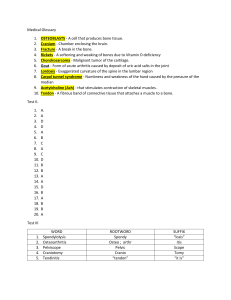
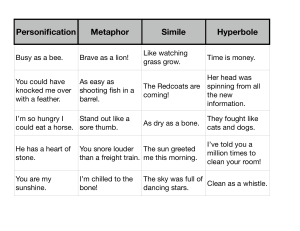
Presentor- Dr Lachhima Bhandari Moderator- Dr Heena 1 Normal bone Parts of bone-1) epiphysis 2)metaphysis 3)diaphysis Macroscopic architecture of bone may be1)Compact bone 2)cancellous/spongy/trabecular bone 2 Microscopic arrangement of bone1)Woven bone- random deposition of collagen 2)Lamellar bone- collagen deposited in orderly manner. 3 osteoid Unmineralised matrix produced by osteoblasts Type I collagen with a minor component of non- collagenous proteins & growth factors On H&E-dense,pink,amorphous intercellular material D/d-collagen, fibrin, chondroid 4 WHO classification of bone tumors Osteogenic Tumours a) Osteoid osteoma b)Osteoblastoma c)Osteosarcoma- conventional - chondroblastic - fibroblastic - osteoblastic d) Telangiectatic e) Small cell f) Low grade central g) Secondary h) Parosteal i) Periosteal j) High grade surface 5 Contd... Catilage tumors a) Osteochondroma b) Chondroma- enchondroma - periosteal chondroma -multiple chondromatosis c) Chondroblastoma d) Chondromyxoid fibroma e) Chondrosarcoma- central, primary and secondary - peripheral - dedifferentiated - mesenchymal - clear cell 6 Contd….. Fibrogenic tumours a)Desmoplastic fibroma b) Fibrosarcoma Fibrohistiocytic tumours a) Benign b) malignant Ewing sarcoma/ primitive neuroectodermal tumour- ewing sarcoma Giant cell tumour Haematopoietic tumours- plasma cell myeloma - malignant lymphoma, NOS Notochordal tumours- chordoma Vascular tumour- hemangioma - angiosarcoma 7 Contd…. Smooth muscle tumour- leiomyoma - leiomyosarcoma Lipogenic tumours- lipoma - liposarcoma Neural tumours- neurilemmoma Miscellaneous tumours- adamantinoma - metastatic malignancy Miscellaneous lesions- aneurysmal bone cyst - simple cyst - fibrous dysplasia - osteofibrous dysplasia - langerhans cell histiocytosis - erdheim chester disease - chest wall hamartoma Joint lesions- synovial chondromatosis 8 Precursor lesions of bone tumours High risk- ollier disease( enchondromatosis) - maffucci syndrome - familial retinoblastoma syndrome - rothmund-thomson syndrome Moderate risk- multiple osteochondromas - polyostotic paget disease - radiation osteitis Low risk- fibrous dysplasia - bone infarct - chronic osteomyelitis - osteogenesis imperfecta - giant cell tumour - osteoblastoma and chondroblastoma - implants 9 Osteogenic tumoursThese are bone forming tumours. 1.OSTEOMA 2.OSTEOID OSTEOMA benign 3.OSTEOBLASTOMA 4.OSTEOSARCOMA malignant 10 OSTEOID OSTEOMA Age-10-30 yrs Sex- male predominance Site –majority seen in metaphysis long bones esp. femur & tibia Clinical features – Painful, Worse at night Relieved by NSAIDs Radiological featuresRadioluscent central nidus(<1.5 cm) surrounded by a peripheral sclerotic reaction. 11 Gross well circumscribed,size <2 cm nidus-small ,red and granular area; periphery- white sclerotic bone M/E Interlacing network of osteoid trabeculae that are variably mineralised Lined by prominent, plump osteoblasts Hypervascular sclerotic bone around tumour 12 Immunophenotype- strong nuclear staining for Runx 2 and Osterix Differential diagnosis 1.Osteomyelitis(Radiological)-Brodie’s abscess 2.Osteoblastoma - indistinguishable histologically - Size main distinguishing factor>2cms 13 OSTEOBLASTOMA Age- mainly between 10-30 yrs Sex-Male predominace(M:F 2.5:1) Site-prediliction for posterior elements of spine and sacrum. Also metaphysis of long bones Clinically-back pain,scoliosis,nerve root compression;pain not relieved by aspirin Radiology- radiolucent lesion with haphazard foci of mineralization with perilesional reactive bone 14 Gross well demarcated scalloped edges ,periosteal reactive bone rich vascular supply( redbrown