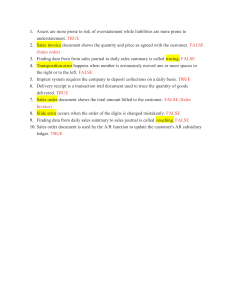
Self-Proning in Non-Intubated Patients with COVID-19: A Strategy to Avoid Intubation Jan Powers Sue Chubinski Michele Kadenko-Monirian rone positioning has become an accepted part of medical treatment for mechanically ventilated patients with acute respiratory distress syndrome (ARDS) (Gattinoni et al., 2010; Guérin et al., 2013; Mancebo et al., 2006; Taccone et al., 2009). Most current literature has focused on the critical care setting. Previous studies demonstrated proning in ventilated critical care patients improved oxygenation by reducing lung ventilation/perfusion mismatch and promoting recruitment of non-aerated dorsal lung regions to optimize oxygenation (Gattinoni et al., 2010; Guérin et al., 2013; Mancebo et al., 2006; Marini, 2016; Taccone et al., 2009). To achieve best results in critically ill patients with ARDS, a pivotal study by Guérin and coauthors (2013) found proning should occur for at least 16 hours/day. Recently, large numbers of patients with coronavirus disease (COVID-19) experiencing oxygenation compromise have been admitted to medical units. Conserving the use of critical care beds and ven- P Patients with coronavirus disease (COVID-19) experiencing oxygenation compromise often are admitted to medical units. Assessment of the impact of self-proning on oxygenation in patients with COVID-19 suggested early self-proning is a viable, nursedriven option to improve oxygenation, prevent transfer to intensive care, and decrease need for invasive mechanical ventilation. tilators also has been a concern. Subsequently, nurses have looked for interventions to decrease or prevent patient deterioration, preventing the need for intubation and transfer to critical care. One intervention identified by nursing staff was prone position for awake, nonintubated patients with COVID-19 in an attempt to improve oxygenation and prevent intubation. Purpose The purpose of this study was to evaluate the impact of self-proning for awake, non-intubated patients with or suspected to have COVID- 19 on medical units. Patients were encouraged to self-prone twice a day for at least 30 minutes, but up to 2 hours. Review of the Literature A literature search was performed in Ovid MEDLINE for 2015-2020 using the search terms prone position, proning, and prone. These terms were combined with awake, self, conscious, or non-intubated; 53 unique articles were identified with 17 relevant for this study. A search also was completed in CINAHL (EBSCO) but yielded no additional articles. Evidence is lacking for the Jan Powers, PhD, RN, CCNS, CCRN, NE-BC, FCCM, is Director for Nursing Research and Professional Practice, Parkview Health, Fort Wayne, IN. Sue Chubinski, PhD, RN, NPD-BC, CMSRN®, is Educator, Nursing Education and Clinical Excellence, Parkview Health, Fort Wayne, IN. Instructions for Contact Hours MSN J2105 Nursing Continuing Professional Development (NCPD) contact hours can be earned for completing the evaluation associated with this article. Instructions are available at amsn.org/journalNCPD Deadline for submission: April 30, 2023 1.3 contact hours Stephani Schultz Christina Lung Tammy Carman Michele Kadenko-Monirian, MS, RN, AGCNS-BC, ACCNS-AG, CCRN, CNRN, is Clinical Nurse Specialist, Parkview Health, Fort Wayne, IN. Stephani Schultz, BSN, RN, CMSRN®, is Educator, Nursing Education and Clinical Excellence, Parkview Health, Fort Wayne, IN. Christina Lung, MSN, RN, CMSRN®, NE-BC, is Nursing Services Manager, Parkview Regional Medical Center, Fort Wayne, IN. Tammy Carman, AD, RN, is Clinical Nurse, Parkview Randallia Hospital, Fort Wayne, IN. Acknowledgment: Authors acknowledge all clinical nurses on the COVID-19-designated medical units who tirelessly assure patients receive the best possible evidence-based care. March-April 2021 • Vol. 30/No. 2 77 Background Prone positioning improves oxygenation in patients experiencing respiratory distress. It is used to decrease mortality in mechanically ventilated patients diagnosed with acute respiratory distress syndrome. However, very little evidence has addressed use of prone positioning in non-intubated patients. Aims Assess the impact of early self-proning on oxygenation in patients who had or were suspected of having coronavirus disease (COVID-19). The goal was to improve oxygenation to avoid escalation to the intensive care unit (ICU) and the need for invasive mechanical ventilation. Methods This descriptive study consisted of a patient cohort from medical units in two hospitals. Data collected were limited to medical record reviews. Identified patients were able to reposition themselves. Results This study enrolled 46 patients who self-proned a total of 180 times (average 4 times