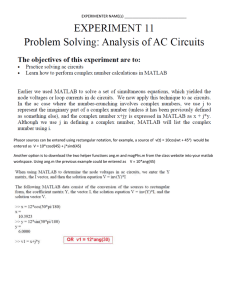
Pagkalinga Paggunita Pagninilay First volume of the PGH Human Spirit Project PAGKALINGA Ang Pagtugon sa Pandemya ng Pagamutan ng Bayan Alvin B. Caballes Amanda Marie A. Cheong Gabrielle P. Flores Markyn Jared N. Kho Alfonso Rafael G. Abaya Marie Bernadine D. Caballes Paul Miguel P. Perez Editors UNIVERSITY OF THE PHILIPPINES MANILA Copyright © 2020 University of the Philippines Manila First Edition December 2020 ISBN: 978-621-454-002-0 All rights reserved. No part of this publication may be copied or used without the permission of the individual authors, photographers and publisher. Book and Cover Design by Alfonso Rafael G. Abaya Cover Photo by Brent Viray Published by the University of the Philippines Manila “To have compassion for those who suffer is a human quality which everyone should possess, especially those who have required comfort themselves in the past and have managed to find it in others.” - Giovanni Boccaccio, The Decameron Contents Foreword i Gerardo D. Legaspi Prefaceiv Alvin B. Caballes “Ang Bagong Maynila”1 Cindy Pearl J. Sotalbo Incubation Countdown to Lockdown: From Patient Zero to Community Quarantine Nefren Roy A. Lobitana 6 Prodrome Hello again18 Sachiko S. Estreller Walang Iwanan21 Paul Miguel P. Perez My Cup Overflows Amanda Marie A. Cheong 24 If28 Robyn Gayle K. Dychiao Musings from a Pulmonologist at the Frontline Jubert P. Benedicto 35 Shifting Gears40 Lily de Amor When Nightingales Cry43 Paulo Ross B. Sison Disease A Battle of Silence52 Cary Amiel G. Villanueva A Normal Day55 Viktoria Ines P. Matibag Let me tell you about PPEs 58 Fish Out of Water: A Dermatologist in COVID 62 Ella Mae Masamayor Amanda Christine F. Esquivel Second Wind65 Erika P. Ong The Long Trek to the Front Justin Bryan D. Maranan 69 Empty Spaces75 Amanda A. Cheong And In Return79 Robyn Gayle K. Dychiao A Matter of Mantras83 Jill Olivia Bañares Overcoming Inertia87 Fr. Marlito Ocon Skin in the Game94 Justin Bryan D. Maranan The Physician in Plastic100 John Jefferson V. Besa Soldiering On102 Hilda Uy Ashen104 Anna Elvira S. Arcellana I don’t feel like a hero105 Ella Mae Masamayor Side Effects Sa Gitna ng Pandemya114 Ian Gabriel A. Juyad Broken Spirits115 Cary Amiel G. Villanueva Mama119 Gabrielle P. Flores Lost to Follow-up122 Anna Elvira S. Arcellana Uncarved Pieta126 Athena Mae Ibon Laru-laruan132 Athena Mae Ibon Suntok sa Buwan135 Athena Mae Ibon From Fighting Cancer to COVID-19: The Battle is Not Over137 Mikki Miranda Pinagtagping Tahanan141 Gabrielle P. Flores Finding a Path in Crisis146 Maria Angela M. Villa Yet Another Uncertainty149 Vince Elic S. Maullon Recovery 03.31.20156 Sachiko S. Estreller The Persistence of Our Memories Juan Raphael M. Perez 158 Science161 Trisha M. Salcedo Hope of Easter162 Thaddeus Hinunangan The Destination of My COVID Dreams Howie Severino 166 “Kumusta ka?”171 Maria Keziah G. Legion In Sickness and In Health175 Genry Criscel R. Consul Life goes on180 Patricia Anne S. Basilio Puhon182 Christi Annah Hipona Glossary185 Contributors 196 Editors207 Photo by Brent Viray 12 Foreword It is said, most especially in the scientific world, that what is not written does not exist. There are those times I would discuss with my residents unique observations in neurosurgery, or a personal innovation of a procedure, and lose it into oblivion because we never got to write them down. As a consolation, I would just tell my residents to “tell the story” of that surgery around a bonfire, or during one of their future drinking sessions. These ideas and stories abound in our daily lives and we never get to immortalize them with words. I can easily relate these experiences to the stories of the Human Spirit. I’m so thankful that this has come about, and done justice to some of those significant human experiences. Surely, all the pages of this book will not capture everything, but it will leave us with enough cues to help us remember the untold details that were also vital to the whole picture. Nevertheless, let me add a few more. After having gotten the concurrence of the UP President and the UPM Chancellor for PGH to accept the role of being a COVID referral center, we had barely a week to prepare. I assembled a COVID Crisis Management Team composed mainly of surgeons who knew what needed to be done and how to do it and do it fast. At the end of that meeting on March 22, 2020, that was a Sunday, I was left in the Director’s office with the COVID operations head. Probably seeing me in deep thought, pondering on the commitment we had just made to the public, he went on to say some of the most comforting words I would hear during those times. “Boss, huwag kang magalala. Ang malaking advantage natin, likas na magaling ang mga taga PGH.” i The frenzy of attending to all the details didn’t leave much time for us to stop and check our bearings. Midway into the preparations, I realized that the PPEs we were expecting to come were not available anymore. Our remaining two-week stock was a far cry from the one and a half months supply we set as a minimum to start the COVID Operations. The logistics coordinator was with me late during that day and I couldn’t keep the doubt to myself anymore. I asked him, “ Magagawa kaya natin lahat ito?” Almost instantly he bantered back, “Wala tayong choice brod, kailangan nating gawin ito!” From that day on, we never looked back and just went full speed ahead. The rest, so they say, is history. Covering the COVID crisis will never be complete without dealing with the fear that pervaded the initial days. In mid-April, more and more of our doctor-friends were succumbing to the infection and the prevailing danger was very palpable. In one of our late night meetings, while walking on the grounds of PGH, our “Voice of Science” in the team, obviously shaken, told me, “Gap ayaw kong mamatay”. It completely caught me by surprise, knowing her as very steady in her demeanour and confident in her ways. Of course it sent chills down my spine, but I had to maintain my composure for the team. Almost instinctively, and naively I think, I retorted “Walang mamamatay.” That was one time when fear gripped me too. Everyday, we encountered stories that inspired us and lifted our spirits. There was a nursing attendant wanting so much to report for duty who decided to walk from her home in the northern part of the city. She was stopped three hours later at a strictly guarded checkpoint. Undeterred, she went up to a TV Crew and convinced them to give her a ride to PGH. She ii was a news sensation that evening! There, too, were the countless employees who braved the floods, vehicles, and the fact that it was their first time to do so on their bicycles, just to get to work. There, too, were the donors, big and small, who believed in what PGH represented and wanted to be part of those who gave hope. This crisis has highlighted what Charles Dickens said in a Tale of Two Cities, “It was the best of times, it was the worst of times.” Although, arguably, we have experienced probably one of the worst times in our history as a people, we definitely have seen the best traits come out. Never mind the worse part. It doesn’t serve anyone any good to be punitive in a pandemic. As of this writing, PGH has been a COVID Referral Center for almost eight months. In the daily routine of hospital work, these stories of the Human Spirit continue. I can’t wait to light the bonfire and open the bottle to start telling more of these. Observing minimum health protocol, of course! (For now.) Gerardo D. Legaspi Director of the Philippine General Hospital 11- 10- 2020 iii Preface This life-filled tome was conceived 17 years ago, following a century-old crisis. The seed came into being on a cold, dark, and rainy March day, when the streets of a bustling Asian city suddenly became deserted. A new pandemic had taken hold. With hospitals shutting in medical staff with their patients to contain the transmission, I decided to cut short my fellowship stint. I went home wanting to keep a step ahead of the contagion. Fortunately, SARS did not spread readily in the country and seemed destined to be but a footnote in local medical lore. But even after the initial alarm had long faded, I strongly felt that we had simply dodged a bullet. The SARS virus was, we got to know in time, a projectile that heralded itself by a rise in the body temperature among those it had already infected. The next infectious disease may not have as obvious a presence, and the established public health lines of defense may thus be rendered inutile. Having seen firsthand the resulting disruptions with SARS on both the greater community as well as a better developed and organized health system, I knew that the ensuing hardships will be much greater with a more potent virus. The instruments of science will, of course, again be harnessed against any new threat. Except that the microbes are not to be found and wrestled in isolated laboratory media but within us. How would strands of foreign biological material affect individual psyches, if not souls? What would be the bodily and mental scars left in the wake of a more severe pandemic? How would it affect us collectively? How would such a cataclysm define a nation? What would humanity lose, and gain? Our people had faced similar circumstances a little over a century ago. As recently reported by Gealogo, the flu pandemic of 1918 had, over successive waves, swept over what was then a colony caught amid a world war and so-called Filipinization of the government hierarchy1. The men being prepared for the conflagration in Europe, having been marshalled from other provinces into a military camp in Rizal, provided a perfect nidus for the spread of the disease. Soldiers ended up dying without ever reaching any battlefields, as the armistice was signed before they could be shipped out while the local viral invasion remained unchecked. iv 1 Gealogo FA. (2009). The Philippines in the World of the Influenza Pandemic of 1918-1919. Philippine Studies. 57(2), 261-92. By the time the scourge subsided, an estimated 80,000 lives were lost across the islands, the most from any single health calamity in the country. But aside from mostly administrative reports, not much else was written about the catastrophe2. The tragedy seemed like a non-event in the country’s history. The paucity in published insights on the 1918 pandemic is not peculiar to the Philippines. Even as it occurred in relatively recent historical times, the world-wide crisis was not a prominent theme in contemporaneous literary works. It is therefore often referred to as “the forgotten pandemic”3. The concurrent war, with its clash of empires and pretensions of glory, may have made for a more compelling subject. Alternately, the pandemic may have simply caused too overwhelming a suffering to instill enough creative inspiration. It is now 2020. An infectious outbreak had precipitated what seemed to be unthinkable in modern times. A lockdown sealed off the city of Wuhan, with its 11 million inhabitants, in January. The virus and the populationwide quarantine measures have since taken root elsewhere, including the Philippines. Following a few days of panic buying and frantic exodus to supposed safer environs, the streets of Metro Manila became empty and silent by the end of March. It was a déjà vu moment, as this was the same eerie landscape that I had experienced in 2003. Except that what was happening seemed to be much worse. And it was happening here, where my loved ones are, where deadlines have to be met, where colleagues mingle, where people go for their regular burger dose, where students endure classes, where friends gather to celebrate, where families leisurely pick out their needs and wants from store shelves, where patients receive care. Struggling, and dying, patients soon became the face of the newly labeled disease, COVID-19. To address the fast-rising tide of afflicted patients, if not the intensifying sense of panic, the Philippine General Hospital (PGH) was converted into a dedicated COVID center. The measure was not without controversy, more so as thousands of other patients who depend on the institution would be deprived of much-needed services. The step also meant that hospital facilities, resources, and processes, had to be re-purposed to amply address the vicissitudes of a still 2 3 Coutant AF. (1918). An epidemic of influenza at Manila, PI. Journal of the American Medical Association. 71(19):1566-7. Vázquez-Espinosa E, Laganà C, Vazquez F. (2020). The Spanish flu and the fiction literature. Revista Española de Quimioterapia. 33(5):296. v enigmatic illness. Above all, it bore upon hundreds of individuals who, by obligation or choice, now had to hold back their fears and apprehensions and confront the virus and its ravages on a very personal level. The COVID-19 pandemic is already historic in many ways. But it would also be important for the current and future generations to learn “not so much about how many people died or how it was treated.”4 These were our history lessons from 1918, and even 2003. The rapidly evolving situation at PGH underscored the aphorism that in times of uncertainty and adversity, everything rested on what every person at task felt, thought, and did. Above all, therefore, the brewing crisis needed to be seen intimately, from the perspectives of the many who had to walk into the miasma. Thus, the seed was sown for what was to be called the “PGH Human Spirit Project”. A general call was made on the 25th of March, 2020 for contributors for a literary compilation. The announcement read, “In this season of difficulty, frustration, and even loss, there will be shining moments of selflessness, fulfillment, and hope. These will have to be preserved for posterity, not to highlight the suffering, but, more importantly, to demonstrate the resilience of the human spirit in the face of seemingly insurmountable odds.” Before long, students, residents, nurses, faculty, and others, lent their imagination, time and talent. Though none were professional writers, their sincerity shone through in their submissions. A core group was organized to efficiently handle the accumulating material. Partnerships between authors and volunteer staff were forged to refine the fresh but untamed works. Many more, however, wanted to participate, particularly those who weren’t directly involved with PGH or only had past associations with the university. Thus, the coverage was expanded, and the original PGH-centered book evolved into a three-volume set. The compendium came to encompass the complex and the mundane, politics and passion, tragedy and humor, divine and secular, a pinch of Defoe, and a good measure of Boccaccio.5,6 Ocampo A, as quoted by Vivas J. (2020). A history lesson on pandemics in the Philippines. Manila Bulletin. Retrieved from URL https://mb.com.ph/2020/09/24/ahistory-lesson-on-pandemics-in-the-philippines/ 5 DeGabriele, P. (2020). Intimacy, Survival, and Resistance: Daniel Defoe’s A Journal of the Plague Year. ELH. 77(1):1-23. 6 Wallace DJ. (1991). Boccaccio: Decameron. Cambridge University Press. 4 vi In keeping with the times, everything was put together remotely, and a social media page was even set up for the project by a clever team of students. I have the utmost appreciation and admiration for the dedication and enthusiasm of all those who came to be part of the effort. It is regrettable that, with the mostly virtual interactions, I have been unable to directly convey my heartfelt gratitude to them. The exceptional outcome of their individual, as well as concerted efforts, are manifest in the succeeding pages. Still, we may just have chronicled the beginning. The toll may yet exceed that for 1918. Nobody knows what bodes for March 2021. Or for 2120. The streets may yet fall silent once again. Pagkalinga, Paggunita, and Pagninilay have finally sprung from a simple planted idea. That many heeded the call to nurture it has been a wondrous and humbling experience. The publications’ multitude of words and images now branch out and bask in the light of day — or the glare of innumerable computer screens. The tales and tableaus will always remind us. A sickness came. Our people suffered. But Oblation’s offspring looked up, raised their arms, and chose to help overcome the despair. For a hospital, a university, and a nation, hope and purpose are rekindled. Alvin B. Caballes vii Ang Bagong Maynila Cindy Pearl J. Sotalbo March 14, 2019 On a normal day, I avoided passing here, even if it was closer to the house. This area, no matter what time of day, was always an assault to the senses compared to the more peaceful path through the UP campus at the back. Today, I had to take this route because there was another PUI1 being received in the triage area where I usually pass. But there were no cliques coming home from a night of drinking, no homeless people preparing their cardboard beds on the sidewalk, no commuters waiting for PUVs2. It was odd passing through here and not hearing the laughter and shouts of the vendors, the noisy jeepney engines, the honking of the cars stuck in between people crossing; not seeing PUVs waiting for passengers, and pedicabs maneuvering their way through the chaos. Even the characteristic, subtle, street smell-- typically a mix of vehicle fumes, spilled petrol, sweat, vomit, other bodily fluids and the distinct scent of the bay-- was absent. It felt strange, almost eerie, being the only person in this segment of the street. Is this going to be the new normal? “It felt strange, almost eerie, being the only person in this segment of the street. Is this going to be the new normal?” Photo by Cindy Pearl J. Sotalbo Copyedited by Amanda Marie A. Cheong 1 2 See glossary. The Philippine General Hospital is at the southwestern edge of the district of Ermita. This and surrounding areas of Manila used to have mostly affluent residences. Following the devastation of the second world war, the area underwent a transformation that reflected the country’s uneven development. High-rise buildings and government facilities were interspersed with dilapidated houses and seedy establishments. Jeepneys-also called Public Utility Vehicles or PUVS-and other means of conveyance clogged the streets, while commuters packed the coaches of the Light Rail Transit running over Taft Avenue, the main road artery. One can find all walks of life on the streets on a regular night, from homeless people looking for refuge, students studying out, workers trying to avoid rush hour, to foreigners hoping to enjoy the city. These establishments, along with public transport, were forced to close down with the imposition of quarantine measures on March 16, 2020. 1 Photo by Maria Keziah Legion INCUBATION 3 4 Incubation /iNGky ’bāSH n/ n. e e The period between the entry of an infectious agent (e.g. viruses, bacteria) and the onset of signs and symptoms of the disease. The incubation period for COVID-19 is reported to be between 1-12.5 days. COVID-19 slithered into many countries, often from individuals not known to already harbor the virus, with reports of overtly sick patients coming out at increasingly alarming numbers in succeeding days. The disease inevitably landed on our shores. The clock ticks and the race to stem the tide is on. 5 2019 Countdown to Lockdown : From Patient Zero to Community Quarantine Nefren Roy A. Lobitana The year started off ominously enough. January 2020 opened with tensions rising in the Middle East. Wildfires reduced Australia’s forests to embers. Indonesia was drowning for weeks in continuous rain and subsequent flooding. Locally, Taal Volcano erupted; and the massive ash fall descended on Southern Luzon and the capital area. Nearly half a million people had to be evacuated. An emerging outbreak in a province of China, first noticed when the previous year was drawing to a close, seemed but an inconsequential side story to these harrowing headlines. In the weeks that followed, however, it quickly became clear that this was no ordinary outbreak. It was coming for everyone, everywhere. World Health Organization DECEMBER The Chinese government reports a cluster of forty-four pneumonia cases in Wuhan, their cause unknown1. Symptoms of Coronavirus This novel syndrome presents with a combination of fever, cough, diarrhea, sore throat, and pneumonia, all of varying severity. Know the symptoms of COVID-19, which can in Cough, shortness of breath or difficulty breathing Center for Disease Control and Prevention DECEMBER 31 Xie Huanchi/Xinhua Via AP 6 Muscle or body aches Vomiting or diarrhea WHO | Pneumonia of unknown cause – China. (2020). WHO. Retrieved April 2, 2020, from http://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-causechina/en/ Symptoms can range from mild to severe illness, and app 1 2020 JANUARY JANUARY JANUARY 12 The genetic sequence of the nowtermed Novel Coronavirus (nCOV) is released4. In the days that followed, other countries such as Japan, the USA, Nepal, France, Australia, Malaysia, South Korea, Vietnam, and Taiwan confirm imported cases, all traced to travelers from Wuhan. Li Wenliang, a Chinese doctor who tried to issue the first warning about the deadly coronavirus outbreak People’s Daily, China Attempts to warn the public are allegedly met with censorship2. Chinese researchers confirm that the disease is not a re-emergence of the 2003 SARS. The outbreak is caused by an entirely new and different virus3. The first case outside China is documented in Thailand5. JANUARY 13 JANUARY 6 UNESCO Bangkok Coronavirus kills Chinese whistleblower doctor. (2020, February 7). BBC News. https://www.bbc.com/news/world-asia-china-51403795 Rose Carmelle Lacuata. (2020). TIMELINE: The new coronavirus outbreak. ABS-CBN News. Retrieved April 2, 2020, from https://news.abs-cbn.com/spotlight/02/04/20/ timeline-the-new-coronavirus-outbreak 4 WHO | Novel Coronavirus – China. (2020). WHO. Retrieved April 2, 2020, from http://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/ 5 Coronavirus Disease (COVID-19)—Events as they happen. (2020). Retrieved April 3, 2020, from https://www.who.int/emergencies/diseases/novel-coronavirus-2019/ events-as-they-happen 2 3 7 2020 JANUARY 24 JANUARY 21 In China, there are 300 documented cases of nCOV infections and four casualties. What everyone feared turned out to be true: Chinese scientists confirm that nCOV can actually spread between people6. The Philippine government deports 135 individuals from Wuhan after arriving at Kalibo International Airport. The STAR/Rudy Santos The deportation, however, was a little too late as these individuals reportedly had already gone around the locale8. The number of new cases continue to increase, culminating in the lockdown of Wuhan with other cities in Central China following suit7. This catapulted the possibility of the virus entering the Philippines into public consciousness. Darley Shen/Reuters JANUARY 23 China confirms human-to-human transmission of new coronavirus. (2020). Retrieved April 2, 2020, from https://www.aljazeera.com/news/2020/01/china-confirmshuman-human-transmission-coronavirus-200120162507948.html/ 7 China new year plans scrapped as Wuhan coronavirus spreads—CNN. (2020). Retrieved April 2, 2020, from https://edition.cnn.com/2020/01/23/china/wuhancoronavirus-update-intl-hnk/index.html 8 Malasig, J. (2020, January 24). Philippine government’s order to deport travelers from Wuhan: Was it too late? Interaksyon. https://www.interaksyon.com/politicsissues/2020/01/24/160692/coronavirus-wuhan-deportation-order-aklan-philippines/ 6 8 2020 FEBRUARY JANUARY 30 The WHO declares the nCOV outbreak as a Public Health Emergency of International Concern9. FEBRUARY 2 There were 7834 confirmed cases, 98 of them were outside China. One of those 98 showed up in the Philippines. The novel coronavirus finally reaches the country10. David Montasco / Google Maps Members of the health sector and several senators in the country strengthen calls for the implementation of a travel ban11. The government issues a travel ban on all Chinese nationals from Hubei and other affected provinces of China12. JANUARY 31 A 44 year-old Male from Wuhan dies at San Lazaro Hospital in Manila. He is eventually found to be positive for nCOV: the first nCOV death outside of China13. DOH confirms a third nCOV case in the country14. FEBRUARY 5 Office of Senator Sherwin Gatchalian IHR Emergency Committee on Novel Coronavirus (2019-nCoV). (2020). Retrieved April 2, 2020, from https://www.who.int/dg/speeches/detail/who-director-general-sstatement-on-ihr-emergency-committee-on-novel-coronavirus-(2019-ncov) 10 Sabalo, 2020 11 Luna, F. (2020). Senators want “Great Wall” vs Chinese visitors amid first Philippine novel coronavirus case. Philstar.Com. Retrieved April 3, 2020, from https://www. philstar.com/headlines/2020/01/30/1989051/senators-want-great-wall-vs-chinese-visitors-amid-first-philippine-novel-coronavirus-case 12 Duterte bans travelers from Wuhan, Hubei as coronavirus spreads. (2020). Retrieved April 2, 2020, from https://www.rappler.com/nation/250640-duterte-banstravelers-from-wuhan-hubei-coronavirus 13 First coronavirus death outside China reported. (2020). NBC News. Retrieved April 3, 2020, from https://www.nbcnews.com/news/world/first-coronavirus-deathoutside-china-reported-philippines-n1128371 14 DOH CONFIRMS 3RD 2019-NCOV ARD CASE IN PH | Department of Health website. (2020). Retrieved April 3, 2020, from https://www.doh.gov.ph/doh-press-release/ doh-confirms-3rd-2019-nCoV-ARD-case-in-PH 9 9 2020 FEBRUARY 11 The WHO announce that the disease would henceforth be named Corona Virus Disease 2019 or COVID-19, This was meant to standardize and the virus as SARS- nomenclature and prevent CoV-2. racial stigmatization, following racially-directed attacks in some countries15. This was also in the light of groups decrying racism directed against the Chinese 16. For the rest of the month, there are no new cases are reported in the Philippines, but cases and deaths continue to rise worldwide. By the end of February, there is a total of 85,403 confirmed cases and 2,924 deaths worldwide18. Researchers from the University of the Philippines National Institute of Health develop a new COVID-19 test kit that is cheaper and faster than the WHO test kits17. FEBRUARY 14 DOST Website Coronavirus Disease (COVID-19)—Events as they happen. (2020). Retrieved April 3, 2020, from https://www.who.int/emergencies/diseases/novel-coronavirus-2019/ events-as-they-happen 16 Groups decry racism against Chinese amid coronavirus outbreak. (2020). Cnn. Retrieved April 22, 2020, from https://www.cnnphilippines.com/news/2020/2/1/groupsdecry-racism-coronavirus-china.html 17 PH eyes local production of test kits for COVID-19 | ABS-CBN News. (2020). Retrieved April 3, 2020, from https://news.abs-cbn.com/news/02/14/20/ph-eyes-localproduction-of-test-kits-for-covid-19 18 WHO | Pneumonia of unknown cause – China. (2020). WHO. Retrieved April 2, 2020, from http://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-causechina/en/ 15 10 2020 MARCH MARCH 7 The 59/F wife of the country’s case number five tests positive, establishing the first local transmission in the country. Veejay Villafranca/Bloomberg Two new COVID cases are confirmed in the country, from a 48/M Filipino who had a travel history to Japan, and a 62/M with no foreign travel history19. The notion of local transmission begins to worry the public, leading senators, such as Risa Hontiveros, to point out the inadequacy of testing in the country20. MARCH 5 This prompts the DOH to raise the COVID-19 Alert System to Code Red Sublevel 1 due to the growing number of cases21. COVID-19 cases in the country reach 20, and the Office of the President puts the country under a State of Public Health Emergency Public and private schools and universities across Metro Manila close down22. MARCH 9 Philippines records 2 new COVID-19 cases. (2020). GMA News Online. Retrieved April 3, 2020, from https://www.gmanetwork.com/news/news/nation/728576/ philippines-records-2-more-covid-19-cases/story/ 20 DOH confirms first 2 Filipinos found with coronavirus locally. (n.d.). Rappler. Retrieved April 22, 2020, from http://www.rappler.com/nation/253584-doh-confirms-2filipinos-positive-coronavirus 21 DOH confirms 6th coronavirus case in PH. (2020). Rappler. Retrieved April 3, 2020, from http://www.rappler.com/nation/253696-doh-confirms-6th-case-coronavirusphilippines 22 Duterte declares state of public health emergency amid rise in coronavirus cases. (2020). Rappler. Retrieved April 3, 2020, from http://www.rappler.com/nation/253833duterte-declares-state-public-health-emergency-rise-coronavirus-cases-march-2020 19 11 2020 MARCH 12 52 MARCH 10 33 confimed COVID-19 cases in the Philippines confimed COVID-19 cases in the Philippines Reuters Travel in and out of the Metro would be restricted, but mass transport would still be allowed given that social distancing measures were implemented23 . 49 confimed COVID-19 cases in the Philippines MARCH 11 12 The Office of the President announces that it would place Metro Manila under community quarantine starting at midnight of March 15 until April 14. In the Philippine General Hospital, clinical clerks are pulled out from their posts. This announcement disturbed the already anxious public. Metro Manila to be placed on lockdown due to coronavirus outbreak. (2020). Retrieved April 3, 2020, from https://www.rappler.com/nation/254101-metro-manilaplaced-on-lockdown-coronavirus-outbreak 23 2020 MARCH 14 111 confirmed cases of COVID-19 in the Philippines Residents, fellows, and consultants are suddenly left to carry on their shoulders the enormous patient load of PGH25. The Association of Philippine Medical Colleges issues a memorandum ordering the pull out of all medical interns from the country’s teaching hospitals. Metro Manila is placed under community quarantine, and the megacity is transformed into an eerie ghost town. People start to flock to grocery stores for food while others flee Metro Manila out of fear of being caught in the community quarantine24. MARCH 13 Reuters MARCH 15 24 25 News, A.-C. (2020-b). Stop “panic buying” due to COVID-19, supplies can be replenished: Trade chief. ABS-CBN News. Retrieved April 3, 2020, from https://lifestyle.mb.com.ph/2020/03/24/pgh-interns-volunteer-despite-apmc-order-to-pull-out/ 13 The clock then ticked past midnight of March 15. Metro Manila transformed from a bustling megalopolis to an eerie ghost town. Streets became devoid of people. The daily din of cars, jeepneys, and all other manner of noisy transportation suddenly vanished into silence. Meanwhile, the doctors, nurses, and other staff of the PGH tried to make sense of what was happening, and prepare for the coming days to unfold. Copyedited by: Gabrielle P. Flores and Amanda Marie Cheong 14 Photo by Markyn Kho PRODROME 15 16 Prodrome /’prō,drōm/ n. The period or state wherein early signs and symptoms are noticeable, heralding the onset of a disease. The most common early symptoms of COVID-19 are cough, fever, and malaise. However, many other early symptoms have been reported, such as gastrointestinal symptoms (e.g., nausea and diarrhea) and a loss of taste and smell. The virus that caused the disease, SARS-CoV-2, was invisible. But the perception that it was both everywhere, yet nowhere, pernicious and spreading, was palpable. Like a low-grade fever settling in, the disease’s worrisome presence was slowly being felt by the public. As the country scrambled to respond to the pandemic, everyone at the Philippine General Hospital--the director, staff, trainees, allied and support workers--braced themselves for what seemed inevitable, yet largely unknown. They kept a watchful wait, wondering if and how the pandemic would change the institution, and its history. 17 Hello, Again Sachiko S. Estreller “Sinulat ko na po dito ang follow-up niyo sa clinic, ha, at ang mga kailangan ninyong gamot.” She gave me a nod while I was doing a quick paracentesis to relieve her dyspnea from the malignant ascites. Though she tried to smile, the worry in her icteric eyes showed through1: “Kailan po kaya tayo magkikita uli, doc?” I shrugged and told her that this would probably take a month or so and we would be back. “Dalhin niyo lang ang lab results ninyo para alam po natin aling mga gamot ang kailangang ituloy.” We went through her medications list one last time and I quizzed her on the symptoms she had to watch out for. She thanked me. I did not say goodbye. Earlier that week, the threat of a Manila lockdown had us scurrying. We were doing laboratories, writing abstracts2, making phone calls, and explaining the hospital’s directive to our patients. In between errands, I smiled apologetically at our students: “Given the events, I think we’ll have to postpone our lecture over breakfast next time. Hindi ko makakalimutan, nagpromise ako.” I told them not to worry because we would definitely find time the coming week, but this never happened. Orders for the pull-out of all clerks and interns2 circulated and we found ourselves in gloomy and undermanned wards, devoid of the usual banter between colleagues while doing hospital work. Later in the week, the nearempty and eerily silent hallways witnessed the flurry of hurried changes as the hospital faced a huge transition— that of being a COVID referral center2. Messages from students flooded in, wishing us well and telling us how they felt bad about not being able to help. I told them that we’re going to be okay, that safety was priority. Most of them volunteered for whatever Our patient looks at the doctor with icteric or yellowish eyes, and an abdomen that’s large and taut, being overfilled with fluid called ascites. Dyspnea is when breathing is difficult because the fluid in her abdomen also pushes against the diaphragm and lungs, restricting the space for air. Taken together, these symptoms point to an underlying liver disease, possibly even cancer. The doctor conducts the paracentesis, a procedure to remove excess fluid from body cavities such as the chest and abdomen. 2 See glossary. 1 18 Sadness breeds in the uncertainty of if and when, we’ll ever get to say hello, again. work the hospital permitted them to do, given the limitations. I told them how thankful and proud we were. See you soon, for sure, no goodbyes. Back then, the changes seemed temporary, with an end in sight. Little did I know that the coming weeks of lockdown and quarantine would be filled with farewells even to the small but significant everyday things. Morning commutes. Late night runs. Unmasked smiles and good mornings. Hands held and pats on the back. A simple cup of coffee ordered before the day’s work. A chat over dinner after clinic hours. Auscultating3 with our stethoscopes. Breathing without fogging your goggles. Scratching that itch on your back. The small things overlooked, left unappreciated. But also beyond these, the weeks of isolation and duties in a COVID-dedicated hospital has made me see that there are bigger things at play as well. The colleagues turned into patients after contracting the virus. Parents unable to keep their children close. Families displaced, livelihoods on hold. The sunken eyes of beggars roaming the streets looking for food to eat. The unemployed figuring out how to make ends meet. Closed schools and cancelled ceremonies. Patients asking when they will get well and go home. Anxious relatives asking for updates about their loved ones. The repeated apologies and condolences exchanged with breaking voices and relentless sobs over the phone. While the mundane allows us to have comfort in memories filled with gratitude and hope, the bigger picture teaches us the hard lessons of missed opportunities, pervasive injustice, and painful partings. We geared up for the most basic of needs to face this pandemic but nothing ever prepared us for its longevity, nor the overwhelming loneliness. As the hours blur into days, we find our weary hearts breaking little by little with each act of letting go. 3 Arguably the most iconic symbol of the medical profession, the stethoscope is an invaluable clinical tool. Auscultation, or the act of listening, most often with the aid of a stethoscope, is an important and routine part of the physical exam. Those taking care of COVID-19 patients up close have to wear the full complement of PPE, with a hood covering the head. Thus, stethoscope’s earpieces cannot be used while wearing the PPE, as this will mean possible contamination. 