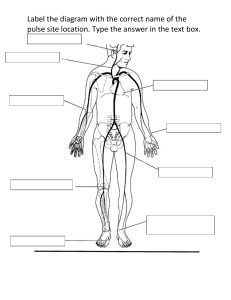
lOMoARcPSD|14725619 305 Exam 1 Review - Blueprint and notes for exam 1 Primary Care Health Assessment (Felician University) Studocu is not sponsored or endorsed by any college or university Downloaded by Jennifer Rangel (jennifer.renee.rangel6@gmail.com) lOMoARcPSD|14725619 NURS 305 Exam 1 - Review Module 1: QSEN, Evidence Based Practice, IOM, Healthy People 2020, Nursing Process Healthy people 2020- agencies, health disparities -CDC launched by Department of Health and Human Services (HHS) and Office of Disease Prevention and Health Promotion (ODPHP) in 2010 4 goals: 1. High quality, longer lives free of preventable disease, disability, injury, and premature death, 2. Health equity, eliminate disparities, and improve health of all groups, 3. Social and physical environment that promotes good health for all, 4. Quality of life, healthy development, and health behaviors across all life stages -health disparities: If a health outcome is seen to a greater or lesser extent between populations, there is disparity Examples: race or ethnicity, sex, sexual identity, age, disability, socioeconomic status, and geographic location all contribute to an individual's ability to achieve good health IOM- (2008) Robert Wood Johnson Foundation (RWJF) approached the Institute of Medicine (IOM) to propose a partnership to transform the nursing profession. 2-Year initiative created on the Future of Nursing Key messages: 1. Nurses should practice to the full extent of their education and training Barriers of nurses continuing education: fragmentation of the health care system, high rates of turnover among nurses, difficult to transition from school to practice and aging workforce. 2002; The Joint Commision developed nurse residency programs to ensure a better school-practice transition 2.Nurses should achieve higher levels of education and training through an improved education system that promotes seamless academic progression. Improved education system is necessary to ensure that current/future generations of nurses can deliver safe, quality, patient-centered care. Increase diversity, gender, race, ethnicity, and culturally relevant care 3.Nurses should be full partners with physicians and other health professionals, in redesigning health care in the U.S. Full partner: taking responsibility for identifying problems/areas of waste, devising/implementing a plan of improvement, tracking improvement, and adjustments. Nurses should serve on advisory committees. Nurses must see policy as something they can shape rather than something that happens to them 4.Effective workforce planning and policy making require better data collection and an improved information infrastructure. Lack of data of the numbers/types of health professionals employed, where they work, what roles, and what activities they perform Downloaded by Jennifer Rangel (jennifer.renee.rangel6@gmail.com) lOMoARcPSD|14725619 Gordon’s Functional health patterns- Developed by Marjory Gordon, Method used by nurses in the nursing process to provide a comprehensive nursing assessment of the patient. Taxonomy II of NANDA Nursing Diagnosis classification is based on Gordon's functional health patterns. 11 Categories : 1.Health Perception - Health Management Pattern- Describes client's perceived pattern of health and well-being and how health is managed. 2. Nutritional - Metabolic Pattern-Describes pattern of food and fluid consumption relative to metabolic need and pattern indicators of local nutrient supply . 3.Elimination Pattern-Describes pattern of excretory function (bowel, bladder) 4.Activity - Exercise Pattern- Describes pattern of exercise, activity, leisure, and recreation. 5.Cognitive - Perceptual Pattern- Describes sensory, perceptual, and cognitive pattern 6.Sleep - Rest Pattern- Describes patterns of sleep, rest, and relaxation. 7.Self-perception - Self-concept Pattern- Describes self-concept and perceptions of self (body comfory, image, feeling state) 8. Role - Relationship Pattern- Describes pattern of role engagements and relationships. 9..Sexuality - Reproductive Pattern- Describes client's pattern of satisfaction and dissatisfaction with sexuality pattern,Describes reproductive patterns. 