per patient). Patients experienced an increase in oxygenation 97% of the time. Limitations and Implications Only patients with the ability to self-prone were included. This was an observational study with no comparison group. Self-proning of awake, non-intubated patients is a nurse-driven practice that may lead to improved patient outcomes. Conclusion In this study, early self-proning was identified as a viable option to improve oxygenation, prevent transfer to ICU, and decrease the need for invasive mechanical ventilation. flow nasal cannula (HFNC) with prone patients, HFNC in patients not prone, noninvasive ventilation (NIV) prone, and NIV without prone positioning. The primary outcome was a decreased rate of intubation. Patients receiving oxygen by HFNC with prone positioning had a significantly greater improvement in oxygenation (p=0.043). The application of prone positioning with HFNC was well tolerated and efficacious. Other researchers also identified feasibility of early prone positioning with similar improvements in oxygenation, avoidance of intubation, improved survival, and reduced patient transfer to ICU (Caputo et al., 2020; Dong et al., 2020; Elharrar et al., 2020; PérezNieto et al., 2020; Sartini et al., 2020). Despite low-quality published reports with small samples, most published studies demonstrated improvements in oxygenation with prone positioning in awake patients. Based on the limited evidence, some support exists for prone positioning in non-ICU patients. Additionally, the Intensive Care Society released guidelines for prone positioning of awake, nonintubated patients (Bamford et al., 2020). Ethics application of prone positioning as a nursing intervention outside the intensive care unit (ICU). Of the identified literature in the search, four articles were procedural reviews of mechanism of action or commentary. Multiple publications consisted of letters reporting small case series (Pérez-Nieto et al., 2020; Sartini et al., 2020; Sun et al., 2020; Thompson et al., 2020; Xu et al., 2020). Eight additional papers presented retrospective or prospective case series or cohort studies (Caputo et al., 2020; Despres et al., 2020; Ding et al., 2020; Dong et al., 2020; Elharrar et al., 2020; GolestaniEraghi & Mahmoodpoor, 2020; Paul et al., 2020; Scaravilli et al., 2015). Before 2019, only one study was completed on awake proning in patients without COVID-19. The 78 study included a patient population with mixed diagnoses. In a retrospective chart review of 15 nonintubated patients with hypoxemic respiratory failure treated with prone positioning, Scaravelli and colleagues (2015) found prone positioning to be feasible and to improve oxygenation. Other published studies on awake prone positioning as a treatment modality with patients with COVID-19 are limited by small samples. A prospective observational cohort study in two teaching hospitals enrolled 20 non-intubated patients with moderate-to-severe ARDS who were placed in the prone position (Ding et al., 2020). Blood gas analysis was used to evaluate oxygenation with four treatment modalities. The four methods included use of high- The study was submitted to the hospital’s Institutional Review Board and, due to low-risk for human subjects, was deemed exempt. A waiver of informed consent also was granted. Sample Selection Study participants were admitted to one of four designated COVID-19 medical units at two hospitals (regional medical center, high-capacity community hospital) which are part of the same hospital system. Non-intubated patients who could turn themselves in the prone position were included. Patients were excluded if they were under age 18, pregnant, or mechanically ventilated in an ICU during the current hospitalization. March-April 2021 • Vol. 30/No. 2 Self-Proning in Non-Intubated Patients with COVID-19: A Strategy to Avoid Intubation FIGURE 1. Awake Prone Algorithm and Procedure Patient not intubated receiving supplemental oxygen Always continue program on PUM protocol as able Patient alert, awake, cooperative, and able to move self Patient on 2-6L/O2 Yes Explain procedure and assist patient in prone position per nursing protocol Follow Procedure Below for Placing Patient in Prone Position Procedure for Patient Preparation Prior to Positioning Prone 1. Assemble supplies before entering room. 2. Follow appropriate precautions. 3. Explain to patient the purpose of prone position and planned length of time that patient will be prone. Goal: Minimum 30 minutes to maximum 2 hours BID 4. Verify patient has not eaten within the last 30 minutes. 5. Assess patient for actual or potential skin breakdown; pad with Mepilex® (bilateral shoulders, chest iliac crest, knees). 