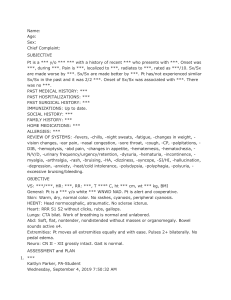
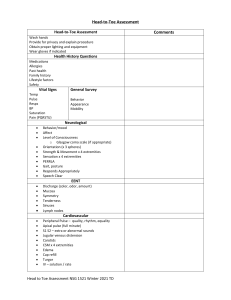
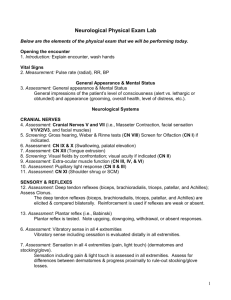
Cc: Headache/Seizure Patient is a known case of Spinal cord compression sec to neuroblastoma st IV (spine), s/p colostomy with biopsy (Sept 2019), s/p adjuvant chemotherapy; s/p partial resection (Aug 2020, PCMC) s/p radiotherapy x 2 cycles (Aug-Sept 2021), S/P Cycle 1 Chemotherapy (9/17/21). Patient was previously admitted at Onco ward 10/11-20/21 due to Urinary Tract Infection and cellulitis on left posterior thoracic area, given with Cefuroxime. Oral Chemotherapy also started last admission. Discharged well and stable with home medications such as cotrimoxazole, metoclopramide, etoposide, paracetamol, morphine, pregabalin and dexamethasone. Apparently well until 2 days prior to consult, upon awakening, patient experienced headache, occipital area, localized, described as "parang sinusuntok", no other associated symptoms such as fever, cough, colds, vomiting, abdominal pain, increase sleeping time, changes in sensorium. No consultation was done. Maintenance medication continued 1 day prior to admission, no noted headache. 10hrs prior to consult, upon awakening, noted crying due to recurrence of headache, occipital area, localized, still no other associated symptoms, given Morphine with relief of symptom. 3hrs prior to consult, still with headache, same character as above, BP was taken noted elevated at 160/100 and suddenly had seizure episode, described as shaking of upper extremities, upward rolling of eyeballs, teeth grinding, perioral cyanosis, cyanosis of fingernails, about 10minutes in duration, brought to Taytay Doctors Hospital, with BP 130/100, RR27, HR 130, febrile at 38.1, still on active seizure, hence, given with diazepam 5mg TIV, still with seizure. Given with midazolam 2.5mg, noted resolution of seizure woth post ictal drowsiness. Advised admission, but mother opted THOC, hence brought in our institution Last seizure: 10/31 1pm ROS: no cough, colds, abdominal distention, blurring of vision PMH: Patient is a known case of Spinal cord compression sec to neuroblastoma st IV (spine), s/p colostomy with biopsy (Sept 2019), s/p adjuvant chemotherapy; s/p partial resection (Aug 2020, PCMC) s/p radiotherapy x 2 cycles (Aug-Sept 2021), S/P Cycle 1 Chemotherapy (9/17/21). Patient was previously admitted at Onco ward 10/11-20/21 due to Urinary Tract Infection and cellulitis on left posterior thoracic area, given with unrecalled antibiotics. Oral Chemotherapy also started last admission. Discharged well and stable with home medications such as cotrimoxazole, metoclopramide, etoposide, paracetamol, morphine, pregabalin and dexamethasone. Under the care of Palliative Service FH: (+)Asthma and HPN on maternal side, denies other heredofamilial diseases DH: Supposedly at Grade 3, stopped due to his current condition but patient is able to write, read, answers simple calculations, unable to walk since August 5, 2021 due to spinal cord compression PSH: only child, usually spends time by playing cellphone games, drawing, writing etc. PE: Awake, with spontaneous eye opening, not in distress BP 120/90 HR 120 RR 24, T 36.5, 99% Anicteric sclerae, pink palpebral conjunctivae, no naso-aural discharge, moist lips, non hyperemic tonsils Symmetric chest expansion, (-) retractions, clear breath sounds Adynamic precordium, regular rhythm, ()murmur Non distended abdomen, normoactive bowel sounds, (+)colostomy, right