Name:
Assigned Unit:
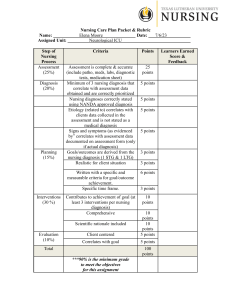
Step of
Nursing
Process
Assessment
(25%)
Diagnosis
(20%)
Planning
(15%)
Interventions
(30 %)
Nursing Care Plan Packet & Rubric
Elena Moore
Date:
Neurological ICU
Criteria
Points
Assessment is complete & accurate
(include patho, meds, labs, diagnostic
tests, medication sheet)
Minimum of 3 nursing diagnosis that
correlate with assessment data
obtained and are correctly prioritized
Nursing diagnoses correctly stated
using NANDA approved diagnosis
Etiology (related to) correlates with
clients data collected in the
assessment and is not stated as a
medical diagnosis
Signs and symptoms (as evidenced
by” correlates with assessment data
documented on assessment form (only
if actual diagnosis)
Goals/outcomes are derived from the
nursing diagnosis (1 STG & 1 LTG)
Realistic for client situation
25
points
5 points
5 points
5 points
3 points
3 points
Written with a specific and
measurable criteria for goal/outcome
achievement.
Specific time frame.
6 points
Contributes to achievement of goal (at
least 3 interventions per nursing
diagnosis)
Comprehensive
10
points
Scientific rationale included
Evaluation
(10%)
5 points
Client centered
Correlates with goal
Total
***90% is the minimum grade
to meet the objectives
for this assignment
3 points
10
points
10
points
5 points
5 points
100
points
7/6/23
.
,
Learners Earned
Score &
Feedback
Texas Lutheran University
Department of Nursing Education
NURS 340 Complex I
Nursing Care Plan Packet & Rubric
Student Name:
Client Initials:
.
SS
Date of Admission:
Healthcare Provider:
Gender: M
Age: 40
Unit/Rm#: NICU - 1121 .
7/4/23 .
Joglekar, Swati, MD /
Admitting Diagnosis:
Intracranial hemorrhage
-
Concurrent Diagnoses: Brain mass, glioblastoma with isocitrate dehydrogenase gene wild type (HCC), seizures
(HCC), malignant neoplasm of the brain (HCC)
Surgery: Craniotomy for resection of frontal mass with SSEP, EMG, and MEP Date: 11/11/21 .
Allergies to Drugs or Foods:
Robaxin (methocarbamol)
Advanced Directives / Code Status:
.
DNR .
Nursing Kardex:
Therapeutic Modalities
Vital Signs and Frequency
I & O/ Fluid Restrictions
Diet
Scheduled Diagnostics
Activity Level
Dressing Changes
Resp. Therapy
Self Care Ability
Daily Weights
SCD, TEDS, CPM
Daily Labs.
Other Treatments:
Vitals taken per unit protocol, BP measured every hour
Strict I&O monitoring, condom catheter
Tube feeding, NG tube - low intermediate suctioning
Labs to be drawn at noon per MD: basic metabolic panel, creatine
phosphokinase, hepatic function level, lactic acid level, triglycerides,
and venous blood gas
Bed bound - repositioning every 2 hours, maintain head of bed at atleast
30 degrees
N/A
ETT tube, vent, flow rate: 2 L/min, mode: SIMV, respiration rate: 14,
PEEP: 5, pressure support: 12, tidal volume: 450, SpO2 = 100%, FiO2 =
40
Full assist
Daily
SCD
QAM - Arterial blood gasses, basic metabolic panel, complete blood
count hemogram, calcium, magnesium, phosphorus; blood sugar checks
Q4H
Aspiration precautions, continuous electroencephalogram
Pathophysiology of Admitting Diagnosis (synthesize your description as if you were teaching a patient)
The admitting diagnosis from the emergency room is an intracranial hemorrhage. An intracranial hemorrhage
can be defined as bleeding within the intracranial vault and results due to “degenerative changes in the vessel
wall characterized by the loss of smooth muscle cells, wall thickening, luminal narrowing, microaneurysm
formation and microhemorrhages” (Caceres & Goldstein, 2012). Intracranial hemorrhages are diagnosed using a
noncontrast computerized tomography (CT) most commonly (Caceres & Goldstein, 2012). An intracranial
hemorrhage can present with symptoms similar to an ischemic stroke such as headaches, nausea, seizures and
generalized neurologic symptoms (Caceres & Goldstein, 2012).