10.Coping - Stress Tolerance Pattern, Describes general coping patterns and effectiveness of the pattern in terms of stress tolerance. 11.Value - Belief Pattern- Describes pattern of values and beliefs, including spiritual and /or goals that guide choices or decisions. EBP -Evidence-Based Practice- The conviction that all patients be treated with the most up to date practices -1.Ask the clinical question, 2.Acquire sources of evidence, 3.Appraise and synthesize evidence, 4.Apply relevant evidence in practice 5.Assess the outcomes Nursing process- all 5 steps Assessment, Diagnosis, Outcome Planning, Implementation, Evaluation Module 2: Standard Precautions, Handwashing, Prioritization, and Documentation Handwashing techniques and policies & protocols Wash your hands before and after every physical patient encounter, After contact with blood, body fluids, secretions, and excretions, After any equipment contaminated with body fluids, Downloaded by Jennifer Rangel (jennifer.renee.rangel6@gmail.com) lOMoARcPSD|14725619 After removing gloves, & Using alcohol-based hand sanitizer takes less time than using soap and water and kills more organisms more quickly/less damaging to the skin Patient satisfaction The HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) What is the hospital consumer assessment of healthcare providers and systems? survey is the first national, standardized, publicly reported survey of patients' perspectives of hospital care Advance directives -power of attorney- a type of advance directive in which you name a person to make decisions for you when you are unable to do so -living will-a written, legal document that spells out medical treatments you would and would not want to be used to keep you alive, as well as your preferences for other medical decisions, such as pain management or organ donation. -DNR- tell your doctor about your preferences. He or she will write the orders and put them in your medical record -changing advanced directives -You can change your directives at any time Meeting your client- general interview: therapeutic communication skills, barriers to communication -Meeting client- general interview: therapeutic communication skills, barriers to communication -Interview- 1st point of contact with a client to collect Subjective Data. The object is not to collect objective data, but you will collect some such as positive physical appearance, ability to carry conversation, and demeanor, Contract- the interview is your contract between you and the client. Needs and expectations from health care/ what you have to offer -Therapeutic communication skills- Equal-Status Seating: comfortably seated at eye level, Introduce yourself: give reason for interview & Open-Ended and Closed/Direct Questions -Barriers-Lack of privacy, Background noise & Nonverbal skills The health history form -biographic data, Name, address, phone number, age, birthdate, birthplace, gender, relationship status, race, ethnic origin, and occupation Downloaded by Jennifer Rangel (jennifer.renee.rangel6@gmail.com) lOMoARcPSD|14725619 -source of history- who is giving you the information -reason for seeking care- reasons for visit in patients words -present health or history of present illness- Location, Character or Quality, Quantity or Severity, Timing (onset, duration, frequency), Setting, Aggravating or Relieving Factors, Associated Factors, and Patient's Perception (PQRSTU) -past health- previous exp with illness -family history- disease patient may be at increase risk for developing -review of systems & functional assessment- evaluate the past and present health state of each body system, to double-check in case any significant data was omitted in the Present Illness section, and to evaluate health promotion practices Functional assessment- Including Activities of Daily Living): measures a person's self-care ability in the areas of general physical health- ADLs such as bathing, dressing, toileting, eating, walking Assessment equipment stethoscopt, otoscope, ophthalmoscope, platform scale with height, sphygomomanometer, thermometer, pulse oximeter,flashlight/penlight Stethoscope -auscultation (diaphragm and bell) Diaphragm -high-pitched sounds (breathing, bowels, normal heart sounds) Bell -soft, low-pitched