hemiabdomen, soft No Stunting, No Wasting F: On D5 0.3 NaCl at MR Initially on NPO R: No dyspnea, no fast breathing, no cough, no colds Symmetrical chest expansion, no retractions, clear and equal breath sounds RR 20s, O2 sat 99% on room air I: With 1 episode of fever last night max temp 38.1, no recurrence thereafter Temp ranges: 36.6-37.4 Full pulses, CRT<2sec, warm extremities NEURO PE: spontaneous eye opening, withdraws to pain, moans to pain CNI - unable to assess CNII- isocoric, 3-4 pupils mm EBRTL (+) Doll’s eye CNV - intact facial sensation CNVII-no facial asymmetry CNVIII: unable to assess CN IX X- intact gag Motor: withdraws to pain on upper extremities Sensory: withdraws to pain on upper extremities DTR: 1 on upper extremities, 0 on lower extremities No nuchal rigidity , no meningeal signs Bilateral clonus, no babinski, no nystagmus Currently on the 1st HD being managed as a case of Status Epilepticus secondary to Hypertensive Encephalopathy; Probable Brain Metastasis; Spinal Cord Compression secondary to Neuroblastoma Stage IV (spine); R/O Sepsis; S/P colostomy with biopsy (Sept 2019), S/P Adjuvant Chemotherapy; S/P partial resection (Aug 2020, PCMC) s/p radiotherapy x 2 cycles (Aug-Sept 2021), S/P Cycle 1 Chemotherapy (9/17/21, NCH); CBC: (post ictal) Hgb 158, Hct 47, wbc 40.1 seg 88, lym 10 plt 339 CRP <6mg/L Awaiting Blood CS results Still for Urinalysis / Urine GSCS and Fecalysis / Stool CS *COVID NPS GENEXPERT: POSITIVE* Current Antibiotics: Ceftriaxone 2grams q12 max dose D1 C: BP: 100-110/70-80, HR 130s Adynamic precordium, tachycardic, regular rhythm, no murmurs, no neck vein distention, warm extremities, pulses full and equal, no cyanosis, no edema H: No pallor, no bleeding CBC: Hgb 158, Hct 47, wbc 40.1 seg 88, lym 10 plt 339 M: No vomiting, no loose stooling, no abdominal distention, on colostomy Na: 141, K: 4.6, Cl: 102, Ca: 2.54 BUN: 10.0 Crea: 36 ALT 666.8 (16x) AST 187.7 (4.6x) HGT ranges: 81-82-145 Meds: Morphine 0.25mkdose q4 IV PRN Lactulose 2.2G/5ml, 30cc ODHS O: Diazepam 0.3mkd PRN Mannitol 5cc/kg q6 D: Initially on NPO May have full diet once fully awake Plans May have full diet once fully awake D5.3NaCL at MR Diagnostics: For repeat CBC today I: IVF: ~1500 Oral: ~ 30-50cc O: unquantified 3 diaper changes since admission (Medium sized adult diaper, moderate-fully soKed) For procalcitonin, d dimer, serum ferritin, LDH Awaiting official results of Cranial CT scan with Contrast and CXR AP-L Awaiting Blood CS Still for: U/A, Urine GS/CS F/A, Stool Culture BM: 3x colostomy changes N: Can maintain wakefulness No recurrence of seizure No recurrence of headache spontaneous eye opening, and movement of extremities CNI - unable to assess CNII- isocoric, 3-4 pupils mm EBRTL (+) Doll’s eye CNV - intact facial sensation CNVII-no facial asymmetry CNVIII: gross hearing intact CN IX X- intact gag Motor:, withdraws to pain on upper extremities Sensory: reacts to light and deep touch withdraws to pain on upper extremities DTR: 1 on upper extremities, 0 on lower extremities No nuchal rigidity , no meningeal signs Bilateral clonus, no babinski, no nystagmus Meds: Phenytoin 5mkday q6 - maintenance Therapeutics: 1. Ceftriaxone 100mkday q12 2. Paracetamol 10mkdose q4 PRN 3. Phenytoin 20mkdose as LD then 5mkday q6 4. Diazepam 0.3mkd PRN 5. Morphine 0.25mkdose q4 IV PRN 6. Mannitol 5cc/kg q6 7. Zinc Sulfate 55mg/5ml, 5ml PO BID 8. Cholecalciferol 2000iu/cap 1 cap OD For transfer to COVID 1 ward For swabbing of mother Thank you po.