Neurology Lecture Notes: Embryology & Cellular Function
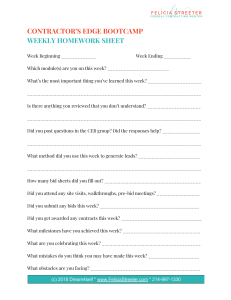
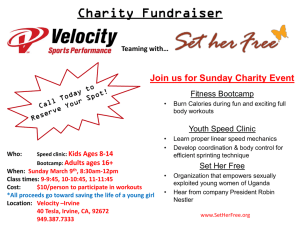
advertisement

TABLE OF CONTENTS Neurology 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. Embryology Cellular Function Ascending Spinal Cord Tracts Descending Spinal Cord Tracts Brainstem Anatomy Cerebral Cortex Radiculopathy Spinal Cord Syndromes Invasive Spinal Cord Disease Demyelinating Disease Conduction Physiology Neuromuscular Junction (NMJ) Cranial Nerves 1-6 Cranial Nerves 7-12 Vision TABLE OF CONTENTS Neurology 16. Auditory Sensation 17. Vertigo 18. Pediatric Brain Tumors 19. Adult Primary Brain Tumors 20. Ischemic Cerebrovascular Accidents 21. Aneurysms and Intracranial Hemorrhage 22. Cerebellum and Ventricles 23. Diencephalon 24. Basal Ganglia 25. Neurotransmitter Activity in Psychiatric Disease 26. Dementia 27. Headache 28. Seizures 29. Traumatic Brain Injuries OUTLINE Neurology: Embryology 1. Embryology ● ● ● ● ● A. Notochord B. Neural Tube C. Meninges D. Origins of Nervous Tissue E. Neural Tube Defects Neurology: Embryology Bootcamp.com • Notochord • Derived from mesoderm • Stimulation of ectoderm à neuroectoderm • ~2.5 weeks gestation • Neural Tube • Derived from medial ectoderm • Fuses dorsally à neural tube • ~3 weeks gestation https://commons.wikimedia.org/wiki/File:2912_Neurulation-02.jpg Neurology: Embryology • Epidural Space • Epidural anesthesia • Epidural hematoma • Dura Mater • Derived from mesoderm • Subdural Space • Subdural hematoma • Arachnoid Mater • Derived from neural crest cells • Subarachnoid Space • Contains CSF • Lumbar puncture • Subarachnoid Hemorrhage • Pia Mater • Derived from neural crest cells Bootcamp.com Neurology: Embryology Bootcamp.com Origins of Nervous Tissue Embryologic Origin Forebrain Midbrain Hindbrain Vesicle High Yield Derivatives Diencephalon Hypothalamus Thalamus Pineal gland Telencephalon Cerebral hemispheres Basal ganglia (not all of it) Mesencephalon Midbrain Metencephalon Cerebellum Pons Myelencephalon Medulla Prosencephalon Mesencephalon Rhombencephalon Neurology: Pathophysiology: Brain • Anencephaly • Failure of rostral neuropore closure • Elevated AFP Bootcamp.com Embryologic Cranial Defects Syndrome Anencephaly Lissencephaly Detail Signs and Symptoms Absence of forebrain Fatal, incompatible with life Lack of cortical sulci and gyri Microcephaly Ventriculomegaly Hydrocephalus Craniofacial abnormalities Neurology: Pathophysiology: Spinal Cord Bootcamp.com Spinal Defects Syndrome Detail Signs and Symptoms Spina Bifida Occulta Vertebral Defect Patch of hair Skin dimple Meningocele Meninges through vertebral defect +/- Motor impairment, developmental delay, bladder and bowel incontinence Myelomeningocele Spinal cord through vertebral defect https://commons.wikimedia.org/wiki/File:Typesofspinabifida.jpg ≣ Item 1 of 1 Question ID: 0001 ◽" Mark ⟽ ⟾ Previous ⚪ A. Failure of closure of the rostral neuropore ⚪ B. Failure of closure of the caudal neuropore ⚪ C. Degeneration of anterior horn cells ⚪ D. Protrusion of meninges through a bony defect ⚪ E. Protrusion of neural tissue through a bony defect Next Test Your Knowledge Difficulty: ✪ Bootcamp.com A 27-year-old female with a past medical history of generalized anxiety disorder and recurring seizures that began during adolescence presents to her obstetrician reporting that she had multiple positive pregnancy tests over the course of the past 18 weeks. She states that she has avoided prenatal care up to this point because she has felt more anxious since she found out she was pregnant. She also states that she has been taking more of her medications to calm her anxiety. When questioned she mentions she is particularly concerned of her higher stress levels precipitating a seizure episode. Her last seizure episode was approximately 4 years prior to this visit. Her vitals are stable. Prenatal and fetal assessments are performed and some of the results are shown below. Which of the following pathologic processes are most consistent with the patient’s lab and imaging results? Urine dipstick negative for protein. Random glucose 108 mg/dL Fetal ultrasound findings are displayed. Amniotic fluid index 44cm (reference range <25cm) Serum alpha fetal protein elevated. https://commons.wikimedia.org/wiki/File:Ultrasound_Scan_ND_145330_1455290_cr.png ≣ Item 1 of 1 Question ID: 0001 ◽" Mark ⟽ ⟾ Previous " A. Failure of closure of the rostral neuropore ⚪ B. Failure of closure of the caudal neuropore ⚪ C. Degeneration of anterior horn cells ⚪ D. Protrusion of meninges through a bony defect ⚪ E. Protrusion of neural tissue through a bony defect Next Test Your Knowledge Difficulty: ✪ Bootcamp.com A 27-year-old female with a past medical history of generalized anxiety disorder and recurring seizures that began during adolescence presents to her obstetrician reporting that she had multiple positive pregnancy tests over the course of the past 18 weeks. She states that she has avoided prenatal care up to this point because she has felt more anxious since she found out she was pregnant. She also states that she has been taking more of her medications to calm her anxiety. When questioned she mentions she is particularly concerned of her higher stress levels precipitating a seizure episode. Her last seizure episode was approximately 4 years prior to this visit. Her vitals are stable. Prenatal and fetal assessments are performed and some of the results are shown below. Which of the following pathologic processes are most consistent with the patient’s lab and imaging results? Urine dipstick negative for protein. Random glucose 108 mg/dL Fetal ultrasound findings are displayed Amniotic fluid index 44cm (reference range <25cm) Serum alpha fetal protein elevated https://commons.wikimedia.org/wiki/File:Ultrasound_Scan_ND_145330_1455290_cr.png OUTLINE Neurology: Cellular Function 1. Neuronal Cells ● ● ● ● A. Cell Types B. Neuronal Anatomy C. Neuronal Injury D. Wallerian Degeneration 2. Sensory Receptors ● ● A. Pain Fibers B. Corpuscles and Disc Receptors Neurology: Cellular Function Bootcamp.com • Schwann Cells (PNS) • • • • 1 cell myelinates 1 axon Neural crest cell origin, S100 positive Efficient in Wallerian degeneration and regeneration Classic pathology associations: GBS, acoustic neuroma • Oligodendrocytes (CNS) • • • • 1 cell myelinates many axons Neuroectoderm origin Not effective in Wallerian degeneration and regeneration (vs Schwann) Classic pathology associations: MS, PML, Oligodendroglioma • Astrocytes • • • • Assist in maintenance of blood-brain barrier Neuroectoderm origin Glial Fibrillary Acidic Protein (GFAP) Marker Classic pathology association: Glioblastoma multiforme • Microglia • • • Phagocytes of CNS Mesoderm origin HIV associated dementia https://commons.wikimedia.org/wiki/File:Oligodendrocyte_HE_stain_ high_mag.jpg https://commons.wikimedia.org/wiki/File:Anaplastic_astrocytoma__gfap_-_very_high_mag.jpg Neurology: Cellular Function Bootcamp.com • Neuron Anatomy • Soma: Primarily contains cell organelles including Nissl substance • Axon: Slender, cylindrical projection for conduction action potentials • Dendrite: Small projections used to receive input, contains Nissl substance • Nissl Substance = Rough endoplasmic reticulum • Neuron Motor Physiology • Kinesin: Motor protein for anterograde transport • Dynein: Motor protein for retrograde transport • Neuron Injury • Cellular edema, peripheral nucleus • Chromatolysis https://commons.wikimedia.org/wiki/File:NisslHippo2.jpg https://commons.wikimedia.org/wiki/File:Blausen_0657_MultipolarNeuron.png Neurology: Cellular Function Bootcamp.com • Wallerian Degeneration • Proximal axonal membrane retained (axonal retraction) • Distal degeneration and clearing of axonal debris • Axotomy PNS • Schwann cells à separate myelin into fragments and promote regeneration • Macrophages remove axonal debris • Axotomy CNS • Oligodendrocytes are inefficient at removing myelin • Macrophages must cross blood-brain barrier https://commons.wikimedia.org/wiki/File:Blausen_0657_MultipolarNeuron.png Neurology: Cellular Function Bootcamp.com Sensory Receptors of the Nervous System Sensory Receptor Size, Myelination Primary Sensory Transmission High Yield Association A! fibers Myelinated Temperature Pain (Mechanical) Fast conduction velocity Higher space constant Lower time constant C fibers Unmyelinated Pain (General) Slow conduction velocity Lower space constant Higher time constant Neurology: Cellular Function Bootcamp.com Sensory Receptors of the Nervous System Sensory Receptor Size, Myelination Primary Sensory Transmission Meissner Corpuscles Can be mixed Fine and light touch Low frequency vibration Located in areas without hair Histology: dermal papillae Pacinian Corpuscles Large, Myelinated Deep touch and pressure High frequency vibration Histology: “Onion-skin” Merkel Discs Large, Myelinated Pressure Proprioception Located on fingertips and areas hair follicles Ruffini Corpuscles Large, Myelinated Low frequency vibration Sustained pressure Joints https://commons.wikimedia.org/wiki/File:Meissners_Corpuscle_(3384752409).jpg https://upload.wikimedia.org/wikipedia/commons/5/58/Pacinian_Corpuscles_%281072806656%2 9.jpg High Yield Association ≣ Item 1 of 1 Question ID: 0002 ◽" Mark ⟽ ⟾ Previous ⚪ A. Glial fibrillary acid protein positive ⚪ B. Multinucleated giant cells ⚪ C. S100 positivity ⚪ D. Embryonic glomerular structures ⚪ E. Cells with a “fried-egg” appearance on histology Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com A 19 year old male college student reports to the emergency room after stating that he can no longer put up with the “sirens going off in his head”. He reports a long history of vertigo since he was a child. He states that he has tried numerous types of medicine and has seen multiple specialists in the past with no resolve. He also reports having to sit in the front row recently during lectures on campus because he cannot hear the professors as well as his classmates. Which of the following pathologic findings would be most consistent with a biopsy of the tumor(s) causing this patient’s symptoms? https://radiopaedia.org/cases/bilateral-acoustic-schwannomas-on-a-background-ofneurofibromatosis-type-2 ≣ Item 1 of 1 Question ID: 0002 ◽" Mark ⟽ ⟾ Previous ⚪ A. Glial fibrillary acid protein positive ⚪ B. Multinucleated giant cells " C. S100 positivity ⚪ D. Embryonic glomerular structures ⚪ E. Cells with a “fried-egg” appearance on histology Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com A 19 year old male college student reports to the emergency room after stating that he can no longer put up with the “sirens going off in his head”. He reports a long history of vertigo since he was a child. He states that he has tried numerous types of medicine and has seen multiple specialists in the past with no resolve. He also reports having to sit in the front row recently during lectures on campus because he cannot hear the professors as well as his classmates. Which of the following pathologic findings would be most consistent with a biopsy of the tumor(s) causing this patient’s symptoms? https://radiopaedia.org/cases/bilateral-acoustic-schwannomas-on-a-background-ofneurofibromatosis-type-2 OUTLINE Neurology: Ascending Spinal Cord Tracts 1. Ascending Spinal Cord Tracts ● ● ● A. Spinothalamic Tract B. Dorsal Column-Medial Leminiscus C. Spinocerebellar Tract 2. Anatomical Considerations ● ● A. Fasciculi of Dorsal Columns B. Visual Representation of Tracts Neurology: Ascending Spinal Cord Tracts Bootcamp.com Ascending Tracts Tract Lateral Spinothalamic Sensation and Function High Yield Neuroanatomy Pain Temperature Travels 1-2 spinal levels superiorly prior to decussation Pain (General) Anterior Spinothalamic Crude Touch Pressure Neurology: Ascending Spinal Cord Tracts Bootcamp.com Ascending Tracts Tract Lateral Spinothalamic Sensation and Function High Yield Neuroanatomy Pain Temperature Travels 1-2 spinal levels superiorly prior to decussation Pain (General) Anterior Spinothalamic Crude Touch Pressure Dorsal Column-Medial Lemniscus (DCML) Fine Touch, Low frequency vibration à (Meissner corpuscles) Proprioception (Muscle spindles) Pressure and High Frequency Vibrationà (Pacinian) Decussation at medulla Fasciculus gracilis: Approximately T6 and below (located medially in dorsal column) Fasciculus cuneatus: Approximately T5 and above (located laterally in dorsal column) Neurology: Ascending Spinal Cord Tracts Bootcamp.com Ascending Tracts Tract Lateral Spinothalamic Sensation and Function High Yield Neuroanatomy Pain Temperature Travels 1-2 spinal levels superiorly prior to decussation Pain (General) Anterior Spinothalamic Crude Touch Pressure Dorsal Column-Medial Lemniscus (DCML) Fine Touch, Low frequency vibration à (Meissner corpuscles) Proprioception (Muscle spindles) Pressure and High Frequency Vibrationà (Pacinian) Decussation at medulla Fasciculus gracilis: Approximately T6 and below (located medially in dorsal column) Fasciculus cuneatus: Approximately T5 and above (located laterally in dorsal column) Spinocerebellar Unconscious proprioception All fibers carry data to the ipsilateral cerebellum. This may involve ”double decussation”. Neurology: Ascending Spinal Cord Tracts https://commons.wikimedia.org/wiki/File:Spinal_cord_tracts_-_English.svg Bootcamp.com ≣ Item 1 of 1 Question ID: 0003 ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com A 24-year-old female with recently diagnosed with Hashimoto’s thyroiditis presents to the emergency room stating that she has been experiencing ⚪ A. Symmetrical demyelination of fasciculus gracilis progressively worsening difficulty walking for the past couple of months. ⚪ B. Fluid filled obstructive syrinx of central spinal canal She reports that her feet go numb and she feels like she is losing her ⚪ C. Molecular mimicry to gangliosides of dorsal columns balance. She is very concerned of falling and reports that today she had a ⚪ D. Oligodendrocyte demyelination optic nerve ⚪ E. Mitochondrial dysfunction of cells in the prefrontal cortex particularly bad episode of acute numbness of both feet prior to arrival. This has been difficult for her to cope with as she had previously been a half marathon runner. She states that she also has had a significant drop in her productivity and energy. Her vital signs and significant lab studies are shown below. Which of the following pathologic findings are most consistent with this presentation? Temperature: 99.0F (37.2C) Heart rate: 101 beats per minute Respiratory rate: 16 breaths per minute Blood pressure: 98/54 Hemoglobin: 9.4 g/dL Mean corpuscular volume: 110 Total bilirubin: 1.2 mg/dL (ref. range 0.3-1.0 mg/dL) Thyroid stimulating hormone: normal Anti-intrinsic factor antibody: positive ≣ Item 1 of 1 Question ID: 0003 ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com A 24-year-old female with recently diagnosed with Hashimoto’s thyroiditis presents to the emergency room stating that she has been experiencing $ A. Symmetrical demyelination of fasciculus gracilis progressively worsening difficulty walking for the past couple of months. ⚪ B. Fluid filled obstructive syrinx of central spinal canal She reports that her feet go numb and she feels like she is losing her ⚪ C. Molecular mimicry to gangliosides of dorsal columns balance. She is very concerned of falling and reports that today she had a ⚪ D. Oligodendrocyte demyelination optic nerve ⚪ E. Mitochondrial dysfunction of cells in the prefrontal cortex particularly bad episode of acute numbness of both feet prior to arrival. This has been difficult for her to cope with as she had previously been a half marathon runner. She states that she also has had a significant drop in her productivity and energy. Her vital signs and significant lab studies are shown below. Which of the following pathologic findings are most consistent with this presentation? Temperature: 99.0F (37.2C) Heart rate: 101 beats per minute Respiratory rate: 16 breaths per minute Blood pressure: 98/54 Hemoglobin: 9.4 g/dL Mean corpuscular volume: 110 Total bilirubin: 1.2 mg/dL (ref. range 0.3-1.0 mg/dL) Thyroid stimulating hormone: normal Anti-intrinsic factor antibody: positive OUTLINE Neurology: Descending Spinal Cord Tracts 1. Motor Neurons ● ● ● A. Types of Motor Neurons B. Fundamental Spinal Cord Anatomy C. Motor Neuron Lesion Presentation 2. Descending Spinal Cord Tracts ● ● ● ● A. Corticospinal Tract B. Corticobulbar Tract C. Extrapyramidal Tracts D. Visual Representation of Tracts Neurology: Descending Spinal Cord Tracts Bootcamp.com • Gray Matter • • • Ventral Horn à !-motor neurons à motor (efferent nerve root fibers) Dorsal Horn à sensory neurons à sensory and reflexes (afferent nerve root fibers) Lateral Horn à Sympathetics (T1-L2) Motor Neurons Type Innervation Significance !-motor neurons Extrafusal muscle fibers Contraction of skeletal muscle "-motor neurons Intrafusal muscle fibers Regulates muscle spindle sensitivity https://commons.wikimedia.org/wiki/File:Spinal_nerve.svg Neurology: Descending Spinal Cord Tracts Bootcamp.com Motor Neuron Lesion Signs Upper Lower Hallmark Location Corticospinal tract UMN Corticobulbar tract UMN Anterior horn à NMJ LMNs Clinical Signs Hypertonia Hyperreflexia Muscle weakness Spastic paresis Babinski sign (upgoing) Hypotonia Hyporeflexia Flaccid paresis Muscle atrophy Fasciculations Neurology: Descending Spinal Cord Tracts Bootcamp.com Descending Tracts Extrapyramidal Pyramidal Tract Primary Sensation and Function High Yield Neuroanatomy Lateral Corticospinal Voluntary Muscle Movement (general) Pyramidal decussation at inferior medulla Terminate in ventral horn Lower extremity à Lateral Anterior Corticospinal Voluntary Muscle Movement (general) Remains ipsilateral in medulla Decussation at termination in ventral horn at specific cervical and thoracic segments Neurology: Descending Spinal Cord Tracts Bootcamp.com Descending Tracts Extrapyramidal Pyramidal Tract Primary Sensation and Function High Yield Neuroanatomy Lateral Corticospinal Voluntary Muscle Movement (general) Pyramidal decussation at inferior medulla Terminate in ventral horn Lower extremity à Lateral Anterior Corticospinal Voluntary Muscle Movement (general) Remains ipsilateral Decussation at termination in ventral horn at specific cervical and thoracic segments Corticobulbar Voluntary Muscle Movement (head and neck) Contralateral innervation only with: -Inferior quadrant of face CN VII -CN XII Neurology: Descending Spinal Cord Tracts Bootcamp.com Descending Tracts Extrapyramidal Pyramidal Tract Primary Sensation and Function High Yield Neuroanatomy Lateral Corticospinal Voluntary Muscle Movement (general) Pyramidal decussation at inferior medulla Terminate in ventral horn Lower extremity à Lateral Anterior Corticospinal Voluntary Muscle Movement (general) Remains ipsilateral Decussation at termination in ventral horn at specific cervical and thoracic segments Corticobulbar Voluntary Muscle Movement (head and neck) Reticulospinal Rubrospinal Tectospinal Vestibulospinal Vestibulospinalà balance and posture Tectospinal à Head movements per vision Contralateral innervation only with -Inferior quadrant of face CN VII -CN XII Rubrospinal à Red nucleus Neurology: Spinal Cord Tracts https://commons.wikimedia.org/wiki/File:Spinal_cord_tracts_-_English.svg Bootcamp.com A Image Credit: Wikipedia PS PS ASA Bootcamp.com A Neurology: Spinal Cord Tracts ≣ Item 1 of 1 Question ID: 0004 ◽" Mark ⚪ A. Inferiorly directed left lens dislocation ⚪ B. Left sided deviation of the tongue ⚪ C. Fasciculations of the left gastrocnemius muscle ⚪ D. Atrophy of the tongue ⚪ E. Bilateral abducens nerve palsy ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪✪ Bootcamp.com A 17-year-old male with a history of Marfan syndrome is brought to the emergency department by his parents for acute onset neck swelling and headache that started 45 minutes prior to arrival. His father reports that his son was riding his bike at which time he hit a curb and fell, bracing his fall with his right arm. A cervical spine collar is placed for immobilization. He also states that his son has a history of seasonal allergies and has never had swelling similar to this in the past. On physical exam he has a heart rate of 103 beats per minute and his vitals signs are otherwise stable. The chest shows a pectus deformity and is otherwise unremarkable. The right upper extremity and left knee have minor lacerations. Muscle strength is 5/5 in the upper and lower extremities. Funduscopic exam is unremarkable with no evidence of optic disc edema. There is also left eye drooping noted and an apparent left sided 3.5 cm neck mass. During the exam, the patient states that he is hearing an intermittent ”buzzing sound” in the room that is not apparently heard by staff. Imaging studies later reveal a left sided internal carotid artery dissection. Which of the following additional findings would be most consistent with this patient’s presentation? ≣ Item 1 of 1 Question ID: 0004 ◽" Mark ⚪ A. Inferiorly directed left lens dislocation $ B. Left sided deviation of the tongue ⚪ C. Fasciculations of the left gastrocnemius muscle ⚪ D. Significant atrophy of the tongue musculature ⚪ E. Bilateral abducens nerve palsy ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪✪ Bootcamp.com A 17-year-old male with a history of Marfan syndrome is brought to the emergency department by his parents for acute onset neck swelling and headache that started 45 minutes prior to arrival. His father reports that his son was riding his bike at which time he hit a curb and fell, bracing his fall with his right arm. A cervical spine collar is placed for immobilization. He also states that his son has a history of seasonal allergies and has never had swelling similar to this in the past. On physical exam he has a heart rate of 103 beats per minute and his vitals signs are otherwise stable. The chest shows a pectus deformity and is otherwise unremarkable. The right upper extremity and left knee have minor lacerations. Muscle strength is 5/5 in the upper and lower extremities. Funduscopic exam is unremarkable with no evidence of optic disc edema. There is also left eye drooping noted and an apparent left sided 3.5 cm neck mass. During the exam, the patient states that he is hearing an intermittent ”buzzing sound” in the room that is not apparently heard by staff. Imaging studies later reveal a left sided internal carotid artery dissection. Which of the following additional findings would be most consistent with this patient’s presentation? https://commons.wikimedia.org/wiki/File:Gray794.png OUTLINE Neurology: Brainstem Anatomy 1. Brainstem Anatomy ● ● ● ● ● A. Midbrain B. Pons C. Tectum D. Medulla D. Introduction to the Rule of 4’s 2. ● Rule of 4’s A. Introductory Review Neurology: Brainstem Anatomy Bootcamp.com Brainstem Syndrome Midbrain Embryonic Origin Mesencephalon Blood Supply Significant Structures Branches of Posterior Cerebral Artery and Superior Cerebellar Artery CN III-IV nuclei Substantia Nigra Red Nucleus Pretectal Area Medial Longitudinal Fasciculus Superior Cerebellar Peduncles Neurology: Brainstem Anatomy • Tectum of Brainstem • Superior Colliculi à Lateral Geniculate Body àVision • Inferior Colliculi à Medial Geniculate Body à Auditory Bootcamp.com Neurology: Brainstem Anatomy Bootcamp.com Brainstem Syndrome Embryonic Origin Midbrain Mesencephalon Pons Metencephalon (hindbrain) Blood Supply Significant Structures Branches of Posterior Cerebral Artery and Superior Cerebellar Artery CN III-IV nuclei Substantia Nigra Red Nucleus Pretectal Area Medial Longitudinal Fasciculus Superior Cerebellar Peduncles Ventral: Basilar Artery Lateral: Anterior Inferior Cerebellar Artery CN V-VIII* nuclei Reticular Activating System Medial Longitudinal Fasciculus Neurology: Brainstem Anatomy Bootcamp.com Brainstem Syndrome Embryonic Origin Midbrain Mesencephalon Pons Metencephalon (hindbrain) Medulla Myelencephalon (hindbrain) Blood Supply Significant Structures Branches of Posterior Cerebral Artery and Superior Cerebellar Artery CN III-IV nuclei Substantia Nigra Red Nucleus Pretectal Area Medial Longitudinal Fasciculus Superior Cerebellar Peduncles Ventral: Basilar Artery Lateral: Anterior Inferior Cerebellar Artery CN V-VIII* nuclei Reticular Activating System Medial Longitudinal Fasciculus Medial: Anterior Spinal Artery and/or Vertebral Arteries Lateral: Posterior Inferior Cerebellar Artery CN VIII* nuclei CN IX-XII nuclei Area Postrema Inferior cerebellar peduncules Neurology: Brainstem Anatomy • Rule 1: • • • • • Injury Site CN III, IV, VI, XII in midline (divisible by 12) Rule 3: • • • • • • Corticobulbar Tract Lesions Rule 2: • • CN I and II NOT in the midbrain CN III-IV nuclei in midbrain CN V-VIII* nuclei in pons CN VIII*-XII nuclei in medulla Bootcamp.com 4 primary midline structures begin with “m” Motor pathway (CST) Medial lemniscus (dorsal column pathway) Medial longitudinal fasciculus (does not extend into medulla) Motor Nuclei of cranial nerves (CN III, IV, V, VI, VII, IX, X, XI XII) Bulbar Palsy LMN Pseudobulbar Palsy UMN Rule 4: • • • • • 4 lateral or side structures begin with “s” Spinothalamic pathway Sensory Nuclei of CN V Sympathetic pathway Spinocerebellar tract ≣ Item 1 of 1 Question ID: 0005 ⚪ A. Mammillary body ⚪ B. Medial temporal lobe ⚪ C. Dorsal medulla ⚪ D. Ventral midbrain ⚪ E. Substantia gelatinosa ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com A laboratory scientist is attempting to test whether dopaminergic depletion in mice via an intra-striatal infusion of 6-hydroxydopamine (6-OHDA) produces similar effects to those seen in the setting of Parkinson Disease in humans. 