6. Evaluate patient’s ability to turn head side to side (in prone position, patient will be asked to turn head to best ROM side). 7. Remove fitted sheet; place flat sheet under patient’s shoulders and Covidien pad at hips. 8. Obtain, document vital signs, including SpO2. If on telemetry, remove EKG electrodes from front and place on back. 9. Remove stat lock from Foley; verify securement of feeding tube, chest tube(s), and IV (if applicable). 10. Correctly position all tubes, taking into account the direction of the turn (tubes in the lower torso aligned with either leg and extended off the bed). Adjust IV pump position close to head of bed; verify tubing has generous length for the turn. Procedure of Manual Pronation 1. Verify position of all tubes, taking into account the direction of the tubes. 2. Instruct patient to raise affected arm with IV overhead. 3. Have patient roll over to prone position; adjust gown-tubing. 4. Place patient in swimmer’s pose (one side slightly off bed, adjust with pillows and position to avoid traction on the brachial plexus and lift diaphragm off bed. Assist patient to best position of comfort. 5. Place patient on continuous SpO2 monitoring. 6. Replace EKG leads on telemetry patients. 7. Assess patient’s response, noting if patient is having any respiratory distress. If patient not tolerating, assist patient to supine position, HOB raised. Use two flat sheet method if patient unable to turn supine. Notify provider and document. HOB = head of bed, IV = intravenous, PUM = persons under monitoring, ROM = range of motion March-April 2021 • Vol. 30/No. 2 79 TABLE 1. Self-Proning Algorithm and Criteria Inclusion Exclusion Alert Documented aspiration risk Awake Patient nauseated/vomiting Cooperative Tracheostomy/laryngectomy >30 minutes from last meal Severe reflux Able to reposition independently from supine to prone and vice versa Continuous gastric tube feedings Hemodynamically stable: Combative HR 50-120 Restraints SBP 90-180 Morbid obesity MAP ≥65 Pregnancy ≥ second trimester No new arrhythmia on EKG Unstable spinal cord Limited neck ROM Respiratory RR <40 Specific surgical and/or trauma precautions per provider order Special Considerations (clarify with provider) Continuous j-feedings (low-no aspiration risk) CPAP/BiPAP (may improve ventilation) Skin breakdown Recent pacemaker implantation (no arm movement on pacemaker side above shoulder x 4 weeks) Recent surgeries to the chest (no proning ≤6 weeks post-CAB) Recent surgical and/or trauma (especially facial, thoracic, cervical and/or spinal, abdominal) CAB = coronary artery bypass, CPAP/BiPAP = continuous positive airway pressure/bilevel positive airway pressure, HR = heart rate, MAP = mean arterial pressure, ROM = range of motion, RR = respiratory rate, SBP = systolic blood pressure Design and Method This retrospective descriptive study evaluated the impact of a nurse-driven protocol for self-prone positioning. The main outcome of interest was oxygenation. Other outcome variables included need for ICU admission, need for intubation/mechanical ventilation, and length of stay. Given the low risk versus high potential for improvement, a small group of clinical nurses, clinical nurse specialists (CNSs), educators, and medical staff at the study institution developed a protocol for selfproning. A simple algorithm was developed to identify patients who could be proned safely while awake (see Figure 1). Instructions were written on how to prone a patient and monitor after proning. The protocol was approved through the site’s COVID Incident Command Center (ICC), which was estab80 lished early in the pandemic to help clinical staff remain current on rapidly changing procedures (see Table 1). As part of the ICC structure, a COVID Commander role was developed and filled by a charge nurse from the primary acute care unit housing affected patients. All nurses and patient care technicians on medical units admitting patients with COVID-19 were instructed on inclusion criteria for implementation and the process for self-proning. Further distribution of the protocol focused on charge nurses, who then introduced the procedure to clinical staff at daily shift huddles. Informal demonstrations of positioning and scripted encouragement to patients were reviewed with staff. The information was reinforced by email and handouts posted at the nurses’ stations and in staff bathrooms. In addition, computer-based educa- tion modules were assigned to all nursing staff. Educators and CNSs provided one-on-one just-in-time education on all shifts, including weekends. Ongoing bedside reinforcement and follow up were provided by charge nurses, educators, CNSs, managers, and COVID Commander. Clinical nurses were very receptive and