color), gritty sensation M/E Anastomosing trabeculae of woven bone rimmed by a single layer of osteoblasts Intertrabecular space-loose fibrovascular stroma and multinucleate giant cells Well circumscribed, no permeation of pre-existing bone 15 Cytology- osteoblast like cells, singly or in groups or row -multinucleated osteoclast like cells - clusters of spindle cells Aggressive /epitheloid osteoblastomasAtypical radiographic & architectural features, tendency of local recurrence m/e- presence of large, epithelioid like osteoblasts with low mitotic activity and absence of permeation of surrounding bone. Differential diagnosis 1. Osteoid osteoma-on basis of size(<2 cm) 2. Osteosarcoma- permeation of surrounding intertrabecular spaces 16 OSTEOID OSTEOMA OSTEOBLASTOMA Trabeculae of woven bone are randomly arranged and interconnect haphazardly. Large osteoblasts rim the woven bone surfaces, and intertrabecular spaces contain loose fibrovascular tissue. 17 OSTEOSARCOMAS - Most common non-hemopoeitic primary malignant tumors of bone Predisposing factors- paget disease radiation exposure chemotherapy(alkylating agents) preexisting benign bone lesion(fibrous dysplasia, bone infarct Genetics- association with Li-Fraumani syndrome(TP53), hereditary retinoblastoma(RB1 gene0, Rothmund Thomson syndrome, Werner syndrome. Osteosarcomas are classified into- conventional - telangiectatic - small cell - parosteal - periosteal - high grade surface 18 a)Conventional osteosarcoma Age- bimodal; first bigger peak 10-14 yrs and 2nd smaller peak >40 yrs. Sex-male predominance( M:F 1.35:1) Site-metaphysis of long bones, distal femur>proximal tibia >proximal humerus Symptoms- enlarging painful mass with warm, erythemtous overlying skin; restricted movement, fracture Radiology- destruction of medullary cavity and cortical bone, resulting in periosteal reaction like codman triangle or sunburst appearance. 19 Gross Large, intramedullay tan-grey- white, gritty mass Reactive periosteal boneformation with lifting off periosteum-codman triangle Cytology Pleomorphic pattern of cells Epithelioid tumour cellsosteoblastic or chondroblastic type Multinucleated tumor cells Mitotic figures(often atypical) Intercellular tumour matrix of osteoid within clusters Cytoplasmic ALPase positive 20 M/E-highly anaplastic tumor, tumor cells may be epithelioid,fusiform,ovoid, clear cells or spindle cells Permeative pattern of growth Accurate identification of osteoidEosinophilic,dense,homoge nous Osteoblastic areas mixed with chondroblastic & fibroblastic areas Predominant matrix-decides the name 21 Conventional osteosarcoma is further subclassified into- osteoblastic - chondroblastic - fibroblastic - giant cell rich - clear cell - epithelioid - osteoblastoma like - chondroblastoma like 22 23 HISTOLOGIC VARIANTS OF OSTEOSARCOMA TYPES CHARACTERISTICS DIFFERENTIAL DIAGNOSIS TELANGIECTATIC OSTEOSARCOMA Blood filled or empty ANEURYSMAL BONE cystic spaces separated by CYST thin septa SMALL CELL OSTEOSARCOMA Small cells with scanty EWING’S SARCOMA cytoplasm associated with osteoid production LOW-GRADE INTRAOSSEOUS/ CENTRAL OSTEOSARCOMA Bland spindle cell background arranged in irregular bundles Low grade fibro-osseous lesions like FIBROUS DYSPLASIA, desmoplastic fibroma 24 Telangiectatic osteosarcoma Blood clot Blood filled cystic spaces 25 s Small cell osteosarcoma- small cells Intraosseous osteosarcomawith scant cytoplasm Fibroblastic stroma with variable 26 amount of osteoid Surface based osteosarcoma DIAGNOSIS LOCATION RADIOLOGICAL FEATURES HISTOLOGICAL FEATURES BEHAVIOUR Parosteal osteosarcoma Distal femur (70%); proximal tibia Arises from bone cortex and surrounding bone; “PASTED-ON” appearance Very bland