19 Photo by John Jefferson Besa Before her discharge, I remembered asking my cancer patient what she wanted to eat at home. Before their pull-out, I asked our interns about their future dreams and plans. I found myself always asking, what will I do? We ask relatives, our patients, what do you want? I ask others, what do you miss? Whats are the easy part, readily answered. But the looming question in the midst of this pandemic that stumps us all is–When? For the time being, we have learned to answer with tales of “at leasts,” “maybe tomorrows,” and “somedays.” Starting sentences with “when this is over…”, ending them with “…and never take it for granted again.” I feel foolish now thinking that this was going to be over in a month. I wonder when we’ll get to run again, feel the sunshine and the breeze on our faces and bask in the warmth of human interaction. I wonder how many more will be sick, how many more will pass away. How many calls will I end up making? How many cries will be there left to hear? I wonder how my patient is now. Is she at home, safe and well? What did she end up eating? I wonder when we’ll get to see our students again, or if we’ll ever get around to having that breakfast. Most of all, I wonder if I should have said goodbye. But I guess at the end of the day, it is not in the unsaid goodbyes where the most sadness lies. Sadness breeds in the uncertainty of if and when, we’ll ever get to say hello, again. Copyedited by Iris D. Ditan 20 Walang Iwanan Paul Miguel P. Perez I was on the tail end of my ward rotation in Internal Medicine1 when the pandemic hit us like a train. Although I was not in the night duty team1 for that day, I stayed in the hospital a bit later than usual to finish charting1 for some patients. At around 9:00 p.m., the announcement came; medical clerks1 were to be pulled out of their rotations for safety concerns. It caught us all off guard. Since night duties are done by a skeleton workforce1, losing three to four extra hands would be crippling for patient care. Interns and clerks1 have a unique role in the hospital because we spend the most time with the patients, really getting to know even their non-medical concerns. The next morning, since I was among the more senior interns of my service1, I took charge of redistributing the clerks’ patients among the remaining interns. The added patient load made our work much more difficult. Aside from having several other patients, we also had to take the time to get to know each new patient and their problems. At this point, however, we still did not know the full extent of the impending pandemic. We were really just struggling to get by. Two days later, it was announced that we were to be pulled out as well. 1 See glossary. The first thing that entered my mind was relief, as we would be safe and able to return to our families. The second thought was concern, and maybe a little guilt, for those whom we would be leaving behind. In our rotation, we had become very close to the IM residents1 and just could not imagine how they could handle all those patients without our help; the wards were packed! Moreover, the patients whom we had grown to be quite emotionally invested in would suffer the greatest if we were to leave. For these reasons, when my co-intern Nick Tan pitched a volunteer program to continue to serve in the hospital, several of us immediately answered the call. Walang iwanan. This was what we were being trained to do. But we had no idea what we were getting back into. When we returned to the hospital, it was a whole new battleground. Physically, it was no different, but the psychological landscape had changed. For one thing, we did not know which patients might have already contracted COVID-19. We could even have been asymptomatic1 carriers ourselves without realizing it. 21 Most of us did not have the support of our parents in volunteering, and we knew we could not go home after being exposed. I guess I had not given these aspects much thought until I was actually there, putting myself at risk. My own fear tempered my initial enthusiasm. But help came. We received a timely delivery of N95 masks1 from our dean, Dr. Charlotte Chiong, as well as a separate delivery from the younger generation of UP medical students who had raised funds to protect us. We were overwhelmed by the amount of food donations that came, most with grateful messages attached. On our first few days back, our volunteerism had even made the headlines! All of this came without our asking, and it was then when I began to understand the true meaning of bayanihan. In a time when our country needed it most, we were humbled to be part of the People Giving Hope (PGH)1, as our hospital director, Dr. Legaspi, named it. Walang Iwanan. This phrase has galvanized us to join the fray. This is the reason we take risks. We have chosen to continue to serve, and, together, to give hope. When it is all over and the dust has settled, I know that we will pick each other up and together embark on a new challenge – a new normal. And in this new normal – sana wala pa ring iwanan. Photos by Adrianne Alfaro and Mary Joy Beneciro Copyedited by Amanda Marie Cheong 22 1 See glossary. Interns who volunteered to come back and serve after the pull-out pose for some group photos in an emptied Medicine ward. Photos by Paul Perez. 23 My Cup Overflows Amanda Marie A. Cheong “Ilan kayo sa duty1?” I do not know. These days, that has been my go to answer for nearly everything. Which department are you volunteering for? When will your internship1 resume? When will you come back home? I do not know. Still, I hazard a guess: “Three?” I shrugged. Two volunteer interns plus one resident1 doctor. Everyone’s schedule lay on shifting sands. They moved to where they were needed. Then, we medical interns tried to fill in the gaps as best we could. “Dala ka na ng tatlong siopao,” my roommate called out, looking through her own volunteer schedule. Interns volunteering to continue working in PGH was probably not what the respective officials anticipated when they were drafting the memo requiring that interns be pulled out of all hospitals during the pandemic. But before that memo was even released, there was already talk of staying behind. The spirit of a handful of interns favored action over sitting on the sidelines. Meetings were scheduled 24 1 See glossary. as plans were drafted, and then revised. Nothing was set in stone. That evening, the department sent out a waiver for medical intern volunteers to sign, detailing how we understood the risks of what we were entering, as well as what the Philippine General Hospital would provide for us. A fair amount of interns zoomed in on the fifth bullet point: “I understand that the hospital shall be providing for my meals 24/7 during this period…” That group chat buzzed with laughter, with humorous stickers to punctuate the conversation. “Don’t worry, guys. Aside from that, we’ll definitely share and feed you with whatever we have also,” our resident quipped. Everyone was willing to help everyone else. It was heartlifting. While we usually faced daily uncertainties with laughter, the apartment I lived in was strangely quiet. I found myself contemplating the three pieces of siopao; the seven interns working under the department for that morning shift; the residents who have to feed us. When you are trying to fill a gap, it is best not to be a burden. “Sige, dala na rin ako ng curry.” The labor and delivery room would be our fortress for that week. Storms might gather; the earth might shake; a pandemic might sweep across nations—but babies still demanded to come out into the world. What a world that would be. I marched into my post, armed with my duty bag slung over my shoulder, and lunch for sharing in a paper bag. The rest was routine. We start with an interview, and if we are lucky, we end with a newborn baby’s strong cry. We were lucky twice that day, and baby number three wasn’t due until late afternoon. Storms might gather; the earth might shake; a pandemic might sweep across nations—but babies still demanded to come out into the world. The clock read eleven, but hungry stomachs do not recognize clocks, especially when your resident brought donuts for sharing. Oh, and I still had my three pieces of siopao. Between sweet and savory, we felt full enough to delay lunch. Perhaps, we would save the curry for an afternoon snack. What we did not know was that lunch made the trip from the Pediatrics Ward all the way to the labor room pantry. “Uy, kain kayo o,” our friend said as she placed the set of meals on the table. “Marami pa daw sa baba.” Our not-so-hungry stomachs could smell the soy chicken inside. “Saan ‘to nanggaling?” we asked with not a small amount of glee, already opening up the plastic spoons and forks. “May nagdonate daw.” 25 All was quiet in the labor front. The only thing making noise was our instant messaging apps. A message from the class president - [N95 MASKS1 FROM DEAN CHIONG FOR INTERN VOLUNTEERS] - appeared on the notifications. I swiped it away—perhaps later, when we were off duty. A little while later, there was another ping from the group chat. Another set of donated food. This one came with a picture taken right at the main entrance of PGH. I showed it to my co-intern. We shared a laugh. I swiped it away again. Ping. Another set of donated food at the DEM callroom1. Ping. A different set in the IM callroom, in case anyone still hasn’t had lunch. Ping. Ping. Ping! The group chat read like an SOS. “Who else hasn’t eaten yet?” “Have we given the residents?” Yes. “Have we offered the nurses?” Yes, and they’re also offering more food. “The nursing assistants? The manongs? The guards?” Ping. Ping. Ping! Flash pictures of foods lined up in stacks. Some of them come with selfies and what are likely happy smiles beneath face masks. We start telling each other to have dinner in PGH instead. Bring some home for tomorrow too. We never did get to eat the curry I brought over. Instead we were given another meal set. “Ilan kayo dito?” Count two volunteer interns, plus one pedia resident, and four nurses. For a total of seven more burgers. A tray of chicken karaage would come in later. I marched out of my post, my duty bag heavier with the extra food that was given, and my heart so much lighter. My duty mate and I stopped by the pedia wards before we went home. “Magbigay tayo ng food sa mga street children,” invited our friend. There were still some sets of soy chicken from lunch. That day was just the beginning. The hospital was more overwhelmed with preparations than with COVID patients. This was the water receding before the crash of the tsunami, and the three of us knew it as we walked home. The street children who used to play in the area were nowhere to be found. But there was always someone to help, and we found him in an old man standing on the sidewalk. “Pang-hapunan niyo po.” That day, I felt like I witnessed a miracle. Someone took a piece of bread, and tore off a bit to give to another. And another. A piece of fish here, and another for you. Somehow, five loaves and two fish became lunch, dinner, and maybe even breakfast for the entire hospital. At the end of the day, I prepare a table before me; my cup overflows. Copyedited by Amanda Christine F. Esquivel 26 1 See glossary. Thanks to the donors and patrons of PGH, many of the hospital staff have received a steady supply of food since the start of the pandemic. Photos by Janel Verceles, Edmond Bries, AJ Limbago, and Markyn Kho. 27 If Robyn Gayle K. Dychiao Another day, another meeting. While the Philippine General Hospital director, Dr. Gerardo “Gap” Legaspi, attended multiple meetings on a daily basis, this particular gathering held heavier implications. In attendance with Gap were Department of Health officials and other hospital directors, all anxiously aware that the pandemic has taken hold in the country. It was time to ally and prepare for battle. What if we appoint centers that can take in severe and critical patients, while other hospitals focus on testing and regular operations? Gap had been mulling over the idea of a dedicated COVID-19 hospital, just like what was done in China. Many hospitals in Metro Manila still had ample time to get this running; surely, someone here will set off to repurpose their respective facility. As Gap brought this up, the officials jumped at this idea and exclaimed, “PGH lang may kaya niyan, ikaw na!” Gap was taken aback. It was a mere suggestion; the prospect of PGH being on the line did not even cross his mind. It couldn’t be, as PGH’s patients relied on its specialized services—which would be less accessible or unavailable elsewhere. The hospital was also in the midst of its own little battles: the sheer volume of people lining up daily at the out-patient department, 28 1 See glossary. severely-ill patients in its temporary emergency room spilling into the corridors, and operating rooms running round-the-clock to make a dent in the unending queue of patients needing urgent surgical interventions. Gap’s job as director was a daily affair of putting out fires, and in PGH, there were many. Converting an already complicated entity into a singular COVID-19 referral center will only sink PGH to the deepest of trenches. The PGH was, to put it plainly, not the hospital of choice. Gap ended the discussion without a clear answer and said that he would propose it to the UP President. In the days that followed, a sense of normalcy pervaded the PGH. The Out-Patient Department (OPD)1, Cancer Institute1, and operating rooms were bustling with the usual overflowing number of patients. However, the veneer of the routine was also perceptively giving way. Like a fog creeping in to blur what was in sight, there were rumors spreading of PGH becoming a COVID-19 referral center. Was PGH the first pick? It’s not true until Gap says it is, everyone thought. The hospital’s slow progress can only be reversed with such a step. And even if Gap did say yes to this, could the hospital hold together for the duration of the pandemic? Thus far, nothing had been officially announced by the hospital’s officials, yet news outlets already started to banner PGH’s taking on the role. Residents’ 1 phones rang with calls from worried parents, telling them to come home immediately because PGH was about to be a warzone — where the virus moved as a wayward bullet, and everyone was fair game. New schedules for the staff were being rolled out each day, and some patients were transferred to other hospitals for no apparent reason. More days passed, and the strident rumors simmered down to an eerie silence. Suddenly, a hospital normally bustling with passion and fervor felt cold and uncertain. In the middle of this usually busy hospital lies the PGH Atrium. Tucked in the corner near the atrium is an unassuming doorfront, the director’s office. Its shut doors masked the chaos in Gap’s mind. The noise from the outside was no match for the cacophony of thoughts that preoccupied him in making this crucial choice. PGH Director Dr. Gap Legaspi is interviewed in front of the administrative offices. Photo by Brent Viray 1 See glossary. Could the PGH structures truly handle this? The emergency room was far from complete; its renovation would have to take a backseat. Gap would need to orchestrate a herculean effort to re-engineer wards. PGH’s usual practice of fitting as many patients in need of care as possible would no longer be appropriate for COVID-19 cases. PPEs, ventilators1, dormitories: how 29 was he going to acquire these in a week to provide for his staff? As much as PGH was not ready for the change, its patients also stood to be jeopardized by the transition. Every year, 40,000 patients come from all over the country to line up in the out-patient clinics. Each month, some 2,500 cases underwent a plethora of surgical procedures in its many operating rooms. The 1,500 in-patient bed capacity has never been enough to accommodate all those in need of in-patient care. People depending on PGH will lose these vital services. Was this really worth it? Everything and everyone seemed to be going against PGH becoming a COVID center; Gap felt pushed against the wall by dissent. Clamor from his colleagues filled his inbox, “What will happen to the residents?”, “The ER is not even fixed yet!”, “Why are you doing this?” There were a few who were on his side, but Gap still felt like the universe was conspiring against him. Then the lines from a timeworn poem of a father to his son came back to him: If you can keep your head when all about you Are losing theirs and blaming it on you If you can trust yourself when all men doubt you But make allowance for their doubting too 30 (From L-R) Dr. Kenny Seng, Dr. Hermogenes Monroy III, and Dr. Orlando Ocampo meet in the Director’s Office to discuss the PGH COVID strategy for the months ahead. Photo by Alvin Caballes What was most at stake was the health and well-being of the people who trusted him. He was taking a leap of faith for 4,000 people. 4,000 lives. ill COVID-19 patients, it would hold off the usual flood of patients and buy the hospital some time to regroup and reorganize. And Gap knew that unspeakable things could happen with a virus as unpredictable as this. Along with the physical risk of treating COVID-19 patients everyday, the mental struggle to stay “resilient and resourceful” could aggravate pent-up frustration in the frontliners. None of them were dispensable. The rising number of COVID-19 cases spoke for itself: someone will catch the virus in due time. Again, the poet’s words filled him: If you can dream—and not make dreams your master; If you can think—and not make thoughts your aim; If you can meet with Triumph and Disaster And treat those two impostors just the same If someone didn’t make it out alive, he acknowledged that he would have to resign as director. The risks, the consequences. All these he weighed, as much as these also weighed on him. For above all these considerations was the institution’s avowed duty to the nation. PGH prides itself in caring for the underserved, and this new formidable enemy has placed all Filipinos in universal suffering. There had to be a concerted effort against COVID-19, and the PGH would not shirk from this responsibility. Hindi puwedeng hindi. This was for the greater good — “the right thing to do.” And so, Gap took the first step for the transition. Yet there was an overriding thought. When the need for action superseded all else, how could PGH say no? Gap akins COVID-19 to a war. The PGH was being recruited to battle in the country’s fight against an invisible enemy. Private hospitals were just as eager to help PGH, with the promise of equipment and facilities if—once—Gap said yes. A “rare moment of solidarity”, indeed. Gap also thought this could be a good tactical move, putting PGH two steps ahead. By being the referral center dedicated to treating critically On 26 March 2020, Gap wrote “People Giving Hope1”, a communique that defined the hospital’s new role, vitiating the nascent uncertainties. The choice was made for the patients, who trusted in the institution. For colleagues who had passed on. For professionals and workers who have yet to rise to the challenge. For the students of the UP-PGH, so their aspirations can find their way into action. The resilience and resourcefulness of all would be put to the test, but Gap was counting on everyone to pitch in, and, together, overcome the adversary. How many people will Gap need to lose before realizing this was a mistake? 1 See glossary. 31 The PGH COVID Command Team shows its support for the hospital workers at the newly renovated PGH Atrium. Photo by Jonas Del Rosario 32 The official announcement for the hospital’s new status came five days later. But this was almost taken for granted, as frenzied preparations were long underway. The on-ground physical transformation was sweeping and extensive. Adjacent wards were re-engineered to provide ICU care for upto 130 patients. An armada started to take shape, assembling and orienting the best soldiers, filling its war chest with armament and supplies, and optimizing communication strategies. Donations from the public poured in; six weeks’ worth of PPEs were collected in four short days. As Gap’s crisis team worked on the logistics, the frontliners honed their arrangements and procedures for patient care. Long-held divisions between medical specialties and service disciplines were set aside. Doctors, nurses, and allied health workers joined new platoons and researchers deployed as intelligence teams to search for effective treatments. If there’s one thing that COVID-19 has unveiled, it’s that mountains can be moved with a united front. The COVID-19 referral unit has become the new normal for the PGH staff. Nonetheless, there remain nagging issues. Was anything missed? Were the wrong choices made? How many more patients with COVID-19 will come? What about the other patients? The contagion continues, but a hospital director’s vision proved to be more infectious. Despite all the trepidations, the PGH, through the sheer dedication of countless individuals, perseveres and slowly rises above the fray. For critically ill patients, disheartened families, imperiled communities, and a desperate nation, it has become a beacon of hope. If you can force your heart and nerve and sinew To serve your turn long after they are gone And so hold on when there is nothing in you Except the Will which says to them: ‘Hold on!’ Soon enough, everything fell into place. And the patients came. Copyedited by Gabrielle P. Flores 33 The Medicine and Surgery wards of PGH prepare their facilities for the COVID patients. Dr. Regina Berba, chief of the Hospital Infection Control Unit (HICU), and Dr. Rodney Dofitas, Dr. Carmela Lapitan, and Dr. Dione Sacdalan of the Department of Surgery, brief the staff on the new protocols for managing patients and layout of the wards. All around the hospital, plastic barriers are installed and COVID signs are hung, a stark reminder of the crucial role PGH was about to take on in this pandemic. Photos by Brent Viray. 34 Musings from a Pulmonologist at the Frontline Jubert P. Benedicto On March 16—also my daughter’s 11th birthday— the Luzon-wide ECQ (Enhanced Community Quarantine)1 was suddenly declared by Malacañang. We were all caught off-guard, since the Metro Manila community quarantine had just been announced four days prior. I never thought that these three letters could forever change the way we work, think and, ultimately, live. Confusion, and a feeling bordering on panic, gripped me while I was driving home with my daughter’s cake (which she specified to be chocolate with moist icing) and her favorite bucket of chicken. Along the way, my wife and I were hearing disheartening news from the radio and hopelessly watching the chaotic traffic and commuter surge outside. Earlier that day, PGH Director Dr. Gerardo “Gap” Legaspi already floated the idea of the hospital being one of the dedicated COVID-19 Referral Centers for the National Capital Region. Unsurprisingly, he received a barrage of queries from the heads of the hospital’s various departments and units. These impassioned inquiries involved the physical set-up, the manpower needed, and our hospital’s general readiness to take on such a herculean task. Why did we even volunteer? PGH na naman? Paano na ang mga pasyente natin? Kaya ba natin? I lauded him for his composed answer then: “We can not afford to NOT play an active role. This will be so out-of-character for the so-called “mga iskolar ng bayan2.” However, it was hard to be comforted and encouraged at that point. I vividly remember the dread, an almost surreal, uneasy gut feeling, for what was about to come. The hospital was about to bear the brunt of a scourge, yet we will be relying not on firsthand knowledge or extensive experience, but on the little that we were able to gather from international literature. Was this enough preparation? The sheer volume of reported deaths, the alarming shortage of medical supplies, and even the rising number of afflicted healthcare workers in developed countries reported in the news were overwhelming enough. Eh, paano pa kaya sa PGH? As the head of all critical care units in PGH, I knew that a greater part of the burden for the care See glossary. Translation: Scholar of the People. Students of the University of the Philippines system are, literally, scholars of the nation as their education is subsidized, in part, by the government. But this title carries a heavier connotation— that of giving oneself to service to the nation. 1 2 35 of these severely ill individuals will eventually and inescapably fall on my shoulders. Even at the time of this writing, COVID-19 remains a clinical enigma. Much of what was known about it, in terms of pathophysiology1, diagnosis and management1, was tentative or inconclusive. However, the hospital simply could not wait for the clouds to clear. We were tasked, right away, to prepare for this unseen, poorlyunderstood enemy: assessment of potential intensive care areas1 in the hospital, crafting of ICU policies and workflows, preparation of all ventilators1 for deployment, and writing a “wish list” for procurement of relevant institutional needs and wants. Dapat meron sa charity1. Dapat meron sa pay. Teka lang, matutuloy ba talaga ito o plano pa lang? The next few days were for the books. We bore witness to the fast-paced and unprecedented turn of events we never thought possible within the lumbering institution that is PGH. We suddenly had wards converted into ICUs. Our established medical and surgical intensive care units were transformed into facilities for confirmed COVID-19 patients. Workflows were established, which included the strict personnel adherence to a “one way” route in and out the ICU. PPEs1 were stockpiled. Complementary manpower was made available. All clinical departments contributed their residents1 to the frontlines, with their consultants1 on board and ready. ICU equipment were prepared, including mechanical ventilators with advanced modes. Donations of various forms from all over the country flooded PGH. 36 1 See glossary. Naku, wala na talaga akong lusot. Trabaho na! The first challenge was to get everyone on the same page. Admittedly, this was easier said than done. We were navigating uncharted and tempestuous waters, and fear and anxiety were palpable. I have to admit that I was also scared— scared because of the many “what ifs” and the lack of reassuring answers on sight. We really did not know how to beat this unseen enemy. And, ultimately, I did not want to get sick. I wanted to be with my wife and children in such trying times. Each time I encountered trainees, nurses, and paramedical personnel, especially during preparatory meetings, I made it a point to put on a firm demeanor. While we shared the same concerns and fears, they were more candid. “It seemed unfair that we did not have a choice,” was one of the tearful yet unsurprising sentiments shared in these meetings. Kami kasi yung nasa ICU… pinili namin ang ganitong buhay. In an attempt to give solace to my co-workers, I would always go through my list of supposedly assuring statements: “PGH will always equip us with adequate PPE”; “Remember, you will have days off just to rest and monitor yourselves for any symptoms1”; and, “We designed our workflows and policies so that contacts with patients will be reduced to the minimum possible.” Until now I honestly do not know whether these words achieved their purpose. I always end the meetings by saying my personal source of encouragement: “Let us just pray and ask God for strength, protection, and direction.” I clearly remember my first day of being thrust to the wards and the emergency complex to attend to the suspected and confirmed COVID-19 patients with my fellow1. I was meticulous with how I donned my PPE— following the posted checklist and reviewing at least twice to see if I did everything correctly, even under the supervision of the safety officer. Mahirap nang malusutan. The first patient I saw was an enthusiastic elderly female diagnosed with a blood dyscrasia, suspected to be infected after suddenly becoming short of breath in the wards. I felt that the pressing symptom was more attributable to her underlying anemia3. She was trying the whole time to strike a cheerful conversation as I attempted to double check the progression of her symptoms. Each time I paused, she asked friendly questions. What province is my family from? Do I know her physician granduncle? I answered her with short phrases, in adherence to the dictum that we spend only the minimum necessary time with our patients. While I tried my best to do a physical examination, it was made extremely challenging with the double layer of gloves 1 3 and the hood covering my ears. The dripping sweat and the fogged goggles added to the discomfort. I eventually placed a pulse oximeter1 on her finger, which registered an oxygen saturation1 reading of 92%— low for someone already on supplemental oxygen via face mask. However, instead of moving on to the next patient, I found myself looking back at her. Instinctively, I proceeded to answer all her previous queries. I even asked if she wanted me to call a family member so I can give them updates about her. She just smiled and thanked me for the thought. I could not purge the value of being humane. I have imbibed this through lifelong training—to see patients as individuals first and foremost rather than mere cases of clinical interest. This virus, unrepentantly, was compelling us to be substandard, uninvested healthcare workers. We simply should not let it do so. My realization right then was that one must really be conscious of one’s conduct during these encounters. There should be mindfulness and compassion for each and every patient. Hindi pwedeng sugod lang nang sugod. See glossary. A blood dyscrasia is a non specific term that refers to diseases of the blood and its components. When it affects red blood cells, it can cause anemia in a patient. This anemia may manifest as sudden shortness of breath, which may be confused with the symptoms of COVID-19. 37 Photo by Brent Viray Subsequent days became quite routine: morning endorsements1 followed by short discussions with fellows before doing rounds1. All these should be done by 11:00 a.m. since laboratory and imaging requests1 will be carried out right after. Meals from the dietary department and donors were welcomed in between. We were all, fortunately, becoming more accustomed to routine donning and doffing of PPEs. Donations provided some needed emotional boost. They also strengthened the belief that this pandemic—as with any calamities and disasters in the past—brings out the generosity that Filipinos are known for. I really treasured the prayers, the letters of support, and uplifting messages I regularly received through various social media platforms; a great number of these were from people I have yet to encounter in person. We were striving to achieve a sense of “normalcy” during this global crisis through telemedicine1 (that we had to get a hold of quickly), Zoom1 meetings (which are the bane of my existence), and myriads of webinars. Nevertheless, it was really challenging to attend to all these affairs, let alone concentrate on one, considering that we were always on our toes to manage afflicted individuals. It did not help that we were leaving them, at least partly, clueless on what we could further do. The apprehensions stayed with us, and the thought was always there; Did I miss anything? 38 1 See glossary. BREATHE, PRAY, MAKE ROUNDS, REPEAT. The unease remained even after I had left the hospital. Though exhausted, I struggled to fall asleep at night. I seemed to have become fully dependent on melatonin tablets4 to ease the effort. I found myself checking my mobile phone for messages at least once every hour out of concern of missing any urgent referrals1. These trepidations doubled when we started admitting and caring for our own colleagues. Referral to our service1 was not exactly reassuring. It was, more likely than not, a harbinger of clinical deterioration1 necessitating further intensive care. While we had protocols to guide us, my faith in their soundness was shaken when I saw familiar faces, not as co-workers, but as patients: Were these guidelines updated? Do they offer the best options? I tried to separate my role from being their physician-in-charge to my attachment to them as a co-worker by being objective as much as possible. This was difficult though. I could not help but pause a little longer at their bedsides and engage them in some light conversation or communicate with a few extra written words written on whiteboards. I was also the bearer of cherished good news, and dreaded bad news, to their family and friends. Inevitably, not all would recover. There would be colleagues-turned-patients who, all too aware of the downturn, still expressed their gratitude for having done your best for them. The comfort would be fleeting, overshadowed by the moment of passing that would inevitably come. There is a pause, a brief time to reflect on the struggle, the seemingly senseless situation, the futility of the cards dealt by the universe. I soon push these aside, and I move on. We learned and are still learning our lessons. We take good notes and apply what our previous patients selflessly taught us to the next. We give our best, wherever we are, with whatever we have. Despite all the odds, we valiantly pursue our goals. I firmly believe that, when the dust finally settles, we will be victorious. At the moment, we can just BREATHE, PRAY, MAKE ROUNDS, REPEAT. Copyedited by Aedrian A. Abrilla 1 4 See glossary. A supplement that improves an individual’s sleep (i.e.commonly used for insomnia, jet-lag). 39 Shifting Gears Lily de Amor Life in the fast lane. That’s the title of a wellknown website covering all things emergency medicine. As an emergency medicine consultant1 at the UP-PGH, it’s a fitting description for my life and my job, too. In an environment where a successful outcome is sometimes defined in seconds, the ability to think and move fast is essential. We aim to put order into chaos every time we step into the fast-paced, action-packed world of emergency medicine. This hectic pace became even more pronounced when the pandemic started to hit in late January this year. For the first few weeks, there was little sleep to be had as we poured our time and effort into developing plans, guidelines, and protocols, as well as dividing the responsibilities that came with them amongst ourselves. It was during these times that keeping one’s head above water took more effort than it usually did. Does this patient have COVID? Should I do chest compression? Is it safe? Should I intubate3 this patient? Would it be safe? Am I wearing the appropriate personal protective equipment? Would I be safe? How do I tell the family that the prognosis for their loved one is poor ? See glossary. Triage. Identify. Treat. The Emergency Department is not a first come, first served system. Most people who arrive in stable condition would need to wait for some time. The ED is designed to zero in, instead, on those who stand at death’s door. Because when the clock starts ticking, it is the ED’s resuscitation team that reels them back to life by treating the long-established ABC’s of emergency. (Airway. Breathing. Circulation.) 3 If a patient cannot breathe properly by themselves, the resuscitation team may place a flexible plastic tube into the windpipe to push oxygen straight into the lungs. If a patient’s heart stops pumping, the resuscitation team may start chest compressions in an attempt to get the heart beating again. Unlike in the movies, these attempts do not always succeed. Sometimes, if the patient came in because of a respiratory virus, this may expose the resuscitation team to contamination risks. 1 2 40 Though most of us working in the Emergency Department (ED) are trained to adapt to any situation that could come our way, this public health emergency has pulled us in every direction. What used to be a straightforward set of actions – triage, identify life-threatening emergencies, and treat2 – now seemed to be inadequate for dealing with the issues and concerns that came with managing patients with COVID-19. Whereas before, a dying or dead patient arriving in the ED would immediately kick the resuscitation team into action, this time there’s a perceptible pause. What used to be an emergency physician’s automatic response was now punctuated with questions that would come in rapid succession. During this time, patients in critical condition, and even some who had already passed away, were arriving at the ED in a constant stream. When I look into the eyes of our young colleagues, the only parts of their face visible under the protective gear, I try to gauge their emotional state. With the constantly changing hospital protocols and the difficult decisions to be made, it was easy to get lost in this COVID storm. But I find a different kind of fighting spirit in them. For still they possessed the desire and determination to fight for their patient right up to the very end. But now, their spirits are tempered by the realization that there may be times that the best decision for their patient is to hold off aggressive management1 when deemed futile, and let go. This scenario has become more and more commonplace in this crisis, and it has started to take its toll on our mental health. When there are more questions than answers, even just a single patient encounter can be emotionally draining. Then, in March, the community quarantine1 was implemented. Suddenly, the world became quiet. Things moved more slowly. The ED drastically shifted from what has always felt like a motorcycle weaving through rush hour traffic to a more sedate state. There were still outbursts of activity, such as when a vehicular crash patient with multiple injuries, a person experiencing chest pain, or a COVID positive patient whose condition deteriorated during transport from another hospital arrives and is 1 See glossary. rushed inside for resuscitation and stabilization. Less and less of the “regular” ED patients were showing up. What used to be a crowded, noisy hospital unit, with the number of patients exceeding its capacity many times over, then became a strangely peaceful place. One warm day in March, I found my way to the hospital parking lot where tents were set up for the purpose of swabbing COVID suspects1. By the time I got there before the evening duty, the place was deserted. There were no more patients, and the health care workers assigned to the post had already left. Without the cars, the place looked pretty, like a patch of a welltended city park. The ground was dotted with the tiny, bright orange flowers from the narra trees, seemingly an invitation to take a break and bask under the late afternoon sun. Feeling the accumulated weariness of the past weeks, I sat on a plastic bench, enjoyed the light breeze, and allowed myself to relish in the tranquility that was so at odds with my state of mind. I have since developed a routine that has served to fulfill my simple needs during this period. I now walk the distance between my place of residence and the hospital. The twenty-minute walk twice a day has been wonderful for my physical and mental health. Walking forces me to be in the moment and allows my mind and soul to relax. It has become the highlight of my day. I’ve always enjoyed climbing, hiking, and running. But now I’ve been given an opportunity to enjoy walking without having to deal with the bustling crowd and the terrible air pollution. 41 I have also been able to reflect more on the role of emergency medicine in the overall health crisis. It is often said that the ED is the safety net of the community’s health care system. The pandemic has highlighted the need for emergency physicians like me to take on a more active role in public health through engagement with local health authorities and agencies involved in managing emergencies and disasters. There is a need to sit down with public health experts and discuss areas for cooperation. The integration of preparedness and response plans, along with community involvement, will enable us to be more ready to meet the major challenges to the health care system, such as what this major crisis has presented. The extended community quarantine period will soon end. I don’t know how the “new normal” will look and feel like. I love my work as an emergency physician. I’ve enjoyed living in the fast lane. But I now know that I have more to offer beyond serving at my chaotic, crazy but comfortable second home, the emergency department. It is time to shift gears. Photo by Brent Viray 42 When Nightingales Cry Paulo Ross B. Sison “Meron daw sa 5th floor.” It started with rumors that one of the pay floors1 was catering to a COVID-positive patient. Hearsay of the first known case entering the hospital premises brought chills down our spines. Half-joking threats of early retirements and AWOLs were heard in staff rooms when the prospect of PGH being converted into a COVID referral center1 was brought up. Given the quantity and spectrum of patients we had to deal with on a daily basis, we were confident PGH wouldn’t overhaul its current structure. If we had to handle COVID cases, we were certain that, at most, only a ward or two would be allocated. “Hindi yan aabot sa atin. Paano na lang mga pasyente natin?” We had never been so wrong, as I soon realized one Friday afternoon. I was almost done with an exhausting eight-hour shift, and I was preparing my logbook for endorsements1 when our chief nurse called for 1 2 an emergency meeting. One of the wards would be converted into a COVID Unit and every Chief Nurse had to turn in one nurse to the Unit’s staffing personnel. “Bawal ang may-edad. Bawal ang may sakit, lalo na sa baga.” I wasn’t that old. I’m actually one of the younger members of our staff, but I have asthma, so I never thought I would be inside the head nurse’s office, being told that I would be our chief nurse’s ‘alay2’ to the COVID Unit. “Mahirap mamili sa staff ko pero sana maintindihan mo bakit ikaw ang pinili ko.” Oddly enough, the shock didn’t register then. It was only when I started erasing and rewriting notes in my logbook, hunched over the nurses’ station tables, that I felt a creeping sense of unease. Suddenly, it hit: the idea of being in direct contact, albeit in complete personal protective equipment1 (PPE), with COVID patients was becoming less illusory. It was now real. See glossary. Its literal English translation is “offering” or “sacrifice”. Duties in the COVID unit are necessary, but always accompanied by dread that created no pool of willing volunteers. But someone has to be chosen; someone has to make a sacrifice for these duties to be carried out properly. 