Therapeutic Regimen
The patient’s admitting diagnosis is an intracranial hemorrhage, however, upon imaging an intracranial
hemorrhage was ruled out. Shortly after arriving at the ER the patient started experiencing seizures, with one
seizure lasting longer than three minutes. The patient was intubated in the ER and transferred to the
neurological intensive care unit. The patient is currently on continuous electroencephalogram monitoring. A
nasogastric tube was placed in the patient during his second day in the intensive care unit to facilitate optimal
nutrition and maintenance low intermediate suctioning is in place. The head of the patient’s bed is to remain at
atleast 30 degrees and aspiration precautions are in place. A condom catheter has been placed on the patient.
Non-violent/non self destructive soft restraints are in place to ensure the patient does not self extubate. Reassess
RASS every 4 hours.
Current health problems and related functional changes
Current health problems include a brain mass, glioblastoma with isocitrate dehydrogenase gene wild type
(HCC), seizures (HCC), and a malignant neoplasm of the brain (HCC). Due to the severity and frequency of
the patient’s seizures, the patient was intubated. Patient is now moderately sedated and bed bound. Patient is to
be repositioned every 2 hours and is a two person assist.
Laboratory
(All normal values taken from Houston Methodist TMC)
Test
Normal Values
Complete Blood Count
Result
Significance of Results
White Cell Count
4.50-11.00 k/uL
7.91 k/uL
Red Blood Cell Count
4.40-6.00 m/uL
4.19 m/uL
Hemoglobin
14-18 g/dL
11.7 g/dL
Hematocrit
41-51%
35.9%
Platelets
150-400 k/uL
107 k/uL
Differential
Other:
N/A
N/A
N/A
N/A
Normal. The white cell count is within normal range
indicating that the patient more than likely does not currently
have an infection.
Low. The red blood cell count can be decreased in patients
who have advanced cancer and dietary deficiencies. The
patient has a malignant neoplasm of the brain and was just
started on tube feeding the day prior; both of which could lead
to a decreased red blood cell count in the patient.
Low. Hemoglobin levels can be decreased in the presence of
neoplasia. The patient has a malignant neoplasm in the brain
which could cause the decreased hemoglobin levels.
Low. The hematocrit closely reflects the hemoglobin and red
blood cell count. The patient's hemoglobin and red blood cell
count are both low, so a low hematocrit would be expected as
well.
Low. Platelet levels can be decreased in the presence of
tumors. The patient has a large brain mass which could cause
the low platelet count seen here.
N/A
N/A
11.5-14.5 seconds
23-36 seconds
13.6 seconds
23 seconds
Results within normal range.
Results within normal range.
1.0
1.0
Results within normal range.
Na
K
Cl
Ca
Phos
135-148 mEq/L
3.5-5.0 mEq/L
98-112 mEq/L
8.3-10.2 mg/dL
2.4-4.5 mg/dL
141 mEq/L
3.8 mEq/L
106 mEq/L
9.1 mg/dL
9.1 mg/dL
Mg
Albumin (7/4/23)
1.6-2.6 mg/dL
3.5-5.0 g/dL
2.3 mg/dL
2.9 g/dL
Pre-albumin
BUN
N/A
6-20 mg/dL
N/A
30 mg/dL
Creatinine
0.70-1.20 mg/dL
0.61 mg/dL
Results within normal range.
Results within normal range.
Results within normal range.
Results within normal range.
High. Enemas containing sodium phosphate can increase
phosphorus levels. It was reported during rounds that the
patient received an enema during the night shift, which could
have caused the increased phosphorus level in the patient.
Results within normal range.
Low. Albumin levels correlate to the nutritional status of the
patient. The patient was vented 7/3/23. Enteral nutrition was
not started until 7/5/23, causing the albumin level to be
lowered.
