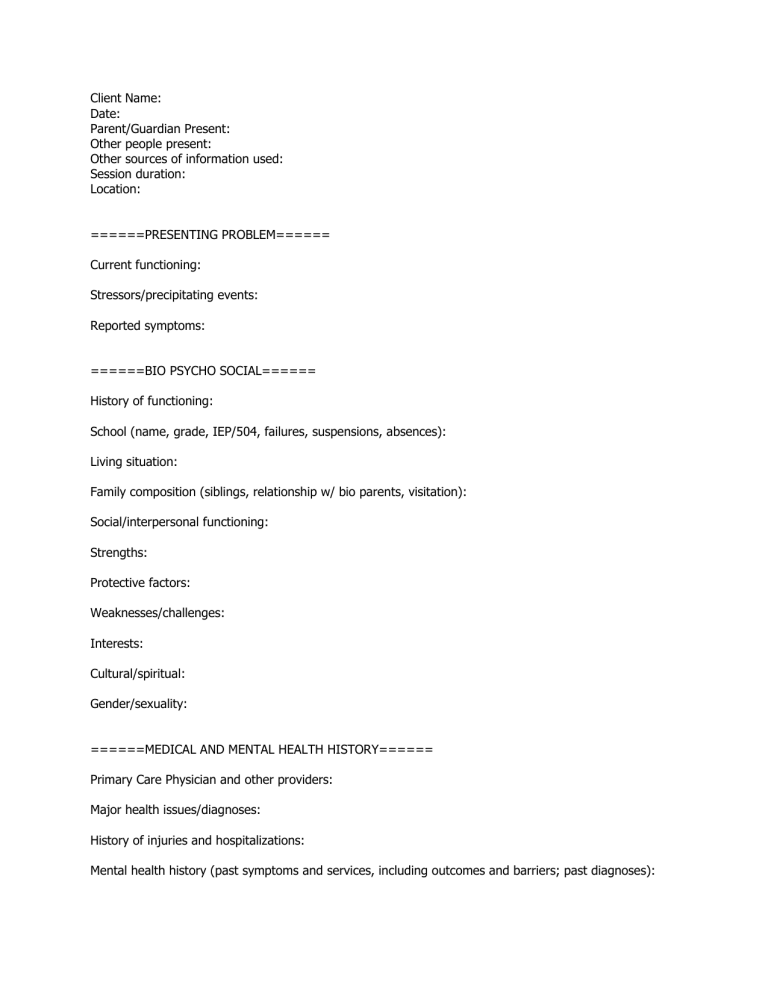
Client Name: Date: Parent/Guardian Present: Other people present: Other sources of information used: Session duration: Location: ======PRESENTING PROBLEM====== Current functioning: Stressors/precipitating events: Reported symptoms: ======BIO PSYCHO SOCIAL====== History of functioning: School (name, grade, IEP/504, failures, suspensions, absences): Living situation: Family composition (siblings, relationship w/ bio parents, visitation): Social/interpersonal functioning: Strengths: Protective factors: Weaknesses/challenges: Interests: Cultural/spiritual: Gender/sexuality: ======MEDICAL AND MENTAL HEALTH HISTORY====== Primary Care Physician and other providers: Major health issues/diagnoses: History of injuries and hospitalizations: Mental health history (past symptoms and services, including outcomes and barriers; past diagnoses): Medications past and present: Developmental history (milestones, etc): Issues or complications with pregnancy and birth/delivery: Family mental health history: ======TRAUMA HISTORY====== Major stressful or traumatic events: Trauma symptoms: Legal history (DSS/CPS, DJJ, police involvement): ======RISK ASSESSMENT====== Suicidality/self-injurious behavior (past and present): Homicidality/aggression (past and present): Substance use (past and present): Other high risk behaviors: Supervision issues/needs: Safety in home/community: ======CLIENT/GUARDIAN PRESENTATION AND PARTICIPATION====== Mental Status Exam: Client participation: Parent/Guardian participation: ======CASE FORMULATION====== ======TREATMENT RECOMMENDATIONS====== Based on this assessment, therapist recommends... [ ] Individual therapy [ ] Family therapy [ ] Group therapy [ ] Higher level of care in the form of ________