•
= .
-
Item 1 of39
Question Id: 6347
2
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
Lab Yallles
m,
rim
Notes
Calculator
;'
ffiffij
3
4
A 36-year-old Caucasian female is seen in the emergency department (ED) for the evaluation of a sudden onset, left lower chest pain and difficulty
s
in breathing. Approximately one year ago, she was diagnosed w ith left lower extremity deep vein thrombosis secondary to smoking and oral
6
contraceptive pill (OC P) use. At that time, her OCPs were discontinued, she quit smoking, and she was treated with six months of warfarin
7
therapy. She does not have any other medical problems. Her mother and maternal aunt have had "problems with blood clots." After performing
8
the appropriate ancillary procedures, results reveal the presence of multiple, left-sided pul monary emboli. A diagnosis of an inherited
9
thrombophilia is suspected. W hich of the following is most likely to be present in this patient?
10
11
Q
A. Factor V Leiden mutation
12
0
0
0
0
B.
13
14
~
6
17
Low protein C levels
C. Prothrombin gene mutation
D. Antiphospho!ipid antibody
E. Antithrombin 111 deficiency
18
19
Submit
20
21
22
•
~
4
25
•
26
27
•
28
29
•
30
31
•
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
•
= .
-
Item 1 of39
Question Id: 6347
2
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
rim
Tutorial
Lab Yallles
Notes
Calculator
\.!..)
1111
;'
ffiffij
3
4
A 36-year-old Caucasian female is seen in the emergency department (ED) for the evaluation of a sudden onset, left lower chest pain and difficulty
s
in breathing. Approximately one year ago, she was diagnosed w ith left lower extremity deep vein thrombosis secondary to smoking and oral
6
contraceptive pill (OC P) use. At that time, her OCPs were discontinued, she quit smoking, and she was treated with six months of warfarin
7
therapy. She does not have any other medical problems. Her mother and maternal aunt have had "problems with blood clots." After performing
8
the appropriate ancillary procedures, results reveal the presence of multiple, left-sided pul monary emboli. A diagnosis of an inherited
9
thrombophilia is suspected. W hich of the following is most likely to be present in this patient?
10
A. Factor V Leiden mutation (83%)
11
12
B. Low protein C levels (3%)
13
C. Prothrombin gene mutation ( 1% )
14
~
D. Antiphospho!ipid antibody (8°/o}
6
E. Antithrombin Ill deficiency (3o/o}
17
18
19
20
Omitted
21
Correct answer
A
22
•
~
4
I 11.
I.ill..
rT', 07 secs
83o/o
\..::J
Answered correctly
Time Spent
~ 02/03/2020
13 Last Updaled
Explanation
25
•
26
The patient in the above scenario has suffered from a second episode of venous thromboembolism in a year. Factor V Leiden is the most
27
•
common cause of inherited or heredity thrombophilia, accounti ng for approxin1ate!y 40-50% of the inherited thrombophilias. These disorders
28
predispose the patient to the development of venous thromboembolism.
29
•
30
31
•
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
•
2
= .
-
Item 1 of39
Question Id: 6347
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
11111
;'
rim
ffiffij
Calculator
3
4
D. Antiphospholipid antibody (8°/o}
s
E. Antithrombin 111 deficiency (3%)
6
7
8
Omitted
9
Correct answer
A
10
IT\
111, 83%
l!!!.
07 secs
I...::.) Time Spent
Answered correct!y
F=1 02/03/2020
El Last Updated
11
12
Explanation
13
14
~
The patient in the above scenario has suffered from a second episode of venous thromboembolism in a year. Factor V Leiden is the most
6
common cause of inherited or heredity thrombophilia, accounting for approximately 40-SOo/o of the inherited thrombophilias. These disorders
predispose the patient to the development of venous thromboembolisn1.
17
18
(Choices B, C, D and E) Other common causes of heredity thrombophilia include prothrombin gene mutation, hyperhomocysteinemia, protein C,
19
protein S, and antithrombin Ill deficiency. Some patients may have more than one type of inherited disorder, and are at even greater risk for
20
venous thromboembolism.
21
Educational Obj ective:
22
•
Factor V Leiden is the most common cause of inherited or heredity thrombophilia, accounting for approximately 40-50% of the inherited
~
thrombophilias.
4
25
•
26
27
•
Foundations of Independent Practice
Hen1atology & Oncology
Inherited thrombophilia
Subject
System
Topic
Copynghl@ ..JWorla A
28
Is
...
29
•
30
31
•
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
1
•
= .
-
ltem2of39
Question Id: 5465
•\
~
Mart<
<]
C>
r,
Previous
Next
Fun Screen
L .J
•!
I'>\
\.!..)
Tutorial
1111
Lab Yallles
m; ',
Notes
rim
ffiffij
Calculator
3
4
A 76-year-old woman is brought to the physician by her son. He is concerned that his mother, who was previously outgoing , does not want to
s
leave her home. She lives alone and works as a part-time volu nteer at a local library. Although she continues to work shelving books, she has
6
stopped attending her weekly meetings at a senior center where she socialized with friends. The patient also seems quieter and more difficult to
7
engage in conversation when he calls her on the telephone. One w eek ago, he found her sitting on a chai r pulled up close to the television. She
8
did not notice his presence immediately but then smiled and nodded as if following the conversation. He became concerned when she asked
9
about her grandchild's upcoming birthday party even though he had just told her the details. Her past medical history is significant for
10
hypertension . The patient reports that her sleep and appetite are fine. She does not use tobacco, alcohol , or illicit drugs . Her medications include
11
valsartan and hydrochlorothiazide. Which of the following is the most likely diagnosis?
12
0
0
0
0
0
13
14
~
6
17
18
19
A. Delirium
B. Dementia
C. Depression
D. Normal aging
E.
Presby cu sis
20
21
Submit
22
•
~
4
25
•
26
27
•
28
29
•
30
31
•
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
Settings
~
~
1
•
= .
-
•\
~
ltem2of39
Question Id: 5465
Mart<
<]
C>
r,
Previous
Next
Fun Screen
L .J
•!
I'>\
\.!..)
Tutorial
1111
Lab Yallles
m; ',
Notes
rim
,
ffiffij
Calculator
Reverse Color
~
~
Text Zoom
Settings
~
~
3
•
4
A 76-year-old woman is brought to the physician by her son. He is concerned that his mother, who was previously outgoing , does not want to
s
leave her home. She lives alone and works as a part-time volunteer at a local library. Although she continues to work shelving books, she has
6
stopped attending her weekly meetings at a senior center where she socialized with friends. The patient also seems quieter and more difficult to
7
engage in conversation when he calls her on the telephone. One w eek ago, he found her sitting on a chair pulled up close to the television. She
8
did not notice his presence immediately but then smiled and nodded as if following the conversation. He became concerned when she asked
9
about her grandchild's upcoming birthday party even though he had just told her the details. Her past medical history is significant for
10
hypertension . The patient reports that her sleep and appetite are fine. She does not use tobacco, alcohol , or illicit drugs . Her medications include
11
valsartan and hydrochlorothiazide. Which of the following is the most likely diagnosis?
12
A. Delirium (0%)
13
B. Dementia (1 9%)
14
~
C. Depression (13°A,)
6
D. Normal aging (8°/o)
17
18
E. Presbycusis (57o/o)
19
20
21
Omitted
22
•
~
E
This patient's clinical features are most consistent with presbycusis, or age-related hearing loss, which has resulted in progressive social
28
withdrawal. Presbycusis is a gradual, symmetrical, sensorineural hearing loss that affects more than 50% of adults by age 75 and can significantly
-
29
•
\.::) nme Spent
07/01/2020
• Last Updated
Explanation
26
27
•
, i \ 01 sec
4
25
•
I 11. 57%
I.!!!.. Answered correctty
Correct answer
30
31
•
TUTOR
https://t.me/USMLEWorldStep3
~
F2ck
SgJ2,d
Eng ock
1
•
= .
-
ltem2of39
Question Id: 5465
•\
~
Mart<
<]
C>
r,
Previous
Next
Fun Screen
L .J
•!
I'>\
\.!..)
Tutorial
1111
Lab Yallles
m; ',
Notes
rim
ffiffij
Calculator
4
This patient's clinical features are n1ost consistent with presbycusis, or age-related hearing loss, which has resulted in progressive social
s
withd rawal. Presbycusis is a gradual , symmetrical, sensorineural hearing loss that affects n1ore than 50% of adults by age 75 and can significantly
6
impair quality of life. Patients typically withdraw fron1 their social lives and may stop leaving home to avoid conversations. Their social interactions
7
deteriorate and they often must listen to the radio or television at high volumes. Physical examination may show no abnormalities except for the
8
hearing loss itself. Although audiometry is used to confirm the diagnosis, the whispered voice test, a simple procedure that can be perfom,ed in
9
the office without equipment, can be used. In this test, the examiner stands behind the patient and whispers letters/numbers while occluding the
non-tested ear. Repeating 3 out of 6 letters/numbers correctly is passing.
10
11
Progressive social withdrawal n1ay contribute to feelings of depression and low self-esteem . However, apart fron1 decreased motivation to
12
socialize, this patient does not exhibit features of major depression (ie, >5 of following 9 symptoms: depressed mood, anhedonia, sleep
13
disturbance, appetite disturbance, psychomotor abnon11alities, impaired concentration, fatigue, guilt, suicidality) (Choice C).
14
Most patients with presbycusis benefit fron1 the use of hearing aids, which should decrease social isolation.
~
(Choice A) Deliriun1 is a reversible, acute confusional state involving fluctuating levels of consciousness and inattention. It is most commonly
6
seen in elderly patients with medical illness.
17
18
(Choice B) Dementia involves an irreversi ble, global deterioration in cognitive abilities and functioning, which frequently includes short-term
19
memory problems, impaired communication skills, and a decli ne in activities of daily living. Although this patient could be experiencing very early
20
signs of dementia, there is insufficient information to support this diagnosis_
21
(Choice D) Although tlle prevalence of presbycusis increases with age, progressive social isolation should not be attributed to normal aging.
22
•
•
Appropriate diagnosis and treatment with a hearing aid should reverse this patient's social withdrawal and improve her quality of life.
~
Educational objective:
4
25
Hearing loss due to presbycusis is one of the most frequent causes of social withdrawal and isolation in the elderly. It must be differentiated fron1
26
depression and dementia. Screening can be accomplished through simple hearing tests perfon11ed in the office.
27
References
28
• Hearing loss and depressive symptoms in elderly patients.
29
•
30
31
Reverse Color
~
~
Text Zoom
Settings
~
~
•
3
•
,
•
https://t.me/USMLEWorldStep3
1
•
= .
-
ltem2of39
Question Id: 5465
3
•\
~
Mart<
<]
C>
r,
Previous
Next
Fun Screen
L .J
•!
I'>\
\.!..)
Tutorial
1111
Lab Yallles
m; ',
Notes
rim
ffiffij
Calculator
hearing loss itself. Although audiometry is used to confirm the diagnosis, the whispered voice test, a simple procedure that can be performed in
4
the office without equipment, can be used. In this test, the examiner stands behind the patient and whispers letters/numbers while occluding the
s
non-tested ear. Repeating 3 out of 6 letters/numbers correctly is passing.
6
7
Progressive social withd rawal may contribute to feelings of depression and low self-esteem. However, apart fron1 decreased motivation to
8
socialize, this patient does not exhibit features of n1ajor depression (ie, >5 of following 9 sympton1s: depressed mood, anhedonia, sleep
disturbance, appetite disturbance, psychomotor abnormalities, impaired concentration, fatigue, guilt, suicidality) (Choice C).
9
10
Most patients with presbycusis benefit fron1 the use of hearing aids, which should decrease social isolation.
11
(Choice A) Deliriun1 is a reversible, acute confusional state involving fl uctuating levels of consciousness and inattention. It is most commonly
12
seen in elderly patients with n1edical illness.
13
(Choice B) Dementia involves an irreversible, global deterioration in cogniiive abilities and functioning, which frequently includes short-term
14
~
men1ory problems, impaired communication skills, and a decline in activities of daily living. Although this patient could be experiencing very early
signs of dementia, there is insufficient information to support this diagnosis.
6
17
(Choice D) Although the prevalence of presbycusis increases with age, progressive social isolation should not be attributed to nom1al aging.
18
Appropriate diagnosis and treatment with a hearing aid should reverse this patient's social withdrawal and improve her quality of life.
19
Educational objective:
20
Hearing loss due to presbycusis is one of the most frequent causes of social withdrawal and isolation in the elderly. It must be differentiated fron1
21
depression and dementia. Screening can be accomplished through simple hearing tests performed in the office.
22
•
References
~
• Hearing loss and depressive symptoms in elderly patients.
4
25
•
26
27
•
Foundations of Independent Practice
Ear, Nose & Throat (ENT)
Hearing loss
Subject
System
Topic
opyng
28
I@ .JWorid
Is
...
29
•
30
31
•
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
Settings
~
~
•
1
•
2
= .
-
ltem 3of39
Question Id: 5231
•\
~
Mart<
<]
C>
r,
Previous
Next
Fun Screen
L .J
•!
I'>\
\.!..)
Tutorial
Lab Yallles
Calculator
week history of worsening lower back pain. He has tried several over-the-counter medications without significant relief. He smokes 2 packs daily
6
and consumes alcohol occasionally. A chest x-ray reveals a right superior lobe mass. Which of the following additional findings, if present, would
7
indicate a worse prognosis requiring urgent intervention?
0
0
0
0
0
11
12
13
14
~
A. Asymmetric upper-extremity deep-tendon reflexes
B.
Right hand muscle atrophy and weakness
C. Right lower-extremity hyperreflexia
D. Pupil size asymmetry and asymmetric palpebral fissures
E. Streaky hemoptysis and weight loss
6
17
Submit
18
19
20
21
22
~
4
25
26
27
28
29
•
ffiffij
s
10
•
Notes
rim
A 55-year-old n,an with a history of chronic low back pain comes to the physician with a 3-week history of progressive right shoulder pain and a 1-
9
•
m; ',
4
8
•
1111
30
31
•
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
Settings
~
~
1
•
2
= .
-
ltem 3of39
Question Id: 5231
•\
~
Mart<
<]
C>
r,
Previous
Next
Fun Screen
L .J
•!
I'>\
\.!..)
Tutorial
1111
Lab Yallles
m; ',
Notes
rim
ffiffij
Calculator
,
Reverse Color
~
~
Text Zoom
Settings
~
~
•
4
A 55-year-old n,an with a history of chronic low back pain comes to the physician with a 3-week history of progressive right shoulder pain and a 1-
s
week history of worsening lower back pain. He has tried several over-the-counter medications without significant relief. He smokes 2 packs daily
6
and consumes alcohol occasionally. A chest x-ray reveals a right superior lobe m ass. Which of the following additional findings, if present, would
7
indicate a worse prognosis requiring urgent intervention?
8
A. Asymmetric upper-extremity deep-tendon reflexes (5°/o)
9
10
B. Right hand muscle atrophy and weakness (1 1°/o)
11
C. Right lower-extremity hyperreflexia (19%)
12
D. Pupil size asymmetry and asymmetric palpebral fissures (44°/o)
13
14
E . Streaky hemoptysis and weight loss (1 8°/o)
~
6
17
Omitted
18
Correct answer
C
19
111.
l!l!.
19%
Answered correctly
,i'\ 01 sec
\::J
Time Spent
F=! 04/03/2020
13 Last Updated
20
21
Explanation
22
•
~
4
Common manifestations of superior pulmonary sulcus tumor
25
•
• Shoulder pai n
26
• Hom er syndrome (invasion of paravertebral sympathetic chain/stellate ganglion)
27
•
o lpsilateral ptosis, miosis, enophthalm os & anhidrosis
28
• Neurologic symptoms in the arm (invasion of C8-T2 nerves)
29
•
30
31
•
https://t.me/USMLEWorldStep3
1
•
2
= .
-
ltem 3of39
Question Id: 5231
•\
~
Mart<
<]
C>
r,
Previous
Next
Fun Screen
L .J
•!
I'>\
\.!..)
Tutorial
1111
Lab Yallles
m; ',
Notes
rim
ffiffij
Calculator
,
Reverse Color
~
~
Text Zoom
Settings
~
~
•
4
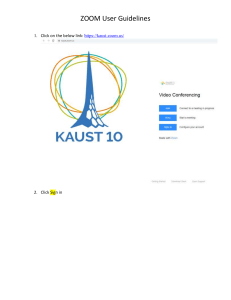
Common manifestations of superior pulmonary sulcus tumor
s
6
• Shoulder pai n
7
, Hom er syndrome (invasion of paravertebral sympathetic chain/stellate ganglion)
o
8
lpsilateral ptosis, miosis, enophthal mos & anhidrosis
, Neurologic symptoms in the arm (invasion of C8-T2 nerves)
9
o Weakness/atrophy of intrinsic hand m uscles
10
o Pai n/paresthesia of 4th/5th digits & medial arm/forearm
11
, Supraclavicular lymphadenopathy
12
, Weight loss
13
14
The description in the vignette is consistent with super ior pulmonary sulcus (Pancoast) tumor, generally a subset of non-sm all cell lung
~
cancer. Shoulder pain is the most common initial presentation. The history and physical examination may assist in assessing the extent of
6
neoplastic spread and determining prognosis.
17
Pancoast syndrome consists of shoulder pain (50%-90°/o), Horner's syndrome (15%-50o/o), and hand muscle atrophy and weakness (10%-20%).
18
However, asymmetric lower-extremity deep-tendon reflexes, particularly in the setting of back pain, suggest that the tumor has spread to the
19
spinal cord . Spinal cord compress ion develop s in up to 25°A. of patients with Pancoast tumor during the course of the disease and m ay result in
20
paraplegia. Early recognition and appropriate therapy (which may include corticosteroid therapy, surgery, and radiation) is im perative to preserve
21
neurologic function and patient autonomy.
22
•
~
Pancoast tumor
4
25
•
Phrenic nerve
26
Sympathetic
trunk
27
•
Vagus nerve~
28
29
•
30
31
•
https://t.me/USMLEWorldStep3
1
•
2
=
ltem 3of39
Question Id: 5231
. ~
<]
C>
~~
G)
il
'!,·
Previous
Next
Fun Screen
Tutorial
Lab varues
Notes
Mart<
\
= ,
Calculator
Reverse Color
~
@
Text Zoom
Settings
neurologic function and patient autonomy.
•
4
s
Pancoast tumor
6
7
Sympathetic
trunk
Phrenic nerve
8
9
Vagus nerve~
10
11
Brachia!
plexus
12
13
14
~
6
Rib 2
17
18
/Rib3
19
20
21
22
•
~
4
25
•
26
27
•
Subclavian
artery & vein
28
29
•
30
31
•
TUTOR
Pancoast
tumor
Recurrent
laryngeal
.- . -
https://t.me/USMLEWorldStep3
~
F2ck
SgJ2,d Eng ock
1
2
4
s
6
7
8
Subclavian
artery & vein
9
10
11
Pancoast
tumor
© UWorld
12
Recurrent
laryngeal
nerve
(Choices A and B) Brachia! plexopathy is a typical complication of superior sulcus tumor that may lead to atrophy of the internal muscles of the
13
hand and asymmetric upper-extremity deep-tendon reflexes.
14
(Choice D) Pupil size asymmetry and asymmetric palpebral fissures result from invasion of the paravertebral sympathetic chain (Horner's
~
syndron1e). Horner's syndrome is considered to be a poor prognostic sig n, but it is not imn1ediately dangerous.
6
17
(Choice E) Streaky hemoptysis and weight loss are typi cal sympton1s of lu ng cancer that are not dangerous per se. Given the peripheral location
18
of Pancoast tumors, pulmonary symptoms tend to occur at a more advanced stage.
19
Educational objective:
20
Spi nal cord compression develops in up to 25% of patients with Pancoast tumor during the course of the disease. Early recognition and
21
appropriate therapy are imperative to preserve neurologic function and patient autonomy.
22
•
References
~
• Superior pulmonary sulcus tumors and Pancoast's syndrome.
4
25
•
26
27
•
Foundations of Independent Practice
Hen1atology & Oncology
Subject
System
opyng
28
I@ ..JWorla
Spinal cord compression
Topic
Is
...
29
•
30
31
•
https://t.me/USMLEWorldStep3
1
•
2
= .
-
Item 4 of39
Question Id: 5136
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
Lab Yallles
m,
;'
Notes
rim
ffiffij
Calculator
3
A 23-year-old woman comes to the physician for treatment of acne vulgaris. She has moderate comedonal acne affecting the face, neck, and
s
shoulders. The patient has attempted treatment with topical azelaic acid without improvement. She has no other med ical problen1s. She is
6
married and has no children. The patient does not smoke but drinks alcohol socially on weekends. W hat additional information is needed before
7
advising this patient on treatment options?
8
0
0
0
0
0
9
10
11
12
13
14
~
A. Family history of skin cancer
B.
History of antibiotic allergies
C. Liver function tests
D. Plans for possible pregnancy
E. Serum lipid levels
6
17
Submit
18
19
20
21
22
•
~
4
25
•
26
27
•
28
29
•
30
31
•
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
1
2
•
= .
-
Item 4 of39
Question Id: 5136
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
rim
Tutorial
Lab Yallles
Notes
Calculator
\.!..)
1111
;'
ffiffij
A 23-year-old woman comes to the physician for treatment of acne vulgaris. She has moderate comedonal acne affecting the face, neck, and
s
shoulders. The patient has attempted treatment with topical azelaic acid without improvement. She has no other med ical problen1s. She is
6
married and has no children. The patient does not smoke but drinks alcohol socially on weekends. W hat additional information is needed before
7
advising this patient on treatment options?
8
10
11
12
13
14
~
A. Family history of skin cancer (0%)
B. History of antibiotic allergies (12%)
C. Liver function tests ( 1°/o)
D. Plans for possible pregnancy (85o/o)
E . Serum lipid levels (0%)
6
17
18
19
Omitted
Correct answer
D
111.
l!l!.
85%
Answered correctly
,i'\ 01 sec
\::J
Time Spent
F=! 03/23/2020
13 Last Updated
20
21
22
•
~
•
28
29
•
Treatement of acne vulgaris
26
27
•
Explanation
4
25
30
31
Reverse Color
~
~
Text Zoom
~
~
Settings
•
3
9
,
Comed onal acne
• Closed or open comedones on forehead, nose & chin
• May progress to inflammatory pustules or nodules
https://t.me/USMLEWorldStep3
1
•
2
= .
-
•\
~
Item 4 of39
Question Id: 5136
Mart<
3
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
1111
;'
rim
,
ffiffij
Calculator
Reverse Color
~
~
Text Zoom
~
~
Settings
•
Treatement of acne vulgaris
s
Comedonal acne
6
• Closed or open comedones on foreh ead, nose & chin
7
• May progress to inflammatory pu stules or nodules
8
• Treatment: Topical retinoids; salicylic, azelaic, or glycolic acid
9
10
Inflammatory acne
11
• Inflamed papules (<5 mm) & pustules; erythema
12
• Treatment:
13
o Mild: Topical retinoids + benzoyl peroxide
14
o Moderate: A dd topical antibiotics (eg , erythromycin, clindamycin)
~
o Severe: Add o ral antibiotics
6
Nodular (cystic) acne
17
18
• Large (>5 mm) nodules that can appear cystic
19
• Nodules may merge to form sinus tracts with possible scarring
20
• Treatment:
o Moderate: Topical re tin oid + benzoyl peroxide + topical antibiotics
21
o Severe: Add oral antibiotics
22
•
•
•
o Unresponsive severe: Oral isotretinoi n
~
©UWorld
4
25
This patien t has m oderate comedonal acne which has failed initial therapy with topical organic acids. In most cases, the appropriate
26
management would be topical retinoid therapy - adapalene, tretinoin, or tazarotene. However, th e potential for pregnancy n1ay influence the
27
choice of treatment for women of childbearing age.
28
For w omen who are pregnant or may become pregnant, topical erythromycin, d indamycin (inflammatory acne), or azelaic acid (comedonal acn e)
-.
29
•
30
31
•
TUTOR
.
https://t.me/USMLEWorldStep3
~
F2ck
SgJ2,d
Eng ock
1
•
2
= .
-
Item 4 of39
Question Id: 5136
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
1111
;'
rim
ffiffij
Calculator
3
This patient has moderate comedonal acn e which has failed initial therapy with topical organic acids. In most cases, the appropriate
management would be topical retinoid therapy - adapalene, tretinoin, or tazarotene. However, the potential for pregnancy may influence the
s
choice of treatment for women of childbearing age.
6
7
For women who are pregnant or may become pregnant, topical erythromycin, d indamycin (inflammatory acne), or azelaic acid (comedonal acne)
8
are designated FDA pregnancy risk category B and are generally considered safe. The risk of teratogenicity with topical retinoids is considered
9
low and most (eg, tretinoin, adapalene) are designated category C. However, tazarotene and the oral retinoid isotretinoin are designated category
X and should never be used in pregnancy. Pregnancy risk of medications for acne includes:
10
11
• Category B: Azelaic acid, topical clindamycin, topical/oral erythromycin
12
• Category C: Adapalene, tretinoin, topical dapsone, benzoyl peroxide, sodium sulfacetamide
13
• Category D: Oral tetracyclines
14
• Category X: Tazarotene, isotretinoin
~
(Choice A) Even though isotretinoin and tazarotene are teratogenic, retinoid medications are not carcinogenic. Therefore, family history of skin
6
cancer is not a specific concern.
17
(Choice B) Topical and oral antibiotics are used for inflammatory and nodulocystic acne but are not used routinely in comedonal acne.
18
(Choices C and E) Liver function tests and serum lipid levels should be performed regularly in patients treated with oral (but not topical) retinoids.
19
20
Educational objective:
21
For treatment of acne in women who n1ay become pregnant, the preferred medications include topical erythromycin, clindamycin (inflamn1atory
22
•
acne), or azelaic acid (comedonal acne); these are designated FDA pregnancy risk category B. Topical tretinoin and benzoyl peroxide should be
~
avoided in pregnancy (category C). Tazarotene and isotretinoin are potent teratogens that are absolutely contraindicated in pregnancy (category
4
X).
25
•
References
26
• The management of acne vulgaris in pregnancy.
27
•
28
Fou ndations of Independent Practice
29
•
30
31
•
Dermatology
Acne vulgaris
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
•
1
•
2
= .
-
Item 4 of39
Question Id: 5136
3
•\
~
Mart<
. . . -.. . ... -.- . ..... .
<]
C>
Previous
Next
r,
I'>\
\.!..)
L .J
Fun Screen
Tutorial
•!
1111
Lab Yallles
.. . .... . -.. - ·---=· . ... · ··-· . . . ...
Exhibit Display
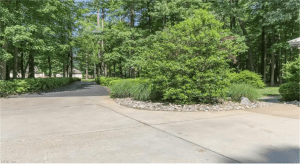
US FDA drug risk categories during pregnancy
7
Category
Studies
Recommendations
A
Human & animal studies with no fetal
risk
Safe for use in
pregnancy
B
Animal studies did not show fetal risk,
no human studies done
or
Animal studies showed fetal risk,
human studies showed no risk
Likely safe to use in
pregnancy
C
Fetal risk in animal studies without
adequate human studies
or
No adequate animal or human studies
Use only If potential
benefit outweighs risk
D
Positive fetal risk in human studies or
postma rketi ng surveillance
X
Fetal risk in animal or human studies
or postmarketing surveillance
8
9
10
11
12
13
14
~
6
17
18
19
20
21
Potential benefit may
justify risk in severe
circumstances
22
•
~
4
25
•
26
•
©_
Zoom In
8_
Zoom Out
C
Reset
fl,
Add To Flash Card
28
rac ice
29
•
Potential benefits
do not Justify use in
any circumstances
OUWodd
27
30
31
•
erma o ogy
cne vu gans
https://t.me/USMLEWorldStep3
;'
Notes
. - .- ..... . -
s
6
m,
rim
ffiffij
Calculator
~
~
,
Reverse Color
Text Zoom
~
~
Settings
•
r5l
~
1
•
2
= .
-
ltem5 of39
Question Id: 6280
•\
~
Mart<
<]
C>
r,
Previous
Next
Fun Screen
L .J
•!
I'>\
\.!..)
Tutorial
1111
Lab Yallles
m; ',
Notes
rim
ffiffij
Calculator
3
4
A 10-month-old boy is brought to clinic for evaluation of decreased activity. The patient has been progressively tired over the past few weeks. He
normally is able to crawl and pull up to a stand, but lately he is so tired that he prefers to sit still. The boy is primarily breastfed and eats some
6
pureed fruits. He has 6 or 7 wet diapers and 3 soft stools per day. He has no known medical conditions or prior hospitalizations. The patient lives
7
with his parents and 3-year-old sister, none of whom have chronic medical conditions. His parents are originally from Ghana and moved to the
8
United States 4 years ago. Temperature is 36.7 C (98 F) and pulse is 100/min. Examination shows n1ild conjunctiva! pallor. The lungs are clear
9
to auscultation. A 2/6 systolic murmur is auscultated over the precordium. The abdomen is soft and nontender, and bowel sounds are present.
Laboratory results are as follows:
10
11
Hemoglobin
8.1 g/dl
13
Mean corpuscular volume
65 µm3
14
Total red blood cell count
3.5 million/mm3 (normal: 4-6)
12
~
Which of the following is the most likely cause of this child's anemia?
6
Q
Q
Q
Q
Q
17
18
19
20
21
22
•
~
A. Breast milk- predominant diet
B. Chronic lead ingestion
C. Deficiency of alpha-hemoglobin chains
D. Deficiency of beta-hemoglobin chains
E. Glucose-6-phosphate dehydrogenase deficiency
4
25
•
26
Submit
27
•
28
29
•
30
31
•
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
Settings
~
~
1
•
2
= .
-
ltem5 of39
Question Id: 6280
•\
~
Mart<
<]
C>
r,
Previous
Next
Fun Screen
L .J
•!
I'>\
\.!..)
Tutorial
1111
Lab Yallles
m; ',
Notes
rim
ffiffij
Calculator
4
A 10-month-old boy is brought to clinic for evaluation of decreased activity. The patient has been progressively tired over the past few weeks. He
normally is able to crawl and pull up to a stand, but lately he is so tired that he prefers to sit still. The boy is primarily breastfed and eats some
6
pureed fruits. He has 6 or 7 wet diapers and 3 soft stools per day. He has no known medical conditions or prior hospitalizations. The patient lives
7
with his parents and 3-year-old sister, none of whom have chronic medical conditions. His parents are originally from Ghana and moved to the
8
United States 4 years ago. Temperature is 36.7 C (98 F) and pulse is 100/min. Examination shows n1ild conjunctiva! pallor. The lungs are clear
9
to auscultation. A 2/6 systolic murmur is auscultated over the precordium. The abdomen is soft and nontender, and bowel sounds are present.
Laboratory results are as follows:
10
11
Hemoglobin
8.1 g/dl
13
Mean corpuscular volume
65 µm3
14
Total red blood cell count
3.5 million/mm3 (normal: 4-6)
12
~
Which of the following is the most likely cause of this child's anemia?
6
17
A. Breast milk- predominant diet (38%)
18
19
B. Chronic lead ingestion (4°/o)
20
C. Deficiency of alpha-hemoglobin chains (18o/o)
21
D. Deficiency of beta-hemoglobin chains (33%)
22
~
E. Glucose-6-phosphate dehydrogenase deficiency (5%)
4
25
•
•
26
Omitted
27
Correct answer
28
A
'"· 38%
l!!!.
Answered correcUy
, i \ 02 secs
\..::J
Time Spent
29
•
30
31
Reverse Color
~
~
Text Zoom
Settings
~
~
•
3
•
,
•
https://t.me/USMLEWorldStep3
06/29/2020
• Last Updated
1
2
•
= .
-
ltem5 of39
Question Id: 6280
•\
~
C>
<]
Mart<
Previous
Next
r,
L .J
Fun Screen
•!
m,
rim
Lab Yallles
Notes
Calculator
I'>\
\.!..)
Tutorial
11111
;'
ffiffij
4
Iron deficiency anemia in young children
6
, Prematurity
7
, Lead exposure
8
• Age <1
9
o
Risk factors
11
Delayed introduction of solids
(ie, exclusive breastfeeding after 6 months)
o
12
Cow's, soy, or goat's milk
, Age >1
13
o >24 oz/day cow's milk
14
o <3 servings/day iron-rich foods
~
6
Diagnosis
, Screening hemoglobin at age 1
• Hemoglobin <11 g/dl, ! MCV, l ROW
17
18
19
Treatment
, Empiric trial of iron supplementation
MCV = mean corpuscular volume; ROW = red blood cell distribution width.
20
21
22
•
•
•
~
4
Iron deficiency is the most common cause of anemia in infants in the United States. It is typically due to inadequate dietary iron, as in breastfed
infants age >6 months who do not eat enough iron-rich foods or any infant who drinks cow's milk before age 1 year. Premature infants are also at
increased risk due to inadequate iron stores.
Most children with iron deficiency are asymptomatic; however, if symptomatic, the most common findings are lethargy, irritability, pallor, and a
25
systolic flow murmur, as seen in this patient. Severe anemia can cause cardiomegaly and tachypnea.
26
Classic laboratory findings include hemoglobin <11 g/dL, often accompanied by low mean corpuscular volume (MCV), elevated red blood cell
27
(RSC) distribution width, and a low RSC count. A Mentzer index (MCV/RBC) >1 3 is also suggestive of iron deficiency and can help differentiate it
28
from thalassemia; in this patient, the Mentzer index is 65/3.5
= 18.6. Alpha and beta thalassemias are also microcyticbut characterized by a
29
•
30
31
Reverse Color
~
~
Text Zoom
Settings
~
~
•
3
10
,
https://t.me/USMLEWorldStep3
1
•
2
= .
-
ltem5 of39
Question Id: 6280
•\
~
Mart<
<]
C>
r,
Previous
Next
Fun Screen
L .J
•!
I'>\
\.!..)
1111
Tutorial
Lab Yallles
m; ',
Notes
rim
,
ffiffij
Calculator
Reverse Color
~
~
Text Zoom
Settings
~
~
•
3
4
Iron deficiency is the most common cause of anemia in infants in the United States. It is typically due to inadequate dietary iron, as in breastfed
infants age >6 months who do not eat enough iron-rich foods or any infant who drinks cow's milk before age 1 year. Premature infants are also at
increased risk due to inadequate iron stores.
6
7
Most children with iron deficiency are asymptomatic; however, if symptomatic, the most common findings are lethargy, irritability, pallor, and a
8
systolic flow murmur, as seen in this patient. Severe anemia can cause card iomegaly and tachypnea.
9
Classic laboratory findings include hemoglobin <11 g/dL, often accompanied by low mean corpuscular volume (MCV), elevated red blood cell
10
(RBC) distribution width, and a low RBC count. A Mentzer index (MCV/RBC) >1 3 is also suggestive of iron deficiency and can help differentiate it
11
from thalassemia; in this patient, the Mentzer index is 65/3.5
12
= 18.6. Alpha and beta thalassemias are also microcytic but characterized by a
Mentzer index <13 (Choices C and D).
13
14
Although breastfeeding is recommended for at least the first year of life, iron-fortified cereals, pureed meats, and foods rich in vitamin C (to
~
enhance iron absorption) should be introduced around age 6 months. In addition to iron-rich foods, this patient will also require oral iron
therapy to replenish iron stores.
6
17
(Choice B) Chronic lead ingestion causes normocytic, hemolytic anemia. This patient with a low MCV and poor dietary iron intake is more likely
18
to have iron deficiency anemia.
19
(Choice E) Glucose-6-phosphate dehydrogenase deficiency is an X-linked disorder that may be asymptomatic until exposure to oxidant
20
medications or substances causes acute hemolytic anemia. Acute hemolytic anemia is typically characterized by a normal MCV. In addition, this
21
patient's history is suggestive of a chronic, gradual process rather than an acute event.
22
•
~
Educational objective :
Iron deficiency anemia is common in infancy and is characterized by hemoglobin <11 g/dl, low mean corpuscular volume, and Mentzer index
4
>13. Although breast milk provides sufficient iron for the first few months of life, introducing iron-rich foods (eg, pureed meats) arou nd age 6
25
•
months is necessary to prevent iron deficiency.
26
References
27
•
• Iron deficiency anemia in predominantly breastfed young children.
28
-
29
•
30
31
•
TUTOR
.
https://t.me/USMLEWorldStep3
~
F2ck
SgJ2,d
Eng ock
1
•
2
= .
