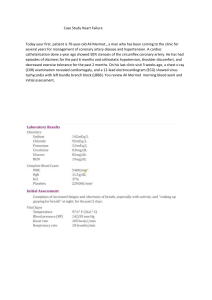
Cardiac Case Study John Watson 56 years old Barbara Durham, DNP, RN, CNE, CHSE 1 Scenario WHAT DATA ARE RELEVANT AND HAVE CLINICAL SIGNIFICANCE FOR THE NURSE? • S- John Watson, a 56-year-old male, was admitted to your telemetry floor from the emergency department (ED) with a medical diagnosis of “cardiomyopathy, coronary artery disease, probable MI.” • B- Mr. Watson has a past health history of hyperlipidemia, hypertension, chronic renal insufficiency, and a recently diagnosed 4 cm suprarenal abdominal aortic aneurysm. His wife brought him to the ED after he reported unrelieved “indigestion.” 2 Scenario • O2 @ 4L/NC to keep sats > 94% ASA 325 mg PO was given • IV #1 with LR @ 75 ml/hr; IV#2 Nitroglycerin @ 5 mcg/min (50 mg/250ml) P-Q-R-S-T Pain Assessment (5th VS) CURRENT VS Temp: 99.1 F/37.3 C Provoking/Palliative Unknown HR: 94 irreg Quality: Sharp RR: 24 Region/Radiation: Chest BP: 202/124 Severity: 9/10 O2 Sat: 93% Timing: Continuous WHAT VS DATA ARE RELEVANT AND HAVE CLINICAL SIGNIFICANCE FOR THE NURSE? 3 What is your priority? PLANNING •At this time, what are 3 priority goals for the telemetry RN assigned to Mr. Watson based on his admitting diagnosis and PMH? Place them in the order of priority. 1. _____________ 2. _____________ 3. _____________ 4 What is your priority? •What are 3 priority interventions for the telemetry RN assigned to Mr. Watson based on goals identified on the previous slide? Place them in the order of priority. 1. _____________ 2. _____________ 3. _____________ INTERVENTIONS BREAK OUT GROUPS 5 Chest Pain • WHAT MEDICATIONS DO YOU ANTICIPATE STARTING AND WHY? • IS MR. WATSON A CANDIDATE FOR TPA? • What is the major risk? • STAT LABS RESULTS HAVE RETURNED • Review the characteristics of stable versus unstable angina and acute coronary syndrome. 6 Comparison: Clinical Manifestations • Angina – chest pain lasting 2-5 minutes, usually relieved by rest • Dyspnea, pallor, tachycardia, anxiety, fear • Women have atypical symptoms • ACS (Unstable angina) – more severe chest pain lasting 10-20 minutes, can occur at rest • Above plus diaphoresis, cool skin, hypotension, lightheaded • AMI – sudden onset of continuous pain that is unrelieved (>20 min) • Sustained ischemia; necrosis occurs over 4-6 hrs • Above plus a sense of impending doom, S&S of HF • Women have worse outcomes 7 Acute Coronary Syndrome Etiology and Pathophysiology • When ischemia is prolonged and is not immediately reversible, acute coronary syndrome (ACS) develops. Deterioration of once stable plague Rupture Platelet aggregation Thrombus • Result • Partial occlusion of coronary artery: UA or NSTEMI • Total occlusion of coronary artery: STEMI 8 STEMI vs NSTEMI STEMI NSTEMI • ST elevation • Progression to Q wave • Full blockage of coronary artery • ST depression • No progression to Q wave • Partial blockage of coronary artery • Positive troponin • More URGENT • Positive troponin • Due to NECROSIS = permanent damage • Severe ISCHEMIA = reversible • Fibrinolytics may be harmful • Fibrinolytics are beneficial • Heparin is often prescribed 9 Pharmacology: • ONAM: • Oxygen, nitro, aspirin, morphine • Lower cholesterol • Statins, bile acid sequestrants, nicotinic acid, fibric acid derivatives • Treat angina • Nitrates, beta-blockers, calcium-channel blockers, aspirin • Treat myocardial infarction • Analgesics, fibrinolytics, antidysrhythmic, antiplatelet 10 Fibrinolytics • Breaks down/dissolves blood clots • Nursing considerations: • Must know contraindications • Recent surgery or trauma, bleeding disorder, uncontrolled HTN • Monitor for signs of bleeding • No invasive procedures • Evaluate