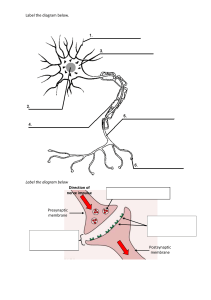
Topic 6: Organisms respond to changes in internal and external environments Topic 6.1.1 Survival and Response • Stimulus → a detectable change in the internal or external environment of an organism that leads to a response • Responding to stimuli increases chances of survival →selection pressure results in evolution • • • • receptors →specific to one type of stimulus coordinator →formulates response →molecular level or involve large organ, e.g. brain effector →carries out response →hormonal or nervous →molecular level or behavioural changes stimulus →receptor →coordinator →effector →response TAXES • • • • simple response whose direction is determined by the direction of the stimulus motile organisms respond by moving the whole body away or towards the stimulus +ve taxis →move towards favourable condition -ve taxis →move away from unfavourable condition • +ve phototaxis →algae moving towards light for photosynthesis • -ve phototaxis →earthworms moving away from light to conserve water KINESIS • simple response where the organism changes the speed of movement and the rate of change of direction in response to a stimulus • rate of turning increases and moves quicker when in unfavourable conditions →increase chance of returning to favourable conditions • organism turns less and moves slower when in favourable conditions →wants to stay there • woodlice changes direction more and moves quicker in dry conditions to return to humid conditions →prevent loss of water • tropism in plants Plant Growth Factors • not hormones →exert influence through growth →made in cells throughout the whole plant • some only affect the tissue that released it →not a distant organ Plants respond to: • light →needed for photosynthesis • gravity →plants firmly anchored in soil • water →needed for photosynthesis and other metabolic processes IAA • Indoleacetic acid →one type auxin • most abundant auxin in plants • found in meristems (mitotic, dividing tissue) at the tip of shoots and roots (also in the middle of the vascular bundle) • controls plant cell elongation →softens cell walls so the cell can take in water to elongate • causes elongation in shoots // inhibits elongation in roots • IAA causes active transport of hydrogen ions from cytoplasm into cell wall →more plastic so it can elongate • exogenous IAA →artificial IAA added to the plant →not those naturally produced or present in the plant Phototropism: 1. Cell at the tip of the shoot produces IAA 2. In normal light, IAA diffuses evenly down the shoot, causing cell elongation on both sides of the shoot 3. Unidirectional light causes IAA to move away from the lightened side 4. A greater concentration of IAA builds up on the shaded side 5. The cells on the shaded side elongate more than those on the lightened side 6. Shoot bends towards the light Gravitropism: 1. Cell at the tip of the root produces IAA 2. IAA is initially transported evenly to all sides of the root 3. Gravity causes IAA to move to the lower side of the root 4. A greater concentration of IAA builds up on the lower side 5. The cells on the upper side elongates more than those on the lower side 6. Root bends downwards towards gravity Uneven distribution of IAA causes growth The amount of IAA produced is the same, it is the concentration of it that causes the bending. IAA cannot travel through the glass so the concentration is the same each side. Concentration of IAA affects growth. IAA diffuses from the tip. Reflex actions • direct connection between sense organ and effector →3 neurone, 2 synapse system • reflexes are - rapid →must be quick to protect body - short-lived →don’t need signal after the response is carried out - localised →avoid moving the whole body →may cause other accidents - involuntary →’thinking’ requires too much time spinal reflex →removing hand from hot object • • cranial reflex →blinking REFLEX ARC 1. Stimulus →pain from a sharp object 2. Receptor →pain receptors in the skin generate an action potential in the sensory neurone 3. Sensory neurone →passes impulse to spinal cord 4. Coordinator (intermediate neurone) →links sensory to motor neurone 5. Motor neurone →passes impulse to muscles in the arm 6. Effector →muscles in the arm contract 7. Response →hand is pulled away from sharp object IMPORTANCE OF REFLEX • • • • involuntary so does not involve brain →not over-loaded →left to carry out more complex responses signal still sent to brain →reflex can be overridden →modify response protect body from harm →effective from birth →not learnt fast →few synapses and no decision-making Topic 6.1.2 Receptors • specific to a single type of stimulus →pacinian corpuscle