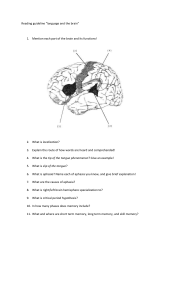
Definitions Chapter 38 o Autonomic Nervous System (ANS): part of the nervous system that is composed of two parts: the sympathetic nervous system and parasympathetic nervous system o Decerebration: Abnormal movement with rigidity characterized by extension of the arms and legs, pronation of the arms, plantar flexion, and opisthotonos (body spasm in which the body is bowed forward). o Decortication: Abnormal motor movement seen in the patient with lesions that interrupt the corticospinal pathways o Electroencephalography (EEG): A diagnostic test that records the electrical activity of the cerebral hemispheres of the brain. The frequency, amplitude, and characteristics of the brain waves are recorded o Glasgow Coma Scale (GCS): A tool used in many acute care settings to establish baseline data in each of these areas: eye opening, motor response, and verbal response. The patient is assigned a numeric score for each of these areas. The lower the score, the lower the patient’s neurologic function o Level of Consciousness (LOC): The degree of alertness or amount of stimulation needed to engage a patient’s attention and can range from alert to comatose o PERRLA: The degree of alertness or amount of stimulation needed to engage a patient’s attention and can range from alert to comatose Chapter 39 o Alzheimer’s Disease (AD): The most common type of dementia that typically affects people older than 65 years. o Agnosia: loss of sensory comprehension, including facial recognition o Amnesia: loss of memory o Anomia: an inability to find words o Aphasia: problems with speech (expressive aphasia) and/or language (receptive aphasia) o Apraxia: inability to use words or objects correctly o Aura: a sensation (visual changes) that signals the onset of a migraine headache or seizure o Bradykinesia/Akinesia: Slow movement / No movement o Dementia: (aka chronic confusional state or syndrome) a general term for progressive loss of brain function and impaired cognition; many types o Dyskinesia: the inability to perform voluntary movement o Epilepsy: a chronic disorder which repeated unprovoked seizure activity occurs o Migraine Headache: a common clinical syndrome characterized by recurrent episodic attacks of head pain that serve no protective purpose o Parkinson Disease (PD): a progressive neurodegenerative disease that affects mobility and is characterized by 4 cardinal symptoms; tremor, muscle rigidity, bradykinesia/akinesia, and postural instability o Seizure: an abnormal, sudden, excessive, uncontrolled electrical discharge of neurons within the brain that may result in a change in LOC o Status epilepticus: medical emergency and is a prolonged seizure lasting longer than 5 minutes or repeated seizures over the course of 30 minutes Chapter 40 o Autonomic Dysreflexia (AD): A potentially life-threatening condition in which noxious visceral or cutaneous stimuli cause a sudden, massive, uninhibited reflex sympathetic discharge in people with high-level spinal cord injury o Dysarthria: difficulty speaking due to slurred speech o Dysmetria: the inability to direct or limit movement o Dysphagia: Difficulty swallowing o Hyperesthesia: increased sensory perception o Hypoalgesia: a decreased sensitivity to pain o Hypoesthesia: decreased sensory perception o Multiple Sclerosis (MS): A chronic disease caused by immune, genetic, and/or infectious factors that affects the myelin and nerve fibers of the brain and spinal cord o Nystagmus: An involuntary condition in which the eyes make repetitive uncontrolled movements o Paraparesis: Weakness that affects only the lower extremities, as seen in lower thoracic and lumbosacral injuries or lesions o Paraplegia: Paralysis that affects only the lower extremities, as seen in lower thoracic and lumbosacral injuries or lesions o Quadriparesis: Weakness involving all four extremities, as seen with cervical cord and upper thoracic injury o Tetraplegia: (AKA Quadriplegia) Weakness involving all four extremities, as seen with cervical cord and upper thoracic injury o Tinnitus: ringing in the ears o Vertigo: dizziness Chapter 41 o Acute Ischemic Stroke: A stroke caused by the occlusion (blockage) of a cerebral or carotid artery by either a thrombus or an embolus o Agnosia: inability to use an object correctly o Amnesia: loss of memory o Aphasia: Problems with speech (expressive aphasia) and/or language (receptive aphasia) o Apraxia: Inability to perform previously learned motor skills or commands; may be verbal or motor o Ataxia: Lack of muscle control and coordination that affects gait, balance, and the ability to walk o Concussion: A traumatic injury to the brain caused by a blow to the head; may or may not result in some period of unconsciousness o Cushing Triad: A classic but late sign of increased intracranial pressure that manifests with severe hypertension, a widened pulse pressure (increasing difference between systolic and diastolic values), and bradycardia o Diplopia: condition where patient has double vision o Dysarthria: Slurred speech caused by muscle weakness or paralysis o Dysphagia: Difficulty swallowing o Embolic Stroke: stroke caused by embolus (dislodged clot) o Hemiparesis: One-sided weakness of the body affecting the arm and/or leg o Hemiplegia: One-sided paralysis of the body affecting the arm and/or leg o Receptive (Wernicke or Sensory) Aphasia: Aphasia that is caused by injury involving the Wernicke area in the temporoparietal area. The patient cannot understand the spoken or written word. Although he or she may be able to talk, the language is often meaningless o Stroke: A neurologic health problem caused by an interruption of perfusion to any part of the brain that results in infarction (cell death) o Thrombotic Stroke: A stroke that is caused by a thrombus (clot) o Transient Ischemic Attack (TIA): A temporary neurologic dysfunction resulting from a brief interruption in cerebral blood flow o Traumatic Brain Injury (TBI): Damage to the brain from an external mechanical force and not caused by neurodegenerative or congenital conditions Brain and Spinal Cord A&P Central Nervous System (CNS): composed of the brain and spinal cord Peripheral Nervous System (PNS): composed of spinal nerves, cranial nerves, and autonomic nervous system Autonomic Nervous System (ANS) o Sympathetic Nervous System (SNS): fight or flight, increase HR and respirations, Epinephrine/Norepinephrine o Parasympathetic Nervous System: rest and digest / feed and breed, digestion, reproduction, slows HR and resps Meninges: form a protective covering of the brain and spinal cord o Dura Mater: Outside layer o Subdural Space: located between the dura mater and the middle layer o Arachnoid: middle layer o Pia mater: innermost layer o Subarachnoid space: between the arachnoid and pia mater, where CSF circulates o Epidural Space: located between the skull and outer layer of the dura mater, extends down the spinal cord Forebrain o Diencephalon: below the cerebrum; made up by thalamus, hypothalamus, epithalamus; relay center of the brain; autonomic nervous control; cognition; connects pathways; regulates emotions o Cerebrum Frontal Lobe Primary motor area (motor cortex); mobility Broca speech center on the dominant side Voluntary eye movement Access to current sensory data; sensory perception Affective response to a situation Behavior regulation Cognition (judgment, ability to develop long-term goals, reasoning, concentration, abstraction) Parietal Lobe Understanding sensory input such as texture, size, shape, and spatial relationships Three-dimensional (spatial) perception Needed for singing, playing musical instruments, and processing nonverbal visual experiences Perception of body parts and body position awareness Taste impulses for interpretation Temporal Lobe Auditory center for sound interpretation Complicated memory patterns Wernicke area for language comprehension Occipital Lobe Primary visual center Cerebellum: receives immediate and continuous info about the condition of the muscles, joints, and tendons o Keep extremity from overshooting intended target o Move from one skilled movement to another in an orderly sequence o Predict distance or gauge the speed with which one is approaching an object o Control voluntary movement o Maintain equilibrium Brainstem o Medulla Cardiac-slowing center Respiratory center Cranial nerve IX, X, XI, and XII and parts of cranial nerve VII, and VIII o Pons Cardiac acceleration and vasoconstriction centers Pneumotaxic center helps control respiratory pattern and rate Cranial nerve V, VI, VII, and VIII o Midbrain Contains cerebral aqueduct or aqueduct of Sylvius Location of periaqueductal gray, which may abolish pain when stimulated Cranial nerve nuclei III and IV Spinal Cord o Controls mobility o Regulates organ function o Processes sensory perception information from the extremities, trunk, and many internal organs o Transmits info to and from the brain Nervous System Cells o Afferent neurons (Sensory neurons): responsible for bringing sensory info from outside world to brain Smells, feelings of pain o Efferent Neurons (Motor neurons): responsible for carrying signals away from the CNS to initiate action o Neuroglia Cells: diverse group of cells that provide developmental physiological and metabolic support for neurons Neuro Assessment Assessment: Recognizing Cues o Patient History o Physical Assessment o Complete Neurological History Mental Status:, consciousness (LOC), cognition (memory and attention) Cranial nerves: test specific CNs related to patient problem Mobility and motor function: involuntary tremors or movements, hand strength (squeeze fingers), cerebral motor or brainstem integrity, posturing Deep tendon reflexes and cutaneous (superficial) reflexes Sensory function: touch discrimination (touch with eyes closed), sharp vs dull, temperature Cerebellar function: Gait and equilibrium (balance with walking, balance with standing with eyes closed), fine coordination of muscle activity (finger to nose to person) Psychosocial Assessment o Responses vary depending on whether condition is acute or chronic o Depression screening tool o Consider cultural and spiritual background Diagnositic Assessment o Labs and Imaging Plain x-rays Cerebral angiography (arteriography) CT scan MRI CT-PET Single Photon Emission CT (SPECT) Magnetoencephalography (MEG) Electromyography (EMG): used to identify nerve and muscle disorders, and spinal cord disease Electroencephalography (EEG): records electrical activity of the cerebral hemispheres Evoked potentials: measure electrical signals to brain generated by touch, sound, or light Lumbar puncture Transcranial doppler ultrasonography Cranial Nerves I: Olfactory o Type: Sensory o Function: Smell II: Optic o Type: Sensory o Function: Central and Peripheral Vision III: Oculomotor o Type: Motor (to eye muscles) o Function: Eye movement; pupil constriction; ciliary muscles IV: Trochlear o Type: Motor o Function: eye movement V: Trigeminal o Type: Both o Function: sensory perception from skin of face and scalp, mucous membranes of mouth and nose; Chewing VI: Abducens o Type: Motor o Function: eye movement VII: Facial o o Type: Both Function: pain and temperature from ear area; deep sensations from face; taste from anterior 2/3 of tongue; muscles of face and scalp; lacrimal, submandibular, and sublingual salivary glands VIII: Vestibulocochlear o Type: Sensory o Function: Hearing; Equilibrium IX: Glossopharyngeal o Type: Both o Function: pain and temperature from ear; taste and sensations from posterior 1/3 of tongue and pharynx; skeletal muscles of throat; parotid glands X: Vagus o Type: Both o Function: Pain and temperature from ear; sensations from pharynx, larynx, thoracic and abdominal viscera; muscles of the soft palate, larynx, and pharynx (swallowing); thoracic and abdominal viscera; cells of secretory glands; cardiac and smooth muscle innervation to the level of splenic flexure XI: Accessory o Type: Motor o Function: Skeletal muscles of pharynx and larynx and sternocleidomastoid and trapezius muscles (swallowing) XII: Hypoglossal o Type: Motor o Function: Skeletal muscles of tongue (swallowing) Level of Consciousness (LOC) The degree of alertness or amount of stimulation needed to engage a patients attention Can range from alert to comatose Alert: awake, engaged, responsive Lethargic: patient is drowsy but easily awakened Stuporous: arousable only with vigorous or painful stimulation Comatose: patient is unconscious and cannot be aroused despite vigorous or noxious stimulation Risk Factors Related to Cerebral Vascular Accident (CVA) AKA Stroke Genetic and environmental risk factors Smoking Obesity HTN DM Elevated cholesterol Substance use disorder (especially cocaine and heavy alcohol consumption) Oral contraceptives in women at risk for CV adverse effects Genetic/Familial predisposition to risk factor also increases stroke risk Transient Ischemic Attack (TIA) Temporary neurologic dysfunction resulting from a brief interruption in cerebral blood flow Symptoms typically resolve within 30 – 60 minutes; can last as long as 24hrs “Warning Sign” Causes o Carotid stenosis o Atherosclerotic plaque buildup o Atrial fibrillation (small clots cause TIAs) S/S o Visual Blurred vision Diplopia Hemianopsia (vision of one or both eyes is affected) Tunnel Vision o Mobility (Motor) Weakness (facial droop, arm or leg drift, hand grasp) Ataxia o Sensory Perception Numbness (face, hand, arm, or leg) Vertigo o Speech Aphasia Dysarthria Assessment o Neurologic assessment o ABCD Assessment Tool A: Age greater than or equal to 60 B: Blood pressure greater than or equal to 140/90 mmHg C: Clinical TIA features (unilateral weakness) D: Duration of symptoms o Labs and Imaging PT/INR aPTT Lipids ECG, CT, MRI, CTA, MRA Treatment/Management o MIS to remove atherosclerotic plaque buildup in the carotid artery o Carotid angioplasty with stenting o Antiplatelet drugs, aspirin or clopidogrel o Reducing high BP, BP medications o Controlling diabetes o Smoking cessation, eating heart healthy foods, increasing mobility and physical activity Hemorrhagic Stroke Vessel integrity is interrupted and bleeding occurs into the brain tissue or into the subarachnoid space Types o Intracerebral Hemorrhage (ICH): bleeding into the brain tissue generally resulting from severe or sustained HTN o Subarachnoid Hemorrhage (SAH): bleeding into the subarachnoid space – space between the pia mater and arachnoid layers of the meninges covering the brain o Aneurysm: abnormal ballooning or blister along a normal artery commonly developing in a weak spot on the artery wall o Arteriovenous Malformation (AVM): angled collection of malformed, thin-walled, dilated vessels without a capillary network (occurs during embryonic development) Causes o Smoking o Obesity o HTN o DM o Elevated cholesterol o Oral contraceptives o Cocaine use o Sedentary lifestyle S/S (General for all strokes) o Sudden confusion or trouble speaking or understanding others o Sudden numbness or weakness of the face, arm, or leg o Sudden trouble seeing in one or both eyes o Sudden dizziness, trouble walking, or loss of balance or coordination o Sudden severe headache with no known cause Assessments o BE FAST o Balance o Eyes (visual changes, blurred vision, nystagmus) o Face droop o Arms/Asymmetry (cant raise arm) o Speech slurred o Time (note time so we know when symptoms started for medication admin reasons) Priority Concerns o Inadequate perfusion to the brain due to interruption of arterial blood flow and possible increase in ICP o Decreased mobility and possible need for assistance to perform ADLs due to neuromuscular or impaired cognition o Aphasia and/or dysarthria due to decreased circulation in the brain (aphasia) or facial muscle weakness (dysarthria) o Sensory perception deficits due to altered neurologic reception and transmission Treatments o Stop bleeding o Monitor ICP for increases o Decrease blood pressure o Manage diabetes o Stop smoking o Healthy lifestyle Ischemic Stroke Caused by the occlusion of cerebral or carotid artery by either a thrombus or an embolus o Thrombotic Stroke: stroke caused by a clot Majority of strokes o Embolic Stroke: stroke caused by a dislodged clot Causes o Smoking o Obesity o HTN o DM o Elevated cholesterol o Oral contraceptives o Cocaine use o Sedentary lifestyle S/S (General for all strokes) o Sudden confusion or trouble speaking or understanding others o Sudden numbness or weakness of the face, arm, or leg o Sudden trouble seeing in one or both eyes o Sudden dizziness, trouble walking, or loss of balance or coordination o Sudden severe headache with no known cause Assessments o BE FAST o Balance o Eyes (visual changes, blurred vision, nystagmus) o Face droop o Arms/Asymmetry (cant raise arm) o Speech slurred o Time (note time so we know when symptoms started for medication admin reasons) Priority Concerns o Inadequate perfusion to the brain due to interruption of arterial blood flow and possible increase in ICP o Decreased mobility and possible need for assistance to perform ADLs due to neuromuscular or impaired cognition o Aphasia and/or dysarthria due to decreased circulation in the brain (aphasia) or facial muscle weakness (dysarthria) o Sensory perception deficits due to altered neurologic reception and transmission Treatments/management o Aspirin use when appropriate Antiplatelet therapy o Blood pressure control BP meds, exercise o Cholesterol management Statins o Smoking cessation o Exercise, healthy diet o Alteplase: after CT/MRI confirm that there is no bleed causing stroke Monitor for bleeding after o Elevate HOB Education o S/S of stroke o BE FAST o Medication information o Avoid smoking, alcohol o Increase daily exercise and healthy diet and lifestyle o Physical therapy Alzheimer’s Disease The most common type of dementia that typically affects people older than 65 years Cause o Genetic and environmental factors o Possibly viral Assessment o Psychosocial Cognitive changes and biochemical and structural dysfunctions affect personality and behavior o Laboratory and Imaging Beta amyloid protein in spinal fluid Genetic testing for apolipoprotein E4 CT and MRI: can show brain degeneration, atrophy, lesions Progression o Steady and gradual decline of cognitive, mobility, and ADL function from mild through severe stages; patients usually die from complications of immobility Risk Factors o Female o Over 65 years of age o Down syndrome o Traumatic brain injury (veterans, PTSD) S/S o Early (Mild), or Stage I (First Symptoms up to 4 Years) Independent in ADLs Denies presence of symptoms Forgets name; misplaces household items Has short-term memory loss and difficulty recalling new information Shows subtle changes in personality and behavior Loses initiative and less engaged in social relationships Has mild impaired cognition and problems with judgment Demonstrates decreased performance, especially when stressed Unable to travel alone to new destinations Often has decreased sense of smell o Middle (Moderate), or Stage II (2 to 3 years) Has impairment of all cognitive functions Demonstrates problems with handling or unable to handle money and finances Is disoriented to time, place, and event Is possible depressed and/or agitated Is increasingly dependent in ADLs Has visuospatial deficits: has difficulty driving and gets lost Has speech and language deficits: less talkative, decreased use of vocabulary, increasingly nonfluent, and eventually aphasic Incontinent Psychotic behaviors, such as delusions, hallucinations, and paranoia Has episodes of wandering; trouble sleeping o Late (Severe), or Stage III Completely incapacitated; bedridden Totally dependent in ADLs Has loss of mobility and verbal skills Possibly has seizures and tremors Has agnosia Priority Concerns o Potential for injury or falls due to wandering or inability to ambulate independently o Potential for elderly abuse by caregivers due to the patient’s prolonged progression of disability and the patient’s increasing care needs o Decreased memory and cognition due to neuronal changes in the brain Treatments o Safety measures to prevent injury, wandering, or falls o Behavior management o ADL and mobility assistance as needed based on stage o No way to prevent AD o Prevention of falls, injury, elder abuse o Medications Cholinesterase inhibitors; NMDA receptor antagonists Education o What to do during a seizure o How to protect from injury o When to call or go to ER o Review medication info with family o Unclutter house, consistent and structured schedule o Lock up hazardous items o Handrails along stairways, bathtub, toilet o Install alarms to prevent wandering o Nightlights o Go along with stories, do not reorient in later stages o Respite care for caregivers, adult daycare o PT to maintain mobility as long as possible Parkinson’s Disease Progressive neurodegenerative disease Affects mobility and is characterized by four cardinal symptoms Cause o Primary Disease: Cause not known, could be a combination of environmental and genetic factors o Secondary: caused by antipsychotic drugs or another condition such as brain tumor or trauma Assessment o History When did it start o Physical Resting vs movement tremors Rigidity assessment Facial expression (masklike) Emotional and speech changes Bowel and bladder changes o Lab and Imaging CSF analysis for decreased dopamine levels SPECT to rule out other CNS problems, and detect decrease in dopamine-producing neurons MRI to differentiate PD from other types of neurodegenerative disorders DaT scan to confirm abnormalities in dopamine transmission in the basal ganglia Progression o Steady and gradual decline (typically 10-20 years) of cognitive, mobility, and ADL function from mild through severe stages o Patients usually die from complications of immobility Risk Factors o Primary Male Over 40 years of age Family History (esp 1st degree relatives) Exposure to certain pesticides / breathing in heavy metals History of concussions o Secondary Traumatic brain injury Brain tumor or other lesions S/S o 4 Cardinal Tremor Muscle Rigidity Bradykinesia or Akinesia Postural Instability o Stage 1: Initial Stage Unilateral limb involvement Minimal weakness Hand and arm trembling o Stage 2: Mild Stage Bilateral limb involvement Masklike face Slow, shuffling gait o Stage3: Moderate Disease Postural instability Increased gait disturbances o Stage 4: Severe Disability Akinesia Rigidity o Stage 5: Complete ADL Dependence Priority Concerns o Decreased Mobility (and possible self-care deficit) due to muscle rigidity; resting tumors, and postural/gait changes o Impaired cognition due to neurotransmitter changes Treatments o Medications Dopamine agonists to stimulate dopamine receptors in the brain Levodopa-carbidopa (3-5 years) body ends up adapting to it Catechol O-methyltransferases (COMT) Inhibitors: prolong action of levodopa MAOIs: avoid tyramine (deli