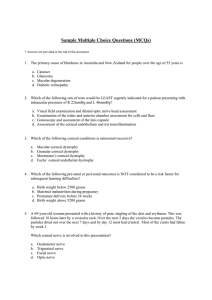
Eye Emergencies Done by : Dr. Obadah Abu Thawabeh Supervisor : Dr. Ghadeer Rbehat Dr. Juma Taha At the end of this presentation we should able to : 1 . Differentiate the types of eye emergency which need immediate intervention 2 . Recognize the signs and symptoms associated with each eye condition 3 .be able to perform a basic eye examination to assess the situation 4 . Perform the suitable first aid to save the eye and the vision as well Sign and symptoms that require immediate referral : • Sudden decrease or loss of vision Hyphaema • Loss of visual field Halos around light • Pain on eye movement • Photophobia Laceration of the lid margin or near medial canthus • Diplopia Subconjunctival hemorrhage • Proptosis of the eye • light flashes and floaters Broken contact lens or shattered eye glasses Suspected globe perforation • Irregular shape pupil • foreign body sensation • Red eye and infected eye Relative Afferent Pupillary Defect (RAPD) done by swinging flashlight test in Dark room. A 7 Years old Female present with painful swelling and redness of upper and lower lid of her right eye. She report having a bug bite near her Right eye . On examination , her eyelid are extremely edematous with well demarcated area of erythema . Ocular examination is normal and normal vision , no RAPD, no proptosis and No motility deficit . What is most likely diagnosis : A) Orbital cellulitis B) Preseptal cellulitis C)Anaphylactic reaction to the insect bite D) Blepheritis Orbital Cellulitis Orbital cellulitis Peri – Orbital cellulitis Post septal cellulitis. Emergency Pre - septal cellulitis Only affects eyelids Orbital cellulitis : Definition : Infection that spreads post orbital septum Etiology : Direct extension ( sinusitis esp. ethmoiditis , dacrocystitis , hordeolum , dental infection) Complication of trauma ( skin trauma with inoculation ) Hematogenous ( if immunocompromised ) Age : Organisms : Mostly in children as orbital septum not fully developed . Gram positive cocci : ( fully developed at age 8 – 9 years old ) H. influenza previously Common also in elderly and immunocompromised . Staphylococcus Streptococcus Aspergillus in DM and immunocompromised Clinical features : Preseptal cellulitis : Lid induration , warm erythema , tenderness , unable to open eye. Additional features seen in orbital cellulitis : Fever Proptosis Chemosis Red flag signs of optic nerve compromises : Reduce vision Reduce color vision ( cons ) RAPD ( specific for optic nerve compromised ) Reduce visual field . Ophthalmoplagia ( pain on eye movement ) Investigation : Management : CBC , CRP , ESR . Admission Blood culture . Broad spectrum antibiotics ( IV for 72 hours then PO for one week ) Imaging ( CT Head = the gold slandered) ENT review to assess for sinus drainage . Repeat CT if any deterioration to exclude posterior extension ( abscess , cavernous sinus thrombosis ). Remember : management of preseptal cellulitis : Warm compresses . PO (10-14 days) and Topical Antibiotics . Complication : Optic nerve inflammation Cavernous sinus thrombosis Meningitis Brain abscess with possible loss of vision Death A 67 years old white man with a history of Coronary artery disease , HTN , DM and a PVD . Present with sudden PAINLESS loss of vision in right eye several hour ago . On examination he has light perception vision , presence of a RAPD and normal anterior segment of the eye . By fundoscopy , fundus appear diffusely white with reddish hue within the macula ( cherry red spot ) . What is the most likely diagnosis ? A ) central retinal artery occlusion B) Anterior ischemic optic neuropathy C) Choroidal ischemia D) Retinal Detachment Central Retinal Artery Occlusion Etiology : Occlusion of blood flow by : 1. Emboli from carotid artery or heart ( AF . Endocarditis , valvular disease ) 2. Thrombus 3. Temporal arteritis Result in acute painless loss of vision due to oxygen starvation of the retinal tissues and eventual cell death . Clinical features : Symptoms : Sudden PAINLESS unilateral loss of vision Signs: RAPD By fundoscopy : - Chery red spot - Retinal pallor - Cotton wool spot (retinal infarct) - Cholesterol emboli (hollenhorst plaque ) Cholesterol emboli (hollenhorst plaque ) Cotton wool spot Chery red spot Treatment : Attempt to restore blood flow within 2 hours ( irreversible retinal damage if > 90 min of complete CRAO ) Massage the globe to dislodge embolus ( compress eye with heel of hand for 10 