-
ltem6 of39
Question Id: 5885
•\
~
Mart<
<]
C>
r,
Previous
Next
Fun Screen
L .J
•!
I'>\
\.!..)
Tutorial
1111
Lab Yallles
m; ',
Notes
rim
ffiffij
Calculator
3
4
A 59-year-old n,an comes to the office complaining of a vague upper abdominal discomfort. The pain has been present for most of the past 3
s
months but has never been severe enough to make him seek immediate medical attention. The discomfort is not associated with eating or
performing any activities. He has no other medical problems. His blood pressure is 120/60 mm Hg, pulse is 84/min, and respirations are 14/min.
7
Abdominal examination reveals the presence of multiple scars from previous surgical procedures around the epigastric area. A 3 x 5-cm, oblong-
8
shaped, firm, and deeply seated mass is palpable in the epigastric area. There is no tenderness on direct palpation of the mass and surrounding
9
epigastric area. The patient says that he previously had similar "things" in the same area "but they were taken out." Which of the following is the
most likely diag nosis?
10
11
Q
Q
Q
Q
Q
12
13
14
~
6
17
A. Dermatofibroma
8 . Desmoid tumor
C. Epidermoid cyst
D. Lipoma
E. Pyogenic granuloma
18
19
20
Submit
21
22
•
~
4
25
•
26
27
•
28
29
•
30
31
•
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
Settings
~
~
1
•
2
= .
-
ltem6 of39
Question Id: 5885
•\
~
Mart<
<]
C>
r,
Previous
Next
Fun Screen
L .J
•!
I'>\
\.!..)
Tutorial
1111
Lab Yallles
m; ',
Notes
rim
,
ffiffij
Calculator
Reverse Color
~
~
Text Zoom
Settings
~
~
•
3
4
A 59-year-old n,an comes to the office complaining of a vague upper abdominal discomfort. The pain has been present for most of the past 3
s
months but has never been severe enough to make him seek immediate medical attention. The discomfort is not associated with eating or
performing any activities. He has no other medical problems. His blood pressure is 120/60 mm Hg, pulse is 84/min, and respirations are 14/min.
7
Abdominal examination reveals the presence of multiple scars from previous surgical procedures around the epigastric area. A 3 x 5-cm, oblong-
8
shaped, firm, and deeply seated mass is palpable in the epigastric area. There is no tenderness on direct palpation of the mass and surrounding
9
epigastric area. The patient says that he previously had similar "things" in the same area "but they were taken out." Which of the following is the
most likely diag nosis?
10
11
A. Dermatofibroma (26°/o)
12
,./ ,
13
14
8 . Desmoid tumor (36%)
C. Epidermoid cyst (9o/o)
~
D. Lipoma (24°/o)
6
17
E. Pyogenic granuloma (3%)
18
19
20
Omitted
21
Correct answer
22
•
8
~
26
This patient presents with an abdominal mass and mild pain consistent with a likely desmoid tumor, w hich is a locally aggressive benign tumor
arising from fibroplastic elements within the muscle or fascia! planes with very low potential for metastasis or differentiation. Desmoid tumors are
28
rare but increased in patients with familial adenomatosis polyposis (i.e., Gardner syndrome) and thought to be due to abnormal wound healing or
.
29
•
'\.::) Time Spent
Answered correctly
03/08/2020
• Last Updated
Explanation
27
•
l!!!.
('j'\ 01 sec
4
25
•
111, 36%
30
31
•
TUTOR
https://t.me/USMLEWorldStep3
~
F2ck
SgJ2,d
Eng ock
1
2
•
= .
-
ltem6 of39
Question Id: 5885
•\
~
Mart<
<]
C>
r,
Previous
Next
Fun Screen
L .J
•!
I'>\
\.!..)
Tutorial
1111
Lab Yallles
m; ',
Notes
rim
ffiffij
Calculator
3
This patient presents with an abdominal mass and mild pain consistent with a likely desmoid tumor, which is a locally aggressive benig n tumor
4
arising from fibroplastic elements within the n1uscle or fascia! planes with very low potential for metastasis or differentiation. Desmoid tumors are
s
rare but increased in patients with familial adenomatosis polyposis (i.e., Gardner syndrome) and thought to be due to abnormal wound healing or
clonal chromosomal abnormalities causing a neoplastic behavior. This tumor has a variable clinical course, can range from slow to rapid growth,
7
and has varying sizes. Desmoid tumors typically present as deeply seated painless or sometimes painful masses in the trunk/extremity,
8
intraabdominal bowel and mesentery, and abdominal wall. They can cause intestinal obstruction and bowel ischemia and have a high rate of
9
recurrence, even after aggressive surgery (as in this patient).
10
11
12
13
14
~
6
17
Computed tomography scan or MRI should be done to evaluate the size of the mass, with biopsy for histologic diagnosis. Surgery is the definitive
therapy for desmoid tumors that are symptomatic, cause risk to adjacent structures or cosmetic issues for the patient, or are recurrent. Patients
who are not surgical candidates can be treated w ith radiation therapy. Close observation is an alternative strategy in patients who are
asymptomatic, have stable masses, or have intraabdominal masses seen in Gardner syndrome. This mildly symptomatic patient has had multiple
surgeries to remove his likely recurrent desmoid tumor and can be treated with close observation, another surgery, or possibly radiation therapy,
dependi ng on his preference and surgical risk.
(Choice A) A dermatofibroma is a benign proliferation of fibroblasts that usually occurs after trauma or insect bite and can also be idiopathic. It is
usually a firm hyperpigmented nodule located on the lower extremities rather than the abdon1en.
18
•
19
(Choice C) An epidermoid cyst is a discrete nodule that is usually located on the skin and a result of the normal epidermal keratin becoming
20
lodged in the dermis. Epidermoid cysts can be seen in Gardner synd rome but are usually located on the extremities rather than the trunk or
21
abdomen and resolve spontaneously without treatment.
22
(Choice D) A lipon1a is an asyn1ptomatic and benign subcutaneous collection of fat cells. It is usually soft without rapid enlargement or recurrence
~
4
25
•
(Choice E) A pyogenic granuloma (granuloma telangiectaticum) is caused by capillary proliferation after trauma and usually presents as a domeshaped papule with recurrent bleedi ng. It is more commonly seen in pregnant women and a less likely cause in this patient.
26
27
•
after resection, n1aking it less likely in this patient.
28
Educational objective:
Desmoid tumors are slow-growing and locally aggressive benign neoplasms w ith a high rate of local recurrence, even after surgical excision.
29
•
30
31
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
Settings
~
~
•
1
•
2
= .
-
ltem6 of39
Question Id: 5885
3
•\
~
C>
<]
Mart<
Previous
Next
r,
L .J
Fun Screen
•!
m,
Lab Yallles
Notes
I'>\
\.!..)
Tutorial
11111
;'
rim
ffiffij
Calculator
therapy for desmoid tumors that are symptomatic, cause risk to adj acent structures or cosmetic issues for the patient, or are recurrent. Patients
4
who are not surgical candidates can be treated w ith radiation therapy. Close observation is an alternative strategy in patients who are
s
asymptomatic, have stable masses, or have intraabdominal masses seen in Gardner syndrome. This mildly symptomatic patient has had multiple
surgeries to remove his likely recurrent desmoid tumor and can be treated with close observation, another surgery, or possibly radiation therapy,
7
depending on his preference and surgical risk.
8
(Choice A) A dermatofibroma is a benign proliferation of fibroblasts that usually occurs after trauma or insect bite and can also be idiopathic. It is
9
usually a firm hyperpigmented nodule located on the lower extremities rather than the abdomen.
10
11
(Choice C) An epidermoid cyst is a discrete nodule that is usually located on the skin and a result of the normal epidermal keratin becoming
12
lodged in the dermis. Epidermoid cysts can be seen in Gardner syndrome but are usually located on the extremities rather than the trunk or
13
abdomen and resolve spontaneously without treatment.
14
(Choice D) A lipon1a is an asymptomatic and benign subcutaneous collection of fat cells. It is usually soft without rapid enlargement or recurrence
~
after resection, n1aking it less likely in this patient.
6
(Choice E) A pyogenic granulon1a (granuloma telangiectaticum) is caused by capillary proliferation after trauma and usually presents as a dome-
17
shaped papule with recurrent bleeding. It is more commonly seen in pregnant women and a less likely cause in this patient.
18
19
Educational objective :
20
Desmoid tumors are slow-growing and locally aggressive benign neoplasms w ith a high rate of local recurrence, even after surgical excision.
21
References
22
•
• The enigma of desmoid tumors.
~
• Desmoid tumor: from surgical extirpation to molecular dissection
4
25
•
26
27
•
Foundations of Independent Practice
Dermatology
Desmoid Tumor
Subject
System
Topic
C
28
I@
29
•
30
31
•
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
Settings
~
~
•
1
2
•
= .
-
ltem7 of39
Question Id: 5335
•\
~
Mart<
<]
C>
Previous
Next
r,
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
L .J
Fun Screen
1111
4
s
6
8
9
10
11
12
13
14
~
17
18
19
20
21
22
.~
25
26
27
•
28
©_
Zoom In
8_
Zoom Out
C
Reset
fl,
Add To Flash Card
29
•
30
31
ffiffij
Calculator
,
Reverse Color
~
~
Text Zoom
~
~
Settings
•
3
•
;'
rim
https://t.me/USMLEWorldStep3
-
[M
1
2
3
4
s
6
8
9
10
11
12
13
14
~
6
17
These lesions increase the risk for which of the following complications?
18
Q A. Basal cell carcinoma
19
20
0
0
0
0
21
22
•
~
4
25
•
C. Liver infiltration by lymphoma
0 . Malignant melanoma
E.
Squamous cell carcinoma
26
27
•
B. Gastric adenocarcinoma
Submit
28
29
•
30
31
•
https://t.me/USMLEWorldStep3
151 -
-
[M
1
2
3
4
s
6
8
9
10
11
12
13
14
~
6
17
These lesions increase the risk for which of the following complications?
18
19
A. Basal cell carcinoma (12%)
20
B. Gastric adenocarcinoma (2%)
21
C. Liver infiltration by lymphoma (1%)
22
•
~
0 . Malignant melanoma (6o/o)
4
E. Squamous cell carcinoma (76%)
25
•
26
27
•
Omitted
28
Correct answer
29
•
30
31
•
11 ..
L!!!.
76%
Answered correctly
IT\ 04 mins
\.::J Time Spent
https://t.me/USMLEWorldStep3
04/06/2020
• Last Updated
151 -
1
•
2
= .
-
ltem7 of39
Question Id: 5335
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
1111
;'
rim
ffiffij
Calculator
4
Actinic keratosis (AK) is a pre-malignant condition caused by excessive sunlight (ultraviolet [UV] light) exposure. AK n1ost commonly occurs in
s
sun-expo sed areas such as the face, scalp, ears, upper chest, and dorsal hands and forearms. AK lesions are characterized by small , rough,
6
erythematous, and keratotic papules that are often easier to feel than they are to see. These lesions occu r on skin that often shows sig ns of
chronic photodamage such as dyspigmentation, wrinkling, thinning, and telangiectasia.
8
AK is considered a premalignant condition that increases the risk of squamous eel I carcinoma (SCC). Estimates of risk vary widely, from <1 °/o to
9
as high as 20o/o. The majority of SCC of the skin arises in pre-existing AK. For this reason, any AK lesions that are detected should be removed
10
or destroyed. Individual lesions can be destroyed with liquid nitrogen cryosurgery or by su rgical excision or curettage. Field therapy (eg, 5-
11
fluorouracil cream, topical diclofenac, imiquimod) is recommended when numerous small lesions are present.
12
(Choice A) Basal cell carcinoma (BCC) is a common skin malignancy of low metastatic potential. The typical appearance is an enlarging fleshy
13
nodule w ith ulceration. BCC is also associated with sun exposure. Patients with a history of heavy UV light exposure may develop both AK and
14
BCC, but BCC does not arise from AK.
~
(Choice B) The Leser-Trelat sign is the acute onset of numerous seborrheic keratoses. The lesions are often pruritic and inflamed . The Leser-
6
Trelat sign is associated with many internal n1alignancies, most comn1only adenocarcinomas of the gastrointestinal tract.
17
18
(Choice C) Mycosis fungoides (cutaneous T-cell lymphon1a) has a highly variable appearance and may present as papulesor plaques, hyper-or
19
hypo-pign1ented patches, nonspecific erythema, or subcutaneous tumors. Extradermal spread of the malignancy may cause regional
20
lymphadenopathy, infiltration of the lung, liver, or spleen, and occasionally, there can be bone marrow and central nervous system involvement.
21
(Choice D) Malignant melanoma is associated with excessive UV exposure, especially in fair-skinned whites of non-Hispanic origin. Large
22
numbers of nevi and atypical nevi also correlate with the risk of melanoma, but AK does not predispose to melanoma.
~
Educational objective:
4
Actinic keratosis is a pre-malignant condition that develops in sun-damaged areas. Patients are at increased risk for squamous cell carcinon1a.
25
•
•
References
26
27
• Management of actinic keratosis.
28
• Actinic keratosis: review of the literature and new patents.
29
•
30
31
Reverse Color
~
~
Text Zoom
~
~
Settings
•
3
•
,
•
https://t.me/USMLEWorldStep3
1
•
2
=
ltem7of39
Question Id: 5335
.~Mart<
\
<]
C>
~~
G)
il
'!,·
Previous
Next
Fun Screen
Tutorial
Lab varues
Notes
4
s
6
8
9
10
11
12
13
14
~
6
17
18
19
20
21
22
~
4
25
•
26
27
•
©_
28
Zoom In
8_
Zoom Out
C
Reset
fl,
Add To Flash Card
29
•
30
31
Calculator
Reverse Color
~
@
Text Zoom
Settings
•
3
•
= ,
•
https://t.me/USMLEWorldStep3
1
•
2
=
ltem7of39
Question Id: 5335
.~Mart<
\
<]
C>
~~
G)
il
'!,·
Previous
Next
Fun Screen
Tutorial
Lab varues
Notes
4
s
6
8
9
10
11
12
13
14
~
6
17
18
19
20
21
22
~
4
25
•
26
27
•
©_
28
Zoom In
8_
Zoom Out
C
Reset
fl,
Add To Flash Card
29
•
30
31
Calculator
Reverse Color
~
@
Text Zoom
Settings
•
3
•
= ,
•
https://t.me/USMLEWorldStep3
1
2
•
= .
-
ltem7 of39
Question Id: 5335
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
1111
;'
rim
ffiffij
Calculator
4
A 65-year-old n,an comes to the physician due to multiple hand lesions. Scaly pink, white, and gray spots have been present on his hands for
s
several years but are slowly increasing in number and size. There is no history of contact skin allergies. The patient's past medical and family
6
history is unremarkable. He takes no medications. He is a retired police officer and spends most of his leisure time on a nearby beach. He does
not use tobacco, alcohol, or illicit drugs. On physical examination, he has numerous small papules and plaq ues on the dorsum of his hands with a
rough scale as shown below.
9
10
11
12
13
14
~
17
18
19
20
21
22
.~
25
•
26
27
•
28
29
•
30
31
Reverse Color
~
~
Text Zoom
~
~
Settings
•
3
8
,
https://t.me/USMLEWorldStep3
1
2
3
4
D. Malignant melanoma (6°/o)
s
6
,./ I
E. Squamous cell carcinoma (76%)
8
9
10
11
Omitted
Correct answer
E
111,
I.!.!.!..
76%
Answered correctty
IT\
\.::.J
04 mins
Time Spent
F=1 04/06/2020
El Last Updated
12
13
Explanation
14
~
6
•
erythematous, and keratotic papules that are often easier to feel than they are to see. These lesions occur on skin that often shows signs of
18
chronic photodamage such as dyspigmentation, wrinkling, thi nning, and telangiectasia.
19
AK is considered a premalignant condition that increases the risk of squamous eel I carcinoma ( SCC). Estimates of risk vary widely, from <1 °/o to
20
as high as 20o/o. The majority of SCC of the skin arises in pre-existing AK. For this reason, any AK lesions that are detected should be removed
21
or destroyed. Individual lesions can be destroyed with liquid nitrogen cryosurgery or by su rgical excision or curettage. Field therapy (eg, 5-
22
fluorouracil cream, topical diclofenac, imiquimod) is recommended when numerous small lesions are present.
~
4
(Choice A ) Basal cell carcinoma (BCC) is a common skin n1alignancy of low metastatic potential. The typical appearance is an enlarging fleshy
nodule w ith ulceration. BCC is also associated with sun exposure. Patients with a history of heavy UV light exposure may develop both AK and
sec, but sec does not arise from AK.
26
27
•
su n-exposed areas such as the face, scalp, ears, upper chest, and dorsal hands and forearms. AK lesions are characterized by small , rough,
17
25
•
Actinic keratosis (AK) is a pre-malignant condition caused by excessive sunlight (ultraviolet {UV] light) exposure. AK most commonly occurs in
28
(Choice B) The Leser-Trela! sign is the acute onset of numerous seborrheic keratoses. The lesions are often pruritic and inflamed . The Leser-
Trelat sign is associated with many internal n1alignancies, most commonly adenocarcinomas of the gastrointestinal tract.
29
•
30
31
https://t.me/USMLEWorldStep3
1
•
2
=
ltem7of39
Question Id: 5335
.~Mart<
\
<]
C>
~~
G)
il
'!,·
Previous
Next
Fun Screen
Tutorial
Lab varues
Notes
4
s
6
8
9
10
11
12
13
14
~
6
17
18
19
20
21
22
~
4
25
•
26
27
•
©_
28
Zoom In
8_
Zoom Out
C
Reset
fl,
Add To Flash Card
29
•
30
31
Calculator
Reverse Color
~
@
Text Zoom
Settings
•
3
•
= ,
•
https://t.me/USMLEWorldStep3
1
•
2
=
ltem7of39
Question Id: 5335
.~Mart<
\
<]
C>
~~
G)
il
'!,·
Previous
Next
Fun Screen
Tutorial
Lab varues
Notes
4
s
6
8
9
10
11
12
13
14
~
6
17
18
19
20
21
22
~
4
25
•
26
27
•
©_
28
Zoom In
8_
Zoom Out
C
Reset
fl,
Add To Flash Card
29
•
30
31
Calculator
Reverse Color
~
@
Text Zoom
Settings
•
3
•
= ,
•
https://t.me/USMLEWorldStep3
1
•
2
=
ltem7of39
Question Id: 5335
.~Mart<
\
<]
C>
~~
G)
il
'!,·
Previous
Next
Fun Screen
Tutorial
Lab varues
Notes
4
s
6
8
9
10
11
12
13
14
~
6
17
18
19
20
21
22
~
4
25
•
26
27
•
©_
28
Zoom In
8_
Zoom Out
C
Reset
fl,
Add To Flash Card
29
•
30
31
Calculator
Reverse Color
~
@
Text Zoom
Settings
•
3
•
= ,
•
https://t.me/USMLEWorldStep3
1
•
2
= .
-
ltem 8of39
Question Id: 9969
•\
~
Mart<
<]
C>
r,
Previous
Next
Fun Screen
L .J
•!
I'>\
\.!..)
Tutorial
1111
Lab Yallles
m; ',
Notes
rim
ffiffij
Calculator
3
4
A 60-year-old n,an has experienced progressive shortness of breath over the last 6 months that is occasionally accompanied by chest pain. He
s
was diagnosed with hypertension 10 years ago. Twenty years ago, he suffered from advanced-stage Hodgkin lymphon1a that w as treated with
6
combination chemotherapy and radiation therapy. He is a lifetime nonsmoker. Blood pressure is 138/90 mm Hg and pulse is 78/min and regular.
7
Physical examination shows a 2/4 early diastolic murmur at the left sternal border. Echocardiogram shows an enlarged left atrium, a normal-size
left ventricle with an ejection fraction of 60°/o, and moderate diastolic dysfunction. Both the mitral and aortic valves appear sclerotic and calcified.
The aortic root is normal-size but is echo bright. There is moderate aortic regurgitation. Cardiac catheterization shows ostial narrowing of the right
9
and left main coronary arteries. Which of the following is the most likely diagnosis?
10
11
12
13
14
~
6
17
18
Q
A. Anthracycline cardiotoxicity
0
0
0
0
B. Hypertensive heart disease
C. Radiation cardiotoxicity
0. Rheumatic heart disease
E. Secondary malignancy
19
20
Submit
21
22
•
~
4
25
•
26
27
•
28
29
•
30
31
•
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
Settings
~
~
1
•
2
= .
-
ltem 8of39
Question Id: 9969
•\
~
Mart<
<]
C>
r,
Previous
Next
Fun Screen
L .J
•!
I'>\
\.!..)
Tutorial
1111
Lab Yallles
m; ',
Notes
rim
ffiffij
Calculator
4
A 60-year-old n,an has experienced progressive shortness of breath over the last 6 months that is occasionally accompanied by chest pain. He
s
was diagnosed with hypertension 10 years ago. Twenty years ago, he suffered from advanced-stage Hodgkin lymphon1a that w as treated with
6
combination chemotherapy and radiation therapy. He is a lifetime nonsmoker. Blood pressure is 138/90 mm Hg and pulse is 78/min and regular.
7
Physical examination shows a 2/4 early diastolic murmur at the left sternal border. Echocardiog ram shows an enlarged left atrium, a normal-size
left ventricle with an ejection fraction of 60°/o, and moderate diastolic dysfunction. Both the mitral and aortic valves appear sclerotic and calcified.
The aortic root is normal-size but is echo bright. There is moderate aortic regurgitation. Cardiac catheterization shows ostial narrowing of the right
9
and left main coronary arteries. Which of the following is the most likely diagnosis?
10
11
A. Anthracycline cardiotoxicity (22%)
12
B. Hypertensive heart disease (8%)
13
14
C. Radiation cardiotoxicity (61%)
~
0. Rheumatic heart disease (5o/o)
6
17
E. Secondary malignancy ( 1% )
18
19
20
Omitted
21
22
Correct answer
C
~
Explanation
26
('j'\ 02 secs
'\.::) Time Spent
complications due to chemotherapy and/or radiation therapy. Radiation therapy causes diffuse fibrosis in the interstitium of the myocardium, along
28
with progressive fibrosis of the pericardia! layers, cells in the conduction system, and the cusps and/or leaflets of the valves. It also causes injury
29
•
03/06/2020
• Last Updated
This patient most likely has radiation-induced cardiotoxicity. Long-term survivors of Hodgkin lymphoma are at risk of developing cardiovascular
27
•
'"· 61
%
l!!!.
Answered
correctly
4
25
•
30
31
Reverse Color
~
~
Text Zoom
Settings
~
~
•
3
•
,
•
https://t.me/USMLEWorldStep3
1
•
2
= .
-
ltem 8of39
Question Id: 9969
•\
~
Mart<
<]
Previous
C>
Next
r,
L .J
Fun Screen
•!
m,
Lab Yallles
Notes
I'>\
\.!..)
Tutorial
11111
;'
rim
ffiffij
Calculator
3
This patient most likely has radiation-induced cardiotoxicity. Long-term survivors of Hodgkin lymphoma are at risk of developing cardiovascular
4
complications due to chemotherapy and/or radiation therapy. Radiation therapy causes diffuse fibrosis in the interstitiu m of the myocardiun1, along
s
with progressive fibrosis of the pericardia! layers, cells in the conduction system, and the cusps and/or leaflets of the valves. It also causes injury
6
to the intimal layer, with arterial narrowing typically involving the ostial parts of coronary vessels. These effects lead to:
7
1. Myocardial ischemia and/or infarction
2. Restrictive cardiomyopathy w ith diastolic dysfunction
9
3. Constrictive pericarditis
10
4. Valvular abnormalities (mitral or aortic stenosis/regurgitation)
11
5. Conduction defects (sick sinus syndrome or variable degrees of heart block)
12
13
(Choice A) The anthracycline class of drugs causes a dose-dependent decline in the ejection fraction, leading to dilated ca rdiomyopathy. It is
14
not associated with valvular disease or coronary artery disease.
~
(Choice B) Chronic severe hypertension can lead to left ventricular hypertrophy with diastolic dysfunction; however, it is not associated with
sclerosis/calcification of valves or ostial narrowing of the coronary arteries.
6
17
(Choice D) Rheumatic heart d isease causes progressive sclerosis of the mitral and/or aortic valve, causing mitral stenosis/regurgitation or aortic
18
stenosis/regurgitation. The additional associated findings - diastolic dysfunction, echogenic aortic root, and ostial narrowing of the coronary
19
arteries - are more consistent with radiation-induced cardiotoxicity.
20
(Choice E) Secondary malignancy (eg , breast, lung or gastrointestinal cancer; acute leukemia, non-Hodgkin lymphoma) is the leading cause of
21
death in survivors of Hodgkin lymphoma. There are no clinical findings suggesting a secondary malignancy in this patient.
22
•
•
~
Educational objective:
Clinical manifestations of radiation-induced cardiotoxicity include coronary disease with myocard ial ischemia and/or infarction, restrictive
4
25
cardiomyopathy with diastolic dysfunction, pericardia! disease, valvular abnormalities, and/or conduction defects.
26
References
27
•
• Cardiac complications of oncologic therapy.
28
• Clinically significant cardiac disease in patients with Hodgkin lymphoma treated with mediastinal irradiation.
29
•
30
31
•
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
Settings
~
~
•
1
•
2
= .
-
ltem 8of39
Question Id: 9969
3
•\
~
Mart<
<]
C>
r,
Previous
Next
Fun Screen
L .J
•!
I'>\
\.!..)
Tutorial
1111
Lab Yallles
m; ',
Notes
rim
ffiffij
Calculator
3. Constrictive pericarditis
s
4. Valvular abnormalities (mitral or aortic sten osis/regu rgitation)
6
5. Conduction defects (sick sinus syndrome or variable degrees of heart block)
7
(Choice A) The anthracycline class of drugs causes a dose-dependent decline in the ejection fraction, leading to dilated cardiomyopathy. It is
not associated with valvular disease or coronary artery disease.
9
10
(Choice B) Chronic severe hypertension can lead to left ventricular hypertrophy with diastol ic dysfunction; however, it is not associated with
11
sclerosis/calcification of valves or ostial narrowing of the coronary arteries.
12
(Choice D) Rheumatic heart disease causes progressive sclerosis of the mitral and/or aortic valve, causing mitral stenosis/regurgitation or aortic
13
stenosis/regurgitation. The additional associated findings - diastolic dysfunction, echogenic aortic root, and ostial narrowing of the coronary
14
arteries - are m ore consistent with radiation-induced cardiotoxicity.
~
(Choice E) Secondary malignancy (eg , breast, lung or gastrointesti nal cancer; acute leukemia, non-Hodgkin lymphoma) is the leading cause of
6
death in survivors of Hodgkin lymphoma. There are n o clinical findings suggesting a secondary m alignancy in this patient.
17
18
Educational objective:
19
Clinical manifestations of radiation-induced cardiotoxicity include coronary disease with myocardial ischemia and/or infarction, restrictive
20
cardiomyop athy with diastolic dysfunction, pericardia! disease, valvular abnormalities, and/or conduction defects.
21
References
22
•
• Cardiac complications of oncologic therapy.
~
• Clinically significant cardiac disease in patients with Hodgkin lymphoma treated with mediastinal irradiation.
4
25
•
26
27
•
Foundations of Independent Practice
Hen1atology & Oncology
Subject
System
opyng
28
I@ ..JWorla
Restrictive cardiomyopathy
Topic
Is
...
29
•
30
31
•
Reverse Color
~
~
Text Zoom
Settings
~
~
•
2. Restrictive cardiomyopathy w ith diastolic dysfunction
4
,
https://t.me/USMLEWorldStep3
1
•
2
= .
-
ltem9 of39
Question Id: 6122
•\
~
Mart<
<]
C>
r,
Previous
Next
Fun Screen
L .J
•!
I'>\
\.!..)
Tutorial
1111
Lab Yallles
m; ',
Notes
rim
ffiffij
Calculator
3
4
An 8-month-old boy with sickle cell disease is brought to an urgent care center by his parents following several hours of intermittent crying.
s
Yesterday afternoon, the patient had been active and crawling around, but he seemed irritable in the eveni ng and was awake most of the night.
6
Today, his parents noticed swelling of his hands and feet, which appear painful to the touch. The pain seems to be only minin1ally relieved with
7
over-the-counter acetaminophen and ibuprofen. The boy has been breastfeeding less than usual due to fussiness but has been voiding
8
appropriately. The patient has never been hospitalized. He takes oral penicillin prophylaxis and a vitamin D supplement. Immunizations,
including an annual influenza vaccination, are up to date. Temperature is 36.7 C (98 F), blood pressure is 90/60 mm Hg, pulse is 158/min, and
10
respirations are 32/n1in. Pulse oximetry is 98% on room air. Physical examination shows a fussy infant who can be consoled for short periods of
11
time but appears restless and grimaces occasionally during the examination . There is symmetric swelling of the hands and feet. There are no
12
rashes or skin abrasions. Lungs are clear to auscultation, and there are no retractions or use of accessory muscles. The abdomen is soft,
nontender, and nondistended; the spleen is not palpable. The remainder of the examination is normal. The last dose of ibuprofen was given 1
13
hour ago. Which of the following is the most appropriate next step in management of this patient?
14
~
Q
A. Apply cold compresses
0
0
0
0
B. Codeine
6
17
18
19
20
21
C. Hydroxyurea
0 . Oxycodone
E. Tramadol
22
•
~
Submit
4
25
•
26
27
•
28
29
•
30
31
•
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
Settings
~
~
1
•
2
= .
-
ltem9 of39
Question Id: 6122
•\
~
Mart<
<]
C>
r,
Previous
Next
Fun Screen
L .J
•!
I'>\
\.!..)
Tutorial
1111
Lab Yallles
m; ',
Notes
rim
ffiffij
Calculator
3
4
An 8-month-old boy with sickle cell disease is brought to an urgent care center by his parents following several hours of intermittent crying.
s
Yesterday afternoon, the patient had been active and crawling around, but he seemed irritable in the eveni ng and was awake most of the night.
6
Today, his parents noticed swelling of his hands and feet, which appear painful to the touch. The pain seems to be only minin1ally relieved with
7
over-the-counter acetaminophen and ibuprofen. The boy has been breastfeeding less than usual due to fussiness but has been voiding
8
appropriately. The patient has never been hospitalized. He takes oral penicillin prophylaxis and a vitamin D supplement. Immunizations,
including an annual influenza vaccination, are up to date. Temperature is 36.7 C (98 F), blood pressure is 90/60 mm Hg, pulse is 158/min, and
10
respirations are 32/n1in. Pulse oximetry is 98% on room air. Physical examination shows a fussy infant who can be consoled for short periods of
11
time but appears restless and grimaces occasionally during the examination . There is symmetric swelling of the hands and feet. There are no
12
rashes or skin abrasions. Lungs are clear to auscultation, and there are no retractions or use of accessory muscles. The abdomen is soft,
nontender, and nondistended; the spleen is not palpable. The remainder of the examination is normal. The last dose of ibuprofen was given 1
13
hour ago. Which of the following is the most appropriate next step in management of this patient?
14
~
Q
A. Apply cold compresses
0
0
0
0
B. Codeine
6
17
18
19
20
21
C. Hydroxyurea
0 . Oxycodone
E. Tramadol
22
•
~
Submit
4
25
•
26
27
•
28
29
•
30
31
•
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
Settings
~
~
1
•
2
= .
-
ltem9 of39
Question Id: 6122
•\
~
Mart<
<]
C>
r,
Previous
Next
Fun Screen
L .J
•!
I'>\
\.!..)
Tutorial
1111
Lab Yallles
m; ',
Notes
rim
ffiffij
Calculator
4
An 8-month-old boy with sickle cell disease is brought to an urgent care center by his parents following several hours of intermittent crying.
s
Yesterday afternoon, the patient had been active and crawling around, but he seemed irritable in the eveni ng and was awake most of the night.
6
Today, his parents noticed swelling of his hands and feet, which appear painful to the touch. The pain seems to be only minin1ally relieved with
7
over-the-counter acetaminophen and ibuprofen. The boy has been breastfeeding less than usual due to fussiness but has been voiding
8
appropriately. The patient has never been hospitalized. He takes oral penicillin prophylaxis and a vitamin D supplement. Immunizations,
including an annual influenza vaccination, are up to date. Temperature is 36.7 C (98 F), blood pressure is 90/60 mm Hg, pulse is 158/min, and
10
respirations are 32/n1in. Pulse oximetry is 98% on room air. Physical examination shows a fussy infant who can be consoled for short periods of
11
time but appears restless and grimaces occasionally during the examination. There is symmetric swelling of the hands and feet. There are no
12
rashes or skin abrasions. Lungs are clear to auscultation, and there are no retractions or use of accessory muscles. The abdomen is soft,
nontender, and nondistended; the spleen is not palpable. The remainder of the examination is normal. The last dose of ibuprofen was given 1
13
hour ago. W hich of the following is the most appropriate next step in management of this patient?
14
~
A. Apply cold compresses (10%)
6
17
B. Codeine (9%)
18
C. Hydroxyurea (38°/o)
19
0 . Oxycodone (33o/o)
20
E. Tramadol (7°A.)
21
22
•
~
4
Omitted
25
Correct answer
26
D
'"· 33%
l!!!.
Answered correcUy
(i\ 41 secs
\.::J Time Spent
¢:::!:i 07/03/2020
13 Last Updated
27
•
28
Explanation
29
•
30
31
Reverse Color
~
~
Text Zoom
Settings
~
~
•
3
•
,
•
https://t.me/USMLEWorldStep3
1
2
•
= .
-
ltem9 of39
Question Id: 6122
•\
~
<]
Mart<
Previous
C>
Next
r,
L .J
Fun Screen
•!
m,
Lab Yallles
Notes
I'>\
\.!..)
Tutorial
11111
;'
rim
ffiffij
Calculator
4
Vaso-occlusive pain episode
s
• Acute, severe pain
6
Cli nical features
8
• Pai n at >1 site (eg, dactylitis)
• ± Low-grade fever
• May be triggered (eg , by dehydration)
10
11
• Analgesics (NSAIDs, opiates)
Management
12
13
14
~
6
•
This patient with symmetric swelling and pain of the hands and feet in the setting of known sickle cell disease (SCD) has dactylitis (hand-foot
syndrome). Dactylitis, resulting from vaso-occlusion of the blood vessels supplying the metacarpals and metatarsals, may be the earliest
18
temperature changes, and dehydration. Low-grade fever may also be present in addition to pain. Initial radiographs reveal only soft-tissue
19
swelling; recurrent episodes can lead to a mottled appearance of the bones. Although most cl1ildren with SCD are diagnosed by hemoglobin
20
electrophoresis on newborn screening, the presence of dactylitis in a previously healthy child should prompt evaluation for SCD.
21
Treatment of dactylitis involves pain control, hydration, and application of heat. Oral nonsteroidal anti-inflammatory drugs (NSA1Ds) and oral
22
opioids are typically initiated for mild to moderate pain. Because this patient still appears uncomfortable after treatment with NSAIDs, a short-
4
acting oral opioid (eg, oxycodone) should be given. If the pain fails to improve, intravenous opioids are indicated.
(Choice A ) Cold compresses are not recommended as they can trigger local intravascular sickling and worsen vase-occlusive pain episodes. In
contrast, heat packs help by promoting vasodilation.
26
27
•
NSAID = nonsteroidal anti-inflammatory drug; RBC = red blood cell.
n1anifestation of SCD in young chi ldren (ages 6 months to 4 years). Similar to other vase-occlusive episodes, triggers include stress, illness,
25
•
• Hydration
• ± RBC transfusion
17
~
28
(Choices Band E) Oral codeine and tramadol are contraindicated in children age <12 because ultra-rapid metabolism of codeine and tramadol
causes an unpredictably high concentration of the active drug in the body, which can result in respiratory depression and death.
29
•
30
31
Reverse Color
~
~
Text Zoom
Settings
~
~
•
3
7
,
https://t.me/USMLEWorldStep3
1
2
•
= .
-
ltem9 of39
Question Id: 6122
•\
~
<]
Mart<
Previous
C>
Next
r,
L .J
Fun Screen
•!
m,
Lab Yallles
Notes
I'>\
\.!..)
