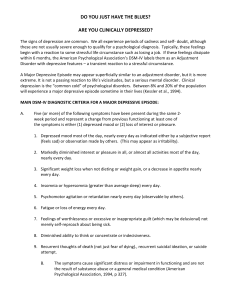
Psychiatry: Top 5 Cases Kishwar Basith, MS4, Class of 2024 Consult information: depression and suicidal ideation Mr. Joe Smith is a 20 y/o male with no significant PMH and substance history of remote marijuana use presents to the ED c/o suicidal ideations x1 day. Case 1 • He was brought to the ED by his roommate who has become concerned about his behavior and saw a gun on his nightstand this morning. Pt denies mental health history or any psychiatric hospitalizations. • During the interview, he notes that 6 months ago his girlfriend of 2 years died suddenly. Initially, he felt quite down but over the past 3 weeks he has been experiencing the following symptoms: he has been sleeping 10-12 hours per day, has low energy, has not been interested in working out, has noticed difficulty focusing on studies, eating only 1-2 small meals per day. In addition, he has been feeling depressed. He also relays that for the past week he has been hearing a voice in his head telling him he is worthless and a failure and commanding that he kill himself. • Of note, the patient has not been to class in 2 weeks due to “feeling too low.” He expresses feeling at fault for the death of his girlfriend because she died in a car accident on the way to pick up food for the two of them. The patient notes that since the loss of his girlfriend he has occasionally wished that he were dead so that he could be with her again. However, over the past day or so the patient states he has been thinking about ”listening to the voice in his head and killing himself.” On further questioning, the patient notes that yesterday evening when he went back home to visit his family, he took the gun and ammunition from his Father’s lock box and is now storing it in his dorm room. • ROS is significant for weight change (loss of 10 lbs in 6 months), decreased appetite. Otherwise negative aside from the symptoms mentioned in the HPI. • Medical History: no significant medical history, no current medications, UTD on immunizations, NKDA • Developmental History: full term birth, no prolonged hospitalizations during childhood/adolescence, no noted developmental delays, reached all developmental milestones on appropriate timeline • Psychiatric History: no significant history, no history of psychiatric hospitalization or previous suicide attempts, does not follow with a psychiatrist or therapist • Substance Use History: remote history of marijuana use, social alcohol use – 1-2 beers weekly, denies use of other substances • Family History: mother –depression, paternal uncle – opioid use disorder with 2 unsuccessful attempts at treatment; no other history of mental illness, substance use disorder, or suicidality in family History • Social History: born and raised in Detroit, MI, grew up with Mom (Eileen) and Dad (Chris), main caretaker was Mom and a part-time nanny for about 5 years in childhood, Mom works as a high school principal, Dad works as an engineer at Ford Motor, no siblings, describes relationship with parents as “good but sometimes stressful due to pressure to excel”, two best friends (one at university, one from childhood), no history of childhood trauma • Not currently in a relationship, was in a long-term monogamous relationship (2 years) with girlfriend (Natalie) before her death. She died 6 months ago in a car accident. • Currently in school at Wayne State University (Junior year) – studying criminology, had a 3.95 GPA at the end of last semester, notes that this semester he has been averaging C’s on most of his assignments/tests and has not been to class in ~2 weeks. • No significant legal history • No history of military service • Currently lives on campus in a dorm (with one roommate), visits home at least once per week because “his parents get angry if he does not see them weekly” • Support network includes his two best friends (though he notes that one of them moved to Texas for school and they have not had much contact in the past year) and his parents • Hobbies include working out (he used to work out every day but has not felt up to it recently), reading Sci-Fi Physical Exam (Mental Status Exam) • Appearance: 21 y/o male, appears stated age, white skin complexion, numerous freckles on face, medium length dark blond hair and brown eyes, thin body habitus, wearing sweatpants and wrinkled t-shirt, fair hygiene and unkempt grooming, sitting slumped in chair, facial expression appears sad, does not look up upon interviewer entering the room • Attitude/Behavior: cooperative but slow to answer questions, tearful throughout encounter • Psychomotor: no psychomotor retardation