only responds to mechanical pressure • acts as a transducer to produce a generator potential →pacinian corpuscle changes mechanical pressure into a nerve impulse PACINIAN CORPUSCLE • respond to mechanical pressure • most abundant on fingers, sole of feet and external genitalia • occur in ligaments and tendons →let us know which joints are changing direction • single sensory neurone in layers of connective tissue →rich in collagen • has stretch-mediated sodium channels →at rest, channels are too narrow to allow Na+ ions to pass • neurone is deformed when pressure is applied →channels stretched→Na+ ions can pass through and enter the neurone • influx of ions depolarises the membrane →generator potential created • stimuli must be over a threshold in order to cause a generator potential →action potential in nerve The Eye • made up of 3 layers →sclera, choroid, retina • retina is made up of 3 layers →rods and cones →bipolar neurones →ganglion neurones (a bundle makes up the optic nerve) • rod and cone cells →transducers converting light energy into electrical energy ROD CELLS • around 120 million per eye • more at the periphery of retina, absent in fovea • can only distinguish black and white light →detect light of low intensity • enough energy from low light intensity to break rhodopsin down → neurotransmitter released →generator potential created • a few rod cells synapsing with 1 bi-polar neurone →retinal convergence (specific example of summation) • small number of neurotransmitter from each rod cell all contribute to signal →greater chance of threshold value being exceeded • single impulse generated from several rods →brain cannot accurately determine where the signal cam from →low visual acuity CONE CELLS • • • • • around 6 million per eye concentrated at the fovea, fewer at the periphery of retina 3 types →red, blue, green →each is sensitive to its own range of wavelength of light can distinguish coloured light →high intensity light lots of energy from high light intensity to break iodopsin down • connected to its own bi-polar neurone →no retinal convergence • impulses generated will be from different cone cells →high visual acuity DISTRIBUTION OF RODS AND CONES • cones are concentrated at the fovea →no rod cells • number of rods increase towards the periphery of the retina →number of cones decrease • no rods or cones at the blind spot →where the optic nerve enters the eye • this graph is taken in line with the blind spot • if the measurement is taken at 90° to the eye →graph will not show blind spot • no dip at 20° from fovea →number of cells will follow trend Rods Cones Rod-shaped Cone-shaped Greater numbers Fewer numbers More at periphery Concentrated at fovea Low visual acuity High visual acuity Sensitive to low light intensity Sensitive to high light intensity 1 type 3 types Topic 6.1.3 Control of heart rate • autonomic nervous system →self-governing →controls involuntary activities →muscles and glands • antagonistic nervous systems SYMPATHETIC NERVOUS SYSTEM • stimulates effectors • speeds up activity PARASYMPATHETIC NERVOUS SYSTEM • inhibits effectors • slows down activity →conserves energy and replenishes resources in the body Control of heart rate • myogenic cardiac muscle →initiates its own contractions →not stimulated by other nerves (neurogenic) • sinoatrial node (SAN) in the right atrium →pace maker →initiates stimulus for contraction • basic rhythm determining hear beat 1. Wave of electrical excitation spreads from the sinoatrial node to both atria 2. Atrial systole 3. Layer of non-conductive tissue (atrioventricular septum) prevents impulse crossing to ventricles 4. Wave of excitation hits the atrioventricular node (AVN)between atria 5. There is a short delay to allow the atria to empty and the ventricles to fill 6. AVN sends electrical impulse along the Purkyne tissue making up the Bundle of His in the septum 7. The impulse hits the base of the septum 8. Impulse is released from the Purkyne tissue causing the ventricles to contract upwards →ventricular systole MODIFYING HEART RATE altered to meet the demands for oxygen during different activities controlled by medulla oblongata in the brain centre increasing heart rate →sympathetic nervous system →SAN centre decreasing hear rate →parasympathetic nervous system →SAN • controlled by receiving signals from chemoreceptors and baroreceptors (pressure) • • • • Chemoreceptors: • in the wall of carotid arteries (going to the brain) and aorta • pH changes due to concentration of carbon dioxide 1. 2. 3. 4. 5. 6. 7. 8. 