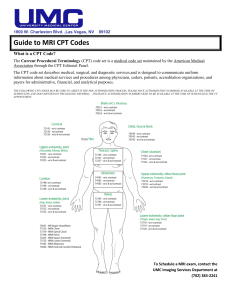
Sample test questions for the CPC exam The following 20 questions were developed by HCPro’s Certified Coder Boot Ca p® instructors for preparation of the Certified Professional Coder (CPC) ® exam. Unless the question states otherwise, assume that a physician documented all the information provided. You have two minutes to complete each question. You may not use any outside materials for this exam other than the 2015 CPT, ICD-9-CM, and HCPCS Level II manuals. JustCoding Platinum members have access to a 150-question practice exam. To learn how to become a Plati u e er, li k o the ta “ee Pri i g Pla s. 1. Dr. Armstrong, a plastic surgeon, completed a bilateral rhytidectomy of the neck and a suctionassisted lipe to of the right upper ar . Whi h ode s should e reported for Dr. Ar stro g’s services? a. 15828-50, 15879-RT-59 b. 15826-59, 15879-RT-59 c. 15828-50, 15878-RT-59 d. 15826-RT, 15828-50, 15878-RT-59 2. Which code describes a cutaneous flap, transposed into a nearby but not immediately adjacent defect, with a pedicle that incorporates an axial vessel into its design? a. 15757 b. 15758 c. 15750 d. 15740 3. Jack fell from a ladder six months ago and broke his left radius. The fracture is not healing as expected and the implant needs to be replaced. Today, Jack underwent a secondary procedure. Dr. Gene completed an open treatment with internal fixation of the radial neck, including replacement of the prostheti radial head. Ho should ou report Dr. Ge e’s ser i es? a. 24666-LT b. 24366-LT c. 25607-LT d. 24587-LT 4. A patient underwent a mini-open repair of her right rotator cuff. How should you report this procedure? a. 29827-RT b. 23410-RT c. 23412-RT d. 23410-RT, 29827-RT-59 5. A 20-year-old smoker had a single 8.2-mm lung nodule reported on CT of the chest. The peripheral nodule was not amendable to biopsy by routine bronchoscopy. The patient agreed to undergo a diagnostic bronchoscopy with computer-assisted navigation under moderate sedation. Dr. Smith completed the procedure and provided moderate sedation with a trained observer. The intra-service time was documented as 45 minutes. How should Dr. Smith report her codes for this procedure? a. 31622, 31627 b. 31622, 31627-51 c. 31622, 31627-51, 76376, 99144, 99145 d. 31622, 31627, 99144, 99145 6. A patient with a benign neoplasm of the bronchus and lung underwent a bronchoplasty with a cartilage auto-graft repair. The thoracotomy site was closed with layered closure and a chest tube was left in place for drainage. How should you report this procedure and diagnosis? a. 212.3, 31770 b. 199.1, 212.3, 31775, 20910-51 c. 209.61, 31825 d. 212.3, 209.61, 31775, 31825-51 7. A 45-year-old male patient suffers from postprandial chest pain and abdominal pain. After workup and testing, he was diagnosed with a large paraesophageal hernia. Today, he underwent a laparoscopic repair ith i pla tatio of esh a d a edge gastroplast . Ho should ou report toda ’s ser i e? a. 43282, 43283 b. 43281, 43282, 43283 c. 43332, 43283-51 d. 43280, 43283 8. A patient underwent a laparoscopic gastric restrictive procedure with placement of only a gastric band. This is considered an individual component placement. How should you report this service? a. 43659-59 b. 43770-22 c. 43659-58 d. 43770-52 9. Which code(s) should Dr. Stone report in the following case? Brief history of present illness: 26-year-old female with a history of nephrolithiasis. She complained of left-sided flank discomfort with hematuria, dysuria, and passage of fragments. This morning she presented to the ED with increased left and right side flank pain. She underwent CT with contrast of the abdomen and pelvis showing approximately eight right renal calculi ranging between 2 and 12 mm and 10 left renal calculi ranging between 5 and 8 mm with possible nephrocalcinosis based on the radiologist’s i terpretatio . Dr. “to e, the urologist, o sulted ith the patie t, re ie ed results of the CT scan, and discussed treatment options. The patient signed an informed consent for the following procedure. Postoperative diagnosis: Bilateral nephrolithiasis Procedure: Lithotripsy, extracorporeal shock wave. She was given 1 g Ancef®, brought to the operating room, and placed supine on the lithotripsy table. With fluoroscopy, the right and left kidneys were evaluated with no overlying bowel gas, stool, or bowel contents; multiple stones were visualized (R. 8 and L. 10). The ureters were examined and showed no stones or fragments present. Stones were targeted for treatment via extracorporeal shock wave with successful breakdown and flush. After treatment, the patient was awakened in the operating room and extubated without difficulty. She was taken to recovery in stable condition. a. 275.49, 592.0, 50590 b. 592.0, 74177, 50590 c. 