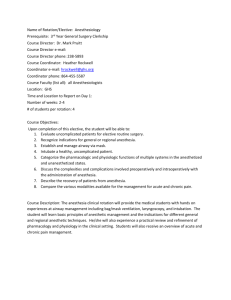
Post Anesthesia Care Unit Postoperative phase Postoperative phase extends from the time the client is admitted to the recovery room, to the time he is transported back into the surgical unit, discharged from the hospital, until the follow up care. Postoperative Nursing Nursing care provided after the client received in the PACU to the follow up evaluation. Goals Restore homeostasis and prevent complication. Maintain adequate cardiovascular and tissue perfusion. Maintain adequate respiratory function. Maintain adequate nutrition and elimination. Maintain adequate fluid and electrolyte balance. Maintain adequate renal function. Promote adequate rest, comfort and safety. Promote and maintain activity and mobility. Provide adequate psychological support. Post Anesthesia Care Unit (PACU) A post anesthesia care unit (PACU), formerly referred to as the recovery room or post anesthesia recovery room, is an area normally attached to operating room suites, designed to provide care for patients recovering from anesthesia. Patient are placed in this unit for easy access to experienced, highly skilled nurses, anesthesiologists or anesthetists, surgeons, advanced hemodynamic and pulmonary monitoring and support, special equipment and medications. Immediate Assessment 1. Before receiving Equipment Proper functioning and monitoring of bedside monitoring equipment, O2 therapy, pulse oximeter, infusion pump and all other equipment. Proper placement 2. After receiving patient Review of intraoperative history and postoperative complication. Type of surgery Post medical history Medication Allergies Intraoperative complication Postoperative instructions Recommended treatment and prophylaxis 1 Airway Patency Oral or nasal airway Laryngeal mask airway Endotracheal tube Breathing Respiratory rate and quality Auscultate breath sounds Pulse oximetry Supplemental O2 Circulation ECG monitoring- rate and rhythm Blood pressure Temperature Capillary refill Color and temperature of skin Peripheral pulses Neurological Level of consciousness Orientation Sensory and motor status Pupil size and reaction Gastrointestinal Nausea, vomiting Intake (fluids, irrigations) Genitourinary Output ( urine, drains) Surgical site Dressings and drainage Pain Incision Other Nursing Diagnosis 1. 2. 3. 4. 5. Ineffective airway clearance related to effects of anesthesia. Impaired gas exchange related ventilation- perfusion imbalance. Ineffective tissue perfusion (cardiopulmonary) related to hypotension postoperatively. Acute pain related to surgical incision and tissue trauma. Impaired skin integrity related to invasive procedure, immobilization and altered metabolic and circulatory state. 6. Risk for imbalanced body temperature related to medications, sedation and cool environment. 7. Risk for deficient fluid volume related to blood loss, food and fluid deprivation, vomiting and indwelling tubes. 8. Risk for injury related to sensory dysfunction and physical environment. 2 Nursing interventions Maintaining patent airway Assess the type of airway and monitor for its patency. Turning the head to one side. 15 to 30 degree unless contraindicated (in spinal cases flat for 68 hours). Proper position of airway. The airway keeps the passage open and prevents the tongue from falling backward and obstructing the air passages. Suction as needed. Monitor for return of gag reflex (coughing/ swallowing) reflex. When the patient is awake and able to protect his own airway, the oral or nasal airway can be discontinued. Maintaining adequate respiration function Ascult the lung sound frequently. Encourage the patient to take deep breaths to aerate the lungs fully and prevent atelectasis, use an incentive spirometer to aid in this function. Periodically evaluate the patient’s level of consciousness. (Note: Alterations in cerebral function may suggest impaired oxygen delivery). Administer humidified oxygen to reduce irritation of airways and facilitate secretion removal. Promoting tissue perfusion Monitor vital signs every 15 mins. Monitor ECG tracing for arrhythmias. Evaluate pulse pressure to determine status of perfusion. (A narrowing pulse pressure indicates impending shock). Monitor intake and output closely. Recognize early symptoms of shock or hemorrhage. Cool extremities, decreases urine output (< 30 ml/hour), slow capillary refill (>3 seconds), decreased BP, narrowing pulse pressure and increased heart rate are usually indicative of decreased cardiac output. Intervene to improve tissue perfusion. Initiate oxygen therapy or increase FiO2 (fraction of inspired oxygen) of existing oxygen delivery system. Increased parenteral fluid infusion as prescribed. Place the patient in the shock position with his feet elevated (unless contraindicated). Minimizing and controlling pain Position the patient to maximize comfort. Assess pain by observing behavioral and physiologic manifestation (change in vital signs may be a result of pain); have the patient rate pain on a scale of 1 to 10. Administer analgesics and document efficacy. 3 Minimize complications of skin impairment Perform hand washing before and after contact with the patient. Inspect dressings routinely and reinforce them if necessary. Record the amount and type of wound drainage. Turn the patient frequently and maintain good body alignment. Stabilizing thermoregulatory status Monitor temperature every 15 mins and be alert for development of both hypothermia and hyperthermia. Report a temperature >101.5º F (38º C) or <95º F (35º C). Report for post anesthesia shivering. Provide warm blankets for patients feeling cold. Provide a therapeutic environment with proper temperature and humidity. Maintaining adequate fluid volume Administer IV solutions as ordered. Monitor intake and output and report it if any abnormalities detected. Monitor electrolyte and recognize evidence of imbalance, such as nausea, vomiting and weakness. Evaluate mental status (skin color and turgor). Recognize signs of fluid imbalance Hypovolemia Decreased blood pressure Decreased urine output Decreased central venous pressure (CVP) Increased pulse Hypervolemia Increased BP Increased CVP Maintaining safety Keep the side rails up until the patient is fully awake. Protect the extremity into which IV fluids are running so that the needle will not become accidentally dislodged. Avoid nerve damage and muscle strain by properly supporting and padding pressure areas. Be aware that patients who have received regional anesthesia may not be complain of an injury, such as the pricking of an open safety pin or a clamp that is exerting pressure. 4 5