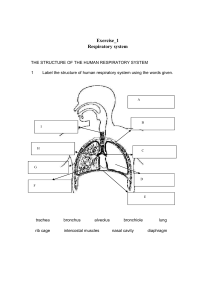
Respiratory Tract Learning Unit 1 – Part 1 Anatomy • The primary function of respiratory system is to supply blood with oxygen and remove carbon dioxide (gaseous exchange) • The respiratory system is divided into upper and lower portions. The upper respiratory system consists of the nasal cavities, sinuses, mouth, pharynx, and larynx. • The lower respiratory system consists of the trachea, bronchi, bronchioles, and alveoli. Upper respiratory tract Anatomy • Air enters the respiratory system through the mouth and the nose. • The air then passes through the nasal cavity and pharynx, through the larynx and the trachea. • The trachea splits into two smaller tubes, left and right main bronchi. • The lungs differ anatomically in that the left lung has two lobes but the right lung has three lobes. • The right bronchus divides into three lobar bronchi, to supply the upper, middle, and lower lobe of the right lung, and the left bronchus branches to supply the upper and the lower lobe of the left lung. Anatomy Anatomy • The bronchial tubes divide further into many smaller tubes, which connect to tiny sacs called alveoli. • The alveoli are the basic functional component of the lungs and are surrounded by capillaries. • Oxygen present in inhaled air passes into the alveoli and diffuses through the capillaries into the arterial blood. Meanwhile, carbon dioxide carried in the blood from the veins is released into the alveoli. • Carbon dioxide follows the same path out of the lungs during exhalation. Function of the Respiratory Tract Upper respiratory tract: • Transportation of air to lungs • Warming and humidifying inspired air • Removing dust particles • Voice production • Plays a role in olfaction • First line of defence against inhaled microorganisms Lower respiratory system: • Warms, moistens and filters the air before it reaches the lungs • Protects against microorganisms • Terminal portion responsible for gaseous exchange Anatomy and Histology Respiratory system is lined by two types of epithelium: • Non-keratinizing stratified Squamous Epithelium • Pseudostratified Columnar (Respiratory) Epithelium Non-keratinizing Stratified Squamous Epithelium • Non-keratinizing squamous epithelium protects & covers areas that are liable to frictional forces such as those caused by swallowing of food or by touch. • These areas include the front part of the nasal cavity, central and lower portions of pharynx, oral cavity and parts of the larynx. • Non-keratinizing squamous epithelium cells commonly exfoliate, will be commonly present in sputum and bronchial specimens. • They can be recognized in respiratory samples as superficial and intermediate squamous and parabasal cells. Pseudo-Stratified Columnar Epithelium • Respiratory epithelium is referred to as pseudostratified columnar epithelium as it appears to be multilayered, even though it consists of a single layer of epithelial cells. • The impression of multilayering is due to the position of nuclei in different levels of the cells in the epithelium. • The trachea, bronchial tree and remainder of the upper airways are lined by specialize columnar epithelium. • This consists of a pseudostratified layer of ciliated tall columnar cells interspersed with mucin secreting goblet cells, which have microvilli on their luminal surfaces. Pseudo-Stratified Respiratory Epithelium • Bronchioles are lined by a single layer of columnar or cuboidal cells epithelium composed of three cell types: ➢ Ciliated columnar cells ➢Mucous – secreting goblet cells ➢Basal or reserve cells (precursors for goblet and columnar cells) ➢ Non- ciliated non mucous secreting Clara cells and Neuro-endocrine cells (line the terminal bronchioles). Cytology of Normal Respiratory Tract Squamous Epithelial Cells • Squamous mucosa is composed of basal, parabasal, intermediate & superficial cells • Superficial and intermediate cells predominate have well-defined cell borders, abundant cytoplasm staining pinkish orange and green respectively, in Pap stained smears. • Superficial cells characterised by pyknotic nuclei. • Intermediate cells are characterized by a round-to-oval vesicular nuclei. Ciliated Columnar cells • These cells seen in bronchial brushings/washings, BALs and FNABs. • Not present in large numbers in sputum except in post- bronchoscopy specimens or following extensive damage to the respiratory epithelium. • The main function of ciliated cells is to move the bronchial secretions toward the pharynx. Ciliated Columnar Cells • Cells lie singly, in short ribbons or flat sheets which have a honeycomb appearance. • The ciliated cells have basal, round to oval shaped nuclei with