seconds , release for 10 seconds , repeat for 5 min ) Decrease IOP - topical BB, IV acetazolamide , IV mannitol - or drain aqueous fluid by anterior chamber paracentesis ( carries risk of infection , lens puncture . Nd:YAG laser embolectomy Intra arterial or intra venous thrombolysis . In embolus is seen refer to an internist or neurologist for stroke management. A 56 years old white male with a history of hypertension and DM , complains of double vision and pain for the past 2 days . On examination , his vision is OD 20/50 and OS 20/25 . He has a larger pupil with a RAPD OD . The lid of his right eye is slightly lower than the left . His right eye is deviated slightly temporally and inferiorly and he has difficulty adducting and elevating the eye . What is the most likely diagnosis ? A)grave’s disease B)Horner syndrome C)3rd nerve palsy D)Myasthenia gravis Third Nerve Palsy What are the nerves that are responsible for eye movement ?? CN 3 : occulomotor nerve CN 4 : Trochlear nerve CN 6 : abducent nerve Extra ocular muscles Remember LR6 SO4 Occulomotor Nerve also supply levator palpebrae superioris. ( elevate eye lid ) and have connection with neurons in ciliary ganglion which innervate the pupillary sphincter ( control constriction of the pupil ) What you see in rd 3 nerve palsy ? Ptosis dilated pupil an eye that is down and out. diplopia with or without pain Etiology Aneurysm ( posterior communicating artery aneurysm ) Intraocular tumor Ischemia ( DM ) Trauma Work up : Complete ocular examination CNS imaging to R/O aneurysm or mass ESR and CRP to R/O GCA Treatment : Treat the underlying causes if present . Patch or prism over affected eye if there is symptomatic diplopia ( but not for < 11 years old for the risk of amblyopia ) What is the most likely diagnosis? A) anterior uveitis B) Optic neuritis C) Acute Angle glaucoma D) Giant cell arteritis Glaucoma Definition : Two main types : Optic nerve Damage due to increase IOP. 1. Open angle glaucoma. 2. Closed angle glaucoma . Normal aqueous pathway Aqueous is made by the ciliary body and secreted into posterior chamber . Aqueous passes through the pupil into the anterior chamber . Most of the aqueous leaves the eye via the trabecular meshwork -> schlemm’s canal -> bloodstream . Small portion ( 4%) drains via uveoscleral pathway . acute angle closure glaucoma Pathogenesis = pupil block mechanism In response to pupil dilatation (e.g. dark condition ) -> peripheral iris bunches up -> increase resistant to aqueous flow . Build up of aqueous in posterior chamber -> bows iris forward -> closes drainage angle . Risk factors : Female Family history Small eye ( long sighted , hypermetropic ) Asian ethnicity . Age >70 years old Mature cataract Shallow anterior chamber Pupil dilation ( topical and systemic anticholinergic , stress , darkness ) Acute angle glaucoma is about 5% of all glaucoma cases . Clinical features : IOP > 40 mmHg ( by tonometry ) Cloudy, injected cornea ( seen by slit lamp ) . Fixed , oval , mid - dilated pupil ( seen by slit lamp ) Halos around the light. Red painful unilateral eye . Reduced vision . Watering . Nausea, vomiting , abdominal pain . Halos around light Complication : irreversible loss of vision within hours to days if untreated . Permanent peripheral anterior synechia result in permanent angle closure . Ocular emergency : aqueous suppressants and hyperosmotic agents : - Decrease aqueous humor formation : Topical BB ( timolol ) Topical alfa adrenergic agonist ( brimonidine ) Topical carbonic anhydrase inhibitor (dorzolamide ) Systemic carbonic anhydrase inhibitor ( acetazolamide IV or oral ) - Increase aqueous outflow : topical prostaglandin analog ( latanoprost ) . Topical carbonic anhydrase inhibitor Topical cholinergic ( pilocarpine : mitotic drops to reserve pupillary block ) Hyperosmotic agent : mannitol ( rarely used now , mostly OR cases ) , or oral glycerin . Definitive treatment : Laser peripheral iridotomy (bilaterally) What is the diagnosis you would most worry about ?? A) Cataract B) Endophthalmitis C) GCA D) Retinal detachment E) Vitreous detachment Retinal Detachment Definition The potential space between the neuroretina and the retinal pigment epithelium (loosely attached in the eye ) become separated . Risk factors : Recent eye trauma Retinal detachment in other eye High myope ( short sighted , large eye ). Clinical features : Flashing light . > 100 floaters Shadow over vision , curtain of blackness . RAPD Decrease