et al., 2016). Narrative incoherence, which is a hallmark of attachment insecurity (Main et al., 2002), is indicative of an unstable sense of self. With a weakened self the individual with an eating disorder has compromised functions such as low self-esteem, poor emotion regulation, and interpersonal ineffectiveness. An attachment-informed psychodynamic treatment for eating disorders As was described earlier, interpersonal problems or sensitivities have become incorporated into CBT-E conceptualizations of the maintenance of eating disorder symptoms for some people (Fairburn, 2008). Interpersonal problems also play a key role in the interpersonal model of eating disorders (Wilfley et al., 1993). We integrate an interpersonal conceptualization into our treatment model by using Strupp and Binder’s (1984) cyclical maladaptive patterns (CMP) framework. We see the CMP as an expression of the interpersonal aspects of attachment insecurity and also as an outcome of the dynamics of the Triangle of Adaptation (Fig. 14.1). Recall that the experience of an incoherent self has an impact on interpersonal sensitivities and affect regulation. Further, maladaptive defense mechanisms can have a direct effect on the quality and nature of one’s relationships. Strupp and Binder’s (1984) model defines interpersonal psychodynamics in terms of acts of self, acts of others, expectations of others, and introject. Acts of Psychodynamic treatment of eating disorders: an attachment-informed approach 213 self are cognitions, emotions, and behaviors that are typically enacted by an individual. They may also include private wishes and needs, so acts of self can be both internally and externally observed aspects of an individual’s experiences. Someone with an eating disorder, for example, may experience a high level of perfectionistic self-presentation that affects the person’s expectations about himself or herself, behaviors toward others, and feelings when the individual inevitably comes up short of perfectionistic standards. Acts of others are others’ actual behaviors toward the self and often in response to the acts of self. The cyclical aspect of the model starts to become evident with the interplay between acts of self and acts of others. For example, if one tends to be passive in relationships, there is a higher probability that others will respond with dominance, as specified by the concept of interpersonal complementarity (Kiesler, 1996). Complementary interactions are highly reinforcing for the people involved; hence, such interactions are relatively stable. Expectations of others are internal cognitive expectations or predictions of how others might behave. For example, attachment-preoccupied individuals may expect others to abandon them, whereas attachment-dismissing individuals may expect others to be unavailable or not useful. These expectations may stem from histories of relationships and may reinforce behaviors and emotions seen in the acts of self. The introject is often considered an outcome of the history of the dynamic interplay between acts of self, acts of others, and expectations of others. The introject represents core beliefs and feelings about the self that then have an impact on how one behaves with others. For example, individuals who fundamentally experience themselves as unlovable may experience depressive affect related to relationship loss, expect others not to love them, and behave in ways that distance others in relationships. On the other hand, someone who experiences the self as a failure or ineffective may experience anxiety or depressive affect related to achievement-related blows to their self-esteem and may see others as uncaring or irrelevant. A negative or critical introject is a key driver of the perfectionism and resulting low selfesteem that is often evident in individuals with eating disorders. Further, problems with the stability of the self and coherence in one’s identity are also indicative of a problematic introject. Strupp and Binder (1984) argued that change in the introject or self-concept is fundamental to achieve lasting improvement through psychotherapy and that change in the introject can be achieved by altering interpersonal patterns identified in the patient’s CMP. The first goal of an attachment-informed psychodynamic therapy is to alter these interpersonal patterns by providing patients with a new understanding (Levenson & Strupp, 2007). This involves cognitive changes in the patient by helping the patient identify his or her dysfunctional interpersonal patterns. By this method, the therapist points out repetitive interpersonal patterns with significant others outside of therapy and with the therapist in the therapy session. The therapist can help the patient to link relationship patterns from past to current relationships, and this provides the patient with some understanding of transference-based relational patterns that may be maladaptive. For example, a patient with an eating disorder may ask a therapist to help the patient to stop binge-eating. However, when the therapist asks the patient to complete a daily food diary, the patient does not comply. The therapist 214 Contemporary Psychodynamic Psychotherapy may experience an urge to double down and demand that the patient follow instructions regarding the food diary “for the patient’s own good.” However, a therapist that is aware of the patient’s CMP (i.e., act of self: wish for caring, not complying; acts of others: dominating and insisting; expectations of others: others will be angry and leave me; introject: “I’m unlovable”) may be able to more easily disentangle himself or herself from the transference-countertransference loop. Such a therapist may be able to help the patient recognize how this pattern perpetuates negative affect and anxiety that results in binge-eating as a means of coping. The therapist may also identify how this interpersonal pattern has played itself out in other relationships, such as those with parents. A second and related goal of this therapeutic approach is to provide the patient with a new experience (Levenson & Strupp, 2007). This involves encouraging the patient to engage in new, more adaptive ways of interacting in therapy and then to generalize these new experiences outside of therapy. Such interventions might provide the patient with experiential learning so that old patterns may be given up. Thus the therapist helps the patient to disconfirm a maladaptive interpersonalaffective schema. A therapist might achieve this by providing a live learning experience, such as by encouraging the patient to try out new behaviors in therapy, and by meta-communication with the patient about these new behaviors, their meaning, and their impact on the patient and therapist. These new ways of being with the therapist may provoke some anxiety in the patient but will provide an emotionally intense experience necessary for new learning to occur. This is akin to Bowlby’s (1988) notion of psychotherapy providing a secure base from which patients may explore their inner experiences and relationships and thus modify their internal working models. An assessment of a patient’s dominant attachment style can help the therapist to identify and direct the most effective interventions (Tasca, Ritchie, & Balfour, 2011). For example, someone who is highly preoccupied or high on attachment anxiety is more likely to need help to become more reflective about his or her emotions and relationships without being overwhelmed by affective experiences. Such an individual’s CMP may be characterized by a fear of abandonment, clingy interpersonal behaviors, close relationships characterized by tension or conflict, expectations of relationship loss, and of a highly self-critical introject. Gaining a better understanding of this interpersonal process and providing new experiences in a stable therapeutic relationship may help such an individual to take a critical step back from his or her emotions before engaging in eating disorder symptoms to gain a temporary sense of affective equilibrium. Conversely, someone who has a dismissing or avoidant attachment may benefit from being gradually exposed to emotional content and experiences. Such an individual may be highly sensitive about, but downplay, the importance of relationships. Individuals with dismissing attachments and an eating disorder do not expect others to be there for them and may have a self-punitive perfectionistic self-concept. In psychotherapy these individuals can gain a better understanding of their needs in relationships and may allow themselves to be cared for by others despite their expectations. Through experiences of being accepted and cared for by an empathic therapist, these patients may Psychodynamic treatment of eating disorders: an attachment-informed approach 215 be able to relax their high standards for how they present themselves to others and reduce the need to quash their internal experiences by extreme dietary restriction. Clinical case example: preoccupied attachment We illustrate this discussion of the utility of the CMP by developing the example of Jane, a 21-year-old woman, who began therapy with Dr. Z. after Jane was discharged from an inpatient unit. Jane was admitted with AN and was severely underweight upon admission. Currently, her weight is normal, but she now binge-eats almost daily, has chaotic eating patterns, does not purge, but is medically stable. Jane described a conflictual relationship with her parents, whom she described as highly controlling regarding her meals. They have been anxious and worried about her eating and low weight and so have tended to watch her closely and to choose Jane’s meals for her. Initially, Jane wanted help to better cope with her emotions, which she described as overwhelming at times. She also wanted help with getting her binges under control, which she found distressing. Dr. Z decided to tackle the binge-eating issues first and asked Jane to monitor her food intake, feelings, thoughts, and circumstances using a standard daily food diary method. Jane initially seemed agreeable to this approach, but after several weeks, it became clear that Jane was not completing the food diaries. Dr. Z explored barriers to Jane completing the diaries and encouraged Jane to do the homework. After some time Dr. Z felt frustrated at Jane’s noncompliance with the task despite her expressed need for help. However, rather than continuing to insist that the patient comply, Dr. Z began to point out how this pattern was similar to what Jane described as a conflictual relationship with her parents. Dr. Z: I find myself wanting to take control and make you do your homework, which I think will be helpful to you. But I know if I continue doing that, then you will not likely comply and become annoyed with me. We’ll get locked in a struggle over it. Jane: Yes, I know what you mean. I’ll probably just sabotage it by saying I’ll do it but then not really do it. Dr. Z: It reminds me of the pattern you get into with your parents, in which you seem to ask for their help with the meals and then you get into these power struggles with them. You always end up feeling like you’ve disappointed them and feel like you’re a “bad” daughter. This pattern is getting in the way of us working well together. Dr. Z also meta-communicated about the conflict, struggle, and frustrations that had become part of their relationship ever since Dr. Z introduced the notion of completing a food diary. That is, Dr. Z realized that Jane’s CMP with her parents were being reenacted in the therapeutic relationship, and this reenactment and Dr. Z’s 216 Contemporary Psychodynamic Psychotherapy collusion with the pattern had caused a rupture in their therapeutic alliance (Safran & Muran, 2000). Dr. Z suggested this interpretation to Jane, who agreed that their relationship had become increasingly tense. Dr. Z then asked Jane to join him in redefining the goals of therapy, that is, to renegotiate that aspect of their therapeutic alliance. Dr. Z: Maybe we can try something different. What do you think is the main thing you want to work on right now? Jane: I would really like to get my emotions under control. I find that I get overwhelmed, and it’s causing problems in just about every part of my life. Dr. Z: Okay, well, your family doctor says that you are not in any immediate medical risk from binging, and your weight is stable. So let’s set aside the food diaries for now and work on your emotions and how you are managing with them. How does that sound? Jane: Yeah, that sound good. Dr. Z: You know, this conversation we’ve had about changing our focus for therapy has felt less tense, and I’ve experienced your approach to this conversation to be much less passive and more assertive. It makes me want to be more respectful of you and your needs. Have you noticed that? Jane: Yeah, it feels different. Like we’re figuring out how to work together. This example illustrates how the therapist was able to disengage from a transference-countertransference pattern that was identified with the CMP. He was able to meta-communicate with the patient about the pervasiveness of the pattern in the patient’s life, including therapy, and invited her to participate in a new experience in the therapy—one in which she was more assertive. Supporting evidence There is evidence that greater attachment anxiety at pretreatment is related to poorer treatment outcomes for eating disorders and that greater attachment avoidance may be related to dropping out of multimodal day treatment (Illing, Tasca, Balfour, & Bissada, 2010; Tasca, Taylor, Bissada, Ritchie, & Balfour, 2004). However, Tasca et al. (2006) reported that patients with BED and greater attachment anxiety benefited more from group psychodynamic-interpersonal psychotherapy (GPIP), a treatment that focuses on interpersonal problems and affect dysregulation, which are key issues for individuals with attachment anxiety. Further, recent research suggests that higher reflective functioning at pretreatment is associated with better outcomes for those with BED (Maxwell, Tasca, Grenon, Faye et al., 2017). In addition, GPIP results in Psychodynamic treatment of eating disorders: an attachment-informed approach 217 improvements in self-reported attachment insecurity up to 1 year post treatment (Maxwell, Tasca, Ritchie, Balfour, & Bissada, 2014). Two recent studies by Maxwell et al. (2017, 2017) that used the AAI (Main et al., 2002) demonstrated that GPIP for BED resulted in improvements in reflective functioning and in reductions in insecure attachment states of mind. Finally, a study by Hill et al. (2015) reported that overall defensive functioning improved after GPIP for BED. Collectively, these studies suggest that a time-limited, psychodynamic, group-based treatment for BED and other eating disorders can result in improved reflective functioning, defensive functioning, and attachment mental states. Historically, some randomized controlled trials have disadvantaged psychodynamic therapy by the design of the study or implementation of the treatments. For example, the studies by Garner et al. (1993) and Poulsen et al. (2014) both instructed the psychodynamic therapists not to initiate a discussion with patients about eating disorder symptoms, which unnecessarily limited the effectiveness of the psychodynamic therapies (for commentaries, see Tasca, Hilsenroth, & Thompson-Brenner, 2014, and Westen et al., 2004). Nevertheless, meta-analyses of group treatments for eating disorders (Grenon et al., 2017) and of individual treatments for eating disorders (Spielmans et al., 2013) found no differences between treatment types (CBT, IPT, psychodynamic therapy) in their outcomes to reduce eating disorder symptoms. A recent narrative review of randomized controlled trials, effectiveness studies, and case studies by Abbate-Daga, Marzola, Amianto, and Fassino (2016) concluded that current data do support the potential effectiveness of psychodynamic therapies for eating disorders, but more well-designed trials are necessary. There are two noteworthy high-quality studies to mention in this research area. First, in a randomized controlled trial of focal dynamic therapy, CBT, and treatment as usual for AN, Zipfel et al. (2014) found equivalent effects for psychodynamic and CBT interventions, but they also reported that focal dynamic therapy was more effective than the other treatments at follow-up. This is an important study because AN is very difficult to treat, and the number of randomized controlled trials for the treatment of AN is very small. Second, in a randomized controlled trial of GPIP, GCBT, and a waiting list control condition, Tasca et al. (2006) found equivalent effects for GPIP and GCBT, which were both more effective than the control condition. The effects were maintained to long-term follow-up and indicate the potential efficacy of GPIP for BED. Summary and conclusions Although still relatively small, a growing evidence base is showing that psychodynamic treatments for eating disorders are effective in reducing eating disorder symptoms and in improving psychological factors such as attachment states of mind, mentalization, and defensive functioning (Hill et al., 2015; Maxwell, Tasca, Grenon, Faye et al., 2017; Maxwell, Tasca, Grenon, Ritchie et al., 2017; 218 Contemporary Psychodynamic Psychotherapy Tasca et al., 2006; Zipfel et al., 2014). In this review of psychodynamic treatment of eating disorders we presented a model describing how attachment insecurities lead to negative affect or anxiety, which in turn may result in maladaptive defense mechanisms and/or eating disorder symptoms. Our research has supported this conceptual model by showing how early experiences lead to attachment insecurity that subsequently leads to affect dysregulation and eating disorder symptoms (Tasca et al., 2009, 2013). Further, our treatment model uses a psychodynamic conceptualization of relational difficulties that affect current and therapeutic relationships. Psychodynamic conceptualizations and treatments for eating disorders that are based on contemporary notions that take into account social and relational contexts and attachment states of mind are more likely to gain currency among practicing psychotherapists. It will be important, however, for psychodynamic researchers and clinicians to test their concepts and treatments empirically in order to verify their efficacy and to legitimize their applications in clinical contexts. References Abbate-Daga, G., Marzola, E., Amianto, F., & Fassino, S. (2016). A comprehensive review of psychodynamic treatments for eating disorders. Eating and Weight Disorders, 21, 553 580. Ainsworth, M. D., & Bell, S. M. (1970). Attachment, exploration, and separation: Illustrated by the behavior of one-year-olds in a strange situation. Child Development, 41, 49 67. American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed). Arlington, VA: American Psychiatric Publishing. Amianto, F., Northoff, G., Abbate Daga, G., Fassino, S., & Tasca, G. A. (2016). Is anorexia nervosa a disorder of the self: A psychological perspective. Frontiers in Psychology, 7, 849. Blatt, S. J., & Blass, R. B. (1990). Attachment and separateness: A dialectic model of the products and processes of development throughout the life cycle. The Psychoanalytic Study of the Child, 45, 107 127. Bowlby, J. (1988). A secure base: Parent-child attachment and healthy human development. New York: Basic Books. Bruch, H. (1988). Conversations with anorexics. New York: Basic Books. Erikson, E. H. (1963). Childhood and society (2nd Ed). New York: Norton. Fairburn, C. G. (2008). Cognitive behavior therapy and eating disorders. New York: Guilford. Fonagy, P. (2001). Attachment theory and psychoanalysis. London: Other Press. Garner, D. M., Rockert, W., Davis, R., Garner, M. V., Olmsted, M. P., & Eagle, M. (1993). Comparison of cognitive-behavioral and supportive-expressive therapy for bulimia nervosa. The American Journal of Psychiatry, 150, 37 46. Goodsitt, A. (1997). Eating disorders: A self-psychological perspective. In D. M. Garner, & P. E. Garfinkel (Eds.), Handbook of treatment for eating disorders (pp. 205 228). New York: The Guilford Press. Grenon, R., Schwartze, D., Hammond, N., Ivanova, I., Mcquaid, N., Proulx, G., & Tasca, G. (2017). Group psychotherapy for eating disorders: A meta-analysis. International Journal of Eating Disorders, 50, 997 1013. Available from https://doi.org/10.1002/eat.22744. Psychodynamic treatment of eating disorders: an attachment-informed approach 219 Hill, R., Tasca, G. A., Presniak, M., Francis, K., Palardy, M., Grenon, R., . . . Bissada, H. (2015). Changes in defense mechanism functioning during group therapy for bingeeating disorder. Psychiatry, 78, 75 88. Hudson, J. I., Hiripi, E., Pope, H. G., Jr., & Kessler, R. C. (2007). The prevalence and correlates of eating disorders in the national comorbidity survey replication. Biological Psychiatry, 61, 348 358. Illing, V., Tasca, G. A., Balfour, L., & Bissada, H. (2010). Attachment insecurity predicts eating disorder symptoms and treatment outcomes in a clinical sample of women. The Journal of Nervous and Mental Disease, 198, 653 659. Ivanova, I. V., Tasca, G. A., Proulx, G., & Bissada, H. (2015). Does the interpersonal model apply across eating disorder diagnostic groups? A structural equation modeling approach. Comprehensive Psychiatry, 63, 80 87. Kiesler, D. J. (1996). Contemporary interpersonal theory and research: Personality, psychopathology, and psychotherapy. Oxford, England: John Wiley. Levenson, H., & Strupp, H. H. (2007). Cyclical maladaptive patterns: Case formulation in time-limited dynamic psychotherapy. In T. D. Eells (Ed.), Handbook of psychotherapy case formulation (2nd ed., pp. 84 115). New York: Guilford Press. Lunn, S., & Poulsen, S. (2012). Psychoanalytic psychotherapy for bulimia nervosa: A manualized approach. Psychoanalytic Psychotherapy, 26, 48 64. Main, M., Goldwyn, R., Hesse, E. (2002). Adult attachment scoring and classification systems. Unpublished manuscript, University of California at Berkeley. Malan, D. (1979). Individual psychotherapy and the science of psychodynamic. London: Butterworths. Masterson, J. F. (1995). Paradise lost—Bulimia, a closet narcissistic personality disorder: A developmental, self, and object relations approach. In R. C. Marohn, & S. C. Feinstein (Eds.), Annals of the American Society for Adolescent Psychiatry. Adolescent psychiatry: Developmental and clinical studies (Vol. 20, pp. 253 266). Hillsdale, NJ: Analytic Press. Maxwell, H., Tasca, G. A., Grenon, R., Faye, M., Ritchie, K., Bissada, H., & Balfour, L. (2017). Change in attachment dimensions in women with binge-eating disorder following group psychodynamic interpersonal psychotherapy. Psychotherapy Research., 28, 887 901. Available from https://doi.org/10.1080/10503307.2017.1278804. Maxwell, H., Tasca, G. A., Grenon, R., Ritchie, K., Bissada, H., & Balfour, L. (2017). Change in attachment states of mind in women with binge-eating disorder. Clinical Psychology and Psychotherapy, 24, 1292 1303. Available from https://doi.org/10.1002/ cpp.2095. Maxwell, H., Tasca, G. A., Ritchie, K., Balfour, L., & Bissada, H. (2014). Change in attachment insecurity is related to improved outcomes 1-year post group therapy in women with binge eating disorder. Psychotherapy, 51, 57 65. Mitchell, J. E., & Crow, S. (2006). Medical complications of anorexia nervosa and bulimia nervosa. Current Opinion in Psychiatry, 19, 438 443. National Collaborating Centre for Mental Health. (2004). Eating disorders: Core interventions in the treatment and management of anorexia nervosa, bulimia nervosa and related eating disorders. Leiceester, UK: British Psychological Society. Northoff, G. (2015). Is schizophrenia a spatiotemporal disorder of the brain’s resting state? World Psychiatry, 14, 34 35. Pinquart, M., Feußner, C., & Ahnert, L. (2013). Meta-analytic evidence for stability in attachments from infancy to early adulthood. Attachment & Human Development, 15, 189 218. 220 Contemporary Psychodynamic Psychotherapy Poulsen, S., Lunn, S., Daniel, S. I. F., Folke, S., Mathiesen, B. B., Katznelson, H., & Fairburn, C. G. (2014). A randomized controlled trial of psychoanalytic psychotherapy or cognitive-behavioral therapy for bulimia nervosa. American Journal of Psychiatry, 171, 109 116. Safran, J. D., & Muran, J. C. (2000). Negotiating the therapeutic alliance: A relational treatment guide. New York: Guilford Press. Satir, D. A., Thompson-Brenner, H., Boisseau, C. L., & Crisafulli, M. A. (2009). Countertransference reactions to adolescents with eating disorders: Relationships to clinician and patient factors. International Journal of Eating Disorders, 42(6), 511 521. Schwartz, H. J. (1988). Bulimia: Psychoanalytic perspectives. In H. J. Schwartz (Ed.), Bulimia: Psychoanalytic treatment and theory (pp. 31 53). Madison, CT: International Universities Press. Spielmans, G. I., Benish, S. G., Marin, C., Bowman, W. M., Menster, M., & Wheeler, A. J. (2013). Specificity of psychological treatments for bulimia nervosa and binge eating disorder? A meta-analysis of direct comparisons. Clinical Psychology Review, 33, 460 469. Strupp, H. H., & Binder, J. L. (1984). Psychotherapy in a new key: A guide to time-limited dynamic psychotherapy. New York: Basic. Tasca, G., & Balfour, L. (2014). Eating disorders and attachment: A contemporary psychodynamic perspective. Psychodynamic Psychiatry, 42, 257 274. Tasca, G., & Lampard, A. (2012). Reciprocal influence of alliance to the group and outcome in day treatment for eating disorders. Journal of Counseling Psychology, 59, 507 517. Tasca, G., Ritchie, K., Zachariades, F., Proulx, G., Trinneer, A., Balfour, L., . . . Bissada, H. (2013). Attachment insecurity mediates the relationship between childhood trauma and eating disorder psychopathology in a clinical sample: A structural equation model. Child Abuse & Neglect, 37, 926 933. Tasca, G. A., Hilsenroth, M., & Thompson-Brenner, H. (2014). Psychoanalytic psychotherapy or cognitive-behavioral therapy for bulimia nervosa: Considering these findings in context. American Journal of Psychiatry, 171, 583 584. Tasca, G. A., Presniak, M. D., Demidenko, N., Balfour, L., Krysanski, V., Trinneer, A., & Bissada, H. (2011). Testing a maintenance model for eating disorders in a sample seeking treatment at a tertiary care center: A structural equation modeling approach. Comprehensive psychiatry, 52, 678 687. Tasca, G. A., Ritchie, K., & Balfour, L. (2011). Implications of attachment theory and research for the assessment and treatment of eating disorders. Psychotherapy, 48, 249 259. Tasca, G. A., Szadkowski, L., Illing, V., Trinneer, A., Grenon, R., Demidenko, N., . . . Bissada, H. (2009). Adult attachment, depression, and eating disorder symptoms: The mediating role of affect regulation strategies. Personality and Individual Differences, 47, 662 667. Tasca, G. A., Mikail, S. F., & Hewitt, P. L. (2005). Group psychodynamic interpersonal psychotherapy: Summary of a treatment model and outcomes for depressive symptoms. In M. E. Abelian (Ed.), Focus on psychotherapy research (pp. 159 188). Hauppauge, NY: Nova Science. Tasca, G. A., Ritchie, K., Conrad, G., Balfour, L., Gayton, J., Lybanon, V., & Bissada, H. (2006). Attachment scales predict outcome in a randomized controlled trial of two group therapies for binge eating disorder: An aptitude by treatment interaction. Psychotherapy Research, 16, 106 121. Psychodynamic treatment of eating disorders: an attachment-informed approach 221 Tasca, G. A., Taylor, D., Bissada, H., Ritchie, K., & Balfour, L. (2004). Attachment predicts treatment completion in an eating disorders partial hospital program among women with anorexia nervosa. Journal of Personality Assessment, 83, 201 212. Thompson-Brenner, H., Glass, S., & Westen, D. (2003). A multidimensional meta-analysis of psychotherapy for bulimia nervosa. Clinical Psychology: Science and Practice, 10, 269 287. Tobin, D. L., Banker, J. D., Weisberg, L., & Bowers, W. (2007). I know what you did last summer (and it was not CBT): A factor analytic model of international psychotherapeutic practice in the eating disorders. International Journal of Eating Disorders, 40, 754 757. Treasure, J., Claudino, A. M., & Zucker, N. (2010). Eating disorders. The Lancet, 375, 583 593. Waters, E., Merrick, S., Treboux, D., Crowell, J., & Albersheim, L. (2000). Attachment security in infancy and early adulthood: A twenty-year longitudinal study. Child Development, 71, 684 689. Westen, D., Novotny, C. M., & Thompson-Brenner, H. (2004). The empirical status of empirically supported psychotherapies: Assumptions, findings, and reporting in controlled clinical trials. Psychological Bulletin, 130, 631 663. Wilfley, D., Agras, W. S., Telch, C. F., Rossiter, E. M., Schneider, J. A., Cole, A. G., . . . Raeburn, S. D. (1993). Group cognitive behavioral therapy and group interpersonal psychotherapy for the nonpurging bulimic individual: A controlled comparison. Journal of Consulting and Clinical Psychology, 2, 296 305. Winnicott, D. W. (1964). The child, the family, and the outside world. London: Pelican Books. Yager, J., Devlin, M. J., Halmi, K. A., Herzog, D. B., Mitchell, J. E., Power, P., & Zerbe, K. J. (2012). Guideline watch (August 2012): Practice guideline for the treatment of patients with eating disorders (3rd ed.). American Psychiatric Association. Retrieved from: http://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/ eatingdisorders-watch.pdf. Zipfel, S., Wild, B., Groß, G., Friederich, H.-C., Teufel, M., Schellberg, D., . . . On Behalf of the ANTOP Study Group. (2014). Focal psychodynamic therapy, cognitive behaviour therapy, and optimised treatment as usual in outpatients with anorexia nervosa (ANTOP study): Randomised controlled trial. The Lancet, 383, 127 137. Psychodynamic psychotherapy with infants and parents 15 Björn Salomonsson Department of Women’s and Children’s Health, Karolinska Institutet, Stockholm, Sweden Psychoanalysts have modified classical technique to reach psychotic and borderline patients, groups, couples and, only lately, the mother infant dyad. Psychodynamic therapy with infants and parents (PTIP) was introduced by Fraiberg (1980) and Dolto (1982, 1985) and is now gaining interest among therapists. A distinction may be drawn between PTIP and methods that mainly support the mother’s ego and encourage her to change her behavior with the baby (developmental guidance, Lojkasek, Cohen, & Muir, 1994; infant massage, Field, 2000; interaction guidance, McDonough, 2004; Aarts, 2000), in that PTIP focuses on the internal worlds of infant and parent and their interaction. The focus of this chapter will be on PTIP. European clinicians restrict “infant” to preverbal children, in line with the Latin in-fans “speechless”; therefore this chapter will focus on therapies with babies under the age of 18 months. But does an in-fans need to take part in therapy to be affected by it? As will be revealed in this review, there is no clear answer that is agreed upon by all. Psychodynamic theory describes humans as struggling with unconscious urges that affect their character, relationships, interests, passions, and cognitive capacities. PTIP helps mothers discern their unconscious ambivalence toward their child, partner, or maternal role, but does such ambivalence also apply to the infant? All PTIP methods agree that the parent blends conscious strivings to bond with the child with unconscious and contrasting urges. In contrast, few of these methods speak of similar factors in the baby. This will be a point of exploration throughout this review, since different positions on this issue will influence therapeutic technique. PTIP modes sometimes agree with classical psychoanalytic theory and sometimes do not. Traditionally, the mother is seen as the primary object, with her body parts or functions being involved in the infant’s fantasies. This maternal primacy is reflected in the dominance of PITP mother baby case presentations, though the father’s contributions are increasingly acknowledged.(Baradon, 2019). Case reports often concern “baby worries”: complaints about breast-feeding, infant sleep, and attachment, as well as mothers’ feelings of guilt, anxiety, or inability to love the baby. The Freudian baby Freud observed everyday mother infant interactions and speculated about what went on in the babies’ minds. He described the baby’s experience of satisfaction—a Contemporary Psychodynamic Psychotherapy. DOI: https://doi.org/10.1016/B978-0-12-813373-6.00015-5 © 2019 Elsevier Inc. All rights reserved. 226 Contemporary Psychodynamic Psychotherapy psychological event—in physiological terms such as a neuronal discharge (Freud, 1895/1950) but also included an interactive dimension; for the baby, satisfaction presupposes an “alteration in the external world (supply of nourishment, proximity of the sexual object)” (p. 318) by “an experienced person” who gets drawn to the child’s state. In simpler words, Freud’s idea was that a baby keeps crying until the mother listens and comforts the baby. Freud’s neurophysiological terminology may obscure his position that an infant forms representations of the mother. When distressed, the baby will perceive mother as a “hostile object” (p. 320). Importantly, the baby rejects this memory, which Freud labels a primary defense (p. 322). The Freudian baby not only biologically registers but also subjectively experiences disturbing events. The baby handles them by interacting with the mother, which leave traces in the baby’s mind. In other words, interactions with mother—in the context of disruptive experience—are internalized as representations in the baby’s mind. Freud wavers between describing the infant as governed by biological forces and psychological motives, but he is convinced that the baby creates positive representations of a satisfying mother and negative ones when he suffers. Freud thus thought babies were “minded.” But since babies are “in-fans,” their representations may merely consist of the “sound-image” or the “thinglike” quality assembled from “auditory, visual and kinaesthetic elements” (1915b, p. 210) in the adult’s communications. Other concepts springing from Freud’s assumptions about the baby’s mind are infantile sexuality (1905), the unconscious (1900, 1915b), primal repression (1915a), and anxiety (1925 26). He also highlighted that our adult character is “based on the memory-traces of our impressions. . .. The impressions which have had the greatest effect on us—those of our earliest youth—are precisely the ones which scarcely ever become conscious” (1900, p. 539). Thus in Freud’s view, infancy is of fundamental importance for one’s future life. Psychodynamic therapies with infants and parents Freud’s speculations on the infant mind’s continuity into adulthood may help us to explain why psychoanalysts were slow in treating babies. Therapy with a baby can be overwhelming. The therapist veers toward a “massive identification with the child . . . it is not always easy to control one’s reactions to [the baby’s] positive or negative provocations” (Watillon, 1993, p. 1045). Another reason for the belated emergence of PTIP is the notion of psychoanalysis as a “talking cure,” which led to the mistake that our primary clinical data are words and not any “representations or signifiers of process” (Olinick, 1985, p. 500). This might have prevented us from viewing the baby as a patient to communicate with. Kleinian analysts have speculated extensively on the infant mind, though mainly to understand infantlike parts of older patients’ personalities (Joseph, 1985; Meltzer, 1992; O’Shaughnessy, 1988). By contrast, ego psychological analysts warn against attributing mental capacities beyond the baby’s development (Fonagy, 1996) and against “adultomorphizing” the baby (Peterfreund, 1978; Stern, 1985). This perspective has contributed Psychodynamic psychotherapy with infants and parents 227 to a reluctance among ego psychologists for viewing the baby as an active psychotherapy participant. Organizational factors have likely also contributed to the relatively slow development of PTIP. Analysts tend to work in private practice and are contacted by people who suffer. In contrast, “baby worries” emerge at child health centers when mothers complain about the child’s stomachache, sleep, or breast-feeding—without feeling that they need therapy. Alternatively, mothers feel sad or anxious and are referred for individual therapy or drugs to a general practitioner or a psychiatrist. The challenge today is to integrate qualified perinatal psychological care with everyday health care. The following provides a brief description of the best-known PTIP methods. Infant parent psychotherapy (Fraiberg) Fraiberg devised brief crisis interventions, interaction guidance-supportive treatments, and infant parent psychotherapy. The first focused on problems arising from a “circumscribed set of external events and when the parents’ psychological capacities suggest that they can make use of a brief focused intervention” (1989, p. 60), as illustrated by a couple’s anxiety about their newborn due to an unresolved mourning of another baby who had died earlier. The second, interaction guidance, addressed parents with limited psychological-mindedness and did not aim to fundamentally alter their psychodynamics. Fraiberg’s infant parent psychotherapy was clearly a mode of PTIP. She applied it when a baby reminded the parents of “an aspect of the parental self that is repudiated or negated” (1989, p. 60). This “ghost in the nursery” marred the parent’s interactions with the baby, who got engulfed in the parental neurosis. To illustrate, a mother felt that her 5-month-old girl did not attach. The mother had been abandoned during her own mother’s postpartum psychosis, and now an extramarital affair added guilt that wiped out any joy of motherhood. A hypothesis was formed: “When this mother’s own cries are heard [by the therapist], she will hear her child’s cries” (1980, p. 109). This way, “the pathology which had spread to embrace the baby” (p. 111) could be withdrawn. Compared with Freud, Fraiberg was more ambivalent about the existence of defenses in a baby. Clinically, she regarded the baby as a “catalyst” (1989, p. 53) who intensified the emotional climate and sometimes engaged in “dialogue” with the adults. Fraiberg’s intention behind such dialogues was to bypass the mother’s perceptions of her baby. Her followers explore parental “negative attributions” that were projected onto the child (Lieberman & Van Horn, 2008; Silverman & Lieberman, 1999). Fraiberg’s parent infant psychotherapy has been subjected to randomized outcome trials comparing it with Interaction Guidance (Robert-Tissot et al., 1996), Watch, Wait, and Wonder (WWW) (Cohen et al., 1999), and nonintervention (Lieberman, Weston, & Pawl, 1991). The study by Cohen et al. (1999) demonstrated that its effects took somewhat longer to materialize than a more 228 Contemporary Psychodynamic Psychotherapy infant-directed technique, while the Lieberman, Weston, and Pawl (1991) study showed good results with insecurely attached infants and their babies. Importantly, these PTIP therapies were lengthier than those in the other studies. Infant parent psychotherapy (Cramer and Palacio Espasa) Based in Geneva, the work of Cramer and Palacio Espasa (Cramer & Palacio Espasa, 1993; Cramer, 1997; Espasa & Alcorn, 2004; Manzano, Palacio Espasa, & Zilkha, 1999; Zlot, 2007) has focused on less disadvantaged families. Distinctions between their approach and that of Fraiberg are subtle. They focus more on the mother’s psychopathology, such as masochistic and narcissistic issues, but also acknowledge the dynamics behind the infant’s symptoms that might express “a repressed tendency in the parent” (Cramer & Palacio Espasa, 1993, p. 85). The result is a “core conflictual relationship” between the baby and the parent’s repressed mentation. This comes close to Fraiberg’s “ghost,” but these authors instead talk about a mother’s “narcissistic scenarios” (Manzano et al., 1999) that prevent her from seeing the baby in his or her own right. In their view, the child then becomes involved in a relationship that the baby cannot comprehend. As for the baby’s role in therapy, Cramer and Palacio Espasa regard the baby as less active than did Fraiberg. Thus with regard to our question about the unconscious these authors seem uncomfortable with applying this concept to babies. Therapeutic consultations with babies (Lebovici) The interventions developed by Serge Lebovici, head of the Centre Alfred Binet in Paris, resembled Winnicott’s (1971) therapeutic consultations and Fraiberg’s (1989) brief crisis interventions. One can recognize Fraiberg’s thinking when reading that the “mother’s internal reality, her unconscious, constitutes the first world offered to the baby” (Lebovici & Stoléru, 2003, p. 289). Whereas Fraiberg focused on the mother’s trauma, Lebovici highlighted how the mother’s infantile sexuality colored the relationship with the baby and contributed to symptoms such as insomnia and breast-feeding difficulties. Lebovici (2000) also focused on what happens in the PTIP therapist’s working mind. Already, Emde (1990) had suggested that the therapist’s empathy is rooted in, and similar to, “the mutuality experiences provided within the early motherchild relationship” (p. 884). Lebovici added that empathy also involves creativity; the therapist is not only “feeling into” the patient but also “forgetting about oneself” (2000, p. 227) and letting the therapist’s associations interact with the patient’s, similarly to when a mother is chatting with her baby. Lebovici’s term enactment refers to the therapist’s body sensations and gestures that may indicate an unacknowledged affect in mother or child. A therapist might come up with a spontaneous metaphor in the session. If analyzed in retrospect, it can indicate the resistances Psychodynamic psychotherapy with infants and parents 229 in the countertransference and thus clarify to the therapist what was indistinct in his or her thinking about the dyad. Lebovici welcomed the baby to the session, which helped him probe the unconscious meanings of the parent’s spontaneous behavior or comments. The baby’s presence also stimulated his use of metaphor, though Lebovici was not inclined to intervene with the baby. He would probably have agreed that the baby’s unconscious exists from early on, but he would disagree with his compatriot Dolto that a baby can understand verbal import. Direct, brief mother baby therapy (Dolto) Françoise Dolto was a Parisian psychoanalyst, recently introduced in English (Hall, Hivernel, & Morgan, 2009). She believed in the young infant’s ability to communicate with his or her caretakers and was convinced that babies could understand some literal meaning of her words. According to neurodevelopmental research, this is clearly inaccurate (Karmiloff & Karmiloff-Smith, 2001). Yet before concluding that her PTIP method was erroneous, we must learn about its theoretical foundations. One baby refused breast-feeding, and Dolto (1985) addressed her: “Everything was OK when you were inside Mom’s tummy. Then you were born. . .. Mom had milk and you were calling for it. . .. One day you heard, together with Mom . . . that things weren’t going well at home. Maybe you told yourself ‘Poor little Mom, I’d better get back into her tummy, ‘cause everything went well as long as I was there’” (p. 211). Dolto thought the baby’s refusal to suckle resonated with the mother’s mourning of her now dead mother and her worries about the home situation. Dolto also claimed that the baby understood the therapeutic intervention verbally. This is easier to disclaim than Dolto’s thought that when this mother concealed embarrassing truths to protect her baby, it may have confounded the baby and stunted her development. PTIP therapists agree that a baby may intuit that “something is wrong” when parents are inauthentic, creating a ghost in the nursery and confusing the baby. However, most would talk to the parents, not the child, about it. Yet once we bypass Dolto’s mistake in attributing language comprehension to a baby, we discern another reason for her speaking directly to the baby: The infant is formed in and informed by language. Dolto thought maturation comes about only to the extent to which the baby manages to replace his or her desire with societally acceptable demands. Therefore adults need to introduce the child to the symbolic order, which first and foremost includes language (Salomonsson, 2017). Already “before the age of words, the presence of a mother speaking to her infant is a nourishment more valuable than the milk she offers at the breast” (Dolto, 1994, p. 605). This will help the child “displace his drive towards another object” (Dolto, 1982, p. 48), for example, by accepting that the milk is offered and therefore belongs to him but the breast belongs to the mother. When the child accepts this, the child can be weaned, learn to speak, and express what he or she wants. 