43 The succeeding week was a blur. All the nurses sent by the chief nurses underwent an orientation on the COVID Unit – the unit’s physical set-up, a demonstration on donning and doffing of PPEs, and a debriefing to process our emotions. Many were afraid and anxious of their predicaments. Some were angry at being chosen. While a few were actually excited – a bright ray of light in the darkness enveloping our dear Pagamutang Bayan. “I know you feel fear. Anger. Anxiety. These are ALL valid feelings.” Since the Spine Unit1 was still undergoing renovations, we were assigned to augment the staff of the units already managing COVID patients—Ward 14A3 and 5RCB24. “Endorsing 10 patients. Nine PUIs, one of which is intubated1. And one COVID-positive.” On my first night as a COVID nurse, I was assigned to Mr. C, the very first COVID-positive patient of the hospital. Despite listening to the news and reading the latest updates on the disease, nothing prepares you for the first time that you have to face a positive patient. We were advised to minimize exposure, so I made a game plan. I would enter the room only once for my shift. In that period of time, I would do everything necessary in one patient interaction – getting the vital signs1, administering the medications, checking up on the patient, and giving patient education, among others. As the clock struck five in the morning, I donned my PPE, making sure that not an inch of my skin would be exposed. I prepared the medications, ran through the to-do list in my mind, and uttered a quick prayer. With a deep breath, I knocked on the door, announced my arrival, and swiftly entered the room. Mr. C was sound asleep. I placed my things on the table and as I tried to remember my to-do list, my brain just went… blank. Maybe it was the fear drowning my logic or the hypoxia1 even as I hyperventilated while wearing an N95 mask1, but I tried my best to snap out of it. “Deep breaths, Paulo,” I told myself, and my mind slowly cleared up. See glossary. A ward in the Philippine General Hospital that formerly housed trauma patients. During the renovation of the hospital’s emergency room, this ward was converted as part of the make-shift emergency room 4 An isolation unit in the pay admitting floors of the Philippine General Hospital 1 3 44 I approached Mr. C and woke him up to take his vitals, quickly assessed him, gave his medications, and instructed him to always wear a mask and ring us if he needed anything. In less than 10 minutes, the brief patient interaction was over. But I trembled as I doffed1 my PPE, praying to the highest of heavens that I had followed each step correctly. Mr. C used to be just a statistic in the hospital’s daily COVID census1 for me. Until that moment he became my patient. The following night, I was pulled out and sent to the emergency department which acted as a holding area for Persons Under Investigation (PUIs) awaiting disposition. Being sent to the ER on a regular, pre-pandemic day was stressful enough, let alone to an ER catering to PUIs. Given the high acuity of the patients in the area, we were advised to wear PPEs for the entire shift. This meant eight-plus hours of shallow breaths beneath a stifling N95 mask that offered maximal protection but minimal comfort; a limited visual field as my breath fogged up the safety goggles; no water in and no water out; (not so) insensible losses via the sweat that drenched me from head to toe; and mumbled prayers of staying strong and keeping it together. Monitor1 patients at bedside. Administer medications. Answer questions left and right. Rinse, wash. Repeat. “Sinulit mo naman ang relieve mo sa amin, sir.” We also had to attend to a patient who went into cardiac arrest twice that night. The patient passed away, but I was still on duty1. I proceeded with the post-mortem care, a procedure so routine, I could do it with my eyes closed. Suddenly, I felt a stream of tears silently run down my cheeks. I was startled. I had always kept myself strong, able to keep my emotions at a distance, as well as professionally console the bereaved. But at that moment, the emotions overcame me, and I realized that I was but human. I let the tears flow, and it was I who needed consoling. “Magbubukas na ang COVID Wards.” Copyedited by Gabrielle P. Flores 1 See glossary. 45 Photo by Brent Viray I realized that I was but human. I let the tears flow, and it was I who needed consoling. 46 47 48 Photo by Jay Almora DISEASE 49 50 Disease /di-’zēz/ n. A condition that impairs the normal functioning of a living organism, and is typically manifested by distinguishing signs and symptoms. Inch by inch, the pandemic has begun to morph the familiar. Fear, doubt and uncertainty lay in the background as the Philippine General Hospital transforms into the COVID-19 referral center it was promised to be. Changes are being made at a feverish pace, and, from illness or demands of work, PGH patients and staff feel increasingly short of breath. Duck, jab, sidestep - the battle is in full swing. 51 A Battle of Silence Cary Amiel G. Villanueva The Philippine General Hospital (PGH) is no stranger to war. During the Second World War in 1945, its walls stood firm as shelling and savage fighting broke out when desperate Japanese troops refused to give ground to determined American forces. Thousands of patients, workers, and refugees sought shelter under its roof1. Seventy-five years hence, the hospital is once again in the middle of another historic struggle, this time against the COVID-19 pandemic. But unlike the Battle of Manila2, which was fought with bursts of gunfire and the din of explosions, the present war against the coronavirus only has deafening silence. We didn’t know that the Department of Health (DOH) had assigned PGH as a COVID-19 referral center until our relatives and friends told us about this being announced in the news. It took days before the hospital administration communicated this officially to the staff and employees. Silence in the wards Any medical resident, intern, or clerk3 would know that Wards 1 and 34 are almost always full, as patients would keep flowing in from the Emergency Department. Yet in a matter of days, the wards and intensive care units3 were totally vacated. The everyday sounds of ventilators whooshing, monitors beeping, and patients coughing were suddenly gone. Dr. Honorato Quisumbing, was a medical intern who continued to work at PGH during World War II. He was shot and killed on February 17, 1945, while trying to get water from a bomb crater near the Cancer Institute. On the same day, the PGH was liberated by American forces. Today, a residential dorm for PGH staff is named in his honor. 2 The Battle of Manila lasted a month and was one of the most destructive urban campaigns in the war. In an attempt to finally retake Manila from Japanese occupation, the American and Filipino forces clashed with the Japanese troops in the city’s densely populated streets, resulting in thousands of military casualties and over a hundred thousand civilian deaths. Entire city blocks were levelled, resulting in the loss of innumerable architectural and cultural landmarks that were part of the nation’s national patrimony. 3 See glossary. 4 Wards 1 and 3 served the patients of the Department of Internal Medicine. Prior to being a COVID Referral Center, these wards had a combined bed capacity of over a hundred and catered to adult patients with diseases ranging from the more common infections, to rare and difficult to diagnose and treat entities. 1 52 Silence in information The Philippine General Hospital (PGH) is no stranger to war. Dr. Jairus Cabajar stands among empty beds in the Medicine Ward as the Philippine General Hospital prepares its staff and facilities to be one of the COVID Referral Hospitals in Metro Manila. Photo by Jairus Cabajar 53 Silence among comrades Reorganizing the workforce into teams coming in for duty1 once every three weeks meant that fewer doctors, nurses, and other personnel could care for patients. The reduced staffing served to add lines of defense, sparing others from exposure. But this meant that many colleagues who had become close friends and confidants would not see each other for weeks, likely months. The usual banter was no more. Silence inside personal protective equipment1 (PPEs). The several layers of full-body protection that we had to wear in the COVID-19 areas made everything more challenging: walking, writing, sitting, and typing. Hearing and being heard became difficult. We have learned to listen to our own thoughts during most of the shift. Silence at home. After doffing1 the PPE and being relieved from duty, one left work in solitude. In order to protect their loved ones, many were forced to make arrangements to live alone. We retired to our own solitude. Copyedited by Amanda Christine F. Esquivel and Gabrielle P. Flores 54 1 See glossary. A Normal Day Viktoria Ines P. Matibag On a normal day, I would go to the hospital at 5:00 a.m. to do rounds1 on patients who were admitted under my service. There would be at least 10 of them that I would have to see. The three OB-GYN wards would be packed, each having at least 50 patients. During peak delivery season, there would be an additional 30 patients crammed inside a small, make-shift recovery room upstairs, waiting for available beds in the wards. I would make my way through the wards to see my patients, hoping for a smooth postoperative course so I could send them home. On a normal day, we would all go to Summary Rounds, which would start at precisely 7:00 a.m. Obstetricians-on-duty for the past 24 hours would endorse1 the cases that they had admitted to all the residents, interns, clerks, and integrated clinical clerks1 (ICCs). When the chief resident chose to probe your patient’s case, 30 minutes would feel like forever. On a normal day, the out-patient department1 (OPD) would be packed with hundreds of people, hoping for a chance to be seen by a physician. 1 2 They would fall in line as early as 3:00 a.m., some of them hailing from far-flung provinces. We would see around 50 new patients in the morning before we checked on our follow-up patients in the afternoon. Lunch breaks were a luxury. Patients who braved the sweltering heat in uncomfortable waiting areas would be seen only for ten minutes, in order for us to accommodate everyone before 5:00 p.m. On a normal day, the OB Admitting Section2 would never rest. Patients would come in one after another. For many of them, it would be their first time setting foot in our institution. “Saan po kayo nagpapacheck-up?” the OB Admitting Section resident would ask. The answer would almost never be PGH. Still, there would be a shopping list of responses on why they came anyway: inadequate local facilities, financial constraints, or a complete naivete to prenatal check-ups. We would admit around 20 patients daily, regardless of their financial status. They had gone to our institution because they had nowhere else to go, and despite the lack of manpower and facilities, we would take them in and ensure their safety. See glossary. The OB Admitting Section or OBAS for short is the emergency room of the Department of Obstetrics and Gynecology. While part of the bigger ER complex, it is practically a self-contained unit where the department receives its patients with obstetric or gynecologic emergencies such as a mother in labor or a cervical cancer patient with profuse vaginal bleeding. At the time of writing, the PGH ER complex was under renovation and the OBAS was temporarily located to ward 15 of the hospital. This makeshift OBAS has 6 beds, but usually serves much more, extending its capacity by accommodating patients on extra stretchers and benches. 55 Today is not a normal day. Tomorrow will not be normal as well. An OB-GYN resident and nurse deliver a baby in full protective gear inside the temporary OB Admitting Section (OBAS). Photo by Issa Matibag 56 On a normal day, the labor room would never be empty. The Labor and Delivery Room (LR/DR) complex has been under renovation for the past two years. Our makeshift labor room could only hold around eight patients, but on a normal day, around 10-15 laboring patients would occupy the room. Some would sit on monobloc chairs in the corner of the room, even if they were in labor. That was how crowded it was. It was neither ideal nor comfortable, but these mothers endured for the sake of their babies’ safety. On a normal day, residents who had just finished their 24-hour duty1 would be in the gynecology operating rooms (OR) to start doing elective surgeries1 on patients. We would be inside the OR until past midnight to finish operating on four or five more patients. It would be another long day before we could finally get some rest; however, our drive to improve our surgical technique and to help our patients would keep us going. Today, I don a bunny suit, an N95 mask, goggles, and a face shield1. It takes a while before I get myself ready to do rounds on patients. I waddle down the now-empty hallway of the Emergency Room to get to Ward 15, the one that used to house over 50 postpartum patients. Today, that same ward has only five COVID-19 suspects. Today is not a normal day. Tomorrow will not be normal as well. We have not had any normal days since the enhanced community quarantine1 started. Our wards have been emptied. Our labor rooms are silent. Our delivery rooms are unused. And today, I think about our patients. This pandemic will not stop these mothers from having complicated pregnancies. It will not stop mothers from having hypertensive or diabetic diseases that will need immediate care. It will not stop mothers from having preterm labor. It will not stop cancer from growing on women’s cervixes and uteri. The presence of the virus does not eliminate the other illnesses that we used to treat; yet, our patients are not here. Today, I ask myself: “Where are our patients?” Copyedited by Marcela Mercedes S. Rodolfo 1 See glossary. 57 Let Me Tell You About PPEs Ella Mae Masamayor Let me tell you about PPEs1, or personal protective equipment. I’m talking about Level 4 ones by the way, the kind we have to wear when we report for COVID ward duties. We’ve used up an awful lot of them as health care workers. I’m sure you’ve seen the seemingly unending stream of social media posts appealing for donations. Believe me, we still need every single donation we can get, so I thought it would be nice to shine a light on what they are and how we use them. Let me first clarify that I am by no means an infectious disease expert. I don’t know the answers to many technicalities. What I can and do intend to do, though, is walk you through the PPE experience. This is all new to me, too. I never imagined that I would have to wear something like this in residency. Yet here we are. First, scrub suits. We have to wear scrub suits before we don the PPE. No other outfit is acceptable. You can bring your own or use whatever hospital-issued scrubs are available (no guarantee you’ll get one that fits you though; today I got one that was three times my size). 58 1 See glossary. Photo by Alla Tan You have to bring a separate pair of shoes, too, worn only when in PPE. you put them on. Before I do, I always take a deep breath to relish the air while I’m still able to breathe freely. Before anything else, hand hygiene. You know the drill. 20 seconds. Over, under, and in between. Once it’s on, it’s goodbye to breathing normally. Next, we put on shoe covers. Yes, they are exactly what they sound like. Shoe covers. Don’t confuse them with your head caps, though, because they do look very much alike. Tape them to your shoes since they’re pretty flimsy and tend to fall off. If you want, you could add a layer of plastic after the shoe covers, just for added protection. After this, put on your first pair of gloves. This pair should never come off for the entirety of your shift. Up next is the bunny suit. It’s basically a thick plastic onesie. They come in sizes, and a good rule of thumb is to make sure that you pick a size that gives you ample room to move around. Even better, grab one a size higher than what you think is large enough. Trust me, you do not want an ill-fitting bunny suit. Get in and zip up. Just so you know, you’ll probably start to sweat at this point. The N95 masks1 come next. It’s not the first time I’ve ever had to wear them; we had tuberculosis patients on a near-daily basis before COVID happened. But I’ll be honest—I’ve never found these masks comfortable. They definitely serve their purpose of defending us against airborne infections and are a very, very scarce resource these days. Still, breathing becomes extra difficult when 1 See glossary. Goggles go on next. Goggles tend to make or break the PPE experience. It’s a given that movement of all sorts is difficult when you’re wearing the entire outfit, but not being able to see clearly is a whole other battle. On a bad day, goggles fog up to the point of zero visibility. There are anti-fog sprays to counter this, thankfully, but sometimes they fog up nonetheless. There are better days, sure, but even on those days don’t expect your vision to be crystal clear. Next, put on your head cap. If you’ve ever seen a shower cap, it’s pretty much the same thing. Again, don’t confuse the shoe covers for the head caps and vice versa. The bunny suit has a hood. At this point, you put that hood on. You strap on a face shield, too. And finally, you put on your outer gloves. Unlike the first pair, this one you have to change periodically each time you see a patient. Think of these as your disposable hands. Just before you go, the safety officers check your PPE. Thank God for them because like I said, all of this is new to me, and I sometimes get confused with the steps. They check if you’ve worn everything properly and tape you up in strategic areas to ensure that there are no breaches. 59 Photos by Isabel Acosta and Alla Tan Final touch: your name gets written on your bunny suit. Remember, when you go in, everyone will be in a bunny suit. Without names, it will be almost impossible to recognize anyone. Even with these makeshift name tags, sometimes I still end up talking to the wrong person. A printed picture of your face is optional, but definitely welcome. Patients like that. It makes them feel like they’re not talking to just spacesuits. 60 After all of this, you’re good to go. Congratulations, you are now an astronaut. I have no way of sugarcoating it: It’s hard in that suit. After I don the PPE on the ground floor, I head over to my assigned area on the second floor. Once I reach the top of the steps, I’m practically out of breath. When I get inside the ward, the work itself isn’t so different from what I’ve been doing before, but there are so many extra layers of challenges with the PPE on. We don’t get to use stethoscopes the way we used to, since the bunny suits cover our ears. We make do with whatever physical exam finding we can get from inspection and palpation. Pulses are harder to check. Blood extractions are harder to get right. My handwriting looks completely different. Even reading and replying to texts becomes a struggle. Come to think of it, sometimes it does feel like I’m an astronaut. Not in the childhood-dreams-reaching-for-thestars kind of way. I’m an astronaut in the sense that I feel alone, on an entirely different planet. In the PPE, even when you’re with your fellow astronauts, you still feel isolated. Distant. Voices are harder to hear and every touch never quite feels the same. Everything, and everyone, feels so far away. At the same time, there’s that ever-present fear for your own safety, as every breach in the PPE significantly raises your risk of infection. I’ve been doing this for close to two months now, but the anxiety never really goes away. Paige Lewis captured that anxiety so eloquently when she said: “I feel as if I’m on the moon listening to the air hiss out of my spacesuit, and I can’t find the rip.” (On the Train, a Man Snatches My Book, Reads) This still feels surreal, even after several weeks in. It feels like we’re a million light years from how things used to be. I’m trying to adapt to the fact that PPEs are the new normal for me, just as everyone else is struggling to find their own new normalcy; our own equilibrium through the constant change. I don’t know what will happen from hereon, but I hope we’ll keep finding ways to adapt, to carry on, to keep exploring what remains uncharted. In the meantime, back to the bunny suit I go. Copyedited by Caeley Lois S. Hao 61 Fish Out of Water: A Dermatologist in COVID Amanda Christine F. Esquivel It started out as a simple conversation. “This Coronavirus is getting out of hand,” one of my dermatology co-residents1 said one February morning. She was browsing her Facebook feed. It was half past seven, and we were enjoying a cup of coffee before the work day started and the deluge of patients and students arrived. “I know,” I said, sighing. I had just seen a report that China’s deaths from the Coronavirus had just exceeded those from SARS. “It’ll get worse.” “I hope not,” she said. “If it comes to the Philippines, we’re not ready.” “I don’t think any country is ready.” “May charts1 na,” our nurse called out with a smile, distracting us with a thick stack of patients’ charts. We residents shrugged at each other, and stood to begin our day. Our conversation was tabled, only to be recalled months later. Our friends from other specialties started drowning in work. Besides doing their usual resident duties of doing rounds1 and charting for the patient, they also suddenly had to carry their own orders out and monitor the vital signs1 of their patients—work that used to be done by clerks1 and interns1. The Department of Dermatology decided to volunteer and return to the emergency room to help in whatever way we could, through whatever way was needed. It hasn’t been an easy transition though, as some of us haven’t been to the ER— except to answer dermatology referrals1—in years2. “Does anyone have an automatic BP app?” one of my seniors called out. “Donated my pulse ox3 last year,” another replied. “Didn’t think I’d need it anymore.” See glossary. The practice of dermatology is largely out-patient based. They are usually in their clinic at the Out-Patient Department when they are not answering ward or ER referrals. 3 A small, portable, electronic device, clipped on to a patient’s finger to measure the oxygen saturation in an artery. 1 62 Looking back, I am stunned at what we were able to foreshadow. A simple conversation; a shot-inthe-dark prediction. When we talked two months ago, I never really thought it would come to this. 2 Doctor first and foremost. Dermatologist, next. “Where’s the ABG4 station now?” someone chimed in. “And where do we get ice? Bantay-antayan1 pa ba?” Eventually, things fell into place. The necessary monitoring materials were scrounged up, found buried in the back of our cabinets. Words of advice were passed on, with the first years informing the third years of how things were in the makeshift ER. Dermoscopes were traded for stethoscopes, skirts and heels for jeans and sneakers. As the first of us headed to the emergency room, we wished them good luck and jokingly said #dERma. The rest of us strove to pick up the pace to cover the work left behind. But that was only the beginning. When PGH was designated as a COVID center, we were called in to help man the triage5. Some of us were tasked to be Safety Officers for the COVIDcapable wards, but then, as the pandemic continued and the number of patients rose, we were reassigned as COVID ward residents as well. Through the humid and foggy layers of her protective gear, Dr. Mandy Esquivel writes down her orders and notes on the charts of COVID patients. Photo by Mandy Esquivel. It snowballs, one thing after another; every week the schedule and tasks keep evolving. Nothing stays the same for anyone, and everyone learns to roll with the punches. If this wasn’t what you signed up for, well, in the flurry of activity, you got over it fairly quickly. As triage officers, we abandoned Fitzpatrick6, our bible, to study COVID algorithms and their respective criterion and management1. See glossary. An Arterial Blood Gas (see glossary: ABG) requires quick processing (≤15 minutes) to yield accurate results; however, this quick turnover may not always be possible due to the sheer number of samples that need to be processed. As a precaution to prevent inaccurate results, ABG samples are put in ice before being sent to the lab. Ice can usually be bought at the sari-sari store next to the Bantay-antayan, a chair-lined area on the premises of PGH where watchers of ICU patients may rest while waiting for news. Currently, the laboratory that is dedicated to processing Arterial Blood Gas samples can be found on the second floor of the Philippine General Hospital. 5 Triage refers to the prioritization of patient care based on their illness/injury, prognosis, severity, and resource availability. A triage system enhances the efficiency and effectiveness of an emergency department. 6 Fitzpatrick’s Dermatology is a textbook that serves as the main reference for residency in Dermatology. 1 4 63 Guidelines changed weekly; everyone struggled to keep up. As safety officers, we mastered donning and doffing1. Mastering the reverse order was trickier, as doffing the suits carried a higher risk of contamination. As ward officers, we brushed up on pneumonia1, respiratory failure, and ventilators. “I’m studying ARDS7,” a co-resident told me. “We’ll probably be in the wards next week.” “I’m still a doctor, aren’t I?” Doctor first and foremost. Dermatologist, next. Early this year, in the midst of clinical and administrative work, we had prepared for exams in March, journal reports in April, research protocols in May, ward rotations in June. We had control over everything; everything had been scheduled and anticipated; everything had been prepared for. “Me too,” another said. “Never thought I’d have to think about mech vents again. Do you guys remember anything about PEEP and tidal volume?8” But then everything changed, and I was not prepared anymore. We were not prepared. And while no one being prepared can be terrifying, it is also, surprisingly, a comfort. Because no one is prepared, we struggle together. With so many unknowns and so much work to be done, all we know is that we appreciate everyone who is willing to step up. This question was met with blank silence, and we broke into laughter. Humor helps us face the uncertainty. Never mind if this is not our comfort zone—this pandemic is no one’s comfort zone. At home, my father came across me reading my internship notes, and stopped to read over my shoulder. “Cardiac arrest?” I shrugged helplessly. “You never know.” I have since put aside that I am training to be a dermatologist. I am willing to bet that my colleagues from other specialties have learned to put their specialties aside as well. Perhaps one of my friends said it best: “We were all doctors before we became specialists.” People ask me how it feels to be a dermatologist called in to help with COVID. The answer is bewilderingly simple. And so, all of us who call ourselves doctors, all of us who are licensed to heal, step up. Copyedited by Sachiko S. Estreller See glossary. ARDS. Acute Respiratory Distress Syndrome. 8 Positive end-expiratory pressure (PEEP) and tidal volumes are commonly manipulated parameters on a mechanical ventilator. Dermatologists-in-training don’t often use these parameters as the patients they treat rarely need mechanical ventilators. 1 7 64 Second Wind Erika P. Ong If this is it, Lord… game na. This was the thought in Peejay’s mind whenever he, still hazy from the medications, surfaced back into lucidity. With his body too weak to form words, these thoughts were confined to his own head, echoing when he was conscious enough to think about his condition. Peejay was 50 years old, working in a BPO, and was in generally good health. He exercised regularly, and did not take any maintenance medications. Nevertheless, when there was news that one of his colleagues could have contracted COVID-19, he chose to err on the side of caution and went into a self-imposed quarantine1, isolating himself from his family. Initially, Peejay’s symptoms1 were very mild: only a low fever. After five days, however, COVID-19 slowly reared its ugly head. When his temperature spiked to 38.5 degrees Celsius, a physician friend advised him to seek consultation. Peejay remembers panting in the shower as he prepared to leave for his checkup. This was when he felt the first tendrils of fear that he had been infected by COVID-19. 1 See glossary. After getting blood tests and having a CT scan done, Peejay returned home. Breathing gradually became more difficult. He was brought to a hospital in Quezon City, where, from thereon, everything happened quickly. A swab later confirmed that he had fallen victim to the virus. His health rapidly deteriorated. However, despite being barely conscious, he was still able to convey his abhorrence to being intubated1. His doctors had advised this, which he knew would be a horrifying experience. His family pleaded with him to reconsider this option. With his family’s pleas, his doctors’ urging, and his awareness of his own physical weakness, Peejay, with trepidation, finally agreed to intubation. For the next two weeks from then, Peejay was completely under. He barely remembers anything that transpired, but he heard the stories from doctors and family: of him being in such a critical state, of his family being told to prepare to let go, of his unconscious self clawing the tube out of his own throat not once, nor twice, but four times. Amidst the merciful drug-induced haze, he thinks he remembers a glimpse of someone in his face, screaming, “Sir, you have to cooperate!” 65 Though Peejay’s memories during these critical two weeks were, for the most part, blank, he remembers brief moments of consciousness, waking up to pain and the constant incomprehensible medical chatter. He just thought, “I am going to die.” After two weeks, Peejay recovered his bearings. He found himself alone and restrained to the bed, with a tube down his throat preventing him from talking. He did not even know that he had been transferred from the hospital in QC to PGH because of the severity of his case. “I could not figure out what was happening and whether my family knew the state of my condition,” recounted Peejay. In hindsight, Peejay mused that his initial lack of consciousness and consequent amnesia were a small mercy. Peejay would frequently do a scissoring motion with his hands, trying to communicate that he wanted the tube out. Breathing with the ventilator1 was a challenge. He was advised, “sabayan ninyo ‘yong machine ”, which to him was easier said than done: “I couldn’t understand. How does one actually do that with a tube stuck down one’s throat?” He felt very weak; even the act of being turned in bed by his nurses to prevent bedsores further strained him. But what was really difficult for Peejay, more than the physical pain, was the crushing isolation. Sometimes he would be conscious for hours with his eyes closed, with only his thoughts to keep him company-Why did I get the virus? How will I survive? Will I survive? Of all people, why me? But the question that wracked him the most with terror was: Did I get my family infected? Waking up to pain and the constant incomprehensible medical chatter, he just thought, “I am going to die.” 66 1 See glossary. Mouth agape with a ventilator helping him breathe, his mind conscious but his body too weak to do anything but nod and shake his head, Peejay spent “two weeks na ceiling lang ang kausap.” Doctors greeted him and introduced themselves, but they were also on rotation. Every few days, a different stranger tended to him. Nurses would inform him of the date and of daily activities like feeding, but there was no one that Peejay could share his loneliness with — no familiar face or hand to hold his. All that distinguished one day from another was the light streaming through the window. Peejay recounted that he really didn’t know where he drew his strength from during those weeks; there was only his faith. Fortunately, a lifeline was thrown. He recovered enough strength to write, and he was provided a whiteboard through which he could finally communicate. He requested for a mobile phone. This phone and its contents provided the first sparks of happiness during this bleak time of his isolation. Family, friends, and officemates took the time to record and send him messages. When asked about any message that was especially moving for him, he explained that it was not the content, but the sheer volume of messages and outpouring of support that touched him. “I did not realize so many people cared about me,” Peejay explained. “We’ve been praying for you!” said many of the messages. His colleagues told Peejay that they prayed for him together during lunch breaks. Around this time, he finally met a doctor whose compassion he felt deeply. The doctor kept reassuring him, “Don’t worry! We’re taking care of you.” These became the things he drew strength from. Peejay, however, couldn’t be kept on a ventilator for long; his throat was already swollen and leaving the tube in any longer put him at risk for other complications. They had to try to extubate1 and see if Peejay could breathe on his own. If he couldn’t, he remembered being told that they would have to do a tracheostomy2. This would mean suffering yet more weeks of being unable to speak. Bracing himself, Peejay prepared for another procedure. An empty bed was prepared next to his, ready with a team to intubate him again if he proved unable to breathe without the ventilator. 1 2 See glossary. Patients cannot remain intubated indefinitely. The tubes are a source of discomfort, and may get plugged with secretions. These can also be infected by new and more virulent bacteria if these stay in for too long. The muscles of the chest can lose their tone, so patients may not be able to breathe on their own if kept intubated and attached to a mechanical ventilator for some time. Sometimes, to enable a more stable airway access while minimizing further discomfort and other complications, a tracheostomy may need to be done. Tracheostomy is a procedure that creates a hole in the patient’s neck, and a short tube is placed directly into the windpipe While it can be attached to a mechanical ventilator, the machine is not necessary if the patient can breathe without it. 67 When the tube was removed, Peejay inhaled air directly into his lungs for the first time in weeks. To his immense joy, there was no need for a tracheostomy. Peejay said, “From that time, I knew that there was only one path I needed to go on, and that was recovery.” Not everything was smooth sailing. Peejay was lucid, but his muscles were still weak from weeks of disuse and he needed help doing some essential things, like washing himself. During these moments, he sometimes pitied himself, but the far worse ordeals he suffered gave him the certainty that he could get past these last few steps to reach the finish line in his recovery. Hope had appeared; each day was a little better. Peejay would go from having to force himself to turn in bed, to eventually attempting to stand all by himself. After two more weeks of breathing and leg exercises, Peejay had two consecutive negative results for COVID-19, and he was finally discharged in the third week of May. Peejay feels that he was given a second chance at life. He knows how close he came to not making it. His doctors told him that a case like his had only a 30% survival rate. At the time of the interview, Peejay had just celebrated his 51st birthday —a day he sees as a new beginning, a start of the “other half of his life; a new cycle.” The second chance he’s been given has imbued his life with new meaning, telling him that he still has a mission in life that he needs to fulfill. What mission this is, Peejay doesn’t know yet. He’s still searching for it. Meanwhile, he’ll just keep doing what he always believed in doing: paying it forward, starting with sharing his story of recovery which he hopes can help others, especially those who would find themselves in a similar position. Though not completely recovered yet, Peejay feels himself getting better day by day. Now, he is working from home, taking it easy, and enjoying another life-changing discovery: Netflix. Copyedited by Gabrielle P. Flores 68 The Long Trek to the Front Justin Bryan D. Maranan By 4:30 a.m. every morning, Mary-Joy departs from her small apartment in Parañaque. She rides with her husband on his motorcycle all the way to PGH, where MaryJoy works as a security guard for the newly-established “Bayanihan Na! Operations Center 1” (otherwise known as the “PGH Hotline”). Even though she does not have to report to work until 7:30 a.m., her husband needs to return to Parañaque as soon as possible to work as a vegetable vendor. Like Mary-Joy, her husband used to be in the security business, working as a private bodyguard. However, much like many other Filipinos during the lockdown1, he found himself unemployed and in need of another job to supplement their income. Security guard Mary-Joy at the entrance of the Bayanihan Na! Operations Center in the PGH Nurses’ Home. Photo by Justin Maranan. 