spindle cell stroma with wellformed trabecular osteoid and bone Low-grade lesion; adequate surgical excision is usually curative D/dosteochondroma Periosteal osteosarcoma Diaphysis of long bones: tibia and femur Thickened cortex with parallel lines of calcified matrix; also frequently lytic Chondroblastic in appearance with focal osteoid formation Intermediategrade lesion; will recur and metastasize in a subset of patients d/dosteochondroma, chondroblastic osteosarcoma High-grade surface osteosarcoma Metaphysis or diaphysis of long bones Arises from cortex; poorly delineated; may involve the bone medullary cavity Similar to conventional osteosarcoma High grade lesion; aggressive behaviour 27 e)Parosteal osteosarcoma most common osteosarcoma of surface of bone Sex- female predominance Age- third decade Site-distal posterior femur(metaphyseal surface) Symptom-painless swelling, inability to flex knee Radiology- heavily mineralized mass attached to cortex with broad base 28 Gross-hard lobulated mass attached to the cortex;encircling the bone m/e- spindle cells with minimum atypia, forming parallely arranged bony trabeculae - Intertrabecular stroma is hypocellular D/D- osteochondromapresence of cartilaginous cap 29 f)PERIOSTEAL OSTEOSARCOMA Age-second & third decade Sex-male predominance Site-diaphysis or diaphyseal-metaphyseal region of long bones,esp. tibia and femur Symptom- limb swelling, mass, pain Radiological- cortical thickening, extrinsic cortical scalloping, periosteal reaction perpendicular to bone’s long axis(hair on end appearance) 30 Gross-a broad based with cortical thickening M/E-prominent cartilaginous component showing varying degrees of cytological atypia D/D 1.Osteochondroma, 2.Conventional chondroblastic osteosarcoma 3.Chondrosarcoma (juxtacortical) 31 g)High grade surface osteosarcoma Age- second decade Sex-male predominance Site- femur>tibia>humerus Gross-situated on the cortical surface of bone,varying in consistency depending on predominant matrix M/E-Same spectrum as conventional osteosarcoma 32 Osteosarcoma arising in special clinical settings a)osteosarcoma in paget’s disease- most cases arise in polyostotic paget disease b)Osteosarcoma of jaw Age-average age 34 yrs. Site-body of the mandible &alveolar ridge of maxilla Relative good prognosis c)Postradiation osteosarcoma Most common location-pelvis and the shoulder region Radiation doses of usually greater than 20Gy High grade osteosarcomas 33 d)Osteosarcomas in course of various benign diseases Three important associations Bone infarct Prosthetic joint Fibrous dysplasia 34 BONE TUMOURS IHC DIFFERENTIAL DIAGNOSIS OSTEOMA NOT USEFUL 1. 2. 3. 4. PAROSTEAL OSTEOSARCOMA JUXTACORTICAL MYOSITIS OSSIFICANS MELORHESTOSIS OSTEOCHONDROMA OSTEOID OSTEOMA NOT USEFUL 1. 2. OSTEOBLASTOMA INTRAOSSEOUS ABSCESS(BRODIE ABSCESS) STRESS FRACTURE 3. OSTEOBLASTOMA NOT USEFUL 1. 2. 3. OSTEOID OSTEOMA ANEURYSMAL BONE CYST OSTEOBLASTOMA LIKE OSTEOSARCOMA OSTEOSARCOMA Not specific, but different markers are: CD99 VIMENTIN S-100 OSTEONECTIN OSTEOCALCIN 1. 2. 3. OSTEOBLASTOMA CHONDROSARCOMA DEDIFFERENTIATED CHONDROSARCOMA MYOSITIS OSSIFICANS GIANT CELL TUMOUR EWING’S SARCOMA ANEURYSML BONE CYST 4. 5. 6. 7. 