N/A
High. The BUN measures the amount of urea nitrogen in the
blood. The BUN can be increased as a result of alimentary
tube feeding and the patient was started on tube feeding the
day prior.
Low. Creatinine is a catabolic product of CPK, which is used
in skeletal muscle contractions. Debilitation can cause
decreased levels of creatinine and the patient is currently bed
Coagulation Studies:
Prothrombin Time (PT)
Partial Thromboplastin
Time (PTT)
International
Normalized Ratio (INR)
Chemistry:
GFR
Creatinine clearance
Urine Specific Gravity
Fasting blood glucose
N/A
N/A
N/A
65-99 mg/dL
N/A
N/A
N/A
144 mg/dL
Hgb A1C
CRP
ESR
Lipid Studies:
Total Cholesterol
Triglycerides
HDLs
LDLs
N/A
N/A
N/A
N/A
N/A
N/A
bound which contributes to the low creatinine level seen here.
N/A
N/A
N/A
High. Patient is on continuous enteral feedings so BG would
not be a fasting level. Slightly elevated BG due to continuous
enteral nutrition is expected.
N/A
N/A
N/A
N/A
N/A
N/A
N/A
N/A
N/A
N/A
N/A
N/A
N/A
N/A
N/A
7.35-7.45
35-45 mmHg
80-90 mmHg
21-28 mmol/L
95-100%
7.54
26 mmHg
222 mmHg
22.1 mmol/L
100%
Arterial Blood Gasses:
Arterial pH
Arterial pCO2
Arterial pO2
Arterial bicarbonate
Arterial O2
currently
;;;;;;;;;;;;;;;;;;;;;;;;;;;;;
High.
Low.
High.
Normal.
Normal.
ABG significance: The ABG values indicate the patient is
currently experiencing respiratory alkalosis. Vent setting may
need to be adjusted.
Diagnostic
Test
Normal Finding
7/3/23 CT Head
without contrast compared to 5/9/23 CT
Head without contrast
No evidence of
pathological
conditions or
abnormalities.
7/4/23 Head CT
without contrast compared with head CT
from 7/3/23
No evidence of
pathological
conditions or
abnormalities.
7/5/23 Head CT
without contrast compared with head CT
No evidence of
pathological
conditions or
Diagnostics Tests
Result for patient
Definition and description of test
Interval increase in size of
necrotic mass in the right
cerebral hemisphere measures
approx. 8x5 cm. There is a
worsening leftward midline
shift which now measures 2
cm. There is trapping of the
lateral ventricles bilaterally
most prominent in the
temporal horns. Right sided
craniotomy. No intracranial
hemorrhage or acute
transcortical ischemia.
CT scans of the head are
composed of a computerized
analysis of multiple tomographic
x-rays that are taken at
consecutive layers in order to
provide a 3D view of the cranial
contents (Pagana et al., 2021).
CT scans can be used to identify
diagnoses such as intracranial
neoplasms, cerebral infarctions,
ventricular displacement or
enlargement, cortical atrophy,
cerebral aneurysms, and
intracranial hemorrhages
(Pagana et al., 2021).
There are no significant
CT scans of the head are
changes. The necrotic
composed of a computerized
partially calcified mass in the analysis of multiple tomographic
right cerebral hemisphere and x-rays that are taken at
the mass effect on the brain
consecutive layers in order to
and ventricles is stable. The
provide a 3D view of the cranial
obstructive hydrocephalus is contents (Pagana et al., 2021).
stable. There is a stable right CT scans can be used to identify
uncal herniation and there is a diagnoses such as intracranial
subfalcine herniation. The
neoplasms, cerebral infarctions,
small amount of hyperdensity ventricular displacement or
in the region of the anterior
enlargement, cortical atrophy,
third ventricle is stable. No
cerebral aneurysms, and
acute intracranial abnormality intracranial hemorrhages
identified.
(Pagana et al., 2021).