IOP 4 – 5 mmHg lower than the other eye Most common presentation is unilateral blurry vision without pain or redness (PAINLESS acute loss of vision ) Treatment Prophylactic : symptomatic tear ( flash or floaters ) can be sealed off with laser / cryotherapy . Therapeutic : Rhegmatogenous : - Scleral buckle procedure - Pneumatic retinopathy - Vitrectomy plus injection of gas ( silicone oil in recurrent detachment ) Tractional : Vitrectomy +/- membrane removal / scleral buckling/ injection of intraocular gas or silicone oil as necessary Exudative : nonsurgical , any underlying disease should be treated if possible . What is your most likely diagnosis ?? A)Endophthalmitis B) Orbital cellulitis C)Acute closed angle glaucoma D)Keratitis E) Retinal detachment Endophthalmitis Definition : Serious but rare inflammation of the interior eye. Risk factors : Recent ocular surgery Complicated surgery Immunocompromised Poor lid hygiene Clinical features : Present within one week of surgery with : - Severe pain - Loss of vision - Red eye - Hypopyon Organisms : Staph aurues Staph epidemidis Treatment IV broad spectrum antibiotics Take sample from aqueous and vitreous Ischemic optic neuropathy It is the most common cause of optic nerve pathology causing visual loss in patients older than 50 years . Caused by blockage of optic nerve blood supply Blockage can be due to : • Inflammation of the arteries as a part of Giant cell arteritis = Arteritic Type or • Without inflammation of arteries = non arteritic type ( most cases are idiopathic ) . Blood supply to the optic nerve Anterior part : optic nerve head , which is supplied primarily by the posterior ciliary circulation . Posterior part : supplied by multiple sources other than posterior ciliary circulation . Classification of ION : 1 - Anterior ION : involve 1mm segment of the optic disc so it will cause disc swelling or edema 2 – Posterior ION : involve any portion of optic nerve posterior to the optic disc so will not cause disc edema . Anterior ION : Arteritic Non arteritic Posterior ION Arteritic Non arteritic Surgical : as a complication from a surgical complication . Non Arteritic is more common than Arteritic type Arteritic ION is much more emergent than Non Arteritic . Anterior ION is more common than Posterior ION. PION is very rare and is generally a diagnosis of exclusion. Arteritic Ischemic Optic Neuropathy ( GCA ) Symptoms : Amaurosis fugax is an early sign . Proximal muscle and joint aches (polymyalgia rheumatic) Sudden PAINLESS visual loss Anorexia Unilateral (may become bilaterally ) Weight loss Age : >= 55 Headache Jaw claudication Scalp tenderness Fever ( may occur ) Signs : Relative Afferent pupillary Defect (RAPD) Visual loss ( counting fingers or worse ) Pale swollen disc High ESR , CRP markedly and may be platelets Visual field defect Palpable tender non pulsatile temporal artery . CRAO or CN ( esp. 6th ) may occur Workup : History : age is a critical Complete ocular examination . ESR , CRP , Platelet. Temporal Artery Biopsy : one week after initiation of systemic steroid . Treatment : Systemic steroid immediately once GCA is suspected Methylprednisolone 250mg IV q 6 h for 12 doses then prednisolone 80-100 mg PO daily . Note that without steroid , other eye can become involved within 1 to 7 days . Treatment should last at least 6 to 12 months with smallest steroid dose that suppresses the disease . Don’t forget to give the patient PPI or H2 blockers and medication to help prevent osteoporosis ( vit D and Ca ) NON Arteritic ION Etiology : Mostly Idiopathic . Risk factors : Atherosclerosis DM HTN Dyslipidemia Anemia Nocturnal hypotension (esp. in pt. with antiHTN medications. Symptoms : Signs : Sudden painless loss of vision (moderate degree) RAPD Unilateral (may become bilateral) Normal ESR and CRP. Age 40 to 60 . Pale optic disc swelling . Treatment : Observation . Consult internist to rule out CVD , DM, HTN and sleep apnea . Avoid antiHTN medications at bedtime to avoid nocturnal hypotension. A 42 year old bookkeeper presents with a complaint of red painful eye and she feels like there is something in her right eye . Discharge and blurry vision. On examination her pupils are equal, round, reactive to light but her right eye has diffuse injected. She also complains photophobia. You perform fluorescein staining, which reveals an area of focal corneal uptake . Which of the following is the most likely diagnosis ? A)Acute angle closure glaucoma