592.0, 592.1, 789.09, 50590 d. 592.0, 50590 10. A patient underwent a complex cystometogram with bladder voiding pressure study and a urethral EMG. Which codes should you use to report these services? a. 51728, 51784-51 b. 51725, 51785-51 c. 51726, 51797-59 d. 51728, 51784-59 11. A patient underwent a transforaminal epidural injection of anesthetic and steroids under ultrasound guidance. The injections were completed at L1, L2, and L3. How should you report the professional services for this procedure? a. 0230T, 0231T x 2 b. 64483, 64484 x2, 76942-26 c. 64493, 64494, 64495 d. 0230T, 0231T x 2, 76942-26 12. Dr. Grant injected Mrs. Brown with two units of chemodenervation (onabotulinumtoxinA) to treat her bilateral blepharospasm. How should Dr. Grant report his services? a. 67345-50, J0585 x 2 b. 67345 c. 64612-50, J0585 x 2 d. 64612 13. Which code range should you use if the same physician provides critical care services to a neonatal or pediatric patient in both the outpatient and inpatient settings on the same day? a. 99460–99463 b. 99291–99292 c. 99468–99476 d. 99281–99285 14. Baby boy Busch was evaluated in the birthing center the morning of his birth. The documentation noted a comprehensive examination and a maternal/fetal/newborn history, and decision-making for discharge was straightforward. Documentation revealed a normal newborn, and the decision was made to discharge later that same day. How should you report this service? a. 99463 b. 99460-25, 99463 c. 99221-25, 99238 d. 99234 15. Dr. Sally, an anesthesiologist, provided general anesthesia for a 72-year-old patient with mild hypertension undergoing an open arthroscopy of the humeral neck. During this procedure Dr. Sally was not supervising or monitoring any other cases. How should Dr. Sally report her code(s) for this case? a. 01630-AA-P2, 99100 b. 01620-AA-P2, 99100 c. 01630-P2 d. 01634-P2 16. A healthy 32-year-old patient required an urgent vaginal hysterectomy following delivery of her third baby. What anesthesia code(s) should you report for this case? a. 01962-P1, 01969-51 b. 01967-P1, 01969 c. 01963-P1 d. 01962-P1 17. How should Dr. Levitt report his services in the following case? Dr. Levitt’s offi e o s a d operates the -ray equipment he used to complete the reading of the films for this patient. At the conclusion of the x-ray and his interpretation, he dictated the following report: Patient: Mrs. Russell X-ray left foot: Three views Impressions: Fracture of distal phalanx, first digit. Fractures of second and third digits (phalangeal). There is a fracture of the proximal portion of the first-digit phalanx. A comminuted fracture is noted in the middle phalanx of the second digit, and an increased density is seen medially in the joint space of the middle phalanx of the third and fourth digits. Oblique films confirm displaced fragment of bone between the second and third digits. No other abnormalities are present or noted. a. 73630-LT b. 73620-26-LT c. 73650-LT d. 73630-26-LT 18. Brooke, a 9-month-old girl, underwent a radiologic exam for osseous survey of the axil and appendicular skeleton to look for current and/or old healed fractures. The radiology order listed the primary diagnosis as probable fracture to right arm and suspected child abuse. How should you report this radiological exam? a. 76499-59 b. 77075-26-TC c. 77076 d. 77072-22 19. Dan is being tested for the presence of a tumor in his bladder. One of the tests completed for Dan was cell enumeration using immunologic selection and identification in fluid specimen. The specialized reference laboratory that completed this test provided the physician interpretation and report. How should the laboratory report this service? a. 86294 b. 88184 c. 86152, 86153 d. 86316, 86153 20. Mathew, a 31-year-old patient, was seen for occupational evaluation January 15. At that time, Dr. Winters determined that Mathew might require additional physical therapy and possible surgery for his injuries. Today, March 18, Dr. Winters reevaluated Mathew’s a ilit to return to work as a heavyequipment operator, after a second endoscopic surgery to his right elbow and extensive physical therap . Ho should Dr. Wi ters report toda ’s ser i e? a. 99213-25, 97001 b. 99213 c. 97003 d. 97004 Answer key: 1. c. You can locate the procedures in the index of the CPT® Professional Edition under Rhytidectomy and Lipectomy/Aspiration (see Liposuction). Once the code range is located in the index, review the codes for anatomic location of the procedure. A parenthetical note under the rhytidectomy codes provides guidance for modifier -50 to report a bilateral procedure. Modifier -RT is reported on the second procedure to clarify the arm involved and -59 to indicate a different site. 2. d. To select the correct answer, review each code and the definitions in the guidelines under Other Flaps and Grafts. 