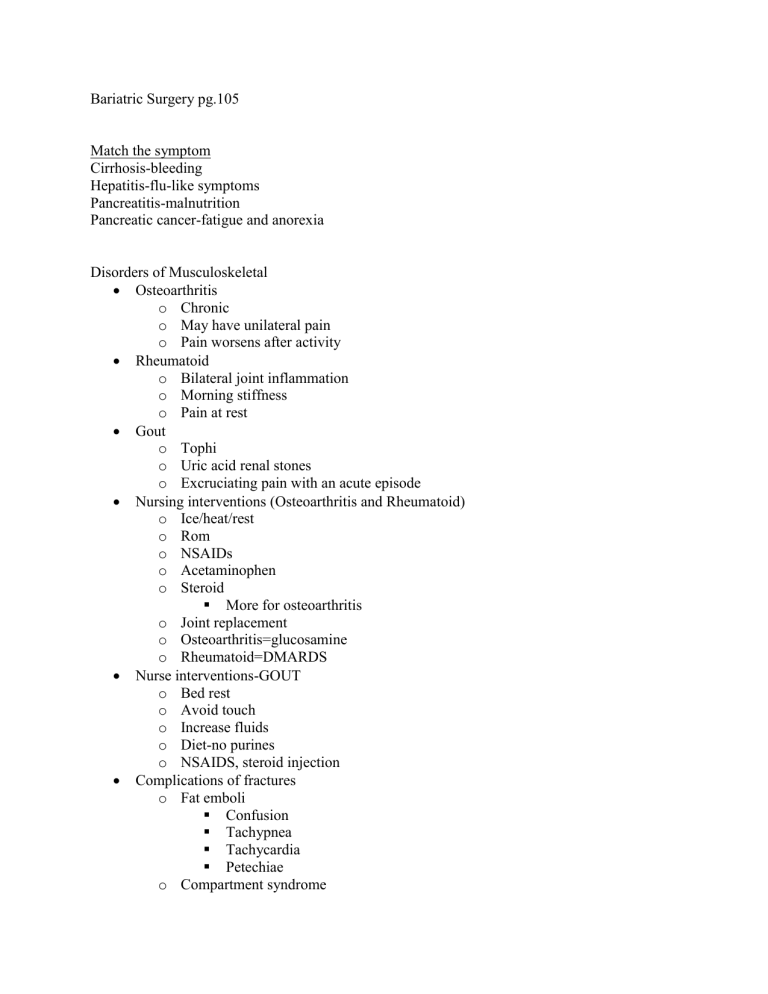
Bariatric Surgery pg.105 Match the symptom Cirrhosis-bleeding Hepatitis-flu-like symptoms Pancreatitis-malnutrition Pancreatic cancer-fatigue and anorexia Disorders of Musculoskeletal Osteoarthritis o Chronic o May have unilateral pain o Pain worsens after activity Rheumatoid o Bilateral joint inflammation o Morning stiffness o Pain at rest Gout o Tophi o Uric acid renal stones o Excruciating pain with an acute episode Nursing interventions (Osteoarthritis and Rheumatoid) o Ice/heat/rest o Rom o NSAIDs o Acetaminophen o Steroid More for osteoarthritis o Joint replacement o Osteoarthritis=glucosamine o Rheumatoid=DMARDS Nurse interventions-GOUT o Bed rest o Avoid touch o Increase fluids o Diet-no purines o NSAIDS, steroid injection Complications of fractures o Fat emboli Confusion Tachypnea Tachycardia Petechiae o Compartment syndrome pain pressure pallor paresthesia paralysis pulselessness ENDOCRINE Function of gland How does hyposecretion look? o Meds, radiation How does hypersecretion look? o Med, radiation, removal of the gland Posterior pituitary-ADH is the problem o Hyposecretion=diabetes insipidus o Hypersecretion=SIADH DIABETES MELLITUS p.123 Diet o Complex carbs Common complications o Retinopathy o Skin ulcers o Hypertension o Neurogenic pain o Proteinuria o Heart attack BLOOD/HEMATOLOGICAL DISORDERS Matching Anemia o Renal diseasedecrease erythropoietin o Iron deficiency weakness or pallor o AplasticLow RBC, WBC, Platelets o Pernicious B12 malabsorption o Hemolyticpremature RBC destruction o Sickle Celljoint pain o Thalassemia facial bone deformities CARDIAC SYSTEM Electrocardiogram o P wave: atrial depolarization o QRS: ventricular depolarization o T wave: ventricular repolarization Basics of rhythm strips o Do you see P wave? o Do you see QRS after every P wave? (Should be followed by T wave o What is the rate? Is it normal, too fast, or too slow? o Is it regular or irregular? o What do the P and QRS waves look like? Cardiac Catheterization o Pre-procedure Informed consent Kidney function-dyes Allergies Metformin? Mark distal pulse Teach: taste, flush o Post-procedure Positioning Immobilize Pressure to the insertion site for at least 15 min Chest pain Vitals Extremity Manifestations of MI o Pain or discomfort o Jaw pain o Arm pain o Back and abdomen pain o Occurs without cause o Not relieved by o **Women, older clients, and diabetics may not experience chest pain Initial interventions for MI o MONA Heart failure o Left-sided (LUNGS) Dyspnea Frothy sputum Crackles Cough o Right-sided (REST OF BODY) JVD Weight gain Edema Oher valve disorders o Valve disorders o Aortic aneurysms o Hypertension (greater than 140/90) VENOUS OR ARTERIAL? o Venous Painless ulcers Lower leg edema hyperpigmentation o Arterial Claudication Delayed CRT Hair loss on legs Cyanotic extremities CABG o Preop Consent Education