sounds (extra heart sounds or murmurs) Blood pressure -force exerted on the wall of the artery creating pressure of blood flow, results in the sounds heard with a stethoscope Systolic -the first distinct sound heard during contraction, when blood is ejercted from the heart Pulse pressure -the difference between systolic and diastolic pressure Diastolic pressure -the last sound heard on auscultation of a blood pressure signifying the relaxation phase of the circulatory status. Brachial pulse -artery located at the brachial/anticubital fossa Bradycardia -heart rate fewer than 50 or 60 beats per minute in the adult Inspection- always comes 1st, observing Palpation- fingertips, assess texture/ temp/ moisture/ organ location and size/ swelling/ vibration Percussion- Tapping on skin with short sharp strokes/ map out location/ density/ abnorm mass Auscultation- listening to sounds (usually stethoscope) Module 3: General Survey and Measurement, Vital signs, and Pain Management: Nursing process and pain management- plan of care for pain Two main pathways: Nociceptive and/or neuropathic processing Downloaded by Jennifer Rangel (jennifer.renee.rangel6@gmail.com) lOMoARcPSD|14725619 Pain can be classified by its duration Acute Chronic (persistent)Duration provides information r/t underlying mechanisms and treatment decisions. Proper vital sign techniques and how to trouble shoot: normal adult values T, P, Bp, RR, Pain Temperature- 37.2 C/ 99 F (Influence by : age/ exercise/ menstrual/ diurnal cycle) - Oral/ rectal/ tempanic Pulse: stoke volume goes in the aorta (70 ml) Rate: 50- 95 beat per min Rhythm- norm = regular even tempo/ Sinus dysrhythmia: one irregularity commonly found in children and young adults Force/ strength : Force of pulse is strength of heart’s stroke volume. Weak, thready pulse reflects a decreased stroke volume (e.g., as occurs with hemorrhagic shock). Full, bounding pulse denotes increased stroke volume, as with anxiety, exercise, and some abnormal conditions. Pulse force recorded using three-point scale • 3+ Full, bounding • 2+ Normal • 1+ Weak, thready • 0 Absent Respirations: ratio about 4:1 pulse to resp rate (12-20 beats per min) Blood Pressure: Blood pressure (BP) is force of blood pushing against side of its container, vessel wall. Strength of push changes with event in cardiac cycle. Systolic pressure: maximum pressure felt on artery during left ventricular contraction, or systole Diastolic pressure: elastic recoil, or resting, pressure that blood exerts constantly between each contraction Pulse pressure: difference between systolic and diastolic • Reflects stroke volume Mean arterial pressure (MAP): pressure forcing blood into tissues, averaged over cardiac cycle (65) Kortocoff sounds: Phases of sound: I through V Note first appearance of sound. Hear muffling of sound. Hear final disappearance of sounds. Physical assessment- general survey- what are you looking at? For? The general survey is a study of the whole person Covers general health state and any obvious physical characteristics Provides an overall impression Includes objective parameters that apply to the whole body Includes areas of physical appearance, body structure, mobility, and behavior Objective Data: Downloaded by Jennifer Rangel (jennifer.renee.rangel6@gmail.com) lOMoARcPSD|14725619 Age /sex/ level consciousness/ skin color/ facial features/ overall app/ body structure/ mobility (gait?)/ behavior(mood/ speech/ dress)/ measurement Module 4: Assessment of Eyes and Ears Different methods for assessment visual acuity What is the PERRLA? Pupils Equal, Round, Reactive to Light and Accommodation What is the Snellen chart? (CN2) Most common for visual acuity Tests central visual acuity -most common abnormalities include myopia (nearsightedness) or hyperopia (farsightedness) What is the Hirschberg test? (CN 4) tests corneal light reflex -parallel alignment of eyes -Patient stares straight ahead, as you hold light 30 in away from face Six cardinal positions of gaze (CN 3,4,6) Inspection of Ocular Fundus: Equipment is needed to conduct proper eye exams Snellen Eye Chart -handheld visual screener -opaque card -penlight -ophthalmoscope Specific conditions of Eyes and Ears: Chalazion, Dacryocystitis, Blepharitis, Hordeolum, vertigo, Tinnitus, Otorrhea, Otalgia