35 Cartilaginous tumors ENCHONDROMA OSTEOCHONDROMA benign CHONDROBLASTOMA CHONDROMYXOID FIBROMA CHONDROSARCOMA malignant 36 tumour Age and sex site symptoms radiology enchondroma Wide range (5 to 80 yrs) M=F Small bones of hand and feet Asymptomatic, incidental finding Well defined, radiolucent to variable calcification osteochondroma 10-20 yrs age; M>F Metaphysis of long bones Asymptomatic, incidental Exophytic osteocartilaginou s lesion, sessile/pedunclat ed; cartilage cap on MRI chondroblastoma 10-25 yrs; M>F Chondromyxoid fibroma 2nd -3rd decade; M>F Epiphysis of Localised pain long bones, immature bone Well defined, multiloculated, lytic lesion Metaphysis of pain long bones,Proximal tibia, distal femur Well defined, with surrounding reactive bone 37 a)Enchondroma Gross- <5cm in size, well defined margins - gritty, yellow( calcification) or red( ossification) foci M/E- lobules of hyaline cartilage separated by normal cancellous bone or marrow - Endochondral calcification seen - Mostly hypocellular with pyknotic nuclei of chondrocytes Genetics- heterozygous IDH1/IDH2 somatic mutations, aberration in chr 6- 38 b)Osteochondroma Gross- tumour has thin layer of fibrous tissue - cartilage cap with variable thickness M/E- cap has hyaline cartilage - Stalk has cortical-cancellous - endochondral calcification at junction of cap and stalk. Genetics- mutation in EXT1(8q22-24.1) or EXT2(11p11-12) gene 39 Variants of osteochondroma 1)Multiple hereditary exostosis- multiple osteochondromas with modeling defects at ends of bones 2) Subungual exostosis(dupuytren exostosis)osteochondroma like lesion involving distal phalanx. Genetics- t(X;6) 3)Bizarre parosteal osteochondromatous proliferation(Nora lesion)- involves surface of small bones of hand and feet. 40 ENCHONDROMA OSTEOCHONDROMA BONE ENCHONDRAL OSSIFICATION FIBROUS PERICHONDRIUM CARTILAGE CAP The well circumscribed nodules encased by a thin rim of reactive bone. Portions of the neoplastic cartilage have undergone ENCHONDRAL OSSIFICATION & remain in the centers of some trabeculae. CARTILAGE CAP undergoing endochondral ossification with orderly arrangement of chondrocytes. CANCELLOUS BONE seen beneath the cartilage cap. Intertrabecular spaces filled by fat and hematopoietic marrow. 41 c)Chondroblastoma Gross-pinkish-tan with ares of haemorrhage, calcification or cystic change. M/E- highly cellular - Sheets of chondroblasts having well defined cytoplasm, round to ovoid nuclei with longitudinal groove and inconspicuous nucleoli. - Osteoclastic type giant cell. - Fine network of pericellular “chicken wire” calcification. Immunophenotype- vimentin, S100, SOX9,cytokeratin 8,18,19 and p63 Genetics- mutations in H3F3B gene 42 Chondroblastoma displaying all three key histologic elements: 1.Numerous small chondroblasts 2. Rare osteoclast-type giant cells, and 3. Ill defined matrix material. Histologic hallmark of chondroblastoma: “CHICKEN WIRE” type of calcification pattern. 43 d)Chondromyxoid fibroma Gross- solid, yellowish-white or tan, well defined margins, replacing bone and thinned cortex. M/E- lobular pattern with stellate or spindle shaped cells in myxochondroid background - Lobules have hypocellular centres with hypercellular periphery Immunophenotype- S100, SOX9. negative for keratin Genetics- rearrangement of 6q13 and 6q25 44 Lobulated architecture with foci of myxoid material separated by incomplete fibrous septae as well as rare multinucleate giant cells. Intramedullary margin of a CMF shows a well demarcated border with the adjacent marrow fat .The tumor has a lobular architecture and varies in the degree of cellularity. 45 e)Chondrosarcoma 3rd m.c primary malignancy of bone Age- older group (>50 yrs) Sex- M>F Site- bones from enchondral ossification, (pelvis;ileum> proximal femur and humerus) Clinical- local swelling, pain, Radiology- radiolucent with variable mineralization, cortical erosion seen Depending on location chondrosarcoma is further divided into-central, peripheral, periosteal 46 Gross- c/s is translucent, lobular, blue-grey or white areas of hyaline cartilage M/E- production of irregulaer lobules of cartilaginous matrix, absent direct bone formation Chondrosarcomas are graded as I,II,III grade