1. General principles of asepsis and antiseptics
Asepsis = no putrefaction
In Western Europe and USA „asepsis“ and „antisepsis“ are synonyms.
The fundamental components of aseptic procedures:
- the environment (the operating room)
- the patient
- the participants in the operation
- the instruments and other materials used
In Eastern Europe there is a difference in the basic meaning of „asepsis“ and „antisepsis“:
Asepsis (Sterilization)
• Where?: In the environment and on the surface of surgical instruments and materials
• How?: In general, by using the laws of Physics
• Why?: Prevention of surgical infection
Antisepsis (Desinfection)
• Where?: In the human body and on the skin surface (patient and participants)
• How?: In general, by using Chemical Substances
• Why?: Prevention of/ Treatment of surgical infection
Asepsis- aseptic agents and methods
- Asepsis is the practice to reduce or eliminate contaminants (e.g. bacteria, viruses, fungi and
parasites) from entering the operative field in surgery to prevent infection
- aseptic procedures concerning the environment, the surgical instruments and materials
Methods:
Steam:
- more effective than dry heat
- high temperature steam - under pressure - duration:
• 115°C - 0,5 atm. - 1 hours
• 120°C - 1,0 atm. - 45min
• 134°C - 2,0 atm. - 30 min
- heat-sensitive tape as an evidence
- steam is mainly used for sterilization of surgical cotton equipment - garments, sheets, bandagematerials, etc.
- less often used for surgical metal instruments
Steam autoclaving
- chemical indicators can be found on medical package and these change colour once the correct
conditions have been met
- color change indicates that the object inside the package has been autoclaved sufficiently
Page 1 of 269
Dry Heat
- air heated up to 160-200°C
- because dry heat can dull sharp instruments and needles, these items should not be sterilized at
temperatures higher than 180°C
- duration: 45-60min
- dry heat is mainly used for sterilization of surgical metal instruments
- devices for that type of sterilization are usually placed in the operation theatre
Gas
- most effective method of gas chemical sterilization is the use of ethylen oxide gas (ETO)
- ETO gas-sterilization period range from 3-7 hours
- used for equipment made of plastics or other polymers - surgical gloves, nasogastric tubes,
catheters, etc.
Different type of rays, etc.
- ultra-violet, infra-red rays, gamma ray sterilization
- used in plants and factories, producing single-use medical equipment - suture materials,
syringes, needles, catheters, tubes, etc.
Aseptic procedures concerning environment
- the traffic in the operation theatre must be limited
- the operation rooms should be equiped with air filters
- positive pressure ventilation
- laminar flow
- regular cleansing or floors, walls, windows, tables, etc. with antibacterial agents
- different operation rooms for „clean“ and „contaminated“ surgical procedures
Antisepsis = against putrefaction
Antisepsis- antiseptic agents and methods
- antisepsis is the prevention or/and treatment of infections by inhibiting or arresting the growth
and multiplication of germs (infectious agents)
- antiseptic procedures are concerning the patient’s preparation for operation and the surgeon’s
preparation for operation
- disinfectants includes several oxidants, halogens or halogen-releasing agents, alcohols,
aldehydes, organic acids, phenols, cationic surfactants and heavy metals
- disinfectants act by the denaturation of proteins, inhibition of enzymes or a dehydration
Antiseptic agents for the disinfection of rooms:
- surface (floor) disinfection employs aldehydes combined with cationic surfactants and oxidants
or, more rarely, acidic or alkalizing agents
- room disinfection: room air and surfaces can be disinfected by spraying or vaporizing of
aldehydes, provided that germs are freely accessible
- cetridine forte
- deconex
Page 2 of 269
Antiseptic procedures concerning environment
- the traffic in the operation theatre must be limited
- the operation rooms should be equiped with air filters
- positive pressure ventilation
- laminar flow
- regular cleansing or floors, walls, windows, tables, etc. with antibacterial agents
- different operation rooms for „clean“ and „contaminated“ surgical procedures
Antiseptic agents for disinfection of the skin or for local use (wound)
- jod-benzinum - 1% iodine solution in light benzin
- jodum/iodine/ -1%-5%-20% - alcoholic solution - tincture of iodine
- ethanol (alcohol) - 70% and 96%
- hydrogen dioxide - 3%
- iodophor compounds (povidone iodine = braunol = jodasept)
- chlorhexidine (hibitane, hibiscrub)
- antibiotics
Antiseptic procedures concerning the patient’s preparation for operation
- antibacterial shower on the night before or the day of operation
- mechanical bowel preparation
- antibiotics - in cases of current infection
- hair clipping of surgical field (the area of the planned operation)
- skin preparation in the area of the procedure with betadine or chlorhexadine
- covering the body of the patient with sterile sheets
Antiseptic procedures concerning the surgeon’s preparation for operation
- covering hair and wearing face masks
- the hands and the arms to the elbow are scrubbed
- the purpose of surgical hand scrub:
• remove dirt from nails, hands and forearms
• reduce resident and transient flora levels
• prevent fast re-growth of bacteria
- essential property of antimicrobial agent used for surgical hand scrub - antimicrobial agents
must have persistent action (also in moist environment) to inhibit bacterial growth
2. Antibiotic therapy and prophylactics in the treatment of surgical patients
Antibiotics - substances produced by microorganisms to suppress the growth of other
microorganisms
Antimicrobial agents - encompasses agents synthesized in laboratory and natural antibiotics
produced by some microorganisms (antimicrobial agent has a broader meaning than antibiotics)
Mechanisms of antimicrobial action
• bactericidal agent -> organisms are killed
• bacteriostatic agent -> organisms stop growing
• both effective as chemotherapeutic antimicrobial drugs
Page 3 of 269
Classification according to the point in the cellular biochemical pathways at which the agent
exerts its primary mechanism of action (5 major groups):
1. Inhibition of synthesis and damage to the cell wall:
- penicillins
- cephalosporins
- monobactams
- carbapenems
- bacitracin
- vancomycin
- cycloserine
2. Inhibition of synthesis or damage to the cytoplasmic membrane
- polymyxins
- polyene antifungals
3. Modification in synthesis or metabolism of nucleic acids:
- quinolones
- rifampin
- nitrofurantoins
- nitroimidazoles
4. Inhibition or modification of protein synthesis
- aminoglucosides
- tetracyclines
- chloramphenicol
- erytromycin
- clindamycin
- spectinomycin
5. Modification in energy metabolism (folic acid metabolism):
- sulfonamids
- trimethoprim
- dapsone
- isoniazid
Drug selection - factors:
1. Identification of the microorganism
• determine the possible pathogen in the infection site (wound exudates, sputum, urine, CSF,
blood,…)
• gram stain - the fastest, simplest and most inexpensive way
• other methods: agglutination, immunoelectrophoresis, direct immunofluorescence techniques
• in cases impossible to obtain a specimen - previous knowledge and experience (emperic
antimicrobial therapy)
2. Antimicrobial susceptibility of the microorganism (disk diffusion method, 18-48 hrs)
3. Bactericidal versus bacteriostatic (bacteriostatic often adequate in uncomplicated infection)
Page 4 of 269
4. Host status (age, renal and hepatic function, allergies, pregnancies, anatomical site of
infection,…)
General principles of antibiotic therapy
• goal is to achieve antibiotic levels at the site of infection that exceed the minimun inhibitory
concentration for the pathogens present
• for mild infections, mostly oral antibiotics are given
• for severe surgical infections, the most initial antibiotic therapy is given intravenously, because
the systemic response to this infection makes the gastrointestinal absorption of antibiotics
unpredictable; also in intra-abdominal infections, the GI function is often directly impaired
• Why is the patient failing to improve? (if obvious improvement not seen)
- initial operative procedure was not adequate
- initial procedure was adequate but a complication has occured
- a superinfection has developed at a new site
- the drug choice is correct but not enough has been given
- another or different drug is needed
• in surgical infections there is no specific duration of antibiotic treatment that is known to be ideal
• antibiotics generally support local host defense until the local response is sufficient to limit further
infection
• for deep-seated or poorly localized infections, longer treatment may be needed (3-5 days in
uncomplicated ones)
• a reliable guideline is to continue antibiotics until the patient has shown obvious clinical
improvement based on clinical examination and has had a normal temperature for 48 hours or
longer (signs of improvement include improve mental status, return of bowel function, resolution
of tachycardia, spontaneous diuresis)
Pharmacological description of an antimicrobial agent
I. Route of administration - oral, intramuscular, intravenous; local - spray, ointment, powder,
solution
II. Pharmacokinetics and pharmacodynamics (absorption, peak serum concentration, metabolism,
excretion)
III. Interval of administration
IV. Toxicity and side effects
V. Prophylaxis with antimicrobial agents (recommended for operations with a high risk of postoperative wound infection; or with low risk of infection, but significant consequences if infection
occurs; administered i.v. directly before operation, single dose mostly sufficient)
VI. Antimicrobial combination of 2 or 3 agents (may result in indifference, syngergism and
antagonism)
- to treat life-threatening infection
- to treat polymicrobial infection
- to prevent emergence of resistant bacteria
- to use a lower dose of one of the antibacterial drugs
- the enhance the antibacterial activity
Page 5 of 269
VII. Bacterial resistance mechanisms
- either intrinsic or acquired
- intrinsic is an inherently resistance to a specific antibiotic
- acquired resistance is due to a change in genetic composition
- molecular mechanisms by which bacteria acquire resistance:
a) decreased intracellular concentration of antibiotics, either by decreas influx or
decreased efflux (e.g. pseudomonas to beta-lactams)
b) neutralization by inactivating enzymes
- most common for antibiotic resistance
- affects all beta-lactam antibiotics
- e.g. beta-lactamases from gram-positive and gram-negative bacteria)
c) alteration of the target at which the antibiotic will act (e.g. pneumococcus to penicillin)
d) complete elimination of the target at which the antibiotic will act
Penicillins
• broadly divided into those that are stable against staphylococcal penicillinase and all others
• antistaphylococcal penicillinsa are active against methicillin-susceptible staphylococcal species,
reduced activity against streptococcal species, no activity against gram-negative rods or
anaerobic bacteria
• remaining penicillins are readily hydrolyzed by staphylococcal penicillinase -> unreliable for
treating staph infections
• all have excellent activity against other gram-positive bacteria except enterococci (variably
resistant)
Cephalosporins
• largest and most frequent used group
• commonly divided into three generations, but there are also important differences between
memebers in each generation
• first generation has excellent activity against methicillin-susceptivel staphylococci and all
streptococcal species
• no cephalosporin in any generation has reliable activity against enterococci, many even seem to
encourage enterococcal overgrowth
• only important difference between members of first generation is the half life: cefazolin has
longer half-life and ca be given every 8 hours rather than every 4 to 6
• second generation cephalosporins have expanded gram-negative activity compared to first
generation, but still lack activity against many gram-negative rods
• 2nd G not reliable for treatment for empirical treatment of hospital-acquired infections with gramnegative rods
• most important distiction within 2nd G is between antibiotics with good acitivty against anaerobes
(cefoxitin and cefotetan) and those without anaerobic activity (cefamandole, cefuroxime,
ceforanide and cefonicid); within each group are antibiotics with rel. short half life ( cefamandole
and cefoxitin) and with rel. long half life (cefuroxime, cefotetan, ceforanide and cefonicid)
• third genereration cephalosporins have greatly expanded activity against gram-negative rods
Page 6 of 269
Sulfonamides
• sulfonamide is the basis of several group of drugs
• original antibacterial sulfonamides are synthetic antimicrobial drugs that contain sulfonamide
group
• allergies to sulfonamides are common (3%)
• because sulfonamides displace bilirubin from albumin, kernicterus (brain damage due to excess
bilirubin) is an important potential side effect
• Antimicrobial sulfonamides:
- short-acting: sulfacetamide, sulfadiazine, sulfadimidine, sulfafurazole, sulfisomidine
- intermediate-acting: sulfadoxine, sulfamethoxazole, sulfamoxole, sulfanitran
- long-acting: sulfadimethoxine, sulfamethoxypyridazine, sulfametoxydiazine
- ultra-long acting: sulfametopyrazine
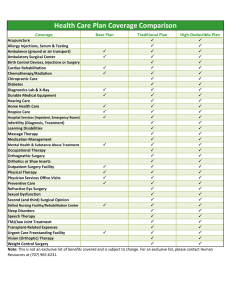
Examples of prophylactic antibiotic selection for various operations
Operation
Standard selection
Penicillin Allergy
MRSA colonization
Breast
Cefazolin
Vancomycin
Vancomycin
Cardiac surgery
Cefazolin/vancomycin
Vancomycin/gentamicin
Cefazolin/vancomycin
Hernia
Cefazolin
Gentamicin/Clindamycin
Vancomycin/gentamicin
Neurosurgery
Cefazolin
Vancomycin
Vancomycin
Plastic surgery
Cefazolin
Vancomycin
Vancomycin
Renal transplantation
Cefazolin
Vancomycin
Vancomycin
Soft tissue
Cefazolin
Vancomycin (foreign
body)
Clindamycin (no foreign
body)
Thoracotomy or
laparotomy
Cefazolin
Vancomycin
Vancomycin
Bariatric surgery
Cefazolin/metronidazole
Vancomycin/
metronidazole
Vancomycin/
metronidazole
Biliary (elective)
Cefazolin
Clindamycin/gentamicin
Cefazolin
Biliary (emergency)
Ceftriaxone
Gentamicin
Colorectal surgery
Cefazolin/metronidazole
Clindamycin/gentamicin
Cefazolin
Gynecology
Cefoxitin or cefazolin/
metronidazole
Clindamycin/gentamicin
Cefoxitin or cefazolin/
metronidazole
Urology (no entry into
urinary tract or
intestine)
Cefazolin
Clindamycin
Cefazolin
Urology (entry into
urinary tract or
intestine)
Cefoxitin
Clindamycin/gentamicin
Cefoxitin
Clean
Clean-contaminated
Page 7 of 269
Operation
Standard selection
Penicillin Allergy
Ceftriaxone/
metronidazole
Clindamycin/gentamicin
MRSA colonization
Contaminated or dirty
Gastrointestinal
(emergency)
3. Perioperative Period. Preparation of the patient for surgical treatment
Preoperative visit
- enables to patient to meet the anesthesiologist and (operating) doctor and to discuss the
procedures and possible worries
- the anesthesiologist may explain in simple term how the patient will be cared for during and
after anesthesia, as well as the ways for postoperative pain relief
- the (operating) doctor can explain the possible risks and complications of the procedure
- at last informed consent is taken
History
- should establish the patient’s surgical problem and the presence of any concurrent disease
- history of previous anesthesia, complications or any problems
- diseases of respiratory and cardiovascular systems
- a history of allergies
- familiy history of hereditary conditions associated with anesthetic problems (porphyria,
malignant hyperthermia, hemophilia, etc.)
- pregnancy — the presence of pregnancy is a contraindication for elective surgery
- a history of jaundice, particularly viral hepatitis or HIV infection
- a medication history — present therapy or drug intolerances (complete history is essential
because many drugs interact with anesthetics or anesthetic techniques)
Physical examination
- a full physical examination should be undertaken and documented in the case records
- the anesthesiologist pays particular attention to the assessment of the ease of tracheal
intubation
• the patient should be inspected for loose teeth, protruding upper incisors or dentures
• the extent of mouth opening and the degree of cervical spine flexion are also very important
• the anatomy of the face and neck of the patient should be evaluated too
• a difficult orotracheal intubation may be predicted by the inability to visualize certain
pharyngeal structures
Malampati classification
Page 8 of 269
Laboratory and other investigations — Guidelines for laboratory testing
a) Urine analysis — every patient
b) Hemoglobin concentration
• all menstruating women
• all patients over 50 years of age
• before major surgery or when significant blood loss is expected
• history of blood loss, pallor
c) Creatinine and serum electrolytes
• history of diarrhea, vomiting, metabolic disease or diabetes
• renal or hepatic disease
• patients receiving medications with diuretics, digoxin, steroids, antihypertensives
• all patients over 60 years of age
d) Liver function test
• hepatic disease
• abnormal nutritional state or metabolic disease
• history of large intake of alcohol
e) Blood sugar concentration
• all patients receiving steroids
• all patients who have diabetes or vascular disease
• all patients over 40 years of age
f)
Coagulation tests
• history of bleeding or bleeding disorders
• patients receiving anticoagulant therapy
• all patients with liver disease
g) Chest X-ray
• history or findings of cardiopulmonary disease
• all patients with malignant disease or echinococcosis
• before thoracic surgery
• all patients over 60 years of age
h) Electrocardiogram
• cardiovascular disease
• all patients with hypertension
• all patients over 40 years of age
Risk assessment
- Anesthetic risk is difficult to ascertain precisely, because it is influenced by a combination of
factors
- the ASA (American Society of Anesthesiologist) grading system is a useful and easy way for risk
assessment:
• Class 1 — a normal healthy patient
• Class 2 — a patient with mild systemic disease
• Class 3 — a patient with severe systemic disease
• Class 4 — a patient with severe systemic disease that is a constant threat to life
• Class 5 — a moribund patient who is not expected to survive without the operation
• Class 6 — a declred brain-dead patient whose organs are being removed for donor
purposes
If the surgery is an emergeny, the physical status classification is followed by „E“
Page 9 of 269
Premedication
- refers to the administration of drugs in the period 1-2 hours before the induction of anesthesia
- the primary reasons for premedicating patients are:
• to relieve anxiety
• to induce sedation and anterograde amnesia
• to promote hemodynamic stability
• to minimize the chances of aspiration of acid gastric contents
• to provide analgesia and enhance the hypnotic effect of general anesthetics
• to prevent postoperative nausea and vomiting
• to control oral secretions
• to control infection
- Drugs used for premedication are benzodiazepines, neuroleptics, opioid analgesics,
anticholinergic drugs, alpha2-adrenergic agonists, H2-receptor agonists
- Antibiotics are given sometimes in the immediate preinduction period for infection control in
particular patients
- Usually one or two drugs, rarely more are prescribed for premedication
4. Trauma. Traumatism. General principles and treatment
Trauma
Etiology
- physical - mechanical (compression and traction), electrical, thermal (high and low temperature),
radioactive, etc.
- chemical
- biological (bites and stings)
Pathogenesis
Effects of traumatic factor on the human body depends on:
- the type of traumatic factor - size, weight, shape, structure, physical status, chemical
structure, bacterial contamination, etc.
- anatomical and physiological status of tissues and organs being damaged
- pathological condition
Every trauma may cause necrosis, vascular and neural disorders and permanent damage of
normal structure and function of regeneration is not complete and sufficient
Clinical signs
- specific - typical for every kind of trauma
- common - can be general (different degrees, from non to life-threatening (shock)) and local,
which always presents pain, hemorrhage, lymphorrhea, infection, loss of function
- according to the integrity of covering tissues, trauma my be blunt or wounds
Page 10 of 269
Blunt trauma
- Blunt-force trauma is that trauma not caused by instruments, objects or implements with
cutting edges; but can have margins and angles
- The nature of the force applied may include blows (impacts), traction, torsion and oblique or
shearing forces
- Blunt-force trauma may have a number of outcomes:
• no injury
• tenderness
• pain
• reddening (erythema)
• swelling (oedema)
• bruising (contusion)
• abrasions (grazes)
• lacerations
• fractures
- Blunt impact injuries can be describes (in terms of force applied) as being weak (e.g. a ‚gentle‘
slap on the face), weak/moderate, moderate, moderate/severe or severe (e.g. a full punch as
hard as possible)
- The more forceful the impact the more likely that visible marks will be evident
- Tenderness is pain or discomfort experienced on palpation by another of an area of injury
- Both pain and tenderness are subjective findings and are thus dependent on (1) the pain
threshold of the individual and (2) their truthfulness
- The other features of blunt-force injury are visible effects of contact
- Reddening describes increased blood flow to areas that have been subject to trauma, but not
to the extent that the underlying blood vessels are disrupted
- Reddening must be distinguished from red bruises by its ability to blanch from finger pressure
Mechanism of blund trauma
1) Hit (impact)
2) Compression
3) Extension
4) Friction
Any injury should be described in detail according to:
- its location (anatomical posture of the body)
- its type, size, color (dating of bruises)
- signs of healing, signs of treatment (sutures)
- concomitant injuries in deeper soft tissues
Classification of blunt trauma
1) Abrasions
2) Contusions - Bruises
3) Lacerations
4) Bone fractures
5) Internal Organ injuries
Contusion (bruises)
Any mechanical trauma caused by a blow, resulting in hemorrhage beneath unbroken skin.
Clinical signs are pain, hemorrhage (subcutaneous or submucosal), local swelling and loss of
function.