Place IVs Baseline VS Meds that have to be given-antibiotic o Postop CCICU May have chest tube or leave chest open Vented for first 3-6 hrs Sterile dressing changes Monitor: for cardiac dysrhythmias EARLY OR LATE SIGNS OF SHOCK o Early Pallor Tachypnea Confusion tachycardia o Late Cold, moist skin Weak thready pulse Anuria Hypotension Metabolic acidosis Indications for dialysis o Chronic renal disease Hemodialysis o interventions Access circulation Hold meds? Yes and no; a morning dialysis pt you hold morning meds If someone has later dialysis you take morning meds but hold evening Weight before and after Vitals Monitor labs o Advantages More efficient clearance Shorter treatment time o Complications Infection Closure Disequilibrium syndrome Hypotension Bleeding Peritoneal dialysis o Interventions Monitor weight Hold meds? No Vital signs Monitor labs-initial labs and recheck fairly frequently when they first start; after it may be monthly o Advantages More Mobility Fewer hemodynamic complications o Complications Infection Poor outflow Cold shock Bowl perforation NEUROSENSORY DISORDERS Neurosensory diagnostics Which tests monitoring for headaches o Lumbar punction Avoid caffeine 8 hrs. prior to the test? o EEG Quickly ID a CVA? o CT scan Requires contrast dye o Angiography Unable to perform is pt has a pacemaker o MRI Cerebrovascular Accidents o F-face; face droop o A-arms; equal strength? o S-speech; has quality changed? o T-time CANCER Mgmt. o Assess for signs of infection o Neutropenic precautions o Assess for signs of bleeding o Encourage high energy conservation BURNS Parkland formula o Administer LR o Formula: 4mL x kg x % TBSA o ½ total in first 8 hr o ½ in the remaining 16 hr o Deducts any fluids given pre-hospital OB/PEDS Newborn:0-1 (trust vs. mistrust) o Posterior fontanel closes 2-3 months o Anterior fontanel closes 8-18 months Toddler:1-3 (autonomy vs. shame and doubt) Preschool: 3-5 (initiative vs. guilt School age: 6-12 (industry vs. inferiority) Adolescence 12-20 (identity vs. role confusion) Young adult: 20-35 (intimacy vs. isolation) Middle adult: 35-65 (generativity vs. stagnation) Older adult: 65+ (integrity vs. despair) Stages of labor 1. 3 phases of dilation a. Latent: 0-3 cm b. Active: 4-7 cm c. Transition: 8-10 cm 2. Pushing stage 3. Delivery of placenta 4. Recovery and bonding Contractions Braxton hicks-false labor o Increase in 3rd trimester o Intermittent o Decrease with Change of position Walking o No cervical changes True labor Amniotomy Risks o Prolapsed cord o Infection o Committed to delivery Interventions o Assess the station of presenting part o Assess FHR before and after o Doc time, amt, color, odor of the fluid o Monitor temp q2h C-section Indications o Fetal distress o Malpresentation o Multiple gestations o Genital herpes Intervention o Pre-op: informed consent, labs, o Post-op: massage fondus PSYCH