meats, aged cheeses, wine, or beer) o Surgical Stereotactic pallidotomy Deep Brain Stimulation Fetal tissue transplantation Education o Physical therapy activities o Safety preparation in house o Declutter house, remove rugs o Review medication information o Adequate fluid and nutrition intake o Routine toileting o Sleep hygiene o Respite care for caregivers Lumbar Puncture (Spinal Tap) Insertion of a spinal needle into the subarachnoid space between the 3rd and 4th (sometimes 4th and 5th) lumbar vertebrae Educations o Instruct patient not to move during procedure (may need 2 assistants, or sedation) Precautions o Not done on patients with severely increased ICP in order to avoid the risk of sudden release of CSF pressure o Not done on patients with skin infections at or near puncture site to avoid introducing infective organisms into the CSF Assessments o Assess patient’s ability to stay still and in side lying position for procedure o Assess for pain during procedure, notify provider o Assess and record opening and closing CSF pressures Normal opening pressure should be no more than 20 mmHg o VS and frequent neurologic checks o Postop Assess insertion site for leakage and notify provider Monitor for complications: N/V, severe headache, photophobia, change in LOC Why needed o Obtain CSF pressure readings with a manometer o Obtain CSF for analysis o Check for spinal blockage caused by spinal lesion o Inject contrast medium or air for diagnostic study o Inject selected drugs Migraines Common clinical syndrome characterized by recurrent episodic attacks of head pain that serve no protective purpose Causes o Combo of neuronal hyperexcitability and vascular, genetic, hormonal, and environmental factors o Thought to be a neurogenic process with secondary cerebral vasodilation followed by sterile brain tissue inflammation Common Triggers o Caffeine o Red wine o Monosodium glutamate (MSG) o High-intensity light o Stress o Excessive fatigue o Change in weather S/S o Common symptoms Throbbing and unilateral pain Nausea Sensitivity to light, sound, or head movement Migraine with Aura (Classic Migraine) o First, Prodromal Phase Aura that develops over a period of several minutes and lasts no longer than 1 hour Well-defined transient focal neurologic dysfunction Pain may be preceded by: Visual disturbances Flashing lights Lines or spots Shimmering or zigzag lights A variety of neurologic changes Numbness, tingling of the lips or tongue Acute confusional state Aphasia Vertigo Unilateral weakness Drowsiness o Second Phase Headache accompanied by nausea and vomiting Unilateral, frontotemporal, throbbing pain in the head that is often worse behind one eye or ear within an hour o Third Phase Pain changing from throbbing to dull Headache, nausea, and vomiting usually lasting 4 to 72 hours (older patients may have aura without headache) Migraine without Aura (Common Migraine) o Migraine beginning without an aura before the onset of the headache o Pain aggravated by performing routine physical activities o Pain that is unilateral and pulsating o One of these symptoms is present Nausea and/or vomiting Photophobia Phonophobia Headache lasting 4 to 72 hours Migraine often occurring in the early morning, during periods of stress, or in those with premenstrual tension for fluid retention Atypical Migraine o Status migrainous Headache lasting longer than 72 hours o Migrainous infarction Neurologic symptoms not completely reversible within 7 days Ischemic infarct noted on neuroimaging o Unclassified Headache not fulfilling all of the criteria to be classified a migraine Assessments o History o Physical, neurologic, and psychological assessment o Neuroimaging: MRI Treatments o Abortive Therapy: aimed at alleviating pain during the aura phase or soon after the headache has started Mild: NSAIDs, acetaminophen, antiemetics, caffeine Severe: triptans, ditans, ergotamine derivatives, isometheptene combination o Preventive Therapy: used when migraine occurs more than twice per week, interferes with ADLs, or is not relieved with acute treatment NSAID, beta-adrenergic blocker, calcium channel blocker, antiepileptic drugs, antidepressants, monoclonal antibody drugs o Trigger identification, avoidance and management o Medical marijuana (needs more clinical evidence, study replication) o External trigeminal nerve stimulator o Complementary and integrative health: yoga, mediation, massage, exercise, biofeedback Education o Avoid triggers o Keep track of when migraines occur, what is done to manage them, triggers, how long they last, etc o Medication info o When to call or go to ER (esp older women s/s of stroke) Seizures and Epilepsy Seizure: abnormal, sudden, excessive, uncontrolled electrical discharge of neurons within the brain that may result in a change in LOC Epilepsy: chronic disorder in which repeated unprovoked seizure activity Types o Tonic-Clonic Lasts 2 -5 minutes Begins with tonic phase that causes stiffening or rigidity of the muscles, particularly the arms and legs, and immediate loss of consciousness Clonic or rhythmic jerking of all extremities follows May bite tongue, become incontinent of urine or feces, fatigue, acute confusion, and lethargy that lasts up to an hour after seizure o Myoclonic Brief jerking or stiffening of the extremities that may occur singly or in groups Lasting for just a few seconds, contractions may be symmetric or asymmetric o Atonic (Akinetic) Sudden loss of muscle tone, lasting for seconds followed by postictal confusion Cause patient to fall which may result in injury Tends to be most resistant to drug therapy o Partial (Focal or Local) Begin in a part of one cerebral hemisphere Further subdivided into Complex partial and Simple partial seizures Most