Fluid & Electrolyte Balance: Lecture Notes on Arrhythmias
advertisement

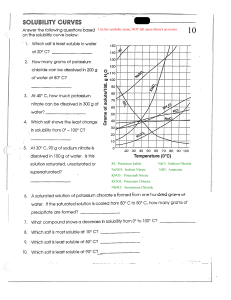
MS 1 Fluid Compartments Fluid and electrolytes • • • Body fluids - Male: LALAKI (6 letters) 60% (made out of muscle) Female: BABAE 50% (made out of fats) Intravascular / Extracellular o IV (Plasma) o Outside the cell o The only one that is measurable Intracellular o Inside the cell o Has the same manifestations as intracellular and interstitial Interstitial o In between the cell o Has the same manifestations as intracellular and interstitial o If no fluid is present in the interstitial, then there is no intracellular fluid Who is prone to dehydration? Male - Infant: BATA-BATA 80% fluid Priority of hydration: infant (then geriatric) male female “IV FLUIDS” Hypertonic - Geria- thirst regulating center (hypothalamus) is delayed More than 0.9% o D50 water (because 50%) o D10 water (because 10%) o o D5LRS (because 5%) D5NM (because 5%) ❖ What is the first sign of o dehydration? Constipation ❖ Where are you supposed to check for skin turgor in the elderly? D5 0.9% NaCl / D5NSS (because 50% dextrose) o D5 0.45% NaCl / D5 half saline solution Board Question: Clavicle - D50W – given for hypoglycemics ;; very high sugar content – note that sugar loves water, so more fluid in the extracellular compartment == too little fluid in cell / cellular dehydration, which is more dangerous - Too much hypertonic solution: o Hypervolemia o Hypertension o Polyuria o Cell will shrink / Cellular dehydration o - Too much isotonic / fast drip o Fluid concentration is increased = Signs of fluid excess o Hypervolemia = high fluid in blood vessels Dry mouth (mouth is made o up of cells) Hypertension = high fluid high pressure o Polydipsia o Rales or crackles o Dry skin o Dyspnea – sign of fluid o Altered mental status (due to dehydrated brain cells) Disorientation (confusion) o overload Pulmonary edema – signs include rales and dyspnea o - Too little isotonic o Weak concentration = signs of fluid deficit o Hypovolemia o o o o Hypotension → become prone to shock Shock (hypovolemic) Dehydration Oliguria Isotonic - Concentration is 0.9% o ALL PLAINS o - plain NSS is 0.9% sodium chloride o Plain LRS o D5W 200 ml There is EQUAL shifting between the Intra and extracellular spaces. Hypotonic - less than 0.9% o 0.25% NaCl (because 0.25%) 0.33% NaCl (because 0.33%) o 0.45% NaCl o D5W higher than 200 ml 0/33% NaCl – very low sodium concentration in the blood vessel, o - so fluid moves towards the cell (cellular hydration) → hypovolemia BON: What is a complication of shock? Renal failure Can you use lotion as a diabetic patient? Yes, due to dry skin, except in between the toes and areas of skin breakdown. o BP is low o Hypotension → hypovolemic During the emergent phase of burns, what do you transfuse? Isotonic PLRS o shock Decreased blood flow to the kidney → oliguria - Cellular hydration – swelling cell o Edema o Ascites o Cerebral edema - Mannitol o It helps you make more urine and to lose salt and excess water from your body. It treats swelling from heart, kidney, or liver disease. It also treats swelling around the brain or in the eyes. Newly inserted D5W is isotonic pH - (normal) 7.35-7.45 PCo2 - 35 – 45 Placement of electrolytes PISO - ELECTROLYTES - - Most abundant in the cell – Potassium (INTRACELLULAR) Most abundant electrolyte in the blood vessel – Sodium (OUTSIDE THE CELL) Interstitial – calcium Sodium (Na+) - 135 – 145 MEQ Potassium (K+) - 3.5 – 4.5 (5.5) MEQ Calcium (Ca+) - 4.5 – 5.5 MEQ - (when ka mu-inom ug gatas – morning + evening) 8-10 mg/dl Magnesium (Mg+) - 1.5 -2.5 MEQ Meeting of sodium and potassium pumping -- (action potential) – cause muscle contraction – of course, if they stop, there is muscle relaxation - This is also what carries stimulus to the brain. muscles in the hand and wrist (i.e., carpopedal spasm) that occurs after the compression of the upper arm with a blood pressure cuff. Hypercalcemia prevents pumping, thus there is decreased muscle contraction. - Bradycardia Hypoventilation Decreased alertness Drowsiness (that’s why you drink - milk) Muscle weakness Hypocalcemia – there is a lot of contraction - Tachycardia Hyperventilation Increased alertness Insomnia - Muscle spasms - The Chvostek sign is a clinical finding associated with hypocalcemia, or low levels of calcium in the blood. This clinical sign refers to a twitch of the facial muscles that occurs when gently tapping an individual's cheek, in front of the ear. - Tetany Trousseau's sign refers to the involuntary contraction of the Normal Sodium 135-145 MEQ Hypernatremia - Sodium attracts water Thus, there is an increase in fluids in the extracellular area Signs of hypertonic are signs of hypernatremia o Hypervolemia o Hypertension o o Cellular dehydration Polyuria – leads to dehydrated cell and blood - vessel Nursing diagnosis: fluid volume - deficit due to polyuria Plan of care: o o Low in sodium Increase fluid intake to o dilute sodium Give hypotonic IVF o Give hypertonic IVF + fast drip isotonic (NSS) Hyponatremia - Too little sodium, too little attraction - thus, fluid goes into the cell signs of hypotonic are signs of hyponatremia o hypovolemia o hypotension o oliguria o edema o ascites nursing diagnosis: fluid volume excess because there is retention - - of fluid in the cells, which are not removed by the kidneys/urinated Plan of Care: o High in sodium diet ▪ ▪ o Normal Potassium 3.5 – 4.5(5.5) MEQ, if international can be up to 6 - NaCl (table salt) MSG (monosodium glutamate) ▪ NaHCo3 ▪ Na Nitrate (processed foods) Restrict fluids Potassium maintains cardiac contraction o Contraction of smooth muscle (internal organs ex. Heart, GIT) o - The most life threatening electrolyte is potassium. Calcium initiates cardiac contraction Hyperkalemia - - - - ▪ Drug of choice: kayexalate Can be caused by renal failure or burns Fast heart contractility o o Tachycardia Arrhythmia o Cardiac arrest ▪ • ▪ effect of calcium (stops sodium- o (given if the patient is diabetic) ▪ D5W + D50W + insulin ▪ ▪ ▪ FIRST Decreases heart rate and thus preventing o arrythmias Kayexelate (Sodium Polysterene / Na Polysterene) Increases the blood sugar to decrease potassium, because potassium follows glucose into the cell Effect in 30 mins Hypokalemia - potassium pump) … thus you should administer this Effect is within 6-8 hours Glucose insulin infusion ▪ administration: Calcium gluconate – glucose insulin o o Hypernatremi a hypokalemia (complication) o Abdominal cramping Affects upper extremities o Increased hyperactivity of the heart and the brain Plan of care: o Order of med o Hypokalemia Side effect: • Increased peristalsis o Diarrhea → could lead to infusion – kayexalate Furosemide – potassium wasting diuretic Diet: low in potassium Antidote: Calcium Gluconate ▪ It antagonizes the Exchanges its sodium into potassium and excretes it into the stool Expected effect: - Decreased cardiac contraction o Bradycardia o Arrhythmia (sinus bradycardia) o Cardiac arrest Decreased peristalsis o Constipation o Abdominal distension o Paralytic ileus (adynamic ileus) ▪ + 20MEQ KCl (post abdominal surgery) to promote peristalsis - - Affects lower extremities o Muscle weakness o Fatigue o Apathy Plan of care: o Diet high in potassium Monitor VS, especially HR, because only the doctor can obtain an ECG. (ABC) o ▪ Apple, Avocado ▪ Banana ▪ Citrus fruits ▪ Ka remember sad ko before na all above ground are high in potassium, all below ground high in sodium Drug of choice ▪ ▪ ORAL: Kalium