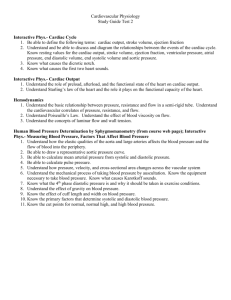
Heart Failure Karen Ruffin RN, MSN Ed. Incidence and Prevalence of Heart Failure • Leading cause of death in the US • More than 5 million Americans are living with heart failure, and 550,000 new cases are diagnosed each year. • About 250,000 people a year die from heart disease. • That means more than 680 Americans a day die from it!!!!!!!! • Women have a poorer survival rate then men Basic Needs: Oxygenation Oxygenation • Oxygen is required to sustain life, primary basic human need • The cardiac & respiratory systems function to supply the body’s oxygen demands • Cardiopulmonary physiology involves delivery of deoxygenated blood to the right side of the heart & to the pulmonary system What are the 3 concepts in oxygenation? • Ventilation • Perfusion • Diffusion What are the 2 mechanisms that drive the function of the heart? • Electrical/conduction • Mechanical/pump What is Heart Failure? • Heart cannot pump enough blood to meet the metabolic demands of the body. • Results from changes in the systolic or diastolic function of the ventricles • There are many causes????? What are they???? http://www.americanheart.org/presenter Types of Heart Failure • Left Sided • Right sided • Systolic • Diastolic Left Sided Heart Failure • Most Common • LV dysfunction causes blood to back up through the left atrium and into the pulmonary system. • Common causes of left heart failure are: HTN, CAD, mitral and/or aortic valve disease, decreased tissue perfusion. What does that patient look like????? Right Sided Heart Failure • Most common cause is left sided heart failure. • Other causes MI or pulmonary HTN • RV dysfunction causes the blood to back up in the right atrium and then the venous circulation. What does that patient look like????? Systolic Failure • Defect in ventricular contraction • Left Ventricle loses ability to generate enough pressure to eject blood forward through the high pressure aorta – Decreased ejection fraction • Afterload – hypertension, cardiomyopathy, and valvular heart disease Diastolic Failure • Impaired ability of ventricles to fill • Decreased filling = decreased stroke volume Which + decreased WHAT? • Pulmonary congestion, pulmonary hypertension, with normal ejection fraction Heart Failure Diagnostic Studies • Goal: Assess the cause & degree of failure • History and Physical Exam • B-Type Natriuretic Peptide level (BNP). – elevated in acute and chronic heart failure – useful in following the response to treatment of congestive heart failure. • ABGs, Serum chemistries, LFTs • Chest x-ray • EKG • Echocardiogram • Nuclear imaging studies • Cardiac catheterization • Hemodynamic monitoring Lets Compare!!!! Classification of Heart Failure • Class 1 – No limitation of physical activity • Class 2 – Slight limitation – fatigue, dyspnea, palpitations • Class 3 – marked limitation. Comfortable at rest; ordinary activities cause symptoms • Class 4 – Inability to carry out any physical activity without symptoms – Pain/discomfort at rest Management and Outcome Measures • Use of ß-blockers at discharge and during admission. • Use of aspirin at discharge and during admission. • Timely and appropriate acute reperfusion (thrombolysis or primary angioplasty). • The use of angiotensin-converting enzyme (ACE) inhibitors for patients with depressed left ventricular systolic function. Similarly, a minority of patients with AMI are potential candidates for this care process, Management and Outcome Measures • The proportion of patients eligible for smoking-cessation counseling is relatively small, and ascertainment can be difficult, given the variability in documentation as well as practice. • Diet and exercise counseling • Cholesterol status assessment and management. Congestive Heart Failure Medical Treatment Goals • Decreasing Intravascular Volume – Decreasing Venous Return • Decreases preload – decreases the volume to the left ventricle during diastole • Med: Diuretics – Lasix (furosemide) • Decreasing Afterload – Decrease systemic vascular resistance • CO increases • Pulmonary congestion decreases • Meds: Nitroglycerine (NTG); Morphine; Calcium Channel Blockers Congestive Heart Failure Medical Treatment Goals • Improving Gas Exchange & Oxygenation – Supplemental oxygen – Morphine • Severe cases – intubation / ventilation • Improving Cardiac Function – Increase cardiac contractility without increasing cardiac oxygen consumption – Hemodynamic Monitoring: • pulmonary artery pressure; pulmonary artery wedge pressure (14-18mmg HG) – Inotropic Meds: Digoxin • Inotropic meds used with hemodynamic monitoring: – Dobutamine – Inodilators: (inotropic & vasodilator): Milrinone Congestive Heart Failure Medical Treatment Goals • Reducing Anxiety – Sedative action of IV Morphine • Complication: respiratory depression • Determine & Treat Underlying Cause – Systolic or Diastolic failure – Aggressive drug therapy So what medical complications do you think can occur??????? What basic needs are being effected? Why and how? Nursing Care for the Patient with Heart Failure • What will you assess???? • What are some potential nursing diagnosis????? • What are your goals for those diagnosis???? • What are your interventions????? • How will you evaluate your goals????? Case Study • A 74-year-old woman is admitted to the hospital with heart failure. She had been growing progressively weaker and has ankle edema, dyspnea on exertion, and three-pillow orthopnea. On admission, she is severely dyspneic and can answer questions only with one-word phrases. She is diaphoretic and has central cyanosis, with a heart rate of 132 beats/min, and blood pressure 98/70. She is extremely anxious. Case Study • 1. Because this client cannot breath or talk easily, prioritize the immediate nursing assessments and intervetions upon admission. • 2. Considering the process of congestive heart failure, explain the symptoms she is having. • 3.Based on assessment, identify nursing diagnoses for this client. • 4. What diagnostic studies do you anticipate being ordered and why? Case Study • 5. The physician orders the following items for this client. (Start an IV, then give dobutamine 3 mcg/kg/min IV; Furosemide (Lasix) 40 mg IV stat; Digoxin 0.5 mg IV stat, then 0.125mg PO every 6 hours for three doses, with ECG before doses 3 and 4; Morphine 2 mg IV stat and then 2 mg IV every 1 to 2 hours prn; Oxygen to maintain O2 sat >94%; Schedule for an echocardiogram; Low Na, Fat, Cardiac diet; Weigh daily and monitor input and output) Explain the rationale for these medications and treatments. Would you ask for any other ORDERDS and why?