response to treatment: Normalized ST segments, relief of chest pain • Stay on bedrest for 6 hours • Monitor for manifestations of reocclusion 11 Chart Review: WHAT LAB DATA ARE RELEVANT AND HAVE CLINICAL SIGNIFICANCE FOR THE NURSE? Lab Result K Na Cl Glu BUN Cr 4.3 mEq/L 139 mEq/L 108 mEq/L 159 mg/dL 23 mg/dL 1.4 mg/dL Lab Cholesterol Triglycerides HDL LDL Troponin T CK-MB BNP Mg Result 225 mg/dL 186 mg/dL 25 mg/dL 160 mg/dL 3.2 ng/mL 10% 78 pg/ml 1.8 mEq/L 12 Mr. Watson continues to report chest pain and a 12-lead ECG is ordered STAT. WHAT IS YOUR INTERPRETATION AND NURSING INTERVENTIONS? The ECG tech hands you Mr. Watson’s 12-lead ECG results… 13 Coronary Arteries: 14 ECG Changes Associated With Acute Coronary Syndrome (ACS) ISCHEMIA INJURY INFARCTION 16 17 Interpret these 12-lead ECGs 18 THE HCP PLANS FOR AN EMERGENT PCI. Mr. Watson is awaiting a cardiac catheterization… WHAT TEACHING WILL YOU PROVIDE REGARDING THE PROCEDURE? • Benefits of PCI: • Locate and open blocked artery • Determine presence of collateral circulation • Evaluate left ventricular function • What complications can be anticipated as a result of the procedure? 19 Nurses role with Cardiac Cath: BEFORE • Allergy to contrast dye • NPO 6-12 hr before procedure • Teaching expectations with the procedure • Sedatives will be given • BASELINE assessment • VS, SpO2, heart/lung sounds, CMS, Labs 20 Balloon angioplasty STENT LAD Circumflex 21 Scenario progression: • Several hours later, Mr. Watson returns from the cardiac catheterization lab. The catheterization report shows 50% occlusion of the proximal left anterior descending coronary artery (LAD), 50% occlusion of the distal LAD, 95% occlusion of the distal right coronary artery (RCA), and old inferior infarction with an ejection fraction of 37%. WHAT POST PROCEDURE NURSING INTERVENTIONS WILL YOU PERFORM? WHAT IS YOUR INTERPRETATON OF THESE RESULTS? 22 Nurses role with Cardiac Cath: AFTER • Keep patient on bedrest • Assess CMS, frequently to extremity • Observe insertion site for signs of bleeding or hematoma over arterial site (q15min x4) • Monitor VS, ECG, dysrhythmias, respiratory distress (PE) • Monitor for chest pain • Monitor IV infusions 23 Closure Devices Angio-seal 24 Closure Devices FemoSTOP TR BAND 25 AMI-1 Aspirin on arrival AMI-2,5, 10 Aspirin, Beta blocker, and Statin prescribed on discharge AMI-3 ACEI or ARB for LVSD AMI-4 Smoking cessation counselling AMI-7 Time to Thrombolytics = 30 min AMI-8 Time to PCI = 90 min 26 Scenario progression: • About an hour after the procedure, you perform a brief nursing assessment and find that Mr. Watson now has a loud grade III/IV systolic ejection murmur at the cardiac apex with palpable thrill, crackles bilaterally in the lung bases, and trace pitting edema of his feet and ankles. Except for a soft systolic murmur, these findings were not present before the catheterization. You get a prescription to draw a CBC and complete metabolic panel. WHAT DO THE CHANGES IN THE PATIENT STATUS SUGGEST? 27 Chart Review: WHAT LAB DATA ARE RELEVANT AND HAVE CLINICAL SIGNIFICANCE FOR THE NURSE? Lab Hgb BNP BUN Cr Result 8.8 g/dL 189 pg/mL 33 mg/dL 3.1mg/dL 28 Pathophysiology-Heart Failure Neurohormonal Responses SNS Stimulation Epi/norepi release, inc MO2 demand and workload RAAS, ADH, proinflammatory cytokines Counter regulatory: BNP is release to vasodilate and enhance diuresis, NO also dilates and dec afterload • How is the heart going to compensate for the low cardiac output and impending failure? Ventricular dilation (remodeling) Initially adaptive, then becomes inadequate Ventricular Hypertrophy Response to beat harder, results in poor contractility, high