Similar-appearing exam
CT scans of the head are
without acute interval
composed of a computerized
hemorrhage or worsening
analysis of multiple tomographic
Significance of the test for your
patient
This test was performed in the
emergency room due to the patient
having a suspected intracranial
hemorrhage. The significance of this
test for my patient is it showed that
the patient was not experiencing an
intracranial hemorrhage, but that the
necrotic mass in his right cerebral
hemisphere actually grew in size.
This test was performed once the
patient was transferred from the
emergency room to the neurological
intensive care unit. The test is
significant for my patient as it shows
there are no major changes from the
CT done on the previous day. The
test does show some uncal and
subfalcine herniation, but they are
stable.
This test was performed to again
rule out any significant intracranial
changes from the day prior. This test
from 7/4/23
abnormalities.
7/4/23 MRI of brain
without contrast compared to multiple
MRIs between 10/29/21
and 5/29/23 and head CT
on 7/4/24
No evidence of
pathological
conditions or
abnormalities.
mass effect.
x-rays that are taken at
consecutive layers in order to
provide a 3D view of the cranial
contents (Pagana et al., 2021).
CT scans can be used to identify
diagnoses such as intracranial
neoplasms, cerebral infarctions,
ventricular displacement or
enlargement, cortical atrophy,
cerebral aneurysms, and
intracranial hemorrhages
(Pagana et al., 2021).
Evidence of further
Magnetic resonance imaging of
progressive disease from 5/29 the brain and meninges are
with increasing extent of
especially accurate in identifying
diffuse necrotic enhancing
benign and malignant neoplasm
mass involving majority of
(Pagana et al., 2021). MRI’s are
the right cerebral hemisphere a noninvasive diagnostic
and crossing midline, now
scanning technique that places
involving more of the right
the patient in a magnetic field,
basal ganglia, right thalamus, but does not expose them to
right midbrain and evidence
ionizing radiation (Pagana et al.,
of subependymal spread of
2021).
tumor and leptomeningeal
disease. Worsening mass
effect with increasing 2.0 cm
right-to-left midline shift,
subfalcine herniation, and
increasing dilatation from
entrapment of the lateral
ventricles with evidence of
transependymal edema.
Worsening of imaging
findings highly suspicious for
tumor progression.
is significant for my patient as it
shows the necrotic mass is stable
and has not changed in size since
admission to the hospital. The test
results again show that there is no
intracranial hemorrhage present.
This test was performed to better
identify pathological changes within
the patient’s brain. The significance
of this test is it showed worsening of
the necrotic mass within the
patient’s brain.
Medication List (All information taken from Davis Drug Guide 18th Ed)
Medication + Route
Pharmacologic
Rationale for Use
Side effects
Contraindications
Nursing
and Dose
Classification
Adverse reactions
Considerations for
Administration
propofol (Diprivan) phenol
This medication has an
Neuro: dizziness,
Hypersensitivity
● Assess respiratory
Route: intravenous
derivative
indication for use in
headache. Resp:
to propofol,
status, pulse, and BP
Dose: 40 mcg/kg/min
sedation of intubated,
APNEA, cough.
soybean oil, egg
continuously
(17.2 mL/hr)
(Therapeutic
mechanically ventilated
CV: bradycardia,
lecithin, or
throughout propofol
Frequency:
class: sedative- patients in the intensive
hypotension,
glycerol
therapy.
continuous IV
hypnotic)
care unit. This patient is
hypertension. GI:
● Maintain patent
infusion
intubated, indicating the
abdominal
airway and adequate
use of this medication.
cramping, hiccups,
ventilation.
nausea, vomiting.
● Assess level of
Derm: flushing.
sedation and level of
Local: burning,
consciousness
pain,
throughout and
stinging,coldness,
following
numbness, tingling
administration.
at IV site. MS:
● Monitor for
involuntary muscle
propofol infusion
movements,
syndrome (severe
perioperative
metabolic acidosis,
myoclonia. GU:
hyperkalemia,
discoloration of
lipemia,
urine (green).
rhabdomyolysis,
Misc: propofol
hepatomegaly,
infusion syndrome,
cardiac and renal
fever.
failure).
docusate sodium
stool softeners
This medication is used to EENT: throat
Hypersensitivity;
● Assess for
liquid
help prevent constipation. irritation. GI: mild Abdominal pain,
abdominal
Route: NG tube
The patient is currently
cramps, diarrhea.