Types of hemorrhage in contusion:
- hematoma - a localized mass of extra-vasated blood that is relatively or completely
confined within an organ or tissue
- petechiae - small hemorrhagic spots, of pinpoint or pinhead size
- ecchymosis - larger than 3 mm in diameter
- suffusion - a superficial hematoma
- suggilation - submucosal hemorrhage
Page 11 of 269
Morell-Lavallee’s syndrome
- specific type of blunt trauma in which the traumatic agent hits the skin in a tangential direction
- this causes rupture of the connection between the skin and subcutaneous fat tissue on one hand
and the underlying fascia on the other -> a cavity filled with lymph (and blood) appears
- local clinical signs are swelling, decreased local temperature, paleness, loss of sensitivty, later
necrotic skin
- treatment include pncture and evacuation of fluid and compressive bandage
Blunt crush of a limb
- the traumatic factor (e.g. a heavy object, vehicle) causes compression and traction on the skin
and all underlying tissues and structures
- skin integrity is preserved, but nerves, blood an lymph vessels, muscles and junctions are
ruptured and bones are fractured
- pain and blood loss result in shock
- possible complication is crush syndrome in which develops shock and acute renal failure
- clinical signs are shock, local physical symptoms - pain, paleness and/ or multiple hematomas,
decreased local temperature, total loss of sensitivity and function, bone fractures, …
Rupture
- break of any organ or soft tissues
- common are ruptures of msucles, tendons and nerves
- clinical signs of muscle rupture include pain, hematoma, loss of function, a furrow can be seen
and palpated; treatment - immobilization and suture
- rupture of a tendon - signs and treatment are similar to those of a muscular rupture and the only
difference is in the location
- clinical signs of a nerve rupture are motor disturbances (loss of ability of active motion) and
sensory disturbances (loss of sensitivity); suture is obligatory for basic nerves
Joint injuries
- Classified as sprain of a joint, subluxation and luxation/dislocation
- Joints that are commonly injured are the shoulder, interphalangeal joints, metacarpophalangeal
joint of thum, the elbow, hip and ankle
Sprain of a joint
- results from a motion greater than normal and develops a partial or complete rupture of the
capsule and ligaments, but without dislocation or fracture
- clinical signs are pain, swelling, loss of function, subcutaneous hematoma
- treatment include immobilization, compressive bandage of the joint, physiotherapy and
nonsteroidal antiinflammatory drugs
Page 12 of 269
Luxation (dislocation)
- It is a disarrangement of the normal relation of the bones entering into the formation of a joint
- The articular surfaces of opposing bones completely (luxation) or incompletely (subluxation) and
persistently separate
- It can be congenital, acquired or traumatic, pathologic (direct and indirect trauma, acute and
recurrent, simple and complicated; complicated by means of: a fracture accompanies the
luxation, an open luxation, nerve/vessel rupture)
- The pathological changes include luxation, rupture of a capsule, ligaments, tendons (st),
hemarthrosis and hematoma
Clinical features:
- pain, swelling and tenderness
- loss of function; active and passive motion are limited in dislocation
- loss of normal joint contour
- fixed position and spring-like resistance
- relative elongation or shortening of the limb
- neurologic injury (sometimes) — the incidence is much higher with dislocations than with
fractures
Diagnosis:
- the examination should include adequate evaluation of the joint involved, mechanism of injury,
previous injury to affected joint, remainder of the affected limb, neurovascular status, overlying
skin/soft tissues, associated injuries
- x-ray — obligatory for establishing diagnosis and before treatment
Treatment:
- anesthesia (analgesia)
- reduction - conservative or surgical (open reduction)
• a manipulation to place the bones into the proper relationship
• early/rapid reduction of the joint to: relieve/prevent ischaemic damage to the overlying soft
tissues (e.g. skin), avoid traction/ischaemic damage to nerves, prevent/relieve external
pressure effects on vascular structures, limit damage to articular cartilage
- immobilization: post-reduction, the joint should be adequately immobilized or stabilized for long
enough to allow soft tissues to heal
- physiotherapy/rehabilitation: early and appropriate joint and soft-tissue rehabilitation should be
performed to protect joint surfaces, minimize risk of recurrences, prevent post traumatic
stiffness, regain range of movement and power, regain function of affected joint or limb
Fracture
Fracture is a break in the continuity of a bone or cartilage
Classification:
1. Degree
- greenstick (one cortex is broken while the other remains intact)
- fissured fracture
- complete fracture
Page 13 of 269
2. Congenital (intrauterine) and acquired
- acquired - traumatic or pathological (produced by less force required to break a normal bone,
at the site of preexisting disease)
3. According to mechanism of fracture (direct and indirect force)
4. Closed (simple) and open (compound) fracture (in open fracture bone protrudes through the
skin)
5. According to fracture line and displacement: Linear (hair-line) fracture without deformities
(transverse, oblique and spiral) and displaced fracture with deformity of the limb (angulation,
rotation, apposition loss, overriding, impaction, distraction)
6. Multiple fracture
Healing process:
There are two types of fracture healing - primary and secondary.
Primary is a direct attempt by the cortex to re-establish itself thereby restoring mechanical
continuity.
Secondary healing can be categorized in three broad phases:
I. Inflammatory phase (hematoma and granulation tissue formation)
II. Reperative phase (fibrocartilaginous callus and bony callus fromation)
III. Remodelling phase
Fracture healing is affected by local and general factors
Local factors:
- blood supply to the fracture area
- type of bone involved and location of fracture within a particular bone
- interposition of soft tissue between fracture ends
- whether the fracture is open or closed and presence of infection within the fracture site
- gap between fracture ends
General factors:
- patient’s age
- patient’s nutritional status
- various metabolic factors
Clinical signs
- pain, swelling and tenderness
- loss of function (pain and loss of structural integrity of the limb cause loss of function)
- deformity - change in length, angulation, rotation and displacement
- attitude - the position of the fractured limb is sometimes diagnostic; the patient with a fractured
clavicle usually supports the limb and rotates his head to the affected side
- abnormal mobility and crepitus - these signs should not be sought deliberately because pain and
injury may result
Page 14 of 269
Treatment
- treatment of shock if present
- anesthesia (analgesia)
- reduction - closed (conservative) or open (surgical) with osteosynthesis
• the fracture must be restored to a normal anatomical position
• muscle spasm should be relieved with traction, analgesics, and muscle relaxants
• bones must be in apposition, properly aligned and in linear and rotatory directions, and set to
proper length
- immobilization
- physiotherapy and early rehabilitation
Abdominal trauma
- can be classified as blunt and penetrating
- penetrating trauma can be uncomplicated and complicated with damage of a hollow (peritonitis)
and/or parenchymatous (hemorrhage) organ
- the initial evaluation of a trauma patient (abdominal or other trauma) consists of rapid primary
survey aimed at identifying and treating immediately life-threatening problems - airways,
breathing, circulation, disability, exposure
- the primary goal in treatment is the identification and control of hemorrhage
- next step is the rapid examination to determine the presence and severity of neurologic injury
- level of consciousness measured by the Glasgow Coma scale score, pupillary response and
movement of extremities are evaluated and recorded
- based on motor responsiveness, verbal performance and eye opening to appropriate stimuli,
Glasgow Coma Scale was designed and should be used to assess the deoth and duration of
coma and impaired consciousness
Severe head injury - score 8 or less
Moderate head injury - score 9 to 12
Mild head injury - score 13 to 15
- the final step is to completely undress the patient and perform a rapid head-to-toe examination
to identify any injuries to the back, abdomen, perineum, or other areas not easily seen in the
supine, clothed position
Page 15 of 269
Management of a patient with an acute abdominal injury:
I. History
II. Examination
- inspection: abrasions, contusions, lacerations
- palpation: guarding, rebound tenderness
- percussion: tympanic (gastric dilatation), dull (haemoperitoneum)
- auscultation - loss of bowel sounds
- perineal examination - blood at urethral meatus, scrotal heamatoma, pelvic fracture
- exploration of the wound - to determine depth
- Nasogastric tube — reduces the risk of aspiration and decompresses stomach acids
- Urinary catheter — if urinary tract injury is suspected, only catheterise after performing
urethrography, cystography
- Evaluation of free intraperitoneal fluid — ultrasonography (US), computertomography (CT)
Indications for laparatomy
- penetrating injury traversing the peritoneal cavity or associated with hypotension
- blunt trauma with positive US or CT scan —> free intraperitoneal fluid
- blunt trauma with haemodynamic instability despite fluid resuscitation
- peritonitis
- x-ray —> free air or retroperitoneal air
Thoracic trauma
The most common life threatening chest injuries:
a) Tension pneumothorax
• airflow is unidirectional on inspiration but cannot escape during expiration due to a one-way
valve
• clinical features include: chest pain, air hunger, shock, neck vein distention, cyanosis,
deviated trachea (opposite side), reduced breath sounds
• x-ray: loss of lung markings of ipsilateral side is commonly seen
• immediate decompression by inserting a large bore needle into the second intercostal space
in the mid-clavicular line
• definitive treatment requires a chest drain
b) Open pneumothorax
• chest wall injury causes direct communication between pleural cavity and external
environment causing a pneumothorax
• immediate management inlcudes closing of the defect with sterile dressing that overlaps the
wound edges thus providing a flutter type valve effect followed by chest drain insertion
c) Flail chest
• segment of chest wall loses bony continuity with rest of the thoracic cage associated with
multiple rib fractures
• there are paradoxical movements of the chest
• management include analgesia, ventilation, intubation and chest drain
Page 16 of 269
d) Massive hemothorax
• loss of more than 1500ml of blood into the chest cavity or intercostal drain
• signs of massive hemothorax include absence of breath sounds and dullness to percussion
on the ipsilateral side and signs of hypovolemic shock
• management is resuscitation and operative hemostasis
e) Cardiac tamponade
• accumulation of pericardial fluid —> geart cannot fill —> pumping stops
• clinical signs are: venous pressure elevation, drop in the arterial pressure and muffled heart
sounds, low voltage ECG
• immediate pericardiocentesis is required
• all patients who have a positive pericardiocentesis (recovery of non-clotting blood) due to
trauma, require open thoracotomy
5. Local anesthesia
Local anesthesia
- Local anesthetics are a group of drugs which reversibly inhibit impulse generation in nerves and
other excitable membranes that utilize sodium channels as the primary means of AP generation
- Produce transient loss of sensory, motor and autonomic functions in a discrete portion of the
body
- Mode of action: local anesthetics bind to sodium channels, preventing membrane
depolarization —> block the propagation of the action potential
- Chemical structure: consist of a lipophilic group (usually a benzene ring), a hydrophilic group
(usually a tertiary amine), bound by an ester or amide linkage
- Potency: correlates with lipid solubility
- Onset of action: depends on the concentration of the local anesthetic and the pKa of the drug
- Duration of action: associated with protein binding, the tissue perfusion at the site of injection
and the type of linkage (ester or amide)
- Metabolism and excretion:
• ester local anesthetics are metabolized by pseudocholine esterase and excreted in the urine;
• amide local anesthetics are metabolized in the liver;
• very little drug is excreted unchanged by the kidneys
- Toxicity: rapid absorption of the anesthetic from the site of administration into the bloodstream
or unintentional intravascular injection raises the concentration of the drug in the blood over
safe limitis —> local anesthetics have their major toxic effects in the brain and myocardium
- Allergy: true hypersensitivity reactions to local anesthetics are quite uncommon (esters are
more likely to induce allergic reaction because they are a derivate of p-aminobenzoic acid (a
known allergen)
Drug classification
- commonly used LA can be classified as esters or amides (according to chemistry)
- they have an aromatic portion, an intermediate chain and an amine portion
- the aromatic portion determines lipophilic properties, the amine portion is hydrophilic
- esters are mostly hydrolyzes in plasma by pseudocholinesterase
- amides are destroyed mainly in the liver
a) Esters of benzoic acid
• cocaini hydrochlorium - pulv.
b) Esters of para-amino benzoic acid (PABA)
• Procaini hydrochlorium - amp. Chlorprocaine
• Benzocaine (Anaesthesium) - pulv.
Page 17 of 269
• Anaesthesol (Benzocaine + Procaine + Levomenthol)
• Tetracini hydrochlorium (Dicain)
• Proxymetacaine (Alcaine)
• Oxybuprocaine (novesine)
c)
Amides
• Lidocain - amp.
• Orofar - oromucosal spray 30ml
• Propipocaine (anaesthesie) spray
• Bupivacaine (Marcaine) - amp.
• Mepivacaine hydrochlorde (Mepivastesin) • Ultracain D-S (Articain + Epinephrine)
• Mesocain - gel
• Mesosept - spray
• Prilocaine
According to clinical use:
- can be applied by different ways: infiltration of the tissue (infiltration anesthesia), injection next
to the nerve branch (conduction anesthesia of the nerve, spinal anaesthesia of segmental
dorsal roots), or by application to the surface of skin or mucosa (surface anesthesia)
- LA are used mainly on mucous membranes in nose, mouth, tracheobronchial tree, and urethra
(topical anesthesia)
Local infiltration
- Lidocaine 0.5%-2% is often used but it is also effective in more dilute solutions
- the effect is prolonged if it is given in adrenaline solution, up to 1 in 200 000, which causes
vasoconstriction and also reduces bleeding
- no more than 3mg/kg body weight should be used, except when given with adrenaline, in
which case up to 7mg/kg body weight may be given
- Lidocaine anaesthesia lasts up to 90 min; may be extended by adding 0.5% lidocaine solution
Technique
- first, a bleb is raised in normal skin a short distance away (appr. 1 cm) —> the needle is
inserted and anaesthetic is gently injected as the tender area is approached
- initially the solution is infiltrated superficially to produce a wheal along the line of the proposed
incision
- if the exposure is deepened, infiltration is taken progressively deeper to create a field block
- the injection is given slowly to avoid pain caused by hydrostatic pressure
- each time the needle is in a new area, aspiration is performed to guard against intravenous
injection
- it is often advised to inject deeper progressively as the operation proceeds rather than attempt
a complete field block at the beginning
- the amount of anaesthetic agent used should be checked constantly to ensure the maximum
amount has not been exceeded
- patient should be asked to report pain or untoward symptoms and signs
- sufficient time (5min for lidocaine) should be allowed for the anaesthetic to act before starting
the operation
Regional anesthesia
- used when it is desirable that the patient remain conscious during the operation
- it is used most often for the surgery of the lower abdomen or the extremities
Adventages of regional anesthesia
- anesthesizing only the part of the body where surgery is being performed
- the patient remain conscious with preserved reflexes
- lung function is less affected
- suitable for one day surgery
- thromboembolic complications may be less
- low drug toxicity
- relatively inexpensive
Page 18 of 269
Spinal and epidural blocks
- spinal anesthesia is achieved by injecting a local anesthetic into the lumbar subarachnoid
space —> blocks the spinal nerve roots and doral root ganglia
- epidural anesthesia is accomplished by injecting a local anesthetic into the epidural space
- spinal and epidural anesthesia are widely used for surgery of the lower abdomen, perineum and
lower extremities
- spinal anesthesia offers better motor blockade, rapid onset of the block and is relatively easy to
perform
- complications associated with spinal and epidural anesthesia includes headache, severe
hypotension, urinary retention, meningitis, epidural hematoma and nerve injury
Peripheral nerve blocks
- the anesthetic is injected near a specific nerve or bundle of nerves to block sensations of pain
from a specific area of the body
- Nerve blocks usually last longer than local anesthesia
- They are most commonly used for surgery on the arms and hands, the legs and feet, or the
face
- Positioning of the needle during a nerve block may result in touching the nerve to be blocked
with the tip of the needle —> When this occurs, you may experience a sharp sensation like an
electrical shock in the part of the body supplied by the nerve (Be sure to let your
anesthesiologist know if you feel such a sensation)
6. Wounds — types. Surgical treatment. Primary and secondary suture.
Wound - Definition:
Wound is damage of the integrity of covering tissues (skin and mucous membranes) caused by
mechanical factors. The morphologic component, the functional disturbances and the healing
process determine the clinical chracateristics of every wound.
Classifaction of wounds by morphology:
1. Incised wound
2. Chopped wound
3. Contused wound
4. Lacerated (avulsed) wound
5. Lacerated-contused wound
6. Puncture (stab) wound
7. Bite wound
8. Gun-shot wound
9. Combined wound
- wounds can be penetrating and non-penetrating
- penetrating wounds: when there is a penetration into body cavities (cranial cavity, the peritoneal
cavity, the pleural cavity, the pericardium, the articular cavity)
- the penetrating wounds can be uncomplicated and complicated (when wounds penetrate into an
organ from the respective body cavity)
- wounds also divided according to the presence of bacterial contamination:
• clean wounds - bacterial contamination < 100 000 bacteria/gram tissue
• contaminated wounds - infection develops which can be:
- aerobic purulent - wound suppuration, sepsis and other infectious complications
- anaerobic, clostridial - tetanus, clostridial myonecrosis
Page 19 of 269
Clincal signs of wounds
1. General clinical signs
- not obligatory
- in some cases massive hemorrhage may lead to shock
- in cases of wound infection the body temperature and pulse rate are increased
- develop symptoms of toxicity - headache, nausea, vomiting, anorexia, etc.
- if there are complications, general symptoms may be result of the complication itself, e.g.
pneumothorax, hemothorax, peritonitis, hemoperitoneum, etc.
2. Local clinical signs
- two subgroups - specific and nonspecific
- specific - characteristic description of different types of wounds
- nonspecific - pain, hemorrhage, lymphorrhage, wound contamination, signs of inflammation
Diagnosis of wounds (through an assessment of the general condition of the patient and the local
status)
- cardiovascular system
- respiratory system
- CNS
- study of local clinical signs of the wound
- study of the limb for neural and/or vascular disturbances
- laboratory tests - Hb, RBC, WBC, etc.
- Instrumental investigations: X-rays of thoray, cranium; CT; US of the abdomen; vulnerography
The wound healing
- depends on many internal and extrernal factors (location, regional arterial blood supply,
presence of co-existing diseases like anemia, diabetes mellitus, hypoproteinemia,
hypovitaminosis, arterial occlusive diseases)
- reparations - replacement of highly differentiated tissues with connective tissue and scar
formation (e.g. parenchymatous organs and brain)
- regeneration - restoring pf specific tissue
- pathophysiologic reactions of organism to trauma include four main phases (overlapping)
I. Inflammation - 1hr to 3 days
II. Granulation - 1 day to 1 (2) weeks
III. Epithelialization - 1 day to 1 week
IV. Firboplasia - 3 day to 1 month
Inflammation phase
• three main processes: necrosis, hemostasis, inflammation
• necrosis of wound egdes and surrounding tissue due to traumatic factor (directly) and disturbed
blood circulation (indirectly)
• hemostasis preceds and initiates inflammation with the ensuing release of chemotactic factors
from the wound site
• inflammation starts as an aseptic process - vasodilation, neutrophils, monocytes and plasma
proteins enter the wound to destroy bacteria, foreign bodies and necrotic tissue
Page 20 of 269
• Monocytes differentiate into macrophages - consume tissue and bacterial debris, are crucial in
process of tissue repair by secreting multiple peptide growth factors with subsequent activation of
fibroblasts, endothelial and epithelial cells
Proliferative phase
• mainly fibroblast activty with the production of collagen and ground substance
(glycosaminoglycans and proteoglycans), growth of new blood vessels as capillary loops and the
re-epithelialization of the wound surface
• fibroblasts require Vit C to produce collagen
• wound tissue formed in the early part of this phase is called granulation tissue
• in latter part, there is an increase in the tensile strength of wound due to increased collagen
(type III)
• epithelialization of wound stops the risk of further contamination and moisture loss
Remodelling phase
• maturation of collagen (type I replacing type III until 4:1 ratio is achieved)
• decreased wound vascularity and wound contraction due to fibroblast and myofibroblast activity
• final outcome of wound healing is white scar formation
Healing by first (primary) intention
• usually in all wounds which are not contaminated, withouth necrosis and anatomical location and
size allow the skin continuity to be restored
• process lasts 6-8 days
• wound is surgically closed by reconstruction of the skin continuity
Healing by second intention
• after wound debrisement and preparation, the wound is left open to achieve sufficient granulation
for spontaneous closure
• caused by infection, excessive trauma, tissue loss, imprecise approximation of tissue and
bacterial contamination
Healing by third intention
• in case of large and deep wound with forming of hollow scars under the skin levels
Treatment of wounds
- The goals of treatment are:
• preventing infection
• acceleration of wound healing
• forming of thin, tiny and regular shaped scar
- treatment of wounds begins with giving first aid
- the main goals are to stop bleeding, to immobilize the patient for patient’s transportation and to
dress the wound, to give the patient tetanus toxoid, human tetanus immune globulin and gas
gangrene antiserum
Page 21 of 269
Surgical operation is performed in the following sequence:
- shaving of the hair widely around the wound
- immediate wound toilet of the skin around the wound with antiseptics (e.g. 20% Hibitan,
Hibiscrub, Decidin, Braunol, Decosept, etc.)
- in case of large injury and massive contamination, pour on plenty of clean water when you toilet
a wound
- local infiltration anaesthesia or general aneaesthesia
- use a scalpel to cut away 0.5 - 1cm of skin margins in healthy tissue
-
remove all necrotic tissue, hematoma and foreign bodies
preserve unaffected blood vessels and nerve trunks
reconstruction of vessels, tendons and nerves are made by specialists in short time
pass a ligature for the bleeding vessels
make a wound toilet with 3% H2O2 several times
Depending on the type of wound, there are different types of wound closure techniques:
- Immediate primary suture —> it is used immediately after wound toilet for fresh and noncontaminated wounds
- Delayed primary suture —> if there is opportunity for development of infection, but at the
moment of admission, there are no signs of infection
• put interrupted monofilament sutures without knot tying them
• if there are no signs of infection and fresh granulation is fromed 3-5 days later, knot the
sutures
- Temporary suture —> if the wound is large and contaminated and there is necessity of a
secondary toilet and sutures, put temporary sutures at the key points, at a larger distance from
one another
- Early secondary suture (2 weeks after injury) —> if granulation tissue is grown, there are no
signs of infection and the edges are soft, put a few interrupted sutures
- Late secondary suture (20-28 days after injury) —> when the infection is overcome, make
secondary wound toilet, excise the granulation, mobilize the wound edges and bring them
together with sutures
Types of wounds
Vulnus scissum
- incised wound
- caused by sharp-edged objects like a knife, scalpel, parts of glass etc.