Tutorial
11111
;'
rim
ffiffij
Calculator
4
Vaso-occlusive pain episode
s
• Acute, severe pain
6
Cli nical features
8
• Pai n at >1 site (eg, dactylitis)
• ± Low-grade fever
• May be triggered (eg , by dehydration)
10
11
• Analgesics (NSAIDs, opiates)
Management
12
13
14
~
6
•
This patient with symmetric swelling and pain of the hands and feet in the setting of known sickle cell disease (SCD) has dactylitis (hand-foot
syndrome). Dactylitis, resulting from vaso-occlusion of the blood vessels supplying the metacarpals and metatarsals, may be the earliest
18
temperature changes, and dehydration. Low-grade fever may also be present in addition to pain. Initial radiographs reveal only soft-tissue
19
swelling; recurrent episodes can lead to a mottled appearance of the bones. Although most cl1ildren with SCD are diagnosed by hemoglobin
20
electrophoresis on newborn screening, the presence of dactylitis in a previously healthy child should prompt evaluation for SCD.
21
Treatment of dactylitis involves pain control, hydration, and application of heat. Oral nonsteroidal anti-inflammatory drugs (NSA1Ds) and oral
22
opioids are typically initiated for mild to moderate pain. Because this patient still appears uncomfortable after treatment with NSAIDs, a short-
4
acting oral opioid (eg, oxycodone) should be given. If the pain fails to improve, intravenous opioids are indicated.
(Choice A ) Cold compresses are not recommended as they can trigger local intravascular sickling and worsen vase-occlusive pain episodes. In
contrast, heat packs help by promoting vasodilation.
26
27
•
NSAID = nonsteroidal anti-inflammatory drug; RBC = red blood cell.
n1anifestation of SCD in young chi ldren (ages 6 months to 4 years). Similar to other vase-occlusive episodes, triggers include stress, illness,
25
•
• Hydration
• ± RBC transfusion
17
~
28
(Choices Band E) Oral codeine and tramadol are contraindicated in children age <12 because ultra-rapid metabolism of codeine and tramadol
causes an unpredictably high concentration of the active drug in the body, which can result in respiratory depression and death.
29
•
30
31
Reverse Color
~
~
Text Zoom
Settings
~
~
•
3
7
,
https://t.me/USMLEWorldStep3
1
•
2
= .
-
ltem9 of39
Question Id: 6122
3
•\
~
Mart<
<]
C>
r,
Previous
Next
Fun Screen
L .J
•!
I'>\
\.!..)
Tutorial
1111
Lab Yallles
m; ',
Notes
rim
ffiffij
Calculator
This patient with symmetric sw elling and pain of the hands and feet in the setting of known s ickle cell disease (SCD) has dactylit is (hand-foot
4
syndrome). Dactylitis, resulting from vaso-occlusion of the blood vessels supplying the metacarpals and metatarsals, may be the earliest
s
manifestation of SCD in young ch il dren (ages 6 months to 4 years). Similar to other vaso-occlusive episodes, triggers include stress, illness,
6
temperature changes, and dehydration. Low-grade fever may also be present in addition to pain. Initial radiographs reveal only soft-tissue
7
swelling; recurrent episodes can lead to a mottled appearance of the bones. Although most children with SCD are diagnosed by hemoglobin
8
electrophoresis on newborn screening, the presence of dactylitis in a previously healthy child should prompt evaluation for SCD.
Treatment of dactylitis involves pain control, hydration, and application of heat. Oral nonstero idal anti-inflammatory drugs (NSAIDs) and oral
10
opioids are typically init iated for mild to moderate pain. Because this patient still appears uncomfortable after treatment with NSAIDs, a short-
11
acting oral opioid (eg, oxycodone) should be given. If the pain fails to improve, intravenous opioids are indicated.
12
13
(Choice A ) Cold compresses are not recommended as they can trigger local intravascular sickling and worsen vaso-occlusive pain episodes. In
14
contrast, heat packs help by promoting vasodilation.
~
(Choices Band E) Oral codeine and tramadol are contraindicated in children age <12 because ultra-rapid metabolism of codeine and tramadol
6
causes an unpredictably high concentration of the active drug in the body, which can result in respiratory depression and death.
17
(Choice C) Hydroxyurea reduces the frequency of vaso-occlusive episodes in patients with SCD but n1ay take several months to take effect. It is
18
not used in the treatn1ent of an acute vaso-occlusive episode.
19
•
20
Educational objective :
21
Dactylitis presents in young children with sickle cell disease as symmetric swelling and pain of the hands and feet. Treatn1ent includes pain
22
control (eg , nonsteroidal anti-inflammatory drugs, oral opioids), hydration, and appl ication of heat.
~
References
4
• Sickle cell disease.
25
•
• Current management of sickle cell anemia.
26
27
•
28
Foundations of Independent Practice
Hematology & Oncology
Sickle cell
Subject
System
Topic
29
•
30
31
•
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
Settings
~
~
•
1
•
2
= .
-
Item 10of 39
Question Id: 5699
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
Lab Yallles
m,
;'
Notes
rim
ffiffij
Calculator
3
4
A 28-year-old Caucasian woman presents to the primary care physician complaining of a painless blistering on the backs of her hands. The
s
blisters appeared one w eek ago after she spent some time gardening outdoors, and are accompanied by an increased fragility of the surrounding
6
skin. The woman states that she has never before had such symptoms, though she suspects her mother may occasionally have had a similar
7
presentation that eventually resolved without treatment. Past medical history is significant for chronic infection with Hepatitis C virus. Current
8
medications include oral contraceptives, which were begun last month. Physical examination also reveals mild hyperpigmentation of the face.
9
What is the most likely diagnosis?
11
Q
A. Allergic contact dermatitis
12
0
0
0
0
B.
13
14
~
6
17
Porphyria cutanea tarda
C. Herpes zoster
D. Dermatitis herpetiformis
E. Impetigo
18
19
Submit
20
21
22
•
~
4
25
•
26
27
•
28
29
•
30
31
•
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
1
•
2
= .
-
•\
~
Item 10of 39
Question Id: 5699
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
rim
Tutorial
Lab Yallles
Notes
Calculator
\.!..)
1111
;'
,
ffiffij
Reverse Color
~
~
Text Zoom
~
~
Settings
•
3
4
A 28-year-old Caucasian woman presents to the primary care physician complaining of a painless blistering on the backs of her hands. The
s
blisters appeared one w eek ago after she spent some time gardening outdoors, and are accompanied by an increased fragility of the surrounding
6
skin. The woman states that she has never before had such symptoms, though she suspects her mother may occasionally have had a similar
7
presentation that eventually resolved without treatment. Past medical history is significant for chronic infection with Hepatitis C virus. Current
8
medications include oral contraceptives, which were begun last month. Physical examination also reveals mild hyperpigmentation of the face.
9
What is the most likely diagnosis?
A. Allergic contact dermatitis ( 12°/o)
11
12
B. Porphyria cutanea tarda (69%)
13
C. Herpes zoster (0°/o)
14
~
D. Dermatitis herpetiformis (15%)
6
E. Impetigo (1°/o)
17
18
19
20
Omitted
21
Correct answer
B
22
•
Ii.. 69%
I.ill.. Answered correctly
~
4
ri', 02 secs
\..::J
Time Spent
~
04/05/2020
13 Last Updated
Explanation
25
•
26
Porphyria cutanea tarda (Choice B) is a condition that arises from the deficiency of uroporphyrinogen decarboxylase, an enzyme in the heme
27
•
•
synthesis pathway. This condition is characterized by painless blisters, an increased fragility of the skin on the dorsal surfaces of the hands, and
28
facial hypertrichosis and hyperpigmentation. It can be triggered by the ingestion of certain substances (e.g., ethanol , estrogens) that should be
29
.
30
31
•
TUTOR
-· ...
·-
. ...
.. ··--
.
-- ··- ·- .. ---··. ··-··-·· - ··- ··-https://t.me/USMLEWorldStep3
·-··
·-
--
~
F2ck
SgJ2,d
Engock
1
•
2
= .
-
Item 10of 39
Question Id: 5699
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
1111
;'
rim
ffiffij
Calculator
3
Explanation
4
s
6
Porphyria cutanea tarda (Choice B) is a condition that arises from the deficiency of uroporphyrinogen decarboxylase, an enzyme in the heme
7
synthesis pathway. This condition is characterized by painless blisters, an increased fragility of the skin on the dorsal surfaces of the hands, and
8
facial hypertrichosis and hyperpigmentation. It can be triggered by the ingestion of certain substances (e.g., ethanol, estrogens) that should be
discontinued if suspect. Diagnosis is confirmed with an elevation of the urinary uroporphyrins. Phlebotomy or hydroxychloroquine may provide
9
relief, as can interferon alpha in those patients simultaneously infected with Hepatitis C virus.
11
Allergic contact dermatitis (Choi ce A) results from direct skin contact with chemicals or allergens. It is characterized by pruritus, erythen1a, and
12
edema, often followed by the development of vesicles and bullae in the irritated region.
13
Herpes zoster (Choice C) is characterized by painful vesicular lesions clustered unilaterally along the course of a nerve. The lesions are typically
14
~
found on the face or trunk, and will be Tzancl< smear positive.
6
Dermatitis herpetiformis (Choi ce D) is characterized by pruritic papules and vesicles that appear n1ainly on the elbows, knees, buttocks, posterior
17
neck, and scalp. The condition arises in the context of gluten-sensitive enteropathy, which may be subclinical.
18
Impetigo (Choice E) is characterized by pruritic and honey-colored macules, vesicles, and bullae on the face and other exposed parts. The
19
condition is caused by Staphylococcus aureus or group A streptococcus.
20
Educational Obj ective:
21
Porphyria cutanea tarda is a condition characterized by painless blisters, hypertrichosis, and hyperpigmentation. It is often associated with
Hepatitis C infection and can be triggered by the ingestion of certain substances (e.g., ethanol, estrogens), which should be discontinued if
22
•
~
suspect.
4
25
•
26
27
•
Foundations of Independent Practice
Dermatology
Porphyria cutanea tarda
Subject
System
Topic
28
29
•
30
31
•
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
[M
1
•
2
= .
-
Item 11 of 39
Question Id: 6281
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
Lab Yallles
m,
rim
Notes
Calculator
;'
ffiffij
3
4
A 15-month-old boy is brought to the clinic due to fatigue. His father states that the patient used to nap for 2 hours in the afternoon but for the last
s
2 weeks has taken a 2-hou r nap in the morning as well. The child is a picky eater and drinks 960 ml (32 oz) of cow's milk each day. He takes no
6
daily medications, and his immunizations are up to date. Physical examination reveals a tired-appearing boy. Conjunctivae are pale and
7
anicteric. Cardiac examination reveals normal heart tones. The abdomen is soft with no hepatomegaly. Capillary refill is <2 seconds; nail beds
8
have pallor. Hemoglobin is 8.1 g/dl , and a capillary lead level is undetectable. A presumptive diag nosis of iron deficiency anemia is made. The
9
boy is prescribed ferrous sulfate, which he takes with orange juice between meals. His cow's milk intake is restricted to 480 ml (1 6 oz) per day.
Which of the following changes is expected to occur first in response to treatment?
10
Q
Q
Q
Q
Q
12
13
14
~
6
17
A. Increase in ferritin levels
8 . Increase in hen1atocrit
C. Increase in hemoglobin
D. Increase in mean corpuscular volume to red blood cell count ratio
E. Increase in reticulocyte count
18
19
20
Submit
21
22
•
~
4
25
•
26
27
•
28
29
•
30
31
•
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
[M
1
•
2
= .
-
Item 11 of 39
Question Id: 6281
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
1111
;'
rim
ffiffij
Calculator
3
4
A 15-month-old boy is brought to the clinic due to fatigue. His father states that the patient used to nap for 2 hours in the afternoon but for the last
s
2 weeks has taken a 2-hou r nap in the morning as well. The child is a picky eater and drinks 960 ml (32 oz) of cow's milk each day. He takes no
6
daily medications, and his immunizations are up to date. Physical examination reveals a tired-appearing boy. Conjunctivae are pale and
7
anicteric. Cardiac examination reveals normal heart tones. The abdomen is soft with no hepatomegaly. Capillary refill is <2 seconds; nail beds
8
have pallor. Hemoglobin is 8.1 g/dl , and a capillary lead level is undetectable. A presumptive diag nosis of iron deficiency anemia is made. The
9
boy is prescribed ferrous sulfate, which he takes with orange juice between meals. His cow's milk intake is restricted to 480 ml (1 6 oz) per day.
Which of the following changes is expected to occur first in response to treatment?
10
A. Increase in ferritin levels (21 °/o)
12
8 . Increase in hen1atocrit (2o/o)
13
14
C. Increase in hemoglobin (5%)
~
0. Increase in mean corpuscular volume to red blood cell count ratio (1 3%)
6
17
E. Increase in reticulocyte count (57%)
18
19
20
Omitted
21
Correct answer
22
•
E
~
Explanation
26
27
•
Iron deficiency anemia in young children
28
• Prematurity
29
•
'\.::) Time Spent
4
25
•
('j'\ 02 secs
'"· 57%
l!!!.
Answered correctly
30
31
•
https://t.me/USMLEWorldStep3
06/29/2020
• Last Updated
,
Reverse Color
~
~
Text Zoom
~
~
Settings
[M
1
•
2
= .
-
Item 11 of 39
Question Id: 6281
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
•!
m,
Lab Yallles
Notes
I'>\
\.!..)
Tutorial
11111
;'
rim
ffiffij
Calculator
3
Iron deficiency anemia in young children
4
s
, Prematurity
6
• Lead exposure
7
, Age <1
8
o
9
Risk factors
10
Delayed introduction of solids
(ie, exclusive breastfeeding after 6 months)
o
Cow's, soy, or goat's milk
• Age >1
12
o
13
o <3 servings/day iron-rich foods
14
~
Diagnosis
>24 oziday cow's milk
• Screening hemoglobin at age 1
• Hemoglobin <11 g/dL, ! MCV,
t RDW
6
Treatment
17
18
• Empiric trial of iron supplementation
MCV = mean corpuscular volume; ROW = red blood cell distribution width .
19
Iron deficiency is the most common nutritional deficiency in children and should be suspected in any child drinking >24 oz of cow's milk per day.
20
Fatigue and pallor may occu r, but patients are often asymptomatic and detected on universal screen around age 1. Given the high prevalence of
21
iron deficiency anemia in infants and toddlers, a presumptive diagnosis of iron deficiency is made when hemogl obi n <1 1 g/dL. Lead level should
22
•
also be measured, but additional studies are usually not needed in the initial workup. An empiric trial of ferrous sulfate is considered the most
~
cost-effective treatment, and the doses should be given with juice between meals as vitamin C facilitates iron absorption . Patients should also be
4
advised to limit milk intake to <20 oz per day and to increase intake of iron-rich foods (eg, meats, fortified cereals).
25
•
•
26
Patients w ith iron deficiency have hypochromic, microcytic red blood cells (RBCs) and decreased reticulocytes as the bone marrow is unable to
27
produce the requisite number of RBCs without adequate iron substrate. Within 1-2 weeks of initiating supplementation, the reticulocyte count
28
increases quickly. However, in patients with moderate to severe iron deficiency, it usually takes about a month for the hen1atocrit and hemoglobin
to increase and a few months to return to regular levels {Choi ces 6 and C). Therefore, after a month of empiric iron supplementation, an
29
•
30
31
•
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
[M
1
•
2
= .
-
Item 11 of 39
Question Id: 6281
•\
~
Mart<
<]
C>
Previous
Next
I'>\
•!
m,
rim
Tutorial
Lab Yallles
Notes
Calculator
r,
L .J
Fun Screen
\.!..)
1111
;'
ffiffij
3
Iron deficiency is the most common nutritional deficiency in children and should be suspected in any child drinking >24 oz of cows milk per day.
4
Fatigue and pallor may occur, but patients are often asymptomatic and detected on universal screen around age 1. Given the high prevalence of
s
iron deficiency anemia in infants and toddlers, a presumptive diagnosis of iron deficiency is made when hemogl obin <1 1 g/dL. Lead level should
6
also be measured, but additional studies are usually not needed in the initial workup. An empiric trial of ferrous sulfate is considered the most
7
cost-effective treatment, and the doses should be given with juice between meals as vitamin C facilitates iron absorption . Patients should also be
8
advised to limit milk intake to <20 oz per day and to increase intake of iron-rich foods (eg, meats, fortified cereals).
9
Patients w ith iron deficiency have hypochromic, microcytic red blood cells (RBCs) and decreased reticulocytes as the bone marrow is unable to
10
produce the requisite number of RBCs without adequate iron substrate. Within 1-2 weeks of initiating supplementation, the reticu locyte count
increases quickly. However, in patients with moderate to severe iron deficiency, it usually takes about a month for the hematocrit and hemoglobin
12
to increase and a few months to return to regular levels (Choi ces 6 and C). Therefore, after a n1onth of empiric iron supplementation, an
13
increase in hemoglobin <!1 g/dl supports the diagnosis of iron deficiency anemia. Ferrous sulfate should be maintained for 2-3 months after
14
hemoglobin normalization to replenish iron stores.
~
(Choice A) Ferritin reflects iron stores and does not begin to rise until after hemoglobin normalizes.
17
(Choice D) The Mentzer index refers to the ratio of mean corpuscular volume (MCV) to total RBC count. Before treatment, patients with iron
18
deficiency anemia generally have low MCV and total RBC counts with a high Mentzer index of >13.
19
Educational objective :
20
Children with presumed iron deficiency anemia due to poor diet are treated with an empiric trial of iron supplementation. Iron therapy increases
21
reticulocyte production followed by an increase in hematocrit and hemoglobin in approximately 1 month.
6
22
•
References
~
• Diagnosis and prevention of iron deficiency and iron-deficiency anemia in infants and young children (0-3 years of age).
4
• Evaluation of anemia in children.
25
•
•
26
27
Foundations of Independent Practice
Hematology & Oncology
Iron deficiency anemia
28
Subject
System
Topic
29
•
30
31
•
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
[M
1
•
2
= .
-
Item 12of 39
Question Id: 13226
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
Lab Yallles
m,
rim
Notes
Calculator
;'
,
ffiffij
Reverse Color
~
~
Text Zoom
~
~
Settings
3
4
A 5-year-old boy is brought to an urgent care center due to fatigue. His mother says, "Normally, my son is running and jumping, but for the past
s
week he has been resting on the couch and sleeping more than usual. His eyes also look a bit yellow." He has had no fevers, vomiting, or
6
d ifficulty breathing. A week ago, the patient had a skin infection that resolved after treatment with oral antibiotics. Review of medical records
7
shows a normal hemoglobi n screening at his 1-year well-child visit. Family history is significant for a maternal uncle who had several similar
8
episodes of tiredness and jaundice. Physical examination reveals a tired-appearing boy lying on the examination table watching television. His
9
neck is supple without lymphadenopathy, and scleral icterus and mild jaundice are present. His cardiac and abdominal examinations are normal.
Laboratory results are as follow s:
10
11
Complete blood count
13
Hemoglobin
7.2 g/dL
14
Mean corpuscular volume
82 µm3
Reticulocytes
7%
17
Platelets
260,000/mm3
18
Leukocytes
8,200/mm 3
~
6
19
20
Liver function studies
21
22
•
~
8.3 mg/dL
Direct bilirubin
0.7 mg/dL
4
Hematology
25
•
Total bilirubin
26
Haptoglobin, serum
12 mg/dL (normal: 30-200)
Direct antiglobulin (Coombs) test
negative
27
•
28
·- ·· - ......... -
29
•
30
31
•
TUTOR
.. ·- .. - ........
-
....
.. .
-
.. - ...... -.
- . . .. - ........
https://t.me/USMLEWorldStep3
~- ...
·- ..... ·-
~
F2ck
SgJ2,d Eng ock
[M
1
•
2
= .
-
Item 12of 39
Question Id: 13226
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
Lab Yallles
m,
rim
Notes
Calculator
;'
ffiffij
3
4
Platelets
260,000/mn,3
s
Leukocytes
8,200/mm3
6
7
Liver function studies
8
9
10
Total bilirubin
8.3 mg/dl
Direct bilirubin
0.7 mg/dl
11
Hematology
13
Haptoglobin, serum
12 mg/dl (normal: 30-200)
Direct antiglobulin (Coombs) test
negative
14
~
6
Peripheral blood smear is notable for red blood cell fragments and intracellular deposits of denatured hemoglobin. Which of the following is the
next best step in the diagnostic workup for this patient?
17
18
Q
Q
Q
Q
Q
19
20
21
22
•
~
4
25
•
B. Cold agglutinin titer
C. Glucose-6-phosphate dehydrogenase assay
D. Hemoglobin electrophoresis
E. Osmotic fragility testing
26
27
•
A. Bone n1arrow biopsy
Submit
28
29
•
30
31
•
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
[M
1
•
2
= .
-
Item 12of 39
Question Id: 13226
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
Lab Yallles
m,
rim
Notes
Calculator
;'
ffiffij
3
4
Platelets
260,000/mn,3
s
Leukocytes
8,200/mm3
6
7
Liver function studies
8
9
10
Total bilirubin
8.3 mg/dl
Direct bilirubin
0.7 mg/dl
11
Hematology
13
Haptoglobin, serum
12 mg/dl (normal: 30-200)
Direct antiglobulin (Coombs) test
negative
14
~
6
Peripheral blood smear is notable for red blood cell fragments and intracellular deposits of denatured hemoglobin. Which of the following is the
next best step in the diagnostic workup for this patient?
17
18
Q
Q
Q
Q
Q
19
20
21
22
•
~
4
25
•
B. Cold agglutinin titer
C. Glucose-6-phosphate dehydrogenase assay
D. Hemoglobin electrophoresis
E. Osmotic fragility testing
26
27
•
A. Bone n1arrow biopsy
Submit
28
29
•
30
31
•
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
[M
1
•
2
= .
-
Item 12of 39
Question Id: 13226
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
Lab Yallles
m,
rim
Notes
Calculator
;'
ffiffij
3
4
Platelets
260,000/mn,3
s
Leukocytes
8,200/mm3
6
7
Liver function studies
8
9
10
Total bilirubin
8.3 mg/dl
Direct bilirubin
0.7 mg/dl
11
Hematology
13
Haptoglobin, serum
12 mg/dl (normal: 30-200)
Direct antiglobulin (Coombs) test
negative
14
~
6
Peripheral blood smear is notable for red blood cell fragments and intracellular deposits of denatured hemoglobin. Which of the following is the
next best step in the diagnostic workup for this patient?
17
18
Q
Q
Q
Q
Q
19
20
21
22
•
~
4
25
•
B. Cold agglutinin titer
C. Glucose-6-phosphate dehydrogenase assay
D. Hemoglobin electrophoresis
E. Osmotic fragility testing
26
27
•
A. Bone n1arrow biopsy
Submit
28
29
•
30
31
•
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
[M
1
•
2
= .
-
Item 12of 39
Question Id: 13226
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
Lab Yallles
m,
rim
Notes
Calculator
;'
,
ffiffij
Reverse Color
~
~
~
~
Text Zoom
Settings
SgJ2,d
Eng ock
3
4
Platelets
260,000/mn,3
s
Leukocytes
8,200/mm3
6
7
Liver function studies
8
9
10
Total bilirubin
8.3 mg/dl
Direct bilirubin
0.7 mg/dl
11
Hematology
13
Haptoglobin, serum
12 mg/dl (normal: 30-200)
Direct antiglobulin (Coombs) test
negative
14
~
6
Peripheral blood smear is notable for red blood cell fragments and intracellular deposits of denatured hemoglobin. Which of the following is the
next best step in the diagnostic workup for this patient?
17
18
19
A. Bone n1arrow biopsy (0%)
20
B. Cold agglutinin titer (4°A.)
21
C. Glucose-6-phosphate dehydrogenase assay (78%)
22
•
~
D. Hemoglobin electrophoresis (5%)
4
E. Osmotic fragility testing (10%)
25
•
26
27
•
Omitted
28
Correct answer
-
29
•
30
31
•
TUTOR
11 ..
L!!!.
78%
Answered correctly
IT\
\.::J
06 mins, 13 secs
Time Spent
https://t.me/USMLEWorldStep3
04/1 0/2020
• Last Updated
~
F2ck
[M
1
•
2
= .
-
Item 12of 39
Question Id: 13226
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
rim
Tutorial
Lab Yallles
Notes
Calculator
\.!..)
1111
;'
ffiffij
3
4
Glucose-6-phosphate deficiency
s
6
Epidemiology
7
• X -linked
• Asian, African, or Middle Eastern descent
8
• Neonatal unconjugated hyperbilirubinemia
9
o Jaundice & anemia day of life 2-3
10
Manifestations
11
• Acute h emolytic episode
o Secondary to oxidative stress (eg, fava beans, sulfa drugs)
o Jaundice, pallor, dark urine, abdominal/back pain
13
• Hemolytic anemia
14
Laboratory findings
~
• Low gl ucose-6-phosphate deficiency assay (may be normal during attack)
6
17
Glucose-6-phosphate dehydrogenase (G6PD) deficiency is an X-linked disorder most con1mon in p atients of Asian, African, or Middle Eastern
18
descent. G6PD normally protects the red blood cells (RBCs) from oxidative stress by producing NADPH, an important cofactor in the pathway of
19
oxidant inactivation. Deficiency of G6PO leads to intra- and extravascular hemolysis triggered by oxidative stress, such as infection, sulfa
20
drugs, or fava beans. In this patient, the recent oral antibiotic was most likely trimethoprim-sulfaniethoxazole, a sulfa drug.
21
Clinical manifestations include j aundice and fatigue. Laboratory evidence of hemolysis ind udes anemia (normocytic, normochromic}, indi rect
22
•
hyperbilirubinemia, low haptoglobin, and elevated lactate dehydrogenase. Peripheral smear show s characteristic bite cells and schistocytes (RBC
~
frag ments); Heinz bodies (accumulations of denatured hem oglobin) may b e seen with special staining.
4
A low G6PD assay. which detects NAOPH formation , is diagnostic. This assay can be falsely negative if measured while the most severely
25
•
G6PO-deficient RBCs are already hemolyzed ; therefore, if the initial result is negative but there i s strong suspicion for G6PO, the assay should b e
26
repeated after the acute episode. The acute h emolytic anemia typically self-resolves in 1-2 weeks a fter removal of the offending oxidant. Patients
27
•
should be counseled on how to avoid common triggers.
28
(Choice A) Bone marrow biopsy is indicated for suspicion of bone n1arrow suppression or failure, which typically presen ts with multiple
29
•
• Bite cells with Heinz bodies on peripheral smear
30
31
•
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
[M
1
•
2
= .
-
Item 12of 39
Question Id: 13226
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
rim
Tutorial
Lab Yallles
Notes
Calculator
\.!..)
1111
;'
,
ffiffij
3
Clinical manifestations include j aundice and fatigue. Laboratory evidence of hemolysis includes anemia (normocytic, normochromic), indi rect
4
hyperbilirubinemia, low haptoglobin, and elevated lactate dehydrogenase. Peripheral smear show s characteristic bite cells and schistocytes (RBC
s
frag ments); Hei nz bodies (accumulations of denatured hemoglobin) may be seen with special staining.
6
Reverse Color
~
~
~
~
Text Zoom
Settings
SgJ2,d
Eng ock
A low G6PD assay, which detects NADPH formation, is diagnostic. This assay can be falsely negative if measured while the most severely
7
G6PD-deficient RBCs are already hen1olyzed ; therefore, if the initial result is negative but there is strong suspicion for G6PD, the assay should be
8
repeated after the acute episode. The acute hemolytic anemia typically self-resolves in 1-2 weeks after removal of the offending oxidant. Patients
9
should be counseled on how to avoid common triggers.
10
(Choice A) Bone marrow biopsy is indicated for suspicion of bone marrow suppression or failure, which typically presents with multiple
11
cytopenias (eg, thrombocytopenia, leukopenia) and a low reticulocyte count. In contrast, this patient has isolated anemia and a compensatory
reticulocytosis.
13
(Choice B) Cold agglutini n titer is elevated in cold agglutini n-mediated autoimmune hemolytic anemia, which can also present with fatigue and
14
~
anemia. However, symptoms typically develop after a viral infection, and a direct antiglobulin test would be positive.
6
(Choice D) Hemoglobin electrophoresis detects hemoglobinopathies such as thalassemia and sickle cell disease. Anemia in thalassemia is
17
microcytic, and patients with sickle cell anemia typically have pain crises starting in infancy and sickled RBCs on peripheral smear. This patient
18
has a nomiocytic anemia with a characteristic peripheral smear of G6PD deficiency.
19
(Choice E) Osmotic fragility testing is abnormal in hereditary spherocytosis, a genetic hemolytic anemia with spherocytes on peripheral smear
20
and splenomegaly on examination, neither of which is seen in this patient.
21
Educational objective :
22
•
~
Glucose-6-phosphate dehydrogenase (G6PD) deficiency is an X-linked disorder in which acute hemolytic anemia is triggered by oxidative stress
(eg , sulfa drug). Presentation includes jaundice and fatigue, and a G6PD assay is diagnostic.
4
25
•
References
• Congenital hemolytic anemia.
26
27
•
28
Foundations of Independent Practice
29
•
•
30
31
•
TUTOR
•
Hematology & Oncology
•
H
G6PD deficiency
a I
https://t.me/USMLEWorldStep3
~
F2ck
1
2
3
4
s
G6PD deficiency anemia
6
7
8
9
10
11
13
14
~
Bite cell
6
17
18
19
20
21
22
•
~
4
25
•
26
27
•
©_
28
Zoom In
8_
Zoom Out
C
Reset
fl,
Add To Flash Card
29
•
30
31
•
https://t.me/USMLEWorldStep3
[M
1
•
2
= .
-
Item 13of 39
Question Id: 5530
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
1111
;'
rim
ffiffij
Calculator
3
4
A 43-year-old n,ale presents to your office with several months history of progressive fatigue and occasional palpitations. He had three episodes
s
of acute respiratory infections over the last year; otheiwise, his past medical history is insignificant. He smokes two packs of cigarettes daily and
6
consumes alcohol occasionally. He is not taking any medications and denies drug abuse. He has been sexually active with several partners
7
recently. The physical examination is insignificant. His laboratory values are:
8
Hb
6.7 g/dl
10
Red blood cells
2.3 million/cmm
11
White blood cells
5,900/cmm
9
12
14
~
Segmented neutrophils
60°/o
Bands
3°/o
Eosinophils
2o/o
Lymphocytes
30°/o
Monocytes
5%
6
17
18
19
MCHC
33°/o
MCV
85 fl
20
21
22
•
His HIV test results are negative. Which of the following is the best next step in the management of this patient?
~
Q
Q
Q
Q
4
25
•
26
27
•
28
A. ESR and serum C-reactive protein
8 . Serum iron and TIBC
C. Reticulocyte count
D. Hemoglobin electrophoresis and Coombs' test
29
•
30
31
•
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
= .
9
•
-
10
Item 13of 39
Question Id: 5530
•\
~
Mart<
11
•
•
•
<]
C>
Previous
Next
r,
L .J
Fun Screen
Hb
6.7 g/dl
Red blood cells
2.3 million/cn1m
White blood cells
5,900/cmm
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
12
14
~
Segmented neutrophils
60°/o
17
Bands
3°/o
18
Eosinophils
2o/o
Lymphocytes
30°/o
Monocytes
5%
6
19
20
21
22
~
4
25
MCHC
33°/o
MCV
85 fl
His HIV test results are negative. Which of the following is the best next step in the management of this patient?
26
Q
Q
Q
Q
Q
27
28
29
30
31
32
33
A. ESR and serum C-reactive protein
B. Serum iron and TIBC
C. Reticulocyte count
D. Hemoglobin electrophoresis and Coombs' test
E. Bone n1arrow biopsy
34
35
Submit
36
37
-~
39
•
T
https://t.me/USMLEWorldStep3
11111
;'
rim
ffiffij
Calculator
,
Reverse Color
~
~
Text Zoom
~
~
Settings
•
= .
9
•
-
10
Item 13of 39
Question Id: 5530
•\
~
Mart<
11
•
•
•
<]
C>
Previous
Next
r,
L .J
Fun Screen
Hb
6.7 g/dl
Red blood cells
2.3 million/cn1m
White blood cells
5,900/cmm
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
11111
;'
rim
,
ffiffij
Calculator
Reverse Color
~
~
Text Zoom
~
~
Settings
•
12
14
~
Segmented neutrophils
60°/o
17
Bands
3°/o
18
Eosinophils
2o/o
Lymphocytes
30°/o
Monocytes
5%
6
19
20
21
22
~
4
25
MCHC
33°/o
MCV
85 fl
His HIV test results are negative. Which of the following is the best next step in the management of this patient?
26
A. ESR and serum C-reactive protein (5°/o)
27
28
B. Serum iron and TIBC (28%)
29
30
C. Reticulocyte count (49%)
31
0 . Hemoglobin electrophoresis and Coombs' test (7%)
32
E. Bone n1arrow biopsy (9%)
33
34
35
36
Omitted
37
Correct answer
-~
39
•
-
T
TUTOR
11 ..
L!!!.
49%
Answered correctly
IT\
\.::J
05 secs
Time Spent
https://t.me/USMLEWorldStep3
02/03/2020
• Last Updated
~
F2ck
SgJ2,d
Eng ock
= .
9
•
-
10
Question Id: 5530
•
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
1111
;'
rim
ffiffij
Calculator
12
Omttted
•
•\
~
-----------------------
11
•
Item 13of 39
14
Correct answer
C
~
( 1,, 49%
l!!!.
(T\ 05 secs
\::.J
Answered correctly
Time Spent
•
02/03/2020
Last Updated
6
17
Explanation
18
19
Normocytic/normochromic anemia is a very broad category. It may be caused by two large groups of disorders: 1) diseases with decreased red
20
blood cell production, and 2) hemolytic disorders. To determine the predominant pathophysiologic mechanism of anemia in this patient, a
21
reticulocyte count must be obtained. An elevated reticulocyte count indicates hemolysis as the cause of anemia; other findings associated with
22
increased RBC destruction should be sought (e.g. elevated indirect bilirubin level, decreased haptoglobin, increased LOH, splenomegaly). A low
~
reticulocyte count indicates a hypoproliferative state; renal disease, hypothyroidism and aplastic anemias may be present.
4
(Choice D) Further evaluation of hemolytic anemias may include hemoglobin electrophoresis and Coombs' test.
25
(Choice A) Anemia of chronic disease may present as normocytic/normochromic anemia; ESR and serum C-reactive protein measurements may
26
help in the diagnosis.
27
(Choice B) Iron deficiency anemia is microcytic/hypochromic.
28
29
(Choice E) Bone marrow biopsy is not indicated at this stage.
30
Educational Obj ective:
31
Obtaining a reticulocyte count helps in determining the predominant pathophysiologic mechanism of normocytic/normochromic anemia.
32
33
34
Foundations of Independent Practice
Hen1atology & Oncology
Hemolytic anemia
35
Subject
System
Topic
36
opyng
I@ ..JWorla
Is
...
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
= .
9
•
-
10
Item 14of 39
Question Id: 10164
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!.)
Tutorial
•!
1111
Lab Yallles
m,
;'
Notes
rim
ffiffij
Calculator
11
•
,
•
12
A 53-year-old woman comes to the emergency department with a 1-day history of hematemesis and hypotension. She w as hospitalized for
13
unprovoked right femoral vein thrombosis and pulmonary embolism 1 month ago and has been taking warfarin since. In the emergency
14
,·,st
department, the patient is resuscitated with intravenous fluids and fresh frozen plasma. Warfarin is discontinued and she is started on intravenous
15
pantoprazole. Upper gastrointestinal endoscopy shows several deep gastric ulcers. Later during the hospital course, the option of inferior vena
16
cava (IVC) filter placement is discussed with the patient. Which of the following complications would this patient be at highest long-term risk for
17
developing following IVC filter placement?
18
Q
Q
Q
Q
Q
19
20
21
22
~
4
A . Perforation through inferior vena cava
B. Portal vein thrombosis
C. Recurrent deep venous thrombosis
D. Recurrent pulmonary thromboembolism
E. Retroperitoneal bleeding
25
26
27
Submit
28
29
30
31
32
33
34
35
36
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
= .
9
•
-
10
Item 14of 39
Question Id: 10164
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!.)