9. higher concentration of carbon dioxide in blood →lower pH chemoreceptors detect the change in pH increased frequencies of impulses are sent to the medulla medulla sends increased frequency of impulses via the sympathetic nervous system to the SAN SAN sends increased frequency of electrical impulses →heart rate increases blood flow is faster →more carbon dioxide removed by lungs [CO2] in blood returns to normal →pH of blood returns to normal chemoreceptors reduce frequency of impulse to medulla medulla reduces frequency of impulses to SAN →heart rate decreases Pressure receptors: • in the wall of carotid arteries and aorta • sensitive to pressure changes 1. 2. 3. 4. when the blood leaves the heart too quickly →blood pressure is higher than normal pressure receptors send an increased frequency of impulses to the medulla medulla sends an increased frequency of impulses via the parasympathetic nervous system to the SAN SAN sends less frequent impulses →heart rate slows →blood pressure is reduced 1. 2. 3. 4. when the blood leaves the heart too slowly →blood pressure is lower than normal pressure receptors send an increased frequency of impulses to the medulla medulla sends an increased frequency of impulses via the sympathetic nervous system to the SAN SAN sends more frequent impulses →heart rate increases →blood pressure is increased Topic 6.2.1 Nerve impulse • coordination required for large organisms • communication through hormonal and nervous system Hormonal system Nervous system Communication by hormones Communication by nerve impulses Transmission by blood stream Transmission by neurones Slow transmission Rapid transmission Hormones travel to all parts →only target responds Travels to specific parts Wide-spread response Localised response Slow response Rapid response Long-lasting response Short-lived response Permanent and irreversible effect Temporary and reversible effect • central nervous system →brain and spinal cord • peripheral nervous system →sensory and motor neurones • voluntary nervous system →carries nerve impulses to striated muscles • autonomic nervous system →carries impulses to glands, smooth and cardiac muscles Neurones: • single cell • a bundle of axons from different neurones surrounded with protective covering →nerve • cell body →cytoplasm →axons are thin extensions from the cell body →nucleus and lots of rough endoplasmic reticulum →production of proteins and neurotransmitters • dendrons →carry nerve impulses towards the cell body • axon →carry nerve impulses from the cell body • myeline sheath →schwann cells surrounding the axon →lots of lipids inside cytoplasm of schwann cells →wrap around neurones forming myelin sheath →nodes of Ranvier between schwann cells →increases speed of nerve conduction →phagocytosis of cell debris →helps with nerve regeneration Sensory neurone: • impulses from receptor to CNS • cell body in the middle Motor neurone: • impulses from CNS to effector • cell body in the CNS Relay neurones: • impulses between sensory and motor neurones • in the CNS Nerve impulse • a self-propagating wave of electrical activity along the axon membrane • momentary reversal in electrical potential difference across the axon membrane →moves along membrane • cell membrane is impermeable to ions →ions must move across by pumps and channels • some channels are gated →only opens in certain conditions →voltage, stretch, ligand • some channels are always open • sodium-potassium pump moves ions across using ATP by active transport RESTING POTENTIAL: Na+ ions pumped out of the axon K+ ions pumped into the axon sodium potassium pump →3 Na+ out for 2 K+ in more sodium outside membrane →more K+ outside membrane electrochemical gradient created →ions are charged facilitated diffusion of ions through open channels →more potassium channels open than sodium channels open →membrane is more permeable to K+ ions • outside of membrane is more positively charged →inside is more negatively charged →70mV • no net movement of K+ ions →resting potential →membrane is polarised • • • • • • • found using the giant squid axon →electrode placed into the membrane →p.d. is -70mV Some single celled organisms living in sea water actively transport ions into the cell to compensate for loss of water ACTION POTENTIAL: • change in potential difference across the membrane • caused by stimulus from receptor or neurotransmitter from synapse →must be past threshold value to trigger action potential • channels in membrane change shape depending on voltage changes →voltage-gated channels 1. Depolarisation • membrane voltage becomes less -ve • energy from stimulus opens sodium voltage-gated channels →Na+ flows into membrane through facilitated diffusion →down electrochemical gradient • rapid influx of Na+ ions →higher [Na+] in membrane →+40mV →reverse