- wounds have smooth edges and walls, acute angles, clean bottom, abundant bleeding from cut
vessels and marked tenderness
- there are usually no conditions for developing infection -> heal by primary intention
- example: surgical wound
Page 22 of 269
Vulnus contusum
- contused wound
- caused by blow with heavy, solid object
- irregular shape and rough edges
- there is a zone of edge’s necrosis and zone of local stupor aroun the edges
- edges are with light blue color, cold and insensitive due to refley spasm and thrombosis of blood
vessels and damage of the nerves
- edges and walls are undermined
- crushed tissues in the bottom of the wound
- hemorrhages in the form of ecchymosis and suffisions around the wound
- most severe contused wounds are caused when vehicle run over the body, or during
compression from heavy objects (crushed wounds)
- good condition to develop infection due to massive tissue necrosis, presence of blot clots and
opportunity of development of secondary necrosis
Vulnus laceratum
- lacerated wound (zerfetzt, zerfleischt)
- edges are rough, with light bleeding and zone of edge’s necrosis
- bleeding is more abundant than bleeding caused by contused wounds
Vulnus lacerocontusum
- lacerated-contused wound
- wound has signs of the two others
- traumatic factor causes compression and traction, which leads to massive damage of tissues
- example: detachement of the epicranial epineurosis (scalp) or detachment of the whole limb
(arrachement), which usually leads to hemorrhagic shock
- good conditions to develope infection
Vulnus conquassatum
- crushing wound
- injury caused by an object that causes compression of the body
- often following a natural disaster or after some form of trauma from a deliberate attack
- common concerns after an injury of this type are rhabdomyolysis (condition in which damaged
skeletal striated muscle breaks down rapidly) and crush syndrome (medical condition
characterized by major shock and renal failure)
Vulnus caesum
- chopped wound
- caused by heavy sharp-edged object, e.g. axes, hatches, swords, sable, etc.
- signs of incised and contused wounds
- signs of sabred wound are regular shape, minimal zone of local stupor, the bleeding usually is
light (in some cases abundant)
- danger of developing an infection
Page 23 of 269
Vulnus punctum
- puncture wound
- caused by an injury with knife or dagger
- similar to incised wound (smooth edges, shape - imprint of the transverse section of the sharp
object, usually abundant bleeding from cut blood vessels)
- if wound caused by injury with stake or similar objects, the wound is similar to stab-contusedlacerated wound, usually with light bleeding due to crushed vessels and their thrombosis
- opportunity for infection development is good due to lack of oxygen access in wound and
presence of foreign objects in it
Vulnus morsum
- bite wound
- bites from insects (e insectibus), animals (e animalibus), snakes and other reptiles (serpentibus)
- insect bite: dot shaped, sting in the center of wound, toxic insect’s products are introduced
causing redness and swelling, allergic reaction could be developed (especially in face and eye
lid region)
- tick bites could cause Lyme disease
- snake bites: two dots on the skin with purple colour, clinical signs are headache and vomiting,
the heart rate is accelerated, soft and shock develops; paralysis of breath and cardiac arrest
later developed due to neuro-toxicity of the poison
- mammal bites: infected lacerated-contused wounds, development of specific infections like
rabies, tetanus, glanders, etc. possible
Vulnus sclopetarium
- gun-shot wound
- big group of wounds with different pathomorphological characteristics
- bullet wounds are similar to stab wounds
- blast and missile’s wounds are similar to lacerated-contused wounds
- morphology structure of wound has three zones:
• zone of destruction -> the wound channel
• zone of immediately traumatic necrosis -> layer of necrotic tissues, which surround the wound
channel
• zone of molecular concussion (local stupor) -> layer of this zone, near the wound channel will
undergo secondary necrosis, the other part will repair
Wound management according to the WHO
Surgical wounds can be classified as follows:
- Clean
- Clean contaminated: a wound involving normal but colonized tissue
- Contaminated: a wound containing foreign or infected material
- Infected: a wound with pus present
- Close clean wounds immediately to allow healing by primary intention
- Do not close contaminated and infected wounds, but leave them open to
- heal by secondary intention
Page 24 of 269
- In treating clean contaminated wounds and clean wounds that are more than six hours old,
manage with surgical toilet, leave open and then close 48 hours later (This is delayed primary
closure)
Factors that affect wound healing and the potential for infection
• Patient:
- Age
- Underlying illnesses or disease: consider anemia, diabetes or immunocompromised
- Effect of the injury on healing (e.g. devascularization)
• Wound:
- Organ or tissue injured
- Extent of injury
- Nature of injury (for example, a laceration will be a less complicated wound than a crush injury)
- Contamination or infection
- Time between injury and treatment (sooner is better)
• Local factors:
- Haemostasis and debridement
- Timing of closure
Wound: Primary repair
- Primary closure requires that clean tissue is approximated without tension.
- Injudicious closure of a contaminated wound will promote infection and delay healing.
- Essential suturing techniques include:
• Interrupted simple
• Continuous simple
• Vertical mattress
• Horizontal mattress
• Intradermal
• Staples are an expensive, but rapid, alternative to sutures for skin closure
- The aim with all techniques is to approximate the wound edges without gaps or tension
- The size of the suture “bite” and the interval between bites should be equal in length and
proportional to the thickness of tissue being approximated
- As suture is a foreign body, use the minimal size and amount of suture material required to close
the wound
- Leave skin sutures in place for 5 days; leave the sutures in longer if healing is expected to be
slow due to the blood supply of a particular location or the patient’s condition
- If appearance is important and suture marks unacceptable, as in the face, remove sutures as
early as 3 days — In this case, re-enforce the wound withskin tapes
- Close deep wounds in layers, using absorbable sutures for the deep layers
- Place a latex drain in deep oozing wounds to prevent haematoma formation
Page 25 of 269
Wound: Delayed primary closure
- Irrigate clean contaminated wounds; then pack them open with damp saline gauze
- Close the wounds with sutures at 2 days
- These sutures can be placed at the time of wound irrigationor at the time of wound closure
Wound: Secondary healing
To promote healing by secondary intention, perform wound toilet and surgical debridement.
1. Surgical wound toilet involves:
- Cleaning the skin with antiseptics
- Irrigation of wounds with saline
- Surgical debridement of all dead tissue and foreign matter (Dead tissue does not bleed when cut)
2. Wound debridement involves:
- Gentle handling of tissues minimizes bleeding
- Control residual bleeding with compression, ligation or cautery
- Dead or devitalized muscle is dark in color, soft, easily damaged and does not contract when
pinched
- During debridement, excise only a very thin margin of skin from the wound edge
- Systematically perform wound toilet and surgical debridement, initially to the superficial layers of
-
tissues and subsequently to the deeper layers
After scrubbing the skin with soap and irrigating the wound with saline, prep the skin with
antiseptic
Do not use antiseptics within the wound
Debride the wound meticulously to remove any loose foreign material such as dirt, grass, wood,
glass or clothing
With a scalpel or dissecting scissors, remove all adherent foreign material along with a thin
margin of underlying tissue and then irrigate the wound again
Continue the cycle of surgical debridement and saline irrigation until the wound is completely
clean
Leave the wound open after debridement to allow healing by secondary intention
Pack it lightly with damp saline gauze and cover the packed wound with a dry dressing
Change the packing and dressing daily or more often if the outer dressing becomes damp with
blood or other body fluids
Large defects will require closure with flaps or skin grafts but may be initially managed with
saline packing
Page 26 of 269
7. Thermal injuries. Burns. Treatment. Chemical and radiation burns
Thermal trauma
• different kind of injuries to the body under action of high and low temperature
• classification of thermal trauma due to temperature:
• high temperature:
- Heat stroke (hyperthermia): surrounding temperature is very high and damages normal
thermoregulating process; clinical symptoms: headaches, elevated body temperature,
pulsating sound in ears, vomiting, dizziness
- Sun exposure (insolatio): excessive exposure to sunlight, clinical symptoms: dizziness,
loss of memory, tachycardia, tachypnea, death and coma may take place if not treated
immediately
- Obredanne syndrome: hyperthermia in operated patients, mainly in newborns and
pediatric age, in early hours after operation, sudden and fast increase in temperature,
reaches up to 41-42°C; Treatment includes: cooling methods, medication, intravenous
infusions, electrolyte solutions
- Burns: Tissue injury from flames, burning fumes and gases, hot fluids, hard objects and
voltage supply
• low temperature:
- general cooling - hypothermia
- freezing - cogelatio
Burns
• measured as a percentage of the total body area (affected rule of „nines“)
- Head and neck - 9%
- Upper extremity - 9%
- Anterior torso (thorax and abdomen) - 2 x 9% = 18%
- Back and lumbar region - 2 x 9% =18%
- Lower extremity with gluteal region - 2 x 9% = 18%
- Anus and perineum - 1%
• only second and third degree burn areas are added together to measure total body burn area
• While first degree burns are painful, the skin integrity is intact and it is able to do its job with fluid
and temperature maintenance
• If more than 15%-20% of the body is involved in a burn, significant fluid may be lost
—> shock may occur if inadequate fluid is not provided intravenously
• As the percentage of burn surface area increases, the risk of death increases as well:
• Patients with burns involving less than 20% of their body should do well
• those with burns involving greater than 50% have a significant mortality risk
• burn location is important: if burn involves face, nose, mouth or neck there is a risk that there will
be enough inflammation and swelling to obstruct the airway and cause breathing problems
Page 27 of 269
Burn classification
Based on the depth of injury to dermis and underlying structures:
- first-degree burn (superficial):
• redness (hyperemia) and edema of skin
• symptoms disappear once the skin cells are shed
• usually heal within three to six days
• mostly treated with home care (soak wound in cool water for five minutes or longer, take
pain relief, apply aloe vera or cream to soothe the skin, use an antibiotic ointment)
• don’t use ice, can make damage worse
• never apply cotton balls, can increase risk of infection
- second-degree (partial thickness):
• bullosa and blisters are seen on skin surface
• some blisters pop open, causing a wet appearance
• frequent bandaging to prevent infection
• some take longer than 3 weeks to heal, most heal within 2-3 weeks
• emergency treatment if burns affect face, hands, buttocks, groin, feet
- third A degree: distribution of necrosis on whole epidermis and part of dermis
- third B degree: total necrosis of all the skin in burned region
- fourth-degree: involves underlying subcutaneous tissue
Degree of burns
Depth of tissue damage
Symptoms
Healing process
1st degree
• Healing within 3–6
• Superficial layers of the • Pain
(superficial burn)
epidermis
days without scarring
• Erythema
• Swelling
• The burn wound
blanches on
applying
pressure and
refills rapidly
2n
2a
(superficial
de partialgr thickness
ee burn)
d
2b (deep
partialthickness
burn)
• Epidermis and upper
layers of the dermis;
dermal appendages
(hair follicles, sweat,
and sebaceous glands)
are spared
•
•
•
•
Pain
• Healing within 1–3
Erythema
weeks with
Vesicles/bullae
hypopigmentation/
The burn wound
hyperpigmentation
blanches on
but without scarring
applying
pressure and
refills slowly.
• Deeper layers of the
dermis
• Minimal pain
• Healing takes 3
weeks or longer and
• Mottled skin
with red and/or
results in scar
white patches
formation
• Vesicles/bullae
• The burn wound
does not
blanch on
applying
pressure.
Page 28 of 269
3rd degree (full
thickness burn)
• Epidermis, dermis, and
subcutaneous tissue
• No pain
• The burn does not
heal by itself
• Tissue necrosis
with black,
white, or gray
leather-like skin
(eschar)
• No vesicles/
bullae
• The burn wound
does not
blanch on
applying
pressure
4th degree
• Deeper structures
(muscles, fat, fascia,
and bones
• Charred tissue
• The tissue is dead
and requires
amputation
Phases of burn injuries:
• 1st phase: Phase of thermal shock - from start to 72 hours; plasmorrhea in region of burns and
outside them which leads to sudden decreased plasma volume, hemoconcentration and
oligoanuria
• 2nd phase: Phase of toxicoinfection - betw. 3-15th days, temperature period starts with septic
temperatures and inflammatory degenartive changes of body organs
• 3rd phase: Phase of healing - 15-28th day, imporved general condition, normal temperature,
decreased inflammatory process, necrotic skin is changed with fresh granulated tissue,
epithelialization of wound edges
• 4th phase: Phase of early cachexia - after 28th day, only in 3rd and 4th degree burns
• 5th phase: Phase of complications from burns - functional dysfunction of body organs, progress
of contractions, keloids and other morphological changes are complications of burns
- airway injury must be suspected with facial burns, singed nasal hairs, carbonaceous sputum and
tachypnea
- progressive hoarseness is a sign of impending airway obstruction
Clinical features
- Clinical features of shock (e.g., hypotension, poor urine output)
- Clinical features of ARDS (e.g., dyspnea)
- Inhalation injury should be suspected when any of the following are present:
• History of being trapped in a confined space
• Facial burns, singed eyebrows and/or nose hair, evidence of soot on the face or in the
airway
• Stridor, dysphonia
• Extensive burns
- In case of circumferential burns around limbs → compartment syndrome: clinical features of
acute limb ischemia (e.g., weak/absent pulse, paresthesia, pallor in the affected limb)
- In case of circumferential burns around abdomen → abdominal compartment syndrome:
impaired function of nearly every organ system (e.g., oliguria, acute pulmonary
decompensation, hypoperfusion) and signs of increased intraabdominal pressure (jugular
venous distension, hypotension, tachycardia)
Page 29 of 269
Treatment of Burns
Managing of a burned patient
• airway control
• breathing and ventilation
• circulation
• disability- neurological status
• exposure with environmental control
• fluid resuscitation
Treatment of burns is specific for each phase of the disease and is local and general
Local treatment:
• includes cleaning by physiological serum
• small damaged tissue is cleaned with forceps
• any fluid must be aspirated
• depends on type of wound, wether the dressing should be done or to be left exposed
• to remove or leave blisters is controversal
• washing burn wound with chlorhexidine solution is ideal
• for initial management of minor burns that are superficial or partial thickness, dressings with a
non-adherent material are often sufficient
• antiinflammatory and adequate pain relief must be provided
• plastic surgical method of treatment
Management based on degree
1st and 2nd-degree burns
- Irrigation
- Topical moisturizers (e.g., calamine lotion) or aloe vera-based gels: relieve symptoms of 1stdegree burns
- Consider antiseptic ointments (e.g., silver sulfadiazine, mafenide) or topical antibiotics
(bacitractin; triple antiobitic ointments are a combination of bactracin neomycin, polymyxin B)
- For periorbital or periocular burns, topical antibiotics (e.g., bacitracin, neomycin, or
erythromycin) are preferred over silver sulfadiazine, which may be irritating and cause ocular
toxicity
- Deroofing bullae/vesicles
- Dressing is indicated in partial thickness (2nd-degree) burns.
3rd and 4th-degree burns
- Early debridement of burnt, necrotic tissue
- Method of tissue coverage varies depending on the specific burn characteristics; Options
include:
• Free skin grafts (split-thickness or full-thickness)
• Flap reconstruction with free or pedicled flaps
- Topical antibiotics (e.g., silver sulfadiazine, bacitracin, neomycin)
Page 30 of 269
General treatment:
• includes intravenous infusion, analgesics, hemotransfusion, antibiotics and symptomatic
treatment
• intravenous infusion
- if more than 15-20% of the body involved in a burn, significant fluid may be lost
-> shock may occur if inadequate fluid
- the „Parkland formula“ estimates the amount of fluid required in the first few hours of care
following a burn: fluids for 24 hours = (4 x kg x % of burn) -> the first 50% given in the first
8 hours and the second 50% over the following 16 hours
- example: patient with 80kg with 25% burn -> 4 x 80kg x 25 = 8000ml fluid in first 24 hours
Electrical trauma (electrocution) divided into:
- atmospheric electricity (fluminatio)
- electrical current: (a) general damage - electrocutio (b) local burn - electrocombustio
Four stages in electrical trauma:
I. muscle spasm without loss of consciousness
II. muscle spasm with loss of consciousness
III. loss of memory and severe respiratory and hemodynamic damage
IV. clinical death
- complications occur in up to 30% of patients with high-voltage injury
- CNS effects such as cortical encephalopathy, hemiplegia, and brainstem dysfunction have been
reported up to 9 months atfer injury
- others report delayed peripheral nerve lesions characterized by demyelination with vacuolization
and reactive gliosis
Chemical burns
- caused by acids or bases
- common products causing chemical burns are: car battery acid, bleach, ammonia, denture
cleaners, teeth whitening products, pool chlorination products,…
- groups at highest risk are infants, older adults and people with disabilities —> may not be able
to handle chemicals properly
- most acids produce a coagulative necrosis by denaturing proteins, forming a coagulum
(e.g. eschar) that limits the penetration of the acid
- bases typically produce more severe injury - liquefactive necrosis
-> involves denaturing of proteins as well as saponification of fats, doesn’t limit tissue penetration
- severity of burn related to a number of factors, including the causing agent, concentration, length
of contact, physical form of agent, area/location of contact (swallowed, inhaled, open wounds or
intact skin)
- classification according to the exten of the injury and the depth of the burn itself:
• first degree burn: injury to the epidermis (superficial burn)
• second degree burn: injury to the dermis (partial thickness injury or dermal injury)
• third degree burn: injury to the subcutaneous tissue (full thickness injury)
Page 31 of 269
- common symptoms:
• blackened or dead skin, which is mainly seen in chemical burns from acid
• irritation, redness, or burning in the affected area
• numbness or pain in the affected area
• loss of vision or changes in vision if chemicals have come in contact with eyes
- longterm effect of caustic dermal burns is scarring
- esophagal and gastric burns can lead to stricture formation
Emergency departement care
- complete removal of offending agent (decontamination) — rinsing under running water for 10-20
min (first aid, even before seeking medical care; if chemical came in contact with eyes, rinse
eyes immediately for at least 20min)
- using litmus paper to measure the pH of the affected area or the irrigating solution is useful
- medication have a limited role in most chemical burns
- topical antibiotic therapy is recommended for dermal and occular burns
- pain medication is important
Radiation burns
- = damage to the skin or other biological tissue as an effect of radiation
- most common type of radiation burn is caused by exposure to UV light (e.g. sun)
- can also be caused by radiation therapy, exposure to high frequency microwaves or radio
waves, and exposure to nuclear energy
- Gamma rays can cause deep tissue gamma burns, while beta particles cause shallower beta
burns, which usually only harm the skin’s surface
- the extent of the damage is often based on the intensity of the radiation, and the amount of time
that the body is exposed to it
Specific types of radiation burns
Radiation Dermatitis
- = radiation burns caused by radiation treatment for cancer
- can be acute and chronic
- acute radiodermatitis occurs shortly following radiation therapy and may cause redness of the
skin and blistering
- chronic radiodermatitis is often dormant for a long period of time, after which carcinomas and
skin reactions develop
Fallout burns
- = radiation burns that are a result of nuclear bomb blasts
- lethal to those within a certain radius of the blast, usually a few miles (body tissues and clothing
are incinerated within milliseconds) — those farther away may experience charring of the skin
and severe internal burns
- radiation from these bombs can affect a wide area, and may cause cancers and deformities in
people that otherwise show no sign of radiation burns
- beta burns are frequently the result of exposure to radioactive fallout
- radiation from bombs has also been known to cause brain death, where the patient drops dead
days later without warning
- Sepsis and radiation sickness can also develop without warning
Page 32 of 269
Treatment
- radiation burns on the skin should be kept moisturized, clean and covered
- bathing should be done in warm water, and skin shuld be carefully patted dry, to avoid tears and
injuries
- sunlight should be avoided and patients should wear loose fitting clothing or bandages over the
affected area
8. Frostbite. Classification by degrees. Treatment
Definition:
A frostbite is a severe localized tissue injury due to freezing of interstitial and cellular spaces after
prolonged exposure to very cold temperatures.