or agitation • Eye contact: poor eye contact, makes minimal eye contact with interviewer • Movement/Tremor/Mannerisms: maintains eye contact on his lap or the floor for majority of interview, frequently covers face with hands and adjusts hood on sweatshirt • Speech: slow rate, monotonous rhythm with little inflections, soft volume, articulates clearly, little spontaneity to speech – briefly answers questions without expounding • Mood: “okay” • Affect: stable affect, constricted range – remained sad/depressed throughout entire conversation, overall depressed affect, appropriate to content • Thought Content: depressive cognitions – frequently spoke of worthlessness, guilt over death of girlfriend, and hopelessness as related to future; frequent suicidal ideations with plan and means (firearm in dorm); no homicidal ideations; depressive delusions suggested by patient stating on multiple occasions that he is at fault for his girlfriend’s death and that because of this he deserves to be dead • Thought Process: appears slowed, easily distracted and loses train of thought; but overall coherent, logical, and goal directed • Perceptions: does not appear to be responding to internal stimuli; however, pt does describe an internal voice that he hears multiple times per day telling him he is worthless, a failure, and commanding him to kill himself – suspect command hallucinations Physical Exam (Mental Status Exam) Continued… . • Suicidal Ideations/Homicidal Ideations: suicidal ideations present – mentioned on multiple occasions during the interview that he would be better off dead and that he has been having thoughts of shooting himself recently; his plan is to go home and wait until his roommate leaves to shoot himself with his Dad’s gun; no homicidal ideations • Orientation: awake, alert, and oriented to person, place, time, and situation • Cognition: mild impairment of immediate and recent memories (unable to correctly recall more than 3 digits from digit span, only able to recall 1 of 3 random object), remote memory intact • Judgment: fair judgment as evidenced by patient’s concern that he has a mental illness • Insight: poor insight as evidenced by patient taking father’s firearm and not seeking help of his own volition despite thoughts of suicide and lethal means Labs/Imagin g • CT head: unremarkable • Labs: • UA, CBC, CMP – all within normal limits • Thyroid tests and urine drug screen - pending • Based on the HPI and MSE what are 3 differential diagnoses that fit this patient’s presentation? What is your top differential at this time? Differential Diagnoses • Major depressive episode with psychotic features • Schizoaffective disorder • Prolonged grief vs normal bereavement • If Mr. Smith’s lab work comes back with thyroid abnormalities and positive for amphetamines, are there other differential diagnoses you would want to add? • Mood disorder due to a medical condition • Substance-induced mood disorder • If you suspect Mr. Smith has MDE/MDD, what is your management strategy? • In the ED – assess safety of patient (self) and others, and patient’s ability to care for themselves • At this time, Mr. Smith is depressed, actively suicidal, has a plan in place, and the means to complete his plan – he is NOT safe to release home and should be placed on suicide precautions while in the ED, 1:1 sitter, and admitted to inpatient psychiatry for further assessment and management Management • Longer-term management – treatment goal is remission • Biopsychsocial model • Biological: • Antidepressant (i.e. SSRI or SNRI) for depression, plus… • Antipsychotic - because he also has psychotic features (depressive delusions and command hallucinations) • Psychological: psychotherapy should be combined with pharmacological treatment • Social: what social factors can be addressed to aid his recovery? Family support, safe storage or getting rid of firearms, minimize school stressors for the time being, support from friends, physical activity, nutrition • General Principles • Assess/ closely monitor patients presenting with depression with psychotic features for – suicidal ideations, suicidal plan, and psychotic symptoms that put them at risk (i.e. auditory hallucinations commanding patient to kill themselves) • First line treatment • Antidepressant plus antipsychotic • Some combinations that have demonstrated efficacy in trials when compared to monotherapy of antidepressants, antipsychotics, or placebo include Guidelines • • • • Sertraline (Zoloft) + Olanzapine (Zyprexa) Fluoxetine (Prozac) + Olanzapine Venlafaxine (Effexor) + Quetiapine (Seroquel) Other combos acceptable too • Treat for 4-6 