6-OHDA is known to be neurotoxic to dopaminergic and noradrenergic neural tissue. The researcher uses desipramine to selectively protect noradrenergic receptors in select mice. Object recognition time and cognitive testing using rodent variants of tests used in humans were evaluated to determine if mice experienced similar effects to humans with Parkinson Disease. Mice were also given physostigmine and rivastigmine to evaluate the nature of reversal of disease process. Which neuroanatomical location is most likely directly impacted by the neurotoxicity of 6-OHDA? ≣ Item 1 of 1 Question ID: 0005 ⚪ A. Mammillary body ⚪ B. Medial temporal lobe ⚪ C. Dorsal medulla " D. Ventral midbrain ⚪ E. Substantia gelatinosa ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com A laboratory scientist is attempting to test whether dopaminergic depletion in mice via an intra-striatal infusion of 6-hydroxydopamine (6-OHDA) produces similar effects to those seen in the setting of Parkinson Disease in humans. 6-OHDA is known to be neurotoxic to dopaminergic and noradrenergic neural tissue. The researcher uses desipramine to selectively protect noradrenergic receptors in select mice. Object recognition time and cognitive testing using rodent variants of tests used in humans were evaluated to determine if mice experienced similar effects to humans with Parkinson Disease. Mice were also given physostigmine and rivastigmine to evaluate the nature of reversal of disease process. Which neuroanatomical location is most likely directly impacted by the neurotoxicity of 6-OHDA? OUTLINE Cerebral Cortex 1. Cerebral Cortex ● ● ● ● ● A. Frontal Lobe B. Temporal Lobe C. Parietal Lobe D. Occipital Lobe E. Internal Capsule Neurology: Cerebral Cortex • Frontal Lobe • Precentral Gyrusà Primary Motor Cortex • Prefrontal Cortex à Personality, concentration, judgement • Front Eye Fields à Conjugate gaze contralateral • Broca's Area (dominant) à Speech production • Lesion to Frontal Lobe • Precentral Gyrusà Contralateral motor • Prefrontal Cortex à Disinhibition • Front Eye Fields à Eye deviation to the side of lesion • Broca’s Area (dominant) à Expressive aphasia • Blood Supply: Medial: ACA, Lateral: MCA https://commons.wikimedia.org/wiki/File:Human_brain_frontal_(coronal)_section.JPG https://commons.wikimedia.org/wiki/File:FrontalCaptsLateral.png Bootcamp.com Neurology: Cerebral Cortex • Temporal Lobe • Primary Auditory Cortex, input from medial geniculate body • Wernicke’s Area (dominant) à Understanding speech • Amygdalaà Memory, decision making, emotions • Optic Radiations à Meyer’s Loop • Lesion to Temporal Lobe • Primary Auditory Cortex à Hearing deficits • Wernicke’s Area (dominant) à Receptive aphasia • Amygdalaà Kluver-Bucy Syndrome • Optic Radiations à Contralateral Superior quadrantanopia • Blood Supply à Mostly MCA https://commons.wikimedia.org/wiki/File:Gray_718-amygdala.png Bootcamp.com Neurology: Cerebral Cortex Bootcamp.com • Parietal Lobe • Postcentral gyrusà Primary Somatosensory Cortex • Angular Gyrus à Visual Cortex • Optic Radiations à Superior Loop • Lesion to Parietal Lobe • Primary Somatosensory Cortex à Contralateral sensory loss • Visual Association Cortex à Gerstmann Syndrome (dominant), Hemineglect (nondominant) • Arcuate Fasciculus à Conduction Aphasia • Optic Radiations à Contralateral Inferior quadrantopsia • Blood Supply à Medial: ACA, Lateral: MCA https://commons.wikimedia.org/wiki/File:Human_brain_frontal_(coronal)_section.JPG Neurology: Cerebral Cortex Bootcamp.com • Occipital Lobe • Primary Visual Cortex, input from lateral geniculate body • Lesion to Occipital Lobe • Primary Visual Cortex à Contralateral homonymous hemianopia, macular sparing • Blood Supply à PCA Neurology: Cerebral Cortex Bootcamp.com • Internal Capsule • Anterior Limb: 1. Ascending sensory fibers: Thalamocortical tracts • Posterior Limb: 1. 2. Descending motor fibers: Corticospinal tract Ascending sensory fibers: Thalamocortical and somatosensory tracts (acoustic, visual) • Genu: 1. Descending motor fibers: Corticobulbar tract • Blood Supply à Lenticulostriate arteries ≣ Item 1 of 1 Question ID: 0006 ⚪ A. Right frontal lobe ⚪ B. Right parietal lobe ⚪ C. Left parietal lobe ⚪ D. Left occipital lobe ⚪ E. Right occipital lobe ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com A 77 year old right-handed female with a past medical history of hypertension and hyperlipidemia presents to the emergency department from a retired living facility for unusual behavior. Paramedics report that the patient was playing a card game with residents of her facility and was unable to hold her cards in her hands. Staff from her living facility also report that she was unable to sign documentation over the past couple of weeks saying that she ”could not remember how to write her signature”. On physical exam cranial nerves III-XII are grossly intact with no deficits in visual acuity. Reflexes are 2+ bilaterally and muscle strength is 5/5 bilaterally in the upper and lower extremities with the exception of handgrip strength testing which was deferred by the patient. Sensory deficits are present to touch and vibration along the right extremities. No tremors are noted. A mini mental status exam is preformed of which deficits are noted when the patient is asked to count backward by sevens. The patient is also unable to hold a pencil in her right hand. No deficits are appreciated in speech or prosody. A CT imaging study of the head reveals a small to medium-sized mass in the cerebral cortex. Which of the following locations of the mass are most consistent with the patient’s presentation? ≣ Item 1 of 1 Question ID: 0006 ⚪ A. Right frontal lobe ⚪ B. Right parietal lobe $ C. Left parietal lobe ⚪ D. Left occipital lobe ⚪ E. Right occipital lobe ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com A 77-year-old right-handed female with a past medical history of hypertension and hyperlipidemia presents to the emergency department from a retired living facility for unusual behavior. Paramedics report that the patient was playing a card game with residents of her facility and was unable to hold her cards in her hands. Staff from her living facility also report that she was unable to sign documentation over the past couple of weeks saying that she ”could not remember how to write her signature”. On physical exam cranial nerves III-XII are grossly intact with no deficits in visual acuity. Reflexes are 2+ bilaterally and muscle strength is 5/5 bilaterally in the upper and lower extremities with the exception of handgrip strength testing which was deferred by the patient. Sensory deficits are present to touch and vibration along the right extremities. No tremors are noted. A mini mental status exam is preformed of which deficits are noted when the patient is asked to count backward by sevens. The patient is also unable to hold a pencil in her right hand. No deficits are appreciated in speech or prosody. A CT imaging study of the head reveals a small to medium-sized mass in the cerebral cortex. Which of the following locations of the mass are most consistent with the patient’s presentation? OUTLINE Neurology: Radiculopathy 1. General Spinal Cord Function ● ● A. Anatomical Considerations B. Reflex by Level 2. Spinal Cord Impingement ● ● ● ● A. Vertebral Disc Herniation B. Radiculopathy by Level C. Spinal Stenosis D. Neuropathic vs Vascular Claudication Neurology: Anatomy & Histology • Spinal Nerve Roots • • C1-C7 exit ABOVE corresponding vertebra C8 and caudal exit BELOW corresponding vertebra • Spinal Cord Anatomical Considerations • • Terminates at L1-L2 in adults Iliac crest at the level of L4 as landmark for lumbar puncture Bootcamp.com Neurology: Anatomy & Histology Bootcamp.com Reflex and Spinal Level Reflex Primary Muscle Spinal Level Tested Biceps Biceps brachii C5-C6 Brachioradalis Brachioradalis C5-C6 Triceps Triceps C7-C8 Cremasteric Cremaster L1-L2 Patellar Quadriceps L2-L4 Achilles Gastrocnemius S1-S2 Bulbospongiosus Bulbospongiosus S2-S4 Sphincteric External Anal Sphincter S2-S4 Neurology: Anatomy & Histology Bootcamp.com • Spinal Disc Herniation • • • L5-S1 is the most common site Affected nerve root usually 1 segment below Ex. L5-S1 disc herniation à S1 radiculopathy https://commons.wikimedia.org/wiki/File:Lagehernia.png https://commons.wikimedia.org/wiki/File:Blausen_0484_HerniatedLumbarDisc.png Neurology: Anatomy & Histology Bootcamp.com Radiculopathy Level Dermatome Classic Finding C5 Anterolateral upper arm Shoulder Loss of Biceps Reflex C7 Middle finger Loss of Triceps Reflex L4 Anteromedial leg Medial malleolus Knee Anterior thigh Loss of Patellar Reflex L5 Most digits of foot Anterior leg Anterolateral thigh Foot Drop S1 Lateral Malleolus Posterolateral leg and thigh Loss of Achilles Reflex Inability to “toe walk” https://commons.wikimedia.org/wiki/File:Grant_1962_663.png Neurology: Anatomy & Histology Bootcamp.com Claudication • Spinal Stenosis • • • • • • Neuropathic claudication (Pseudo) Affected by changes in posture Back pain (classically low back) Worse in extension Initial test à Radiography spine Confirmatory test à MRI spine Neuropathic (Pseudo) Vascular Localization Bilateral Unilateral Pain Location Back, radiating down proximal lower extremities Distal lower extremity Type of Pain Sharp, stabbing, radiating Tight, crampy Worse Spinal extension Movement Better Spinal flexion Rest Initial Diagnostic Study Radiography of spine Ankle Brachial Index ≣ Item 1 of 1 ◽" Mark Question ID: 0007 ⚪ A. Left L4 nerve root ⚪ B. Right L4 nerve root ⚪ C. Left L5 nerve root ⚪ D. Left S1 nerve root ⚪ E. Left S2 nerve root ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪ Bootcamp.com A 29-year-old male with no significant past medical history reports shooting, “electric-like” pain down the left buttock and lower extremity when sitting for the past two weeks. He also states that occasionally when he attempts to run for more than five minutes, the pains progressively worsen to the point where he is unable to walk. Pertinent findings on physical exam include 2+ reflexes at the patellar tendon bilaterally and right Achilles tendon. No reflex was obtained during testing of the left Achilles tendon. The patient is able to perform heel-walk, although he is unable to stand on the toes. There is also a loss of sensation to touch and vibration at the lateral malleolus. No pain is appreciated when palpating the lower back and there is no evidence of any “step off” signs. Lumbar radiography and MRI are shown. Which of the following nerve roots are most likely involved in the cause of this patient’s symptoms? Image Credit: Radiopaedia Image Credit: wikiradiography ≣ Item 1 of 1 ◽" Mark Question ID: 0007 ⚪ A. Left L4 nerve root ⚪ B. Right L4 nerve root ⚪ C. Left L5 nerve root " D. Left S1 nerve root ⚪ E. Left S2 nerve root ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪ Bootcamp.com A 29-year-old male with no significant past medical history reports shooting, “electric-like” pain down the left buttock and lower extremity when sitting for the past two weeks. He also states that occasionally when he attempts to run for more than five minutes, the pains progressively worsen to the point where he is unable to walk. Pertinent findings on physical exam include 2+ reflexes at the patellar tendon bilaterally and right Achilles tendon. No reflex was obtained during testing of the left Achilles tendon. The patient is able to perform heel-walk, although he is unable to stand on the toes. There is also a loss of sensation to touch and vibration at the lateral malleolus. No pain is appreciated when palpating the lower back and there is no evidence of any “step off” signs. Lumbar radiography and MRI are shown. Which of the following nerve roots are most likely involved in the cause of this patient’s symptoms? Image Credit: Radiopaedia Image Credit: wikiradiography OUTLINE Neurology: Spinal Cord Syndromes 1. Spinal Cord Syndromes ● ● ● ● ● ● A. Anterior Cord Syndrome B. Posterior Cord Syndrome C. Central Cord Syndrome D. Brown-Sequard Syndrome E. Cauda Equina Syndrome F. Conus Medullaris Syndrome Neurology: Spinal Cord Syndromes https://commons.wikimedia.org/wiki/File:Spinal_cord_tracts_-_English.svg Bootcamp.com Neurology: Spinal Cord Syndromes Bootcamp.com https://commons.wikimedia.org/wiki/File:Cord_s.svg Spinal Cord Syndromes Syndrome Blood Supply Classic Causes Presentation Anterior Anterior Spinal Artery: Anterior 2/3 Artery of Adamkiewicz: Primary Blood Supply Below T8 in Spinal Cord Vertebral Burst Fracture Hypoperfusion Aortic Surgery Bilateral loss of pain and temperature Vibration and proprioception spared Muscle weakness Neurology: Spinal Cord Syndromes Bootcamp.com https://commons.wikimedia.org/wiki/File:Cord_s.svg Spinal Cord Syndromes Posterior Cord Syndrome Syndrome Blood Supply Classic Causes Presentation Anterior Anterior Spinal Artery: Anterior 2/3 Artery of Adamkiewicz: Primary Blood Supply Below T8 in Spinal Cord Vertebral burst fracture Hypoperfusion Aortic Surgery Bilateral loss of pain and temperature Vibration and proprioception spared Muscle weakness Posterior Spinal Arteries: Posterior 1/3 bilaterally Tabes Dorsalis SCD Friedreich Ataxia Loss of vibration and proprioception below Posterior Neurology: Spinal Cord Syndromes Bootcamp.com https://commons.wikimedia.org/wiki/File:Cord_s.svg Spinal Cord Syndromes Syndrome Important Anatomy Classic Causes Presentation Anterior Anterior Spinal Artery: Anterior 2/3 Artery of Adamkiewicz: Primary Blood Supply Below T8 in Spinal Cord Vertebral burst fracture Hypoperfusion Aortic Surgery Bilateral loss of pain and temperature Vibration and proprioception spared Muscle weakness Posterior Spinal Arteries: Posterior 1/3 bilaterally Tabes Dorsalis SCD Friedreich Ataxia Loss of vibration and proprioception below Spinothalamic and portions of anterior corticospinal tracts traversing anterior white commissure Syringomyelia Whiplash (hyperextension) Elderly patient Bilateral loss of pain and temperature Muscle weakness (arm>leg) Posterior Central Neurology: Spinal Cord Syndromes Bootcamp.com https://commons.wikimedia.org/wiki/File:Brown-Sequard.svg https://commons.wikimedia.org/wiki/File:Cord_s.svg Spinal Cord Syndromes Syndrome Important Anatomy Classic Causes Presentation Anterior Anterior Spinal Artery: Anterior 2/3 Artery of Adamkiewicz: Primary Blood Supply Below T8 in Spinal Cord Vertebral burst fracture Hypoperfusion Aortic Surgery Bilateral loss of pain and temperature Vibration and proprioception spared Muscle weakness Posterior Spinal Arteries: Posterior 1/3 bilaterally Tabes Dorsalis SCD Friedreich Ataxia Loss of vibration and proprioception below Central Spinothalamic and portions of anterior corticospinal tracts traversing anterior white commissure Syringomyelia Whiplash (hyperextension) Elderly patient Bilateral loss of pain and temperature Muscle weakness (arm>leg) Brown Sequard Spinothalamic tract travels superiorly 1-2 levels prior to decussation. Penetrating Injury (stab wound) Ipsilateral LMN at level Ipsilateral UMN below level Contralateral pain/temp loss 1-2 below Posterior Neurology: Spinal Cord Syndromes Bootcamp.com Distal Spinal Cord Injury Syndrome Conus Medullaris Cauda Equina Level Affected T12-L2 Caudal to L2 Distinguishing Features Acute onset sphincter incontinence Bilateral saddle anesthesia Tends to be less severe pain Mix of UMN and LMN features Gradual onset sphincter incontinence Unilateral saddle anesthesia Tends to be more severe pain Primarily LMN features ≣ Item 1 of 1 Question ID: 0008 ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com A 36-year-old male is rushed to the emergency room after being found unconscious outside for an undetermined length of time. His temperature is 96F, blood pressure 102/56, heart rate 106 beats per minute, and respiratory rate is 16 breaths per minute. He is saturating 95% on room air. The patient is found to have a bullet entry wound in the left flank proceeding medially with acute angulation in near proximity to the spinal cord. Which of the following features would be least consistent with this presentation? ⚪ A. Loss of all sensation to innervated structures ipsilateral at the level of the lesion ⚪ B. Left-sided hyperreflexia and muscle weakness below the level of the lesion ⚪ C. Left-sided loss of proprioception and vibration sense below the level of the lesion ⚪ D. Right-sided loss of temperature and pain sensation below the level of the lesion ⚪ E. Left-sided pupillary contraction and drooping of the eyelid ≣ Item 1 of 1 Question ID: 0008 ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com A 36-year-old male is rushed to the emergency room after being found unconscious outside for an undetermined length of time. His temperature is 96F, blood pressure 102/56, heart rate 106 beats per minute, and respiratory rate is 16 breaths per minute. He is saturating 95% on room air. The patient is found to have a bullet entry wound in the left flank proceeding medially with acute angulation in near proximity to the spinal cord. Which of the following features would be least consistent with this presentation? ⚪ A. Loss of all sensation to innervated structures ipsilateral at the level of the lesion ⚪ B. Left-sided hyperreflexia and muscle weakness below the level of the lesion ⚪ C. Left-sided loss of proprioception and vibration sense below the level of the lesion ⚪ D. Right-sided loss of temperature and pain sensation below the level of the lesion " E. Left-sided pupillary contraction and drooping of the eyelid https://commons.wikimedia.org/wiki/File:Brown-Sequard.svg OUTLINE Neurology: Invasive Spinal Cord Disease 1. Infectious ● ● ● ● ● A. Tetanospasmin Toxin B. Rabies Virus C. Poliomyelitis D. Varicella Zoster Virus E. Neurosyphilis 2. Other ● A. Spinal Muscular Atrophy Neurology: Invasive Spinal Cord Disease • Mechanism of Action • Tetanospasmin travels à Renshaw cells in spinal cord • Cleaves SNARE proteinsà ↓ inhibitory neurotransmitter • GABA, Glycine are primary inhibitory neurotransmitters • !