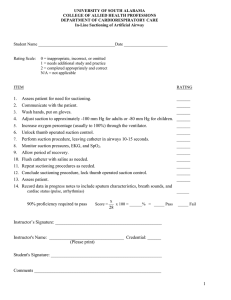
Factors affecting learning: perceived benefit, cognitive and physical ability, active participation, age and education level appropriate methods. Barriers to learning are fear, anxiety, depression, physical discomfort, pain, fatigue, sensory and perceptual deficits, psychomotor deficits. Registered dietician: assess, plans for and educates regarding nutrition needs. Examples of when to refer: A client has low albumin level, and recently had unexplained weight loss. Occupational therapist: assess and plans for client to regain activities of daily (ADL) skills, especially motor skills of the upper extremities. Psychomotor learning takes place when clients practice preparing insulin injections. General adaptation syndrome known as “stress syndrome” has 3 stages: - alarm stage - resistance stage - exhaustion stage Adherence: commitment and ability of the client and family to follow a treatment regimen. Negative coping mechanisms can cause nonadherence. Sick role: expectations of others and society regarding how one should behave when sick. Chest physiotherapy: involves the use of chest percussion, vibration, postural drainage to help mobilize secretions. Chest percussion and vibration facilitate movement of secretions in the central airways. For postural drainage, one or more positions allow gravity to assist with the removal of secretions from specific areas of the lungs. Nursing actions for chest physiotherapy: collect sputum specimens by suctioning during coughing Whenever possible, encourage coughing. Coughing is more effective than artificial suctioning at moving secretions in the upper trachea and laryngopharynx. Suction orally, nasally, endotracheally, not routinely but only as needed. Maintain surgical asepsis when performing any form of tracheal suctioning to avoid bacterial contamination of the airways. Vibration: use of shaking movement during exhalation to help move secretions Percussion: use of cupped hands to clap rhythmically on the chest to break up secretions Older patients: decreased respiratory muscle strength, chest wall compliances => higher risk for aspiration. Use medical asepsis for suctioning of the mouth Use surgical asepsis for other types of suctioning. Suction no more than 120 mmHg Limit suction attempt no longer than 10-15 seconds Modifications to improve home safety: remove items that can cause the client to trip such as throw rugs or loose carpets. Place electrical cords and extension cords against a wall behind furniture. Monitor gait and balance. Provide aids PRN. Grab bars near the toilet and in the tub or shower. Use a nonskid mat in the tub or shower. Place a shower chair in the shower. Provide a bedside commode PRN and adequate lighting. Have a family exit plan for fires. Review oxygen safety measures. For hearing loss patient: advise patient to keep the volume as low as possible when wearing headphones. Wear ear protection for loud noise exposure. Client education for hearing aids: - Use the lowest setting that allows hearing without feedback - When the hearing is not in use, turn it off and remove the battery to conserve battery power. Avoid corrosion of hearing aid. - Use mild soap and water to clean the ear mold while keeping the hearing aid dry. Patient self-centered care for body image: - Establish a therapeutic relationship with the client. - Ensure privacy and confidentiality. Let the client know sensitive issues are safe to discuss - Arrange for a visit from a volunteer who has experienced a similar issue.