B) Corneal abrasion C)Subconjuctival hemorrhage D)Uveitis . Corneal abrasion Definition : Scratch on your eye . injury is limited to the epithelium of the cornea . Clinical features : Symptoms : Signs : History of scratching or hitting the eye . Epithelial defect that stains with fluorescein . Sharp pain Absence of underlying corneal opacification that indicates infection or inflammation . Photophobia Foreign body sensation Tearing Discomfort with blinking Investigation : Slit lamp examination : use fluorescein dye Evert the eye lid to ensure no foreign body is present Treatment : Topical antibiotic : - Non contact lens wearer : ointment or drops e.g. Ointment ( erythromycin , bacitracin q 2 - 4 hours ) Drops ( fluroquinolones q 6 hours . - Contact lens wearer : should have antipseudomonas coverage ( fluroqinolones q 6 hours , ointment or drops ) • Patching is rarely necessary : can cause serious abrasions if not used properly . • Cycloplegic agents for traumatic irtis which may develop 24 – 72 hour post trauma . • Consider topical NSAID for pain control Ointment vs. Drops Ointment offer better barrier and lubrication between eyelid and abrasion Ointment tend to blur vision temporarily . May use the ointment to augment drops at bedtime . Prefer frequent ointment . Corneal Ulcer Etiology : Local necrosis of corneal tissue due to infection. Injury extend to the stroma of the cornea . Infection is usually bacterial , rarely viral , fungal or protozoa 2ry to corneal exposure to abrasion . Foreign body , contact lens use ( 50% of ulcers) Also associated with conjunctivitis , blepharitis , keratitis , vit A deficiency Clinical picture : • Pain , photophobia , tearing , foreign body sensation , decrease visual acuity if central ulcer • Corneal opacity • Corneal epithelial defect that stains with fluorescein . • May develop corneal edema • Bacterial ulcers may have purulent discharge , viral ulcers may have watery discharge . Complication Investigations Decrease vision . Fluorescein stain . Corneal perforation Iritis Endophthalmitis Treatment : Must treat vigorously to avoid complications Culture prior to treatment Topical antibiotic every hour What is your most likely diagnosis ? A)Acute angle closure glaucoma B) Bacterial keratitis C)Viral keratitis D)Anterior uveitis E) Endopthamitis Bacterial Keratitis : Definition : Inflammation of the cornea . Commonly infective (bacterial , viral , fungal ) Risk Factors : Contact lenses . A breech in the corneal epithelium ( e.g. Trauma ) Dry eye . Prolonger use of steroid drops. Etiology : Pseudomonas ( most common in CL wearer ) Staphylococcus Streptococcus Moraxella Serratia species Clinical features Painful eye Red eye Purulent discharge Blurred vision Hypopyon ( collection of WBCs) White corneal opacity = corneal ulcer Photophobia Investigation : Stain with fluorescein see epithelial defect Corneal scrape : gram stain and culture Management : Stop wearing contact lenses until healed . Topical antibiotic drops : ciprofloxacin , ofloxacin . A 35 years old woman comes to your office with an acutely inflamed and painful left eye . Her symptoms started 2 days ago. There is some visual blurring . On examination there is a diffuse inflammation of the left conjunctiva. On fluorescein staining , dendritic ulcer is seen in the center of the cornea. Visual acuity is intact What is the most likely diagnosis ? A) Corneal abrasion B) Herpetic corneal ulcer C) Adenoviral ulcer D) Bacterial keratitis . Dendritic ulcer Viral keratitis : Herpes simplex keratitis ( HSV 1, 90% of population are carriers ) May be triggered by stress , fever , sun , exposure , immunosuppression . Clinical features • Reduced vision ( depend on the location and the size of the ulcer ) • Pain • Photophopia • Red eye • Watery discharge Fluorescein staining : Dendritic ulcer Complication : Corneal scarring ( can lead to loss of vision ) Chronic interstitial keratitis due to penetration of virus into stroma Secondary iritis , secondary glaucoma . Treatment : Antiviral eye drops ( acyclovir ) Oral acyclovir for sever infection Cycloplagic drops (cyclopentolate) to relive pain caused by ciliary spasm. topical antibiotics for ulcers suspected of being infected by bacteria . Topical corticosteroids are absolutely Contraindicated in dendritic ulcer . A 55 years old man presented to ER complaining of ocular pain and irritation . He reports accidently splashing ammonia in both eyes . His visual acuity is OD 20/100 and