often seen in adults and generally are less responsive to medical treatment o Complex Partial May cause syncope for 1-3 minutes Automatisms Patient can be unaware and wander at the start of the seizure Amnesia after Temporal lobe involvement o Simple Partial Patient remains conscious throughout episode Often report aura before seizure takes place (offensive smell, sudden onset of pain) One sided movement of extremity, unusual sensations, autonomic symptoms (HR change, skin flushing, epigastric discomfort) Causes o Primary (Idiopathic Epilepsy) Not associated with identifiable brain lesion or specific cause o Secondary Underlying brain lesion Tumor Trauma Metabolic disorders Acute alcohol withdrawal Electrolyte disturbances (hyperkalemia, water intoxication, hypoglycemia) High fever Stroke Head injury Substance abuse Heart disease Risk Factors o Increased physical activity o Emotional stress o Excessive fatigue o Alcohol or caffeine consumption o Certain foods or chemicals S/S o Depends on type of seizure and patient Assessments o Number, timing, pattern of seizure o Preictal phase o Other medical history o EEG, CT, MRI, SPECT/PET Treatments o Protect patient from injury o Do not force anything in their mouth o Turn patient to the side to prevent aspiration and keep airway clear o Remove objects that might injure patient o Suction oral secretions if possible without force o Loosen any restrictive clothing o Do not restrain or try to stop movement; guide movements if necessary o Record the time the seizure began and ended o Place in recovery position after seizure o Talk to them about the seizure o o Assessment full head to toe after seizure Medications Antiepileptic drugs (AEDs): Dilantin (phenytoin) Education o Know drug info (name, dose, admin) o Regular lab draws for therapeutic or toxic levels o Do not take any drugs (OTC) without checking with provider o Wear medical alert bracelet o Follow up with neurologist or PCP o Do not drive or operate heavy machinery o Avoid alcohol and excessive fatigue Status Epilepticus Seizures that last longer than 5 minutes or frequent seizures in 30 minutes Causes o Sudden withdrawal from antiepileptic drugs o Infection o Acute alcohol or drug withdrawal o Head trauma o Cerebral edema o Metabolic disturbances Treatment/Management o IV lorazepam or diazepam o Phenytoin/fosphenytoin Education o Know drug info (name, dose, admin) o Regular lab draws for therapeutic or toxic levels o Do not take any drugs (OTC) without checking with provider o Wear medical alert bracelet o Follow up with neurologist or PCP o Do not drive or operate heavy machinery o Avoid alcohol and excessive fatigue Intracranial Pressure Increased ICP S/S o Decreased LOC o Behavior changes: restlessness, irritability, confusion o Headache o N/V (projectile) o Aphasia o Change in speech pattern (dysarthria) o Change in sensorimotor status Pupillary changes: Dilated and non-reactive (blown); constricted and non-reactive (very late sign) Cranial nerve dysfunction Ataxia o Seizures (usually within the first 24 hours) o Cushing Triad Severe HTN Widened pulse pressure Bradycardia o Abnormal posturing (very late sign) Decerebrate Decorticate Preventing or managing increasing ICP o Elevate HOB per protocol to improve perfusion pressure o Provide Oxygen therapy to prevent hypoxia when O2 < 95% o Maintain head in a midline, neutral position to promote venous drainage from the brain and intracranial dynamics o Avoid the clustering of nurse procedures; may cause dramatic ICP elevation o Hyperoxygenate the patient before and after suctioning to avoid transient hypoxemia and resultant ICP elevation from cerebral artery dilation o Provide airway management to prevent unnecessary suctioning and coughing that can increase ICP o Maintain a quiet environment for the patient experiencing a headache, which is common o Keep room lights low o Closely monitor blood pressure, heart rhythm, oxygen saturation, blood glucose, and body temp to prevent secondary brain injury and promote positive outcomes after stroke Decerebrate Posturing Abnormal movement with rigidity characterized by extension of the arms and legs, pronation of the arms, plantar flexion and opisthotonos (body spasm in which the body is bowed forward) When would we see it Pushed out o Dysfunction in the brainstem area Treatments o Emergency treatment right away o Breathing assistance and placement of a breathing tube Decorticate Posturing Abnormal motor movement where the patients arms, wrists, and fingers are flexed with internal rotation and plantar flexion of the legs Pulled in When would we see it o Lesions that interrupt the corticospinal pathways Treatments o Emergency treatment right away o Breathing assistance and placement of a breathing tube Spinal Cord Injury Types o Complete: one in which the spinal cord has been damaged in a way that eliminates all innervation below the level of the injury o Incomplete: injuries that allow some function or movement below the level of the injury Mechanisms of Injury o Hyperflexion: sudden forceful acceleration of the head forward causing extreme flexion of the neck Head on MVA or diving accident o Hyperextension: when the head is suddenly accelerated then decelerated Rear ending MVA and falls when patients chin is struck o Axial Loading or Vertical Compression: vertebral compression Blow to the top of the head, diving accidents, falls on buttocks, jump where person lands on feet o Excessive Rotation Injuries caused by turning head beyond normal range o Penetrating Trauma: object causes injury to spinal cord Knife or bullet wound Low speed: directly damage the site or local damage to spinal cord and nerves High speed: cause direct and indirect damage Assessments o