quickly became advocates of the self-proning practice. Before the study, patient positioning fields were added to the electronic health record to document selfproning. For data collection and study inclusion, a report was built to identify any patient who had documentation turned self-prone to identify patients for inclusion. Patient charts were reviewed based on inclusion criteria. The study was conducted April 1-May 31, 2020. Data were collected on all patients who had at least one episode of self-proning and were not intu- March-April 2021 • Vol. 30/No. 2 Self-Proning in Non-Intubated Patients with COVID-19: A Strategy to Avoid Intubation bated. Few or no arterial blood gases were available for the sample. As a result, the key indicator for oxygenation was oxygen saturation (SpO2) using pulse oximetry. Information on patient age, oxygenation support, date/time of selfproning, length of prone episode, and length of stay was collected. Patient transfer to the ICU or intubation also was documented. Findings During the data collection period, 46 participants had 180 selfproning episodes. Average prone episodes per patient was four (range 1-42), with average time in the prone position 136 minutes (range 20-360). Patients’ average age was 57 (range 26-100). Thirty participants had confirmed COVID-19 and 16 were presumed to have COVID-19. However, none of the suspected cases had positive results at further evaluation. The average SpO2 for participants before prone positioning was 93% (84%-100%), and the average after returning supine was 96% (90%100%). Patients experienced an increase in SpO2 with prone position in 175 (97%) episodes. Participants who did not experience an increase in SpO2 or had oxygenation that remained the same or slightly decreased, represented 1%2%. Only five episodes (3%) of selfproning required an increase in oxygen delivery. No complications or adverse events were documented during any self-prone episode. Of 46 participants, three (6.5%) were transferred to ICU but only one required intubation and mechanical ventilation. The average hospital length of stay was 7.1 days (range 2-14). Almost all participants were discharged to home (n=41; 89.1%); only 4 (8.7%) went to an extended care or rehabilitation facility. One older patient was transitioned to palliative care at the family’s request and expired. Discussion This study is one of the largest cohorts published to date and the only one implemented by nurses. Results of this study demonstrated positive outcomes with improved oxygenation for non-intubated, selfproning medical patients. Nurses initiated this protocol with interprofessional collaboration for patients with or suspected of having COVID19. The interprofessional collaboration created an energized atmosphere on the units as successes were shared and celebrated. Self-proning may prevent deterioration, and conserve use of ICU beds and ventilators. The process was feasible, safe, and required no additional equipment for independent self-proning. Findings demonstrated higher rates of improved oxygenation (97%) after self-proning compared to other studies reporting 13%-20% improvement (Elharrar et al., 2020; Scaravelli et al., 2015). However, this study differed from prior research in that arterial blood gas results were not available, so SpO2 was used to determine outcome (Ding et al., 2020; Dong et al., 2020; Scaravilli et al., 2015). Other studies also consistently reported improved avoidance of intubation; in the current study, only one (2%) patient subsequently required intubation. This is a notable finding compared to other studies with higher reported intubation rates. In studies by Pérez-Nieto and coauthors (2020) and Ding and colleagues (2020), intubation rates were cited as 33% and 45% respectively. Data from the current study are similar to the report by Sun (2020), who also found notable improvements in oxygenation. Most participants in this study were discharged to home (89%). Some were discharged to rehabilitation or skilled nursing facilities (8.7%). The death of a centenarian patient resulted in this study’s 2% mortality compared to 5%-20% mortality in previously published studies (Ding et al., 2020; PérezNieto et al., 2020; Scaravilli et al., 2015). This one death in the current study resulted from a change to a palliative care focus for this patient. Duration of prone time varied in this study, which is similar to other studies (range 30 minutes-12 hours, March-April 2021 • Vol. 30/No. 2 mean 2.5 hours). Frequency of proning in previous studies ranged from twice a day with variable duration times based on patient’s ability to tolerate prone positioning (Ding et al., 2020; Dong et al., 2020; Elharrar et al., 2020). Results