230 Contemporary Psychodynamic Psychotherapy Parents with babies speak, frown, shake their head, sigh, smile, giggle, and so on —and they talk. Infants seem to experience words according to their emotional qualities, as a comforting, intimidating, or captivating sound (Markova & Legerstee, 2006). Infant research indicates that young babies regard speech as a special mode of communicating (Ferry, Hespos, & Waxman, 2010; Gervain, & Mehler, 2010). It is as if the baby were thinking, “It’s special, Mum’s facial movements plus sounds I can’t produce. It seems to indicate something, but I don’t get what.” While the mother in therapy is entangled with her baby, the therapist is in a better position to, in Dolto’s words, parler vrai to baby and mother. To sum up her response to our two questions, she would have argued that a baby’s unconscious contributes to pathology when the baby’s instinctual urges do not get a satisfactory and clearly expressed outlet. Second, the baby needs to be addressed with regard to the underlying emotional muddle and, in doing so, be introduced into the symbolic order. Mother infant psychoanalytic treatment (Norman) The Swedish analyst Norman (2001, p. 85) claimed “(1) that a relationship can be established between the infant and the analyst; (2) that the infant has a primordial subjectivity and self as a basis for intersubjectivity and for the search for containment; (3) that the infant has a unique flexibility in changing representations of self and others that diminishes as the ego develops, and (4) that the infant is able to process certain aspects of language.” Norman’s mother infant psychoanalytic treatment emphasized the infant’s “disability” or ego immaturity, which made the baby prone to become involved in an emotional disturbance with mother—and to look for containment from whoever offered it. This opened a window of chance for undoing the effects of trauma. In therapy Norman addressed the baby—more so than the parents—while disagreeing with Dolto that babies understand the lexical meaning of words. Moreover, Norman worked in lengthy treatments, whereas Dolto worked in brief consultations. Norman (2001) describes a baby girl, Lisa, whose mother became depressed after delivery. Lisa did not recognize her mother when her mother returned from the hospital and avoided her mother’s eyes. Norman told her, “You don’t seem afraid of me when we talk to each other, but I see that you avoid looking at Mother” (p. 89). He then explained to Lisa the events and their emotional impact. He concluded that her mother’s mood improved mainly because Lisa managed to wake her up, which resulted from his containing her pain of separation and dread of rejection. He described a vicious interactive circle: “Lisa’s mother had a psychic pain that she could not bear. As Lisa’s distress and sense of rejection increased her mother’s own distress and pain, the mother was reluctant to open up the emotional links . . . Both . . . appeared to feel threatened by the other’s pain and rejection. They were locked in mutual avoidance” (p. 90). This formulation coincides with Psychodynamic psychotherapy with infants and parents 231 Fraiberg’s and Cramer’s perspectives. While Cramer might focus more on the mother’s narcissistic affront by the child’s rejection, Fraiberg would have recognized Lisa’s avoidance but focused on helping mother understand the “ghosts” that marred her contact with the baby. Unlike most PTIP therapists, Norman rarely used attachment or developmental research concepts, favoring instead Bionian terms such as container/contained and reverie (Bion, 1962). He also used Freud’s term primal repression (Freud, 1915a, 1915b) to explain the incipient psychopathology of the baby. In cases like Lisa’s, unless a PTIP is instituted early, vicious interactions may fossilize into such repressions (Salomonsson, 2014) and create recalcitrant character traits. The infant as subject In Melbourne, PTIP therapists work at the Royal Children’s Hospital (Thomson Salo, 2007). Their work, often with sick babies, resembles Norman’s technique, such as their dialogue with the baby. They “enter treatment through the infant’s world rather than primarily through the parents’ representations” (p. 965) and recognize the baby as a subject. Nevertheless, there are divergences in their infant focus in comparison with Norman’s. Their direct work with the infant does not aim to encourage the baby’s stormy feelings to flourish vis-à-vis both the mother and the therapist. Rather, it aims to enable the parents to see “that their fantasies of having totally damaged or killed off the infant are not reality” (Thomson Salo et al., 1999, p. 59). This comes closer to Fraiberg’s and Cramer’s techniques. They also seem to focus less on the baby’s negative transference than Norman did. Watch, wait, and wonder The WWW technique (Lojkasek et al., 1994) originated among Toronto clinicians who criticized that most PTIP techniques focus on changing the mother’s behavior or representations of her infant. In contrast, their infant-led method is founded in attachment theory, which emphasizes the caregiver’s physical presence with the baby. The mother’s participation is encouraged, as in other PTIP methods, but these authors criticize PTIP methods for overlooking the infant in therapy. In WWW the mother gets down on the floor, observes the baby, and interacts with him or her at the baby’s initiative, almost like play therapy, to gain “insight into the infant’s inner world and relational needs” (Cohen et al., 1999, p. 433). The baby will negotiate “his relationship with his mother, and thus begins to master his environment” (1999, p. 433). The therapist empowers the mother to describe how she experiences her infant, which allows her “to examine her internal working models of her relationship with her infant and to modify or revise them to be more in line with her new experiences” (Lojkasek et al., 1994, p. 214). Though WWW may resemble Norman’s approach, it aims more to provide “a safe, supportive environment. . .. 232 Contemporary Psychodynamic Psychotherapy The mother and the therapist discuss the mother’s observations of her infant’s activity” (Cohen et al., 1999, p. 434). Unlike Norman’s approach, the therapist does not seem to address the baby or interpret the meaning behind the baby’s activity. The Anna Freud Centre PIP team These London clinicians (Baradon, Biseo, Broughton, James, & Joyce, 2016) are also influenced by attachment theory, which they integrate with Freudian metapsychology, infant research, and developmental psychology. Their classical psychoanalytic framework implies that “unconscious material is to be understood and, where appropriate, addressed, because it shapes the way a person functions, both in health and pathology” (p. 52). “The therapy will address impingements of conflict, f/phantasy, negative affect and maladaptive defences” (p. 52). Another psychoanalytic influence is D.W. Winnicott, in that they emphasize his notions such as the good-enough mother and the true self. In their technique they also address the baby, though this seems to occur less insistently than in Norman’s and Dolto’s methods. This certainly does not preclude them from observing the infant’s contact with the therapist and from using countertransference to understand the baby. A recurrent term is scaffolding, whereby “the parent recognises, labels, and structures the baby’s motor, mental and emotional experiences ahead of his capacity to do this himself” (Baradon et al., 2016, p. xxiii). This task falls upon the therapist, too. Baradon et al. concede that “putting such diverse theories together inevitably reveals contradictions and gaps” (p. 3). Their solution is of “roaming between traditions and using each theory as convenient” (p. 3). The method was recently submitted to an RCT (Fonagy, Sleed, & Baradon, 2016). The sample was one of babies with mothers who had mental health problems. No effects between active therapy and routine care were found on infant development, attachment, or dyadic interaction. In contrast, the therapy mothers developed less hostile and helpless representations of their child, and they reported less stress and depression and more warmth toward the child. The impact of the setting and the clinical sample Almost all the authors reviewed above worked in public health clinics. Fraiberg founded a program in Ann Arbor, Michigan, which later moved to San Francisco. Cramer founded a similar center in Geneva. Dolto’s Maisons Vertes, still in operation, are walk-in facilities for brief and improvised psychotherapeutic interventions. Norman started as a consultant at a Child Health Center in Stockholm, but his published cases were derived mainly from private practice. This enabled lengthy highfrequency treatments, which he strongly recommended. The presented methods were thus devised for families from different circumstances. Norman’s and Cramer’s parents seemed reasonably well-motivated and psychologically minded. Psychodynamic psychotherapy with infants and parents 233 In contrast, Fraiberg often treated adolescent or immigrant mothers with a low educational and economic status (Dowling, 1982), similar to the population treated by the London PIP team. The Melbourne therapists treat families with sick children. Such differences in settings and populations may contribute to the parents’ trust in the clinician, motivation for therapeutic work, and means of participating in therapy. This presents a further obstacle in attempting to compare these various approaches of PTIP. Nevertheless, an overview of different theoretical perspectives and technical recommendations can help clinicians grasp the major questions that any approach to PTIP must face. Conclusions Two questions were formulated: (1) Which role does a PTIP mode attribute to a baby in therapy? (2) If it claims to work by helping parents come to grips with their unconscious attitudes toward the baby, does it also speak of unconscious conflicts in the infant? All PTIP therapists wish the baby to be affected by the therapeutic process, and they seek to grasp the baby’s nonverbal communication (Salomonsson, 2007) to help the process evolve. The main dividing line is whether the therapists regard the infant as a catalyst fueling the therapeutic process in the mother, or as someone who wants and needs to communicate with the therapist. In the first model, the therapist will talk to the mother about her baby. The second model will lead the therapist to talk to the baby about the baby’s suffering. As for the second question, no author seems entirely comfortable with attributing to a baby an unconscious in the systematic sense. Norman (2004), however, assumed that the baby “has an unconscious in the dynamic sense of the word” (p. 1107). The two questions are in fact related. The more a therapist highlights unconscious forces at work in a baby, the more she or he will intervene directly with the baby. If the therapist thinks the baby harbors conflicting affects vis-à-vis mother, then addressing both participants seems logical. As illustrated by Norman’s case of Lisa avoiding her depressed mother’s eyes, any PTIP therapist would agree that the mother is caught up in an unconscious conflict with her child. Many, however, would claim that the baby is not capable of a similar conflict. Stern, for example, suggests that early sleep or feeding problems “are not signs or symptoms of any intrapsychic conflict within the infant. . .. They are the accurate reflection of an ongoing interactive reality, manifestations of a problematic interpersonal exchange, not psychopathology of a psychodynamic nature” (Stern, 1985, p. 202, emphasis added). This runs counter to Norman’s argument. When discussing the second question, we must recall that unconscious meanings behind a patient’s symptom cannot be revealed directly; we need a setting in which to interpret them. Therefore mundane observations of babies say nothing for or against the existence of unconscious conflicts. We may observe a crying baby and conclude that he or she is hungry;—so does the mother, who then breast-feeds the baby. If the baby calms down, we will never know whether he or she cried 234 Contemporary Psychodynamic Psychotherapy from hunger or was trapped in an unconscious conflict. Another baby avoids the mother’s eyes, and we infer that the baby is shy. In another interpretation the baby’s avoidance reflects an unconscious conflict with his or her mother, in which case a PTIP therapist may unravel the pertaining affects and fantasies in the mother infant relationship. Sometimes the baby will show that the therapist’s intervention or, expressed more cautiously, the containment has affected the baby beneficially; this can be judged from the baby’s smiling, playing, or laughing and new bodily movements. In other situations the therapist may have identified and formulated aptly a point of intense psychic pain. This can release a breakthrough of affects. The baby might cry and scream, and the mother might become deeply affected. If this is followed up by further containment, that is, compassion and verbal interventions, it can have a dramatic effect on both baby and mother. The baby neither speaks nor understands words but has a mind that seeks to avoid displeasure, experience pleasure, and create relationships to help him or her reach these goals. To achieve such aims is the goal of all the presented PTIP methods, though their arguments and techniques may differ. References Aarts, M. (2000). Marte Meo: Basic manual. Netherlands: Harderwijk. Baradon, T. (Ed.), (2019). Working With Fathers in Psychoanalytic Parent-Infant Psychotherapy (discussants: Björn Salomonsson&Kai von Klitzing). London: Karnac Books. Baradon, T., Biseo, M., Broughton, C., James, J., & Joyce, A. (2016). The practice of psychoanalytic parent-infant psychotherapy - Claiming the baby (2nd ed.). London: Routledge. Bion, W. R. (1962). Learning from experience. London: Karnac Books. Cohen, N. J., Muir, E., Parker, C. J., Brown, M., Lojkasek, M., Muir, R., . . . Barwick, M. (1999). Watch, wait and wonder: Testing the effectiveness of a new approach to mother-infant psychotherapy. Infant Mental Health Journal, 20(4), 429 451. Cramer, B. (1997). The scripts parents write and the roles babies play. Northvale: Jason Aronson Inc. Cramer, B., & Palacio Espasa, F. (1993). La pratique des psychothe´rapies me`res-be´be´s. E´tudes cliniques et techniques (The practice of mother-infant psychotherapies. Clinical and technical studies). Paris: PUF. Dolto, F. (1982). Se´minaires de psychanalyse d’enfant, vol. 1 (Seminars on child psychoanalysis, vol. 1). Paris: Editions du Seuil. Dolto, F. (1985). Se´minaires de psychanalyse d’enfant, vol. 2 (Seminars on child psychoanalysis, vol. 2). Paris: Editions du Seuil. Dolto, F. (1994). Solitude. Paris: Gallimard. Dowling, S. (1982). Review of “Clinical studies in infant mental health. The first year of life”: Edited by Selma Fraiberg. Psychoanalytic Quarterly, 51, 430 434. Emde, R. N. (1990). Mobilizing fundamental modes of development: Empathic availability and therapeutic action. Journal of the American Psychoanalytic Association, 38(4), 881 913. Psychodynamic psychotherapy with infants and parents 235 Espasa, F. P., & Alcorn, D. (2004). Parent-infant psychotherapy, the transition to parenthood and parental narcissism. Journal of Child Psychotherapy, 30(2), 155 171. Ferry, A. L., Hespos, S. J., & Waxman, S. R. (2010). Categorization in 3- and 4-month-old infants: An advantage of words over tones. Child Development, 81, 472 479. Field, T. (2000). Infant massage therapy. In C. H. J. Zeanah (Ed.), Handbook of infant mental health (pp. 494 500). New York: The Guilford Press. Fonagy, P. (1996). Discussion of Peter Wolff’s paper “Infant observation and psychoanalysis”. Journal of the American Psychoanalytic Association, 44(2), 404 422. Fonagy, P., Sleed, M., & Baradon, T. (2016). Randomized controlled trial of parent infant psychotherapy for parents with mental health problems and young infants. Infant Mental Health Journal, 37(2), 97 114. Fraiberg, S. (1980). Clinical studies in infant mental health. New York: Basic Books. Fraiberg, S. (1989). Assessment and therapy of disturbances in infancy. Northvale: Jason Aronson. Freud, S. (1895/1950). Project for a scientific psychology. London: Hogarth Press, SE 1. Freud, S. (1900). The interpretation of dreams. SE 4-5. Freud, S. (1905). Three essays on sexuality (pp. 123 246). SE 7. Freud, S. (1915a). Repression (pp. 141 158). SE 14. Freud, S. (1915b). The Unconscious (pp. 159 216). SE 14. Freud, S. (1925 26). Inhibitions, symptoms and anxiety (pp. 87 178). SE 20. Gervain, J., & Mehler, J. (2010). Speech perception and language acquisition in the first year of life. Annual Review of Psychology, 61, 191 218. Hall, G., Hivernel, F., & Morgan, S. (Eds.), (2009). Theory and practice in child psychoanalysis: An introduction to Françoise Dolto’s work. London: Karnac. Joseph, B. (1985). Transference: The total situation. International Journal of Psychoanalysis, 66, 447 454. Karmiloff, K., & Karmiloff-Smith, A. (2001). Pathways to language. Cambridge, MA: Harvard University Press. Lebovici, S. (2000). La consultation thérapeutique et les interventions métaphorisantes (The therapeutic consultation and the metaphorizing interventions). In M. Maury, & M. Lamour (Eds.), Alliances autour du be´be´. De la recherche à la clinique (pp. 223 243). Paris: PUF. Lebovici, S., & Stoléru, S. (2003). Le nourisson, sa me`re et le psychanalyste. Les interactions pre´coces. (The baby, his mother and the psychoanalyst. Early interactions). Paris: Bayard. Lieberman, A. F., & Van Horn, P. (2008). Psychotherapy with infants and young children Repairing the effects of stress and trauma on early attachment. New York: Guilford Press. Lieberman, A. F., Weston, D. R., & Pawl, J. H. (1991). Preventive intervention and outcome with anxiously attached dyads. Child Development, 62(1), 199 209. Lojkasek, M., Cohen, N. J., & Muir, E. (1994). Where is the infant in infant intervention? A review of the literature on changing troubled mother-infant relationships. Psychotherapy: Theory, Research, Practice, Training, 31(1), 208 220. Manzano, J., Palacio Espasa, F., & Zilkha, N. (1999). The narcissistic scenarios of parenthood. International Journal of Psychoanalysis, 80(3), 465 476. Markova, G., & Legerstee, M. (2006). Contingency, imitation, and affect sharing: Foundations of infants’ social awareness. Developmental Psychology, 42(1), 132 141. McDonough, S. (2004). Interaction guidance. Promoting and nurturing the caregiving relationship. In A. J. Sameroff, S. C. McDonough, & K. L. Rosenblum (Eds.), Treating parent-infant relationship problems (pp. 79 96). New York: The Guilford Press. 236 Contemporary Psychodynamic Psychotherapy Meltzer, D. (1992). The claustrum. Perthshire, Scotland: Clunie Press. Norman, J. (2001). The psychoanalyst and the baby: A new look at work with infants. International Journal of Psychoanalysis, 82(1), 83 100. Norman, J. (2004). Transformations of early infantile experiences. International Journal of Psychoanalysis, 85(5), 1103 1122. O’Shaughnessy, E. (1988). W.R. Bion’s theory of thinking and new techniques in child analysis. In E. Bott Spillius (Ed.), Melanie Klein today. Developments in theory and practice. Volume 2 (pp. 177 190). London: Tavistock/Routledge. Olinick, S. L. (1985). The primary data of psychoanalysis. Contemporary Psychoanalysis, 21, 492 500. Peterfreund, E. (1978). Some critical comments on psychoanalytic conceptualizations of infancy. International Journal of Psychoanalysis, 59, 427 441. Robert-Tissot, C., Cramer, B., Stern, D. N., Serpa, S. R., Bachmann, J.-P., & Palacio-Espasa, F. (1996). Outcome evaluation in brief mother-infant psychotherapies: Report on 75 cases. Infant Mental Health Journal, 17(2), 97 114. Salomonsson, B. (2007). Semiotic transformations in psychoanalysis with infants and adults. International Journal of Psychoanalysis, 88(5), 1201 1221. Salomonsson, B. (2014). Psychoanalytic therapy with infants and parents: Practice, theory and results. London: Routledge. Salomonsson, B. (2017). The function of language in parent-infant psychotherapy. International Journal of Psychoanalysis, 98, 1597 1618. Available from https://doi.org/ 10.1111/1745-8315.12666. Silverman, R., & Lieberman, A. (1999). Negative maternal attributions, projective identification, and the intergenerational transmission of violent relational patterns. Psychoanalytic Dialogues, 9(2), 161 186. Stern, D. N. (1985). The interpersonal world of the infant. New York: Basic Books. Thomson Salo, F. (2007). Recognizing the infant as subject in infant-parent psychotherapy. International Journal of Psychoanalysis, 88, 961 979. Thomson Salo, F., Paul, C., Morgan, A., Jones, S., Jordan, B., Meehan, M., . . . Morse, S. (1999). “Free to be playful”: Therapeutic work with infants. Infant Observation, 31(1), 47 62. Watillon, A. (1993). The dynamics of psychoanalytic therapies of the early parent-child relationship. International Journal of Psychoanalysis, 74, 1037 1048. Winnicott, D. W. (1971). Therapeutic consultations in child psychiatry. London: The Hogarth Press. Zlot, S. (2007). The parenthood conflict in the light of mother-infant psychotherapy. Mellanrummet, 16, 11 22. Child psychodynamic therapy: contemporary trends in treatment development 16 Geoff Goodman1,2 and Nick Midgley3 1 Clinical Psychology Doctoral Program, Long Island University, Brookville, NY, United States, 2Institute for Psychoanalytic Training and Research, NY, United States, 3Anna Freud National Centre for Children and Families, University College London, London, United Kingdom Child psychodynamic therapy (CPDT) has existed at least since Hug-Hellmuth (1921), Klein (1923), and Freud (1928) first began using children’s play as an entrée into children’s internal worlds for therapeutic purposes. Almost 100 years later, the treatment first used by these psychoanalytic pioneers has changed, along with the entire field of psychodynamic therapy (PDT); but for many working in the field of child mental health there is relatively little understanding of contemporary psychodynamic developments. Certainly, there is far less research evaluating the effectiveness of CPDT than evaluating either PDT with adults or other forms of child treatment, such as cognitive-behavioral therapy (CBT). However, a number of narrative reviews of the evidence base have now been published (e.g., Fonagy et al., 2015; Midgley, Ensink, Lindqvist, Malberg, & Muller, 2017; Midgley & Kennedy, 2011; Midgley, O’Keefe, French, & Kennedy, 2017; Palmer, Nascimento, & Fonagy, 2013). Collectively, these reviews offer good preliminary evidence for the value of CPDT. In the only meta-analysis to date (Abbass, Rabung, Leichsenring, Refseth, & Midgley, 2013), short-term CPDT was found to be effective for a wide range of psychiatric diagnoses, including anxiety, emerging borderline personality disorder, depression, eating disorders, and mixed disorders. Short-term CPDT was also associated with persistent changes after termination, leading these authors to conclude that “certain blocks to personal and psychological development are positively affected by these interventions” (Abbass et al., 2013, p. 873). An increasing number of researchers have also been interested in understanding the process of CPDT (for a review, see Midgley, 2007), with studies exploring the mechanisms by which CPDT may work. The recent development of the child psychotherapy process Q-Set (CPQ; Schneider, 2004; Schneider & Jones, 2004) has enabled this area of research to flourish, especially through the medium of empirically informed single-case studies (e.g., Gastaud, Carvalho, Goodman, & Ramires, 2015; Goodman, 2015; Goodman & Athey-Lloyd, 2011; Goodman, Midgley, & Schneider, 2016; Goodman, Reed, & Athey-Lloyd, 2015; Ramires, Carvalho, Schmidt, Fiorini, & Goodman, 2015; Ramires, Godinho, Carvalho, Gastaud, & Contemporary Psychodynamic Psychotherapy. DOI: https://doi.org/10.1016/B978-0-12-813373-6.00016-7 © 2019 Elsevier Inc. All rights reserved. 238 Contemporary Psychodynamic Psychotherapy Goodman, 2017; Ramires, Schwan, & Midgley, 2012; Schneider, Midgley, & Duncan, 2010). In contrast to the flourishing of case study research, one reason for the relative paucity of clinical trials evaluating CPDT has been the reluctance of practitioners to systematize their work in the form of treatment manuals; most new developments are described in the form of narrative case studies or clinical reports. This is partly due to the fear that treatment manuals cannot capture the richness and subtlety of a psychodynamic approach (Wallerstein, 2003), but as a result, it has been harder for contemporary developments in CPDT to be clearly communicated to practitioners working in child mental health and much more challenging to evaluate CPDT approaches using randomized controlled trials (RCTs), in which treatment specification is usually required. Nevertheless, attempts to articulate models of contemporary CPDT in the form of treatment manuals are now increasingly available, and this makes it possible to set out more clearly contemporary developments in clinical practice as well as creating a foundation for future evaluation research. This chapter will therefore present five different manualized CPDTs: supportive expressive play psychotherapy (SEPP) (Kernberg & Chazan, 1991), short-term psychoanalytic child therapy (PaCT) (Göttken & von Klitzing, 2014; Göttken, White, Klein, & von Klitzing, 2014), child and adolescent anxiety psychodynamic psychotherapy (CAPP) (Milrod, Shapiro, Fonagy, & Target, 2009; Milrod et al., 2013; Silver, Shapiro, & Milrod, 2013), regulation-focused psychotherapy for children (RFP-C) (Hoffman, Rice, & Prout, 2016; Prout, Goodman, Hoffman, Rice, & Sherman, 2018), and time-limited mentalization-based treatment for children (MBT-C) (Midgley, Ensink, et al., 2017). In what follows, we present the aims and methods of each of these forms of CPDT, provide an overview of the treatment course, and offer any empirical evidence that currently exists to support its effectiveness. Finally, we will discuss some of the similarities and differences among these five CPDTs and suggest future directions of research. Supportive expressive play psychotherapy SEPP (Kernberg & Chazan, 1991) is perhaps the first published, manualized CPDT in the literature. Designed for school-age children with conduct disorders, SEPP is not time-limited, which sets it apart from the other four manualized CPDTs. Treatment lasts from 3 months to 3 years. SEPP draws on ego psychology and object relations theory as well as attachment theory, temperament theory, and social learning theory. While SEPP is clearly derived from models of supportive expressive psychotherapy used with adults, the approach is adapted to the developmental needs of school-age children and draws on traditional techniques used in CPDT, such as the therapeutic use of play, defense analysis, and the therapist as a “developmental object” (Freud, 1965). The approach is based on the psychodynamic formulation that conduct-disordered children have decoupled their behaviors from Child psychodynamic therapy: contemporary trends in treatment development 239 their mental states; therefore behaviors and mental states need to be connected within the context of a therapeutic play relationship. A “failure in integration between positive and negative states” (Kernberg & Chazan, 1991, p. 7) produces this observed disconnection between cause and effect and the lack of continuity in these children’s interpersonal relationships. The aim of SEPP is to connect “children’s actions . . . to their thoughts, ideas, and feelings” (Kernberg & Chazan, 1991, p. 7). SEPP uses a series of interventions to achieve this integration of mental states and thus a connection of behaviors with mental states that permits greater control over these behaviors. The child’s identification with the therapist’s functions of “monitoring, approving and disapproving” (Kernberg & Chazan, 1991, p. 27) also facilitates ego and superego functioning, which in turn enhances behavioral control. It is hypothesized that through this process, children can increase their awareness of their own perception of their external world and change their behaviors toward it. SEPP uses three categories of interventions to achieve its aims: supportive interventions, expressive interventions, and interpretive interventions. Supportive interventions are designed to facilitate building a therapeutic relationship and strengthening the child’s ego functions. Thus the therapist will supply materials, make suggestions, and explain game rules. Encouragement and empathic comments are also included in this category. For example, a SEPP therapist might introduce a puzzle for a restless child to complete, which represents an alternative activity for the child besides running around the office. Expressive interventions are designed to facilitate the child’s reflection on his own perceptions, feelings, and thoughts; this may be done through comments such as “How did you feel when that happened?” and “How would that approach work?” Finally, interpretive interventions are designed to “focus the child’s attention on events, affects, behaviors and issues and to imply the possibility of new meanings and connections” (Kernberg & Chazan, 1991, p. 15). These interventions can include explanations of how the child protects himself or herself from unacceptable thoughts or feelings (a more traditional CPDT strategy). SEPP progresses through a series of three phases. In Phase 1 the therapist works with the parents to develop a therapeutic alliance and help them to set firm limits on the child’s behavior at home. At the same time, the therapist is working individually with the child to create a nonjudgmental, validating, authentic environment in which rapport can be established through the use of play. In Phase 2 the play becomes more unstructured to allow the child to express his or her thoughts and feelings. In this phase the child gradually learns to understand others’ feelings and intentions and begins to realize that others’ thoughts and behaviors are only loosely connected to his or her own thoughts and behaviors. In Phase 3 the child shifts from fantasy play to reflecting on his or her emotional life. The play becomes more symbolic and open to interpretation. Phase 3 also includes preparing the child and the parents for treatment termination by reviewing the progress made and expressing appreciation to the parents for their collaboration. To accomplish these aims, Kernberg and her colleagues (Kernberg & Chazan, 1991) recommend twice-weekly child sessions and once-weekly parallel sessions 240 Contemporary Psychodynamic Psychotherapy with the parents. The same therapist works with both the child and the parents. In addition, the therapist establishes regular contacts with the child’s schoolteachers and other school personnel to obtain a more comprehensive picture of the child’s behavior in settings other than the home setting. The therapist can discuss with the child pertinent information obtained from these contacts. Modest support exists for SEPP (Eresund, 2007). In a small pretest-posttest study, nine boys ages 6 10 years demonstrated improvement in social functioning, especially for the boys who were not assigned a comorbid diagnosis of attentiondeficit/hyperactivity disorder (ADHD). Collaborative meetings with schoolteachers predicted better treatment outcomes. SEPP was in some respects ahead of its time, developed when there was still a great deal of suspicion and hostility to the idea of manualizing CPDT. Kernberg and Chazan’s (1991) work can now be seen as the first serious attempt to publish a psychodynamic treatment manual for work with school-age children, but its impact on practice and research has not been not as significant as may have been hoped. Short-term psychoanalytic child therapy PaCT (Göttken & von Klitzing, 2014; Göttken et al., 2014) is a new, time-limited manualized CPDT designed for children ages 4 10 years diagnosed with internalizing disorders. Göttken and von Klitzing (2014) and Göttken et al. (2014) also emphasize that therapists can use PaCT with children diagnosed with externalizing behaviors, as long as anxiety or depression underlie these behaviors. PaCT relies on an amalgamation of psychoanalytic theories, including Anna Freudian ego psychology, object relations theory, and mentalization theory espoused by Fonagy, Gergely, Jurist, and Target (2002). The aim of PaCT is to identify and modify the central conflict theme in both intrapsychic mental representations and interpersonal relationships that are believed to underlie the child’s symptoms and potential family dysfunction. Play is the vehicle through which the child and therapist work through this central conflict theme. The authors also claim that, as suggested by Freud (1945), the aim of this treatment is to restore the child’s course of normal development rather than simply to reduce the child’s symptoms. An additional aim is to improve the parents’ insight into the child’s mental states. PaCT uses both clarification and interpretation as the principle methods of achieving its aims. The therapist helps the child to identify his or her and others’ mental states within the play. In contrast to SEPP, which recognizes the importance of identifying and working with the positive transference early in treatment and minimizes identifying and working with the negative transference, PaCT works with the negative transference early in treatment. To guide the therapist’s understanding of the central conflict theme, the therapist must pay close attention to countertransference reactions that serve as nonverbal communication channels coming from the child and parents. This understanding then guides the content of the interpretive strategy. Although PaCT claims to facilitate mentalization capacity in Child psychodynamic therapy: contemporary trends in treatment development 241 the parents as well as the child, the emphasis seems to tilt in favor of exploring conflict rather than enhancing an understanding of the connections among feeling, thinking, and behavior. PaCT progresses through a series of three phases that total 20 25 sessions. In Phase 1 (Sessions 1 5) the therapist works on developing a working alliance with the child as well as the parents. Each session in Phase 1 has a particular focus, such as determining suitability for PaCT (Session 1); working with the parents on obtaining information about the parents, their relationship, and the relationship with the child (Sessions 2 and 3); and an assessment of the child’s self and object representations (Sessions 4 and 5). In these sessions the therapist is also seeking to integrate his or her understanding of the parents’ conflicts with the child’s conflicts. The therapist is attempting to formulate a transgenerational conflict that limits the parents’ understanding of the child. The therapist can then use this formulation in his or her parent collateral sessions. In Phase 2 (Sessions 6 19) the therapist begins communicating the central conflict theme identified in Phase 1 to the child whenever this theme emerges during the child’s play. The therapist and child together test possible solutions to this central conflict theme through the child’s play. In the parent sessions the therapist promotes the parents’ insight into the child’s mental states and their connection to the child’s behaviors. The therapist also focuses on the parents’ own mentalization capacity. Finally, the therapist conveys his or her interpretation of the central conflict theme. In Phase 3 (Sessions 20 25) the therapist enters into the termination phase of treatment by summarizing the work with the child as well as with the parents. The therapist explicitly discusses the child’s and parents’ loss of the therapist as well as fears of living without the therapist. To accomplish these aims, Göttken and von Klitzing (2014) and Göttken et al. (2014) recommend 20 25 weekly child sessions and five or six parallel sessions with the parents (i.e., every fourth child session). As was mentioned earlier, these sessions with parents provide an opportunity for the therapist to address the central conflict theme and its relationship to the child’s symptoms. Modest support exists for PaCT (Göttken et al., 2014). In a small waiting list control study, 27 children ages 4 10 years experienced reductions in internalizing and total problems relative to the waiting list control group; these reductions were also observed at 6-month follow-up. Two-thirds of the PaCT children no longer met formal criteria for an anxiety disorder compared to no children in the waiting list control group. Child and adolescent anxiety psychodynamic psychotherapy CAPP (Milrod et al., 2009, 2013; Silver et al., 2013) is a new, time-limited CPDT designed for children ages 8 16 years diagnosed specifically with generalized 242 Contemporary Psychodynamic Psychotherapy anxiety disorder (GAD), separation anxiety disorder (SAD), or social phobia (SP). The CAPP treatment manual (Milrod et al., 2009) is a modification of the treatment manual for panic-focused psychodynamic psychotherapy-extended range (Busch, Milrod, Singer, & Aronson, 2012; Milrod, Busch, Cooper, & Shapiro, 1997) that also includes a significant influence of mentalization-based treatment (MBT) (Bateman & Fonagy, 2004b). According to Milrod et al. (2013), the aims of CAPP are to “decod[e] emotional meanings of anxiety symptoms and use transference interpretation to illustrate conflicts of separation and attachment in understanding anxiety” (p. 361). Further, the authors rely on the concept of compromise formation—a compromise between unacceptable wishes and defense mechanisms that protect the ego from those wishes—to understand the origin of anxiety, which suggests a series of interpretations to alleviate this anxiety. Unlike other CPDTs reviewed, CAPP does not primarily use play as a vehicle for change, nor does it emphasize parallel sessions with the parents. For example, with younger children the therapist meets with the parents separately because “developing and maintaining an alliance with parents is important,” yet the authors mention nothing else about the work with parents (Silver et al., 2013, p. 87). An additional aim is to improve the child’s mentalization skills, “which allows the child to develop capacities of self regulation, and the ability to envision and think about mental states in oneself and therefore the capacity for empathy and intimacy” (p. 85). CAPP uses a combination of mentalizing interventions and traditional interpretations (including transference interpretations) to achieve its aims. In a concise table Milrod et al. (2013, p. 362) list the probable underlying unique conflicts that accompany GAD, SAD, and SP along with the types of interventions that a therapist would use to target each of these conflicts. For example, SP is understood as a symptom that reflects a conflict between fears of embarrassing oneself and wishes to be the center of attention. The therapeutic strategy would therefore be to “explore defenses against conflicted wishes to stand out . . . and conflicted, unacceptable aggression” (p. 362). On the other hand, SAD is understood as a symptom arising from “conflicts between normal strivings for autonomy and concerns about hurting or infuriating the emotionally-needed parent” (p. 362). The therapeutic strategy in this case would be to “explore transference, an emotionally vibrant paradigm for understanding and altering separation fears” (p. 362). Interestingly, mentalization is not mentioned as a therapeutic strategy for any of the three diagnoses listed in Milrod et al.’s table (p. 362). Like SEPP and PaCT, CAPP progresses through a series of three phases that total 20 24 sessions. In Phase 1 the therapist collects a history from the parents and child and facilitates the unfolding of the narrative of symptoms in the context of the child’s life events. Near the end of Phase 1 the therapist presents the psychodynamic formulation to the child, focusing on the meaning of the symptoms for the child. The therapist also focuses on symptoms, regardless of whether the child brings them up in session (Silver et al., 2013). In Phase 2 the therapist makes interpretations of the meaning of the symptoms that the child brings up. At this time, the therapist looks for signs that the child is beginning to be “reflective and self-observing about anxiety” (Silver et al., 2013, p. 86). Child psychodynamic therapy: contemporary trends in treatment development 243 In Phase 3 the authors note that the specter of termination often produces the rearousal of anxiety symptoms. This rearousal provides the therapist with an opportunity to make transference interpretations, focusing on the underlying ambivalence and rage directed toward the therapist. This process diminishes the tendency to withdraw and fall back into the repetitive anxiety-driven patterns of behavior (Silver et al., 2013). To accomplish these aims, Milrod and her colleagues (Milrod et al., 2009, 2013; Silver et al., 2013) recommend twice-weekly child sessions over 12 weeks. Modest support exists for CAPP (Milrod et al., 2013). In a small pretest-posttest study, nine children ages 8 16 years demonstrated significant, clinically meaningful improvement in the severity of anxiety symptoms and in global functioning. These children maintained these improvements at 6-month follow-up. All nine children were no longer diagnosed with an anxiety disorder at posttest or follow-up. Regulation-focused psychotherapy for children RFP-C (Hoffman et al., 2016; Prout et al., 2018) is a new, time-limited manualized CPDT designed for school-age children diagnosed with externalizing behaviors (oppositional-defiant disorder, conduct disorder, disruptive mood dysregulation disorder, ADHD). RFP-C relies on classic ego psychology (Sigmund and Anna Freud, Berta Bornstein) and object relations theory (Otto and Paulina Kernberg) as well as mentalization theory (Peter Fonagy and Mary Target). The aim of RFP-C is to restore emotion regulation to the child by addressing the child’s defensive maneuvers to avoid painful affects. RFP-C assumes that emotion dysregulation is the driving force behind behavioral dysregulation and that emotion dysregulation occurs when a child avoids awareness of painful affects such as sadness, shame, guilt, and worry. Affective expression through play is the medium through which the therapist makes defense interpretations, which heighten the child’s awareness of these painful affects concealed by the child’s unconscious mind. The therapist also explores with the child alternative ways of coping with these disturbing affects. A second aim of RFP-C is to facilitate the child’s identification of the meaning of the child’s behavior in the context of its appearance. A third aim is to assist the parents in supporting their child in increasing emotion regulation at home by understanding the meaning of the child’s disruptive behaviors. RFP-C organizes its intervention strategy with the child and parents around a trio of questions derived from Malan’s (1979) Triangle of Conflict as adapted by McCullough et al. (2003). These questions address the what, how, and why of the conflict experienced by the child: (1) What is the activating feeling that is being avoided? (2) How is the adaptive feeling being avoided? (3) Why is that feeling being avoided? In other words, what is the excessive inhibitory affect (Hoffman et al., 2016)? The first question is designed to uncover the concealed feeling; the second question is designed to identify the type of defense used against this concealed feeling; and the third question is designed to explore the (irrational) need to avoid or defend against the concealed feeling in the first place. Interestingly, although mentalization skills are not developed in the RFP-C child sessions, the 244 Contemporary Psychodynamic Psychotherapy development of mentalization in the parents is an important aspect of parallel sessions with the parents (Hoffman et al., 2016). The therapist leads the parents in mentalization exercises about their child. Like SEPP, PaCT, and CAPP, RFP-C progresses through a series of three phases that total 16 twice-weekly sessions and four parallel sessions with parents (i.e., every fourth session). These parallel sessions assist the parents in thinking differently about their children’s behaviors as evolving out of unacceptable mental states that the child is defending against. In Phase 1 (Sessions 1 and 2) the therapist engages in both unstructured play (e.g., using Play-Doh, paints, dolls, and/or puppets) and structured play (e.g., drawing a family, a person, or oral story completion) with the child. As much as possible, the therapist allows the child to take the lead in the sessions (Hoffman et al., 2016). In Phase 2 (Sessions 3 11) the therapist attributes meaning to the child’s play, including the ways in which the child avoids certain painful affects aroused by the enacted play themes or the interactions with the therapist. The authors identify common signals from the child when he or she is avoiding painful affects. First, the child might stop talking to the therapist or might avoid play and other types of activity. Second, the therapist might observe a spontaneous change in topic. Third, the therapist might notice an abrupt change in play activity. Fourth, the therapist might become aware of the child’s resistance to exploring the original topic. Fifth, the therapist might observe the child’s denial of the painful affects or the child’s expression of the opposite affects (i.e., reaction formation). Sixth, the therapist might notice the child’s engagement in compulsive rituals to reduce anxiety aroused by exploring the original topic (Hoffman et al., 2016). In Phase 3 (Sessions 12 16) the therapist prepares the child for termination and follows the same steps as in Phase 2 to address directly the painful affects aroused by the impending loss of the therapist. The therapist reviews the gains made by the child with the child as well as with the parents (Hoffman et al., 2016). Findings from a small pilot study indicated that RFP-C led to a decrease in oppositional-defiant symptoms (Prout et al., in prep.). An RCT is currently underway at Ferkauf Graduate School of Psychology to test the effectiveness of RFP-C (Hoffman, personal communication, May 30, 2017). In a study of treatment model prototypes using the CPQ (Prout et al., 2018), RFP-C was highly significantly correlated with both a CPDT prototype (r 5 0.55) and a child reflective functioning prototype (r 5 0.44). In spite of the lack of explicit focus on mentalization in RFP-C child sessions, the correlation with the reflective functioning prototype suggests that it is possible that enhancement of mentalization is an implicit focus of RFP-C child sessions. Time-limited mentalization-based treatment for children MBT-C (Midgley, Ensink, et al., 2017; Midgley, O’Keefe, et al., 2017) is a new, time-limited manualized CPDT designed for children ages 5 12 years with “a range of emotional and behavioral difficulties” (Midgley, Ensink, et al., 2017; Child psychodynamic therapy: contemporary trends in treatment development 245 Midgley, O’Keefe, et al., 2017, p. 65). The MBT-C treatment manual draws theoretical inspiration from the model of MBT created originally for the treatment of adults diagnosed with borderline personality disorder (Bateman & Fonagy, 2004b), as well as aspects of developmental therapy developed by Anna Freud and her colleagues (e.g., Hurry, 1998). The time-limited approach also builds on a number of models of open-ended MBT with children that have previously been developed within the CPDT tradition (Fonagy & Target, 2000; Goodman, 2013a; Perepletchikova & Goodman, 2014; Verheugt-Pleiter, Zevalkink, & Schmeets, 2008; Zevalkink, Verheugt-Pleiter, & Fonagy, 2012). The aim of time-limited MBT-C, which is deliberately transdiagnostic in its focus, is “to help develop and enhance mentalizing processes in the child but also in the parents, which will in turn help the child to become aware of and regulate emotions and/or develop explicit mentalizing skills that can help them manage key difficulties” (Midgley, Ensink, et al., 2017; Midgley, O’Keefe, et al., 2017, p. 68). A second aim of MBTC is “to develop the capacity to recognize, endure, and regulate emotions” (p. 68). This capacity makes it possible for the child to engage in complex social interactions, experience self-control, and foster a coherent sense of self. A third aim of MBT-C is “to strengthen and deepen the child’s ability to form and maintain relationships” (p. 69; italics in original). A fourth aim of MBT-C is “to strengthen [the parents’] parental reflective functioning” (p. 69; italics in original). MBT-C uses a variety of techniques to enhance mentalization. The work of therapy takes place through observations of the therapist patient relationship, focusing on the mental states of therapist and patient and with a particular emphasis given to working from a “mentalizing stance.” The authors suggest a number of techniques that aim to enhance this mentalizing stance, such as “clarifying and naming feeling states,” “stop and rewind,” and “mentalizing the relationship” (Midgley, Ensink, et al., 2017; Midgley, O’Keefe, et al., 2017, pp. 148, 154, 156). In stop and rewind, the therapist invites the child to stop the interaction and reflect on what has just transpired between