1111
;'
rim
ffiffij
Calculator
11
•
,
•
12
A 53-year-old woman comes to the emergency department with a 1-day history of hematemesis and hypotension. She w as hospitalized for
13
unprovoked right femoral vein thrombosis and pulmonary embolism 1 month ago and has been taking warfarin since. In the emergency
14
,·,st
department, the patient is resuscitated with intravenous fluids and fresh frozen plasma. Warfarin is discontinued and she is started on intravenous
15
pantoprazole. Upper gastrointestinal endoscopy shows several deep gastric ulcers. Later during the hospital course, the option of inferior vena
16
cava (IVC) filter placement is discussed with the patient. Which of the following complications would this patient be at highest long-term risk for
17
developing following IVC filter placement?
18
A . Perforation through inferior vena cava ( 18o/o)
19
20
B. Portal vein thrombosis ( 12°/o)
21
C. Recurrent deep venous thrombosis (55%)
22
~
D. Recurrent pulmonary thromboembolism (5%)
4
E. Retroperitoneal bleeding (7%)
25
26
27
Omitted
28
Correct answer
C
29
111.
I.!.!!..
55%
Answered correctly
(T'\ 02 secs
\.::) Time Spent
04/26/2020
• Last Updated
30
31
Explanation
32
33
Inferior vena cava (IVC) filters are an option for patients with acute deep venous thrombosis (DVT) who have contraindications to
34
anticoagulation (eg, recent surgery, hemorrhagic stroke, bleeding diathesis, active bleeding). IVC filters can be permanent or retrievable and are
35
usually placed via a transvenous approach. They inhibit progression of lower extremity clots through the IVC toward the lungs.
36
Acute complications of IVC filter placement include guidewire entrapment w ithin the filter and post-procedural complications (eg, acute insertion
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
= .
9
•
-
10
Item 14of39
Question Id: 10164
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!.)
1111
;'
rim
,
ffiffij
Calculator
Reverse Color
~
~
~
~
Text Zoom
Settings
SgJ2,d
Eng ock
11
•
,
12
Inferior v ena cava (IVC) filter s are an option for patients with acute deep venous thrombosis (DVT) who have contraindications to
13
anticoagulation (eg , recent surgery, hemorrhagic stroke, bleeding diathesis, active bleeding). IVC filters can be permanent or retrievable and are
14
,·,st
usually placed via a transvenous approach. They inhibit progression of lower extremity clots through the IVC toward the lungs.
15
•
Acute complications of IVC filter placement include guidewire entrapment w ithin the filter and post-procedural complications (eg, acute insertion
16
site thrombosis, hematoma, arteriovenous fistula). The main long-term complication of IVC filter placement is recurrent DV Ts. The filter can
17
prevent clot progression to a pulmonary embolism, but it does not prevent future DVTs or treat the underlying thrombotic predisposition. As a
18
result, patients can develop both acute and recurrent thrombosis at the insertion site. IVC thrombosis can also occur due to thrombogenicity of the
19
filter, new local thrombus formation, or trapped embolus. IVC filters do not appear to affect overall mortal ity significantly.
20
(Choice A ) IVC filter migration and perforation through the IVC are much less common complications than recurrent DVT.
21
(Choice B) IVC filters are usually placed in the IVC just below the renal veins to decrease risk of venous thromboen1bolism from all likely venous
22
~
pathways. The portal vein drains into the liver above this level and would be unl ikely to be affected by an IVC filter.
4
(Choice D) Small thrombi can extend through the IVC filter or go through collateral circulation, but most studies have shown that recurrent
25
pulmonary thromboembolism is an uncommon complication of IVC filters.
26
(Choice E) Retroperitoneal bleeding is most commonly due to trauma to the lower back, vascular procedures near the retroperitoneal space (eg,
27
cardiac catheterization, aortic catheter), anticoagulation, or hemorrhage from a malignancy in the retroperitoneal organs (eg , pancreas). However,
28
retroperitoneal bleeding is not a common complication of IVC filter placement.
29
30
Educational objective:
31
Inferior vena cava (IVC) filters are an option for patients with acute deep venous thrombosis (DVT) who have contraindications to anticoagulation.
32
Long-term complications of IVC filter placement include recurrent DVTs and IVC thrombosis. IVC filters do not appear to affect overall mortality
33
significantly.
34
References
35
• Vena caval filters: current knowledge, uncertainties and practical approaches
36
• Eight-year follow-up of patients with permanent vena cava filters in the prevention of pulmonary embolism: the PREPIC (Prevention du Risque
- -- - - - - - ... - - - - - - -- - - -
37
-~
39
•
--
T
TUTOR
. --
https://t.me/USMLEWorldStep3
~
F2ck
= .
9
•
-
10
Item 14of 39
Question Id: 10164
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!.)
1111
;'
rim
ffiffij
Calculator
11
•
prevent clot progression to a pulmonary embolism, but it does not prevent future DVTs or treat the underlying thrombotic predisposition . As a
12
result, patients can develop both acute and recurrent thrombosis at the insertion site. IVC thrombosis can also occur due to thrombogenicity of the
13
,
•
filter, new local thrombus formation, or trapped embolus. IVC filters do not appear to affect overall mortality significantly.
14
,·,st
15
(Choice A) IVC filter migration and perforation through the IVC are much less common complications than recurrent DVT.
16
(Choice B) IVC filters are usually placed in the IVC just below the renal veins to decrease risk of venous thromboembolisn1 from all likely venous
17
pathways. The portal vein drains into the liver above this level and would be unlikely to be affected by an IVC filter.
18
(Choice D) Small thrombi can extend through the IVC filter or go through collateral circulation, but most studies have shown that recurrent
19
pulmonary thromboembolism is an uncommon complication of IVC filters.
20
21
(Choice E) Retroperitoneal bleeding is most commonly due to traun1a to the lower back, vascular procedures near the retroperitoneal space (eg ,
22
cardiac catheterization, aortic catheter), anticoag ulation, or hen1orrhage from a m alignancy in the retroperitoneal organs (eg, pancreas). However,
~
retroperitoneal bleeding is not a common complication of IVC filter placement.
4
Educational objective:
25
Inferior vena cava (IVC) filters are an option for patients with acute deep venous thrombosis (DVT) who have contraindications to anticoagulation.
26
Long-term complications of IVC filter placement include recurrent DVTs and IVC thrombosis. IVC filters do not appear to affect overall mortality
27
significantly.
28
References
29
• Vena caval filters: current knowledge, uncertainties and practical approaches
30
• Eight-year follow-up of patients with permanent vena cava filters in the prevention of pulmonary embolism: the PREPIC (Prevention du Risque
31
d'Embolie Pulmonaire par Interruption Cave) randomized study.
32
33
34
Foundations of Independent Practice
Hen1atology & Oncology
35
Subject
System
36
opyng
I@ ..JWorla
Venous thromboembolism
Topic
Is
...
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
= .
9
•
-
10
Item 15of 39
Question Id: 18285
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
Lab Yallles
m,
;'
Notes
rim
ffiffij
Calculator
11
•
•
12
13
The following vignette applies to the next 2 items. The items in this set must be answered in sequential order. Once you click Proceed to Next
14
Item, you will not be able to add or change an answer.
A 2-year-old boy is brought to the clinic by his parents due to worsening right ear pain. His mother states, "He started tugging at his ear 3 days
ago and had a fever, but I could not take time off from work to bring hi m in." This morning, the pain increased , and his father notes that "his ear
17
seems more prominent, like it's sticking out from his head ." The patient has been less active than normal but has had no vomiting, diarrhea, or
18
rash. He had an episode of acute otitis media 2 months ago that resolved with oral antibiotics. Immunizations are up to date, and he takes no
19
daily medications. Temperature is 40 C (104 F), blood pressure is 100/40 mm Hg, pulse is 132/min, and respirations are 30/niin. Examination
20
shows a tired, irritable boy who screams with any attempt to examine his ear. Swelling, erythema, and tenderness to palpation are noted posterior
21
to the right ear. Otoscopy reveals an erythematous and bulging tympanic membrane with loss of normal landmarks and light reflex.
22
Item 1 of 2
~
Involvement of which of the following structures is most likely responsible for this patient's presentation?
4
Q A. Epidural space
25
26
0
0
0
0
27
28
29
30
31
B. External auditory canal
C. Labyrinth
0 . Mastoid air cells
E. Meninges
32
33
Submit
34
35
36
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
= .
9
•
-
10
Item 15of 39
Question Id: 18285
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
1111
;'
rim
ffiffij
Calculator
11
•
•
12
13
The following vignette applies to the next 2 items. The items in this set must be answered in sequential order. Once you click Proceed to Next
14
Item, you will not be able to add or change an answer.
A 2-year-old boy is brought to the clinic by his parents due to worsening right ear pain. His mother states, "He started tugging at his ear 3 days
ago and had a fever, but I could not take time off from work to bring hi m in." This morning, the pain increased , and his father notes that "his ear
17
seems more prominent, like it's sticking out from his head ." The patient has been less active than normal but has had no vomiting, diarrhea, or
18
rash. He had an episode of acute otitis media 2 months ago that resolved with oral antibiotics. Immunizations are up to date, and he takes no
19
daily medications. Temperature is 40 C (104 F), blood pressure is 100/40 mm Hg, pulse is 132/min, and respirations are 30/niin. Examination
20
shows a tired, irritable boy who screams with any attempt to examine his ear. Swelling, erythema, and tenderness to palpation are noted posterior
21
to the right ear. Otoscopy reveals an erythematous and bulging tympanic membrane with loss of normal landmarks and light reflex.
22
Item 1 of 2
~
Involvement of which of the following structures is most likely responsible for this patient's presentation?
4
25
A. Epidural space (0%)
26
B. External auditory canal (8°/o)
27
C. Labyrinth (6%)
28
29
0 . Mastoid air cells (83°/o)
30
E. Meni nges (0%)
31
32
33
34
Omitted
35
Correct answer
D
36
11 ..
l!!!.
83%
Answered correcUy
(i'\ 02 secs
\.::J
Time Spent
¢=:I 07/01/2020
l==.I Last Updated
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
= .
9
•
-
10
Item 15of 39
Question Id: 18285
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
1111
;'
rim
ffiffij
Calculator
11
•
12
Mastoiditis
13
•
14
Mastoid
air cells
17
18
19
20
21
22
~
4
25
26
27
28
This febrile child with a bulging tympanic m embrane who has mastoid tenderness and displacement of the external ear likely has acute
29
mastoiditis, th e most common suppurative complication of acute otitis media (AOM). The mastoid air cells are in continuity with the middle ear,
30
allowing spread of the infection. In addition to the symptoms of fever and ear pai n seen in AOM, infection of the mastoid causes erythema and
31
tender swelling, which can result in outward and/or vertical displacement of the auricle . The tympanic n1embrane n1ay show evidence of AOM
32
(eg , erythen,a, bulging, perforation) or may not be visible due to swelling of the external auditory canal.
33
As with AOM, mastoiditis is most commonly seen in children age ~2 and is commonly caused by Streptococcus pneumoniae, Streptococcus
34
pyogenes, and Staphylococcus aureus. Pseudomonas aeruginosa has occasionally been implicated, especially in patients with recurrent
35
infections or recent antibiotic use.
36
(Choices A and E) lntracranial extension (eg , epidural space, meninges, brain) of AOM can occur and cause n1eningitis, an epidural abscess,
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
= .
9
•
-
10
Item 15of 39
Question Id: 18285
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
1111
;'
rim
ffiffij
Calculator
11
•
•
12
This febrile child with a bulgi ng tympanic membrane who has mastoid tenderness and displacement of the external ear likely has acute
13
mastoi ditis, the most common suppurative complication of acute otitis media (AOM). The mastoid air cells are in continuity with the middle ear,
14
allowing spread of the infection. In add ition to the symptoms of fever and ear pain seen in AOM , infection of the mastoid causes erythema and
tender swelling, which can result in outward and/or vertical displacement of the auricle. The tympanic membrane may show evidence of AOM
(eg, erythen1a, bulging, perforation) or may not be visible due to swelling of the external auditory canal.
17
As with AOM, mastoiditis is most commonly seen in children age ~2 and is commonly caused by Streptococcus pneumoniae, Streptococcus
18
pyogenes, and Staphylococcus aureus. Pseudomonas aeruginosa has occasionally been implicated, especially in patients with recurrent
19
infections or recent antibiotic use.
20
(Choi ces A and E) lntracranial extension (eg , epidu ral space, meninges, brain) of AOM can occur and cause meningitis, an epidural abscess,
21
lateral sinus thrombosis, or a brain abscess. However, in addition to the symptoms of fever and otalgia common in AOM, patients with intracranial
22
extension typically have signs of meningeal irritation and increased intracranial pressure (eg, vomiting).
~
(Choice B) Infection of the external auditory canal results in otitis externa, which is characterized by pain, erythema, and edema of the external
4
auditory canal, not the mastoid process. It is not typically seen as a complication of AOM, and the tympanic membrane would not be bulging or
25
erythematous.
26
27
(Choice C) Suppurative labyrinthitis can occur as a complication of AOM due to spread of the infection to the bony labyrinth of the inner ear. In
28
addition to symptoms of fever and otalgia due to AOM, patients with suppurative labyrinthitis typically have severe vertigo with nystagmus, nausea
29
and vomiting, and significant hearing loss.
30
Educational objective:
31
Acute mastoiditis, a complication of acute otitis media (AOM), i s caused by spread of the infection from the middle ear space to the mastoid air
32
cells. In addition to the fever and otalgia often present in AOM, patients also have mastoid inflammation, resulting in tenderness of the mastoid
33
process and displacement of the auricle.
34
35
36
Foundations of Independent Practice
Ear, Nose & Throat (ENT)
Mastoiditis
Subjecl
System
Topic
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
=
9
•
10
Item _15of39
Question Id: 18285
• ~Mart<
\
<]
C>
~~
G)
il
'!,·
Previous
Next
Fun Screen
Tutorial
Lab varues
Notes
= ,
Calculator
Reverse Color
~
@
Text Zoom
Settings
11
•
12
13
•
r5l
Exhibit Display
Suppurative complications of acute otitis media
14
Brain abscess
17
18
19
r
20
21
Meningitis
22
~
4
25
•
26
27
r
28
29
30
Mastoiditis
31
32
o titis media
33
34
4i>UWotld
35
©_
36
Zoom In
8_
Zoom Out
C
Reset
fl,
Add To Flash Card
37
· ~39
,
T
https://t.me/USMLEWorldStep3
~
=
9
•
10
Item _15of39
Question Id: 18285
<]
C>
~~
G)
il
'!,·
Previous
Next
Fun Screen
Tutorial
Lab varues
Notes
• ~Mart<
\
= ,
Calculator
Reverse Color
~
@
Text Zoom
Settings
11
•
12
r5l
Exhibit Display
13
•
Signs ol menl ngeal Irritation
14
Brudzinsld sign
17
18
19
20
21
22
~
,, '
,
,,
4
25
Komlg sign
26
27
28
----
29
30
.-.
, ..
'
,,
'
,,
Leg exlel'l$ion on so°-IIO><ed
hip causes ~ & resistance
31
32
33
34
35
©_
36
-
Zoom In
8_
Zoom Out
C
Reset
fl,
Add To Flash Card
37
· ~39
,
T
https://t.me/USMLEWorldStep3
~
= .
9
•
-
10
Item 16of 39
Question Id: 18286
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
Lab Yallles
m,
;'
Notes
rim
ffiffij
Calculator
11
•
•
12
Item 2 of 2
13
CT scan of the temporal bones is obtained which reveals fluid in the mastoid air cells with erosion of bony septa. Which of the following is the
14
most appropriate step in management?
Q
Q
Q
Q
Q
17
18
19
20
21
22
~
A. Combination ototopical antibiotics and glucocorticoids
B. Lumbar puncture and CSF culture
C. Middle ear drainage and IV antibiotics
D. Oral antibiotics and follow-up CT scan in a week
E. Sinus surgery and nasal irrigation
4
Submit
25
26
27
28
29
30
31
32
33
34
35
36
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
10
= .
-
Item 16of 39
Question Id: 18286
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
1111
;'
rim
ffiffij
Calculator
11
•
•
12
Item 2 of 2
13
CT scan of the temporal bones is obtained which reveals fluid in the mastoid air cells with erosion of bony septa . Which of the following is the
14
most appropriate step in management?
A. Combination ototopical antibiotics and glucocorticoids (2o/o)
17
B. Lumbar puncture and CSF culture (3°/o)
18
19
20
21
22
~
C. Middle ear drainage and IV antibiotics (77°A.)
D. Oral antibiotics and follow-up CT scan in a week (1 2°/o)
E. Sinus surgery and nasal irrigation (3%)
25
Omitted
26
Correct answer
C
11 .. 77%
l!!!. Answered correcUy
, i \ 02 secs
\..::,/ Time Spent
F=1 07/01/2020
13 Last Updated
27
28
29
Explanation
30
31
Mastoiditis
32
• Infection of the mastoid air cells
33
34
Pathophysiology
• Complication of acute otitis media
35
• Most commonly due to Streptococcus pneumoniae
36
• Fever & otalgia
37
. rsl
-~
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
= .
9
•
-
10
•\
~
Item 16of 39
Question Id: 18286
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
1111
;'
rim
ffiffij
Calculator
11
•
Mastoiditis
12
13
•
• Infection of the mastoid air cells
14
Pathophysiology
• Complication of acute otitis media
• Most commonly due to Streptococcus pneumoniae
• Fever & otalgia
17
Clinical findings
18
• Inflammation of mastoid
• Protrusion of the auricle
19
• Opacification of m astoid air cells on CT scan or M RI
20
21
Management
22
~
Complications
• In travenous antibiotics
• Drainage of purulent m aterial (eg, tympanostomy, mastoidectomy)
• Extracranial extension (subperiosteal abscess, facial nerve palsy, hearing loss, labyrinthitis)
• ln tracranial extension (brain abscess, meni ngitis)
4
25
Acute mastoiditis can often be diagnosed clinically. Imaging (eg, CT scan, MRI) is indicated if the diagnosis is unclear, if there is suspicion for
26
further complications (eg, meningitis, neurologic deficits), if the child appears toxic, or if the condition does not respond to initial treatment. In
27
these cases, CT scan shows destruction of the bony septa in the mastoid air cells, confirming the diagnosis of acute coalescent mastoiditis.
28
29
Treatment of mastoiditis requires intravenous antibiotic therapy with activity against common upper respiratory pathogens (eg, Streptococcus
30
pneu,noniae), as well as Streptococcus pyogenes and Staphylococcus aureus. Expanded coverage for Pseudomonas (eg, cefepime) sh ould be
31
used if there is a history of recent antibiotic use. Drainage of the purulent m aterial i s also required. This can be achieved by tympanostomy (±
ear tube placement) or mastoidectomy.
32
33
Patients should be monitored to ensure that they do not develop more severe compl ications due to extracranial (eg, subperiosteal abscess,
34
hearing loss) or intracranial (eg, meningitis, brain abscess) exten sion.
35
(Choice A) Combination ototopical antibiotics and glucocorticoids would be appropriate treatment for otitis externa, but they do not appropriately
36
treat acute mastoiditis.
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
10
11
•
•
12
Acute mastoiditis can often be diagnosed clinically. Imagi ng (eg, CT scan, MRI) is indicated if th e diagnosis is unclear, if there is suspicion for
13
further complications (eg, meningitis, neu rologic deficits), if the child appears toxic, or if the condition does not respond to initial treatment. In
14
these cases, CT scan shows destruction of the bony septa in the mastoid air cells, confirming the diagnosis of acute coalescent mastoiditis.
Treatment of mastoiditis requires intra ven ou s antibiotic therapy with activity against common upper respiratory pathogens (eg, Streptococcus
pneu,noniae), as well as Streptococcus pyogenes and Staphylococcus aureus. Expanded coverage for Pseudomonas (eg, cefepime) should be
17
used if there is a history of recent antibiotic use. Drainage of the purulent material is also required. This can be achieved by tympanostomy (±
18
ear tube placement) or mastoidectomy.
19
20
Patients should be monitored to ensure that they do not develop more severe compl ications due to extracranial (eg, subperiosteal abscess,
21
hearing loss) or intracranial (eg, meningitis, brain abscess) exten sion.
22
(Choice A) Combination ototopical antibiotics and glucocorticoids would be appropriate treatment for otitis externa, but they do not appropriately
~
treat acute mastoiditis.
4
(Choice B) Meningitis is a possible complication of AOM or mastoiditis. Lumbar puncture and CSF culture would be obtained for diagnosis.
25
However, this patient does not h ave clinical signs (eg, vom iting, nuchal rigidity) or radiographic evidence (eg , effacement of ventricles indicating
26
increased intracranial pressure) of meningitis.
27
(Choice D) Oral antibiotics would be an appropriate treatment for uncomplicated AOM . However, this patient's CT scan showing destruction of
28
the bone is diagnostic of acute mastoiditis, which requires more aggressive treatn1ent.
29
30
(Choice E) Sinus surgery with n asal irrigation may be indicated for complications of acute sinusitis (eg, orbital cellulitis). However, mastoiditis is a
31
complication of AOM rather than sinusitis b ecause the mastoid air cells are in continuity with th e middle ear, not the paranasal sinuses.
32
Educational objective :
33
Acute mastoiditis should be treated with intravenous antibiotic therapy and drainage of the purulent material in the middle ear either by
34
tympanostomy (± ear tube placement) or mastoidectomy.
35
36
Foundations of Independent Practice
37
-~
39
•
• •
T
TUTOR
Ear, Nose & Throat (ENT)
s
• ..
Mastoiditis
• •
https://t.me/USMLEWorldStep3
~
F2ck
SgJ2,d
Engock
= .
9
•
-
10
Item 16of 39
Question Id: 18286
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
11111
;'
rim
ffiffij
Calculator
11
•
•
these cases, CT scan shows destruction of the bony septa in the mastoid air cells, confirming the diagnosis of acute coalescent mastoiditis.
12
13
Treatment of mastoiditis requires intravenous antibiotic therapy with activity against common upper respiratory pathogens (eg, Streptococcus
14
pnewnoniae), as well as Streptococcus pyogenes and Staphylococcus aureus. Expanded coverage for Pseudomonas (eg, cefepime) should b e
used if there is a history of recent antibiotic use. Drainage of the purulent material is also required. This can be achieved by tympanostomy (±
ear tube placement) or mastoidectomy.
17
Patients should be monitored to ensure that they do not develop more severe compl ications due to extracranial (eg, subperiosteal abscess,
18
hearing loss) or intracranial (eg, meningitis, brain abscess) extension.
19
(Choice A) Combination ototopical antibiotics and glucocorticoids would be appropriate treatment for otitis externa, but they do not appropriately
20
treat acute mastoiditis.
21
(Choice B) Meningitis is a possible complication of AOM or mastoiditis. Lumbar puncture and CSF culture would be obtained for diagnosis.
22
~
However, this patient does not have clinical signs (eg, vomiting, nuchal rigidity) or radiographic evidence (eg , effacement of ventricles indicating
increased intracranial pressure) of meningitis.
4
25
(Choice D) Oral antibiotics would be an appropriate treatment for uncomplicated AOM. However, this patient's CT scan showing destruction of
26
the bone is diagnostic of acute n1astoiditis, which requires more aggressive treatment.
27
(Choice E) Sinus surgery with nasal irrigation n1ay be indicated for complications of acute sinusitis (eg, orbital cellulitis). However, mastoiditis is a
28
complication of AOM rather than sinusitis because the mastoid air cells are in continuity with the middle ear, not the paranasal sinuses.
29
Educational objective:
30
Acute n1astoiditis should be treated with intravenous antibiotic therapy and drainage of the purulent material in the middle ear either by
31
tympanostomy (± ear tube placement) or n1astoidectomy.
32
33
34
Foundations of Independent Practice
Ear, Nose & Throat (ENT)
Mastoiditis
35
Subject
System
Topic
36
Copynghl@ .JWorid A
Is
...
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
=
9
•
10
• ~
Item _
16 of 39
Question Id: 18286
Mart<
\
<]
C>
~~
G)
il
'!,·
Previous
Next
Fun Screen
Tutorial
Lab varues
Notes
= ,
Calculator
Reverse Color
~
@
Text Zoom
Settings
11
•
1 -
12
-
,.
-
,. 1
II ;
,-
I
11.
1- 111
-1 ..
I
1- I ..
t I ,.
-
11
I
11
1- I
,. f l t
I
..
-
f ,. -
14
17
18
19
20
21
22
~
4
25
26
27
28
29
30
31
32
33
34
35
©_
36
Zoom In
8_
Zoom Out
C
Reset
fl,
Add To Flash Card
37
- ~39
•
T
I
,.
t f
r5l
Exhibit Display
13
•
- 1
https://t.me/USMLEWorldStep3
~
= .
9
•
-
10
Item 17of 39
Question Id: 5492
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
Lab Yallles
m,
rim
Notes
Calculator
;'
ffiffij
11
•
12
A 65-year-old Caucasian male presents to your office and complains of a hearing impairment. He is a manager and runs his own business. He
13
•
noticed that it is now difficult for him to understand his employees during business meetings. He hears well and speaks fluently while on the
14
~
15
•
16
a
m
-
phone or when talking to his wife, but he poorly understands 'the people talking on TV shows'. His past medical history is insignificant. He is
physically active, and works out in the gym three times a week. He does not smoke or consume alcohol. He is not taking any medications. You
perform a speech discrimination test that turns out to be normal. Which of the following actions w ill most likely reveal an impaired speech
discrimination in this patient?
18
Q A. Speaking slowly
19
20
0
0
0
0
21
22
~
4
25
B.
Decreasing visual stimulation
C. Creating background noise
D. Decreasing the intensity of sounds
E. Using more familiar vocabulary
26
27
Submit
28
29
30
31
32
33
34
35
36
37
. rsl
-~
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
= .
9
•
-
10
Item 17of 39
Question Id: 5492
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
m,
Lab Yallles
;'
Notes
rim
,
ffiffij
Calculator
Reverse Color
~
~
~
~
Text Zoom
Settings
SgJ2,d
Eng ock
11
•
12
A 65-year-old Caucasian male presents to your office and complains of a hearing impairment. He is a manager and runs his own business. He
13
•
noticed that it is now difficult for him to understand his employees during business meetings. He hears well and speaks fluently while on the
14
~
15
•
16
a
m
-
phone or when talking to his wife, but he poorly understands 'the people tal king on TV shows'. His past medical history is insignificant. He is
physically active, and works out in the gym three times a week. He does not smoke or consume alcohol. He is not taking any medications. You
perform a speech discrimination test that turns out to be normal. Which of the following actions w ill most likely reveal an impaired speech
discrimination in this patient?
18
19
A. Speaking slowly (2°/o)
20
B. Decreasing visual stimulation (8%)
21
C. Creating background noise (74%)
22
~
D. Decreasing the intensity of sounds (1 2°/o)
4
E. Using more familiar vocabulary (2°/o)
25
26
27
28
Omitted
29
Correct answer
C
30
Ii.. 74%
I.ill.. Answered correctly
~
ri', 02 secs
\..::J
04/21/2020
13 Last Updaled
Time Spent
31
32
Explanation
33
34
This patient presents with sympton1s and signs suggestive of presbycusis, a sensorineural hearing impairment in elderly individuals. Usually, the
35
disease is gradually progressive, and initially affects the high-frequency range of hearing. The decreased ability to discriminate speech is
36
. rsl
-~
.
especially obvious in a noisy, distracting environment. This is why the paJient can participate in a phone conversation and talk to his wife, but
37
.
T
TUTOR
..
- . ··-
-- .. -- -- ·- -- -
-- ·- ·- . - . .. ..
·- ·-https://t.me/USMLEWorldStep3
... -
·-
.
..
. .. - ..
. - ..
~
F2ck
= .
9
•
-
10
Item 17of 39
Question Id: 5492
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
11111
;'
rim
ffiffij
Calculator
11
•
12
E. Using more familiar vocabulary (2°/o}
13
•
14
~
15
•
16
a
m
-
Omrtted
Correct answer
C
'"·
l!!!.
fT\ 02secs
\::.J Time Spent
74%
Answered
correcUy
•
04/21/2020
Last Updated
18
19
Explanation
20
21
This patient presents with symptoms and signs suggestive of presbycusis, a sensorineural hearing impairment in elderly individuals. Usually, the
22
~
disease is gradually progressive, and initially affects the high-frequency range of hearing. The decreased ability to discriminate speech is
especially obvious in a noisy, distracting environment. This is why the patient can participate in a phone conversation and talk to his wife, but
4
has difficulties in understanding spoken language during business meetings and while watching TV shows. The speech discrimination score may
25
be normal in these patients; however, introducing background noise can reveal the hearing loss.
26
(Choices A and E) Patients with presbycusis have difficulties understanding rapid speech and a complex or less familiar vocabulary.
27
28
(Choices D and B) Decreasing the intensity of sounds and decreasing visual stimulation are less useful in eliciti ng the hearing problem in this
29
patient.
30
Educational Obj ective:
31
The decreased ability to discriminate speech in patients w ith presbycusis is especially obvious in a noisy, distracting environment.
32
33
34
Foundations of Independent Practice
Ear, Nose & Throat (ENT)
Hearing loss
35
Subject
System
Topic
36
Copynghl@ .JWorid A
Is
...
37
. rsl
-~
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
= .
9
•
-
10
Item 17of 39
Question Id: 5492
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
11111
;'
rim
ffiffij
Calculator
11
•
12
E. Using more familiar vocabulary (2°/o}
13
•
14
~
15
•
16
a
m
-
Omrtted
Correct answer
C
'"·
l!!!.
fT\ 02secs
\::.J Time Spent
74%
Answered
correcUy
•
04/21/2020
Last Updated
18
19
Explanation
20
21
This patient presents with symptoms and signs suggestive of presbycusis, a sensorineural hearing impairment in elderly individuals. Usually, the
22
~
disease is gradually progressive, and initially affects the high-frequency range of hearing. The decreased ability to discriminate speech is
especially obvious in a noisy, distracting environment. This is why the patient can participate in a phone conversation and talk to his wife, but
4
has difficulties in understanding spoken language during business meetings and while watching TV shows. The speech discrimination score may
25
be normal in these patients; however, introducing background noise can reveal the hearing loss.
26
(Choices A and E) Patients with presbycusis have difficulties understanding rapid speech and a complex or less familiar vocabulary.
27
28
(Choices D and B) Decreasing the intensity of sounds and decreasing visual stimulation are less useful in eliciti ng the hearing problem in this
29
patient.
30
Educational Obj ective:
31
The decreased ability to discriminate speech in patients w ith presbycusis is especially obvious in a noisy, distracting environment.
32
33
34
Foundations of Independent Practice
Ear, Nose & Throat (ENT)
Hearing loss
35
Subject
System
Topic
36
Copynghl@ .JWorid A
Is
...
37
. rsl
-~
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
= .
9
•
-
10
Item 18of 39
Question Id: 6140
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
Lab Yallles
m,
;'
Notes
rim
ffiffij
Calculator
11
•
12
A 65-year-old Caucasian female presents to the emergency department with progressive shortness of breath on mini mal exertion and fatigue.
13
•
She was diagnosed with myelodysplasia two years ago, and has been receiving supportive therapy with frequent RBC transfusions. Her
14
last transfusion was 3 months ago. She experienced an episode of severe pneumonia one year ago that required hospitalization and IV antibiotic
therapy. She is taking no medications cu rrently and has no known allergies. Her blood pressure is 120/70 mmHg and heart rate is 95/min.
.~
Physical examination reveals pallor. Systolic murmur with intensity of IINI is heard over the cardiac apex. Laboratory findings are significant for
17
hematocrit of 24% and hemoglobin level of 5.7 mg/dl. You consider RBC transfusion in this patient. Blood grouping and cross-matching
are done, but the blood bank is unable to find suitable blood . This is the first time such an incompatibility has occurred. What is the most likely
19
reason for this incompatibility?
20
21
22
~
4
25
26
27
Q
A
Autoantibodies
0
0
0
0
B.
Alloantibodies
C. Anti-Rh (D) antibodies
D. Anti-HLA antibodies
E. ABO incompatibility
28
29
Submit
30
31
32
33
34
35
36
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
= .
9
•
-
10
Item 18of 39
Question Id: 6140
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
m,
;'
Lab Yallles
Notes
rim
,
ffiffij
Calculator
Reverse Color
~
~
~
~
Text Zoom
Settings
SgJ2,d
Engock
11
•
12
A 65-year-old Caucasian female presents to the emergency department with progressive shortness of breath on mini mal exertion and fatigue.
13
•
She was diagnosed with myelodysplasia two years ago, and has been receiving supportive therapy with frequent RBC transfusions. Her
14
last transfusion was 3 months ago. She experienced an episode of severe pneumonia one year ago that required hospitalization and IV antibiotic
therapy. She is taking no medications cu rrently and has no known allergies. Her blood pressure is 120/70 mmHg and heart rate is 95/min.
.~
Physical examination reveals pallor. Systolic murmur with intensity of IIN I is heard over the cardiac apex. Laboratory findings are significant for
17
hematocrit of 24% and hemoglobin level of 5.7 mg/dl. You consider RBC transfusion in this patient. Blood grouping and cross-matching
are done, but the blood bank is unable to find suitable blood . This is the first time such an incompatibility has occurred. What is the most likely
19
reason for this incompatibility?
20
21
A . Autoantibodies (16°/o}
22
./ '
~
B.
Alloantibodies (54o/o)
4
C. Anti-Rh (D) antibodies (4°/o}
25
D. Anti-HLA antibodies (19%)
26
E. ABO incompatibility (4°/o}
27
28
29
30
Omitted
31
Correct answer
' "·
I.!.!!..
B
32
54%
Answered correcUy
(i'\ 02 secs
\.::.) Tillie Spent
02/03/2020
• Last Updated
33
34
Explanation
35
36
After blood is ordered for transfusion , the following compatibility testing is usually performed . First, the patient's ABO and Rh types are
···-- ,
- ·-.
-· ..
- ·. -- .
-· .
·-
37
-~
39
•
·--
T
TUTOR
..
--
--·--
-- -- -----https://t.me/USMLEWorldStep3
---
--·
~
F2ck
= .
9
•
•
•
-
10
Item 18of 39
Question Id: 6140
11
Omttted
12
Correct answer
13
B
•\
~
Mart<
<]
C>
Previous
Next
I II, 54%
l!!!.
r,
L .J
Fun Screen
" ' 02 secs
Answered correctly
\.::; Time Spent
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
1111
~
;'
rim
ffiffij
Calculator
02/03/2020
13 Last Updated
14
.~
Explanation
17
After blood is ordered for transfusion , the following compatibility testing is usually performed. First, the patient's ABO and Rh types are
determined. After this, the patient's serum is screened for unexpected antibodies, a procedure called pretransfusion antibody screening.
19
Pretransfusion antibody screening is intended to detect any of all clinically significant RBC antibodies. If negative, the patient can be safely
20
transfused. If positive, further investigation is usually w arranted to evaluate the identity of the antibody. The major problem that leads to difficulties
21
finding cross-matched blood in patients with a history of multiple transfusions is alloantibodies (e.g. , in patients with sickle cell anemia or
22
myelodysplasia)_ The most commonly implicated RBC antigens in that case are E, L and K. Moreover, these patients tend to develop multiple
~
alloantibodies that make finding compatible blood even more difficult.
4
(Choices C and E) Finding ABO and Rh-compatible blood is usually not a big challenge.
25
26
(Choice A) Autoantibodies are less likely to cause difficulties in cross-matching in this patient; they are commonly implicated as a cause of the
27
incompatible cross-match in patients w ith autoimmune anemia and taking certain drugs (e.g., methyldopa and procainamide).
28
(Choice D) HLA allosensitization increases risk of graft rejection in patients awaiting organ or bone marrow transplantation and platelet
29
refractoriness in those requiring subsequent platelet transfusion support. Remember that RBCs do not express HLA antigens.
30
Educational Obj ective:
31
The major problem that leads to difficulties finding cross-matched blood in patients with a history of multiple transfusions is alloantibodies.
32
33
34
Foundations of Independent Practice
Hen1atology & Oncology
Blood transfusion
35
Subject
System
Topic
36
opyng
I@ ..JWorla
Is
...
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
= .
