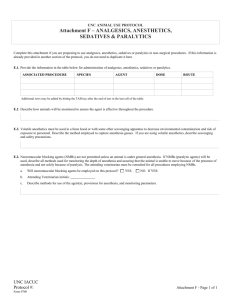
ANESTHETICS By Dr. Faraza Javaid Local Anesthetics Drugs used to provide local anesthesia are also used to achieve regional anesthesia. Regional anesthesia is an injection of a local anesthetics around nerves so that the area supplied by these nerves will not send pain signals to the brain. They anesthetized area is usually larger than the area affected by local anesthesia. Mechanism of action ▶ Mechanisms: Nonionized form crosses axonal membrane - From within, ionized form blocks the inactivated Na+ - channel Slows recovery and prevents propagation of action potentials When local anesthetics are applied to the area that they numb, they need to get to the axon by crossing to the membrane. Only non ionized forms R-NH2 can enter the axon through the membrane. Upon entering the axon, only the ionized forms can block the sodium channels which causes depolarization of the sodium channel consequently numbing the area. Ionized form RNH3+ Classification of Local Anesthetics based on chemical group ▶- Esters: Procaine, Cocaine, Benzocaine are metabolized by plasma and tissue esterases ▶- Amides: Lidocaine, Bupivacaine, Mepivacaine are metabolized by liver amides May also be classified into a. b. c. Short acting – Cocaine, Procaine Intermediate acting – Lidocaine, Mepivacaine, Dibucaine, Prilocaine Long acting – Tetracaine, Bupivacaine, Etidocaine Metabolism ▶Esters are metabolized by the plasma by enzymes CHOLINEesterase ▶Amides are metabolized by liver by the enzyme hepatic amidases ALLERGIC REACTIONS Patient reports of allergic reactions to local anesthetics are fairly common True allergy to an amide local anesthetic is exceedingly rare, while the ester procaine is more allergenic and has largely been removed from the market. Allergy to one ester rules out use of another ester, because the allergenic component is the metabolite paraaminobenzoic acid, produced by all esters. A patient may be allergic to other compounds in the local anesthetic, such as preservatives in multidose vials. Local anesthetic systemic toxicity (LAST) The signs, symptoms, and timing of local anesthetic systemic toxicity (LAST) are unpredictable. One must consider the diagnosis in any patient with altered mental status, seizures, or cardiovascular instability following injection of local anesthetic. Treatment for LAST may include seizure suppression, airway management, and cardiopulmonary support. Clinical note Don’t give amides to patients with poor liver function. Eg. patient with any form of hepatitis! WHY? The amides will pile up due inability of the liver to metabolize. Hence elicit a complete history in your patient. In cases where patients have liver problem; your local anesthesia should be an ester. ▶ How do we know which cocaine derivative is an amides or ester? ▶The trick: the letter i ▶ in almost all cases if an i precedes the “caine” sound, the drug is an amide but if not, it is an ester. Amides Esters ▶ Articaine ▶ Butacaine ▶ Bupivacaine ▶ Cocaine ▶ Dibucaine ▶ Ethyl ▶ Etidocaine ▶ Lidocaine ▶ Mepivacaine ▶ Prilocaine ▶Roppivacaine aminobenzoate (benzocaine) ▶ Hexylcaine ▶ Tertracaine ▶ Cloroprocaine ▶ Procaine ▶ propoxycaine Limiting local anesthetics ▶ All local anesthetics should be co-administered with alpha-1 agonist. E.g. phenylephrine, metoximine. WHY? Reason; The alpha-1 agonist will cause a powerful vasoconstriction and limit the access of surrounding tissues to the local anesthetics. The Cocaine saga ▶I am the only local anesthetics that does not need an alpha-1 agonist. WHY? ▶ANS: I am a NEP re-uptake blocker. NOTE: it causes NEP build up in the synapsis. From the synapsis NEP binds to the alpha-1 receptors and causes vasoconstriction in the surrounding tissues. Therefore you don’t need an alpha-1 agonist after administration of cocaine. Anesthetic Adjuncts Adjuncts are a critical part of the practice of anesthesia and include drugs that affect gastrointestinal (GI) motility, PONV, anxiety, and analgesia. Adjuncts are used in collaboration to help make the anesthetic experience safe and pleasant. Thank you Any question?