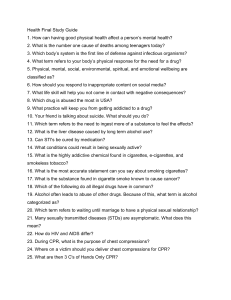
Chapter 9: Professional Rescuer CPR Chapter 9 Professional Rescuer CPR Professional Rescuer CPR • To maintain breathing and heartbeat, perform rescue breathing and chest compressions together. • 70% of cardiac arrest patients are in V-fib. – Heart muscle is quivering. – Not effectively pumping blood – AEDs can help these patients. Circulatory System • Consists of heart, blood vessels, blood • Heart pumps blood to lungs and rest of body. • Pulse is generated when heart contracts. Major Arteries • Neck or carotid pulse • Wrist or radial pulse (1 of 2) Major Arteries • Arm or brachial pulse • Groin or femoral pulse (2 of 2) Cardiac Arrest • Occurs when the heart stops contracting • No blood is pumped through the blood vessels. • Brain damage begins within 4 to 6 minutes after cardiac arrest. (1 of 2) Cardiac Arrest • May be caused by: – Heart attack or stroke – Untreated respiratory arrest – Medical emergencies (eg, electrical shock, epilepsy, poisoning) – Drowning – Suffocation – Trauma or shock from massive blood loss (2 of 2) Components of CPR • Requires three types of skills, (CAB method): – Circulation (Compression) – Airway – Breathing • CPR can keep patients alive until more advanced care is administered. Cardiac Chain of Survival • Early recognition of cardiac arrest and activation of 101 system • Early bystander CPR • Early defibrillation • Early advanced care • Integrated post– cardiac arrest care When to Start CPR • CPR should be started on all nonbreathing, pulseless patients, except when reliable signs of death exist: – Decapitation – Rigor mortis – Tissue decomposition – Dependent lividity When to Stop CPR • Effective spontaneous circulation and ventilation are restored. • Care is transferred to another trained person. • Physician assumes responsibility. • Transfer to EMS personnel occurs. • Obvious death is recognized. • You are too exhausted to continue or continuing would place you or others in danger. External Cardiac Compressions • Manual chest-pressing method • Mimics the squeezing and relaxation cycles of a normal heartbeat • Place patient on a firm, flat surface. (1 of 2) External Cardiac Compressions • Technique – Place heel of one hand on the center (middle) of the victim’s chest (which is the lower half of the sternum). – Place heel of other hand on top and interlock fingers. • For effective compressions: – Push fast – Push hard – Allow chest to fully recoil – Minimize any interruptions (2 of 2) One-Rescuer Adult CPR • Check patient’s level of consciousness and Check for breathing at the same time. • Place patient on back. • Check for signs of circulation (carotid pulse). • Deliver 30 chest compressions • Use a rate of at least 100 compressions per minute. • Open the airway and give two rescue breaths 1 second each. • Continue ratio of 30 compressions to two breaths. Two-Rescuer CPR • • • • More effective than one-rescuer CPR. One rescuer gives chest compressions. The other rescuer delivers ventilations. Compressions and ventilations should remain rhythmic and uninterrupted. Switching CPR Positions • The rescuer giving chest compressions will get tired if performing CPR for an extended time. • Switching positions after every five cycles improves quality of compressions. • The switch should be accomplished as quickly as possible (ideally in less than 5 seconds) to minimize interruptions in chest compressions. One rescuer Infant CPR • Principles are the same, but techniques are modified: – Use brachial pulse. – Press on middle of sternum with two fingers. – Compress sternum approximately 4cm. – Give small puffs of air. – Compression to ventilation rate 30/2 . Two-Rescuer Infant CPR • Use the two-thumb/encircling hands technique. • Compress the sternum at a rate of at least 100 compressions per minute. • Perform compressions and ventilations at a ratio of 15 to 2. Child CPR • Child is defined as a person between 1 year of age and the onset of puberty (12 to 14 years). • In small children, use only one hand. • Use less force to compress the chest. • Use less force to ventilate. (1 of 2) Child CPR (2 of 2) • • Locate top and bottom of sternum. Place the heel of your hand in the center of the chest, (the lower half of the sternum). Signs of Effective CPR • Patient’s skin color improves. • Chest visibly rises during ventilations. • Compressions and ventilations are delivered at the appropriate rate and depth. Complications of CPR • Broken ribs – Check and correct your hand position. • Gastric distention – Caused by too much air blown too fast and too forcefully into stomach • Regurgitation – Be prepared to deal with it! Creating Sufficient Space • Create or find a space where you can perform CPR. • Have 3 to 4 feet on all sides of patient. • Two options – Quickly rearrange furniture. – Quickly drag patient into open area. (1 of 2) Creating Sufficient Space (2 of 2) Defibrillation • Roughly 250,000 people die each year in the U.S. of coronary heart disease in out-of-hospital setting. • More than 70% of out-of-hospital cardiac arrest patients have V-fib. – Rapid, disorganized, and ineffective vibration of the heart – Electric shock can defibrillate. Ventricular fibrillation Defibrillation Normal sinus rhythm (1 of 3) Defibrillation An automated external defibrillator. (2 of 3) Defibrillation • Patients in cardiac arrest have greatest chance for survival when early defibrillation is available. • AEDs identify V-fib and advise rescuers to deliver shock if needed. • Learn how to use your specific AED. • Get required training and practice! (3 of 3) CPR Training • First responders should complete CPR course through recognized agency. • Update your skills through recertification courses. • Schedule periodic reviews of CPR theory and practice for all first responders. Legal Implications of CPR • Start CPR on all patients unless obviously dead. • Physician at the hospital will determine whether you should stop. • Check your department’s protocols and state regulations.