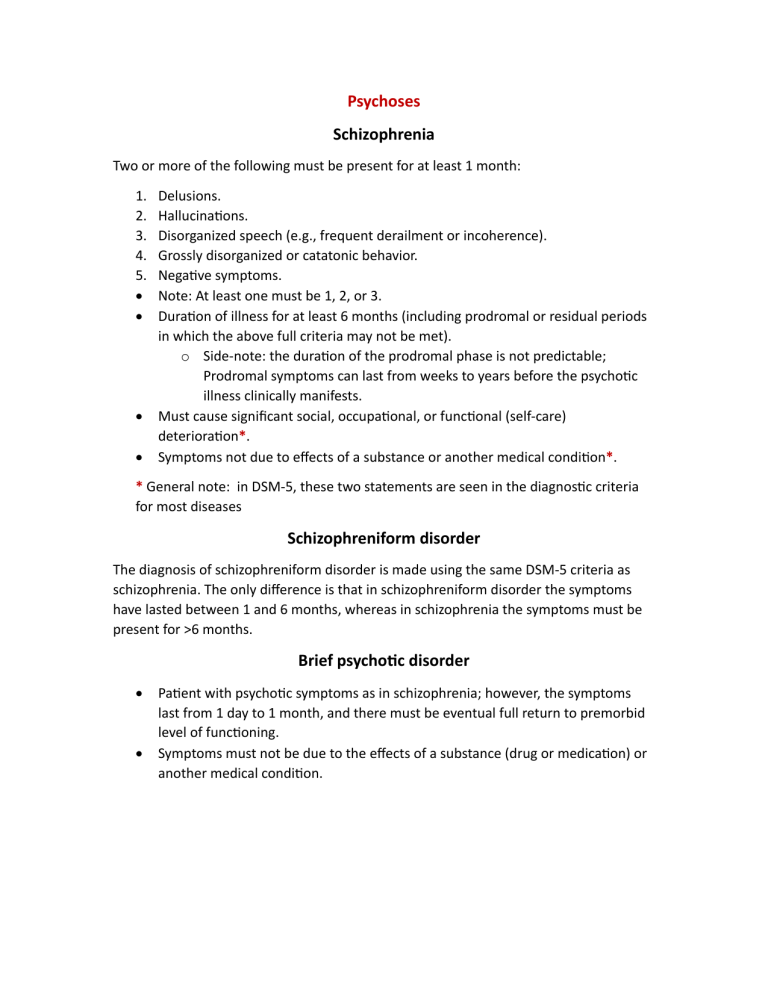
Psychoses Schizophrenia Two or more of the following must be present for at least 1 month: 1. 2. 3. 4. 5. • • • • Delusions. Hallucinations. Disorganized speech (e.g., frequent derailment or incoherence). Grossly disorganized or catatonic behavior. Negative symptoms. Note: At least one must be 1, 2, or 3. Duration of illness for at least 6 months (including prodromal or residual periods in which the above full criteria may not be met). o Side-note: the duration of the prodromal phase is not predictable; Prodromal symptoms can last from weeks to years before the psychotic illness clinically manifests. Must cause significant social, occupational, or functional (self-care) deterioration*. Symptoms not due to effects of a substance or another medical condition*. * General note: in DSM-5, these two statements are seen in the diagnostic criteria for most diseases Schizophreniform disorder The diagnosis of schizophreniform disorder is made using the same DSM-5 criteria as schizophrenia. The only difference is that in schizophreniform disorder the symptoms have lasted between 1 and 6 months, whereas in schizophrenia the symptoms must be present for >6 months. Brief psychotic disorder • • Patient with psychotic symptoms as in schizophrenia; however, the symptoms last from 1 day to 1 month, and there must be eventual full return to premorbid level of functioning. Symptoms must not be due to the effects of a substance (drug or medication) or another medical condition. Schizoaffective disorder • • • • Meet criteria for either a major depressive or manic episode during which psychotic symptoms consistent with schizophrenia are also met. Delusions or hallucinations for 2 weeks in the absence of mood disorder symptoms (this criterion is necessary to differentiate schizoaffective disorder from a mood disorder with psychotic features). o Note: psychotic symptoms are dominant; they develop first and remit last[1]. Mood symptoms present for a majority of the psychotic illness. Symptoms not due to the effects of a substance (drug or medication) or another medical condition. Delusional disorder • • • One or more delusions for at least 1 month. Does not meet criteria for schizophrenia. Functioning in life not significantly impaired, and behavior not obviously bizarre. Mood disorders Major Depressive disorder A. Five (or more) of the following symptoms have been present during the same 2 week period and represent a change from previous functioning; at least one of the symptoms is either (1) depressed mood or (2) loss of interest or pleasure (note: the two major features) 1. Depressed mood most of the day, nearly every day, as indicated by either subjective report (e.g., feels sad, empty, hopeless) or observation made by others (e.g., appears tearful). (Note: In children and adolescents, can be irritable mood.) 2. Markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day (as indicated by either subjective account or observation.) (Note: “do you still enjoy the activities and hobbies you used to enjoy?”, or “do they alleviate the sadness or boredom for you like they used?”) 3. Significant weight loss when not dieting or weight gain (e.g., a change of more than 5% of body weight in a month), or decrease or increase in appetite nearly every day. (Note: In children, consider failure to make expected weight gain.) 4. Insomnia or hypersomnia (note: less typical) nearly every day. 5. Psychomotor agitation or retardation nearly every day (observable by others, not merely subjective feelings of restlessness or being slowed down). 6. Fatigue or loss of energy nearly every day. 7. Feelings of worthlessness or excessive or inappropriate guilt (which may be delusional) nearly every day (not merely self-reproach or guilt about being sick). 8. Diminished ability to think or concentrate, or indecisiveness, nearly every day (either by subjective account or as observed by others). 