-motor neurons unregulated • Clinical Signs and Symptoms • Spastic paralysis • Trismus (Lock jaw) • Risus Sardonicus • Opisthotonos • Foul smelling umbilical stump (neonates) Bootcamp.com https://en.wikipedia.org/wiki/Tetanus#/media/File:Neur otransmitter_vesicle_before_and_after_exposure_to_ Tetanus_Toxin.jpg https://en.wikipedia.org/wiki/Tetanus#/m edia/File:Opisthotonus_in_a_patient_suff ering_from_tetanus__Painting_by_Sir_Charles_Bell__1809.jpg Neurology: Invasive Spinal Cord Disease • Mechanism of Action • Rabies virus binds to nicotinic acetylcholine receptor • Retrograde migration (dynein) à Brainà Encephalitis • Long incubation period • Reservoir • Worldwide: Rabid dogs • U.S.: Bats (also skunks, raccoons, and other animals) • Clinical Signs and Symptoms • Nonspecific overall • Hydrophobia • Photophobia • Paralysis Bootcamp.com Neurology: Invasive Spinal Cord Disease Bootcamp.com • Classic Presentations of Paralytic Poliomyelitis • Unvaccinated child • Classically affects the proximal muscles • Severe muscle pain • Ascending asymmetric flaccid paralysis (LMN) • Remember your LMN Signs • Fasciculations • Hyporeflexia • Hypotonia • Muscle atrophy Image credit: https://en.wikipedia.org/wiki/Polio#/media/File:Polio_spinal_diagram-en.svg Neurology: Invasive Spinal Cord Disease Bootcamp.com • Varicella Zoster Virus • • • • Primary infection à chicken pox Remains dormant in dorsal root ganglia Reactivation à shingles Reactivation classically in immunocompromised patients • Classic Presentations of Shingles • • Painful erythematous rash à vesicular Dermatomal distribution, does NOT cross midline • Variants • • Herpes Ophthalmicus Herpes Oticus (Ramsay Hunt Syndrome) • Treatment • • Acyclovir, Valacyclovir Post-herpetic neuralgia major complication to untreated https://en.wikipedia.org https://en.wikipedia.org/wiki/Herpes_zoster_ophthalmicus https://en.wikipedia.org/wiki/Shingles#/media/File:Shingles.JPG /wiki/Trigeminal_nerve #/media/File:Trigeminal_herpes_with_uveitis_and_keratitis .jpg https://en.wikipedia.or g/wiki/Shingles#/medi a/File:Herpes_zoster_ chest.png Neurology: Invasive Spinal Cord Disease • Classic Presentations of Neurosyphilis • Immunocompromised patient or poor access to medical care • Possible new onset dementia at an early age • Tabes Dorsalis à broad-based ataxia, positive Romberg • Loss of proprioception • Areflexia • Argyll Robertson Pupil • Light-near dissociation • Classically associated with neurosyphilis https://commons.wikimedia.org/wiki/File:Argyll_Robertson_pupil_light_reflex_vs_accommodation_reflex.jpg Bootcamp.com Neurology: Invasive Spinal Cord Disease • Classic Presentation of Werdnig-Hoffman Disease (SMA Type I) • Onset between 0-6 months of age, death by 2 years of age • Symmetric flaccid paralysis • Cranial nerves classically spared (normal eye movements) • Lower motor neuron disease • General Information • Autosomal recessive mutation in SMN1 gene, chromosome 5 • Muscle biopsy: Atrophy of motor units https://commons.wikimedia.org/wiki/File:Polio_spinal_diagram-en.svg Bootcamp.com ≣ Item 1 of 1 Question ID: 0009 ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com A researcher is attempting to understand the pathogenesis of the Rabies virus. It is thought that the Rabies virus has interactions with p75 neurotrophin receptors (p75NTR) at peripheral neurons. This interaction has been postulated to allow the virus to enter the neuronal tissue and travel along the axon. It was found that the Rabies virus transport kinetics revealed a preference for transport in p75NTR-dependent compartments when compared to p75NTR-independent compartments. The researcher attempts to study the transport kinetics of the Rabies virus when adding a cell permeable molecular target, TAT-Pep50 in mice. Assuming TATPep50 administration demonstrated an overall decrease in mortality in mice infected with rabies virus, which of the following would best explain it’s mechanism of action? ⚪ A. Upregulation of dynein motor proteins along axonal microtubules in the central nervous system ⚪ B. Upregulation of dynein motor proteins along axonal microtubules in the peripheral nervous system ⚪ C. Upregulation of p75NTRs at peripheral nerves ⚪ D. Upregulation of acetylcholine receptors in peripheral nerves ⚪ E. Upregulation of ATPase inhibitors selective to dynein motor proteins at sites of high p75NTR expression ⚪ F. Upregulation of ATPase inhibitors selective to kinesin motor proteins at sites of high p75NTR expression ≣ Item 1 of 1 Question ID: 0009 ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com A researcher is attempting to understand the pathogenesis of the Rabies virus. It is thought that the Rabies virus has interactions with p75 neurotrophin receptors (p75NTR) at peripheral neurons. This interaction has been postulated to allow the virus to enter the neuronal tissue and travel along the axon. It was found that the Rabies virus transport kinetics revealed a preference for transport in p75NTR-dependent compartments when compared to p75NTR-independent compartments. The researcher attempts to study the transport kinetics of the Rabies virus when adding a cell permeable molecular target, TAT-Pep50 in mice. Assuming TATPep50 administration demonstrated an overall decrease in mortality in mice infected with rabies virus, which of the following would best explain it’s mechanism of action? ⚪ A. Upregulation of dynein motor proteins along axonal microtubules in the central nervous system ⚪ B. Upregulation of dynein motor proteins along axonal microtubules in the peripheral nervous system ⚪ C. Upregulation of p75NTRs at peripheral nerves ⚪ D. Upregulation of acetylcholine receptors in peripheral nerves $ E. Upregulation of ATPase inhibitors selective to dynein motor proteins at sites of high p75NTR expression ⚪ F. Upregulation of ATPase inhibitors selective to kinesin motor proteins at sites of high p75NTR expression OUTLINE Neurology: Demyelinating Disease 1. Demyelinating Disease ● ● ● ● ● ● ● A. Guillain-Barre Syndrome B. Multiple Sclerosis C. Progressive Multifocal Leukoencephalopathy D. Charcot Marie Tooth Disease E. Metachromatic Leukodystrophy F. Central Pontine Myelinolysis G. Subacute Sclerosing Panencephalitis 2. Lesions of Vision in Multiple Sclerosis ● ● ● A. Optic Neuritis B. Marcus Gunn Pupil C. Internuclear Ophthalmoplegia Neurology: Demyelinating Disease Neurology: Invasive Spinal Cord Disease • Classic Presentations of GBS • • • • Recent GI infection or URI Ascending symmetric flaccid paralysis (LMN) Campylobacter jejuni is the most important to remember overall Cytomegalovirus is the most common virus • Cerebrospinal Fluid Differential • • • Albuminocytological dissociation in both Poliomyelitis and GBS Pleocytosis more classic for Poliomyelitis GBS unlikely with pleocytosis • Management • • Plasmapheresis or intravenous immunoglobulins No corticosteroids Bootcamp.com Bootcamp.com Neurology: Demyelinating Disease Neurology: Invasive Spinal Cord Disease • Pathophysiology • Demyelination in CNS, oligodendrocyte axonal degeneration • Classic Presentation • • Young patient, classically Caucasian female Optic Neuritis à Painful, unilateral Bootcamp.com Bootcamp.com Neurology: Demyelinating Disease Neurology: Invasive Spinal Cord Disease • Pathophysiology • Demyelination in CNS, oligodendrocyte axonal degeneration • Classic Presentation • • • Young patient, classically Caucasian female Optic Neuritis à Painful, unilateral Marcus Gunn Pupil (relative afferent pupillary defect) Bootcamp.com Bootcamp.com Neurology: Demyelinating Disease Neurology: Invasive Spinal Cord Disease • Pathophysiology • Demyelination in CNS, oligodendrocyte axonal degeneration • Classic Presentation • • • • Young patient, classically Caucasian female Optic Neuritis à painful, unilateral Marcus Gunn Pupil (relative afferent pupillary defect) Unilateral/Bilateral Internuclear Ophthalmolpegia (lesion to MLF) Bootcamp.com Bootcamp.com Neurology: Demyelinating Disease Neurology: Invasive Spinal Cord Disease Bootcamp.com Bootcamp.com • Pathophysiology • Demyelination in CNS, oligodendrocyte axonal degeneration • Classic Presentation • • • • • • • • Young patient, classically Caucasian female Optic Neuritis à painful, unilateral Marcus Gunn Pupil (relative afferent pupillary defect) Bilateral Internuclear Ophthalmolpegia (lesion to MLF, heavily myelinated) Uhthoff phenomenon Bladder or bowel incontinence Lhermitte's sign Upper motor neuron signs Neurology: Demyelinating Disease Neurology: Invasive Spinal Cord Disease Bootcamp.com Bootcamp.com • Imaging: MRI • • Periventricular white matter lesions Dawson’s fingers • Lumbar Puncture • • Oligoclonal bands ↑ WBC, predominantly lymphocytes • Management • • • Acute setting consider high dose steroids Interferon-! Natalizumab à increased risk of progression to PML https://radiopaedia.org/cases /multiple-sclerosis-dawsonsfingers-3 Neurology: Demyelinating Disease Neurology: Invasive Spinal Cord Disease Bootcamp.com Bootcamp.com • Pathophysiology • • Reactivation of JC virus, typically in immunocompromised host Oligodendrocyte destruction à demyelination • Classic Presentations of PML • • Poorly controlled HIV history or recent treatment with natalizumab Unusual behavioral changes +/- focal neurologic deficits • Diagnostics • • Widespread non-enhancing white matter lesions JC Virus PCR in CSF https://en.wikipedia.org/wik i/Progressive_multifocal_le ukoencephalopathy https://radiopaedia.org/ar ticles/progressivemultifocalleukoencephalopathy?lan g=us Neurology: Demyelinating Disease Neurology: Invasive Spinal Cord Disease • Charcot-Marie-Tooth Disease • • • • Triad: Hammer toe, pes cavus, foot drop Distal, symmetric, sensory and motor neuropathy PNS Lower motor neuron signs • Metachromatic Leukodystrophy • • • • Autosomal recessive, deficiency of arylsulfatase A Build up of cerebroside sulfate leading to demyelination CNS and PNS Motor skill development regress in infants and young children • Central Pontine Myelinolysis • • Rapid sodium correction “Locked in” Syndrome (similar to pontine basilar infarction) • Subacute Sclerosing Panencephalitis • History of persistent measles infection Bootcamp.com Bootcamp.com ≣ Item 1 of 1 Question ID: 0010 ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com A 28-year-old fully vaccinated male with no significant past medical history presents to an urgent care clinic for abdominal cramping and watery ⚪ A. Apoptosis of ventral horn cells diarrhea. He is given a short course of antibiotics and his diarrhea ⚪ B. Molecular mimicry and destruction to Schwann cells resolves. Three weeks later he presents to the emergency room after a ⚪ C. Molecular mimicry and destruction to oligodendrocytes ⚪ D. Replication and reactivation of virus in dorsal root ganglia fall episode. He states he was attempting to walk on the treadmill at his ⚪ E. Inhibition of glycine release via SNARE proteins local fitness center when he lost his balance and fell backward. He states that over the past week he has had difficulty climbing the stairs and thought it was because he was sleeping awkwardly on his legs. Muscle strength testing is 3/5 bilaterally at the lower extremities and reflexes are absent at S1 bilaterally. A lumbar puncture is performed with findings shown below. Which of the following is most consistent with the pathologic mechanism likely causing this patient’s current presentation? Opening Pressure: 10cm H2O Appearance: Clear White Blood Cells: 3 cell/uL (reference range: 0-5 cells/uL) Protein: 722 mg/L (reference range: <40 mg/dL) Glucose: 55 mg/dL (reference range: 40-70 mg/dL) Gram Stain: Negative No oligoclonal bands are present ≣ Item 1 of 1 Question ID: 0010 ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com A 28-year-old fully vaccinated male with no significant past medical history presents to an urgent care clinic for abdominal cramping and watery ⚪ A. Apoptosis of ventral horn cells $ B. Molecular mimicry and destruction to Schwann cells diarrhea. He is given a short course of antibiotics and his diarrhea resolves. Three weeks later he presents to the emergency room after a ⚪ C. Molecular mimicry and destruction to oligodendrocytes ⚪ D. Replication and reactivation of virus in dorsal root ganglia fall episode. He states he was attempting to walk on the treadmill at his ⚪ E. Inhibition of glycine release via SNARE proteins local fitness center when he lost his balance and fell backward. He states that over the past week he has had difficulty climbing the stairs and thought it was because he was sleeping awkwardly on his legs. Muscle strength testing is 3/5 bilaterally at the lower extremities and reflexes are absent at S1 bilaterally. A lumbar puncture is performed with findings shown below. Which of the following is most consistent with the pathologic mechanism likely causing this patient’s current presentation? Opening Pressure: 10cm H2O Appearance: Clear White Blood Cells: 3 cell/uL (reference range: 0-5 cells/uL) Protein: 722 mg/L (reference range: <40 mg/dL) Glucose: 55 mg/dL (reference range: 40-70 mg/dL) Gram Stain: Negative No oligoclonal bands are present OUTLINE Neurology: Conduction Physiology 1. Conduction Physiology Concepts ● ● ● ● A. Extracellular Electrolyte Dynamics B. Sodium-Potassium-ATPase C. Resting Potential D. Electrolyte Equilibrium Potential 2. Action Potential ● ● ● ● A. Stages of the Action Potential B. Pathology Affecting Current in the Action Potential C. Saltatory Conduction D. Length and Time Constant Neurology: Conduction Physiology Neurology: Invasive Spinal Cord Disease • Electrolyte Physiologic Extracellular Concentrations: • Sodium (primarily extracellular) ~140 mmol/L • Potassium (primarily intracellular) : ~5 mmol/L • Chloride (primarily extracellular) ~105 mmol/L • Extracellular pH = 7.4 • Negatively charged proteins (primarily intracellular) Bootcamp.com Bootcamp.com Neurology: Conduction Physiology Neurology: Invasive Spinal Cord Disease • • Bootcamp.com Bootcamp.com Resting Potential: membrane potential of a neuron (or muscle cell) at rest • Sum of all extracellular and intracellular ions • Ion semi-permeability: Potassium easy transfer, Sodium difficult transfer • Na+/K+ ATPase: Active transport pump. Hydrolyze 1 ATP, 2 K+ enter cell, 3 Na+ leave cell Equilibrium Potential: membrane potential of one ion • Potassium negative • Chloride negative • Sodium positive Neurology: Conduction Physiology Neurology: Invasive Spinal Cord Disease • Action Potential: Voltage-gated induction of a neuronal impulse • Stage 1: Resting Potential ~ -70-90mV • Stage 2: Action Potential formed if threshold potential is reached • Stage 3: Depolarization driven by sodium ion influx • Stage 4: Repolarization driven by potassium ion efflux • Stage 5: Afterhyperpolarization https://commons.wikimedia.org/wiki/File:Acti on_potential.svg https://commons.wikimedia.org/wiki/File :SynapseSchematic_en.svg Bootcamp.com Bootcamp.com Neurology: Conduction Physiology Neurology: Invasive Spinal Cord Disease • • Bootcamp.com Bootcamp.com Inhibitors of Sodium Channels: • Ciguatoxin à extended depolarization • Tetrodotoxin à inhibited depolarization • Lidocaine à inhibited depolarization Activators of Chloride Channels: • GABA and Glycine • Benzodiazepines à ↑ frequency of Cl- channel opening • Barbiturates à ↑ duration of Cl- channel opening https://commons.wikimedia.org/wiki/File:Acti on_potential.svg Neurology: Conduction Physiology Neurology: Invasive Spinal Cord Disease • • • • • • • • • Conduction Velocity: Speed of travel of axonal signal Continuous Conduction: Unmyelinated nerves • Action potential travels throughout cell membrane Saltatory Conduction: Myelinated nerves • Nodes of Ranvier • Faster conduction velocity than similar unmyelinated nerves • Longer length constant than similar unmyelinated nerves • Shorter time constant than similar unmyelinated nerves Nerve Fiber Diameter: Proportional to conduction velocity Axial Resistance: Inversely proportional to conduction velocity Membrane Resistance: Proportional to conduction velocity Membrane Capacitance: Inversely proportional to conduction velocity Length (Space) Constant: Length of travel of axonal signal before decay Time Constant: Responsiveness of membrane potential to membrane permeability Bootcamp.com Bootcamp.com ≣ Item 1 of 1 ◽" Mark Question ID: 0011 Equilibrium Potential ECl -75 mV EK -90 mV ENa +60 mV ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪✪✪ Bootcamp.com A 44-year-old male with a history of major depressive disorder and generalized anxiety disorder presents to the emergency department in a lethargic state after his roommate reportedly called paramedics. His respiratory rate is approximately 8 breaths per minute and his oxygen saturation is 86% on room air. His roommate states that the patient took the entire bottle of his prescribed ”anxiety medicine”. Oxygen by nasal cannula and flumazenil are administered. The patient subsequently becomes more alert, and his respiratory depression improves. Equilibrium potentials at physiologic conditions are given as a reference. Which of the following best describes the changes in neuronal conduction occurring after administration of flumazenil? ⚪ A. Increase in frequency of chloride channel opening ⚪ B. Increase in duration of chloride channel opening ⚪ C. Neuronal potentials will more closely approach chloride equilibrium potentials ⚪ D. Neuronal potentials will more closely approach potassium equilibrium potentials ⚪ E. Neuronal potentials will more closely approach sodium equilibrium potentials ≣ Item 1 of 1 ◽" Mark Question ID: 0011 Equilibrium Potential ECl -75 mV EK -90 mV ENa +60 mV ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪✪✪ Bootcamp.com A 44-year-old male with a history of major depressive disorder and generalized anxiety disorder presents to the emergency department in a lethargic state after his roommate reportedly called paramedics. His respiratory rate is approximately 8 breaths per minute and his oxygen saturation is 86% on room air. His roommate states that the patient took the entire bottle of his prescribed ”anxiety medicine”. Oxygen by nasal cannula and flumazenil are administered. The patient subsequently becomes more alert, and his respiratory depression improves. Equilibrium potentials at physiologic conditions are given as a reference. Which of the following best describes the changes in neuronal conduction occurring after administration of flumazenil? ⚪ A. Increase in frequency of chloride channel opening ⚪ B. Increase in duration of chloride channel opening ⚪ C. Neuronal potentials will more closely approach chloride equilibrium potentials ⚪ D. Neuronal potentials will more closely approach potassium equilibrium potentials $ E. Neuronal potentials will more closely approach sodium equilibrium potentials OUTLINE Neurology: Neuromuscular Junction 1. Physiology of the Neuromuscular Junction ● ● ● A. Action Potential B. Synaptic Transmission C. Acetylcholinesterase 2. Medications Relevant to the Neuromuscular Junction ● ● ● A. Antiepileptics B. Organophosphates C. Acetylcholinesterase Inhibitors 3. Diseases Relevant to the Neuromuscular Junction ● ● ● A. Myasthenia Gravis B. Lambert-Eaton Syndrome C. Botulinum Toxin 4. Neuromuscular Blocking Agents ● ● A. Nondepolarizing B. Depolarizing Neurology: Diseases the Neuromuscular Neurology: InvasiveofSpinal Cord Disease Junction • • • • • • Bootcamp.com Bootcamp.com Action Potential Reaches Pre-Synaptic Motor End-Plate Pre-Synaptic Calcium Channel Opens Fusion of ACh Quanta with Neuronal Cell Membrane via SNARE Proteins (calcium required) ACh Quanta Released ACh Generates Endplate Potentials on Post-Synaptic Membrane • Ligated-gated sodium channels • ↑ endplate potential à if threshold potential is reached à action potential generation • Acetylcholinesterase destroys ACh in synaptic cleft Action Potential Triggered Through Sarcolemma • Voltage-gated sodium channels Neurology: Diseases the Neuromuscular Neurology: InvasiveofSpinal Cord Disease Junction • • • Bootcamp.com Bootcamp.com Antiepileptics: • Phenytoin: Inhibition of voltage gated sodium channels • Carbamazepine: Inhibition of voltage gated sodium channels • Gabapentin: Inhibition of presynaptic voltage gated calcium channels • Levetiracetam: Disrupts vesicle fusion Organophosphates: • Pesticides, Sarin gas: Nonspecific, irreversible inactivation of acetylcholinesterase Acetylcholinesterase Inhibitors: • Edrophonium, Physostigmine, Pyridostigmine: Inhibits acetylcholinesterase Neurology: Diseases the Neuromuscular Neurology: InvasiveofSpinal Cord Disease Junction • • • • • • • • Bootcamp.com Bootcamp.com Pathophysiology: Anti-acetylcholine receptor antibodies (most classic) • Binds to post-synaptic nicotinic acetylcholine receptors à inhibition of muscle activation Presentation: Fatigable muscle weakness, worse with activity, improves with rest • Extraocular à Ptosis, diplopia • Bulbar à Dysphagia, dysarthria • Respiratory à Dyspnea • Limb weakness à proximal muscles • Reflexes tend to be normal Diagnostics: AChR Antibodies, Chest CT, EMG Other: Ice pack test, Edrophonium test Associated Pathology: Thymoma Associated Diseases: Hashimoto thyroiditis, SLE, RA Management: Thymectomy, Pyridostigmine, Glucocorticoids https://commons.wikime dia.org/wiki/File:Anterior Myasthenic Crisis: Trigger à severe exacerbation à respiratory failure, Rx: IVIG, _mediastinal_mass_thy plasmapheresis moma_diagram.jpg Neurology: Diseases the Neuromuscular Neurology: InvasiveofSpinal Cord Disease Junction • • • • • • Pathophysiology: Anti-voltage-gated calcium channels antibodies (most classic) • Binds to pre-synaptic voltage-gated calcium channels à ↓ acetylcholine release Presentation: Improving muscle weakness with activity • Limb weakness à proximal muscles • Autonomic symptoms à constipation, dry oral mucosa, orthostatic hypotension • Reflexes tend to be reduced or absent Diagnostics: Anti-VGCC Antibodies, Chest CT, EMG Associated Pathology: Small cell lung cancer Associated Diseases: Hashimoto thyroiditis, SLE, RA Management: Amifampridine Bootcamp.com Bootcamp.com Neurology: Diseases the Neuromuscular Neurology: InvasiveofSpinal Cord Disease Junction • • • • • • Bootcamp.com Bootcamp.com Pathophysiology: Cleaves SNARE proteins (most classic) • Prevents fusion of neurotransmitter at pre-synaptic cleft à ↓ acetylcholine release • Pathogen: Clostridium botulinum, gram + rod, obligate anaerobe, spore forming • Botulinum toxin produced by Clostridium botulinum Presentation: Descending flaccid paralysis • Ocular à Dilated pupil, diplopia • Bulbar à Dysphagia, dysarthria, facial muscle weakness • Autonomic symptoms à dry oral mucosa • Respiratory à Dyspnea Foodborne: Preformed toxin in food, classically canned foods, raw honey and juice (infants) Infant Botulism: Floppy baby syndrome (also other causes) Wound Botulism: Preformed toxin into wound, long incubation period, classic IVDU Management: Always airway first à Immune globulin (equine vs human) Neurology: Diseases the Neuromuscular Neurology: InvasiveofSpinal Cord Disease Junction • • Bootcamp.com Bootcamp.com Nondepolarizing: Competitive antagonists of post-synaptic nicotinic acetylcholine receptors • Vecuronium, Rocuronium Depolarizing: Competitive agonist of post-synaptic nicotinic acetylcholine receptors • Succinylcholine Neurology: Diseases the Neuromuscular Neurology: InvasiveofSpinal Cord Disease Junction Bootcamp.com Bootcamp.com Neuromuscular Junction Pathology Disease Process Pathophysiology Hallmark Findings Reflexes Association Myasthenia Gravis Anti-AChR Abs (usually) (postsynaptic) Fatigable muscle weakness Normal Thymoma Lambert-Eaton Syndrome Anti-VGCC Abs (pre-synaptic) Improving muscle weakness with activity Decreased/absent Small cell lung cancer Botulism Protease cleaving SNARE preventing ACh release (presynaptic) Descending flaccid paralysis Variable Canned foods and honey (infants) Guillian-Barre Syndrome Molecular mimicry to PNS Ascending symmetric flaccid paralysis Decreased/absent Previous illness ≣ Item 1 of 1 Question ID: 0012 ◽" Mark ⚪ A. Significantly lower than standard dosing is optimal ⚪ B. Slightly lower than standard dosing is optimal ⚪ C. Standard dosing is optimal ⚪ D. Slightly greater than standard dosing is optimal ⚪ E. Significantly greater than standard dosing is optimal ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪✪ Bootcamp.com A 37-year-old-male with a past medical history of asthma comes into the emergency room stating that he is having trouble breathing. He states that he went for a walk outside and became very weak and short of breath. He also states that he over the past year he has noticed worsening double vision toward the end of the day, but it seems to resolve after sleeping. He also reports difficulty chewing meats, dysphagia, and has since decided to become a vegetarian. An image of his eyes is depicted below. Prior to any breathing treatment, the patient’s respiratory distress acutely worsens. Succinylcholine is given for muscle relaxation in addition to general anesthesia to facilitate endotracheal intubation. Which of the following will most likely be true regarding the optimal dose of succinylcholine for this patient? https://commons.wikimedia.org/wiki/File:Congenitalptosis.JPG ≣ Item 1 of 1 Question ID: 0012 ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪✪ Bootcamp.com A 37-year-old-male with a past medical history of asthma comes into the emergency room stating that he is having trouble breathing. He states that ⚪ A. Significantly lower than standard dosing is optimal he went for a walk outside and became very weak and short of breath. He ⚪ B. Slightly lower than standard dosing is optimal also states that he over the past year he has noticed worsening double ⚪ C. Standard dosing is optimal vision toward the end of the day, but it seems to resolve after sleeping. He ⚪ D. Slightly greater than standard dosing is optimal $ E. Significantly greater than standard dosing is optimal also reports difficulty chewing meats, dysphagia, and has since decided to become