weeks at target drug doses before assessing effectiveness, monitor for adverse effects and change regimen as needed • Psychotherapy • ECT may be used for severe presentations for patients at imminent risk of harm, severe suicidality, or malnutrition 2/2 food refusal or resistant/refractory to previous treatment attempts • Depression with psychotic features resistant to treatment • Add lithium to regimen • Specific forms of psychotherapy – i.e. Acceptance and Commitment therapy Case 2 • 27-year-old man in law school presents to PCP’s office d/t inc stress. Difficulty sleeping at night, fatigues, and has muscle tension. Symptoms have been persistent over the years but have worsened recently. Has a girlfriend and plans to get married after law school. Has been worried about boards, school, wedding planning, and staying connected with his parents. He had a difficult childhood, and his parents got divorced. He worries that his own marriage may end in divorce. He worries about not landing a job and his student loans. All these stresses have prevented him from performing as well as he wants to on his schoolwork. He denies any other psychiatric symptoms, as well as psychiatric history or medical problems. Denies any alcohol or drug use. Denies family history of psychiatric history. Mental Status Exam • Casually dressed w/ good hygiene • Cooperative but avoids eye contact • Appears to choke on his words, then has periods of fast but not pressured speech • Trembling hands, and tightly crosses the fingers of both hands • Restless, shaky, taps his foot on the floor • Mood is reported as overwhelming • Affect is anxious and restless • Thought process is linear, logical, and goal directed w/ a preservation of future worries • Thought content is focused on how he will manage all the worries of his life • No SI or HI, and no auditory or visual hallucinations Labs/Imaging • UDS • Vitals Diagnosis • Diagnostic Criteria for Generalized Anxiety Disorder • Persistent, excessive, uncontrollable anxiety/worry for 6+ months • Struggles to control the worry • At least 3 of the following: • • • • • • Disrupted Sleep Fatigue Impaired Concentration Irritability Muscle Tension Restlessness • Sx not better explained by another psychiatric disorder • Not caused by direct effects of a substance or medication or medical illness • Clinically significant distress or impairment of psychosocial functioning Treatment • Most effective: Two-pronged approach • Psychotherapy: Cognitive behavioral therapy • Identifying and changing dysfunctional thought patterns in order to positively impact one’s emotions and behaviors • First-line meds: SSRIs • If no response to first one, switch to another • Consider SNRIs or TCAs • Full benefit can be seen after 4 to 8 weeks • Second-line meds for augmentation: benzodiazepines, hydroxyzine, buspirone, mirtazapine • Word of caution with benzos: addictive, sedative, cognitive impairment • Fall risk in the elderly • May develop tolerance and experience withdrawal or rebound anxiety Case 3: Bipolar Disorder • Overview: • Mood • Energy • Activity • Sleep • Cognition • Behavior Definitions • Manic episode • ≥ 7 days • Elevated, expansive, or irritable mood • + ≥ 3 of: • • • • • • • Inflated self-esteem Decreased need for sleep Pressured speech Flight of ideas Distractibility Increased goal-directed activity Excessive risky behavior/activities • Hypomanic episode • Same as above except ≥ 4 consecutive days and absent significant impairment in functioning/hospitalization Mnemonic • DIG FAST = • • • • • • • Distractibility Irresponsibility Grandiosity Flight of ideas Activity increase Sleeplessness Talkativeness Definitions, continued • Major depressive episode • ≥ 2 weeks of ≥ 5 of: • • • • • • • • • Depressed mood Anhedonia Change in appetite Feelings of worthlessness/guilt Insomnia/hypersomnia Diminished concentration Psychomotor agitation/retardation Fatigue Suicidal ideation • (at least one of five must be anhedonia or depressed mood) Mnemonic 2 • SIG E CAPS = • • • • • • • • Sleep Interest Guilt Energy Concentration Appetite Psychomotor Suicide Bipolar I • At least one manic episode • Major depressive and hypomanic episodes often accompany, but are not required for diagnosis Bipolar II • At least one hypomanic episode AND one major depressive episode • Absence of veritable mania required to make diagnosis Rapid Cycling • ≥ 4 episodes of depression, mania, or hypomania within a single year Cyclothymia • Persistent instability of mood with periods of depression and hypomania • Symptoms not severe or persistent enough to diagnose bipolar • ≥ 2 years of symptoms, present at