nausea, or
distention, presence
Dose: 100 mg
bed bound so ensuring
Derm: rashes
vomiting,
of bowel sounds,
Frequency: BID
that the stool stays soft
especially when
and usual pattern of
and passes is needed since
associated with
bowel function.
the patient is not moving.
fever or other
● Assess color,
signs of an acute
consistency, and
Recommended
Dose
Range
Adults: 5-50
mcg/kg/min
*Dose should be
reassessed every
24 hours*
Adults: 50-400
mg in 1-4
divided doses
abdomen.
heparin
Route: subcutaneous
injection
Dose: 5000 units
Frequency: Q8H
antithrombotics
This medication is
indicated for use in the
prevention of thrombus
formation. Due to the
patient being bed bound
and on a vent,
thrombolytic therapy is
needed.
Derm: alopecia
(long-term use),
rash, urticaria. GI:
drug-induced
hepatitis. Hemat:
bleeding, heparininduced
thrombocytopenia,
anemia. Local:
pain at injection
site. MS:
osteoporosis
(long-term use).
Misc: fever,
hypersensitivity
reactions.
amount of stool
produced.
● Do not administer
within 2 hr of other
laxatives, especially
mineral oil. May
cause increased
absorption.
Hypersensitivity;
● Assess for signs of
Uncontrolled
bleeding and
bleeding; History
hemorrhage
of heparin(bleeding gums;
induced
nosebleed; unusual
thrombocytopenia;
bruising; black,
Severe
tarry stools;
thrombocytopenia;
hematuria; fall in
Open wounds (full
hematocrit or BP;
dose)
guaiac positive
stools). Notify
health care
professional if these
occur.
● Subcut: Observe
injection sites for
hematomas,
ecchymosis, or
inflammation.
● Assess patient for
evidence of
additional or
increased
thrombosis.
● Monitor platelet
count every 2– 3
days during therapy.
● Administer deep
Subcut
(Adults): 5000
units every 8-12
hr
lacosamide
(Vimpat) in NaCl
0.9% IVPB
Route: intravenous
Dose: 100 mg in 50
mL NaCl
Frequency: Q12H
functionalized
amino acid
(Therapeutic
class:
anticonvulsant)
This medication is used to
decrease the incidence
and severity of
partial-onset seizures and
generalized tonic-clonic
seizures. The patient has
been having seizures
continuously since being
admitted from the
emergency room,
indicating this
medications use.
CV: ventricular
arrhythmias,atrial
fibrillation/flutter,
bradycardia, heart
block, syncope.
Derm: drug
reaction with
eosinophilia and
systemic
symptoms (dress),
stevens-johnson
syndrome, toxic
epidermal
necrolysis, rash.
EENT: diplopia.
GI: nausea,
vomiting. Hemat:
agranulocytosis.
Neuro: ataxia,
suicidal thoughts,
dizziness,
hallucinations,
syncope, vertigo.
Misc: physical
dependence,
psychological
dependence.
Hypersensitivity;
severe hepatic
impairment
into subcut tissue.
Alternate injection
sites between the
arm and the left and
right abdominal
wall above the iliac
crest.
● Rotate injection
sites frequently.
● Assess location,
duration, and
characteristics of
seizure activity.
Institute seizure
precautions.
● Monitor closely for
changes in behavior
thatcould indicate
the emergence or
worsening of
suicidal thoughts or
behavior or
depression.
● IV: Assess ECG
prior to therapy in
patients with
preexisting cardiac
disease before
starting after
titration to
steady-state
maintenance.
Monitor patients
with cardiac
conduction
problems, on
PO, IV
(Adults):
Adjunctive
therapy - 50 mg
twice daily; may
↑ weekly by 100
mg/day in 2
divided doses up
to a maintenance
dose of 100– 200
mg twice daily;
may also initiate
therapy with
200-mg single
loading dose
followed 12 hr
later by 100 mg
twice daily; may
↑ weekly by 100
mg/day in 2
divided doses up
to a maintenance
dose of 100– 200
mg twice daily.
dexAMETHasone
in NaCl 0.9% IVPB
Route: intravenous
Dose: 10 mg in 200
mL NaCl
Frequency: Q6H
corticosteroids
(systemic)
This mediation is
indicated for use in
patients with cerebral
edema. The patient had a
craniotomy back in 2021;
this medication is being
used to aid in the
prevention of swelling
and inflammation due to
the necrotic mass in the
patient's brain.
