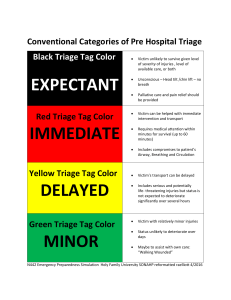
DR-HANI SAMIR AL-HAITHAM HEAD OF ED SHIFA HOSPITAL Definition of triage Triage is a French word that means to sort. Napoleon’s surgeon is thought to be the first physician to use triage on a battlefield in the 1800s to sort out soldiers who could be treated in a nearby hospital and returned to duty How does triage occur at a scene? 1 : the sorting of and allocation of treatment to patients and especially battle and disaster victims according to a system of priorities designed to maximize the number of survivors 2 : the sorting of patients (as in an emergency room) according to the urgency of their need for care EmergencySeverity Index The Emergency Severity Index (ESI) is a simple to use, five-level triage instrument that categorizes emergency department patients by evaluating both patient acuity and resources. Initially the triage nurse assesses only acuity level. If a patient does notmeet high acuity level criteria (ESI level 1 or 2), the triage nurse then evaluates expected resource needsto help determine a triage level (ESI level 3, 4, or 5). In an MCI, field triage is expanded from solely evaluating an individual patient to assessing priorities to identify the sickest patients and ensure they are transported and treated first Although several systems exist for triaging victims of multicasualty incidents, the basic concept generally identifies four groups of patients: Red (immediate): Critical or immediately life- threatening illness or injury (e.g., tension pneumothorax, hypovolemic shock) Yellow (delayed): Serious but not immediately life-threatening illness or injury (e.g., most types of fractures) Green (minor): “Walking wounded” (e.g., anxiety attack after witnessing event) Black (dead/dying, or expectant): Dead or resource-intensive victims (e.g., 100% total body surface area burn). Triage tags or colored tape is used to clearly indicate the categories of patients to assist in rapid assessment on scene What triage system is most commonly used The triage system currently in most common use is START (simple triage and rapid treatment), A Centers for Disease Control and Prevention (CDC) working group has also proposed a national triage method referred to as SALT (sort, saving interventions, and treat/transport). assess, life- Numerous other triage systems exist, such as JumpSTART for pediatrics, MASS (move, assess, sort, send) triage, Fire Department of New York (FDNY) modified START triage, and Sacco triage method (STM). There is ongoing research to determine which system is the most accurate. Variables such as age (very young or very old), comorbidities, and type of incident (e.g., chemical exposure) may influence the accuracy of currently accepted triage methods. Tell me more about START. is designed to triage a patient in less than 30 seconds . First, those able to ambulate are immediately classified as walking wounded and sorted to a separate area (green). Priority is then given to the remaining victims on the ground The triage officer assesses for breathing and spontaneous respirations. If breathing or circulation is abnormal and the patient is alive (has a pulse), a basic airway maneuver is attempted, such as a jaw thrust or the insertion of an oropharyngeal airway (OPA), and the patient is categorized as red if the patient is not breathing and has no pulse, he or she is triaged into the black category. Assuming normalrespirations, perfusion is assessed by radial pulse and capillary refill time (if absent radial pulse and capillary refill >2 seconds, patient is triaged as red). Finally, mental status is assessed by the patient’s ability to follow commands (if no, triaged to red, and if yes, triaged to yellow). An easy mnemonic used to remember this approach is RPM: 30 to 2, can do, where RPM denotes respirations, perfusion, and mental status, and 30 to 2, can do indicates respiratory rate less than 30, capillary refill less than 2 seconds, and ability to follow commands Red patients are prioritized for transport, followed by the yellow patients. Green patients may not actually need a formal evaluation at the hospital, or may be able to be transported en masse This sort of rapid assessment allows for maximum use of the limited resources that are available at a disaster scene. What is the difference between START and SALT triage systems? SALT first performs a global sorting by assessing for the ability to ambulate. Those who can walk are assessed last. Next, if victims can follow a simple command (such as “Raise your hand if you can hear me”), they are considered less emergent and assessed second. Priority for assessment is given to those not responding, who are then triaged as either red, black, or gray based on their injuries and response to simple life-saving interventions (such as a needle decompression for a tension pneumothorax). An important distinction between the two systems is that SALT triage incorporates a gray color designation for patients who are deemed expectant, meaning those who have little likelihood to survive their injuries, even with adequate resources. This also allows for palliative interventions for these patients, so they are not simply left to die Which one is better, START or SALT? Retrospective analysis has shown START to be a reliable and easy-to-learn triage system for first responders Studies comparing the START and SALT triage systems have found START easier to learn and use in a real disaster scenario. Notably, both are prone to overtriaging patients (identifying victims as more sick than they really are), which can be detrimental to the overall system because it may divert limited resources to people who do not truly need them