Nuclear size hyperchromasia cellularity mitoses I Plump,Uniform size + moderate absent II Nuclear atypia + hypercellular + III Nuclear pleomophism more than GdII + More than gdII ++ 47 Cytology- low grade(grade1,2)- predominantly tissue fragments high grade(grade3)- predominantly single cells - abundant eosinophilic, vacoulated cytoplasm - chondromyxoid material 48 CHONDROSARCOMA VARIANTS CLEAR CELL CHONDROSARCOMA DEDIFFERENTIATED CHONDROSARCOMA MESENCHYMAL CHONDROSARCOMA DEFINITION Low grade malignant neoplasm of cartilage with characteristic large cells and clear cells. Malignant tumor of cartilage with second, high grade, non cartilaginous component. High grade malignant biphasic neoplasm of benign cartilage and primitive small round blue cells. MICROSCOPIC APPEARANCES Large clear cells with 2 main components: prominent cytoplasmic • Central area of borders, round to oval nuclei conventional with vesicular chromatin, chondrosarcoma(grade 1) prominent nucleoli • High grade component of Matrix include woven bone osteosarcoma, and hyaline cartilage. fibrosarcoma, MFH Osteoclast like giant cells also seen. Biphasic population of cells: • Well differentiated hyaline cartilage. • Small round to oval to spindle cells with scant cytoplasm DIFFERENTIAL DIAGNOSIS 1. 1. 2. IMMUNOPHE NOTYPE Chondroblastic osteosarcoma Osteoblastoma S100, type II and type X collagen positive 1. 2. 3. 4. Chondroblastic osteosarcoma Chondrosarcoma MFH Fibrosarcoma Weak IDH 1/2 positive, TP53 over expression , HRAS mutation 2. 3. Chondroblastic osteosarcoma Ewing’s sarcoma Dedifferentiated chondrosarcoma SOX9, CD99 positive 49 Clear cell dedifferentiated 50 TUMORS ANCILLARY TESTS ENCHONDROMA VIMENTIN S100 IDH1/IDH2 mutations OSTEOCHONDROM A S100 Inactivating mutations of 1. EXT1 and EXT2 genes on 2. 3. Ch-8q24 and 11p11-12 MUTATIONS CHONDROBLASTOM S100,SOX9, RANKL, A H3F3 K36M protein Mutation in chromatin histone gene,H3F3A CHONDROMYXOID FIBROMA SOX9 S100 CHORDOMA CYTOKERATIN 8, 18,19 EMA Loss of INI 1 BRACHYURY, S100 Clonal rearrangement of ch-6 involving bands q13 and q25. Involvement of GRM1 gene CHONDROSARCOMA S100 IDH1 and IDH2 mutations DIFFERENTIAL DIAGNOSIS 1. 2. Low grade chondrosarcomas Chondroblastic osteosarcoma Chondrosarcoma Parosteal osteosarcoma Bizarre parostel osteochondromatous proliferation 1. 2. 3. Giant cell tumor Aneurysmal bone cyst Chondromyxoid fibroma 1. 2. 3. 4. Chondroblastoma Enchondroma Chondroblastic osteosarcoma Chondrosarcoma 1. 2. 3. 4. Chondrosarcoma Metastatic adenocarcinoma Giant notochordal rest Extraskeletal myxoid chondrosarcoma 1. 2. 3. Enchondroma Chondromyxoid fibroma Chondroblastic osteosarcoma 51 Ewing sarcoma Small round cell sarcoma of bone 2nd m.c bone sarcoma in children Age- 5-20 yrs Site- metaphysis or diaphysis of long bones Symptoms- pain, fever, leukocytosis( simulates osteomyelitis) Immunophenotype- CD99, anti FLI1 and ERG antibodies Genetics- t(11;22)(q24;q12), t(21;22)(q22;q12). 52 Gross- tan-grey in colour, destructive borders with invasive margins with areas of necrosis and haemorrhage. M/Ea)Classical Ewing- uniform, small round cells with PASpositive, scant clear or eosinophilic cytoplasm. b) Atypical Ewing- large cells, prominent nucleoli and irregular contour Cytology- dissociated cells and clusters of loosely cohesive cells - Two cell types-large pale cells and small dark cells -Abundant cytoplasmic glycogen -Occasionally rosette-like structures 53 Typical ONION PEEL multilayered appearance of periosteal new bone formation along the cortices. The tumor is poorly defined and invades into the soft tissues, forming a subtle mass Typical thin, linear, HAIR ON END / SUNBURST PERIOSTEAL REACTION around a highly permeative, aggressive tumor. A CODMAN TRIANGLE is present along the medial proximal cortex 54 Cytology-mixture of cells with Large pale staining nuclei and Cells with small, dark nuclei; Note cytoplasmc vacoules and clear spaces in large cell cytoplasm Individual cells have round nuclei with indentation, finely dispersed chromatin, small nucleoli, variable mitotic activity and clear cytoplasm caused by intracytoplasmic glycogen. 