1 2 Prior to the extended community quarantine (ECQ)1, Mary-Joy used to take the FX 2 from Sucat to Pedro Gil, which cost her only ₱35. Due to the shutdown of public transportation, she has had no choice but to trouble her husband for the early commute to work. However, their current setup is much better than their alternative from less than a month ago, when the couple were forced out of their home in a small Parañaque subdivision. See glossary. Also known as UV Express, it refers to a type of public utility vehicle, oftentimes an SUV, or van. It was colloquially adapted from Tamaraw FX, which is an SUV model that is often employed to function as a PUV. 69 “Pinalayas kami ng presidente nung subdivision. Mayroon daw kasing memo na bawal ang mga nagtatrabaho sa PGH doon sa community namin. Wala kaming magawa, so umalis na lang kami.” While she was temporarily homeless, Mary-Joy spent her nights at Alvior Hall3 along with her co-workers. Some of them were also forced out of their homes due to the discrimination against hospital workers. Others simply could not find a way to commute between home and work. Thankfully, people took notice of the situation Mary-Joy and her fellow guards faced. During the early days of the ECQ, Mary-Joy was instructed by her supervisor to hold onto the key to Alvior Hall until the arrival of a certain consultant1. “Ayaw ko pa ibigay nung simula ” laughed Mary-Joy, recalling when she was approached by someone asking for the key. “Sabi ko, ‘Kay Dr. Tony Perez ko lang daw po ibibigay itong susi.’ ” “Alam ko, ako si Tony Perez eh,” said the chair of the donations arm of PGH’s Bayanihan Na! Operations Center1. Not long after that first meeting, Dr. Tony Perez saw MaryJoy with her other co-workers, lying on makeshift mattresses of cardboard. 1 3 70 “Nilapitan kami ni Dr. Tony… [and he asked], ‘Bakit kayo nakahiga dyan? ’” After learning of their plight, Dr. Perez talked with the other administrative officers on how they could help out. Mary-Joy and her coworkers were allowed to stay at Alvior Hall, and were provided with mattresses and sanitary products. “Kung may kailangan pa daw kami, sabihan lang daw namin sila,” Mary-Joy recalled. Another doctor, Dr. Lacambra from Family Medicine, had checked in with the workers staying at Alvior. “Tinatanong niya kami kung nakakakain ba kami ng tama, lalo na kasi wala kaming lutuan doon dati. Sabi namin, ‘once a day nakakakuha naman po kami ng pagkain galing kay Father.’” The kind doctor threw the question back at them, “Isang beses lang ba kumakain isang tao sa isang araw? ” Thereafter, the workers started receiving at least three free meals daily (from the Dietary department and from outside donations), without fail. Mary-Joy was initially overwhelmed by the support from the doctors, feeling almost guilty for accepting their help. Despite the discrimination she has faced as a hospital worker, she acknowledges that she has been luckier than others. See glossary. Alvior Hall is a building on the UP Manila campus, in the area of the College of Medicine. The building itself is a landmark, being architecturally unique compared to the more aged buildings adjacent to it (i.e. Calderon Hall, Lara Hall). It was converted into the donation hub for the Bayanihan Na! Operations Center during the pandemic. “Swerte pa rin dahil nakakapagtrabaho kami ngayon, inaalagaan pa kami dito sa PGH. Pero paano naman yung mga tao sa labas; nagugutom din sila diba? Di man sila mamatay sa COVID pero namatay naman sila sa gutom.” Thankful for being able to go to work another day, MaryJoy walks to the Nurses’ Home1 building at 8 a.m. to start her shift, right after the morning formation of guards at Alvior Hall. As the PGH hotline volunteers arrive for their stint, Mary-Joy checks their temperatures and bags, while asking those with personal gadgets (e.g., laptops) to log their belongings on a ledger. She also texts Dr. Tony Perez when she notices any shortages in supplies, such as facemasks. Beyond her official responsibilities, she also maintains the cleanliness of the lobby outside the hotline facility, which doubles as a dining area during mealtimes. At the start of every meal, Mary-Joy ensures that there is enough food for the call-center personnel on duty. This is how she became a favorite among hotline volunteers—who usually spend their meal breaks chatting with the friendly guard. I asked Mary-Joy during one of those lunchtime conversations: given the chance, would she take the opportunity to work outside PGH during this pandemic? “Di po siguro, Doc. Ewan ko bakit hinahanap ko PGH. Kung gusto ko talaga umalis, nag-resign na rin ako agad nung naglockdown.” She laments over how much the volunteers and staff in PGH have given up for the fight against this pandemic. “Sila rin may mga pamilya, pero inuuna pa rin nila yung mga pasyente na kailangan sila. Lahat tayo dito, di ba lumalaban tayo para sa ibang tao?” Mary-Joy ends her shift at 8:00 p.m.. Before leaving, she always ends up bringing home excess food-items— untouched meals from the PGH hotline that volunteers insist she take with her. She only keeps one of these for her husband; the rest of the food, she gives away to the homeless around their new apartment in Parañaque. She is always careful not to disclose that she works at PGH. It would be difficult to find another place of residence during the ongoing pandemic. At the end of the day, Mary-Joy silently recites a prayer of gratitude. As a religious person, these daily prayers will have to do for now. “Pagkatapos ng COVID na ‘to, una kong gagawin ay magsimba sa Quiapo at magpasalamat sa Panginoon para sa mga blessings na binigay niya sa amin.” She then goes to sleep, ready for tomorrow’s work, and blessings. Copyedited by Iris D. Ditan 1 See glossary. 71 Lahat tayo dito, di ba lumalaban tayo para sa ibang tao? The dedicated security guards of the PGH Emergency Room. Photo by Brent Viray. 72 Within days of their pull-out from the hospital, many soon-to-be doctors of the UP-PGH Interns Batch 2020 volunteered their time and resources into helping the administration set-up the Bayanihan Na! Operations Center (BNOC). In the weeks ahead, the interns served as call-center agents who coordinated monetary and material donations and responded to COVID-related queries from anyone who calls in to the hotline. Photos by Yas Salces and Jonas Del Rosario. 73 Photos by Markyn Kho and Justin Maranan. 74 Empty Spaces Compiled by Amanda A. Cheong Disclosure: The piece contains the text exchange between two friends, and starts on the first morning of the ICU1 confinement of one of them. The names of persons and institutions have been changed for privacy purposes. Some lines, which referred to transactional concerns that came up in the early part, were not included. Typographical details were maintained. Grief rests in places where loved ones used to stand—in the lonely seat at the dining table; in the quiet of a vacant office; in the empty space where a reply should have been. MARCH 21, 2020, SATURDAY CHRIS 6:54am Kamusta ang prison life? RIC 7:04am . Sakit sa likod hehe They’re giving me meds. I’ve been taking. Hopefully the IV antibiotics will help CHRIS 7:08am Ok. Sana mabilis wifi diyan. CHRIS 7:10am Btw nagtatanong si Rosa kung kamusta ka. Ok to tell them PUI1 ka, stable naman, pero admitted at PGH pending test result and for isolation purposes? RIC 8:28am . Ok to tell them, Chris. Thanks. 1 See glossary. 75 MARCH 23, 2020, MONDAY MARCH 24, 2020, TUESDAY CHRIS (edited) 5:41am Good morning Ric. Hope things are better again this morning. Friends from outside NCR are asking about your status. Do I confirm, or baka you want to do so? Okay lang if neither. RIC 12:20am . Chris, just in case I’ll be intubated , kindly call my sons & explain to them. Just update them daily please. They know your number. Thanks RIC 8:05am . Sana tuloy tuloy na Chris. Ok lang. Thanks CHRIS 8:16am Post individually o sa Viber1 group: Ric is feeling better & is eager to go home soon - after the checkpoints and quarantine1 measures are lifted! We all hope & pray for Ric’s as-fast-as-a-Harley recovery, fortitude for his family, and the wellbeing of all our other affected colleagues. RIC 8:17am . Hahaha thanks RIC 8:20am . Sabihan mo rin ako kung nakapasok si Joan sa medical school . 1 Huwag mo munang sabihin of course. Baka lang me mangyari sa akin. . CHRIS 12:22am OK Ric. Do you feel worse? Anything else you need done? RIC 12:30am . Wala naman na, Chris. Thanks RIC 12:31am . Na istorbo lang ako hourly monitoring.1 Every time I sleep biglang gigising. Hirap na bumalik sa tulog RIC 12:32am . Stats is 95-96-97 CHRIS 12:33am Really hoping for the better. Can only imagine how depressing & distressing ang pinagdadaanan mo. Am not a religious person, but do believe we are children (& often act like so!) of God - whose presence we feel when we are most in need of comfort. Hope you get to feel this despite the many disheartening moments. Do not worry about your kids. Be proud & inspired w/ what they are already able to do. Will be checking on them, while you work fulltime at getting better. CHRIS 12:34am Huwag mo na tignan pulse ox.1 Drops ng IV na lang bilangin mo para makatulog ka na. RIC 12:35am . Hahaha 76 1 See glossary. MARCH 24, 2020, TUESDAY RIC 6:24am . Do you think I should transfer, Chris? CHRIS 7:38am Ok. Prepare yourself Ric. CHRIS 7:00am Good morning Ric. Just read your message. Why are you thinking about transferring? RIC 7:06am . Walang duty na fellow1 akong nakita RIC 7:06am . Paano kung ma intubate? RIC 7:08am . Puro nurses ang interaction ng Px sa gabi CHRIS 7:09am Don’t know if makakalipat ka, & where makakapunta. CHRIS 7:10am BTW, just Vibered your sons. Sabi ko just to keep in touch. RIC 7:30am . Salamat. preemptive intubation is being discussed now 1 CHRIS 7:32am Baka you will have to stay put there then. RIC 7:33am . Ok Chris. Pwede mo sila tutukan everyday? Thanks 1 See glossary. RIC 7:45am . Ok Chris RIC 10:13am . CHRIS 10:19am Akala ko sedated ka! RIC 10:20am . Paki remind na lang that Huwag na patagalin in case me improvement. Thanks CHRIS 10:23am You mean extubate ka soonest? Guess call nila. Will relay updates only to your kids unless they say otherwise. RIC 10:24am . Thanks, Chris 👍🙏 CHRIS 10:25am Huwag mo na muna labanan ang sedation at matulog ka na muna. CHRIS 7:35pm Sana ay may nag-re-recharge ng phone mo. Sabi if need virtual company. 77 MARCH 25, 2020, WEDNESDAY RIC 1:33pm . Chris, is okay to checkout he cough if the kids. Ty CHRIS 1:45pm Will do. We will take care of the rest, you take care of yourself. MARCH 26, 2020, THURSDAY CHRIS 11:22pm Don’t know if you have been told that Joan has been listed for interview @ med school. There were no more forthcoming messages from Ric. In the empty spaces where we can paint a picture of a loved one’s last moments, we can imagine the struggle — a plea reaching out to ask “Chris, is it okay to check if the kids have a cough? Ty.” We can imagine the mental haze that typed out jumbled words; but imagine, too, that unrelenting need to know that his children were safe. In the empty spaces of this piece where a father can no longer write his thoughts, imagine love. Warm sunlight instead of the lonely cold; laughter and stories over dinner instead of the incessant beep beep of too many machines. In the empty spaces where he might have seen that last text, imagine pride melting into peace. MARCH 31, 2020, TUESDAY, at 6:25 am Ric passed away from complications due to COVID-19 78 And In Return Robyn Gayle K. Dychiao Aparent’slove:adeepfondnessthatlastsfrombirthtodeath. Afirstlovethatleadstoalifetimeofdelightandwarmth. As a parent loves his child, so does the love of a child for his parents abound. On September 8, 2020, Dr. Jonas del Rosario was invited to share his COVID-19 story on a Catholic evangelization ministry Dominus Est’s online program. He spoke of his battle against this unforgiving disease, being a doctor, son, and patient through this pandemic. “Ako po si Dr. Jonas del Rosario. Isa po akong pediatric cardiologist, at ako rin po ang spokesperson ng Philippine General Hospital. Noong nagkaroon ng pandemya, n crisis aging aktibo ako sa team ng PGH. At dahil doon, k inailangan kong magbasa at mag-aral tungkol sa sakit na ito. Marami akong natutunan at naging malalim ang aking kaalaman sa COVID-19. Ngunit l ingid sa aking kaalaman na ito pala ay magiging isang personal na karanasan na swill abi nga’y shakemetotheverycoreofmybeing . “May tatlong buwan na simula nang kumalat ang COVID-19 noon. Sinasabi ng mga magulang ko, ‘Ikaw ay nasa ospital na maraming mga may COVID-19, at ikaw ay mag-ingat.’ Lagi silang nag-aalala para sa akin, at ganoon rin ako sa kanila. Lagi ko sinasabi sa kanila na sila rin ay mag-ingat. 1 See glossary. “Ngunit, noong July 11, dinala ko ang aking ama sa PGH. Siya ay almost 90 years old. Dahil nahihirapan siyang huminga at ubo siya nang ubo, pina-admit ko siya sa PGH. Doon ay nakitaan na mayroon siyang COVID-19 pneumonia1. Talagang kinabahan ako. Alam ko na kung ikaw ay may katandaan na, maaaring maging malubha ang COVID-19, at maaari nila itong ikamatay. “Ngunit t inago ko itong takot na ito. Kailangan kong maging matapang para sa aking ama, dahil nakikita ko sa kanyang mukha na siya’y malungkot. Ilang araw na lang ay kanyang i-ce-celebrate ang kanyang 90th birthday . Ngunit dali-dali ko siyang dinala at pina-admit sa PGH. Kapag kayo’y nagka-COVID-19, solo lang kayo sa kwarto ninyo. Ngunit hindi ko puwedeng i iwan ang aking ama, kaya ako’y naglakas ng loob at sinuot ko ang aking PPE, para ipadama sa kanya na hindi siya nag-iisa. Araw-araw, pinupuntahan ko siya dalawang beses sa isang araw para pakainin siya ng tanghalian at hapunan, at para na rin makapag-kwentuhan kami nang malaman niya na ako ay nasa tabi niya. “Napakabigat para sa isang anak na doktor na makita ang kanyang ama na ganoon. Nahihirapan siyang huminga, naka-oxygen pa siya. Ngunit ang tadhana ay parang mapagbiro. Akala ko ay ‘yun na ang pinaka-dagok ng istoryang ito. Ngunit noong gabi bago ang 90th 79 birthday ng aking ama, ang akin pong 85-year old na ina ay nilagnat at inubo. “Nakikita ko sa aking ina ang pangamba; ninenerbyos siya na siya ay dadalhin sa ospital. Hinatid ko siya sa kanyang kwarto. Pagkatapos noon, ay pinuntahan ko ang aking ama para batiin siya sa kanyang 90th birthday at dala ang mga regalo at video messages mula sa aming pamilya. Hindi ko masabi sa kanya sa mga panahon na iyon na ang kanyang asawa ay nasa PGH din. Nagtaka rin siya kung bakit hindi yata siya binabati ng aking ina. “Ang aking ina, pagkaraan ng tatlong araw, ay naging malubha at k inailangang ma-intubate1 at ilagay sa ICU. Habang siya’y ini-intubate, ako’y nasa kwarto niya’t nakasuot ng level 4 PPE1. Binubulungan ko siya na huwag siyang matakot dahil tutulungan lang siyang huminga ng ventilator 1. Hindi niya nakikita na ako ay lumuluha sa aking suot na PPE, dahil k inakabahan talaga ako. Marahil, dahil alam ko na ang mga matatandang may COVID-19 na nai-intubate ay maliit ang chance na maka-recover. “Sa susunod na mga dalawa hanggang tatlong l inggo, maliban sa pagiging spokesperson ng PGH at paggawa ng aking mga tungkulin sa ospital, araw-araw ay pupuntahan ko po ang aking ama at ang aking ina. Magsusuot ako sa umaga ng PPE, bibisitahin ko sila. Pagkaraan ng tanghali, ako’y maghuhubad, maliligo, magpapalit ulit, magtratrabaho nang sandali, at bago maghapunan ay babalikan ko sila. Siguro dahil sa halo-halo na pagod at pag-aaalala, hindi ko rin masyado namalayan na ako pala ay nagkakasakit na rin. “Kinailangan ko na ring magpa-admit sa PGH dahil ako ay may moderate to severe pneumonia na dulot ng COVID-19.So,kamingtatlo,akoatangakingmgamagulang,aymagkakatabisaisangfloor.Ngunithindiko na sila pwedeng puntahan dahil ako ay may COVID-19 na rin, at kailangan akong iisolate at gamutin. Ni hindi ko sila mahawakan, hindi ko sila mabulungan, at hindi ko sila mabigyan ng encouragement na lumaban. “Isang gabi, noong halos ako’y gumagaling na, ay bigla kong nakita na ang aking ama ay hirap na hirap huminga. Sa loob ng sampung oras binabantayan ko ang aking ama sa remote video monitor ng iPad ko hanggang siya ay maintubate kinalaunan. Nakatingin po ako sa monitor, kausap ko po yung mga doktor, binibigyan ko sila ng instruction. Sa kasawiang palad po, siya ay nagkaroon ng cardiac arrest at parang bigla na lang siyang kinuha sa amin. 80 1 See glossary. A child’s love: a devotion that flourishesdespite the unbearable struggle. “Namatay po ang aking ama na kami po ay nasa ospital pa. Ako ay hindi pa nakakalabas. Ito ay August 8, 2020. “Napakasakit at napakabigat sa pakiramdam… Ako ay doktor na, at g usto mo sanang nandoon ka para may magawa… ngunit wala akong magawa. Ang nagawa ko na lamang ay naki-usap ako sa kanila na kung maaari ay payagan nila akong lumabas sa aking silid bago dalhin sa morgue ang aking ama, at makapagmano, mayakap, magpasalamat, at humingi na rin ng tawad na hindi ko siya naisalba. “Pumunta ako sa kwarto niya dala ang aking cellphone, na aking inilapit sa kanyang tainga, para marinig niya ang boses ng kanyang mga anak, apo, at kamag-anak na dinadasalan siya. Ako ay nakatayo lang sa kwarto niyang iyon, at doon ay nakita ko siyang nakahiga at wala nang buhay. Niyakap ko siya, binigay ko ang aking rosaryo, at sinabi ko, ‘ Tay, marami pong salamat, magpahinga ka na. Kami na po bahala kay Nanay.’ “Ako ay na-discharge soon after. Dinaanan ko ang aking ina, at siya ay gising na naka-intubate . Hindi ko masabi sa aking ina na namatay na ang kanyang kabiyak. Nagdadasal kami araw-araw, at lagi ko pong sinasabi sa tatay ko na, ‘alam ko na kayo’y close at lagi kayong lumalabas at magkasama. Kumbaga, ‘inseparable’. Pero, huwag mo muna siyang kunin sa amin. Huwag mo muna siyang sunduin. Bigay mo muna sa amin si Nanay dahil napakabigat kung pareho kayong mawawala. Bigyan niyo po kami ng pagkakataon na makapiling pa siya at makabawi.’ “Ngunit ngayon ay napakahirap, dahil ang aking ina ngayon ay k ritikal. Siya ay comatose na.Sabi ng mga doktor, ‘Doc, maliit nalang po ang chance para siya’y magising pa.’ 81 “Pero hindi pa kami nawawalan ng pag-asa. Kami ay laging nagdadasal, nananalangin na sana ay bigyan pa kami at makapiling pa namin ang aming ina. Mula po ng pagkamatay ng aking ama, ay halos apat na linggo na pong lumilipas. Kami po ay laging nagdadasal, Divine Mercy… At ang aming panalangin ay iligtas niyo po si Nanay. “Ako ay patuloy na nagpapagaling. Nilalabanan ko ang aking pagdadalamhati. Physically, ako ay halos recovered na, pero mabigat ang aking dinadala. Alam ko na kailangan ko po bumalik sa trabaho at kailangan kong gampanan ang aking katungkulan na maging spokesperson ng PGH. “Paminsan natatanong ko kung bakit ba sa akin nangyari ito. Sabi nga nila, ‘There’s always a reason for everything. Sometimes there’s a higher meaning to this that only God knows.’ Hinahanap ko iyon. Minsan nagra-rationalize ako na siguro, gusto ako sabihan ng Panginoon na kaya po akong binigyan ng ganito kabigat na pasan dahil may gusto siyang iparating sa akin. Ipagawa sa akin. Minsan’y mahirap isipin ‘yun dahil nangingibabaw ang pagkawala ng aking ama, at ngayon, malaki rin ang pagkakataon na baka kunin din ang aking ina. “Ngunit, kahit na ako ay doktor at lumaki ako sa siyensya -- ‘Man of Science’ ika nga -- masasabi ko na nagawa namin ang what is humanly possible for my parents. Kahit na nandiyan lahat: gamot, mga doktor, at mga dalubhasa, ang pinapanghawakan ko ay ang aking faith. Huwag bibitiw sa paniniwala na tayo’y mahal ng Panginoon at maaaring in God’s time ang gusto Niyang mangyari. Masakit man kung minsan, ay dapat itong tanggapin. “Ang COVID-19 para sa akin ay napaka-personal. Hindi lang ito na para bagang ako’y isang eksperto na nagsasabi sa mundo na ganito ang COVID-19, dahil ako’y nagkaroon ng karanasan bilang tagapagsalita. Higit sa lahat, bukod sa pagiging pasyente, ako’y naging isang anak na nawalan ng magulang dahil sa sakit na ito.” Dr. Jonas del Rosario’s mother passed away from complications due to COVID-19 on the day of this sharing. A child’s love: a devotion that flourishes despite the unbearable struggle. Copyedited by Vince Elic S. Maullon 82 A Matter of Mantras Jill Olivia Bañares I’ve been an emergency room (ER) nurse for the past three years. The Department of Emergency Medicine (DEM) has always been on the frontline, its staff trained to handle all sorts of emergencies. Bleeding. Breathing difficulties. Heart attacks. Stroke. We deal with different cases. Our patients entrust their lives to us, and we do our best for them. Day in, day out, I’d execute my tasks as an ER nurse to the best of my abilities. It was the least I could do for both my patients and co-workers. When things got tough, I’d tell myself: Focus. Stay calm. Do your best. I’d repeat my mantra until my task was finished and I was ready to face another challenge. Most of the time, it worked. 1 1 See glossary. Last March, it didn’t. COVID-19 caught us by surprise. Just like everyone else, we were unprepared. There was a limited supply of face masks, personal protective equipment (PPEs)1, and face shields. Protocols were not properly laid out; the government’s plans were vague. More importantly, we knew so little about the virus. How does it work? How do we know if someone is infected? What should be done to keep people from getting infected? As a member of the department that would face the first wave head-on, I struggled to keep my anxiety at bay. We were all terrified. An invisible enemy had waged a war, and backing down— giving up—is never an option, most especially for us. After all, we were—still are, and always will be—the gatekeepers of the hospital. 83 The makeshift emergency room triage stands before the entrance to PGH, where patients are screened for symptoms of COVID-19. Photo by Brent Viray. The first few weeks proved to be the most challenging. Since the interns and other services1 were pulled out, ER doctors and nurses struggled to keep the ER running. Moreover, the fear of admitting persons-under-investigation (PUIs) or COVID-19-positive patients made it difficult to admit a patient to the wards, causing patients to pile up in our ER. We had to adapt to the situation before it completely overwhelmed us. For every eight-hour shift, there were two to three nurses assigned to man the PUI1 zone. We would call them “alay” (“sacrifice”). Their main task was to monitor the patients’ vital signs1. However, since their relatives or friends were not allowed in the ER, the nurses on duty1 also performed most of the bedside care. This included bathing, wiping, lifting, and feeding the patient. We turn their beds and change their diapers—no complaints. 84 1 See glossary. We worked harder. We tried to do better. Unfortunately, the glaring reality was still present. We had limited workforce, inadequate facilities, and insufficient equipment. Even with our best efforts, it was still a disaster. The scenario outside of the Philippine General Hospital was not any better either. I had to constantly remind myself that I was not walking through a set of a post-apocalyptic movie. Deserted streets. Eerily quiet nights. Whenever I walked along Padre Faura and Pedro Gil2, I yearned for the deafening noise I’ve grown accustomed to. My footsteps were quick and light, but my mind was heavy. My heart ached as it held on to my colleagues’ eyes—eyes that betrayed the fear they hid with their smiles. I was pushed to my limits. My mind was reeling with fear and my body, beyond exhausted. Drops of sweat stung our eyes. The N95 masks1 that were meant to protect us made breathing painful. We were so drenched in sweat we could squeeze out our perspiration from our clothes. Our faces were not spared either. The pressure points of goggles and masks left scars. These marks earned the moniker “battle scars”, and we wore them with unwavering pride. Even if COVID-19 robbed us of social interaction and the comfort of physical touch, seeing the smiles on their faces and hearing the laughter in their voices kept me going. “Lilipas din ‘to!” my co-workers cheered. “Tayo pa? DEM tayo. Kayang-kaya!” I was blessed to be surrounded by such wonderful people. Their indomitable spirits kept me going. The situation was—is—tough, but we are tougher. Yes, our healthcare system is flawed. HCWs are overwhelmed. There is so much disquiet and it is saddening that some leaders still choose to turn a blind eye towards their people. Despite this, I still firmly believe that everything is happening in God’s time; and that this, too, shall pass. Until then, I will carry out my tasks with diligence and discipline, replaying the mantra in my head: Focus. Stay calm. Do everything with love. Focus. Stay calm. Do your best. When it didn’t do the trick, I’d add: Do it for them—my family, my friends, my co-workers. Copyedited by Marcela Mercedes S. Rodolfo 1 2 See glossary. The UP Manila - Philippine General Hospital complex is flanked by these two streets. Lined with colorful food establishments, massage parlors, shops, condos, and dorms, Padre Faura and Pedro Gil, as well as the streets that intersect them, serve as an extended network of the experience of being a PGH worker and a UP Manila student. 85 Frontliners in the PGH Emergency Room work tirelessly round-the-clock as more and more COVID patients arrive from all around Metro Manila and the surrounding provinces. Photos by Brent Viray. 86 Overcoming Inertia What moves us to go beyond our comforts and means? Fr. Marlito Ocon In Physics, an object can only be moved by a force greater than gravity or the weight of the object itself. What greater force, then, can move us to do more and to be more for others, especially when the gravity that keeps us in our comfort zones is naturally strong? It is God’s grace! It is God’s grace at work in each of us that moves us to go beyond ourselves. And when we move as one, bringing our acts together as a graced community, God’s grace reveals itself to be even stronger and more effective. Our primary role as chaplains is to cater to the spiritual needs of the patients and the hospital staff. But in a hospital that is committed to the care of indigent patients like PGH, opening one’s eyes to the spiritual needs is a gateway to many other basic needs which yearn for a humane response. As chaplains, we cannot simply sit down and comfortably say, “I am here only for their spiritual needs.” We find ourselves challenged to do more. We look for ways to respond that are deeply divine and deeply human at the same time. That is how Jesus responded when he encountered the multitudes. When they were hungry, he fed them. When they were sick, he healed them. When they were sorrowing, he comforted them. When they were lost, he shepherded them. When COVID-19 struck, our field of vision gradually expanded, and thus our sense of mission also shifted with the emerging needs. We saw not only indigent patients but also the multitude of frontliners—nurses, doctors, caregivers, security guards, janitors, maintenance, and utility personnel. At the outset of the community quarantine1, when it became difficult to buy food after night shifts, we started to provide some 400 food packs 1 See glossary. 87 daily for healthcare workers on afternoon and evening duties. We did this until the service became unnecessary as the hospital was already able to provide for them. Then, another need came to the fore—the daily sustenance of our outsourced personnel: the security guards and the janitors. With the approval of the deputy director for administration, we were able to provide daily lunch and dinner to 125 security guards and 143 janitors. Bread and bottled water were provided to those in the COVID charity wards1 and emergency rooms. For this service, we are grateful to our generous and reliable meal donors2, all of whom have pledged to help while community quarantine is still in effect. As we journeyed with the whole UP-PGH community in day-to-day combat with COVID-19, we discovered many other needs. As such, we partnered with PGH to help fill the gaps. As telemedicine1 emerged, so did telechaplaincy. The telechaplaincy program, in coordination with the medical social services, did online counselling, 1 2 88 provided spiritual direction, and prayed with families of patients and healthcare workers alike. Needless to say, we continued with our official duty of providing for the spiritual needs of our patients and health workers. We took turns with my brother chaplains for the 24-hour shifts. We were all afraid to get sick, but we could not and did not allow our fears to dampen our compassion and our sense of mission. We did room-to-room and bed-to-bed visits to COVID patients. When I visited patients, in chronic and critical conditions, it made me wonder: Bakit sila pa ang naCOVID? A stage IV cancer patient? A diabetic patient on dialysis1 whose husband is in a coma due to a stroke? A psychiatric patient who harmed himself? Isang matanda na may cancer sa mata? O mag-asawang doktor na kapapanganak lang ng asawa? Even a dutiful nurse tending to COVID patients. Bakit sila pa? See glossary. Our generous donors include the Tanging Yaman Foundation-Simbahang Lingkod ng Bayan-Ateneo de Manila University through Fr. Manoling Francisco, SJ and Ms. Marites Ingles, as well as Mr. Chips Guevara and friends of the Guevara family At one point, it moved me to tears until my glasses, my goggles, and even my face shield turned misty and blurred. I could no longer read my prayers. I had to stop and say, “Lord ikaw na bahala, alam mo naman na ang tanging dasal ko ay para mapagaling sila at makapatuloy ng pagsisilbi sa mga may sakit.” Being around sick and dying people every day is draining, especially when all feel helpless. The rich, the poor, even I myself felt helpless. It can be so depressing. The patients normally asked for our prayers. Their biggest concern was, of course, suffering and death. We all want to live and live happily, but death is also real, and we know it will come. What helps us cope is when we feel that we have helped them prepare well for any eventualities. We see them at peace and become more accepting and trusting of the Lord, even as the end draws near. It helps us to believe that we have helped them rejoin the Lord. At the start, simply seeing health workers in full PPEs1 scared us, and thinking about visiting them scared us all the more. However, as we reflected about it more deeply, we realized that since it scares us, there must be something in it that we must respond to with courage, not fear. We feel that this is the very essence of our mission and this is where we are called to respond as the chaplains of PGH. While we went around doing our spiritual work, they would always say, “Huwag na kayo umikot father baka mahawa pa kayo.” How can we do that? That’s part of our work: to let them know that we are with them. We cannot just hide in the safety of our rooms; that is not what we are here for! We have to take risks, just as they take the risks, because we are together in this fight. My face shield turned misty and blurred. I could no longer read my prayers. 1 See glossary. 89 The frontliners asked for prayers too: that they be protected all the time and that they remain healthy and strong. But their needs went beyond that; we heard them saying they didn’t have enough masks, alcohol, and PPEs. Certainly the hospital had supplies, but they were not enough at the start. I saw how the experiences brought about by COVID-19 served to strengthen and deepen their faith. They said, “Do or die, and with prayers, nawala takot ko, Father”. Whenever I went around, some nurses would raise their hands and shout from a distance because I couldn’t come closer, “Father, protected tayo ni Lord di ba?” I knew they were all tired and afraid, but they served with a smile and looked cool and calm, and we never saw them faltering in their faith. It is not easy, and it will never be easy. What moves us to do this and go beyond the bounds of our comfort zones, and even beyond our means is God’s grace! Photo by Maria Keziah Legion Copyedited by Leander T. Quilang 90 Photo by Maria Keziah Legion With PGH in sudden need of additional resources to care for its patients and support its hospital staff, Fr. Ocon and his brother chaplains take the lead in collecting and distributing food donations to healthcare workers and outsourced personnel. They also continue their ministry of seeing and comforting sick patients not only in person, but also through the safer and innovative “telechaplaincy” program. Photos by Marlito Ocon 91 Photos by Marlito Ocon 92 Photos by Marlito Ocon 93 Skin in the Game Justin Bryan D. Maranan “There was definitely a ‘shifting dullness,’” confessed Sofia Naval, a 2nd year Ophthalmology resident1, about working in the COVID wards. Anyone who undergoes medical training knows the awkward feeling of rust and being “out of place” during the first few days of shifting into a new rotation—a phenomenon dubbed as “shifting dullness,” a play on words, referencing a time-worn physical exam finding “Even the census1 [was different] …I’m sure it made sense for an Internal Medicinea resident, but I was definitely lost.” Carl Uy, a 2nd Year Pathology1 resident, whose typical work did not involve patient interactions, had to dig out the IM Platinum book 2 he used during clerkship and internship1. “This reference, on top of the revised algorithms for COVID-19, helped me reconstitute what little clinical skills I had despite spending more than two years of residency training without direct patient care.” The need for this drastic move soon became clear to Martin, however, when COVID-19 patients poured into the hospital. The Department of Internal Medicine’s patient census skyrocketed. Conversely, the doctor-to-patient ratio of “cutting fields3” like ORL and Ophthalmology skewed to the opposite extremes; their wards emptied out and elective admissions1were effectively reduced to zero. Interdepartmental cooperation was needed to balance the collective burden among PGH’s different residents. “I soon realized,” Martin recalled, “that this situation goes beyond what is expected from our respective departments—everyone had their ‘skin in the game,’ and to conquer this pandemic, we all needed to do our part together. With that mindset, I steeled myself and entered the COVID wards without fear or hesitation.” See glossary. IM platinum is a book which serves as a condensed guide to internal medicine. It mainly references the famous book, Harrison’s Principles of Internal Medicine, as well as includes local practice guidelines, and unique pearls of knowledge. It is written by Jamie Alfonso M. Aherrera, M.D., Marc Gregory Y. Yu, M.D., Marc Denver A. Tiongson, M.D., Deonne Thaddeus V. Gauiran, M.D., Jose Eduardo D.L. Duya, M.D., and Enrico Paolo C. Banzuela, M.D., and is edited by Geraldine Zamora, M.D. 3 Cutting field is a colloquial term used to refer to specialties that involve surgical procedures. 1 2 94 Meanwhile, for Martin Ilustre, a 2nd year Otorhinolaryngology (ORL)1 resident, diseases of the head and neck were what he had expected to train for when he applied for residency in PGH. “My first [reaction] was to question why we had to go into these COVID wards in the first place.” Though not used to a medical ICU setting, many physicians and nurses from other hospital departments who were reassigned to the COVID wards selflessly took on the challenge of caring for these critically ill patients. Photos by Sofia Naval, Carl Uy, and Martin llustre. 95 Their duty schedules1—a PGH resident’s circadian rhythm of “pre-duty,” “duty,” and “post-duty”— were thrown out the window as a new system was implemented to minimize the active workforce at any given shift. They now needed to work eight-hour shifts starting at either 6:00 a.m., 2:00 p.m., or 10:00 p.m., for seven days straight. “The anxiety was the worst part of that first shift,” said Carl. “During the first few hours, I was functionally blind. My glasses and goggles conspired against me as I wasn’t used to wearing PPEs1 yet. It was only through the guidance of the outgoing General Medicine resident that I was able to get a semblance of the goings on in the wards. ‘Shifting dullness’ was an understatement.” “What the hell am I doing?” Sofia would think to herself, as she tried to find her footing. The beeping ventilators1 were a far cry from the visual acuity charts she had grown accustomed to in Ophthalmology. Even Martin, who had primed himself to power through the haze, remarked that every new update in protocols threw him off balance. In spite of these curve balls, they knew they still had to fulfill the role of the resident-on-duty (ROD). “It all happened too fast to process appropriately,” Carl recalls. “There was so little information on what was expected from us as RODs. So I used what little time I had to just breeze through my references—-hoping to absorb as much as I could.” 1 4 96 Sofia, on the other hand, admits that she had grown so accustomed to the five-point eye exam4, a staple for any ophthalmologist, that she had to revisit the basics of a full physical examination. Despite the need to brush up on the subject matter, Sofia was especially grateful for the Infectious Disease Specialty (IDS)1 fellows who rotated with her, citing a newfound respect for the people whom she saw laughing, making jokes, and bringing food to lighten people’s spirits despite the gloomy environment in the wards. “These doctors have been working non-stop since the crisis began. Our eighthour duties seem like nothing compared to what they do,” she says. And while fear and anxiety were rampant among the residents manning the COVID-19 wards, so was kindness. “I had not extracted blood or inserted an IV line1 in a very long time. I was worried I couldn’t do it, especially with all these layers of PPE hampering my movement.” Sofia recounts. While she was talking to her patient, however, Ma’am Jo and Sir Eric—her nurses on duty—stopped her. “Doktora, dapat naka Level 4 PPE ka.” “Kailangan ba talaga, ma’am? Kakasuot ko lang nitong Level 3, sayang naman,” Sofia countered. But Ma’am Jo looked at her with caring eyes and said, “Para sa’yo rin ‘yan, Doktora.” See glossary. The basic eye examination done on patients in a general ophthalmologic consult. It consists of five components: visual acuity, gross examination, checking of extraocular movements, digital tonometry, and fundoscopy. And so she changed, with the nurses flashing her two thumbs up from the station saying, “Thank you, Doktora! ” “As if I was the one who should have been thanked!” Sofia said. While extra preparation and help from others proved to be good countermeasures to shifting dullness, Martin recalls a time when they weren’t enough. His patient’s body convulsed with a seizure during his first duty1. “I referred to Neurology1, but the needed medication wasn’t available. “I had no idea what to do. I felt so helpless just watching my patient,” Martin said. “I was displaced from my comfort zone; I had to adjust and relearn things I had forgotten since internship.” Facing challenges like these, shifting dullness became all the more familiar for our three residents. But while Sofia, Martin, and Carl essentially performed the same functions and accomplished the same work during their tours of duty, their experiences and takeaways were unique. Probably a function of the gap that existed between the residency training they had signed up for, and the COVID-19 work they found themselves in. “As a Pathology resident,” says Carl, “to have been given the opportunity to handle patients again during these troubling times is a worthwhile experience that I will forever cherish. To have been able to reduce the burden on the services conventionally involved in managing this pandemic, and to have been able to contribute what little I could as an out-of-place Pathologist-in-training, meant the world to me.” Wildly displaced from his comfort zone, Martin says, “I had to adjust and relearn things I had forgotten. “But while preparing to go into the COVID wards, I saw a video on Facebook about the pandemic, and one thing stuck with me. They used this statement: ‘skin in the game.’ How I understood that is we all have a stake in reaching a common goal, and we all have to risk something in order to achieve it. This is what it means to serve the Filipino people: to put my ‘skin in the game’, and do whatever I can as we all go through this pandemic together.” Copyedited by Lorena Margarita B. Osorio 1 See glossary. 97 Surgeons and nursing staff continue to perform life-saving operations under the uncomfortable, restricting, triple-layer PPEs. An operating room staff turns on the UV box as part of the disinfection protocols between procedures. Photos by Brent Viray. 98 Photos by Brent Viray. 99 The Physician in Plastic John Jefferson V. Besa N.B. was an 81-year-old female who had gone through multiple episodes of pneumonia1 and a stroke that left her bedridden. She was dependent on her son and granddaughter, who fed her and bathed her. She was COVID-19 positive, for admission in our wards. I was her resident1, decked in a plastic bunny suit. My mask is suffocating, the layers of gloves are numbing, and the goggles keep on fogging up. Walking is awkward. I looked like an astronaut covered in plastic, traversing an unknown planet for the first time. She had to be admitted alone because relatives were not allowed inside. After being a resident for more than a year, we have learned to recognize people who were in bad shape. And she was in bad shape. I called her family and talked to her son. I tried to be objective in laying down the facts—what studies have shown so far, what survival rates were, what we know, and what we don’t know. I told him that she needed a tube 1 2 100 down her windpipe to help her breathe. I told him it wasn’t a comfortable procedure. I told him what the chances of his mother getting better were, despite that tube. It is my duty to get an advance directive, as part of protocol, from the family members of patients whose prognosis we deem to be poor. In these uncertain times, it is also my duty to confess the limits of medicine. Her son accepted them. “Do not intubate1” and “Do not resuscitate”. No tubes. No CPR 2. As the days went by, her condition worsened. Her oxygen levels steadily went down, and she became less responsive. My medical training said that I have to hook her to a machine to help her breathe immediately, but I had a document saying I shouldn’t. I dialed her son’s number. I wanted to update him on his mother’s status. He did not pick up the phone. See glossary. An advance directive is a legal document wherein patients or their relatives specify the actions that should be done regarding their healthcare, in the event that they are not able to make those decisions themselves. A “Do not resuscitate” (DNR) order, is a type of advance directive. Once a DNR form is signed, it signifies that they do not want CPR performed on them if their heart stops beating. Another type of advance directive is a “Do not intubate” (DNI) order. This legal document is signed to indicate that a patient does not want to be intubated, even in the setting of respiratory failure. The medical staff will respect these decisions to preserve the patient’s autonomy. Photo by Brent Viray The blood pressure apparatus did not register any measurement. Was it just the double layer of gloves or was there really no pulse? Her chest was not rising and falling as it normally should. I called my co-resident to double check, because to be honest, I was doubting myself. He confirmed what I thought. I called the time of death—8:45 P.M. Her son was still not picking up. I tried the other number in her records, and her granddaughter answered. I made sure my voice was clear, calm, and empathic. I broke the bad news. She wailed. I found myself out of words; I had just introduced myself to her a few seconds ago—and I did not know how to comfort her. Her cry was deafening. I let it pass into silence. Then we talked—of how her grandmother brought them joy with her quirks, of how they took care of her at home, of how she did while she was admitted, of how her son arrived at a hard decision, of why they will never see her body again. The morgue gave them the final instructions. Being with patients with COVID-19, I realized that this pandemic strips off the humanity at the core of the art of medicine. N.B. died alone away from her family. When the end of the line is reached, a physician’s role is “to comfort always.” But with my gloved hands, I doubt that I was able to do so. I have witnessed countless deaths as a doctor, but this is different. This is not how I want to take care of my patients. The virus is inhumane. Copyedited by Vince Elic S. Maullon 101 Soldiering On Hilda Uy It was Tuesday, on the 17th of March of this fateful year, when PGH’s Department of Out-Patient Services (OPD)1 officially closed under indefinite terms. While almost everyone in the staff rejoiced in response to the unexpected break, I did not, for something inauspicious was seemingly brewing. The excitement quickly fizzled out when the grim reality sunk in. If an entire PGH department closes, especially in the middle of a national public health emergency, it can only mean one thing: we, its workforce, are “going in” – quite literally so. Re-assignment to posts within the in-patient facilities caused a lot of anxiety for the OPD staff. Placing nurses like us, with professional years devoid of direct bedside patient care, back in the hospital proper is akin to deploying soldiers with old and unmaintained arms. We were being called to the frontlines of war, nevertheless. We were bound by our sworn pledge to pick up these likelyfaulty guns, pull the trigger when the right circumstances arose, and hope that they fired. Nurse Michelle in full protective gear as she goes on duty in one of the COVID wards. Photo by Michelle Palomar. 102 1 See glossary. What we knew about the ravaging foe compelled the young and healthy to lead the charge; it was no surprise, therefore, that I was among those first sent to no man’s land. It was still dark when I came in, riding a borrowed bicycle, to work on my “new” first day. My feet were weary with an unfamiliar ache. I parked my bike and entered the anteroom of the Spine Unit1 where one of the first COVID wards was located. I knocked–there was no response. I knocked again and, during that moment, a part of me hoped for continued silence (as the door creaking away from me would be the beginning of it all). Eventually, a nurse in a scrub suit unlocked the door and swung it open. She seemed to be smiling at me underneath the face mask. “Hi, are you ready?” “I need to be.” Our 113-year old institution abruptly transformed into this barely recognizable battlefield. Everywhere I was placed for duty1 was uncharted territory: at the COVID triage, then at the COVID general wards, and even at a COVID intensive care unit1. We were shuffled often. The agony of not knowing where I would be assigned next every day for a whole week did nothing but intensify my uneasiness for the unseen and for my own fate. I didn’t have a choice but to take care of acutely and critically ill patients outside my expertise, and to do so very carefully during my first week. On top of everything, the 8-hour shifts that we had to endure without breaks and in sweltering heat while in a bunny suit were unprecedented battles on their own. At the end of each shift, I yearned for the first ambient and relatively cooler wind that caressed my skin as I removed my suit, the first unfiltered breath I took as I took off my N95 respirator1, and the first drop of water that touched my lips as I quenched my thirst. These mundane routines of near-instinct, luxuries at the heart of the moment, were my little victories – a validation that I had withstood the restlessness, agony, and discomfort of that day. Not even the thought of having to go through all of this again tomorrow could make these victories less sweet. Perhaps, the greatest victory I can clinch for now is I was helping those that had been scourged by this virus, rather than being at the receiving end of such rendered care. At the end of the day, I still get to realize what I want and love – to be a nurse. Being in such a perfect storm of circumstances is part and parcel of the oath I took years ago, and I ought to keep it no matter how uncomfortable, scared and uncertain I feel right now. You see, we have always been in the line of danger, the world just hadn’t noticed before. We are not heroes in the truest sense of the word, and we never were. We are just soldiering on day by day until this is all over. Copyedited by Aedrian A. Abrilla 1 See glossary. 103 Ashen Anna Elvira S. Arcellana “Last seen well” A moment not so long ago, Now seemed like forever; Fleeting as the wind, Etched as a bittersweet memory. It began with a treacherous cough, Then a battle of spiking heat and chills, bone deep Leaving the battered warrior weak and weary Alone against formidable enemies An arduous struggle in solitude. A frantic search for cure Unleashed a growing armamentarium. Allies clad in white rallied him into battle. Only, wars are not won with transient victories Turning those once hopeful days into waning weeks. All efforts overflowed All aboard, pushing the limits of science. Yet the fierce menace still engulfed him, Waves of grief washed over their virtual reality As distress beckoned to his loved ones. He desperately gasped for air, Clinging through the tube with his dwindling strength. Ready aim. Fire the adrenaline, hot through his veins To give him a final shot at life Invigorated with prayers whispered from close hearts afar. But with the battle eventually lost– A ghastly face silently departed. Devoid of all but embered companionship, A fallen warrior sank to ashes; A jar taking on the last embrace. A loss made more painful By insurmountable distance That flowing tears could never bring back. Yet, the memories stay even in deathly gray The ruins of burning love. Copyedited by Sean Kendrich N. Cua 104 I Don’t Feel Like a Hero Ella Mae Masamayor Right before we enter the donning1 area, there’s a sign above the entrance that reads: Welcome Heroes. It’s a lovely sight to read in the morning; it reminds me of McDreamy’s2 famous line, “It’s a beautiful day to save lives,” from Grey’s Anatomy. I don’t know who put up that sign, but I am grateful for their kindness. It was their way of trying to lift our spirits before the 8-hour shift ahead. However, if I’m completely honest with myself—I don’t really feel like a hero. A sign saying ‘Welcome Heroes!’ hangs above the entrance of the COVID wards. Photo by Brent Viray 1 2 See glossary. McDreamy is the moniker of Dr. Derek Shepherd, a character in the medical drama Grey’s Anatomy. In the series, other characters call Shepherd “McDreamy” because the charming and attractive neurosurgeon is considered by most as their “dream man”. 105 I have nothing but admiration and gratitude for other doctors like me, as well as our nurses, pharmacists, medical and radiologic technologists1, utility workers, service and delivery personnel, security guards—all of whom show up everyday to keep the lights on. But when I come back to myself, somehow, I don’t feel deserving of the same applause. People have tagged me on Facebook and thanked me online for being a frontliner, a hero. But if heroes are strong men and women with extraordinary powers and courageous hearts, then I’m definitely not one. I know very little about this disease; the unknowns and uncertainties worry me a lot. There are still so many questions unanswered and probably even more unasked, and I don’t know how I’ll be able to fill in all the blanks. Before all of this, I was but a second year resident1, with still much to learn and much to master. I’ve always had this vague feeling of inadequacy as a trainee, and the feeling has grown all the more palpable in these times of constant change. 106 1 See glossary. Every day, I ask myself if I’m the right person for the job. I question if I do know what to do, if I can deliver when the situation calls for it. And each time someone dies or deteriorates in front of me, I wonder if I have done something wrong, if I have made the right decisions, or if the patient could have been saved had someone else been in my place. I am terrified, for myself and for my loved ones. I’m scared of getting the disease and of passing it on, to my mom, my dad, my brother. I cannot begin to tell you the number of times I’ve wanted to sit this one out. Before each duty1, I lie awake running through every worst case scenario, not feeling any more prepared. I struggle to look for things I can control, and find myself horrified that there are very few. I am drowned by the what ifs and buts and oh noes I have to handle each day. For the first time in a while, I have started to question why I ever wanted to be in this vocation— I’m pretty sure the little girl in me didn’t have this in mind when she said she wanted to be a doctor. It turns out I’m not so brave after all. alongside them. I am scared for my patients. For the ones infected with the virus, I can only imagine how terrifying this must be for them. The disease itself is horrific; the thought of gasping for air, needing intubation1, and that possibility of being an addition to that ever-rising list of deaths. Then there’s the isolation, being all alone; no one to assure you when you’re getting better and no one to hold on to when you take a turn for the worse. I imagine how scared they are of infecting their loved ones, their little kids, or their aging parents. How they place their hope on whatever drug or intervention could work, never mind that the data is less than robust. We’re all scared of this pandemic, and we wake up each day with an eerie sense of helplessness. But going on hospital duties, when I see all our patients and all the hospital staff, I see people who refuse to give up on hope---people who still want to give it their best shot. I realize that I may not have the strength expected of socalled heroes, but I am blessed with the extraordinary privilege to help, to fight this villain of a virus, and to let our patients know that even until the end, we must muster up the courage to not give up on them. I am scared for our non-COVID patients, too. I think of all the dialysis1 sessions missed, the chemotherapies1 skipped, the blood sugars and blood pressures that have probably gone off the charts by now. I can hear my patients asking, “Doc, paano na po kami?” The lack of an answer adds up to even more fear. Here’s a big thank you to those who believe in us, to those who support us—those who cheer us on, those who stay at home, those who donate their money, food, or whatever they have to give. All this kindness and care give us insurmountable strength. Thank you for believing in us even when we’re scared, even when we’re unsure, even when we don’t know what’s going to happen. When I think about it, I can always quit my job and retreat to the sidelines. But I cannot find the heart to turn my back on these people, all of whom are probably more terrified than I am. It goes beyond just a call of duty or an oath we’ve made to the profession. I realize that our patients are fighting, and they need us to fight I do not feel like a hero, and I can’t promise I’ll eventually be one, too. But I will continue to try my best, to fight my hardest, and most importantly, to hope. Hope for myself, hope for my patients, hope with every little bit of hope left. For courage and perseverance. For better days ahead. Copyedited by Sachiko S. Estreller 1 See glossary. 107 Hospital staff celebrate the recovery of a pediatric COVID patient. Photo by Marlito Ocon 108 109 110 Photo by Brent Viray SIDE EFFECTS 111 112 Side effect /’sīd i-’fekt/ n. A secondary, typically undesirable effect of a drug or medical treatment. The casualties of our war with COVID-19 have stacked high and each day brings more worries. Within, and beyond the walls of the Philippine General Hospital, lives of patients, families, and workers shift and tumble as the pandemic’s consequences reach further than anticipated. 113 Sa Gitna ng Pandemya Ian Gabriel A. Juyad Isang bisikletang Dala’y pagkaing hindi sa kanya Mga estudyanteng Naglilikom ng pera para sa iba May naghahatid ng gamot Sa matandang mag-asawang kapitbahay May pawisang balot na balot Umaaruga sa nag-aagaw-buhay Mga maliliit na kaskaho Sa malalaking blokeng bato Magkakaisa’t bubuong Isang konkretong kastilyo Bawat sulat, tula’t kantang inilikha Bawat pagkai’t kanlungang inihanda Bawat panahon na ibinigay Bawat dasal na inialay Sa bawat patak ng ambon May nagtatampisaw na mga punlang tutubo Mamumuong panibago Isang buhay na mundo Ikaw at ako – Isang tipak ng bato Isang patak ng ulan Sa iisang lupang pananahanan 114 Photo by Adrianne Alfaro Broken Spirits Cary Amiel G. Villanueva Everything was unsettling. We signed up for a noble profession, one committed to serving humanity. We enlisted and took on the Oath of Hippocrates. We promised to care for the sick to the best of our abilities. But we never could have imagined that being sworn as licensed health professionals—not too long ago for some of us—would mean that we were being drafted to fight skirmishes in this pandemic. And it is this departure from what we had envisioned to become that leaves us with broken spirits. There is a medieval adage that speaks of the goals of medicine: “To cure sometimes, to relieve often, to comfort always.” Yet even the act of comforting can be a herculean task in these trying times. A dialysis-requiring1 father in the COVID-19 ward cried in frustration as I did rounds1 one morning. As the family breadwinner, he felt useless being unable to provide for his wife and daughters. He longed to be of service to his family and their barangay as a kagawad. Yet here he was, detained for his illness. What words of comfort could I have told him, other than to say that his cooperation and confinement was for his family’s sake? Photo by Isabel Acosta 1 See Glossary 115 On another occasion, I granted the request of a daughter to let her dying father hear a voice message they sent in by phone. Beside the unresponsive old man, I played the audio file on loudspeaker. I listened to the daughter say, “Pa, sorry.” Her voice cracked. “Sorry po na hindi kami makapunta diyan. Gustuhin man namin makapunta, hindi kami puwede makapunta diyan.” Tears flooded my eyes and dripped down my face. Being in PPE1, I could not even wipe them. I sobbed as I listened to that five-minute recording. I felt helpless realizing that there was nothing I could do to comfort this man’s family. Under the usual circumstances, we would allow the patients’ loved ones to come in, to be by their side and to bid farewell. Yet in this extraordinary situation, we could not afford to grant even that simple request. When the moral wounds are fresh, we may not notice them because of the adrenaline. Only when we retreat and confront what happened do we feel the pains. What else could I have done? Was it a system failure? Guilt rings true; fear, anger, and hopelessness can crush. The imposed isolation made it even more difficult to process our emotions. As one nurse in New York related crying in a viral video, sometimes we cannot even process our experiences with our family because they would worry, and we do not want to be a burden to our colleagues who may also have too much on their emotional plate. Who comforts those who are used to comforting others? The truth is that the healer needs to be comforted, too. The patients die alone. They slip away without the solace of their family, without a final hug, without a whisper of goodbye, without even the last rites. We are left asking ourselves: What more could we do? Our souls are disturbed. Our spirits are broken. Everything was unsettling In recent years, this phenomenon has gained a name. It was first described in soldiers who came close to real danger and faced their mortality in ways difficult for the ordinary person to fathom. It is called moral injury, and for us healthcare workers, we face this when we “know what care our patients need, but… are unable to provide it due to constraints that are beyond our control”2 . Despite doing the best we can, we feel that whatever we do will never be enough. See glossary Dean W, Talbot S, Dean A. Reframing Clinician Distress: Moral Injury Not Burnout [published correction appears in Fed Pract. 2019 Oct;36(10):447]. Fed Pract. 2019;36(9):400-402 1 116 Sustaining wounds while fighting may be inevitable, especially in the present circumstances, but maybe we can at least ease the pain. To do so, we first have to recognize it. Pain, we were told in medical school, alerts us of actual or potential damage. We are wired for preservation. Perhaps at this time, we are being warned of the risk of losing things valuable: our own humanity, our capacity to recognize innate dignity, our ability to care for others, our capacity for love. The cascade of pain signals cannot stop at the site of damage. It must reach the head, else we will keep our 2 hand on the stove and burn. The reaction to the noxious stimuli should not only be initiated individually, but also collectively. Our leaders and mentors therefore need to attend not only to the physical requisites, but also look after the emotional and spiritual well-being of those grappling with the somber realities of the COVID-19 frontline. War is dehumanizing. In the raging battles against COVID-19, what echoes is the silence of inner suffering. The broken spirits have to be mended, so we can continue to live up to our calling to help and heal others. Copyedited by: Amanda Christine F. Esquivel and Gabrielle P. Flores Photo by Brent Viray 117 Pain, we were told in medical school, alerts us of actual or potential damage. We are wired for preservation. Perhaps at this time, we are being warned of the risk of losing things valuable: our own humanity, our capacity to recognize innate dignity, our ability to care for others, our capacity for love. Photo by Isabel Acosta 118 Mama Gabrielle P. Flores “Ito talaga calling ko eh,” he shrugged. Under the scorching sun in the grimy Manila humidity, with nary a functioning fan in sight and only a flimsy tarpaulin tent to offer shade, Dr. Krystark swabbed one patient after the other. Tark, as friends call him, is a dentist. He is one of the first UP dentist-volunteers to augment PGH’s workforce for COVID-19 testing. When elective procedures1 were cancelled, Tark stayed in the comforts of his family’s home. But this reprieve from dental duty did little to calm him—quite the opposite, actually. Every day, he watched the numbers balloon. Every day, his unease grew. “Hindi ako mapakali na nakaupo lang ako.” Seemingly endless days filled with frustration and longing for purpose dragged on, until he received a phone call from the president of the UP Dental Alumni Association. It was a call to duty. Without a second thought, he jumped at the opportunity to be a PGH volunteer for COVID testing. Ironically, it was the prospect of being in the frontlines that calmed his frayed nerves. Like applying a salve to an unbearable itch, it afforded him a sense of peace. 1 See Glossary 119 Tark’s parents are devout Catholics, and they prayed together as a family every night. That evening, they prepared for their nightly routine as they always did, but Tark knew this night was different. Before a single word of prayer could be uttered, he gently looked at his mother and said, “Ma, hindi na ‘to kaya ng doktor lang. Kailangan na ng mas maraming tao.” His mother had never prayed as fervently as she did that night. Tark soon after made his way to PGH, and joined the ranks of the volunteers who took samples from patients. Though fully decked in protective gear, and properly trained to perform the procedure safely, the conditions were often uncomfortable, and still carried some exposure risks. While his mother stormed the heavens for her son’s safety, Tark started off on his first shift. One of his patients introduced herself as a PGH nurse. Before Tark could start the process, she hesitated and admitted, “Teka… iyakin ako.” True to her word, her fear surfaced as her eyes welled with tears. “May baby akong bine-breastfeed.“ Tears rolled down her cheek—one by one, then all at once. Photos by Brent Viray 120 “Pa’no ko siya papakainin? Sinong mag-aalaga sa kaniya?” “Ito talaga calling ko eh.” He was trained for the job. He thought he had anticipated every possible situation, but he wasn’t prepared for this. How does one comfort a mother’s aching heart? Under the scorching sun in the grimy Manila humidity, with nary a functioning fan in sight and only a flimsy tarpaulin tent to offer shade, a mother wept for her child. Miles away, a mother clasped her hands as she pleaded with God to keep her son safe, each prayer was said more fervently than the last. These two women have never crossed paths, and yet, at that very moment, they shared the same pain. Photo by Krystark Gomez 121 Lost to Follow-up Anna Elvira S. Arcellana Mr. PM’s follow-up instructions read: Last seen March 13, 2020. To be seen at the OPD (Outpatient Department)1 with laboratory results on April 16, 2020. The April 16 appointment never came. Beginning March 16, 2020, the usually crowded hallways of the OPD became deserted. Lines disappeared. What used to be a cramped parking lot filled with vans and ambulances carrying patients from far-flung provinces became a glaringly empty space, and the dusty windows gave passersby glimpses of a now bare OPD. Mr. PM, a 56-year old with thyroid cancer, was just one among thousands of patients who felt the heavy weight of the OPD doors closing in on them. The fear of the department being unable to continue its essential services due to the dangers of transmitting COVID-19 had been lingering in their minds for weeks prior to the lockdown1. And, as they had feared, the doors had to close swiftly, one could say almost harshly, in the interest of saving more lives. 122 1 See glossary As April 16 drew nearer, Mr. PM sent anxious, almost frantic, text messages to me daily. “Lockdown po, paano na po ang follow-up ko?” “Hindi na po nagawa ang post-therapy body scan, paano na po mababantayan ang kanser ko?” His burning fears emanated from the embers of his recurrent and metastatic thyroid cancer; he had to undergo radioactive iodine therapy twice, unlike most patients in whom only one dose is enough. Patients with differentiated thyroid cancer have relatively better prognosis than patients with other types of cancers, but this fact did little to allay Mr. PM’s fears. Because of the lockdown, Mr. PM missed a test essential in the monitoring of his treatment response. That missed scan was a handicap in the management1 of his disease. We could get by with the information that we currently have, but his situation was still far from ideal. Because of the closed OPD doors, struggling patients like Mr. PM were not only bound to miss laboratory examinations and clinic visits, more alarmingly, they’re likely to miss medications as well. Mr. PM was a determined individual with a strong health-seeking behavior and a desire to conquer cancer, and he was keen on battling his disease—whatever it took. Mr. PM’s next text update was heart-rending. With his elderly body scarred by cancer, he walked four kilometers under the scorching heat from his home in Sta. Maria to Bocaue, Bulacan to buy Levothyroxine2 and calcium tablets. He has to rely on these two essential medications for life, and walking this overwhelming distance was his only recourse. Pharmacies that were both open and well-stocked were few and far in between. The long distances are magnified several times over by the lack of public transportation. With Mr. PM’s tragic message, I felt powerless, fumbling for words of consolation and comfort to offer a wounded soul. With most laboratories closed, pharmacies running out of stock, medical supplies reaching critically low levels —patients, even those who are free from COVID-19, are bearing the brunt of this crisis. Mr. PM may feel desolate and alone in his struggle, but he is hardly the only one. More and more patients are facing the perils of interrupted care. Sadly, while they may all be sailing against the wrath of the same enormous storm, many still feel alone: in vastly different boats kept at socially-distanced lengths from one another. Meanwhile, there was Ms. MC, a 24-year old pregnant woman with uncontrolled young-onset diabetes mellitus and hyperthyroidism, striving to cope with difficult medication adjustments because of the absence of guiding laboratory tests. Everyday, she worries about where she can safely deliver her baby. Some patients have had to put their definitive treatment on hold. Ms. CP, a 34-year old female with a large mass on her pituitary gland3 secreting excess growth hormone, was slowly losing her vision. She was also suffering from diabetes: the metabolic consequence of the disease. The cure is surgery, but it was postponed with no final date in sight. The last time I saw Ms. CP, she was in tears. The pituitary mass was already giving her bouts of headaches, and she had already waited years for this potentially curative surgery. I could only share her tears because the end of her waiting time was still so far out of reach. Levothyroxine, L-thyroxine. A manufactured form of the thyroid hormone thyroxine (T4). This is a medicine used to treat a patient who is diagnosed with an underactive thyroid gland (hypothyroidism) or has had their thyroid gland completely or partially removed. 3 The pituitary gland is a small mass of tissue nested in its own groove at the center of the base of our skulls. It controls important metabolic processes through the secretion of hormones. Any growing mass within the skull would cause headaches that could bring anyone to their knees. A growing mass specifically on the pituitary can disrupt carefully coordinated metabolic processes such as bone growth, and anatomical relations, such as visual tracts. There are no medicines that could permanently take the headache and those vision problems away--only surgery. 2 123 Sadly, while they may all be sailing against the wrath of the same enormous storm, many still feel alone: in vastly different boats kept at socially-distanced lengths from one another. There’s also Ms. AR, a 53-year old breast cancer patient with diabetes, striving not to miss doses of her chemotherapy and insulin. Ms. AR works as an elementary school teacher, and with schools closed, her source of income was threatened amidst her battle with breast cancer. continuity of tertiary-level care. A video call cannot fully replace a face-to-face encounter or a consoling tap on the shoulder, but it still forges a connection that we commit to never break. These stories of arduous struggles continue to unfold, and innumerable faces take part in an almost never-ending narrative. For some patients, however, the only answer we can offer is deafening silence. Those stuck in far-flung places, without mobile or internet connections, remain unreachable. How about these patients whom we have lost contact with? Their untold stories, the unknowns, make us fear for the worst. As doctors, we strive to comfort those who tell us of their distress, and we labor to reach the unseen and the unheard. Weeks into the ordeal, rays of hope have emerged. Telemedicine resurfaced and provided an avenue to hold consults, send words of encouragement and support, and replenish prescriptions while clinics remain closed. The various subspecialties of Medicine, Endocrinology being only one of many, opened their own hotlines to ensure the 124 “Paano naman kami?” Still, each new day offers the chance of reconnecting with another patient. There is still hope that the lost may find their way back to care. As doctors, we strive to comfort those who tell us of their distress, and we labor to reach the unseen and the unheard. Empty chairs line the emergency room hallway in preparation for the surge of COVID patients. Photo by Brent Viray. Copyedited by: Gabrielle P. Flores 125 Uncarved Pieta Athena Mae Ibon Alvior Hall1 is a modest building that has been used for different purposes, in response to the exigencies of the College of Medicine, over the years. It has now been chosen to store the donations being sent to PGH. The area’s location was strategic, being removed from the main hospital and thus with less risk of exposure of staff and donors. For a month or so, Alvior Hall embraced the bulk of donations, with at least five volunteer medical interns2 and doctors handling, recording, and channeling these. I found my way to Alvior Hall, having volunteered to help out in the work there. I grabbed the golden doorknob of a varnished wooden door. The door opened to a crowded hall filled with donated supplies— masks, isolation gowns, hazmat suits, handmade face shields, hygiene kits, underwear, and a lot more. My heart softened, seeing how people had selflessly forgone their material wealth to respond to the needs of frontliners. As I entered the room, I was given a brief orientation by a co-intern on certain tasks in the area. To be honest, I had fun on my first day; it was a good change from the lazy quarantine1 routines. “Guys, kuha kayo ng food. Kain muna kayo ng breakfast. O, may juice at sandwich pa!” offered one of our co-interns. “Hello po,” I moved closer to her. “Pwede ko po ba kayong makausap?” Up close, she seemed warm and welcoming, but I could feel her aura was that of a worn out machine. Elvira is 54 years old with three children and two grandchildren. Seated next to her was Jesusa, a 55 year-old woman with a boyish demeanor. Both of them started working in PGH as maintenance personnel in 2001: effectively rendering 19 years of service. “Kumusta naman po kayo sa trabaho?” I asked. “Mahirap,” they both replied. Alvior Hall. A building within the campus of the University of the Philippines - Manila, College of Medicine. It holds various housing conference rooms, and offices. During the COVID pandemic, it was converted into a donation center for the Bayanihan Na! Operations Center. 2 See glossary 1 126 I was seated comfortably with my friend, Al, when I noticed the middle-aged woman sitting down on a plastic stool at the corner of the room to my left. She was staring blankly while leaning back against a cabinet. She was wearing a blue scrub suit, a disposable face mask, and rubber slippers, with her hair a little unkempt. But what really caught my attention was her moistened eyes and pained expression. It was not merely the nature of work they found hard, but the circumstance they were in. “Sa trabaho hindi magkaparehas, minsan toxic 2 , minsan tamang-tama lang,” they added. Before the pandemic, they were assigned at the OPD2, which has been closed indefinitely. In the meantime they have been assigned outside the COVID wards, just so that they remain readily available once the OPD reopens. Should they be exposed in the COVID wards during their shift, they too would be quarantined, leaving the staff even more undermanned. “Ma’am? Sorry po?” “Hindi na po ako umuuwi,” she wistfully said. “So, saan na po kayo natutulog?” I questioned. “Tatlong araw na po akong naglalakad, apat na oras din bago ako makarating sa trabaho. Ganun din sa pag-uwi,” Elvira said while pointing at her feet—swollen, with abraded marks on each surface from the friction of her worn-out rubber slippers. “Nabasag ko na po ang aking pigg y bank,” Jesusa claimed. She used the money to buy a bicycle online for ₱2,000. By foot, she arrives to work in an hour or two; by bike, her travel time is cut by about 45 minutes. “May vitamins din namang naibibigay. Pero nakakapag-absent talaga, lalo na sa unang araw ng paglalakad dahil sa pagod,” Jesusa added. Working was the only option because they had no paid leaves left. These institutional workers claimed to not having received hazard pay, and they too were denied eligibility of DOLE’s cash aid. Soft mumbled words caught my ear, I shifted back to Elvira. 2 See glossary Photo by Gianne Pagulayan 127 There was a brief pause. A few days ago, our auxiliary workers spent nights beside flashing red and blue lights with the ringing of the ambulance sirens. The first nights were traumatic and sleepless. “Nagsisiksikan kami sa opisina. Natutulog kami sa hapag ng karton. ‘Pag mamatay…’pag namamatay… at ‘pag patay na… kitang-kita ng dalawang mata namin bawat pasyenteng dumarating, nahihirapan, nagbubuntong hininga.” The dread, concealed anxiety, and unexpressed trauma were conveyed by the cracks and shivers in Elvira’s voice. “Natatakot po kami.” Being able to go home later, she recalled, was small consolation. After having to walk for four hours, Elvira arrived home. She remembers the event vividly. She halts, then clings on to the bars of their gate. She is now home—where her family is within view, a hand wave apart, and six feet away from a warm and tight hug. And six feet it must stay. “Hindi po ako makakalapit. Hindi rin ako makakapasok. Takot po ang mga residente sa akin. Ayaw ko rin naman manghawa sa pamilya ko,” Elvira spoke Even the Blessed Mother was able to hold her only son when they brought Him down from the cross, her sorrow carved into immortality in Michelangelo’s Pieta. But this mother, walking back to the hospital, has no solace. Heroes are the frontliners who, while bearing their own crosses, bravely face the world in masks and shields. In the midst of piles of medical supplies in an inconspicuous building and away from the tumult of the battlefront, I found them. She halts, then clings on to the bars of their gate. She is now home—where her family is within view, a hand wave apart, and six feet away from a warm and tight hug. And six feet it must stay. 128 Photo by Trixie Bacalla Photos by Amanda Oreta The Dr. Gregorio T. Alvior Hall, a small two-level annex behind Calderon Hall (UP College of Medicine), was often used for alumni meetings, small department or student gatherings, and office space. When the pandemic hit, it was designated as the PGH Bayanihan Na! Donations Center. Everyday, volunteers receive, inventory, sort, and repack countless boxes filled with food, PPE, and material donations coming from the government, individual donors, public and private groups all over the country and abroad. 