of this study are consistent with other studies in finding self-proning safe and effective for patients with suspected or positive COVID-19. Limitations Because there are limited reported data on self-proning in a nonICU setting, an initial descriptive study design was an appropriate beginning approach. However, there are limitations in drawing conclusions, relationships, or inferences. In addition, retrieving data from the electronic medical record was dependent on consistency in charting and accurate application of charting choices in the patient position section. A limited time was selected for study, resulting in a small convenience sample from two sites that may not be representative. However, this study recruited a greater number of participants than prior research and provides preliminary data for designing the next study. Finally, there was no comparison group to determine if outcomes improved as a result of proning interventions. Recommendations for Future Research Future studies are needed to determine optimal frequency and duration of proning within a 24hour period. Future research also should include a control group and comparison (pre/post) to delineate the benefits of self-proning in these lower-risk patients. A longer collection period, with data collected prospectively during proning, should be considered to reduce challenges associated with retrospective data collection. Identification of potential confounders, such as mobility progression, medications, or other respiratory therapies, should be considered. Expanding application of this preventive nurs81 ing intervention to patients in the Emergency Department with COVID-19, community patients positive for COVID-19 recovering at home, and patients with other diagnoses (e.g., pneumonia) also should be explored. Expanding awake proning to include adults and children with acute and chronic respiratory disease should be considered, as the intervention may prove useful. Future research also should explore nurses’ experience through a qualitative approach. Nursing Implications Patient positioning is within the autonomous scope of nursing practice; self-proning also can be completed independently by the patient. The self-proning procedure is low-risk and can be implemented easily on any medical unit with no additional resources. Nurses should be empowered and encouraged to implement this practice for their patients. This study suggested the use of nurse-driven proning protocols can help prevent further respiratory deterioration in medical patients. Throughout the global pandemic, nurses were able to ask clinical practice questions, review available evidence, and implement nurse-driven interventions to prevent and improve patient outcomes. During this study, nurses reported excitement over having a powerful intervention they could initiate independently that often resulted in rapid improvement in patients’ oxygenation. This intervention also decreased patients’ anxiety about their difficulty in breathing. Before this study, medical nurses viewed proning as a physician-driven ICU intervention that required a team to implement for critically ill patients. Medical nurses quickly adopted the practice as a safe and effective tool to improve their patients’ respiratory condition, preventing escalation of care and conserving critical care beds within the facility. With more experience, nurses may be able to recruit participants as they report positive outcomes. With the initial prone session, nurses must be present to supervise and guide the patient proning procedure to assure safety and establish patients’ baseline response. Further nursing assessment should focus on how patients tolerate the position, including monitoring oxygen saturation and vital signs. In this study, some patients initially desaturated and required time to adjust to the position change. Recovery time was dependent on patient condition. Ongoing nursing assessments of proning effectiveness may provide data to improve proning practices. Conclusion Even though this observational study had a small sample, benefits were positive. No additional risk to patients was identified. This study confirmed use of nurse-driven proning protocols can assist with preventing further respiratory deterioration in medical patients. Additionally, nurses were able to use the intervention of self-proning with no additional resources. Nurses empowered through evidencebased practice were able to provide positive clinical outcomes for patients during a pandemic. REFERENCES Bamford, P., Bentley, A., Dean, J., Whitmore, D., & Wilson-Baig, N. (2020). ICS guidance of the prone positioning for the conscious COVID patient 2020. https:// emcrit.org/wp-content/uploads/2020/ 