durule (potassium tablets) IV: KCL • never give IV push • incorporate in IV or via solu-set - Widening of QRS – hyperkalemia Narrowing of QRS - hypokalemia ST elevation – hyperkalemia ST depression - hypokalemia Flattened T wave – hypokalemia Tall or Peaked T wave hyperkalemia The presence of u-wave indicates hypokalemia. This also indicates digitalis toxicity. NORMAL CALCIUM: 4.5 – 5.5 MEQ OR 8-10 MG/DL - initiates cardiac contraction - responsible for the contraction of - the large and skeletal muscles largest amount in the bone the effect of calcium is the opposite to potassium o high potassium in the blood = increase muscle contraction o high calcium in the blood = decrease in muscle contraction Hypercalcemia - - decreased muscle contraction / there is muscle relaxation o bradycardia o hypoventilation o o decreased alertness drowsiness o lethargy o o muscle weakness apathy Trousseau's sign – carpopedal spasms Plan of care: o Diet high in calcium (milk and dairy products) o Vitamin D helps absorb o - calcium o Calcium supplement o Drug of Choice: Calcium Gluconate o renal calculi (stone) plan of care: o diet low in calcium o increased fluid intake (due to renal calculi) o vitamins C to increase acidity or neutralize the alkaline (because hypocalcemia is alkaline // o note milk) drug of choice: magnesium sulfate Hypocalcemia - muscle contraction is increased o o o tachycardia hyperventilation increased alertness o o insomnia muscle spasms o o leg cramps fatigue o o osteoporosis Chvostek – facial twitching o Tetany – extreme facial twitching (more extreme hypocalcemia) What controls the BP? Sodium Cardiovascular Disorders “ARRHYTHMIAS” - - 50-200 joules, maximum of 3 – 4 attempts (50, 100, 150, 200) Synchronized (synch mode) to the R wave == meaning you deliver a shock on the R wave What indicates effective cardioversion? When the P wave returns to normal - Defibrillators - - flutter o Has 2 paddles o 1 paddle on the sternum (labeled) o 1 paddle on the apex (labeled) Considerations/ Nursing Safety; o Shave the area (chest) – o o Atrial fibrillation and atrial o ▪ ▪ ▪ Procainamide (Pronestyl) Quinidine Anti-coagulant (heparin /coumadin) optional Apply gel on the paddles to prevent burning of the skin Clear the area – be sure no one is touching the patient, anyone touching might die from the 360 joules introduced; thus, this is the most significant Complication is thrombus / clot formation Drug of Choice: Defibrillation - Indicated in ventricular arrhythmias Problem in the QRS complex 200 – 360 joules (200, 250, 300, 360) maximum of 4 attempts = larger because the ventricles are larger Cardioversion - Indicated in atrial arrhythmias Problem in the P wave No need to synchronize Drug of Choice: ▪ Magnesium Sulfate ▪ Lidocaine Followed by Ventricular fibrillation o (-) breathing & (-) pulse o Cardiac arrest o - o P wave is atrial depolarization QRS wave is ventricular depolarization Defibrillation first before CPR - Lastly, asystole (PEA – pulseless electrical activity) o o o No breathing no pulse Cardiac arrest CPR first then defibrillation Cardiac arrest - This arrhythmia is seen before - cardiac arrest. - Starts with Ventricular tachycardia o Wide and bizarre QRS o (-) Breathing & (+) Pulse o Respiratory Arrest o Needs rescue breathing ▪ Conscious – can no longer talk but can feel the treatment being given – can only give low energy ▪ (cardioversion) Unconscious – can no longer feel - ▪ ▪ (defibrillation) (+) pulse (ideal) – cardioversion (-) pulse – defibrillation because this will increase cardiac contractility Acid base imbalance: metabolic acidosis (due to cell deprivation of O2// blood is no longer moving, therefore no exchange of O2) o Drug of choice: sodium bicarbonate – this will reverse the acidosis