Patient Medical Record: Numbness & Treatment at San Lazaro Hospital
advertisement

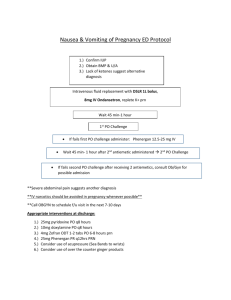
Three (3) weeks prior to confinement, the patient tripped on a rock with steel having a linear lacerated wound on his right knee. The wound was cleaned with alcohol. No consultation and no medication taken. One (1) week prior to confinement, the patient started feeling numbness on the right leg which prompted him to seek consultation at San Pablo Community General Hospital and was admitted for one (1) week. The patient was inserted with an endotracheal tube in San Pablo Community General Hospital. The patient was then referred to San Lazaro Hospital. Past Medical History Patient VAB has hypertension but no maintenance medication taken for the past one (1) year. The patient has no asthma or diabetes. He is not taking vitamins and other medications except over-the-counter drugs when he has a fever or not feeling well. The patient has a history of falls involving his left leg. He has never undergone any type of surgery. He has no known allergy to food and medication. Family History (+) Hypertension (+) Diabetes Mellitus (-) Cancer Personal and Social History The patient is a 47-pack year smoker. He consumes two (2) bottles of beer twice a week. He prefers to eat rice, fish, and vegetables. He enjoys his leisure time gardening. He gets along with his neighbors pretty well. He likes going to his friends by walking. He is a sweet and loving husband. Admission Order The patient was admitted on August 20, 2020, at 12:05 am with a chief complaint of numbness of the right leg and was admitted to satellite ICU of San Lazaro Hospital, hooked to PNSS 1L at 150 cc/hr. The patient was subjected to the following laboratory procedures: CBC, BUN, Creatinine, SGPT, SGOT, ABG, RBS, UA. Patient was given Tetanus Toxoid 0.5ml IM, Metronidazole 500 mg IV every 6 hours, Diazepam 10 mg IV every 4 hours, Baclofen 10 mg 1tab TID, Clopidogrel 75 mg 1tab OD, Atorvastatin 40mg/tab 1tab ODHS, Losartan 50 mg 1tab OD, Amlodipine 10 mg 1tab OD, Paracetamol 300mg TIV q4 prn, Omeprazole 40mg/capsule 1tab OD, Piperacillin + Tazobactam 4.5g/TIV q6, Acetylcysteine 600 mg/tab OD/HS, Tranexamic Acid 500mg IV q8 prn, Ferrous Sulfate 1tab OD, Budesonide 200 mcg/dose q12 and Ceftriaxone 2g OD. Additional diagnostic tests were also conducted the following days are GS/CS test, CBG, CT Scan with contrast, Chest X-ray, Na, K and ECG. Bedside care implemented to the patient includes proper positioning, bedsore precaution, turning the patient to side at least every 2 hours, I&O monitoring, suctioning of secretions prn, monitoring of vital signs, LOC, and neurologic status, monitoring of fever, spasm, and hypotensive episodes. Crackles were also monitored including dyspnea and respiratory distress. Edema, decubitus ulcer and phlebitis were also assessed and monitored. The patient was also provided oxygen therapy via tracheostomy, a pulse oximeter monitor was attached to the patient, physical examinations were conducted, tracheostomy care was provided, chest physiotherapy was initiated and OF through NGT was given and bladder training was also conducted.