least half the time, never absent more than 2 months at a time Labs • UDS • • • • • • Alcohol Phencyclidine Amphetamine Cocaine Benzodiazepines Glucocorticoids Differential • Bipolar I • Bipolar II • Cyclothymia • Substance-/medication-induced bipolar and related disorders • Bipolar and related disorders due to another medical condition • Endocrine disorders (e.g., Cushing disease) • Autoimmune disorders (e.g., MS) • Neurologic disorders (e.g., stroke, traumatic brain injury, delirium) Management • Assess for suicidal ideation and acute mania • Both require hospitalization • Acute mania • Lithium • Valproic acid • Antipsychotics (olanzapine, quetiapine, risperidone, haloperidol) • Acute depression • Atypical antipsychotics (quetiapine, lurasidone) PLUS mood stabilizer (lithium, valproic acid) Management, continued • Long-term maintenance • Non-pharmacologic: psychotherapy (e.g., CBT) • Pharmacologic • • • • • • • • Lithium Valproic acid Lamotrigine Quetiapine Aripiprazole Olanzapine Carbamazepine Oxcarbazepine • Note: antidepressants can precipitate a manic episode in those with bipolar Case 4 • Patient is a 34-year-old woman who presents to the ED with a chief complaint of "heart palpitations". The patient states that she was in her living room watching tv when out of nowhere her heart started racing. Additional symptoms include chest pain, numbness in her fingertips, and shortness of breath. The patient states that she "feels like she is going to die". She says she has had similar episodes a few times in the past and that the symptoms resolve on their own. History PMH: Asthma PSH: C-section Medications: Albuterol inhaler as needed Allergies: Peanuts Immunizations: Up to date FH: Depression, hypertension, CAD Social History: smokes ½ ppd, denies any alcohol, marijuana, or any other recreational drug use. She works at a tech company and is seated at her desk most of the day. She denies any exercise and says she mostly eats fast food. Physical exam Vital signs and general physical examination – To evaluate for hypertension, tachycardia, diaphoresis, dyspnea Non-specific and such as mild tachypnea, cool, clammy skin Labs/Imaging Electrocardiogram – To evaluate for arrhythmia, evidence of coronary artery disease Chemistry panel including calcium – To evaluate for disturbance in fluid or electrolytes Complete blood count with differential Thyroid panel – To evaluate for thyroid disorder or dysfunction Urine pregnancy testing individuals of childbearing age Toxicology screen – To assess for substances such as stimulants, opioids, sedatives (ie, benzodiazepines), or marijuana Differential Myocardial Infarction Pulmonary Embolism Asthma exacerbation Panic Attack MI • myocardial ischemia • High risk in older men, smokers, patients with history of CAD • Increased troponin • electrocardiographic (ECG) changes • chest pain, shortness of breath, new heart failure, sudden cardiac arrest, or new changes on an electrocardiogram should have the diagnosis considered • Chest pain > Shortness of breath PE • dyspnea followed by chest pain • Cough • DVT • Wells score (DVT? Tachy? Immobilization? Surgery recently? Hemoptysis? Malignancy?) Tells us about the risk of being an actual PE with 91% specificity. • Wells score <2: Low • >2 and <6: Moderate • >6: HIGH Asthma Exacerbation • worsening asthma symptoms and lung function • patients with a known asthma diagnosis in response to a "trigger" such as viral upper respiratory infection, allergen, air pollution or other irritant exposure, lack of adherence to controller medication, or an unknown stimulus • breathlessness, wheezing, cough, and chest tightness. Panic Disorder discrete episode of intense fear that begins abruptly and lasts for several minutes to an hour patients experience recurrent untriggered panic attacks with one month or more of worry about future attacks, or a maladaptive change in behavior related to the attacks. Presents with non-specific symptoms and labs are usually normal Management • First line: CBT (cognitive behavioral therapy) and or/ Medication (no advantage of one over the other although relapse less common in CBT) • First line med: SSRIs (intubation period of 4-6 weeks) • Patient who cannot last 4-6 weeks take long-acting benzo before bed (clonazepam). After that period, taper down clonazepam • If SSRIs adequate, continue for 12 months or longer • If SSRIs inadequate and no substance use history, add clonazepam to SRI • If SSRIs inadequate and substance use history or benzos inadequate, gabapentin, pregabalin, nortriptyline, mirtazapine Case 5 • 26-year-old woman in medical school with no prior psych Hx referred