p.d. across membrane • positive feed back →more Na+ flowing in →membrane is more depolarised →more channels open • all-or-nothing →cannot control degree of depolarisation →threshold value met = depolarise, not met = nothing 2. Repolarisation • at +40mV →sodium voltage-gated channels close →no more influx of Na+ ions into membrane • potassium voltage-gated channels open →rapid movement of K+ ions out of membrane →facilitated diffusion down the electrochemical gradient • inside of membrane becomes more polarised again →outflow of positive ions 3. Hyperpolarisation • outward diffusion of K+ ions overshoot →more K+ ions outside than that at resting potential • potential difference in membrane is more -ve than resting potential →-85mV • potassium voltage-gated channels close →no K+ ion move out • refractory period →sodium potassium pump moves Na+ and K+ back to resting potential • axon is repolarised REFRACTORY PERIOD: • sodium-voltage gated channel closed →influx of sodium ions prevented • no action potentials generated - action potentials only move in one direction →action potential cannot propagate towards a section in the refractory period - each impulse is discrete →new action potential cannot be formed immediately behind the first one - number of action potentials is limited →separate action potentials = number of action potentials on one neurone at the same time limited = strength of stimulus detected is limited Movement of action potential • action potential at each section of the membrane triggers sequence of it along the axon • each depolarisation triggers depolarisation in the next region • size of action potential remains the same across the axon 1. At resting potential →membrane is polarised →higher [Na+} outside and higher [K+] inside 2. Stimulus causes influx of Na+ →reversal of charge on the axon membrane →local currents created between sections of different charges 3. Local electric currents stimulates sodium-voltage gated channels to open in the next section →depolarisation 4. Potassium voltage-gated channels open in the previous section →repolarisation 5. Action potential propagates along the axon →nerve impulse MYELINATED AXON: • myeline sheath is an electrical insulator across the membrane →no ion flow allowed • depolarisation →flow of ions can only occur at Nodes of Ranvier • local currents occur between the nodes • impulses move along the axon through saltatory conduction →much faster as less distance is covered Speed of the nerve impulse FACTORS: 1. Myelin sheath • electrical insulator allowing impulses to jump between nodes of Ranvier →saltatory conduction • increases speed of nerve impulse • vertebrates have myelinated nerves →all voluntary nerves myelinated →not all autonomic nerves myelinated • invertebrates (e.g. giant squid) do not have myelin sheaths 2. Diameter of axon • larger diameter →faster speed of conduction • less leakage of ions from a larger axon →easier to maintain membrane potential 3. Temperature • rate of facilitated diffusion of ions affected →through channels • temperature denatures proteins and enzymes →pumps and channels in the membrane • especially in ectotherms • temperature affects speed and strength of muscle contractions ALL OR NOTHING PRINCIPLE: • • • • • impulses will only be generated when the stimulus surpasses the threshold value below threshold value →no impulse action potentials are all the same size strength of stimulus determined by frequency of impulses + number of neurones stimulated higher frequency + more neurones stimulated →stronger stimulus Topic 6.2.2 Synaptic transmission Synapse • where one neurone communicates with another →links different neurones together →coordinate activities STRUCTURE: • synaptic cleft (20-30nm)→mostly chemical coordination • pre-synaptic neurone releases neurotransmitters →synaptic knob is the end of the axon →lots of mitochondria and endoplasmic reticulum →energy needed to manufacture neurotransmitters • neurotransmitter stored in synaptic vesicles FUNCTION: • act as junctions →one impulse along one neurone can initiate more new impulses on multiple neurones →one stimulus can result in a coordinated response • multiple impulses can result in one response UNIDIRECTIONALITY: • synapse can only pass information in one direction • neurotransmitters can only be released from the pre-synaptic membrane →can only be received on the receptors on the post-synaptic membrane SUMMATION: • spatial summation →different presynaptic neurones release enough neurotransmitters in total • temporal summation →one presynaptic neurone release neurotransmitters many times over a short period • total number of neurotransmitters exceed threshold