Never electrocute the heart without electrical activity. Myocardial Infarction - Common cause: thrombus - formation (clot formation), coronary artery thrombosis Most commonly affected part of treatment – can give high energy Drug of Choice: epinephrine – the heart: left ventricle because - it has the thickest myocardium Major manifestation: chest pain Characteristic: chest tightness o Universal sign: levine sign = chest-hand clutching Complications of MI: o Most life-threatening a. Manifested by ST elevation b. STEMI (ST elevation MI) i. Presence of extensive damage c. Non-STEMI (Non-ST elevation MI) o - complication: ventricular i. Negative for arrhythmia / dysrhythmia ▪ The most unstable is extensive damage 3. Infarction (Occlusion) within the first 6-8 ▪ - o PVC Most specific and most sensitive diagnostic test: TROPONIN I o Sensitive – result within 1-3 o - hours Safest time is after 24-48 hours hours and remains elevated up to 7 days Specific – only becomes positive once presence of tissue necrosis ▪ Angina still has no a. Pathologic Q-wave PVC = premature ventricular contraction - tissue necrosis Most commonly used to diagnosed MI: ECG o Findings: look for the zones of MI - Contains no P waves Bizarre QRS Widening of the QRS Need to count = 6-8 PVCS per minute should be reported Trigeminal PVC – should also be reported 1st line drug: o Lidocaine o Xylocaine ▪ Both of these decreases the heart rate (bradycardia) PVC with Bradycardia o - Atropine sulfate – an anticholinergic 2nd line drug: when the first line drugs are not available o Amiodarone o Cordarone Three Zones of MI 1. Ischemia (low O2) a. Inverted T wave 2. Injury (Cardiac Damage) MS 2 o o o MYOCARDIAL INFARCTION Oxygen Nitroglycerin Aspirin = this is antiplatelet Occlusion: - - - Thrombus formation o Most common cause of MI Atherosclerosis – plaque formation - Arteriosclerosis – hardening of plaques Priority: o Morphine Sulfate – narcotic analgesic ▪ Analgesic is to relieve pain ▪ Narcotic is a CNS depressant (makes ▪ ▪ ▪ brain sleep) – reduces anxiety, muscle relaxant, main use in MI is decreasing O2 demand thereby decreasing oxygen consumption Leads to respiratory depression Decreased RR = check RR, hold if less than 12 BPM Antidote: Narcan Myocardial Ischemia/ Myocardial Insufficiency - relieve ischemia in the myocardium o 1-5 LPM nasal cannula o 5-10 LPM (high flow) face mask o Can also be used for - Caused by Myocardial Ischemia - Relieved by oxygen BON: - which is also a narcotic What oxygen is initially given for MI? High Oxygen 6-8 Liters to saturate the ischemic myocardium - Demerol (Meperidine) Respiratory alkalosis – use rebreather Chest Pain (Naloxone) • Seen as an inverted T wave Insufficient oxygen High flow O2 (6-8L) is given to What is priority first for MI? Morphine - What is most commonly used first? Oxygen - Drug of choice for angina – nitroglycerin If the cause is due to thrombus o MONAT ▪ Thrombolytics – to dissolve thrombus ▪ Streptokinase ▪ t-PA (tissue- - 3 tablets at 5 minutes interval o Give for anginal pain o Pain unrelieved by Nitroglycerin, it may be MI MorPhine Sulfate – anticipate MI - Aspirin Thrombolytics Heparin o o plasminogen Complication: causes bleeding activator) - if due to hypertension o MONA + Beta Blockers ▪ To treat ▪ ▪ hypertension All -olol Propanolol Three types of Angina - - - Stable (typical) o Predictable pain o Occurs on activity Unstable (atypical) o Unpredictable pain o Often occurs at rest Prinzmetal (variant) o Exposure to cold o Vasospasm Nitroglycerine – cardiac nitrates ANGINA or UNKNOWN CHEST PAIN - Effect: vasodilatation - Side effect: hypotension Check: o Blood pressure = hold if systolic BP is less than Priority RONPATH - - Rest (sit) – same as morphine, to decrease O2 demand