• -
10
Item 19 of 39
Question Id: 5709
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
Lab Yallles
m,
rim
Notes
Calculator
;'
ffiffij
11
•
•
•
12
A 57-year-old woman comes to the primary care physician for a follow-up visit after undergoing a screening colonoscopy. The colonoscopy
13
revealed adenocarcinoma of the ascending colon and 2 well-differentiated, sessile, adenomatous polyps of the sigmoid colon. The patient has a
14
history of mitral valve prolapse and fibromyalgia. She has also had a prior hysterectomy. Her medications include hormone replacement therapy
~
and ibuprofen. The patient eats a high-fiber vegetarian diet and has consumed 3-4 alcoholic beverages per day for the past 30 years. She
smoked 1 pack of cigarettes a day for nearly 5 years, but quit 30 years ago. There is no family history of cancer. The patient is very concerned
6
about bei ng diagnosed with colon cancer. Which of the following was her most significant risk factor for developing colon cancer?
17
18
Q
Q
Q
Q
Q
20
21
22
~
4
A . Alcohol intake
B. High-fiber diet
C. Hormone replacement therapy
D. Nonsteroidal antiinflamn1atory drug intake
E. Tobacco use
25
26
27
Submit
28
29
30
31
32
33
34
35
36
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
= .
• -
10
Item 19 of 39
Question Id: 5709
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
Lab Yallles
m,
;'
Notes
rim
,
ffiffij
Calculator
Reverse Color
~
~
~
~
Text Zoom
Settings
SgJ2,d
Eng ock
11
•
•
•
12
A 57-year-old w oman comes to the primary care physician for a follow-up visit after undergoing a screening colonoscopy. The colonoscopy
13
revealed adenocarcinoma of the ascending colon and 2 well-differentiated, sessile, adenomatous polyps of the sigmoid colon. The patient has a
14
history of mitral valve prolapse and fibromyalgia. She has also had a prior hysterectomy. Her medications include hormone replacement therapy
~
and ibuprofen. The patient eats a high-fiber vegetarian diet and has consumed 3-4 alcoholic beverages per day for the past 30 years. She
smoked 1 pack of cigarettes a day for nearly 5 years, but quit 30 years ago. There is no family history of cancer. The patient is very concerned
6
about bei ng diagnosed with colon cancer. Which of the following was her most significant risk factor for developing colon cancer?
17
18
A . Alcohol intake ( 40o/o)
20
B. High-fiber diet ( 1°/o)
21
C. Hormone replacement therapy (3%)
22
~
D. Nonsteroidal antiinflamn1atory drug intake (2%)
4
E. Tobacco use (53%)
25
26
27
Omitted
28
'"·
I.!.!!..
Correct answer
29
A
40%
Answered correctly
(T'\ 02 secs
\.::) Time Spent
05/08/2020
• Last Updated
30
31
Explanation
32
33
Risk factors for colorectal cancer (CRC) include family history, polyposis syndromes (eg, familial adenomatous polyposis), inflammatory bowel
34
disease, and A frican-American race. Other risk factors include alcohol intake, cigarette smoking, and obesity. Several studies have suggested
35
that even moderate alcohol intake (2-3 drinks/day) is associated with increased CRC risk, though the highest risk was seen in heavy drinkers (;:4
36
drinks/day). Alcohol likely interferes with folate absorption, and heavy drinkers may also have decreased folate intake. Cigarette smoking is also
37
-~
39
•
---
T
TUTOR
-https://t.me/USMLEWorldStep3
...
~
F2ck
9
•
10
11
•
12
13
•
Explanation
14
.~
Risk factors for colorectal cancer (CRC) include family history, polyposis syndromes (eg, familial adenomatous polyposis), inflammatory bowel
disease, and African-American race. Other risk factors include alcohol intake, cigarette smoking, and obesity. Several studies have suggested
17
that even moderate alcohol intake (2-3 drinks/day) is associated with increased CRC risk, though the highest risk was seen in heavy drinkers (:::4
18
drinks/day). Alcohol likely interferes with folate absorption, and heavy drinkers may also have decreased folate intake. Cigarette smoking is also
associated with increased CRC risk, but the risk is primarily seen in current long-term smokers (eg, >30 years). This patient has a remote history
20
of light tobacco use; her heavy alcohol intake was a more likely contributor to her risk for CRC (Choice E).
21
(Choices B, C, and D) Regular nonsteroidal antiinflammatory drug intake, hormone replacement therapy in postmenopausal women, and a high-
22
fiber diet that is rich in fruits and vegetables are all thought to offer some protection against developing CRC.
~
Educational objective :
4
Risk factors for colorectal cancer include family history, polyposis syndromes (eg, familial adenomatous polyposis ), inflamn1atory bowel disease,
25
and African-American race. Other risk factors include alcohol intake, cigarette smoking, and obesity. Protective factors incl ude a high-fiber diet
26
rich in fruits and vegetables, regular nonsteroidal antiinflammatory drug use, hormone replacement therapy, and regular exercise.
27
References
28
29
, Alcohol intake and colorectal cancer: a pooled analysis of 8 cohort studies.
30
, Smoking and colorectal cancer. a meta-analysis.
31
, Alcohol drinking and colorectal cancer risk: an overall and dose-response meta-analysis of published studies.
32
33
34
Foundations of Independent Practice
Hen1atology & Oncology
35
Subject
System
36
Copynghl@ ..JWorla A
Colorectal polyps and cancer
Topic
Is
...
37
-~
39
•
T
https://t.me/USMLEWorldStep3
9
•
= .
• -
10
ltem 20of 39
Question Id: 6153
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
Lab Yallles
m,
rim
Notes
Calculator
;'
ffiffij
11
•
12
A 44-year-old Caucasian female presents to your office complaining of severe, episodic dizziness for the last year or two. During the episodes,
13
•
•
she feels that the room is spinning and she can't walk. The episodes last for one or two hours and resolve spontaneously. She also noticed
14
periodic decreased hearing and ringing sensation in her left ear. She has right knee osteoarthritis, and takes Tylenol and aspirin 2-3 times a day
~
to cope with the pain. She does not smoke or consume alcohol. Her blood pressure is 130/83 mmHg and heart rate is 74/min while standing, and
6
128/85 mmHg and 76/min, respectively, while supine. What is the most likely d iagnosis in this patient?
17
18
19
21
22
~
4
Q
A. Acoustic neuron1a
0
0
0
0
B. Benign positional vertigo
C. Aspirin toxicity
D. Meniere's disease
E.
Multiple sclerosis
25
26
Submit
27
28
29
30
31
32
33
34
35
36
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
= .
• -
10
ltem 20of 39
Question Id: 6153
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
1111
;'
rim
ffiffij
Calculator
11
•
12
A 44-year-old Caucasian female presents to your office complaining of severe, episodic dizziness for the last year or two. During the episodes,
13
•
•
she feels that the room is spinning and she can't walk. The episodes last for one or two hours and resolve spontaneously. She also noticed
14
periodic decreased hearing and ringing sensation in her left ear. She has right knee osteoarthritis, and takes Tylenol and aspirin 2-3 times a day
~
to cope with the pain. She does not smoke or consume alcohol. Her blood pressure is 130/83 mmHg and heart rate is 74/min while standing, and
6
128/85 mmHg and 76/min, respectively, while supine. What is the most likely d iagnosis in this patient?
17
18
A. Acoustic neuron1a (4°A.)
19
B. Benign positional vertigo (6%)
C. Aspirin toxicity (19%)
21
22
./ •
~
D . Meniere's disease (69%)
E.
4
Multiple sclerosis (0%)
25
26
27
Omitted
28
Correct answer
D
29
"" 69%
l!!!.
Answered correcUy
(T\ 02 secs
\..::,I Time Spent
~
04/21/2020
13 Last Updated
30
31
Explanation
32
33
This patient presents with a classic triad of periodic vertigo, unilateral hearing loss and tinnitus that is characteristic for Meniere's disease.
34
Although many patients initially experience only some symptoms, most eventually go on to experience the full complement of the disease.
35
Meniere's disease should be differentiated from a range of other conditions having similar presentations.
36
(Choice B) Benign paroxysmal positional vertigo (BPPV) is characterized by typical acute vertigo attacks that are provoked by a change in
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
10
11
•
12
13
•
Omitted
14
Correct answer
D
.~
Ii..
l!!!.
("j\ 02 secs
69%
Answered correcUy
\.::) Time Spent
~
04/21/2020
1.:.::J Last Updated
17
Explanation
18
19
This patient presents with a classic triad of periodic vertigo, unilateral hearing loss and tinnitus that is characteristic for Meniere's disease.
21
Although many patients initially experience only some symptoms, most eventually go on to experience the full complement of the disease.
22
Meniere's disease should be differentiated from a range of other conditions having similar presentations.
~
(Choice B) Benign paroxysmal positional vertigo (BPPV) is characterized by typical acute vertigo attacks that are provoked by a change in
4
position; however, unlike Meniere's disease, BPPV is not accompanied by hearing loss.
25
(Choice A) Acoustic neuroma is an important consideration in this patient, but acute vertigo episodes are uncommon in patients with acoustic
26
neuroma due to its gradual tumor growth.
27
(Choice C) Aspirin toxicity may n1anifest as tinnitus and vestibular symptoms, but unilateral hearing loss does not occur w ith this condition.
28
29
(Choice E) Multiple sclerosis can sometimes mimic Meniere's disease but usually presents with more w idespread non-localized symptoms.
30
Educational Obj ective:
31
A classic triad of periodic vertigo, unilateral hearing loss and tinnitus is characteristic for Meniere's disease.
32
33
34
Foundations of Independent Practice
Ear, Nose & Throat (ENT)
Meniere disease
35
Subject
System
Topic
36
opyng
I@ .JWorid
Is
...
37
-~
39
•
T
https://t.me/USMLEWorldStep3
9
•
= .
• -
10
ltem 21 of 39
Question Id: 5422
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
Lab Yallles
m,
rim
Notes
Calculator
;'
ffiffij
11
•
•
•
12
A 13-year-old girl comes to the physician for evaluation of her third episode of maxillary sinusitis during the past 7 months. She con1plai ns of
13
fever, headache, nasal congestion, and facial pain that began 3 days ago. Except for previous sinusitis episodes, her medical history is
14
unremarkable. The patient has no known allergies. Her family history is unremarkable, but both parents smoke cigarettes. On exami nation, she
~
has maxillary sinus tenderness and purulent nasal discharge. The remainder of the exami nation is normal. Computed tomography scan
6
demonstrates mucosa! thickening, opacification , and air-fluid levels in the maxillary sinuses .
17
Which of the following should the physician say to the patient's parents?
18
Q
Q
Q
Q
Q
19
20
22
~
4
25
A. Her sinusitis is caused by granulomatosis with polyangiitis
B. Her sinusitis is due to a hereditary immunodeficiency
C. She might be using cocaine
D. Secondhand smoke is associated with her disease
E. She should be evaluated for Kartagener syndrome
26
27
Submit
28
29
30
31
32
33
34
35
36
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
= .
• -
10
ltem 21 of 39
Question Id: 5422
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
1111
;'
rim
ffiffij
Calculator
11
•
•
•
12
A 13-year-old girl comes to the physician for evaluation of her third episode of maxillary sinusitis during the past 7 months. She con1plai ns of
13
fever, headache, nasal congestion, and facial p ain that began 3 days ago. Except for previous sinusitis episodes, her medical history is
14
unremarkable. The patient has no known allergies. Her family history is unremarkable, but both parents smoke cigarettes. On exami nation, she
~
has maxillary sinus tenderness and purulent nasal discharge. The remainder of the exami nation is normal. Computed tomography scan
6
demonstrates mucosa! thickening, opacification , and air-fluid levels in the m axillary sinuses .
17
W hich of the following should the physician say to the patient's parents?
18
19
A. Her sinusitis is caused by granulomatosis with polyangiitis (1 %)
20
B. Her sinusitis is due to a hereditary immunodeficiency ( 4°/o)
C. She might be using cocaine (0°/o)
22
~
D. Secondhand smoke is associated with her disease (87%)
4
E. She should be evaluated for Kartagener syndrome (6%)
25
26
27
28
Omitted
29
Correct answer
D
30
Ii..
I.ill..
ri', 05 secs
87%
\..::J
Answered correctly
Time Spent
~
03/11/2020
13 Last Updaled
31
32
Explanation
33
34
This patient presents with recurrent sinusitis, most likely due to secondhand smoke exposure. Cigarette smoke and air pollution can damage the
35
cilia responsible for moving mucus through the sinuses. The mucus builds up and obstructs the sinuses, resulting in secondary bacterial
36
overgrowth. Other common causes of recurrent sinusitis in otherwise healthy people include inadequately treated acute sinusitis, structural
37
abnormalities of the nasal septum or palate, and allergic rhinitis.
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
= .
• -
10
ltem 21 of 39
Question Id: 5422
.
11
•
•
Mart<
.
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
1111
;'
rim
ffiffij
Calculator
12
This patient presents with recurrent sinusitis, most likely due to secondhand smoke exposu re. Cigarette smoke and air pollution can damage the
13
•
. .
•\
~
cilia responsible for moving mucus through the sinuses. The mucus bu ilds up and obstructs the sinuses, resulting in secondary bacterial
14
overgrowth. Other common causes of recurrent sinusitis in otherwise healthy people incl ude inadequately treated acute sinusitis, structural
~
abnormalities of the nasal septum or palate, and allergic rhinitis.
6
17
(Choice A) Granulomatosis with polyangiitis (Wegener's) is a systemic necrotizing vasculitis marked by glomerulonephritis, chronic pneumonitis,
18
and recurrent sinusitis/otitis media. It occurs most commonly in older adults and is unlikely in this patient.
19
(Choice B) Hereditary immunodeficiencies are usually recessive or X-linked and marked by multiple sites of recurrent infection. This patient has
20
no other recurrent infections and an unremarkable family history, making this diagnosis unlikely.
(Choice C) Cocaine abuse may cause chronic or recurrent sinusitis. This patient does not have other associated symptoms, such as
22
nosebleeds, agitation, hypertension, and weight loss. It is inappropriate to declare this suspicion to the parents without further evaluation (eg, drug
~
testing) and discussion with the patient.
4
(Choice E) Kartagener syndrome is an autosomal recessive disorder consisting of situs inversus, chronic sinusitis, and airway disease leading to
25
bronchiectasis. It is a subgroup of a congenital mucociliary disorder known as primary ciliary dyskinesia. This patient has no other recurrent
26
infections, n1aking this diagnosis unlikely.
27
28
Educational objective:
29
Exposure to cigarette smoke and air pollution causes recurrent or chronic sinusitis by damaging the cilia responsible for moving mucus through
30
the sinuses. Other common causes of chronic or recurrent sin usitis include inadequately treated acute sinusitis, structural abnormalities of the
31
nasal septum or palate, and allergic rhinitis.
32
References
33
• Relationship between passive smoking, recurrent respiratory tract infections and otitis media in children.
34
35
36
Fou ndations of Independent Practice
Ear, Nose & Throat (ENT)
Sinusitis
Subject
System
Topic
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
10
11
•
•
12
13
overgrowth. Other common causes of recurrent sinusitis in otherwise healthy people include inadequately treated acute si nusitis, structural
14
abnormalities of the nasal septum or palate, and allergic rhinitis.
.~
(Choice A) Granulomatosis with polyangiitis (Wegener's) is a systemic necrotizing vasculitis marked by glomerulonephritis, chronic pneumonitis,
and recurrent sinusitis/otitis media. It occurs most commonly in older adults and is unlikely in this patient.
17
(Choice B) Hereditary immunodeficiencies are usually recessive or X-li nked and marked by multiple sites of recurrent infection. This patient has
18
no other recurrent infections and an unremarkable family history, making this diagnosis unlikely.
19
(Choice C) Cocaine abuse may cause chronic or recurrent sinusitis. This patient does not have other associated symptoms, such as
20
nosebleeds, agitation, hypertension, and weight loss. It is inappropriate to declare this suspicion to the parents without further evaluation (eg, drug
testing) and discussion with the patient.
22
~
(Choice E) Kartagener syndrome is an autosomal recessive disorder consisting of situs inversus, chronic sinusitis, and airway disease leading to
4
bronchiectasis. It is a subgroup of a congenital mucociliary disorder known as primary ciliary dyskinesia. This patient has no other recu rrent
25
infections, making this diagnosis unlikely.
26
Educational objective :
27
Exposure to cigarette smoke and ai r pollution causes recurrent or chronic sinusitis by damaging the cilia responsible for moving mucus through
28
the sinuses. Other common causes of chronic or recurrent sin usitis include inadequately treated acute sinusitis, structural abnormalities of the
29
nasal septum or palate, and allergic rhinitis.
30
References
31
• Relationship between passive smoking, recurrent respiratory tract infections and otitis media in children.
32
33
34
Foundations of Independent Practice
Ear, Nose & Throat (ENT)
Sinusitis
35
Subject
System
Topic
36
Copynghl@ .JWorid A
Is
...
37
-~
39
•
T
https://t.me/USMLEWorldStep3
9
•
= .
• -
10
ltem 22of 39
Question Id: 6 1 81
•\
~
Mart<
<]
C>
Previous
Next
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
r,
L .J
Fun Screen
\.!..)
1111
;'
rim
,
ffiffij
Calculator
Reverse Color
~
~
~
~
Text Zoom
Settings
SgJ2,d
Eng ock
11
•
•
•
12
A 55-year-old Caucasian male presents to your office complaining of easy fatigability. He used to be physically active and always preferred to
13
walk to work, which is five blocks away from where he lives. Now he says, "Doc, I get short of breath when I w alk even two blocks." He denies
14
any palpitations, chest pain, cough, or lower extremity swelling. He does not feel down and has no problems with sleep. His past medical history
~
is insignificant. He is currently not taking any medications. His blood pressure is 120170 mm Hg and heart rate is 95/min. The physical
6
examination is significant for pallor of the conjunctivae and oral mucosa. His laboratory values are:
17
18
19
20
Hemoglobin
7.2 g/L
Erythrocyte count
3.5 ml/mm3
MCHC
27%
MCV
72 fl
Platelets
200,000/mn,3
Leukocyte count
4,500/mm3
21
23
24
25
26
Neutrophils
56%
27
Eosinophils
1%
Lymphocytes
33%
30
Monocytes
10%
31
Serum ferriti n
28
29
24 ng/mL
32
Blood sn1ear analysis show s microcytic erythrocytes with anisocytosis. What is the best next step in the management of this patient?
33
34
Q
Q
35
36
37
-~
39
•
'
T
TUTOR
A. Direct Coombs test
B. Fecal occult blood test
-~~···-·--
-··-https://t.me/USMLEWorldStep3
~
F2ck
9
•
= .
• -
10
ltem 22of 39
Question Id: 6 1 81
•\
~
Mart<
11
•
•
•
<]
Previous
C>
r,
L .J
Next
Fun Screen
Erythrocyte count
3.5 ml/mm3
13
MCHC
27%
14
MCV
72 fl
Platelets
200,000/mm3
17
Leukocyte count
4,500/mm3
18
Neutrophils
56%
Eosinophils
1%
Lymphocytes
33%
Monocytes
10%
•!
m,
Lab Yallles
Notes
I'>\
\.!..)
Tutorial
11111
;'
12
~
6
19
20
21
23
Serum ferritin
24
25
24 ng/mL
Blood smear analysis shows microcytic erythrocytes with anisocytosis. What is the best next step in the managen1ent of this patient?
26
Q A. Direct Coombs test
27
28
0
0
0
0
29
30
31
32
33
B. Fecal occult blood test
C. Hemoglobin electrophoresis
D. Rheumatoid factor
E. Serum B 12 and folate levels
34
35
Submit
36
37
-~
39
•
T
https://t.me/USMLEWorldStep3
rim
ffiffij
Calculator
,
Reverse Color
~
~
Text Zoom
Settings
~
~
•
9
•
= .
• -
10
ltem 22of 39
Question Id: 6 1 81
•\
~
Mart<
11
•
•
•
<]
C>
Previous
Next
r,
L .J
Fun Screen
Erythrocyte count
3.5 ml/mm3
13
MCHC
27%
14
MCV
72 fl
Platelets
200,000/mm3
17
Leukocyte count
4,500/mm3
18
Neutrophils
56%
Eosinophils
1%
Lymphocytes
33%
Monocytes
10%
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
11111
;'
rim
,
ffiffij
Calculator
Reverse Color
~
~
Text Zoom
~
~
Settings
•
12
~
6
19
20
21
23
24 ng/mL
Serum ferritin
24
25
Blood smear analysis show s microcytic erythrocytes with anisocytosis. What is the best next step in the managen1ent of this patient?
26
A. Direct Coombs test (6%)
27
28
B. Fecal occult blood test (86%)
29
30
C. Hemoglobin electrophoresis (4%)
31
D. Rheumatoid factor (Oo/o)
32
E. Serum B12 and folate levels ( 1% )
33
34
35
36
Omitted
37
Correct answer
-~
39
•
-
T
TUTOR
11 ..
L!!!.
86%
Answered correctly
IT\
\.::J
04 secs
Time Spent
https://t.me/USMLEWorldStep3
03/30/2020
• Last Updated
~
F2ck
SgJ2,d
Eng ock
9
•
= .
• -
10
ltem 22of 39
Question Id: 6 1 81
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
1111
;'
rim
ffiffij
Calculator
11
•
Explanation
12
13
•
•
14
The diagnosis of iron deficiency anemia may not seem straightforward in this patient. Although microcytic/hypochromic anemia with anisocytosis
~
is consistent with iron deficiency anemia, the serum ferritin value could be considered troublesome because the traditional ferritin cutoff point for
iron deficiency is 15 ng/ml. Almost all patients with serum ferritin concentrations <15 ng/ml are iron deficient. There is no other clin ical situation
6
that explains such an extremely low level of serum ferritin. With the use of a 15 ng/ml cutoff point, the sensitivity of serum ferritin for detecting iron
17
deficiency is 59°/o and specificity is 99%. However, since the sensitivity of serun1 ferritin is only 59% with this cutoff, a significant number of
18
patients may have a value which is "borderline low" from 15-30 ng/ml; therefore, a value >15 ng/ml does not exclude the diagnosis. In fact, the
19
sensitivity of serum ferritin rises to 92o/o when 30 ng/ml is used as the cutoff, and specificity ren1ains similar. One, therefore, needs to be aware
20
that the traditional cutoff of 15 ng/ml for diagnosing iron deficiency anemia is not an absolute. Iron deficiency anemia is not excluded by the
21
ferritin level of 24 ng/ml in this patient; in fact, iron deficiency is the most likely diagnosis given the clinical scenario. The gastrointestinal tract is
the major source of blood loss leading to iron deficiency anemia in males; therefore, a fecal occult blood test is a reasonable initial choice for this
23
patient. A series of three fecal occult blood tests helps to maximize the sensitivity of the test, although endoscopy would likely be needed even if
24
negative. Colonoscopy is typically performed before E GD in these pdtl@I Its di lleSS ti 181 IS d pa, uccllar reason to suspect an upper gastrointestinal
25
source of bleed ing, such as NSAID use.
e
26
(Choice A) Autoimmune hemolytic anemia is usually norrnocytic/norrnochromic.
27
28
(Choice C) Although thalassemias can manifest as microcytic anemia, these usually present earlier in life, and characteristic findings on the blood
29
smear may be observed ("target cells").
30
(Choice D) Rheumatoid arthritis causes chronic inflammation and is a common cause of anemia of chronic disease. However, the serum ferritin
31
level is typically normal to elevated in anemia of chronic disease since it is an acute-phase reactant.
32
(Choice E) Vitamin 812 and folate deficiency anemias are usually macrocytic.
33
34
Educational objective :
35
Almost all patients with serum ferritin concentrations of less than the traditional cutoff of 15 ng/ml are iron deficient. However, the sensitivity using
36
this cutoff is only modest at best and it cannot be used to exclude the diagnosis of iron deficiency since the majority of patients with a level of 15-
37
30 mg/nl are also iron deficient. The gastrointestinal tract is the major source of blood loss leading to iron deficiency anemia in males.
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
= .
• -
10
Question Id: 6 1 81
11
•
•
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
1111
;'
rim
ffiffij
Calculator
that explains such an extremely low level of serum ferritin. With the use of a 15 ng/ml cutoff point, the sensitivity of serum ferritin for detecting iron
12
deficiency is 59°/o and specificity is 99%. However, since the sensitivity of serum ferritin is only 59% with this cutoff, a significant number of
13
•
ltem 22of 39
patients may have a value which is "borderline low" from 15-30 ng/ml; therefore, a value >15 ng/ml does not exclude the diagnosis. In fact, the
14
sensitivity of serum ferritin rises to 92o/o when 30 ng/ml is used as the cutoff, and specificity remains similar. One, therefore, needs to be aware
~
that the trad itional cutoff of 15 ng/ml for diagnosing iron deficiency anemia is not an absolute. Iron deficiency anemia is not excluded by the
6
ferritin level of 24 ng/ml in this patient; in fact, iron deficiency is the most likely diagnosis given the clinical scenario. The gastrointestinal tract is
17
the major source of blood loss leading
18
patient. A series of three fecal occult blood tests helps to maximize the sensitivity of the test, although endoscopy would likely be needed even if
19
negative. Colonoscopy is typically performed before E GD in these patients unless there is a particular reason to suspect an upper gastrointestinal
20
source of bleeding, such as NSAID use.
21
to iron deficiency anemia in males; therefore, a fecal occult blood test is a reasonable initial choice for this
(Choice A) Autoimmune hemolytic anemia is usually normocytic/normochromic.
23
(Choice C) Although thalassemias can manifest as microcytic anemia, these usually present earlier in life, and characteristic findings on the blood
24
smear may be observed ("target cells").
25
(Choice D) Rheumatoid arthritis causes chronic i nflammation and is a common cause of anemia of chronic disease. However, the serum ferritin
26
level is typically normal to elevated in anemia of chronic disease since it is an acute-phase reactant.
27
(Choice E) Vitamin 8 12 and folate deficiency anemias are usually macrocytic.
28
29
Educational objective:
30
Aln1ost all patients with serum ferritin concentrations of less than the traditional cutoff of 15 ng/ml are iron deficient. However, the sensitivity using
31
this cutoff is only modest at best and it cannot be used to exclude the diagnosis of iron deficiency since the majority of patients with a level of 15-
30 mg/nl are also iron deficient. The gastrointestinal tract is the major source of blood loss leading to iron deficiency anemia in males.
32
33
34
Foundations of Independent Practice
Hen1atology & Oncology
35
Subject
System
36
opyng
I@ ..JWorla
Iron deficiency anemia
Topic
Is
...
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
•
10
=
ltem23 of 39
Question Id: 6054
.~Mart<
\
<]
C>
~~
G)
il
'!,·
Previous
Next
Fun Screen
Tutorial
Lab varues
Notes
= ,
Calculator
Reverse Color
~
@
Text Zoom
Settings
11
•
12
r5l
Exhibit Display
13
•
•
14
~
6
17
18
19
20
21
22
25
26
27
28
29
30
31
32
33
34
35
©_
36
Zoom In
8_
Zoom Out
C
Reset
fl,
Add To Flash Card
37
· ~39
,
T
https://t.me/USMLEWorldStep3
~
9
•
10
11
•
•
The following vignette applies to the next 2 items.
12
13
A 62-year-old n1an comes to the community health center due to a "flaky and itchy" scalp. He is uncertain when the symptoms began and
14
believes his brother has a similar problem. The patient has not attempted any specific treatments but washes his hai r with a mild shampoo every
other day and washes his face with cold water once daily. Medical history is notable for coronary artery disease, type 2 diabetes mellitus, benign
.~
17
18
prostatic hyperplasia, and diverticulosis. The patient is a recovering alcoholic and has lived in a group home for the last 3 months. Vital signs are
normal. Physical examination shows oily skin with faint erythema and scaling of the scalp, eyebrows, and ears, as shown below. During the
course of the visit, the patient repeatedly scratches his head and eyebrows, but the remainder of the skin examination is normal.
19
20
21
22
25
26
27
28
29
30
31
32
33
34
35
36
37
. rsl
-~
https://t.me/USMLEWorldStep3
-
[M
9
•
10
11
•
12
13
•
•
14
~
6
17
18
19
20
21
'
22
25
26
27
28
29
30
31
32
33
34
Item 1 of 2
35
36
W hich of the following is the best initial treatment for this patient?
37
. rsl
-~
https://t.me/USMLEWorldStep3
151 -
-
[M
9
•
10
11
•
12
13
•
•
14
~
6
17
18
19
20
21
22
Item 1 of 2
25
Which of the following is the best initial treatment for this patient?
26
Q A. Oral griseofulvin
27
28
0
0
0
0
29
30
31
32
33
B.
Oral ketoconazole
C. Permelhrin cream
0 . Selenium sulfide shampoo
E.
Topical nystatin
34
35
Submit
36
37
-~
39
•
T
https://t.me/USMLEWorldStep3
151 -
-
[M
9
•
151 -
10
11
•
12
13
•
•
14
~
6
17
18
19
20
21
22
Item 1 of 2
25
Which of the following is the best initial treatment for this patient?
26
A. Oral griseofulvin (4%)
27
28
B. Oral ketoconazole (4°/o)
29
30
C. Permelhrin cream (6o/o)
31
0 . Selenium sulfide shampoo (80°/o)
32
E. Topical nystatin (4°/o)
33
34
35
36
Omitted
37
Correct answer
-~
39
•
-
T
TUTOR
11 .. 80%
L!!!. Answered correctly
fT\ 11 secs
\.::J Time Spent
https://t.me/USMLEWorldStep3
07/1 4/2020
• Last Updated
~
F2ck
SgJ2,d
Engock
9
•
= .
• -
10
•\
~
ltem23 of 39
Question Id: 6054
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
rim
Tutorial
Lab Yallles
Notes
Calculator
\.!..)
1111
;'
,
ffiffij
Reverse Color
~
~
~
~
Text Zoom
Settings
SgJ2,d
Eng ock
11
•
12
Seborrheic dermatitis in adults
13
•
•
14
Clinical features
~
• Erythematous, pruritic plaques w ith greasy scales
• Scalp, central face, ears, chest
6
17
Risk factors
18
•
Central nervous system disease (eg, Parkinson disease)
• HIV
• Topical antifungals (eg, seleni um sulfide, ketoconazole)
19
Treatment
20
• Topical glucocorticoids
• Topical calcineurin inhibitors (eg, pimecrolimus)
21
22
This patient's erythematous, scaly rash has the typical appearance of seborrheic dermatitis (SD). SD predominantly affects areas with heavy
concentrations of sebaceous glands, including the scalp (where it is referred to as "dandruff"), central face (eg, eyebrows, nasolabial folds), and
ears. In addition, SD may occasionally be seen on the chest, upper b ack, axilla, and ing uinal/pubic area. SD is most common in the first year of
25
life and again in adulthood . The diagnosis of SD is primarily clinical, with typical findings characterized by pruritic, erythematous plaques with
26
loose, greasy-looking scales.
27
Ma/assezia species may play a role in the pathogenesis of SD, and topical antifungal agents (eg , ketoconazole, selenium sulfide) are effective in
28
treating this condition. Other treatments that can be helpful include topical glucocorticoids, keratolytic agents (eg , salicylic acid), coal tar sh ampoo,
29
and topical calcineurin inhibitors (eg, pimecrolimus, tacrolimus).
30
31
(Choice A) Griseofulvin is used in tinea capitis, a derniatophyte infection most commonly seen in children, and tinea corporis, which causes
32
annular plaques with peripheral scaling and cen tral clearing. Griseofulvin is not effective against Ma/assezia species and can worsen SD.
33
(Choice B) Oral antifungals (eg, itraconazole, ketoconazole) are occasionally u sed in SD , but they are not first-line treatments and are u sed
34
primarily in severe, refractory cases.
35
(Choice C) Permethrin is used to treat scabies, which presents with intensely pruritic papules and vesicles between the fingers as well as on the
36
volar wrists, elbows, axillae, lower abdomen , or genitalia. Crusted scabies can cause large, scaly patches but is not pruritic and occurs most
37
-~
39
•
--- - --
T
TUTOR
-
- -
- -
- - ·- - - - - -
. -
- -- -
--
. - - - .
-
.
.
https://t.me/USMLEWorldStep3
~
F2ck
9
•
10
11
•
12
This patient's erythematous, scaly rash has the typical appearance of seborrheic dermatitis (SD). SD predominantly affects areas with heavy
13
•
concentrations of sebaceous glands, including the scalp (where it is referred to as "dandruff'), central face (eg, eyebrows, nasolabial folds), and
14
ears. In addition, SD may occasionally be seen on the chest, upper back, axilla, and inguinal/pubic area. SD is most common in the first year of
life and again in adulthood . The diagnosis of SD is primarily clinical, with typical findings characterized by pruritic, erythematous plaques with
.~
loose, greasy-looking scales.
17
Ma/assezia species may play a role in the pathogenesis of SD, and topical antifungal agents (eg , ketoconazole, selenium sulfide) are effective in
18
treating this condition. Other treatments that can be helpful include topical glucocorticoids, keratolytic agents (eg , salicylic acid), coal tar shampoo,
19
and topical calcineurin inhibitors (eg, pimecrolimus, tacrolimus).
20
21
(Choice A ) Griseofulvin is used in tinea capitis, a dermatophyte infection most commonly seen in children, and tinea corporis, which causes
22
annular plaques with peripheral scali ng and central clearing. Griseofulvin is not effective against Malassezia species and can worsen SD.
(Choice B) Oral antifungals (eg, itraconazole, ketoconazole) are occasionally used in SD, but they are not first-line treatments and are used
primarily in severe, refractory cases.
25
(Choice C) Permethrin is used to treat scabies, which presents with intensely pruritic papules and vesicles between the fingers as well as on the
26
volar wrists, elbows, axillae, lower abdomen , or genitalia. Crusted scabies can cause large, scaly patches but is not pruritic and occurs most
27
commonly in immunocompromised patients (eg , lymphoma, AIDS).
28
29
(Choice E) Topical nystatin is used primarily to treat intertrigo and other disorders caused by Candida species yeasts; it is not used in SD.
30
Educational objective:
31
Seborrheic dermatitis is characterized by erythematous plaques with loose, greasy-looking scales on the scalp ("dandruff'), central face, and ears.
32
Treatment options include topical antifungal agents (eg, ketoconazole, selenium sulfide), keratolytic agents (eg, salicylic acid), coal tar, topical
33
glucocorticoids, and topical calcineurin inhibitors (eg , pimecrolimus, tacrolimus).
34
References
35
• Diagnosis and treatment of seborrheic dermatitis.
36
37
-~
39
•
T
https://t.me/USMLEWorldStep3
-
[M
9
•
10
11
•
12
13
•
•
14
~
6
17
18
19
20
21
22
25
26
27
28
29
30
31
32
33
34
•
35
©_
36
ys em
37
· ~39
,
Zoom In
T
8_
Zoom Out
C
Reset
fl,
I
Add To Flash Card
op,c
https://t.me/USMLEWorldStep3
cil -
9
•
= .
• -
10
ltem 24of 39
Question Id: 6055
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
rim
Tutorial
Lab Yallles
Notes
Calculator
\.!..)
1111
;'
ffiffij
11
•
12
Item 2 of 2
13
•
•
The patient returns to the clinic after 4 weeks of treatment. His rash has nearly resolved , but he is concerned because his brother developed
14
recurrent symptoms after similar treatment. Which of the following is the most appropriate guidance for long-term management of this patient's
~
condition?
6
17
0
0
0
0
0
18
19
20
21
22
A. Avoiding contact with the offending agent is needed to prevent recurrence.
8. Clothing and bed linens should be laundered to eliminate the causative agent.
C. Household members should be treated to prevent relapse.
D. One course of treatment usually leads to long-lern1 remission.
E.
Weekly re-treatment may be needed to prevent recurrence.
25
Submit
26
27
28
29
30
31
32
33
34
35
36
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
= .
• -
10
•\
~
ltem 24of 39
Question Id: 6055
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
rim
Tutorial
Lab Yallles
Notes
Calculator
\.!..)
1111
;'
,
ffiffij
Reverse Color
~
~
~
~
Text Zoom
Settings
SgJ2,d
Eng ock
11
•
12
Item 2 of 2
13
•
•
The patient returns to the clinic after 4 weeks of treatment. His rash has nearly resolved , but he is concerned because his brother developed
14
recurrent symptoms after similar treatment. Which of the following is the most appropriate guidance for long-term management of this patient's
~
condition?
