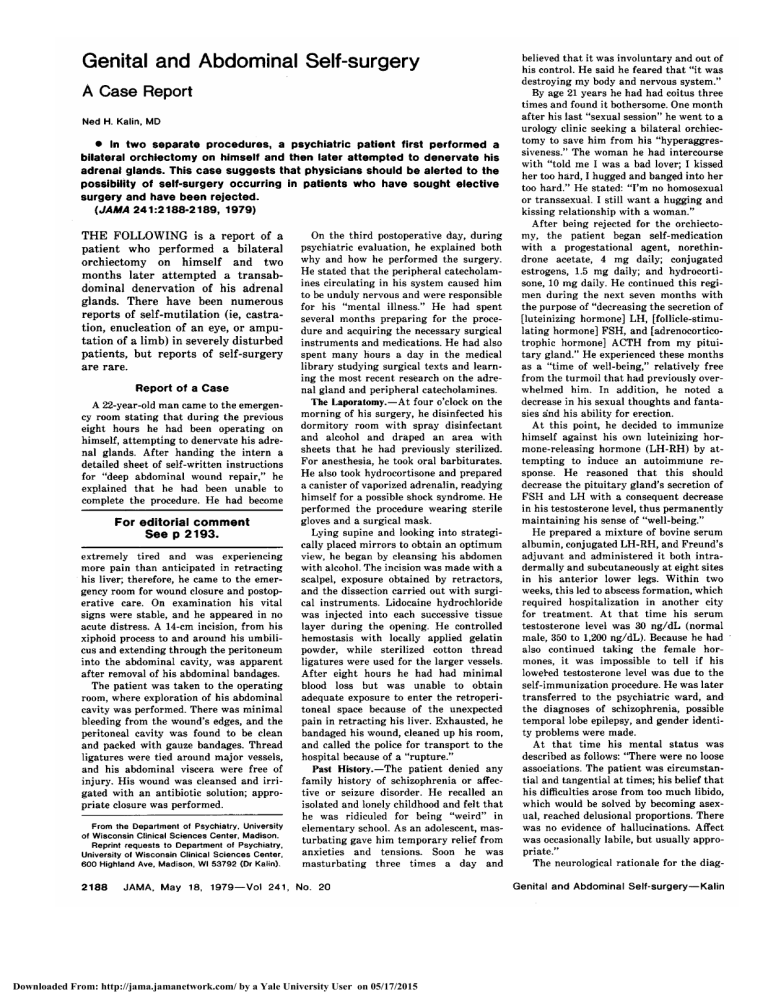
Genital and Abdominal Self-surgery A Case Report Ned H. Kalin, MD In two separate procedures, a psychiatric patient first performed a bilateral orchiectomy on himself and then later attempted to denervate his adrenal glands. This case suggests that physicians should be alerted to the possibility of self-surgery occurring in patients who have sought elective surgery and have been rejected. (JAMA 241:2188-2189, 1979) THE FOLLOWING is a report of a patient who performed a bilateral orchiectomy on himself and two months later attempted a transab¬ dominal denervation of his adrenal glands. There have been numerous reports of self-mutilation (ie, castra¬ tion, enucleation of an eye, or ampu¬ tation of a limb) in severely disturbed patients, but reports of self-surgery are rare. Report of a Case A 22-year-old man came to the emergen¬ cy room stating that during the previous eight hours he had been operating on himself, attempting to denervate his adre¬ nal glands. After handing the intern a detailed sheet of self-written instructions for "deep abdominal wound repair," he explained that he had been unable to complete the procedure. He had become For editorial comment See p 2193. extremely tired and was experiencing more pain than anticipated in retracting his liver; therefore, he came to the emer¬ gency room for wound closure and postop¬ erative care. On examination his vital stable, and he appeared in no acute distress. A 14-cm incision, from his xiphoid process to and around his umbili¬ cus and extending through the peritoneum into the abdominal cavity, was apparent signs were after removal of his abdominal bandages. The patient was taken to the operating room, where exploration of his abdominal cavity was performed. There was minimal bleeding from the wound's edges, and the peritoneal cavity was found to be clean and packed with gauze bandages. Thread ligatures were tied around major vessels, and his abdominal viscera were free of injury. His wound was cleansed and irri¬ gated with an antibiotic solution; appro¬ priate closure was performed. From the Department of Psychiatry, University of Wisconsin Clinical Sciences Center, Madison. Reprint requests to Department of Psychiatry, University of Wisconsin Clinical Sciences Center, Highland Ave, Madison, WI 53792 (Dr Kalin). 600 On the third postoperative day, during psychiatric evaluation, he explained both why and how he performed the surgery. He stated that the peripheral catecholamines circulating in his system caused him to be unduly nervous and were responsible for his "mental illness." He had spent several months preparing for the proce¬ dure and acquiring the necessary surgical instruments and medications. He had also spent many hours a day in the medical library studying surgical texts and learn¬ ing the most recent research on the adre¬ nal gland and peripheral catecholamines. The Laporatomy.—At four o'clock on the morning of his surgery, he disinfected his dormitory room with spray disinfectant and alcohol and draped an area with sheets that he had previously sterilized. For anesthesia, he took oral barbiturates. He also took hydrocortisone and prepared a canister of vaporized adrenalin, readying himself for a possible shock syndrome. He performed the procedure wearing sterile gloves and a surgical mask. Lying supine and looking into strategi¬ cally placed mirrors to obtain an optimum view, he began by cleansing his abdomen with alcohol. The incision was made with a scalpel, exposure obtained by retractors, and the dissection carried out with surgi¬ cal instruments. Lidocaine hydrochloride was injected into each successive tissue layer during the opening. He controlled hemostasis with locally applied gelatin powder, while sterilized cotton thread ligatures were used for the larger vessels. After eight hours he had had minimal blood loss but was unable to obtain adequate exposure to enter the retroperitoneal space because of the unexpected pain in retracting his liver. Exhausted, he bandaged his wound, cleaned up his room, and called the police for transport to the hospital because of a "rupture." Past History.—The patient denied any family history of schizophrenia or affec¬ tive or seizure disorder. He recalled an isolated and lonely childhood and felt that he was ridiculed for being "weird" in elementary school. As an adolescent, mas¬ turbating gave him temporary relief from anxieties and tensions. Soon he was masturbating three times a day and Downloaded From: http://jama.jamanetwork.com/ by a Yale University User on 05/17/2015 believed that it was involuntary and out of his control. He said he feared that "it was destroying my body and nervous system." By age 21 years he had had coitus three times and found it bothersome. One month after his last "sexual session" he went to a urology clinic seeking a bilateral orchiec¬ tomy to save him from his "hyperaggressiveness." The woman he had intercourse with "told me