them, opening up for exploration what both the child and the therapist might have been thinking or feeling. The therapist investigates the interaction in a somewhat naı̈ve way that acknowledges that the child might have perceived the interaction in a way unanticipated by the therapist. The therapist demonstrates an interest in and understanding of the child’s perspective. The therapist works in the here-and-now, placing emotions stimulated by the therapeutic relationship in a context of sequential mental experiences. The authors are careful to distinguish this type of intervention from transference interpretation because the goal is not to provide insight into repetitive patterns of relating but rather to provide an opportunity to explore the mind of the therapist, observe its essential benevolence toward the child, and generalize this process to other interpersonal relationships. Because the approach is informed by developmental research on the capacity to mentalize and the impact of maltreatment and trauma on this capacity, careful attention is paid to support the building blocks of mentalization, such as attention and affect regulation (Zevalkink et al., 2012) as well as noting the points where an emerging capacity to mentalize may break down. 246 Contemporary Psychodynamic Psychotherapy Like SEPP, PaCT, CAPP, and RFP-C, MBT-C progresses through a series of three phases that total 12 sessions. In Phase 1 (Sessions 1 3) the therapist communicates a focus formulation for the treatment (e.g., “‘finding out what chimpanzees need to be proud and happy’”) (Midgley, Ensink, et al., 2017; Midgley, O’Keefe, et al., 2017, p. 129). In Phase 2 (Sessions 4 8) the therapist actively stimulates the mentalizing capacity of both child and parents. In Phase 3 (Sessions 9 12) the therapist explores with the child and parents how best to maintain the gains beyond termination (p. 72). To accomplish these aims, Midgley, Ensink, et al. (2017) and Midgley, O’Keefe, et al. (2017) recommend 12 weekly child sessions and 12 weekly parallel sessions with the parents that coincide with the child sessions to enhance the parents’ own mentalization of themselves and their child. Unlike the other CPDTs, MBT-C also recommends three or four assessment meetings prior to the onset of treatment that yields a mentalizing profile of the child and parents. The therapist then shares this assessment with the child and parents and uses the results to determine suitability for MBT-C and to consider an appropriate treatment focus. The approach also builds in a review meeting after 8 sessions, where there is an option to consider up to two further blocks of 12 sessions, giving some flexibility to the overall length of the therapy. Although there is some preliminary evidence from a small pretest-posttest evaluation for the effectiveness of MBT with families (Keaveny et al., 2012) and schoolage children (Thorén, Pertoft Nemirovski, & Lindqvist, in prep.), the approach has not been tested in clinical trials, although plans are currently underway for further studies. Discussion The five CPDTs reviewed here—SEPP, PaCT, CAPP, RFP-C, and MBT-C—have certain characteristics in common. Other than SEPP, all are short-term and/or timelimited and identify clear “phases” of therapy. Whether this time-limited element is seen as a necessary evil in the era of managed care (Salyer, 2002) or a positive recognition of the effectiveness of short-term interventions (McLaughlin, Holliday, Clarke, & Ilie, 2013), this aspect of these therapies stands in contrast to the tradition of more open-ended, long-term work in CPDT. Nevertheless, all of these CPDTs use psychodynamic principles to stimulate therapeutic change in the child. These principles include letting the child take the lead, focusing on affects (especially painful affects), helping the child to understand the motivation behind his or her own and others’ behavior, working on the here-and-now of the child’s relationship with the therapist, and soliciting the parents’ active involvement in parallel sessions. Although all of these approaches refer back to the main traditions in psychodynamic thinking, such as the work of Anna Freud, Melanie Klein, Donald Winnicott and others, they all tend to be more integrative; in particular integrating the findings Child psychodynamic therapy: contemporary trends in treatment development 247 of developmental (and neuroscientific) research with attachment theory and psychoanalysis as well as features of other forms of child therapy. Three of these five CPDTs (PaCT, CAPP, MBT-C) explicitly rely on mentalization theory to formulate their treatment goals and their underlying theory of change. To what degree is there a shared mechanism of change underlying these different models of contemporary CPDT, or to what degree do they each depend on model-specific therapeutic processes? One hypothesis is that mentalization—the process of interpreting one’s own and others’ behaviors as connected to mental states such as feelings and intentions—is the effective therapeutic ingredient common to all effective psychotherapies (Bateman & Fonagy, 2004a), and this may be especially so in the case of psychodynamic treatments, given the focus on meaning making and unconscious states of mind. According to this hypothesis, “The potential effectiveness of all treatments depends not so much on their frame but on their ability to increase a patient’s capacity to mentalize” (Bateman & Fonagy, 2004a, p. 46). Regarding this hypothesis, analysis of session prototypes of a variety of adult and child treatments ranging from CBT to child-centered play therapy and CPDT indicate that a focus on promoting reflective functioning as the operationalization of the capacity to mentalize is significantly positively correlated with all these prototypes (Goodman, 2013b; Goodman et al., 2016; Prout et al., 2018). A more refined version of this hypothesis, which balances both common and unique factors, draws on the fact that mentalization is a construct that encompasses a number of dimensions: (1) implicit/ explicit, (2) self/other, and (3) cognitive/affective (Choi-Kain & Gunderson, 2008). Goodman et al. (2016) have speculated that different treatment models might enhance different dimensions of mentalization. We might wish to apply these two hypotheses to the five CPDTs reviewed here (three of which explicitly derive inspiration from mentalization theory). Is it possible that the “secret sauce” of all five CPDTs is their effectiveness at enhancing a child’s mentalizing abilities? Or do these five CPDTs go about enhancing different dimensions of mentalization? Goodman et al. (2016) have suggested that while CPDT might enhance self and other mentalization as well as implicit and affective mentalization, CBT might focus on self-mentalization in addition to explicit and cognitive mentalization. Similarly, Hoffman (2015) has suggested that externalizing children exhibit deficits in two domains—negative valence systems and systems for social processes—and that RFP-C addresses primarily the negative valence systems, while MBT-C addresses primarily the systems for social processes. Consistent with this line of thinking, is it possible that especially RFP-C and CAPP, but also PaCT and SEPP, primarily promote implicit, affective, and other dimensions of mentalization, while MBT-C primarily promotes explicit, cognitive, and self dimensions of mentalization? A related hypothesis concerns the clinical techniques used to enhance these mentalizing processes in children with various diagnostic profiles (e.g., externalizing or internalizing behaviors). For example, RFP-C purportedly targets the defensive processes that prevent the externalizing child from mentalizing his or her own affects, which is understood to reestablish affect regulation. In a sense, one could view RFP-C as a form of graduated exposure to unpleasant affects that gradually become 248 Contemporary Psychodynamic Psychotherapy metabolized. By contrast, MBT-C purportedly targets the inhibitions in thinking about others’ (and the child’s own) thoughts about affects and behaviors and their connections to each other, which is also understood to reestablish affect regulation. Under what set of conditions each set of techniques is most therapeutic (e.g., child’s diagnostic profile, length of treatment, child’s developmental level) remains an unanswered question. Psychotherapy researchers can empirically test these hypotheses, but we first need valid coding systems that can reliably measure Choi-Kain and Gunderson’s (2008) three dimensions of mentalizing (and other as yet unidentified dimensions) in various psychotherapy settings. Therapists could use such instruments to highlight specific mentalization deficits in children seeking treatment, as well as determine which CPDTs are best suited for which children. Finally, additional laboratory and naturalistic studies need to be completed to test the effectiveness of these five CPDTs, which are all based on strong conceptual foundations and integrate knowledge from developmental research with clinical wisdom but as yet have only minimal evidence of clinical- or cost-effectiveness. According to the National Registry of Evidence-Based Programs and Practices (n.d.) (http://nrepp.samhas. gov), none of these CPDTs yet qualifies as a program with “effective” or “promising” outcomes. The current generation of CPDT therapists and researchers need to take on the challenge of establishing and promoting the evidence base if a case is to be made for the contemporary relevance of psychodynamic thinking to therapeutic work with children. Author note The authors wish to thank Sarah Angeli and Jesse Silberstein for their assistance with manuscript preparation. Valeda Dent assisted with locating references. References Abbass, A. A., Rabung, S., Leichsenring, F., Refseth, J. S., & Midgley, N. (2013). Psychodynamic psychotherapy for children and adolescents: A meta-analysis of shortterm psychodynamic models. Journal of the American Academy of Child and Adolescent Psychiatry, 52, 863 875. Bateman, A. W., & Fonagy, P. (2004a). Mentalization-based treatment of BPD. Journal of Personality Disorders, 18, 36 51. Bateman, A. W., & Fonagy, P. (2004b). Psychotherapy for borderline personality disorder: Mentalization-based treatment. Oxford: Oxford University Press. Busch, F., Milrod, B., Singer, M., & Aronson, A. (2012). Panic Focused Psychodynamic Psychotherapy: eXtended Range: Psychodynamic psychotherapy for anxiety disorders: A transdiagnostic treatment manual. New York/Hove: Taylor & Francis. Child psychodynamic therapy: contemporary trends in treatment development 249 Choi-Kain, L. W., & Gunderson, J. G. (2008). Mentalization: Ontogeny, assessment, and application in the treatment of borderline personality disorder. American Journal of Psychiatry, 165, 1127 1135. Eresund, P. (2007). Psychodynamic psychotherapy for children with disruptive disorders. Journal of Child Psychotherapy, 33, 161 180. Fonagy, P., Cottrell, D., Phillips, J., Bevington, D., Glaser, D., & Allison, E. (2015). What works for whom? A critical review of treatments for children and adolescents (2nd ed.). New York: Guilford Press. Fonagy, P., Gergely, G., Jurist, E. L., & Target, M. (2002). Affect regulation, mentalization, and the development of the self. New York: Other Press. Fonagy, P., & Target, M. (2000). Mentalization and personality disorder in children: A current perspective from the Anna Freud Centre. In T. Lubbe (Ed.), The borderline psychotic child: A selective integration (pp. 69 89). London: Routledge. Freud, A. (1928). The theory of child analysis, . The writings of Anna Freud (Vol. 1, pp. 162 175). New York: International Universities Press, 1974. Freud, A. (1945). Indications for child analysis. The Psychoanalytic Study of the Child, 1, 127 149. Freud, A. (1965). Normality and pathology in childhood: Assessments of development. New York: International Universities Press. Gastaud, M. B., Carvalho, C., Goodman, G., & Ramires, V. R. R. (2015). Assessing levels of similarity to a “psychodynamic prototype” in psychodynamic psychotherapy with children: A case study approach (preliminary findings). Trends in Psychiatry and Psychotherapy, 37, 161 165. Goodman, G. (2013a). Encopresis happens: Theoretical and treatment considerations from an attachment perspective. Psychoanalytic Psychology, 30, 438 455. Goodman, G. (2013b). Is mentalization a common process factor in transference-focused psychotherapy and dialectical behavior therapy sessions?. Journal of Psychotherapy Integration, 23, 179 192. Goodman, G. (2015). Interaction structures between a child and two therapists in the psychodynamic treatment of a child with borderline personality disorder. Journal of Child Psychotherapy, 41, 141 161. Goodman, G., & Athey-Lloyd, L. (2011). Interaction structures between a child and two therapists in the psychodynamic treatment of a child with Asperger’s disorder. Journal of Child Psychotherapy, 37, 311 326. Goodman, G., Midgley, N., & Schneider, C. (2016). Expert clinicians’ prototypes of an ideal child treatment in psychodynamic and cognitive-behavioral therapy: Is mentalization seen as a common process factor?. Psychotherapy Research, 26, 590 601. Goodman, G., Reed, P., & Athey-Lloyd, L. (2015). Mentalization and play therapy processes between two therapists and a child with Asperger’s disorder. International Journal of Play Therapy, 24, 13 29. Göttken, T., & von Klitzing, K. (2014). Manual for short-term psychoanalytic child therapy (PaCT). London: Karnac. Göttken, T., White, L. O., Klein, A. M., & von Klitzing, K. (2014). Short-term psychoanalytic child therapy for anxious children: A pilot study. Psychotherapy, 51, 148 158. Hoffman, L. (2015). Mentalization, emotion regulation, countertransference. Journal of Infant, Child, and Adolescent Psychotherapy, 14, 258 271. Hoffman, L., Rice, T., & Prout, T. (2016). Manual of regulation-focused psychotherapy for children (RFP-C) with externalizing behaviors: A psychodynamic approach. London and New York: Routledge. 250 Contemporary Psychodynamic Psychotherapy Hug-Hellmuth, H. V. (1921). On the technique of child-analysis. International Journal of Psycho-Analysis, 2, 287 305. Hurry, A. (1998). Psychoanalysis and developmental therapy. London: Karnac Books. Keaveny, E., Midgley, N., Asen, E., Bevington, D., Fearon, P., Fonagy, P., & Wood, S. (2012). Minding the family mind: The development and initial evaluation of mentalization-based treatment for families. In N. Midgley, & I. Vrouva (Eds.), Minding the child: Mentalization-based interventions with children, young people and their families (pp. 98 112). London: Routledge. Kernberg, P. F., & Chazan, S. E. (1991). Children with conduct disorders: A psychotherapy manual. New York: Basic Books. Klein, M. (1923). The development of a child. International Journal of Psycho-Analysis, 4, 419 474. Malan, D. (1979). Individual psychotherapy and the science of psychodynamics. London: Butterworth. McCullough, L., Kuhn, N., Andrews, S., Kaplan, A., Wolf, J., & Hurley, C. L. (2003). Treating affect phobia: A manual for short-term dynamic psychotherapy. New York: Guilford Press. McLaughlin, C., Holliday, C., Clarke, B., & Ilie, S. (2013). Research on counselling and psychotherapy with children and young people: A systematic scoping review of the evidence for its effectiveness from 2003 2011. Leics: BACP. Midgley, N. (2007). Researching the process of psychoanalytic child psychotherapy. In E. Kennedy, & N. Midgley (Eds.), Process and outcome research in child, adolescent and parent-infant psychotherapy (pp. 8 53). London: North Central London Strategic Health Authority. Midgley, N., Ensink, K., Lindqvist, K., Malberg, N., & Muller, N. (2017). Mentalizationbased treatment for children: A time-limited approach. Washington, DC: American Psychological Association. Midgley, N., & Kennedy, E. (2011). Psychodynamic psychotherapy for children and adolescents: A critical review of the evidence base. Journal of Child Psychotherapy, 37, 232 260. Midgley, N., O’Keefe, S., French, L., & Kennedy, E. (2017). Psychodynamic psychotherapy for children and adolescents: An updated narrative review of the evidence base. Journal of Child Psychotherapy, 43(3), 307 329. Milrod, B., Busch, F., Cooper, A., & Shapiro, T. (1997). Manual of panic-focused psychodynamic psychotherapy. Arlington, VA: American Psychiatric Publishing. Milrod, B., Shapiro, T., Fonagy, P., & Target, M. (2009). CAPP manual. Unpublished manuscript, Weill Cornell Medical College, New York. Milrod, B., Shapiro, T., Gross, C., Silver, G., Preter, S., Libow, A., & Leon, A. C. (2013). Does manualized psychodynamic psychotherapy have an impact on youth anxiety disorders? American Journal of Psychotherapy, 67, 359 366. National Registry of Evidence-Based Programs and Practices. (n.d.). Retrieved from ,http:// nrepp.samhsa.gov/landing.aspx.. Palmer, R., Nascimento, L. N., & Fonagy, P. (2013). The state of the evidence base for psychodynamic psychotherapy for children and adolescents. Child and Adolescent Psychiatric Clinics of North America, 22, 149 214. Perepletchikova, F., & Goodman, G. (2014). Two approaches to treating preadolescent children with severe emotional and behavioral problems: Dialectical behavior therapy adapted for children and mentalization-based child therapy. Journal of Psychotherapy Integration, 24, 298 312. Child psychodynamic therapy: contemporary trends in treatment development 251 Prout, T. A., Goodman, G., Hoffman, L., Rice, T., & Sherman, A. (2018). Expert clinicians’ prototype of an ideal treatment in Regulation Focused Psychotherapy for Children (RFP-C). Journal of Psychotherapy Integration, 28, 401 412. Prout, T. A., Rice, T., Murphy, S., Gaines, E., Aizin, S., Stein, D., & Hoffman, L. (in prep.). Regulation Focused Psychotherapy for Children (RFP-C) Preliminary results of a new treatment approach for treatment resistant externalizing behaviors. Ramires, V. R. R., Carvalho, C., Schmidt, F. M. D., Fiorini, G. P., & Goodman, G. (2015). Interaction structures in the psychodynamic therapy of a boy diagnosed with Asperger’s disorder: A single-case study. Research in Psychotherapy: Psychopathology, Process and Outcome, 18, 129 140. Ramires, V. R. R., Godinho, L. B. R., Carvalho, C., Gastaud, M., & Goodman, G. (2017). Child psychoanalytic psychotherapy process: A single case study. Psychoanalytic Psychotherapy, 31, 75 93. Ramires, V. R. R., Schwan, S., & Midgley, N. (2012). Mentalization-based therapy with maltreated children living in shelters in southern Brazil: A single case study. Psychoanalytic Psychotherapy, 26, 308 326. Salyer, K. (2002). Time limited therapy: A necessary evil in the managed care era? Reformulation, Autumn, 9 11. Schneider, C. (2004). The development of the Child Psychotherapy Q-Set (Doctoral dissertation). University of California, Berkeley (Dissertation Abstracts International, 65(2-B), 1039). Schneider, C., & Jones, E. E. (2004). Child Psychotherapy Q-Set coding manual. Berkeley: University of California, Unpublished manuscript. Schneider, C., Midgley, N., & Duncan, A. (2010). A “motion portrait” of a psychodynamic treatment of an 11-year-old girl: Exploring interrelations of psychotherapy process and outcome using the Child Psychotherapy Q-Set. Journal of Infant, Child and Adolescent Psychotherapy, 9, 94 107. Silver, G., Shapiro, T., & Milrod, B. (2013). Treatment of anxiety in children and adolescents: Using the child and adolescent anxiety psychodynamic psychotherapy (CAPP) therapy. Child and Adolescent Psychiatric Clinics of North America, 22, 83 96. Thorén, A., Pertoft Nemirovski, J., & Lindqvist, K. (in prep.). Short-term mentalizationinformed psychotherapy. A way of treating common childhood mental disorders. Verheugt-Pleiter, A. J. E., Zevalkink, J., & Schmeets, M. G. J. (Eds.), (2008). Mentalizing in child therapy: Guidelines for clinical practitioners. London: Karnac Books. Wallerstein, R. S. (2003). Psychoanalytic therapy research: Its coming of age. Psychoanalytic Inquiry, 23, 375 404. Zevalkink, J., Verheugt-Pleiter, A. J. E., & Fonagy, P. (2012). Mentalization-informed child psychoanalytic psychotherapy. In A. Bateman, & P. Fonagy (Eds.), Handbook of mentalizing in mental health practice (pp. 129 158). Arlington, VA: American Psychiatric Publishing. Further reading Midgley, N., & Vrouva, I. (Eds.), (2012). Minding the child: Mentalization-based interventions with children, young people and their families. New York: Routledge. Whitaker, R. B. (2012). Anatomy of an epidemic: History, science, and the case against psychiatric drugs. In N. A. Cummings, & W. O’Donohue (Eds.), Restoring psychotherapy as the first line intervention in behavioral care (pp. 179 222). Dryden, NY: Ithaca Press. Psychodynamic psychotherapy for adolescents 17 Dana Atzil-Slonim Psychology Department, Bar-Ilan University, Ramat Gan, Israel According to the World Health Organization (2013), 20% of all adolescents, globally, experience a mental health problem every year. Adolescents’ mental health problems have important implications for all facets of their lives, including their ability to study, engage in social life, and find their own way in the world (Midgley, O’Keeffe, French, & Kennedy, 2017). Adolescent psychotherapy research has advanced considerably in the last two decades (cf., Midgley et al., 2017), but compared to the abundance of literature on adult psychotherapy, adolescent psychotherapy still lags far behind. Adolescence is a period of transformation from childhood and preparation for adulthood. It is a developmental period characterized by a large number of biological, psychological, and social changes. The combination of these factors makes this period extremely important yet also very challenging. Psychodynamic theoreticians have described the developmental challenges that characterize this phase as well as the possibilities for growth and change through psychotherapy for adolescents who experience difficulties during this critical stage of development. This chapter focuses on adolescent psychodynamic psychotherapy. The first part of the chapter provides a brief overview of psychodynamic theories of adolescence, from the early days of psychoanalysis to more contemporary views. The second part of the chapter describes psychodynamic psychotherapy in practice. The third part of the chapter reviews recent findings from psychodynamic psychotherapy research on adolescents. The fourth part of the chapter includes a short case illustration, which describes the process of change of one adolescent in psychodynamic psychotherapy. Psychodynamic theories of adolescence Psychodynamic psychotherapy with adolescents draws on psychoanalytic ideas while integrating concepts from other disciplines, including developmental psychology and attachment theory (Lanyado & Horne, 2009). Although the term psychodynamic psychotherapy covers a range of approaches, most share the central idea that the adolescent’s problems make some kind of emotional sense. Their roots lie in the internal world of adolescents that builds up from their earliest experiences and relationships. Contemporary Psychodynamic Psychotherapy. DOI: https://doi.org/10.1016/B978-0-12-813373-6.00017-9 © 2019 Elsevier Inc. All rights reserved. 254 Contemporary Psychodynamic Psychotherapy Classical psychodynamic perspective of adolescence Classical Freudian theory paid relatively little attention to adolescent development and discussed it solely in terms of psychosexual development. In “Three Essays on Sexuality,” a chapter devoted to puberty, Freud (1905) described adolescence as a period of transition between diffuse infantile and genitally centered adult sexuality. According to Freud, the main events in this process are the subordination of the erogenous zones to the genital zone, the setting up of new sexual aims (different for males and females), and the finding of new sexual objects outside the family. Anna Freud (1958) further developed these ideas and described the adolescent as primarily engaged in an emotional struggle of extreme urgency and immediacy. In her view, the threat to ego integrity derived from both the strength of pubertal drives and the regressive pull toward the objects of infancy and childhood. Her emphasis was on adolescent defenses that protect the ego from being overwhelmed by anxiety caused by the impulses of the id and love objects in the individual’s oedipal and preoedipal past. Blos (1967) amplified one of Anna Freud’s themes by emphasizing the way in which the adolescent disengages from the internalized love and hate objects of childhood in order to find extrafamilial love and hate objects in the external world. Blos defined his concept of adolescence as a second individuation process in which the adolescent sheds family dependencies and loosens infantile object ties to become an individuated adult member of society. Throughout this demanding process, the adolescent longs for comfort from infantile objects but at the same time fears reinvolvement with these objects. Blos viewed ego regression as an essential component in the progressive development of the adolescent. Erikson (1968) described adolescence as the period during which the individual must establish a sense of personal identity. Adolescents must find answers to questions about where they came from, who they are, and what they will become. The rebellion against parents that characterizes this period is intended to help adolescents clarify their distinct identity. During this period, the peer group serves as a key important factor in helping adolescents formulate their own identity and define who they are. The need for extrafamilial relationships to cope with transformation in relationships with parents is emphasized as well in the self psychology literature on adolescence. Following Kohut’s lead, Wolf, Gedo, and Terman (1972) suggested that one of the most upsetting and painful processes of adolescence is the transition from the need to have the parent function as an idealized selfobject (a figure whose presence, power, wisdom, or goodness contributes to one’s sense of self) to disillusionment with the parent as an ideal. Parallel to adolescents’ growing ability to view their parents more realistically, there is a need for substitute idealized selfobjects such as peers, cult heroes, and ideologies. Winnicott (1971) broadened the idea of the evolving experience of self in adolescence and the importance of the surroundings in its development by relating to adolescence as a world unto itself with its own unique dynamics. His main emphasis was upon acknowledging the authenticity of the troubling and distressing Psychodynamic psychotherapy for adolescents 255 psychological states that emerge during this period of life. According to Winnicott (1971, p. 146), adolescents “struggle to feel real” and reject society’s false solutions: “Immaturity is a precious part of the adolescent scene. In this is contained the most exciting features of creative thought, new and fresh feelings, ideas for new living. Society needs to be shaken by the aspirations of those who are not responsible”. Winnicott also highlighted the function of aggression and destruction in the maturational process. If the other survives without retaliating or withdrawing under attack, the adolescent can start to know the other as a person with his or her own subjectivity. Relational psychodynamic theoreticians have further developed Winnicott’s notions and emphasized the importance of the object’s survival in the face of adolescents’ destruction (e.g., Benjamin, 1995). According to Benjamin (1995), when an adolescent’s destructiveness damages neither the parent nor the self, external reality comes into view as a sharp, distinct contrast to the inner fantasy world. The outcome of this process is not simply reparation or restoration of the good object, but love, the sense of discovering and recognizing the other. Contemporary psychodynamic perspective of adolescence The more contemporary relational perspective of adolescence (e.g., Briggs, Maxwell, & Keenan, 2015; Levy-Warren, 2000) differs in several ways from earlier psychodynamic views. The centrality of relationships The relational perspective emphasizes that development occurs through participation in an expanding series of interpersonal fields. While the classical psychoanalytic view tends to emphasize that the main goal in adolescence is to achieve autonomy and independence (Schafer, 1973), the relational theory views individuals as interdependent at every stage of life and posits that only the dimension of connectedness evolves. The internal representations of the child parent relationship and the relationship itself are continuously revised and reorganized throughout childhood. Adolescence merely continues this process at an accelerated pace. Individuals who successfully traverse adolescence still need and make use of the continuing relationship to their parents but need less frequent direct contact and help and are more capable of using the parental relationship as an inner resource. Therefore the adolescent’s assertive desire to make decisions and establish greater privacy and freedom from supervision is seen not as striving for autonomy but as striving for a new kind of relating. The increased level of parent child conflicts during adolescence is seen as normative ambivalence toward change and a negotiation about the new form of relating that is being created by both parties. Thus the essence of adolescents’ new relational needs consists of being known and recognized by others at a time when the adolescents are learning to know and recognize themselves. To be known by another, one must know oneself. It is only then that individuals can be sure that what others know about them feels real (LevyWarren, 2000). Feeling known is a critical component of intimacy. Lack of 256 Contemporary Psychodynamic Psychotherapy fulfillment of the need for intimacy creates loneliness, which can be one of the most painful of all states. Individual and contextual differences Relational theories on development take into account the multiple forces that interact and create a very different experience of growth for each individual. It is not just individual differences that determine whether adolescence is turbulent or proceeds in a smooth transition to adulthood, but rather the social context in which some groups are more vulnerable than others especially in terms of race, gender, class, and sexuality. Multiplicity versus singularity of the self According to the relational view, progress and development are achieved through the growing ability to tolerate experiencing multiple versions of oneself alongside a sense of continuity and integrity of the self. Within this approach, psychopathology is viewed as narrowness in perception, that is, a tendency to truncate new experiences into rigid stereotyped patterns (Mitchell, 1993). Although an important component of adolescent development is defining the sense of self and relationships to know who one really is, it is equally important for adolescents to be able to move between different states of mind in their relationships to themselves and others (Briggs, 2002). The ability to sustain negative thoughts and feelings The relational view highlights the importance of tolerating negative experiences in order to be able to change and grow (Ogden, 2005). Adolescents need to make use of the resources provided in childhood to understand, make sense of, and contain the impact of anxiety, conflict, ambiguity, and uncertainty of their ongoing internal changes. If the adolescent and the primary caregiver can tolerate the negative experiences that accompany change, the quality of turbulence is transformed (Briggs, 2002). The struggle between the need to grow and the fear to change At every period of developmental transition there is always an inner conflict between the need to develop and the dread of change (Mitchell, 1993). In adolescence the rapidity of change guarantees that there will be some vacillation between wanting to be treated like the grown-up one is becoming and wanting to be treated like the child one does not want to leave behind. Still, in most cases, forward movement will never stop for long. When anxiety severely prevents adolescents from accessing their inner resources or if there is a persisting sense of unmet needs in past and present relationships, forward movement may be blocked. This indicates a deviation from a healthy developmental path, which may lead to the need for treatment. Psychodynamic psychotherapy for adolescents 257 Psychodynamic practice with adolescents The psychodynamic conceptualizations of adolescence described above serve as guideposts for adolescent psychotherapy, which is one of the great challenges for therapists, since it involves formulating an intervention for an individual in transition. In adolescent psychodynamic psychotherapy the central goal is to help the teenager return to the path of normal development and mastery of age-appropriate tasks (Lanyado & Horne, 2009). To encourage optimal psychic functioning in harmony with the self and the client’s social world, psychodynamic psychotherapy aims to help the adolescent develop the capacity to tolerate painful emotions, which are known to be intensified during this period (Briggs, Maxwell, & Keenan, 2015). Successful treatment should not only relieve symptoms but also foster the positive presence of psychological capacities and resources. Depending on the adolescent and the circumstances, these might include the capacity to have more fulfilling relationships, make more effective use of one’s talents and abilities, maintain a realistically based sense of self-esteem, tolerate a wider range of affect, understand the self and others in more nuanced and sophisticated ways, and face life’s challenges with greater freedom and flexibility. The course of psychotherapeutic work with adolescents is widely acknowledged to be difficult, ambiguous, and challenging. Adolescents contribute unique attributes to the therapy process that distinguish them from other therapy populations (Briggs, Maxwell, & Keenan, 2015). Adolescents are usually referred to treatment by parents, teachers, or counselors and rarely seek help on their own initiative. Frequently, adolescents are at odds with their referrers about what the goals of therapy should be (Kazdin, 2004). The very nature of adolescent development, which includes a tendency toward impulsive behavior rather than being reflective, often means that the length of treatment is unpredictable. Adolescents tend to have an ambivalent attitude toward treatment, and dropout rates within this age group are relatively high (Kazdin, 2004). A brief description of the main characteristics of psychodynamic psychotherapy with adolescents is provided below. Establishing and maintaining a therapeutic relationship with adolescents Forming positive therapeutic relationships with adolescents can pose a formidable challenge to therapists (Marks-Mishne, 2010). As the young person is attempting to separate from the family, form an identity, and make important peer attachments, he or she is often reluctant to enter into a relationship and form attachments with a new adult. Some adolescents cannot enter therapy and sustain an alliance because of an overpowering wish to keep their private life private. Some are fearful of sharing sexual and masturbatory fantasies. Others are mortified by shame, envy, and profound self-consciousness and are oblivious to the universality of the ageappropriate anxiety that burdens them. Fear of therapy, of a new powerful adult and the discovery of one’s inner troubled self, is generally much stronger than the wish 258 Contemporary Psychodynamic Psychotherapy for assistance. Many authors concur that significant modifications of technique are usually necessary in applying psychodynamically oriented psychotherapy with adolescents (e.g., Lanyado & Horne, 2009; Marks-Mishne, 2010). For example, the unstructured invitation “to say everything that comes to mind” and a passive silence during the therapeutic hour may be anxiety-provoking for adolescents. Often, therapists take on a more active role in treatment with adolescents than they would with adults (Shefler, 2000). Empathic warmth, active attentive listening, active participation, and a respectful attitude are considered essential to the formation of a positive therapeutic relationship with adolescents (Marks-Mishne, 2010). The transference countertransference relationship In adolescent psychodynamic psychotherapy, perhaps more than in therapy for any other client population, the main crucible for new experiences is the work associated with the therapeutic relationship (Karver, Handelsman, Fields, & Bickman, 2006). The main emphasis is on generalizing the adolescent’s new experiences developed in the therapeutic relationship to relationships with others outside therapy (Levy-Warren, 2000). Through the relationship with the therapist in a consistent setting, adolescents may begin to feel able to express their most troubling thoughts and feelings. Confused, frightened, hurt, angry, or painful feelings can gradually be put into words rather than actions. The therapist can help adolescents make sense of their own experience and develop their own individuality and potential. The adolescent’s sense of who he or she is and how others will react to him or her are very much affected by expectations based on past and present family relationship. Throughout treatment the transference countertransference relationship becomes a representative sample of adolescents’ ways of relating to the people who are important to them. As a result, specific anxieties and painful conflicts come alive and can be worked with, sometimes at first within the contained context of the therapeutic relationship. The emotional changes resulting from the working through of these issues gradually become more generalized and a part of the adolescent’s repertoire in everyday relationships (Lanyado & Horne, 2009). Many other aspects of ordinary developmental processes can be experienced within the therapeutic relationship. For example, a patchy pattern of attendance at therapy in which helpful and fruitful sessions are interspersed with sessions missed without explanation may express the back-and-forth dynamic of the need to gain more autonomy while staying related in the relationship with parents as well as the internal war between wanting to move forward and wanting to stay the same. Adolescents often elicit complex feelings and reactions in the therapist because of the tensions and ambiguities that characterize this age period, which involve mixed emotions, thoughts and actions about separateness and intimacy, independence and dependence, the need to grow and the fear of change—all of which can become easily confused and confusing (Briggs, Maxwell, & Keenan, 2015). In working with adolescents, an important path to the heart of the work, in which new possibilities for listening and understanding can arise, is through the therapists’ analysis of their own countertransferential responses. The exploration of the Psychodynamic psychotherapy for adolescents 259 particular qualities of the transference countertransference relationship helps the therapist know more about the client’s fantasies, relationships, functioning, and expectations. In this way the therapist’s emotions and reactions to the client are viewed as valuable assets in providing guidance to deal with taxing treatment dilemmas. Commonly, a frank and nonanxious examination of feelings facilitates the resolution of various therapeutic impasses (Lanyado & Horne, 2009). The most important growth that leads to deep change in the client’s relationships and internal world is gained from what happens in the consulting room, in the here-and-now of the meeting of two people: the therapist and the adolescent. It is important to bear in mind that alongside the transference countertransference relationship between the client and the therapist, there will always be a real relationship between them, as reflected in the degree to which each is genuine with the other and perceives the other in ways that befit the other (Gelso, 2011). Adolescents need the therapist to be a separate object with whom they can identify and negotiate their evolving separate identity (Erlich, 1993). Therapists cannot replace the significant others with whom adolescents live their lives. However, they can provide a new relationship experience that can be generalized and open up new possibilities with others in the adolescent’s world, particularly with regard to parents. Anxieties and defenses Anxieties in adolescence can stem from a variety of sources including the changing body, the need to redefine the sense of self and identity, the need to redefine old and present relationships, and the need to create intimacy. Increased anxiety leads to the use of a range of defenses, some of which are considered more adaptive while others can be destructive, depending on the extremeness and rigidity in which they are applied. When distressing feelings come alive within the therapeutic relationship, treatment can sometimes be painful. In working with defenses in therapy, there are two aims: to explore the defenses that are neither age appropriate nor helpful and to increase the range of appropriate defenses available to the adolescent for coping with unbearable anxiety or emotional pain. In addition, anxiety—in all its irrationality—needs to be faced gradually and made sense of within an attentive, holding relationship (Horne, 2001). The dialectic between internal and external worlds The dynamic interaction between people’s experience of their internal world and the external world, which includes the client’s real relationships outside therapy, is pivotal in psychodynamic psychotherapy with adolescents. Obviously, the internal and external worlds affect each other. The external world is perceived through the eyes of the internal world filter, which in turn is affected by what has actually happened in the external world. In a traditional, open-ended, psychoanalytic treatment the outside world is often in the background; however, in therapy with 260 Contemporary Psychodynamic Psychotherapy adolescents, family dynamics are frequently so complex and intertwined that to treat this age group effectively, therapists must be open to the possibility that involving the family might at times be not only recommended but absolutely essential to facilitate an effective outcome (Cohen, 2005). This requires the therapist to find a balance between the opposing but complementary forces of the individual and the family. Both parents and adolescents oscillate between separation and maintaining closeness, between wanting to find new ways to relate and wanting to stay the same. If the therapist can help the adolescent tolerate experiences of uncertainty, anxiety, change, and ambiguity—and if the adolescent’s environment can be encouraged to support this process—the quality of internal and external conflicts can be transformed (Briggs, 2002). Since internalization processes are still under construction and the real objects are very present in the client’s life, changes achieved through psychotherapy with adolescents can have a crucial influence both on the consolidation of internal representations and on actual relationships, especially with parents. Psychodynamic psychotherapy research on adolescents Research on adolescents’ psychodynamic psychotherapy has advanced considerably in the past two decades (cf. Midgley et al., 2017). This is particularly noteworthy because adolescent therapy research, in sharp contrast to research on adult psychotherapy, received little attention for many years. Recent reviews of the literature (Abbass, Rabung, Leichsenring, Refseth, & Midgley, 2013; Midgley et al., 2017; Palmer, Nascimento, & Fonagy, 2013) underscore the effectiveness of psychodynamic psychotherapy for adolescents for a wide range of disorders. These reviews also suggest that adolescents with emotional or internalizing disorders seem to respond better to psychodynamic psychotherapy than do adolescents with disruptive or externalizing disorders. Adolescents with more disruptive disorders are more difficult to engage and more likely to drop out of psychodynamic treatment, but there is evidence that when they engage in treatment, it can be effective and that the frequency of treatment may be important. Another consistent finding is the notion of a sleeper effect, in which the gains from therapy continue to increase after the end of therapy. Effectiveness studies constitute an important step in confirming the validity and usefulness of psychodynamic psychotherapy for adolescents. However, researchers have argued that to better understand how and why psychodynamic psychotherapy works, relying solely on effectiveness studies would be accepting too narrow a definition of research (e.g., Kazdin, 2004). This has triggered a heated debate on the methodologies needed to better study what works for whom in psychodynamic psychotherapy for young people (e.g., Fonagy, Target, Cottrell, Phillips, & Kurtz, 2002). The key issue is how to investigate the complex processes that take place in psychodynamic psychotherapy with adolescents that can lead to change, so that what goes on in treatment itself can be related to changes in outcome. In the field Psychodynamic psychotherapy for adolescents 261 of psychodynamic psychotherapy for adolescents, relatively few studies have conducted process analyses or attempted to link specific processes derived from the psychodynamic theoretical model to outcomes, but those that have done so show great promise. For example, Di Lorenzo, Maggiolini, and Suigo (2015) examined the typical features of adolescent psychodynamic psychotherapy as compared to other adolescent psychotherapeutic approaches in terms of the therapists’ responses to adolescent clients. Their results indicated that the therapeutic process was characterized by prioritizing helping adolescents make sense of their own experience by focusing on current relationships and emotions rather than on past relationships. In the IMPACT-ME longitudinal research project led by Nick Midgley, qualitative interviews were used to better understand the quantitative results. For instance, one substudy examined hopes and expectations from therapy among depressed adolescents and found that differing expectations were likely to have implications for the way in which young people engage with treatment (Midgley et al., 2016). In another study, Fernandez, Krause, & Pérez (2016) investigated the role of the quality of the therapeutic alliance in the first sessions and therapeutic outcomes of adolescent psychotherapy to assess which perspectives (those of adolescents, therapists, or parents) and which times of evaluation (first, second, or third session) had greater impact. The results showed the importance of the initial construction of the working alliance by both the adolescents’ and the therapists’ perspectives. Wright, Briggs, and Behringer (2005) examined the association between attachment styles and suicidality among adolescents in psychodynamic psychotherapy and found that high-risk adolescents tended to communicate their distress in therapy in a more preoccupied/enmeshed manner. Another process-outcome study reported an association between an increase in the flexibility of interpersonal patterns and a decrease in symptoms among adolescents in psychodynamic psychotherapy (Atzil-Slonim, Shefler, Dvir-Gvirsman, & Tishby, 2011). Despite these significant advances in the field of adolescent psychodynamic psychotherapy research, we still know far less about what works for whom than is the case in adult psychotherapy research. Prominent researchers in the field consistently highlight the need for more studies to further explore the process of psychodynamic psychotherapy for adolescents and determine which mechanisms lead to positive outcomes that can help adolescent clients return to a healthy developmental path and expand their freedom and choices (e.g., Kazdin, 2004; Midgley et al., 2017). Case illustration The following example illustrates the processes of change of one adolescent client over 1 year of psychodynamic psychotherapy. This case was chosen from a larger sample of adolescents in psychodynamic psychotherapy, in which clients went through in-depth interviews according to the Core Conflictual Relationship Theme (CCRT) method (Luborsky & Crits-Christoph, 1998) at the beginning of treatment and a year later (for further details, see Atzil-Slonim, Shefler, & Tishby, 2015). 