Pathophysiology:
- Damage occurs via direct cold-induced cell death as well as delayed inflammation from
reperfusion injury
- Starts with vasoconstriction which later turns into vasodilation
- Electrolyte flux can also occur if intracellular ice crystals form
Classification:
I. First degree:
- Numbness, erythema, edema
- Possible development of white or pale plaques
- No blistering or tissue infarction
II. Second degree:
- Erythema, edema
- Development of clear or pale colored superficial blisters
III. Third degree:
- Tissue freezing with death of subcutaneous tissues and skin resulting in hemorrhagic
vesicles
- The area has a deep numb feeling followed later by burning and throbbing pain
IV. Fourth degree:
- Tissue necrosis, gangrene and eventual full-thickness tissue loss
- The affected area initially appears hard, cold, white and is anesthetic
Clinical features:
- Acute frostbite can occur in isolation or as a complication of hypothermia
- Hypothermia = core body temperature under 35°C
- Areas most frequently affected: face (nose, cheeks, chin), ears, fingers, and toes
- It can vary from the superficial involving, only skin and subcutaneous adipose tissue, to deeper
damage involving muscles, ligaments, and joint
- Cold and paresthesia of affected region
- Pale (white or greyish-yellow), blue-red, or blistered hard or waxy skin
Diagnostics:
- Clinical diagnosis
- CT, MRI/MRA, bone scan to determine extent of nonviable tissue
Treatment
- Remove wet clothing; avoid walking on frostbitten feet
- Evaluate for concurrent hypothermia and treat that first
• It is imperative that rewarming begins at the trunk
• Immediate warming of the periphery results in peripheral vasodilation, causing cold acidemic
blood to return to the trunk, which can lead to life-threatening arrhythmias!
Page 33 of 269
- Rewarming
• Passive: remove wet clothing, cover with blankets, warm room (preferably 28°C)
• Active: immerse affected extremity in a warm (preferably 37-39°C (in the book 40-42°C for
20-30min) ) circulating water bath
- Analgesia and tetanus prophylaxis
- Manage suspected infections aggressively with antibiotics and sterile dressings otherwise leave
the wound site open to air
! Patients are often affected with both hypothermia and frostbite. Treatment of hypothermia should
take priority because it can be acutely life-threatening!
9. Bleeding. Types. Non-surgical hemostasis. Hemostatic agents
Bleeding - Definition
Hemorrhage (bleeding) is an escape of blood through:
- ruptured vessel wall
- unruptured vessel wall
Examples
1) ruptured vessel walls - any kind of trauma
2) unrupted vessel walls
a) erosion of vessel wall
- tumors
- foreign bodies, causing compression
- acids (peptic ulcer), enzymes, etc.
b) diapedesis (passage of blood through intact vessel walls)
- vasopathy
- thrombocytopathy
- coagulopathy
Classification:
I. Etiology of surgical hemorrhage
- rupture (vessel injury)
- erosion
II. Type of vessels
- arterial hemorrhage
- venous hemorrhage
- capillary hemorrhage
- parenchymatous hemorrhage
III. Period of time
- primary hemorrhage
- secondary hemorrhage - early (within 48 hours), late (after 48 hours)
IV. Place where blood passes
- external hemorrhage
- internal hemorrhage - obvious or not
V. Postoperative hemorrhage
- technical „mistakes“
- progressive development of the disease
Page 34 of 269
The clinical symptoms can be general, which are nonspecific symptoms (rapid pulse, fall of blood
pressure, anemia) and local symptoms, which are specifc.
Types of bleeding:
- Class I Hemorrhage: involves up to 15% of blood volume, typically no change in vital signs, fluid
resuscitation usually not necessary
- Class II Hemorrhage: 15-30%, patient often tachycardic, narrowing betw. systolic and diastolic
blood pressure, body tries to compensate with peripheral vasoconstriction, skin may look pale
and be cool, volume resuscitation with crystaloids
- Class III Hemorrhage: 30-40%, blood pressure drops, heart rate increases, peripheral perfusion,
capillary refill and mental status worsens,fluid resuscitation with crystaloids and blood
transfusion usually necessary
- Class IV Hemorrhage: > 40% loss of circulating blood volume; the limit of the body’s
compensation are reached and aggressive resuscitation is required to prevent death
- Cerebral hemorrhage
-
-
• sudden, severe headache in hemorrhagic stroke, especially indicative when accompanied by
stiff neck, facial pain, pain between eyes, vomiting, unequal pupils etc.
• intracerebral hemorrhages may be caused by burst aneurysms or arteriovenous malformation,
but most often by hypertension
Hemopericardium = effusion of blood in the pericardial activity
• caused by rupture of atrium, perforation of ventricle or rupture of coronary artery
• manifests by heart tamponade and very sudden death
Hemothorax = collection of blood in the pleural cavity
• can cause collapse of lung and dyspnea, absence of breath sounds and pallor of mucosae
Hemoptoe = expectoration of blood or of blood-streaked sputum from the larynx, trachea,
bronchi or lungs (caused by e.g. carcinoma, tuberculosis and other infectious diseases)
Hemoperitoneum = blood in peritoneal cavitiy (most common causes: traumatic injuries, antraabdominal tumors, aortic dissection, coagulopathies, peritoneal carcinomatosis, etc.)
Hematuria = presence of blood in urine(e.g. sign for hypernephroma, renal tuberculosis,
trauma)
Hemarthrosis = bleeding into joint spaces
Upper GI hemorrhage
• Hematemesis: vomiting of frank bright red blood or coffee-rgound material positive for occult
blood
• Melena: passage of black, tarry stools containing digestes blood
• most common causes: peptic ulcer, gastroesophageal varices, arteriovenous malformationsn
Mallory-Weiss tears, erosive gastritis, neoplasms (benign and malignant)
• in case of major bleeding:
- aggressive replacement of volume with intravenous solutions, blood products, oxygen
therapy, continuously monitoring vital signs
- early endoscopy recommended (diagnostic and therapeutic) - injection of adrenaline or
other sclerotherapy, electrocautery, endoscopic clipping or banding or varices
- hemostatic drugs
- surgical artifical hemostasis (temporary or definitive)
Resuscitation is the key to initial treatment of hemorrhage. Should begin with intra-venous fluids.
Page 35 of 269
Hemostasis - process which stops bleeding
- sponatneous
- artificial (surgical and non surgical)
Spontaneous hemostisis
„A complex, interdependent set of events resulting in the formation of a stable clot. Hemostatic
mechanisms can stop bleeding from small vessel, i.e. arterioles, venules and capillaries.
Hemorrhage caused by injury from veins and arteries cannot be stopped spontaneously. There are
three phases of spontaneous hemostasis - vascular, platelet and coagulation phase.“
Vascular phase
1. Endothelium:
- inverts inside (towards the lumen)
- subendothelial collagen is exposed
2. Smooth muscle fivers fall into a state of vasoconstriction
Mechanisms of vasoconstriction:
- nervous reflexes (sympathetic NS) elicited by pain in the injured tissue
- local myogenic contraction of the blood vascular smooth muscle initiated by direct damage to
the vascular wall
- vasoconstrictors (local humoral factors from traumatized tissues) such as serotonin,
thromboxane A2 (from platelets that adhere to the walls of damaged vessels)
3. Adventitia - envelops the vessel
- this response will last up to 30 min and is localized to damaged area
Platelet phase
1. Platelet adhesion
- platelets attach to the exposed subendothelium collagen
- damaged endothelial cells lining the blood vessel release von Willebrand’s factor. This
substance makes the surface of the endothelial cells ‚sticky‘ = platelet adhesion
- attached platelets are activated and release substances from cytoplasmic granules
-> platelet factor
2. Platelet aggregation - a platelet plug is formed
- adhered platelets now begin to secrete Adenosin diphosphate, which is released from stuck
platelets -> causes the aggregation of nearby free platelets which attach to the fixed platelets
and each other
- aggregation leads to formation of platelet plug
- the plug closes the minute ruptures in very small blood vessels that occur hundreds of times
daily
- platelet plug doesn’t occlude vessel itself, only the wall in its wall
Coagulation phase (plasma stage)
Page 36 of 269
-
begins 30 sec to several minutes after phase I and II have commenced
1st phase - begins with forming of thrombokinase
2nd phase - thrombokinase induces conversion of prothrombin to thrombin
3rd phase - thrombin induces the forming of unstable fibrin from fibrinogen, which later becomes
in its stable form
4th phase - fibrinolyis - part of formed fibrin is degraded to fibrin degradation products and the
blood vessels recover its permeability - vessel recanalizes
the process of fibrinolysis is running parallel with the forming of blood clot, when bleeding has
stopped
fibrinolysis is mediated by the fibrin splittin protease (plasmin)
plasmin is formed from a precursoer, plasminogen, by plasminogen activators called t-PA and
urokinase-type plasminogen activator (u-PA)
there are 13 coagulation factors, most of them coming from the liver
• Different substances that enhance the three phases of spontaneous hemostasis for local, enteral
and parenteral administration (non surgical artificial hemostasis)
- vasoprotective (angioprotective) substances - Vit. C, rutascorbin, stiptanon, etc.
- vasocontrictors - adrenalin, noradrenalin, ergotamin, etc.
- anti-thrombocytolytics - urbason
- coagulants - Ca++, fibrinogen, antihemophilic globulin, NaCl, Surgigel
- antifirbinolytics - PAMBA, Aminocaproic acid, tranexamic acid, etc.
• the basic disturbances of haemostasis are haemorrhage, thromboembolism, microcirculation
disturbances and disseminated intravascular coagulation (DIC syndrome)
• disturbances are divided into two groups:
- hemorrhagic diathesis -> disorders characterized by permanent tendencies to
hemorrhages (vasopathies, thrombocytopathies, coagulopathies (hemophylia))
- thrombotic diathesis - disorders of hemostasis characterized by permanent tendencies to
vascular thrombose
10. Methods for temporary and final hemostasis.
Temporary hemostasis
- There are methods of surgical artificial temporary hemostasis, which are used as emergency
measures in any situation (not in a hospital)
- their aim is to stop bleeding and prevent life threatening blood loss
- It is used as long as the bleeding stops or definitive surgical hemostasis is performed
Methods:
• Lifting a limb (hydrostatic pressure decreases)
• Digital compression - in loco laesionis (in region of lesion)/ in loco selectonis (selected region)
(ILS)
• Compressive bandage - in loco laesionis (ILL)
• Tamponade - ILL
• Esmarch’s method - ILS
Page 37 of 269
- in its modern form it is a narrow hard rubber tourniquet with a chain fastener that is used to
control bleeding by applying it arround a limb
- prevents the blood to flow from or to a distal area
- should not be used longer than 60 min in upper limb and 90 min in lower limb
• Maximal flexure (bending) of a limb - Adelmann’s method
• Pressing the abdominal aorta - Momburg’s method
- a rubber tube, two meters in length and about 1 cm in diameter, is wound around th body
just below the costal arch
- the femoral pulse should be tested at each turn of a belt, and just as this pulse disappears
the ends of the tube are tied and held securely by means of a clamp
Final / Definitive hemostasis
- Surgical artifical hemostasis can be definitive
- It needs a specialist and special (surgical) equipment
- Often methods for definitive surgical hemostasis are combined with nonsurgical methods
Definitive surgical hemostasis - methods
1. Mechanical:
• tripsion (crushing) of the vessel
• torsion (rotating around the axis) of the vessel
• ligation of the vessel in loco laesionis and in loco selectionis
• vascular suture
• endoscopic hemoclips
2. Thermal
• high temperature - cautery effects hemostasis by denaturation of proteins, which results in
coagulation of large areas of tissues (electrocautery, LASER)
• low temperature - cooling also has been applied to control bleeding and acts by increasing the
local intravascular hematocrit and decreasing the blood flow by vasoconstriction. Cryogenic
surgery uses temperatures between -20 and -180°C
3. Chemical and biological methods
• some chemicals act as vasoconstrictors, others are procoagulants, and others have
hygroscopic properties that aid in plugging disrupted blood vessels
• local hemostatic materials include gelantin foam, cellulose and micronized collagen
• topical sealants and adhesives - fibrin sealants and synthetic glues
Page 38 of 269
11.) Blood transfusion. Blood groups. Complications
The ABO system
- The major blood groups of this system are A, B, AB, and O
- O type RBCs lack A or B antigens.
- The genes that determine the A and B phenotypes are found on chromosome 9p
- The gene products are glycosyl transferases, which confer the enzymatic capability of attaching
the specific antigenic carbohydrate
- H substance is the immediate precursor on which the A and B antigens are added
- This H substance is formed by the addition of fucose to the glycolipid or glycoprotein backbone
- The subsequent addition of N-acetylgalactosamine creates the A antigen, whereas the addition
of galactose produces the B antigen
- Individuals who lack the “A” and “B” transferases are phenotypically type “O,” whereas those
who inherit both transferases are type “AB.”
- Rare individuals lack the H gene, which codes for fucose transferase, and cannot form H
substance
- => they are homozygous for the silent h allele (hh) and have Bombay phenotype (Oh).
- The ABO blood group system is important because essentially all individuals produce
antibodies to the ABH carbohydrate antigen that they lack
- The naturally occurring anti-A and anti-B antibodies are termed isoagglutinins
- => type A individuals produce anti-B, whereas type B individuals make anti-A
- Neither isoagglutinin is found in type AB individuals, whereas type O individuals produce both
anti- A and anti-B
- => persons with type AB are “universal recipients” because they do not have antibodies
against any ABO phenotype whereas persons with type O blood can donate to essentially all
recipients because their cells are not recognized by any ABO isoagglutinins
- The rare individuals with Bombay phenotype produce antibodies to H substance (which is
present on all red cells except those of hh phenotype) as well as to both A and B antigens and
are therefore compatible only with other hh donors.
- In most people, A and B antigens are secreted by the cells and are present in the circulation
The Rh system
- the second most important blood group system in pretransfusion testing
- The Rh antigens are found on a 30- to 32-kDa RBC membrane protein that has no defined
function
- The presence of the D antigen confers Rh “positivity,” whereas persons who lack the D antigen
are Rh negative
- Two allelic antigen pairs, E/e and C/c, are also found on the Rh protein
- The three Rh genes, E/e, D, and C/c, are arranged in tandem on chromosome 1 and inherited
as a haplotype, i.e., cDE or Cde
- Two haplotypes can result in the phenotypic expres sion of two to five Rh antigens
- The D antigen is a potent alloantigen. About 15% of individuals lack this antigen
- Exposure of these Rh-negative people to even small amounts of Rh-positive cells, by either
transfusion or pregnancy, can result in the production of anti-D alloantibody
Others
- More than 100 blood group systems are recognized, composed of more than 500 antigens
- The presence or absence of certain antigens has been associated with various diseases and
anomalies
- Examples
1. Lewis system
2. I system
3. P system
4. MNSsU system
5. Kell protein
6. Duffy antigens
Page 39 of 269
Pretransfusion testing
1. Typing
- The “forward type” determines the ABO and Rh phenotype of the recipient’s RBC by using
antisera directed against the A, B, and D antigens
- The “reverse type” detects isoagglutinins in the patient’s serum and should correlate with
the ABO phenotype
2. Alloantibody screen
- identifies antibodies directed against other RBC antigens
- performed by mixing patient serum with type O RBCs that contain the major antigens of
most blood group systems and whose extended phenotype is known
- The specificity of the alloantibody is identified by correlating the presence or absence of
antigen with the results of the agglutination
3. Cross-matching
- ordered when there is a high probability that the patient will require a packed RBC (PRBC)
transfusion
- Blood selected for cross-matching must be ABO compatible and lack antigens for which
the patient has alloantibodies
- Nonreactive cross-matching confirms the absence of any major incompatibility and
reserves that unit for the patient
- In an emergency, Rh-positive blood can be safely transfused to an Rh-negative patient who
lacks anti-D
- however, the recipient is likely to become alloimmunized and produce anti-D
- Rh-negative women of childbearing age who are transfused with products containing Rhpositive RBCs should receive passive immunization with anti-D (RhoGam or WinRho) to reduce
or prevent sensitization
Blood transfusion
- Most donated blood is processed into components: PRBCs, platelets, and fresh-frozen plasma
(FFP) or cryoprecipitate
- Whole blood is first separated into PRBCs and platelet-rich plasma by slow centrifugation
- The platelet-rich plasma is then centrifuged at high speed to yield one unit of random donor
(RD) platelets and one unit of FFP
- Cryoprecipitate is produced by thawing FFP to precipitate the plasma proteins and then
separated by centrifugation
- Plasma derivatives such as albumin, intravenous immunoglobulin, antithrombin, and
coagulation factor concentrates are prepared from pooled plasma from many donors and are
treated to eliminate infectious agents
Whole Blood
- provides both oxygen-carrying capacity and volume expansion
- the ideal component for patients who have sustained acute hemorrhage of ≥25% total blood
volume loss
- stored at 4°C to maintain erythrocyte viability, but platelet dysfunction and degradation of some
coagulation factors occurs
- In addition, 2,3-bisphosphoglycerate levels fall over time, leading to an increase in the oxygen
affinity of the hemoglobin and a decreased capacity to deliver oxygen to the tissues, a problem
with all red cell storage
- Fresh whole blood avoids these problems, but it is typically used only in emergency settings
(i.e., military)
- Whole blood is not readily available, because it is routinely processed into components
Packed RBCs
- increases oxygen-carrying capacity in the anemic patient
- Adequate oxygenation can be maintained with a hemoglobin content of 70 g/L in the
normovolemic patient without cardiac disease; however, comorbid factors may necessitate
transfusion at a higher threshold
- In the critical care setting, liberal use of transfusions to maintain near-normal levels of
hemoglobin has not proven advantageous
- In most patients requiring transfusion, levels of hemoglobin of 100 g/L are sufficient to keep
oxygen supply from being critically low
Page 40 of 269
- PRBCs may be modified to prevent certain adverse reactions
- The majority of cellular blood products are now leukocyte reduced, and universal prestorage
leukocyte reduction has been recommended
- These PRBC units contain <5 × 106 donor white blood cells (WBCs), and their use lowers the
incidence of posttransfusion fever, cytomegalovirus (CMV) infections, and alloimmunization.
- Plasma, which may cause allergic reactions, can be removed from cellular blood components
by washing
Platelets
- Thrombocytopenia is a risk factor for hemorrhage, and platelet transfusion reduces the
incidence of bleeding
- The threshold for prophylactic platelet transfusion is 10,000/μL. In patients without fever or
infections, a threshold of 5000/μL may be sufficient to prevent spontaneous hemorrhage
- For invasive procedures, the usual target level is 50,000/μL platelets
- In an unsensitized patient without increased platelet consumption (splenomegaly, fever,
disseminated intravascular coagulation [DIC]), two units of transfused RD per square-meter
body surface area (BSA) is anticipated to increase the platelet count by about 10,000/μL
Fresh frozen plasma
- FFP contains stable coagulation factors and plasma proteins
- => fibrinogen, antithrombin, albumin, and proteins C and S
- Indications for FFP include correction of coagulopathies, including the rapid reversal of
warfarin; supplying deficient plasma proteins; and treatment of thrombotic thrombocytopenic
purpura
- should not be routinely used to expand blood volume
- it is an acellular component and does not transmit intracellular infections, e.g., CMV
- Patients who are IgA-deficient and require plasma support should receive FFP from IgAdeficient donors to prevent anaphylaxis
Cryoprecipitate
- a source of fibrinogen, factor VIII, and von Willebrand factor (VWF)
- ideal for supplying fibrinogen to the volume-sensitive patient
- When factor VIII concentrates are not available, cryoprecipitate may be used because each unit
contains approximately 80 units of factor VIII
- Cryoprecipitate may also supply VWF to patients with dysfunctional (type II) or absent (type III)
von Willebrand’s disease
Plasma derivatives
- Plasma from thousands of donors may be pooled to derive specific protein concentrates,
including albumin, intravenous immunoglobulin, antithrombin, and coagulation factors
- donors who have high-titer antibodies to specific agents or antigens provide hyper- immune
globulins, such as anti-D (RhoGam, WinRho), and antisera to hepatitis B virus (HBV), varicellazoster virus, CMV, and other infectious agents
Transfusion Complications
Acute hemolytic reaction
- Donor erythrocytes carrying either A and/or B erythrocyte antigens bind to the recipient’s anti-A
or anti-B antibodies
- Results in complement formation, membrane attack complex, and immediate haemolysis
- Cytokine and chemokine release mediates sympathetic inflammatory response characterized
by sudden onset of hypotension, tachycardia, pyrexia, breathlessness, tachypnoea, and back
pain
- Bilirubinaemia, anaemia, and haemoglobinuria as a result of haemolysis ensue
- Treatment:
- Stop the transfusion immediately and give basic life support if required
- Keep the bag and giving set for analysis; inform haematology.
- Give crystalloid and furosemide to encourage diuresis.
- Dialysis may be required
Page 41 of 269
Anaphylaxis/alllergic reaction
- Normally, IgE-mediated histamine release reactions to plasma, platelets, and red blood cells
- Mild allergic reactions are relatively common and are characterized by erythematous papular
rashes, wheals, pruritus, and pyrexia
- => treated by stopping the transfusion and administering chlorpheniramine (10mg IV).