finely granular (open) chromatin. • The luminal part (facing the lumen) is covered by cilia; these are numerous and at their point of attachment form a terminal plate • Cells have delicate/foamy cyanophilic cytoplasm Ciliated bronchial epithelial cells Goblet Cells • Goblet cells are present in a ratio of approximately one per six ciliated cells. • Cells less commonly seen in sputum specimens. • Goblet cells secretes mucous which coats the airways with a sticky layer within which inhaled particles, organisms and cell debris are trapped • Common in patient with chronic tracheobronchial disease, such as asthmatic bronchitis, chronic bronchitis and bronchiesctasis (permanent dilation of one or more bronchi) Mucous Secreting Goblet Cells • Cells are columnar in shape. • Also have a basally located nucleus, fine vesicular chromatin but they lack cilia. • Cells have microvilli on luminal surface. • Cytoplasm is distended by single/multiple vacuoles filled with mucus. Goblet Cells Reserve Cells • Small reserve cells rest on the basement membrane, forming an undifferentiated stem cell population from which regeneration of goblet & columnar cells takes place after injury. • They are rarely present in sputum but are sometimes seen in brushings and lavage specimens, mainly in reactive states. • They form sheets of small regular cells slightly larger than lymphocytes, with a high nuclear/cytoplasmic ratio, coarse chromatin and a narrow rim of green cytoplasm. Reserve Cells Neuroendocrine Cells • Rarely identified in cytology samples • Neuroendocrine cells are situated towards the basement membrane. • Known as Feyrter or K (Kultschitzsky) cells. • They contain neurosecretory granules producing locally active hormones into the blood Clara Cells • Line the terminal bronchioles. ➢ ➢ ➢ Cells are cuboidal or tall / columnar Non ciliated Non mucous secreting • Cells secrete various protein that clears the airways and have the potential to differentiate into ciliated cells. • Cannot be recognized or identified in routine cytology samples Alveolar Cells Type I & II Pneumocytes • Alveolar air sacs lined by cells known as type I and type II pneumocytes. • Type I pneumocytes are large, thin cells stretched across a large surface and cover the areas where gaseous exchange takes place. • Type II pneumocytes manufacture surfactant, a surface active material that prevents collapse of the air-sacs on expiration. • Type II pneumocytes also act as reserve cells or progenitor cells and can differentiate into type I pneumocytes when they need to be replaced. • Type II pneumocytes are round, single cells with central nuclei, small nucleoli, and vacuolated cytoplasm Alveolar Macrophages • Alveolar macrophages (also known as histiocytes) are macrophages found in the pulmonary alveolus which are derived from bone marrow. • The presence of this cells indicate that a sputum specimen is satisfactory as they indicate that the sample comes from the deep lungs • They are phagocytes; their role is engulfing, digesting, and removal of inhaled particles and pathogens in the alveoli. • They also stimulate lymphocytes and other immune cells to respond to foreign matter. • Alveolar macrophages vary in appearance depending on their activity. • The cytoplasm may be vacuolated and evidence of inhaled particles (usually carbon) may be seen as brown granules with Papanicolaou stain. Alveolar macrophages • Single-lying/ small clusters • Eccentric or central single/ binucleate/ multinucleate nuclei • Nuclear shape: round-oval-beanshaped • Granular chromatin • Inconspicuous nucleoli • Cytoplasm basophilic, foamy/ finely vacuolated/ ingested particles Carbon-laden alveoli macrophages Summary of different cell types in respiratory tract Inflammatory Cells • Mainly neutrophils and lymphocytes, are invariably present in low numbers and are only of diagnostic significance if markedly increased. - Acute inflammation: seen in patients with pneumonia, acute bronchitis and alveolar abscess - Chronic Inflammation: seen in patients with follicular bronchitis, viral infections • A predominance of one inflammatory cell type may however be significant, for example, when eosinophils are conspicuous (frequently noted from patient with asthma or those with infections due to fungi or parasites. Non-Cellular Components • Non-living structures may be present in specimens RT • Some indicate specific problem; while others only serve to confuse and produce incorrect diagnosis • Structures may be derived from: - patient (endogenous) - contaminant after specimen collection (exogenous) - Inhaled material • Their recognition is important to avoid misinterpretation. Curschmann’s Spiral • Strands of