262 Contemporary Psychodynamic Psychotherapy Client description and presenting problem Ahmed, a 16-year-old male Israeli Arab, was referred for treatment by the school counselor because his level of functioning at school has declined significantly. Ahmed was diagnosed with moderate depression. In the intake meeting he said that in the last few months he had gradually realized that he was homosexual. He felt that he could not disclose this to his parents, since they are religious Muslims and would not accept it. Ahmed felt caught in a complex dilemma: He felt obliged to choose between a life of conformity to his parents’ values, which would mean negating who he really was, and being true to himself but hiding his true nature from close friends and family. His struggle to establish a sense of personal identity (Erikson, 1968), along with age-appropriate conflicts in the relationship with his parents, exceeded tolerable levels of distress, leading to treatment referral. The course of treatment is described through the relational narratives the client told about meaningful interactions during psychotherapy, at the beginning of treatment and 12 months later. Ahmed’s CCRT at the beginning of treatment Relationship with mother, first interview: Mom calls my cell phone in the afternoon. She asks how I am, if I did my homework and what my plans are for the rest of the day. I can’t tell her where I really am, because I’m going to a meeting at the “Open House” (a club for gay and lesbian teenagers). I try to end the conversation as quickly as possible, my answers are minimal. She doesn’t understand that I don’t want to talk to her and she continues snooping. I give her the answers she wants to hear and try to be as polite as I can. She doesn’t know a thing about me and I don’t want her to know. I just want her to leave me alone. Relationship with the therapist, first interview: in the last session I was telling her only good things about myself. I thought, what a waste of time, there are so many bad things that I did that I’m not sharing with her. She just listened. And then I told her things about me that are kind of good but may look not so good in the eyes of an adult. I wanted to see how she reacted to that. She continued listening, asked questions about it and she wasn’t judgmental at all. It made me feel good that she didn’t criticize me. However, it was a waste of time, because I didn’t talk about all the bad things. In these narratives from the initial phase of treatment it seems that Ahmed was mainly occupied with hiding from his mother what he was doing and thinking. He experienced his mother as invasive and not understanding, and he made an effort to avoid conflict with her. In the process of preventing himself from expressing his emotions to his mother, his emotions were apparently not available to him either. The theme of hiding versus disclosing thoughts and emotions was also present in the relationship that started to develop with his therapist at the beginning of treatment and may represent the development of transference. He described an interaction in which he tried to present something to the therapist to test whether she Psychodynamic psychotherapy for adolescents 263 accepted it or not. Although the therapist seemed to pass the test, Ahmed was aware of how much was still hidden in the relationship. Ahmed’s CCRT after a year of treatment Relationship with mother, second interview: Last Saturday, I was sitting on her bed while she was folding the laundry. She asked me whether I wanted a girlfriend. I felt angry with her, she really doesn’t understand who I am. For her, the idea of having a girlfriend before being married is considered being open minded. I started to reply, with the answer I thought she wanted to hear, but then suddenly I felt bad about what I was doing. I thought that I try so hard to make her happy that I don’t even hear my own voice when I’m around her. I thought to myself: “does she really want to know how I feel and who I am? Why am I trying so hard to please her?” It made me sad. Anyway, the conversation continued and we changed the subject and began talking about the fact that people can live in all kinds of lifestyles, not only the traditional style of marriage. I found myself arguing with her. I was surprised that she listened and didn’t completely reject my opinion. Then she gave an example as if she wanted to refute what I said, so she said ‘if for example a son tells his mother he is gay, she doesn’t have to accept it, does she?’ I told her what I thought about the importance of accepting people as they are. We were not talking about ourselves, only hypothetically about the subject, but I was really surprised that we could talk this way. This was actually the first time I heard her saying this word (gay), and I didn’t know it even existed in her thoughts. I was very much surprised. On the one hand she talked about it as if it was forbidden, and that really made me sad, but on the other hand it was kind of a strange feeling. . . because she raised the subject and I was sort of glad. . .not exactly glad. . .kind of excited that I could answer her and that we could talk about this subject. Of course I would have liked her to be understanding and accepting but I don’t really expect that from her. She is too religious and limited to be able to do it, but I was moved by the fact that we were both a little more real in that conversation. Relationships with the therapist, second interview: We talked about something that we have already talked about before many times. This is something I also think about a lot. However, this time I opened up about it more than in previous sessions and I told her details that I have never disclosed before. While I was talking about it with her, I started to think about it in a different way than I used to. Suddenly it didn’t sound as terrible as before. I don’t remember what she said but I remember feeling that she really accepted me despite what I did and that it’s not only because she was doing her job as a psychologist, but because she understood it as a person. It’s not that I thought that what I did was OK, she didn’t think that either, but we both knew I regret what I did and that it didn’t mean I am a bad person. I started to cry. . . I felt that she really got what I felt in that moment because she also knew what I felt about it before. I was very sad. . .it ‘s painful. . . all this time I spent hating myself for what I did. . .I cried a lot in that session. . . but at the same time 264 Contemporary Psychodynamic Psychotherapy I felt relieved because finally I let everything out and I realized I could feel different about it. Ahmed’s flexibility, reflectivity, and access to emotion appeared to increase throughout the year of treatment. Ahmed’s positive and negative internal representations toward his mother grew richer and more complex through treatment. After a year of treatment Ahmed was still feeling not accepted, angry, and misunderstood by his mother, and he still experienced himself as closed and distant. At the same time, however, new themes emerged. He expressed more willingness to accept his mother as limited because of her religious beliefs, and he experienced himself and her as a little more open, real, and authentic in the interaction. While in the first interview he described himself as holding in his anger, in the second interview he was still angry but also very sad. He appeared to have become more in touch with his inner world and better able to sustain and tolerate his negative emotions. These differences between the first and second interviews were also noticeable in the relationship with his therapist. After a year of treatment Ahmed’s narrative about the therapist included an interaction in which he could open up to his therapist about something that he had not been able to trust her with in the past that evoked feelings of shame and guilt. He described how it was possible for him to explore these emotions with his therapist and to tolerate them together. He continued to describe a moment in therapy when new ways of experiencing himself and the therapist emerged. Psychodynamic psychotherapy aims to help adolescents get to know the conscious and unconscious parts of themselves that were not previously available to them so that they can experience themselves and others more fully and have a broader range of choices in their interpersonal interactions (Mitchell, 1993; Ogden, 2005). For Ahmed the opportunity to work through his internal representations in the relationship with his therapist may have opened up new possibilities for him to experience himself and others. Therapy also made it possible for him to generalize these new experiences to the relationship with his mother and hopefully to other relationships. This process may have contributed to Amhed’s achieving clinically significant change measured with standardized symptom scales. His own words about the therapist beautifully describe the process of change: She listens and she is not judgmental about things I have done that I felt ashamed about before, and it helps me because now I can listen to myself better and accept myself as I am. References Abbass, A. A., Rabung, S., Leichsenring, F., Refseth, J. S., & Midgley, N. (2013). Psychodynamic psychotherapy for children and adolescents: A meta-analysis of shortterm. Journal of the American Academy of Child and Adolescent Psychiatry, 52(8), 863 867. Atzil-Slonim, D., Shefler, G., Dvir-Gvirsman, S., & Tishby, O. (2011). Changes in rigidity and symptoms among adolescents in psychodynamic psychotherapy. Psychotherapy Research, 21(6), 685 697. Psychodynamic psychotherapy for adolescents 265 Atzil-Slonim, D., Shefler, G., & Tishby, O. (2015). Internal representations of the therapeutic relationship among adolescents in psychodynamic psychotherapy. Clinical Psychology and Psychotherapy, 22, 502 515. Benjamin, J. (1995). Sameness and difference: Toward an “overinclusive” model of gender development. Psychoanalytic Inquiry, 15, 125 142. Blos, P. (1967). The second individuation process of adolescence. Psychoanalytical Study of the Child, 22, 162 186. Briggs, S. (2002). Working with adolescents: A contemporary psychodynamic approach. New York: Palgrave Macmillan. Briggs, S., Maxwell, M., & Keenan, A. (2015). Working with the complexities of adolescent mental health problems: Applying time-limited adolescent psychodynamic psychotherapy (TAPP). Psychoanalytic Psychotherapy, 29(4), 314 329. Cohen, P. (2005). The yin and yang of it: Working with the adolescent in the context of the family. Journal of Infant, Child and Adolescent Psychotherapy, 4, 171 180. Di Lorenzo, M., Maggiolini, A., & Suigo, V. A. (2015). A developmental perspective on adolescent psychoanalytic psychotherapy. An Italian study with the Adolescent Psychotherapy Q-Set. Research in Psychotherapy: Psychopathology, Process and Outcome, 18(2), 102 113. Available from https://doi.org/10.7411/RP.2015.106. Erikson, E. (1968). Identity: Youth and crisis. London: Faber. Erlich, H. S. (1993). Reality, fantasy, and adolescence. Psychoanalytic Study of the Child, 48, 209 223. Fernandez, O. M., Krause, M., & Pérez, J. C. (2016). Therapeutic alliance in the initial phase of psychotherapy with adolescents: different perspectives and their association with therapeutic outcomes. Research in Psychotherapy: Psychopathology, Process and Outcome. Fonagy, P., Target, M., Cottrell, D., Phillips, J., & Kurtz, Z. (2002). What works for whom? A critical review of treatment for children and adolescents. New York: Guilford Publications. Freud, A. (1958). Adolescence. Psychoanalytic Study of the Child, 13, 255 278. Freud, S. (1905). Three essays on the theory of sexuality (Standard ed., 7). London: Hogarth Press. Gelso, C. J. (2011). The real relationship in psychotherapy: The hidden foundation of change. Washington, DC: American Psychological Association. Horne, A. (2001). Brief communications from the edge: Psychotherapy with challenging adolescents. Journal of Child Psychotherapy, 27(1), 3 18. Karver, M. S., Handelsman, J. B., Fields, S., & Bickman, L. (2006). Meta-analysis of therapeutic relationship variables in youth and family therapy: The evidence for different relationship variables in the child and adolescent treatment outcome literature. Clinical Psychology Review, 26, 50 65. Kazdin, A. E. (2004). Psychotherapy for children and adolescence. In A. E. Bergin, & S. L. Garfield (Eds.), Handbook of psychotherapy and behavior change (4th ed, pp. 543 594). New York: Wiley. Lanyado, M., & Horne, A. (2009). Child and adolescent psychotherapy: Psychoanalytic approaches. London: Routledge. Levy-Warren, M. (2000). The adolescent journey. Jason Aronson, Incorporated. Luborsky, L., & Crits-Christoph, P. (Eds.), (1998). Understanding transference: The core conflictual relationship theme method (2nd ed.). Washington, DC: American Psychological association. Marks-Mishne, J. (2010). Clinical work with adolescents. London: Free Press. 266 Contemporary Psychodynamic Psychotherapy Midgley, N., Holmes, J., Parkinson, S., Stapley, E., Eatough, V., & Target, M. (2016). “Just like talking to someone about like shit in your life and stuff, and they help you”: Hopes and expectations for therapy among depressed adolescents. Psychotherapy Research, 26 (1), 11 21. Midgley, N., O’Keeffe, S., French, L., & Kennedy, E. (2017). Psychodynamic psychotherapy for children and adolescents: An updated narrative review of the evidence base. Journal of Child Psychotherapy, 43(3), 307 329. Mitchell, S. A. (1993). Hope and dread in psychoanalysis. Basic Books. Ogden, T. H. (2005). This art of psychoanalysis: Dreaming undreamt dreams and interrupted cries. New York, NY: The New Library of Psychoanalysis, Routledge, Taylor & Francis Group. Palmer, R., Nascimento, L. N., & Fonagy, P. (2013). The state of the evidence base for psychodynamic psychotherapy for children and adolescents. Child and Adolescent Psychiatric Clinics of North America, 22(2), 149 214. Schafer, R. (1973). Concepts of self and identity and the experience of separationindividuation in adolescence. The Psychoanalytic Quarterly, 42(1), 42 59. Shefler, G. (2000). Time-limited psychotherapy with adolescents. Journal of Psychotherapy Practice & Research, 9(2), 88 99. Winnicott, D. W. (1971). Playing and reality. London: Tavistock. Wolf, E., Gedo, J., & Terman, D. (1972). On the adolescent process as a transformation of the self. Journal of Youth and Adolescence, 1, 257 272. World Health Organization. (2013). Caring for children and adolescents with mental disorders: Setting WHO directions. Geneva: WHO. Retrieved from ,http://www.who.int/ mental_health/media/en/785.pdf.. Wright, J., Briggs, S., & Behringer, J. (2005). Attachment and the body in suicidal adolescents: A pilot study. Clinical Child Psychology and Psychiatry, 10(4), 477 491. Further reading Gaines, R. (1999). The interpersonal matrix of adolescent development and treatment. In A. H. Esman (Ed.), Adolescent psychiatry: The annals of the american society for adolescent psychiatry (Vol. 24, pp. 25 47). Hillsdale, NJ: The Analytic Press. Psychodynamic practice and LGBT communities 18 Vittorio Lingiardi and Nicola Nardelli Department of Dynamic and Clinical Psychology, Faculty of Medicine and Psychology, Sapienza University of Rome, Rome, Italy The acronym LGBT (lesbian, gay, bisexual, and transgender) is widely used in politics, health, and the social sciences to refer to sexual and gender minorities. However, not only is the LGBT term overly inclusive, but each category described by the acronym is reductive in and of itself. For this reason, research and practice in health and the social sciences do not always benefit from considering LGBT people a homogenous group. Although it is true that sexual and gender minorities are often subjected to social disapproval and discrimination, it is also true that members of each sexual and gender minority are subjected to a variety of specific experiences. Moreover, the LGBT acronym excludes intersexual, queer, and questioning people as well as women who have sex with women and men who have sex with men. Rather than referring simply to LGBT people, researchers and practitioners should include the 1 symbol (LGBT 1 ) to refer to any sexual and gender minority member who might possibly recognize himself or herself in a label. However, whether or not the LGBT and LGBT 1 acronyms are useful (mostly from a sociological or political perspective), in psychodynamic psychotherapy individual differences, characteristics, and specificities (idiographic features) are often more relevant than general categories (nomothetic features). The aim of this chapter is to provide a framework for psychodynamic practice with members of sexual and gender minorities. It is of crucial importance that mental health professionals listen to and help members of sexual and gender minorities, as such individuals continue to be subjected to discrimination throughout the life cycle, even in progressive societies. Therapists who work with such clients must understand and treat their clients without prejudicial bias. For many decades, sexual and gender minorities were pathologized by health professionals. Many health professionals studied and were trained to recognize such minorities as deviating from expected developmental paths. Although all mental health scientific and professional organizations and associations have since approved guidelines aimed at preventing the discrimination of minorities and providing therapists with appropriate responses to sexual orientation (Lingiardi, Nardelli, & Drescher, 2015), only the second edition of the Psychodynamic Diagnostic Manual (PDM-2) contains specific sections dedicated to the well-being of minorities (Lingiardi & McWilliams, 2017). Some professionals still have prejudice and/or negative attitudes toward these populations (e.g., King, 2015; Lingiardi, Nardelli, & Tripodi, 2015). For Contemporary Psychodynamic Psychotherapy. DOI: https://doi.org/10.1016/B978-0-12-813373-6.00018-0 © 2019 Elsevier Inc. All rights reserved. 268 Contemporary Psychodynamic Psychotherapy this reason, although a specific psychodynamic therapeutic approach for LGBT people may not be needed, we consider the PDM-2 a useful treatise for our professional community. In this chapter we discuss or at least mention the main topics addressed in the “Psychological Experiences That May Require Clinical Attention” section of the Manual. A brief history of clinical approaches to sexual and gender minorities Sigmund Freud first contributed to moving the topic of sexual orientation from a moral and religious framing to a scientific and psychological one. His approach was dual-sided. On the one hand, he considered homosexuality a form of developmental fixation; on the other hand, he stated that it should not be considered an illness and therefore should not be “cured.” Moreover, in a famous letter to Ernst Jones that circulated among the institutes and was cosigned by Otto Rank (1921), Freud affirmed that homosexuality in itself was not a sufficient reason to exclude a potential candidate from becoming a psychoanalyst: “We cannot exclude such persons without other sufficient reasons, as we cannot agree with their legal prosecution. We feel that a decision in such cases should depend upon a thorough examination of the other qualities of the candidate” (cit. in Lewes, 1988, p. 33). Unfortunately, until the late 1970s, many psychoanalysts (e.g., Bieber, Hatterer, Ovesey, Socarides) took a heteronormative stance and pathologized nonheterosexual sexualities (Drescher, 1998; Mitchell, 1981/2002; Roughton, 2003). According to Kernberg (2002), homosexuality is a shining example of how ideology can have a deleterious impact on psychoanalytic theory and practice. A nonpathological view of homosexuality was not put forward until the end of the 20th century. The depathologizing journey started with the Kinsey Reports, which pointed out that homosexual behavior was more common than expected. A further milestone was achieved by Hooker (1957), who administered three projective tests (Rorschach, TAT, and MAPS) to nonclinical participants grouped according to sexual orientation. Three expert judges blind-rated the protocols and were unable to distinguish the heterosexual group from the homosexual one. However, the most significant change occurred in the late 1970s. Just as many female psychoanalysts had talked in the first person about female sexuality, correcting the bias of a male-centric approach in psychoanalysis, a growing number of gay psychoanalysts began to come out of their personal and institutional closets and talk about themselves and their experiences (Drescher, 1998; Isay, 1989; Magee & Miller, 1996; Roughton, 2002). Until the latter half of the 20th century, transgender presentations also tended to be classified as pathological. However, the clinical approach to gender minorities has undergone notable revisions, and debates around the treatment of such groups are ongoing (Drescher, Cohen-Kettenis, & Reed, 2016; Giovanardi, 2017). The DSM-5 (APA, 2013) acknowledges the difference between assigned gender at Psychodynamic practice and LGBT communities 269 birth and experienced or expressed gender. It replaced the DSM-IV’s diagnosis of gender identity disorder (GID) with gender dysphoria (GD), which referred to a condition of personal suffering rather than a psychiatric disorder. Moreover, by placing the clinical focus on dysphoria—and not on identity per se—the diagnosis of GD was able to capture the distress that could accompany gender incongruence. Unlike GID, GD allows transgender people to “exit” from the diagnosis. Following the American Psychiatric Association, also the World Health Organization changed in the ICD-11 the diagnosis of GID to “gender incongruence,” moving it from the category of “mental disorders” to the category of “conditions related to sexual health.” Prejudices and stigma against LGBT 1 individuals Stigma against LGTB 1 people is so deeply rooted that almost everyone is exposed to its expression, ranging from seemingly innocuous mockery to hate speech and hate crimes. It can be useful to distinguish stigma associated with nonnormative sexual identities (i.e., nonheterosexual identities) from stigma based on nonnormative gender identities (i.e., noncisgender identities). The term homophobia is generally used to indicate the former type of stigma, and transphobia is generally used for the latter type. According to Herek (2016), these terms are reductive for two reasons. First, the -phobia suffix focuses primarily on individual causes and neglects social and cultural components. Second, neither of these conditions shows evidence of psychopathological processes related to an extreme irrational fear of an object or circumstance. Unlike individuals with common phobias, people who act against LGBT 1 people (1) consider their negative reactions normal and justifiable, (2) do not find that their attitudes compromise social functioning, (3) do not experience distress or feel the need to dispose of their negative attitudes, and (4) sometimes show avoidance behaviors alongside behaviors characterized by active aversion or deliberate aggression. Viable alternatives to the term homophobia include sexual stigma and sexual prejudice; viable alternatives to the term transphobia include gender minority stigma and gender minority prejudice. Note that stigma is a sociological construct, whereas prejudice is a psychological construct (Herek, 2016). Since sexual and gender minority prejudices are deep-rooted, LGBT 1 people may also be haunted by prejudices against themselves, which may be more or less conscious. These prejudices may lead LGBT 1 individuals to develop negative feelings and attitudes toward themselves, ranging from distress to self-hatred. This phenomenon is called internalized homophobia, internalized transphobia, or, according to Herek (2016), self-stigma. Self-stigma is based on the internalization of social stigma: “a kind of self-directed prejudice, whereby the self-concept is congruent with the stigmatizing responses of society” (Herek, 2016, p. 398). It is often related to a lack of self-acceptance and self-esteem and may be expressed as selfloathing; feelings of inferiority, guilt, and shame; an inability to integrate one’s 270 Contemporary Psychodynamic Psychotherapy own sexual and gender identities; and self-identification with negative stereotypes (e.g., the belief that being LGBT 1 entails loneliness or a life that can never be as satisfying as that lived by heterosexual individuals). It usually involves a feeling of not having “the right stuff” and is often associated with a fear of letting down one’s parents. Such feelings can compromise normative developmental paths, personality functioning, and interpersonal relationships. Self-stigma can also undermine psychological and physical well-being and may give rise to anxiety, depressive symptoms, and suicidal ideation. For this reason self-stigma, accompanied by the fear of disappointing one’s parents and not meeting societal expectations, is the basis of many requests for reparative therapy (see the section below titled “On and around sexual orientation change efforts”). Patients exhibiting self-stigma may show heightened dependency on defense mechanisms. Therapists may find it useful to differentiate those defenses that are directed toward sexual orientation (e.g., “I’m not a gay person, it’s just a passing phase of my life”) from those that are more closely related to self-stigma (e.g., “I’m okay with being gay, but I consider it a private matter, and I don’t like my colleagues to know it”). High levels of self-stigma may lead a person to develop pervasive feelings of shame and guilt and heightened use of defenses that might express themselves as symptoms and waste many psychological resources. When the distress due to self-stigma is very high, conflicting mental contents may be dissociated. In these cases, they may be compartmentalized in different parts of the consciousness, as if they were put in different “mental drawers,” affecting the well-being and compromising the behavioral, cognitive and affective processes (Nardelli, Baiocco, Tanzilli, & Lingiardi, 2019). Although gender and sexual orientation are different constructs, some stigmarelated issues that concern sexual identity are gender-specific, because they are directed against gender expressions that do not comply with cultural and social expectations (e.g., gay men being called “sissies”). Moreover, heteronormativity holds that men should be attracted to women and women should be attracted to men. Thus two phenomena can characterize the development of children who grow up to be LGB: gender confusion and gender stress (Drescher, 1998). A person showing gender confusion might interpret same-sex attraction using gender stereotypes, and some of these interpretations may involve self-stigma. Gender stress often arises from a feeling that one is failing to meet cultural and social expectations of one’s assigned gender. Such stress can occur over a protracted period of time, and many LGB people recall experiencing gender stress in their attempts to integrate their same-sex attraction into their identity. In the following brief case illustration, Albert recalls being bullied as a child at school, with other boys calling him names such as “sissy” and “fag.” Gradually, he became marginalized by both boys and girls. During his first year of psychotherapy Albert gradually became more content in relation to his gender confusion. He recalled how, repeatedly, he had told himself: “You’re not a girl! You have to engage with a girl! You’re a guy.” He also recalled that his family had been worried about his gender-nonconforming behavior and how he had felt “wrong and without the right credentials,” as he was not as his parents would have wished. Psychodynamic practice and LGBT communities 271 Some months later, Albert began to accept some “female” aspects of himself and to integrate his same-sex attraction into his sexual identity, achieving a more integrated sense of himself. Two years into the psychotherapy, a “real twist” happened. He told his therapist: Tidying my room, I found a handbag I had not used in years. I saw it and I decided to carry it with me all evening. How happy I was! I do not have the words to explain it to you . . . Okay, my bag stays with me today! [. . .] I understood why I had stopped carrying it: the same reason why, when I cross my legs in front of other people, I immediately put them back in a regular position. I mean . . . every time I felt I was ‘feminine’, I tried to be more ‘masculine’. I used to be embarrassed, but now I’m no longer ashamed. Sometimes I feel an urge to uncross my legs. But I just don’t do it. And that’s good. I’m glad. I am so glad I am learning to grow as a man, but not the ‘kind of man’ my parents wanted me to be. What a relief to discover that there is not ‘masculinity’ but ‘masculinities’. Minority stress Although the international scientific community recognizes that homosexuality is a normal variant of human sexuality and GID is better framed as GD or gender incongruence in order to avoid psychopathological implications (Drescher, Cohen-Kettenis, & Reed, 2016), LGBT 1 individuals still face harassment and other stressful and traumatic experiences. Further, they can be subjected to a very particular form of minority stress because, unlike members of other minorities, they cannot always rely on family or school support. On the contrary, the family (or school context) may serve as an additional source of stress. Sexual and gender minority stigma can occur in a sociocultural context that is indifferent or even collusive. Episodes of discrimination and violence can have a very strong emotional impact on not only the direct victims, but also other individuals who cannot avoid thinking that such episodes might happen to them as well. Minority stress can have long-term effects and often affects the quality of one’s relationships. It also represents a risk factor for partner abuse. Stressful or traumatic experiences related to stigma (e.g., bullying, family rejection, harassment) might result in relational difficulties throughout life (Lingiardi & Nardelli, 2012). Moreover, stigma and self-stigma may constitute a significant obstacle to seeking help (e.g., if one believes that, as an LGBT 1 person, one deserves abuse or antigay reactions from authorities and family members). Minority stress may even occur in LGBT 1 communities themselves. For example, a lesbian woman may be ridiculed for being too masculine and a gay man for being too feminine. These individuals may be called “trans” a term that insults both the subjects of the name calling and transgender people as well, because of the derogatory use of the term. Most of these dynamics depend on identification with the aggressor as a defense mechanism against certain expressions of sexual and gender identity. 272 Contemporary Psychodynamic Psychotherapy However, minority stress does not necessarily lead to negative health outcomes. The relationship is moderated by resilience, an important protective factor that should be recognized and consolidated. For example, a client may need to tackle stereotypes, accept her or his belonging to the LGBT 1 community, and affirm himself or herself as LGBT 1 . The following vignette, excerpted from Lingiardi and Giovanardi (2017, p. 696), briefly illustrates how the support of the LGBT 1 community and psychodynamic psychotherapy can be useful in dealing with GD and drug abuse: Maria always declared a very early onset of gender dysphoria. Nevertheless, having grown up in a small town in a conservative family environment, she had a hard time during her school years in dealing with her femininity as a boy. She was, in her words, ‘forced to live as a very depressed boy’ without friends or flirts, and in late adolescence, she temporarily abused cannabis and cocaine. When she moved to Rome to attend college, she became more and more involved in LGBT associations. At age 25, following the advice of a senior member of her LGBT group, she began a long-term psychodynamic psychotherapy to deal with both gender dysphoria and addiction. She successfully overcame drug abuse and started experimenting with different gender roles. Then, aged 30, she started her transition process, which eventually led to gender reassignment surgery (GRS). Homophobic/transphobic bullying Since the term homophobic bullying is widespread and given that homophobic and transphobic bullying are very similar in their presentations and effects, the term homophobic bullying will be used here to refer to both kinds of bullying. Homophobic bullying is directed toward victims’ atypical expressions of gender or actual or presumed homosexual orientation. In some cases victims may be harassed because their parents or relatives are openly lesbian, gay, bisexual, or transgender. Obviously, homophobic bullying may also affect children who grow up to be heterosexual. Nevertheless, when homophobic bullying affects children who grow up to be LGBT 1 , it complicates their already complex process of coming out because victimization due to homophobia increases victims’ fears and inhibits them from expressing themselves as LGBT 1 , thus jeopardizing their self-acceptance. Victims of homophobic bullying are at risk of dropping out of school; developing stress-related, posttraumatic, or depressive disorders; and, in extreme cases, suicide (Russell & Horn, 2017). Homophobic bullying has several unique presentations that add to a victim’s overall risk of being bullied: G G The victim’s inferior position with regard to the perpetrator(s)—a common feature of all bullying—is further increased by the social stigma against LGBT 1 individuals, and the abuse may resonate with expressions of homophobia and transphobia that characterize juvenile contexts. The victim may experience difficulty in seeking help from adults because doing so draws attention to the victim’s sexuality. Such difficulty may be associated with feelings of Psychodynamic practice and LGBT communities G G 273 anxiety, shame, and fear of disappointing expectations of heterosexuality and conformity to the norms associated with one’s assigned gender. The victim may have particular trouble finding support and protection among peers because of the risk that anyone who helps the victim might be perceived as gay or transgender themselves (and thus subject to bullying). The victim may develop sexual and gender minority prejudice as a result of one’s experienced hostility, as a defense against self-stigma. Bullies may engage in homophobic bullying to try to show that they are “normal,” to affirm conformity to conventional gender expectations, and to externalize possible internal conflicts about their own gender experiences and/or same-sex attraction. In dealing with the consequences of homophobic bullying, mental health professionals should consider whether LGBT 1 clients may have been victimized by peers even though they may deny it. A clinical setting marked by a climate of acceptance and security is important for the exploration of traumatic memories. On and around sexual orientation change efforts Experiences of feeling different vary between individuals, and it may be clinically useful for therapists to understand patients’ raised awareness of their sexual orientation. As Sand (2015) notes, melancholia may accompany this discovery, owing to the awareness that access to the privileges granted to heterosexual people will be denied to the patient. This melancholia may continue to present itself, for example, through an incomplete processing of the “loss” of heterosexuality, and may work against identity integration. Some individuals struggle with their sexual orientation and search for therapies to change it. Such efforts are often related to self-stigma and the social pressure to conform to an ideal of heterosexuality. Named conversion therapies or reparative therapies, these sexual orientation change efforts (SOCE) lack any empirical support, and many studies have reported that they cause significant harm (see the website of the Center for the Study of Inequality at Cornell University: https:// whatweknow.inequality.cornell.edu). Many mental health associations have adopted position statements against SOCE, and the use of these interventions on minors is banned in some countries. As was noted above, some professionals do not consider homosexuality a “normal variant of human sexuality”; rather, they see it as a psychological impairment or simply something “worse” than heterosexuality (in this case we could speak of heterophilia). Such an attitude is likely to lead to potentially harmful interventions, for example, by exacerbating patients’ self-stigma or denying them access to a broad range of experiences. Some clinical interventions, even though they are not expressly SOCE, may be affected by prejudices and insufficient information. Therefore the boundaries between SOCE and other types of biased intervention are not always distinct (Lingiardi, Nardelli, & Drescher, 2015). 274 Contemporary Psychodynamic Psychotherapy Intersecting identities and the double minority status A clinical presentation may be more complicated by intersections between conflicting identities. To cite a common example, religious individuals who belong to a sexual or gender minority may experience a real and strong internal struggle with respect to their faith and often report deleterious effects on their well-being as a result of this struggle. For these individuals, alignment with one of these identities may polarize and reinforce an internal conflict. Clinical work with such patients should foster their integration of both sides of the conflict and look for a “third solution,” enabling them to feel both LGBT 1 and devout. Some studies have demonstrated that a more personal and flexible interpretation of scripture and precepts can ameliorate self-acceptance and well-being. It is important that therapists recognize and deal with clients’ double minority status, as such clients may be subjected to discrimination and violence as a result of both their LGBT 1 identity and other stigmatized characteristics. Furthermore, clients’ communities of belonging (be they ethnic, religious, institutional, etc.) can be stigmatizing and rejecting of LGBT 1 members. Consider, for example, the situation of a refugee lesbian, an older gay man, a Jewish transgender person, or a Muslim gay man. Coming out Heterosexuality is usually an assumed quality of all children at birth. Thus heteronormativity is internalized at an early age, and this can make it difficult for children who grow up as lesbian, gay, or bisexual to recognize their own sexual orientation and integrate it at an identity level. Similarly, gender is assigned on the basis of biological sex. When one’s assigned gender is discordant with one’s gender identity, a person may experience distress due to GD. Unlike other minorities, members of sexual and gender minorities cannot always rely on the recognition and support of their own family. On the contrary, as has already been emphasized, family and school rejection may be significant sources of hostility and suffering. Children frequently associate terms related to LGBT 1 people with devaluating or unpleasant ideas or feelings before they understand the real meaning of these terms. Many studies have found that terms such as gay or lesbian are used by students as insults. For lesbians and gay men, coming out is both a process and an act: a process through which they psychologically prepare themselves for the act of voluntarily disclosing their sexual orientation. The coming-out process starts when children who grow up as LGB begin to feel their first same-sex attraction. The more they begin to integrate their same-sex attraction into their identity, the more comfortable they become with their desires, affects, behaviors, and relationships. At this point, they may declare it to others—an act that is colloquially referred to as “coming out of the closet.” People who remain “closeted” for many years of Psychodynamic practice and LGBT communities 275 their lives (or even for a lifetime) often consider their same-sex attraction unacceptable and generally live parallel and split lives (Nardelli, Baiocco, Tanzilli, & Lingiardi, 2019). Coming out can have a psychological cost, and LGB individuals must continuously consider this cost throughout their lifetime. Some studies have shown that coming out to a best friend during adolescence may serve as an important protective factor against social stigma and minority stress. However, the decision must sometimes be made in a short time frame within heteronormative communication (e.g., when a woman is automatically asked about her husband or a man is asked about having a wife), and this places the person at risk of experiencing unpredictable reactions. For this reason the decision to come out generally requires psychological resources and coping skills. In clinical work with adolescents, coming out can be a very important topic. Young women or young men who are economically dependent on their parents should evaluate their risk of getting kicked out of their home. On the other hand, coming out and its “ghosts” may be followed by a new homeostasis and more authentic and improved relationships with parents, friends, teachers, and colleagues. For transgender individuals the situation is quite different, as they may lack supportive communities. Sometimes, LGB people are hostile toward transgender people as a result of their own prejudices and/or defensive mechanisms against gender nonconformity. Through sex reassignment interventions, transgender individuals may align their gender identity with the gender that is perceived by others. According to Zimman (2009), in these cases coming out does not mean revealing one’s gender identity but rather revealing one’s personal gender history, as characterized by the transition from one gender to another. Therefore it may be useful to distinguish between two types of coming out: declaration and disclosure. The former is used before transition and refers to declaring one’s transgender identity; the latter is used after transition and refers to self-disclosing one’s gender history. In general, for both sexual and gender minorities, coming out is a developmental experience. However, in many cases it is problematic or demanding. Clinicians should always consider clients’ personal meaning of coming out, their previous experiences of it, and their imaginings and mentalizations of what it will be like in the near future. Reflections on clinicians’ self-disclosure In the past, self-disclosure by clinicians to clients was not recommended. Now it is acknowledged that such self-disclosure may have therapeutic benefits. While the issue of self-disclosure is a complex one that cannot be discussed fully here, in this section we hope to simply provide some food for thought. The choice of whether or not to self-disclose (about sexual or gender identity and many other topics) should be spontaneous and premeditated at the same time. 276 Contemporary Psychodynamic Psychotherapy Clinicians should not naively believe that they do not leave telltale signs about their private life, and they cannot ignore that hiding their own sexual and gender identities may generate cognitive and affective dissonance in clients who realize that their therapist holds these identities. While the decision of whether or not to self-disclose is a relational issue, clinicians should make every effort to ensure that it is also therapeutic. It is fundamental for clinicians to understand the urges and goals behind it—whether it is useful for the therapeutic alliance or arises from a need of the clinician—as well as why and when it is elicited by the client and on what grounds. Finally, clinicians should be aware that their reluctance to communicate their own sexual and gender identities may suggest unresolved concerns, shame, or embarrassment, especially if it follows from specific questions or hints made by a client. LGBT 1 clients and their children Recent social and legislative changes in many countries have deeply modified selfand other LGBT 1 representations and, conversely, many of the issues dealt with in the therapeutic space. Concerns related to secrecy, hiding, and passing one’s sexual or gender identity were more prevalent a decade ago. Today, in our consulting rooms, LGBT clients also relate stories of love, parenting, and family projects. Whereas many lesbian and gay parents previously had children in heterosexual relationships, an increasing number of same-sex couples are now choosing to have children within nonheterosexual relationships. Each country has its own laws on this matter. In some countries, LGBT 1 and heterosexual parents have equal rights; in other countries, parenting (including adoption) by LGBT 1 individuals is outlawed. The social and juridical context in which LGBT 1 people raise children exerts a significant impact on their daily lives and sense of security and also affects wider mental representations of LGBT 1 parenting (Campion, Morrissey, & Drazen, 2015). In addition to facing legal barriers, LGBT 1 people may encounter prejudice about their parenting skills or the child’s best interest. The most common prejudices concern the lack of distinction between mother/father and maternal/paternal functions in families with same-sex parents, rooted in the idea that a child with same-sex parents will have difficulty developing her or his own gender identity and sexual orientation. These prejudices have been addressed by decades of scrupulous empirical research (Baiocco et al., 2015). The results of this research can be summarized in the following statement of the American Psychoanalytic Association (2012): [. . .] Accumulated evidence suggests the family factors that are important for children’s outcomes and well-being are family processes and the quality of interactions and relationships. Evaluation of an individual or family for these parental qualities should be determined without prejudice regarding actual or perceived sexual orientation, gender identity or gender expression. There is no credible evidence that shows that a parent’s sexual orientation or gender identity will adversely affect the development of the child. Psychodynamic practice and LGBT communities 277 APsaA opposes any discrimination based on actual or perceived sexual orientation, gender identity or gender expression, against individuals in regard to their rights as biologic, custodial, foster, or adoptive parents. Children deserve to know that their relationships with their parents are stable and legally recognized. [. . .] In order to process their own position toward LGBT 1 parents and the well-being of their children, clinicians should be informed and up to date about research and clinician narratives in this area and, in this way, ensure respectful and empathic listening to their clients. Moreover, health professionals must be prepared to address specific issues that they may encounter in clinical contexts with LGBT 1 parents. For example, the sense of powerlessness related to the difficulty of having children; feelings of inadequacy related to being LGBT 1 ; a fear of raising children in an unusual family context; and jealousy or envy directed toward the child’s biological parent. A final vignette from a lesbian mother may be useful for exemplifying these issues: Even adopted children have “more than two” parents, biological parents and “affective” parents, who are the “actual” ones! Just as, one day, an adoptive mother will tell her child about the biological but “absent” parents, and she will have to help the child to understand that they could not or did not want to keep their baby, I will also tell my daughter that she has an “absent” parent, her “biological father.” It is not a gentleman who abandoned her as a child, but a gentleman who helped me and his other mother to give birth to—it has to be said—a project full of love and desire. It is important that psychotherapists recognize their prejudices relating to donor or gestational mothers in order to understand—together with the social parents—the shadows, worries, projections, and fears that should not be neglected but rather should be expressed and elaborated. After all, every family has its own story to tell. Awareness of the complexities discussed in this chapter can better equip therapists to consider the psychodynamics associated with issues such as social stigma, internalized homophobia, and intersecting identities in their work with LGBT 1 clients. Rather than delivering a particular set of interventions for those who identify as LGBT 1 , therapists can draw upon this awareness as an aid to understanding and responding to the client’s unique individual situation and needs, as in any wellconducted psychodynamic therapy. References American Psychoanalytic Association. (2012). Position statement on parenting. Retrieved from http://www.apsa.org/sites/default/files/2012%20%20Position%20Statement%20on %20Parenting.pdf. Baiocco, R., Santamaria, F., Ioverno, S., Fontanesi, L., Baumgartner, E., Laghi, F., . . . Lingiardi, V. (2015). Lesbian mother families and gay father families in Italy: Family functioning, dyadic satisfaction, and child well-being. Sexuality Research and Social Policy, 12(3), 202 212. Available from https://doi.org/10.1007/s13178-015-0185-x. 278 Contemporary Psychodynamic Psychotherapy Campion, E. W., Morrissey, S., & Drazen, J. M. (2015). In support of same-sex marriage. New England Journal of Medicine, 372(19), 1852 1853. Available from https://doi.org/ 10.1056/NEJMe1505179. Drescher, J. (1998). Psychoanalytic therapy and the gay man. Hillsdale, NJ: Analytic Press. Drescher, J., Cohen-Kettenis, P. T., & Reed, G. M. (2016). Gender incongruence of childhood in the ICD-11: Controversies, proposal, and rationale. The Lancet Psychiatry, 3(3), 297 304. Available from https://doi.org/10.1016/S2215-0366(15)00586-6. Giovanardi, G. (2017). Buying time or arresting development? The dilemma of administering hormone blockers in trans children and adolescents. Porto Biomedical Journal, 2(5), 153 156. Available from https://doi.org/10.1016/j.pbj.2017.06.001. Herek, G. M. (2016). A nuanced view of stigma for understanding and addressing sexual and gender minority health disparities. LGBT Health, 3(6), 397 399. Available from https:// doi.org/10.1089/lgbt.2016.0154. Hooker, E. (1957). The adjustment of the male overt homosexual. Journal of Projective Techniques, 21(1), 18 31. Available from https://doi.org/10.1080/08853126.1957. 