History How injury occurred Mechanism of injury Pre-hospital care o Physical Priority ABCs Sensory perception and mobility assessment Skin assessment Vital signs o Psychosocial Anxiety Shock Depression o Laboratory and Imaging Basic Labs (CBC, CMP, UA) Spine CT and MRI X-rays Priority Concerns o Potential for respiratory distress/failure due to aspiration, decreased diaphragmatic innervation, and/or decreased mobility o Potential for cardiovascular instability (shock and autonomic dysreflexia) due to loss or interruption of sympathetic innervation or hemorrhage o Potential for secondary spinal cord injury due to hypoperfusion, edema, or delayed spinal column stabilization o Decreased mobility and sensory perception due to spinal cord damage and edema Treatments o Airway management o Teach coughing and deep breathing o Adequate hydration with IV and oral fluids o Assess mobility and sensory function o Take vital signs, pulse ox, pain every 1-4 hours o Traction, orthoses, collars for spinal immobilization o Therapeutic/Psychosocial management o Meds Atropine if pulse falls below 50-60bpm Dopamine Sympathomimetic agents PPIs Muscle relaxants o Surgery Within 24 hours to stabilize vertebral column Removal of bone fragments, hematomas, penetrating objects (bullet) Wiring and spinal fusion Steel or metal rods Education o Mobility skills o Pressure injury prevention o ADL skills o Bowel and bladder program o Sexuality education o Prevention of autonomic dysreflexia o Health care resources Autonomic Dysreflexia Potentially life-threatening condition in which visceral or cutaneous stimuli cause a sudden, massive, uninhibited reflex sympathetic discharge in people with high-level SCI Causes o GI, GU, Vascular stimulation o Pain o Circumferential constriction of the thorax, abdomen, or an extremity o Contact with sharp objects o Temperature fluctuations S/S o Sudden significant in systolic and diastolic BP, accompanied by bradycardia o Profuse sweating above the level of lesion – especially in the face, neck, and shoulders (rarely below level of lesion) o Goose bumps above or possibly below level of lesion o Flushing of skin above level of lesion – especially in the face, neck, and shoulders o Blurred vision o Spots in the patient’s visual field o Nasal congestion o Onset of severe throbbing headache o Flushing about the level of the lesion with pale skin below the level of the lesion o Feeling of apprehension Risk Factors o Bladder distention o UTI o Epididymitis o Scrotal compression o Bowel distention or impaction from constipation o Irritation of hemorrhoids Treatments o Prevention Scheduled toileting, bladder scan, catheter maintenance, bowel regimen, peri care, don’t leave irritants in chair, avoid pressure on GU o Look for causative agent (kink in catheter, bowel impaction) o Move them into bed to assess possible cause o HOB 30 due to high BP and low HR o Call provider Education o S/S of autonomic dysreflexia o Prevention methods o When to call or go to ER Glasgow Coma Scale Standard rapid neurologic assessment tool Used to establish baseline data in each of these areas o Eye opening o Motor response o Verbal response The lower the score the lower the patients neurologic function Intubated patients who cannot talk have score recorded with a “t” Highest possible score is 15 A decrease of 2 or more points total is clinically significant and should be reported to provider immediately NIH Stroke Scale Commonly used valid and reliable assessment tool that nurses complete as soon as possible after the patient arrives in the ED Used as one assessment to determine eligibility for IV fibrinolytics No standard for when or how often to use the tool Category and Measurement o 1a. LOC 0 = Alert; keenly responsive 1 = Not alert; but arousable by minor stimulation to obey, answer, or respond 2 = Not alert; requires repeated stimulation 3 = Responds only with reflex motor or autonomic effects, or totally unresponsive, flaccid, areflexic o 1b. LOC Questions 0 = Answers questions correctly 1 = Answers one question correctly 2 = Answers neither question correctly o 1c. LOC Commands 0 = Performs two tasks correctly 1 = Performs one task correctly 2 = Performs neither task correctly o 2. Best Gaze 0 = Normal 1 = Partial gaze palsy; gaze abnormal in one or both eyes, forced deviation or total gaze paresis 2 = Forced deviation, or total gaze paresis o 3. Visual 0 = No visual loss 1 = Partial hemianopia 2 = Complete hemianopia 3 = Bilateral hemianopia (blind including cortical blindness) o 4. Facial Palsy 0 = Normal symmetric movements 1 = Minor paralysis (asymmetry on smiling) 2 = Partial paralysis (total or near total paralysis of lower face) 3 = Complete paralysis of one or both sides (absence of facial movement in the upper and lower face) o 5. Motor (Arm) 0 = No drift; limb holds 90 (or 45) degrees for full 10 seconds 1 = Drift; limb holds 90 (or 45) degrees, but drifts down before full 10 seconds; does not hit bed or other support 2 = Some effort against gravity; limb cannot get to or maintain (if cued) 90 (or 45) degrees; drifts down to bed but has some effort against gravity 3 = No effort against gravity; limb falls 4 = No movement Untestable = Amputation or joint fusion o 6. Motor (Leg) 0 = No drift; leg holds 30-degree position for full 5 seconds 1 = Drift; leg falls by the end of the 5-second period but does not hit bed 2 = Some effort against gravity; leg falls to bed by 5 seconds but has some effort against gravity 3 = No effort against gravity; leg falls to bed immediately 4 = No movement o 7. Limb Ataxia 0 = Absent 1 = Present in one limb 2 = Present in two limbs o o o o Untestable = Amputation or joint fusion 8. Sensory 0 = Normal; no sensory loss 1 = Mild-to-moderate