6
17
A. Avoiding contact with the offending agent is needed to prevent recurrence. ( 4% )
18
8 . Clothing and bed linens should be laundered to eliminate the causative agent. (10%)
19
20
C. Household m embers should be treated to prevent relapse. (4°/o)
21
D. One course of treatment usually leads to long-tern1 remission. (6°/o)
22
E. Weekly re-treatment may be needed to prevent recurrence. (74%)
25
26
Omitted
27
Correct answer
28
E
11 .. 74%
L!!!. Answered correcl!y
(T\ 02 secs
~ Time Spent
07/1 4/2020
• Last Updated
29
30
Explanation
31
32
Seborrheic dermatitis (SD) is a chronic, relapsing condition. Initial treatment can provide significant improvement in symptoms but is rarely
33
adequate to induce long-term remission (Choice D). As a result, p atients usually benefit from intermittent re-treatment. Typical regimens include
34
topical ketoconazole or ciclopirox every 1-2 weeks.
35
(Choi ce A ) Contact dermatitis usually presents with pruritic vesicles, papules, or plaques on exposed skin. Distribution typically follows
36
characteristic patterns depending on the causative agent (eg, linear streaks on the legs in poison ivy dermatitis). SD is not triggered by contact
37
-~
39
•
..
T
TUTOR
·-·-·
..
--~https://t.me/USMLEWorldStep3
~
F2ck
9
•
= .
• -
10
ltem 24of 39
Question Id: 6055
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
11111
;'
rim
ffiffij
Calculator
11
•
../ '
12
E . Weekly re-treatment may be needed to prevent recurrence. (74o/o)
13
•
•
14
~
Omitted
Correct answer
6
E
17
Iii, 74%
l!!!. Answered correcUy
(i\ 02 secs
\.::J
Time Spent
~
07/1 4/2020
!=I Last Updated
18
19
Explanation
20
21
Seborrheic dermatitis (SD) is a chronic, relapsing condition. Initial treatment can provide significant improvement in symptoms but is rarely
22
adequate to induce long-term remission (Choice D). As a result, patients usually benefit from intermittent re-treatment. Typical regimens include
topical ketoconazole or ciclopirox every 1-2 weeks.
(Choice A) Contact dermatitis usually presents with pruritic vesicles, papules, or plaques on exposed skin. Distribution typically follows
25
characteristic patterns depending on the causative agent (eg, linear streaks on the legs in poison ivy dermatitis). SD is not triggered by contact
26
with an external irritant or allergen.
27
(Choices B and C) Management of scabies requires the treatment of household contacts, as well as the laundering of bedding and clothing.
28
These measures are not effective in SD.
29
Educational objective:
30
Seborrheic dermatitis is a chronic, relapsing condition. Initial treatment can provide significant improvement in symptoms, but patients usually
31
benefit from intermittent re-treatment.
32
33
34
Foundations of Independent Practice
Dermatology
Seborrheic dermatitis
35
Subject
System
Topic
36
C
I@
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
= .
• -
10
ltem 25of 39
Question Id: 5486
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
Lab Yallles
m,
;'
Notes
rim
ffiffij
Calculator
11
•
•
•
12
A 13-year-old boy is brought to the office for an itchy rash he developed yesterday during a camping trip with his father. The rash started on his
13
legs and spread to his arm this morning. His father developed a similar rash on his legs and face. They came to the office immediately after
14
returning early from the trip due to the boy's pain and intense itching. The patient's father applied topical diphenhydramine, which did not provide
~
relief. He has no other medical issues and takes no other medications. Other than a family trip to Eu rope last month, the patient has not traveled
6
out of the United States. Physical examination shows an uncomfortable-appearing boy. Scattered areas of erythematous papules are present on
17
the right arm, with several overlying vesicles filled w ith clear fluid. Many linear erythematous lesions are also found on the anterior lower
18
extremities, some of which have vesicles oozing a serous fluid. Which of the following is the best recommendation for reducing the spread of this
19
patient's condition?
20
Q
Q
Q
Q
Q
21
22
23
24
26
A. Begin topical antibiotic therapy
B. Prescribe oral ivermectin for patient and household contacts
C. Promptly ad minister oral antihistamines
D. Remove contaminated apparel
E. Treat infected bedding with insecticide
27
28
29
Submit
30
31
32
33
34
35
36
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
10
= .
• -
ltem 25of 39
Question Id: 5486
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
1111
;'
rim
ffiffij
Calculator
11
•
•
•
12
A 13-year-old boy is brought to the office for an itchy rash he developed yesterday during a camping trip with his father. The rash started on his
13
legs and spread to his arm this morning. His father developed a similar rash on his legs and face. They came to the office immediately after
14
returning early from the trip due to the boy's pain and intense itching. The patient's father applied topical diphenhydramine, which did not provide
~
6
relief. He has no other medical issues and takes no other medications. Other than a family trip to Eu rope last month, the patient has not traveled
out of the United States. Physical examination shows an uncomfortable-appearing boy. Scattered areas of erythematous papules are present on
17
the right arm, with several overlying vesicles filled w ith clear fluid. Many linear erythematous lesions are also found on the anterior lower
18
extremities, some of which have vesicles oozing a serous fluid. Which of the following is the best recommendation for reducing the spread of this
19
patient's condition?
20
A. Begin topical antibiotic therapy (3o/o)
21
22
B. Prescribe oral ivermectin for patient and household contacts (5%)
23
C. Promptly ad minister oral antihistamines (13%)
24
D. Remove contaminated apparel (75%)
26
E. Treat infected bedding with insecticide (1%}
27
28
29
30
31
Omitted
Correct answer
D
I11.
I.!!!..
75%
Answered correctty
, i \ 03 secs
I...::) nme Spent
32
33
34
Explanation
35
36
37
. rsl
-~
https://t.me/USMLEWorldStep3
03/07/2020
• Last Updated
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
10
•
=
ltem25of39
Question Id: 5486
.~Mart<
\
<]
C>
~~
G)
il
'!,·
Previous
Next
Fun Screen
Tutorial
Lab varues
Notes
11
•
12
13
•
•
14
~
6
17
18
19
20
21
22
23
24
26
27
28
29
30
31
32
33
34
35
36
37
. rsl
-~
https://t.me/USMLEWorldStep3
= ,
Calculator
Reverse Color
~
@
Text Zoom
Settings
-
[M
9
•
10
11
•
12
13
•
•
14
~
6
17
18
19
20
21
22
23
24
26
27
28
29
30
31
32
Poison ivy contact d ermatitis is a type IV (cell-mediated) hypersensitivity reaction that classically presents with linear papules and clear, fluid-
33
filled vesicles on exposed areas. Pain and intense pruritus are typical. Nonlinear lesions can also be present from subsequent spread via
34
contact with residual plant resin on contaminated clothing. Immediate rem oval of contaminated apparel and gentle cleansing of exposed areas
35
are recommended to mi nimize spread of dermatitis.
36
Treatment is supportive (eg, cool compress, topical corticosteroids). Oral corticosteroids are indicated in severe dermatitis or dermatitis involving
37
. rsl
-~
https://t.me/USMLEWorldStep3
151 -
--
9
•
10
11
•
•
Item 25 of 39
• ?' Mart<
Question Id: 5486
<l
Previous
·=-
'C
11-
r,
C>
.,
-
L .J
Fun Screen
Next
G)
Tutorial
i
l
Lab varues
Ii!,·
Notes
=
Calculator
12
Poison ivy contact d ermatitis is a type IV (cell-mediated) hypersensitivity reaction that classically presents with linear papules and clear, fluid-
13
filled vesicles on exposed areas . Pain and intense pruritus are typical. Nonlinear lesions can also be present from subsequent spread via
14
contact with resid ual plant resin on contaminated clothi ng. Immediate removal of contaminated apparel and gentle cleansing of exposed areas
.~
are recommended to mi nimize spread of dermatitis.
Treatment is supportive (eg, cool compress, topical corticosteroids). Oral corticosteroids are indicated in severe dermatitis or dermatitis involving
17
the face or genitalia to reduce inflammation. Antihistamines (eg, diphenhydramine) are not effective as the pruritus in poison ivy dermatitis is not
18
histamine-mediated (Choice C).
19
(Choice A) Topical antibiotic therapy is indicated for bacterial superinfection of poison ivy contact dermatitis . Presentation includes honey-crusted
20
lesions or an exudative discharge. This patient's vesicles are filled with clear fluid and oozing serous fluid.
21
22
(Choice B) Oral ivermectin is the treatment for scabies, which also presents w ith an intensely pruritic rash. Distribution of the rash, however,
23
classically involves the web spaces of the hands and feet, axillary folds, and genitalia.
24
(Choice E) Insecticides are indicated in the management of bedbug infestation. Presentation includes small (2-3 mm) erythematous papules,
often in a linear pattern, on exposed areas. Pruritus is common, but pain and vesicular lesions are atypical. In addition, this patient's recent
26
camping history makes poison ivy contact dermatitis more likely.
27
Educational objective :
28
Poison ivy contact dermatitis presents as pruritic, li near papules and/or vesicles on exposed areas. Reduction of spread is achieved by avoiding
29
both direct (eg, skin-to-plant contact) and indirect (eg, clothing) exposure to the allergen.
30
References
31
• Diagnosis and management of contact dermatitis.
32
33
34
Foundations of Independent Practice
Dermatology
Contact dermatitis
35
Subject
System
Topic
36
C
AD
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
•
AA
Text Zoom
X
®
Settings
9
•
= .
• -
10
ltem26 of 39
Question Id: 10009
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
Lab Yallles
m,
rim
Notes
Calculator
;'
ffiffij
11
•
•
•
12
A 43-year-old woman comes to the physician for a rash on her hands. The rash began 8-1 0 weeks ago. She n1oved to the community
13
approximately 4 months ago and works as a nurse in the dialysis unit at a nearby hospital. The patient's past medical history is significant for
14
hypertension treated with hydrochlorothiazide. She also takes naproxen regularly for headaches. Her hands are shown in the image below:
~
Which of the following is the most likely diagnosis?
6
17
Q
Q
Q
Q
Q
18
19
20
21
22
~
A. Contact dermatitis
B. Phototoxic dermatitis
C. Psoriasis
D. Scabies
E. Tinea manuun1
4
25
Submit
27
28
29
30
31
32
33
34
35
36
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
= .
• -
10
ltem26 of 39
Question Id: 10009
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
Lab Yallles
m,
rim
Notes
Calculator
;'
ffiffij
11
•
•
•
12
A 43-year-old woman comes to the physician for a rash on her hands. The rash began 8-1 0 weeks ago. She n1oved to the community
13
approximately 4 months ago and works as a nurse in the dialysis unit at a nearby hospital. The patient's past medical history is significant for
14
hypertension treated with hydrochlorothiazide. She also takes naproxen regularly for headaches. Her hands are shown in the image below:
~
6
17
18
19
20
21
22
~
4
25
27
28
29
30
31
32
33
Which of the following is the most likely diagnosis?
34
Q
35
36
( ) B. Phototoxic dermatitis
37
-~
39
•
A. Contact dermatitis
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
10
11
•
12
13
•
14
-~
17
18
19
20
21
22
1231
~
25
Which of the following is the most likely diagnosis?
Q A. Contact dermatitis
27
28
0
0
0
0
29
30
31
32
33
B.
Phototoxic dermatitis
C. Psoriasis
0 . Scabies
E.
nnea manuum
34
35
Submit
36
37
-~
39
•
T
https://t.me/USMLEWorldStep3
9
•
10
11
•
12
13
•
14
-~
17
18
19
20
21
22
1231
~
25
Which of the following is the most likely diagnosis?
27
A. Contact dermatitis {67o/o)
28
B.
Phototoxic dermatitis (8%)
29
30
C. Psoriasis (2°A.)
31
0 . Scabies (1°/o)
32
E.
33
nnea manuum (21 %)
34
35
36
Omitted
37
Correct answer
-~
39
•
T
11 .. 67%
L!!!. Answered correctly
IT\
\.::J
16 secs
Time Spent
https://t.me/USMLEWorldStep3
03/26/2020
• Last Updated
9
•
= .
• -
10
•\
~
ltem26 of 39
Question Id: 10009
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
Lab Yallles
m,
rim
Notes
Calculator
;'
,
ffiffij
Reverse Color
~
~
Text Zoom
~
~
Settings
11
•
•
•
12
This patient has typical features of irritant contact dermatitis (ICD). Clinical findings characteristic of ICD include pruritus, erythema, and scaling of
13
the skin. As symptoms become chronic, hyperkeratosis and painful fissuring are also commonly seen. Symptoms are often worst where skin is
14
the thinnest, at the dorsum of the hands, fingertips, and finger webs. The diagnosis is primarily clinical , but patch testing to rule out allergic
~
dermatitis may be useful on occasion.
6
ICD is the cause of 80°/o of all cases of occupational hand dermatitis. It is due to repeated exposure to irritants (eg, detergents, solvents, oxidizing
17
agents) over time and may occur after days, weeks, or months of exposure to the irritant. ICD is especially common in patients with underlying
18
atopic dermatitis and in health care workers who use occlusive gloves frequently.
19
Other causes of hand dermatitis with similar features include allergic contact dermatitis, which is immune n1ediated, and dyshidrotic eczema,
which is characterized by vesicular lesions involving the palms and soles. In practice, all of these disorders are initially managed in similar fashion
20
21
with:
22
~
• Identification and avoidance of the offending agents
• Washing hands with lukewarm water and mild cleansers
4
• Frequent use of emollients
• Topical glucocorticoids
25
27
(Choice B) Phototoxic dermatitis can be induced by systemic medications such as diuretics, antibiotics, nonsteroidal anti-inflammatory drugs, and
28
various other drugs. The reaction consists of erythema with or without bullae and vesiculation over sun-exposed areas such as the dorsal hands,
29
forearms, upper chest, and face.
30
(Choice C) Psoriasis is an inflamn1atory disorder characterized by localized plaques with erythen1a and scaling. It may involve the hands, but is
31
most common at the extensor surfaces of the elbows and knees.
32
33
(Choice D) Scabies manifests with pruritic papules, possibly with an associated scale and thin linear burrows, in the finger webs, lateral palms,
34
wrists, ankles, and genital region.
35
(Choice E) linea manuum causes annular erythema with a trailing scale on the dorsal or ventral hands. Mild itching is typically present.
36
Classically only one hand is involved, although tinea pedis is often present as well.
37
-~
39
•
~
T
TUTOR
-·
--·
-
https://t.me/USMLEWorldStep3
~
F2ck
SgJ2,d Eng ock
9
•
•
10
=
ltem26of39
.~Mart<
Question Id: 10009
\
<]
C>
~~
G)
il
'!,·
Previous
Next
Fun Screen
Tutorial
Lab varues
Notes
= ,
Calculator
Reverse Color
~
@
Text Zoom
Settings
11
•
12
13
•
•
14
~
6
17
18
19
20
21
22
~
4
25
27
28
29
30
31
32
33
34
35
©_
36
37
· ~39
,
~
T
TUTOR
..
..
~
Zoom In
8_
Zoom Out
C
Reset
l?,
Add To New Card
I Existing Card
-
https://t.me/USMLEWorldStep3
~
F2ck
SgJ2,d Eng ock
9
•
•
10
=
ltem26of39
.~Mart<
Question Id: 10009
\
<]
C>
~~
G)
il
'!,·
Previous
Next
Fun Screen
Tutorial
Lab varues
Notes
= ,
Calculator
Reverse Color
~
@
Text Zoom
Settings
11
•
12
13
•
•
14
~
6
17
18
19
20
21
22
~
4
25
27
28
29
30
31
32
33
34
35
©_
36
37
· ~39
,
~
T
TUTOR
..
..
~
Zoom In
8_
Zoom Out
C
Reset
l?,
Add To New Card
I Existing Card
-
https://t.me/USMLEWorldStep3
~
F2ck
SgJ2,d Eng ock
9
•
•
10
=
ltem26of39
.~Mart<
Question Id: 10009
\
<]
C>
~~
G)
il
'!,·
Previous
Next
Fun Screen
Tutorial
Lab varues
Notes
= ,
Calculator
Reverse Color
~
@
Text Zoom
Settings
11
•
12
13
•
•
14
~
6
17
18
19
20
21
22
~
4
25
27
28
29
30
31
32
33
34
35
©_
36
37
· ~39
,
~
T
TUTOR
..
..
~
Zoom In
8_
Zoom Out
C
Reset
l?,
Add To New Card
I Existing Card
-
https://t.me/USMLEWorldStep3
~
F2ck
SgJ2,d Eng ock
9
•
•
10
=
ltem26of39
.~Mart<
Question Id: 10009
\
<]
C>
~~
G)
il
'!,·
Previous
Next
Fun Screen
Tutorial
Lab varues
Notes
= ,
Calculator
Reverse Color
~
@
Text Zoom
Settings
11
•
12
13
•
•
14
~
6
17
18
19
20
21
22
~
4
25
27
28
29
30
31
32
33
34
35
©_
36
37
· ~39
,
~
T
TUTOR
..
..
~
Zoom In
8_
Zoom Out
C
Reset
l?,
Add To New Card
I Existing Card
-
https://t.me/USMLEWorldStep3
~
F2ck
SgJ2,d Eng ock
9
•
•
10
=
ltem26of39
.~Mart<
Question Id: 10009
\
<]
C>
~~
G)
il
'!,·
Previous
Next
Fun Screen
Tutorial
Lab varues
Notes
= ,
Calculator
Reverse Color
~
@
Text Zoom
Settings
11
•
12
13
•
•
14
~
6
17
18
19
20
21
22
~
4
25
27
28
29
30
31
32
33
34
35
©_
36
37
· ~39
,
~
T
TUTOR
..
..
~
Zoom In
8_
Zoom Out
C
Reset
l?,
Add To New Card
I Existing Card
-
https://t.me/USMLEWorldStep3
~
F2ck
SgJ2,d Eng ock
9
•
•
10
=
ltem26of39
.~Mart<
Question Id: 10009
\
<]
C>
~~
G)
il
'!,·
Previous
Next
Fun Screen
Tutorial
Lab varues
Notes
= ,
Calculator
Reverse Color
~
@
Text Zoom
Settings
11
•
12
r5l
Exhibit Display
~
13
•
•
14
~
6
17
18
19
20
21
22
~
4
25
27
28
29
30
31
32
33
34
35
©_
36
37
· ~39
,
~
T
TUTOR
..
..
~
Zoom In
8_
Zoom Out
C
Reset
l?,
Add To New Card
I Existing Card
-
https://t.me/USMLEWorldStep3
~
F2ck
SgJ2,d Eng ock
9
•
•
10
=
ltem26of39
Question Id: 10009
.~Mart<
\
<]
C>
~~
G)
il
'!,·
Previous
Next
Fun Screen
Tutorial
Lab varues
Notes
11
•
12
13
•
•
14
~
6
17
18
19
20
21
22
~
4
25
27
28
29
30
31
32
33
34
35
©_
36
Zoom In
8_
Zoom Out
C
Reset
l?,
Add To New Card
37
· ~39
,
T
https://t.me/USMLEWorldStep3
I Existing Card
= ,
Calculator
Reverse Color
~
@
Text Zoom
Settings
9
•
= .
• -
10
ltem 27of 39
Question Id: 4968
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
Lab Yallles
m,
rim
Notes
Calculator
;'
ffiffij
11
•
12
A 42-year-old Caucasian woman comes to the physician because of "patchy hair loss" for the past six weeks. Her other n1edical problems include
13
•
•
hypothyroidism, gastroesophageal reflux disease, and bipolar disorder. She has smoked one pack of cigarettes daily for the past 15 years. She
14
drinks 1-2 ounces of alcohol daily, and is a vegetarian. Her mother has thyroid disease, bipolar disorder and breast cancer. The patient's
~
medications include lansoprazole, L-thyroxine and valproic acid. On physical examination, her vital signs are within normal limits. Scalp exa m
6
reveals several well-demarcated circular areas of complete hair loss. Fingernail pitting is also present. Which of the following is the most likely
17
cause of her hair loss?
18
19
20
21
22
~
4
25
Q
A. Alopecia areata
0
0
0
0
B.
Medication side effect
C. Psoriasis
D. nnea capitis
E. Trichotillomania
26
Submit
28
29
30
31
32
33
34
35
36
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
= .
• -
10
•\
~
ltem 27of 39
Question Id: 4968
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
•!
1111
I'>\
\.!..)
Tutorial
Lab Yallles
m,
;'
Notes
rim
,
ffiffij
Calculator
Reverse Color
~
~
~
~
Text Zoom
Settings
SgJ2,d
Engock
11
•
12
A 42-year-old Caucasian woman comes to the physician because of "patchy hair loss" for the past six weeks. Her other n1edical problems include
13
•
•
hypothyroidism, gastroesophageal reflux disease, and bipolar disorder. She has smoked one pack of cigarettes daily for the past 15 years. She
14
drinks 1-2 ounces of alcohol daily, and is a vegetarian. Her mother has thyroid disease, bipolar disorder and breast cancer. The patient's
~
medications include lansoprazole, L-thyroxine and valproic acid. On physical examination, her vital signs are within normal limits. Scalp exa m
6
reveals several well-demarcated circular areas of complete hair loss. Fingernail pitting is also present. Which of the following is the most likely
17
cause of her hair loss?
18
19
A. Alopecia areata ( 49°/o)
20
B.
21
Medication side effect (13%)
C. Psoriasis (20%)
22
~
D. nnea capitis (7%)
4
E. Trichotillomania (9°/o)
25
26
28
Omitted
29
Correct answer
A
30
Ii..
I.ill..
49%
Answered correctly
~
ri', 03 secs
\..::J
06/11/2020
13 Last Updaled
Time Spent
31
32
Explanation
33
34
Alopecia areata is a type of non-scarring hair loss that can affect any hai r-bearing area. It is thought to be an autoimmune process that targets
35
genetically predisposed individuals. The classic clinical description is of a well-demarcated , often round, non-scarred patch of complete hair loss.
36
The presence of so-called "exclamation point hairs" (hairs which are tapered near the insertion into the scalp}, especially at the periphery of an
37
-~
39
•
--- - - T
TUTOR
-- ----- -----····. - ·- -- - . - --- ...
- - . - -----.
https://t.me/USMLEWorldStep3
~
-- ----.
-- .
~
F2ck
9
•
10
11
•
•
•
12
= .
• -
ltem 27of 39
Question Id: 4968
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
rim
Tutorial
Lab Yallles
Notes
Calculator
\.!..)
1111
;'
ffiffij
Alopecia areata is a type of non-scarring hair loss that can affect any hair-bearing area. It is thought to be an autoimmune process that targets
genetically predisposed individuals. The classic clinical description is of a well-demarcated, often round, non-scarred patch of complete hair loss.
13
The presence of so-called "exclamation point hairs" {hairs which are tapered near the insertion into the scalp), especially at the periphery of an
14
alopecic plaque, is considered pathognomonic of, but not necessary for, the diagnosis. Areas of involvement may be single or multiple. Nail
~
6
17
18
19
20
pitting is a commonly associated finding. The affected areas of skin are typically asymptomatic, but the disease can be emotionally traumatic and
socially stigmatizing. Alopecia areata is often self-li mited, but may be relapsing and remitting or chronic and progressive. Patients with alopecia
areata are at increased risk for other autoimmune conditions including autoimmune thyroid disease, vitiligo, and pernicious anemia.
(Choice B) Certain medications may cause hair loss via a telogen or anagen effluvium. Medication-related hair loss typically n1anifests as diffuse
non-scarring thinning, rather than as discrete bald patches. Telogen effluvium usually begins about 3 months after some precipitating event, such
as an illness, stressor, or new medication . Beta-blockers, anti-coagulants, systemic retinoids, anti-convulsants, and anti-thyroid medications are
21
frequently impl icated causes of telogen effluvium. Chemotherapeutics {e.g. antimetabolites, alkylating agents, mitotic inhibitors) can cause
22
anagen effluvium, which usually begins w ithin 1-2 weeks of chemotherapy initiation.
~
4
25
26
(Choice C) Psoriasis is a chronic inflammatory skin disorder characterized by well-demarcated erythematous plaques with silvery scale. The
extensor extremities, periumbilical area, gluteal cleft, lumbosacral area, and scalp are among the areas n1ost commonly involved . Associated hair
loss is usually minimal. Nail changes are common in psoriasis and may include pitting, onycholysis, as well as thickening and yellowing of the nail
plate.
28
(Choice D) Tinea capitis is a dermatophyte infection of the scalp that affects children most commonly. Trichophyton tonsurans and Microsporum
29
canis are the most common causes of tinea capitis in the United States. The clinical presentation varies by causative organism, but may consist
30
31
32
of erythema, scaling, "black dot" alopecia {secondary to breakage of hairs near the scalp), pustules, or boggy plaques with posterior cervical or
posterior auricular lymphadenopathy. While patchy or diffuse alopecia is common, the accompanying inflammation , scale, and lymphadenopathy
are typically sufficient to distinguish tinea capitis from alopecia areata .
33
(Choice E) Trichotillomania is a psychiatric impulse control disorder where hai rs are plucked, twisted, or otherwise broken from the scalp. On
34
physical exami nation, irregularly shaped areas of hair loss containing hairs of many different lengths are typical.
35
36
Educational objective :
The classic presentation of alopecia areata consists of well-demarcated, non-scarred, round patches of hair loss, which may have "exclamation
37
. rsl
-~
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
= .
• -
10
Question Id: 4968
11
•
•
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
rim
Tutorial
Lab Yallles
Notes
Calculator
\.!..)
1111
;'
ffiffij
as an illness, stressor, or new medication. Beta-blockers, anti-coagulants, systemic retinoids, anti-convulsants, and anti-thyroid medications are
12
frequently implicated causes of telogen effluvium. Chemotherapeutics (e.g. anti metabolites, alkylating agents, mitotic inhibitors) can cause
13
•
ltem 27of 39
anagen effluvium, which usually beg ins w ithin 1-2 weeks of chemotherapy in itiation.
14
~
(Choice C) Psoriasis is a chronic inflammatory skin disorder characterized by well-demarcated erythematous plaques with silvery scale. The
extensor extremities, periumbilical area, gluteal cleft, lumbosacral area, and scalp are among the areas most commonly involved . Associated hair
6
loss is usually minimal. Nail changes are common in psoriasis and may include pitting, onycholysis, as well as thickening and yellowing of the nail
17
plate.
18
19
(Choice D) Tinea capitis is a dermatophyte infection of the scalp that affects children most commonly. Trichophyton tonsurans and Microsporum
20
canis are the most common causes of tinea capitis in the United States. The clinical presentation varies by causative organism, but may consist
21
of erythema, scaling, "black dot" alopecia (secondary to breakage of hairs near the scalp}, pustules, or boggy plaques with posterior cervical or
22
posterior auricular lymphadenopathy. While patchy or diffuse alopecia is common, the accompanying inflammation , scale, and lymphadenopathy
~
are typically sufficient to distinguish tinea capitis from alopecia areata.
4
(Choice E) Trichotillomania is a psychiatric impulse control disorder where hairs are plucked, twisted, or otherwise broken from the scalp. On
25
physical examination, irregularly shaped areas of hair loss containing hairs of many different lengths are typical.
26
Educational objective :
The classic presentation of alopecia areata consists of w ell-demarcated, non-scarred, round patches of hair loss, which may have "exclamation
28
point'' hairs. Affected patients are more likely to have a personal or family history of other autoimmune conditions, including autoimmune thyroid
29
disease, pernicious anemia, and vitiligo.
30
References
31
• Diagnosing and treating hair loss.
32
33
34
Foundations of Independent Practice
Dermatology
Hair loss
35
Subject
System
Topic
36
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
= .
• -
10
ltem28of 39
Question Id: 12614
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
Lab Yallles
m,
;'
Notes
rim
ffiffij
Calculator
11
•
•
•
12
A 3-year-old boy is brought to the office due to ear drainage. His mother reports that he was well until the previous day, when he developed a
13
fever of 38.9 C (1 02 F), accompanied by crankiness, decreased appetite, and frequent crying. He w as given acetaminophen for his sympton1s,
14
but they did not improve. Today his mother put him in his roon1 for a nap; when she returned, thick w hite liquid was leaking from his right ear.
~
Since waking from his nap, he has not been cranky, but the drainage has persisted . Temperature is 38.3 C (101 F), pulse is 114/min, and
6
respirations are 18/n1in. On physical examination, he appears alert and active. The pupils are equal and reactive; the nasal turbi nates are clear,
17
and there is no erythema or exudate in the pharynx. The left tympanic membrane is normal, but the right tympanic membrane is not visible due to
18
copious purulent drainage in the canal. The pinna appears norn1al and there is no tenderness on manipulation of the ear. The neck is supple
19
without lymphadenopathy. Cardiopulmonary examination is within normal limits. W hat is the most likely explanation for this patient's findings?
20
0
0
0
0
0
21
22
~
4
25
26
27
29
A. Bacterial otitis externa
B. Necrotizing otitis externa
C. Serous otitis media
D. Superinfected foreign body
E.
Suppurative otitis media
Submit
30
31
32
33
34
35
36
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
= .
• -
10
ltem28of 39
Question Id: 12614
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
Lab Yallles
m,
;'
Notes
rim
ffiffij
Calculator
11
•
•
•
12
A 3-year-old boy is brought to the office due to ear drainage. His mother reports that he was well until the previous day, when he developed a
13
fever of 38.9 C (1 02 F), accompanied by crankiness, decreased appetite, and frequent crying. He w as given acetaminophen for his sympton1s,
14
but they did not improve. Today his mother put him in his roon1 for a nap; when she returned, thick w hite liquid was leaking from his right ear.
~
Since waking from his nap, he has not been cranky, but the drainage has persisted . Temperature is 38.3 C (101 F), pulse is 114/min, and
6
respirations are 18/n1in. On physical examination, he appears alert and active. The pupils are equal and reactive; the nasal turbi nates are clear,
17
and there is no erythema or exudate in the pharynx. The left tympanic membrane is normal, but the right tympanic membrane is not visible due to
18
copious purulent drainage in the canal. The pinna appears norn1al and there is no tenderness on manipulation of the ear. The neck is supple
19
without lymphadenopathy. Cardiopulmonary examination is within normal limits. What is the most likely explanation for this patient's findings?
20
A. Bacterial otitis externa (13o/o)
21
22
B. Necrotizing otitis externa (1% )
~
C. Serous otitis media (6%)
4
25
D. Superinfected foreign body (13°,{,)
26
E. Suppurative otitis media (64%)
27
29
Omitted
30
Correct answer
31
E
111.
I.!!!..
64%
, i \ 02 secs
Answered correctty
I...::) nme Spent
32
33
Explanation
34
35
36
Perforated otitis media
37
-~
39
•
T
https://t.me/USMLEWorldStep3
03/06/2020
• Last Updated
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
= .
• -
10
ltem28of 39
Question Id: 12614
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
1111
;'
rim
,
ffiffij
Calculator
Reverse Color
~
~
~
~
Text Zoom
Settings
SgJ2,d
Eng ock
11
•
Perforated otitis media
12
13
•
•
14
~
6
17
18
19
20
21
22
~
4
25
26
27
29
30
31
32
©UWorld
33
34
This patient had fever and crankiness followed by purulent drainage from his ear. The tympanic membrane is obscured by otorrhea, and there is
35
no tenderness to manipulation of the pinna. This is a classic presentation of suppurative otitis media (also called acute otitis media or
36
bacterial otitis media) with tympanic membrane perforation.
37
· ~39
,
'
T
TUTOR
https://t.me/USMLEWorldStep3
~
F2ck
9
•
10
11
•
12
bacterial otitis media) with tympanic membrane perforation.
13
•
14
Suppurative otitis n1edia occurs when fluid in the middle ear cavity is infected by bacteria from the nasopharynx. Infection creates pressure on the
tympanic membrane, causing it to bulge. If the condition is untreated, in some cases the pressure will cause the membrane to rupture, leaking
.~
purulent fluid. Often (as in this case), membrane rupture relieves pressure and some of the patient's pain, with improvement in symptoms such as
17
crankiness. Tympanic membrane perforation can occur during an episode of otitis media caused by any organism, but it is most common in those
18
caused by group A Streptococcus .
19
(Choice A) Bacterial otitis externa is an infection of the outer auditory canal usually caused by Pseudomonas aeruginosa. Although it does result
20
in ear pain and purulent ear drainage, fever is generally absent, pain on manipulation of the ear is almost alw ays present, and episodes generally
21
follow water exposure.
22
~
(Choice B) Necrotizing ("malignant") otitis externa is an aggressive Pseudomonas infection of the external ear canal that invades the neighboring
skull bone. Fever, pain, and purulent drainage are expected; however, this diagnosis occurs almost exd usively in elderly patients with diabetes
and in immunocompromised individuals.
25
26
(Choice C) Serous otitis media occu rs when an effusion is present in the middle ear canal in the absence of infection and inflammation. It
27
typically follows episodes of suppurative otitis media, but it is not associated with fever, pain , crankiness, tympanic membrane rupture, or purulent
drainage.
29
(Choice D) An otic foreign body may be encountered in young children (age <6) and may present with ear drainage; however, superinfection and
30
fever are uncommon, copious drainage is rare, and the object is typically visualized on otoscopic exami nation .
31
Educational objective :
32
Suppurative otitis media is typically accompanied by fever, pain, and crankiness, and if untreated can be followed by tympanic membrane
33
perforation, acute purulent otorrhea in the external auditory canal . and reduction in pain after membrane rupture. Pain is usually absent on
34
manipulation of the pinna.
35
36
Fou ndations of Independent Practice
37
-~
39
•
T
Ear, Nose & Throat (ENT)
Otitis media
https://t.me/USMLEWorldStep3
9
•
= .
• -
10
Question Id: 12614
11
•
•
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
;'
ffiffij
Calculator
tympanic membrane, causing it to bulge. If the condition is untreated, in some cases the pressure will cause the membrane to rupture, leaking
purulent fluid. Often (as in this case), membrane rupture relieves pressure and some of the patient's pain, with improvement in symptoms such as
14
crankiness. Tympanic membrane perforation can occur during an episode of otitis media caused by any organism, but it is most common in those
~
caused by group A Streptococcus.
6
(Choice A ) Bacterial otitis extema is an infection of the outer auditory canal usually caused by Pseudomonas aeruginosa. Although it does result
17
in ear pain and purulent ear drainage, fever is generally absent, pain on manipulation of the ear is almost alw ays present, and episodes generally
18
follow water exposure.
19
20
(Choice B) Necrotizing ("n1alignant") otitis externa is an aggressive Pseudomonas infection of the external ear canal that invades the neighboring
21
skull bone. Fever, pain, and purulent drainage are expected; however, this diagnosis occurs almost exd usively in elderly patients with diabetes
22
and in immunocompromised individuals.
~
(Choice C) Serous otitis media occurs when an effusion is present in the middle ear canal in the absence of infection and inflammation. It
4
typically follows episodes of suppurative otitis media, but it is not associated with fever, pain , crankiness, tympanic membrane rupture, or purulent
25
drainage.
26
(Choice D) An otic foreign body may be encountered in young children (age <6) and may present w ith ear drainage; however, superinfection and
27
fever are uncommon, copious drainage is rare, and the object is typically visualized on otoscopic examination.
29
Educational objective:
30
Suppurative otitis media is typically accompanied by fever, pain, and crankiness, and if untreated can be followed by tympanic n1embrane
perforation, acute purulent otorrhea in the external auditory canal , and reduction in pain after membrane rupture. Pain is usually absent on
31
manipulation of the pinna.
32
33
34
Foundations of Independent Practice
Ear, Nose & Throat (ENT)
Otitis media
35
Subject
System
Topic
36
opyng
I@ .JWorid
Is
...
37
-~
39
•
1111
rim
Suppurative otitis media occurs when fluid in the middle ear cavity is infected by bacteria from the nasopharynx. Infection creates pressure on the
12
13
•
ltem28of 39
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
= .
• -
10
ltem28of 39
Question Id: 12614
•\
~
Mart<
<]
C>
Previous
Next
r,
I'>\
\.!..)
L .J
Fun Screen
Tutorial
•!
1111
Lab Yallles
11
•
12
13
•
•
14
Otitis media with effusion
~
6
17
18
19
20
21
22
~
4
25
26
27
29
30
31
32
33
34
© uw..1d
35
©_
36
Zoom In
8_
Zoom Out
C
Reset
fl,
Add To Flash Card
37
· ~39
,
T
https://t.me/USMLEWorldStep3
m,
;'
Notes
rim
ffiffij
Calculator
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
= .
• -
10
ltem 29of 39
Question Id: 621 4
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
rim
Tutorial
Lab Yallles
Notes
Calculator
\.!..)