04/2020-04-12-Guidance-for-consciousproning.pdf Caputo, N.D., Strayer, R.J., & Levitan, R. (2020). Early self‐proning in awake, non‐intubated patients in the emergency department: A single ED’s experience during the COVID‐19 pandemic. Academic Emergency Medicine, 27(5), 375378. Despres, C., Brunin, Y., Berthier, F., Pili-Floury, S., & Besch, G. (2020). Prone positioning combined with high-flow nasal or conventional oxygen therapy in severe COVID-19 patients. Critical Care, 24, Article No. 256. https://doi.org/10.1186/ s13054-020-03001-6 Ding, L., Wang, L., Wanhong, M., & Hangyong, H. (2020). Efficacy and safety of early prone positioning combined with HFNC or NIV in moderate to severe ARDS: A multi-center prospective cohort study. Critical Care, 24, Article No. 28. Dong, W., Gong, Y., Feng, J., Bai, L., Qing, H., Zhou, B., … Xu, S. (2020). Early awake prone and lateral position in non-intubated severe and critical patients with COVID-19 in Wuhan: A respective cohort study. medRxiv. https://doi.org/10.1101/ 2020.05.09.20091454 Elharrar, X., Trigui, Y., Dols, A.M., Touchon, F., Eloi Prud’homme, S.M., & Papazian, L. (2020). Use of prone positioning in nonintubated patients with COVID-19 and hypoxemic acute respiratory failure. JAMA, 323(22), 2336-2338. Gattinoni, L., Carlesso, E., Taccone, P., Polli, F., Guérin, C., & Mancebo. J. (2010). Prone positioning improves survival in severe ARDS: A pathophysiologic review and individual patient meta-analysis. Minerva Anestesiologica, 76(6), 448‐ 454. Golestani-Eraghi, M., & Mahmoodpoor, A. (2020). Early application of prone position for management of COVID-19 patients. Journal of Clinical Anesthesia, 66, 109917. Guérin, C., Reignier, J., Richard, JC., Beuret, P., Gacouin, A., Boulain, T., Mercier, E, … Ayzac, L. (2013). Prone positioning in severe acute respiratory distress syndrome. New England Journal of Medicine, 368(23), 2159-2168. Mancebo J., Fernández R., Blanch L., Rialp, G., Gordo, F., Ferrer, M., Rodriguez, F., ... Albert, R. (2006). A multicenter trial of prolonged prone ventilation in severe acute respiratory distress syndrome. American Journal of Respiratory and Critical Care Medicine, 173(11), 1233‐1239. Marini, J., Joseph, S., Mechlin, M., & Hurford, W. (2016). Should early proning be a standard of care in ARDS with refractory? Respiratory Care, 61(6), 818-829. Paul, V., Patel, S., Royse, M., Odish, M., Malhotra, A., & Koening, S. (2020). Proning in non-intubate (PINI) in times of COVID-19: Case series and a review. Journal of Intensive Care Medicine, 35(8), 818-824. Pérez-Nieto, O.R., Guerrero-Gutiérrez, M.A., Deloya-Tomas, E., & Ñamendys-Silva, S.A. (2020). Prone positioning combined with high-flow nasal cannula in severe noninfectious ARDS. Critical Care, 24(1), 114. Sartini, C., Tresoldi, M., Scarpellini, P., Tettamanti, A., Carcò, F., Landoni, G., & Zangrillo, A. (2020). Respiratory parameters in patients with COVID-19 after using noninvasive ventilation in the prone position outside the intensive care unit. JAMA, 323(22), 2338-2340. Scaravilli, V., Grasselli, G., Castagna, L., Zanella, A., Isgrò, S., Lucchini, A., … Pesenti, A. (2015). Prone positioning improves oxygenation in spontaneously breathing nonintubated patients with hypoxemic acute respiratory failure: A retrospective study. Journal of Critical Care, 30(6), 1390-1394. https://doi.org/ 10.1016/j.jcrc.2015.07.008 continued on page 87 82 March-April 2021 • Vol. 30/No. 2 Self-Proning continued from page 82 Sun, Q., Haibo, Q., Huang, M., & Yang, Y. (2020). Lower mortality of COVID-19 by early recognition and intervention: experience from Jiangsu Province. Annals of Intensive Care 10, Article No. 33. https://doi.org/10.1186/s13613-02000650-2 Taccone P, Pesenti A, Latini R, Polli, F., Vagginelli, F., Mietto, C., … Gattinoni, L. (2009). Prone positioning in patients with moderate and severe acute respiratory distress syndrome: A randomized controlled trial. JAMA, 302(18),1977-1984. Thompson, A.E., Ranard, B.L., Wei, Y., & Jelic, S. (2020). Prone positioning in awake, nonintubated patients with COVID-19 hypoxemic respiratory failure. JAMA Internal Medicine, 180(11), 1537-1539. https://doi.org/10.1001/jamainternmed.2 020.3030 Xu, Q., Wang, T., Qin, X., Jie, Y., Zha, L., & Lu, W. (2020). Early awake prone position combined with high-flow nasal oxygen therapy in severe COVID-19: A case series. Critical Care, 24, Article No. 250. https://doi.org/10.1186/s13054-02002991-7 March-April 2021 • Vol. 30/No. 2 87 Copyright of MEDSURG Nursing is the property of Jannetti Publications, Inc. and its content may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express written permission. However, users may print, download, or email articles for individual use.