129 Photos by Denica Tan Yu 130 Photo by Trixie Bacalla Photo by Ven Ponce 131 Laru-laruan Athena Mae Ibon “Doktora! Teka lang po, teka lang! Hinahabol po kami ng pulis!” These pacing words rang over my ears on the phone. The call was then dropped. The sun had gone down. Streets were busy and crowds were rushing in panic. “Lockdown1 na daw po!” People chased time before the clock ticked six. I entered my room, took my seat, immediately searched for my phone to call again. I got to three rings, but the phone on the other line wasn’t picking up. I woke up early the next day, and tried again. Finally, this time, I heard an answer. “Hello po, Doktora. Pasensya na po at hindi ko po kayo nakausap nang maigi.” Jonel, as she wanted to be called, was 30 years old, and all by herself, took care of her widowed 73 year-old father, a niece, and a nephew—Rose and Nick—both of whom were orphans. Rose, 14 years old, had been one of the patients assigned to me during my pediatric internship1 rotation in PGH. She was struggling to breathe when she was admitted— dyspnea from severe angioedema and glossitis. She had several excoriations from head to foot with discoid lesions 132 1See glossary and thinned out hair. Everytime a question was thrown at her, all she gave was a blank stare. The only sounds she could make were incomprehensible. She was accompanied by her grandfather, who stood slouched, and couldn’t walk properly due to low back pain. He could hardly answer us when we asked for details about Rose’s sickness. It made my heart ache to see him walk in pain every time he got back from hours of lining up to get Rose’s medication. When I asked about Rose’s parents, Tatay, as I called him, answered “Namatay na po sila limang taon na ang nakakalipas. Nagkasakit, at dahil wala po kaming pera, ay hinayaan nalang namin hanggang sa sila na ay tuluyan nang pumanaw.” Every time I approached her bedside, people would stare in disgust as flies hovered around her pungent space. “Tatay, punasan po natin ng basang bimpo si Rose. Kayo po ba ay nakaligo na rin?” I would ask, even as I wondered if there was indeed a place for them to bathe and change. After a series of examinations, Rose was diagnosed with Systemic Lupus Erythematosus (SLE), in flare, with concurrent pneumonia1 in an immunocompromised host. She was treated with antibiotics and steroids2. My resident-in-charge1 told me how compassion can hasten healing—with Rose, I got to see the truth of those words myself. On the third day, Rose was already trying to form words. After five days, she gave a hoarse whisper, “Ate.” After Rose’s first discharge from PGH, she was able to work as a computer shop attendant—being paid two thousand pesos a month with meals covered. Rose got better. At least for a time. “Doktora, pasensya na po, pinapaalis po kasi kami ng pulis. Tumatakbo kami ng gabing iyon kasi pinapaalis na kami at kinukuha po ang aming mga gamit,” she explained. Jonel, along with her extended family, lived on the streets of Blumentritt. I thought of Tatay limping away, his back aching. Mostly, I thought of Rose. During this COVID-19 crisis, they had been affected by the shortage of medications, specifically Hydroxychloroquine3. This was the medicine for her SLE but was, at that time, being considered as an off-label treatment option for COVID-19. When I called, Rose had missed her medications for two weeks already. Jonel said that they were about to go to PGH for Rose’s readmission, but due to the lockdown, couldn’t get past checkpoints. I had to inform her that PGH had already been turned into a dedicated COVID-19 hospital—her fifth admission for therapy would likely be postponed. I felt a surge of worry as I asked about their situation, but before we could move forward, the call got interrupted. There was a loud noise, a commotion. We temporarily dropped the call and when we reconnected, I asked, “Ano po ba ang nang yari?” “Nagtitinda si Nick ng laruan sa may tapat ng simbahan. Apat na libo po sana kada buwan ang kita pero dalawang buwan na, ay isang libo na lang ang binibigay. Kadalasan pa ay hindi siya sinasali sa mga pinapakain.” See glossary Systemic Lupus Erythematosus (SLE) is an autoimmune disease where the immune system attacks the patient’s own body tissues. The widespread inflammation and damage can cause the patient’s symptoms including the inflamed tongue (glossitis) and recurrent episodes of swelling of the face or the body (acquired angioedema). The swelling can make breathing difficult. Medical interventions and lifestyle changes can help control SLE, but there is no cure for it. 3 Hydroxychloroquine. HCQ is one of the therapeutic drugs that has been studied for the prevention and treatment of COVID-19. When the drug was reported as a potential treatment for COVID-19, many people bought this drug, causing a decrease in the supply. The treatment studies for HCQ were later discontinued because the initial data showed no improvement in mortality rates. 1 2 133 “Wala na rin po kaming makain. Pinapalipas na lang namin ang araw. Di na po kami nakakapagbenta at hindi rin kami nabibig yan ng ayuda. Kahapon ay pumunta sa pindutan4 pero zero balance po ang card namin kasi hindi daw kasali sa tutulungan yung mga walang mga anak na pinapaaral. Lalo po kaming nahihirapan ngayong panahon ng COVID-19. Tiis-tiis na lang po hanggang sa may darating na tulong.” These scenarios are the painful scars that line the archipelago of the Philippines, much like excoriations with discoid lesions on a 14 year-old child with SLE. These may be scars of endurance, but also mean worsening disease. The hunger games of this crisis cannot be overlooked. The poor will get poorer; the hungry, hungrier; the sick, sicker. “Teka lang po, teka lang!” Hanggang kailan ang habulan? Hanggang kailan ba tayo maging larularuan? Like how one person might call all photocopy machines “Xerox”, it is not uncommon to hear Filipinos substitute an object’s name with a word that best encapsulates their own experience or associations with the said object. For this family, an ATM is pindutan, named for the number pad one has to press to make transactions. 4 134 Suntok sa Buwan Athena Mae Ibon Scattered leaves sweep through shriveled ground as northern wind passes by. The surrounding air is warm and dry, but the sweet, soft breeze sings along during siesta. Mang Leigh, 34, sits on a wooden chair outside his doorstep. He dons his mask and breathes deeply as he listens to the subtle sounds of nature. The view is calm, but he misses the loud cheers of children playing. This is no longer one of the ordinary days. Mang Leigh sits with apprehension as he recollects events that started in 2009. “Napapansin ko na lang na may nakakapa akong bukol sa bandang kaliwa ng tiyan ko,” he started. The mass became bothersome. His older sister advised him to consult a hematologist, and so he went to PGH. Mang Leigh, a tricycle driver and a father to three, was diagnosed with chronic myelogenous leukemia (CML)1. “Tinatabi ko ang konting pera galing sa kinikita ko para sa aking gamot.” Mang Leigh only earns ₱500 a day, but he needed to take a total of ten Imatinib 400 mg tablets2, costing him around ₱14,000 a month. “‘Overshort’ na rin kami sa gastusin at kinakatakutan ko talaga na mamaga ulit ang spleen ko,” he adds, referring to the splenomegaly associated with CML. He was scheduled to follow up on April 3, 2020, but the circumstances changed due to the COVID-19 crisis. “Ngayon na lockdown na, ay di na kami makapagbiyahe. Nakakakain kami galing sa konting tulong-tulong dito sa barangay,” he expresses. What worries him most is that the unseen enemy attacks those with weak immune systems; he himself is at high risk because of his cancer. Last year, he had already been admitted due to pneumonia3-a consequence of his immunocompromised state. In their home, meticulous preventive measures are observed to avoid contact with the virus: frequent handwashing, segregating items which could be fomites3, and observing a healthy lifestyle. Mang Leigh, a man battling cancer amid this COVID-19 crisis, and who barely has funds to support his family’s needs, still manages to say: “Masaya po ako, na kahit ang karang yaan man ay suntok lang sa buwan, huwag po tayong makalimot sa Itaas. Maging masaya at magpasalamat sa arawaraw. Kahit papaano, masuwerte ka pa rin kasi nagigising at nabubuhay ka pa rin sa bawat araw.” We all have our own trepidations in these times. But a humble man, faced with a more daunting situation, has the serenity of acceptance, if not selflessness. “Kahit ako na lang ang matamaan, huwag lang ang sino man sa aking pamilya,” he said. “Bawat araw, kailangan nating magdasal at lumaban para ang lahat ng ito ay ating malagpasan.” Chronic Myelogenous Leukemia is a type of bone marrow cancer which causes the increased formation of abnormal white blood cells. Imatinib is an oral medication that is used to treat certain types of leukemia and other disorders/cancers of the blood cells. It works by preventing the proliferation of cancer cells. 3 See glossary 1 2 135 This man’s spirit made me realize that while those who live comfortably can feel immense discomfort, simply having a life to live, for those without such luxury, becomes an absolute comfort. Thank you, Mang Leigh. I needed this reminder. Photo by Maria Keziah Legion 136 From Fighting Cancer to COVID-19: The Battle is Not Over Mikki Miranda I was halfway through my senior residency when I was diagnosed with cancer in 2019. The night before my surgery, I called our chief resident1 telling her that I had to go on leave for an indefinite amount of time. That “indefinite amount of time” turned out to be nine months where I underwent six grueling cycles of chemotherapy. And since chemotherapy1 rendered me prone to getting sick, I couldn’t go to work and finish my residency. I wasn’t able to graduate with my colleagues. All plans, whether career or travel, were placed on hold — indefinitely. I was optimistic, though. Maybe after fully recovering I can start working again without fear of catching something. Thankfully, I went into remission. I started writing a postcancer bucket list to celebrate the year 2020, knowing I have a new lease in life. Well, fast forward to this year: the COVID-19 pandemic began. While most people were still getting used to the “New Normal,” I realized I was already “quarantined”1 back in 2019—before COVID-19 told everyone to stay at home. “An Ode to Filipina Frontliners” Mixed Media, 2020 By Mikki Miranda 1 See glossary. As a cancer patient, I could not go out of the house without wearing a mask. This was the time when wearing a mask on the street was meant for sick people or celebrities. Also, I had 137 to stay clean every single day, every single time. When I craved food, I would have to buy from a delivery service. I couldn’t go out and eat in crowded restaurants. And my parents had to ensure the food served was neither raw nor under-cooked. Too bad, I loved sashimi. Apart from the physical toll caused by chemotherapy, there was the constant mental torture of having no control over my own life. If I had to go out of the house, it was because I had to go to the clinic to receive chemo or have blood tests or scans done. This meant I spent long, long days at home. Time felt really, really slow. I had many days where I just stared out the window and watched the day eventually turn to dusk, then to dark. I was able to witness seasons change. I saw how a tree slowly grew its flowers, then saw its leaves wither and fall, and finally, grow new leaves again. Yesterday was the same as the next day; most of the days looked exactly the same. But then again being under “quarantine” had its quirks. I found ways to entertain myself. I watched so many movies and TV shows that I grew sick of watching them. I tried “studying” again but didn’t feel any volition if there wasn’t any guarantee of going back to normal. I was only allowed to take in a few visitors at home, and they had to make sure they were not sick. Since most of my friends were doctors working at the hospital, we had to carefully coordinate a visiting plan where everyone was healthy and cold-free. Their visits were brief, yet fun, and I entertained them by showing my different wigs. I discovered so many hobbies. I learned how to paint just by watching people on YouTube create art in the comfort of their own homes or studios. I practiced painting all the mundane things I see in our house: our family dog, the fruits and vegetables I eat, old vacation photos, and the flowers that grow in the garden and on the porch. When my skills improved, I gave them to my generous patrons: my dad, my mom, my siblings, my family relatives, and my friends. And then I gave one to benefit cancer patients like me. Most people don’t know that some great painters of history thrived while being under “quarantine.” Frida Kahlo was bedridden and battling a spinal injury when she started painting her powerful self-portraits. She planned to study medicine, but she was severely injured due to a bus accident. During her lengthy recovery from her spine and pelvic injury, she turned her energies into making provocative art. In order to adapt, she had an easel and mirror attached to her bed. That is why she made a lot of self-portraits. 138 I guess that the arrival of the COVID-19 pandemic made a lot of people turn to the same things as I did during my mandatory quarantine back in 2019. Many have started their own “Frida Kahlo moments” and started diverting their pandemic anxieties into artistic endeavors. A some-sort-of routine at home made them regain control over the anxiety brought by the pandemic. Most friendly gatherings are now brief, and most times done in the online cloud. And like all cancer patients are supposed to do, everyone started to wear masks in order to protect themselves from acquiring a terrible infection. In the two months of ECQ, time felt really, really slow for them, too. This pandemic forced a lot of us to contemplate about time. Much like the “butterfly effect”, the pandemic forced us to look at time in both ways: retrospectively and prospectively. Retrospectively, we contemplate on the choices and actions we made in the past year and see how they have reflected into our lives during this pandemic. Like, for example, if a person had chosen to stay in a job that affords work-from-home arrangements instead of resigning, it would have made a difference in their ability to financially survive this year. Or if I would have been diagnosed with cancer this year, maybe my family and I would have had a more difficult time getting treatment. The children’s playground in front of the Department of Rehabilitation Medicine stands silent as fewer outpatients are allowed into the main building due to the COVID pandemic. Photo by Maria Keziah Legion 139 Prospectively, we contemplate on the decisions we plan to make with respect to the following months and years to come. All excitement about traveling and exploring the world is very much replaced with fear of traveling even to the nearest crowded shopping center. We now think about making decisions that could impact our lives in order to survive in the long term. It becomes even harder to contemplate on the situation if you are a cancer patient. People with cancer shouldn’t have to suffer and die because protocols get delayed or they can’t get a scan because of restrictions. Just like viruses, cancerous cells don’t rest during a pandemic. This so-called “new normal” is something people will have to live with for a long time. And yes, this new normal doesn’t feel new at all to me since I was a shut-in for nine months. But for the most vulnerable among us— we simply cannot let this be their “normal”, too. And it depends on the majority to be socially responsible in order for the rest of us to survive. The battle is not over. As of this writing, Dr. Mikki Miranda is a graduating resident at UP-PGH. 140 Pinagtagping Tahanan1 Gabrielle P. Flores “Are you sure you want to do this?” “For heaven’s sake, Rochelle! I’m not even 60 yet!” With a virus that hits harder the older you get, Dr. Rochelle’s trepidations were fair. Dr. Boncan, head of St. Luke’s dentistry department and father of five, had just signed up to be a volunteer nasopharyngeal swabber2 in PGH. And Dr. Rochelle “Chelle”, his colleague, had called him to question his decision for a third time. It made sense for him to volunteer. He knew about infection control—the subject of which he used to teach at the UP College of Dentistry. He was no stranger to occupational risks, either. Dentists have one of the highest occupational risks for practically any infectious disease—COVID-19, included. Photo by Brent Viray Despite the logic, the image of losing a colleague and leaving five kids fatherless, under a program that she facilitated as the president of the UP Dental Alumni Association, left Doc Chelle with a bitter taste in her mouth. Doc Chelle had always been cautious. Her pre-pandemic clinic was pristine: appointment-only, referral-only, and with a pre-consult phone interview to boot. Scenes from the COVID Triage and Swabbing Station placed just after the Padre Faura entrance of PGH. Photo by Jonas Del Rosario Named after one of the songs produced by the author’s class UPCM Class of 2021, Pinagtagping Tahanan is about an unlikely family formed in the middle of Malate. The song was part of UPCM Class of 2021 stage musical entry “P.I. (At Iba Pang Mura Sa Mundo)” to the annual interclass stage play competition in 2018. 2 See glossary 1 141 Her impressive safety measures in much fairer weather should have been indications that she would not take this volunteer program lightly. “She told me she wanted to cry when I said I was volunteering,” Dr. Boncan said, laughing and shaking his head. And cry, she did. In the nights that led up to the program’s launch, she was tearful and sleepless. Doc Chelle could not deny, however, that she needed him onboard. The team she had put together from a Facebook post on the UPDAA page had swarms of interested volunteers. But transportation, comorbidities, and cold feet whittled the roster down to just four dentists: Dr. Krystark “Tark”, Class of 2011 and civilian dentist for the navy; college friends, Dr. Eula and Dr. Thea, Class of 2013 and a private dental associate and Masters student in the middle of writing a thesis; and Eunice, Class of 2019, a fresh grad just starting out. This bunch was tenacious, one could say even stubbornly so. Dr. Boncan, a gentle, soft-spoken professor who seemed to always speak and move with purpose, served to temper the team’s energy. His addition proved to be invaluable when they saw the initial state of PGH. It was chaos. Swabbing2 turned out to be only a tiny fraction of their job. The mound of complex paperwork and logistical hoops that accompanied each patient towered over the team. “We had to do everything,” Thea recalls. Their first home base was “Phi walk,” a small bricklined path at the entrance of Padre Faura St. that led to a pavilion next to PGH’s Spine Unit2. Black wrought iron rails sectioned the area from the driveway and parking lot it faced, but besides the rails, nothing else served to partition the swabbers from the elements of nature. They all watched their lives jerk to a halt when the pandemic peaked and most dental services in the country were forced to close. They were smart, voracious learners; quick to jump at the opportunity to volunteer. But they were young. Eunice, the youngest of them all at 22, confidently declared, “I’m not 18 anymore,” when phoned by Doc Chelle to ask if her parents were aware of her volunteering. Photo by Steff 142 2 See glossary The breeze was welcome. “Iyong Level 4 PPE2, parang sauna suit,” said Tark of the heat he felt under complete PPE. “Pati sapatos ko puno ng pawis!” Any semblance of ventilation is a treat for someone constantly hungry for air. But the viral media bottles, clinking dangerously like chimes when a breeze blew past, were less amenable to the gusts of wind. And so they moved to the PGH Chapel. Then moved to the spot outside the ER. And again to the lot outside the Ambulatory Care Unit. “The directives changed literally everyday,” Eula said. Like pollen, they moved with the changing winds, with Dr. Boncan at the helm. And just like the seeds, they bloomed where they were planted. Very quickly, they established their own little routine. Dr. Boncan would always volunteer to swab first, setting an example of proper technique. “It was like having a clinical professor around,” Thea remarked. An educator herself, Thea was equal parts embarrassed and grateful when Dr. Boncan called her over to correct the angle at which she directed the swab. Eventually, their hands grew accustomed to the process. Despite the nasopharynx being “uncharted territory” for the young dentists whose comfort zones were bordered by the confines of the mouth, muscle memory kicked in. When Eunice came in as a late addition to the team, Eula and Thea made sure to show her the ropes. “Students her age are usually my students, and she was such a trooper,” Thea 2 See glossary Photo by Steff 143 recalled. With a propensity to fainting spells and a vicious intolerance to heat, Eunice pushed through a day’s work in full PPE, all while trying to conceal the episodes of tunnel vision kicking in—a warning that she was about to faint—from the rest of the team. While she may have succeeded at hiding the spells, her heat intolerance did not go unnoticed. Laughing good-naturedly, Thea conjures the image of Eunice’s first time to doff2 the PPE. Her hair, matted with sweat, clung wildly to her face as she emerged from the PPE’s hood; she looked like she had taken a plunge in a pool. Like a well-oiled, albeit makeshift, engine, they chugged along the days the best they could. Day in and day out, a cacophony of spluttering, coughing, and violent retching serenaded the swabbers as they inserted a long cotton swab into patients’ noses, pushing it back until it hits the sweet spot: the nasopharyngeal wall, an exquisitely sensitive patch of tissue. They would deftly swirl the tip, triggering the nerve endings to go into a frenzy of ticklish pain. They’d pull the swab out. Only to repeat the process in the other nostril, much to the chagrin of patients who, at this point, are often gagging and in tears. “I’ll equate it to having accidentally breathed in water from a pool,” Dr. Boncan said of the experience. Photo by Ephraim Leynes Photos by Brent Viray Swab. Sign. Repeat. 144 2 See glossary The monotony of the days was broken by Doc Chelle’s regular check-ins. “Doc, don’t worry! We’re big girls,” Thea assured her through the phone. But old habits die hard, and when Doc Chellle caught whiff of her alumni struggling to find places that served lunch, a massive effort was coordinated with other dental alumni to bring them cooked meals, everyday, without fail. “Tatawagan ko pa yung guard. Tatanungin ko: Guard, nadala na ba?” Doc Chelle admitted. She steeled herself against comments that she was babying her alumni, saying, “I’m not going to deploy them like soldiers, unprepared for battle. If I can cover all the bases, I will.” The meticulous coordination that went on behind the scenes did not go unnoticed by the “Swab Squad.” “She’s the most protective person I know,” Eunice admits. This unlikely grouping of people looked out for each other. They had to. When their very profession was suspended in limbo, and the nature of their normal work far removed from that of the medical doctors in the hospital, they naturally clung to the familiarity of each other. In whispers outside his earshot, the younger dentists would call Dr. Boncan “dad.” Perhaps unknowingly, he took the role in stride. He picked up Eula and Eunice when rides were scarce. He gave Thea a pep talk as she was about to swab an important figure in the hospital. Photo by Steff And he always tried to volunteer first when a swabber was needed. Knowing this, Eula recalls how they tried to game the decking system to limit Dr. Boncan’s exposure; they looked out for him, too. Doc Chelle never failed to make her presence felt—even from a distance. In their one-week stint that extended to almost two months, Tark, Eula, Thea, and Eunice were regularly given getout-of-jail cards by Doc Chelle. “If at any point, even just 30 minutes in, you want to stop. Just tell me, and I will pull you out of there,” she told each one individually. But they all chose to stay. How could they not? Their sense of pride in their duty was swathed comfortably in the blanket of security Doc Chelle and Dr. Boncan gave. And so, in the shade of the swabbing tents, basking in the symphony of sounds, the air hanging heavy with spit and snot and sweat, this family of dentists settled into their new home: each other. 145 Finding a Path in Crisis Maria Angela M. Villa Last February, my chief resident1 asked me to attend the PGH Physicians’ Association (PGHPA) election as the representative of the Pediatrics Department. There, I was voted the PGHPA president. I thought to myself: given a position of tremendous responsibility, what can I possibly do to help our doctors? The PGHPA stands as the collective voice of more than 600 residents and fellows1 of the hospital. How can we, as an Association, truly represent our doctors and take better care of their welfare? Less than a month later, the COVID pandemic arrived in our country—and this same question, and other equally pressing ones, gained additional importance. At the onset of the crisis, when PGH declared war against COVID-19 by assuming the role of a COVID referral center1, it was chaos. There were numerous new policies, duty1 schedule revisions, postponed lectures, fewer patients, lesser colleague interactions, increasing anxiety over an ambiguous future, and loss of daily hospital routine. The fear was undeniable. The grief of losing some of our beloved mentors to the disease burdened our hearts even more. In spite of the fear and anxiety, we heeded the call, and attended to our duties. The work assignments and routines had to be greatly adjusted, for which we had to adapt to the best of our abilities. See glosssary Tao Rin Pala (TRP) is an annual program held by the UP Medical Students’ Society. It provides an opportunity for medical students, staff, faculty, and professionals to showcase their talents in the performing and visual arts. There is a different theme per year, but the constant reminder that physicians are also human beings pervades, hence the name, “Tao Rin Pala”. 1 2 146 The last time we saw the jovial and radiant Dr. Sally Gatchalian, then President of the Philippine Pediatric Society, was when she eagerly taught doctors during bedside rounds1 with patients in Ward 9. The next thing we knew, she was intubated1, and eventually, lost to the very disease she led her society to fight against. One by one, other physicians, some of whom were also our faculty, also succumbed to the disease. The shock of our mentors’ deaths made it all too real: COVID-19 could kill us. Gone were the times that we could just go in and out of hospital duties without fearing the infectivity of a simple respiratory tract infection. Gone were the times of going home to our families or roommates with the peace of mind that our clothes or bags or even our hands were not harboring deadly microbes. This crisis magnified the exhaustion that is second nature to a PGH trainee. Tired bodies made for easier targets for this virus. It was a grotesque reminder of the phrase “tao rin pala2.” They say a crisis reveals what the core of a person is. While heading the PGHPA, I had a unique opportunity of seeing firsthand how selfless the PGH doctors are during a crisis. The PGHPA set up a Telegram group3 exclusively for residents and fellows. It was a platform where doctors were able to voice out their concerns and connect directly to the PA, who relayed these concerns to the PGH administration in hopes of resolution. These issues ranged from PPE concerns, residency/fellowship training-related questions, to better communication with the PGH administration. There were also exchanges on matters not directly related to training or services, such as concerns regarding transportation, housing, salaries, and discrimination against healthcare workers. It also became the “food announcement” medium. We believed that no doctor should go hungry, especially when on duty. So departments which received extra food donations sent notices and arranged delivery to those who were less fortunate, or just more hungry! There is nothing glorious in the process of becoming a doctor. We’ve felt the demand to answer the needs of sick patients since the start of clerkship1— when we learned how to weigh soiled diapers, push stretchers, haggle for wheelchairs so our patients can sit while waiting in the ER, and compress a dying patient’s chest in an attempt to rescue him or her from the throes of imminent death. Now that we are residents in training, the demand is the same, if not greater. See glossary Telegram is an electronic, multi-platform messaging application. Messages on Telegram are securely encrypted. It is one of the most frequently used messaging applications in PGH at the time of writing 1 3 147 I distinctly remember one night when, while I was on duty, I received a message from a doctor from a different department. I personally did not know her, and I doubt we had met before. Her message was simple: “Thank you for doing what you do, for making an effort to inspire us to help each other.” The message was an inspiration to help each other. A reminder that we are going through this together. A certainty of hope that something good can come out of this crisis. As I write this, I still could not believe that only three months have passed. It feels way longer than that. As the crisis slowly unfolds and evolves, I still grapple with the question of how PGHPA can serve the doctors better. I am also reminded of my commitment to serve, not just as the Association’s president, but first and foremost, as a doctor serving in the frontlines. A part of me may sometimes be afraid and tired, but I am willing to hold on to the truth that I am not alone in this struggle. Perhaps herein lies the answer, that of holding a common resolve. We may have differing opinions, diverse and strong Type A personalities, passionate emotions, and altruistic epiphanies as doctors serving in one of the nation’s COVID referral centers. But, together, I believe we will be able to weather this pandemic and take pride in the fact that during this time of crisis, we became #OnePGH. 148 Yet Another Uncertainty Vince Elic S. Maullon “Oh mommy, dapat marunong ka na magdress ng wound ha. Magpapractical exam tayo bukas. Grade-an kita.” “Hala Doook, nakaka-pressure hahaha. Wait.” Mommy V, a bantay1, is feeling the pressure. Not because she’s part of the “tough 10,” but because she’s scared of dressing her husband’s non-healing wound. But Mr. V, a chronic diabetic, doesn’t seem to mind. He’s actually pretty chill about it. I made sure to teach Mommy V proper wound dressing, and instructed her how to change these twice a day. News about the steadily increasing number of COVID-19 cases was at the back of everyone’s minds, so I wasn’t entirely sure if we’d be seeing each other the next day. Mr. V was my last patient, assigned under my care that same day when it was announced that clerks1 were to be pulled out from PGH, to be followed by the interns1 a few days after. Mommy V would probably be relieved that I won’t show up. Walang practical exam eh. “Hoy! Kita-kita na lang sa June ha. Mamimiss ko mga pagmumukha niyo, hahaha.” That “June” quip was made with an element of exaggeration. We thought things would be normal by April, or May—a lockdown1 until May even seemed to be quite a stretch back then. Little did we know that that was the last semblance of normalcy we were going to have for the next few months. I went back home to Quezon City the next day, and some of my classmates went home to their provinces before Manila closed its borders. Our block’s typical daily noisy banter in the callroom1 was now limited to our Telegram group chat (it’s like Viber1, but for the bagets). 1 See glosssary 149 Messages would range from the different hobbies we were preoccupying ourselves with, to the status of our mentors and colleagues with the virus, and of course, to discussions on the almost-daily shows of ineptitude in our country’s pandemic response, care of our own national government. By this time, everybody seemed to be preoccupied with how the world was seemingly falling apart. For many of us, however, the elephant in the room remained: paano na ang clerkship natin? You see, being a clerk in PGH is weird. We’re medical students, yes, but we also actively take part in the management1 of our patients. We see them on a daily basis: taking their histories, diagnosing their diseases, and even creating and carrying out management plans for them, all under the supervision of our seniors, of course. As clinical clerks, we were among the “youngest” (i.e., least experienced) in the hospital workforce. We were also among the first ones to be pulled out from the hospital. But even though we’re technically on a “break,” after a few months, we were still to go back to the hospital as interns, about to face an unseen enemy. Like cadets being prepared to face the battleground, training had to go on. We can’t fight an enemy ill-equipped. After weeks of ironing things out, the UPCM Dean’s But at the end of the day, once we had finished our academic requirements, turned off our laptops, and everything went quiet, then we started entertaining our own personal thoughts and musings. The uncertainties of the future awaiting us soon-to-be doctors seemed very daunting. I always tell my friends that one of the things I hate the most is uncertainty. But in the profession we chose, uncertainties are a fact of life. Sometimes you may know how to manage a patient and you’re able to do it well, but there are times when you do your best, yet you see no improvement, and you just… well, hope for the best. Sana our patient can pull through. Sana kayanin niya. Now, we’re faced with a challenge we haven’t seen the end of yet. In a pre-COVID world, most of us would have probably mapped out how our internship, graduation, and post-med school plans would go. But COVID made us scrap all that. We can’t even think of what will happen next month. Even the next two weeks can be a bit of a haze. See glossary An SGD or small group discussion is an academic activity wherein students gather to discuss a fictional or real case, usually with the help of guide questions. It is usually facilitated by a consultant, who is there to answer any questions that may arise or emphasize any key points in the discussion. 1 150 Management Team made arrangements and virtual learning activities commenced. For several weeks, medical education at the comfort of our homes became the new norm for us. “Yung tipong nag-e-SGD2 kayo tapos tumatahol aso mo habang nagrerecite ka, gan’on.” “May dog barking,” our consultant1 quipped as my dog started yapping to his heart’s extent. Mukhang may gustong makisali sa aking medical education. 2 Together with our current interns—who will be taking their licensure exams later this year—our role as soon-to-be newly minted doctors in the post-COVID world is another uncertainty. The sick and those needing medical attention for other conditions will always be there. The young child with cancer, the pregnant woman, and the lola with diabetes and hypertension will always be there. Our patients will always be there. But, at least for the immediate future, so will this virus. These patients were the ones whom we used to face on a daily basis, attending to their needs. But right now, as much as doctors would want to face them, a virus remains in the way. How long would it take before things go back to normal? How long would it take before we will be able to face our patients again? These are questions to which no one knows the answers. All these are yet uncertainties. We can only do so much, and sometimes hope’s all that’s left. Sana our patients can pull through. Sana kayanin nila. It is fairly easy to get demoralized these days, but I would like to believe that not all hope is lost. Every day, patients get extubated1, patients get well, and patients get to meet their families again. Bit by bit, the familiarity of living life as we know it is coming back, and we have our People Giving Hope1 to thank for that: the frontliners, the backliners, and everybody doing their part to keep us safe and make our lives even a little bit easier to bear during these trying times. Indeed, during times like these, no matter how much uncertainty there may be, it is hope which gets us through. And for us medical students, the call of duty to serve our fellow men beckons us to prepare ourselves to fight the unseen enemy when it is our turn to be in the frontlines. After all, this only happens once in a lifetime. “From the PGH-DDHO: For the next batch of Interns (20202021), Internship will start on July 1, 2020 until June 30, 2021. All Interns will report on July 1, 2020.” 3 Walang alarm, walang anything. Ito, literal na “call of duty” na talaga. It was now the middle of May, and the inevitable seemed to be closer. We were going to be interns, and we’re going back to the hospital. “Hala Doook, nakaka-pressure hahaha. Wait.” Suddenly, I understood what Mommy V meant. See glossary This was the announcement given at the time of writing. However, due to the volatile situation caused by the pandemic, many of these earlier announcements were changed several times in consideration of safety. 1 3 151 152 Photo by Alla Tan RECOVERY 153 154 Recovery /r ’k v( )rē/ n. e e e The act of returning to a normal or healthy state. The war against COVID-19 rages on, but the People Giving Hope1 remain steadfast to their duty to serve. They refuse to wait for the smoke to clear and for the dust to settle. The hospital community continues to protect and serve the people, most especially the vulnerable. The country and the institution goes on the still difficult, unsteady, and uncertain path to healing. 1 See glossary 155 03.31.20 Sachiko S. Estreller I counted. 50 admissions. 27 discharges. 3 mortalities. This was our General Medicine service census for the month of March1 . 4:00 a.m. rounds. 3 residents. 