OS 20/80 . Both eyes are injected with corneal edema . What is the immediate first step in treatment of chemical injuries to eye ?? A)Complete ocular examination B)Manual removal of particulate material followed immediately by irrigation with water or saline until the PH is 7 C)Application of topical glycerin to clear corneal edema D)Topical anesthetic with debridement of surface epithelium Chemical injury to the eye Accidently or intentional exposure of the eye to chemical agent with potentially blinding complications. Most patients will remember a chemical insult . Alkali injury are frequently more severe than acids as it can penetrate deep into the eye and lead to substantial intraocular inflammation and damage . Clinical features : Pain Photophobia Reduced vision Difficulty in eye opening Investigations : PH measurement Complications : Glaucoma Cataract Permanent corneal opacification Treatment : Immediate irrigation of the eye wilt normal saline A drop of topical anesthetic after PH measurement . Irrigation should continue until PH is 7.0 – 7.5 Swab should be used to sweep any particular matter Remember : NEVER neutralize. A 20 years old male presents to the ER with bloody eye after he was hit in it. His visual acuity is hand motion only , he also has moderate lids edema but still can open his eye . By slit lamp the pupil appears normal . Motility is normal and no diplopia . what is the most important first step in evaluation of this patient : A)Detection of a RAPD B) Patching until the heme clears C)Evaluation for possible open globe D)CT scanning to evaluate for an orbital fracture Traumatic Hyphema Open globe: Clinical features : Symptoms History of eye Trauma blunt or penetrating Signs : Hyphema ( blood )in the anterior chamber Pain Full thickness scleral or corneal laceration Decrease vision Severe subcongunctival hemorrhage Loss of fluid from the eye Irregular pupil Intraocular contact may be outside of the globe . Investigations : CT scan of brain and orbits to rule out intraocular foreign body Seidal test . Treatment : Admission to the hospital Systemic antibiotics within 6 hours of the injury Tetanus toxoid if needed Antiemetic PRN for Nausea and vomiting Pain killers Arrange for surgery ASAP . Eyelid laceration Partial or full thickness defect in the eyelid after facial trauma . Often associated with other ocular injuries ( corneal abrasions, foreign bodies , open globe …. Symptoms : • Peri orbital pain • Tearing • Bleeding Investigations : • Complete ocular examinations • CT scan of brain , orbits , midface if history of severe blunting or penetrating injury to rule out fracture, retained FB , rupture globe or intracranial injury . Treatment : Consider Tetanus prophylaxis Systemic antibiotics for 7 – 10 days if contamination or FB is suspected ( amoclan 625 1x2 or 1x3 , 1gm 1x2 ..) For human or animal bites consider penicillin and rabies prophylaxis . Repair eyelid laceration in minor room surgery Corneal and conjuctival foreign body Clinical features : Foreign body sensation Tearing History of trauma Work up : • Visual acuity • Slit lamp examination • Evert the eyelids to exclude retained foreign bodies Treatment Apply topical anesthetic Remove the FB Treat the corneal abrasion if present ( epithelial defects Topical antibiotics and preservative free artificial tears my be given in case of conjunctival FB Blowout fracture A 14 years old boy is bought to the emergency after suffering a high impact injury when football his right eye , no loss of consciousness but complaining of right facial pain . By imaging , orbital blowout fracture is seen . Which bone most likely to be involved ?? a)Maxillary bone b)Zygomatic bone c)Frontal bone d)Sphenoid bone Definition : break of one or more of the bones that surrounds the eye . Why does it occur ? Object strikes the eye -> force is transmitted into the orbit -> thinnest orbital bones fracture . the release of this force protects the eye from more serious injury . Most common fracture sites : Orbital floor ( esp. maxillary bone ) Medial wall . Clinical Feature : Eyelid swelling Pain Reduced vision Diplopia ( if inferior rectus affected) Surgical emphysema Enophthalmous or proptosis ( retrobulbar hemorrhage ) Hypoesthesia bellow lower lid ( infraorbital nerve injury ) Investigations Imaging : Management : ABC (multitraum ) - facial XR Antibiotics : broad spectrum - CT Tetanus vaccine if open wound. Refer to ophthalmology and oromaxillofacial .