value of the postsynaptic membrane →new action potential triggered INHIBITION: • some synapses reduce the likelihood of the creation of a new impulse →inhibitory synapses • neurotransmitter released by presynaptic neurone binds to chloride ion channels on the postsynaptic membrane • chloride channels open →Cl- ions move into the neurone by facilitated diffusion • potassium channels also open →K+ ions move out of the neurone into the synapse by facilitated diffusion • more negative ions inside neurone and more positive ions outside • membrane potential increases to -80mV →hyperpolarisation of membrane • larger influx of Na+ needed to produce a new action potential →less likely • excitatory post-synaptic potential →sodium channels opening due to neurotransmitters allowing influx of Na+ ions →if it exceeds threshold →action potential will be generated Transmission across a synapse • neurotransmitters diffuse across the synapse • cholinergic synapse has acetylcholine as neurotransmitters →common in vertebrates →in CNS and neuromuscular junctions 1. Release of neurotransmitters • action potential arriving at the pre-synaptic membrane opens calcium channels →increased membrane permeability to Ca2+ ions • higher concentration of Ca2+ ions outside →diffuse into the membrane • causes synaptic vesicles to fuse with pre-synaptic membrane →exocytosis of neurotransmitter (acetylcholine) 2. Stimulation of the post synaptic membrane • acetylcholine binds to the receptor site of a sodium channel →ligand-gated channels • sodium channel opens and Na+ ions flow into the membrane • action potential generated if there is sufficient acetylcholine • number of functioning receptors on the membrane affects the degree of depolarisation 3. Inactivation of the neurotransmitter • receptors are emptied so they can react to the next impulses • acetylcholine is hydrolysed by acetylcholinesterase into acetate and choline • they diffuse across the synapse and is taken up by the pre-synaptic membrane • they are re-synthesised back into acetylcholine using energy from the mitochondria →packaged into synaptic vesicles Topic 6.3 Muscles • • • • effector organs responding to nervous stimulations →voluntary and involuntary nerve impulses cardiac muscles →in the heart (myogenic →does not require a nerve impulse) smooth muscles →walls of blood vessels and the gut →involuntary control skeletal muscle →attached to bones →voluntary control Structure of muscles • muscle made up of bundles of muscle fibres • muscle fibre →several cells fused together forming an elongated cell →share nuclei • sarcoplasm →cytoplasm • lots of mitochondria and endoplasmic reticulum within the cell • inside the cell →myofibril ACTIN AND MYOSIN: • actin →thinner protein filament →2 strands of globular proteins twisted around each other • tropomyosin forming a fibre strand around the actin →blocks the binding site of actin • myosin →thicker protein filament • long tails with bulbous heads projected to the side • bulbous heads bind to the binding site on actin • • • • I-band →only actin (lighter band) Z-line →where adjacent actin filaments are connected A-band →where actin and myosin overlap →from one end to the other (darker band) H-zone →only myosin During contraction: • I-band is narrower + Z-lines are closer together →sarcomere shortens • H-zone is narrower + A-band remains the same length • evidence for sliding filament theory TYPES OF MUSCLE FIBRE 1. Slow-twitch muscle fibres • contract more slowly • less powerful contractions • contracts over a longer period →adapted to endurance work • more aerobic respiration →avoid build-up of lactic acid • large store of myoglobin →higher affinity for O2 compared to Hb →store O2 in muscle cells • rich supply of blood vessels →O2 and glucose supply • lots of mitochondria 2. Fast-twitch muscle fibres • contract more rapidly • more powerful contractions • contract over a short period →adapted to intense exercise →short bursts of intense activity • thicker and more myosin filaments →more power strokes • higher concentration of glycogen →easily broken down to glusose • higher concentration of enzymes for anaerobic respiration →provides ATP quickly • store of phosphocreatine →can donate phosphate group to form ATP from ADP →provide energy for muscle contractions NEUROMUSCULAR JUNCTION: • • • • • motor neurone meets a skeletal muscle fibre lots of junctions along a muscle →reduce time taken for wave of contraction to travel across muscle ensure all muscle filaments contract simultaneously →rapid and powerful movement motor unit →muscle fibres supplied by one motor neurone greater force needed →more units stimulated action potential arrives