2 admitting duties2. Unlimited inpatient charting and out-patient consults in between. All these before the half of March was through. Before 6 General Medicine services merged into 3 teams attending to both non-COVID and COVID patients. Before 24-hour duties turned into staggered 7-day 8-hour shifts. Before 2 internal medicine wards and intensive care units re-organized into COVID-dedicated facilities. Before life took a 180-degree turn. Veterans at dealing with an inordinate number of patients at any given point, it is not unusual for services (see glossary entry: Service) of the Department of Internal Medicine to attend to more than 50 patients a month - the census categorized into those still in the hospital, those who went home, and those who had passed on. With the wave of COVID-19 and the subsequent conversion of PGH into a COVID referral center, the numbers, and what they represent, have shifted. 2 Each department has their own way of assigning or decking patients. The Department of Internal Medicine, as well as some other departments, employs a winner-takesall system wherein all patients coming into the ER for a particular shift get decked to the service (see glossary entry: Service) on admitting duty. 1 156 Photo by Brent Viray Now the numbers are not mere admissions and discharges, but confirmed cases and deaths. 16 days into this lockdown. 2,084 sick. 88 deceased. 17 colleagues. Many awaiting results, many untested. We counted. Because in this time filled with ambiguities, where days are not measured by hours and the hospital and our vocation are filled with blurred lines, maybe we can scavenge a little sense of control, a little strength, by counting the numbers that make up our new reality. And though the sick, homeless and hungry are innumerable, the tears shed unmeasurable, the sacrifices made non-compensable, on this 31st day of March, we count 49 recovered. One of the numbers that matters most. Tomorrow, we welcome a new month. Filled with wishes and plans—all definite but uncertain at the same time. Slowly. Surely. Cases and deaths rising, then hopefully lowering. That elusive curve flattening. Ticking more days into isolation, counting down to when our efforts come into fruition. In the unpredictable months that will follow, one thing is sure—we will count, and the nation will remain counting. Copyedited by: Iris D. Ditan 157 The Persistence of Our Memories Juan Raphael M. Perez I was having coffee with my friend from Occupational Therapy when we saw the news: we listened to while studying—reminding us that we were studying medicine, but not entirely yet. CLASSES SUSPENDED FOR THE REST OF THE WEEK. Despite how visceral these experiences were, I was at a loss. I had sworn to serve the underserved, but how? What could I possibly do in situations— medical ones—I had not experienced before? Our initial reactions were sighs of relief. Wala nang gagawin! I distinctly remember how the coffee tasted slightly sweeter than usual—the hint of bitterness is still there, but subtle. It was naïve of me to think that the pandemic would change only that week’s schedule. Instead, it would fundamentally change how we lived and how we came up with reasons for choosing medicine. When everything started spiraling out of control, I realized that the path of medicine wasn’t what I had envisioned—a realization which forced a lot of heavy introspection on the paths we had decided on. Nighthawks (Hopper, 1942)1 Growing up, we were told stories of doctors akin to how Gilgamesh and Lam-Ang were praised for their heroism. A refrain of good fortune is ingrained in us, should we show any sign, no matter how small, of taking interest in med. Being a doctor (or lawyer) is good, because you will get a lot of money. Being a doctor is good, because you get to “serve.” Being a doctor is good, because you can help your family. I am pretty sure that when we pledged during the interview that we would serve the underserved, we all had different perceptions of what that promise would mean. PGH did not fail to make us realize just what we had agreed to though. Crossing the gates of Calderon Hall for the first time flung us, INTARMED2 kids, into an entirely new realm. We received text blasts when meningococcemia ran amok in the ER. In our bedrooms, we became familiar with the sound of the ambulance siren complementing the playlists But these myths about medicine are inaccurate depictions of reality. An oil painting by American painter, Edward Hopper. It depicts a diner on a corner where two streets meet. As the viewer looks on to the customers inside, it evokes the feeling of isolation and fear in an urban or new environment. 2 A program offered by the University of the Philippines that allows students to complete a Medical Degree in seven years instead of the usual nine to ten years, including undergraduate education. It consists of two years of general education and five years of medical school. 1 158 Then, the rumors reached us. “Meron daw sa fifth floor.” What the Water Gave Me (Kahlo, 1938)3 Being a child of INTARMED means being at a crossroads. It means accepting, at very young ages, the harsh realities of Philippine healthcare. It also means questioning our capabilities during pandemics, since we’re supposed to know what to do. We’re studying medicine after all, never mind that we’re still in preparatory courses! Anxieties about our futures constantly bloom. Did I make the right choice? Sometimes, being in medicine is demoralizing. We see our ates and kuyas tired and debilitated after 24-36 hours of duty4. We greet them as we pass by PGH, worried about their visible lack of sleep. We hear about the ruckus in the OPD4 and ER, remembering that just that morning, our buddies5 talked about running duties in those parts of the hospital. Being the observers in medicine is a constant shout for “mag-ingat ka,” hoping that the people we care for hear us. And hasn’t this pandemic turned into a black hole of “mag-ingat ka”? The same buddies are now frontliners, battling an enemy that cannot be seen. The same demoralizing structures are now ubiquitous: the paralyzing exhaustion felt from duties, the extreme lack of resources, the loudest cries for help. Here, a change in perspective is a must. It is tiring, but this demystification needs to happen if we wish to move forward. Medicine is not a perfect path. It will not always be a glorious celebration of life and health. We will not always save everyone. Frontliners are heroes, but they are also human. We are not Gilgamesh or Lam-Ang who will save everyone all the time—especially when resources remain scarce. Painted in surrealist style by the famous Mexican painter, Frida Kahlo, “What the Water Gave Me” also known as “What I Saw in the Water” is a meditation on the many facets and emotions in life. The woman bathing in the reflections on the river suggests an acceptance of whatever is handed to us, and learning to adapt to new predicaments. 4 See glossary 5 Referring to the buddy system, buddies are members of a “buddy line” wherein there is at least one representative from each batch in the UP College of Medicine. It is meant to be a support system where one can ask their buddies for advice on school and life in the hospital. 3 159 The First Days of Spring (Dali, 1929)6 Medicine in the Philippines seems to be a vicious cycle of suffering. Day by day, we discover new reasons to stray from the path. It might be the inadequate supplies, the inhumane work hours, the expensive pills, even the harsh politics. But despite all of these, we will go back to the lessons we learned before the white uniform, during the time of the virus. Compassion. Respect. Love for humanity. These are the values which the college and the hospital have equipped us with, and this historical moment will be the strongest reminder of the pledge we took. Moving forward, everyday must be an opportunity to discover a new reason to stay in medicine. It might be the support systems, the ates and kuyas who listen to our struggles while attempting to study stacks of transes7. It might be the professors, who enliven our classes with wisdom, all the while doing their best at saving lives. But most importantly, and hopefully, it will be the patients, who fight for their lives all the time, in a constant tug-of-war with darkness, even if medicine is imperfect. Through our seven years (or more, due to uncertainty) of study, we will strive to inspire others and contribute to a greater cause—one for humanity—against all odds. The reason might be hazy, or foggy, or maybe uncertain as of now. But, the reason is there. The reason is here. We must not only accept it, but also embrace it. To serve the underserved. And hasn’t this pandemic turned into a black hole of “mag-ingat ka”? Copyedited by: Frances Dominique V. Ho A famously eccentric figure, Salvador Dali painted this picture inspired by Sigmund Freud’s The Interpretation of Dreams. While a depiction of the association of dreams, this is a painting that makes one appreciate that the light of day will still return no matter what nightmares are encountered. 7 Transes. Transcription. This is the product of a centralized, note-taking system within UPCM classes. 6 160 Science Trisha M. Salcedo We who pass through the roads of Pedro Gil know this all-too-familiar sculpture: Scientia, the Triumph of Science over Death1. A nude woman atop a skull, bearing a lit torch, welcomes us to the UP College of Medicine. Much of the artist’s thought was devoted to creating an imagery of knowledge, the transcendent arm of humankind. Carved with reverent hands, this nude woman stands as the citadel of Science; she gives us hope in the face of death. She is a concrete memorial in every right — rigid, unyielding, austerely structured. Yet, this nude woman’s creator has left voids and hollows within her solidity. In how Science is far from immaculate, this corporeal work of art has her own unholy parts. Science, transcendent as she is, has her gaps. As I write, Science does not know. As I write, we face Death. He hides in the guise of a plague seemingly plucked from the sacred scriptures. When Science does not know, Death surmounts all else2. As the plague hastily overwhelms Science, Death holds his own chisel. He then proceeds with his sacrament: inscribing a multitude of epitaphs. We who pass through the roads of Pedro Gil know Scientia, a citadel of Science. As we wait for Science to reincarnate her truth, we use her oftforgotten roots as our stronghold. Until then — in the uncertainty, in the ‘not yet’, in the becoming — we hail her humanity. Copyedited by: Iris D. Ditan “science, a villanelle” by Trisha Salcedo A sculpture by Dr. Jose Rizal, it depicts a nude woman, standing on a skull while bearing a torch high with both hands. While the original is displayed in the Rizal Shrine Museum at Fort Santiago in Intramuros, Manila, a concrete replica of this sculpture, endearingly nicknamed “Lady Med”, stands proudly in front of Calderon Hall, the main building of the UP College of Medicine. As its name suggests, it is meant to represent victory over death through knowledge and scientific advancement. 2 The sculpture “Triumph of Science over Death” has a lesser known counterpart, the “Triumph of Death over Life”. In direct contrast to the former, Rizal shows Death, represented as a grim reaper, embracing a limp nude lady with uncanny resemblance to the woman in “Triumph of Science over Death”. It is a reminder that despite our advances in science, Death is inevitable. 1 161 Hope of Easter Thaddeus Hinunangan April 12, 2020 Manila In this pandemic, even when all public transportation and means for donors to visit the hospital were suspended, the blood needs of the hospital persisted. Just because COVID began hogging all the attention didn’t mean that other diseases took a vacation. Some of them even felt like working overtime. Because of this, the donation process, which used to be a straightforward trip to the Blood Donor Center in the PGH complex, now had to be done with online questionnaires and home visits, with bleeding performed at safe venues outside the hospital. Responding to the needs of its patients suffering from COVID, the Philippine General Hospital has also started doing plasmapheresis for compassionate use for critically ill patients battling COVID1. With the recent successful plasmapheresis donation by Ian Frias, a seafarer from the cruise ship Diamond Princess2, and nurses Gale Arranz and Kai Soriano, my Facebook post’s call for help had gone viral with more than 19,000 likes and 16,000 shares. Plasmapheresis is a process in which the plasma (the yellowish liquid component of the blood) is separated from the blood cells. The donated blood is received by an apheresis machine, which separates the blood into the following components: white blood cells, red blood cells, platelets, and plasma. The plasma is isolated and collected while the others are returned to the body. Usually, the collected plasma is replaced with another solution. During the COVID-19 pandemic, this is especially important because of its role in convalescent plasma therapy. Recovered COVID-19 patients contain antibodies against SARS-CoV-2 in their plasma. Through plasmapheresis, they can donate it to critically-ill COVID-19 patients and help them combat the disease. 2 On 20 January 2020, the Diamond Princess departed from the Port of Yokohama for a round-trip tour of Southeast Asia during the Lunar New Year period. One passenger boarded the ship despite having a cough. At the end of its tour, 567 out of the 2666 passengers and 145 out of the 1045 crew disembarked were infected. Fourteen of them passed away. 1 162 COVID-19 survivors donate their plasma in the hopes that the antibodies within may be used to give others a fighting chance. Photo by Thad Hinunangan Photo by Markyn Kho Dr. Thad Hinunangan conducts a predonation visit at the home of a potential donor of convalescent plasma. There, the team interviews the donor and collects blood samples for laboratory analysis. Photo by Thad Hinunangan 163 My inbox was full of messages expressing people’s support along with intentions to donate food, medications, and equipment. Most importantly, there were those who inquired about donating blood, and we set out to meet them on Easter. It was the 6th consecutive day of duty3 for Team A, and on that day my co-resident, Dr. Sandy Maganito, our medical technologist, Sir Jang Amizola, and I were tasked to go on pre-donation visits. We would explain the procedure, its risks and benefits, and answer the concerns of our five potential donors. Hopefully, we’d end up with their consent to donate before we left. We gathered outside the hospital with the essentials in our hands: syringes and blood collection tubes, consent forms, masks, alcohol, and a little bit of optimism, embarking on our journey shortly after the sunrise. Our journey consisted of going to Quezon City, Greenhills, Pasig City, and Cainta, Rizal. Even on a normal day, a day trip like this would take several hours, not counting the time set aside for the actual visit. The roads were thankfully clear with no traffic in sight. But many streets had been barricaded, so we had to look for alternative routes and pass through multiple checkpoints, to arrive at our destination. Despite the wondrous guidance of Waze3, and stopping every so often to ask for directions, we still took wrong turns and stopped at the wrong houses. At one point, when it became apparent that we were just going around in circles around Quezon City, we parked the car and decided to walk instead. By now, my head was throbbing. The lack of sleep, the glare of the blazing sun, and the pangs of hunger were all taking their toll. Our path eventually led us to a wary-looking girl who hesitantly opened her front doors as she saw us searching for one of our prospective donors. We were directed to the last residence in the row of apartments. We thanked the neighbor and were just about to go on our way when she asked me curiously what was going on, eyeing our hospital kit hiding in an eco bag. I sighed, gathered myself, and took a deep breath. This might be the best and only time to educate someone. “Are you familiar with Convalescent Plasma therapy3?” She shook her head. 3 164 See glossary Motioning for my companions to wait for a bit, I took my time to explain what this all meant to her, taking extra care with my word choice because I knew the moment she figured out that one of her neighbors had recovered from COVID, she might dwell on the words “COVID positive” and panic. I emphasized recovered and made sure to keep things as simple as possible. Thankfully, she was receptive to my explanations and, at one point, I even tried explaining what a polymerase chain reaction (PCR)3 was and why it was superior to lateral immunochromatography4 … but I guess I went a little too far. the dust of today’s drive and watched Sir Jang dozing lightly at the back. Today was one of the most exhausting days so far, and yet Easter continued to give us the greatest gift of all: hope. Though we now find ourselves journeying into the night, a new dawn promises to greet us tomorrow. Five possible plasmapheresis donors—not bad! Copyedited by: Sean Kendrich N. Cua Nevertheless, I drove my point home: there was nothing to fear in someone who had already recovered, tested negative, and had been asymptomatic3 for two weeks as long as everyone observed the same precautions—physical distancing, wearing a mask, washing hands, among others. I knew first-hand that a lack of correct knowledge could lead to wrong assumptions, and these, in turn, could bring about discrimination. We left the area having accomplished our initial task, earning something just as valuable in between. At the end of the day, as the car went over one of the bridges traversing the Pasig river, the skies cleared as the sun set over the horizon, bathing everything in sight with a gilded haze. I smiled and wiped the grime from my forehead, I looked at Sandy’s wrinkled white T-shirt with Photo by Markyn Kho See glossary A method used to detect the presence of a target substance in a liquid sample without using specialized and expensive equipment. This is a technique used by several test systems in order to detect the presence of antibodies against COVID-19. 3 4 165 The Destination of My COVID Dreams Howie Severino The place where they extracted the treasure from my body was at the end of what felt like an impromptu treasure hunt. I was informed the procedure would be at the Philippine General Hospital, but the actual venue turned out to be an academic building at the UP College of Medicine1. I walked down a lonely hallway with desks stacked against the wall, a mute testament to classes that were abruptly suspended until God knows when. Beyond the security guards at the entrance, there was absolutely no one. I thought I was in the wrong place until I saw the room number I was looking for. Inside was a classroom converted into a makeshift clinic with two young doctors. In the weeks since I was hospitalized elsewhere for COVID-19, this simple space with a special machine was the destination of my COVID dreams. Reaching it meant I had recovered and I could finally donate my plasma2, and be of value to someone else. Before that momentous day, there was a month of suspense and anxiety. Even after I was discharged from the hospital, the uncertainty about my fate was not over. My symptoms2 were gone, but I was still not considered recovered until I tested negative twice for the virus. It was not until then that I could end my isolation and rejoin my family. Alas, after one negative result I was stunned to learn that I had tested positive again for the virus several days after leaving the hospital. The Dr. Maria Paz Mendoza Memorial Medical Building, commonly called Paz Men, is a structure found within the UP-Manila campus. Named after Dr. Maria Paz Mendoza-Guazon, an esteemed medical practitioner, scientist educator, and civic leader, this facility houses classrooms which are used by medical students for lectures, laboratory sessions, and small-group discussions (SGDs). 2 See glossary 1 166 Even as I was recovering, I had already been receiving appeals for my plasma from doctors and loved ones of desperately ill patients. There were only a few dozen known COVID survivors by early April, and not all of them were plasma donors. The official survivors then were outnumbered by the deaths in the Department of Health’s count, filling me with the dreaded uncertainty of which column I would eventually end up in. The appeals for my plasma felt like a vote of confidence in my survival, and gave me further motivation to eat well and boost my immunity2 while in isolation so I could join the thin ranks of plasma donors. Had I been reinfected? Or did the PCR 2 test merely detect viral fragments from the original infection, as the latest science now indicates? New theories about this disease have unfolded every day, sometimes upending conventional wisdom. Now even the vaunted immunity supposedly bestowed on recovered patients, the one major consolation from suffering from COVID, was in doubt. referral center2. First, though, I had to be screened through an interview by a pathology resident2 and a blood test. After waiting for an hour, I learned I had qualified to give my plasma. Demoralized and lonely in my quarantine2 quarters, I decided to go home where I saw my family but could not get near them. But seeing them was enough. Perhaps the solitude of quarantine, far from loved ones, was a source of stress that was affecting my ability to recover, or at least rid myself of the virus once and for all. After a few days, both PCR tests yielded negative results, officially making me a recovered COVID patient. On top of that, I was positive for antibodies on two rapid tests3, further proof that I had in my blood the anti-virus warriors coveted in the battle against the disease. I was now an automatic member of a growing club of COVID survivors worldwide blessed with a special power. I think that was the reason I was met by looks of appreciation by the PGH medical staff in that converted classroom. They explained that they stationed the plasma donation clinic in a classroom in order to be physically separated from the hospital which served as a COVID Photo courtesy of Howie Severino See glossary A rapid antibody test can quickly screen whether a patient infected with COVID-19 has developed antibodies that fight off the infection. Because the test does not detect the virus itself, it is more useful for procedures like plasma donation than it is for diagnosis. 2 3 167 They sat me in a permanently reclined chair and casually mentioned that there might be some discomfort, an occasional code word, I’ve realized, for pain. I proudly said, “Pagkatapos ng karanasan ko sa ospital, kayang-kaya ko yan!” Truthfully, they were brave words said to mask a sudden unease. A needle was inserted into a vein in my arm, a tube was attached to the needle, and I was then connected to an apheresis machine, the equipment that would separate the plasma from my blood and return the rest of the blood components – red cells, white cells and platelets2 – to the donor, me. To divert my attention from any “discomfort,” I got into a long geeky conversation about Magellan’s voyage with the baby-faced director of the PGH blood bank, Dr. Mark Ang. As the blood components were moving back into my veins from the machine, I did feel a little sting, but it was tolerable. I actually felt more giddy than anything else. This was an important moment in my journey as a COVID patient—a kind of graduation with honors. Photo courtesy of Howie Severino 168 2 See glossary Not every patient survives, and not every survivor qualifies to donate plasma. I was able to do both. But this personal achievement matters only because it can save the life of another person. There are still many unknowns about COVID-19, but there’s a growing medical consensus about the lifegiving value of plasma that came from a recovered patient with antibodies. That is why the doctors present during my donation called plasma “liquid gold.” With far fewer recovered patients than confirmed cases, the plasma from the two or three donors a day at PGH are treated like treasures. There is a great need for donors, which is why those who have already donated need to assure fellow survivors that it is a safe process that will make the donor happy that they gave. I dare say what I gave is even more valuable than gold. You can buy gold, but you cannot buy my plasma. I was told that a committee of doctors would decide on the recipient, surely a patient with my blood type and probably someone who may not survive without the infusion of plasma. This precious liquid would be given for free. As I sat there feeling the slight pang of blood moving out of and then back into my veins, I felt a sense of fulfillment from having lived up to a promise. When I was still very sick in the hospital, I vowed to myself and to the cosmos that if I survived, I would pay it forward. After less than two hours, the procedure was over. The medical technicians2 handed me the small bag of liquid treasure, the yellow plasma they had just extracted from my body, so I could hold it like a mother with 2 See glossary 169 her newborn. After all, from my body just came this golden symbol of life. They had me pose with it as the medical staff gathered around me for photographs. I held it up like a trophy as they applauded. Returning home that night, I reflected on the personal significance of that event. One of the worst things about being a patient is the feeling of being a burden. For all of its terrible attributes, COVID enables a beautiful epiphany: if one survives this disease, that feeling of being a burden can be replaced by a sense of wonder that you gave another patient out there a fighting chance. Just like others who have given before him, broadcast journalist Howie Severino volunteers his time and plasma in the hopes it may benefit other patients infected with COVID-19. Photo courtesy of Howie Severino Copyedited by: Amanda Christine F. Esquivel 170 Kumusta ka? Maria Keziah G. Legion “Kumusta ka?” Animo’y ordinaryong mga kataga ngunit may mas malalim na pag-uusisa. Napatulala na tila huminto ang oras at pintig ng dibdib, ni hindi na maulinigan ang iba pang sinambit at ang tanging tumatak sa isipa’y, “Positibo.” Unti-unting bumuhos ang luhang nangingilid na ‘di mawari kung paano na ang hakbang na gagawin. Naglakad nang may agam-agam sa isip, “Ako, positibo?” at biglang napatingin sa langit, sabay sambit ng, “Positibo. Kaya ko ito.” Isang maikli ngunit taimtim na dalangin para sa araw na iyon sapagkat ikalawa ko nang pamamalagi sa ospital ‘pag nagkataon. Hindi bilang isang nars na kumakalinga sa maysakit ngunit bilang isang pasyente ng kinakatakutang COVID 19. 171 Nung una ay wari ako’y sinubok ng Panginoon dahil sa aking pagiging asmatiko, ako’y nagkipaglaban. Gumaling at patuloy na nagsilbi para sa bayan, ngunit sa isang iglap lang ay nahawaan nang ‘di kinakitaan ng anumang sintomas. Sa pagkakataong ito’y ako’y napaisip, sa sarili ay aking nasambit, “Kumusta ako? Kumusta nga ba ako?” Mabuti na lang at maraming gustong dumamay mga kapamilya at kaibigang handang umagapay. Sa huli’y ang pagiging matatag ang naging sandata di lamang sa puso’t isip lalo’t higit sa pananampalataya. Natutong huminga pa ng mas malalim at magpatuloy, sapagkat nais ko rin na ako naman ang makiramay at magsabi sa dulo ng lahat ng ito ng, “Kumusta ka?” 172 173 With the Enhanced Community Quarantine prevailing over Metro Manila and many hair salons and barbershops unable to operate, ResCute Operations, a team of barbers, stylists, and their sponsors, set up shop at the lobby of the PGH Outpatient Department (OPD) and offered free haircuts and hair styling to hospital frontliners. Photos by Harjoland Obenieta. 174 In Sickness and In Health Genry Criscel R. Consul “Walang ibibigay na hindi mo kaya.” Dr. Carlo confidently declared as he sat next to his wife, Dr. Mela, when asked to recount the last two months. Nothing had gone according to plan. As type A personalities, watching their carefully laid out plan burn to the ground was a nightmare. The plan was for Carlo to be on duty1 in Tarlac as Mela enjoyed her maternity leave at home. It was to go shopping for baby things, preparing to welcome the twins while surrounded by family. It definitely did not include undergoing a role reversal from doctors to patients. Nor did it include giving birth a month before the due date, or being COVID patients, stuck in a hospital for 52 excruciatingly long days. To Have and to Hold Meeting in medical school, becoming licensed to save lives, starting internal medicine1 residency, tying the knot, and being pregnant with twins seemed like forever ago He was on the line of duty, assigned to the ICU1, when Carlo first got sick. His 24-hour flu, three-day diarrhea, and an episode of vomiting were nothing to his wife who nursed him to recovery. At that time, swabbing1 was exclusively for PUIs1-- health care workers were not part of the priority. He went to the hospital to get checked and admitted but was sent home for a two-week home quarantine1 instead. A week later, she got sick too. Symptoms, which were worse than his, started showing. As the cough got worse, Mela felt weaker. The couple opted to have an x-ray done. This showed bilateral pneumonia1. Mukhang hindi ito COVID, he thought, not wanting to think of the worst. Feeling ko positive na talaga ako, alam ko, she thought, as she listened to her body that housed two other lives. Even before she got her result, she was already mentally preparing for it. Or at least doing the best she could. 1 See glossary 175 Photo by Alvin Caballes They entered a private facility to self-quarantine. Not long after, she was swabbed and then brought to the hospital, her and her husband’s place of work. This time as a horrified pregnant patient in an unstable state: gasping for air, hot with high fever. As soon as she set foot in that familiar building, she felt suffocated and overwhelmed. She just wanted to leave. As doctors, beyond denial and panic, they both had the gut feeling that the swab result would come out positive. Logic dictated that. At the back of their minds, behind all the thoughts of terror and trepidation, they knew. For Better or Worse From there, everything felt like a blur. While waiting for the swab result, she was transferred to the ICU for close monitoring1. Her body was deteriorating—shortness of breath, desaturation1—she was not looking well. “Iyak siya nang iyak noon,” she mused as her husband continued to narrate their story. He couldn’t stop the tears as the results confirmed their nightmare. It was a plethora of emotions. He was distraught 1 176 See glossary to see his wife in agony, worried for the other people they shared a residence with, and afraid of the possibility of losing the three most important people in his life. As his duty as a husband never faltered, he also did not abandon his duty as a son. He immediately called his parents and did his own contact tracing. Dr. Mela was 28 weeks pregnant2. Giving birth prematurely comes with a slew of complications and the hospital did not have a neonatal specialist1 who could ensure adequate care for the twins. Their consultants1 arranged the transfer to PGH, and they were set to journey to Manila to seek the best care possible. Kriminal ba ako? She thought as she was swarmed with stares from people in the hallway. The path between her hospital room and the ambulance was adorned with makeshift plastic barriers. As she peeked through the window, she felt as if everyone was staring at her. In PGH, patients weren’t allowed to have companions. She thought she could handle this, but being alone within four walls during the pandemic took a toll on her physical, mental, and emotional wellbeing. Physically, she had general body weakness and a high grade fever. Mentally, she could not handle all the calls and questions being thrown at her. Being ill alone whilst not knowing exactly what lies ahead was torture. Emotionally, she was afraid of not only her own health but also of the lives she was carrying. In another part of the hospital, a worried husband merely wanting to comfort his wife waited endlessly for updates. After four hours, he got word about her current state. With the permission of the Infectious Disease specialist on her case, he was finally allowed to be by her side two hours later. In Sickness and in Health “Naisip ko lang lahat ng COVID patients na unstable, kailangan talaga ng kasama,” he lamented. Not being together during those vital hours put them both in misery. After all, there was solace to be found in being with a loved one or family, much more than any hospital staff could provide. “Manganganak ata ako nang wala sa oras dito,” Dr. Mela laughed as she remembered the ultrasound machine that malfunctioned every five seconds in the PGH ER when she needed it most. “Hindi ako gagaling agad kung wala siya sa tabi ko,” she agreed, saying she felt secure and relieved when he was finally allowed to be by her side. It was heartwarming. He was her hands when she couldn’t See glossary A full-term pregnancy is a pregnancy that lasts between 39 weeks, 0 days and 40 weeks, 6 days. Babies born before the pregnancy reaches full-term are called “pre-term” and are more prone to infections and breathing and feeding problems. They may have to be placed in the neonatal intensive care unit (NICU) where they will be properly cared for by specialists. 1 2 177 move, her voice when she couldn’t speak, and her guardian during all of it. It felt like their four-month old marriage aged in years with what they experienced together. Thinking out loud, he said that though every relationship is unique, all have one experience in common—challenges to surmount. While most face these at the middle or at the end, theirs was tested at the beginning. He smiled while saying he was only honoring the vows he made in front of God and their loved ones. “Kailangan pangatawanan mo ‘yun… kapag may isang mahina, kailangan yung isa strong.” Soon, he was admitted as a patient too. He was swabbed as part of routine contact tracing, tested positive, and got his minute companion’s bed converted into a more comfortable patient’s bed. Their boxy hospital room turned into an exclusive apartment where they bathed, cleaned, did their laundry, and lived for 52 days. They fully embraced a domestic life in a PGH room supposedly meant for one. A few weeks later, the twins could no longer wait to come out. Mela was wheeled into the operating room where an emergency cesarean procedure was done. Drifting in and out of consciousness from the sedation, Mela heard someone say “Saan natin ilalagay ‘to, Doc? Formalin!” She could not believe what she was hearing. Unsure if the formalin was for her children, she blacked out again, terrified of what she heard3. She arrived in her room bawling. They knew nothing about their children except that one was intubated1 and the other was connected to a CPAP machine1. The pain felt by these first time parents was unimaginable. They were not allowed to see their children. There was an aching feeling in their hearts that could not be mended by medication. For the new mother, it was agonizing to carry the twins inside her for eight months and for them to be away from her arms. The couple did not even know what they looked like. In her head she thought, “kailangan na nila ng mommy.” Crying together and praying together became the couple’s way of coping. Two weeks later, they were finally allowed to see their miracles. Immediately after they were discharged and cleared for visitation, they rushed to the Neonatal Intensive Care Unit, where her twins were. Mela was overcome with emotion. Clothed in a full PPE suit1, she held her children for the first time. It was a touching reunion, one that was long time coming, and happiness filled the NICU. They whispered to their children who were finally bundled up in their mother’s arms, “Stay strong, keep fighting, and have faith in the Lord.” They will all be reunited one day, See glossary Formalin is a clear aqueous solution of methanol and formaldehyde. Since it functions as a disinfectant and an antiseptic, it can be used to preserve specimens for further studies. Often, it is the placenta of a premature birth. However, a fetus that died within the womb may also be considered a specimen. To a mother coming in and out of sedation, it’s not hard to imagine the worst. 1 3 178 hopefully soon, in God’s time. Even with COVID, We Will Not Part The shift from being doctors to becoming patients was enlightening for the couple. They came to learn that only the patients truly know what and how they feel. During their time as patients, they promised to take a few things they have learned back to their practice. Admitting that they have not always been constantly passionate doctors, they vowed to emulate the health workers who treated them not only skillfully but also compassionately. This experience has changed them forever, and they will get back to their residency as better versions of themselves, who aim to treat holistically, with compassion and genuine care. Dr. Carlo and Dr. Mela will traverse parenthood together hand in hand. Along with their children, who gave them hope to persist amidst the adversities, the strength and grit shown by this couple will touch many lives, with love and devotion. Theirs is a family of fighters. In the lives of these young doctors, fear is not welcomed, especially when their faith is bigger than the trials thrown their way. Copyedited by: Juan Raphael M. Perez 179 Life goes on Patricia Anne S. Basilio Life goes on. That’s what you’ve learned, from hours of fitful sleep, staring out as the world flashes by, every raging storm and sunny day, wishing you were everywhere and nowhere at once, afraid of time slipping past your fingers before you’ve even lived— Life goes on. The fear sets in, once the unwanted visitor, knocking at your door when you least want it, when you least expect it. It’s an old friend now. The one that tucks you in at night, the one that greets you when you open your eyes and realize that it’ll be the same day over again, and again, and again… Life goes on. Perhaps it’s fate that brought you to this path, this bumpy road; fate that you’ve been witness to the worst and the best, of love and hate, of life and— Death. So much death. Oh, how easy it is to be swept and drowned in that torrent of unshed tears, forgotten dreams, missed opportunities, never-ending regrets, And yet. Somehow, someway… LIFE. GOES. ON. 180 Life blooms even in the darkest of places. Random acts of kindness. Family and friends. Quiet smiles exchanged with strangers on the street. The warmth of home cooked meals. Those terrible dad jokes and puns that make you laugh (even if you try not to). Even when you can’t see past this day; even when things don’t ever seem to go your way. Life goes on. For you. For us. Another dawn. A chance at trying, and failing, and trying again. Hope stays even in the saddest of places. The old tune you sang when you first learned to dream, through hours of fitful sleep, impatient to see the sun rise again— Things will get better. You know it will, maybe tomorrow, a new day. So you keep singing that old busted melody. Belt it from rooftops. Let it echo until the sun sets and you’re tucked in at night, To keep dreaming that, To keep praying that, Life will keep going, On and on, And on, And on. Copyedited by: Juan Raphael M. Perez 181 Puhon1 Christi Annah Hipona Plucked from our familiar; Removed from our normal; We all tried to make sense of it. Some of us stayed at home and learned to rest. Some slowed down and meditated. Some asked “Are we ever going back to normal?” Some cried tears—not of weakness but of witness. Some gathered resources resolutely. Some stayed at the front lines and despite fear, stared death in the face. Yet all of us prayed. Puhon We will heal. Puhon We will all be together again. Puhon We will see the goodness of God. Looking upward with eyes of hope; That when this evil shall pass, We will grieve what we lost; Pick ourselves up; Pray new prayers; And dream new dreams. Puhon, we will live our lives in remembrance of how God has carried us through. 