a vegetarian. An image of his eyes is depicted below. Prior to any breathing treatment, the patient’s respiratory distress acutely worsens. Succinylcholine is given for muscle relaxation in addition to general anesthesia to facilitate endotracheal intubation. Which of the following will most likely be true regarding the optimal dose of succinylcholine for this patient? https://commons.wikimedia.org/wiki/File:Congenitalptosis.JPG OUTLINE Neurology: Cranial Nerves I-VI 1. Cranial Nerves ● ● ● ● ● ● A. Olfactory Nerve B. Optic Nerve C. Oculomotor Nerve D. Trochlear Nerve E. Trigeminal Nerve F. Abducens Nerve 2. High Yield Considerations ● ● A. Compression vs Ischemic Lesions of Oculomotor Nerve B. Cavernous Sinus Neurology: Cranial Nerves I-VI • Cranial Nerve I (Olfactory Nerve) • • • Not located in brainstem No thalamic relay Sensory nerve • Etiology of Lesions • • Ethmoid bone fracture (cribriform plate) Meningioma • Presentation • Anosmia Bootcamp.com Neurology: Cranial Nerves I-VI Bootcamp.com • Cranial Nerve II (Optic Nerve) • • • • Not located in brainstem Sensory nerve responsible for vision Afferent limb of the pupillary light reflex Travels through optic canal • Etiology of Lesions • • • Multiple sclerosis Microvascular disease Ethambutol • Presentation • • • • Optic neuritis à loss of vision with painful eye movements Marcus Gunn pupil à swinging flashlight test Loss of ipsilateral and consensual light reflex when affected nerve is tested Anopsia Neurology: Cranial Nerves I-VI Bootcamp.com • Cranial Nerve III (Oculomotor Nerve) • • • • • Nucleus in midline midbrain Motor sensation to superior, inferior, and medial rectus, inferior oblique, and levator palpebrae superioris Efferent limb of light reflex Parasympathetic fibers to pupillary sphincter and ciliary muscles Travels through the superior orbital fissure • Etiology of Lesions • • • • Posterior communicating artery aneurysm Multiple sclerosis (specifically affecting the MLF, CN III downstream) Uncal herniation Microvascular disease • Presentation • • • • • Ptosis, pupillary dilation +/- anhidrosis if Horner Syndrome Internuclear ophthalmoplegia Loss of ipsilateral light reflex when affected nerve is tested Loss of consensual light reflex when unaffected nerve is tested ”Down and Out” Gaze; Impaired adduction; Diagonal diplopia Neurology: Cranial Nerves I-VI • Oculomotor Nerve Anatomical Considerations • Parasympathetic fibers running superficial to motor fibers • Ischemic and/or Demyelinating Lesions • • • • Motor >= Parasympathetic dysfunction Microvascular disease (diabetes) Ocular vasculitis Demyelinating injury (to MLF for example) • Compressive Lesions • • • Motor < Parasympathetic dysfunction Posterior communicating artery aneurysm Uncal herniation Bootcamp.com Neurology: Cranial Nerves I-VI • Cranial Nerve IV (Trochlear Nerve) • • • Nucleus midline midbrain Motor sensation to superior oblique muscle Travels through superior orbital fissure • Etiology • Microvascular disease • Presentation • • • • Inability to depress and adduct the eye Worsened when looking down away from the affected side Head tilt to the opposite side Vertical and torsional diplopia Bootcamp.com Neurology: Cranial Nerves I-VI • Cranial Nerve V (Trigeminal Nerve) • • • • • • • • • • Nucleus lateral pons Sensory to face: Three divisions (V1, V2, V3) Sensory to anterior 2/3 of the tongue (V3) Motor sensation to muscles of mastication Afferent and efferent limb of jaw jerk reflex (V3) Afferent corneal and lacrimation reflexes (V1) Cranial nerve V1 travels through superior orbital fissure Cranial nerve V2 travels through foramen rotundum and inferior orbital fissure Cranial nerve V3 travels through foramen ovale Etiology • • • • • Bootcamp.com Foraminal Lesions Trigeminal Neuralgia Temporomandibular Joint (TMJ) Dysfunction Herpes Zoster Ophthalamicus Presentation • • • Lesion to V1 à Sensation in V1, loss of corneal and lacrimation reflexes Lesion to V2à Sensation in V2 Lesion to V3à Sensation in V3, anterior 2/3 of the tongue, contralateral paralysis in muscles of mastication (Jaw deviates ipsilateral to lesion) https://commons.wikimedia.org/wiki/File:Trig_innervation.svg Neurology: Cranial Nerves I-VI Bootcamp.com • Cranial Nerve VI (Abducens Nerve) • • Nucleus midline pons Motor sensation to lateral rectus muscle • Etiology • Elevations in intra-cranial pressure (herniation, hemorrhage, hematoma, pseudo-tumor cerebri) • Presentation • • Inability to perform abduction of affected eye Horizontal diplopia Neurology: Cranial Nerves I-VI Bootcamp.com • Etiology • • Infectious cause à retrograde through valveless venous system Hypercoagulable states • Presentation • • • • • • Signs of increased intracranial pressure (bilateral papilledema, headaches) Fever Painful eye movements Degree of paralysis with eye movements Loss of facial sensation Absent corneal reflex (afferent limb) https://upload.wikimedia.org/wikipedia/commons/b/bf/Gray571.png https://commons.wikimedia.org/wiki/File:Papilledema.jpg ≣ Item 1 of 1 Question ID: 0013 ◽" Mark A B C D E https://commons.wikimedia.org/wiki/File:Skull_foramina_labeled.svg ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪✪ Bootcamp.com A 76-year-old male current everyday smoker is being evaluated in by his primary care physician for an “enlarging pimple” on his nose that he first noticed 3 days ago. He states that prior to noticing the lesion, he had been experiencing severe stinging pain on the skin. He states that the pain has been localized to the left side of the tip of the nose. He recently started a short course of steroids for an exacerbation of his underlying chronic bronchitis and emphysema. He denies any shortness of breath today. On physical exam, the lesion appears to be moderately tender to touch and vesicular in nature. Small blisters are formed centrally in the lesion draining minor quantities of serous exudate. Valacyclovir is initiated and the patient is instructed to return immediately if the rash is worsening or if he experiences any fever or vision changes. Which of the following is most likely traversed by the primary nerve involved in this patient’s presentation? ⚪ A. ⚪ B. ⚪ C. ⚪ D. ⚪ E. ≣ Item 1 of 1 Question ID: 0013 ◽" Mark A B C D E https://commons.wikimedia.org/wiki/File:Skull_foramina_labeled.svg ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪✪ Bootcamp.com A 76-year-old male current everyday smoker is being evaluated in by his primary care physician for an “enlarging pimple” on his nose that he first noticed 3 days ago. He states that prior to noticing the lesion, he had been experiencing severe stinging pain on the skin. He states that the pain has been localized to the left side of the tip of the nose. He recently started a short course of steroids for an exacerbation of his underlying chronic bronchitis and emphysema. He denies any shortness of breath today. On physical exam, the lesion appears to be moderately tender to touch and vesicular in nature. Small blisters are formed centrally in the lesion draining minor quantities of serous exudate. Valacyclovir is initiated and the patient is instructed to return immediately if the rash is worsening or if he experiences any fever or vision changes. Which of the following is most likely traversed by the primary nerve involved in this patient’s presentation? ⚪ A. $ B. ⚪ C. ⚪ D. ⚪ E. OUTLINE Neurology: Cranial Nerves VII-XII 1. Cranial Nerves ● ● ● ● ● ● A. Facial Nerve B. Vestibulocochlear Nerve C. Glossopharyngeal Nerve D. Vagus Nerve E. Spinal Accessory Nerve F. Hypoglossal Nerve 2. High Yield Considerations ● A. Facial Nerve Anatomy Neurology: Cranial Nerves VII-XII Bootcamp.com • Cranial Nerve VII (Facial Nerve) • • • • • • Nucleus in lateral pons Taste anterior 2/3 of tongue (chorda tympani branch) Motor to facial muscles Efferent limb of corneal and lacrimation reflex Parasympathetic control over lacrimation and salivation Afferent somatic fibers from the pinna and external auditory canal • Etiology of Lesions • • • Parotid gland mass (sialadenitis, pleomorphic adenoma, mucoepidermoid carcinoma) Bell’s Palsy (Idiopathic Facial Nerve Palsy) Temporal bone trauma • Presentation • • • • • • Loss of taste sensation over anterior 2/3 of tongue Impaired eye closure, drooping of face, impaired ability to smile Loss of corneal reflex (efferent) Disappearance of nasolabial fold Impaired lacrimation https://commons.wikimedia.org/wiki/File:Parotid_gland_en.png Hyperacusis (stapedius) Neurology: Cranial Nerves VII-XII Bootcamp.com • Central Lesion (ex. CVA) • • Upper Facial Muscles: Dual innervation, remain intact Lower Facial Muscles: Dysfunction contralateral to the lesion • Peripheral Lesion (ex. Bell’s Palsy) • • Upper Facial Muscles: Dysfunction ipsilateral to the lesion Lower Facial Muscles: Dysfunction ipsilateral to the lesion https://commons.wikimedia.org/wiki/File:Cranial_nerve_VII.svg Neurology: Cranial Nerves VII-XII Bootcamp.com • Cranial Nerve VIII (Vestibulocochlear Nerve) • • Nucleus in lateral pons and medulla Sensory modalities in balance, auditory, and equilibrium • Etiology of Lesions • • • Bilateral Acoustic Neuromas: Neurofibromatosis Type 2 Basilar Skull Fracture Temporal bone trauma • Presentation • • • • • Sensorineural hearing loss Vertigo Balance Impairment Horizontal Nystagmus Basilar Skull Fracture à ”Raccoon eyes” (periorbital ecchymoses) https://commons.wikimedia.org/wiki/File:Bilateral_periorbital_ecchymosis_(raccoon_eyes).jpg https://www.researchgate.net/figure/Vestibular-schwannomas-Axial-A-and-coronal-B-enhancedT1-weighted-MR-images_fig1_38012259 Neurology: Cranial Nerves VII-XII Bootcamp.com • Cranial Nerve IX (Glossopharyngeal Nerve) • • • • • • • Nucleus in lateral medulla Sensory innervation and taste to posterior 1/3 of tongue Sensory innervation to eustachian tube, upper pharynx, and inner surface of tympanic membrane Motor to pharyngeal muscles à swallowing (Stylopharyngeus) Afferent limb of gag reflex Baroreceptors and Chemoreceptors Parasympathetics for salivation (otic ganglion à auriculotemporal n.à parotid gland ) • Etiology of Lesions • Iatrogenic • Presentation • • • • Loss of gag reflex Dysphagia Loss of taste sensation in posterior 1/3 of tongue Sensory loss in upper pharynx, posterior tongue, middle ear cavity Neurology: Cranial Nerves VII-XII Bootcamp.com • Cranial Nerve X (Vagus Nerve) • • • • • • Nucleus in lateral medulla Sensory innervation distal to posterior tongue Motor to pharyngeal muscles à swallowing and speech Efferent limb of gag reflex Baroreceptors and Chemoreceptors Parasympathetics for visceral organ and vessel function • Etiology of Lesions • Recurrent Laryngeal Nerve à Thyroid tumor, apical lung tumor • Presentation • • • Hoarseness, dysphagia, dysphonia Uvula deviated away from the side of the lesion Impaired gag reflex https://commons.wikimedia.org/wiki/File:Recurrent_laryngeal_nerve.svg Neurology: Cranial Nerves VII-XII Bootcamp.com • Cranial Nerve XI (Spinal Accessory Nerve) • • Nucleus in lateral medulla Motor to SCM and trapezius muscles • Etiology of Lesions • Iatrogenicà Cervical lymph node dissection • Presentation • • Weakness with head turning to the contralateral side Ipsilateral shoulder drooping https://commons.wikimedia.org/wiki/File:Gray793.png Neurology: Cranial Nerves VII-XII Bootcamp.com • Cranial Nerve XII (Hypoglossal Nerve) • • Nucleus in midline medulla Motor to intrinsic and extrinsic tongue muscles except palatoglossus • Etiology of Lesions • • Internal carotid artery dissection Iatrogenic • Presentation • • Supranuclear injury à tongue deviation away from side of lesion, UMN signs Hypoglossal nerve injury à tongue deviation toward side of lesion, LMN signs ≣ Item 1 of 1 Question ID: 0014 ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com A 54-year-old female with a history of medullary carcinoma of the thyroid presents to her local urgent care clinic with complaints of difficulty speaking. She states that she is employed as a marketing manager and is having difficulty completing presentations. Her voice seems to “disappear” after thirty minutes of talking. She reports she has been consuming more water than usual to try to “clear her throat”. She denies any globus sensation, cough, or recent infection. On physical exam the lungs are clear to auscultation bilaterally and the heart has a regular rate and rhythm. The uvula and tongue are noted to be midline with no asymmetry in soft palate elevation. No focal neurologic deficits are noted in the extremities, and she has appropriate muscle strength with shoulder shrugging. She reports recently undergoing a total thyroidectomy and neck dissection prior to her first noticing these symptoms. Which of the following lesions are most consistent with this patient’s presentation? ⚪ A. Metastatic spread of primary tumor to the hypoglossal canal ⚪ B. Metastatic spread of primary tumor to the jugular foramen ⚪ C. Iatrogenic injury in proximity to distal inferior thyroid artery ⚪ D. Iatrogenic hypoperfusion injury at the dorsal motor nucleus ⚪ E. Metastatic spread of primary tumor to the foramen magnum ≣ Item 1 of 1 Question ID: 0014 ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com A 54-year-old female with a history of medullary carcinoma of the thyroid presents to her local urgent care clinic with complaints of difficulty speaking. She states that she is employed as a marketing manager and is having difficulty completing presentations. Her voice seems to “disappear” after thirty minutes of talking. She reports she has been consuming more water than usual to try to “clear her throat”. She denies any globus sensation, cough, or recent infection. On physical exam the lungs are clear to auscultation bilaterally and the heart has a regular rate and rhythm. The uvula and tongue are noted to be midline with no asymmetry in soft palate elevation. No focal neurologic deficits are noted in the extremities, and she has appropriate muscle strength with shoulder shrugging. She reports recently undergoing a total thyroidectomy and neck dissection prior to her first noticing these symptoms. Which of the following lesions are most consistent with this patient’s presentation? ⚪ A. Metastatic spread of primary tumor to the hypoglossal canal ⚪ B. Metastatic spread of primary tumor to the jugular foramen $ C. Iatrogenic injury in proximity to distal inferior thyroid artery ⚪ D. Iatrogenic hypoperfusion injury at the dorsal motor nucleus ⚪ E. Metastatic spread of primary tumor to the foramen magnum OUTLINE Neurology: Vision 1. Visual Pathway ● ● ● ● ● ● A. Retina and Optic Nerve B. Optic Chiasm C. Peri-chiasm D. Lateral Geniculate Nucleus E. Optic Radiations F. Primary Visual Cortex 2. Pupillary Light Reflex ● ● A. Afferent Pupillary Defect B. Efferent Pupillary Defect Neurology: Vision Bootcamp.com • Visual Pathway: • Retina à optic n. à optic chiasm à optic tract à LGN à optic radiations à visual cortex • Pupillary Light Reflex Pathway: • Retina à optic n. à optic chiasm à optic tract à pretectal area à EWP nucleus à CN III • Terminology: • • Temporal visual field à projects onto nasal retina Nasal visual field à projects onto temporal retina • Classifying Lesions: • • • • • Anopia Hemianopia Quadrantanopia Homonymous Nasal/Temporal Neurology: Vision Bootcamp.com • Structures Involved: Retina, optic nerve • Visual field and retinal fibers are inversely related • General Presentation: • • • Ipsilateral scotoma (partial) Ipsilateral anopia (complete) Loss of afferent limb of pupillary light reflex • Etiology of Lesions: • • • • • • • • Macular degeneration Central retinal artery occlusion Central retinal vein occlusion Optic neuritis (multiple sclerosis) Ethambutol Optic atrophy Diabetic retinopathy https://en.wikipedia.org/wiki/Fundus_(eye Retinitis pigmentosa )#/media/File:Fundus_photograph_of_nor mal_right_eye.jpg https://commons.wikimedia.org/wiki/File:Cherry_red_spot_in_pati ent_with_central_retinal_artery_occlusion_(CRAO).jpg Neurology: Vision • Structures Involved: Optic Chiasm • Contains temporal visual field / nasal retinal fibers • General Presentation: • Bitemporal heteronymous hemianopia • Etiology of Lesions: • • • Pituitary lesion (prolactinoma) Craniopharyngioma Anterior communicating artery aneurysm Bootcamp.com Neurology: Vision • Structures Involved: Peri-chiasm • Contains nasal visual field / temporal retinal fibers • General Presentation: • Ipsilateral nasal hemianopia • Etiology of Lesions: • • Internal carotid artery aneurysms Internal carotid artery calcification Bootcamp.com Neurology: Vision Bootcamp.com • Structures Involved: Optic tract, lateral geniculate nucleus • Contains ipsilateral nasal visual field fibers and contralateral temporal visual field fibers • General Presentation: • Contralateral homonymous hemianopia • Etiology of Lesions: • Middle cerebral artery infarction Neurology: Vision Bootcamp.com • Structures Involved: Optic radiations • • Meyer’s Loop (Temporal lobe): Inferior bundle containing ipsilateral superior nasal visual field fibers and contralateral superior temporal visual field fibers Superior Loop (Parietal lobe): Superior bundle containing ipsilateral inferior nasal visual field fibers and contralateral inferior temporal visual field fibers • General Presentation: • • Meyer’s Loop: Contralateral superior homonymous quadrantanopia Superior Loop: Contralateral inferior homonymous quadrantanopia • Etiology of Lesions: • • Middle cerebral artery infarction Lesion to posterior limb of internal capsule Neurology: Vision Bootcamp.com • Structures Involved: Visual Cortex • • Contains projections of ipsilateral nasal and contralateral temporal visual field fibers Occipital Lobe • General Presentation: • Contralateral homonymous hemianopia with macular sparing • Etiology of Lesions: • Posterior cerebral artery infarction ≣ Item 1 of 1 Question ID: 0015 ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪✪ Bootcamp.com A 67-year-old male with a past medical history of type 2 diabetes mellitus presents to the emergency department for color blindness that “comes and goes”. He states that everything appears to have a transient blue-like discoloration. He denies any loss of vision but reports after staring at certain objects his vision tends to become increasingly blurry. His vital signs are notable for a blood pressure of 92/58. He states that his blood pressure was borderline high about one year ago but has since been improved since he started taking sildenafil for his erectile dysfunction. His visual acuity is normal and there are no deficits in the visual fields. The risks and benefits to sildenafil use are discussed with the patient and he is subsequently discharged. One week later he returns to the emergency in a panic with complete loss of vision in the right eye. His extraocular movements are intact with no other apparent focal neurologic deficits. Which of the following findings would most likely be consistent with this patient’s presentation? ⚪ A. Significant miosis bilaterally prior to pupillary light reflex testing ⚪ B. Failure to obtain a direct and consensual response when light is shone in the left eye ⚪ C. Failure to obtain a direct response when light is shone in the left eye; consensual response without deficits ⚪ D. Failure to obtain a direct response when light is shone in the right eye; consensual response without deficits ⚪ E. Appropriately normal direct and consensual response when light is shone in the left eye ≣ Item 1 of 1 Question ID: 0015 ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪✪ Bootcamp.com A 67-year-old male with a past medical history of type 2 diabetes mellitus presents to the emergency department for color blindness that “comes and goes”. He states that everything appears to have a transient blue-like discoloration. He denies any loss of vision but reports after staring at certain objects his vision tends to become increasingly blurry. His vital signs are notable for a blood pressure of 92/58. He states that his blood pressure was borderline high about one year ago but has since been improved since he started taking sildenafil for his erectile dysfunction. His visual acuity is normal and there are no deficits in the visual fields. The risks and benefits to sildenafil use are discussed with the patient and he is subsequently discharged. One week later he returns to the emergency in a panic with complete loss of vision in the right eye. His extraocular movements are intact with no other apparent focal neurologic deficits. Which of the following findings would most likely be consistent with this patient’s presentation? ⚪ A. Significant miosis bilaterally prior to pupillary light reflex testing ⚪ B. Failure to obtain a direct and consensual response when light is shone in the left eye ⚪ C. Failure to obtain a direct response when light is shone in the left eye; consensual response without deficits ⚪ D. Failure to obtain a direct response when light is shone in the right eye; consensual response without deficits $ E. Appropriately normal direct and consensual response when light is shone in the left eye OUTLINE Neurology: Auditory 1. Fundamental Concepts ● ● ● A. Basic Ear Anatomy B. Stapedius, Tensor Tympani C. Acoustic Reflex 2. Clinical Diagnostics for Hearing Loss ● ● ● ● A. Weber Test B. Rinne Test C. Conductive Hearing Loss D. Sensorineural Hearing Loss 3. Causes of Conductive Hearing Loss ● ● ● A. Cerumen Impaction B. Otitis Media C. Otosclerosis 4. Causes of Sensorineural Hearing Loss ● ● ● ● A. Acquired Noise Hearing Impairment B. Vestibular Schwannoma C. Presbycusis D. Meniere Disease Neurology: Auditory Bootcamp.com • Auditory Ossicles: • • • Malleus Incus Stapes • Skeletal Muscles: • • Tensor tympani: mandibular branch of trigeminal nerve Stapedius: facial nerve à stapedius nerve • Acoustic Reflex: • Contraction of tensor tympani and stapedius in response to loud noises https://commons.wikimedia.org/wiki/File:Anatomy_of_the_Human_Ear.svg Neurology: Vision Bootcamp.com • Structures Involved: Visual Cortex • • Contains projections of ipsilateral nasal and contralateral temporal visual field fibers Occipital Lobe • General Presentation: • Contralateral homonymous hemianopia with macular sparing • Etiology of Lesions: • Posterior cerebral artery infarction Neurology: Auditory • Weber Test • • Normal: vibration equal bilaterally Abnormal: vibration asymmetric (lateralization) • Rinne Test • Normal: air conduction > bone conduction* • Conductive Hearing Loss • • • External or middle ear Lateralizes to affected ear Bone conduction > air conduction in affected ear • Sensorineural Hearing Loss • • • Inner ear, cochlear nerve Lateralizes to unaffected ear Air conduction > bone conduction in both ears Bootcamp.com Neurology: Auditory Bootcamp.com Weber and Rinne Tests Weber Rinne Left Ear Rinne Right Ear Normal (no lateralization) AC > BC AC > BC Normal hearing Bilateral sensorineural hearing loss Normal (no lateralization) BC > AC BC > AC Bilateral conductive hearing loss (symmetric) Right lateralization AC > BC BC > AC Right conductive hearing loss Left lateralization BC > AC AC > BC Left conductive hearing loss Right lateralization AC > BC AC > BC Left sensorineural hearing loss Left lateralization AC > BC AC > BC Right sensorineural hearing loss Neurology: Auditory • Cerumen Impaction • External auditory canal, conductive • Otitis Media • Infection of middle ear cavity, conductive • Otosclerosis • Stapes fixed against oval window, conductive • Obstructing Mass in External Auditory Canal: • Conductive Bootcamp.com Neurology: Auditory Bootcamp.com • Mechanical Sound Transduction Into Nerve Impulse (organ of Corti) • • • Tympanic membrane à oval window à basilar membrane à Hair cell cilia move against tectorial membrane Depolarization and hyperpolarization through cochlear nerve fibers • Acquired Noise-Induced Hearing Impairment • • Prolonged damage to stereociliated hair cells High frequency, bilateral, sensorineural • Vestibular Schwannoma • • • Trigeminal, facial, and vestibulocochlear nerve in proximity Cerebellopontine angle Sensorineural, usually unilateral (unless NF Type 2) • Presbycusis • Older age, high frequency, bilateral, sensorineural • Meniere Disease • Low frequency tinnitus, sensorineural https://commons.wikimedia.org/wiki/File:Akustikusneurinom_Mrt.jpg https://commons.wikimedia.org/wiki/File:Organ_of_corti.svg ≣ Item 1 of 1 Question ID: 0016 ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪✪ Bootcamp.com A 24-year-old male presents to his family medicine physician for foulsmelling drainage from the left ear. He also states that he has experienced worsening hearing loss from his left side for the past year. He states that he works as a librarian and rarely listens to music. He denies any loss of sensation on the face or fever. A fundoscopic exam is performed revealing a gray-brown irregularly shaped mass with dark discoloration to the surrounding epithelia. Scant amounts of discharge are noted. Which of the following results of the Weber and Rinne test would be most consistent with the finding in this patient? ⚪ A. Left AC > BC, Right BC > AC, lateralization to the right ⚪ B. Left AC > BC, Right AC > BC, lateralization to the left ⚪ C. Left BC > AC, Right AC > BC, lateralization to the left ⚪ D. Left AC > BC, Right AC > BC, lateralization to the right ⚪ E. Left AC > BC, Right AC > BC, no lateralization Legend: Air conduction: AC Bone conduction: BC https://commons.wikimedia.org/wiki/File:Cholesteatom_kuppelraum_1a.jpg ≣ Item 1 of 1 Question ID: 0016 ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪✪ Bootcamp.com A 24-year-old male presents to his family medicine physician for foulsmelling drainage from the left ear. He also states that he has experienced worsening hearing loss from his left side for the past year. He states that he works as a librarian and rarely listens to music. He denies any loss of sensation on the face or fever. A fundoscopic exam is performed revealing a gray-brown irregularly shaped mass with dark discoloration to the surrounding epithelia. Scant amounts of discharge are noted. Which of the following results of the Weber and Rinne test would be most consistent with the finding in this patient? ⚪ A. Left AC > BC, Right BC > AC, lateralization to the right ⚪ B. Left AC > BC, Right AC > BC, lateralization to the left $ C. Left BC > AC, Right AC > BC, lateralization to the left ⚪ D. Left AC > BC, Right AC > BC, lateralization to the right ⚪ E. Left AC > BC, Right AC > BC, no lateralization Legend: Air conduction: AC Bone conduction: BC https://commons.wikimedia.org/wiki/File:Cholesteatom_kuppelraum_1a.jpg OUTLINE Neurology: Vertigo 1. Fundamental Concepts ● ● A. Vestibular System Anatomy B. Peripheral vs Central Vertigo 2. Peripheral Vertigo ● ● ● A. Benign Paroxysmal Positional Vertigo B. Vestibular Neuritis, Labyrinthitis C. Meniere’s Disease, Acoustic Neuroma 3. Central Vertigo ● ● ● ● A. Cerebellar Infarction B. Brainstem Lesions C. Brain Tumor (Posterior Fossa) D. Multiple Sclerosis Neurology: Vertigo • Vestibular System • • • Semicircular canals: detect angular acceleration in 3 planes Saccule: detect linear motion in vertical plane Utricle: detect linear motion in horizontal plane Bootcamp.com Neurology: Vertigo • Peripheral Vertigo • • • • Lesion à inner ear or vestibulocochlear nerve Vertigo ceases or improves with visual fixation Positional Motor, gait, coordination generally intact • Central Vertigo • • • • Lesion à Cerebellum, brainstem nuclei Vertigo does not cease with visual fixation Non-positional, generally continuous Motor, gait, coordination impairment may be present Bootcamp.com Vertigo Peripheral Central Neurology: Vertigo Bootcamp.com Peripheral • Pathophysiology: • Dislodged endolymphatic debris (otoconia) à disrupted semicircular canal function • Presentation: • • • Paroxysmal à sudden onset, lasting less than 1 minute Positional à precipitated by specific head movements Nystagmus • Diagnostics and Management: • • Clinical diagnosis Dix-Hallpike maneuver à if + test à Epley maneuver Neurology: Vertigo • Pathophysiology: • Inflammatory reaction of vestibular nerve • Presentation: • • • • • Persistent à degree of vertigo present continuously Positional à precipitated by specific head movements Previous viral URI or otitis media Nystagmus Labyrinthitis: Similar presentation + hearing loss, possibly tinnitus • Diagnostics and Management: • Clinical diagnosis Bootcamp.com Peripheral Neurology: Vertigo • Pathophysiology: • Bootcamp.com Peripheral Impaired resorption of endolymph à ↑ volume of endolymph • Presentation: • • • • • • Episodic, no trigger (usually) lasts for minutes to hours Unilateral (usually) Tinnitus Sensorineural hearing loss (normal Rinne test, lateralization of Weber test to unaffected) Nystagmus Acoustic Neuroma: Similar presentation, but not episodic • Diagnostics and Management: • • • Acute attack à Vestibular suppressants (meclizine) Secondary prevention à Low sodium diet, avoid triggers Chronic management (refractory) à Thiazide diuretics Neurology: Vertigo • Cerebellar Infarction: • Brain tumor (posterior fossa): • • Adults: Ependymoma, meningioma, metastatic disease Children: Medulloblastomas • Central Nervous System Demyelinating Disease: • • Multiple sclerosis Progressive multifocal leukoencephalopathy Bootcamp.com Central Neurology: Vertigo Bootcamp.com Peripheral Vertigo Disease Pathophysiology Presentation Diagnostics Management Benign paroxysmal positional vertigo Dislodged otoconia, semicircular canals <1 minute episode Worsened with head movements Clinical Dix-Hallpike maneuver Epley (Canalith repositioning) maneuver Vestibular Neuritis Inflammatory reaction to vestibular nerve Continuous worsened with head movements Recent URI (+ hearing loss if labyrinthitis) Clinical Supportive Meniere Disease Endolymph accumulation Minutes to hours Episodic Tinnitus, unilateral hearing loss Clinical, audiometry Acute: Vestibular suppressants Acoustic Neuroma Benign Schwann cell tumor at cerebellopontine angle Progressive worsening Tinnitus, unilateral hearing loss +/- CN V3, VII involvement MRI with contrast Supportive vs surgical/radiation therapy ≣ Item 1 of 1 Question ID: 0017 ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com A 57-year-old female presents to her primary care physician stating that she had three episodes of dizziness over the past week. She states that the first episode occurred when watering flowers in her garden and took a few seconds to resolve. She thought she may have been dehydrated. She reports two more episodes later in the week, at which time she awoke from a partial sleep. She states that she rolled over to her left side in the middle of the night and the dizziness began almost immediately. She states that she is afraid to lay in her bed and has been consuming more water than usual despite feeling nauseous after each episode. She denies any tinnitus or hearing impairment. She also denies any recent illness and states that she receives her flu-shot every year. Physical examination findings are relatively unrevealing. Findings after otoscopy are shown. A Dix-Hallpike maneuver is performed and a horizontal nystagmus with reproducible “dizziness” is observed. ⚪ A. Post-infectious neuronal inflammatory reaction ⚪ B. Dislodged endolymphatic debris ⚪ C. Accumulation of endolymphatic fluid ⚪ D. Obstruction of the eustachian tube ⚪ E. Emboli into the anterior inferior cerebellar artery Which of the following is most likely the underlying pathophysiology explaining this patient’s symptoms? https://commons.wikimedia.org/wiki/File:TM_RIGHT_NORMAL.jpg ≣ Item 1 of 1 Question ID: 0017 ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com A 57-year-old female presents to her primary care physician stating that she had three episodes of dizziness over the past week. She states that the first episode occurred when watering flowers in her garden and took a few seconds to resolve. She thought she may have been dehydrated. She reports two more episodes later in the week, at which time she awoke from a partial sleep. She states that she rolled over to her left side in the middle of the night and the dizziness began almost immediately. She states that she is afraid to lay in her bed and has been consuming more water than usual despite feeling nauseous after each episode. She denies any tinnitus or hearing impairment. She also denies any recent illness and states that she receives her flu-shot every year. Physical examination findings are relatively unrevealing. Findings after otoscopy are shown. A Dix-Hallpike maneuver is performed and a horizontal nystagmus with reproducible “dizziness” is observed. ⚪ A. Post-infectious neuronal inflammatory reaction $ B. Dislodged endolymphatic debris ⚪ C. Accumulation of endolymphatic fluid ⚪ D. Obstruction of the eustachian tube ⚪ E. Emboli into the anterior inferior cerebellar artery Which of the following is most likely the underlying pathophysiology explaining this patient’s symptoms? https://commons.wikimedia.org/wiki/File:TM_RIGHT_NORMAL.jpg OUTLINE Neurology: Pediatric Brain Tumors 1. Pediatric Brain Tumors ● ● ● ● A. Medulloblastoma B. Pilocytic Astrocytoma C. Craniopharyngioma D. Ependymoma 2. Infant Cranial Soft Tissue Injuries ● ● ● A. Cephalohematoma B. Caput Succedaneum C. Subgaleal Hemorrhage Neurology: Pediatric Brain Tumors • • • • Bootcamp.com General Rules: Almost all infratentorial (exception: craniopharyngioma) Headaches worse at night or early morning +/- Noncommunicating hydrocephalus if in proximity to cerebellum and/or 4th ventricle https://commons.wikimedia.org/wiki/File:Illu_tentorium.jpg Neurology: Pediatric Brain Tumors • Origin: Primitive neuroectoderm • (“Primitive neuroectodermal tumors (PNETs)) • Severity: Aggressive • Location: Cerebellum (vermis), infratentorial (usually) • Microscopic: Primitive cells, poorly differentiated • • • ↑ mitotic figures Small round blue anaplastic cells with minimal cytoplasm Homer-Wright pseudorosettes • Presentation: Gait ataxia, noncommunicating hydrocephalus • Association: Drop metastases https://commons.wikimedia.org/wiki/File:1317_CFS_Circulation.jpg https://commons.wikimedia.org/wiki/File:Micrograph_of_Homer_Wright_pseudorosettes.jpg https://commons.wikimedia.org/wiki/File:Structure_of_a_Homer_Wright_pseudorosette.jpg https://commons.wikimedia.org/wiki/File:Structure_of_a_rosette_in_pathology.jpg Bootcamp.com Neurology: Pediatric Brain Tumors • Origin: Astrocytes (glial cells) • • • • • • • Neuroectoderm Glial Fibrillary Acidic Protein (GFAP) Marker Severity: Benign Location: Cerebellum, infratentorial (usually) Macroscopic: Cystic Microscopic: Well-differentiated, hair-like projections, Rosenthal fibers Presentation: Gait ataxia, emesis, failure to thrive https://commons.wikimedia.org/wiki/File:Rosenthal_HE_40x.jpg Bootcamp.com Neurology: Pediatric Brain Tumors Bootcamp.com • Origin: Rathke’s Pouch • Surface ectoderm • Severity: Benign • Location: Suprasellar region • In proximity to pituitary • Macroscopic: Cystic with dystrophic calcification (cholesterol crystals) • Microscopic: “Wet keratin” • Presentation: Bitemporal hemianopsia, hypopituitarism, central diabetes insipidus https://commons.wikimedia.org/wiki/File:Illu_tentorium.jpg https://radiopaedia.org/articles/craniopharyngioma https://upload.wikimedia.org/wikipedia/commons/9/9e/Adamantinomatous_craniopharyngioma_-_intermed_mag.jpg Neurology: Pediatric Brain Tumors • Origin: Ependymal cells • • • • • Neuroectoderm Severity: Variable Location: Peri-ventricular (4th ventricle), infratentorial (usually) Microscopic: Perivascular pseudorosettes Presentation: Intraventricular à obstructive hydrocephalus https://commons.wikimedia.org/wiki/File:Ependymom_sag_FLAIR.jpg https://commons.wikimedia.org/wiki/File:1317_CFS_Circulation.jpg https://commons.wikimedia.org/wiki/File:Micrograph_of_perivascular_pseudorosettes.jpg https://commons.wikimedia.org/wiki/File:Structure_of_a_perivascular_pseud orosette.jpg Bootcamp.com Neurology: Pediatric Brain Tumors • Caput Succedaneum • • • Between skin and epicranial aponeurosis Swelling crosses suture lines Generally benign • Subgaleal Hemorrhage • • • • Between epicranial aponeurosis and periosteum Shearing of emissary veins Significant risk of hemorrhage Can cross suture lines • Cephalohematoma • • Between periosteum and skull Does not cross suture lines https://commons.wikimedia.org/wiki/File:Scalp_hematomas.jpg Bootcamp.com ≣ Item 1 of 1 Question ID: 0018 ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com A 12-year-old female is brought to the emergency department with family following a visit earlier in the day with her pediatrician. She reportedly had two episodes of non-bloody emesis during her check-up. Her parents state that she has “migraine episodes” during the evening or during bedtime. The patient has multiple bruises along her knees and elbows. When questioned, the parents state that she has been in two falls when riding her bicycle over the past month and has been “bumping into things” more than usual. Imaging is performed in the emergency department. A histopathologic specimen is subsequently obtained of the tumor identified and shown below. Which of the following features is most consistent with the origin of tumor cells identified in the specimen? ⚪ A. Phagocytic cells of mesodermal origin ⚪ B. Benign tumor cells of surface ectodermal origin ⚪ C. Glial fibrillary acidic protein positivity ⚪ D. Simple columnar glial cells known to produce cerebrospinal fluid ⚪ E. S100 positive cells of neural crest origin https://commons.wikimedia.org/wiki/File:Ependymoma_pseudorosette.jpg https://neuropathology-web.org/chapter7/chapter7dEpendymoma.html ≣ Item 1 of 1 Question ID: 0018 ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com A 12-year-old female is brought to the emergency department with family following a visit earlier in the day with her pediatrician. She reportedly had two episodes of non-bloody emesis during her check-up. Her parents state that she has “migraine episodes” during the evening or during bedtime. The patient has multiple bruises along her knees and elbows. When questioned, the parents state that she has been in two falls when riding her bicycle over the past month and has been “bumping into things” more than usual. Imaging is performed in the emergency department. A histopathologic specimen is subsequently obtained of the tumor identified and shown below. Which of the following features is most consistent with the origin of tumor cells identified in the specimen? ⚪ A. Phagocytic cells of mesodermal origin ⚪ B. Benign tumor cells of surface ectodermal origin ⚪ C. Benign tumor cells of neural crest cell origin $ D. Simple columnar glial cells known to produce cerebrospinal fluid ⚪ E. S100 positive cells of neural crest origin https://commons.wikimedia.org/wiki/File:Ependymoma_pseudorosette.jpg https://neuropathology-web.org/chapter7/chapter7dEpendymoma.html OUTLINE Neurology: Adult Primary Brain Tumors 1. Adult Primary Brain Tumors ● ● ● ● ● A. Glioblastoma Multiforme B. Vestibular Schwannoma C. Oligodendroma D. Meningioma E. Primary Central Nervous System Lymphoma Neurology: Adult Primary Brain Tumors • • • • General Rules: Almost all supratentorial (exception: vestibular schwannoma, hemangioblastoma) Headaches worse at night or early morning GFAP +: Marker of glial origin, classic case = GBM • • • Bootcamp.com Technically, observed in most forms of adult primary brain tumors NOT observed in meningiomas Synaptophysin +: Marker of neuroendocrine cells • NOT observed in meningiomas https://commons.wikimedia.org/wiki/File:Illu_tentorium.jpg Neurology: Adult Primary Brain Tumors • Origin: Astrocytes (glial cells or pluripotent neural stem cells) • Neuroectoderm • Severity: Aggressive • Location: Cerebral hemispheres • Butterfly glioma: crossing of corpus callosum • Microscopic: Primitive cells, poorly differentiated • • • Pseudopalisading necrosis Peripheral vascular proliferation (neovascularization) ↑ mitotic figures • Molecular: Overexpression epidermal growth factor receptor (EGFR) • Presentation: New onset seizures, headache, FNDs https://commons.wikimedia.org/wiki/File:GBM_pseudopalisading_necrosis.jpg https://radiopaedia.org/articles/butterfly-glioma?lang=us Bootcamp.com Neurology: Adult Primary Brain Tumors Bootcamp.com • Origin: Schwann cells (PNS) • Neural crest cell • Severity: Benign • Location: Cerebellopontine angle (infratentorial) • • Unilateral: Spontaneous Bilateral: Neurofibromatosis type 2 • Molecular: S100 positive (neural crest cell origin) • Presentation: • • • • Vestibular portion of CN VIII: Disequilibrium, vertigo Cochlear portion of CN VIII: Sensorineural hearing loss, tinnitus Facial nerve (CN VII): Facial muscle motor impairment, impaired corneal reflex Trigeminal nerve (CN V): Facial muscle numbness https://commons.wikimedia.org/wiki/File:Akustikusneurinom_Mrt.jpg Neurology: Adult Primary Brain Tumors Bootcamp.com • Origin: Oligodendrocytes (CNS) • Severity: Benign • Location: Cerebral hemisphere • Frontal lobe is classic • Microscopic: “Fried egg” appearance to cells • Capillaries à “Chicken-wire” pattern • Presentation: Seizures, headaches, FNDs, (if frontal lobe à personality changes) https://www.neurocirugiabarcelona.com/en/pathologies/brain-tumours/glialtumours/oligodendrogliomas/ https://commons.wikimedia.org/wiki/File:Flickr_-_cyclonebill_-_Vagtel-spejl%C3%A6g.jpg https://commons.wikimedia.org/wiki/File:Oligodendroglioma1_high_mag.jpg Neurology: Adult Primary Brain Tumors • Origin: Arachnoid cells • Severity: Benign • Slow growing • Location: Parasagittal region of cerebral hemispheres • In proximity to dural reflections (falx cerebri, foramen magnum) Macroscopic: Extra-axial • • Microscopic: Psammoma bodies • Eosinophilic whorls with layered appearance (onion) • Molecular: Negative for GFAP and synaptophysin • Presentation: Asymptomatic vs seizures, headaches, FNDs https://commons.wikimedia.org/wiki/File:MRIMeningioma.png https://commons.wikimedia.org/wiki/Category:Psammoma_bodies#/media/File:Psammoma_bodies.jpg https://commons.wikimedia.org/wiki/File:Meningioma_high_mag.jpg Bootcamp.com Neurology: Adult Primary Brain Tumors Bootcamp.com • Origin: B-cells (typically) • Common subtype: Diffuse large B-cell lymphoma • Severity: Aggressive • Macroscopic: Lesions throughout white and gray matter • • • • • Ring-enhancing lesion on CT Microscopic: Aggregates of atypical lymphoid cells Molecular: CD20, CD79a Presentation: Immunocompromised (poorly controlled HIV/AIDs), FNDs, seizure Association: Epstein—Barr virus https://radiopaedia.org/cases/primary-cns-lymphoma-2 ≣ Item 1 of 1 Question ID: 0019 ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪✪✪ Bootcamp.com A 44-year-old female presents to the emergency room after experiencing an episode of loss of consciousness with generalized uncontrollable and rhythmic muscle contractions. Her husband reports that she has been unable speak well since the incident. He believes that she may be embarrassed due to the episode of bladder incontinence she suffered when paramedics arrived. Lacerations on the tongue are noted and the patient is visibly aphasic. A review of the patient’s medical history reveals a history of hypothyroidism and no history of previous seizure episodes. Her husband states that she has no family history of seizures, and she does not consume alcohol. A head CT and subsequent biopsy of identified mass lesion is performed and shown. Which of the following is most consistent with the patient’s tumor? ⚪ A. Derived from tissue of neuroectoderm ⚪ B. Derived from tissue of neural crest cell origin ⚪ C. Glial fibrillary acidic protein positive ⚪ D. Synaptophysin positive ⚪ E. Strong staining for CD20 https://commons.wikimedia.org/wiki/File:Contrast_enhanced_meningioma.jpg https://commons.wikimedia.org/wiki/File:Meningioma_showing_Psammoma_body.jpg ≣ Item 1 of 1 Question ID: 0019 ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪✪✪ Bootcamp.com A 44-year-old female presents to the emergency room after experiencing an episode of loss of consciousness with generalized uncontrollable and rhythmic muscle contractions. Her husband reports that she has been unable speak well since the incident. He believes that she may be embarrassed due to the episode of bladder incontinence she suffered when paramedics arrived. Lacerations on the tongue are noted and the patient is visibly aphasic. A review of the patient’s medical history reveals a history of hypothyroidism and no history of previous seizure episodes. Her husband states that she has no family history of seizures, and she does not consume alcohol. A head CT and subsequent biopsy is performed and shown. Which of the following is most consistent with the patient’s mass lesion? ⚪ A. Derived from tissue of neuroectoderm $ B. Derived from tissue of neural crest cell origin ⚪ C. Glial fibrillary acidic protein positive ⚪ D. Synaptophysin positive ⚪ E. Strong staining for CD20 https://commons.wikimedia.org/wiki/File:Contrast_enhanced_meningioma.jpg https://commons.wikimedia.org/wiki/File:Meningioma_showing_Psammoma_body.jpg OUTLINE Neurology: Ischemic Cerebrovascular Accidents 1. Types of Ischemic Cerebrovascular Accidents ● ● ● A. Thrombotic B. Embolic C. Global 2. Histopathology ● ● A. Liquefactive Necrosis B. Histologic Changes by Time 3. Cerebrovascular Accident by Cerebral Territory ● ● ● ● A. Middle Cerebral Artery B. Anterior Cerebral Artery C. Posterior Cerebral Artery D. Lenticulostriate Arteries 4. Lacunar Infarction ● ● ● A. General Overview B. Pure Motor, Pure Sensory, Sensorimotor Variants C. Subthalamic Infarction 5. Brainstem Infarction ● ● ● ● A. Medial Medullary Syndrome B. Lateral Medullary Syndrome C. Lateral Pontine Syndrome D. ”Locked In” Syndrome 6. Basics of Cerebrovascular Accident Management ● ● A. Acute Management- tPA B. Secondary Prevention Neurology: Cerebrovascular Accidents Bootcamp.com CVA Ischemic Thrombotic Hemorrhagic Subarachnoid Other Intracranial Intraparenchymal Embolic Epidural Hematoma Lobar Lacunar Subdural hematoma Lacunar Hypoperfusion Intraventricular Neurology: Cerebrovascular Accidents Bootcamp.com Transient Ischemic Attack FNDs without tissue infarction Normal imaging Typically resolve without intervention <24 hours • Thrombotic: • Etiology à Atherosclerotic plaques à vessel occlusion • Embolic: • • • Remember UMN Signs! Hyperreflexia Hypertonia Spasticity (Clasp-knife) Babinski sign (upgoing plantar reflex) Etiology à Atrial fibrillation, bacterial endocarditis Classic