1111
;'
ffiffij
11
•
•
•
12
A 60-year-old n,ale with hypertension and hypercholesterolemia comes for a follow-up visit. His blood pressure in the office is 160/ 100 mmHg,
13
and his readings are consistently elevated w hen he checks his blood pressure at home. An antihypertensive agent is added to his current
14
regimen . He takes a brief vacation in Florida, and calls after a few days because he has developed an erythematous rash on the exposed parts of
~
his body. Which of the following agents is most likely responsible for his rash?
6
0
0
0
0
0
17
18
19
20
21
22
~
A. Furosemide
B.
Hydrochlorothiazide
C. Lisinopril
D. Amlodipine
E. Metoprolol
4
25
Submit
26
27
28
30
31
32
33
34
35
36
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
= .
• -
10
ltem29of39
Question Id: 621 4
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
1111
rim
,
ffiffij
Calculator
;'
Reverse Color
~
~
~
~
Text Zoom
Settings
SgJ2,d
Engock
11
•
•
•
12
A 60-year-old n,ale with hypertension and hypercholesterolemia comes for a follow-up visit. His blood pressure in the office is 160/ 100 mmHg,
13
and his readings are consistently elevated w hen he checks his blood pressure at home. An antihypertensive agent is added to his current
14
regimen . He takes a brief vacation in Florida, and calls after a few days because he has developed an erythematous rash on the exposed parts of
~
his body. Which of the following agents is most likely responsible for his rash?
6
17
A. Furosemide (8o/o)
18
B.
Hydrochlorothiazide (45%)
19
C. Lisinopril (22%)
20
21
D. Amlodipine ( 18%)
22
E. Metoprolol ( 4%)
~
4
25
Omitted
26
111.
l!l!.
Correct answer
27
B
,i'\ 02 secs
45%
\::J
Answered correctly
Time Spent
F=! 06/11/2020
13 Last Updated
28
Explanation
30
31
32
The patient is likely to have a photosensitivity reaction, which is most commonly associated with the use of hydrochlorothiazide. Thiazides are
33
sulfonamides; therefore, these can cause photosensitivity or generalized dermatitis. Treatment of the rash includes discontinuation of
hydrochlorothiazide, use of sunscreen, and avoidance of sun exposure.
34
35
(Choice A) Furosemide can cause a Stevens-Johnson syndrome type of reaction that is seen w ith the use of sulfonamide antibiotics. Urticaria!
36
rash can also occur; however, furosemide is not usually recommended for the management of hypertension alone.
37
-~
39
•
.. ·T
TUTOR
---
.
.
.. . .
..
. ·-
-· - ·-···· .. .
... - -· .
https://t.me/USMLEWorldStep3
-
'.
.
..... -·
.
-·
~
F2ck
9
•
= .
• -
10
ltem 29of 39
Question Id: 621 4
•\
~
Mart<
<]
C>
Previous
Next
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
r,
L .J
Fun Screen
\.!..)
11111
;'
rim
ffiffij
Calculator
11
•
•
•
12
Omitted
13
Correct answer
14
B
~
6
fT\ 02 secs
111, 45%
l!!!.
~ Time Spent
Answered correcHy
~
06/11/2020
El Last Updated
Explanation
17
18
The patient is likely to have a photosensitivity reaction, which is most commonly associated with the use of hydrochlorothiazide. Thiazides are
19
sulfonamides; therefore, these can cause photosensitivity or generalized dermatitis. Treatment of the rash includes discontinuation of
20
hydrochlorothiazide, use of sunscreen, and avoidance of sun exposure.
21
(Choice A) Furosemide can cause a Stevens-Johnson syndrome type of reaction that is seen w ith the use of sulfonamide antibiotics. Urticaria!
22
rash can also occur; however, furosemide is not usually recommended for the management of hypertension alone.
~
(Choice C) lisinopril is an ACE inhibitor and can be associated with angioedema and urticaria. Photosensitivity rash is uncommon. Occasionally,
4
lisinopril can lead to aggravation of psoriatic rash .
25
26
(Choice D) Amlodipine therapy can be associated with significant fluid retention and urticaria! rash .
27
(Choice E) Metoprolol can cause urticaria in up to 5% of patients. Photosensitivity rash can occur, but it is much more uncommon compared to
28
hydrochlorothiazide.
Educational objective:
30
Thiazides are sulfonamides; therefore, hydrochlorothiazide use can cause photosensitivity rash, and treatment of this rash includes
31
discontinuation of the thiazide, use of sunscreen, and avoiding sun exposure.
32
33
34
Foundations of Independent Practice
Dermatology
Adverse drug reaction
35
Subject
System
Topic
36
C
I@
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
= .
• -
10
ltem 30of 39
Question Id: 16723
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
Lab Yallles
m,
;'
Notes
rim
ffiffij
Calculator
11
•
•
•
12
A 49-year-old w oman comes to the emergency department due to hearing loss. Upon awakeni ng this morning, she was unable to hear out of her
13
right ear. She also hears a loud ringing noise in her right ear. The patient has no ear pain or dizziness. This has never occurred before. She has
14
no other medical cond itions and takes no medications. Vital signs are within normal limits. On examination, the ear canals and tympanic
~
men1branes are clear. There is no middle ear effusion . Weber tuning fork examination lateralizes to the left. Air cond uction is greater than bone
6
conduction bilaterally. The remainder of the neurologic examination is normal. Which of the following is the most appropriate next step in
n1anagement of th is patient?
17
18
Q
Q
Q
Q
Q
19
20
21
22
~
4
A . Amoxicillin-clavulanic acid
B. Aural irrigation
C. Ciprofloxacin ear drops
D. Reassurance and follow-up in 6 weeks
E. Urgent otolaryngology evaluation
25
26
27
Submit
28
29
31
32
33
34
35
36
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
10
= .
• -
ltem 30of 39
Question Id: 16723
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
•!
1111
I'>\
\.!..)
Tutorial
Lab Yallles
m,
;'
Notes
rim
ffiffij
Calculator
11
•
•
•
12
A 49-year-old w oman comes to the emergency department due to hearing loss. Upon awakeni ng this morning, she was unable to hear out of her
13
right ear. She also hears a loud ringing noise in her right ear. The patient has no ear pain or dizziness. This has never occurred before. She has
14
no other medical cond itions and takes no medications. Vital signs are within normal limits. On examination, the ear canals and tympanic
~
6
17
men1branes are clear. There is no middle ear effusion . Weber tuning fork examination lateralizes to the left. Air cond uction is greater than bone
conduction bilaterally. The remainder of the neurologic examination is normal. Which of the following is the most appropriate next step in
n1anagement of th is patient?
18
A . Amoxicillin-clavulanic acid (1%)
19
20
B. Aural irrigation (9%)
21
C. Ciprofloxacin ear drops (0%)
22
~
D. Reassurance and follow-up in 6 weeks (25°/o)
4
E. Urgent otolaryngology evaluation (63o/o)
25
26
27
28
29
Omitted
Correct answer
E
07/04/2020
• Last Updated
(T'\ 01 sec
' "· 63%
I.!.!!..
Answered correctly
\.::) Time Spent
31
32
Explanation
33
34
35
36
Interpretation of Rinne & Weber tests
Rinne result
Weber result
37
. rsl
-~
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
= .
• -
10
•\
~
ltem 30of 39
Question Id: 16723
Mart<
<]
C>
r,
Previous
Next
Fun Screen
L .J
•!
I'>\
\.!..)
Tutorial
1111
Lab Yallles
m; ',
Notes
rim
ffiffij
Calculator
11
•
12
Interpretation of Rinne & Weber tests
13
•
•
14
~
Normal
6
17
Conductive hearin g loss
18
19
Weber resu lt
AC > BC in both ears
Midline
BC > AC in affected ear, AC > BC in unaffected
Lateralizes to affected ear
ear
Sensorineural hea ring
20
Rinne result
AC > BC in both ears
loss
Lateral izes to unaffected ear, away from affected
ear
21
22
Mixed hearin g loss
~
4
BC > AC in affected ear, AC > BC in unaffected
Lateralizes to unaffected ear, away from affected
ear
ear
AC = air conduction; BC = bone conduction.
25
This patient has a sudden hearing loss w ith no history of trauma or pain, a normal ear exami nation, and an otherwise normal neurologic
26
examination . Tuning fork examination shows the hearing loss is sensorineural rather than conductive (Table). The etiology of sudden
27
sensorineu ral hearing loss (SSNHL) is often not determined. Most cases likely represent viral infection, microvascular events, or an
28
autoimmune process; in some cases, a tumor (eg, schwannoma) or other cause of sensorineural hearing loss is identified . SSNHL can lead to
29
permanent hearing loss. Therefore, once isolated SSNHL (ie, otherwise normal examination) is recognized , urgent otolaryngology eval uation is
indicated.
31
32
Although study results have not been definitive, high-dose corticosteroids (and/or corticosteroids injected into the middle ear) are recommended
33
soon after the onset of SSNHL (ideally within 24 hours) as they may improve hearing outcomes, particularly among patients with severe hearing
34
loss. Their efficacy decreases over time, with no effect after 6 weeks; therefore, reassurance is inappropriate (Choice D). Many patients recover
35
at least some (but often not all) hearing over a few weeks. Antiviral therapy (eg , valacyclovir) in combination with corticosteroids was not found to
improve outcomes but is sometimes used if a viral etiology (eg , herpes simplex) is suspected.
36
37
-~
39
•
In addition, an MRI should be obtained to exclude vestibular schwannoma, and a formal audiogran1 should be performed for full characterization of
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
Settings
~
~
9
•
= .
• -
10
ltem 30of 39
Question Id: 16723
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
1111
;'
rim
ffiffij
Calculator
11
•
•
•
12
Although study results have not been definitive, high-dose corticosteroids (and/or corticosteroids injected into the n1iddle ear) are recommended
13
soon after the onset of SSNHL (ideally within 24 hours) as they may in1prove hearing outcomes, particularly among patients with severe hearing
14
loss. Their efficacy decreases over tin1e, with no effect after 6 weeks; therefore, reassurance is inappropriate (Choice D). Many patients recover
~
at least some (but often not all) hearing over a few weeks. Antiviral therapy (eg , valacyclovir) in combination with corticosteroids was not found to
improve outcomes but is sometimes used if a viral etiology (eg , herpes simplex) is suspected.
6
17
In addition, an MRI should be obtained to exclude vestibular scllwannoma, and a formal audiogram should be performed for full characterization of
18
the hearing loss and follow-up.
19
(Choice A) Amoxicillin-clavulanic acid is often used to treat acute otitis media, w hich can cause a sudden hearing loss. However, the hearing
20
loss would be conductive rather than sensorineural, the patient would likely have significant pain, and examination of the ears would show an
21
opaque, bulging tympanic membrane.
22
~
(Choice B) Aural irrigation is sometimes used to remove cerumen. Cerumen impaction can cause acute hearing loss, but it would be conductive
rather than sensorineural, and the impaction w ould prevent examination of the tympanic membranes.
4
25
(Choice C) Ciprofloxacin ear drops may be used to treat otitis externa. Although it can cause an acute conductive hearing loss, patients would
26
have pain and itching of the ear, and examination would show a swollen, erythematous external auditory canal.
27
Educational objective:
28
Sudden hearing loss should be evaluated to determine if it is conductive or sensorineural. Sudden sensorineural hearing loss should be evaluated
29
urgently by otolaryngology w ith a formal audiogram, MRI , and corticosteroid therapy.
References
31
• Clinical practice guideline: sudden hearing loss.
32
33
34
Foundations of Independent Practice
Ear, Nose & Throat (ENT)
Hearing loss
35
Subject
System
Topic
36
opyng
I@ .JWorid
Is
...
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
10
= .
• -
ltem 31 of 39
Question Id: 10014
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
Lab Yallles
m,
rim
Notes
Calculator
;'
ffiffij
11
•
•
•
12
A 23-year-old woman comes to the physician with skin lesions. She noticed a small papule 2 w eeks ago and now has additional similar lesions.
13
There is no associated pain. The patient has had no systemic sympton1s except 1 day of diarrhea that resolved 3 w eeks ago. She has no
14
previous medical problems and works as an assistant at a veterinary facility. The patient has been sexually active with a new partner. She drinks
~
6
alcohol socially, but does not use tobacco or illicit drugs. Her vital signs are normal. Physical examination is normal except for the lesions as
shown below.
17
18
19
20
21
22
~
4
25
26
27
28
29
30
32
33
34
35
36
37
. rsl
-~
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
10
11
•
12
13
•
14
-~
17
18
19
20
21
22
~
25
26
27
28
Which of the following is the most likely cause of her skin lesions?
29
30
32
33
34
35
36
0
0
0
8 . Fungal infection
0
D. Occupational exposure
0
E.
A. Autoimmune condition
C. Insulin resistance
Skin-to-skin contact
37
-~
39
•
T
T
https://t.me/USMLEWorldStep3
9
•
10
11
•
12
13
•
14
-~
17
18
19
20
21
22
~
25
Which of the following is the most likely cause of her skin lesions?
26
27
Q
A. Autoimmune condition
28
0
0
0
0
B.
29
30
32
33
Fungal infection
C. Insulin resistance
0 . Occupational exposure
E.
Skin-to-skin contact
34
35
Submit
36
37
-~
39
•
T
https://t.me/USMLEWorldStep3
9
•
10
11
•
12
13
•
14
-~
17
18
19
20
21
22
~
25
Which of the following is the most likely cause of her skin lesions?
26
27
A. Autoimmune condition (7°/o)
28
B.
Fungal infection (4o/o)
29
C. Insulin resistance (3%)
30
0 . Occupational exposure (16°/o)
32
E.
33
Skin-to-skin contact (68°/o)
34
35
36
Omitted
37
Correct answer
-~
39
•
T
11 .. 68%
L!!!. Answered correctly
IT\
\.::J
08 secs
Time Spent
https://t.me/USMLEWorldStep3
03/26/2020
• Last Updated
9
•
= .
• -
10
ltem 31 of 39
Question Id: 10014
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
rim
Tutorial
Lab Yallles
Notes
Calculator
\.!..)
1111
;'
ffiffij
11
•
•
•
12
Molluscum contagiosum (MC) is a self-limited, localized skin infection caused by a poxvirus. It is characterized by small skin-colored papules
13
with indented centers that may occur anywhere except the palms and soles. The lesions may be accompanied by pruritus and surrounding
14
dermatitis. Child ren are most commonly affected, but adolescents, adults, and immunocompromised individuals can also develop MC .
~
Transmission is through skin-to-skin contact or contact with contaminated fomites. MC is often transmitted through sexual contact and may be
seen in association with other sexually-transmitted diseases. It is also frequently seen in patients with HIV and may be more widely disseminated
6
17
and persistent in these patients. HIV testing should be considered in patients w ith MC, especially for lesions that are widespread or involve the
18
face.
19
MC diagnosis is clinical and based on characteristic findings. The condition is typically self-limited, but treatment may be considered to prevent
20
further spread , reduce symptoms, or improve cosmesis. There are a number of techniques to ren1ove lesions including physical destruction via
21
curettage/cryotherapy or chemical removal w ith topical agents (eg, podophyllotoxin).
22
(Choice A ) Gottron's papules are red/purple papules or plaques associated with dermatomyositis. These typically involve the dorsal and radial
~
surfaces of the metacarpophalangeal joints, proximal interphalangeal j oints, and proximal phalanx.
4
(Choice B) Extrapulmonary blastomycosis is an uncommon cause of skin papules that may be seen with or without an acute pulmonary
25
syndron1e. Lesions are typically wart-like or pustular. Blastomycosis follows a characteristic geographic distribution. Sporotrichosis causes
26
ulcerating nodular lesions that are most commonly seen on the hands or arms.
27
28
(Choice C) Common cutaneous signs of insulin resistance include skin tags, acanthosis nigricans, and xanthelasma.
29
(Choice D) Contagious ecthyma (orf) is caused by a poxvirus of sheep and goats and begins as a single erythematous papule on the hand.
30
Milker's nodules are n1aculopapular/vesicular lesions caused by a parapoxvirus of cows. Both of these conditions are self-limited and very
uncommon.
32
Educational objective :
33
Molluscum contagiosum (MC) causes single or multiple skin-colored, small papules with indented centers and is transmitted via skin-to-skin
34
contact. The lesions can be either asymptomatic or pruritic and can occasionally be accompanied by surrounding dern1atitis. Treatment is
35
usually conservative. HIV testing should be considered in patients with MC, especially if they have lesions involving the face.
36
References
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
•
10
=
ltem31of39
Question Id: 10014
.~Mart<
\
<]
C>
~~
G)
il
'!,·
Previous
Next
Fun Screen
Tutorial
Lab varues
Notes
= ,
Calculator
Reverse Color
~
@
Text Zoom
Settings
11
•
12
r5l
Exhibit Display
13
•
•
14
~
6
17
18
19
20
21
22
~
4
25
26
27
28
29
30
32
33
34
35
©_
36
· ~39
8_
Zoom Out
C
Reset
l?,
Add To New Card
References
37
,
Zoom In
T
https://t.me/USMLEWorldStep3
I Existing Card
~
9
•
•
10
=
ltem31of39
Question Id: 10014
<]
C>
~~
G)
il
'!,·
Previous
Next
Fun Screen
Tutorial
Lab varues
Notes
.~Mart<
\
= ,
Calculator
Reverse Color
~
@
Text Zoom
Settings
11
•
12
r5l
Exhibit Display
13
•
•
14
~
Geographic distribution of blastomycosis
6
17
WA
18
MT
19
ND
MN
OR
20
ID
SD
21
NY
WV
22
~
NV
~
UT
4
CA
PA
IA
NE
IL
co
MO
KS
KY
25
26
AZ
27
OK
NM
\
VA
AR
MS
28
29
OH
IN
AL
LA
TX
30
32
33
©UWorld
34
35
©_
36
· ~39
8_
ZoomOut
C
Reset
l?,
Add To New Card
References
37
,
Zoom In
T
https://t.me/USMLEWorldStep3
I Existing Card
MA
~
9
•
•
10
=
ltem31of39
Question Id: 10014
.~Mart<
\
<]
C>
~~
G)
il
'!,·
Previous
Next
Fun Screen
Tutorial
Lab varues
Notes
= ,
Calculator
Reverse Color
~
@
Text Zoom
Settings
11
•
12
r5l
Exhibit Display
13
•
•
14
~
6
17
18
19
20
21
22
~
4
25
26
27
28
29
30
32
33
34
35
©_
36
· ~39
8_
Zoom Out
C
Reset
l?,
Add To New Card
References
37
,
Zoom In
T
https://t.me/USMLEWorldStep3
I Existing Card
~
9
•
•
10
=
ltem 31 of 39
Question Id: 10014
. ~ Mart<
\
<]
C>
~~
G)
il
'!,·
Previous
Next
Fun Screen
Tutorial
Lab varues
Notes
11
•
12
13
•
•
14
~
6
17
18
19
20
21
22
~
4
25
26
27
28
29
30
32
33
34
35
©_
36
· ~39
8_
Zoom Out
C
Reset
l?,
Add To New Card
References
37
,
Zoom In
T
https://t.me/USMLEWorldStep3
I Existing Card
= ,
Calculator
Reverse Color
~
@
Text Zoom
Settings
9
•
•
10
=
ltem 31 of 39
Question Id: 10014
. ~ Mart<
\
<]
C>
~~
G)
il
'!,·
Previous
Next
Fun Screen
Tutorial
Lab varues
Notes
11
•
12
13
•
•
14
~
6
17
18
19
20
21
22
~
4
25
26
27
28
29
30
32
33
34
35
©_
36
· ~39
8_
Zoom Out
C
Reset
l?,
Add To New Card
References
37
,
Zoom In
T
https://t.me/USMLEWorldStep3
I Existing Card
= ,
Calculator
Reverse Color
~
@
Text Zoom
Settings
9
•
•
10
=
ltem 31 of 39
Question Id: 10014
. ~ Mart<
\
<]
C>
~~
G)
il
'!,·
Previous
Next
Fun Screen
Tutorial
Lab varues
Notes
11
•
12
13
•
•
14
~
6
17
18
19
20
21
22
~
4
25
26
27
28
29
30
32
33
34
35
©_
36
· ~39
8_
Zoom Out
C
Reset
l?,
Add To New Card
References
37
,
Zoom In
T
https://t.me/USMLEWorldStep3
I Existing Card
= ,
Calculator
Reverse Color
~
@
Text Zoom
Settings
9
•
= .
• -
10
ltem 32of 39
Question Id: 110n
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
Lab Yallles
m,
;'
Notes
rim
ffiffij
Calculator
,
Reverse Color
~
~
Text Zoom
~
~
Settings
11
•
•
•
12
13
A 26-year-old woman, gravida 1 para 0, comes to the office to initiate prenatal care. The patient has had no nausea, abdominal pain, or vaginal
bleedi ng since her last menstrual period 8 weeks ago. She has no chronic medical conditions. She had an appendectomy as a child but no other
14
surgery. The patient takes a daily prenatal vitamin and does not use tobacco, alcohol, or illicit drugs. She is a vegetarian and emigrated from
~
Southeast Asia 5 years ago. Blood pressure is 110/75 mm Hg and pulse is 80/min. BMI is 21 kg/m2. Pelvic examination reveals an 8-week-sized,
6
nontender uterus and no ad nexal masses or tenderness. Laboratory results are as follows:
17
Hemoglobin
10.4 g/dL
Platelets
210,000/mm3
Leukocytes
5,200/mm3
Mean corpuscular volume
68 fn13 (normal : 80-96 fm3 )
Mean corpuscular hemoglobin
22 pg/cell (normal: 28-32 pg/cell)
Red blood cells
5.6 million/mm3 (normal 3.6-5.0 million/mm3 )
26
Red cell distribution width
14.2% (normal: 11.5%-1 4.5%)
27
Ferritin
316 ng/mL (normal: 15-200 ng/mL)
18
19
20
21
22
~
4
25
28
A transvaginal ultrasou nd reveals an 8-week intrauterine gestation with a normal heartbeat. Which of the following is the most likely cause of this
29
patient's anemia?
30
31
36
0
0
0
0
37
11 E. Thalassemia trait
33
34
35
-~
39
•
T
A. Folate deficiency
B. Glucose-6-phosphate dehydrogenase deficiency
C. Iron deficiency
0 . Physiologic anemia of pregnancy
T
https://t.me/USMLEWorldStep3
9
•
= .
• -
10
ltem 32of 39
Question Id: 110n
11
•
•\
~
-
•
C>
Previous
Next
-
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
-
11111
;'
rim
ffiffij
Calculator
nontender uterus and no adnexal masses or tenderness. Laboratory results are as follows:
12
13
•
Mart<
<]
Hemoglobin
10.4 g/dL
Platelets
210,000/ mm3
Leukocytes
5,200/mm3
Mean corpuscular volume
68 fn13 (normal: 80-96 fm3 )
Mean corpuscular hemoglobin
22 pg/cell (normal: 28-32 pg/cell)
20
Red blood cells
5.6 million/mm3 (normal: 3.6-5.0 million/mm3 )
21
Red cell distribution width
14.2"/c, (normal: 11 .50/o-14.5%)
Ferritin
316 ng/mL (normal: 15-200 ng/mL)
14
~
6
17
18
19
22
~
4
A transvaginal ultrasound reveals an 8-week intrauterine gestation with a normal heartbeat. Which of the following is the most likely cause of this
25
patient's anemia?
26
Q
Q
Q
Q
Q
27
28
29
30
31
33
A. Folate deficiency
B. Glucose-6-phosphate dehydrogenase deficiency
C. Iron deficiency
0 . Physiologic anemia of pregnancy
E. Thalassemia trait
34
35
Submit
36
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
= .
• -
10
ltem 32of 39
Question Id: 110n
11
•
•
Mart<
-
<]
C>
Previous
Next
-
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
-
11111
;'
rim
ffiffij
Calculator
nontender uterus and no adnexal masses or tenderness. Laboratory results are as follows:
12
13
•
•\
~
Hemoglobin
10.4 g/dL
Platelets
2 10,000/ mm3
Leukocytes
5,200/mm3
Mean corpuscular volume
68 fn13 (normal: 80-96 fm3 )
Mean corpuscular hemoglobin
22 pg/cell (normal: 28-32 pg/cell)
Red blood cells
5.6 million/mm3 (normal: 3.6-5.0 million/mm3 )
Red cell distribution width
14.2"/c, (normal: 11 .50/o-14.5%)
Ferritin
316 ng/mL (normal: 15-200 ng/mL)
14
~
6
17
18
19
20
21
22
~
4
A transvaginal ultrasound reveals an 8-week intrauterine gestation with a normal heartbeat. Which of the following is the most likely cause of this
25
patient's anemia?
26
A. Folate deficiency (1%)
27
28
B. Glucose-6-phosphate dehydrogenase deficiency (1%)
29
30
C. Iron deficiency (22%)
31
0 . Physiologic anemia of pregnancy (23%)
E. Thalassemia trait (5 1%)
33
34
35
36
Omitted
37
Correct answer
-~
39
•
T
11 .. 51 %
L!!!. Answered correctly
IT\
\.::J
07 secs
Time Spent
https://t.me/USMLEWorldStep3
05/26/2020
• Last Updated
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
= .
• -
10
•\
~
ltem 32of 39
Question Id: 110n
Mart<
<]
C>
r,
Previous
Next
Fun Screen
L .J
•!
I'>\
\.!..)
Tutorial
m; ',
1111
Lab Yallles
Notes
rim
ffiffij
Calculator
11
•
12
Parameter
Iron deficiency
anemia
a-thalassemia minor
13-thalassemia minor
~
MCV
!
!
l
ROW
1'
Normal
Normal
18
RBCs
•
I
Normal
Norn1al
Peripheral smear
Microcytosis, hypochromia
Target cells
Target cells
Serum iron studies
! Iron & ferritin
i TIBC
Normal/t iron & ferritin (RBC
Normal/f iron & ferritin (RBC
turnover)
turnover)
f Hem oglobin
No improvement
No im provemen t
Normal
Normal
13
•
•
14
6
17
19
20
21
22
~
Response to iron
4
supplementation
25
Hemoglobin electrophoresis
26
i
Hem oglobin A2.
MCV = mean corpuscular volume; RBCs = red blood cells; ROW = red cell distribution width; TIBC = total iron-binding capacity.
27
28
Screening for anemia is routine at the first pren atal visit. Patients with thalassemia minor (ie, thalassem1a trait) have mild microcytic,
29
hypoch romic anemia, as indicated by a low mean corpuscular volume (MCV) and mean corpuscular hemoglobin , respectively. They also h ave
30
mildly elevated ferritin due to increased red blood cell (RBC) turnover. The RBC count n1ay be normal or increased, but the red cell
31
distribution width (ROW) is normal as almost all RBCs are uniformly small. In addition, the anemia is relatively mild in comparison with the
decrease in MCV.
33
This patient's results are consistent with thalassemia minor, which is common in those of Mediterranean, Middle Eastern, Southeast Asian,
34
African, and Indian descent. A maternal hemoglobin electrophoresis sh ould b e ordered to confirm the diagnosis and distinguish a- from 13-
35
thalassem ia minor. Electrophoresis is normal in patients with a-thalassemia; 13-thalassemia causes abnormally elevated hem oglobin A2. levels.
36
After confirmation of maternal thalassemia, a paternal hemoglobin electrophoresis is indicated to determine the fetal risk of thalassemia n1aj or.
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
Settings
~
~
9
•
•
•
•
= .
• -
10
•\
~
ltem 32of 39
Question Id: 110n
-
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
1111
;'
rim
,
ffiffij
Calculator
11
.
12
This patient's results are consistent with thalassemia minor, which is common in those of Mediterranean, Middle Eastern, Southeast Asian,
13
African, and Indian descent. A maternal hemoglobin electrophoresis should be ordered to confirm the diagnosis and distinguish a- from 13·
14
thalassemia minor. Electrophoresis is normal in patients with a-thalassemia; 13-thalassemia causes abnorn1ally elevated hemoglobin A2. levels .
~
.
Mart<
<]
Reverse Color
~
~
~
~
Text Zoom
Settings
SgJ2,d
Eng ock
After confirn1ation of maternal thalassemia, a paternal hemoglobin electrophoresis is indicated to determine the fetal risk of thalassemia major.
6
Maternal conditions requiring partner testing include cl inically significant maternal hemoglobinopathies (eg , SS, SC, hemoglobin S/!3-thalassemia)
17
as well as carrier states (a- and 13-thalassemia minor).
18
(Choice A ) Folate deficiency causes a macrocytic anemia (high MCV). Vegetarians usually have adequate folate due to their plant-based diets.
19
20
(Choice B) Glucose-6-phosphate dehydrogenase deficiency is an X-linked disorder common in those of African descent. Heterozygous women
21
are usually asymptomatic. Men and homozygous women can develop hemolytic anemia from an infection, after exposure to various drugs or
22
chemicals, or during diabetic ketoacidosis. G6PD deficiency does not cause microcytic, hypochromic anemia.
~
(Choice C) Vegetarians are at risk of iron deficiency anemia, particularly during pregnancy. Iron deficiency anemia is characterized by a
4
microcytic, hypochromic anemia, with significantly low MCV and a proportional drop in hemoglobin level. In addition, patients with iron deficiency
25
have a high ROW in the setting of low ferritin and RBC counts.
26
(Choice D) Physiologic anemia of pregnancy is characterized by mild normocytic, normochromic anemia. This results from a greater expansion
27
of plasma volume relative to the increase in RBC mass (ie, dilutional anemia). The nadir typically occurs during the late second to early third
28
trimester.
29
30
Educational objective:
31
Screening for anemia is routine at the first prenatal visit. Thalassemia trait is characterized by a microcytic, hypochromic anemia; mildly elevated
ferritin; and normal red cell distribution width. Partners of women with thalassemia minor should undergo hemoglobin analysis to assess fetal risk
of inheriting thalassemia.
33
34
References
35
• Serum concentrations of vitamin B12 and folate in British male omnivores, vegetarians and vegans: results from a cross-sectional analysis of
36
the EPIC-Oxford cohort study.
37
-~
39
•
al
T
TUTOR
a
a
'" •
a
•
•
~ az
https://t.me/USMLEWorldStep3
~
F2ck
9
•
= .
• -
10
ltem 33of 39
Question Id: 61 25
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
Lab Yallles
m,
rim
Notes
Calculator
;'
ffiffij
11
•
•
•
12
A 16-month-old full-term girl is brought to the office to establish well-child care. The patient's family recently moved to the area and they have no
13
concerns about her development. The patient weaned from breastfeed ing at age 12 months, and her current diet mainly consists of whole cow's
14
milk. She has no chronic medical conditions and takes no medications. She was born to a 24-year-old primigravida Greek woman and a 30-year-
~
old African American man. The patient's father has sickle cell trait and her first cousin has sickle cell anemia; maternal family history is
6
noncontributory. Physical examination reveals pallor of the conjunctivae but is otherwise unremarkable. laboratory results are as follows:
17
18
19
20
Hemoglobin
9.2 g/dl
Red blood cell distribution width
16.So/o (n=13.5-15.3)
Mean corpuscular volume
64 µm3
l ead
<5 µg/dl
21
22
~
Hemoglobin electrophoresis reveals 40% HbS and 60% HbA. Which of the following is the most likely cause of this patient's anemia?
4
25
Q
A Alpha thalassemia
26
0
0
0
0
B. Anemia of chronic disease
27
28
29
30
31
C. Beta thalassemia
0. Hemoglobin SC disease
E. Iron deficiency anemia
32
Submit
34
35
36
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
= .
• -
10
ltem 33of 39
Question Id: 61 25
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
1111
;'
rim
ffiffij
Calculator
11
•
•
•
12
A 16-month-old full-term girl is brought to the office to establish well-child care. The patient's family recently moved to the area and they have no
13
concerns about her development. The patient weaned from breastfeed ing at age 12 months, and her current diet mainly consists of whole cow's
14
milk. She has no chronic medical conditions and takes no medications. She was born to a 24-year-old primigravida Greek woman and a 30-year-
~
old African American man. The patient's father has sickle cell trait and her first cousin has sickle cell anemia; maternal family history is
6
noncontributory. Physical examination reveals pallor of the conjunctivae but is otherwise unremarkable. laboratory results are as follows:
17
18
19
20
Hemoglobin
9.2 g/dl
Red blood cell distribution width
16.So/o (n=13.5-15.3)
Mean corpuscular volume
64 µm3
l ead
<5 µg/dl
21
22
~
Hemoglobin electrophoresis reveals 40% HbS and 60% HbA. Which of the following is the most likely cause of this patient's anemia?
4
A . Alpha thalassemia (9%)
25
26
B. Anemia of chronic disease (0%)
27
28
C. Beta thalassemia (12%)
29
D. Hemoglobin SC disease (31 %)
30
E. Iron deficiency anemia (46%)
31
32
34
Omrtted
35
Correct answer
E
36
111.
l!!!.
46%
Answered correctly
(T'\ 03 secs
'.::.) T1111e Spent
37
-~
39
•
T
https://t.me/USMLEWorldStep3
07/10/20 20
• Last Updated
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
10
= .
• -
ltem 33of 39
Question Id: 6125
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
•!
m,
rim
Lab Yallles
Notes
Calculator
I'>\
\.!..)
Tutorial
1111
;'
ffiffij
11
•
12
13
•
•
Iron deficiency anemia in young children
• Prematurity
14
~
• Lead exposure
• Age <1
6
o
17
18
Risk factors
• Age >1
20
o >24 oz/day cow's milk
21
o
22
Diagnosis
4
25
(ie, exclusive breastfeeding after 6 months)
o Cow's, soy, or goat's milk
19
~
Delayed introduction of solids
Treatment
<3 servi ngs/day iron-rich foods
• Screeni ng hemoglobin at age 1
• Hemoglobin <11 g/dl, ! MCV, T ROW
• Empiric trial of iron supplementation
26
27
MCV = mean corpuscular volume; ROW= red blood cell distribution width.
28
This patient's anemia is most likely caused by iron deficiency. In children age >1, excessive m ilk intake (>24 oz/day) and low intake of iron-rich
29
foods (eg, meats, cereals) contribute to the development of iron deficiency anemia. Given the high prevalence of iron deficiency in children age
30
<2, these findings are sufficient to begin an empiric trial of iron supplementation.
31
32
Iron deficiency is typically diagnosed based on clinical history and low hemoglobin. However, in patients with a family history of hemoglobinopathy
(eg , sickle cell anemia), hemog lobin electrophoresis must be ordered. The presence of HbA and HbS in a 60:40 ratio, respectively, is
consistent w ith sickle cell trait, which is generally asymptomatic and not a cause of anemia and n1icrocytosis. This patient's microcytic anemia
34
(low mean corpuscular volume) with an elevated red cell distribution wi dth is most likely due to iron deficiency anemia.
35
36
(Choice A) Alpha thalassemias are characterized by the presence of Hb Barts (4 gamma chains) on electrophoresis, not seen in this patient.
37
. rsl
-~
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
= .
• -
10
Question Id: 6125
11
•
•
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
rim
Tutorial
Lab Yallles
Notes
Calculator
\.!..)
1111
;'
ffiffij
<2, these findings are sufficient to begin an empiric trial of iron supplementation.
12
Iron deficiency is typically diagnosed based on cl inical history and low hemoglobin. However, in patients with a family history of hemoglobinopathy
13
•
ltem 33of 39
(eg , sickle cell anemia), hemoglobin electrophoresis must be ordered. The presence of HbA and HbS in a 60:40 ratio, respectively, is
14
consistent w ith sickle cell trait, which is generally asymptomatic and not a cause of anemia and microcytosis. This patient's microcytic anemia
~
(low mean corpuscular volume) with an elevated red cell distribution wi dth is most likely due to iron deficiency anemia.
6
17
(Choice A) Alpha thalassemias are characterized by the presence of Hb Barts (4 gamma chains) on electrophoresis, not seen in this patient.
18
(Choice B) Anen1ia of chronic disease is a nom,ocytic, nom,ochromic anemia that occurs in patients with chronic medical conditions (eg, renal
19
failure, rheumatoid arthritis).
20
(Choice C) Beta thalassemias are due to mutations in the beta globin genes; they are not associated with the presence of HbS. Sickle-beta
21
thalassemia is comprised predominantly of HbS with <30% HbA. HbF and HbA2 are also typically elevated.
22
~
(Choice D) HbSC is a less-severe variant of sickle cell disease characterized by a mild nom1ocytic anemia. Hemoglobin electrophoresis showing
almost equal amounts of HbS and HbC is diagnostic.