O2 needs, and inc risk for dysrhythmias 29 Mr. Watson goes into heart failure and requires an IABP while waiting for surgery. A Swan-Ganz catheter is inserted. Result CVP 13 mmHg PAP 38/23 mmHg PAWP 21 mmHg SVR 1623 dynes/sec CI 1.8 L/min HOW DO YOU INTERPRET THE RESULTS OF THE SWAN-GANZ CATHETER? WHAT IS THE NURSES ROLE IN CARING FOR PATIENTS WITH AN IABP? 30 Intraaortic Balloon Pump (IABP) • Balloon inserted into femoral artery and placed in thoracic aorta • Confirm placement with x-ray • Inflate balloon with helium in conjunction with ECG Copyright © 2017, Elsevier Inc. All Rights Reserved. Intraaortic Balloon Pump (IABP) • Complications of IABP therapy • Vascular injuries • Thrombus and embolus formation • Thrombocytopenia • Ischemia to periphery, kidneys, bowel • Infection Copyright © 2017, Elsevier Inc. All Rights Reserved. Intraaortic Balloon Pump (IABP) • To decrease risks of IABP therapy • Frequent assessments • Keep patient immobile and limited to side-lying or supine positions with HOB <45 degrees • Wean from IABP by gradually reducing assist ratio Copyright © 2017, Elsevier Inc. All Rights Reserved. HF-1 Discharge Instructions* Activity , Diet , Follow-up , Medications , Symptoms Worsening , Weight Monitoring HF-2 Evaluation of LV Function* Assessed before or during hospital stay Or documentation that LV will be assessed p/DC HF-3 Add ACEI or ARB LV systolic dysfunction = EF < 40% HF-4 Adult Smoking Cessation Counseling* 34 35 ACE inhibitors May develop persistent, dry cough Angiotensin II receptor blockers -Adrenergic blockers Diuretics Vasodilators Positive Inotrope (Digitalis) Antidysrhythmics CAM - Hawthorne Nursing Considerations: Monitor BP, weight, check pulse Careful with position changes Keep hydrated; don’t take diuretics after 5pm Monitor for S&S dig toxicity and hypokalemia Be careful with OTC meds Notify HCP if experience any changes, keep follow up appointments Diet and weight reduction: Individualize recommendations and consider cultural background Recommend Dietary Approaches to Stop Hypertension (DASH) diet. Sodium is usually restricted to 1.5 – 2 g per day. Fluid restriction not generally required Daily weights are important Same time, same clothing each day Weight gain of 3 lb (1.4 kg) over 2 days or a 3- to 5-lb (2.3 kg) gain over a week should be reported to health care provider. 36 One day later, Mr. Watson begins to report sharp, severe stabbing chest pain. It is worse on inspiration. WHAT ADDITIONAL ASSESSMENTS DO YOU WANT TO DO? HOW DO YOU TREAT THE PAIN? HOW DO YOU POSITION THE PATIENT NOW? WHAT ARE COMPLICATIONS ASSOCIATED WITH THIS CONDITION? HOW WOULD YOU KNOW THE COMPLICATION HAS OCCURRED? 37 Caused by inflammation around pericardial sac Normally has a lubrication function (10-15 ml) Clinical Manifestations: Severe, sharp, stabbing chest pain Worse on inspiration and supine Pain can be referred to trapezius muscle Pericardial friction rub Nursing Management: Elevate HOB 45 o Anti-inflammatory meds 38 Complications: Pericardial Effusion – ▪ Dyspnea, distant heart sounds, cough, hiccups, hoarseness Cardiac tamponade ▪ Beck’s triad ▪ Muffled heart sounds**, hypotension with a narrowing pulse pressure, and JVD ▪ Pulsus paradoxus - drop>10 mm Hg SBP during inspiration ▪ Confused, restless, anxious, CP, dec CO 39 Scenario progression: • Two days later, Mr. Watson undergoes coronary artery bypass surgery of 2 coronary arteries (CABG X 2). WHAT ARE SOME COMPLICATIONS RELATED TO CARDIOPULMONARY BYPASS? REVIEW TYPES OF SURGERY FOR BYPASS. DISCUSS THE NURSING INTERVENTIONS FOR A PATIENT POST BYPASS SURGERY. 