I was a bad lover; I kissed her too hard, I hugged and banged into her too hard." He stated: "I'm no homosexual or transsexual. I still want a hugging and kissing relationship with a woman." After being rejected for the orchiecto¬ my, the patient began self-medication with a progestational agent, norethindrone acetate, 4 mg daily; conjugated estrogens, 1.5 mg daily; and hydrocortisone, 10 mg daily. He continued this regi¬ men during the next seven months with the purpose of "decreasing the secretion of [luteinizing hormone] LH, [follicle-stimu¬ lating hormone] PSH, and [adrenocorticotrophic hormone] ACTH from my pitui¬ tary gland." He experienced these months "time of well-being," relatively free from the turmoil that had previously over¬ whelmed him. In addition, he noted a decrease in his sexual thoughts and fanta¬ sies and his ability for erection. At this point, he decided to immunize himself against his own luteinizing hor¬ mone-releasing hormone (LH-RH) by at¬ tempting to induce an autoimmune re¬ sponse. He reasoned that this should decrease the pituitary gland's secretion of FSH and LH with a consequent decrease in his testosterone level, thus permanently maintaining his sense of "well-being." He prepared a mixture of bovine serum as a albumin, conjugated LH-RH, and Freund's adjuvant and administered it both intradermally and subcutaneously at eight sites in his anterior lower legs. Within two weeks, this led to abscess formation, which required hospitalization in another city for treatment. At that time his serum testosterone level was 30 ng/dL (normal male, 350 to 1,200 ng/dL). Because he had also continued taking the female hor¬ mones, it was impossible to tell if his lowered testosterone level was due to the self-immunization procedure. He was later transferred to the psychiatric ward, and the diagnoses of schizophrenia, possible temporal lobe epilepsy, and gender identi¬ ty problems were made. At that time his mental status was described as follows: "There were no loose associations. The patient was circumstan¬ tial and tangential at times; his belief that his difficulties arose from too much libido, which would be solved by becoming asex¬ ual, reached delusional proportions. There was no evidence of hallucinations. Affect was occasionally labile, but usually appro¬ priate." The neurological rationale for the diag- nosis of temporal lobe epilepsy was based on the patient's history. Apparently, he had had a convulsive episode at 4 years of age. For the past ten years he had suffered with migraine headaches over the left temporal region, and two recent EEGs disclosed a single spike in the left prefrontal region. A computerized axial tomographic scan showed no focal abnormali¬ ties but was read as minimal dilation of both temporal horns of his lateral ventri¬ cles. It was believed that his current disor¬ ganized state and his premorbid personali¬ ty were similar to those described in some temporal lobe epileptics. He remained hospitalized for five more weeks and was treated with neuroleptic and anticonvulsant agents with minimal improvement. Nevertheless, he was discharged receiving chlorpromazine hydrochloride, 800 mg daily, and carbamazepine, 200 mg daily. Four months later he came to the gender clinic of another well-known hospi¬ tal. After extensive evaluation and psycho¬ logical testing, it was decided that he be given a nonfeminizing, antiandrogen hor¬ mone, medroxyprogesterone acetate, be¬ cause: "At the present time, the obsession to suppress masculine sexual feelings and functions is so intense and overwhelming that the patient is not about to relinquish taking estrogens, because it gives him some measure of relief." Two months later, in another location, he was unable to find a physician who would agree to continue his treatment with the medroxyprogesterone acetate. After approximately four months, or two months before admission to our hospital, the patient performed a bilateral transscrotal orchiectomy on himself. The proce¬ dure lasted eight hours, and he again used oral phénobarbital and local lidocaine for anesthesia. He taped shut the bilateral scrotal incisions and went to the emergen¬ cy room requesting that a urologist evalu¬ ate the surgery and close the incision. Both spermatic cords were ligated within the scrotum with strings that extended through the incision and were taped to his thighs. He was taken to the operating room for revision of his orchiectomy and wound closure. Present History.