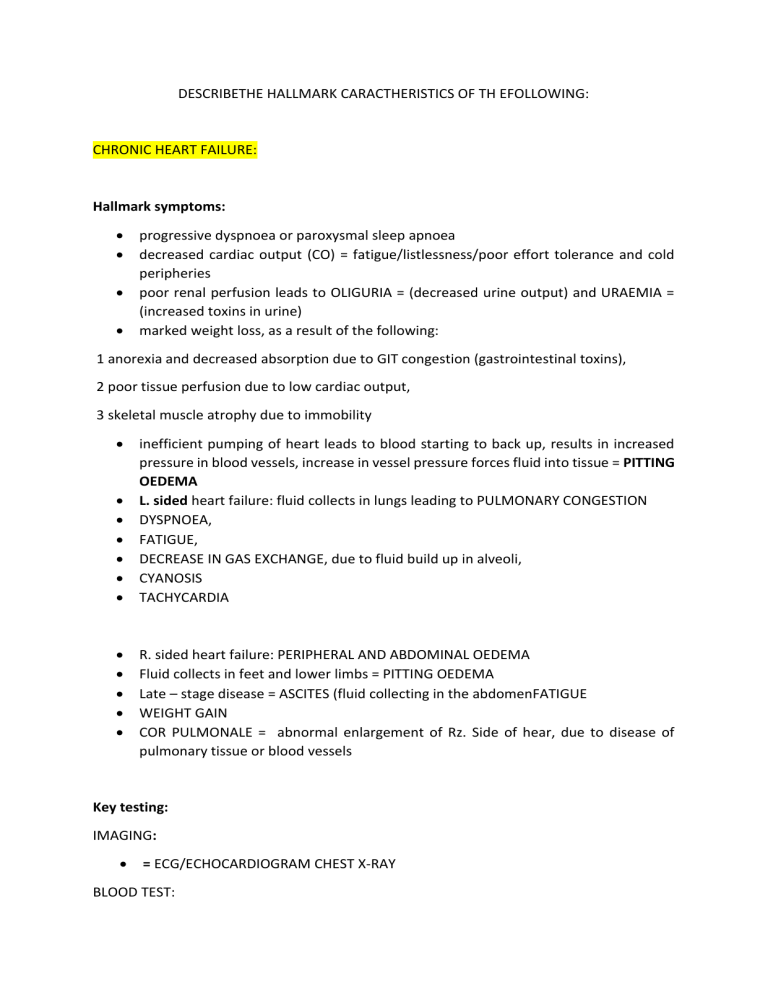
DESCRIBETHE HALLMARK CARACTHERISTICS OF TH EFOLLOWING: CHRONIC HEART FAILURE: Hallmark symptoms: progressive dyspnoea or paroxysmal sleep apnoea decreased cardiac output (CO) = fatigue/listlessness/poor effort tolerance and cold peripheries poor renal perfusion leads to OLIGURIA = (decreased urine output) and URAEMIA = (increased toxins in urine) marked weight loss, as a result of the following: 1 anorexia and decreased absorption due to GIT congestion (gastrointestinal toxins), 2 poor tissue perfusion due to low cardiac output, 3 skeletal muscle atrophy due to immobility inefficient pumping of heart leads to blood starting to back up, results in increased pressure in blood vessels, increase in vessel pressure forces fluid into tissue = PITTING OEDEMA L. sided heart failure: fluid collects in lungs leading to PULMONARY CONGESTION DYSPNOEA, FATIGUE, DECREASE IN GAS EXCHANGE, due to fluid build up in alveoli, CYANOSIS TACHYCARDIA R. sided heart failure: PERIPHERAL AND ABDOMINAL OEDEMA Fluid collects in feet and lower limbs = PITTING OEDEMA Late – stage disease = ASCITES (fluid collecting in the abdomenFATIGUE WEIGHT GAIN COR PULMONALE = abnormal enlargement of Rz. Side of hear, due to disease of pulmonary tissue or blood vessels Key testing: IMAGING: = ECG/ECHOCARDIOGRAM CHEST X-RAY BLOOD TEST: brain natriuretic peptide - (produced by cardiac myocytes in response to ventricular stretch, similar action to ANP serum urea & electrolytes = checking for reduced kidney function Treatment: LIFESTYLE MANAGEMENT: Patient education, dietary modifications, decrease in alcohol use and smoking, increase in exercise PHARMACOLOGICAL MANAGEMENT: st 1 line: DIURETICS –FRUSEMIDE, SPIRONOLACTONE nd 2 line: ACE INHIBITORS – RAMIPRIL, PERINDOPRIL, ANGINOTENSIN II receptor blockers – LOSARTAN, CANDESATRAN rd 3 line: VASODILATORS, VENODILATORS NITRATES - reduced preload, ARTETIAL DILATORS – reduced afterload th 4 line: ANTI-ARRYTHMIC DRUGS e.g. AMIODARONE, DIGOXIN – reduce BP, increase contractility SURGICAL MANAGEMENT: transplantation etc. ATRIAL FIBRILLATION: Hallmark symptoms: palpitation, angina, fatigue, pre – syncope, oedema, weakness, dyspnoea decreased cardiac output signs may precipitate or aggravate heart failure poor effort tolerance 3 CLASSIFICATIONS: Paroxysmal = intermittent, self – terminating, episodic Persistent = prolonged episode Permanent = disease progression will result in permanent presence TACHYCARDIC ARRYTHMIAS: increased automaticity – increased rate of cardiac action potential generation re-entry –retrograde depolarisation of cardiac tissue, causing premature depolarisation –ECTOPIC PAIN results in: PALPITATIONS, DIZZINESS, DYSPNOEA, CHEST DISCOMFORT BRADYCHARDIC ARRYTHMIAS: decreased automaticity – decreased rate of cardiac action potential generation blocked/slow conduction rate results in: SYMPTOMS OF LOW CARDIAC OUTPUT, FATIGUE, PRE – SYNCOPE etc. Key testing: IMAGING: ECG, ECHOCARDIOGRAPHY PHYSICAL EXAMINATION: PULSE = irregularly irregular AUSCULTATION: = possible murmur at persistent stage Treatment: PHARMACEUTICAL INTERVENTION: - aim is rate and rhythmic control ANTI-ARRYTHMICS – AMIODARONE BETA BLOCKERS CA++CHANNEL BLOCKERS ANTIPLATELETS – ASPIRIN ?ANTICOAGULANTS SURGICAL INTERVENTION Catheter ablation pacemaker implantable cardioverter defibrillator (ICD) HYPERTHROPHIC OBSTRUCTIVE CARDDIOMYOPATHY: Hallmark symptoms: it is a genetic cardiovascular disease -L. ventricle hypertrophy ventricle stiffness leads to decrease in filling capacity – resulting in heart failure all symptoms are aggravated by exertion dyspnoea light headedness -? due to positional changes, or Valsalva’s type