- Anaphylaxis characterized by hypotension, bronchospasm, and angioedema
- Stop the transfusion immediately and disconnect connection tubing
- Basic life support may be required
- Treat bronchospasm and angioedema with adrenaline (1mL of 1:10 000 IV),
chlorpheniramine (10mg IV), and hydrocortisone (100mg IV)
Non-haemolytic febrile reaction
- common and normally mild reactions
- caused by recipient antibodies directed against donor human leucocyte antigen (HLA) and
leucocyte-specific antigen on leucocytes and platelets
- Cytokine release mediates mild pyrexia, typically over an hour after transfusion is started
- Antipyrogens such as paracetamol 1g PO/PR limit pyrexia, but antihistamines are not helpful
- Severe reactions feature high grade fever, rigors, nausea, and vomiting
- The severity of symptoms is proportional to the number of leucocytes in the transfused blood
and the rate of transfusion
- Leucocyte-depleted blood helps prevent these reactions
Delayed extravascular haemolytic reaction
- Although pre-transfusion antibody testing is negative, these patients experience accelerated
destruction of transfused red blood cells 7–10 days following transfusion
- This is an antibody-mediated reaction, usually by a patient’s antibody (commonly Rh E, Kell,
Duffy, and Kidd), present in levels too low to be detected clinically until produced in larger
amounts on exposure to circulating antigen
- characterized by an unexpected fall in haematocrit a few days post- transfusion,
hyperbilirubinaemia, and positive Coombs’ test
Transfusion-related acute lung injury
- Non-cardiogenic pulmonary oedema, typically within 6h of transfusion
- mediated by recipient antibodies against donor HLA
- Activated recipient leucocytes migrate to the lung, releasing proteolytic enzymes that cause a
localized capillary leak syndrome and pulmonary oedema.
Bacterial infection
- Serious bacterial contamination of stored blood may occur
- platelets, which are usually stored at room temperature, are at greater risk
- Common organisms include Staphylococcus spp., Enterobacter, Yersinia, and Pseudomonas
spp.
- The recipient becomes pyrexial at >40°C and hypotensive
- may occur during the transfusion or hours after completion and unlike febrile transfusion
reactions, is not self-limiting
- Volume resuscitation
- Culture the patient and send bag and giving sets to microbiology. • Start empirical broadspectrum antibiotics
Non-bacterial infection
- Pre-transfusion testing includes screening for hepatitis B (HbsAg, anti- HBc), hepatitis C (antiHCV), HIV (anti-HIV-1/2, HIV-1 p24 antigen), HTLV (anti-TLC-1/2), and syphilis
- HIV can be transmitted by an infective, but seronegative, donor for about 15 days after infection
- The HCV window is 20 days
- CMV is common in the donor population (40–60%) and immunocompromised donors must
receive leucocyte-depleted or CMV- negative blood
- Malaria may be transmitted by blood transfusion as may new variant Creutzfeldt–Jakob disease
(nvCJD)
Page 42 of 269
Fluid overload
- Characterized by hypotension, acute dyspnoea, high CVP, and hypoxia.
- Stop the transfusion
- Give high flow O2 and loop diuretics (40mg furosemide IV)
Massive transfusion
- Replacement of the patient’s circulating volume within 24h
- Stored red cells are depleted of ATP and 2,3-DPG and leak K+ and the fluid contains citrate
- Large volumes of this blood lead to a blood volume that has poor O2 carrying capacity, high K+,
hypothermic (if blood is not warmed), and coagulopathic due to Ca2+ sequestration
- Reduce the effect of massive transfusion by:
- Use infusion warmers and a warming blanket
- Monitor central circulation and respiratory function closely.
- Consider giving Ca2+ supplements (with care!)
- Check platelets, APTT, and fibrinogen: replace if needed
- Check potassium regularly
12.) Shock. Definition. Classification. Pathogenesis. Clinical symptoms Treatment
General
- Shock is the clinical syndrome that results from inadequate tissue perfusion
- => hypoperfusion-induced imbalance between the delivery of and requirements for oxygen and
substrate leads to cellular dysfunction
- The cellular injury created by the inadequate delivery of oxygen and substrates also induces the
production and release of damage-associated molecular patterns (DAMPs) and inflammatory
mediators that further compromise perfusion through functional and structural changes within
the microvasculature
- => leads to a vicious cycle in which impaired perfusion is responsible for cellular injury that
causes maldistribution of blood flow, further compromising cellular perfusion
- ultimately causes multiple organ failure (MOF) and leads to death
- Clinical shock is usually accompanied by hypotension ( mean arterial pressure <60 mmHg in
previously normotensive persons)
Recognizing shock
- ↑ BP, ↑ pulse, and cold, clammy, pale, sweating
- Confused—may be agitated or drowsy
- Young patients will compensate, with the only signs being decreased pulse pressure,
tachycardia, and decreased urine output
Emergency management
- Assess the airway. If patent, give high flow O2 by non-rebreathing mask
- Check carotid or femoral pulse
- Secure IV access and start giving 500mL crystalloid rapidly
- Recheck BP. If low and falling fast, call crash team
- Take a rapid history and examine patient to differentiate between the following types of shock
Hypovolaemic shock
Etiology
- Trauma, ruptured abdominal aortic aneurysm (AAA), ruptured ectopic pregnancy, postoperative haemorrhage, profound dehydration, burns or pancreatitis
Treatment
- Lie patient flat; high flow O2
- lift legs to autotransfuse if no IV access
- Repeat fluid infusion 500mL IV rapidly: you should see rise in BP
- Take blood and send for FBC, U&E, clotting, and cross-match
- Take arterial blood gas (ABG): estimate Hb, K+ as well as ABG.
Page 43 of 269
- Treat ↑ K+
- If no rapid improvement in BP, look for other causes
Anaphylactic shock
- Causes: Drug allergy, blood product reaction, latex allergy
Symptoms
- History of sudden onset after administration of drug
- Stridor or bronchospasm
- angioedema, urticaria, pruritus, rash
Treatment
- Sit patient up; give high flow O2; call anaesthetist if stridor
- If IV access: give 1mL of 1:10 000 adrenaline bolus; flush; then 100mg hydrocortisone bolus;
flush; then 10mg chlorpheniramine IV
- Repeat again in 5–10min if no improvement
- If no IV access: give 1mL 1:1000 adrenaline IM. Then secure IV access
- If wheezy, give 5mL nebulized salbutamol
Septic shock
- caused by overwhelming sepsis
- Symptoms may be the same as hypovolaemic shock or, if established, with circulatory collapse
- Earlier in the evolution, the patient may look ‘septic’—pyrexial, flushed, bounding pulses
Treatment
- As for hypovolaemic shock
- Take blood cultures; then give IV cefuroxime 750mg tds
Cardiogenic shock
Etiology
- cardiac tamponade (trauma, post-cardiac surgery), arrhythmias, tension pneumothorax
- Fluid overload and congestive cardiac failure (CCF)
- MI, PE, subacute bacterial endocarditis (SBE)
- aortic dissection, decompensated valvular heart disease
Symptoms
- History of recent surgery/trauma, chest pain, dyspnoea, palpitations
Treatment
- Give high flow O2
- Give 2.5mg morphine IV (anxiolytic, venodilator, analgesic, anti-arrhythmic)
- Put patient on cardiac and sats monitors; request 12-lead ECG
- Treat arrhythmias
- Treat myocardial ischaemia with 0.1mg GTN, 300mg aspirin
- Auscultate heart sounds and lung fields
- Treat tension pneumothorax , cardiac tamponade
- Discuss with ITU
- Consider central venous and peripheral arterial monitoring
- Send blood for ABGs, FBC, U&E, clotting, troponin
- Catheterize the patient
- Request CXR—look for pulmonary oedema
- Treat fluid overload with diuretics: furosemide 40mg IV
- Consider transthoracic echo to exclude pericardial effusion and valvular lesions, and to assess
LV function
Page 44 of 269
13.) Infection of the soft tissue. Abcesses and phlegmons. Furunculosis, Carbunculosis.
Hidrosadenitis and Erysipel.
Abscesses
General
- a collection of pus that has built up within the tissue of the body
- Signs and symptoms of abscesses include redness, pain, warmth, and swelling
- The swelling may feel fluid-filled when pressed
- The area of redness often extends beyond the swelling
- Carbuncles and boils are types of abscess that often involve hair follicles, with carbuncles
being larger
Pathological features
- Contain polymorphonuclear neutrophils (PMNs)/macrophages, lymphocytes (live and dead),
bacteria (dead and viable), and liquefied tissue products
- May rupture (‘pointing’), discharge into another organ (forming a fistula eventually), or open
onto another epithelial surface (sinus)
- Incomplete treatment due to resistant organisms (mycobacteria) or poor treatment may lead to
chronic abscesses
- Complete elimination of the organisms in a chronic abscess without drainage can lead to a
‘sterile abscess’
Typical causes
- Suppuration of tissue infection (e.g. renal abscess from pyelonephritis)
- Contained infected collections (e.g. subphrenic abscesses)
- Haematogenous spread during bacteraemias (e.g. cerebral abscesses)
Symptoms
- Deep abscesses are characterized by swing fever, rigors, high WCC, and high CRP
- Untreated, they lead to catabolism, weight loss, and a falling serum albumin
Diagnosis
- Ultrasound, CT, MRI, or isotope studies may be necessary to confirm the diagnosis
Treatment
- Drain the pus, by:
- incision and drainage (perianal abscess)
- CT-guided drain (renal abscess)
- closed surgical drainage (chest empyema)
- or surgical drainage and debridement (intra-abdominal abscess)
- IV antibiotics (may require course of several weeks, indicating PICC line insertion).
Phlegmon
- a localized area of acute inflammation of the soft tissues
- the term which may be used for inflammation related to a bacterial infection or non-infectious
causes (e.g. pancreatitis)
- Most commonly, it is used in contradistinction to a "walled-off" pus-filled collection (abscess),
although a phlegmon may progress to an abscess if untreated
- can be localized anywhere in the body
Symptoms
- As with any form of inflammation, phlegmon presents with inflammatory signs dolor (localized
pain), calor (increase local tissue temperature), rubor (skin redness/hyperemia), tumor (either
clear or non-clear bordered tissue swelling), functio laesa (diminish affected function)
- There may be systemic signs of infection, such as fever, general fatigue, chills, sweating,
headache, loss of appetite
- Location-specific:
- Intestinal: abdominal pain, fever, nausea, vomiting
- Appendix: pain, fever, vomiting, diarrhea, intestinal blockage
Page 45 of 269
- Eye: pain, floaters, disrupted vision, flu-like symptoms
- Mouth floor (here called Ludwigs angina): dental pain, fatigue, ear pain, confusion, swelling
of tongue and neck, difficulty breathing
- Pancreas: fever, leukocytosis, increased levels of amylase, stomach pain, nausea and
vomiting
- Tonsils: fever, sore throat, difficulty speaking, hoarseness
Etiology
- Commonly caused by bacterial infection, as in the case of cellulitis or diverticulitis
- Non-infectious causes of phlegmon include acute pancreatitis, where inflammation is caused
by leaking of pancreatic digestive enzymes into the surrounding tissues
- Factors affecting the development of phlegmon are virulence of bacteria and immunity strength
Treatment
- depends on the location and seriousness of the infection
- A skin phlegmon, if minor, may be treated with oral antibiotics
- Surgical debridement may be needed to clean dead tissue from the area and stop the infection
from spreading
- Oral phlegmon can spread quickly and can be life-threatening
- Aggressive early use of antibiotics is recommended along with intubation
- Surgery as soon as possible to drain the area and stop the spread of the infection is also
recommended.
Furunculosis
Definition
- A boil, also called a furuncle, is a deep folliculitis, infection of the hair follicle
- Most commonly caused by coagulase-positive Staph. Aureus infection
- Results In a painfully swollen area on the skin caused by the accumulation of pus and dead
tissue
- Clustered furuncles are called Carbuncles
Clinical features
- Deep follicular infection that starts as firm red nodule which rapidly becomes painful and then,
after a few days, fluctuant
- Heals with scarring over weeks
- In some individuals, chronic-recurrent
- Localization: Neck, face, axillae, groin, upper back There is a risk of sepsis in
immunosuppressed patients
Complications
- most common are scarring and infection or abcesses of the skin, spinal chord, brain, kidneys or
other organs
- May spread via the bloodstream (bacteremia) and become life- threatening
Diagnosis
- clinical evaluation and culturing of the lesion
Therapy
- avoid manipulation
- Topical antibiotics, systemic antibiotics (penicillinase-resistant penicillin or first-generation
cephalosporin for 7-10 days)
- Solitary furuncle: Systemic antibiotics, incision and drainage after several days
- Recurrent furunculosis;
- Systemic antibiotics (often clindamycin 300 mg q.i.d. for 7-10 days)
- Search for predisposing factors (diabetes mellitus, immunosupression, perineal or nasal
carriage of Staphylococcus aureus)
- Careful skin hygiene
Page 46 of 269
Carbuncle
- cluster of furuncles caused by bacterial infection (most commonly Staph aureus or Step
pyogenes)
- Infection with MRSA (methicillin-resistant staph aureus) has recently become more common
- It is contagious and may spread to other areas of the body or other people
Etiology
- initial cause often hard to determine
- May be folliculitis or friction due to clothing or shaving
- Poor nutrition, weakened immunity
- Poor personal hygiene
Treatment
- like Furunculosis treated with antibiotics and incision/drainage
Hidradenitis
- also known as acne inversa
- a long term skin disease
- characterized by the occurrence of inflamed and swollen lumps
- => typically painful and break open releasing serous fluid or pus
- The areas most commonly affected are the underarms, under the breasts, and groin
- Scar tissue remains after healing
- Self-consciousness or depression may result
Predisposing factors
- Postpubescent individuals are more likely to exhibit HS
- Plugged apocrine (sweat) gland or hair follicle
- Excessive sweating
- Androgen dysfunction
- Genetic disorders that alter cell structure
Triggering factors
- Obesity (exacerbating) rather than a triggering factor (mechanical irritation, occlusion, and skin
maceration)
- Tight clothing, and clothing made of heavy, non-breathable materials.
- Deodorants, depilation products, shaving of the affected area
- Drugs, in particular oral contraceptives
- Hot and especially humid climates
Staging (Hurleys staging system)
I
Solitary or multiple isolated abcess formation without scarring or sinus tracts (may be mistaken for
acne)
II
Recurrent abscesses, single or multiple widely separated lesions with sinus tract formation
III
Diffuse or brad involvement across a regional areawith multiple interconnected sinus tracts and
abscessed
Treatment
- depends on presentation and severity
- Medical:
- Antibiotics (combination or rifampin and clindamycin concurrently for 2-3 months)
- Corticosteroid injections
- Anti- TNF alpha drugs like infliximab or etanercept
- Surgery
- When the process becomes chronic, wide surgical excision is the procedure of choice
- Wounds in the affected area do not heal by secondary intention, and immediate or delayed
application of a split-thickness skin graft is an option
Page 47 of 269
Erysipelas
- Acute infection of the upper dermis and superficial lymphatics due to Streptococcus pyogenes
- characterized by an abrupt onset of fiery-red swelling of the face or extremities
Risk factors
- most common among infants and the elderly
- Immune deficiency, diabetes, alcoholism, diabetes, skin ulceration, fungal infections and
impaired lymphatic drainage
Symptoms
- The distinctive features of erysipelas are well-defined indurated margins, particularly along the
nasolabial fold, rapid progression; and intense pain
- Systemic symptoms include high fevers, shaking, chills, fatigue, headaches and vomiting
within 48 hours of the infection
- More severe infections can result in vesicles, blisters and petechiae with possible skin necrosis
- Repeated infection of the extremities can lead to lymphangitis
- Does not affect the subcutaneous tissue
- Does not release pus, only serum or serous fluid
Diagnosis
- appearance of the rash and inflammation
- The antistreptolysin O titer elevated after 10 days
- Diff Diagnosis: herpes zoster, angioedema, contact dermatitis and diffuse inflammatory breast
cancer
- Can be distinguished from Cellulitis by raised advancing edges and sharp borders
Treatment
- depending on severity, oral or IV antibiotics (penicillin, clindamycin or erythromycin)
14.) Lymphedema of the eytremities: types, stages. Elephantiasis
General
- chronic condition caused by impaired transport of lymph and characterized by swelling of one
or more limbs
- Fluid accumulates in interstitial tissueswhen there is an imbalance between lymph production
and lymph absorption
- Deficiency, reflux or obstruction of lymph vessels pertubs the ability of the lymphatic system to
reabsorb proteins that had been filtered by blood vessels
- The tissue osmotic load promotes interstitial ccumulation
- Persistent lymphedema leads to inflammatory and immune responses characterized by
infiltration of mononuclear cells, fibroblasts and adipocytes, leading to fat and collagen
deposition in the skin and subcutaneous tissues
Types
1. Primary
- Sporadic
- Genetic diseases ( like Milroys disease, Meiges disease, Lymphedema-distichiasis
syndrome, Turners syndome, Parkes-Weber syndrome…)
2. Secondary
- Bacterial lymphangitis
- Lymphogranuloma venereum
- Tuberculosis
3. Neoplastic
- Lymphoma
4. Miscellaneous
- Contact dermatitis
- Rheumatoid arthritis
- Pregnancy
Page 48 of 269
Stages
Stage 0 (or Ia)
Latent, subclinical, swelling is not evident despite
impaired lymph transport. May be years until overt
edema
Stage I
Early accumulation, fluid high in protein content,
subsides with limb elevation
Stage II
Limb elevation rarely reduces tissue swelling, pitting
is manifest. Late in this stage, the limb may not pit
as excess fat and fibrosis supervene
Stage III
Lymphostatic elephantiasis. Pitting can be absent.
Trophic skin changes have developed (like
acanthosis, further deposition of fat and fibrosis
and warty overgrowths)
Diagnosis
1. Abdominal/pelvic ultrasound and CT (used to detect obstructing lesions such as neoplasms)
2. MRI (may reveal honeycomb pattern in the epifascial compartment and identify enlarged
lymphatic channels and lymph nodes
3. Lymphoscintigraphy and lymphangiography are rarely indicated
Treatment
- pat must be instructed to take care of their feet to prevent recurrent lymphangitis
- Prophylactic antibiotics are often helpful
- Fungal infections should be treated aggressively
- exercise and limb elevation my reduce swelling
- Physical therapy may be helpful
- Liposuction in conjunction with decongestive physiotherapy may be considered, especially in
postmastectomy lymphedema
15.) Tetanus. Etiology, clinical symptoms and treatment
General
- an acute disease manifested by skeletal muscle spasm and autonomic nervous system
disturbance
- Caused by the neurotoxin (tetanospasmin) of bacterium Clostridium tetani
- Completely preventable by vaccination
- Established tetanus is a severe disease with a high mortality rate
Etiology
- C. Tetani is an anaerobic, gram-positive spore forming rod
- The spores are highly resilient (resist boiling and disinfection)
- They enter the body through abrasions, wounds or, in neonates, the umbilical stump
- Once in a suitable anaerobic environment, they grow, multiply and release the toxin
- Very low amounts may cause tetanus (minimum lethal human dose: 2.5 ng/kg)
Pathogenesis
- tetanus toxin undergoes retrograde transport into the central nervous system (in opposition to
botulinum toxins, which remain at the neuromuscular junction)
- The Toxin is transported by intra-axonal transport to motor nuclei of the cranial nerves or
ventral horns of the spinal cord
- Once inside the neuron, the toxin enters a retrograde transport pathway, whereby it is
transported proximally to the motor neuron body in what appears to be a highly specific
process
- At the synapses, it cleaves vesicle-associated membrane protein 2 (VAMP2, synaptobrevin).