and O2 consumption - 100mmHg Headache – most common Oxygen administration (high) – to saturate the ischemic myocardium - complaint upon the 1st take Route: tablets sublingual (under o - Give for chest pain Nitroglycerine – drug of choice for angina the tongue) o The largest blood vessel is sublingual - - Burning / tingling sensation under the tongue is normal, this indicates vasodilatation Give three tablets at five-minute interval Nitroglycerin spray is used the Partial Thromboplastin time (ptt [looks like an H ang duha ka t]) Coumadin (warfarin) [in war there is killing] ▪ - same as the tablets o If you accidentally do 2 sprays at the same time, o Antidote: Vitamin K o INR (international Normalize Ratio) consider that as second - dose, give the last/ 3rd spray after 5 minutes. Stored in dark and air tight container due to photosensitivity Storage is only up to 6 months. Should be taken before any strenuous activity (since these increase O2 consumption) Prothrombin Time (pt) normal value: 1012 seconds Partial Thromboplastin time (ptt) normal value: 30-45 seconds International Normalize Ratio (INR): 12 seconds MI sex: - Anticoagulants - Only prevent blood from furthering clotting / clot formation - Heparin (in heaven there is peace) o Antidote: protamine sulfate o Check lab: Can resume sex after 6-wks post MI when they are able to climb at least 2 flights of stairs without SOB - sex before eating - non-weight bearing Left Sided Congestive Heart Failure 1. Complication of MI 2. These is tissue necrosis in the left CONGESTIVE HEART FAILURE Signs and Symptoms ventricle, making it unable to pump blood out, thus there is backflow back into the lungs. 3. Manifestations are related to the lungs 1. presence of S3 – ventricular gallop 2. “Murmur” 3. FAILURE – L first before R, you can see left sided failure manifestations before right sided failure Right Sided Congestive Heart Failure o o Breathing manifestations ▪ Dyspnea ▪ Orthopnea ▪ Rales / crackles ▪ Pulmonary edema Decreased cardiac output ▪ Fainting ▪ 1. Complication of COPD 2. There is mitral stenosis, leading to backflow of blood towards the system 3. There should be systemic manifestations o These can all be seen by the naked eye o Jugular vein distension o o Distended neck veins Cardiac cirrhosis – ischemic liver ▪ o o Edema ▪ ▪ Ascites Jaundice ▪ Hepatomegaly Oliguria Weight gain Laennec’s cirrhosis if due to alcohol ang liver cirrhosis. ▪ ▪ ▪ ▪ ▪ Syncope due to decreased brain blood Dizziness Light-headedness Weakness Fatigue Apathy Plan of Care for CHF • Goal: To decrease cardiac workload → to decrease O2 consumption o Bedrest o Diazepam (Valium) ▪ Sedatives ▪ • • higher the better due to dyspnea (sitting, upright, high backrest) Muscle relaxant Increase cardiac output o Digoxin / Lanoxin → Right CHF = position of choice: LOW FOWLERS/ 30 degrees angle – to measure the jugular vein distension Digitalis: ▪ Decrease HR • Check apical pulse, hold if less than 60 bpm ▪ Increase cardiac ▪ ▪ will increase: expect polyguria (diuresis) // normal • Report for oliguria – indicates toxicity ▪ o /overdose Potassium wasting • Complication: hypokalemia More than 4 cm JVD is indicative of Right-sded CHF POC if general: high fowlers because left sided CHF is always seen first contractility Increase force of ventricular contraction Increase Cardiac output • Blood flow to the kidney (note presence of u-wave) ▪ Do not give together with Furosemide Left CHF= position of choice, the • • Give oxygen to left sided CHF Restrict fluids due to fluid excess • Restrict sodium because sodium causes water retention Diuretics = to eliminate excess • fluid o Effective if there is clear lung sounds or absence of crackles upon auscultation Signs of Digitalis Toxicity / Overdose [BANDAV] where ANDA is all GI • • • Bradycardia Anorexia (loss of appetite) Nausea = 1st sign • • Diarrhea Abdominal cramping • Visual disturbance o - - vision Antidote of Digoxin: DIGIBIND • IMMUNO FAB o productive cough o airway problem (problem oxygen entering) Wil complain of seeing the color green or yellow halo • Cough is common in the morning / early morning cough (smoker’s cough) s/s: o inflammation of the bronchus - o dyspnea with cyanosis o o o “Blue Bloaters” Fat Dyspnea at rest Breathing technique: diaphragmatic breathing Emphysema - RESPIRATORY DISORDERS: COPD / CAL (Chronic Airflow / Airway Limitation) - - Common cause: smoking Common cause: chronic bronchitis, asthma, congenital (rare – smoker mother) Over-distension of the alveoli that eventually leads to rupture → collapse of the alveoli → hypoxia Non-productive cough s/s o overdistension of the alveoli o o Asthma no longer counted because it is reversible. expansion (problem with Chronic Bronchitis - Common cause: smoking - Inflammation of the bronchus with accumulation of secretions - Productive cough that lasts for 3 months in 2 consecutive years non-productive cough breathing problem – lung o o o - CO2 not going out) dyspnea without cyanosis (because here you can’t take CO2 out) “Pink Puffers” Thin but with barrel chest o Dyspnea on activity Breathing technique: pursed lip breathing - o Upright o High back rest Drug of choice o Bronchodilators ▪ Salbutamol (Ventolin) o Steroids (antiinflammatories) o Cough medications ▪ suppresses cough (ex. Dextromethorphan, BON: - - - - What breath sounds will the nurse auscultate in COPD? Diminished breathe sounds due to collapsed alveoli. Acid base imbalance in COPD? ▪ Respiratory Acidosis due to CO2 retention o Hypoventilation If CO2 is high → patient breaths only at low level of oxygen (hypoxic drive) if CO2 is high and O2 is also high then breathing will be suppressed → apnea (complication) Antitussive – ▪ - codeine) Mucolytics – liquifies secretions (ex. Mucomyst /mucosolvan, Carbocysteine, nacetylcysteine) Expectorants – expels secretions (ex. Guiafenesine, rubitussin) Encourage coughing and deep breathing - Increase fluid intake to liquify secretions - Decreased O2 admin = safest is 2LPM via venturi mask (most accurate) o Plan of Care for COPD - Position of choice: o orthopneic (sitting + leaning forward) BEST! o Sitting - Nasal cannula (most comfortable) Promote rest Diet o Should be small frequent meals o Composed of: ▪ ▪ ▪ calorie (HIGH to provide energy), carbohydrates (LOW, because the more carbohydrates, the more CO2 – cns - - Care: Check the patient’s heart rate Initial Action: Stop the source Priority: safety of victim and rescuer You will die from arrhythmia depressant) - Check heart rate protein (HIGH to - Lightning – when thunder roars, go - help in the inside, hands and feet must touch absorption of the ground bronchodilators) o THIS IS WHERE WE STOPPED OUR ANKI After struck by lightning, not electrically charge, can touch (NAG-brownout – check nalang ang screenshot) BURNS Types: Thermal Burn - Chemical Burn Due to exposure to hot surfaces NLE: What to do when a small - portion of the body area is exposed to burn? Put on running water - Due to strong acid NLE: evidence o o Management: o Powder Chemical Burn ▪ Scrape ▪ Remove with a brush o Liquid Chemical Burn (ex. Electrical Burn - Due to exposure of electrical - source Life-threatening complication: arrhythmia Liquefaction necrosis Presence of stain Liquid sosa?) ▪ Flood with water for at least 20 mins - Radiation Burn - UV exposure (ex. Sun burn, o Presence of blisters Examples o Ulceration o Scalding – boiling water radiation therapy) - Management o Apply cold packs o Avoid alcohol, lotion, powder FULL THICKNESS - Here nerves