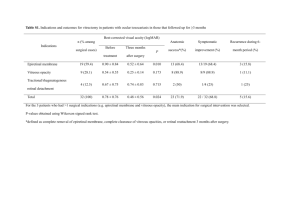
Vitreous Detachment Maitra-MedTech, IISc, Bangalore VITREOUS DETACHMENT What is vitreous Detachment? Vitreous detachment is a condition of the eye in which the vitreous (a gel-like substance) separates from the retina. The vitreous is the gel-like fluid that fills your eye. It’s full of tiny fibres that attach to your retina (the light-sensitive layer of tissue at the back of the eye). As you get older, the fibres of your vitreous pull away from the retina. This is called vitreous detachment. Fig:1.1 Vitreous Detachment What are the causes of vitreous detachment? The eyeball is filled with vitreous gel. This gel is made mostly of water and a protein called collagen. As you age, the gel becomes more liquid and the attachment of the back surface of the gel to the retina dissolves, leading to the gel separating from the retina. 1 Vitreous Detachment Maitra-MedTech, IISc, Bangalore What are the symptoms of vitreous detachment? The symptoms of vitreous detachment are: • Floaters: People say they look like bugs, cobwebs, hairs or dust floating in the field of vision. They’re sometimes shaped like a circle or oval, called a Weiss ring. • Flashes of light: People with PVD report seeing streaks of light, usually at the side of their vision. Flashes may be more noticeable when you’re in darker environments. Epidemiology of vitreous detachment. The statistics on the prevalence of posterior vitreous detachment are largely lacking. The data collected from hospital-based and postmortem studies suggest age is an important factor for the development of posterior vitreous detachment. Risk Factors of vitreous detachment? • Old age: The incidence of posterior vitreous detachment after 50 years of age is 53%, and between ages 66 to 86 years is 66%. Postmortem studies revealed that PVD was present in 27% of eyes by the seventh decade and 63% of the eyes by the eighth decade of life. • Female gender: The progression of a posterior vitreous detachment is faster in women than in men at age 60 or more. This implies that the macular pathologies linked with posterior vitreous detachment occur at a younger age in females. • Myopia: The incidence of posterior vitreous detachment depends on the axial length of the eyeball. The eyes with axial length more than 30 mm have a greater chance of developing posterior vitreous detachment than eyes with axial length less than 29 mm. • Underlying diseases like retinitis pigmentosa and sticklers syndrome. • Menopause: Post-menopausal female patients may be more prone to develop posterior vitreous detachment because of a lack of Estrogen. Estrogen may have a protective effect against PVD in premenopausal females. • Vitamin B6: Vitamin B6 has an anti-oestrogen effect. A higher intake of vitamin B6 may increase the incidence of posterior vitreous detachment in females. • Inflammation: Long-standing inflammation involves cellular proliferation and, eventually, fibrosis. Fibrosis of the vitreous cause traction over the retina resulting in posterior vitreous detachments or retinal breaks • Trauma: Posterior vitreous detachment occurs as a consequence of penetrating injury to the eye. It was noted as separation at the level of the internal limiting membrane or as a cleavage within the vitreous in a study. 2 Vitreous Detachment Maitra-MedTech, IISc, Bangalore • Ocular surgery: Various vitreous modifications occur during ocular surgeries, including cataract extraction and intraocular lens placement, LASIK (laser in situ keratomileusis), and others. These modifications may be involved in the development of postoperative posterior vitreous detachment. • Retinal lase. • Retinal cryo • The vitreous gel contains various angiogenic factors. These factors are responsible for neovascularization by endothelial cell proliferation. The posterior hyaloid face acts as a scaffold for the growth of the retinal or optic disc new vessels. So, the presence of a complete PVD may prevent the process of neovascularization and protects the eye from the progression of proliferative diabetic retinopathy. What is the diagnostic method for vitreous detachment? An eye doctor can diagnose PVD as part of a dilated eye exam. This exam the doctor puts Eye drops into a person’s eyes to widen or dilate the pupils. Then, the doctor will examine the eye for PVD and other eye issues. A dilated eye exam is typically painless but may be uncomfortable if the doctor presses on the eyelids to check for tears in the retina. What is the treatment for vitreous detachment? Acute symptomatic posterior vitreous detachment without vitreous hemorrhage and peripheral retinal breaks should be followed up at 2-4 weeks for precise peripheral retinal examination with scleral indentation. A patient complaining of floaters is conservatively managed. Patients are reassured that adaptation will develop to the visual symptoms overtime, or the floaters may resolve. However, in many cases, floaters may persist beyond six months to one year. The vitreous haemorrhage associated with acute PVD is usually mild, with a blob of haemorrhage just in front of the posterior pole. There may be intraretinal haemorrhage near the optic disc. Usually, a circular circumferential attachment of the vitreous to the retina is noted around the equator with some preretinal bleed settled inferiorly just behind the posterior vitreous face. Most associated breaks lie in the superior retina. In case of vitreous haemorrhage precluding the complete examination, the patient is advised a propped up position, bed rest, and bilateral eye patching is an option in such cases. 3 Vitreous Detachment Maitra-MedTech, IISc, Bangalore In cases with highly symptomatic floaters that are clinically significant and persistent and impact the quality of life, the interventional options are as follows. • Vitrectomy • Nd YAG Laser Vitriolises. • Vitriolises by Drugs • Laser Retinopexy • Cryo-retinopexy Can I be normal by having retinal detachment? People with PVD can usually go about their normal activities with no restrictions. Although the condition doesn’t go away, floaters and flashes become less noticeable over time. It’s common to develop PVD in the other eye in the next year or two after your first diagnosis. If you experience symptoms in the other eye, a repeat exam is needed to be sure there isn’t a retinal tear or detachment in your second eye. Most people don’t develop complications such as a retinal tear. But you should have an eye exam to make sure you don’t have a more serious condition. 4 Vitreous Detachment Maitra-MedTech, IISc, Bangalore BIBILOGRAPHY 1. Posterior Vitreous Detachment (PVD): What Is It, Symptoms & Treatments (clevelandclinic.org) 2. Vitreous Detachment | National Eye Institute (nih.gov) 3. Vitreous detachment: What it is, causes, and risk factors (medicalnewstoday.com) 4. epidemology of vitreius detachment - Search (bing.com) 5. Posterior Vitreous Detachment - StatPearls - NCBI Bookshelf (nih.gov) 6. Vitreous detachment: What it is, causes, and risk factors (medicalnewstoday.com) 5