What is chalazion? nodule, looks like stye, but not on lid edge and it not infection What is dacryocystisis? infection of the tear (lacrimal) sac and is caused by blockage of nasolacrimal duct What is blepharitis? inflammation of the eyelids --> red, itrritated , and itchy--> forms dandruff like scales around eyelashed What is hordeolum? commonly called a "stye" and is an infection of an oil gland at the edge of the eyelid What is tinnitus? Downloaded by Jennifer Rangel (jennifer.renee.rangel6@gmail.com) lOMoARcPSD|14725619 ringing in the ear What is otorrhea? suggests infect canal or perforated eardrum What is toalgia? occurs from ear disease or is referred pain from a problem in teeth or mouth Exophthalmos? bulging eyes seen in hyperthyroidism Presbycusis? gradual sensorineural hearing loss caused through the aging process Ptosis? drooping upper eyelid. assess by comparing both eyes. observe distance between papillary fissures. Presbyopia? difficulty with near vision in the elderly. loss of elasticity. Rinne test? air conduction is great than bone conduction Mydriasis? dilated pupils Health history form for ear examination -Earaches? Location/ pain/ character/ -Infections? How frequent -Discharge? -Hearing Loss? (Presbycusis)= gradual onset over years bilateral -Enviornmental noise? -Tinnitus ? ringing/ roaring/ bothersome 6 months or longer -Vertigo- room spinning How to conduct a proper ear exam- what are the steps, what equipment do you use equipment needed: otoscope with a bright light 1. pull pinna/auricle up and back *adult) to straighten out the ear canal 2. hold otoscope upside down 3. insert the speculum in SLOWLY with the correct tip size 4. Rotate the otoscope in visualize the entire eardrum Tuning Fork: -Measures air( thru ear canal more sensitive) or bone conduction Developmental differences for the ear structures: babies/children vs. adults Downloaded by Jennifer Rangel (jennifer.renee.rangel6@gmail.com) lOMoARcPSD|14725619 -Children (shorter and wider ear canals--> more susceptible to ear infections) -ear positioned 10 degrees of vertical/ pinna should match imaginary line to occiput -adults(ear canal gets longer and opening narrows --> less ear infections) Module 5: Assessment of Head, Neck, Nose, Mouth, and Throat Review specific conditions of Head, Neck, Nose, Mouth, and Throat i.e.Enlarged tonsils, dysphagia, torticollis, goiter, bruit, gingivitis, leukoplakia, epistaxis, rhinorrhea What is the 4 point grading scale for tonsils? 1+=visible 2+= halfway between tonsillar pillars and Uvula 3+Touching Uvula 4+ Touching One Another What is dysphagia? swallowing difficulties, feels like something is in throat What is torticollis? hematoma in one sternomastoid muscle causing head to tilt to one side, and limit necks ROM What is goiter? Abnormal enlargement of thyroid gland What is bruit? turbulent flow through artery, abnormal narrowing of vessels What is gingivitis? inflammation of the gums What is leukoplakia? chalky, white, thick, raised path with well defined borders; lesion is firmly attached and does not scrape off --> usually on tongue, can also be on cheeks -caused by chronic irritation of smoking and alcohol use What is epistaxis? nosebleed What is rhinorrhea? "runny nose" Normal anatomical findings and landmarks for head & neck examination -head -neck: Carotid arteries (palpate one at a time, to prevent patient from passing out) Downloaded by Jennifer Rangel (jennifer.renee.rangel6@gmail.com) lOMoARcPSD|14725619 -lymph nodes (should not be tender, typically small and soft, moveable) -throat: looks like windpipe or trachea is not midline--tracheal shift Review health history & assessment form for face, head, & neck in Jarvis Symmetry-do both sides of the face look symmetrical *edema-is there any swelling in the mouth or throat *thyroid gland-feel for enlargement *tracheal alignmen Review terminology for neck and mouth Via buccal route? placed inside patients cheek Via sublingual route? under the tongue Via orally? put in mouth and swallow Equipment used during head, neck, & mouth examination otoscope/penlight--> mainly used for light (should not touch patients mouth) Downloaded by Jennifer Rangel (jennifer.renee.rangel6@gmail.com)