- =>This molecule is necessary for presynaptic binding and release of neurotransmitter
Page 49 of 269
- => tetanus toxin prevents transmitter release and effectively blocks inhibitory interneuron
discharge
- The increased circulating catecholamine levels in severe tetanus are associated with
cardiovascular complications
Clinical manifestations
- The most common initial symptoms are trismus (lockjaw), muscle pain and stiffness, back pain,
and difficulty swallowing
- As the disease progresses, muscle spasm develops
- Generalized muscle spasm can be very painful
- Commonly, the laryngeal muscles are involved early or even in isolation
- => life-threatening event as complete airway obstruction may ensue
- Spasm of the respiratory muscles results in respiratory failure
- Without ventilatory support, respiratory failure is the commonest cause of death in tetanus
- Spasms strong enough to produce tendon avulsions and crush fractures have been reported,
but this is rare
- Autonomic disturbance is maximal during the second week of severe tetanus, and death due to
cardiovascular events becomes the major risk
- Blood pressure is usually labile, with rapid fluctuations from high to low accompanied by
tachycardia
- Episodes of bradycardia and heart block can also occur
- Autonomic involvement is evidenced by gastrointestinal stasis, sweating, increased tracheal
secretions, and acute (often high-output) renal failure
Diagnosis
- treatment should not be delayed while laboratory tests are conducted
- Culture of C. tetani from a wound provides supportive evidence
- Serum anti-tetanus immunoglobulin G may also be measured in a sample taken before the
administration of antitoxin or immunoglobulin
- => Serum levels >0.1 IU/mL are deemed protective and do not support the diagnosis of tetanus
- Polymerase chain reaction also has been used for detection of tetanus toxin, but its sensitivity
is unknown
Differential Diagnosis
- The few conditions that mimic generalized tetanus include strychnine poisoning and dystonic
reactions to antidopaminergic drugs
- Abdominal muscle rigidity is characteristically continuous in tetanus but is episodic in the latter
two conditions
- Cephalic tetanus can be confused with other causes of trismus, such as oropharyngeal
infection
- Hypocalcemia and meningoencephalitis are included in the differential diagnosis of neonatal
tetanus
Treatment
- If possible, the entry wound should be identified, cleaned, and debrided of necrotic material in
order to remove anaerobic foci of infection and prevent further toxin production
- Metronidazole (400 mg rectally or 500 mg IV every 6 h for 7 days) is the preferred antibiotic
- An alternative is penicillin (100,000–200,000 IU/kg per day), although this drug theoretically may
exacerbate spasms
- Antitoxin should be given early in an attempt to deactivate any circulating tetanus toxin and
prevent its uptake into the nervous system
- Two preparations are available: human tetanus immune globulin (TIG) and equine antitoxin
- TIG is the preparation of choice (less anaphylactoid reactions)
- Recommended therapy is 3000–5000 IU of TIG as a single IM dose, a portion of which
should be injected around the wound
- Equine- derived antitoxin used in low-income countries at a dosage of 10,000–20,000 U
administered IM as a single dose or as divided doses after testing for hypersensitivity
- Spasms are controlled by heavy sedation with benzodiazepines
- Chlorpromazine and phenobarbital are commonly used worldwide, and IV magnesium
sulfate has been used as a muscle relaxant
Page 50 of 269
- establish a secure airway early in severe tetanus (usually tracheostomy, because tracheal
secretions are increased, and dysphagia due to pharyngeal involvement combined with
hyperactivity of laryngeal muscle makes endotracheal intubation difficult)
- Cardiovascular stability is improved by increasing sedation with IV magnesium sulfate
(plasma concentration, 2–4 mmol/L or titrated against disappearance of the patella reflex),
morphine, or other sedatives
Prognosis
- In assessing prognosis, the speed at which tetanus develops is important
- The incubation period (time from wound to first symptom) and the period of onset (time from
first symptom to first generalized spasm) are of particular significance
- shorter times are associated with worse outcome
- In neonatal tetanus, the younger the infant is when symptoms occur, the worse the prognosis
16.) Maxillofacial injuries: types - diagnosis and treatment
General
- commonly encountered in the practice of emergency medicine
- More than 50% of patients with these injuries have multisystem trauma that requires
coordinated management between emergency physicians and surgical specialists in oral and
maxillofacial surgery, otolaryngology, plastic surgery, ophthalmology, and trauma surgery
- Trauma to the maxillofacial region mandates special attention
- => Important sensory systems are contained within the face (e.g. vision, auditory, somatic
sensation, gustatory, olfaction and vestibular)
- => Also, vital structures in the head and neck region are intimately associated (airway,
blood vessels, nerves and gastrointestinal tracts)
- => Lastly, the psychological impact of disfigurement can be devastating
Th face is divided into 3 equal parts
1. The upper face
- from the hairline to the glabella
- Fractures in this region involve the frontal bone and frontal sinus
2. The midface
- from the glabella to the base of the columella
- Fractures is this region involve the maxilla, nasal bones, nasoethmoidal complex (NOE),
zygomaticomaxillary complex (ZMC), and orbital floor.
3. The lower face
- from the base of the columella to the soft tissue menton
- The lower third is subdivided in an upper third from the columella base to the lip
commissure and two lower thirds from the lower lip to menton
- Fractures in this region involve the dentoalveolar segments and the mandible
Types
1. Frontal Bone fractures
- usually result from a high velocity blunt trauma to the forehead (e.g. MVA)
- The anterior and/or posterior table of the frontal sinus may be involved
- More than one-third of patients with frontal sinus fractures are likely to have
concomitant intracranial injury
2. Orbital floor fractures
- Injury to the orbital floor can result in an isolated fracture or can be accompanied by a
medial wall fracture
- There are three recognized theories regarding mechanism of injury; globe-to-wall theory,
hydraulic theory and bone conduction theory
- Most injuries are associated with traumatic injury through interpersonal violence, sport
or road-traffic collision
3. Nasal fractures
- Because of the prominence of the nose and its central location on the face, nasal
fractures are the most common facial fracture
4. Nasoethmoidal fractures (NOE)
Page 51 of 269
- Due to the degree of force and the vectors involved, NOE fractures rarely occur as
isolated events
- Associated injures often include central nervous system injury, cribriform plate fracture,
5.
6.
7.
8.
9.
cerebrospinal fluid rhinorrhea, and fractures of the frontal bone, orbital floor, and middle
third of the face, as well as injury to the lacrimal system
Zygomaticomaxillary complex fractures (ZMC)
- result from direct trauma
- Fracture lines extend through zygomaticotemporal, zygomaticofrontal, and
zygomaticomaxillary sutures and the articulation with the greater wing of the sphenoid
bone
- The majority of these fractures result from trauma inflicted in altercations followed by
MVA
Maxilllary fractures
- classified as LeFort I, II or III
1. LeFort I
- a horizontal maxillary fracture across the inferior aspect of the maxilla
- separates the alveolar process containing the maxillary teeth and hard palate from
the rest of the maxilla
- The fracture extends through the lower third of the septum and includes the medial
and lateral maxillary sinus walls extending into the palatine bones and pterygoid
plates
2. LeFort II
- a pyramidal fracture starting at the nasal bone and extending through the ethmoid
and lacrimal bones downward through the zygomaticomaxillary suture
- => continuing posteriorly and laterally through the maxilla, below the zygoma; and
into the pterygoid plates
3. LeFort III
- is a separation of all of the facial bones from the cranial base with simultaneous
fracture of the zygoma, maxilla, and nasal bones
- The fracture line extends posterolaterally through ethmoid bones, orbits, and
pterygomaxillary suture into the sphenopalatine fossa.
Mandibular fractures
- can occur in multiple locations secondary to the U-shape of the jaw and the weak
condylar neck
- Fractures occur secondary to direct or indirect facial injury, including motor vehicle
accidents, falls, sports, and assaults with blunt weapons or guns
- Close to half of all patients with maxillofacial injuries have concomitant mandibular
fractures
Alveolar fractures
- can occur in isolation from a direct low-energy force or can result from extension of the
fracture line through the alveolar portion of the maxilla or mandible
Panfacial fractures
- usually are secondary to a high-energy mechanism resulting in injury to the upper face,
midface, and lower face
- These fractures must be composed of at least 3 of the possible 4 facial units in order to
be labeled panfacial
Etiology
- In developing countries, motor vehicle accident (MVA) is the most common cause of jaw
fracture, whereas, in developed countries, assault is the most common cause and MVA is the
second most common
- The review by Nalliah et al using the Nationwide Inpatient Sample found assault as the leading
cause for hospitalization for reduction in facial fractures in the United States (36.5%), followed
by MVA (16%), falls (15%), and other transportation accidents (3.5%)
Diagnosis
1. Orbital floor fractures
- Presentation includes disruption or crepitus of the supraorbital rims, subcutaneous
emphysema, and paresthesia of the supraorbital and supratrochlear nerves
- In the conscious patient, facial pain is a common symptom
Page 52 of 269
- Lacerations, contusions, or hematoma to the forehead should make the surgeon suspect
frontal sinus injury
- Visible depression of the forehead is also an important sign
- => can be easily missed in the acute presentation due to the accompanying soft tissue
edema
- Cerebrospinal fluid (CSF) leak can present in as many as 19% of the patients with
posterior table involvement
- A halo sign or B2-transferrin analysis can be useful to confirm leakage
2. Nasal fractures
- Periorbital edema, crepitus, ecchymosis, enophthalmos, and ocular injury can be present
- Infraorbital nerve damage can cause paresthesia or anesthesia of the lateral side of the
nose, upper lip, and maxillary gingiva on the affected side
- Lateral and upward gaze dysfunction may occur secondary to entrapment of the medial
and inferior rectus muscles
- Diplopia may be demonstrated on upward gaze due to entrapment of the inferior rectus
muscle
- If true entrapment is encountered, emergent surgical intervention is indicated, especially in
children, to prevent atrophy of the inferior rectus muscle
- Thorough ocular exam by an ophthalmologist is essential to rule out ocular injury
3. Nasoethmoidal fractures
- Severely displaced NOE fractures can demonstrate telecanthus (increased distance
between the medial canthi of the eyelids), epistaxis, cerebrospinal fluid rhinorrhea, and
epiphora (ie, tears spilling over the lid) secondary to blockage of the nasolacrimal duct
- In patients with severe facial edema, the position of the medial canthal ligament can
appear asymmetric
- A traction test to the medial canthus while palpating the nasal bridge can be helpful in
differentiating fracture of the NOE from nasal bridge edema
4. Zygomatic arch fractures
- Fracture of the arch of the zygoma may exhibit a palpable defect over the area involved
- Pain upon palpation and limitation of movement of the mandible resulting from
interference with movement of the coronoid process of the mandible may be found upon
physical examination.
5. Zygomaticomaxillary comlex fracture
- Clinical findings of ZMC fractures may include a depressed malar eminence, resulting in
flattening of the cheekbone and pain upon palpation of the zygomatic eminence
- The "flame sign" may be present due to disruption and depression of the lateral canthal
tendon
- Evidence of a lateral subconjunctival hemorrhage is present
- A step defect is often palpated along the lateral orbital, infraorbital rim, or
zygomaticomaxillary buttress
- Paresthesia of the lateral side of the nose and upper lip may be present due to
impingement of the infraorbital nerve
- Diplopia may be demonstrated on upward gaze due to entrapment of the inferior rectus
muscle
- Trismus may occur because of a depressed zygomatic arch impinging on the coronoid
process of the mandible thereby preventing the patient from opening their mouth or more
commonly due to concurrent injury to the temporalis muscle
- Intraoral ecchymosis or gingival disruption is possible.
6. Maxillary fractures
- Potential findings of LeFort I fracture include facial edema and mobility of the hard palate
and maxillary alveolus and teeth
- Clinical presentations of LeFort II fractures include facial edema, telecanthus,
subconjunctival hemorrhage, mobility of the maxilla at the nasofrontal suture, epistaxis,
and possible CSF rhinorrhea
- Characteristic findings of LeFort III fractures include massive edema with facial rounding,
elongation, and flattening
- An anterior open bite may be present due to posterior and inferior displacement of the
midfacial skeleton
Page 53 of 269
- Movement of all facial bones in relation to the cranial base with manipulation of the teeth
and hard palate, epistaxis, and CSF rhinorrhea may also be found upon physical
examination
7. Alveolar fractures
- Clinical findings include gingival bleeding, mobility of the alveolus, and loose or avulsed
teeth
8. Mandibular fractures
- Condyle fractures are the most often overlooked
- The area anterior to the meatus of the ear will be tender to palpation
- The condyle on the fractured side will not move when the mandible is opened and closed
- Common findings of mandibular fractures include painful jaw movement and malocclusion
of the teeth and an inability to open the mouth or bite down hard
- Mobility and crepitus can be palpated along the symphysis, angles, or body
- Intraoral edema, ecchymosis, gingival bleeding, or tears may be present
- An anterior open bite can occur with bilateral condylar or angle fractures
- Disruption of the inferior alveolar nerve, including the mental branch, may cause
paresthesia or anesthesia of half of the lower lip, chin, teeth and gingiva when the fracture
involves the mandibular angle, body, or parasymphysis
9. Panfacial fractures
- Physical findings depend on the combination of fractures sustained
- As in any trauma situation, initially address all life-threatening injuries and follow the ATLS
protocol
- A systematic approach to the history and physical examination ensures adequate assessment
of a maxillofacial trauma
- Obtain information regarding allergies, medications, tetanus status, past medical and surgical
history, most recent meal, and events surrounding the injury
Treatment
1. Frontal bone fractures
- The goals in the treatment of frontal sinus injuries are to provide an esthetic outcome,
restore function, and prevent complications
- Nondisplaced anterior sinus wall fractures are treated by observation
- Displaced anterior sinus wall fractures require open surgical repair via a coronal approach
or an endoscopic approach
2. Orbital floor fractures
- Blowout fractures of the orbital floor require consultation with an ophthalmologist and
maxillofacial trauma specialist
- Several approaches are available including subciliary, subtarsal, transconjunctival, and
transconjunctival with lateral canthotomy
- The subciliary approach has the most complications (eg, ectropion) and the
transconjunctival approach the least complications
- The indications and timing for fracture repair are debated; however, most literature
supports a 2-week window for repair
- The goal of surgery is simply to reconstruct the defect area of the fractured wall
- As such, delaying the operation until the edema is resolved is feasible
- The indications for surgery on orbital floor fractures are controversial
- Strong indications include enophthalmos greater than 2 mm, significant hypoglobus, or
diplopia
- Certain consensus also prevails regarding the need for surgery when there is an increase
of orbital volume more than 1 cm3
3. Nasal fractures
- should be managed between days 2-10
- => allows time for resolution of the edema and therefore assists in obtaining the best
reduction possible
- After 10 days, achieving good closed reduction results may be difficult and it may be
necessary to wait for as long as 6 months to obtain satisfactory good results via an open
reduction technique
4. Nasoethmoidal fractures
- demands consideration of both the hard and soft tissues
- should be treated as soon as possible
Page 54 of 269
- Delayed repair is contraindicated especially in type III injuries, which involve the canthal
ligaments
- Once healing and scarring have begun, finding the avulsed medial canthal ligament
5.
6.
7.
8.
9.
becomes difficult, and the scarring may prevent adequate correction of the intercanthal
distance, even with proper reduction of the bones
Zygomatic arch fractures
- usually do not require treatment unless it caused a facial asymmetry
- Marked displacement and/or impingement of the coronoid process of the mandible,
preventing the patient from opening their mouth, requires admission and an open
reduction via transoral (Keen) or temporal (Gillies) approach
- In cases of a severe comminuted fracture an open reduction with internal fixation (ORIF)
may be required
Zygomaticomaxillary complex fracture
- When the impact is sufficient to sustain a fracture of the ZMC consultation with an
ophthalmologist is warranted to rule out ocular injury
- Like the zygomatic arch fracture, surgical treatment of a ZMC fracture is indicated when a
cosmetic deformity or functional loss is noted
- Waiting 4-5 days for the edema to be reduced is helpful to properly assess the situation
- A variety of techniques can be used to produce a satisfactory outcome
- The standard of care is open reduction and internal fixation with miniplates and screws
- The orbital floor is frequently explored and repaired if necessary
Maxillary fractures
- When the impact is severe enough to cause mobility of the maxilla or to a part of it, the
patient should be placed in intermaxillary fixation and open reduction with internal fixation
should be performed at the piriform rim and zygomaticomaxillary buttress
- Patients with a maxillary fracture should be placed on sinus precautions
- If the injury is associated with subcutaneous emphysema, antibiotics coverage is
warranted to cover for the bacterial flora which could have been forced by the air into the
subcutaneous planes
Mandibular fractures
- Temporary stabilization in the emergency department can be addressed with the
application of a Barton bandage
- Bring the teeth into occlusion and wrap the bandage around the crown of the head and
jaw.
- => stabilizes the jaw and greatly reduces pain and hemorrhage
- => A symphysis or body fracture can be reduced temporarily with a bridal wire (a 24gauge wire wrapped around 2 teeth on either side of the fracture)
- => This greatly reduces hemorrhage, pain and infection
- Non displaced mandibular fractures may be treated by closed reduction and intermaxillary
fixation for 4-6 weeks
- many patients do not tolerate closed reduction and prefer open reduction
- Initially, the fracture is stabilized with intermaxillary fixation followed by open reduction and
rigid fixation using titanium miniplates, mandibular plates, or reconstruction plates,
depending on where the fracture is located
- Nondisplaced fractures of the condyle require intermaxillary fixation for 10 days, followed
by physiotherapy to help restore improved function
- Ankylosis of the joint is rare and is believed to be caused by an untreated intracapsular
injury or fracture
Panfacial fractures
- At the time of surgery, tracheostomy or submandibular intubation is required
- A submandibular intubation, which avoids a tracheostomy, is performed by first intubating
orally, and then surgically bringing the tube out through the submandibular space
- Nasoendotracheal intubation is definitely contraindicated
- Facial bones are repositioned beginning at the cranium
- After the occlusion is established by intermaxillary fixation, the remaining facial bones are
repaired with open reduction and internal fixation
Page 55 of 269
17.) Tumors of the maxillofacial region
Epulis fissuratum
General
- an oral pathologic condition that appears in the mouth as an overgrowth of fibrous connective
tissue
- Also referred to less commonly as inflammatory fibrous hyperplasia, denture epulis, and
denture induced fibrous hyperplasia
- is associated with the edges of a denture that does not fit well
- The word, "epulis", can be used to describe any gingival tumor, but it is widely used in
association with this specific condition
Clinical presentation
- Epulis fissuratum appears as a single or multiple fold of tissue that grown in excess around the
alveolar vestibule, which is the area where the gums meet the inner cheek
- Usually, the edge of the denture rests in between two of the folds
- The excess tissue is firm and fibrous, and ulcerations may be present
- The size of the affected tissue varies widely, since almost the entire length of tissue around a
denture can be affected
- More commonly found in women, it can appear in either the mandible or maxilla, but is more
commonly found in the anterior portions of the mouth rather than in the posterior.
- Fibroepithelial polyps, pedunculated lesions of the palate beneath an upper denture are
possible complications
Diagnosis
- microscopically it is an overgrowth of cells from fibrous connective tissue
- The epithelial cells are usually hyperkeratotic and irregular
- hyperplastic rete ridges are often seen
Treatment
- consists of surgical removal with the fixing of a denture in a process called a "reline" or with
making a new denture
Pleomorphic adenoma
General
- a benign neoplastic tumor of the salivary glands
- It is the most common type of salivary gland tumor and the most common tumor of the parotid
gland
- derives its name from the architectural pleomorphism seen by light microscopy
- also known as "Mixed tumor, salivary gland type", which describes its pleomorphic appearance
as opposed to its dual origin from epithelial and myoepithelial elements
Presentation
- usually solitary and presents as a slow growing, painless, firm single nodular mass
- Isolated nodules are generally outgrowths of the main nodule rather than a multinodular
presentation
- It is usually mobile unless found in the palate
- may cause atrophy of the mandibular ramus when located in the parotid gland
- When found in the parotid tail, it may present as an eversion of the ear lobe
- Though it is classified as a benign tumor, pleomorphic adenomas have the capacity to grow to
large proportions and may undergo malignant transformation, to form carcinoma ex
pleiomorphic adenoma, a risk that increases with time
- Although it is "benign" the tumor is aneuploid, it can recur after resection, it invades normal
adjacent tissue and distant metastases have been reported after long (+10 years) time intervals
Page 56 of 269
Diagnosis
- The diagnosis of salivary gland tumors utilize both histopathological sampling and radiographic
studies
- Histopathological sampling procedures include fine needle aspiration(FNA) and core needle
biopsy (bigger needle comparing to FNA)
- Both of these procedures can be done in an outpatient setting
- Diagnostic imaging techniques for salivary gland tumors include ultrasound, computer
tomography(CT) and magnetic resonance imaging(MRI)
- Fine needle aspiration biopsy (FNA), operated in experienced hands, can determine whether
the tumor is malignant in nature with sensitivity around 90%
- FNA can also distinguish primary salivary tumor from metastatic disease.
- Core needle biopsy is more invasive but is more accurate compared to FNA with diagnostic
accuracy greater than 97%
- Furthermore, core needle biopsy allows more accurate histological typing of the tumor.
- In terms of imaging studies, ultrasound can determine and characterize superficial parotid
tumors
- Ultrasound is frequently used to guide FNA or core needle biopsy
- CT allows direct, bilateral visualization of the salivary gland tumor and provides information
about overall dimension and tissue invasion
- => excellent for demonstrating bony invasion
- MRI provides superior soft tissue delineation such as perineural invasion when compared to CT
only
Treatment
- the mainstay of the treatment for salivary gland tumor is surgical resection
- Needle biopsy is highly recommended prior to surgery to confirm the diagnosis
- More detailed surgical technique and the support for additional adjuvant radiotherapy depends
on whether the tumor is malignant or benign
- Generally, benign tumors of the parotid gland are treated with superficial or total
parotidectomy with the latter being the more commonly practiced due to high incidence of
recurrence
- The facial nerve should be preserved whenever possible
- The benign tumor of the submandibular gland is treated by simple excision with preservation of
mandibular branch of the trigeminal nerve, the hypoglossal nerve, and the lingual nerve
- other benign tumors of minor salivary glands are treated similarly.
- Malignant salivary tumors usually require wide local resection of the primary tumor
- if complete resection cannot be achieved, adjuvant radiotherapy should be added to improve
local control
- This surgical treatment has many sequelae such as cranial nerve damage, Frey's syndrome,
cosmetic problems, etc
Ranula
General
- a type of mucocele found on the floor of the mouth
- swelling of connective tissue consisting of collected mucin from a ruptured salivary gland duct,
which is usually caused by local trauma
Etiology
- The gland that most likely causes a ranula is the sublingual gland
- Nonetheless, the submandibular gland and minor salivary glands may be involved
Clinical presentatiom
- An oral ranula is a fluctuant swelling with a bluish translucent color that somewhat resembles
the underbelly of a frog
- If it is large ( >2cm ) it may affect the location of the tongue.