mucous seen in lumen of small bronchioles • Conditions of excess mucous production • Coiled/ spiral like appearance, dark staining center and translucent periphery • Associated with asthma, chronic bronchitis, smoking, cancer Ferruginous (Asbestos) Bodies • Ferruginous (containing particles of iron) or asbestos bodies are formed when inhaled filamentous particles (dust) become coated in protein and iron. • Segmented or bamboo shaped with knobbed or bulbous ends (dumbbell), ranging from 5 to 200 μm in length, they stain goldenyellow to black with Papanicolaou stain and blue with Prussian blue stain Charcot- Leyden Crystals • Needle-shaped, elongated, orangeophilic/pink/yellow structures formed from breakdown products of eosinophil granules. • May be seen in patients with severe allergic disorders like asthma, allergy, parasitic or fungal infections or eosinophilic pneumonia Corpora Amylacea • Non-calcified small glycoprotein of alveolar space – rounded, concentrically laminated not calcified with radial striations acidophilic structures • They stain pale pink, are Congo red positive • Significance unclear in the lung, often associated with benign conditions Psammoma Bodies • Concentrically laminated calcified structures contain phosphate, iron and magnesium • Seen in malignant tumors that have papillary architecture, like primary pulmonary adenocarcinoma, mesothelioma, and metastatic thyroid or ovarian cancer. • They are also seen in benign conditions like pulmonary tuberculosis and alveolar microlithiasis. Contaminants • Any structure breathed into the respiratory passage or any particle of masticated food may appear on respiratory specimens: -Alternaria (arial or water born)forms light brown conidia with an internal segmented structure -Food- includes fragments of plant tissue- characteristic rectangular shape, thick cellulose walls and dark nuclei meat fibre are elongated and may show radial striations -Colonial growth of normal flora – include bacteria and yeast, occur when delay in specimen preparation - Pollen • Common source of error Contaminants Alternaria Meat Fibre Vegetable cells Specimen Collection And Sample Processing • Cytologic specimens from the respiratory tract are one of the most common cytologic specimens received by the laboratory. • Indications for respiratory cytology: • Diagnosis of malignancy (primary and metastatic) • Diagnosis of infection, particularly in immunosuppressed individuals. • Diagnosis of benign lesions. Sampling Methods • Sputum • Bronchial washings • Bronchial brushings • Bronchoalveolar lavage • FNA • Transbronchial • Transthoracic Sputum • Once the most frequently examined specimen from RT – easy to obtain / little discomfort to patients • Complex mucoid product from airways containing variety of cellular non-cellular material produced by host or inhaled • Microscopic examination may indicate benign or malignant conditions of the airways • Most specific for squamous cell carcinoma Sputum • The adequacy of a sputum sample is established by finding numerous pulmonary macrophages. • Specimens consisting merely of squamous cells, bacteria, and Candida organisms are unsatisfactory because they represent only oral contents. • The presence of numerous macrophages indicates that a satisfactory, deep cough specimen of the lower respiratory tract has been obtained. Method Of Collection • Produced by deep coughing • Early morning deep cough specimens preferred • Patient must brush teeth/ rinse mouth – remove any exfoliated oral cells that would contaminate the sputum sample • Patient must inhale deeply repeatedly and exhale with an explosive cough into sterile container • Sputum induced – patient inhale nebulized water or saline • If delay in specimen prep, patient must expectorate into a 70% ethanol solution to prefix specimen • Multiple samples collected over three days increases sensitivity of test Lab Preparation • Usually prepared by the “pick and smear” method • Saccomanno Method Sputum Preparation “Pick and smear” method: • Pour sputum sample into Petri dish • Examine sample for areas of tissue fragments or bloody material • Material is smeared between two glass slides. • Fixed in alcohol and stained by the Papanicolaou method Sputum Preparation Saccomano Method: • Samples collected in mixture of 50% ethanol and 2% carbowax • Blending at high speeds – using a blender • Samples concentrated by centrifugation and preparing the smears from the centrifuged cell button Sputum Advantages Disadvantages Easily, painlessly obtained, if spontaneous Difficult if not spontaneous Good for detection of central tumours Poor for detection of peripheral tumours Extensive area sampled Cannot localise