areas affected à MCA, ACA, or PCA division (large vessel disease) Asymmetric pattern of scattered infarcts • Hypoperfusion (Global): • • • Watershed areas affected Wedge-appearing areas of necrosis bilaterally (autopsy) Hippocampus = vulnerable to hypoxia https://commons.wikimedia.org/wiki/File:Human_brain_frontal_(coronal)_section.JPG Neurology: Cerebrovascular Accidents Bootcamp.com https://commons.wikimedia.org/wiki/File:MCA-Stroke-Brain-Human-2.JPG • Liquefactive Necrosis: • • • Irreversible injury approximately 4-5 minutes of hypoxia Neural cell irreversible injury à hydrolytic enzymes (lysosomes) à liquefactive necrosis (weeks) Microglia digestion à cystic spaces surrounded by gliosis (months), pale infarct Cerebrovascular Accident Histopathology by Timeline Pathophysiology Time Post-Injury 1 hour 12-24 hours 1-3 days 3-7 days 1-2 weeks 2 weeks and beyond Histologic Presentation Failure of ATP-gated ion channels ↑ glutamate Minimal changes Cytotoxic edema Activity and dissolution of Nissl bodies Irreversible chromatin condensation Red neurons à eosinophilic cytoplasm (loss of Nissl bodies) Pyknotic nuclei à small, basophilic nuclei Neutrophilic invasion Disruption of tight junctions of BBB Liquefactive necrosis ↑ local neutrophil density Vasogenic edema Macrophage and microglial invasion Phagocytosis ensues ↑ local macrophage and microglial density Reactive gliosis Astrocyte proliferation, glial hypertrophy Vascular proliferation at peripheral sites to necrosis Dense astrocytic processes surrounding cavity of necrotic debris Cystic spaces surrounded by glial scarring Neurology: Cerebrovascular Accidents Bootcamp.com Cerebrovascular Accident Presentation by Territory Artery Lenticulostriate MCA ACA PCA High Yield Territories Classic Lesion Presentation Basal ganglia Internal capsule (posterior limb) Chorea, tremor, bradykinesia, rigidity, altered behavior C/L motor and sensory impairment Primary motor cortex- Frontal Broca’s area (D)-Frontal Wernicke’s area (D)-Temporal Angular gyrus (D)- Parietal (ND)- Parietal Frontal eye fields- Frontal Optic radiations C/L upper extremity and lower face, motor and sensory impairment Nonfluent aphasia (Expressive) Fluent aphasia (Receptive) Gerstmann Syndrome C/L: Hemineglect Conjugate deviation to side of lesion C/L homonymous hemianopia or quadrantanopia Anteromedial primary motor and sensory cortex C/L lower extremity, motor and sensory impairment B/L urinary incontinence, altered behavior (abulia) Primary visual cortex- Occipital C/L homonymous hemianopia with macular sparing (D): Dominant (usually left) (ND): Non-dominant (usually right) C/L: Contralateral B/L: Bilateral Neurology: Cerebrovascular Accidents Bootcamp.com https://commons.wikimedia.org/wiki/File:CT_of_lacunar_strokes.jpg https://commons.wikimedia.org/wiki/File:Blausen_0076_BasalGanglia.png • Artery: Lenticulostriate arteries • Association: #1 Chronic poorly controlled hypertension • Location: Basal ganglia, posterior limb internal capsule, cerebellum • Presentation: • • • Internal capsule: Contralateral hemiparesis +/- hemisensory loss Basal ganglia: Tremor, bradykinesia, chorea, rigidity, altered behavior Unusual to observe cortical signs • Lacunar Ischemia: Hypertensive arteriolar sclerosis • • • Microatheroma à lipid-laden macrophage accumulation, commonly at branch points Lipohyalinosis à foamy macrophages, vascular wall thickening Lacunar Hemorrhage: Hypertensive vasculopathy • Charcot-Bouchard aneurysms Neurology: Cerebrovascular Accidents Bootcamp.com • Pure Motor: Contralateral upper and lower extremity, face • Posterior limb of internal capsule (most common) • Pure Sensory: Contralateral upper and lower extremity, face • • Ventroposterolateral and/or ventroposteriomedial thalamus (common) Posterior limb of internal capsule (rare) • Mixed Sensorimotor: Contralateral upper and lower extremity, face • Posterior limb of internal capsule (common) • Hemiballismus: Contralateral involuntary large flinging movements of extremities • Subthalamic nucleus Neurology: Cerebrovascular Accidents • Medial Medullary (Dejerine) Syndrome: • • • • (D): Dominant (usually left) (ND): Non-dominant (usually right) I/L: Ipsilateral C/L: Contralateral B/L: Bilateral Lateral Medullary (Wallenberg) Syndrome: • • • • • • Anterior spinal artery or vertebral artery CN XII à I/L tongue palsy (deviation to side of lesion) Medial tracts à C/L weakness of limbs, C/L loss of vibration and proprioception Bootcamp.com Posterior inferior cerebellar artery (PICA) or vertebral artery CN VIII à vertigo, nystagmus, hearing loss CN IX, X à dysphagia, dysphonia, impaired gag reflex Lateral tracts à loss of temperature and pain sensation I/L face, C/L trunk and limbs, I/L ataxia, dysmetria, dysdiadochokinesia Sympathetic (lateral) tract à Horner syndrome I/L (miosis, ptosis, anhidrosis) Lateral Pontine Syndrome: • • • • • Anterior inferior cerebellar artery (AICA) CN VII à facial muscle weakness, hyperacusis, loss of taste anterior 2/3 of tongue CN VIII à vertigo, nystagmus, hearing loss Lateral tracts à loss of temperature and pain sensation I/L face, C/L trunk and limbs, I/L ataxia, dysmetria, dysdiadochokinesia Sympathetic (lateral) tract à Horner syndrome I/L (miosis, ptosis, anhidrosis) Neurology: Cerebrovascular Accidents Bootcamp.com • Artery: Basilar artery (bilateral ventral pontine CVA) • Location: Ventral pons • Presentation: • • • • Quadriparesis Horizontal gaze palsy (vertical eye movements and voluntary blinking preserved) Anarthria, dysphagia Cheyne-Stokes's respirations • Osmotic Demyelination Syndrome (Central Pontine Myelinolysis): • • Etiology: rapid overcorrection of chronic hyponatremia Symmetric pontine demyelination on MRI Neurology: Cerebrovascular Accidents • Anti-platelet therapy: Aspirin, clopidogrel • HMG-CoA Reductase Inhibitor: Atorvastatin, rosuvastatin, pravastatin • Lifestyle Modifications: Diet, exercise, smoking cessation • Tissue Plasminogen Activator (tPA) • < 4.5 hours of onset of symptoms Bootcamp.com ≣ Item 1 of 1 Question ID: 0020 ◽" Mark ⟽ Previous ⟾ Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com A 59-year-old male presents to the emergency room stating, “I can’t feel my left arm or leg.” He reports that he suddenly felt weak while washing dishes after dinner and nearly lost his balance. He denies falling and states that he was able to sit down immediately after symptom onset. He denies any confusion or loss of consciousness. He states that he has no difficulty speaking and denies any dysphagia. He has a long history of chronic hypertension and no previous medical or family history of cerebrovascular disease or hemorrhage. He reports that he has not refilled his antihypertensive prescription medications because of a demanding work schedule over the past month. Physical examination reveals generalized sensory loss on the left upper and lower extremities and 4/5 muscle strength of the left thigh, shoulder, and biceps. No abnormal involuntary motor movements are noted. Extraocular eye movements are intact bilaterally, and no nystagmus is observed. Non-contrast CT of the head is performed and shown. Which of the following findings would be most consistent with this patient’s presentation at this time? ⚪ A. Infarction and cytotoxic edema within the subthalamic nucleus ⚪ B. Lipohyalinosis of vessels supplying the posterior limb of the internal capsule ⚪ C. Symmetric pontine demyelination represented bilaterally ⚪ D. Cavitary lesion overlying the lenticulostriate artery distribution surrounded by glial hypertrophy ⚪ E. Bilateral renal enlargement with diffuse cystic disease https://upload.wikimedia.org/wikipedia/en/0/04/Brain_CT_scan.jpg ≣ Item 1 of 1 Question ID: 0020 ◽" Mark ⟽ Previous ⟾ Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com A 59-year-old male presents to the emergency room stating, “I can’t feel my left arm or leg.” He reports that he suddenly felt weak while washing dishes after dinner and nearly lost his balance. He denies falling and states that he was able to sit down immediately after symptom onset. He denies any confusion or loss of consciousness. He states that he has no difficulty speaking and denies any dysphagia. He has a long history of chronic hypertension and no previous medical or family history of cerebrovascular disease or hemorrhage. He reports that he has not refilled his antihypertensive prescription medications because of a demanding work schedule over the past month. Physical examination reveals generalized sensory loss on the left upper and lower extremities and 4/5 muscle strength of the left thigh, shoulder, and biceps. No abnormal involuntary motor movements are noted. Extraocular eye movements are intact bilaterally, and no nystagmus is observed. Non-contrast CT of the head is performed and shown. Which of the following findings would be most consistent with this patient’s presentation at this time? ⚪ A. Infarction and cytotoxic edema within the subthalamic nucleus $ B. Lipohyalinosis of vessels supplying the posterior limb of the internal capsule ⚪ C. Symmetric pontine demyelination represented bilaterally ⚪ D. Cavitary lesion overlying the lenticulostriate artery distribution surrounded by glial hypertrophy ⚪ E. Bilateral renal enlargement with diffuse cystic disease https://upload.wikimedia.org/wikipedia/en/0/04/Brain_CT_scan.jpg OUTLINE Neurology: Aneurysms and Hemorrhagic Cerebrovascular Accidents 1. Cerebral Blood Supply ● A. Circle of Willis 2. Cerebrovascular Aneurysm ● ● ● ● A. Saccular Aneurysm B. Charcot-Bouchard Aneurysm C. Posterior Communicating Artery Aneurysm D. Anterior Communicating Artery Aneurysm 3. Intracranial Hemorrhage ● ● ● ● ● A. Epidural Hematoma B. Subdural Hematoma C. Subarachnoid Hemorrhage D. Intraparenchymal Hemorrhage E. Intraventricular Hemorrhage Neurology: Cerebrovascular Accidents Bootcamp.com CVA Ischemic Thrombotic Hemorrhagic Subarachnoid Other Intracranial Intraparenchymal Embolic Epidural Hematoma Lobar Lacunar Subdural hematoma Lacunar Hypoperfusion Intraventricular Neurology: Brain Blood Supply and Aneurysms Bootcamp.com https://commons.wikimedia.org/wiki/File:2123_Arteries_of_the_Brain.jpg https://case.edu/med/neurology/NR/MagnResnAngiogrMRA/MagnResnAngiogrMRA.htm Neurology: Brain Blood Supply and Aneurysms Bootcamp.com https://commons.wikimedia.org/wiki/File:2123_Arteries_of_the_Brain.jpg • Saccular: • • • Arise at branch points Anterior communicating artery + anterior cerebral artery junction = MC Rupture à Subarachnoid hemorrhage à FNDs not usually present • Charcot-Bouchard: • • • *if present - would depend on aneurysm size/ location* Association with chronic hypertension and diabetes Lenticulostriate vessels affected Rupture à Lacunar Hemorrhage à FNDs (may vary) Neurology: Brain Blood Supply and Aneurysms Bootcamp.com https://commons.wikimedia.org/wiki/File:2123_Arteries_of_the_Brain.jpg • Posterior Communicating Artery Aneurysm: • • Oculomotor nerve (CN III) palsy à dilated (first) à “down and out” pupil, ptosis Anterior Communicating Artery Aneurysm: • Optic chiasm à Bitemporal hemianopia Neurology: Brain Blood Supply and Aneurysms Bootcamp.com https://commons.wikimedia.org/wiki/File:EpiduralHematoma.jpg https://commons.wikimedia.org/wiki/File:Subduralandherniation.PNG https://commons.wikimedia.org/wiki/File:SubarachnoidP.png • Epidural Hematoma: • • • • • • Subdural Hematoma: • • • • • Middle meningeal artery (branch of maxillary artery) Area between skull and dura mater Transient LOC à Lucid interval à LOC Biconvex hematoma (lens-shape) Uncal herniation à ipsilateral dilated pupil, ipsilateral lateral rectus palsy Bridging cortical veins Area between dura and arachnoid mater Acute vs chronic, elderly patient, shaken baby syndrome Crescent hematoma Subarachnoid Hemorrhage: • • • • • • Rupture of saccular (berry) aneurysm or AV malformation Area between arachnoid and pia mater ”Worst headache of life”, thunderclap headache, neck stiffness/pain Mental status progressively worsens Blood pooling in basal cisterns Focal neurologic deficits are unusual (vs intracerebral hemorrhage) Head Imaging Post-Trauma à CT scan without contrast Remember signs of ↑ ICP! Papilledema Cushing Reflex Headache Lateral rectus palsy, I/L mydriasis Neurology: Brain Blood Supply and Aneurysms • Cerebral Vasospasm • • • • • • Cerebral ischemia delayed from initial SAH 4-12 days after initial SAH Focal neurologic deficits (unlike with initial SAH) Head CT without contrast usually negative Prevent with Nimodipine Rebleeding generally first 24 hours • Associations • Bootcamp.com Suspicion for SAH Head CT without contrast Blood in basal cisterns = Diagnostic Negative ADPKD, Ehler’s Danlos Lumbar Puncture Negative Unlikely SAH Xanthochromia (or ↑ RBC) Likely SAH Neurology: Brain Blood Supply and Aneurysms • Lobar Hemorrhage: • • • • Signs of ↑ ICP, FNDs Elderly patient with cerebral amyloid angiopathy Temporal lobe à Uncal (transtentorial) herniation High tendency for recurrence Bootcamp.com Remember signs of ↑ ICP! Papilledema Cushing Reflex Headache Lateral rectus palsy, I/L mydriasis • Lacunar Hemorrhage: • • • • • Charcot-Bouchard aneurysms Hypertensive vasculopathy Putamen = MC site, thalamus = 2nd MC site Internal capsule: Contralateral hemiparesis +/- hemisensory loss Basal ganglia: Tremor, bradykinesia, chorea, rigidity, altered behavior Neurology: Brain Blood Supply and Aneurysms • Association: Premature (or low birth weight) newborn • Location: Germinal matrix • Presentation: • • • First few days after birth Bulging anterior fontanelle New onset FNDs +/- seizures and other signs of ↑ ICP • Differential: • Forceps or vacuum assisted delivery à Bootcamp.com ≣ Item 1 of 1 ◽" Mark Question ID: 0021 ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com https://case.edu/med/neurology/NR/MagnResnAngiogrMRA/MagnResnAngiogrMRA.htm E A D C B A 33-year-old female presents to the emergency room with gross hematuria. She states that she has been experiencing progressively worsening flank pain bilaterally over the past six months. She denies any recent trauma but reports that she nearly collided with another vehicle while driving a few weeks ago because the other car “came out of nowhere”. Since that time, she has avoided driving and playing sports with friends. Her family history is significant for cerebral hemorrhage in her father and grandmother. Blood pressure is 164/80, heart rate 78/min, respiratory rate 12/min. Peripheral visual field findings are shown. Renal ultrasound reveals significant diffuse cystic disease in the bilateral kidneys. Which of the following single lesion sites would best explain this patient’s presentation? ⚪ A. ⚪ B. ⚪ C. ⚪ D. ⚪ E. ≣ Item 1 of 1 ◽" Mark Question ID: 0021 ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com https://case.edu/med/neurology/NR/MagnResnAngiogrMRA/MagnResnAngiogrMRA.htm E A D C B A 33-year-old female presents to the emergency room with gross hematuria. She states that she has been experiencing progressively worsening flank pain bilaterally over the past six months. She denies any recent trauma but reports that she nearly collided with another vehicle while driving a few weeks ago because the other car “came out of nowhere”. Since that time, she has avoided driving and playing sports with friends. Her family history is significant for cerebral hemorrhage in her father and grandmother. Blood pressure is 164/80, heart rate 78/min, respiratory rate 12/min. Peripheral visual field findings are shown. Renal ultrasound reveals significant diffuse cystic disease in the bilateral kidneys. Which of the following single lesion sites would best explain this patient’s presentation? ⚪ A. ⚪ B. ⚪ C. ⚪ D. $ E. OUTLINE Neurology: Cerebellum and Ventricles 1. Anatomical Considerations ● ● ● ● ● A. Sagittal Brain MRI B. Ventricular Brain Anatomy C. Flow of Cerebrospinal Fluid D. Cerebellar Anatomical Zones E. Area Postrema 2. Hydrocephalus ● ● ● ● ● A. Noncommunicating Hydrocephalus B. Communicating Hydrocephalus C. Normal Pressure Hydrocephalus D. Hydrocephalus Ex Vacuo E. Pseudotumor Cerebri 3. Sensory vs Cerebellar Ataxia ● ● ● A. Sensory Ataxia B. Cerebellar Ataxia C. Romberg Test 4. Cerebellar Pathology ● ● ● ● ● A. Ataxia Telangiectasia B. Friedreich Ataxia C. Paraneoplastic Cerebellar Degeneration D. Dandy-Walker Malformation E. Arnold-Chiari Malformation Neurology: Cerebellum and Ventricles Bootcamp.com https://radiopaedia.org/articles/sagittal-midline-of-the-brain-an-approach-1 • • • • • • • • Sagittal MRI Key Landmarks: Thalamus Pons Cerebellum Area Postrema Corpus Callosum Lateral Ventricle 4th Ventricle Neurology: Cerebellum and Ventricles CSF produced at choroid plexus Lateral ventricle Interventricular foramina of Monro Third Ventricle Bootcamp.com Cerebral aqueduct (of Sylvius) Fourth ventricle Exits via foramina of Luschka or foramen of Magendie Subarachnoid space Arachnoid granulations Venous circulation https://commons.wikimedia.org/wiki/File:CSF_circulation.png Neurology: Cerebellum and Ventricles Bootcamp.com https://commons.wikimedia.org/wiki/File:Papilledema.jpg https://radiopaedia.org/articles/normal-pressure-hydrocephalus https://radiopaedia.org/images/15747811?case_id=39554 https://commons.wikimedia.org/wiki/File:Blausen_0896_Ventricles_Brain.png • Noncommunicating (Obstructive) Hydrocephalus: • • • • • • Communicating Hydrocephalus: • • • • Normal ICP, ventriculomegaly out of proportion to cortical atrophy Etiology: Impaired CSF absorption Triad: ataxia (“magnetic gait”), urinary incontinence, dementia Hydrocephalus Ex Vacuo: • • • • ↑ ICP, diffuse ventriculomegaly Etiology: Scarring due to ↓ resorption at arachnoid granulations, ↑ production Classic Causes: Subarachnoid hemorrhage, choroid plexus papilloma Normal Pressure Hydrocephalus: • • • • ↑ ICP, ventriculomegaly proximal to obstruction Etiology: Scarring, mass lesions Malformations: Arnold-Chiari malformation, Dandy-Walker malformation Infectious: CMV, meningitis, toxoplasmosis Other classic causes: Intraventricular bleed Normal ICP, ventriculomegaly in proportion to cortical atrophy Etiology: Diffuse cortical atrophy Association: Dementia (AD), AIDS, Huntington disease Pseudotumor Cerebri (Idiopathic Intracranial Hypertension): • • ↑ ICP, normal ventricular size Association: Young, obese female, excessive vitamin A Neurology: Cerebellum and Ventricles Bootcamp.com • Midline Cerebellar Lesions: Truncal ataxia, wide-based gait • Lateral Cerebellar Lesions: Ipsilateral dysmetria, intention tremor • Inferior Cerebellar Lesions: Vertigo, nystagmus Cerebellum Overview Cerebellar Territory Location Primary Function Classic Lesion(s) Vermis Midline Motor via medial descending motor systems Truncal ataxia Wide-based gait Flocculonodular Lobe Inferiorly Balance, eye movements via vestibular nuclei and medial longitudinal fasciculus Vertigo*, nystagmus* Intermediate Hemisphere Lateral to vermis Motor via lateral descending motor systems Lateral Hemisphere Lateral to intermediate hemisphere Motor planning Intention tremor Ipsilateral dysdiadochokinesia Ipsilateral dysmetria *May also observe with lesions to inferior vermis https://commons.wikimedia.org/wiki/File:CerebellumDiv.png https://dizziness-and-balance.com/disorders/central/cerebellar/cerebellar.htm Neurology: Cerebellum and Ventricles Bootcamp.com • Cerebellar Ataxia: • • Classic Regions Involved: Cerebellum Etiology: Ataxia Telangiectasia, cerebellar tumor • Sensory Ataxia: • • Classic Regions Involved: Peripheral nervous system, DCML Etiology: Vitamin B12 deficiency, tertiary syphilis (tabes dorsalis) Romberg Test Eyes open Unsteadiness present Unspecified form of ataxia Eyes closed No unsteadiness present Unlikely cerebellar ataxia Unsteadiness worsening or failure to maintain posture Sensory and/or vestibular ataxia Minimal changes to unsteadiness (compared with eyes open) Cerebellar ataxia No unsteadiness present Unlikely sensory and/or vestibular ataxia Neurology: Cerebellum and Ventricles Bootcamp.com https://radiopaedia.org/cases/dandy-walker-malformation-11 https://radiopaedia.org/articles/chiari-ii-malformation https://commons.wikimedia.org/wiki/File:Dermoscopy_nodular_basal_cell_carcinoma.jpg • • • • • Ataxia Telangiectasia: • Triad: Cerebellar ataxia, telangiectasias (spider angiomas), IgA deficiency • Mutation à ATM gene Friedreich Ataxia: • Adolescent or older child • Deficiency of frataxin, trinucleotide repeat expansion of GAA on chromosome 9 • UMN and LMN signs • Progressive cerebellar and sensory ataxia • Association: Scoliosis, pes cavus, hammertoes, diabetes mellitus, HOCM Paraneoplastic Cerebellar Degeneration: • History of cancer (Breast, ovarian, uterine, small cell lung) • Rapid deterioration and worsening of cerebellar symptoms • Anti-Yo, anti-Hu, anti-P/Q Dandy-Walker Malformation: • Infant with developmental delay • Hypoplasia (or complete absence) of cerebellar vermis • Enlarged posterior fossa and dilation of fourth ventricle Arnold-Chiari Malformation (Chiari II): • Infant with developmental delay à obstructive hydrocephalus • Inferior displacement of cerebellar tonsils and vermis • Association with myelomeningocele Neurology: Cerebellum and Ventricles • Area Postrema: • • • Chemoreceptor trigger zone Direct stimulation via substance P à NK1 receptors in brainstem (↓ BBB) Indirect stimulation via serotonin à 5-HT3 receptors on vagal afferents • Antiemetic Pharmacology • • Ondansetron à selective 5-HT3 receptor antagonist Aprepitant à NK1 receptor antagonist Bootcamp.com ≣ Item 1 of 1 Question ID: 0022 ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪ Bootcamp.com A 77-year-old female with a past medical history of atrial fibrillation and hypertension presents to the emergency department with an acutely worsening occipital headache and nausea. She states that she had one episode of non-bloody emesis en route to the hospital. She denies any vertigo, tinnitus, or vision changes. She admits to a 34-pack year history of tobacco use. Her medications include warfarin, lisinopril, and a multivitamin. Her temperature is 97.6 F (36.4 C), blood pressure is 194/90, heart rate is 94/min, respirations are 12/min. Electrocardiogram reveals sinus rhythm. Laboratory studies are as follows: Hemoglobin 14.2 g/dL Leukocytes 5,000/mm3 Platelets 285,000/mm3 Prothrombin time prolonged Activated partial thromboplastin time normal ⚪ A. Coarse hand tremor worsened with targeted movement ⚪ B. Pill-rolling hand tremor worsened with stress Noncontrast CT of the head is shown. Which of the following findings ⚪ C. Left-sided upper extremity weakness ⚪ D. Bilateral pes cavus would most likely be observed given the patient’s presentation? ⚪ E. Urinary incontinence ⚪ F. Hyperorality https://radiopaedia.org/articles/cerebellar-haemorrhage ≣ Item 1 of 1 Question ID: 0022 ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪ Bootcamp.com A 77-year-old female with a past medical history of atrial fibrillation and hypertension presents to the emergency department with an acutely worsening occipital headache and nausea. She states that she had one episode of non-bloody emesis en route to the hospital. She denies any vertigo, tinnitus, or vision changes. She admits to a 34-pack year history of tobacco use. Her medications include warfarin, lisinopril, and a multivitamin. Her