at the junction →synaptic vesicles fuse with presynaptic membrane acetylcholine diffuses across synapse and binds to receptors on the postsynaptic membrane sodium channels open →influx of Na+ ions →depolarisation action potential triggered in muscle fibre →travels deep into fibre through a system of T-tubles branching throughout the sarcoplasm of the muscle • T-tubles are continuous with the endoplasmic reticulum • ER actively transports Ca2+ ions out of the sarcoplasm • action potential in tables open calcium channels →influx of Ca2+ ions into the cytoplasm down the concentration gradient • • • • Neuromuscular junction vs Cholinergic synapse: • both have neurotransmitters transported by diffusion • both have receptors →cause influx of Na+ ions on the postsynaptic membrane • both use sodium-potassium pumps to restore resting potential • both use enzymes to break down neurotransmitters Neuromuscular junction Cholinergic synapse excitatory excitatory and inhibitory neurones to muscles neurones to neurones or other effectors motor neurones motor, sensory or intermediate neurones end of an action potential new action potential can be produced acetylcholine binds to muscle fibre membrane acetylcholine binds to neurone membrane Muscle contraction • muscles attached to bones →incompressible • muscles can only pull →antagonistic muscles needed →pulling in opposite directions • sliding filament mechanism Evidence for sliding filament mechanism: • I-band is narrower + Z-lines are closer together →sarcomere shortens • H-zone is narrower + A-band remains the same length 1. Ca2+ ions released causes the tropomyosin to more away from the actin binding site 2. Myosin head has an ADP attached to it 3. Myosin head binds to the exposed binding site forming an actinomyosin cross-bridge 4. Myosin head changes angle, pulling the actin →power stroke 5. ADP is released from the myosin head and an ATP molecule binds to it 6. Myosin head detaches from the binding site 7. Ca2+ ions active ATPase which hydrolyses ATP into ADP 8. Energy is released for the myosin to return to its original position →cycle starts again • myosin molecules joint by their tails →myosin heads are in the opposite directions →pull actin filaments towards the centre of sarcomere MUSCLE RELAXATION: • no action potential arrives at the muscle fibre • Ca2+ ions actively transported back into the endoplasmic reticulum →energy from hydrolysis of ATP • lack of Ca2+ ions →tropomyosin blocks the actin filament again • myosin heads cannot bind →no contraction • muscle relaxes →antagonistic muscle pulls the actin filaments outwards between the myosin to its uncontracted length ENERGY SUPPLY DURING CONTRACTION: • for movement of myosin heads • for reabsorption of Ca2+ ions back into the ER • ATP regenerated from ADP through respiration in mitochondria →lots of mitochondria in muscles • muscles can respire anaerobically in a lack of oxygen - more glycolysis - phosphocreatine can donate phosphate group to turn ADP into ATP - store of phosphocreatine replenished using phosphate from ATP after muscle relaxation Topic 6.4.1 Homeostasis • physiological systems that maintain the internal environment within restricted limits • limit the effect of external changes →body responds to stimuli to maintain dynamic equilibrium • return each component to its optimum IMPORTANCE OF HOMEOSTASIS • enzyme function →slight change in pH or temperature can affect rate of reaction • water potential →cells can shrink or burst due to osmotic effects →blood glucose must be maintained to control water potential →allowed mammals to explore a wider geographical range CONTROL MECHANISMS • levels fluctuate around the optimum point • receptors and effectors control to return levels to the optimum • communicated via the nervous or hormonal system Negative feedback: • alters the system to return to its optimum point • control of blood glucose Positive feedback: • increases effect that has triggered response • sodium influx in neurones, giving birth Topic 6.4.2 Control of blood glucose concentration Hormones • • • • • organic chemicals →proteins (insulin, glucagon) or steroids (oestrogen, testosterone) can act as transcription factors or just signalling molecules produced by endocrine glands →released directly into the blood, ductless acts on target cells →specific receptors complementary to the hormone effective at low concentrations →widespread and long-lasting effects SECOND MESSENGER MODEL: • protein hormones require secondary messengers inside the cell →too big to diffuse across phospholipid bilayer • steroids are non-polar →receptors are inside the cell Adrenaline-stimulated cAMP synthesis 1. adrenaline