10380742. Isay, R. A. (1989). Being homosexual: Gay men and their development. New York: Farrar, Straus and Giroux. Kernberg, O. F. (2002). Unresolved issues in the psychoanalytic theory of homosexuality and bisexuality. Journal of Gay & Lesbian Psychotherapy, 6(1), 9 27. King, M. (2015). Attitudes of therapists and other health professionals towards their LGB patients. International Review of Psychiatry, 27(5), 396 404. Available from https:// doi.org/10.3109/09540261.2015.1094033. Lingiardi, V., & Giovanardi, G. (2017). Challenges in assessing personality of individuals with gender dysphoria with the SWAP-200. Journal of Endocrinological Investigation, 40(7), 693 703. Available from https://doi.org/10.1007/s40618-017-0629-7. Lingiardi, V., & McWilliams, N. (Eds.), (2017). Psychodynamic diagnostic manual (PDM-2) (2nd ed.). New York: Guilford. Lingiardi, V., & Nardelli, N. (2012). Partner relational problem: Listening beyond homoignorance and homo-prejudice. In P. Levounis, J. Drescher, & M. E. Barber (Eds.), The LGBT casebook (pp. 223 230). Arlington, VA: American Psychiatric Publishing. Lingiardi, V., Nardelli, N., & Drescher, J. (2015). New Italian lesbian, gay and bisexual psychotherapy guidelines: A review. International Review of Psychiatry, 27(5), 405 415. Available from https://doi.org/10.3109/09540261.2015.1064875. Lingiardi, V., Nardelli, N., & Tripodi, E. (2015). Reparative attitudes of Italian psychologists toward lesbian and gay clients: Theoretical, clinical, and social implications. Professional Psychology: Research and Practice, 46(2), 132 139. Available from https://doi.org/10.1037/pro0000016. Magee, M., & Miller, D. C. (1996). Psychoanalytic views of female homosexuality. In R. P. Cabaj, & T. S. Stein (Eds.), Textbook of homosexuality and mental health (pp. 191 206). Arlington, VA: American Psychiatric Association. Mitchell, S. A. (1981/2002). The psychoanalytic treatment of homosexuality: Some technical considerations. Studies in Gender and Sexuality, 3(1), 23 59. Available from https:// doi.org/10.1080/15240650309349187. Nardelli, N., Baiocco, R., Tanzilli, A., & Lingiardi, V. (2019). Not in the same mental drawer: Internalized sexual stigma, dissociation, and the role of religion in a sample of Italian gay men. Journal of Homosexuality, 31 43. Available from https://doi.org/ 10.1080/00918369.2019.1591786. Psychodynamic practice and LGBT communities 279 Roughton, R. (2002). Being gay and becoming a psychoanalyst: Across three generations. Journal of Gay & Lesbian Psychotherapy, 6(1), 31 43. Roughton, R. (2003). The international psychoanalytical association and homosexuality. Journal of Gay & Lesbian Psychotherapy, 7(1-2), 189 196. Available from https://doi. org/10.1300/J236v07n01_11. Russell, S. T., & Horn, S. S. (Eds.), (2017). Sexual Orientation, Gender Identity, and Schooling: The Nexus of Research, Practice, and Policy. New York: Oxford University Press. Available from https://doi.org/10.1093/med:psych/9780199387656.001.0001. Sand, S. (2015). Coming out, being out: Reconciling loss and hatred in becoming whole. Psychoanalysis, Culture & Society, 20(3), 250 266. Available from https://doi.org/ 10.1057/pcs.2014.18. Zimman, L. (2009). ‘The other kind of coming out’: Transgender people and the coming out narrative genre. Gender and Language, 3(1), 53 80. Available from https://doi.org/ 10.1558/genl.v3i1.53. Working with immigrants and refugees in psychodynamic psychotherapy 19 Pratyusha Tummala-Narra Department of Counseling, Developmental and Educational Psychology, Boston College, Chestnut Hill, MA, United States It is estimated that in 2015 there were close to 244 million international migrants and 16 million refugees, not including Palestinian refugees (Migration Policy Institute, 2017; Pew Research Center, 2017). Increasingly, mental health professionals have been called upon to address the unique needs of immigrants and refugees. Despite a long history of neglect of sociocultural dimensions of intrapsychic and interpersonal experience within psychoanalysis, contemporary scholars recognize the importance of examining the diverse experiences of immigrants and refugees and the role of culture, language, race, gender, ethnicity, social class, and intersectionality in psychotherapy process (Ainslie, Tummala-Narra, Harlem, Barbanel, & Ruth, 2013). While the topic of psychoanalysis with respect to immigration and exile has a broad scope, this chapter aims to present some common patterns and experiences that are critical to culturally informed psychodynamic practice. The chapter consists of a consideration of the premigration and postmigration contexts, acculturation and related stress, and trauma. The implications of these factors for the negotiation of separation and loss and for the dynamics of the therapeutic relationship are discussed. Context of migration Psychoanalytic understandings of the impact of migration on individuals and communities consider the distinct premigration and postmigration contexts of immigrants and refugees. Specifically, refugees migrate as a result of being forced from their homes owing to war; political, religious, or ethnic persecution; and/or environmental disasters. Many refugees are displaced and relocated multiple times before reaching their final destination of resettlement (APA, 2012). They are at high risk for severe physical, sexual, and emotional trauma and, at times, for torture, and they may have lived in a number of refugee camps before arriving in what will become their adopted country (APA, 2010; Robjant, Hassan, & Katona, 2009). In contrast to refugees, immigrants, in particular those who are adults, typically have a choice in leaving their birth countries. The reasons for migrating to a new country Contemporary Psychodynamic Psychotherapy. DOI: https://doi.org/10.1016/B978-0-12-813373-6.00019-2 © 2019 Elsevier Inc. All rights reserved. 282 Contemporary Psychodynamic Psychotherapy are varied, such as fleeing poverty and political and social unrest, seeking educational and employment opportunities, and reuniting with family members (APA, 2012). The premigration context of immigrants, like that of refugees, can involve experiences of interpersonal, social, and political trauma, which may become the impetus for the decision to migrate (Ainslie et al., 2013). Psychoanalytic perspectives on the migration process emphasize the full range of intrapsychic, interpersonal, and social experiences that involve complex affective states. Many immigrants and refugees experience various types of anxiety, such as separation anxiety, disorienting anxiety, and depressive anxiety (Akhtar, 2011; Grinberg & Grinberg, 1989). Akhtar (2011) has described in detail the detrimental effects of environmental change and loss of familiar objects on an individual’s ego, such that feelings of disorientation and regret may overwhelm an initial sense of excitement when the person encounters a new, unfamiliar physical and cultural landscape. Anxiety, sadness, confusion, and grief may coexist with feelings of hope and optimism among immigrants and refugees. Further, experiences of psychological distress coexist with individual and collective resilience among these individuals and communities and shift over the course of time and context (APA, 2012). The postmigration context presents dilemmas that are driven not only by the immigrant’s or refugee’s experience of a new, unfamiliar environment, but also by realities such as the person’s ability to secure basic needs, such as housing, food, health care, and education, and by other people’s perceptions of immigrants and refugees. It also encompasses the reception of immigrants and refugees in the adopted country. Negative sentiment toward immigrants in the dominant society leads to increasing anxiety for racial and religious minority immigrants and compromises their attempts to acculturate to the new cultural context. Acculturation While there is no “right” or “best” pathway to acculturation, it is worth noting that certain aspects of acculturation may pose risks to immigrants and refugees. Specifically, research indicates that acculturation to dominant U.S. culture may be associated with higher-risk behaviors (APA, 2012). A majority of studies of racial minority immigrants in the United States indicate that U.S.-born children of immigrants fare worse with regard to physical health, mental health, and educational outcomes when compared with foreign-born counterparts, a phenomenon that has been described as the immigrant paradox (Alegria et al., 2008; Garcı́a-Coll & Marks, 2012). These findings raise questions about how the first generation (those arriving as adults to the United States) and the second generation (those born and raised in the United States) experience acculturation and the accompanying stress. Psychoanalytic scholars have written extensively about the ways in which migration and acculturative stress consists of anxiety, depression, and confusion (Akhtar, 2011). In the sections that follow, I focus specifically on two aspects of the acculturation process: family life and social location. Working with immigrants and refugees in psychodynamic psychotherapy 283 Family life Immigrant families often face new challenges, as the structure of the family and the functions of different family members can change, sometimes dramatically. Gender roles can be transformed in some families after migration in ways that affect the day-to-day lives of parents, children, and extended family members such as grandparents. Often, immigrant parents struggle with observing and helping their children navigate the U.S. cultural context and at the same time retaining their cultural, religious, and linguistic heritage. Immigrant parents tend to rely on other immigrants of similar ethnicity in negotiating parenting in the adopted country, as commonalities in language, culture, food, and religion bring a sense of security and “emotional refueling” (Akhtar, 2011). For many immigrants and refugees there is a strong desire to pass on the heritage culture as a way of maintaining a sense of cultural continuity and connection with the people in their former country from whom they are separated. This is evident in one patient’s description of her anxiety about her son’s acculturation to the United States: “If I don’t keep reminding him of where we come from, he may totally forget, become too American. And then, how do we live with that? Why did we come here?” Parents’ conscious and unconscious affective experiences of migration, experiences of oppression, cultural attachments, and wishes and fears accompanying migration and separation from the country of origin are transmitted intergenerationally and internalized by children (Eisold, 2012; Saketopoulou, 2015; White, 2015). Importantly, cultural perspectives transform for both parents and children throughout the life span, reengaging old and presenting new intrapsychic and interpersonal conflicts. Children of immigrants and refugees struggle with their parents’ dreams and aspirations as they recognize their parents’ resilience in surviving obstacles of reaching the new country and/or coping with an unfamiliar context. On the one hand, the second generation is driven to attain what their parents were unable to access; on the other hand, they look to engage in the dominant culture beyond the constraints of parents. Parents’ and children’s unique acculturation trajectories can contribute to intergenerational conflicts, which can be a source of stress for family life and individual psychological health (Sherry & Ornstein, 2014). Unfortunately, conflicts and the external demands of acculturation (e.g., adjusting to workplace or school, experiences of racism) are often left unspoken within the home and remain invisible to people outside the home. Social location Immigrants and refugees experience significant shifts in social location, as various aspects of identity such as those related to gender, race, ethnicity, religion, language, social class, physical disability, and immigration status, carry different psychological meanings and social consequences in the adopted country. An individual’s social identity—rooted in the heritage culture—is carried into the new cultural context, despite new norms concerning social location (Ainslie, 2011). For example, an adolescent who escaped violence in his country of origin might, 284 Contemporary Psychodynamic Psychotherapy because of the color of his skin, be labeled African American in the United States, but this label would be foreign to him and would not reflect his cultural identity. In such a case, aspects of social location have intrapsychic, interpersonal, and social consequences for the individual. The implications of social location can be considered through an examination of social mirroring (Suárez-Orozco, 2000), which is a concept that extends Winnicott’s (1971) conceptualization of mirroring to describe the range of messages received by immigrants outside of their homes, particularly in the dominant culture. When immigrants and refugees experience the postmigration context as accepting of their ethnic, linguistic, and religious heritage, they have access to a wider range of choices with regard to acculturation and identity development in the new country. However, negative messages regarding their social location (e.g., race, culture, gender, religion, social class, disability, national origin, immigration status) constrict this range of options, contributing to defenses that promote isolation, invisibility, and resentment toward the dominant culture. In some cases, perceptions and meanings of social location in the country of origin conflict with those in the adopted country. My patient Shruti, a 43-year-old immigrant from Bangladesh, shared her frustration with feeling marginalized in Bangladesh because of her caste and in the United States because of her lower income and racial status. She said, “In Bangladesh there are so many problems because of caste—people looking down on you, like my husband’s family. They come from a higher caste, and so they were totally against the marriage. Here, we work hard, but if you are not rich and you are brown like us, people look down on us. There is no winning anywhere.” Shruti’s experiences reflect negative mirroring in both premigration and postmigration contexts. She further shared how these experiences shaped her selfperceptions: “I try not to let it get to me, but sometimes, it feels bad inside, like I’m not good enough no matter where I go.” Bicultural and bilingual identity Identity development among immigrants and refugees involves a negotiation of physical and psychological distance between the country of origin and the adopted country (Akhtar, 2011). This negotiation involves the use of various defenses, including splitting (idealization and devaluation of one’s country of origin and/or adopted country), withdrawal (affiliation only with one’s own cultural group), and counterphobic assimilation (development of an “as-if” identity in which one rapidly identifies with the host culture) (Akhtar, 2011; Lijtmaer, 2001). These defenses are central to the immigrant’s and refugee’s sense of psychological home, a point of reference that can shift across the life span (Tummala-Narra, 2009). Whereas some psychological theories assume a linear process in the development of acculturation and cultural identity, psychoanalytic theorists assume a dynamic, fluid understanding of cultural identity (Tummala-Narra, 2016; Yi, 2014). Cultural identity for immigrants and refugees is a culmination of psychological Working with immigrants and refugees in psychodynamic psychotherapy 285 connections with family, cultural groups, language, and physical environment (e.g., country of origin, dominant society); intrapsychic and interpersonal conflicts; unconscious wishes and fears; and defenses adopted to navigate multiple, contradictory cultural, linguistic, and physical spaces and belief systems. Cultural identity is also thought to be a dynamic process that shapes the psyche and interpersonal relationships in transformative ways across the life span. Cultural beliefs and practices shift across context and time, shaping and reshaping one’s sense of self and of others. Additionally, the meanings and use of language can also vary with time in the course of adjusting to and living in a new cultural environment. My patient Monica, who emigrated from Spain first to Scotland and then to the United States as an adolescent increasingly “gave up” her heritage language, Spanish, as a way of acculturating to her life in predominantly English-speaking countries. To her parents’ dismay, as Monica became more fluent in English, she spoke less frequently to them in Spanish. As an adult she decided to communicate only in English with family and friends until she entered a relationship with a bilingual partner who speaks English and Spanish. Monica noted that within the context of this relationship she was able to connect not only with speaking in Spanish, but also with childhood memories and emotional experiences that had been processed in Spanish and later suppressed from conscious memory as she had worked to master her English speaking skills. The intrapsychic and interpersonal aspects of bilingualism and multilingualism among immigrants and refugees have implications for how individuals, families, and communities define the role of heritage language in identity formation and relational life (Ainslie et al., 2013; Akhtar, 2011). One’s connection to the heritage language and/or adopted language may indicate a sense of authenticity or sense of belonging within either an ethnic community or dominant society. As culture is embedded in language, the expression of cultural beliefs, attitudes, and experiences are connected with the use of any particular language. Bilingual and multilingual individuals may experience memories and emotions in unique ways in each separate language, with implications for whether and how life experiences are articulated within and outside of psychotherapy (Ainslie et al., 2013; APA, 2012; Foster, 1996). The experience of intersectionality Increasingly, psychoanalytic scholars have written about the centrality of intersectionality in the development of identity (Crenshaw, 1989; Ruth, 2012; Suchet, 2004). The term intersectionality refers to the ways in which an individual’s sense of self is shaped by multiple cultural and group identities (Mahalingam, Balan, & Haritatos, 2008). The creation of intersectional cultural space can engage creativity and freedom in ways that may not have been possible in one’s country of origin. At the same time, the development of intersectional identity involves both conscious and unconscious conflict across each aspect of identity (Ruth, 2012), where an individual internalizes aspects of key relationships, including others’ perceptions of 286 Contemporary Psychodynamic Psychotherapy one’s cultural group. These conflicts are negotiated in ways that can be adaptive and damaging at varying times (Tummala-Narra, 2016). Lobban (2016) noted that the nature of responses directed toward immigrants in the adopted cultural context regarding their otherness shape immigrants’ sense of double consciousness (Du Bois, 1994) and their ability to “stand in the spaces” (Bromberg, 2006) and freely experience and express their hybridity and multiplicity. When some aspects of identity either are not seen or are devalued in the broader dominant culture, they can become dissociated, and over time this contributes to a loss of contextual continuity (Boulanger, 2015; Ipp, 2010). It is also important to consider that many immigrants and refugees identify with aspects of their heritage culture and the adopted culture that are not recognized by others. This is evident in the case of an immigrant from Canada who is perceived by others as a native-born White American in the United States, in the case of a refugee who speaks English with a nondominant accent and is therefore perceived as not fluent in English, or in the case of a third-generation Mexican American who is perceived to be a foreigner. In these examples the experience of invisibility of identity influences how a person internalizes messages about his or her social position and sense of belonging in the heritage and adopted cultural contexts. Traumatic stress Psychoanalytic perspectives consider the overlaps and distinctions between experiences of interpersonal violence and political persecution and violence, all of which can involve fear of individual and group annihilation, identification with the aggressor, and individual and collective memories of traumatic events (Ainslie et al., 2013; Luci, 2017). In contemporary psychodynamic theory there is growing interest in the role of social and political contexts in the lives of immigrants and refugees, including issues such as war, torture, terrorism, genocide, civil war, colonization, deportation, and gender-based and race-based violence. The conceptualization of complex trauma (Herman, 1992) has been central to psychodynamic understandings of traumatic stress within the context of broader systemic injustice and violence. The experience of terror has been thought to pervade the intrapsychic life of survivors of these atrocities, as manifested in dissociation, dysregulated affect and sense of self, and bodily memories (Boulanger, 2008; Herman, 1992; Luci, 2017; Rothe, 2008). Harlem (2010) has written about dissociation as a core psychological state of exile. He stated, “An exile is not simply one who cannot (physically) return; she is someone who cannot ‘remember’ other versions of herself, who cannot bridge the gaps between versions of self, rooted in disparate times, physical spaces and relationships, who cannot ‘stand in the spaces’ between self-states” (Harlem, 2010, p. 460). The focus here is on the physical and psychological space between fleeing the country of origin and arriving in the new country, where parts of the self are lost, particularly as exile does not involve the choice of leaving the country of origin. Working with immigrants and refugees in psychodynamic psychotherapy 287 Severe traumatization among refugees has also been thought to cause a “loss of the freedom of inner movement,” referring to one’s freedom to think and make connections between thoughts and concepts, including “thinking and fantasizing about the past and future” (Harnischfeger, 2013, p. 24). This type of constriction poses challenges to an individual’s ability to explore various aspects of the self and to freely express his or her traumatic experience to others. Many immigrants and refugees cope with multiple forms of marginalization as they endure experiences of interpersonal violence and/or discrimination within their ethnic and religious communities in addition to oppression in the dominant cultural context (Tummala-Narra, 2016; Yi, 2014). For example, my patient Patrick, a gay Black immigrant from South Africa in his 50s, described his experience of growing up in the apartheid era and later emigrating to the United States, where racial discrimination took a new form: “When I was younger, I lived in fear of White people in South Africa. I still have to watch myself as a Black man here (in the U.S.). They can shoot me, pull me over.” In explaining what it feels like to be a gay South African American man, he stated, “There is no real acceptance within my family or my Church. I have to keep my distance and not say much to many people. Otherwise, my family gets hurt or feels ashamed.” Patrick was sexually assaulted as a child by a relative and has struggled with staying connected with his South African cultural heritage and community: “It’s hard to see people in my family and the Church not want to talk about violence against kids. They don’t want to open up any problems, just keep quiet. It’s hard to be with them.” Patrick’s experiences of marginalization within and outside of his ethnic and religious communities underscore the complicated nature of multiple types of trauma across contexts and its influence on identity. Considerations for psychodynamic psychotherapy Psychodynamic psychotherapy with immigrants, refugees, and their children must address the full range of complexity that is produced in the premigration, migration, and postmigration context and across the course of the life span. There are several considerations for a culturally informed psychoanalytic approach. In previous work I have outlined five core areas within psychodynamic psychotherapy that attend to sociocultural context: (1) recognizing clients’ and therapists’ indigenous cultural narrative and related conscious and unconscious meanings and motivations; (2) recognizing context in the use of language and the expression of affect in psychotherapy; (3) attending to the ways in which the client’s experiences of social oppression and stereotyping influence the therapist, client, therapeutic process, and outcome; (4) recognizing that culture is dynamic and that individuals negotiate complex, intersecting cultural identifications in both creative, adaptive ways and selfdamaging ways; and (5) expanding self-examination to include an exploration of historical trauma and neglect of sociocultural issues in psychoanalysis on psychoanalytic theory and practice (Tummala-Narra, 2016). In this framework, cultural 288 Contemporary Psychodynamic Psychotherapy competence is “a process of recognizing, understanding, and engaging with sociocultural context and its influence on intrapsychic and interpersonal processes, including the therapeutic relationship” (Tummala-Narra, 2016, p. 77). In a recent qualitative study with seasoned psychoanalytic psychologists, conceptualizations of cultural competence in psychoanalytic psychotherapy support these areas of emphasis in practice as they underscore the role of unconscious processes (e.g., affect, conflict, defenses) in identity development, relational life, and in the therapeutic process (Tummala-Narra et al., 2018). Bearing in mind this framework, I detail below specific areas of focus for working with immigrants and refugees in psychoanalytic or psychodynamic psychotherapy, particularly mourning and witnessing and also attending to transference and countertransference. Mourning and witnessing Psychotherapy with immigrants and refugees should consider the myriad ways in which separation, loss, and trauma are experienced by patients across the life span. The act of speaking about the details about separation, loss, and trauma in psychotherapy can trigger emotional and somatic experiences that have been dissociated for significant periods of time. As experiences of loss and trauma become dissociated, patients often do not actively initiate discussions about these experiences. It is important to consider that aspects of cultural and linguistic contexts are internalized in early, preverbal experiences with caregivers and that traumatic experiences can be encoded within the physical body rather than being symbolized in verbal language (Ainslie et al., 2013; Harnischfeger, 2016; Luci, 2017; Winnicott, 1971). Ainslie (1998) has used the term cultural mourning to describe the processes and strategies (including defenses) involved in repairing the loss of and/or separation from one’s heritage culture. Mourning in psychotherapy has been thought to be a core aspect of psychodynamic psychotherapy with immigrants, particularly as it influences an individual’s “third individuation” (Akhtar, 1999), which is characterized by attempts to consolidate cultural loss and change critical for identity formation. Another important part of mourning for many immigrants and refugees relates to the loss of hope for achieving a particular conceptualization of betterment, such as the “American dream,” that may have been a driving force for migration (Eng & Han, 2000). In nontraumatic and traumatic circumstances, immigrants and refugees can reflect in psychotherapy on various types of losses, such as the loss of extended family networks, changes in the family structure, the loss of heritage language use, and the loss of access to places of worship. Psychotherapy offers an important physical and psychological space in which an individual can freely explore complex feelings toward the heritage culture and toward the dominant society, thereby moving away from constrictions within sense of self, identity, and relationships. Therapists can initiate dialogue about patients’ experiences of the heritage culture, family, ethnic and religious communities, and experiences of migration, adjustment, loss, and hope within the dominant culture as a way of bridging cultural spaces while recognizing separation and loss. For example, a refugee patient may come to realize that he or she may never be able to visit Working with immigrants and refugees in psychodynamic psychotherapy 289 his or her birth country, and an immigrant patient may come to realize that his or her children may never understand the patient’s physical and psychological experience of living in the country of origin. In both cases the patient’s sense of self continues to shift in relation to the dominant culture and to the heritage culture. In other instances internal shifts required to adapt to the new cultural context are challenged by the fear of losing connection to the heritage culture or loved ones. Here, psychotherapy provides an opportunity for exploring split, discontinuous cultural experiences and identifications and for creating a transitional space in which the patient and therapist explore possibilities of the self that have not been previously considered (Oguz, 2012; White, 2015; Winnicott, 1971). Psychotherapy can also bridge the heritage and new languages when both languages can be present in the context of a bilingual psychotherapy, and the patient can access and express experiences by shifting across two or more languages. When the patient has suffered traumatic experiences, psychotherapy further involves an active engagement in which the patient feels validated as the therapist becomes a witness to the traumatic events and a container for the patient’s experiences of terror and alienation (Boulanger, 2008, p. 650). The act of witnessing involves listening to and responding to the realities of social, cultural, and political contexts and social oppression and to the patient’s ability to survive traumatic events and conditions. This process may also require the therapist to adopt nontraditional roles, such as advocating for the patient’s basic rights in a courtroom, workplace, medical facility, or school setting (Rothe, 2008; Tummala-Narra, 2016). Listening to the patient’s narrative through witnessing in psychotherapy allows for developing the capacity to “stand in the spaces between” various dissociated self-states (Bromberg, 2006; Yi, 2014). Yi (2014, p. 43) has described “cultural corrective experience” as critical to psychotherapy in which the therapist carefully becomes attuned to the patient’s traumas in addition to the patient’s family history and life experiences, as such attunement opens the possibility for the patient to transform his or her perceptions regarding culture, ethnicity, and other aspects of identity. The ability of the therapist to remain open to the ways in which the patient experiences loss and trauma and to how the patient expresses affective experiences to the therapist over time plays a significant role in the patient’s capacity for examining and working through defenses that constrict the possibility of mourning (Tummala-Narra, 2016). Transference and countertransference Working with immigrant and refugee patients in psychotherapy entails the complexities of negotiating cultural identifications. Because the process of migration is dynamic, it is important to bear in mind that the therapist may tend to focus on one aspect of sociocultural identity at the cost of attending to other aspects. Therapists and patients bring to their interaction their own life experiences, including their sociocultural histories and identifications. Roland (2005) pointed out that our cultural experiences are readily accessed through “comparative experiences” (p. 288). In other words, we tend to consciously recognize our own cultural worldviews when we encounter a patient from a culture that we perceive as different from our 290 Contemporary Psychodynamic Psychotherapy own. In the face of cultural difference a range of feelings are produced, such as anxiety, discomfort, curiosity, and excitement. These emotional experiences contribute to various behavioral responses in the therapeutic relationship. For example, the therapist who has read that Asian Americans prefer more directive forms of interaction with an authority figure may make an effort to engage with an Asian American client in what the therapist perceives would be a culturally sensitive manner. Yet this particular client may not prefer this type of interaction but rather is seeking a less directive therapist. The therapist’s approach in this case, while carrying positive intentions, does not take into account the heterogeneity of sociocultural experiences and cultural identifications among Asian Americans. Psychodynamic psychotherapy is particularly well suited for addressing the unique nature of sociocultural experiences, and therapists should remain open to listening for patients’ cultural experiences that seem contradictory and/or unexpected to therapists. This issue is also salient when the therapist and the client have cultural identifications that are less visible to each other (e.g., religious minority, sexual minority, survivor of political persecution and war) (Tummala-Narra, 2016). It is also critical to examine transference and countertransference dynamics rooted in cultural experiences and cultural bias. Contemporary psychoanalytic scholars note the importance of intersubjectivity in the therapeutic relationship, the mutual influence of the therapist and the client in transferential processes, and the role of sociocultural context in enactments in psychotherapy (Altman, 2010; Harlem, 2010; Yi, 2014). Patients’ and therapists’ unconscious experiences of and reactions to each other are shaped by their life experiences, of which sociocultural histories are a core component. Broader social, political, economic, and racial dynamics and discourse are reflected and often reproduced within the therapeutic relationship (Tummala-Narra, 2016). A patient, for example, may assume that a therapist with a name not typically associated with dominant culture is an immigrant or refugee with an accent. A therapist may assume that an immigrant or refugee patient with few economic resources does not have legal documentation to reside in the country. It is important to note that positive transference may also develop as a reflection of broader social dynamics and personal relationships. For instance, within a cross-cultural therapeutic dyad a therapist may develop positive feelings toward a new patient largely on the basis of the therapist’s experience with a friend or family member whose ethnicity is similar to that of the patient. Attending to transference-countertransference dynamics involves the therapist’s ability to carefully listen to the patient’s cultural or indigenous narrative while remaining aware of the potential impact of his or her own sociocultural experiences on what the therapist hears in the patient’s words (Seeley, 2005; Tummala-Narra, 2016). The therapist’s reactions to the patient’s worldviews and assumptions that contradict or conflict with those of the therapist can contribute to the therapist’s frustration with the client and avoidance of engaging in conflictual sociocultural and traumatic material in psychotherapy. The patient may also choose to avoid discussing certain topics as a result of a perception that the therapist is uncomfortable with these areas. In other instances a therapist and client who share Working with immigrants and refugees in psychodynamic psychotherapy 291 a common sociocultural background may not explore certain aspects of identity in an effort to avoid experiencing negative feelings toward each other. Akhtar (2011) highlighted several dilemmas facing immigrant analysts and therapists, including maintaining cultural neutrality, considering the patient’s motivation for the choice of an ethnoculturally different or similar analyst, examining the patient’s associations for culturally related transferences, conducting therapy or analysis in a nonheritage language, and avoiding shared projections, acculturation gaps, and collusions characterized by nostalgia. Immigrant analysts and therapists have also written about the impact of their own experiences of separation, loss, trauma, and discontinuity on their work with patients (Akhtar, 2006; Ipp, 2010; Khouri, 2012; Lobban, 2013). These writers have noted that their interactions with patients have been influenced by both their patients’ perceptions of them—due to their phenotype, accent, and bilingualism—and their own migration, cultural adjustment, social location, and clinical training experiences. Psychoanalytic scholars have cautioned against assumptions of sameness and difference regarding cultural experience within similar ethnic and cross-ethnic dyads (Akhtar, 2011; Lobban, 2013). This point is related to the importance of attending to intersectionality and the complexity of cultural experience. For example, my secondgeneration Indian American patient, who was similar in age to me, stated, “Well, you know how it is with Indian parents. I’m sure that you have had to deal with how strict they are. You were born here—so you know.” This patient’s fantasy that I was born in the United States because of my mainstream American accent and that I had been raised by parents perceived as strict and traditional was one that I related to only in part. In an effort to learn about her unique experience and to differentiate our experiences as Indian Americans, I responded to her by stating, “I do have Indian parents, but I don’t know what your Indian parents were like when you were growing up. Tell me about them and your experience of them.” The patient then proceeded to describe an experience of her parents that diverged significantly from my own life experiences. Conclusion Working with immigrants and refugees in psychodynamic psychotherapy involves engaging with multiple layers of intrapsychic, interpersonal, and sociocultural experiences, all of which shape identity, relational life, and psychological wellbeing. The heterogeneity of experiences among immigrants and refugees stands alongside shared experiences of separation, loss, and trauma. Cultural change, identity, and relationships are negotiated in adaptive and maladaptive ways, largely in the unconscious, across the life span. Psychodynamic psychotherapy offers a critical space for immigrants and refugees to mourn separation, loss, trauma, and discontinuity and to bridge cultural experiences and transform identity. The therapist is in a unique position to become attuned to multiple cultural narratives and aspects of identity, witness painful memories, and help patients to discover new possibilities for defining themselves amid cultural adjustment and change. 292 Contemporary Psychodynamic Psychotherapy References Ainslie, R. C. (1998). Cultural mourning, immigration, and engagement: Vignettes from the Mexican experience. In M. Suárez-Orozco (Ed.), Crossings: Immigration and the sociocultural remaking of the North American space (pp. 283 300). Cambridge, MA: Harvard University Press. Ainslie, R. C. (2011). Immigration and the psychodynamics of class. Psychoanalytic Psychology, 28(4), 560 568. Ainslie, R. C., Tummala-Narra, P., Harlem, A., Barbanel, L., & Ruth, R. (2013). Contemporary psychoanalytic views on the experience of immigration. Psychoanalytic Psychology, 30(4), 663 679. Available from https://doi.org/10.1037/a0034588. Akhtar, S. (1999). Immigration and identity: Turmoil, treatment, and transformation. Northvale, NJ: Jason Aronson. Akhtar, S. (2011). Immigration and acculturation: Mourning, adaptation, and the next generation. New York: Jason Aronson. Alegria, M., Chatterji, P., Wells, K., Cao, Z., Chen, C., Takeuchi, D., . . . Meng, X. (2008). Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatric Services, 59(11), 1264 1272. Available from https://doi.org/ 10.1176/appi.ps.59.11.1264. Altman, N. (2010). The analyst in the inner city: Race, class, and culture through a psychoanalytic lens (2nd ed.). New York: Routledge. American Psychological Association. (2010). Resilience and recovery after war: Refugee children and families in the United States. Washington, DC: Author. American Psychological Association. (2012). Crossroads: The psychology of immigration in the new century, Report of the APA Presidential Task Force on Immigration. Washington, DC: Author. Boulanger, G. (2008). Witnesses to reality: Working psychodynamically with survivors of terror. Psychoanalytic Dialogues, 18(5), 638 657. Boulanger, G. (2015). Seeing double, being double: Longing, belonging, recognition, and evasion in psychodynamic work with immigrants. The American Journal of Psychoanalysis, 75, 287 303. Bromberg, P. (2006). Awakening the dreamer: Clinical journeys. Mahwah, NJ: Analytic Press. Crenshaw, K. W. (1989). Demarginalizing the intersection of race and sex: A black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. University of Chicago Legal Forum, 1989, 139 167. Du Bois, W. E. B. (1994). The souls of Black folk. New York, NY: Dover. Eisold, B. (2012). The implications of family expectations, historical trauma, and prejudice in psychoanalytic psychotherapy with naturalized and first-generation Chinese Americans. Contemporary Psychoanalysis, 48(2), 238 266. Eng, D. L., & Han, S. (2000). A dialogue on racial melancholia. Psychoanalytic Dialogues, 10(4), 667 700. Available from https://doi.org/10.1080/10481881009348576. Foster, R. P. (1996). What is a multicultural perspective for psychoanalysis? In R. P. Foster, M. Moskowitz, & R. A. Javier (Eds.), Reaching across boundaries of culture and class: Widening the scope of psychotherapy (pp. 3 20). Northvale, NJ: Jason Aronson. Garcı́a-Coll, C., & Marks, A. (Eds.), (2012). The immigrant paradox in children and adolescents: Is becoming American a developmental risk? Washington, DC: American Psychological Association Press. Working with immigrants and refugees in psychodynamic psychotherapy 293 Grinberg, L., & Grinberg, R. (1989). Psychoanalytic perspectives on migration and exile. New Haven, CT: Yale University Press. Harlem, A. (2010). Exile as a dissociative state: When a self is “lost in transit. Psychoanalytic Psychology, 27, 460 474. Harnischfeger, J. (2016). Helpful thoughts: Some reflections on the psychodynamic treatment of traumatized refugees. International Journal of Applied Psychoanalytic Studies, 14(1), 22 34. Herman, J. L. (1992). Trauma and recovery. New York: Basic Books. Ipp, H. (2010). Nell—A bridge to the amputated self: The impact of immigration on continuities and discontinuities of self. International Journal of Psychoanalytic Self Psychology, 5(4), 373 386. Khouri, L. Z. (2012). The immigrant’s Neverland: Commuting from Amman to Brooklyn. Contemporary Psychoanalysis, 48(2), 213 237. Lijtmaer, R. M. (2001). Splitting and nostalgia in recent immigrants: Psychodynamic considerations. Journal of the American Academy of Psychoanalysis, 29, 427 438. Available from https://doi.org/10.1521/jaap.29.3.427.17301. Lobban, G. (2013). The immigrant analyst: A journey from double consciousness toward hybridity. Psychoanalytic Dialogues, 23(5), 554 567. Luci, M. (2017). Disintegration of the self and the regeneration of ‘psychic skin’ in the treatment of traumatized refugees. Journal of Analytical Psychology, 62(2), 227 246. Mahalingam, R., Balan, S., & Haritatos, J. (2008). Engendering immigrant psychology: An intersectionality perspective. Sex Roles, 59, 326 336. Migration Policy Institute (2017). Frequently requested statistics on immigrants and immigration in the United States. Retrieved from http://www.migrationpolicy.org/article/frequently-requested-statistics-immigrants-and-immigration-united-states Oguz, T. F. (2012). Concrete expressions of an “unformulated” discontinuity: Glimpses into the dissociative world of the immigrant. Contemporary Psychoanalysis, 48(1), 54 71. Pew Research Center (2017). Key findings about U.S. immigrants. Retrieved from http:// www.pewresearch.org/fact-tank/2017/05/03/key-findings-about-u-s-immigrants/ Robjant, K., Hassan, R., & Katona, C. (2009). Mental health implications of detaining asylum seekers: systematic review. The British Journal of Psychiatry, 194, 306 312. Roland, A. (2005). Between civilizations: Psychoanalytic therapy with Asian North Americans. Counselling Psychology Quarterly, 18(4), 287 293. Rothe, E. M. (2008). A psychotherapy model for treating refugee children caught in the midst of catastrophic situations. The Journal of the American Academy of Psychoanalysis and Dynamic Psychiatry, 36(4), 625 642. Ruth, R. (2012). Contemporary psychodynamic perspectives on multiple minority identities. In R. Nettles, & R. Balter (Eds.), Multiple minority identities: Applications for practice, research, and training (pp. 163 184). New York: Springer. Saketopoulou, A. (2015). Diaspora, exile, colonization: Masculinity dislocated. Studies in Gender and Sexuality, 16, 278 284. Seeley, K. (2005). The listening cure: Listening for culture in intercultural psychological treatments. The Psychoanalytic Review, 92(3), 431 452. Available from https://doi.org/ 10.1521/prev.92.3.431.66539. Sherry, S., & Ornstein, A. (2014). The preservation and transmission of cultural values and ideals: Challenges facing immigrant families. Psychoanalytic Inquiry, 34(5), 452 462. Suárez-Orozco, C. (2000). Identities under siege: Immigration stress and social mirroring among the children of immigrants. In A. Robben, & M. Suárez-Orozco (Eds.), Cultures 294 Contemporary Psychodynamic Psychotherapy under siege: Social violence & trauma (pp. 194 226). Cambridge, UK: Cambridge University Press. Suchet, M. (2004). A relational encounter with race. Psychoanalytic Dialogues, 14(4), 423 438. Tummala-Narra, P. (2009). The immigrant’s real and imagined return home. Psychoanalysis, Culture & Society. Special Issue: Immigration, 14(3), 237 252. Tummala-Narra, P. (2016). Psychoanalytic theory and cultural competence in psychotherapy. Washington, DC: American Psychological Association. Tummala-Narra, P., Claudius, M., Letendre, P., Sarbu, E., Teran, V., & Villalba, W. (2018). Psychoanalytic psychologists’ conceptualizations of cultural competence in psychotherapy. Psychoanalytic Psychology, 35(1), 46 59. White, C. J. (2015). Strangers in paradise: Trevor, Marley, and me: Reggae music and the foreigner other. Psychoanalytic Dialogues, 25(2), 176 193. Winnicott, D. W. (1971). Playing and reality. New York: Routledge. Yi, K. (2014). From no name to birth of integrated identity: Trauma-based cultural dissociation in immigrant women and creative integration. Psychoanalytic Dialogues, 24(1), 37 45. Dissociative processes bias the psychodynamics underlying the subjective experience of self and the organization of mind 20 Richard A. Chefetz1,2 1 Washington Baltimore Center for Psychoanalysis, Washington, DC, United States, 2 Institute of Contemporary Psychotherapy & Psychoanalysis, Washington, DC, United States A dear friend of mine was recovering from a cardiac valve replacement in the home of his girlfriend, who was away on travel. They had become increasingly close to each other and had been dating for several years. I asked him, “So how are things going with her?” He replied, “Oh, she’s just been totally wonderful. She was so present and responsive after my surgery. I wish she were here now. It feels funny being in her home without her.” “You must miss her a lot,” I observed. “Oh, I do,” he said. “You know, I just thought about something as you asked me about her, but I hadn’t put things together. She has this odd habit of eating several crackers before she comes to bed. I always tell her to keep the crackers on her side of the bed. I don’t want to sleep on cracker crumbs. When we’re at my place, I won’t even let her in the bedroom with her crackers. What I thought of when you said I must miss her is that ever since I started staying here without her, I find myself taking several crackers to bed with me and eating them before I go to sleep!” How did my friend not know what he was doing when he was doing it and then develop awareness of it only when we talked about his loving feelings for his girlfriend? Direct infant observation (Bick, 1968; Bowlby, 1958) eventually led to an appreciation of the impact of environmental disturbances on the developing mind in contrast to metapsychological drives gone awry (Bacciagaluppi, 1994; Rayner, 1991). Similarly, a multiple self-state model of mind (Bromberg, 1998; Federn, 1940; Ferenczi, 1955; Mitchell, 1991; Stern, 1997) was a paradigm-shifting embrace of interpersonal trauma guiding the formation of mind, whether that be developmental (parental preoccupation, dismissiveness, or alternating frightening and nonfrightening behavior) or blunt trauma (rape, bullying, beating). Dissociative processes are on an equal footing with associative processes in the achievement of a coherent mind (Chefetz, 2015a; Howell, 2005). We ignore dissociative processes at our personal and clinical peril. They provide parsimonious explanations for some seemingly insoluble clinical problems: Contemporary Psychodynamic Psychotherapy. DOI: https://doi.org/10.1016/B978-0-12-813373-6.00020-9 © 2019 Elsevier Inc. All rights reserved. 296 Contemporary Psychodynamic Psychotherapy sadomasochism, addictions, treatment-resistant depression, somatization disorders, unremitting posttraumatic stress disorder, bulimia, anorexia, chronic depersonalization, fugue, and multiple personality disorder, now known as dissociative identity disorder (DID). In DID there is an inability to maintain a single, coherent, whole sense of self; the sense of self is in disarray, and a person with DID is often at a loss as to explain his or her subjective experience: “How is it that I can be so competent at work one day and then with just the slightest emotional strain end up feeling like a child who wants to hide under the desk rather than tell the boss the additional merits of my project that I just told her about yesterday?” For the bulimic patient the lament sounds like this: “I was doing so well, and then for reasons I don’t understand, when 10 p.m. came around, I became fretful, and the next thing I knew, I had ordered a pizza. My belly hurt so badly by the time I finished stuffing my mouth that I ended up hugging the toilet bowl again; and that’s the last thing I remember before waking up this morning on the bathroom floor.” It’s not that all the conditions listed above always have underlying active dissociative processes, and it’s also true that dissociative processes gone awry are common enough that the therapist should remain open to the possibility of noticing something that could be life-changing for some individuals. For example, about 40% or more of people with borderline personality disorder have a dissociative disorder, and 40% or more of people with DID have borderline personality disorder (Brand & Lanius, 2014). Dissociative symptoms in borderline personality disorder are exceedingly important in regard to recalcitrance (Korzekwa, Dell, & Pain, 2009; Kleindienst et al., 2011; Zanarini, Frankenburg, Jager-Hyman, Reich, & Fitzmaurice, 2008; Zanarini, Ruser, Frankenburg, & Hennen, 2000). Parsing the differences between dissociative and borderline adaptations to living is critical to an effective approach to psychotherapy. A delicate balance between associative and dissociative processes Heuristically, as perception evolves, there is an unconscious sorting of mental content for salience, linking together felt experience with the ongoing narrative of the moment, and, ideally, creation of an intellectually honest and coherent appraisal. While an associative process establishes higher relevance, a dissociative process does the opposite, pruning from awareness what a mind unconsciously and automatically assesses doesn’t fit. The dissociative process also protects a mind from overload, facilitating focused attention by removing the extraneous from perception (e.g., the feeling of eyeglasses sitting on a nose), and can be actively enlisted via conscious intent (e.g., “I’m not going to think about that now, I don’t have time for it”) (Loewenstein, 1991). When our worldview can neither assimilate painful new experience nor enlarge itself to accommodate perceived danger (Horowitz, 1986), association may be halted (“I can’t think, it’s too upsetting!”), and dissociation may hold sway. Dissociative processes bias the psychodynamics underlying the subjective experience 297 Dissociation truncates destabilizing perception (e.g., “When the attack started, there was this odd calm that took me over, and my mind stayed clear while my body wasn’t in the picture. I didn’t notice I was bleeding until it was all over.”). Persistent, intensified, dissociative processes create a problem (e.g., “There’s never been a time in my life when I felt any different even though I knew other people had reactions I wasn’t having, and I don’t think I’m normal.”). Dissociation is normal, just like association. However, too much dissociation distorts and robs us of coherent reality, just as too much association is characteristic of obsessional styles of thinking (Chefetz, 2015a) and may become an obsessional plague of isolated affect, denial, and undoing (S. Freud, 1909). Some specific bias of unconscious activity by dissociative processes Dissociative processes are multidimensional: psychological, psychophysiological, neurobiological, and somatic. The more intense, sustained, and persistent dissociative processes wreak havoc upon perception and readily decontextualize painful experience into colorless, meaningless pablum. For example, psychic pain is enormous when a sadistic perpetrator physically or sexually brutalizes somebody and then softens the approach: “I can see you’re really hurting. I can see you’re really mad. I understand. I know you want to hit me. It’s okay. You can do it. It’ll be alright. Come on. Do it. You’ll feel a whole lot better if you just let go and hit me. I know you want to, don’t you?” Even a flicker of recognition in the victim that he or she wishes to lash out produces the perpetrator’s desired effect. If there is no flicker, the wish is correctly assumed: “See, you’re such a coward. You don’t have the guts to even try and protect yourself. The fact is, I know you like what I did to you. It’s just that you’re even more pathetic than I thought you were. You can’t even say it, you’re just pond scum and nothing more. If you were even a shadow of a person, you’d already have hit me, but you are nothing. You don’t even deserve to live. You’d do the world a favor if you just killed yourself. I’d do it, but you’re not worth the effort.”1 A child or adult mind crumbles under this onslaught. The shame of even existing predominates and cements in place a complex mix of selfhatred, fear, loathing, humiliation, and rage—none of which can be expressed outwardly, since the perpetrator then follows the diatribe with “The only thing you’re good for is to be hurt, just the way you like it.” And then the perpetrator hurts the target person yet again. Clinicians often write about anxiety or fear but rarely about terror. Intensity on the level of terror or profound shame can evoke a dissociative response. Anxiety 1 To read about the sequence of grooming efforts for pedophilic manipulation, see http://www.wvva.com/ story/16007807/penn-state-scandal-view-the-sandusky-grand-jury-transcript, the grand jury report on the activities of Jerry Sandusky at Pennsylvania State University. 298 Contemporary Psychodynamic Psychotherapy allows thinking to proceed, but fear or terror truncates that possibility (Davis, Walker, Miles, & Grillon, 2010; LeDoux & Pine, 2016). When a mind registers terror, it’s never just a little bit. There is no such thing as being half-terrified. To be in the grip of terror is to suffer an indignity, a profound sense of shame over loss of efficacy and agency. Rage may flicker to life under such an assault but is then humiliated and welded to the shame (Lewis, 1987). Fear of expressing anger often results. The circuit breaker of a dissociative process ensures emotional numbness, out-of-body experience (depersonalization), perceiving a veil covering what can be seen (derealization), partial or complete amnesia, identity confusion (forgetting one’s name), and identity alteration (e.g., “Who is that poor kid on the floor being raped? Glad I’m up here on the ceiling, safe. I’m Richard, and that kid down there is not me.”). Dissociative processes also include things like denial, isolation of affect, and disavowal. Yes, standard mechanisms of defense (Freud, 1936) have a dissociative engine under the hood. In denial the facts of a situation are kept unlinked from the counterfeit story of the event, while disavowal unlinks the reality of a behavior. In the wake of profound interpersonal trauma and dissociation, self-assertion and relatedness are feared. Anger is neither possible nor bearable. Humiliation is not tolerable. Confrontation and engaging in controversy are outside of the bounds of probability. Think of George and Martha in Who’s Afraid of Virginia Woolf (Albee, 1990) or the family scene in A Delicate Balance (Albee, 1966), or perhaps a Cat on a Hot Tin Roof is more to your illustrative liking (Williams, 2014). The toxicity of these family scenes is well known as the hell of adults. But what if you are 3 years old and in the middle of it all? An intensely activated dissociative process can be merciful at its inception, but it is a devil’s bargain when persistent. The parsimony of a multiple self-state model of mind An activated dissociative process leads to unintegrated remnants of infancy, childhood, latency, teenage, and early adult years, naturalistically congealing isolated self-states, as if without meaning or relationship, into a disorganized/disoriented arrangement (Main & Morgan, 1996). A model of mind in the clinician’s mind that is a match for the patient’s mind is uplifting for the patient and contributes to the feeling of being understood. A person wrote to me, after a recent consultation at which I administered the Cambridge Depersonalization Scale, “. . . the test you had me do was the first one given to me that actually spoke to me, that came closest to articulating what I am feeling, which is that I feel more fractured and disintegrated of late and it really isn’t fun.” This feeling of the clinician “getting it about me” is worth its weight in gold and then some. The challenge is to have a model that both fits the way people are and is anchored firmly in science. It is our good fortune that clinical science has finally caught up with our humanity. Sophisticated analyses of mother infant interaction show microattunements to nonverbal experience (Beebe et al., 2016) that likely underlie the feeling of being Dissociative processes bias the psychodynamics underlying the subjective experience 299 understood. The mental states of infancy persist into adulthood as patterned behaviors (Hesse, 1999; George, Kaplan, & Main, 1996; Lyons-Ruth, 2003; Main & Goldwyn, 1985; Ogawa, Sroufe, Weinfield, Carlson, & Egelend, 1997; Van IJzendoorn, 1995). Bowlby’s original descriptions of deactivation, segregated subsystems, and defensive exclusion (all dissociative processes) are part of enduring internal working models of self and the world (self-state formation) elaborated as the patterns of attachment in relation to discrete, repetitive, enduring behavioral states (Bowlby, 1980; Bretherton, 1992). Bowlby noted Anna Freud and Dorothy Burlingham’s observations at the Hampstead clinic: “children will cling even to mothers who are continually cross and sometimes cruel to them. The attachment of the small child to his mother seems to a large degree independent of her personal qualities” (Burlingham & Freud, 1942, p. 47, in Bowlby, 1958, p. 353). Bowlby also observed, “The extent to which the attachment seems to be independent of what is received is very plain in these records.” The child has a social tie to the mother, a way of “being with” the mother. These ways of being are what I observe in my adult dissociative patients who have “different ways of being” for different relational constellations that solidify into “different ways of being me.” The fabric of mind is relational. A multiple self-state model of mind is inclusive of these perspectives. Putnam’s discrete behavioral state model of mind (Putnam, 1997) was based significantly upon the observational work of Peter Wolff (1987) and later advanced that model (Putnam, 2016) to make use of the concept of “state spaces” promulgated by the work of the “baby watchers” in their study of infants and sleep patterns. The organization of self occurs in a naturalistic fashion (Stechler & Kaplan, 1980) that creates a knitting together of multiple states of being to provide the illusion of a unitary self. These are the states of mind that undergird the feeling of having a mind (Siegel, 1999). Wolff’s careful descriptions of the behavioral islands that infants occupy in one state or another—sleep, active alert, distress, hungry, and so on—easily comport with the notion of the healthy parent who builds bridges between islands as the attuned mother knows when her baby is about to need something. Healthy parents can feel the need before they can even tell you how they know it. Bowlby recognized how parents who never learned to be responsive to the needs of others—who lack bridge-building skills or who oppose building bridges that might threaten their own stability—can have a powerful formative effect on the mind of the child, as psychodynamics take a direct hit and become indelibly biased toward isolating selfstates and favoring discontinuity of self and other perception. Putnam’s borrowed concept of the state space derived from mapping things such as heart rate, respiratory rate, and physical movement in three dimensions allowed computer plotting of behavioral patterns. These patterns repeated as a sequential and somewhat predictable series of state changes that involved movement from states such as active alert to hungry, satiated, sleepy, inactive alert, and so on. Of note was that some state space shifts were unidirectional, for example, from satiated to sleepy; shifts from sleepy to satiated did not occur. It is more challenging to track state-space shifts in adults, but in highly dissociative individuals the switches 300 Contemporary Psychodynamic Psychotherapy are more obvious, since there may be a change in posture, a change in the person’s fund of knowledge, an abridged life history, a constricted range of affect, time distortion (state-related flashback quality misattributions of year, place, and situation), or elevated adrenalin secondary to anticipation of abuse. Wise clinicians learn to watch a patient’s respiratory rate and depth of respiration, degrees of physical tension, stigmata of rapid heart rate (e.g., venous neck pulsations), and tapping of fingers or foot or leg movement as signs of affective disturbance that may not be conscious for the patient and represent an impending or already completed statespace change that would predict future behavior. These switches are observable as unpredictable or unreliable behaviors and a changeable worldview; discontinuity of experience is the password for understanding such a person’s life and clinical presentation (Chefetz, 2015b). It’s as if two different people, with different sensibilities, take turns speaking while appearing to be one person. It can be confusing. For example, an especially sophisticated upper-level manager in a large corporation had, in her early childhood, hidden in a closet to escape repetitive violent rape. A shift in ergonomic planning by her company and a move to a new headquarters building completely undid her usual calm at work. Bereft of her familiar office and unable to unconsciously hide and regroup herself emotionally with the new open office glass walls, she became uncharacteristically frightened of going to work. She accumulated some degree of absenteeism before reporting the change to me. Asking her to tell me the details of her experience led (after barely 10 seconds of her effort) this 50-year-old woman in business attire, but now with fear on her face, to draw her knees under her chin while sitting in the chair in my office. Making an apparent effort to wedge herself into the corner of the upholstery, she began to squeal a distress call that was somehow both muffled and also pierced the air between us as a keening that was nearly unbearable to hear. I was confronted with the childlike state space of the past, manifested as a more organized self-state accompanied by flashback-quality experience. Sadly, this is frequently the standard work in the psychotherapy of complex posttraumatic stress disorder and the dissociative disorders. This is not regression; it is a dissociative process in action. Another theoretical approach to the psychology of mental states and “the way we are” is the theory of mentalization (Bateman & Fonagy, 2006; Fonagy, Gergely, Jurist, & Target, 2003; Fonagy & Target, 2007; Gergely, Nadasdy, Csibra, & Biro, 1995; Gergely & Watson, 1996) that is unintentionally supportive of a multiple self-state model of mind while focusing on the importance of mental states. Cognitive-affective-interpersonal schemas (Luyten, Blatt, & Fonagy, 2013) are an extension of the early theory of mentalization, which emphasizes some of the core concerns of a multiple self-state psychology (Chefetz & Bromberg, 2004). The achievement of reflective function and theory of mind arises from the developmental trajectory described by mastering psychic equivalence, pretend, and teleological modes of thinking. This builds on earlier work regarding intentionality and causality (Dennett, 1971) as modes of thinking. The notion of the alien self (Fonagy et al., 2003) is in lockstep with the multiple self-state model but is not noted as such. Achieving a capacity for reflective functioning, the ability to imagine the mental states of others, is predictive of positive outcome in psychotherapy Dissociative processes bias the psychodynamics underlying the subjective experience 301 (Cologon, Schweitzer, King, & Nolte, 2017). The ability to first imagine and then attune to isolated mental states in one’s own mind is also predictive of positive outcome in the psychotherapy of DID, in my experience. Some regulatory tasks creating coherent consciousness The psychodynamics of self-states tend to be organized around two unconscious tasks: narrative regulation and affect regulation. When dissociative processes hold sway and go beyond simple pruning to maintain everyday coherent mentation, they act in the service of achieving a counterfeit assimilation or accommodation of a worldview by eliminating memories (amnesias) or distorting the facts of the events (typically denial and disavowal) to change the narrative into a consciously acceptable story (e.g., “I had a normal childhood and a typical family life”) and/or reducing one’s capacity to know feeling (e.g., “That doesn’t mean anything to me, I feel nothing about what happened or who was involved, it just is”). This is typical of complex PTSD (Herman, 1992) or borderline personality disorder (Zanarini et al., 2008). Deflection, dissembling, and grossly misleading statements or actions befuddle and confuse the uneducated therapist. Active or passive neglect in childhood, blunt or developmental trauma, repetitive childhood medical or surgical illness, bullying (Teicher, Samson, Sheu, Polcari, & McGreenery, 2010), parental alcoholic rages, emotionally violent marital discord, traumatic narcissism (Shaw, 2013), and dissociatively held parental trauma (Yehuda et al., 2014) generate these constellations of dissociative adaptation in childhood. Psychodynamics are profoundly influenced by dissociative processes that hide from awareness the underlying meanings of experience, behavior, and motivation. Affect regulation often succumbs to depersonalized numbness, obsessional isolation, secondary alexithymia, and explosive failures to contain the unbearable as it demands expression. Profound bias of psychodynamics by dissociative processes A 35-year-old man with DID, who had been in twice-weekly psychotherapy for 10 years, was increasingly disturbed by tension with his wife and his awareness of his deep love for her simultaneous with his wish to not be touched and his frequent, but entirely intermittent, fascination with the bodies of men. As his psychotherapy progressed, he became aware of a self-state oriented to about age 4 who occupied an internal transitional space (Chefetz, 2015a) complete with the subjective experience of being on a raft. Being touched interrupted the reverie of the emotional isolation contingent with being on the raft and put him at risk of emotional overload. Fascination with the bodies of men began with an experience during his teenage years that left him and others wondering whether he was homosexual. His profound depersonalization, of which he had earlier been unaware, and his lack of being able 302 Contemporary Psychodynamic Psychotherapy to feel himself alive in his body produced a longing to know what it felt like to be an alive man, a man with a body. Consciousness of these dynamics and a deep discussion directly with the isolated self-states of the patient (Kluft, 2006) led to resolution of his need to keep at a physical distance from his wife and to the rekindling of their sexual relationship. Preoccupations with men’s bodies dissolved as his depersonalization grossly decreased. Without an understanding of dissociative processes, an unknowing clinician might simply have found these problems unresolvable or assumed that the patient was more interested in being with men than with women. Dissociative processes distort psychodynamics and are essential to our understanding of our humanity in the wake of developmental or frank traumatic experience. Conclusion In the study of being human it is often true that extremes teach us much about what is in the middle. Dissociative processes are normal. When they are provoked to a higher level of activation and persist long after their utility has expired, they distort subjective experience and psychodynamics. The clinician who is interested in cases that don’t improve after much effort should take a good look at dissociative experience and how those processes guide psychodynamics. If it doesn’t help a particular person now, this new knowledge and curiosity will likely not wait for long before it is rewarded with growth in another human being. References Albee, E. (1966). A delicate balance: a play in three acts. Samuel French, Inc. Albee, E. (1990). Edward Albee’s Who’s Afraid of Virginia Woolf? Dramatists Play Service Inc. Bacciagaluppi, M. (1994). The relevance of attachment research to psychoanalysis and analytic social psychology. Journal of the American Academy of Psychoanalysis, 22(3), 465. Bateman, A., & Fonagy, P. (2006). Mentalization-based treatment for borderline personality disorder. Oxford: Oxford University Press. Beebe, B., Messinger, D., Bahrick, L. E., Margolis, A., Buck, K. A., & Chen, H. (2016). A systems view of mother infant face-to-face communication. Developmental psychology, 52(4), 556 571. Bick, E. (1968). The experience of the skin in early object relations. International Journal of Psychoanalysis, 49, 484 486. Bowlby, J. (1958). The nature of the child’s tie to his mother. The International journal of psycho-analysis, 39, 350. Bowlby, J. (1980). Attachment and loss: Volume III. Loss: Sadness and depression. New York: Basic Books. Dissociative processes bias the psychodynamics underlying the subjective experience 303 Brand, B. L., & Lanius, R. A. (2014). Chronic complex dissociative disorders and borderline personality disorder: disorders of emotion dysregulation? Borderline personality disorder and emotion dysregulation, 1(1), 13. Bretherton, I. (1992). The origins of attachment theory: John Bowlby and Mary Ainsworth. Developmental psychology, 28(5), 759 775. Bromberg, P. M. (1998). Standing in the spaces. Hillsdale, N.J.: The Analytic Press. Burlingham, D., & Freud, A. (1942). Young children in war-time. London: Allen and Unwin. Chefetz, R. A. (2015a). Intensive psychotherapy for persistent dissociative processes: The fear of feeling real. New York: W.W. Norton. Chefetz, R. A. (2015b). Ten Things to Consider on the Road to Recognizing Dissociative Processes in Your Psychotherapy Practice. Psychiatry, 78(3), 288 291. Chefetz, R. A., & Bromberg, P. M. (2004). Talking with “Me” and “Not-Me”: A dialogue. Contemporary Psychoanalysis, 40(3), 409 464. Cologon, J., Schweitzer, R. D., King, R., & Nolte, T. (2017). Therapist reflective functioning, therapist attachment style and therapist effectiveness. Administration and Policy in Mental Health and Mental Health Services Research, 44, 614 625. Davis, M., Walker, D. L., Miles, L., & Grillon, C. (2010). Phasic vs sustained fear in rats and humans: role of the extended amygdala in fear vs anxiety. Neuropsychopharmacology, 35(1), 105 135. Dennett, D. C. (1971). Intentional systems. The journal of Philosophy, 68(4), 87 106. Federn, P. (1940). The determination of hysteria versus obsessional neurosis. Psychoanalytic Review, 27, 265 276. Ferenczi, S. (1955). Confusion of tongues between adults and the child (1933) (Original title: “The passions of adults and their influence on the sexual character development of children). Final contributions to the problems and methods of psychoanalysis (pp. 155 167). New York: Basic Books. Fonagy, P., & Target, M. (2007). The rooting of the mind in the body: New links between attachment theory and psychoanalytic thought. Journal of the American Psychoanalytic Association, 55(2), 411 456. Fonagy, P., Gergely, G., Jurist, E. J., & Target, M. (2003). Affect regulation, mentalization and the development of the self. New York: Other Press. Freud, A. (1936). The Ego and the Mechanisms of Defense. New York: International Universities Press, (p. 1946). Freud, S. (1909). Notes upon a case of obsessional neurosis. In J. Strachey (Ed.), The Standard Edition (Vol. 10). London: Hogarth Press. George, C., Kaplan, N., & Main, M. (1996). Adult attachment interview. The Authors. Gergely, G., & Watson, J. S. (1996). The social biofeedback theory of parental affect-mirroring: The development of emotional self-awareness and self-control in infancy. International Journal of Psychoanalysis, 77, 1181 1211. Gergely, G., Nadasdy, Z., Csibra, G., & Biro, S. (1995). Taking the intentional stance at 12 months of age. Cognition, 56, 165 193. Herman, J. L. (1992). Complex PTSD: a syndrome in survivors of prolonged and repeated trauma. Journal of Traumatic Stress, 5(3), 377 391. Hesse, E. (1999). The adult attachment interview: Historical and current perspectives. Horowitz, M. J. (1986). Stress response syndromes. New York: Jason Aronson. Howell, E. F. (2005). The dissociative mind. Hillsdale, NJ: Analytic Press. Kleindienst, N., Limberger, M. F., Ebner-Priemer, U. W., Keibel-Mauchnik, J., Dyer, A., Berger, M., et al. (2011). Dissociation predicts poor response to dialectial behavioral 304 Contemporary Psychodynamic Psychotherapy therapy in female patients with borderline personality disorder. Journal of personality disorders, 25(4), 432 447. Kluft, R. P. (2006). Dealing with alters: a pragmatic clinical perspective. Psychiatric Clinics of North America, 29, 281 304. Korzekwa, M. I., Dell, P. F., & Pain, C. (2009). Dissociation and borderline personality disorder: An update for clinicians. Current psychiatry reports, 11(1), 82 88. LeDoux, J. E., & Pine, D. S. (2016). Using neuroscience to help understand fear and anxiety: a two-system framework. American Journal of Psychiatry, 173(11), 1083 1093. Lewis, H. B. (1987). The role of shame in symptom formation. Hillsdale, N.J: Lawrence Earlbaum Associates, Inc. Loewenstein, R. J. (1991). An office mental status examination for complex chronic dissociative symptoms and multiple personality disorder. In R. J. Loewenstein (Ed.), Psychiatric Clinics of North America (Vol. 14, pp. 567 604). Philadelphia: W.B. Saunders Company. Luyten, P., Blatt, S. J., & Fonagy, P. (2013). Impairments in self structures in depression and suicide in psychodynamic and cognitive behavioral approaches: Implications for clinical practice and research. International Journal of Cognitive Therapy, 6(3), 265 279. Lyons-Ruth, K. (2003). Dissociation and the parent-infant dialogue: a longitudinal perspective from attachment research. Journal of the American Psychoanalytic Association, 51(3), 883 911. Main, M., & Goldwyn, R. (1985). Adult attachment interview. Growing points of attachment theory. Monographs of the Society for Research in Child Development. Main, M., & Morgan, H. (1996). Disorganization and disorientation in infant strange situation behavior: phenotypic resemblance to dissociative states. In L. K. Michelson, & W. J. Ray (Eds.), Handbook of dissociation: Theoretical, empirical, and clinical perspectives (pp. 107 138). New York: Plenum Press. Mitchell, S. A. (1991). Contemporary perspectives on self: Toward an integration. Psychoanalytic Dialogues, 1, 121 147. Ogawa, J. R., Sroufe, L. A., Weinfield, N. S., Carlson, E. A., & Egelend, B. (1997). Development and the fragmented self: Longitudinal study of dissociative symptomatology in a nonclinical sample. Development and Psychopathology, 9, 855 879. Putnam, F. W. (1997). Dissociation in children and adolescents. New York: The Guilford Press. Putnam, F. W. (2016). The Way We Are: How states of mind influence our identities, personality, and potential for change. New York: IPBooks.net. Rayner, E. (1991). The independent mind in British psychoanalysis. Jason Aronson. Shaw, D. (2013). Traumatic narcissism: Relational systems of subjugation. New York, NY: Routledge. Siegel, D. J. (1999). The developing mind: Toward a neurobiology of interpersonal experience. New York: Guilford Press. Stechler, G., & Kaplan, S. (1980). The development of the self—A psychoanalytic perspective. Psychoanalytic Study of the Child, 35, 85 105. Stern, D. B. (1997). Unformulated experience: From dissociation to imagination in psychoanalysis. Hillsdale, N.J.: The Analytic Press. Teicher, M. H., Samson, J. A., Sheu, Y.-S., Polcari, A., & McGreenery, C. E. (2010). Hurtful words: Association of exposure of peer verbal abuse with elevated psychiatric symptom scores and corpus callosum abnormalities. American Journal of Psychiatry, 167(12), 1464 1471. Dissociative processes bias the psychodynamics underlying the subjective experience 305 Van IJzendoorn, M. H. (1995). Adult attachment representations, parental responsiveness, and infant attachment: A meta-analysis on the predictive validity of the Adult Attachment Interview. Psychological Bulletin, 117(3), 387. Williams, T. (2014). Cat on a hot tin roof. Bloomsbury Publishing. Wolff, P. (1987). The development of behavioral states and the expression of emotions in early infancy: New proposals for investigation. Chicago: University of Chicago Press. Yehuda, R., Daskalakis, N. P., Lehrner, A., Desarnaud, F., Bader, H. N., Makotkine, I., et al. (2014). Influences of maternal and paternal PTSD on epigenetic regulation of the glucocorticoid receptor gene in holocaust survivor offspring. Amercian Journal of Psychiatry, 171, 872 880. Zanarini, M. C., Frankenburg, F. R., Jager-Hyman, S., Reich, D. B., & Fitzmaurice, G. (2008). The course of dissociation for patients with borderline personality disorder and axis II comparison subjects: A 10-year follow-up study. Acta Psychiatrica Scandanavica, 118(291-296). Zanarini, M. C., Ruser, T., Frankenburg, F. R., & Hennen, J. (2000). The dissociative experiences of borderline patients. Comprehensive Psychiatry, 41(3), 223 227. Psychodynamic psychotherapy with former child soldiers: meeting the murderous self 21 Nel Draijer and Pauline Van Zon Private practice Introduction UNICEF (2007) defined a child soldier as any person below 18 years of age who is or has been recruited or used by an armed force or armed group in any capacity, including but not limited to children, both boys and girls, used as fighters, cooks, porters, messengers, or spies or for sexual purposes (p. 7). Child soldiers are used by both rebel armies and government troops. Africa has the largest number of child soldiers. Most of these children are forcibly recruited and abducted by armed groups. Others join the groups for the purposes of survival or to avenge slain family members (Betancourt et al., 2010; Schauer & Elbert, 2009). The consequences of being a child soldier are considerable. These youths grow up in extreme and savage conditions in which only the strongest survive. They form the bottom of the pecking order and therefore are the target of constant abuse, molestation, and harassment. These children are deprived of necessary care and protection by family and community and miss key services such as healthcare and education. The majority of child soldiers have been victims, witnesses, and/or perpetrators of severe violence and cruelties, such as combat situations, bombings, decapitations and amputations, burning people alive, and rape (Betancourt et al., 2010). After war they are vulnerable to reintegration failure not only because they were exposed to traumatic events but also because they are blamed and stigmatized because of their affiliation with the conflict (Schauer & Elbert, 2009). If granted asylum in more stable countries, they are often subjected to lengthy and exhausting asylum procedures. Once again, they are confronted with an inability to fully participate in society because of the minimal rights they are granted during the asylum procedure. They suffer from the loss of their social role, future possibilities, and their own cultural surroundings, such as language of origin, customary food, and social networks. Contemporary Psychodynamic Psychotherapy. DOI: https://doi.org/10.1016/B978-0-12-813373-6.00021-0 © 2019 Elsevier Inc. All rights reserved. 308 Contemporary Psychodynamic Psychotherapy Trauma and dissociation among former child soldiers Prolonged exposure to toxic forms of violence, especially in childhood, has devastating long-term consequences. In response to threat, aggressive states quickly and dramatically alternate with fearful flight or avoidance states. Because children are often physically incapable of fighting off their captors or fleeing a situation, the most common reaction to traumatic events is to detach themselves from the external and internal worlds through dissociation, by which they experience numbing, depersonalization, and derealization (Schauer & Elbert, 2009). Youths who are exposed to such a degree of violence and threat are often unable to complete developmental tasks such as forming safe attachment relationships, a stable and integrated concept of self and others, and the competence to self-regulate emotion and behavior (Van der Kolk, 2005). The reaction of many former child soldiers to repeated and prolonged interpersonal trauma may be best described in terms of concepts such as complex trauma or developmental trauma disorder (Cloitre, 2009; Klasen, Daniels, Oettingen, Post, & Hoyer, 2010; Van der Kolk, 2005). The symptom profile refers to the presence of PTSD with additional disturbances in the domains of affect regulation, interpersonal relatedness, and self-identity. In addition to complex PTSD, these patients often suffer from depression and DID, in which both the memories of atrocities and participating “perpetrator parts” are totally split off from awareness. These selfstates (or alters) are often described as “protector parts”; they are emotional parts of the personality that are “fixated in the protective ‘fight’ subsystem, and attempt to manage the difficult emotions of rage and anger and to avoid feelings of hurt, fear or shame” (Van der Hart, Nijenhuis, & Steele, 2006, p. 82). For former child soldiers, relatively minor stressors can trigger classic fight, flight, or freeze reactions, manifested by severe aggression and/or regressed dissociative states. These individuals have difficulties controlling aggressive impulses and perceive violence as a legitimate means of achieving one’s aims. Consequently, they tend to have insufficient skills to handle daily life without aggression. When treating such patients, clinicians are pulled into the reenactments of old trauma scenarios and become part of a wild therapeutic dance of approach and avoidance that can feel like war, often facing severe transference and countertransference challenges. Transference-focused psychotherapy and its application Transference-focused psychotherapy (TFP), an evidence-based, manualized, psychodynamic treatment based on object relations theory (Clarkin, Levy, Lenzenweger, & Kernberg, 2007; Clarkin, Yeomans, & Kernberg, 2006; Doering et al., 2010; Yeomans, Clarkin, & Kernberg, 2002), is well suited for working with the fundamental core of aggression and oppression that is common among individuals who have experienced complex trauma, such as former child soldiers. It was developed to treat patients Psychodynamic psychotherapy with former child soldiers: meeting the murderous self 309 suffering from severe personality disorders, that is, with a borderline personality organization (Kernberg, 1984). The term borderline personality organization refers to a psychological structure characterized by identity diffusion (a fragmented and fluctuating sense of self involving oscillation of self-and-other representations and emotions linked between them) and “primitive” defenses (splitting, denial, and projective identification) with reality testing generally intact but prone to distortions under stress. The patient communicates not only verbally and nonverbally but also via projective identification (so-called belly talk), in which untolerated emotional states are externalized and induced in and sensed by the therapist. The aim of TFP is to integrate these conflicting inner self-and-other states into a more coherent personality structure. The basic assumption of TFP is that human beings are social animals (who want to bond and be autonomous as well) whose inner worlds consist fundamentally of relational elements, dyads, consisting of images of self and other (the object) and the linking emotion. In borderline personality organization this inner world is divided into all-good and all-bad dyadic elements that are perceived as being in conflict with each other and kept apart through the process of splitting. In severely traumatized patients this basic division is further accentuated by dissociation. The theoretical questions about how splitting and dissociation interrelate and whether splitting itself is a dissociative, trauma-related phenomenon are beyond the scope of this chapter. In fact, in severely traumatized patients splitting and dissociation are totally intertwined. Nevertheless, the key idea is that splitting is driven by conflict: the conflict between the tendency to approach, to seek intimacy, and to bond and the tendency to avoid contact and dependency and to defend against being hurt or controlled (i.e., the dynamics of love vs aggression). The all-good dyads consist of longing and perfect loving relationships with an ideal object, such as perfect mothers or fathers. These all-good dyads, because they are not integrated with true shortcomings and disappointments, are unrealistic and can thus contribute to pathological frustration and a rapid shift into the reverse allbad dyads. All-bad dyads consist of images of persecutory or dominating relationships based on a mix of past subjective reality, one’s own aggressive affects, identification with aggressors, and strong fears. In relationships and in psychotherapy the inner dyads oscillate: the anxious victim inside, fearing retaliation by an overpowering other, can suddenly switch into a dominating force attacking the now-weak other. If the therapist is experienced as a bad object, the patient may attack to protect himself or herself from being overpowered, thus enacting aggression without full awareness of being aggressive. This model of object relations thinking has the therapist exploring these projections empathically with the patient, looking as if through the patient’s eyes. This perspective is very helpful in understanding and handling the constant push and pull in moment-to-moment interactions in the treatment of patients with personality disorders as well as severe dissociative disorders (Draijer, 2009, 2010a,b). TFP interventions consist of exploring the inner world of the patient and his or her view from that world of the therapist. To be able to do this, it is particularly important to fully experience the transference in the here-and-now (“What is the patient making of me?”), empathically following the patient in his or her creation 310 Contemporary Psychodynamic Psychotherapy of the therapist, containing the dyad expressed in it, and presenting this to the patient. Thus an intervention might be constructed as follows: “When I properly listen to you, it is as if you see me as a cruel and dominating person. That must be a very scary situation for you.” When patients experience being understood properly by the containment of having the relationship articulated the way they perceive it, they suddenly calm down, even if in an angry state of mind, and are able to start reflecting on what is happening. Once the reflective functioning of the patient begins to improve—which can take quite a while—the task for the