3. a. You can find the procedure in the index of the CPT® Professional Edition under Fracture/Radius/Head/Neck/Open Treatment. The location of the treatment (bone and area) is important when coding for fractures. 4. c. You can locate the procedure in the index of the CPT® Professional Edition under Rotator Cuff/Repair. The parenthetical note under code 23412 indicates arthroscopic procedure use 29827. The note under code 29827 refers back to 23412 for open or mini-open repair. Reading the parenthetical notes helps with proper code selection. 5. a. You can locate the main procedure in the index of the CPT® Professional Edition under Bronchoscopy/Exploration. You can find the add-on procedure under Bronchoscopy/Computer-assisted Navigation. Modifier -51 is not used with add-on codes. Review (Appendix A) in the CPT® Professional Edition. Moderate sedation is included with the procedure codes in this question. Lastly, always review the parenthetical notes with add-on codes to help with reporting. 6. a. You can locate this procedure in the index of the CPT® Professional Edition under Bronchoplasty/Graft Repair. The graft and closure repairs are included. You can find the diagnosis code in the ICD-9-CM index under Neoplasm/Bronchus/Benign. 7. a. You can locate the procedure in the index of the CPT® Professional Edition under Hernia Repair/Paraesophageal/Laparoscopic. Review of the codes and parenthetical notes in this section will assist with code selection. 8. d. Review the parenthetical note under code 43770 for modifier assignment. 9. d. You can locate the procedure in the index of the CPT® Professional Edition under Lithotripsy/Kidney. The hospital would be responsible for coding the CT. Dr. Stone’s review of the report does not constitute coding for that study. The definitive diagnosis should be reported. In this case, the diagnosis is found in the postoperative statement. Signs and symptoms associated routinely with a disease process are not reported unless instructional notes in ICD-9-CM indicate otherwise. To find this rule, review the ICD-9-CM introduction for conditions that are an integral part of the disease process. 10. a. The guidelines for urodynamic codes direct coders to use modifier -51 when multiple procedures are performed in the same investigative session. 11. a. You can locate the procedure in the index of the CPT® Professional Edition under Injection/Anesthetic Agent/Spine/Lumbar. This procedure was completed with ultrasound guidance, which should be reported with a Category III code. Review the parenthetical note below code 64483 for additional reporting guidance. 12. c. Notice in this code the word muscle(s), which means you should report this code once regardless of the number of muscles treated. See the parenthetical notes under codes 64612–64614 for guidance with modifier -50 and reporting per session. Per the guidelines in this section, the supply of chemodenervation (drug) agent is reported separately. 13. c. You can find this answer in the CPT® Professional Edition in the guidelines for inpatient neonatal and pediatric critical care codes. 14. a. The code 99463 included newborn care services with place of service, admission, and discharge on the same date. 15. a. You can locate the correct code range in the index of the CPT® Professional Edition under Anesthesia/Arthroscopic Procedures/Shoulder. Review the codes in this range to determine the correct code for an open procedure. Modifiers are required for clarification of an anesthesiologist working on the case (found in HCPCS Level II) and the patient’s physical status. The add-on code is reported due to the patient’s age. 16. d. You can locate this code in the index of the CPT® Professional Edition under Anesthesia/Hysterectomy. The key to selecting the correct code in this question is the description of the procedure as urgent. Notice this code does not specify the route of the procedure. 17. a. You can find the procedure in the index of the CPT® Professional Edition under X-ray/Foot. This report is for a three-view x-ray and reported without modifier -26 or -TC because Dr. Levitt completed both the professional and technical components. 18. c. You can locate the procedure in the index of the CPT® Professional Edition under Xray/Bone/Osseous Survey. The correct code indicates infant in the description. 19. c. You can locate the procedure in the index of the CPT® Professional Edition under Immunology. After locating this code range, review the codes for the specific type of test performed. In this case, you would report the codes for cell enumeration. 20. d. You can locate the procedure in the index of the CPT® Professional Edition under Occupational Therapy/Evaluation. This is a reevaluation visit reported by code 97004.