binds to a transmembrane protein receptor on liver cell 2. binding causes conformational change of the G-protein 3. adenylate cyclase activated 4. ATP converted into cAMP 5. cAMP (second messenger) activates protein kinase A 6. protein kinase A catalyses the breakdown of glycogen into glucose PANCREAS • large gland in the upper abdomen • exocrine gland →protease, amylase, lipase produced for digestion • endocrine gland →insulin and glucagon produced Islets of Langerhan: • α cells →produce glucagon • β cells →produce insulin • surrounded by capillaries →direct diffusion of hormones into blood • enzyme-producing cells around the islets Adrenaline activates glycogenolysis in the liver LIVER • made of hepatocytes • insulin and glucagon acts on the liver Glycogenesis • conversion of glucose into glycogen • occurs when blood glucose level is high • insulin acts on the cells to remove glucose from the blood Glycogenolysis • conversion of glycogen into glucose • occurs when blood glucose level is low • glucagon acts on cells to allow glucose to diffuse into the blood Gluconeogenesis • producing glucose from sources other than carbohydrates (amino acids, glycerol) • occurs when there are not enough glycogen • glucose produced to raise blood glucose levels Regulation of blood glucose • glucose provides energy to cells →especially brain cells • affects water potential of blood Blood glucose levels affected by: • diet →glucose absorbed through the intestines by hydrolysis of carbohydrates • glycogenesis • gluconeogenesis INSULIN AND B-CELLS • β-cells have receptors →detect the rise in blood glucose level • insulin released directly into the blood plasma • all body cells have glycoprotein receptors for insulin on the cells membrane • insulin binding causes a conformational change of the glucose transporter on the membrane • insulin binding causes vesicles containing transporter to fuse with the membrane →increase in number of glucose transporter • increased facilitated diffusion of glucose into the cell →reduced blood glucose level • insulin binding activates enzymes that cause glycogenesis and conversion of glucose to fat Blood glucose level reduced by: • increased rate of absorption into cell • increased respiratory rate of glucose • increased rate of glycogenesis • increased rate of conversion of glucose to fat • lowered blood glucose level detected by β-cells • secretion of insulin reduced GLUCAGON AND A-CELLS • • • • • • α-cells have receptors that detect the decrease in blood glucose level glucagon released into blood plasma glucagon attaches to receptors causing second messenger →similar to adrenaline enzymes activated for glycogenolysis and gluconeogenesis blood glucose level increased back to optimum α-cells reduce secretion of glucagon • insulin and glucagon are antagonistic →highly sensitive • negative feedback →self-regulating system • blood glucose levels still fluctuate →lag between hormone production and action Diabetes • inability to control blood glucose concentration TYPE 1 (INSULIN DEPENDENT) • • • • body unable to produce insulin childhood disease →can be an autoimmune reaction →immune system attacks β-cells in pancreas controlled by injection of insulin →cannot be taken by mouth →protein digested in the stomach glucose concentration monitored by biosensors TYPE 2 (INSULIN INDEPENDENT) • • • • due to glycoprotein receptors not responding to insulin can also be inadequate supply of insulin from pancreas caused by obesity and poor diet controlled by regulating diet and lifestyle Topic 6.4.3 Control of blood water potential Structure of the kidney • fibrous capsule →outer membrane protecting the kidney • cortex →outer region made up of the Bowman’s capsule, convoluted tubules and blood vessels • medulla →inner region made up of the loops of Henle, collecting ducts and blood vessels • renal pelvis →collects urine into ureter • ureter →kidney to bladder NEPHRON • • • • • Bowman’s capsule →made up of podocytes, surrounds the glomerulus (mass of blood capillary) proximal convoluted tubule →loops surrounded by blood capillaries loop of Henle →long hairpin loop extending from the cortex to the medulla distal convoluted tubule collecting duct →a few nephrons empty into it, becomes wider towards to the pelvis of the kidney BLOOD VESSELS • afferent arteriole →enters the renal capsule of the nephron →larger diameter than efferent arteriole • glomerulus →branched capillaries in the Bowman’s capsule →fluid forced out the blood here • efferent arteriole →leaves the renal capsule →smaller diameter than afferent arteriole so blood pressure increases in the glomerulus • blood capillaries →surrounds the tubules in the