55 Ewing sarcoma arising in the medullary cavity permeates the cortex and extends to the surface . Prominent HOMER WRIGHT ROSETTE formations 56 TUMOR IHC GENETIC DIFFERENTIAL DIAGNOSIS EWING’S SARCOMA • • • 1. • CD99(0-13, HBA-74) FLI-1, ERG antibodies sensitive not specific CD3,20,34,45 and TDT negative • • LYMPHOMA • • • Reciprocal translocation between Ch11 &22 and between 21 &22 Translocations of Ch 7 & 22, 17 & 22, 2 & 22 Inversion of Ch22 DLBCL:CD45 & CD20, CD79a, PAX5+ ALCL:CD30+, EMA, CD3, CD4, ALK1 + lymphoblastic lymphoma:CD99+, TdT, PAX5, CD34, CD79a S100(cartilage MESENCHYMAL CHONDROSARCO component) CD99(small cells) MA SOX9, osteocalcin + Translocation not seen 2. 3. 4. 5. 6. Lymphoblastic Lymphoma Osteomyelitis Metastatic neuroblastoma Mesenchymal chondrosarcoma Small cell osteosarcoma Embryonal rhabdomyosarcoma 1. 2. 3. 4. Ewings sarcoma Metastatic carcinoma Myeloma Sarcoma in tumours with extensive fibrosis 1. Chondroblastic osteosarcoma Ewing sarcoma Dedifferentiated chondrosarcoma 2. 3. 57 GIANT CELL RICH TUMOURS GIANT CELL RICH LESION OF SMALL BONE GIANT CELL TUMOUR OF BONE 58 Giant cell tumour age- >20 yrs, F>M Site- epiphysis and metaphysis of long bones Symptoms- pain, swelling Radiology- well defined, expansile, eccentric , osteolytic lesion Immunophenotype- vitronectin receptor(CD51), weak positivity for CD45,CD33, CD 68 Genetics- IDH2-R172S mutation, H3F3A gene mutation 59 Gross- c/s solid or friable, variegated red-brown and yellow appearence; hemorrhage and necrosis; thin cortex with reactive bone M/E- 2 main component-Stromal cells- mononuclear, round to oval to spindle shaped -Giant cells- large number of osteoclast like giant cells (>20 nuclei)uniformly scattered in stromal cells - Secondary changes- hemorrhage, necrosis, fibrohistiocytic change, aneurysmal bone cyst, hemosiderin deposition Cytology- cellular smear, -dual population of osteoclast giant cells and mononuclear spindle cells, -giant cells attached to periphery of cluster of spindle cells 60 The tumor is radiolucent and destroys the lateral cortex. Cytology- showing cluster of spindle cells with giant cell at periphery 61 GCT of bone has destroyed the cortex and displaced the periosteum, which has produced a thin shell of reactive woven bone rimmed by osteoblasts . GCT is composed of many large multinucleated osteoclast-type giant cells. The giant cells contain numerous nuclei that are similar in appearance to the nuclei in the neoplastic mononuclear cells. 62 TUMORS IHC S100, CD1a LANGERHANS Langerin+ CELL HISTIOCYTOSIS CD68+ Negative CD45,AE1/3, CD15 and CD30 GIANT CELL LESION OF BONE P63+ GIANT CELL TUMOR OF BONE RANK P63 GENETIC STUDIES Recurrent abn of chromosomal loci 9p and 22q DIFFERENTIAL DIAGNOSIS 1. 2. 3. 4. 5. Osteomyelitis Granulomatous inflammation HL NHL Fibrohistiocytic lesions of bone 1. USP6 rearrangement 2. Giant cell tumor of bone Aneurysmal bone cyst Nonossifying fibroma Ossifying fibroma 1. Mutation in H3F3A histone 2. 3. gene Aneurysmal bone cyst Benign fibrous histiocytoma Chondroblastoma Giant cell rich osteosarcoma 3. 4. 4. 