are already damaged → painless 3rd degree - Epidermis + dermis + subcutaneous tissue White eschar 4th degree Degrees of Burn - This can also be used for bedsores PARTIAL THICKNESS 1st degree (superficial partial) - Epidermis S/S: o Signs of inflammation [PRS] ▪ ▪ ▪ - Painful Redness Swelling Best example: sun burn o Exfoliation o Dermatitis 2nd degree (deep partial) - Epidermis + Dermis - S/S o The most painful - Epidermis + Dermis + - Subcutaneous tissue + Muscle (Bone) Black Eschar Charred Eschar Constrictures – stiffening of the muscles o Management: range of motion exercises Eschar is fresh - EJ Basically eschar is still healing, scab if dry nya naa nay like coagulation, then scar na after - PHASE OF BURNS Fluid will shift back from interstitial into blood vessel o Hypervolemia o Increase bp from previously low BP, not necessarily hypertension o Polyuria (diuresis) o Hemodilution o Decreased viscosity of blood st A: Emergent Phase (occurs 1 48 hours) - Stage of shock - Stage of fluid shift Priority here is fluid replacement Fluids shift from IV (plasma) → to interstitial o Blood vessel fluid is low (hypovolemia) o o o o BP is low (prone to shock: hypovolemic shock) Oliguria (due to decreased fluid going to the kidney) Hemoconcentration Blood viscosity is high – prone to thrombus – management is IV fluid o o replacement Increased hematocrit Hyperkalemia (metabolic acidosis) o Hyponatremia (because sodium rushed into the cells, basically mura daw siyag fireman) o o Low HCT Hypokalemia (Metabolic Alkalosis) o Hyponatremia because sodium is excreted through diuresis C: Recovery Phase (5-6 days after) - Hypokalemia (all potassium are in - the cell; potassium is used in cellular repair) Hypocalcemia (calcium is used in - scar formation) Priority: o Pain management: DOC: Narcotic analgesic OR Morphine Sulfate o B: Diuretic Phase (occurs after 48 hours) - Stage of fluid remobilization Prevent infection: reverse isolation + private room + hand washing + DOC: antibiotic as cream [causative agent is pseudomonas → sulfamylon penetrates in the skin + painful, so need to administer analgesic 30 mins to 1 hour before application] ▪ Best Way to apply antibiotic Cream? With gloved hands to control the pressure Alarm - Press the fire alarm Scream/ Yell “Help!” Confine or contain the fire - Close the door Extinguish the fire - H2O Fire extinguisher If immunosuppressed: private room If you are infectious: isolation room Collaborative Management in Burn Cases: 1. On the scene o Priority: o Use only on onset of fire o o o o o Use the abbreviation PASS Pull the pin Aim low Squeeze the lever Sweeping manner IF OUTSIDE [ARCE] Alarm Rescue Confine Extinguish Small Fire: - IF INSIDE [RACE} Rescue Waste basket Fire is not taller than you Priority is Extinguish 2. After the burn process: o Priority → establish airway o - Remove the victim (if the patient is on fire) tell them - to drop and roll on the floor Throw a blanket Check for stridor, hoarseness, wheezing == all o o these indicate laryngospasms Restlessness – indicates hypoxia Cherry red mucus – indicates smoke inhalation 3. On emergent phase (stage of 4ml PLRS x % of Burns (TBSA) x wt (kg) = 24 hours Example: 4ml PLRS x 31.5% x 50kgs = 6300 ml (24 hours 1st 8H (transfuse 50%) -- 3150 ml shock) o 3rd: Parklands Rule/ Hartmann’s Rule Priority: fluid resuscitation / replacement o IVF PLRS (Crystalloid – o hyper hypo iso) Effective if there is normal hematocrit – indicates adequate fluid STEPS IN FLUID REPLACEMENT 1st: get the weight in kilograms 2nd: apply the rule of 9 The remaining 1% is the genital. Entire chest is 9. Half of chest is 4.5. 2nd 8H (transfuse 25%) – 1575 ml 3rd 8H (transfuse 25%) – 1575 ml 6300 ml = transfused at 7AM How much was transfused at 11 PM? 4725 ml