sensory loss; patient feels pinprick less sharp or dull on the affected side; or loss of superficial pain with pinprick, but patient aware of being touched 2 = Severe-to-total sensory loss; patient not aware of being touched in the face, arm, and leg 9. Best Language 0 = No aphasia; normal 1 = Mild-to-moderate aphasia; some obvious loss of fluency or facility of comprehension, without significant limitation on ideas expressed or form of expression 2 = Severe aphasia; all communication is through fragmentary expression; great need for inference, questioning, and guessing by the listener 3 = Mute, global aphasia; no usable speech or auditory comprehension 10. Dysarthria 0 = Normal 1 = Mild-to-moderate dysarthria; patient slurs at least some words and, at worst, can be understood with some difficulty 2 = Severe dysarthria; patient’s speech so slurred as to be unintelligible in the absence of or out of proportion to any dysphasia or is mute/anarthric Untestable = Intubated or other physical barrier 11. Extinction and Inattention (Neglect) 0 = No abnormality 1 = Visual, tactile, auditory, spatial, or personal inattention or extinction to bilateral simultaneous stimulation in one of the sensory modalities 2 = Profound hemi-inattention or extinction to more than one modality; does not recognize own hand or orients to only one side of space Brain Death Four Classic Prerequisites o Coma of known cause established by history, clinical examination, laboratory testing, and neuroimaging o Normal or near-normal core body temperature (higher than 96.8F or 36C) o Normal systolic BP (higher or equal to 100mmHg) o At least one neurologic examination (some states and health care systems require 2) Testing that can be used to determine brain death o Electroencephalography (EEG) o Cerebral Computed Tomography Angiography (CTA) o Transcranial Doppler Ultrasonography Meningitis Causes o Viral Meningitis: enterovirus, herpes simplex virus-2, varicella zoster virus, mumps, HIV o Bacterial Meningitis: streptococcus pneumoniae, Neisseria meningitidis (vaccine for this) o Fungal Meningitis: cryptococcus neoformans, fulminant invasive fungal sinusitis (fungal usually associated with HIV infection) S/S o Decreased LOC o Disorientation to person, place, and time o Pupil reaction and eye movements Photophobia (light sensitivity) Nystagmus (involuntary condition in which the eyes make repetitive uncontrolled movements) o Motor Response Normal early in disease process Hemiparesis (weakness on one side of the body) Hemiplegia (paralysis on one side Decreased muscle tone possible later Cranial nerve dysfunction especially CN III, IV, VI, VII, VIII o Memory Changes Attention span (usually short) Personality and behavior changes o Severe, unrelenting headaches o Generalized muscle aches and pain Risk Factors o HIV infection (Fungal and Viral) o Infection in the eyes, ears, nose, mouth, neck/throat o Immunocompromised patient (cancer treatment, immunosuppressant drugs) o High population density (college dorms, military barracks, crowded living areas) o Ages 16-21 Assessments o CSF analysis o CT scan o CBC with elevated WBCs o X-rays, CT, or MRI Treatments o Prevention with vaccination against Haemophilus influenzae type B (Hib), pneumococcal, mumps, varicella, meningococcal organisms o Broad spectrum antibiotics for bacterial cause Education o S/S of meningitis o Get vaccinated to prevent Concussion TBI Causes o Blow to the head o Head trauma S/S o Impaired cognition (memory and thinking) o Headache o Vomiting/nausea Risk Factors o Military personnel o People who participate in recreational or professional sports Education o Avoid getting concussion o Wear a helmet Multiple Sclerosis (MS) Chronic disease that affects the myelin and nerve fibers of the brain and spinal cord Characterized by periods of remission and exacerbation (flare) Types o Relapsing-remitting o Primary progressive o Secondary progressive o Progressive-relapsing Causes o o S/S o o o o o o o o o o o o o o o o o o o Immune, genetic, and/or infectious factors Colder climate can trigger flare Muscle weakness and spasticity Fatigue (usually with continuous sensitivity to temperature) Intention tremors (tremor when performing an activity) Flexor muscle spasms Dysmetria (inability to direct or limit movement) Numbness or tingling sensations (paresthesia) Hypoalgesia (decreased sensitivity to pain) Ataxia (decreased motor coordination) Dysarthria (difficulty speaking due to slurred speech) Dysphagia (difficulty swallowing) Nystagmus (involuntary condition in which eyes make repetitive uncontrolled movements) Scotomas (changes in peripheral vision) Decreased visual and hearing acuity) Blurred or double vision (diplopia) Tinnitus (ringing in ears) Vertigo (dizziness) Bowel and bladder dysfunction (flaccid or spastic) Alterations in sexual function (impotence) Cognitive changes (memory loss, impaired judgment, decreased ability to solve problems or perform calculations) o Depression Diagnosis o Symptom based o Ruling out all other possibilities o MRI with contrast to show plaques and lesions o CSF with elevated proteins and WBCs Priority cues o Decreased or impaired mobility due to muscle spasticity, intention tremors, and/or fatigue o Impaired immunity due to the disease and drug therapy for disease management o Decreased visual acuity and cognition due to dysfunctional brain neurons Treatments o Staying mobile, moving as tolerated o Encourage resting and prevention of exacerbation o Medications Immunomodulators Anti-inflammatory Education o Avoid crowds and sick people o Properly cook food o Hand hygiene o S/s of infection o Organize house to help with ease of maneuvering o Decrease stress o Physical activity as tolerated