nephron; glucose, water and salts reabsorbed Role of nephron in osmoregulation • maintain water potential of blood plasma and tissue fluid 1. FORMATION OF GLOMERULAR FILTRATE BY ULTRAFILTRATION • blood in the glomerulus have a high pressure →diameter of efferent arteriole is smaller than diameter of afferent arteriole • glomerular capillaries are made up of endothelial cells • water, glucose and ions are pushed out of the glomerulus to form the glomerular filtrate →ultrafiltration • ultrafiltration is resisted by →endothelial cells and connective tissue of the capillary →hydrostatic pressure of fluid in the renal capsule →low water potential of the blood in the glomerulus • adaptations →podocytes have spaces between them →allow filtrate to pass through gaps rather than through the cell →endothelium of the capillaries have pores to allow filtrate through instead of the through the cells →hydrostatic pressure of blood can overcome the resistance • filtrate contains urea but not cells or plasma proteins 2. REABSORPTION OF GLUCOSE AND WATER • occurs in the proximal convoluted tubule • 85% of the filtrate is reabsorbed • Na+ ions actively transported out of the cells into the blood →lowers [Na+] in cell • Na+ ions diffuse down the concentration gradient from the lumen of the proximal convoluted tubule into the cell • through facilitated diffusion across carrier proteins • glucose is co-transported into the cell • water reabsorbed by osmosis • microvilli →large surface area for reabsorption • infoldings at the base →large surface area • high density of mitochondria →ATP for active transport 3. MAINTAINING NA+ ION GRADIENT • loop of Henle extends into the medulla →concentrates urine to a lower water potential than blood • concentration of urine related to length of loop of Henle • descending limb →narrow with thin walls →permeable to water • ascending limb →wider with thick walls →impermeable to water • concentration of ions increase down into the medulla →water potential decreases • water moves through aquaportins (water channel proteins) →ADH alters number of aquaporins 1. 2. 3. 4. Na+ ions actively transported out of the ascending limb using ATP Low water potential between 2 limbs Impermeable walls of ascending limbs don’t allow water to move out Permeable walls of descending limbs allow water to move into the interstitial space and then blood capillaries by osmosis 5. Filtrate in the loop loses water potential down into the medulla →lowest water potential at the hairpin 6. Na+ ions diffuse out of the hairpin due to high ion concentration 7. Water potential in loop increases up the ascending limb 8. Collecting duct is permeable to water →always at a higher water potential than the interstitial space →counter-current multiplier effect 9. Water moving out of the collecting duct decreases water potential of loop →still higher than the interstitial space distal convoluted tubule makes final adjustments to water potential →controls pH of blood • microvilli and mitochondria allow reabsorption of material by active transport • Regulation by hormones • water potential of blood affected by →water being consumed →sweating occurring →amounts of ions being taken in 1. 2. 3. 4. 5. 6. Osmoreceptors in the hypothalamus of the brain detects the fall in water potential Water is lost from the osmoreceptor cells by osmosis →cells shrink Change causes impulses to be sent via the sympathetic nervous system to the pituitary gland Antidiuretic hormone released from the posterior pituitary gland into the blood ADH reaches the epithelial cells of the distal convoluted tubule and collecting duct in the kidney ADH binds specifically to receptors causing phosphorylase to be activated 7. Activation of phosphorylase causes vesicles with aquaporins to fuse with the cell membrane 8. Increase in number of aqauporins increases permeability of the cell to water 9. More water move out of the collecting duct →more water reabsorbed 10. Water reabsorbed is from blood in the first place →ADH only prevents blood water potential from getting lower, does not increase it NEGATIVE FEEDBACK • increase reabsorption causes rise in water potential in blood →detected by osmoreceptors • fewer impulses sent to the pituitary gland • less ADH produced →permeability of collecting duct returns to previous state RESPONSE TO RISE IN WATER POTENTIAL • osmoreceptors detect rise in water potential →increase in frequency of nerve impulses through the parasympathetic nervous system to the pituitary gland • release of ADH reduced • less ADH decreases permeability of collecting duct • less water absorbed into blood • water potential of blood falls →returns to normal ADH levels