lesion Accurate esp. squamous and small cell carcinomas Less accurate for adenocarcinoma Bronchoscopy Bronchial Aspirates and Washing • Sampling of the lower respiratory tract occurred with the development of the flexible fiberoptic bronchoscope in the late 1960s. • Allows any part of RT to be sampled • Bronchial secretions can be aspirated directly from the lower respiratory tract through the bronchoscope, or an alternative (and more common) method is to “wash” the mucosa by instilling 3 to 10 ml of saline and suctioning the washings into a trap. • Fluid centrifuged , concentrate used to make smears Brochoalveolar Lavage • BAL the bronchoscope is wedged into position as far as it will go in order to sample the distal airways, which are flushed with sterile saline. • Specimen is centrifuged and cell palate is used to make smears • BAL is particularly useful for the diagnosis of opportunistic infections in immunocompromised patients, TB and malignancy (adenocarcinoma). • The specimen can be examined cytologically and a portion also submitted for microbiologic studies. Fine Needle Aspiration Biopsy • Diagnostic procedure that can be carried out on an outpatient basis. • A needle is passed through the chest wall (transthoracic) or through the bronchial wall (transbronchial) into the pulmonary wall. • The contents of the needle are expelled onto a slide and a smear is made with a second slide by pulling the slides apart. • Fix or air-dry & stained in lab with pap stain Transbronchial (TFNA) • Transbronchial FNA is a special modification of needle aspiration used when the lung neoplasm has not invaded through the bronchial mucosa and is not accessible through sputum or bronchial brushing/washing • Used for sampling of mediastinal lymph nodes (mediastinum area between lungs that contain heart, aorta, trachea and lymph nodes) • TBNA is also used diagnosis of lung cancer and also staging procedure • Procedure involves insertion of a needle a flexible through fibreoptic bronchoscope • Penetration of bronchial wall and aspiration of cytological material lying beyond Transthoracic Fine Needle Aspirations • Performed under Computed tomography (CT) guidance • Involves insertion of fine needle through the thoracic wall and pleura to obtain specimen. • Indicated for peripheral lesions Homework List the advantages and disadvantages of different sampling techniques in respiratory cytology. Feedback to be given in our next class. Routine Staining Method • Papanicolaou stain widely used as routine stain – results in welldefined nuclear detail and cytoplasmic transparency • Romanowsky staining, such as May-Grunwald-Giemza or Diff-Quik used to compliment Pap stain – allow better visualization of cytoplasmic features and enhance cell size Ancillary Test Immunocytochemistry (ICC): • Immunocytochemistry is an ancillary technique that is used in the anatomical pathology laboratory for the detection and visualization of proteins and peptides (antigens) in cells using biomolecules (antibodies) capable of binding the protein of interest (antigenantibody interaction). • ICC divided into direct and indirect methods ICC Direct Method • Direct method rely on direct visualization of antigen-antibody reaction using primary antibody that is conjugated with a visible marker (probe, tag or label) – fluorescent dye Disadvantage • Poor sensitivity – due low concentration of antigenic components might be undetectable ICC Indirect method • Secondary antibody is applied after a primary antigen-antibody reaction takes place, the second antibody is tagged or several antibodies bind to a primary antibody Advantage • Amplifies the signal- increased sensitivity ICC • The tag is an enzyme, which in itself is invisible. Only when a chromogenic substrate or chromogen is applied does the reaction become visible. • A coloured product indicates a positive immunoreaction between antibody and the antigen of interest. • Horseradish peroxidase used as tag. • This enzyme cannot be seen directly, the addition of hydrogen peroxide and the colourless substance 3,3’diaminobenzidene (DAB) produces a brown reaction product which is easily recognized microscopically. Brown ICC reaction indicates the site of antigen-antibody reaction Ancillary Tests Special Stains • Used to ID specific elements in cytological preparations after routine evaluation by pap and Romanowsky stained slide • Example: o Periodic acid Schiff (PAS) o Grocott’s methenamine silver o Alcian Blue PAS o Congo Red • PAS- used to demonstrate carbohydrates. Glucose produces by cell or organism reacts with Schiff reagent to produce magenta colour – used to id some pathogenic fungi and other constituents of a cell