therapist is to confront the patient carefully with inconsistencies and oscillations between dyads, raising the patient’s empathic curiosity about his or her own inner world. An example intervention would be the following: “That is interesting. Just a few minutes ago our conversation seemed quite intimate, and you shared your sadness with me, apparently perceiving me as a safe and reliable listener, but suddenly it seemed that you perceived me as a threat that you have to protect yourself against by reclaiming total power. How do you combine these two states of mind?” Finally, when the patient is able to reflect on and experience the therapeutic relationship as supportive, at least some of the time, it is the task of the therapist to interpret the defensive layering of opposing dyads. Interpretation in TFP is a process that leads to presenting the positive and negative dyads simultaneously to the patient, relating them. For example, “Could it be that your anger is so extreme, distancing you from me, because you feel so vulnerable when you realize that you long deeply for a safe relationship with a reliable parental figure?” or “Could it be that you seem to prefer to see me as totally unreliable, because perceiving me as trustful and reliable makes you feel so terribly sad about your losses? Could it be that by doing this, you protect your heart against losing a loved one for a second time?” So interpretation is concerned primarily with “you and me” in the here-and-now rather than the exposition of links between present and past. This whole step-by-step interactional and interpretational process (Caligor, Diamond, Yeomans, & Kernberg, 2009) results in the gradual mitigation of anger and rage and eventually in the integration of the personality. In TFP the patient is held responsible for his or her own recovery; this means that in the beginning of treatment a contract is made about (self-)destructive acting out, and the therapist explains to the patient that this behavior is in opposition to a development toward health. When the patient might point out that he or she knows only one solution for conflict—to use violence—the therapist holds the patient responsible for preventing it: “All feelings are welcome and respected, even murderous rage, as long as we can talk about it and not act on it.” When the patient has noticed a tendency to act out or when he or she actually does, the patient is asked to mention it first thing in the next session. To prevent repetition of the cycle of abuse, “the soldier needs to learn how to talk.” Supporting Evidence Empirical support for the effectiveness of TFP has been established through a series of randomized controlled trials by different research groups (see Chapter 10: Psychodynamic psychotherapy with former child soldiers: meeting the murderous self 311 Transference-focused psychotherapy for borderline and narcissistic personality disorders, for a summary of this work). For example, studies by Clarkin et al. (2007) and Doering et al. (2010) have shown that TFP was equally as effective as or more effective than various comparison treatments (including dialectical behavioral therapy, supportive dynamic therapy, and treatment by experienced community psychotherapists) for patients with borderline personality disorder. These studies also demonstrated that TFP is uniquely associated with improvements in reflective functioning and attachment as well as positive change in personality organization and functioning. Although the effectiveness of TFP for former child soldiers has not yet been investigated, the available evidence is nonetheless relevant, as the patients included in the previous studies also tended to carry with them histories of complex traumas (but, of course, not related to such violence as witnessed and experienced by former child soldiers). Transference-focused psychotherapy illustrated in case material Ishmael is a 24-year-old man from Sierra Leone who has been in the Netherlands since 2003. The first time the therapist met him, Ishmael had unsuccessfully been in psychotherapy for 3 years in which stabilization and support were the key focus. It soon became clear that Ishmael was highly ambivalent about treatment; he was motivated but scared of the intimacy inherent in psychotherapy. Ishmael’s biggest fear was of losing control of his aggression when being triggered and harming an innocent person. He had gotten into fights with others, including his girlfriend. He met criteria for DID, PTSD, and depression as well as personality disorder not otherwise specified. He suffered from amnesia and brief psychotic episodes, including auditory comments and visual hallucinations. He had been suicidal occasionally and hospitalized once. He reported feelings of severe distrust, guilt, and shame; extreme loneliness; a sense of not belonging; and a sense of being dehumanized. He said, “Sometimes I feel I am more an animal than a human being.” Ishmael described his early years in Sierra Leone as moderately happy. When he was 8 years old, rebels killed his mother in front of him, and he was captured. He has never seen his father and sister since. Ishmael was forced by the rebels to stay with them in the jungle as a child slave. There, he experienced and witnessed innumerable cruelties and was forced to participate in them. After five years he was able to escape and managed to stay alive in Freetown. Currently, he is in the middle of an asylum procedure. The main problem in the first phase of psychotherapy was Ishmael’s inability to remain psychologically present while relating to others. This would manifest in the form of dissociation (e.g., switching into other states of mind, being absent) or in extreme dominance, aggression, and oppression of the therapist. He reported paranoid feelings; having extreme fears of being abused, exploited, or humiliated; and feelings of not being cared for. He was unable to use the affect regulation techniques that were taught to him. When exposed to his aggression, the therapist often 312 Contemporary Psychodynamic Psychotherapy felt overwhelmed by fear and struggled to reflect on what was going on. TFP offered a framework that made sense in understanding these confusing forces, the pushing and pulling, the reenactments. Moving to TFP marked the transition from a one-person model of understanding the patient and his symptoms to a two-person model of understanding the patient and the dynamic interpersonal forces he experiences. When asked about the differences in approach after this transition, the first thing that came to the therapist’s mind was this: “So much more contact and understanding of what he is going through, since I empathically explore and see through his eyes the person he is making of me. Dissociation and aggression became understandable as a means to regulate distance and intimacy in our relationship.” Using Clarkin et al.’s (2006) overview of the dominant dyads in the transference and countertransference, we illustrate some of these in this case example (see Table 21.1). The following transference-countertransference interaction demonstrates the dynamic nature of dyadic relationships. In reaction to his vulnerability in sharing with the therapist one of his most traumatic experiences and becoming sad, Ishmael suddenly switched into a different state. The therapist experienced the following: I feel overwhelmed by his sudden shift to aggression. His eyes sharpen, and in a derogative manner he says, “Can’t you see? There is fighting everywhere around you.” His gaze hardens and becomes indifferent. His lips slightly curl in a sadistic smile. It seems that I am part of the reliving of a violent and cruel traumatic experience in which we are facing each other in a combat situation. I no longer see the Ishmael I know; I see an extremely dangerous and threatening rebel who’s capable of anything. I wonder if he sees the same threat in me. I feel confused. My body is warning me that there is danger, and I am hyperaroused. I catch myself looking at his hands, wondering if he could attack. Right now I want to stay sharp, but chaos takes hold of me. I am no longer able to reflect on what is going on and am drowning in a flood of fear. In the meantime I’m desperately searching for my therapeutic framework and tools, but they seem to be washed away. I feel paralyzed and helpless. I can’t win this battle, he’s stronger, and I surrender to him . . . Is this what he wants to achieve with his aggression? I point out his aggression and ask what is happening inside of him. He seems startled; his aggression suddenly disappears, he denies being angry or afraid; now he is the one who’s confused and vulnerable. I am suddenly the perpetrator, and he is the victim. I don’t want to be the perpetrator. There’s confusion again. Table 21.1 Dominant dyads in transference-countertransference. Patient Therapist Controlling, omnipotent self Abused victim Out-of-control, angry child Dependent, gratified child Friendly, submissive self Weak, slavelike other Sadistic attacker/persecutor Incompetent, useless parent Perfect provider Doting, admiring parent Psychodynamic psychotherapy with former child soldiers: meeting the murderous self 313 Here we see an aggressive defense against sadness and vulnerability as well as the reenactment of trauma but in the reversed, dominant position, unwittingly scaring the therapist to a terrifying submission and confusion. The patient seems to evoke in the therapist the extreme fear that the patient is unable to verbalize. There is an oscillation between the sadistic attacker/persecutor and the abused victim. The first task of the therapist is to tolerate—and not act upon—this almost unbearable fear. If the therapist is able to survive this fear and to keep reflecting on what is happening between her and the patient, taking a respectful and neutral stance, she is increasingly able to contain the bad object projected onto her and to try to engage the patient in reflecting on or symbolically holding what had previously existed as a raw, unsymbolized affect state. The therapist’s empathic curiosity engages the patient in seeing that the intense state that overwhelms him may exist in a broader context of other internal states and thus not comprise the whole of reality or of the relationship. This shared curiosity in turn has the effect of modifying the object, especially its intensity and its one-dimensional quality. Room for reflection, be it just a second or two, and tolerance for affect are slowly but gradually growing as all affects are accepted, tolerated, and contained by the therapist. A process takes place within the patient in which he slowly brings together representations of the attacker he fears and the empathic and reflecting other he experiences and may secretly long for—both of which are reflections of internal states within him. This is thought to be an integrative process in which the persecutory objects and selfstates in the patient become gradually detoxified (Scharff & Tsigounis, 2003). Sometime later, the therapist struggles with overwhelming feelings of powerlessness and sadness, empathizing with the patient. Now the patient seems to be better able to tolerate his vulnerable state as well as being connected with the therapist, with the therapist noting the following: Ishmael expresses intense feelings of worthlessness related to atrocities he experienced as a victim. He longs for peace of mind and death. I feel his selfloathing and pain. Unable to tolerate it, I try to change his guilty and shameful perspective on himself but notice it does not fit his needs. He lets me know that he has no room for it. I tell him that I understand that wanting to change his perspective was a futile attempt to deal with my own feelings of powerlessness that his sadness induced. I add: “We could let the sadness exist here as we sit together, without having to talk about it.” He remarks that he would like that, especially because there is nowhere else where he can just let his sadness exist. Our eyes meet and his sadness hits me. He sees that my eyes become moist, and I say that his sadness affects me. For a moment he turns his head away but then meets my gaze again, and I can see that he allows his sadness to exist in my presence. There is an intense moment of meeting. At the end of the session, Ishmael tells me that through experiencing and sharing his sadness, he feels “more connected” and less lonely. From a dyadic perspective the therapist’s feelings of powerlessness and sadness emerge from the patient’s perceptions of and interactions with her (i.e., projection 314 Contemporary Psychodynamic Psychotherapy and projective identification). In this instance the therapist first wanted to comfort the patient prematurely and get away from the sadness, acting out the way the patient regularly does. Then the patient was aware of the sadness in the therapist, as she was willing to sit it out with the patient, tolerating the sadness together. Being there in the sadness together restored his tolerance for connection, for relatedness, for the mother that he had lost. After 18 months of TFP, the therapist notices a remarkable increase in and tolerance for intimacy and vulnerability in the therapeutic relationship. This development represents access to the previously split-off libidinal segment of the patient’s internal world. He is more able to verbalize and tolerate painful experiences and strong emotions. There are fewer oscillations between emotional states, and there is less black-and-white thinking. The aggression has become less wild, destructive, and scary and seems to be gradually melting away. Aggressive feelings, thoughts, and fantasies are openly shared in therapy. Ishmael is better able to regulate emotions and to assert himself nonviolently. At the symptom level there are fewer nightmares, fewer flashbacks and less reliving of states of terror, less dissociation, less avoidance of traumatic material, less distrust, and fewer feelings of guilt and shame. Auditory comments and visual hallucinations have receded. With respect to DID, patients are more able to stay in the present moment, emotional states are less fragmented and less separated by amnesia. Emotional states are less fragmented and less separated by amnesia. Severe traumatic experiences concerning atrocities are no longer told only through the murderous self but now are also told in sad and more reflective states. Ishmael lives a less isolated life; he has more contact with the outside world through his volunteer work, hobbies, and even a budding friendship. Discussion In the treatment of former child soldiers from Africa with DID and PTSD, TFP helps to address the aggression of these patients and their tendency to seek total control and dominance over or oppression of the therapist. TFP provides a useful model for understanding the severe problems with split-off aggression as well as the sudden and confusing shifts in the mental states of the patient, addressing transference-countertransference, the therapeutic dance of push-and-pull interactions, and reenactments between patient and therapist instead of addressing primarily symptoms situated in the patient. This touches also on the discussion of working from either a one-person or a two-person psychology perspective in understanding and treating extreme trauma. The case described here moved from a one-person perspective with limited success (focusing on symptoms and psychopathology perceived solely in the patient) to a two-person psychological model in which the focus was on the dynamics as perceived between the patient and the therapist in the form of splitting, projective identification, and oscillating self-and-other states. This helped the patient to emotionally regulate, to start mentalizing, to socialize, and to Psychodynamic psychotherapy with former child soldiers: meeting the murderous self 315 integrate more, both internally and externally. Instead of following the traditional phase-oriented trauma therapy, affect regulation was strengthened by focusing on enhancing secure attachment in the therapeutic relationship. This represents a move from PTSD seen primarily as an anxiety disorder toward (complex) PTSD (and DID) perceived primarily as relational disorders characterized by isolation, loneliness (disconnection), distrust of others, lack of soothing, lack of comforting inner relationships, rage toward mankind, shame, and guilt. In other words, complex stress-related disorders such as DID are seen as disorders of personality, identity, and affect regulation—relational disorders altogether—and are well suited to psychodynamic treatments that work in the here-and-now of the therapeutic relationship. After 18 months of TFP, we observed improved affect regulation as well as mentalization and relatedness in this patient. The improved affect regulation could possibly be attributed to the fine attunement by the therapist to, and containment of, the dominant dyads and the emotional states linked to them in the here-and-now of the interaction. Supporting this hypothesis is a study by Levy, Clarkin, et al. (2006) and Levy, Meehan, et al. (2006) that showed a development toward improved reflective functioning and security of attachment in borderline patients after 1 year of TFP; more secure attachment leads to better affect regulation (Schore, 2005). One could argue that TFP is similar to mentalization-based therapy; the major difference is that in TFP the oscillation, the conflict between different dyads, is central. Moreover, as the transference is addressed, the therapist is less of a coach and more of a participant in the dance; TFP is thus more experiential than cognitive. Finally, TFP respects aggression as a central dynamic force to be addressed in the therapy relationship. Views on aggression and how to treat it diverge considerably. Some treatment models do not address it at all (assuming that it comes from an “alien self”), others solely try to control it (more cognitive-behavioral types of anger management) or suppress it (e.g., through medication). However, in TFP it is considered essential and vital (and in a way healthy) in the inner dynamics. We have the clinical impression that in severely traumatized patients for whom aggression does not surface in treatment directly, aggression may be channeled through nightmares and self-harm. In this way it is projected onto inner representations of perpetrators as a safe way to experience aggression (expressing it internally). Such patients also have (aggressive) oppressive inner representations that vie for total control, arising from identification with their childhood aggressors. From a TFP perspective, in order to reach some form of integration, balance, and health, it is essential that the patient’s aggression is addressed and acknowledged as belonging to the patient himself or herself. We observe that not all patients are able or willing to face this, and they feel that there is no way forward but to stay oppressed by holding onto their identity as a victim, perpetually attacked by projected aggression. The TFP therapist takes part in the dance but tries to keep reflecting on what happens between them. The therapist does this in a respectful way, remaining neutral toward the conflicts in the patient, accepting the challenging emotional states 316 Contemporary Psychodynamic Psychotherapy that may be evoked by the patient’s perceptions and interactions. To use the metaphor of a harbor, all ships are allowed in; no ship needs to stay at sea (i.e., all feelings and mental states, however negative they may be, are welcome in the relationship with the therapist). The therapist then acts as a reflecting mirror in which the patient sees a more integrated image of himself or herself than what the patient is projecting. The containment of aggression and hatred is a precondition on the road toward the integration of good and bad. The “murderous self” needs to be seen, respected, welcomed, and appreciated for what it means to the entire person: It is the keeper of horrible memories, and it watches over the patient to avoid being hurt again. This aspect of self is extremely lonely (dehumanized) and convinced that no one will ever like it or be close to it. If this dangerous and hateful part of the patient feels that it is understood, respected, and appreciated, the patient’s hate slowly starts to melt (see Draijer, 1999). Only then is there room for mourning and deep sadness. Patients who have killed need to mourn, and rituals of mourning and regret may be introduced. Finally, for the therapist to learn to make himself or herself emotionally available to the inner world of the patient, to participate in this dance and to recognize it and reflect on it in order to make an intervention, supervision is a conditio sine qua non. To develop this emotional availability, this mental skill and awareness of induced feelings and processing them into an intervention, the therapist needs a safe and accepting relationship with a supervisor. Conclusion Extreme aggression and a self-state of a killer poses severe problems for patients with dissociative disorders, alienating them from other people, preventing intimacy, and inducing fear in their psychotherapists. This problem is hardly addressed in much of the theory or research on PTSD, in which treatment focuses primarily on anxiety. Anger and aggression are central in severe traumatization, causing patients to feel guilty, bad, and isolated, leaving them struggling for control, and alienating them from fellow humans. This is particularly the case when patients have been forced to kill. In the treatment of former child soldiers with DID suffering from split-off aggression, TFP helps to address these aggressive parts and their tendency to seek total control over, or oppression of, others, including the therapist. It also helps to free patients from their internal oppression. The authors thank Dr. Frank Yeomans, MD, PhD, for his very helpful remarks. This chapter is an extended version of: Nel Draijer PhD & Pauline Van Zon MA (2013): Transference-Focused Psychotherapy with Former Child Soldiers: Meeting the Murderous Self, Journal of Trauma & Dissociation, 14:2, 170 183. Copyright © Taylor & Francis Group, LLC ISSN: 1529-9732 print/1529-9740 online DOI: 10.1080/15299732.2013.724339 Psychodynamic psychotherapy with former child soldiers: meeting the murderous self 317 References Betancourt, T. S., Borisova, I. I., Williams, T. P., Brennan, R. T., Whitfield, T. H., de la Soudiere, M., . . . Gilman, S. E. (2010). Sierra Leone’s former child soldiers: A followup study of psychosocial adjustment and community reintegration. Child Development, 81, 1077 1095. Caligor, E., Diamond, D., Yeomans, F. E., & Kernberg, O. F. (2009). The interpretive process in the psychoanalytic psychotherapy of borderline personality pathology. Journal of the American Psychoanalytic Association, 57, 271 301. Chemtob, C. M., Novaco, R. W., Hamada, R. S., Gross, D. M., & Smith, G. (1997). Anger regulation deficits in combat-related posttraumatic stress disorder. Journal of Traumatic Stress, 10(1), 17 36. Chu, J. A. (1998). Rebuilding shattered lives. New York, NY: Wiley. Clarkin, J. F., Levy, K. N., Lenzenweger, M., & Kernberg, O. F. (2007). Evaluating three treatments for borderline personality disorder. American Journal of Psychiatry, 164, 922 928. Clarkin, J. F., Yeomans, F. E., & Kernberg, O. F. (2006). Psychotherapy for borderline personality: Focusing on object relations. Arlington, VA: American Psychiatric Publishing. Cloitre, M. (2009). Effective psychotherapies for posttraumatic stress disorder: A review and critique. CNS Spectrums, 14(1), 32 43. Doering, S., Hörz, S., Rentrop, M., Fischer-Kern, M., Schuster, P., Benecke, C., . . . Buchheim, P. (2010). Transference-focused psychotherapy v. treatment by community psychotherapists for borderline personality disorder: Randomised controlled trial. British Journal of Psychiatry, 196(5), 389 395. Draijer, N. (1999). Pathologische haat en traumatisering; de worsteling met afstand, nabijheid en herinnering [Pathological hatred and traumatization: The struggle with approach, avoidance and memory]. In G. F. Koerselman, & W. Tilburg (Eds.), Haat [Hatred] (pp. 55 74). Tricht, Netherlands: Foundation Psychoanalysis and Psychiatry. Draijer, N. (2009, November). Transference focused psychotherapy (TFP) techniques in the treatment of DID. In Preconference workshop at the international conference of the International Society for the Study of Trauma and Dissociation. Washington, DC. Draijer, N. (2010a, April). Transference focused psychotherapy (TFP) techniques in the treatment of DID. In 2nd international conference of the European Society for Trauma and Dissociation. Belfast, Ireland. Draijer, N. (2010b, October). An object-relational approach to problematic (counter) transference, working with patients with severe trauma related disorders (DID, C-PTSD, BPD). In Workshop at the international conference of the International Society for the Study of Trauma and Dissociation. Atlanta, GA. Ehntholt, K. A., & Yule, W. (2006). Practitioner review: Assessment and treatment of refugee children and adolescents who have experienced war-related trauma. Journal of Child Psychology and Psychiatry, 47, 1197 1210. Glancy, G., & Saini, M. A. (2005). An evidenced-based review of psychological treatments of anger and aggression. Brief Treatment and Crisis Intervention, 5(2), 229 248. Kernberg, O. F. (1984). The structural interview. In O. F. Kernberg (Ed.), Severe personality disorders: Psychotherapeutic strategies (pp. 27 51). New Haven, CT: Yale University press. Klasen, F., Daniels, J., Oettingen, G., Post, M., & Hoyer, C. (2010). Posttraumatic resilience in former Ugandan child soldiers. Journal of Trauma & Dissociation, 14, 170 183, 2013 183. 318 Contemporary Psychodynamic Psychotherapy Levy, K. N., Clarkin, J. F., Yeomans, F. E., Scott, L. N., Wasserman, R. H., & Kernberg, O. F. (2006). The mechanisms of change in the treatment of borderline personality disorder with transference focused psychotherapy. Journal of Clinical Psychology, 62, 481 501. Levy, K. N., Meehan, K. B., Kelly, K. M., Reynoso, J. S., Weber, M., Clarkin, J. F., & Kernberg, O. F. (2006). Change in attachment patterns and reflective function in a randomized control trial of transference-focused psychotherapy for borderline personality disorder. Journal of Consulting and Clinical Psychology, 74(6), 1027 1040. Mills, J. (2005). Treating attachment pathology. Oxford, England: Rowman & Littlefield. Nicholl, C., & Thompson, A. (2004). The psychological treatment of post traumatic stress disorder (PTSD) in adult refugees: A review of the current state of psychological therapies. Journal of Mental Health, 13(4), 351 362. Orth, U., & Wieland, E. (2006). Anger, hostility, and posttraumatic stress disorder in traumaexposed adults: A meta-analysis. Journal of Consulting and Clinical Psychology, 74, 698 706. Saini, M. A. (2009). Meta-analysis of the psychological treatment of anger: Developing guidelines for evidence-based practice. Journal of the American Academy of Psychiatry and the Law Online, 37, 473 488. Scharff, J. S., & Tsigounis, S. A. (2003). Self-hatred in psychoanalysis: Detoxifying the persecutory object. New York, NY: Brunner-Routledge. Schauer, E., & Elbert, T. (2009). The psychological impact of child soldiering. Retrieved from http://www.fotres.ch/index.cfm?action 5 act_getfile&doc_id 5 100518. Schore, A. N. (2005). Attachment, affect regulation, and the developing right brain: Linking developmental neuroscience to pediatrics. Pediatrics in Review, 26, 204 211. UNICEF. (2007). Paris principles: Principles and guidelines on children associated with armed forces or armed conflict. New York, NY: Author. Van der Hart, O., Nijenhuis, E. R. S., & Steele, K. (2006). Structural dissociation and the treatment of chronic traumatization. New York, NY: Norton. Van der Kolk, B. A. (2005). Developmental trauma disorder: Towards a rational diagnosis for chronically traumatized children. Psychiatric Annals, 35, 401 408. Yehuda, R. (1999). Managing anger and aggression in patients with posttraumatic stress disorder. Journal of Clinical Psychiatry, 60(15), 33 37. Yeomans, F. E., Clarkin, J. F., & Kernberg, O. F. (2002). A primer of transference focused psychotherapy for the borderline patient. Northvale, NJ: Jason Aronson. Psychodynamically informed treatment for trauma in the context of refugee crises and political violence 22 Christiane Steinert1,2, Johannes Kruse1,3, Falk Leichsenring1, Helga Mattheß4 and Wolfgang Wöller5 1 Department of Psychosomatics and Psychotherapy, University of Giessen, Giessen, Germany, 2Department of Psychology, MSB Medical School Berlin, Berlin, Germany, 3 Department of Psychosomatics and Psychotherapy, University of Marburg, Marburg, Germany, 4University of Worcester, Worcester, United Kingdom, 5Rhein-Klinik, Hospital for Psychosomatic Medicine and Psychotherapy, Bad Honnef, Germany According to the United Nations, more than 65 million individuals are currently displaced as a result of armed conflicts and persecution (United Nations Refugee Agency, 2016). Most of these refugees either are displaced internally or have fled across national borders to neighboring countries. For example, more than one million refugees have entered the region of Europe since 2015, leading to the largest inflow of refugees since World War II (Silove, Ventevogel, & Rees, 2017; United Nations Refugee Agency, 2016). Consequently, there is a huge gap between the need for mental health services and the availability of such services in low-income countries, postconflict settings, and regions facing large numbers of refugees. As a result, many care systems are faced with a need for effective, low-threshold, and culturally adaptable mental health treatments, including brief forms of trauma therapy, since many refugees experience war, violence, and other traumatic events. Epidemiological data on mental health problems among refugees have accumulated since the inclusion of posttraumatic stress disorder (PTSD) in the DSM-III (for an up-to-date overview, see Silove et al., 2017). For example, the largest review so far reported data on more than 81,000 refugees and other conflictaffected populations from 40 countries (Steel et al., 2009). The prevalence rates of PTSD and depression were about 30% each, with very large variations across studies (0% 99% and 3% 85.5%, respectively). According to Silove et al. (2017), more rigorously designed studies yielded noticeably lower prevalence rates, reducing the estimate for PTSD to 15%, which still by far exceeds the PTSD estimate among nonrefugee populations (e.g., Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). Although long-term follow-ups of refugees are rare, available evidence indicates that a majority of refugees experience mild or no symptoms, while a significant minority of refugees gradually recover, and a small group shows a chronic course of symptoms and impairment (Silove et al., 2017). Contemporary Psychodynamic Psychotherapy. DOI: https://doi.org/10.1016/B978-0-12-813373-6.00022-2 © 2019 Elsevier Inc. All rights reserved. 320 Contemporary Psychodynamic Psychotherapy Psychotherapeutic treatments that have been systematically studied in postconflict settings or the context of refugee crises have usually comprised brief interventions based on cognitive-behavioral techniques (Nickerson, Bryant, Silove, & Steel, 2011), including trauma confrontational methods such as narrative exposure therapy (Ertl, Pfeiffer, Schauer, Elbert, & Neuner, 2011; Neuner et al., 2008) or EMDRR-TEP [eye movement desensitization and reprocessing (EMDR)-recent traumatic episode protocol], which is an EMDR application focusing on recent traumatic events with an extended time perspective (Acarturk et al., 2016). While the efficacy of treatments that include trauma confrontation is generally well established (Bisson & Andrew, 2007), there have long remained uncertainties about the efficacy of other forms of psychological treatments for PTSD, especially those not focusing on traumatic memories. This question may be particularly important in work with refugees suffering not only from mental health problems but also from postmigrational stressors such as insecure residency status, restricted access to services, and a lack of opportunities to work or study. Clients facing such complicated conditions may not have “the motivation, resilience or cognitive capacity to engage in exposure therapies or to implement the techniques of cognitive behavioral therapy which require active practice to be effective” (Silove et al., 2017, p. 132). In recent years, evidence for psychotherapy without trauma confrontation has emerged. These forms of treatment are primarily based on psychodynamic or interpersonal principles. For example, a randomized controlled trial (RCT) by Markowitz et al. (2015) compared interpersonal therapy (IPT), a nonexposure based psychotherapy, and prolonged exposure (PE), a cognitive-behavioral form of trauma treatment and the current gold standard in PTSD treatments. It was shown that IPT was noninferior to PE. The effectiveness of psychodynamically based, nonconfrontative, resourceoriented approaches has been documented in (nonrandomized) controlled studies with patients suffering from complex trauma (Lampe, Hofmann, Gast, Reddemann, & Schussler, 2014; Sachsse, Vogel, & Leichsenring, 2006) and refugees from former Yugoslavia (Kruse, Joksimovic, Cavka, Wöller, & Schmitz, 2009). This form of treatment has also been successfully applied in a naturalistic setting, treating a large sample of tsunami survivors with complex trauma and PTSD in Aceh in Indonesia (Bumke & Sodemann, 2010). Recent evidence for this kind of therapy also comes from an RCT conducted in Cambodia. The trial investigated whether 5 sessions of resource-oriented psychodynamic trauma therapy combined with EMDR resource installation, known for short as ROTATE (the treatment that will be described in this chapter), was more effective than a waiting list control group (WLCG). ROTATE showed significant reductions in PTSD symptoms (the primary outcome) compared to the WLCG (between-group effect size Cohen’s d 5 2.59, a large effect). The same was true for all secondary outcomes, that is, anxiety, depression, and functioning. Thus a psychodynamic approach to treating trauma-related and comorbid disorders showed promising effects both in refugees and in individuals from postconflict communities. It is the aim of this chapter to highlight important aspects and main principles of this approach. Psychodynamically informed treatment for trauma in the context of refugee crises 321 Resource-oriented trauma therapy combined with EMDR resource installation Development and main principles ROTATE is a psychodynamically informed, manual-guided approach to treating PTSD and comorbid disorders that was developed by psychodynamically oriented clinicians and researchers in Germany and further refined through training courses that have been delivered in China, Haiti, Thailand, and Indonesia (Mattheß & Sodemann, 2014; Reddemann, 2012; Wöller, Leichsenring, Leweke, & Kruse, 2012; Wöller & Mattheß, 2016). Despite including EMDR elements, it does not involve any form of trauma confrontation. Instead, resource development and installation (RDI), a resource-building EMDR technique, is used (Korn & Leeds, 2002). ROTATE is especially suitable for clients with complex trauma conditions such as PTSD, comorbid disorders, and impaired psychosocial functioning. However, it should be noted from the beginning that ROTATE is not a comprehensive psychotherapy for clients suffering from complex trauma conditions that usually go along with a broad range of trauma-related symptoms and interpersonal problems and for which longer treatments are usually needed. The Consensus Model of Trauma Therapy (Horowitz, 1973; Reddemann, 2012) describes stabilization, trauma processing, and reintegration phases of treatment for complex trauma conditions. ROTATE represents the stabilization phase and thus is an important step to reduce severe posttraumatic symptoms. Such stabilization is especially vital for clients living in low-income countries or postconflict regions and for refugees; these individuals often face multiple social challenges and a lack of availability of long-term psychotherapy. ROTATE is thus designed as a short-term intervention. Normally, 5 10 therapy sessions of 50 minutes each seem appropriate. However, more sessions can be added if necessary. ROTATE adheres to two main principles: (1) a psychodynamic relationship orientation and (2) resource orientation and installation. Psychodynamic relationship orientation Psychodynamic theory has provided the deepest understanding of relationship issues, and from the very beginning, psychodynamic authors underscored the importance of trust and relationship themes involved in interpersonal trauma (Ferenczi, 1949; Reddemann, 2012). The psychodynamic relationship orientation implies an understanding of the client’s symptoms against the background of current and earlier interpersonal relationships. Hence psychodynamic work generally aims not only at modifying the client’s symptoms, but also at taking into account and influencing interpersonal relationships that contribute to the current symptom pattern. Psychodynamic therapy operates on a supportive-expressive continuum of interventions (Luborsky, 1984). Supportive interventions aim to foster a secure therapeutic alliance, which itself may be regarded as a prerequisite for strengthening 322 Contemporary Psychodynamic Psychotherapy psychosocial abilities (ego functions) that are temporarily not available to a client, for example, because of traumatic events. The use of more supportive or more interpretive (insight-enhancing) interventions depends on the client’s needs. The more severely disturbed a client is or the more acute the client’s problem is, the more supportive and less interpretive interventions are required and vice versa (Luborsky, 1984; Wallerstein, 1989). Regarding ROTATE, there is a clear focus on the supportive side of this continuum with the aim of building and maintaining ego functions (e.g., emotion regulation). The repertoire of psychodynamic interventions to strengthen a client’s ego functions has been broadened by incorporating other techniques, such as guided imagery (Reddemann, 2012). For example, the safe place imagination technique can help clients improve their feeling of safety, while the container technique is a useful distancing technique for flashbacks in PTSD (see below). Applying ROTATE as a psychodynamically based intervention does not imply using a neutral or abstaining therapeutic style. Instead, a therapeutic style that actively addresses a client’s needs and encourages problem solving and resource activation is recommended. Moreover, the therapist invites his or her clients to regularly practice and perform exercises on their own. If needed, the therapist provides calming, relieving, and other supportive interventions, addresses maladaptive and self-destructive behavior patterns, and encourages more adaptive behaviors. This type of therapeutic style is in line with modern relational and structural psychodynamic approaches (e.g., Rudolf, 2013). Resource orientation and resource installation Considering that trauma interferes with a client’s access to positive emotions and coping capacities, resource activation is a key element of the ROTATE approach. In this context, activation of positive emotions and images is considered crucial for the development of resilience. A vast amount of research suggests a strong relationship between positive emotions, adaptive coping, and resilience (Folkman & Moskowitz, 2000). Resources can be differentiated into internal and external resources. Internal resources include capacities or competencies, pleasant activities, positive memories of the past, positive visions of the future, and positive inner images created by guided imagery. External resources include support by others (family members, friends, or organizations), work, or exercise. The goal of resource activation is to help clients evoke positive emotional states by activating internal resources (the central therapeutic tool for improving emotion regulation) and external resources (e.g., the ROTATE therapist may assist clients in contacting people or organizations that may give the clients the support they need). This can be accomplished by evoking memories of positive relationship experiences or by stimulating inner awareness of positive experiences. In terms of psychodynamic ego psychology, activation of internal resources means enhancing a client’s mastering and coping competencies (Bellak, Hurvich, & Gediman, 1973), as ideally the ego will gain new strength and a feeling of control. In terms of psychodynamic object relations theory (Kernberg, 1976) it can be understood as a process of restoring the ability to activate positive internalized object relationships. As was mentioned above, Psychodynamically informed treatment for trauma in the context of refugee crises 323 ROTATE also contains a modification of RDI, a resource-developing and resourceactivating EMDR technique. Unlike the standard EMDR protocol (Shapiro, 2001), RDI does not focus on traumatic memories, given that activating and working with traumatic memories is not the goal. Rather, RDI is a strategy to develop and strengthen coping strategies, resources, and positive emotional states (Korn & Leeds, 2002). If necessary, ROTATE may be combined with traditional trauma confrontational techniques (Wöller et al., 2012). In this context it serves as a preparatory stabilization phase for confrontative techniques to be safely applied. However, ROTATE as it is described here does not contain such techniques. Cultural adaptation and advantages of ROTATE in the context of postconflict settings and refugee crises Resource-activating interventions can be modified according to the specific needs of the client and the context; thus ROTATE techniques can be applied in a transcultural context. ROTATE therapists are strongly encouraged to modify the protocols according to the culture and personality of the clients. If a therapist finds it too difficult for a client to closely follow a treatment protocol, the therapist should use local metaphors and exercises so that the client can understand the protocol easily and work on it effectively (see examples below). ROTATE takes into account the complex nature of trauma in, for example, victims of human-made disasters and genocide. Thus instead of focusing solely on PTSD symptoms, ROTATE also considers the mental comorbidities that are typically found in these clients, notably depression and anxiety. For this reason ROTATE can be safely applied even to complex trauma conditions; no major side effects have been observed so far. The approach is especially suitable for clients from nonwestern countries, since traditional healing resources, bodily reactions, and other somatic aspects can be integrated in an overall framework of resource activation. Also, ROTATE is not solely language based and can therefore probably be viewed as more culturally flexible than other forms of psychotherapy. As another advantage, its basic elements can be taught to paraprofessionals (e.g., lay counselors) or peers with a cultural background similar to that of the client who receive basic training in psychotraumatology and trauma-related disorders and can provide interventions such as stabilization, psychoeducation, and resource activation under professional supervision (Wöller, 2016). The latter aspect is of importance not only for disseminating the approach’s basic elements among the vast number of traumatized clients, but also for overcoming language barriers (Wöller, 2016). Applying ROTATE in clinical practice: basic techniques Establishing feelings of safety and control in the therapeutic relationship There are various reasons, external and internal, why a sense of safety may be difficult to obtain. Examples include ongoing violence, a somatic disease, suicidal 324 Contemporary Psychodynamic Psychotherapy impulses, lack of housing or other adverse economic conditions, and negative transference in the form of an unconscious fear of being humiliated or rejected by the therapist. To improve a client’s feeling of safety, the ROTATE therapist might ask the client what he or she needs to feel more comfortable in the therapeutic situation. This may include talking outside of the therapy room in case a patient feels uncomfortable or locked up when inside the room. Actively inquiring about a client’s feeling of safety is necessary, as clients will usually not spontaneously disclose feeling uncomfortable or unsafe in a therapeutic situation. For example, the therapist may say something like the following: Please tell me what you need to feel safer and more comfortable in this room. Please make sure both of our seating positions are okay. Maybe you would like me to sit closer or farther away from you? Maybe you would like to relocate your chair? In consideration of traumatized clients’ frequent fears of losing control, their sense of being in control is extremely important and should be strengthened whenever possible. Therefore the therapist needs to explain that the client will maintain full control over whatever happens during treatment. Thus to avoid the client feeling dominated, the therapist strives to involve the client in all decisions concerning the therapy, and clients are routinely asked whether they find the therapist’s recommendations helpful. Another important aspect of establishing a sense of safety and control concerns dealing with self-endangering behavior and suicidal impulses, which should be addressed with top priority throughout therapy. For emergency situations the therapist and client develop a detailed emergency plan. The client should know what to do and whom to contact when suicidal thoughts become unmanageable. Therapeutic goals Next to feeling safe and comfortable, a good therapeutic relationship also implies that an agreement on goals and tasks has been established. Rather than giving the client premature advice about what to do, the therapist should take his or her time to find out what the client’s objectives for treatment are. The therapist should ask detailed questions to ensure a clear understanding of the client’s goals and regularly check whether the client is still “on the same boat.” In this context, the therapist may also educate the client about realistic goals as well as limits of what can be achieved by this approach. Instead of defining abstract therapy goals, the ROTATE therapist asks clients to describe in detail what positive effects will occur if the therapy turns out to be successful. Thus clients should develop a positive and realistic vision of the changes they expect if therapy works well. Generally, the therapist is more focused on solutions than on how the problem has developed. Given the limited number of sessions available, the therapist will design a treatment plan and carefully select the most appropriate therapeutic procedure(s). For example, if intrusions are the main problem, the therapist may teach a client the container technique Psychodynamically informed treatment