9. Recurrent thoughts of death (not just fear of), recurrent suicidal ideation without a specific plan, or a suicide attempt or a specific plan for committing suicide. B. The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning. C. The episode is not attributable to the physiological effects of a substance or to another medical condition (note: e.g., an endocrinopathy) D. The occurrence of the major depressive episode is not better explained by schizoaffective disorder, schizophrenia, schizophreniform disorder, delusional disorder, or other specified and unspecified schizophrenia spectrum and other psychotic disorders. E. There has never been a manic episode or a hypomanic episode (note: as this would turn it into bipolar affective disorder) Manic Episode A- Distinct period of abnormally and persistently elevated, expansive, or irritable mood, lasting at least 1 week. B- During the period of mood disturbance three (or more) of the following symptoms have persisted (four if the mood is only irritable) and have been present to a certain degree& represent a noticeable change from usual behavior. 1. Inflated self-esteem or grandiosity. 2. Decreased need for sleep (e.g., feels rested after only 3 hours of sleep) (note: NOT insomnia; rather, it is that all of the sudden this patient just does not need to sleep) 3. More talkative than usual or pressure to keep talking 4. Flight of ideas or subjective experience that thoughts are racing. 5. Distractibility (i.e., attention too easily drawn to unimportant or irrelevant external stimuli) 6. Increase in goal-directed activity (either socially, at work or school, or sexually) psychomotor agitation. 7. Excessive involvement in pleasurable activities that have a high potential for painful consequences (e.g. Engaging in unrestrained buying sprees, sexual indiscretions, or foolish business investments). C- The mood disturbance is sufficiently severe to cause marked impairment in social or occupational functioning or to necessitate hospitalization to prevent harm to self or others, or there are psychotic features. D- The episode is not attributable to the physiological effects of a substance (note: commonly stimulants) or to another medical condition. Anxiety disorders Panic disorder • • • Recurrent, unexpected panic attacks without an identifiable trigger. One or more of panic attacks followed by ≥1 month of continuous worry about experiencing subsequent attacks or their consequences, and/or a maladaptive change in behaviors (e.g., avoidance of possible triggers). Not caused by the direct effects of a substance, another mental disorder, or another medical condition. Agoraphobia • • • • • Intense fear/anxiety about more than two situations due to concerns of difficulty escaping or obtaining help in case of panic or other humiliating symptoms: 1. Outside of the home alone. 2. Open spaces (e.g., bridges). 3. Enclosed places (e.g., stores). 4. Public transportation (e.g., trains). 5. Crowds/lines. The triggering situations cause fear/anxiety out of proportion to the potential danger posed, leading to endurance of intense anxiety, avoidance, or requiring a companion. This holds true even if the patient suffers from another medical condition such as inflammatory bowel disease (IBS) which may lead to embarrassing public scenarios. Symptoms cause significant social or occupational dysfunction. Symptoms last ≥6 months. Symptoms not better explained by another mental disorder. Specific phobia • • • • • • Persistent, excessive fear elicited by a specific situation or object which is out of proportion to any actual danger/threat. Exposure to the situation triggers an immediate fear response. Situation or object is avoided when possible or tolerated with intense anxiety. Symptoms cause significant social or occupational dysfunction. Duration ≥6 months. Symptoms not solely due to another mental disorder, substance (medication or drug), or another medical condition. Social anxiety disorder The diagnostic criteria for social anxiety disorder (social phobia) are similar to specific phobia except the phobic stimulus is related to social scrutiny and negative evaluation. The patients fear embarrassment, humiliation, and rejection. This fear may be limited to performance or public speaking, which may be routinely encountered in the patient’s occupation or academic pursuit. Generalized anxiety disorder (gad) • • • • • Excessive, anxiety/worry about various daily events/activities ≥6 months. Difficulty controlling the worry. Associated ≥3 symptoms: restlessness, fatigue, impaired concentration, irritability, muscle tension, insomnia. Symptoms are not caused by the direct effects of a substance, or another mental disorder or medical condition. Symptoms cause significant social or occupational dysfunction. Obsessive-compulsive disorder (OCD) • • • • Experiencing obsessions and/or compulsions that are time-consuming (e.g., >1 hr/day) or cause significant distress or dysfunction. Obsessions: Recurrent, intrusive, anxiety-provoking thoughts, images, or urges that the patient attempts to suppress, ignore, or neutralize by some other thought or action (i.e., by performing a compulsion). Compulsions: Repetitive behaviors or mental acts the patient feels driven to perform in response to an obsession, or a rule aimed at stress reduction or disaster prevention. The behaviors are excessive and/or not realistically connected to what they are meant to prevent. Not caused by the direct effects of a substance, another mental illness, or another medical condition. Posttraumatic stress disorder (PTSD) and acute stress disorder • • • Note: 4 major symptoms • • • • • Exposure to actual or threatened death, serious injury, or sexual violence by directly experiencing or witnessing the trauma. o Note: PTSD and a grief reaction should not be mistaken; it has to be a traumatic event, e.g., death has to be due to an accident or violence and not from natural causes [Dr. Mahmoud] Recurrent intrusions of re-experiencing the event via memories, nightmares, or dissociative reactions (e.g., flashbacks); intense distress at exposure to cues relating to the trauma; or physiological reactions to cues relating to the trauma. Active avoidance of triggering stimuli (e.g., memories, feelings, people, places, objects) associated with the trauma. At least two of the following negative cognitions/mood: dissociative amnesia, negative feelings of self/others/world, self-blame, negative emotions (e.g., fear, horror, anger, guilt) (note: + worthlessness), anhedonia, feelings of detachment/ estrangement, inability to experience positive emotions. At least two of the following symptoms of increased arousal/reactivity: hypervigilance, exaggerated startle response, irritability/angry outbursts, impaired concentration, insomnia. Symptoms not caused by the direct effects of a substance or another medical condition. Symptoms result in significant impairment in social or occupational functioning. The presentation differs in children. PTSD The symptoms last for at least a month May occur immediately after the trauma or with delayed expression ASD Symptoms last for less than 1 month The onset of symptoms occurs within 1 month of a trauma Others Substance abuse Abuse is a pattern of substance use leading to impairment or distress for at least 1 year with one or more of the following manifestations: 1. 2. 3. 4. Failure to fulfill obligations at work, school, or home Use in dangerous situations (i.e., driving a car) Recurrent substance-related legal problems Continued use despite social or interpersonal problems. Substance Use Disorder ≥2 of the following, occurring within a 12-month period 1. 2. 3. 4. 5. Taking the substance in larger amounts or for longer than you're meant to Wanting to cut down or stop using the substance but not managing to Spending a lot of time getting, using, or recovering from use of the substance Cravings and urges to use the substance Not managing to do what you should at work, home, or school because of substance use 6. Continuing to use, even when it causes problems in relationships 7. Giving up important social, occupational, or recreational activities because of substance use 8. Using substances again and again, even when it puts you in danger 9. Continuing to use, even when you know you have a physical or psychological problem that could have been caused or made worse by the substance 10. Needing more of the substance to get the effect you want (tolerance) 11. Development of withdrawal symptoms, which can be relieved by taking more of the substance Autism spectrum disorder A. Persistent deficits in social communication& social interactions • Deficits in social-emotional reciprocity • Deficits in nonverbal communicative behaviors used for social interactions. • Deficits in developing, maintaining, understanding relationships B. Restricted, repetitive patterns of behavior, interests or activities • Stereotyped or repetitive motor movements, use of objects or speech • Insistence on sameness (e.g., distress to changes, difficulties with transition, same food, etc.) • Hyper or hypo reactivity to sensory input or unusual interests in sensory aspects of environment. C. Symptoms cause clinically significant impairment in social, occupational functioning. D. These disturbances are not better explained by intellectual disability or global developmental delay. E. Symptoms must be present in the early developmental period.