temperature is 97.6 F (36.4 C), blood pressure is 194/90, heart rate is 94/min, respirations are 12/min. Electrocardiogram reveals sinus rhythm. Laboratory studies are as follows: Hemoglobin 14.2 g/dL Leukocytes 5,000/mm3 Platelets 285,000/mm3 Prothrombin time prolonged Activated partial thromboplastin time normal $ A. Coarse hand tremor worsened with targeted movement ⚪ B. Pill-rolling hand tremor worsened with stress Noncontrast CT of the head is shown. Which of the following findings ⚪ C. Left-sided upper extremity weakness ⚪ D. Bilateral pes cavus would most likely be observed given the patient’s presentation? ⚪ E. Urinary incontinence ⚪ F. Hyperorality https://radiopaedia.org/articles/cerebellar-haemorrhage OUTLINE Neurology: Diencephalon 1. Hypothalamus ● ● ● ● ● A. Hypothalamic Nuclei B. Jet Lag Syndrome C. Kallman Syndrome D. Wernicke-Korsakoff Syndrome E. Disorders of Temperature Regulation 2. Thalamus ● ● ● ● ● A. Thalamic Nuclei B. Thalamic Syndrome C. Lacunar Stroke D. Hydrocephalus Ex Vacuo E. Pseudotumor Cerebri 3. Pineal Gland ● ● A. Suprachiasmatic Nucleus B. Parinaud Syndrome 4. Limbic System ● ● ● A. Hippocampus B. Amygdala C. Kluver-Bucy Syndrome Neurology: Diencephalon Bootcamp.com • Hypothalamus: • Homeostasis à regulating appetite, temperature, circadian rhythm, and growth • Thalamus: • • • • • • Ventral lateral thalamic nucleus: Inà Cerebellum, basal ganglia : Out à Primary motor cortex Ventral posterolateral nucleus (VPL): Inà Spinothalamic tract, DCML : Out à Somatosensory cortex Ventral posteromedial nucleus (VPM): In à Trigeminal nerve, taste sensation : Out à Somatosensory cortex Lateral geniculate nucleus (LGN): In à Optic pathway, superior colliculi : Out à Primary visual cortex Medial geniculate nucleus (MGN): In à Inferior colliculi : Out à Primary auditory cortex Dorsomedial nucleus: In à Substantia nigra, amygdala, temporal cortex : Out à Prefrontal cortex • Pineal Gland: • • Receives input from suprachiasmatic nucleus Regulation of sleep wake cycle via circadian release of melatonin • Limbic System: • • Hippocampus: Memory formation, affected in Alzheimer’s dementia and early in hypoxia Amygdala: Emotion, fear, aggression Neurology: Diencephalon Bootcamp.com Hypothalamic Nuclei Function Lesion Regulation Heat loss Hyperthermia + Parasympathetics - Sympathetics Heat retention Hypothermia + Sympathetics Lateral Hunger Poor appetite + Ghrelin - Leptin Ventromedial Satiety Hyperphagia + Leptin Anterior Posterior Function Lesion Arcuate Dopamine secretion ↑ prolactin Preoptic GnRH secretion Kallman syndrome ↓ GnRH Paraventricular Supraoptic Suprachiasmatic Mamillary Body Oxytocin and ADH secretion CRH, TRH release Somatostatin release Central diabetes insipidus Oxytocin and ADH secretion Circadian rhythm Regulation of melatonin release (pineal gland) Insomnia Episodic memory Wernicke Encephalopathy Neurology: Diencephalon • • • • Jet Lag Disorder: • Suprachiasmatic nucleus dyssynchrony Kallman Syndrome (Hypogonadotropic hypogonadism): • Anosmia à impaired migration of GnRH-neurons • ↓ GnRH à ↓ FSH, ↓ LH • Males: cryptorchidism, females: primary amenorrhea Wernicke Encephalopathy: • History of chronic alcohol use • Vitamin B1 (thiamine) deficiency à Avoid dextrose without thiamine supplementation • Acute and reversible • Ataxia, oculomotor disease, and encephalopathy • Mamillary body (atrophy or Korsakoff Syndrome: • Chronic Vitamin B1 deficiency • Vitamin B1 (thiamine deficiency) • Chronic and irreversible • Confabulation with poor insight, anterograde (and/or retrograde) amnesia, personality changes • Attention, cognition, and long-term memory generally preserved Bootcamp.com Neurology: Diencephalon • • • Heat exhaustion: • T less than or equal to 104 F (40 C) • No deficits in central neurologic functioning Nonexertional Heatstroke: • T greater than 104 F (40 C) • Bimodal distribution (children and elderly) • Deficits in central neurologic functioning • +/- absence of diaphoresis Exertional Heatstroke: • T greater than 104 F (40 C). • Healthy adults • Deficits in central neurologic functioning Bootcamp.com Neurology: Diencephalon Bootcamp.com https://commons.wikimedia.org/wiki/File:Osborn_wave.gif • • • Mild hypothermia: • T 90-95 F (32-35 C) • Tachycardia, tachypnea, possibly altered mental status Moderate hypothermia: • T 82-90 F (28-32 C) • Bradycardia, irregular breathing, possibly lethargy and general nervous system depression Severe hypothermia: • T less than 82 F (28 C) • Hypotension, pulmonary edema, apnea, ventricular fibrillation Neurology: Diencephalon • • Bootcamp.com Thalamic Syndrome: • Severe contralateral burning, sharp pain affecting regions involved by previous stroke Lacunar Stroke Affecting the Thalamus: • Pure Sensory à Ventroposterolateral and/or ventroposteriomedial thalamus (common) • Contralateral sensory loss of face, upper and lower extremities (affecting multiple pathways) Neurology: Diencephalon Bootcamp.com https://commons.wikimedia.org/wiki/File:Tumor_Pineocytoma1.JPG • • Kluver-Bucy Syndrome: • Hyperorality, hyperphagia, and hypersexuality +/- HSV encephalitis Parinaud Syndrome: • Vertical gaze palsy, pseudo-Argyll Robertson pupils, convergence-retraction nystagmus • Pinealoma may cause compression of cerebral aqueduct (obstructive hydrocephalus) • Precocious puberty may be observed in setting of pinealoma ≣ Item 1 of 1 Question ID: 0023 ◽" Mark ⟽ Previous ⟾ Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com A 55-year-old male with no known past medical history presents to the emergency department by paramedics after being found unconscious for an undetermined length of time. His initial glucose in the field was 28 mg/dL. The patient is managed acutely and admitted to the hospital. The following day a more formal history is attempted, however the patient repeatedly interrupts the physician stating, “everything looks blurry”. He appears to be generally disinterested in the conversation and displays inattentiveness throughout the interview. No tremors are noted. His BMI is approximately 15 kg/m2 with otherwise normal vital signs. Physical exam reveals horizontal nystagmus and significant postural ataxia. MRI of the brain and EEG are performed. EEG is unremarkable. Previous medical records reveal that he was admitted one month prior for an episode of acute pancreatitis and had previously reported living in a homeless shelter for the past year. During his last admission, there is no mention of disorientation or confusion. Which of the following findings on MRI would be most consistent with this patient’s presentation? ⚪ A. Diffuse atrophy of the frontal and temporal lobes bilaterally ⚪ B. Prominent cerebral sulci and ventriculomegaly ⚪ C. Pronounced atrophy of the caudate nucleus and ventriculomegaly ⚪ D. Pronounced atrophy of the mammillary bodies ⚪ E. Hyperintensity throughout the basal ganglia, temporal, and frontal cortices ≣ Item 1 of 1 Question ID: 0023 ◽" Mark ⟽ Previous ⟾ Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com A 55-year-old male with no known past medical history presents to the emergency department by paramedics after being found unconscious for an undetermined length of time. His initial glucose in the field was 28 mg/dL. The patient is managed acutely and admitted to the hospital. The following day a more formal history is attempted, however the patient repeatedly interrupts the physician stating, “everything looks blurry”. He appears to be generally disinterested in the conversation and displays inattentiveness throughout the interview. No tremors are noted. His BMI is approximately 15 kg/m2 with otherwise normal vital signs. Physical exam reveals horizontal nystagmus and significant postural ataxia. MRI of the brain and EEG are performed. EEG is unremarkable. Previous medical records reveal that he was admitted one month prior for an episode of acute pancreatitis and had previously reported living in a homeless shelter for the past year. During his last admission, there is no mention of disorientation or confusion. Which of the following findings on MRI would be most consistent with this patient’s presentation? ⚪ A. Diffuse atrophy of the frontal and temporal lobes bilaterally ⚪ B. Prominent cerebral sulci and ventriculomegaly ⚪ C. Pronounced atrophy of the caudate nucleus and ventriculomegaly " D. Pronounced atrophy of the mammillary bodies ⚪ E. Hyperintensity throughout the basal ganglia, temporal, and frontal cortices OUTLINE Neurology: Basal Ganglia 1. Anatomical Considerations ● ● ● ● ● ● A. Substantia Nigra B. Caudate Nucleus C. Putamen D. Globus Pallidus E. Lentiform Nucleus F. Striatum 2. Basal Ganglia Physiologic Circuits ● ● A. Direct Pathway B. Indirect Pathway 3. Disorders of the Basal Ganglia ● ● ● ● ● A. Huntington Disease B. Wilson Disease C. Hemiballismus D. Parkinson Disease E. Dystonia Neurology: Basal Ganglia Bootcamp.com https://commons.wikimedia.org/wiki/File:Human_brain_frontal_(coronal)_section_description_2.JPG https://commons.wikimedia.org/wiki/File:Brain_human_coronal_section.svg • • • • • Caudate nucleus Putamen Globus pallidus Lentiform nucleus Striatum Neurology: Basal Ganglia Bootcamp.com https://commons.wikimedia.org/wiki/File:Basal_ganglia_circuits.svg • • • • • Direct pathway à excitatory Indirect pathway à inhibitory Substantia nigra pars compacta à dopamine à net result ↑ motor activity Substantia nigra pars reticularis à GABA à net result ↓ motor activity Subthalamic nucleus à glutamate à net result ↓ motor activity Substantia nigra pars compacta D1 (+) striatum: direct pathway D2 (-) striatum: indirect pathway Both net result ↑ motor activity Neurology: Basal Ganglia Bootcamp.com https://radiopaedia.org/articles/huntington-disease • • • • • Huntington Disease: • Trinucleotide repeat expansion, CAG on huntingtin (HTT) gene on chromosome 4 • Autosomal dominant, anticipation, gain of function mutation • Caudate nucleus atrophy, ventriculomegaly • Chorea (hyperkinetic) à Bradykinesia (hypokinetic) • Late stage: Aggressive behavior, dementia, psychosis Wilson Disease: • Hepatolenticular degeneration (atrophy of lentiform nucleus) • Hepatic disease, neuropsychiatric changes • Kayser-Fleischer rings (slit-lamp) • Wing-beating tremor Hemiballismus: • Contralateral subthalamic nucleus lesion • Involuntary, flinging movements Parkinson Disease: • Substantia nigra degeneration • Bradykinesia, rigidity, resting tremor Dystonia: • Cervical dystonia (spasmodic torticollis) • Blepharospasm (uncontrollable blinking à closure of eyelids) • Acute iatrogenic dystonia (neuroleptics) ≣ Item 1 of 1 Question ID: 0024 ◽" Mark ⟽ Previous A 41-year-old female presents to her primary care physician for worsening memory loss. She states that she is concerned she may have Alzheimer’s dementia. Last week she states that she forgot her car keys in her vehicle. She reports that she had a fall episode recently as well, at which time she simply lost her balance while cooking dinner. She feels as if her arms “have a mind of their own”. She is noted to demonstrate involuntary, irregular movements of the upper limbs and writhing movements of the fingers. Nystagmus is also noted when performing testing of the extraocular muscles. L4 reflex is 3+ bilaterally. She is unaware of any family history of disease as she was adopted at a very young age. Which of the following structures is most likely to be affected given the patient’s presentation? ⟾ Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com https://commons.wikimedia.org/wiki/File:Human_brain_frontal_(coronal)_section_description_2.JPG A B C ⚪ A. ⚪ B. ⚪ C. ⚪ D. ⚪ E. D E ≣ Item 1 of 1 Question ID: 0024 ◽" Mark ⟽ Previous A 41-year-old female presents to her primary care physician for worsening memory loss. She states that she is concerned she may have Alzheimer’s dementia. Last week she states that she forgot her car keys in her vehicle. She reports that she had a fall episode recently as well, at which time she simply lost her balance while cooking dinner. She feels as if her arms “have a mind of their own”. She is noted to demonstrate involuntary, irregular movements of the upper limbs and writhing movements of the fingers. Nystagmus is also noted when performing testing of the extraocular muscles. L4 reflex is 3+ bilaterally. She is unaware of any family history of disease as she was adopted at a very young age. Which of the following structures is most likely to be affected given the patient’s presentation? ⟾ Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com https://commons.wikimedia.org/wiki/File:Human_brain_frontal_(coronal)_section_description_2.JPG A B C " A. ⚪ B. ⚪ C. ⚪ D. ⚪ E. D E OUTLINE Neurology: Neurotransmitter Activity in Psychiatric Disease 1. Dopaminergic Pathways ● ● ● ● A. Mesocortical B. Mesolimbic C. Tuberoinfundibular D. Nigrostriatal 2. Neurotransmitters in Psychiatric Disease ● ● ● ● ● A. Acetylcholine B. Serotonin C. Dopamine D. Norepinephrine E. GABA Neurology: Neurotransmitter Activity in Psychiatric Disease Bootcamp.com https://commons.wikimedia.org/wiki/File:Dopaminergic_pathways.svg • Mesolimbic: • Lesion à Positive symptoms of schizophrenia • Mesocortical: • Lesion à Negative symptoms of schizophrenia • Tuberoinfundibular: • Lesion à ↓ dopamine à ↑ prolactin • Nigrostriatal: • • Inhibition à Parkinsonism, extrapyramidal symptoms Stimulation à Chorea Neurology: Neurotransmitter Activity in Psychiatric Disease Bootcamp.com • Nucleus Basalis of Meynert: • Acetylcholine: ↑ Parkinson Disease : ↓ Alzheimer’s Dementia, Huntington's Disease • Substantia Nigra pars compacta, Arcuate nucleus: • Dopamine: ↑ Huntington disease, Schizophrenia (+ symptoms) : ↓ Parkinson Disease • Locus Coeruleus: • Norepinephrine: ↑ Anxiety : ↓ Depression • Raphe Nucleus: • Serotonin: ↑ Schizophrenia : ↓ Depression, Anxiety • Nucleus Accumbens: • GABA: ↓ Huntington’s Disease, Anxiety Schizophrenia Negative s/s: ↓ dopamine in Mesocortical pathway Positive s/s: ↑ dopamine in Mesolimbic pathway ≣ Item 1 of 1 Question ID: 0022 ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com A 26-year-old male is seen by his primary care physician with his spouse for an annual physical. His spouse reports that he began to demonstrate peculiar behavior approximately two months earlier that has now become increasingly concerning. She states that he had been stressed out from working more hours than usual. Initially, he was having difficulty sleeping and became paranoid of those around him. He repeatedly tried to convince her that he was receiving messages from a secret underground location and that he was engaged in intermittent discussions with a spy from another country. She states that he has recently begun talking to himself when alone. During the encounter he continues to repeat select phrases used by the physician and displays chaotic tangential speech. Which of the following is most consistent with the pattern of neurotransmitter activity in this patient’s central nervous system? ⚪ A. ↑ Norepinephrine, ↓ Dopamine ⚪ B. ↑ Norepinephrine, ↓ Serotonin ⚪ C. ↑ GABA, ↓ Dopamine ⚪ D. ↑ GABA, ↑ Serotonin ⚪ E. ↑ Serotonin, ↑ Dopamine ≣ Item 1 of 1 Question ID: 0025 ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com A 26-year-old male is seen by his primary care physician with his spouse for an annual physical. His spouse reports that he began to demonstrate peculiar behavior approximately two months earlier that has now become increasingly concerning. She states that he had been stressed out from working more hours than usual. Initially, he was having difficulty sleeping and became paranoid of those around him. He repeatedly tried to convince her that he was receiving messages from a secret underground location and that he was engaged in intermittent discussions with a spy from another country. She states that he has recently begun talking to himself when alone. During the encounter he continues to repeat select phrases used by the physician and displays chaotic tangential speech. Which of the following is most consistent with the pattern of neurotransmitter activity in this patient’s central nervous system? ⚪ A. ↑ Norepinephrine, ↓ Dopamine ⚪ B. ↑ Norepinephrine, ↓ Serotonin ⚪ C. ↑ GABA, ↓ Dopamine ⚪ D. ↑ GABA, ↑ Serotonin $ E. ↑ Serotonin, ↑ Dopamine OUTLINE Neurology: Dementia 1. Dementia Differential ● ● ● ● ● ● ● ● ● ● ● ● ● A. Alzheimer Dementia B. Parkinson Disease C. Vascular Dementia D. Frontotemporal Dementia E. Lewy Body Dementia F. Creutzfeldt-Jakob Disease G. Normal Pressure Hydrocephalus H. Hypothyroidism I. Major Depressive Disorder J. Neurosyphilis K. Vitamin B12 Deficiency L. Huntington Disease M. HIV-Associated Dementia Neurology: Dementia Bootcamp.com https://commons.wikimedia.org/wiki/File:Cerebral_amyloid_angiopathy_-2a-_amyloid_beta_-_high_mag.jpg https://upload.wikimedia.org/wikipedia/commons/3/3c/MRI_Location_Hippocampus_up..png https://commons.wikimedia.org/wiki/File:Tauopathy_in_Alzheimer%27s_disease.jpg https://upload.wikimedia.org/wikipedia/commons/a/af/Amyloidosis%2C_lymph_node%2C_polarizer.jpg • Pathophysiology: • • • • Histopathology: • • • • • Disproportionate hippocampal and/or temporoparietal lobe atrophy Generalized cortical atrophy +/- hydrocephalus ex vacuo Associations: • • Primary Early Finding: Progressively worsening short term memory loss Other findings: Executive dysfunction; visuospatial, behavioral and language impairment Imaging: • • • Senile plaques (Aβ + dystrophic neurites, extracellular) Stain positive with Congo red (apple-green birefringence) Neurofibrillary tangles (hyperphosphorylated tau protein, intracellular) Amyloid angiopathy Presentation: • • • Amyloid precursor protein (APP) gene on chromosome 21 β-amyloid plaques (Aβ)à neurotoxic ↓ ACh (nucleus basalis of Meynert) Cerebral amyloid angiopathy Management: • • Acetylcholinesterase inhibitors à Donepezil, Rivastigmine, Galantamine NMDA receptor antagonist à Memantine Neurology: Dementia • Pathophysiology: • • • • Histopathology: • • • Intracellular eosinophilic inclusions (!-synuclein) = Lewy bodies Predominantly observed in substantia nigra and locus coeruleus Presentation: • • • • Dopaminergic depletion in substantia nigra pars compacta ↑ Stimulation to Gpi à ↓ net motor movement ↑ Acetylcholine, ↓ Serotonin and norepinephrine Bradykinesia, rigidity (Cogwheel), resting tremor Imbalance and postural instability Shuffling gait Management: • • • • • • • Dopamine analog à Levodopa DOPA-decarboxylase (peripheral) inhibitor à Carbidopa Catechol-O-methyltransferase (COMT) inhibitors à Entacapone and tolcapone Dopamine agonist à Bromocriptine, pramipexole, and ropinirole Monoamine oxidase-B (MAO-B) inhibitor à Selegiline Anticholinergic à Benztropine and trihexyphenidyl Mix of targets à Amantadine Bootcamp.com MPTP Consumption: -Metabolite causes Parkinsonism -MPTP metabolized via MAO-B -Rx: Selegiline Iatrogenic -Typical antipsychotics: Haloperidol -Metoclopramide Neurology: Dementia • Pathophysiology: • • Primary Early Finding: Step-wise decline, executive dysfunction Other findings: Memory impairment, behavioral changes Asymmetric sensory or motor defects, homonymous hemianopia or quadrantopia, upper motor neuron signs Imaging: • • • Glial scar formation, cavitary lesions Presentation: • • • • Recurrent infarctions and cerebral ischemia Histopathology: • • Bootcamp.com Multiple cortical and/or lacunar infarcts with white matter lesions +/- hydrocephalus ex vacuo Associations: • • Small vessel à Significant cardiovascular and cerebrovascular risk factors (hypertension, hyperlipidemia, diabetes) Large vessel à Atrial fibrillation, patent foramen ovale Neurology: Dementia Bootcamp.com https://commons.wikimedia.org/wiki/File:Histology_of_frontotemporal_lobar_degeneration.jpg https://commons.wikimedia.org/wiki/File:Pick%27s_disease.png • Histopathology: • • Presentation: • • • • Cytoplasmic circular inclusions (hyperphosphorylated tau protein, Pick bodies) Primary Early Finding: Personality and behavioral changes Other findings: Disinhibition, hyperorality, compulsive behavior Memory deficits are minimal Imaging: • Frontotemporal atrophy Neurology: Dementia Bootcamp.com https://commons.wikimedia.org/wiki/File:Lewy_bodies_(alpha_synuclein_inclusions).svg Parkinson Disease vs Lewy Body Dementia • • • • Intracellular eosinophilic inclusions (!