63 Notochordal tumours-CHORDOMA • Primary low grade malignant tumor of bone showing notochordal differentiation • Site: Axial skeleton, base of skull, sacrococcyx • Gross- expansile, lobulated structure, c/s is slate-grey, gelatinous matrix • M/E- a) chordoma,NOS- large cells with clear to eosinophilic cytoplasm, separated by fibrous sepate into lobules. b) chondroid chordoma- Tumor with areas of conventional chordoma and regions resembling lowgrade, hyaline-type chondrosarcoma c) Dedifferentiated chordoma- biphasic tumour with features of chordoma, NOS and high grade 64 undifferentiated spindle cell tumour TUMOR CELLS lobular growth pattern separated by fibrous septa. The stroma is usually prominent, basophilic, and myxoid in appearance and contains abundant glycosaminoglycans. The tumor cells are arranged in cords and aggregates, variable in size. Classic chordoma cells are large, polyhedral, contain abundant eosinophilic cytoplasm , and have oval to round nuclei with fine chromatin. 65 NUCLEI WITH PROMINENT NUCLEOLI VACUOLES HYALINE CARTILAGE TUMOR CELLS Characteristic of chordoma is the PHYSALIPHOROUS CELL.The cell contains intracytoplasmic, sharp, clear vacuoles , which cause it to have a bubbly appearance . The cell nuclei may contain prominent nucleoli. The tumor is composed of conventional chordoma with areas that closely resemble neoplastic hyaline cartilage. In the chondroid regions, the cells are distributed singly and reside in lacunar spaces 66 ANEURYSMAL BONE CYST CYSTIC LESIONS SIMPLE BONE CYST FIBROUS DYSPLASIA 67 ANEURYSMAL BONE CYST Age and sex- 10-20 yrs; F>M Site- vertebrae and flat bones Radiology- radiolucent lesion, thin cortex, covered by thin shell of reactive bone Gross- hemorrhagic mass covered by thin shell of reactive bone M/E- large blood filled spaces, separated by cellular septa containing inflammatory cells, fibrovascular tisssue, giant cells, foci of osteoid and bone D/D-Giant cell tumour Simple bone cyst hemangioma Telangiectatic Osteosarcoma Genetics- USP6 gene on chr 17 68 ABC shows a cellular neoplasm with multiple bloodfilled cystic spaces. The tumor is arising in the medullary cavity of the bone and scallops the inner surface of the cortex. Note the solid portion of the tumor The wall of an ABC displays reactive woven bone that is blue-purple in color (so called BLUE BONE). The bone has osteoblastic rimming and the wall contains bland, spindle-shaped cells and scattered osteoclast-type giant cells. 69 SIMPLE BONE CYST / UNICAMERAL BONE CYST Benign, intraosseous, fluid-filled, fibrous walled cyst. FIBROBLASTS FIBROBLASTS CEMENTUM The cyst wall is composed of spindled fibroblasts and collagen. Note that fibroblasts line the surface st of the cyst wall, mimicking a true epithelial cyst lining. The underlying endosteal surface of the cortex has an undulating contour. The wall of a UBC is distorted by abundant intramural fibrin. Fibrin is commonly seen in the walls of UBC and can histologically mimic cementum and neoplastic bone. The luminal portion is lined by a thin layer of fibroblasts 70 Fibrous dysplsia Benign, fibro-osseous lesion Age- children and adults Sex- M=F Site- craniofacial and femur Gross- bone is expanded, tan-grey in colour, firm to gritty in consistency M/E- a)Fibrous component- bland, fibroblastic cells b)Osseous component- irregular, curvilinear, trabeculae of woven bone 71 Bland fibrous background with curvilinear fragments of trabecular bone, no osteoblastic rimming 72 CYSTIC LESIONS IHC/ genetic studies SIMPLE BONE CYST DIFFERENTIAL DIAGNOSIS 1. ABC 2. Intraosseous ganglion ANEURYSMAL BONE CYST • CDH11-USP6 fusion genes +(detected by FISH) • Spindle fibroblasts: SMA+ • Osteoclast: CD68+ FIBROUS DYSPLASIA Missense mutation in GNAS gene(20q13) 1. Telangiectatic osteosarcoma 2. Giant cell tumor 3. Chondroblastoma 4. Osteoblastoma 5. Simple bone cyst 6. Giant cell reparative granuloma 73 Thank you 74