for trauma in the context of refugee crises 325 (see below). If low self-esteem is the main problem area, the therapist will strive for an understanding of the situations and relationships in which problems arise. Then the therapist will choose resource-activating techniques to enhance selfesteem. For example, the therapist may activate a positive memory of a (small) success or have the client practice the point of power technique (Wöller & Mattheß, 2016). If the client is afraid of a stressful situation in the near future, the therapist may activate memories of competencies and skills that were successfully used in former situations (see “Absorption technique” section). Talking about traumatic experiences: yes or no? The ROTATE therapist does not encourage traumatized clients to talk in detail about their traumatic experiences. It is the philosophy of ROTATE that talking about details of traumatic experiences is not therapeutic per se. On the contrary, doing so may worsen the client’s condition; an absence of prior stabilization and resource activation risks the client becoming overwhelmed by traumatic memories. Sometimes, however, traumatized clients express a deep wish to talk about their traumatic experiences. They urgently need someone to listen and witness what happened to them. The possibility of talking about traumatic experiences in a good and safe relationship can give them great relief and a feeling of being understood. If these clients do not suffer from intrusive symptoms such as flashbacks, the therapist can consider facilitating discussion about traumatic experiences within a safe framework, that is, with prior resource activation and for a limited period of time during the session. For example, the client might start with a resource-activating exercise, talk about his or her trauma for, say, 10 or 20 minutes, and close the session again with a resource-activating exercise. It is of utmost importance that the client leaves the session in a stable and resourceful emotional state. Psychoeducation Information about the presenting problem, its origin, and treatment options is an important element of ROTATE. Clients should be able to develop a basic understanding of the disorder to which their symptoms belong, be it PTSD, depression, dissociative disorder, somatoform disorder, or another trauma-related disorder. However, the extent to which explanations are given should be adapted to the client’s cultural and educational background. It is better to give small and simple bits of information that the client can digest than to overwhelm the client with a large quantity of information that he or she is unable to integrate. Flashback management: The container technique The container technique is a valuable tool for managing flashbacks (i.e., intrusive or disturbing memories). This exercise of guided imagery is appropriate for distancing from negative affect states and intense traumatic memories. It gives the client control over the traumatic material and is helpful for allowing the client to 326 Contemporary Psychodynamic Psychotherapy consciously dissociate, at least for a period of time (see Box 22.1 for a detailed verbatim example of this technique). The container technique can also be used if a traumatized client is flooded by undifferentiated negative trauma-related emotional states. Typically, these emotional states contain elements originating in the traumatic past and elements originating in the current situation. They are characterized by feelings of powerlessness, abandonment, and other strong negative emotions. The therapist helps the client to differentiate these affect states into components with respect to their origin in the past or in the present and to regulate the negative affect arising from the traumatic component. To this end, clients are educated to use imaginative techniques to separate those parts of the feeling belonging to the traumatic past from those belonging Box 22.1 Container technique G G G G G G Please imagine a container that can be locked. Look at it closely: What size?, . . . Material?, . . . Color?, . . . How to close the door?, . . . Noises?, . . . How to lock it?, . . . Which kind of lock(s)? If you look at your container: Is it absolutely safe? If not, change it until it is (check material, solid walls, strong locks, . . .). Put whatever you want to lock up into a box, take it to your container, open the door, and put it inside. Then close the door and decide where to leave the key. Then bring your container to a place where you can reach it when you wish to, but not too close by. If it is difficult to put the experiences into the container, it can help to materialize them. For example: G G G G G G G Affects (e.g., extreme fear or body sensations such as pain): Give it a form or shape and shrink it to a very small size until it fits into a box. Thoughts: Write it down on a paper with unreadable special ink, put it into an envelope, and put the envelope into the container. Pictures: Handle as a photo, maybe shrink it, let the color fade out, put another paper in front of it, and then put it into an envelope. Inner films: Handle as a video, if necessary use the remote control to take charge of color, sound, etc. Turn off the TV and take the videocassette to the container. Sounds: Handle as if on a CD or audiocassette, turn off the volume, fast rewind, and take it to the container. Smells: Pour them into a bottle, and close it. Taste: Give it form and color, shrink it, and store it in a glass. Check whether everything is gone. If there is something left, put it away into the container as you did before. The client locks traumatic material in and decides whether and when he or she wants to take “pieces” out to look at them. Psychodynamically informed treatment for trauma in the context of refugee crises 327 to the present. By using the container technique (see Box 22.1), clients are invited to “pack away” the parts that belong to the past (Wöller et al., 2012). Therapist: Try to imagine this feeling of rage as an object that you can see and grasp. Client: I’ll try. . . . Okay, I got it. Therapist: Now identify the part of the feeling that fits the real situation and the part of the feeling that fits the past. What percentage of the feeling fits the real situation? Client: About 20 percent. Therapist: Keep that 20 percent and put the remaining 80 percent into the “container.” Improving emotion regulation Traumatized clients tend to be flooded by severe negative emotions. Mostly, they suffer from undifferentiated emotional states that involve fear, rage, despair, shame, feelings of abandonment, and guilt. Normally, these emotions are triggered by daily life stimuli associated with an earlier traumatic experience. Therefore the main aim of ROTATE is to increase the client’s ability to master and modulate negative emotional states and extreme arousal. To improve emotion regulation, the therapist may choose several techniques: G G G Finding activities that help the client to get out of negative emotional states or transform them (e.g., listening to music, jogging or taking a walk, swimming, praying, singing, meeting friends). Not all activities will work for all clients; each client will have to find his or her own favorite activities. Encouraging the client to identify, remember, and vividly imagine memories of small successes or positive experiences or encounters. The therapist may follow these steps, repeating them as necessary: Ask the client to identify a positive memory during the past months or years. Invite the client to imagine a scene that represents this positive experience. The client should feel the pleasant emotion as well as pleasant bodily sensation connected with the positive memory. Using imagination exercises. Several aspects have to be kept in mind when working with imaginations: All imagination techniques need practice. At first, the ROTATE therapist will explain the technique to the client. Then, the therapist and client will practice it together. Finally, the client will practice the exercise alone. Clients should understand that it is normal to face difficulties when practicing imagination exercises for the first time. Therefore the therapist will encourage clients to report all occurring difficulties and help clients modify an imagination exercise until it feels comfortable. The therapist may take into account a client’s preference for specific imagination exercises. It is not necessary that each client master and practice all exercises the therapist is introducing. Rather, the client should identify one or two imagination exercises that she or he likes. 328 Contemporary Psychodynamic Psychotherapy Sometimes, clients’ cultural backgrounds necessitate modifications to imagination exercises. For example, in Cambodia some clients needed to draw their own safe place or inner garden to make them completely safe. They kept these drawings with them and looked at them when they felt uncomfortable or stressed. For the container technique, therapists sometimes had to bring a real container (small box) to show their clients before working on the exercise, or some clients chose other objects, such as a big wooden box. For the tree exercise (see Box 22.2), some therapy sessions were done near or under a real tree. In Rwanda, therapists reported that clients living in rural areas preferred putting negative material into a river rather than into a container; for them it was safer to see the material being swept away. Finally, while resource-activating techniques may be helpful, the ROTATE therapist should always bear in mind that techniques aimed at evoking positive emotions must not minimize or degrade a client’s suffering. Most clients with a history of complex trauma display problems with self-care and self-protection. A psychodynamically informed investigation of such problems typically reveals an internalized prohibition of self-care and self-protection resulting from childhood abusive relationships with key figures. The ROTATE therapist educates the client about the importance of self-care and self-protection in the sense Box 22.2 The tree exercise This is an exercise to create a resourceful state. G G G G G G G First of all, imagine a landscape where you feel comfortable and where you like to be. It may be a landscape you know and that exists, but it can also be imagined, existing only in your mind. In this landscape there is a tree that attracts you, and you approach it and get in touch with it. You can look at it, but you can also physically touch it. Maybe you like to imagine that you lean against it or embrace it. And then perceive the tree, its trunk, the structure and nature of its bark, its smell, how the trunk branches out, the leaves, etc. Take the time to perceive this tree exactly. Now try to find out what it means to the tree that it has roots that branch out in the earth and to be nurtured this way. And try to find out what it means to the tree to have leaves that can take in the sunlight and transform it. And then think about the question of how you yourself want to be nurtured now. What kind of nourishment would you like now for your body, for your emotions, for your mind, or for your spiritual being? Specify that as exactly as possible. Now you may imagine that you get this nourishment from the earth and from the sun. And imagine that what you got from the sun and from the earth unites with each other within you. And that you grow by that, physically, emotionally, mentally, or spiritually. Now step back from the tree and say goodbye. If you like, you can make plans to come back to your tree often. Perhaps you can promise to come back. You can also, if you like, thank your tree for supporting and helping you. Now please take the time you need to come back to this room with full awareness and notice the contact of your body to the ground. Psychodynamically informed treatment for trauma in the context of refugee crises 329 that these are necessary to improve self-regulation. The therapist might explain this in a simple way, for example, by saying that it is the inner voice of a traumatizing key figure that prevents the client from caring for himself or herself. At the same time, the therapeutic relationship itself may present the client with a model that counters these internalized prohibitions. Reorientation techniques to get out of dissociative states If a client is engulfed in a dissociative state, the therapist will use reorientation techniques to help the client out. Reorientation techniques are simple strategies that help clients come back to the here-and-now of the therapy room. To this end, the therapist asks the client to focus on the external world rather than the inner world that is full of overwhelming traumatic emotions. When a client has lost contact with external reality because of an acute dissociative state, the therapist actively helps the client out of this state by directing his or her attention toward external visual, acoustic, or bodily stimuli or toward rational thinking. If a client is in a dissociative state (i.e., if the client feels or behaves as if she or he were in a situation of the traumatic past), the therapist may follow these steps: 1. Stay calm, speak slowly, and use simple and very clear language. 2. Address the person and introduce oneself: “I am Mr./Ms. . . .. I am here to help you.” 3. Say very clearly, “You are safe here. This location here is . . .. We are in the year 20. . .. There is no danger now.” 4. Ask the client to divert his or her attention away from the inner experiences and direct it toward the outer reality. Say very clearly, “Open your eyes. Look at me. I am . . .. Look at . . . (e.g., that building). Do you know what it is? Look at that tree. Do you know what it is? Look at this person. Do you know who it is?” 5. Try to touch the person gently (and observe whether or not this helps, as sometimes touching causes fear). Never touch a client without having asked his or her permission before. It is best to discuss this briefly at the beginning of therapy. 6. Give the client an object, such as a pencil, and have the client touch and grasp it. 7. Ask the client to smell something, to walk around the room, to observe something, to feel his or her own body, to carry out a mental arithmetic operation, etc. (e.g., “While you feel the ground below your feet, you can look around in the room. Look at this room. How many red objects are there in this room?”). Absorption technique Absorption technique is an EMDR-based resource-activating technique that aims to strengthen specific coping skills (Hofmann, 2009). It is a modification of the EMDR protocol for RDI that was originally developed by Korn and Leeds (2002). To strengthen and generalize resources to cope with difficult and stressful situations in the present or in the future, the therapist asks the client which memory or skill would best help the client to cope with the situation. The therapist then uses short sets of four to eight bilateral eye movements (taps or tones) to enhance the client’s 330 Contemporary Psychodynamic Psychotherapy inner awareness and the intensity of activated positive emotions and coping resources. The therapist proceeds as follows: 1. The therapist asks the client to identify a stressor in the present or in the near future (e.g., an exam or a job interview). This technique can also be used to help the client face difficult memories and be able to talk about them afterwards. 2. The therapist asks the client to evaluate the stress level of this stressor on a scale ranging from 0 (no stress at all) to 10 (maximum stress). 3. To cope with this stressor, the therapist asks the client to identify the resources (capacities, competencies) needed to cope with it. The client should identify three resources that are not too similar (e.g., courage, calm, energy, self-esteem). 4. For this purpose the therapist encourages the client to search for situations in the client’s life history in which the client had access to these resources. The client should be asked to remember three resourceful scenes. 5. The therapist then asks the client to imagine one of the three resourceful scenes vividly. The client should feel the positive emotional state and the positive body feeling connected with the scenes. 6. To install the resource, the therapist anchors it with four to eight sets of slow bilateral stimulations. The therapist continues bilateral stimulations as long as the positive feeling is increasing. At the end, all three resources are imagined at the same time and anchored again with bilateral stimulation. 7. Finally, the therapist asks the client to evaluate the stress level of facing the original stressor again (0 5 no stress at all, 10 5 maximum stress). This procedure typically decreases the stress connected with the difficult life situation. Potential difficulties during therapy Psychodynamic techniques to handle difficult transference and countertransference phenomena have been well elaborated (Dalenberg, 2000; Gabbard, 1995). Considering aspects of transference and countertransference is necessary to establish a working alliance with complex trauma clients, even in short-term approaches such as ROTATE. Transference reactions Some difficulties can result from clients’ transferences to the therapist. Transference is a common phenomenon in which a person in treatment directs feelings for important figures in his or her former life onto the therapist (Freud, 1917). Transferences can become a problem in the treatment of traumatized clients. In the worst case they can disrupt the therapeutic relationship and hinder therapeutic progress. Psychodynamic theory distinguishes several types of transferences. In the treatment of traumatized clients, two of these deserve special attention: negative (perpetrator) transferences and overly positive or idealized (rescuer) transferences. Psychodynamically informed treatment for trauma in the context of refugee crises 331 A negative (perpetrator) transference directed toward the therapist means that the client consciously or unconsciously projects negative feelings from earlier traumatizing key figures onto the therapist; for example, the client may be afraid of being hurt, humiliated, or rejected by the therapist. Negative transference phenomena typically occur when a client gets triggered by a certain therapist behavior or by certain circumstances of the therapeutic situation that remind the client of past traumatic experiences. Such a negative transference may result in a negative attitude toward the therapy and can make cooperation impossible. One typical consequence of a negative transference toward the therapist is that the client does not talk about shame issues or failures because she or he consciously or unconsciously expects criticism or humiliation from the therapist. An overly positive (idealized, rescuer) transference means that the client adopts an idealizing view of the therapist and projects onto the therapist wishes to be healed and rescued by him or her. The client perceives the therapist as an omnipotent rescuer and expects to be completely healed or rescued by the therapist without contributing to the process of therapy. In a similar manner the client expects that the therapist will have a solution for all of the client’s problems. This passive stance will not only disrupt cooperation, but also result in severe disappointment over the therapist’s inevitable failure to satisfy expectations. To deal with such problems, the therapist should carefully and gently check for transference reactions that prevent the client’s feeling of safety and cooperation in therapy. Likewise, the therapist should carefully monitor subtle disruptions of the therapeutic alliance as a result of transference phenomena. Not infrequently, repairing alliance deficits can provide an opportunity for strengthening the alliance (Muran et al., 2009). Clarifying transference reactions includes educating the patient about the reality of the therapeutic situation. Countertransference and therapist’s self-care Countertransference refers to the totality of the therapist’s reactions toward the client (Heimann, 1950). While this includes the therapist’s reactions to the client’s transference in therapy, there are several other sources of countertransference. One important source of countertransference reactions is the therapist’s own trauma history. A client’s disclosure of his or her traumatic experiences can evoke emotions such as compassion and sadness in the therapist. When the therapist recognizes familiar aspects of the client’s trauma story that may be related to the therapist’s experience, overidentification with the client may be a problem. At worst this may lead to professional burnout or secondary traumatization of the therapist. Another countertransference reaction that is difficult to deal with is rage toward the client’s perpetrator. Intensive rage can distract the therapist from the treatment process and lead to overidentification with the client. The therapist may have difficulty keeping a professional stance, thus hindering his or her capacity to think rationally. Some countertransference reactions toward a client can be understood as a result of defense mechanisms to counterbalance negative emotions when listening to the client’s trauma stories. Some therapists unconsciously use distancing strategies by 332 Contemporary Psychodynamic Psychotherapy developing a disconnection from the emotional aspects of the client’s traumatic event description. Others minimize the dimension of the client’s traumatic experience and convince themselves that the client is exaggerating in what he or she says. Although understandable, these defense mechanisms can disrupt or damage the therapeutic relationship with the client. The ROTATE therapist should be aware of his or her own countertransference reactions toward the client in order to provide a secure emotional presence and reliable therapeutic boundaries. Conclusion This chapter provided a practical introduction to a resource-oriented form of psychotherapy that is based on psychodynamic principles. Comprising only about five sessions, ROTATE is a short form of therapy that is suitable for a wide range of clients suffering from trauma-related disorders. Importantly, rather than trauma confrontation, ROTATE focuses on establishing a secure therapeutic relationship and strengthening resilience and coping capacities by activating positive personal resources. References Acarturk, C., Konuk, E., Cetinkaya, M., Senay, I., Sijbrandij, M., Gulen, B., . . . Cuijpers, P. (2016). The efficacy of eye movement desensitization and reprocessing for posttraumatic stress disorder and depression among Syrian refugees: Results of a randomized controlled trial. Psychological Medicine, 46, 2583 2593. Bellak, L., Hurvich, M., & Gediman, H. K. (1973). Ego functions in schizophrenics, neurotics, and normals: A systematic study of conceptual, diagnostic, and therapeutic aspects. New York: Wiley. Bisson, J., & Andrew, M. (2007). Psychological treatment of post-traumatic stress disorder (PTSD). Cochrane Database of Systematic Reviews, 18(3), CD003388. Bumke, P. J., & Sodemann, U. (2010). The efficacy of EMDR in a new context: Some findings from the ACEH survey. Paper presented at the 1st EMDR Asia conference, Bali, Indonesia. Retrieved from ,http://emdria.omeka.net/items/show/20301. (Accessed 02.07.15). Dalenberg, C. J. (2000). Countertransference and the treatment of trauma. Washington, DC: American Psychological Association. Ertl, V., Pfeiffer, A., Schauer, E., Elbert, T., & Neuner, F. (2011). Community-implemented trauma therapy for former child soldiers in Northern Uganda: A randomized controlled trial. JAMA, 306, 503 512. Ferenczi, S. (1949). Confusion of the tongues between the adults and the child (the language of tenderness and of passion). The International Journal of Psycho-Analysis, 30, 225 230. Folkman, S., & Moskowitz, J. T. (2000). Positive affect and the other side of coping. American Psychologist, 55, 647 654. Psychodynamically informed treatment for trauma in the context of refugee crises 333 Freud, S. (1917). Introductory lectures on psychoanalysis. The standard edition of the complete psychological works of Sigmund Freud. London: Hogarth. Gabbard, G. O. (1995). Countertransference: The emerging common ground. International Jounal of Psychoanalysis, 76, 475 485. Heimann, P. (1950). On countertransference. International Journal of Psychoanalysis, 31, 81 84. Hofmann, A. (2009). The absorption technique. In M. Luber (Ed.), Eye movement desensitization and reprocessing (EMDR). Scripted protocols (pp. 275 280). Horowitz, M. J. (1973). Phase oriented treatment of stress response syndromes. American Journal of Psychotherapy, 27, 506 515. Kernberg, O. F. (1976). Object-relations theory and clinical psychoanalysis. New York: Aronson. Kessler, R. C., Sonnega, A., Bromet, E., Hughes, M., & Nelson, C. B. (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52, 1048 1060. Korn, D. L., & Leeds, A. M. (2002). Preliminary evidence of efficacy for EMDR resource development and installation in the stabilization phase of treatment of complex posttraumatic stress disorder. Journal of Clinical Psychology, 58, 1465 1487. Kruse, J., Joksimovic, L., Cavka, M., Wöller, W., & Schmitz, N. (2009). Effects of traumafocused psychotherapy upon war refugees. Journal of Traumatic Stress, 22, 585 592. Lampe, A., Hofmann, P., Gast, U., Reddemann, L., & Schussler, G. (2014). Long-term course in female survivors of childhood abuse after psychodynamically oriented, trauma-specific inpatient treatment: A naturalistic two-year follow-up. Zeitschrift fur Psychosomatische Medizin und Psychotherapie, 60, 267 282. Luborsky, L. (1984). Principles of psychoanalytic psychotherapy. Manual for supportiveexpressive treatment. New York: Basic Books. Markowitz, J. C., Petkova, E., Neria, Y., Van Meter, P. E., Zhao, Y., Hembree, E., . . . Marshall, R. D. (2015). Is exposure necessary? A randomized clinical trial of interpersonal psychotherapy for PTSD. American Journal of Psychiatry, 172, 430 440. Mattheß, H., & Sodemann, U. (2014). Trauma-aid, humanitarian assistance program Germany. Journal of EMDR Practice and Research, 8, 225 232. Muran, J. C., Safran, J. D., Gorman, B. S., Samstag, L. W., Eubanks-Carter, C., & Winston, A. (2009). The relationship of early alliance ruptures and their resolution to process and outcome in three time-limited psychotherapies for personality disorders. Psychotherapy (Chic), 46, 233 248. Neuner, F., Onyut, P. L., Ertl, V., Odenwald, M., Schauer, E., & Elbert, T. (2008). Treatment of posttraumatic stress disorder by trained lay counselors in an African refugee settlement: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 76, 686 694. Nickerson, A., Bryant, R. A., Silove, D., & Steel, Z. (2011). A critical review of psychological treatments of posttraumatic stress disorder in refugees. Clinical Psychology Review, 31, 399 417. Reddemann, L. (2012). Psychodynamic imaginative trauma therapy PITT Manual. Stuttgart: Klett-Cotta. Rudolf, G. (2013). Structural psychotherapy. Stuttgart: Schattauer. Sachsse, U., Vogel, C., & Leichsenring, F. (2006). Results of psychodynamically oriented trauma-focused inpatient treatment for women with complex posttraumatic stress disorder (PTSD) and borderline personality disorder (BPD). Bulletin of the Menninger Clinic, 70, 125 144. 334 Contemporary Psychodynamic Psychotherapy Shapiro, F. (2001). Eye movement desensitization and reprocessing (EMDR): Basic principles, protocols and procedures (2nd ed.). New York, NY: The Guilford Press. Silove, D., Ventevogel, P., & Rees, S. (2017). The contemporary refugee crisis: An overview of mental health challenges. World Psychiatry, 16, 130 139. Steel, Z., Chey, T., Silove, D., Marnane, C., Bryant, R. A., & Van Ommeren, M. (2009). Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement. JAMA, 302, 537 549. United Nations Refugee Agency. (2016). Global trends report: World at war. Geneva: United Nations High Commissioner for Refugees. Wallerstein, R. (1989). The psychotherapy research project of the Menninger Foundation: An overview. Journal of Consulting and Clinical Psychology, 57, 195 205. Wöller, W. (2016). Trauma-informed peer counselling in the care of refugees with traumarelated disorders. Psychotherapie, Psychosomatik, Medizinische Psychologie, 66, 349 355. Wöller, W., Leichsenring, F., Leweke, F., & Kruse, J. (2012). Psychodynamic psychotherapy for posttraumatic stress disorder related to childhood abuse Principles for a treatment manual. Bulletin of the Menninger Clinic, 76, 69 93. Wöller, W., & Mattheß, H. (2016). Resource-oriented trauma therapy and resource installation with EMDR. Treatment Manual. Retrieved from ,http://www.rhein-klinik.de/fileadmin/ content/rhein/Publikationen/2016_07_05_Woeller___Matthess_2016_ROTATE_ Manual_Version_1.0.pdf.. Internet-based psychodynamic psychotherapy 23 Robert Johansson1,2 1 Department of Psychology, Stockholm University, Stockholm, Sweden, 2Department of Behavioural Sciences and Learning, Linköping University, Linköping, Sweden Introduction This chapter will describe a recent innovation in the field of psychodynamic treatments. While the use of technology and the Internet within the mental health field is not new, only recently has any empirical research been conducted on this topic in relation to psychodynamic therapy. Importantly, this chapter is not about conducting traditional psychodynamic or psychoanalytic therapy via Internet-based video services. Rather, it is about internet interventions in the form of guided self-help. One definition of such interventions is the following: “a therapy that is based on self-help books, guided by an identified therapist who gives feedback and answers to questions, with a scheduling that mirrors face to face treatment” (Andersson et al., 2008, p. 164). Other definitions exist, but in general, internet-based psychotherapy in its most common form can be said to consist of a manualized form of psychotherapy, translated to self-help text, that is delivered via the internet in a module-based format with additional therapist support, commonly in a format similar to e-mail (Andersson, 2016). While well over 100 randomized controlled trials (RCTs) exist that have tested the efficacy of CBT in this format (ICBT), only recently have psychodynamic interventions been tested as guided self-help via the internet (Johansson, Frederick, & Andersson, 2013). This chapter will focus on work from four RCTs carried out at Linköping University, Sweden. These studies investigated two distinct models of internetbased psychodynamic therapy in the form of guided self-help. The first model, based on a psychoanalytic treatment translated to self-help, is SUBGAP, which stands for (1) Seeing unconscious patterns that contribute to emotional difficulties, (2) Understanding these patterns, (3) Breaking such unhelpful patterns, and (4) Guarding Against Patterns and/or relapses in the future (Silverberg, 2005). The second model, an internet-based form of experiential dynamic therapy (EDT) (Lilliengren, Johansson, Lindqvist, Mechler, & Andersson, 2016), is EDT-I, which is based on “Living like you mean it” by Frederick (2009). This chapter will focus on describing these two models in detail. In addition to the work conducted by the Contemporary Psychodynamic Psychotherapy. DOI: https://doi.org/10.1016/B978-0-12-813373-6.00023-4 © 2019 Elsevier Inc. All rights reserved. 338 Contemporary Psychodynamic Psychotherapy Swedish group, there exist preliminary data from a small pilot trial of an online group model of Dynamic Interpersonal Therapy (Lemma & Fonagy, 2013; Lemma, Target, & Fonagy, 2011). Finally, a German research group has recently presented new data on the efficacy of internet-based psychodynamic treatment provided after inpatient care (Zwerenz, Becker, Johansson, et al., 2017) and to support return to work (Zwerenz, Becker, Gerzymisch, et al., 2017). Description of treatment models/approaches Treatment environment and therapist support Communication, including modules, e-mails, and measurements, takes place in a highly secure online environment. Self-help modules are text-based with additional illustrations. A typical module is about 20 pages long. It is possible for the patient to download these modules to his or her own computer in PDF format. Furthermore, the therapist and patient keep in contact in a text-based medium similar to e-mail. Patients are informed that contact with the therapist will primarily be a once-weekly message concerning the patient’s reporting of the past week’s treatment-related work. However, patients are also invited to contact the therapist as needed, with the possibility of receiving shorter answers within 24 hours during weekdays. No chat, video call, or any other “live” communication is used. A majority of the correspondence in guided self-help treatments tends to be in the form of encouragement and support. It typically consists of short text messages sent about once a week, which means that the therapist may spend about 10 15 minutes per client each week (for example, in a 10-week treatment program). In internet-based psychodynamic therapy these messages could be anything from praise (e.g., “Good work!”) to the therapist’s summaries of the patient’s work (e.g., “With interest I read that over the past week you worked with the exercise ‘Awareness of defenses.’ You realized that intellectualization was one of your major defenses, and now you’re concerned that this has kept you at a distance from other people.”). Sporadically, therapist communication could include more challenging interventions, primarily concerning boundaries of the treatment (e.g., “If you keep postponing this work, then the consequences will be that I will be unable to help you, as we part ways in a couple of weeks.”). Importantly, there is an assumption that the core working mechanisms in internet-based therapy are in the self-help material and not necessarily in the contact with the therapist. Hence the primary goal of the minimal therapist contact is to strengthen compliance with the treatment protocol through praise and reinforcement; providing insights and interpretations is only a secondary goal. Transference work in guided self-help psychotherapy is a possibility. Therapists have not been prohibited from such work, but it has not been part of existing protocols. A further discussion of the role of the therapist in internet-based psychodynamic therapy is available elsewhere (Johansson, Frederick, et al., 2013). Internet-based psychodynamic psychotherapy 339 SUBGAP The SUBGAP model was introduced by Farrell Silverberg in the book “Make the Leap” (Silverberg, 2005). This book aims to translate psychoanalytic thinking into self-help format. For the purpose of the studies conducted, the book was translated into Swedish and adapted to the guided self-help format. In the self-help manual the reader is guided through nine treatment modules: (1) introduction to the treatment in general and to the SUBGAP method in particular, (2) systematic practice in discovering one’s own unconscious patterns, (3) understanding patterns from a historical perspective as well as a here-and-now perspective, (4) different methods that can be used to break the patterns that one discovers, (5) minimizing the risk of falling back into one’s formerly unproductive patterns, (6) applying the knowledge one gains about patterns with a focus on solving the dilemmas of working life, (7) applying knowledge about patterns with a focus on improving personal relationships, (8) the relationship between unconscious patterns and clinical symptoms, and (9) a summary of the treatment and guidelines for the future. The main adaptations to the text were in the eighth module, which was a completely new module and differed between trials that addressed generalized anxiety disorder (GAD) or depression. For example, in the trial for depression the module provided several examples of unconscious patterns that were specific to the lives of depressed individuals. These examples included unresolved grief, guilt about feelings of anger toward close people, and a constant feeling of not being seen by other people. In total, the treatment consisted of about 160 pages of text. SUBGAP has a strong focus on gaining a psychodynamic understanding of how problems in life, including symptoms of depression and anxiety, are related to underlying unconscious patterns. We can see similarities between such an insight-oriented approach and Luborsky’s supportive expressive (S E) therapy (Luborsky, 1984). However, the processes involved in carrying out the two different therapies are fundamentally different. The SUBGAP method is based on self-help material with additional text-based therapist support, while the S E method relies on the therapist’s active involvement. The S E method is heavily dependent on the therapist’s in-session interpretations of the subject and relies on the transference relationship that happens in therapy as one focus for interpretation (Luborsky, 1984). Importantly, though, there are examples of both supportive and expressive elements in SUBGAP. Supportive elements in the text include creating positive expectancies, patient engagement, and hope. The following passage from the first module illustrates this: “[By taking part in this material] you can learn how to uncover the moments of opportunity and weed out the traps. You can learn a method that shows you what to do to live a more successful and fulfilled life. You may want to learn this system to improve your entire life, or possibly you will want to learn it to improve one particularly clouded area of your life in which you feel your potential is not being met” (Silverberg, 2005, p. 8). Expressive elements in the text are mainly in the form of case examples; throughout the treatment, various case stories and interpretations explaining the consequences of patients’ life patterns are presented. The ultimate aim of 340 Contemporary Psychodynamic Psychotherapy these case stories is to enhance patients’ self-understanding by reading about people’s experiences in which they may recognize themselves. Also, the questions at the end of the chapter invite further self-understanding. In a way, these questions can be said to invite expressive interventions in self-help format. This invitation can be illustrated by the questions presented at the end of module 7: “Based on what you have read in this module, what patterns can you see that happen for you in close relationships?” and “How are the relationships affected by such patterns?” In summary, the SUBGAP treatment contains both supportive and expressive elements, both in the text and in the therapeutic relationship. While the treatment may seem similar to SE therapy in its underlying principles, the SUBGAP was not explicitly designed to mimic SE therapy. However, SUBGAP may serve as a potential foundation for an internet-based SE therapy model. EDT-I The EDT-I model that is described in this chapter is based on a subgroup of shortterm dynamic therapies known as Experiential Dynamic Therapy (Lilliengren et al., 2016) and based on the idea that psychodynamic conflicts may be conceptualized as affect phobias (Frederick, 2009; Julien & O’Connor, 2017; McCullough et al., 2003). This conceptualization builds upon the so-called triangle of conflict and triangle of persons schemas (Malan, 1995). The triangle of conflict is a model of the dynamics between underlying adaptive affects, the inhibitory affects they may evoke, and the defenses used to avoid, prevent, or diminish the tension between conflicting affective states. The triangle of persons illustrates how such avoidance patterns are typically developed in earlier relationships, are evoked and maintained in current relationships, and may be enacted with a therapist. Affect phobias are assumed to underlie a number of clinical problems and psychiatric disorders (McCullough et al., 2003). For example, from this perspective, excessive worrying (as in GAD) may be understood as a defensive reaction to emotional experiences. Furthermore, social anxiety disorder may be understood as a consequence of learned secondary anxiety and/or shame reactions triggered by underlying emotions arising in relationships. The experiential dynamic therapies can be said to descend from the work by Alexander and French (1946), who were among the first to attempt to shorten psychoanalytic therapy and increase its efficacy. Alexander and French (1946) regarded the experience of warded off affect a major therapeutic factor. By focusing on affect, Alexander and French were moving the therapeutic task from interpretation on a cognitive level to actively promoting expression and experience of buried feelings within the therapeutic relationship (Osimo & Stein, 2012). This intensive experiencing of previously buried feelings in a new setting was called the corrective emotional experience (Alexander & French, 1946) and has been assumed to be fundamental for therapeutic change in EDT (Alexander & French, 1946). Internet-based psychodynamic psychotherapy 341 In the EDT-I protocol, patients are helped to conceptualize their problems in terms of internal affect phobias, identify underlying adaptive affects, become aware of defensive behaviors, and work toward resolution of the internal conflicts in current interpersonal contexts. Experiencing and expressing warded-off affects are assumed to be a central factor in therapy. In later revisions of the model, work on self-compassion was also included. The book “Living Like You Mean It” by Frederick (2009) was the principal source for the self-help material used to develop the EDT-I model. Frederick’s book was translated into Swedish and adapted for the internet format. The main additions to the material in the book were the homework activities and the structuring of the exercises already contained in the book. Fundamental for the EDT-I model is the overarching concept of “emotional mindfulness” (Frederick, 2009). This involves teaching participants to mindfully pay attention to emotional experience through various insight-oriented and skillsbuilding exercises. The material guides the client through understanding the relationships between feelings, anxiety, and defenses (the triangle of conflict) as well as the developmental theory of affect phobias (the triangle of persons). Throughout treatment, participants are taught to mindfully approach their feelings, notice and relinquish their defenses, and regulate their anxiety. The themes of the nine modules are as follows: (1) introduction to the affect phobia-model, (2) understanding the causes of affect phobias, (3) reducing shame and increasing self-compassion, (4) identification and acceptance of feelings through practicing emotional mindfulness, (5) recognizing and restructuring defenses, (6) anxiety regulation, (7) deepening of emotional experience, (8) affect expression and restructuring image of self, and (9) treatment summary, evaluation of progress, and advice for the future. In total, the self-help material consists of about 250 pages. Similar to EDT in general, the EDT-I model uses several means to approach emotional experiences, regulate anxiety, and address defenses. The treatment also aims to increase self-understanding, which is done very much on an emotional level with the aim of helping the patient have corrective emotional experiences. In the trials that were conducted, the therapeutic relationship was mostly supportive, and use of the transference was not standard procedure. Importantly, affect phobia treatment views transference work as a possibility but not a necessity (McCullough et al., 2003). While EDT-I is similar to affect phobia treatment, it differs from that model mainly in that it makes ample use of self-help techniques instead of expressive work by the therapist. The goal of experiential dynamic therapies is to facilitate self-understanding on an emotional level. This aim follows the work by Alexander and French (1946) on the corrective emotional experience: insight acquired at an emotional level via new emotional experiences. This is often described as something happening within the therapeutic relationship. Importantly, corrective emotional experiences were described by Alexander and French (1946) as also happening outside of the therapeutic relationship: “Reexperiencing the old, unsettled conflict but with a new ending is the secret of every penetrating therapeutic result. Only the actual experience of a new solution in the transference situation or in his everyday life gives the 342 Contemporary Psychodynamic Psychotherapy patient the conviction that a new solution is possible and induces him to give up the old neurotic patterns” (p. 338, emphasis added). Furthermore, “In this connection it is important to remember that the patient’s new emotional experiences are not confined to the therapeutic situation; outside the treatment he has emotional experiences which profoundly influence him” (p. 339). Although the therapeutic relationship in guided EDT-I tends to be more supportive, there is no reason to believe that corrective emotional experiences do not occur. Moreover, through emotional mindfulness and defense work, EDT-I guides the patient toward the possibility of corrective emotional experiences in the patient’s everyday life. Future research should clarify whether there are any differences in mechanisms of change between EDT-I and other forms of EDT. Presentation of supporting evidence In this section the evidence base supporting internet-based psychodynamic therapy is summarized, and results are described from two trials that were based on SUBGAP and two trials that were based on the EDT-I model. SUBGAP The internet, health, and clinical psychology research group at Linköping University led by professor Gerhard Andersson has conducted two RCTs testing the efficacy of SUBGAP: one for GAD and one for depression. As was mentioned above, both were based on the book Make the Leap (Silverberg, 2005), but they were adapted with examples and material to fit GAD and depression, respectively. The GAD trial, published in 2012 by Andersson et al. (2012), compared an internet-based psychodynamic therapy protocol based on SUBGAP (IPDT) to an established internet-based cognitive behavior therapy protocol for GAD (ICBT). Both treatments involved weekly therapist contact. A waiting list condition was also included as a control. All three groups (27 participants in each group) had substantial symptom reductions on the primary outcome measure (Penn State Worry Questionnaire) after treatment, with no significant differences between groups. However, at a 3-month follow-up, there was a significant effect of both the IPDT protocol (d 5 0.64) and the ICBT protocol (d 5 0.76) compared to the control. Treatment gains were maintained at 18-month follow-up. Also published in 2012, Johansson et al. tested the efficacy of a 10-week SUBGAP treatment specifically adapted for depression. The treatment was compared to a supportive treatment with psychoeducation about depression (i.e., a highly active control condition
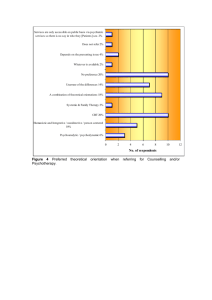
![UW2 - Psychiatric Treatments [2014]](http://s3.studylib.net/store/data/006859622_1-db6167287f6c6867e59a56494e37a7e7-300x300.png)