manouvres pre/syncope – “greying out”, relieved by laying down arrythmias, palpitations, angina Key testing: PHYSICAL EXAMINATION: double apical impulse palpable at apex of heart percussion = cardiomegaly auscultation = murmur IMAGING: echocardiogram – diagnoses it! Treatment: lifestyle management – total abstinence from strenuous activity avoidance of heavy lifting Beta-blockers, Ca++ channel blockers Implantable cardiac defibrillator if severe DESCRIBETHE HALLMARK CARACTHERISTICS OF TH EFOLLOWING: PERIPHERAL ARTERIAL DISEASE STAGE II: Hallmark symptoms: tropic changes (changes to soft tissue in response to nerve or circulatory damage) = TOENAIL FUNGUS, PALLOR OR SHINY SKIN ON LEGS, COOL OR COLD LOWER LIMBS possible reduction in sensory testing possible balance issues – wider gait, turning with one foot on the ground or steppage gait patterned pain on exertion, e.g.(walking), gets rapidly alleviated by rest – pain most commonly in the calf pain possible but uncommon in buttock , hip, thigh or foot cycle of exacerbation and alleviation, collateral vascular supply created but disease continues to progress Key testing: OBSERVATION: cyanosis, digital clubbing, pallor on elevation, skin & nail dry and brittle, tropic changes to extremities, muscle wastage, loss of hair on legs, reduced pedal pulses INVESTIGATION: Ancle Brachial Pressure Index – doppler comparison of BP in arm to ankle – if lower in ankle = PAD likely Treatment: HISTORY: management is usually challenging, Rx = complicated, patients usually elderly and sedentary, comorbidities or end stage diseases common LIFESTYLE MODIFICATIONS: management of the risk factors, supervised exercise programme PHARMACEUTICAL INTERVENTIONS: ANTI-HYPERTENSIVES, ANTI-PALTELETS, STATINS, OPIOIDS for pain management (morpheein in stage III, IV) MANAGEMENT OF CONCORDANT CONDITIONS: Diabetes mellitus, heart failure, etc. SURGICAL INTERVENTION: amputation ABDOMINAL AORTIC ANEURYSM: Hallmark symptoms: often asymptomatic diffuse pain in central abdomen, back loin, iliac fossa or groin possible pulsatile sensation, palpable mass possible nausea/early satiety/urinary disfunction dependent on area of compression Key testing: OBSERVATION: Pt history observe for tropic changes observe for pulsatile mass AUSCULTATION: auscultate for abdominal bruit PALPATION: palpate abdominal aorta – dependent on pt size, may not be palpable palpate pedal pulses IMAGING: USG for diagnosis CT to provide an accurate information on size and extent Treatment: MONITOR: AAA is monitored until size equal of larger then 5.5 cm- until this time surgical risk higher then rupture risk exception – if AAA becomes symptomatic or distal embolus is occurring SURGERY: aneurismal segment replaced with prosthetic graft if the surgery is survived for +30 DAYS = prognosis of normal life expectancy RUPTURE = sudden onset pain +/- pulsatile mass and syncope 65% die before reaching hospital DEEP VEIN THROMBOSIS: Hallmark symptoms: pain erythema swelling oedema engorged superficial veins, but may be asymptomatic Key testing: HOMAN’S sign may be positive, but not confirmative of diagnostic - (Homan’s sign: pt supine, actively extends the knee, clinician raises straight leg 10 degrees and dorsiflexes foot abruptly while squeezing calf Beware, risk of pulmonary embolism! Treatment: HISTORY: patient history physical examination IMAGING: doppler USG (ultrasound) BLOOD TEST: D –dimer test (substance that is created after Fibrin is broken down) – high levels of D-dimer suggest recent presence of cloth PHARMACEUTICAL INTERVENTION: ANTI-COAGULANS – to reach the target of 2,5 INR PHYSICAL INTERVENTION: bed rest until fully anti-coagulated elastic stocking