40 Internal Mammary Artery and Saphenous Vein Grafts Copyright © 2017, Elsevier Inc. All Rights Reserved. Nursing Management Acute Coronary Syndrome • Coronary revascularization: CABG ICU for first 24–36 hours Pulmonary artery catheter Intraarterial line Pleural/mediastinal chest tubes Continuous ECG ET tube with mechanical ventilation Epicardial pacing wires Urinary catheter NG tube Copyright © 2017, Elsevier Inc. All Rights Reserved. Nursing Management Acute Coronary Syndrome • Complications related to CPB Bleeding and anemia from damage to RBCs and platelets Fluid and electrolyte imbalances Hypothermia as blood is cooled as it passes through the bypass machine Infections Copyright © 2017, Elsevier Inc. All Rights Reserved. Nursing Management Acute Coronary Syndrome • CABG: postoperative nursing care Assess patient for bleeding Monitor hemodynamic status Assess fluid status Replace blood and electrolytes PRN Restore temperature Monitor for atrial fibrillation (which is common) Copyright © 2017, Elsevier Inc. All Rights Reserved. Nursing Management Acute Coronary Syndrome • CABG: postoperative nursing care Surgical site care • Radial artery harvest site • Leg incisions • Chest incision Pain management DVT prevention Pulmonary hygiene Cognitive dysfunction Copyright © 2017, Elsevier Inc. All Rights Reserved. Scenario progression: • After 3 days in the heart center, Mr. Watson’s condition is stable and he is returned to the telemetry floor. Now, 5 days later, he is ready to go home and you are preparing him for discharge. WHAT SHOULD BE INCLUDED IN THE DISCHARGE INSTRUCTIONS POST AMI, PCI, AND CABG? 46 Nursing Management Acute Coronary Syndrome • Ambulatory Care Cardiac rehabilitation Patient and caregiver teaching Physical activity • METs scale • Monitor heart rate • Low-level stress test before discharge • Isometric versus isotonic activities Copyright © 2017, Elsevier Inc. All Rights Reserved. Nursing Management Acute Coronary Syndrome • Ambulatory Care Resumption of sexual activity • Teach when discuss other physical activity • Erectile dysfunction drugs contraindicated with nitrates • Prophylactic nitrates before sexual activity • When to avoid sex • Typically 7–10 days post MI or when patient can climb two flights of stairs Copyright © 2017, Elsevier Inc. All Rights Reserved. Nursing Management Acute Coronary Syndrome • Dietary Considerations Low cholesterol (<200 mg/day) Low in saturated fats (<7% of calories) DASH diet for HTN (reduced salt/Na) Inc fiber, fruits and vegetables National Guidelines for treating high LDL Risk scores are calculated based on • Age • Gender • Use of tobacco • Systolic BP • Use of BP medications • Total cholesterol • HDL cholesterol level • Framingham Heart Study Treatment • Therapeutic lifestyle changes (TLC) Diet Physical activity Weight management • Drug therapy • DHHS NIH NHLBI 50 National Guidelines for treating high LDL DHHS NIH NHLBI Healthy People Goals • Less than 7 % of your daily calories from saturated fat • Achieve and maintain a healthy weight • Less than 200 mg a day of cholesterol • Reduce salt and sodium intake • 25–35 % of daily calories from total fat • Increase level of physical activity • Diet options you can use for more LDL lowering Plant stanols or sterols Soluable fiber • Avoid use of all tobacco products • Limit alcohol intake to small to moderate amounts (12 oz beer, 4 oz wine, 1 oz hard liquor) • Only enough calories to reach or maintain a healthy weight • • At least 30 minutes of a moderate intensity physical activity, such as brisk walking, on most, and preferably all, days of the week. Chose a diet that is low in dietary cholesterol and total and saturated fat, and high in fruits and vegetables 51