—Following the orchiec¬ tomy, he began to see a psychiatrist week¬ ly, who described him as being "distant and inaccessible." It was two months after the orchiectomy that he attempted to denervate his adrenal glands. When the patient's mental status was first evaluated by psychiatrists, he was described as a "slight young man wearing tinted sunglasses, sitting in his bed, at times moving in a rocking motion and grasping at his genital area. While talking he maintained no eye contact and spoke in a monotone. He stated his mood was depressed and exhibited occasional inap¬ propriate smiling. His thought processes were tangential and circumstantial. He admitted to auditory hallucinations in the past, hearing his mother talk to him, but denied any currently. He believed that the nurses weren't feeding him because they were secretly trying to kill him. He denied grandiose, somatic, self-referential, or passive-control delusions. He was totally preoccupied with his self-surgical proce¬ any dures and catecholamine theories." The report of psychological testing stated that his major defense mechanisms in the face of anxiety were projection and delusional thinking. The Minnesota Multi- phasic Personality Inventory suggested a schizophrenic psychosis. An EEG was normal; the neurology consultant believed the diagnosis of temporal lobe epilepsy was questionable and recommended against treatment with anticonvulsants. The diagnosis of paranoid schizophrenia was made, and the patient was treated with thiothixene for two weeks, with mini¬ mal improvement. At the time of this writing the patient is researching the prospect of administering spinal anesthe¬ sia to himself in reattempting his adrenal surgery. Comment This patient's self-taught under¬ standing of medical concepts is im¬ pressive, not to mention his applica¬ tions of this knowledge. The induction of an autoimmune response to an LHRH has been performed in rabbits, with resultant gonadal atrophy,' but has never before been attempted in a human. Unfortunately, coadministration of the female hormones masked the direct results of this procedure on his plasma testosterone level. Consid¬ ering that he had never before seen an operation performed, the amount of preparation and necessary skill used in his surgery seems profound. Lowy and Kolivakis2 and Money and DePriest3 have described four pa¬ tients who performed genital selfsurgery, but none of these patients seemed as well prepared or skilled in their surgical technique. I have been unable to locate any accounts of ab¬ dominal self-surgery in the literature. In some ways this patient is similar to the ones described by the afore¬ mentioned authors. Three out of four of their patients' conditions were diagnosed as schizophrenic, and all of the patients actively sought out a physician to perform the surgery but were turned away. Perhaps these cases should be a warning to surgeons who, for whatever reasons, reject patients seeking elective plastic sur¬ gery. One interesting difference is that these four patients supposedly Downloaded From: http://jama.jamanetwork.com/ by a Yale University User on 05/17/2015 acted out of transsexual motivations; they had strong wishes to alter their gender. This was not the underlying dynamic force for this patient. He stated: "I'm no homosexual or trans¬ sexual. I still want a hugging and kissing relationship with a woman." His sexual aim was to express affec¬ tion to a woman without the arousal. The physician is put in a difficult position by this patient's demands. One might argue that if the bilateral orchiectomy had been done at the patient's request, then his abdominal surgery might have been circum¬ vented. But this is unlikely, given his unrelenting history of self-treat¬ ments. In fact, giving in to him would reinforce his delusional belief that his testosterone caused his great intrapsychic pain. This case demonstrates the importance of accurate evaluation of the motives in patients who seek sex-change operations. There is a tragic paradox in this patient's dilemma. He has mastered the concepts and techniques of medi¬ cines in an attempt to cure himself, when in reality, we have little to offer him that would result in effective treatment. He is relatively unrespon¬ sive to antipsychotic agents and has been unable to form a working alliance with his psychotherapist. It seems the only hope is to engage him in a long and intensive psychotherapy in which a therapeutic alliance could be established and maintained. At the same time, his urge to operate on himself must be brought under con¬ trol. Unfortunately, he does not see the relevance of such a difficult and laborious task and is much more comfortable spending hours in the medical library preparing for his next "curative" operation. James Jefferson, MD, and Susan Pacheco, RN, assisted in the preparation of this manuscript. Nonproprietary Names and Trademarks of Drugs Carbamazepine—Tegretol. Norethindrone Nor-QD. acetate—Micronor, Norlutin, Thiothixene—Navane. References 1. Arimura A, Sato H, Kumasaka T, et al: Production of antiserum to LH-releasing hormone (LH-RH) associated with gonadal atrophy in rabbits: Development of radioimmunoassays forLH-RH. Endocrinology 93:1092-1103, 1973. 2. Lowy FH, Kolivakis TL: Autocastration by a male transsexual. Can Psychiatr Assoc J 16:399-405, 1971. 3. Money J, DePriest M: Three cases of genital self-surgery and their relationship to transsexualism. J Sex Res 12:283-294, 1976.