Adverse
reactions/side
effects are much
more common
with high-dose/
long-term
therapy.
CV: hypertension.
Derm: acne, ↓
wound healing,
ecchymoses,
fragility, hirsutism,
petechiae. EENT:
cataracts, ↑
intraocular
pressure. Endo:
pheochromocytom
a, adrenal
suppression,
cushingoid
appearance (moon
face, buffalo
hump),
hyperglycemia. F
and E: fluid
retention
Active untreated
infections (may
be used in patients
being treated for
some forms of
meningitis)
medications that
prolong PR interval,
or with severe
cardiac disease
(myocardial
ischemia, heart
failure) closely,as
IV lacosamide may
cause bradycardia or
AV block.
● Assess for changes
in level of
consciousness and
headache during
therapy.
● Monitor intake and
output ratios and
daily weights.
Observe patients for
peripheral edema,
steady weight gain,
rales/crackles, or
dyspnea. Notify
health care
professionals if
these occur.
● Administer with
meals to minimize
GI irritation
● Instruct patient to
inform health care
professional
promptly if severe
abdominal pain or
tarry stools occur.
PO, IM, IV
(Adults)
Cerebral edema10 mg IV, then 4
mg IM or IV
every 6 hr until
maximal
response
achieved, then
switch to PO
regimen and
taper over 5– 7
days.
(long-term high
doses),
hypokalemia,
hypokalemic
alkalosis. GI:
peptic ulceration,
anorexia, nausea,
vomiting. Hemat:
thromboembolism,
leukocytosis,
thrombophlebitis.
Metab: weight
gain. MS: muscle
wasting,
osteoporosis,
avascular necrosis
of joints, muscle
pain. Neuro:
depression,
euphoria,
headache,
personality
changes,
psychoses,
restlessness. Misc:
↑ susceptibility to
infection.
Cognitive / Neurosensory:
-Level of consciousness:
moderately sedated, responds to
voice
-Pupils: PERRLA
-Eye opening spontaneously
Physical Assessment
Cardiovascular:
-HR 64 bpm
-ECG indicates normal sinus
rhythm
-Left pedal pulse: weak
-Right pedal pulse: weak
-Left brachial pulse: moderate
-Right brachial pulse: moderate
-No edema noted within any
extremities
Gastrointestinal:
-No pain noted upon palpation of
abdomen.
-Abdomen is rounded, no distention
is observed.
-Last BMI was on overnight shift
-Bowel sounds present upon
auscultation of all four quadrants.
-No masses felt upon palpation of
the abdomen.
Genitourinary:
-Negative for hematuria
-Condom catheter in place
-Urine output is low, MD aware
-Urine color: yellow
Integument:
-Lips: dry
-Skin: warm to touch
-No apparent rashes or lesions
-IVs: patent
Nutrition:
-Enteral nutrition started
-NG tube in place - titrating flow
rate up
-Maintenance low intermediate
suctioning
-BS check every 4 hours
-Residual: 10 mL
Respiratory
-Breath sounds: diminished,
inspiratory wheezes
-Cough: productive
-ETT tube, flow rate: 2 L/min,
mode: SIMV, respiration rate: 14,
PEEP: 5, pressure support: 12, tidal
volume: 450, SpO2 = 100%, FiO2 =
40
-Continuous pulse ox on finger
-Inline suction catheter
-Secretions: small amount, white in
color, thick consistency
Musculoskeletal:
-Right upper extremity motor
response: responds occasionally
-Right/left hand grip strength: weak
-Left upper extremity motor
response: movement to painful
stimuli (jerked arm during blood
draw)
-Right/left upper extremity motor
strength: flicker of muscle
-Eye opening
-Slight tremors
Pain Assessment:
-Patient shook head no when asked
if he was experiencing any pain
Wound / Surgical Incision Assessment:
Assessment
Type of wound
and Stage
Location
Wound #1
Wound #2
Wound #3
N/A
N/A
N/A
N/A
N/A
N/A
Length
N/A
N/A
N/A
Width
N/A
N/A
N/A
Depth
N/A
N/A
N/A
Drainage
N/A
N/A
N/A
Odor
N/A
N/A
N/A
Undermining /
Tunneling
Wound bed tissue
type
N/A
N/A
N/A
N/A
N/A
N/A
Three priority nursing diagnosis for patient rank in order by priority:
1) Impaired physical mobility
2) Powerlessness
3) Compromised family coping
Nursing
Diagnosis Priority:
Goal/ Outcome
Nursing Interventions
Short Term Goal: Over the
next 24 hours the patient
will remain free of
complications from
immobility as evidenced by
intact skin, absence of
thrombophlebitis, normal
bowel pattern, and clear
breath sounds.