4
25
Educational objective:
26
Iron deficiency, commonly caused by excessive milk intake and insufficient iron-rich foods in young children, results in a microcytic anemia with an
27
elevated red cell distribution width . The presence of HbA and HbS in a 60:40 ratio, respectively, on hemoglobin electrophoresis is consistent with
28
sickle cell trait, which is asymptomatic and does not cause anemia.
29
References
30
• Iron deficiency and other types of anemia in infants and children.
31
32
• Evaluation of anemia in children.
34
Foundations of Independent Practice
Hen1atology & Oncology
35
Subject
System
36
opyng
I@ ..JWorla
Iron deficiency anemia
Topic
Is
...
37
-~
39
•
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
= .
• -
10
ltem 34of 39
Question Id: 17306
•\
~
Mart<
<]
C>
r,
Previous
Next
Fun Screen
L .J
•!
I'>\
\.!..)
Tutorial
1111
Lab Yallles
m; ',
Notes
rim
ffiffij
Calculator
11
•
•
•
12
A 19-year-old woman comes to the office due to a bothersome rash on her shoulders and upper arms for the last 5 years that is associated with
13
significant itchi ng during cold, dry weather. The patient says, "I had eczema when I was a baby that got better when I got older. I kept thinking this
14
would go away too, but it just gets worse." Medical history is otherwise un remarkable, and she takes no medications. Skin examination findings
~
are shown in the exhibit. Which of the following is the most appropriate next step in management of this patient's skin condition?
6
0
0
0
0
0
17
18
19
20
21
22
~
A. Gluten-free diet
B.
HIV testing
C. Oral minocydine
D. Skin biopsy
E. Urea cream
4
25
Submit
26
27
28
29
30
31
32
33
35
36
37
. rsl
-~
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
Settings
~
~
9
•
= .
• -
10
ltem 34of 39
Question Id: 17306
•\
~
Mart<
<]
C>
r,
Previous
Next
Fun Screen
L .J
•!
I'>\
\.!..)
Tutorial
1111
Lab Yallles
m; ',
Notes
rim
ffiffij
Calculator
11
•
•
•
12
A 19-year-old woman comes to the office due to a bothersome rash on her shoulders and upper arms for the last 5 years that is associated with
13
significant itchi ng during cold, dry weather. The patient says, "I had eczema when I was a baby that got better when I got older. I kept thinking this
14
would go away too, but it just gets worse." Medical history is otherwise un remarkable, and she takes no medications. Skin examination findings
~
are shown in the exhibit. Which of the following is the most appropriate next step in management of this patient's skin condition?
6
17
A. Gluten-free diet (19°/o)
18
B.
HIV testing (3%)
19
C. Oral minocycline (14o/o)
20
21
D. Skin biopsy (3%)
22
./ '
~
E . Urea cream (58%)
4
25
Omitted
26
Correct answer
27
E
111.
l!l!.
58%
Answered correctly
,i'\ 02 secs
\::J
Time Spent
F=! 03/11/2020
13 Last Updated
28
29
Explanation
30
31
32
This patient has a papular rash consistent with kerat osis pilaris (KP). KP ("chicken skin") is a benign condition characterized by retained keratin
33
plugs in the hair follicles. It presents with small, painless papules, a roughened skin texture, and mottled perifollicular erythema. KP can occur
anywhere but is most common on the posterior surface of the upper arm. It is usually asymptomatic but can become pruritic in cold, dry w eather
and can occasionally form small pustules.
35
36
KP can occur alone or in association with atopic disorders (eg, atopic dermatitis, asthma). The diagnosis is typically obvious based on
37
appearance; biopsy can reveal keratin plugs, dilated hair follicles, and a sterile lymphocytic infiltrate but is rarely needed for diagnosis (Choice D).
. rsl
-~
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
Settings
~
~
9
•
= .
• -
10
ltem 34of 39
Question Id: 17306
•\
~
Mart<
<]
C>
r,
Previous
Next
Fun Screen
L .J
•!
I'>\
\.!..)
Tutorial
1111
Lab Yallles
m; ',
Notes
rim
ffiffij
Calculator
11
•
Explanation
12
13
•
•
This patient has a papular rash consistent with keratosis pilaris (KP). KP {"chicken skin") is a benign condition characterized by retained keratin
14
plugs in the hair follicles. It presents with small, painless papules, a roughened skin t exture, and mottled perifollicular erythema. KP can occur
~
anywhere but is most common on the posterior surface of the upper ann. It is usually asymptomatic but can become pruritic in cold, dry w eather
6
and can occasionally form small pustules.
17
KP can occur alone or in association with atopic disorders (eg, atopic dermatitis, asthma). The diagnosis is typically obvious based on
18
appearance; biopsy can reveal keratin plugs, dilated hair follicles, and a sterile lymphocytic infiltrate but is rarely needed for diagnosis (Choi ce D).
19
Treatment, when necessary, includes emollients and topical keratolytics (eg, salicylic acid, urea), which can help soften the papules.
20
21
(Choice A) Dermatitis herpetiformis is a skin disorder associated with celiac disease that generally improves with a gluten-free diet. It presents
22
with intensely pruritic papules, vesicles, and bullae on the elbows, back, knees, and buttocks.
~
(Choice B) HIV increases the risk for infectious skin diseases, such as molluscum contagiosum. Patients with HIV can develop numerous
4
molluscum lesions, but these papules are smooth, firm, and umbilicated; would not be limited to the shoulders and arms; and usually resolve
25
spontaneously.
26
(Choice C) Oral minocycline is used for treatment of inflamn1atory acne, which presents with inflamed papules and pustules. Although the
27
shoulders and upper arms can be affected, the central face is usually also involved .
28
29
Educational objective:
30
Keratosi s pilaris is characterized by retained keratin pl ugs in the hair follicles. It presents with small papules; a roughened skin texture; and
mottled, perifollicular erythema, most commonly on the posterior surface of the upper arn1. Treatment includes emollients and topical keratolytics
31
(eg, salicylic acid, urea).
32
33
35
36
Foundations of Independent Practice
Dermatology
Keratosis pilaris
Subject
System
Topic
I@
37
. rsl
-~
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
Settings
~
~
9
•
10
= .
• -
ltem 35of 39
Question Id: 5815
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
rim
Tutorial
Lab Yallles
Notes
Calculator
\.!..)
1111
;'
ffiffij
11
•
•
•
12
A 64-year-old woman comes to the physician due to thickeni ng and discoloration of her toenails. Her nails are rough, and this is starting to cause
13
pain and making it difficult to wear shoes with socks. A few months ago, she first noticed that the big toes of both feet were affected, subsequently
14
several other nails became affected as well. On physical examination, the affected nails appear rough, brittle, and discolored as shown in the
~
image below. Potassium hydroxide preparation of nail scrapings shows dermatophytic hyphae and arthrospores.
6
17
18
19
20
21
22
~
4
25
26
27
28
29
30
31
32
33
34
36
37
. rsl
-~
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
10
11
•
12
13
•
14
.~
17
18
19
20
21
22
~
25
Which of the following is the most effective treatment regimen for this patient's condition?
26
Q A. Ciclopirox
27
28
0
0
0
0
29
30
31
32
33
B.
Fluconazole
C. Griseofulvin
0 . Ketoconazole
E.
Terbinafine
34
Submit
36
37
. rsl
-~
T
https://t.me/USMLEWorldStep3
9
•
10
11
•
12
13
•
14
.~
17
18
19
20
21
22
~
25
Which of the following is the most effective treatment regimen for this patient's condition?
26
27
A. Ciclopirox (Oo/o)
28
B.
Fluconazole (5°/o)
29
30
C. Griseofulvin (19%)
31
0 . Ketoconazole (7%)
32
E.
33
Terbinafine (66%)
34
36
Omitted
37
Correct answer
. rsl
-~
T
11 ..
L!!!.
66%
Answered correctly
IT\
\.::J
06secs
Time Spent
https://t.me/USMLEWorldStep3
03/29/2020
• Last Updated
9
•
•
10
=
ltem 35of 39
Question Id: 5815
. ~
\
<]
C>
~~
G)
il
'!,·
Previous
Next
Fun Screen
Tutorial
Lab varues
Notes
Mart<
11
•
Onychomycosis
12
13
•
•
14
~
6
17
18
19
20
21
22
~
4
25
26
Risk factors
•
•
•
•
Examination
fi ndings
Thick, brittle, discolored nails
27
28
29
Advanced age
n nea pedis
Diabetes
Peripheral vascular disease
30
31
32
33
34
Diagnosis
KOH, periodic acid-Schiff stain, culture
Treatment
• First line: terbinafine, itraconazole
• Second line: griseofulvin,
36
37
. rsl
·~
T
https://t.me/USMLEWorldStep3
= ,
Calculator
Reverse Color
~
@
Text Zoom
Settings
9
•
10
= .
• -
ltem 35of 39
Question Id: 5815
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
rim
Tutorial
Lab Yallles
Notes
Calculator
\.!..)
1111
;'
ffiffij
11
•
13
•
•
Risk factors
•
•
•
•
Examination
findings
Thick, brittle, d iscolored nails
12
14
~
6
17
Advanced age
nnea pedis
Diabetes
Peripheral vascular disease
18
19
Diagnosis
KOH, periodic acid-Schiff stain, culture
Treatment
• First line: terbinafine, itraconazole
• Second line: griseofulvin,
fluconazole, ciclopirox
20
21
22
~
4
25
KOH = potassium hydroxide.
©UWor1d
26
27
28
29
30
Onychomycosis is a fungal infection of the toenails or fingernails. The most common form of onychomycosis is distal subungual onychomycosis,
which is caused by the dermatophyte Trichophyton rubrum. Because nail dystrophies caused by other diseases (eg, psoriasis, lichen planus,
eczematous conditions) can mimic the appearance of onychomycosis, confirmation with potassium hydroxide (KOH) preparation or periodic
acid-Schiff staining of nail scrapings is recommended. If KOH examination is negative, then eval uation by culture is appropriate.
31
Patients often request treatment of onychomycosis for cosmetic reasons; such treatment may be considered in carefully selected patients.
32
However, patients should be advised about the risks of treatment (primarily hepatotoxicity), and the potential of treatment failure and recurrence.
33
Medical indications for treatment of onychomycosis include significant pain or functional limitation, history of cellulitis in the affected extremity, or
34
additional risk factors for cellulitis (eg, diabetes). Oral terbinafine is considered first-line therapy, and oral itraconazole is an acceptable
alternative. Infection of the fingernails requires 6 weeks of therapy, and infection of the toenails requires 12 w eeks.
36
(Choice A) Ciclopirox is a topical antifungal nail lacquer approved for the treatment of mild-to-moderate onychomycosis. Although ciclopirox is
37
considered safe studies show its efficac to be minin1al.
. rsl
-~
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
= .
• -
10
ltem 35of 39
Question Id: 5815
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
11111
;'
rim
ffiffij
Calculator
11
•
•
•
acid-Schiff staining of nail scrapings is recommended. If KOH examination is negative, then eval uation by culture is appropriate.
12
13
Patients often request treatment of onychomycosis for cosmetic reasons; such treatment may be considered in carefully selected patients.
14
However, patients should be advised about the risks of treatment (primarily hepatotoxicity), and the potential of treatment failure and recurrence.
~
Medical indications for treatment of onychomycosis include significant pain or functional limitation, history of cellulitis in the affected extremity, or
17
alternative. Infection of the fingernails requires 6 weeks of therapy, and infection of the toenails requires 12 w eeks.
18
(Choice A ) Ciciopirox is a topical antifungal nail lacquer approved for the treatment of mild-to-moderate onychomycosis. Although ciclopirox is
19
considered safe, studies show its efficacy to be minimal.
additional risk factors for cellulitis (eg, diabetes). Oral terbinafine is considered first-line therapy, and oral itraconazole is an acceptable
6
20
(Choice B) Fluconazole is an option in the treatment of onychomycosis, and its weekly dosage may be particularly appealing for those patients
21
with complex medication regimens. However, it is less effective and more expensive than terbinafine and itraconazole.
22
~
(Choices C and D) Griseofulvin and ketoconazole are rarely used now that terbinafine and itraconazole are available. These older medications
required lengthy treatment regimens (often up to 18 months) with frequent laboratory monitoring, and were associated with high relapse rates and
4
numerous adverse effects.
25
26
Educational objective :
27
Because nail dystrophies caused by other diseases (eg, psoriasis, lichen planus) can mimic the appearance of onychomycosis, confirmation
28
with potassium hydroxid e (KOH) preparation or culture of nail scrapings is recommended. Terbinafine is the preferred first-line therapy.
29
References
30
• Oral therapy for onychomycosis: an evidence-based review.
31
• Onychomycosis: Current trends in diagnosis and treatment.
32
33
34
36
Foundations of Independent Practice
Dermatology
Onychomycosis
Subject
System
Topic
C
I@
37
. rsl
-~
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
= .
• -
10
ltem 36of 39
Question Id: 5195
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
\.!..)
Tutorial
•!
1111
Lab Yallles
m,
rim
Notes
Calculator
;'
ffiffij
11
•
•
•
12
A 62-year-old Caucasian man comes to the office with complaints of a dull, non-throbbing headache, hearing loss on the left side, and persistent
13
tinnitus. His symptoms have been getting progressively worse for the last two weeks. He has a history of small cell cancer of the lung, which w as
14
treated with a combination of chemotherapy and radiotherapy four months ago. His lung mass has reduced considerably in size after its
~
treatment. A contrast-enhanced magnetic resonance imaging scan shows a 1 x 2 cm circumscribed mass in the left cerebellopontine angle
compressing the eighth cranial nerve. There is another small 0.5 x 1 cm mass in the left frontal lobe cortex with significant edema surrounding the
6
lesion. Which of the following is the most likely cause of this patient's symptoms?
17
18
19
Q
A
Acoustic neuron1a
20
0
0
0
0
B.
Medulloblastoma
21
22
~
4
25
C. Metastatic cancer
D. Meningioma
E. Astrocytoma
26
27
Submit
28
29
30
31
32
33
34
35
37
. rsl
-~
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
= .
• -
10
ltem 36of 39
Question Id: 5195
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
1111
;'
rim
ffiffij
Calculator
11
•
•
•
12
A 62-year-old Caucasian man comes to the office with complaints of a dull, non-throbbing headache, hearing loss on the left side, and persistent
13
tinnitus. His symptoms have been getting progressively worse for the last two weeks. He has a history of small cell cancer of the lung, which w as
14
treated with a combination of chemotherapy and radiotherapy four months ago. His lung mass has reduced considerably in size after its
~
treatment. A contrast-enhanced magnetic resonance imaging scan shows a 1 x 2 cm circumscribed mass in the left cerebellopontine angle
compressing the eighth cranial nerve. There is another small 0.5 x 1 cm mass in the left frontal lobe cortex with significant edema surrounding the
6
lesion. Which of the following is the most likely cause of this patient's symptoms?
17
18
19
A . Acoustic neuron1a (20o/o)
20
B.
Medulloblastoma (1%)
21
C. Metastatic cancer (74%)
22
~
D. Meningioma ( 1%)
4
E. Astrocytoma (1%)
25
26
27
Omitted
28
Correct answer
C
29
'"·
I.!.!!..
74%
Answered
correctly
(T'\ 02 secs
\.::) Time Spent
04/05/2020
• Last Updated
30
31
Explanation
32
33
34
Brain tumors are classified into tumors that originate in the brain itself (primary brain tumor), and those that originate elsewhere in the body and
35
metastasize to the brain from another primary site (secondary brain tumor). Secondary brain tumors are the more common type of brain tumors.
The common prin1ary sites of origin of brain metastasis, in the order of frequency, are: lung, breast, unknown primary, melanoma, and colon
37
. rsl
-~
cancer.
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
10
11
•
12
13
•
14
Omitted
Correct answer
C
.~
11 ..
l!!!.
74%
f'i', 02 secs
Answered correctly
\.::) Time Spent
04/05/2020
• Last Updated
17
18
Explanation
19
20
Brain tumors are classified into tumors that originate in the brain itself (primary brain tumor), and those that originate elsewhere in the body and
21
metastasize to the brain from another primary site (secondary brain tumor). Secondary brain tumors are the more common type of brain tumors.
22
The common primary sites of origin of brain metastasis, in the order of frequency, are: lung, breast, unknown primary, melanon1a, and colon
~
cancer.
Small cell lung cancer has a predilection for early metastasis to the brain . The most common route of spread of the cancer is by hematogenous
25
spread. The diagnostic imaging of choice to evaluate a patient with suspected metastatic disease is a contrast-enhanced MRI scan. The clues to
26
the presence of a metastatic brain lesion (as compared to a primary brain tumor) on radiographic imaging are the presence of multiple, well-
27
circumscribed lesions, and a relatively large amount of vasogenic eden1a as compared to the size of the lesion. In the above vignette, the patient's
28
symptoms is most likely being caused by a metastatic lung cancer which has compressed the eighth cranial nerve.
29
Educational Obj ective:
30
Metastatic lesions to the brain are the most common cause of brain tumors. These account for more than half of all the brain tumors seen in adult
31
patients.
32
33
34
Foundations of Independent Practice
Hen1atology & Oncology
Brain tumors
35
Subject
System
Topic
Copynghl@ ..JWorla A
Is
...
37
. rsl
-~
T
https://t.me/USMLEWorldStep3
9
•
= .
• -
10
ltem 37of 39
Question Id: 5843
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
rim
Tutorial
Lab Yallles
Notes
Calculator
\.!..)
1111
;'
ffiffij
11
•
•
•
12
A 48-year-old woman complains of persistent fatigue and daytime sleepiness. Her other medical problems include hypertension and rheumatoid
13
arthritis. Her medications include naproxen, enalapril, and a multivitamin supplement with iron. She has no known drug allergies. Vital signs are
14
within normal limits. Examination shows conjunctival pallor and bilateral hand joint deformities with tenderness to palpation at
~
metacarpophalangeal joints. Stool testing for occult blood is negative.
6
Laboratory results are as follows:
17
18
Hemoglobin
8.2 g/dL
Hematocrit
27°/o
21
Mean corpuscular volume
84 fl
22
Platelet
450,000/µL
Leukocyte
6 ,000/µL
Iron , serum
80 µg/dL
27
Iron-binding capacity, serum
200 µg/dL (normal 250-370 µg/dL)
28
Ferritin
300 ng/mL
Serum erythropoietin
500 mU/mL (normal > 100 mU/mL)
Erythrocyte sedimentation rate
80 mm/h
19
20
~
4
25
26
29
30
31
32
33
Which of the following would be the most appropriate next step in n1anaging this patient's anemia?
34
35
( ) A. F olinic acid
36
Q
38
39
T
B. lnfliximab
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
10
11
•
12
13
•
•
14
~
Mean corpuscular volume
84 fl
Platelet
450,000/µL
Leukocyte
6,000/µL
Iron, serum
80 µg/dl
Iron-binding capacity, serum
200 µg/dl (normal 250-370 µg/dl)
Ferritin
300 ng/ml
Serun1 erythropoietin
500 mU/mL (normal >100 mU/mL)
Erythrocyte sedimentation rate
80mm/h
6
17
18
19
20
21
22
~
4
25
Which of the following would be the most appropriate next step in n1anaging this patient's anemia?
26
Q A. Folinic acid
27
28
0
0
0
0
29
30
31
32
33
B.
lnlliximab
C. Intravenous iron
0 . Plasmapheresis
E. Splenectomy
34
35
Submit
36
38
39
T
https://t.me/USMLEWorldStep3
9
•
10
11
•
12
Mean corpuscular volume
84 fl
Platelet
450,000/µL
Leukocyte
6,000/µL
Iron, serum
80 µg/dl
Iron-binding capacity, serum
200 µg/dl (normal 250-370 µg/dl)
Ferritin
300 ng/ml
Serun1 erythropoietin
500 mU/mL (normal >100 mU/mL)
Erythrocyte sedimentation rate
80mm/h
13
•
14
.~
17
18
19
20
21
22
~
25
Which of the following would be the most appropriate next step in n1anaging this patient's anemia?
26
27
A. Folinic acid (11o/o)
28
B.
lnlliximab (67°/o)
29
30
C. Intravenous iron (11°/o}
31
0 . Plasmapheresis (7% )
32
E. Splenectomy (2%)
33
34
35
Omitted
36
Correct answer
-
38
39
T
TUTOR
11 .. 67%
L!!!. Answered correctly
fT\ 04 secs
\.::J Time Spent
https://t.me/USMLEWorldStep3
04/08/2020
• Last Updated
~
F2ck
SgJ2,d
Engock
9
•
= .
• -
10
•\
~
ltem 37of 39
Question Id: 5843
Mart<
<]
C>
Previous
Next
r,
I'>\
•!
m,
rim
Tutorial
Lab Yallles
Notes
Calculator
\.!..)
L .J
Fun Screen
1111
,
ffiffij
;'
Reverse Color
~
~
~
~
Text Zoom
Settings
SgJ2,d
Eng ock
11
•
12
13
•
•
Iron studies in microcytic anemia
14
~
6
MCV
Cause
Iron
Transferrin
saturation
Ferritin
TIBC
17
(lron/TIBC)
18
19
Iron deficiency
I
I
I
I
I
Thalassemia
II
I
I
I
II
Anemia of
chronic disease
(inflammation)
Normal/I
I
I
Normal/f
Normal/I
20
21
22
~
4
25
26
MCV = mean corpuscular volume; TIBC = total iron binding capacity.
27
©UWor1d
28
Anen1ia of chronic disease (ACD, anen1ia of chronic inflamn1ation) is a common complication of rheumatoid arthritis and other inflammatory
29
diseases. The precise etiology is not fully understood but is generally thought to be due to suppression of hematopoiesis by inflamn1atory
30
cytokines. Hen1atologic studies typically show a low serum iron, elevated ferritin levels, and normal transferrin saturation (approximately 25% of
31
ACD patients may have low transferrin saturation). Mean corpuscular volume is usually low-norn,al to mildly decreased. ACD is usually a
32
relatively mild anemia, but approximately 20°/o of patients n1ay have hemoglobi n <8 g/dl. In these more severe cases, clinicians should rule out
33
additional concurrent causes of anemia such as iron deficiency, myelodysplasia, and thalassemia.
34
The foundation of treatment for ACD is addressing the underlying inflan1matory disorder. In rheun1atoid arthritis, anti-TNF-a antibody (eg,
35
infliximab) infusions have been shown to lessen the severity of anemia. If patients have low or inappropriately nom1al erythropoietin levels, they
36
may respond to injections of erythropoietin or darbepoetin. Patients with appropriately elevated erythropoietin levels (especially >500 mU/n1L) do
- -
38
39
T
TUTOR
-- -
--
.
·-
- - -
- - - -
- -- - - -
. . - -
- - - -- - -
·- -
-
-
-
. - -
-
-
-
- - ---
--
.
-
-
--
https://t.me/USMLEWorldStep3
. - -
-- -
- - -
-
- --
- -
--
~
F2ck
9
•
10
= .
• -
ltem 37of 39
Question Id: 5843
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
rim
Tutorial
Lab Yallles
Notes
Calculator
\.!..)
1111
;'
ffiffij
11
•
•
•
12
Anemia of chronic disease (ACD, anemia of chronic inflamn1ation) is a common complication of rheumatoid arthritis and other inflammatory
13
diseases. The precise etiology is not fully understood but is generally thought to be due to suppression of hematopoiesis by inflammatory
14
cytokines. Hen1atologic studies typically show a low serum iron, elevated ferritin levels, and normal transferrin saturation (approximately 25% of
~
ACD patients may have low transferrin saturation). Mean corpuscular volume is usually low-normal to mildly decreased. ACD is usually a
18
The foundation of treatment for ACD is addressing the underlying inflammatory disorder. In rheumatoid arthritis, anti-TNF-a antibody (eg,
19
infliximab) infusions have been shown to lessen the severity of anemia. If patients have low or inappropriately normal erythropoietin levels, they
20
may respond to injections of erythropoietin or darbepoetin. Patients with appropriately elevated erythropoietin levels (especially >500 mU/mL) do
21
not respond. Those who have severe, symptomatic anemia who do not improve with initial measures may need period ic red cell transfusions.
22
(Choice A) Folinic acid (leucovorin) is a folic acid derivative. It can be given orally or parenterally to counteract the effects of antifolate drugs
6
17
~
relatively mild anemia, but approximately 20°/o of patients n1ay have hemoglobin <8 g/dl . In these more severe cases, clinicians should rule out
additional concurrent causes of anemia such as iron deficiency, myelodysplasia, and thalassemia.
such as methotrexate used in autoimmune disorders and cancer. Folinic acid would not be helpful in this patient, w ho is not on methotrexate.
4
25
26
27
(Choice C) Iron supplen1entation may be useful in patients with rheumatoid arthritis and ACD who have co-existing iron-deficiency anemia, which
can result from gastrointestinal bleeding secondary to drug therapy or decreased absorption of dietary iron. If oral supplementation is not
adequately absorbed, as may occur in patients with rheumatoid arthritis, parenteral iron may be needed. However, supplemental iron would not
be helpful in patients such as this who have adequate iron stores.
28
29
30
31
(Choice D) Plasmapheresis is used to reduce levels of circulating autoantibodies in conditions such as Guillain-Barre syndrome, myasthenia
gravis, and thrombotic thrombocytopenic purpura. It has been used historically for rheumatoid arthritis but is no longer recommended and is not a
standard treatment for anemia of chronic disease.
32
(Choice E) Splenectomy can be considered in patients with hypersplenism and hemolytic anemia (eg, autoimmune hemolytic anemia, hereditary
33
spherocytosis ). ACD, however, is not due to hypersplenism or hemolysis, and splenectomy would not be helpful.
34
35
36
38
39
Educational objective :
Anemia of chronic disease (anemia of chronic inflammation) is a common complication of inflammatory conditions such as rheumatoid arthritis .
Management generally involves treating the underlying condition and ruling out concurrent causes of anemia. Anti-TNF-<t agents improve anemia
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
10
11
•
12
not respond. Those who have severe, symptomatic anemia who do not improve with initial measures may need period ic red cell transfusions.
13
•
14
(Choice A ) Folinic acid (leucovorin) is a folic acid derivative. It can be given orally or parenterally to counteract the effects of antifolate drugs
such as methotrexate used in autoimmune disorders and cancer. Foli nic acid would not be helpful in this patient, w ho is not on methotrexate.
.~
(Choice C) Iron supplementation may be useful in patients with rheu matoid arthritis and ACD who have co-existing iron-deficiency anemia, which
17
can result from gastrointestinal bleeding secondary to drug therapy or decreased absorption of dietary iron. If oral supplementation is not
18
adequately absorbed, as may occur in patients with rheumatoid arthritis, parenteral iron may be needed. However, supplemental iron would not
19
be helpful in patients such as this who have adequate iron stores.
20
21
(Choice D) Plasmapheresis is used to reduce levels of circulating autoantibodies in conditions such as Guillain-Barre syndrome, myasthenia
22
gravis, and thrombotic thrombocytopenic purpura. It has been used historically for rheumatoid arthritis but is no longer recommended and is not a
~
standard treatment for anemia of chronic disease.
(Choice E) Splenectomy can be considered in patients with hypersplenism and hemolytic anemia (eg, autoimmune hemolytic anemia, hereditary
25
spherocytosis ). ACD, however, is not due to hypersplenism or hemolysis, and splenectomy would not be helpful.
26
Educational objective :
27
Anen1ia of chronic disease (anemia of chronic inflammation) is a common complication of inflammatory conditions such as rheumatoid arthritis.
28
Management generally involves treating the underlying condition and ruling out concurrent causes of anemia. Anti-TNF-a agents improve anemia
29
of chronic disease in patients w ith rheumatoid arthritis.
30
References
31
• Anaemia in inflammatory rheumatic diseases.
32
33
34
Foundations of Independent Practice
Hen1atology & Oncology
35
Subject
System
36
Copynghl@ ..JWorla A
38
39
T
Anemia of inflammation
Topic
Is
...
https://t.me/USMLEWorldStep3
9
•
10
= .
• -
ltem 38of 39
Question Id: 55&2
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
rim
Tutorial
Lab Yallles
Notes
Calculator
\.!..)
1111
;'
ffiffij
11
•
12
13
•
•
14
~
6
17
The following vignette applies to the next 2 items
A 41-year-old man conies to the physician with a faint skin rash over his upper body. He first noticed it in the spring season, but it worsened
during the summer. The patient has mild itching, but otherwise the rash is asymptomatic. He takes omeprazole for acid reflux but his medical
history is otherwise unremarkable. He does not use tobacco, alcohol , or illicit drugs. The patient has been sexually active with 2 partners during
the last year, and uses condoms on most occasions. The physical examination findings are shown below.
18
19
20
21
22
~
4
25
26
27
28
29
30
31
32
33
34
35
36
37
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
10
11
•
12
13
•
14
.~
17
18
19
20
21
22
~
25
26
27
28
29
30
31
32
33
Item 1 of 2
34
35
36
37
Which of the following is the most likely diagnosis in this patient?
Q
A. Atopic dermatitis
https://t.me/USMLEWorldStep3
9
•
10
11
•
12
13
•
•
14
~
6
17
18
19
20
21
22
~
4
25
Item 1 of 2
Which of the following is the most likely diagnosis in this patient?
26
27
Q
A. Atopic dermatitis
28
0
0
0
0
B.
29
30
31
32
33
Pityriasis rosea
C. Seborrheic dern1atitis
0 . Secondary syphilis
E.
nnea versicolor
34
35
36
Submit
37
https://t.me/USMLEWorldStep3
9
•
10
11
•
12
13
•
14
.~
17
18
19
20
21
22
~
25
Item 1 of 2
Which of the following is the most likely diagnosis in this patient?
26
27
A. Atopic dermatitis (7°A>)
28
B.
Pityriasis rosea (7%)
29
30
C. Seborrheic dern1atitis (2°A>)
31
0. Secondary syphilis (2o/o)
32
33
E.
nnea versicolor (81°/o)
34
35
36
Omitted
37
Correct answer
11 .. 81 %
L!!!. Answered correctly
IT\
\.::J
12 secs
Time Spent
https://t.me/USMLEWorldStep3
03/26/2020
• Last Updated
9
•
10
= .
• -
ltem 38of 39
Question Id: 55&2
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
1111
;'
rim
ffiffij
Calculator
11
•
•
•
12
Tinea versicolor (TV) is a non-invasive fungal infection of the skin caused by M a/assezia species (Ma/assezia furfur, Ma/assezia g/obosa,
13
Ma/assezia sympodialis). Clinical findings are u sually very characteristic and include multiple, often coalescing, small circular m aculae that m ay
14
vary in color (white, pink, or brown). The rash is typically more prominent in the summer as the organism inhibits pigment transfer to keratinocytes
~
6
and makes the affected skin paler than the unaffected tanned skin. Lesions may occasionally exhibit hyperpigmentation compared to surrounding
skin due to a localized mild inflammatory response.
17
Other than cosmetic effects, TV is usually asymptomatic, although mild pruritus m ay be present. Typically, the lesions are located on the upper
18
trunk, but the rash may also involve the upper arms, neck, and abdomen . TV diagnosis can be confirmed with a potassium hydroxide (KOH)
19
preparation showing hyphae and yeast.
20
21
22
~
4
(Choice A) Atopic dermatitis (eczema) typically affects the extremities and produces scaling and severe pruritus.
(Choice B) Pityriasis rosea is an acute inflamn1atory (presumed post-viral) rash characterized by an initial "herald patch" on the trunk that is
followed by smaller pink/tan lesion s on the trunk and proximal extremities.
(Choice C) Seborrheic demiatitis is an inflammatory disorder characterized by erythematous patches with oily scales, predominantly involving
25
areas with many sebaceous glands ( especially the face and scalp). It is also associated with A4a/assezia species, though the exact
26
pathophysiology is unclear.
27
28
(Choice D) Secondary syphilis causes widespread mucocu taneous lesions. It has a highly variable appearance, but typical lesions are
erythematous or pale pink macules that predominantly involve the flexor surfaces of the extremities as well as the p alms and soles.
29
30
Educational objective:
31
Tinea versicolor is a non-invasive fungal infection of the skin characterized by m ultiple, often coalescing, small circular maculae that may vary in
32
color (white, pink, or brown). It is often more apparent in the spring and su mmer months. Diagnosis is confirmed by potassium hydroxide
33
34
35
preparation of skin scrapings showing yeast and hyphae.
References
• Superficial fungal infections.
36
37
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
•
10
=
ltem 39of 39
Question Id: 5563
. ~ Mart<
\
<]
C>
~~
G)
il
'!,·
Previous
Next
Fun Screen
Tutorial
Lab varues
Notes
11
•
12
Item 2 of 2
13
•
•
W hich of the following is the best treatment for this patient?
14
~
0
0
0
0
0
6
17
18
19
20
21
A. Intramuscular penicillin
8 . Oral erythromycin
C. Oral griseofulvin
D. Topical corticosteroids
E.
Topical ketoconazole
22
~
Submit
4
25
26
27
28
29
30
31
32
33
34
35
36
37
T
https://t.me/USMLEWorldStep3
= ,
Calculator
Reverse Color
~
@
Text Zoom
Settings
9
•
= .
• -
10
ltem 39of 39
Question Id: 55&3
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
1111
;'
rim
ffiffij
Calculator
11
•
12
Item 2 of 2
13
•
•
W hich of the following is the best treatment for this patient?
14
~
17
8 . Oral erythromycin (0%)
18
C. Oral griseofulvin (10o/o)
A. Intramuscular penicillin (1 °/o}
6
19
D. Topical corticosteroids (6%)
20
E.
21
Topical ketoconazole (81°/o)
22
~
4
Omitted
25
Correct answer
26
E
II,,
I.!.!!..
81%
(T\ 04 secs
Answered correctly
1...::.,1
n me Spent
•
03/26/2020
Last Updated
27
28
Explanation
29
30
The treatment of choice for patients with tinea versicolor is topical anti-fungal therapy. Any anti-yeast topical agent (eg, selenium sulfide,
31
terbinafine, clotrimazole, ketoconazole) can be used . The success rate w ith topical anti-fungal agents exceeds 80°/o.
32
With extensive disease or recalcitrant infection, oral antifungals (ketoconazole, itraconazole, or fluconazole) are preferred. Topical terbinafine is
33
effective, but oral terbinafine and oral griseofulvin are ineffective (Choice C).
34
(Choice A) Intramuscular benzathine penicillin G is used for the treatment of primary, secondary, and early latent syphilis.
35
36
(Choice B) Oral erythromycin has been advocated for use in patients w ith pityriasis rosea. However, evidence for this practice is mixed and it is
37
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings
9
•
= .
• -
10
ltem 39of 39
Question Id: 55&3
•\
~
Mart<
<]
C>
Previous
Next
r,
L .J
Fun Screen
I'>\
•!
m,
Tutorial
Lab Yallles
Notes
\.!..)
11111
;'
rim
ffiffij
Calculator
11
•
12
Omitted
13
•
•
11 ..
l!!!..
Correct answer
14
E
~
81 %
ri\ 04 secs
Answered correctty
I...::) Time Spent
¢=l 03/26/2020
l::!.I Last Updated
6
Explanation
17
18
19
The treatment of choice for patients with tinea versicolor is topical anti-fungal therapy. Any anti-yeast topical agent (eg, selenium sulfide,
20
terbinafi ne, clotrimazole, ketoconazole) can be used. The success rate w ith topical anti-fungal agents exceeds 80°/o.
21
W ith extensive disease or recalcitrant infection, oral antifungals (ketoconazole, itraconazole, or fluconazole) are preferred. Topical terbinafine is
22
effective, but oral terbinafine and oral griseofulvin are ineffective (Choice C).
~
(Choice A) Intramuscular benzathine penicillin G is used for the treatment of primary, secondary, and early latent syphilis.
4
(Choice B) Oral erythromycin has been advocated for use in patients w ith pityriasis rosea. However, evidence for this practice is mixed and it is
25
not currently recommended.
26
(Choice D) Topical corticosteroids are commonly used in patients with eczema and other non-infectious inflammatory dermatoses.
27
28
Educational objective:
29
The treatment of choice for tinea versicolor is topical anti-fungal therapy.
30
References
31
• Pityriasis versicolor:
32
a systematic review of interventions.
33
34
Foundations of Independent Practice
Dermatology
Tinea
35
Subject
System
Topic
36
C
I@
37
T
https://t.me/USMLEWorldStep3
,
Reverse Color
~
~
Text Zoom
~
~
Settings