to your office by the dean of students. Her friends are concerned that she has not been going to classes for over a month. Over the past 6 months, she hasn’t been acting like herself, she’s been more withdrawn, and she doesn’t seem to be doing as well in her classes. When her friends went to go check on her, they were alarmed to see their apartment filthy, aluminum foil taped over all the windows, and the patient kept telling them to leave ‘before they become targets too’. She appears disheveled as though she hasn’t showered or brushed her hair in over a week. She’s holding a notebook to her chest with all the ‘proof of the conspiracy’ written inside. When asked to see the notebook, you see that it is covered in random scribbles. She reports feeling depressed because ‘they will eventually capture her and torture her for information’. She denies changes in sleep or appetite but has been too scared to leave her apartment to get groceries. She used to love playing basketball, but states that she no longer has time as she needs to to ‘protect the secrets.’ Mental Status Exam • Unkempt, poor eye contact, eyes constantly darting around the room • Affect is blunted • Suspicious, asking you several times if ‘you are in on it?’ • Denies hearing voices but you notice her turning to the side and mumbling • Denies using drugs or alcohol because ‘I’ve got to stay sharp and ahead of them!’ • Denies SI and HI Differential Diagnosis • Substance intoxication/withdrawal • Substance or medication induced psychosis • Psychotic disorder d/t other medical condition • Primary psychotic disorder Schizophrenia Diagnostic Criteria • 2+ of the following Sx for at least 1 month • • • • • Delusions Hallucinations Disorganized speech Disorganized or catatonic behavior Negative Symptoms • Significant social/occupational dysfunction • Some Sx required to be present for at least 6 months, can include only negative Sx or less intense positive Sx • Schizoaffective disorder and mood disorder w/ psychotic features need to be ruled out • Condition cannot be d/t a substance or another medical condition Labs/Imaging • USD, med history, serum drug levels, ask about OTC medications and supplements • Screen for endocrinopathies, neurologic diseases • • • • • • Blood glucose UA CBC CMP TSH Pregnancy test Differentiate Further • Mood disorders w/ psychotic features • Psychosis only in the context of mood symptoms (depression/mania/mixed) • Schizoaffective Disorder • Psychotic symptoms occur at least 2 weeks without mood Sx • Mood Sx must also be present for 2 weeks without psychotic Sx • Prognosis: mood disorder w/ psychotic features, schizoaffective, schizophrenia Important Definitions • Active phase: presence of positive and negative symptoms • Catatonia: a neuropsychiatric syndrome that presents w/ 3+ psychomotor Sx • Stupor, catalepsy, waxy flexibility, mutism, negativism, posturing, grimacing, mannerism, stereotypy, agitation, echopraxia, echolalia • Delusions: fixed false beliefs that lack cultural sanctioning • Disorganized speech: expressions of thoughts lacking logical connections • Hallucinations: false perceptions in any sensory modality w/o an external stimulus • Auditory are most common in schizophrenia spectrum disorders, usually in the form of voices • Ideas of reference: misinterpretation of aspects of external environment having particular significance for the patient • Ex: special messages from the TV or radio Important Definitions Continued • Negative Symptoms • • • • • Lack of emotional responses and thought process seen in the general population Decreased expression of emotions Flattening of affect Alogia (decreased spontaneous speech) Avolition (decreased motivation) • Positive Symptoms • • • • • Symptoms experienced by the patient not experienced by others in the population Hallucinations Delusions Ideas of reference Disorganized speech and behavior Treatment • Holistic Approach – Psychoeducation is crucial • Assess the patient’s home life and support system • Provide information to their families and loved ones, and how to manage • Case manager, local community resources • Craft medication regimens tailored to the patient • Atypical antipsychotics: less side effects, increased efficacy w/ negative symptoms • General side effects: metabolic syndrome • Clozapine is most effective BUT is only used after failed trials of two other medications • Agranulocytosis • Olanzapine • Typical Antipsychotics: higher chance of extrapyramidal symptoms (akathisia, dystonias, parkinsonism) • Hyperprolactinemia, tardive dyskinesia • Neuroleptic malignant syndrome: AMS, fever, dysautonomia, muscle rigidity