182 A Cebuano word that roughly translates to “soon”, it is an expression more akin to a prayer. Used in the background of hoping for a right, it is meant to convey “hopefully in the future, God-willing”. 1 183 184 Glossary 185 A ABG Arterial Blood Gas. A laboratory exam that measures the pH and levels of oxygen, carbon dioxide and other gases in blood drawn from an artery. This is an especially important exam to accurately determine if a person has enough oxygen in their blood. Abstract A document which summarizes a patient’s clinical condition, including their diagnosis, medical history, physical exam findings, and relevant laboratory result. Asymptomatic If in reference to a patient, this pertains to an individual who may already be infected or have a disease but does not exhibit any symptoms. Bayanihan Na! Operations Center Bayanihan Na! Operations Center. BNOC. It is a volunteer operation that acted as a call center for incoming calls to PGH for COVID-19 related concerns and as an organizing body for the donations being sent to the hospital. C Callroom A room where health workers can rest and eat in the hospital. These rooms will usually have bunk beds, workstations, and occasionally, a bathroom. Cancer Institute A complex found within the Philippine General Hospital where cancer patients are treated. B Census A record enumerating the patients admitted to the facility at a specific time. Bantay Companion. A relative or friend who watches over an admitted patient and also facilitates certain hospital processes such as getting the patient’s medication and discharge papers. Charity Charity wards. A hospital ward that is dedicated for the patients who receive free services. Benign A colloquial term used to describe an easy or unremarkable duty or shift; the opposite of “toxic” (See Toxic entry). As a clinical term, this refers to a lesion or condition that is not cancerous. Bilateral pneumonia Pneumonia (see entry: pneumonia) in both lungs. 186 Chart A patient’s document containing their healthcare team’s notes, and therapeutic plans. Chemotherapy Although the term chemotherapy broadly means the use of a drug to treat a disease, it is usually used to refer to the treatment of cancer patients with anti-cancer drug. Clerks Medical students in their fourth year of education. They take active roles in patient management including interviewing and examining patients, facilitating laboratory work, and going on duties (see entry: Duty). CPAP machine Continuous positive airway pressure (CPAP). A mode of respiratory ventilation that is usually used to reduce the amount of effort necessary to inhale oxygen properly in patients who find it difficult to breathe. Clinical deterioration The worsening of a patient’s condition as measured by clinical parameters. Sometimes, the patients need to be admitted to the ICU (see entry: ICU). D Consultant A physician with usually the most senior rank on the team. They are responsible for overseeing all patient care in their service (see entry: Service), and teaching trainees, in addition to other administrative duties they may hold. COVID referral center A designated medical facility that provides care for COVID-19 patients. In the National Capital Region, the Philippine General Hospital, along with Dr. Jose M. Rodriguez Memorial Hospital and the Lung Center of the Philippines, are the COVID referral centers. COVID suspects New classification used by the Department of Health to refer to a patient who presents with pneumonia-like symptoms with no other disease likely to explain the condition OR a person with flulike symptoms AND a history of travel to a place with COVID transmission or contact with a confirmed case of COVID-19. People in the vulnerable group (i.e. elderly, patients with existing diseases like hypertension) with respiratory symptoms may also fall under this classification. Desaturation Short for oxygen desaturation, or the often sudden lowering of oxygen levels in the blood. This usually indicates a severe pulmonary or cardiac event. (see entry: Oxygen saturation) Dialysis A procedure done using a specialized machine to remove specific waste products and excess fluids in the blood. This is done on patients whose kidneys are not working properly. Doffing and donning Doffing is the practice of removing an item of clothing (e.g. PPE) while donning is the practice of putting it on. Duty Part of the pre-duty, duty, post-duty cycle where each part of the cycle denotes a person’s responsibilities for the day. Usually referring to the night shift, duties range from 12 to 24 hours where one must be in the hospital. Night duties involve taking care of all admitted patients, including the patients of those who are not on duty. Dyspnea Labored or difficult breathing. 187 E more senior colleague on a patient’s medical condition either for advice on patient management or as an academic exercise. Elective admission An admission that has been arranged in advance (i.e. not an emergency case). Extubate The removal of an endotracheal tube from the airway. Emergency Medicine A medical specialty dedicated to the diagnosis and treatment of illnesses or injuries that require immediate medical attention. Endorsement In medical colloquial terms, this usually pertains to a discussion between outgoing and incoming duty teams focused on pertinent information on patients’ current conditions and important tasks to be accomplished. It may also refer to a junior colleague reporting to a more senior colleague on a patient’s medical condition either for advice on patient management or as an academic exercise. F Fellow A physician who has completed their residency training, and is currently undergoing further training in a more specific field. For example, a resident in Internal Medicine may go into Cardiology for their fellowship training. Extubate The removal of an endotracheal tube from the airway. Fomite An inanimate object which can be contaminated by infectious agents. When a fomite is exposed to pathogenic bacteria, viruses, or fungi, it can transfer disease to a new host. Elective admission An admission that has been arranged in advance (i.e. not an emergency case). H Emergency Medicine A medical specialty dedicated to the diagnosis and treatment of illnesses or injuries that require immediate medical attention. Hypoxia A pathological condition in which the body (or a certain region) does not get enough oxygen into the cells and tissues. Endorsement In medical colloquial terms, this usually pertains to a discussion between outgoing and incoming duty teams focused on pertinent information on patients’ current conditions and important tasks to be accomplished. It may also refer to a junior colleague reporting to a 188 Photo by Brent Viray I IDS Infectious Disease Section or Specialist. Can refer to the unit or the individual specialists handling infectious conditions. Imaging request A form which specifies what imaging service is needed (e.g., x-ray, CT scan, MRI, ultrasound) and for what condition or organ of concern. Immunity A state of having enough biological defenses to fight specific infections or diseases. Integrated clinical clerks (ICCs) Medical students in their third year of medical education. They get to have more clinical experiences, with more patient interaction and, under the supervision of faculty, are introduced to providing care to patients. They rotate through the hospital’s various departments. Intensive care Highly specialized and resource-intensive medical care which is provided for seriously ill patients. Intensive care unit (ICU) Also known as intensive treatment unit or intensive therapy unit (ITU) or critical care unit (CCU).A hospital unit where critically ill or injured patients are given specialized care. Internal medicine The medical specialty dealing with the prevention, diagnosis, and treatment of multi-system disease processes in adults. After completing their residency program and becoming board certified, internists may choose to subspecialize (e.g. cardiology, pulmonology). Interns Physicians in their last year of training, before taking the licensure exam. One year senior to clerks, interns have additional clinical responsibilities. They rotate through selected departments. Aside from assisting in the care of assigned patients, they also help introduce clerks to the nuances of patient care. Intubation Endotracheal intubation. A procedure which involves the insertion of a flexible plastic tube into the windpipe. The tube is connected to a ventilator machine which pushes oxygen into the lungs. This is frequently done to critically ill or injured patients to help them breathe. IV antibiotics Administration of antibiotics through an IV line (see entry: IV line). Intravenous antibiotics are used to treat infections that are resistant to oral antibiotics or for infections that require doses of antibiotics that cannot be administered orally. IV line Intravenous line. A soft, flexible tube which is connected at one end to a fine catheter or needle that is threaded into a vein and to the other with a bottle or container of fluids or medications. Solutions and even blood products are infused directly into the vein through the line and indwelling catheter. L Lockdown An emergency protocol that prevents people from leaving an area, and restricts their movement within that area. 189 M Management A description of the interaction between the healthcare team and the patient. This includes communication, evaluation, diagnosis, prognosis, and intervention. It may also refer solely to the healthcare team’s therapeutic plan for the patient. Medical Technologists Med techs. Health professionals who perform and analyze the results of scientific tests on blood and bodily fluids. They are also tasked with the processing of specimens and running of the RT-PCR test systems used to detect COVID-19. Medical Technologists The observation of a condition, disease, or medical parameter. It is also often used to refer to the practice of regularly checking a patient’s vital signs (see entry: Vital signs). Healthcare workers use medical monitors and medical tests in order to check on a patient’s condition. N Nasopharyngeal swabber An individual who is required to perform a nasopharyngeal swab (see entry: swabbing). Neonatal specialist Neonatologist. A neonatologist is a medical doctor specializing in the medical care of newborns, most especially those who are in critical condition. 190 Neurology The branch of medicine that deals with the diagnosis, treatment, and management of patients with conditions and diseases that involve the nervous system. N95 mask N95 Respirator. A type of mask that can filter out at least 95% of very small (0.3 micron) particles. These masks protect the wearer from airborne particles, from small particle aerosols to large droplets, which may contain bacteria and viruses. Nasopharyngeal swabber An individual who is required to perform a nasopharyngeal swab (see entry: swabbing). Neonatal specialist Neonatologist. A neonatologist is a medical doctor specializing in the medical care of newborns, most especially those who are in critical condition. Neurology The branch of medicine that deals with the diagnosis, treatment, and management of patients with conditions and diseases that involve the nervous system. Nurses’ Home A building within the Philippine General Hospital premises that serves as a dorm for employees of the hospital, and a function hall for social events. It was converted into the call center for Bayanihan Na! Operations Center during the pandemic. O Ophthalmology The branch of medical science which deals with the anatomy, functions, and diseases of the eye. Otorhinolaryngology (ORL) A surgical subspecialty dealing with the surgical and medical management of conditions involving the head and the neck. It is sometimes referred to as “ENT” for Ear, Nose, Throat. Also termed as ORL-HNS, or Otorhinolaryngology-Head and Neck Surgery. Out-Patient Department Outpatient department (OPD). This is the hospital department that provides diagnosis and/or treatment to patients in a clinic setting. The PGH Out-Patient department is located along Padre Faura street. Oxygen saturation (SO2, “sats”) This is one of the several measures that can be used to measure oxygen levels, often by a pulse oximeter attached to a finger. It refers to the percentage of oxygenated blood in circulation.. A decrease in oxygen saturation may herald clinical deterioration (see entry: clinical deterioration). P Pandemic A worldwide and rapid spread of a new disease. Pathology A branch of medical science that deals with the origin, nature, and course of diseases. Pathologists examine surgically-removed organs, tissues (biopsy samples), bodily fluids, and if necessary, the whole body (autopsy) for diagnostic or forensic purposes. They may examine the specimen with the naked eye or under a microscope. Pathophysiology The specific changes in the normal body functions associated with a particular disease or injury. It seeks to explain the functional changes that occur in an ill individual. Each disease has a different pathophysiology, and at the time of writing, the pathophysiology of COVID was poorly-understood. Pay floors Floors in the Philippine General Hospital with rooms reserved for private patients. People Giving Hope People Giving Hope is the moniker given by the hospital director, Dr. Gerardo Legaspi, to the Philippine General Hospital staff during the COVID-19 pandemic. He used this to address them in a letter which was released before the announcement that PGH would serve as a COVID referral center. Personal Protective Equipment (PPE) Equipment and apparel which are worn in order to protect the user against health or safety hazards. While commonly associated with the “full” version with full-body suits, goggles and masks, less items are needed for lower-level hazards. Plasma Blood plasma. The yellowish liquid component that is responsible for about 55% of the body’s total blood volume. It carries the nutrients, blood components, hormones, and proteins to the different parts of the body. 191 Platelets Thrombocytes. A type of blood cell. Platelets help the body form clots in order to stop bleeding. Pneumonia An acute inflammatory condition of the lung/s. It is usually caused by viral or bacterial infections, which is usually spread via air-borne droplets from a cough or sneeze. Polymerase chain reaction (PCR) A laboratory technique that is used in order to make multiple copies of a DNA segment. Post-duty Part of the pre-duty, duty, post-duty cycle, each part of the cycle denotes a person’s responsibilities for the day. Post-duty refers to the status or a person who has just completed a duty (see entry: Duty). The tasks that must be accomplished vary according to the service. The cycle restarts after post-duty status. PPE levels (1,2,3,4) This is the scheme implemented in the Philippine General Hospital during the COVID-19 pandemic. Level 1 PPE - This is used for low-risk areas like the non-COVID-19 wards and the outpatient clinic. The staff can opt to wear either of the two options: 1. Face shields and a surgical mask or 2. Goggles and a surgical mask. Level 2 PPE - This is used for areas with bathrooms where healthcare workers can shower after duty. They need to wear 1. Cap and goggles 2. N-95 mask 3. Gloves 4. Gown or coveralls 192 Level 3 PPE - This is used by the staff who are assigned to man the triage areas and parts of the hospital where PUIs are admitted. The PPE consists of 1. Cap and goggles, or a face shield 2. N-95 mask 3. Gloves 4. Gown or coveralls Level 4 PPE - Staff assigned to the COVID-19 wards and operating rooms are required to wear the following: 1.Coveralls 2. Surgical cap 3. N-95 mask 4. Scrub suits 5. Goggles/face shield 6. Double gloves 7. Dedicated shoes 8. Shoe covers Pre-duty Part of the pre-duty, duty, post-duty cycle, each part of the cycle denotes a person’s responsibilities for the day. Pre-duty refers to taking the morning shift, usually lasting 10-12 hours, and precedes the duty status. The specific responsibilities vary depending on the assigned service. Preemptive intubation The intubation (see entry: intubation) of a patient. This is done not because the patient needs it at that exact moment but because there is a high chance that the patient will have to be intubated shortly. Often, this decision is made because there is progessive worsening of the patient’s condition. PUI Person Under Investigation. A term in the old classification system used to pertain to an individual who has not yet had a positive COVID-19 laboratory test but has symptoms of COVID-19 (e.g. fever, shortness of breath) in combination with a travel history to China or a history of exposure to a confirmed case of COVID-19. Pulmonary specialist Pulmonologist. Pulmonary specialists are trained to diagnose and treat diseases involving the respiratory system. Pulse oximeter (Pulse ox) A small, portable, electronic device, clipped on to a patient’s finger to measure the oxygen saturation of arterial blood. Q Quarantine A state of enforced isolation. During the COVID-19 pandemic, it was used to keep someone who might have been exposed to COVID-19 away from others. This practice helps prevent the spread of the disease. Those in quarantine were asked to stay home for two weeks while regularly monitoring body temperature and watching out for COVID symptoms. R Radiologic technologists Rad techs, radiographers. Health professionals who specialize in the imaging of human anatomy. Red cells Red blood cells (RBC) or erythrocytes. A type of blood cell. RBCs contain a protein called hemoglobin which carries oxygen to the different parts of the body. Referral A request from one department or service to another, seeking consultation for their patient on a particular disease or issue. As an example, an IM service may make a referral to the Department of Ophthalmology for their patient with vision problems. Resident A licensed physician currently undergoing training in their chosen field. Resident-on-duty (ROD) The resident (see entry: Resident) assigned to oversee patient care during that shift. Their tasks may include admitting patients, making initial notes, and planning patient management. Rounds Done either by the healthcare team or the physician-in-charge, it is the act of going from patient-to-patient to check on and/or discuss their conditions as well as prescribe the succeeding course of treatment. S Sats Slang. See entry: oxygen saturation. Sedate To calm an individual through the use of a sedative. When a person is sedated, the medical management team can conduct medical, 193 diagnostic, or minor surgical procedures which would otherwise cause pain or discomfort to the patients. Patients who are being ventilated are given sedative drugs, so they can tolerate the presence of an endotracheal tube in their trachea. Service As a medical colloquial term, this refers to a team composed of attending consultants, fellows, residents, interns, and medical students. Patients are decked to a service who takes care of them when they are admitted into the hospital. V Ventilators A machine that helps a patient breathe by pumping oxygen into the lungs and removing carbon dioxide through a tube, using a series of controlled pressures and volumes. Viber A phone application used to call or message another individual. Signs Medical sign. An observable physical exam finding, unlike symptoms which pertain to the subjective experience of a patient. Examples of signs are rashes, bruises, and elevated blood pressure. Virus A submicroscopic infectious agent. Viruses infect living organisms and cause diseases. For example, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is the strain of coronavirus that causes the corona virus disease 2019 (COVID-19). T Vital signs Clinical measurements of the patient’s essential functions (e.g. pulse rate, temperature, respiratory rate, and blood pressure). Telemedicine The use of telecommunication technologies to enable long-distance clinician and patient contact. W Toxic A medical colloquial term usually used to describe a difficult duty or shift, usually marked by an overload of tasks, patients, or patient deaths. It may also be used to refer to the person in a difficult shift, or a person with a reputation of being unreasonably strict. Waze A GPS navigation software application. 194 White cells White blood cells (WBC) or leukocytes. A type of blood cell. WBCs are a component of the immune system, in charge of helping the body fight infections and diseases. Z Zoom Zoom is a software platform used for teleconferencing, distance education, social relations, and the like. It gained popularity during the COVID-19 pandemic where a lot of people had to work and study from home. 195 Contributors 196 Authors Lily de Amor (pseudonym) Anna Elvira S. Arcellana, M.D Anna Elvira Arcellana served as the chief fellow of the Division of Endocrinology, Diabetes, and Metabolism. She has a passion for writing, which she hopes to use as an instrument in becoming a better patient advocate. Jill Olivia E. Bañares, R.N. Jill Olivia E. Bañares is an ED nurse who graduated from the University of the Philippines Manila College of Nursing in 2016. She loves serving the underserved and believes in the importance of quality health care for all. Patricia Anne S. Basilio, M.D. John Jefferson V. Besa, M.D. John Jefferson V. Besa aspires to be a clinician-public health physician hybrid. Probably a journalist in an alternate universe, he has a keen eye for the people around him. In his eureka moments, he hopes to make a difference one tweet at a time. Genry Criscel R. Consul From the mundane to the curious, Genry enjoys stories— listening to them, reading them, and writing them. At present, she is studying to become a physician to pursue her call to serve the least, the last, and the lost. Robyn Gayle K. Dychiao but ended up in Medicine. She dreams of working for NASA one day. Robyn is a second year medical student at the UP College of Medicine. When she’s not buried in her books, one can find her trying new recipes, running her business, and catching up on medical dramas. Jubert P. Benedicto, M.D. Amanda Christine F. Esquivel, M.D. Icia Basilio went to UP for Comparative Literature, Dr. Jubert P. Benedicto is a certified pulmonary critical care specialist based in Philippine General Hospital (PGH) and Lung Center of the Philippines (LCP). During this pandemic, he was primarily tasked with mobilizing intensive care services and resources in PGH, coordinating and addressing ICU-related issues, and served as a consultant frontliner going on regular 24-hour duties with his pulmonary team. Mandy is a graduate of the UP College of Medicine Class 2019 and is currently a first year resident of the Department of Dermatology. She has always been interested in exploring the nuances of the art and science of medicine. 197 Sachiko S. Estreller, M.D. Ian Gabriel A. Juyad Sachiko S. Estreller, an internal medicine resident, is a lover of prose, pastries, and positivity. She keeps a journal of unhurried stories at happysleepysloth.wordpress.com. Ian Juyad is a medical intern from the UP College of Medicine. Growing up fascinated by stories, both fictional and real (and everything in between), he finds solace in writing about them - when he’s not busy reading medical textbooks or in clinical rotations. Thaddeus Hinunangan, M.D. Thad Hinunangan is a pathology resident, a columnist for Health and Lifestyle Magazine, and a contributor to Philippine Daily Inquirer. His essays have been published in various anthologies like From the Eyes of a Healer and Youngblood 4. Maria Keziah G. Legion, R.N. Christi Annah Hipona, M.D. Nefren Roy A. Lobitana, M.D. Tia Hipona is a fellow in child and adolescent psychiatry who loves to write about her God and the hope He offers. UPCM 2020. A small town boy with big internist dreams. Writes what will become history. Has a mind full of thoughts but are mostly either food or Taylor Swift lyrics. Athena Mae L. Ibon, M.D. Dr. Athena is a pure bred Cebuana, (a graduate of Matias H. Aznar Memorial College of Medicine) who was awarded for Academic Excellence, Best in Surgery and Leadership in 2019 and Gloria Macapagal Arroyo Medallion in Leadership in 2006. She is a compassionate hustler for the community who always minds the welfare of others. At the same time, she is a lover of music, diving, and an obsessed mother of cats and dogs. 198 A well-rounded artist. A loving daughter anchored with Christian values. A compassionate nurse and peoplecentered leader. Justin Bryan D. Maranan, M.D. A recent graduate of the UP College of Medicine (Class 2020) who served as an intern of PGH at the onset of the COVID-19 pandemic. Also a literary enthusiast who hopes to read more books (and perhaps even write one) in the future - if he ever finds the time. Ella Mae I. Masamayor, M.D. Erika P. Ong Ella Mae I. Masamayor is an internal medicine resident, blogger, and a believer in moving forward, one day at a time. She writes her thoughts at https://ellathinksaloud. wordpress.com/ or on twitter as @ellamimasamayor. Intarmed student Erika Ong is constantly working on improving herself to one day have a shot at improving the world. Her favorite skills to level up include her medical knowledge, stock trading ability, German fluency, and discernment through reading poetry and prose. Viktoria Ines P. Matibag, M.D. A third year OB-GYN resident trying to survive the training program one day at a time. Vince Elic S. Maullon Vince Maullon is currently a medical intern at the Philippine General Hospital. He really misses going on hospital duties. Mikki Miranda, M.D. Dr. Mikki is from UPCM Class of 2016. She loves to paint, travel, watch musicals, and visit art museums. Fr. Marlito Ocon, S.J. He is the head chaplain of the UP-PGH Catholic Chaplaincy. Juan Raphael M. Perez Beyond being a struggling medical student, Raffy Perez is interested in dissecting how the world works. They believe in reason, virtue and compassion, and would do anything to continuously learn as much as they can. Trisha M. Salcedo Trisha Salcedo is a public health graduate with a penchant for marrying her degree with the humanities. Howie Severino Journalist H. Severino survived twice in the first months of 2020 -- he was in his house on the shores of Taal Lake as Taal Volcano erupted. Then, he survived COVID-19 after 11 days in the hospital. Paulo Ross B. Sison, R.N. A guy in his mid-20s having a quarter-life crisis in the middle of a health crisis. Takes care of patients for a living. 199 Cindy Pearl J. Sotalbo, M.D. Cary Amiel G. Villanueva, M.D. Dr. Cindy Sotalbo is a specialist in diagnostic imaging, and vascular and interventional Radiology. She is an avid fan of street photography, creative hobbies, travel and food adventures, and rock music. Cary Amiel G. Villanueva, M.D. pursued internal medicine residency at the Philippine General Hospital after graduating from the University of the Philippines College of Medicine under the Integrated Liberal Arts and Medicine (INTARMED) program in 2017. He enjoys #MedTwitter and evidence-based medicine, and aspires to become a critical care specialist and bioethicist. Amiel is also a project manager of Universitas Foundation, a non-profit organization dedicated to forming principled leaders. Hilda Uy, R.N. Hilda Uy is a Nurse III at the Department of OutPatient Services; but due to the pandemic, she was assigned at the COVID wards for several months. She is now having her duty at Telemedicine since June when the Online Consultation Request and Appointment (OCRA) System officially started. Maria Angela M. Villa, M.D. Dr. Maria Angela M. Villa is a graduating senior resident of the UP-PGH Pediatrics. She is also the president of the PGH Physicians’ Association, representing the association in the healthcare workers’ advocacy group Healthcare Professionals Alliance Against COVID-19 (HPAAC). She writes this article especially for the Filipino healthcare workers. 200 Photo Contributors Isabel Acosta, M.D. Mary Joy Beneciro, R.N. Isabel is a 3rd year resident of PGH’s straight residency training program in plastic surgery. Her first gift from Santa was a film camera —and she has loved taking photos since then. Joy is a devoted mother, wife and nurse. She works at PGH and is currently assigned at Ward 3 (Adult Male Medicine Ward), enthusiastically rendering patient care service to COVID-19 patients. She enjoys watching series and forensic documentaries in her time away from the hospital. Adrianne Alfaro, R.N. Adrianne, more commonly known as Adi, is a graduate of the Pamantasan ng Lungsod ng Maynila College of Nursing Class of 2014, and is currently taking up a degree of Master of Arts in Nursing at the same university. At the same time, she works as a nurse at PGH, taking care of COVID-19 patients at the Adult Male Medicine Ward. In her free time, she enjoys playing game consoles, baking, crocheting, and watching various series on Netflix. Trixie Bacalla, M.D. Trixie is a graduate of San Beda University Manila College of Medicine Class of 2019. She had her postgraduate internship at PGH, and aspires to be an OB-Gyne someday to serve in far-flung areas. She is involved in sociocivic activities and is fond of playing speed cubes and watching korean dramas. Edmond Bries, M.D. Edmond is a first year resident in the urology residency program of PGH. His hobbies include jogging, listening to new wave music and enjoying the finer things in life. His Christmas wish is for this pandemic to be over. Jairus Cabajar, M.D. Jairus Cabajar is a doctor who served as a frontliner during his last year of residency in internal medicine. If he isn’t seeing patients, he spends a lot of time tweeting. He can’t wait until he can tweet that this pandemic is over. Jonas Del Rosario, M.D. Jonas D. Del Rosario, MD is a graduate of the UP College of Medicine Class of 1991. He is an interventional pediatric cardiologist who enjoys photography, playing basketball and biking. He is currently the spokesperson of PGH and UPCM. 201 Martin Ilustre, M.D. Sofia Naval, M.D. Martin is a graduate of the UP College of Medicine Class of 2018 and is currently taking his residency training in Otorhinolaryngology-Head and Neck Surgery in PGH. Pre-pandemic, you would often find him at the beach, playing ultimate Frisbee or hanging with friends. During COVID, he now frequents the halls of his condominium and enjoys long walks to Ward 10 and back. Sofia is a second year ophthalmology resident at PGH. During her free time, she enjoys calming nature walks, taking care of animals, and practicing yoga. Ephraim Leynes, M.D. Epi is a graduate of the UP College of Medicine Class of 2016, and is currently a family and community medicine resident in PGH. He describes himself as a weekday physician and a weekend musician, but his interests reach photography and occasional videography as well. AJ Limbago, M.D. AJ is a graduate of the UP College of Medicine Class of 2019, and is currently a neurosurgery resident in PGH. On the side, he enjoys trying out different kinds of food as well as occasionally watching K-drama. Mikki Miranda, M.D. Dr. Mikki is from UPCM Class of 2016. She loves to paint, travel, watch musicals, and visit art museums. 202 Harjoland Obenieta, M.D. Harj is a graduate of the UP College of Medicine Class of 2018 and is currently a resident of the Department of Orthopedics in PGH. He’s a fun guy with a mean streak, obsessed with anything Muji, soft sheets, and Jollibee peach mango pie. Amanda Oreta, M.D. Amanda is a graduate of the UP College of Medicine Class of 2020, and intends to pursue training in the specialty of ophthalmology. As a form of stress relief, she enjoys baking and cooking, sometimes layout editing, and she has a passion for traveling and experiencing different cultures — most especially through food. Ma. Michelle Palomar, R.N. Michelle is a nurse from the Department of Orthopedics and Spine Unit of PGH, and was also deployed to the COVID units. She likes to watch TV series, loves to travel and explore new places and things, and values friendships and family ties very much. Gianne Pagulayan, M.D. Alla Tan, M.D. Gianne is a graduate of the UP College of Medicine Class of 2020. She enjoys photography and has been part of the documentation team of various organizations she belongs to like the Phi Lambda Delta Sorority, Regionalization Students Organization, UP Medical Students Society, and UP PAGSAMA. Alla is a graduate of the UP College of Medicine Class of 2018. Currently a dermatology resident of the UPPGH, she also works behind the scenes as part of the COVID-19 IEC Committee, creating the official infographics released by the hospital. Her favorite things include photography, graphic design, spicy toro maki, and her dog, RamboTan. Ven Ponce, M.D. Ven is a graduate of the UP College of Medicine Class of 2020, and is currently an incoming resident at the Philippine General Hospital Department of Medicine. When the pandemic hit Manila, she volunteered at the wards to help her seniors and since then, she found her calling in medicine. Trisha M. Salcedo Trisha Salcedo is a public health graduate with a penchant for marrying her degree with the humanities. Yasmin Salces, M.D. Yas is a graduate of the UP College of Medicine Class of 2020, and is an incoming first year resident of PGH Department of Obstetrics and Gynecology. She is a proud member of the Mu Sigma Phi Sorority and UP Medrhythmics. Carl Uy, M.D. Carl is a graduate of the UP College of Medicine (Class of 2017), currently in his second year of residency training in anatomic and clinical pathology at the Philippine General Hospital. Beyond medicine, he spends most of his time either buried in books or indulging in the way of life that is football. Janel Verceles, M.D. Janel is a graduate of the UP College of Medicine Class of 2019, and is currently rotating in general surgery as a first year resident of the plastic surgery program of PGH. She is a lover of dance and music, and enjoys watching movies in her free time. Steff (pseudonym) 203 Brent Viray, M.D. Dr. Brent Viray is the father of two cute kids – Maya and Mareon. He was a Doctor to the Barrio in Dingalan, Aurora, where he was married to Nurse Maycel and also found the marriage of public health and surgery. Denica Tan Yu, M.D. Denica is a graduate of UST - Faculty of Medicine and Surgery Class of 2019 and had her internship at UPPGH. She is currently taking a gap year enjoying some sun and sand back at the province. Her life off-duty would be spent immensed between the pages of a novel, curled up on the couch watching TV, and travelling to appreciate other cultures and meet new people. 204 Editorial Assistants Vince Elic S. Maullon Assistant Editor Vince Maullon is currently a medical intern at the Philippine General Hospital. He really misses going on hospital duties. Denisse Ann L. Tiangco, M.D. Assistant Editor A newly minted physician, Denisse has great love for old school music and cooking. She’s a doctor in the city but an island girl at heart. Copy Editors Aedrian A. Abrilla Ma. Ysabel D. Caballes Sean Kendrich N. Cua Iris D. Ditan Caeley Lois S. Hao Frances Dominique V. Ho Manuel S. Ocampo Jr., M.D. Lorena Margarita B. Osorio Leander T. Quilang, M.D. Marcela Mercedes S. Rodolfo Ma. Chrielle R. San Pedro Nikolai Nzar A. Tubog Social Media Editors Karen Bernasor Amora Trisha Angelie F. Thadhani 205 Communications Team Pamela Bianca M. Pasco Media Head Alicia Anne B. Lantican Content Editor Karmel Althea L. Samonte Content Editor Alena Marie B. Mariano Design Editor Jemil Austin M. Lacson Externals Head Jean Rachel D. Ang Photo Editor Carlo Magno C. Vistro Photo Editor 206 Jana Marie M. Negre Jeremiah V. Reyes Nina Therese S. Domingo Simoune Raphaella P. Licuanan Arlyn Jave B. Adlawon Editors 207 Editors Alvin B. Caballes, M.D. Alfonso Rafael G. Abaya Dr. Alvin Caballes is a pediatric surgeon and is a Professor of the U.P. College of Medicine. He developed an early penchant for creative writing, and honed this by composing letters daily to woo his wife, and conjuring bedtime stories for their three kids. Rafa is a clerk-from-home of the UPCM Class of 2022. If he’s not editing videos or making pubs, he’s probably studying medicine. Editor Amanda Marie Cheong, M.D. Associate Editor Mandi is a newly licensed physician who enjoys writing fiction on the side. She is living the plantita life with her three pet turtles. Gabrielle P. Flores Associate Editor Gaby is an intern from UPCM Class of 2021. She likes going on leisurely walks and diving down Wikipedia hyperlink rabbit holes. Markyn Jared N. Kho, M.D. Photos Editor Markyn is a graduate of the UP College of Medicine Class 2020, and plans to pursue a residency in General Surgery. On the side, he enjoys covering events through photography, binge-watching YouTube videos, traveling to new and exciting places, and devouring all kinds of food. 208 Layout Editor Marie Bernadine D. Caballes Layout Editor Marie is from UPCM Class 2021 and is an intern at PGH. She spends her free time watching movies and watercolor painting. Paul Miguel P. Perez, M.D. Business Editor Paul is a graduate of the UP College of Medicine, studying for the Physician Licensure Exam at the time of writing and is now an Internal Medicine resident at PGH. The PGH facade was lit up in the colors of the Philippine flag on Independence Day 2020 to honor the healthcare workers and hospital staff who have served during the pandemic. Photo by WABS Lights and Sounds 209