1) Reposition/turn the
patient at least every 2
hours (Ignatavicius et
al., 2021).
Rationale
1) Frequent repositioning
will help prevent
Impaired Physical
complications of immobility
Mobility
such as pressure injuries or
clot formation (Ignatavicius
Related to: mechanical
2) Perform mouth care at et al., 2021).
ventilation and
least every 12 hours
continuous sedation
(Ignatavicius et al.,
2) Consistent oral care
2021).
performed at least every 12
As evidenced by:
hours is correlated with
reliance on assistive
Long Term Goal: Lab
3) Assess the need for
reduced incidences of
devices/inability to
values will indicate ability to suctioning every 2 hours ventilator-associated
ambulate
potentially wean from
and suction only as
pneumonia (Ignatavicius et
mechanical ventilators
needed. (Ignatavicius et al., 2021).
within 72 hours as evidenced al., 2021).
by normal ABG levels and
3) Frequent suctioning
hemodynamic stability.
4) Educate the family
maintains airway patency
and patient on modes of and reduces the likelihood
Correlation of Etiology (related to) to
communication that can of developing infections
Pathophysiology
be used as sedation is
such as ventilator-associated
Mechanical ventilation is used to help improve gas
weaned
(Ignatavicius
et
pneumonia (Ignatavicius et
exchange and lower the effort required for effective
al., 2021).
al., 2021).
breathing (Ignatavicius et al., 2021). Sedation is
oftentimes needed for vented patients to decrease anxiety
4) Communication can be
and agitation as well as prevent self extubation
frustrating and produce
(Ignatavicius et al., 2021). Due to the use of sedatives,
anxiety among ventilated
patients will experience decreased mobility due to
patients and their families
decreased muscle function.
(Ignatavicius et al., 2021).
Discharge Teaching:
● Ensure the patient's family is informed regarding new functional changes of the patient.
● Provide information regarding palliative care and hospice services.
Evaluation of Goal
Achievement
Short Term Goal: Patient is
free of complications from
immobility after 24 hours as
evidenced by intact skin,
absence of thrombophlebitis,
normal bowel pattern, and clear
breath sounds. {Unable to assess
if the goal was met}.
Long Term Goal: ABG levels
have returned to normal and
hemodynamic stability has been
achieved after 72 hours.
{Unable to assess if the goal
was met}.
Nursing Notes
References
Caceres, J. A., & Goldstein, J. N. (2012). Intracranial Hemorrhage. Emergency medicine clinics of North
America, 30(3), 771–794. https://doi.org/10.1016/j.emc.2012.06.003
Ignatavicius, D. D., Workman, M. L., Rebar, C. R., & Heimgartner, N. M. (2021). Medical-Surgical
Nursing: Concepts for Interprofessional Collaborative Care (Tenth Edition). Elsevier Inc.
Pagana, K. D., Pagana, T. J., & Pagana, T. N. (2021). Mosby’s Diagnostic & Laboratory Test Reference
(Fifteenth Edition). Elsevier, Inc.
Vallerand, A. H., & Sanoski, C. A. (2022). Davis’s Drug Guide for Nurses (Eighteenth Edition). F. A.
Davis Company.