-synuclein) = Lewy bodies Located diffusely throughout the brain Presentation: • • • Parkinson Disease: Motor THEN Cognitive Lewy Body Dementia: Motor AND Cognitive Histopathology: Primary Early Finding: Fluctuating cognition, Parkinsonism, visual hallucinations Other Findings: Visuospatial and executive impairment Associations: • Increased sensitivity to antipsychotics REM Sleep Behavior Disorder ↓ REM sleep atonia à Dream enactment Possible early marker of PD or LBD Neurology: Dementia • Pathophysiology: • • • • Histopathology: • • Primary Early Finding: Rapidly progressive dementia + myoclonus Diagnostics: • • • Large intracytoplasmic vacuoles (spongiform) Presentation: • • PrPc = normal structure conformation of prion protein PrPSC = abnormal structure resistant to enzymatic breakdown PrPSC can convert PrPc à PrPSC ↑ 14-3-3 protein EEG: Triphasic periodic sharp waves Associations: • Iatrogenic (corneal or dural graft transplant) Bootcamp.com Neurology: Dementia • • • • • Bootcamp.com Normal Pressure Hydrocephalus: • Classic Triad: Gait ataxia (“magnetic gait”), urinary incontinence, dementia • Ventriculomegaly in or out of proportion to cortical atrophy (vs Hydrocephalus ex vacuo) • NPH: Ventriculomegaly tends to be the prominent finding • Hydrocephalus ex vacuo: Sulci enlargement and cortical atrophy tend to be the prominent findings • Symptomatic improvement with high-volume lumbar puncture and/or VP shunt Major Depressive Disorder: Reversible Causes of Dementia • Pseudodementia Major depressive disorder Thyroid disease • Normal neurologic evaluation and neuroimaging Neurosyphilis Vitamin B12 Deficiency: Vitamin B12 deficiency • Peripheral neuropathy, subacute combined degeneration Huntington Disease: • Trinucleotide repeat expansion, CAG on huntingtin (HTT) gene on chromosome 4 • Autosomal dominant, anticipation, gain of function mutation • Caudate nucleus atrophy, ventriculomegaly • Chorea (hyperkinetic) à Bradykinesia (hypokinetic) • Late stage: Aggressive behavior, dementia, psychosis HIV-Associated Dementia: • More common in severe disease (AIDS, CD4<200) • Progressive cognitive decline • Target: Microglial cells (phagocytes of CNS) • Multinucleated giant cells and microglial nodules ≣ Item 1 of 1 Question ID: 0026 ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com A 48-year-old female employed as an analytical chemist with no past medical history is seen in the emergency department for chemicalinduced keratitis. She is emergently seen by an ophthalmologist who performs a corneal graft transplantation of the affected eye. She tolerates the procedure well and is subsequently discharged from the hospital. Two weeks later she returns to the emergency department with her son who reports that she has been behaving erratically. She demonstrates involuntary, jerking movements of all four extremities that are worsened by loud noises. A CT scan of the head and MRI are relatively unrevealing. Lumbar puncture is performed revealing an increase in S100 and 14-3-3 protein. Which of the following would be most consistent with the findings observed on a brain specimen of this patient? ⚪ A. Diffuse extracellular neuritic plaques scattered throughout the gray matter ⚪ B. Intracellular rod-shaped eosinophilic aggregates in the hippocampus ⚪ C. Intracytoplasmic vacuoles within neurons of the cerebral cortex ⚪ D. Liquefactive necrosis and cystic cavity formation localized to the internal capsule ⚪ E. Significant depletion of dopaminergic neurons within the substantia nigra pars compacta ≣ Item 1 of 1 Question ID: 0026 ◽" Mark ⟽ ⟾ Previous Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com A 48-year-old female employed as an analytical chemist with no past medical history is seen in the emergency department for chemicalinduced keratitis. She is emergently seen by an ophthalmologist who performs a corneal graft transplantation of the affected eye. She tolerates the procedure well and is subsequently discharged from the hospital. Two weeks later she returns to the emergency department with her son who reports that she has been behaving erratically. She demonstrates involuntary, jerking movements of all four extremities that are worsened by loud noises. A CT scan of the head and MRI are relatively unrevealing. Lumbar puncture is performed revealing an increase in S100 and 14-3-3 protein. Which of the following would be most consistent with the findings observed on a brain specimen of this patient? ⚪ A. Diffuse extracellular neuritic plaques scattered throughout the gray matter ⚪ B. Intracellular rod-shaped eosinophilic aggregates in the hippocampus $ C. Intracytoplasmic vacuoles within neurons of the cerebral cortex ⚪ D. Liquefactive necrosis and cystic cavity formation localized to the internal capsule ⚪ E. Significant depletion of dopaminergic neurons within the substantia nigra pars compacta OUTLINE Neurology: Headache 1. Headache Differential ● ● ● ● ● A. Tension Headache B. Migraine C. Cluster Headache D. Idiopathic Intracranial Hypertension E. Trigeminal Neuralgia Neurology: Headache • Presentation: • • • • • • Triggers: • • Stress #1, lack of sleep, anxiety Associations: • • • Band-like, bilateral “achy, tight, or dull”, “vice-like” headache Classically bifrontal Musculoskeletal tenderness No neurologic symptoms Duration: Variable Women > Men Generally, no genetic predisposition Management: • NSAIDs and/or conservative Bootcamp.com Neurology: Headache Bootcamp.com https://commons.wikimedia.org/wiki/File:ScintillatingScotoma3.jpg • Pathophysiology • • • Presentation: • • • • • Alcohol, nicotine, stress, poor sleeping habits Associations: • • • Unilateral, ”throbbing, pulsating” headache +/- Aura à reversible neurologic symptoms +/- Photophobia, nausea, emesis Duration: 4-72 hours Triggers: • • ↑ CNS excitability à abnormal activation of trigeminal fibers à ↑ CGRP Calcitonin gene-related peptide: Vasodilation and inflammatory response Women > Men Genetic predisposition Migraine POUND: Pulsatile One day of duration Unilateral Nausea, emesis Debilitating Acute Management: • • Sumatriptan: 5-HT1B/1D agonist à Inhibition of CGRP, vasoconstriction Ergotamine, Dihydroergotamine: 5-HT1B/1D activity + !-adrenergic activity à vasoconstriction Neurology: Headache • Presentation: • • • • • • Triggers: • • Clustered in similar times daily, +/- during sleep Associations: • • • • Severe acute onset, “sharp” unilateral periorbital and temporal headache Ipsilateral autonomic symptoms (nasal congestion, lacrimation, rhinorrhea, miosis) No aura Duration: <3 hours, multiple attacks per day Repeating in “clusters”, cyclical association between attacks Men > Women Tobacco use +/- Genetic predisposition Acute Management: • • Oxygen, 100% FiO2 Sumatriptan: 5-HT1B/1D agonist à Inhibition of CGRP, vasoconstriction Bootcamp.com Neurology: Headache Bootcamp.com https://commons.wikimedia.org/wiki/File:Fundus_photograph_of_normal_left_eye.jpg https://commons.wikimedia.org/wiki/File:Papilledema.jpg • Presentation: • • • • • • Associations: • • • Young, obese female Frequent non-localized headaches Signs of ↑ ICP à Bilateral symmetric papilledema, lateral rectus palsy Pulsatile tinnitus Transient visual disturbances and/or diplopia Women > Men Vitamin A Management: • • • MRI à Generally unremarkable LP à ↑ opening pressure, diagnostic and therapeutic Acetazolamide: Carbonic anhydrase inhibitor Neurology: Headache • Presentation: • • • • • Triggers: • • Older patient (55-70 years of age) Unilateral, severe, sudden onset, “shooting or stabbing”, “electric shock” pain V2 and V3 distributions classically affected Duration: Several seconds, recurring many times throughout the day Talking, chewing, touch Management: • • MRI à Generally unremarkable Carbamazepine: Inactivation of depolarizing Na+ channels Bootcamp.com Neurology: Headache Bootcamp.com High Yield Headache Disease Process Classic Presentation Duration Neurologic Symptoms Key Associations Acute Management Preventative/Chronic Management Tension Headache Band-like Bilateral “Achy”, “tight”, or “dull” “Vice-like” headache Variable None, no aura n/a NSAIDs and/or conservative Avoid precipitating factors Migraine “Throbbing, pulsating” Unilateral Nausea 4-72 hours +/- Aura Photophobia Women Genetic predisposition Sumatriptan Ergotamine β-blocker TCA Topiramate (low yield) Cluster Headache ”Sharp” unilateral, periorbital Repeating in “clusters” Cyclical association between attacks (similar times daily) <3 hours No aura Ipsilateral autonomic symptoms Men Tobacco use Oxygen 100% FiO2 Sumatriptan Verapamil (low yield) Idiopathic Intracranial Hypertension Non-localized Signs of ↑ ICP (ex. Papilledema) Variable Pulsatile tinnitus Diplopia (ex. Lateral rectus palsy) Women (Young, obese) Vitamin A Therapeutic high volume lumbar puncture Acetazolamide n/a Trigeminal Neuralgia Sudden onset Localized to V2 and V3 distribution “Electric”, “shock-like” “Shooting” or “stabbing” Worse with talking, chewing, and shaving Seconds n/a > Age (55*-70) n/a to Step 1 Carbamazepine Keep in mind: Test writers may use adjectives such as “sharp” to describe a migraine headache in a question stem. Classic descriptions are not pathognomonic. ≣ Item 1 of 1 Question ID: 0027 ◽" Mark ⟽ Previous ⟾ Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com https://commons.wikimedia.org/wiki/File:Fundus_photograph_of_normal_right_eye.jpg A 34-year-old female with a past medical history of generalized anxiety disorder presents to the emergency department for a headache that has been ongoing for the past 2 hours. The patient reports that she was in a meeting at her office when she suddenly saw “stars” and felt her left arm go numb. She initially thought she may be having a stroke, however her symptoms resolved within five minutes. Shortly thereafter she developed a left-sided 8/10 throbbing headache. She has been unable to eat due to significant nausea. She requests that the lights remain dimmed in the room. Her grandmother has a history of recurrent headaches with no other significant family history. Oral contraceptives are the only prescribed medication that she is currently taking. Vital signs and fundoscopy are shown below. Physical examination is unremarkable. Temperature: 98F (36.7C) Blood Pressure: 130/62 Heart Rate: 104/min Respiratory Rate: 12/min Oxygen Saturation: 100% on room air Non-contrast head CT is unremarkable. A serotonin agonist is prescribed to acutely manage the severity of this patient’s headache. Which mechanism of action is most likely consistent with the medication prescribed? ⚪ A. ⚪ B. ⚪ C. ⚪ D. ⚪ E. Inhibition of enzymatic carbonic anhydrase Binding to inactive voltage-gated sodium channels in cortical tissue Inhibition of calcitonin gene-related peptide release from trigeminal afferent neurons Stimulation of trigeminal afferent neuronal fibers to release substance P Intracranial vessel vasodilation secondary to binding of target receptors on smooth muscle tissue ≣ Item 1 of 1 Question ID: 0027 ◽" Mark ⟽ Previous ⟾ Next Test Your Knowledge Difficulty: ✪✪ Bootcamp.com https://commons.wikimedia.org/wiki/File:Fundus_photograph_of_normal_right_eye.jpg A 34-year-old female with a past medical history of generalized anxiety disorder presents to the emergency department for a headache that has been ongoing for the past 2 hours. The patient reports that she was in a meeting at her office when she suddenly saw “stars” and felt her left arm go numb. She initially thought she may be having a stroke, however her symptoms resolved within five minutes. Shortly thereafter she developed a left-sided 8/10 throbbing headache. She has been unable to eat due to significant nausea. She requests that the lights remain dimmed in the room. Her grandmother has a history of recurrent headaches with no other significant family history. Oral contraceptives are the only prescribed medication that she is currently taking. Vital signs and fundoscopy are shown below. Physical examination is unremarkable. Temperature: 98F (36.7C) Blood Pressure: 130/62 Heart Rate: 104/min Respiratory Rate: 12/min Oxygen Saturation: 100% on room air Non-contrast head CT is unremarkable. A serotonin agonist is prescribed to acutely manage the severity of this patient’s headache. Which mechanism of action is most likely consistent with the medication prescribed? ⚪ A. ⚪ B. $ C. ⚪ D. ⚪ E. Inhibition of enzymatic carbonic anhydrase Binding to inactive voltage-gated sodium channels in cortical tissue Inhibition of calcitonin gene-related peptide release from trigeminal afferent neurons Stimulation of trigeminal afferent neuronal fibers to release substance P Intracranial vessel vasodilation secondary to binding of target receptors on smooth muscle tissue OUTLINE Neurology: Seizures 1. Overview ● ● ● ● A. Classification B. Epilepsy C. General Terms D. Triggers and Inciting Causes 2. Focal Seizure ● ● A. Focal Aware B. Focal Impaired Awareness 3. Generalized Onset Seizure ● ● ● ● ● A. Absence B. Tonic-Clonic C. Myoclonic D. Atonic E. Simple Febrile 4. Status Epilepticus ● ● A. Definition B. Management 5. Antiepileptic Medications ● ● ● A. Narrow Spectrum B. Broad Spectrum C. Other/Varied Neurology: Seizure • Seizure Classification: • • • • Epilepsy: • • • Ictal: Occurring during the time of seizure Post-ictal: Occurring after the time of seizure Triggers à Reflex: • • • • ≥2 unprovoked separated by >24 hours 1 seizure with high risk for subsequent seizure General Terms: • • • Unprovoked: No clear etiology Reflex: Trigger that predisposes to seizure risk (↓ seizure threshold) Provoked: Concurrent with systemic illness or central nervous system pathology Flashing lights High fever (infants and young children) Lack of sleep Inciting Causes à Provoked: • • • Cerebrovascular accident Traumatic brain injury Electrolyte imbalance Bootcamp.com Neurology: Seizure • Origin: • • • Focal Aware (Simple Partial): • • • Awareness and consciousness remains intact No post-ictal state Focal Impaired Awareness (Complex Partial): • • • • • Single hemisphere (à +/- global generalization) Localized symptoms at onset Awareness impaired, ”blank stare” Post-ictal state (common) à Todd paralysis Automatisms Common origin à Temporal lobe Etiology: • #1 Focal cerebral lesion Bootcamp.com Frontal: Jerking movement of contralateral extremity Temporal: Auditory hallucinations Parietal: Numbness of contralateral extremity Occipital: Visual hallucinations Jacksonian March: Spread of abnormal electrical activity to nearby areas of the motor cortex Focal Seizure Presentation à Contralateral Face or Limb Automatisms Myoclonus Tonic and/or clonic Contractions Sensory disturbances Behavioral changes Neurology: Seizure • • • • • Origin: • Global generalization • Generalized symptoms at onset Absence: • Loss of consciousness, “blank stare” for short intervals (~ 5-15 seconds) • Generally, no post-ictal state, consciousness returns immediately following ictal-state • Child or adolescent • EEG à 3-Hz spike-wave complex • First-line Rx: Ethosuximide Tonic-Clonic (grand mal): • Loss of consciousness • Post-ictal state (common) • Bilateral muscle contractions (tonic) and rhythmic twitching (clonic) • “Eyes rotate to the back of the head” • Lateral tongue lacerations • Urinary or stool incontinence • First-line Rx: Broad-spectrum AEDs (e.g., Levetiracetam) Myoclonic: • Nonrhythmic jerking movements • No loss of consciousness, no post-ictal state Atonic: • “Drop seizure” • Acute onset diffuse loss of muscle tone Bootcamp.com Neurology: Seizure • Pathophysiology: • • Presentation: • • • • • Significant fever (>104F) 6 months to 5 years of age Simple Febrile Seizure: Brief generalized, nonrecurring seizure Complex Febrile Seizure: Long lasting focal at onset, recurring seizure Associations: • • • Hyperthermia à ↑ CSF cytokines/interleukins Viral infection: Classic cause = Roseola à HHV-6 Genetic predisposition Management: • • Simple febrile seizure: Conservative NSAIDs, acetaminophen à ↓ PGE2 à ↓ Central hypothalamic temperature setpoint Bootcamp.com Neurology: Seizure • Definition: • • • Single seizure, ≥5 minutes Multiple seizures, incomplete level of consciousness regained between each episode Management: • • Abort seizure: Intravenous benzodiazepines à GABAA agonists à hyperpolarizing Prevention of recurrence: Intravenous phenytoin Bootcamp.com Neurology: Seizure Bootcamp.com https://commons.wikimedia.org/wiki/File:Gingivitis_(crop).jpg • • • Valproate: Adverse effects: Neural tube defects Levetiracetam: Binds SV2A à modulation of glutamate and GABA release Lamotrigine: Adverse effects: Stevens-Johnson syndrome • Phenobarbital: • Primary use: Neonatal seizure • MOA: GABA-A agonist, ↑ duration of chloride channel opening • Cytochrome P450 inducer Lorazepam: • Primary use: Abort acute seizure activity and status epilepticus • MOA: GABA-A agonist, ↑ frequency of chloride channel opening • • Other • • Broad Fetal Hydantoin Syndrome Fingernail hypoplasia Excess hair production Intrauterine growth restriction Phenytoin: • MOA: Inhibition of pre-synaptic voltage-gated sodium channels • Adverse effects: Teratogenic, gingival hyperplasia, hirsutism • Cytochrome P450 inducer, zero order elimination Carbamazepine: • Primary use: Focal seizures and trigeminal neuralgia • MOA: Inhibition of pre-synaptic voltage-gated sodium channels • Cytochrome P450 inducer (strong) • Adverse effects: SJS, Aplastic anemia, teratogenic Gabapentin: Inhibition of pre-synaptic voltage-gated calcium channels Ethosuximide: Inhibition of voltage-gated T-type calcium channels in thalamus Narrow • ≣ Item 1 of 1 Question ID: 0028 ◽" Mark ⟽ Previous ⟾ Next Test Your Knowledge Difficulty: ✪✪ A 6-year-old female with no significant past medical history is seen by her pediatrician for worsening academic performance. Her father is convinced that she has attention deficit disorder. He references three occasions of which he was contacted by his daughter’s teacher to inform him of her “day-dreaming”. He also states that she stares off into the distance when playing with her friends outside. The patient has no history of missed milestones and height, and weight are within the appropriate reference ranges for her age. Her temperature is 98F (36.7C) with otherwise unremarkable vital signs. On physical examination no focal neurologic deficits are appreciated. Tongue lacerations are absent. Electroencephalography is performed in the setting of hyperventilation. The results are shown below. A medication is prescribed by her pediatrician. Which mechanism of action is most likely consistent with the medication prescribed? ⚪ A. ⚪ B. ⚪ C. ⚪ D. ⚪ E. ⚪ F. Reversible inhibition of cyclooxygenase-1 enzymes Increase in frequency of chloride channel opening Increase in duration of chloride channel opening Inhibition of inactivated sodium channels Selective norepinephrine reuptake inhibitor Inhibition of thalamic T-type calcium channels Bootcamp.com https://commons.wikimedia.org/wiki/File:Spike-waves.png ≣ Item 1 of 1 Question ID: 0028 ◽" Mark ⟽ Previous ⟾ Next Test Your Knowledge Difficulty: ✪✪ A 6-year-old female with no significant past medical history is seen by her pediatrician for worsening academic performance. Her father is convinced that she has attention deficit disorder. He references three occasions of which he was contacted by his daughter’s teacher to inform him of her “day-dreaming”. He also states that she stares off into the distance when playing with her friends outside. The patient has no history of missed milestones and height, and weight are within the appropriate reference ranges for her age. Her temperature is 98F (36.7C) with otherwise unremarkable vital signs. On physical examination no focal neurologic deficits are appreciated. Tongue lacerations are absent. Electroencephalography is performed in the setting of hyperventilation. The results are shown below. A medication is prescribed by her pediatrician. Which mechanism of action is most likely consistent with the medication prescribed? ⚪ A. ⚪ B. ⚪ C. ⚪ D. ⚪ E. $ F. Reversible inhibition of cyclooxygenase-1 enzymes Increase in frequency of chloride channel opening Increase in duration of chloride channel opening Inhibition of inactivated sodium channels Selective norepinephrine reuptake inhibitor Inhibition of thalamic T-type calcium channels Bootcamp.com https://commons.wikimedia.org/wiki/File:Spike-waves.png OUTLINE Neurology: Traumatic Brain Injury and Herniation 1. Diffuse Axonal Injury ● ● ● ● A. Etiology B. Pathophysiology C. Histopathology D. Imaging 2. Intracranial Hypertension ● ● ● ● ● A. Classic Etiologies B. Cushing Reflex C. Signs of Increased Intracranial Pressure D. Imaging Findings E. Management 3. Brain Herniation ● ● ● A. Uncal (Transtentorial) Herniation B. Subfalcine (Cingulate) Herniation C. Tonsillar Herniation 4. Decerebrate vs Decorticate Posturing ● ● ● A. Decerebrate Posturing B. Decorticate Posturing C. Absence of Motor Tone Neurology: Traumatic Brain Injury and Herniation Bootcamp.com https://commons.wikimedia.org/wiki/File:Diffuse_axonal_injury-_cMRT_nach_3_Tagen.jpg https://commons.wikimedia.org/wiki/File:Contrecoup.svg • Etiology: • • • • Widespread shearing of white matter tracts Histopathology: • • • Coup-contrecoup injury, extreme rotational acceleration/deceleration forces Motor vehicle accidents Penetrating and blast trauma Pathophysiology: • • Initial diagnostics in TBIà Head CT Axonal bulb formation (diffuse axonal edema) Accumulation of axonal transport proteins Imaging: • • Head CT scan: Generally unremarkable Brain MRI: Diffuse punctate hemorrhages at the site of the gray-white matter junction and corpus callosum Neurology: Traumatic Brain Injury and Herniation Bootcamp.com CPP = MAP - ICP • • • • • Classic Etiologies: • Mass lesion (brain tumor, aneurysm, hematoma) • Idiopathic intracranial hypertension • Hydrocephalus • Intracranial hemorrhage Cushing Reflex: • Hypertension (↑ MAP) • Bradycardia • Irregular respirations à Respiratory depression Signs of ↑ Intracranial Pressure • Bilateral papilledema • Lateral rectus palsy • Ipsilateral fixed, dilated pupil, “down and out” eye +/- ptosis • Bulging fontanelle (infants) Imaging Findings: • Active hemorrhage, midline shift • Ventriculomegaly Management: • Hyperventilation (↓PaCO2 à vasoconstriction à ↓ cerebral blood volume) • Elevate head of the bed • Intravenous mannitol Neurology: Traumatic Brain Injury and Herniation Bootcamp.com https://commons.wikimedia.org/wiki/File:Brain_herniation_types-2.svg • Uncal (Transtentorial) Herniation: • • • • • Subfalcine (Cingulate) Herniation: • • • • Medial temporal lobe beneath tentorium cerebelli Initial Sign: Ipsilateral fixed, dilated pupil (CN III) à “down and out” positioning +/- ptosis Ipsilateral and/or contralateral weakness (cerebral peduncle) Contralateral homonymous hemianopia with macular sparing or blindness (PCA) Cingulate gyrus under falx cerebri Contralateral lower extremity weakness (ACA territory) Obstructive hydrocephalus (foramen of Monro) Tonsillar Herniation: • • Classic Cause: Chiari malformations Obstructive hydrocephalus (cerebral aqueduct) Neurology: Traumatic Brain Injury and Herniation Bootcamp.com https://commons.wikimedia.org/wiki/File:Decorticate.PNG https://commons.wikimedia.org/wiki/File:Decerebrate.jpg • Decorticate (Flexor) Posture: • • • Decerebrate (Extensor) Posture: • • • Lesion to neural tissue above the red nucleus ↑ neuronal activity to the upper limb flexors (Flexors > Extensors) Lesion to neural tissue below the red nucleus ↓ neuronal activity to the upper limb flexors (Flexors < Extensors) Absence of Motor Tone: • Classic Cause: Cervical spinal cord injury ≣ Item 1 of 1 Question ID: 0029 ◽" Mark ⟽ Previous ⟾ Next Test Your Knowledge Difficulty: ✪✪ A 67-year-old female is brought to the emergency department by paramedics following acute onset right-sided lower extremity weakness and numbness. The patient has a past medical history of chronic hypertension, iatrogenic hypothyroidism, and atrial fibrillation. A list of medications is provided by the patient’s spouse including lisinopril, levothyroxine, and rivaroxaban. The patient’s spouse states that she was in her usual state of health this morning but has become increasingly confused en route to the hospital. Vitals signs are shown below. An emergent non-contrast CT of the head is performed and shown. An immediate neurosurgical consultation is placed. Temperature: 99.0 F (37.2 C) Blood pressure: 170/68 mmHg Heart rate: 58/min Respirations: 10/min Oxygen saturation: 99% on room air Glasgow coma scale: 12 Which of the following best explains the cause of neurologic deficit in this patient? ⚪ A. ⚪ B. ⚪ C. ⚪ D. ⚪ E. Widespread cerebral hypoperfusion Hemispheric herniation inferior to the falx cerebri Diffuse shearing of white matter tracts Localized shearing of cortical bridging veins Acute high-impact fracture to the left pterion Bootcamp.com https://commons.wikimedia.org/wiki/File:Subfalcine-herniation-001.jpg ≣ Item 1 of 1 Question ID: 0029 ◽" Mark ⟽ Previous ⟾ Next Test Your Knowledge Difficulty: ✪✪ A 67-year-old female is brought to the emergency department by paramedics following acute onset right-sided lower extremity weakness and numbness. The patient has a past medical history of chronic hypertension, iatrogenic hypothyroidism, and atrial fibrillation. A list of medications is provided by the patient’s spouse including lisinopril, levothyroxine, and rivaroxaban. The patient’s spouse states that she was in her usual state of health this morning but has become increasingly confused en route to the hospital. Vitals signs are shown below. An emergent non-contrast CT of the head is performed and shown. An immediate neurosurgical consultation is placed. Temperature: 99.0 F (37.2 C) Blood pressure: 170/68 mmHg Heart rate: 58/min Respirations: 10/min Oxygen saturation: 99% on room air Glasgow coma scale: 12 Which of the following best explains the cause of neurologic deficit in this patient? ⚪ A. $ B. ⚪ C. ⚪ D. ⚪ E. Widespread cerebral hypoperfusion Hemispheric herniation inferior to the falx cerebri Diffuse shearing of white matter tracts Localized shearing of cortical bridging veins Acute high-impact fracture to the left pterion Bootcamp.com https://commons.wikimedia.org/wiki/File:Subfalcine-herniation-001.jpg