- Though normally above the mylohyoid muscle, if a ranula is found deeper in the floor of the
mouth, it can appear to have a normal color
- A ranula below the mylohyoid muscle is referred to as a “plunging or cervical ranula", and
produces swelling of the neck with or without swelling in the floor of the mouth
Page 57 of 269
- As with mucoceles, ranulas may be subject to recurrent enlargement with occasional rupturing
of its contents
- If it gets large enough it may interfere with swallowing, and cervical ranulas may even interfere
with breathing
Treatmemt
- could involve either a procedure known as "marsupialization" or more often excision of both the
gland and lesion
- Ranulas are likely to reoccur if the sublingual gland or other gland causing them is not also
removed with the lesion
- There is little morbidity or mortality connected with treatment
Hemangioma
General
- an abnormal build up of blood vessels in the skin or internal organs
Clinical presentation
- The classically recognized hemangioma is a visible red skin lesion that may be in the topskin
layers (capillary hemangioma), deeper in the skin (cavernous hemangioma), or a mixture of
both.
- They are usually present at birth, although they may appear within a few months after birth,
often beginning at a site that has appeared slightly dusky or differently colored than the
surrounding tissue
- Hemangiomas, both deep and superficial, undergo a rapid growth phase in which the volume
and size increase rapidly
- This phase is followed by a rest phase, in which the hemangioma changes very little, and an
involutional phase
- During the involutional phase they may disappear completely
- Large cavernous hemangiomas distort the skin around them and will ultimately leave visible
changes
- A superficial capillary hemangioma may involute completely, leaving no evidence of its past
presence
- may be present anywhere on the body
- However, they are most disturbing to parents when they are on the infant's face or head.
- Hemangiomas of the eyelid may interfere with the development of normal vision and must be
treated in the first few months of life
- On rare occasions,the size and location of hemangiomas may interfere with breathing, feeding,
or other vital functions => These lesions also require early treatment.
- Large cavernous hemangiomas may develop secondary infections and ulcerate
- Bleeding is common and may be significant following injury
Exams
- are diagnosed by a physical examination
- In the case of deep or mixed lesions, a CT scan or MRI scan may be performed to ensure that
deeper structures are not involved
Treatmemt
- Superficial or "strawberry" hemangiomas often are not treated
- When they are allowed to disappear on their own, the result is usually normal appearing skin
- In some cases, a laser may be used to eradicate the small vessels
- Cavernous hemangiomas that involve the eyelid and obstruct vision are generally treated with
injections of steroids or laser treatments that rapidly reduce the size of the lesions, allowing
normal vision to develop
- Large cavernous hemangiomas or mixed hemangiomas are treated, when appropriate, with oral
steroids and injections of steroids directly into the hemangioma
- Recently, lasers have been used to reduce the bulk of the hemangiomas
- Lasers emitting yellow light selectively damage the vessels in the hemangioma without
damaging the overlying skin
- Some physicians are using a combination of steroid injection and laser therapy together
Page 58 of 269
Papilloma
General
- benign tumors that are composed of fibrous or connective tissue
- They can grow in all organs, arising from mesenchyme tissue
- The term "fibroblastic" or "fibromatous" is used to describe tumors of the fibrous connective
tissue
- When the term fibromais used without modifier, it is usually considered benign, with the term
fibrosarcoma reserved for malignant tumors
- The term fibroid can also refer to tumors of smooth muscle, as in uterine fibroids
- Types
1. Hard Fibroma
- fibroma durum consists of many fibres and few cells, e.g. in skin it is called
dermatofibroma (fibroma simplex or nodulus cutaneous)
- A special form is the keloid which derives from hyperplastic growth of scars
2. Soft Fibroma
- The soft fibroma (fibroma molle) or fibroma with a shaft (acrochordon, skin tag, fibroma
pendulans) consist of many loosely connected cells and less fibroid tissue
- mostly appears at the neck, armpits or groins
3. Angiofibroma
- consists of many often dilated vessels,
- a vasoactive tumor occurring almost exclusively in adolescent males
4. Myxofibroma
- produced by liquefaction of the underlying soft tissue
Treatmemt
- Benign fibromas can be removed or left alone
- examine the fibroma and determine whether it may be malignant
- If there is any question as to whether it may be cancer-related, it should be removed
- This is usually a brief outpatient procedure
18.) Neck: diseases, injuries, inflammation and tumors
Thyroglossal cyst, sinus and fistula
General:
- Thyroglossal cyst is a fluid-filled sac resulting from incomplete closure of the thyroglossal duct
- Thyroglossal sinus results from persistence of the whole duct
Presentation
- Usually presents in children or young adults
- Ninety per cent present as a painless midline cyst
- Ten percent appear on one side of the midline, usually the left
- Seventy-five per cent appear in front of the hyoid bone and the majority of the rest at any point
to the root of the neck
- The cyst elevates on protruding tongue if attached to hyoid or if attached to isthmus of thyroid
elevates on swallowing
- Five per cent become infected presenting as a painful, red neck swelling
- Fifteen per cent have a fistula to the skin (due to infection or incomplete excision)
- Papillary carcinoma of the thyroglossal ductal cells is rare (Treatment is by excision )
Diagnosis
- Ultrasound scan => investigation of choice
- CT scan will often reveal a well circumscribed cyst related to the midline of the hyoid bone
- Fine needle aspiration may reveal a cloudy infected fluid or a straw- coloured fluid
Treatment
1. Infected thyroglossal cyst
- Majority respond to antibiotics
- Surgical drainage if abscess formed or failure to respond to antibiotics
Page 59 of 269
- Elective excision of the cyst once acute infection has resolved
2. Surgery
- Excision is recommended for most cysts.
- Remove through a transverse midline incision in a skin crease
- Divide the platysma muscle and excise the cyst using sharp and blunt dissection
- On the deep surface, it is attached to the hyoid bone; excise approximately 1cm of the
bone in midline, removing any underlying thyroglossal duct epithelium (Sistrunk’s
procedure)
- Close the wound in layers with a suction drain
- If there is a fistula or sinus in the neck, excise it through a transverse
elliptical incision. Again use blunt dissection and remove the middle part of the hyoid bone
Complications
- The important structures that must be considered when operating on the thyroid gland include:
1. Recurrent laryngeal nerve
2. Superior laryngeal nerve
3. Parathyroid glands.
4. Trachea
5. Common carotid artery
6. Internal jugular vein
Brachial cyst, sinus, fistula
General
- A branchial fistula is a tract running from the neck skin through to the posterior pillar of the
fauces; these are very rare
- A branchial sinus occurs when the lower part of this tract remains open on to the neck skin
surface
- A brachial abscess is an infected branchial cyst
Etiology
- Theories include:
- Cystic degeneration of epithelial derivatives of the first, second, or third branchial clefts
- Cystic degeneration of epithelial elements in a cervical lymph node
Presentation
- Presents as a neck lump, usually painless
- typically in early adulthood
- Sixty to seventy percent are anterior to the upper third of the sternomastoid muscle with the
posterior border lying beneath the sternomastoid
- Other sites include: Parotid gland, Anterior to the lower two-thirds of the sternomastoid,
Anterior to the pharynx and In the posterior triangle of the neck
- Two-thirds occur on the left side; 2% are bilateral
- May present with an acute branchial cyst abscess causing pain, increased swelling, and
occasionally, pressure symptoms (difficulty swallowing or breathing)
Diagnosis (branchial cyst or abcess)
- Ultrasound scan is first investigation of choice. CT/MRI for complex cases
- Fine needle aspiration biopsy:
1. Abscesses. Purulent fluid is obtained that may culture organisms
2. Cysts. Straw-coloured fluid containing cholesterol crystals
Treatment
1. Branchial abscess
- Drain via a transverse incision in the neck at the point of maximum convexity.
- Suture a Yeates type drain.
- Give antibiotics and make no attempt to remove the cyst until the infection has resolved
completely
Page 60 of 269
2. Branchial cyst
- Most cysts are excised to achieve a diagnosis and prevent symptoms or complications
- Place a transverse incision over the cyst, preferably in a transverse skin crease, long enough
to match the size of the cyst
- Divide the platysma and the deep fascia over the anterior border of the sternomastoid and
retract the muscle posteriorly
- Remove the cyst, usually by blunt/sharp dissection
- Use suction drainage and close the wound in layers
- If the cystic lesion is in the parotid gland and cannot be distinguished from any other parotid
lesion, extend a preauricular incision into the neck as for a superficial parotidectomy
3. Branchial fistula
- Excise a sinus of fistula through a horizontal elliptical incision around the neck opening
- Blunt and sharp dissection of sinus tract as far as possible
- If the upper end of the tract cannot be reached, make a further transverse incision at a higher
level (‘stepladder’ incisions)
- Sometimes the tract runs between the internal and external carotid arteries and sometimes
up to the pharyngeal wall in the region of the middle constrictor
- Close the wounds in layers with suction drainage
Salivary calculi
General
- occur most commonly within the submandibular ductal tree (80%), 20% in the parotid
- Composed of calcium phosphate and carbonate; may be related to sialadenitis (inflammation of
a salivary gland)
Presentation
- Pain and swelling of the affected gland on eating and drinking
- If there is partial obstruction of the duct, the swelling can last minutes to several hours
- Complete obstruction leads to persistent swelling and infection
- The patient may also experience colicky pain in the duct when eating
Diagnosis
- Ultrasound scanning of parotid and submandibular glands is often the choice of investigation
- Radiographs of the submandibular gland, parotid gland, and ducts are helpful
- Twenty per cent of submandibular and 80% of parotid calculi are radiolucent
- Lower occlusal X-ray of the teeth will show a stone in the distal portion of submandibular duct
- A lateral oblique X-ray or orthopantomogram (OPT) of the mandible will show a calculus in the
submandibular gland
- Parotid sialography may show a filling defect. Sialectasis is often seen. May provide therapeutic
benefit due to flushing out of debris in the ductal tree
Treatment
- Stones in the intra-oral part of the ducts can be removed under local anaesthesia
- => Steady the stone with a Babcock’s forceps and incise directly over it
- => Remove the stone; leave the duct marsupialized
- => Stones within the submandibular gland require removal of the gland itself
- Removal of a calculus from the parotid gland is a rare operation
- => Most calculi are at the distal end of parotid duct (as it does an ‘S’ bend through
buccinator muscle) and can be released by intra-oral incision of parotid duct papilla
- Most parotid gland obstructive/inflammatory disease is treated conservatively with sialogogues
and intermittent massage of the gland towards the duct
- => Duct dilation using lacrimal probes is useful as most strictures/obstruction occur at the
‘S’ portion noted above
Page 61 of 269
Acute parotitis
General
- inflammation of the parotid gland
- Elderly, debilitated, dehydrated patients with poor oral hygiene or who are on anticholinergic
drugs are at greatest risk
- The most common pathogen is Staphylococcus aureus
- Causes include:
- Acute or chronic obstruction (now commonest cause)
- Bacterial (ascending parotitis), less common
- Viral infection, e.g. paramyxovirus (mumps), HIV.
- Inflammatory disorders, e.g. Sjögren’s syndrome, sarcoidosis
- Any cause of inflammation of lymph nodes within the parotid gland
Presentation
- Presents as an acutely painful preauricular swelling
- often a history of recurrent, intermittent swelling of the gland
- usually tender on palpation
- patient may be toxic with fever and raised WCC, and pus may exude from the opening of the
parotid duct opposite the crown of the second upper molar tooth
Diagnosis
- Plain X-rays to determine whether radio-opaque calculi are present in the duct or gland
- Ultrasound or CT scanning may help differentiate between stones, inflammation, and tumour
- If pus is present, take a bacteriology swab
Treatment
1. Acute
- Most patients respond to antibiotics:
- Give amoxicillin 500mg tid , IV if necessary
- Rehydrate dehydrated and debilitated patients
- Good oral nursing care with chlorhexadine mouth rinses
- Review patients by clinical examination after the infection has subsided to make sure that the
obstruction was not due to a parotid tumour
- If a parotid abscess develops, it should be drained surgically:
- Make an incision over the abscess under general anaesthetic where it appears to be
pointing, parallel to the branches of the facial nerve to avoid damaging them
- Open the abscess with sinus forceps and place a Yeates drain in the
wound
2. Recurrent
- Teach patients with recurrent parotitis to massage the gland in order to express saliva from
the duct
- Dilatation of the duct with lacrimal probes can assist drainage
- Remove radio-opaque calculi, if possible
- If recurrent parotitis persists for months or years, a total parotidectomy is curative
Salivary gland tumors
Presentation
- rare, accounting for 0.4% of all malignant tumours
- 80% arise in the parotid gland
- Most patients present with a slow-growing lump in the affected gland
- Pain, paraesthesia (e.g. lingual nerve in submandibular gland), facial palsy (parotid gland) imply
malignancy
- Salivary tumours of minor glands in upper aerodigestive tract (UADT) present as a lump
- => 50% of these are malignant
Page 62 of 269
Types:
Benign
1. Pleomorphic adenoma
- 80% of benign parotid tumours
- Peak incidence 30–50y
- Composed of epithelial and mesothelial cells that form a mucous matrix, often with
chondromatous components
- grows slowly and has no true capsule so that strands of tumour cells protrude into normal
surrounding tissue
- Local extension may be widespread with recurrence if excision is incomplete
- Malignant change (adenocarcinoma) occurs in 20% after 10y and is seen in asymptomatic
deep lobe parotid tumours
2. Warthins tumor
- Usually affects men >50y
- 10% are bilateral
- Benign and presents as a slow-growing soft swelling.
- Successfully treated by wide local excision
Malignant
3. Mucoepidermoid tumor
- Low grade malignancy, though variable behaviour
- Most grow slowly, invading locally and eventually metastasizing to neck
lymph nodes, lung, and skin
4. Adenoid cystic carcinoma
- slow growing malignant tumour with indolent behaviour
- Perineural invasion propensity and facial palsy common with extension through
stylomastoid foramen
- Lung metastasis common
- Often regarded as incurable, but individuals can lead a normal life over 20–30y
- Treatment is extensive wide local excision, with nerve/organ preservation where possible.
- Radiotherapy used for controlling lung symptoms if they arise
5. Acinic cell carcinoma
- slow-growing, but may metastasize unexpectedly
- Surgery is the treatment of choice
6. Squamous cell carcinoma, adenocarcinoma, undifferentiated carcinoma
- generally high grade malignant tumors
- Often rapid local invasion into extraparotid tissues and infratemporal fossa, leading to pain
and trismus
- There may be skin fixation or ulceration with facial nerve palsy and invasion of the external
auditory canal
- incurable; palliative radiotherapy
19.) Endemic and sporadic goiter
General
- a goiter is an enlarged thyroid gland
- Biosynthetic defects, iodine deficiency, autoimmune disease, and nodular diseases are causes
Etiology
- Biosynthetic defects and iodine deficiency are associated with reduced efficiency of thyroid
hormone synthesis, leading to increased TSH, which stimulates thyroid growth as a
compensatory mechanism to overcome the block in hormone synthesis
- In Graves' disease, the goiter results mainly from the TSH-R-mediated effects of TSI
- The goitrous form of Hashimoto's thyroiditis occurs because of acquired defects in hormone
synthesis, leading to elevated levels of TSH and its consequent growth effects
- Lymphocytic infiltration and immune system-induced growth factors also contribute to thyroid
enlargement in Hashimoto's thyroiditis
- Nodular disease is characterized by the disordered growth of thyroid cells, often combined with
the gradual development of fibrosis
Page 63 of 269
- the management of goiter depends on the etiology => the detection of thyroid enlargement on
physical examination should prompt further evaluation to identify its cause
- Thyroid nodules may be solitary or multiple, and they may be functional or nonfunctional
Diffuse nontoxic (simple) goiter
- occurs in the absence of nodules and hyperthyroidism
- referred to as simple goiter, because of the absence of nodules, or colloid goiter, because of
the presence of uniform follicles that are filled with colloid
- most commonly caused by iodine deficiency
- termed endemic goiter when it affects >5% of the population
- Termed sporadic goiter in nonendemic regions (cause usually unknown)
- goiter is more common in women than men, probably because of the greater prevalence of
underlying autoimmune disease and the increased iodine demands associated with pregnancy
- In iodine-defficient areas, thyroid enlargement reflects a compensatory effort to trap iodide
and produce sufficient hormone under conditions in which hormone synthesis is relatively
ineffcient
- TSH levels are usually normal or only slightty increased, suggesting increased sensitivity to TSH
or activation of other pathways that lead to thyroid growth
- Endemic goiter is also caused by exposure to environmental goitrogens such as cassava root,
which contains a thiocyanate
- vegetables of the Cruciferae family (known as cruciferous vegetables) (e.g. Brussels sprouts,
cabbage and cauliflower); and milk from regions where goitrogens are present in grass
Examination
- If thyroid function is preserved, most goiters are asymptomatic
- Examination of a diffuse goiter reveals a symmetrically enlarged, nontender generally soft gland
without palpable nodules
- goiter is defined as a lateral lobe with a volume greater than the thumb of the individual being
-
examined
If the thyroid is markedly enlarged it can cause tracheal or esophageal compression
These features are unusual in the absence of nodular disease and fibrosis
Substernal goiter may obstruct the thoracic inlet
Pemberton's sign refers to symptoms of faintness with evidence of facial congestion and
external jugular venous obstruction when the arms are raised above the head, a maneuver that
draws the thyroid into the thoracic inlet
Diagnosis
- Respiratory flow measurements and CT or MRI should be used to evaluate substernal goiter in
patients with obstructive signs or symptoms
- Thyroid function tests should be performed in all patients with goiter to exclude thyrotoxicosis
or hypothyroidism
- It is not unusual, particularly in iodine deficiency to find a low total T4, with normal T3 and TSH,
reflecting enhanced T4 -T3 conversion
- A low TSH with a normal free T3 and free T4, particularly in older patients, suggests the
possibility of thyroid autonomy or undiagnosed Graves' disease and is termed subclinical
thyrotoxicosis
- The benefit of treatment (typically with radioiodine) in subclinical thyrotoxicosis versus followup and implementing treatment if free T3 or free T4 levels become abnormal is unclear, but
treatment is increasingly recommended in the elderly to reduce the risk of atrial fibrillation and
bone loss
- TPO antibodies may be useful to identify patients at increased risk of autoimmune thyroid
disease
- Low urinary iodine levels (<50 g/L) support a diagnosis of iodine deficiency
- Thyroid scanning is not generally necessary but will reveal increased uptake in iodine deficiency
and most cases of dyshormonogenesis
- Ultrasound is not generally indicated in the evaluation of diffuse goiter unless a nodule is
palpable on physical examination
Page 64 of 269
Treatment
- lodine replacement induces variable regression in iodine deficiency, depending on how long it
has been present and the degree of fibrosis that has developed
- Surgery is rarely indicated for diffuse goiter
- Exceptions include documented evidence of tracheal compression or obstruction of the
thoracic inlet which are more likely to be associated with substernal MNGs
- Surgery should be followed by replacement with levothyroxine with the aim of keeping the TSH
level at the lower end of the reference range to prevent regrowth of the goiter
Nontoxic multinodular goiter
General
- There is typically a wide variation in nodule size
- most nodules within an MNG are polyclonal in origin suggesting a hyperplastic response to
locally produced growth factors and cytokines
- TSH which is usually not elevated may play a permissive or contributory role
- Monoclonal lesions also occur within an MNG, reflecting mutations in genes that confer a
selective growth advantage to the progenitor cell
Clinical manifestations
- Most patients with nontoxic MNG are asymptomatic and euthyroid
- typically develops over many years and is detected on routine physical examination when an
individual notices an enlargement in the neck or as an incidental finding on imaging
- If the goiter is large enough it can ultimately lead to compressive symptoms including difficulty
swallowing, respiratory distress (tracheal compression or plethora (venous congestion), but
these symptoms are uncommon)
- Symptomatic MNGs are usually extraordinarily large and/or develop fibrotic areas that cause
compression
- Sudden pain in an MNG is usually caused by hemorrhage into a nodule but should raise the
possibility of invasive malignancy
- Hoarseness, reflecting laryngeal nerve involvement also suggests malignancy
Diagnosis
- On examination, thyroid architecture is distorted and multiple nodules of varying size can be
appreciated
- Because many nodules are deeply embedded in thyroid tissue or reside in posterior or
substernal locations it is not possible to palpate all nodules
- Pemberton's sign, characterized by facial suffusion when the patient's arms are elevated above
the head suggests that the goiter has increased pressure in the thoracic inlet
- A TSH level should be measured to exclude subclinical hyper- or hypothyroidism but thyroid
function is usually normal
- Tracheal deviation is common but compression must usually exceed 70% of the tracheal
diameter before there is significant airway compromise
- Pulmonary function testing can be used to assess the functional effects of compression, which
characteristically causes inspiratory stridor
- CT or MRI can be used to evaluate the anatomy of the goiter and the extent of substernal
extension or tracheal narrowing
- A barium swallow may reveal the extent of esophageal compression
- The risk of malignancy in MNG is similar to that in solitary nodules
- Ultrasonography can be used to identify which nodules should be biopsied based on
sonographic features and size
- For nodules with more suspicious imaging characteristics (e.g. hypoechogenicity,,
microcalcications, irregular margins), biopsy is recommended when over 1 cm
Treatment
- Most nontoxic MNGs can be managed conservatively
- T4 supression is rarely effective for reducing goiter size and introduces the risk of subcliniιal or
overt thyrotoxicosis, particularly if there is underlying autonomy or if it develops during
treatment
Page 65 of 269
- If levothyroxine is used, it should be started at low doses (50 μ9 daily) and advanced gradually
while monitoring the TSH level to avoid excessive suppression
- Contrast agents and other iodine-containing substances should be avoided because of the risk
of inducing the Jod-Basedow effect, characterized by enhanced thyroid hormone production
by autonomous nodules
- Radioiodine is used with increasing fre quency in areas where large goiters are more prevalent
because it can decrease goiter size and may selectively ablate regions of autonomy
- Dosage depends on the size of the goiter and radioiodine uptake but is usually about 3.7 MBq
(0.1 mCi) per gram of tissue
Toxic multinodular goiter
-
The pathogenesis of toxic MNG appears to be similar to that of nontoxic MNG
the major difference is the presence of functional autonomy in toxic MNG
The molecular basis for autonomy in toxic MNG remains unknown
As in nontoxic goiters, many nodules are polyclonal whereas others are monoιlonal and vary in
their clonal origins
Genetic abnormalities known to confer functional autonomy such as activating TSH-R or G,α
mutations are not usually found in the autonomous regions of toxic MNG goiter.
In addition to features of goiter, the clinical presentation of toxic MNG includes subclinical
hyperthyroidism or mild thyrotoxicosis
The patient is usually elderly and may present with atrial fibrillation or palpitations, tachycardia,
nervousness, tremor or weight loss
Recent exposure to iodine from contrast dyes or other sources may precipitate or exacerbate
thyrotoxicosis
The TSH level is low
The uncombined T4 level may be normal or minimally increased
T3 is often elevated to a greater degree than T4 Thyroid scan shows heterogeneous uptake
with multiple regions of increased and decreased uptake
24-h uptake of radioiodine may not be increased but is usually in the upper normal range.
Prior to definitive treatment of the hyperthyroidism, ultrasound imaging should be performed to
assess the presence of discrete nodules corresponding to areas of decreased uptake ("cold"
nodules)
the cytology results, if indeterminate or suspicious, may direct the therapy to surgery
Treatment
- Antithyroid drugs normalize thyroid function and are particularly useful in the elderly or ill
patients with limited lifespan
- In contrast to Graves' disease, spontaneous remission does not occur and so treatment is
long-term
- Radioiodine is generally the treatment of choice; it treats areas of autonomy as well as
decreasing the mass of the goiter
- Sometimes a degree of autonomy remains, presumably because multiple autonomous regions
emerge as soon as others are treated and further radioiodine treatment may be necessary
- Surgery provides definitive treatment of underlying thyrotoxicosis as well as goiter
- Patients should be rendered euthyroid using an antithyroid drug before operation
20.) Grave’s and thryotoxicosis. Inflammatory diseases of the thyroid gland
Thyrotoxicosis
General
- defined as the state of thyroid hormone excess
- not synonymous with hyperthyroidism (the result of excessive thyroid function)
- the major etiologies of thyrotoxicosis are hyperthyroidism caused by Graves' disease, toxic
MNG, and toxic adenomas
Page 66 of 269
Causes
1. Primary Hyperthyroidism
- Graves Disease
- Toxic multinodular goiter
- Toxic adenoma
- Functioning thyroid carcinoma metastases
- Activating mutation of theTSH receptor
- Activating mutation of Gso (McCune-Albright syndrome)
- Struma ovarii
- Drugs: iodine excess (Jod-ßasedow phenomenon)
2. Thyrotoxicosis without Hyperthyroidism
- Subacute thyroiditis
- Silent thyroiditis
- Other causes of thyroid destruction: amiodarone, radiation, infarction of adenoma
- Ingestion of excess thyroid hormone (thyrotoxicosis factitia) or thyroid tissue
3. Secondary Hyperthyroidism
- TSH-secreting pituitary adenoma
- Thyroid hormone resistance syndrome (occasional patients may have features of
thyrotoxicosis)
- Chorionic gonadotropin-secreting tumor
- Gestational thyrotoxicosis
Symptoms
- Hyperactivity
- irritability
- dysphoria
- Heat intolerance and sweating
- Palpitations
- Fatigue and weakness
- Weight loss with increased appetite
- Diarrhea
- Polyuria
- Oligomenorrhea
- loss of libido
Signs
-
Tachycardia; atrial fibrillation in the elderly
Tremor
Goiter
Warm, moist skin
Muscle weakness, proximal myopathy, Lid retraction or lag
Gynecomastia
Destructive Thyroditis
- (subacute or silent thyroiditis)
- typically presents with a short thyrotoxic phase due to the release of preformed thyroid
hormones and catabolism of Tg
- True hyperthyroidism is absent as demonstrated by a low radionuclide uptake
- Circulating Tg levels are usually increased
TSH secreting pituitary adenoma
- a rare cause of thyrotoxicosis
- characterized by the presence of an inappropriately normal or increased TSH level in a patient
with hyperthyroidism, diffuse goiter, and elevated T4 and T3 levels
- Elevated levels of the alpha subunit of TSH, released by the TSH-secreting adenoma, support
this diagnosis, which can be confirmed by demonstrating the pituitarγ tumor on MRI or CT scan
- A combination oftranssphenoidal surgery, sella irradiation, and octreotide may be required to
normalize TSH, because many of these tumors are large and locally invasive at the time of
diagnosis
- Radioiodine or antithyroid drugs can be used to control thyrotoxicosis
Page 67 of 269
Graves Disease
General
- accounts for 60-80% of thyrotoxicosis.
- prevalence varies among populations, reflecting genetic factors and iodine intake (high iodine
intake is associated with an increased prevalence of Graves' disease)
- The disorder rarely begins before adolescence and typically occurs between 20 and 50 years of
age
- also occurs in the elderly
Etiology
- The exact cause is unclear; however, it is believed to involve a combination of genetic and
environmental factors
4. Genetic
- A genetic predisposition for Graves' disease is seen, with some people more prone to
develop TSH receptor activating antibodies due to a genetic cause
- Human leukocyte antigen DR (especially DR3) appears to play a role
- To date, no clear genetic defect has been found to point to a single-gene cause
- Genes believed to be involved include those for thyroglobulin, thyrotropin receptor, protein
tyrosine phosphatase nonreceptor type 22, and cytotoxic T-lymphocyte–associated
antigen 4, among others
5. Enviromental
- Indirect evidence suggests that stress is an important environmental factor, presumably
operating through neuroendocrine effects on the immune system
- Smoking is a minor risk factor for Graves disease and a major risk factor for the
development of ophthalmopathy
- Sudden increases in iodine intake may precipitate Graves' disease
- there is a three fold increase in the occurrence of Graves' disease in the postpartum
period.
- may occur during the immune reconstitution phase a er highly active antiretroviral therapy
(HAART) or alemtuzumab treatment
Lab evaluation
- In Graves' disease the TSH level is suppressed and total and unbound thyroid hormone levels
are increased
- In 2-5% of patients (and more in areas of borderline iodine intake), only T3 is increased (T3
toxicosis)
- The converse state of T4 toxicosis, with elevated total and unbound T4 and normal T3 levels
is occasionally seen when hyperthyroidism is induced by excess iodine providing surplus
substrate for thyroid hormone synthesis
- Measurement of TPO antibodies or TRAb may be useful if the diagnosis is unclear clinically but
is not needed routinely
- Associated abnormalities that may cause diagnostic confusion in thyrotoxicosis include
elevation of bilirubin, liver enzymes and ferritin
- Microcytic anemia and thrombocytopenia may occur.
Treatment
- the hyperthyroidism of Graves' disease is treated by reducing thyroid hormone synthesis, using
antithyroid drugs or reducing the amount of thyroid tissue with radioiodine thyroidectomy
- Antithyroid drugs are the predominant therapy in many centers in Europe and Japan whereas
radioiodine is more often the first line of treatment in North America
- => no single approach is optimal and patients may inquire multiple treatments to achieve
remission
- The main antithyroid drugs are the thionamides such as propylthiouracil, carbimazole and the
active metabolite of the latter methimazole
- AII inhibit the function of TPO, reducing oxidation and organification of iodide
- These drugs also reduce thyroid antibody levels by mechanisms that remain unclear and they
appear to enhance rates of remission
- Propylthiouracil inhibits deiodination of T4→T3
Page 68 of 269
- The initial dose of carbimazole or methimazole is usually 1 0-20 mg every 8 or 1 2 h, but oncedaily dosing is possible after euthyroidism is restored
- Propylthiouracil is given at a dose of 1 00-200 mg every 6-8 h
- The starting dose of antithyroid drugs can be gradually reduced (titration regimen) as
thyrotoxicosis improve
- Propranolol (20-40 mg every 6 h) may be helpful to control adrenergic symptoms especially in
the early stages before antithyroid drugs take effect
- Radioiodine causes progressive destruction of thyroid cells and can be used as initial treatment
or for relapses after a trial ofantithy roiddrugs
Surgery
- Subtotal or near-total thyroidectomy is an option for patients who relapse after antithyroid
drugs and prefer this treatment to radioiodine
- Some experts recommend surgery in young individuals, particularly when the goiter is very
large
- careful control of thyrotoxicosis with antithyroid drugs followed by potassium iodide (3 drops
55KI orally tid) is needed prior to surgery to avoid thyrotoxic crisis and to reduce the vascularity
of the gland
- The major complications of surgery-bleeding, laryngeal edema, hypoparathyroidism and
damage to the recurrent laryngeal nerves-are unusual when the procedure is performed by
highly experienced surgeons
- Recurrence rates in the best series are <2%, but the rate of hypothyroidism is only slightly less
than that following radioiodine treatment
Thyroiditis
General
- Thyroiditis, or inflammation of the thyroid gland, encompasses a diverse group of disorders
characterized by some form of thyroid inflammation
- clinically significant types of thyroiditis:
1. Hashimoto thyroiditis (or chronic lymphocytic thyroiditis)
2. granulomatous (de Quervain) thyroiditis
3. subacute lymphocytic thyroiditis
Chronic lymphocytic (Hashimoto) Thyroiditis
- the most common cause of hypothyroidism in areas of the world where iodine levels are
suffcient.
- characterized by gradual thyroid failure secondary to autoimmune destruction of the thyroid
gland
- It is most prevalent between the ages of 45 and 65 years and is more common in women than in
men, with female predominance in a ratio of 10:1 to 20:1
- Although it is primarily a disease of older women, it can occur in children and is a major cause of
nonendemic goiter in children
Pathogenesis
- caused by a breakdown in self- tolerance to thyroid autoantigens
- Thus, circulating autoantibodies against thyroid antigens are present in the vast majority of
patients, who demonstrate progressive depletion of thyroid epithelial cells (thyrocytes) and their
replacement by mononuclear cell infiltration and fibrosis
- The inciting events leading to breakdown in self-tolerance have not been fully elucidated, but
multiple immunologic mechanisms that may contribute to thyrocyte damage have been identified
,including
1. CD8+ cytotoxic T cell–mediated cell death
- CD8+ cytotoxic T cells may cause thyrocyte destruction.
2. Cytokine-mediated cell death:
Page 69 of 269
- Excessive T cell activation leads to the production of inflammatory cytokines such as
interferon-γ in the thyroid gland, with resultant recruitment and activation of macrophages
and damage to follicles
3. Binding of antithyroid antibodies (antithyroglobulin, and antithyroid peroxidase antibodies),
followed by anti- body-dependent cell–mediated cytotoxicity
- A significant genetic component to the disease pathogenesis is supported by the
concordance of disease in as many as 40% of monozygotic twins, as well as the presence
of circulating antithyroid antibodies in approximately 50% of asymptomatic siblings of
affected patients
- Increased susceptibility to Hashimoto thyroiditis is associated with polymorphisms in
multiple immune regulation–associated genes, the most significant of which is the linkage
to cytotoxic T lymphocyte–associated antigen-4 gene (CTLA4), which codes for a negative
regulator of T cell function
Morphology
- The thyroid usually is diffusely and symmetrically enlarged
- The cut surface is pale and gray-tan in appearance, and the tissue is firm and somewhat friable.
- Microscopic examination reveals widespread infiltration of the parenchyma by a mononuclear
inflammatory infiltrate containing small lymphocytes, plasma cells, and well-developed germinal
centers
- The thyroid follicles are atrophic and are lined in many areas by epithelial cells distinguished by
the presence of abundant eosinophilic, granular cytoplasm, termed Hürthle, or oxyphil, cells.
- This is a metaplastic response of the normally low cuboidal follicular epithelium to ongoing
injury; on ultrastructural examination, the Hürthle cells are characterized by numerous prominent
mitochondria
- Interstitial connective tissue is increased and may be abundant
- Less commonly, the thyroid is small and atrophic as a result of more extensive fibrosis ( fibrosing
variant)
Subacute Granulomatous (de Quervain) Thyroiditis
- much less common than Hashimoto disease
- De Quervain thyroiditis is most common between the ages of 30 and 50 and, like other forms of
thyroiditis, occurs more frequently in women than in men
- Subacute thyroiditis is believed to be caused by a viral infection or an inflammatory process
triggered by viral infections
- A majority of patients have a history of an upper respiratory infection just before the onset of
thyroiditis
- By contrast with autoimmune thyroid disease, the immune response is not self-perpetuating, so
the process is limited.
Morphology
- The gland is firm, with an intact capsule, and may be unilaterally or bilaterally enlarged
- Histologic examination reveals disruption of thyroid follicles, with extravasation of colloid leading
to a polymorphonuclear infiltrate, which is replaced over time by lymphocytes, plasma cells, and
macrophages
- The extravasated colloid provokes an exuberant granulomatous reaction with giant cells, some
containing fragments of colloid.
- Healing occurs by resolution of inflammation and fibrosis
Page 70 of 269
Subacute Lymphocytic thyroiditis
- also is known as silent or painless thyroiditis
- in a subset of patients the onset of disease follows pregnancy (postpartum thyroiditis)
- This disease is most likely to be autoimmune in etiology, because circulating antithyroid
antibodies are found in a majority of patients
- mostly affects middle-aged women, who present with a painless neck mass or features of
thyroid hormone excess
- The initial phase of thyrotoxicosis (which is likely to be secondary to thyroid tissue damage) is
followed by return to a euthyroid state within a few months
- In a minority of affected persons the condition eventually progresses to hypothyroidism
- Except for possible mild symmetric enlargement, the thyroid appears normal on gross inspection
- The histologic features consist of lymphocytic infiltration and hyperplastic germinal centers within
the thyroid parenchyma
21.) Thyroid malignancies: staging and treatment
General
- the major concern in patients with palpable thyroid nodules is the possibility of a malignant
neoplasm
- benign neoplasms outnumber thyroid carcinomas by a ratio of nearly 10:1
- Morphologic examination by fine needle aspiration and surgical resection bears the most
information about the nodule
- neoplasms of the thyroid can be divided into adenomas, carcinomas and congenital
abnormalities
Adenomas
- typically discreet solitary masses, derived from follicular epithelium (=> follicular adenomas)
- Generally are not forerunners for carcinomas
- although the vast majority of adenomas are non-functional, a small fraction produce thyroid
hormones and produce clinically apparent thyrotoxicosis
Pathogenesis
- some are caused by somatic mutations of the TSH receptor signaling pathway
- => present in over half of toxic thyroid nodules
- in some, toxic multi nodular goiter is found
- a minority of non-functioning follicular adenomas have mutations of RAS or PIK3CA, which
encode a subunit of the PI-3 kinase, or bear a PAX8-PPARG fusion gene
- => genetic alterations they share with follicular carcinomas
Morphology
- solitary, spherical, encapsulated lesion
- demarcated from the surrounding thyroid parenchyma by a well-defined intact capsule
- => (make it distinct from multi nodular goiter, which contain multiple nodules)
- Average 3 cm in diameter, but they can grow to about 10 cm in diameter
- Color changes from grey-white to red-brown, depending on cellularity and colloid content
- areas of hemorrhage, fibrosis, calcification and cystic change are typical
Clinical picture
- many present as unilateral painless masses
- larger masses may produce local symptoms (like difficulty swallowing)
- On radionuclide scanning, nonfunctional nodules appear as cold nodules, relative to adjacent
thyroid tissue, because they take up Iess radioactive iodine than does normal parenchymal
tissue
- => about 10 % of cold nodules are malignant
- Follicular adenomas do not reoccur or metastasise and have an excellent prognosis
Page 71 of 269
Carcinomas
- account for approximately for 1,5% of cancers
- there is a female predominance
- the major subtypes are:
1. Papillary carcinoma ( 85%)
2. Follicular carcinoma (5-15%)
3. Anaplastic (undifferentiated) carcinoma (5%)
4. Medullary carcinoma (5%)
Pathogenesis
- medullary carcinoma are the ones that do not arise from follicular epithelium
- all 3 follicular derived malignancies are caused by genetic alterations of the growth factor
receptor singling pathways
Papillary Carcinoma
- most common form
- most often between the ages of 25 and 50
- Majority of thyroid carcinomas associated with previous exposure to ionising radiation
Morphology
- may be solitary of multifocal
- some are well circumscribed or even encapsulated, others infiltrate the adjacent parenchyma
and have ill-defined margins
- may contain areas of fibrosis and calcification and are often cystic
- They may con Tain branching papillae having a fibrovascular stalk covered by a single to m
multiple layers of cuboidal epithelial cells
- the nuclei of the cells contain finely dispersed chromatin, which imparts and optically clear or
empty appearance (groundglass or Orphan Annie eye nuclei)
- Invaginations of the cytoplasm may give the appearance of intranuclear inclusions
- Psamomma bodies (concentrically calcified structures)are often present, usually within the cores
of papillae (strong indicators for papillary carcinoma)
Clinical course
- most present as asymptomatic thyroid nodules, but the first manifestation may be a mass in a
cervical lymph node
- Interestingly, the presence of an isolated, cervical node metastasis does not have significant
influence on the prognosis
- Hoarseness, dysphagia, cough and dyspnea suggest an advanced stage
- Fine-needle aspiration analysis are a reliable tool for diagnosis
- They have an excellent prognosis, with a 10-year survival rate in excess of 95%
- 5-20% have local or regional reoccurrences and 5-10% have distant t metastases
Follicular Carcinoma
- more frequent in areas with dietary iodine deficiency , where they constitute 25- 45% of thyroid
cancers
- more common in women (3:1)
- peak incidence is between 40 and 60 years of age
Clinical course
- present as slowly enlarging painless nodules
- most often they are cold nodules oh scintigraphy
- but sometimes rare, better-differentiated lesions may be hyperfunctional and hot
- The prognosis largely depends on extend of invasion and stage of presentation
- it often presents with systemic metastases and about 50% of patients succumb to nthey disease
within 10 years
- Most are treated with a total thyroidectomy
Page 72 of 269
Anaplastic carcinoma
- Undifferentiated tumors of the thyroid follicular epithelium
- very aggressive, with a mortality rate reaching 100%
- mean age of 65
Clinical Picture
- usually present as a rapidly enlarging bulgy neck mass
- in most cases the carcinoma has already spread past the capsule into the neck or has
metastasised into the lungs
- there are symptoms related to infiltration and compression: dyspnea, dysphagia, hoarseness
and coughing
- there are no effective therapies
- in most cases, death occurs within 1 year
Medullary carcinoma
- derived from parafollicular cells (or C cells) of the thyroid
Staging
T1
Tumor < 2cm in greatest dimension, limited to the thyroid
T2
> 2cm but < 4cm in greatest dimension limited to the thyroid
T3
> 4cm limited to the thyroid or gross extrathyroidal extension invading only strap muscles
T4
Includes gross extrathyroidal extension into major neck structures
Treatment
- Most cancers are treated with removal of the thyroid gland (thyroidectomy)
- small tumors that have not spread outside the thyroid gland may be treated by just removing
the side of the thyroid containing the tumor (lobectomy)
- If lymph nodes are enlarged or show signs of cancer spread, they will be removed as well
- - it is important to identify the parathyroid glands, the recurrent laryngeal nerve and other vital
neck structures as to not cause damage to them
Thyroidectomy types
- Hemithyroidectomy—Entire isthmus is removed along with 1 lobe. Done in benign diseases of
only 1 lobe
- Subtotal thyroidectomy—Removal of majority of both lobes leaving behind 4-5 grams
(equivalent to the size of a normal thyroid gland) of thyroid tissue on one or both sides
- Partial thyroidectomy—Removal of gland in front of trachea after mobilization. Done in nontoxic
MNG
- Near total thyroidectomy—Both lobes are removed except for a small amount of thyroid tissue
(on one or both sides) in the vicinity of the recurrent laryngeal nerve entry point and the superior
parathyroid gland
- Total thyroidectomy—Entire gland is removed. Done in cases of papillary or follicular carcinoma
of thyroid, medullary carcinoma of thyroid. This is now also the most common operation for
multinodular goitre
Page 73 of 269
22.) Diseases of the parathyroid gland: Diagnosis and treatment
Hyperparathyroidism
- occurs in two major forms, primary and secondary, and, less commonly, as tertiary
hyperparathyroidism
- The first condition represents an autonomous, spontaneous overproduction of PTH, while the
latter two conditions typically occur as secondary phenomena in patients with chronic renal
insufficiency
Primary Hyperparathyroidism
- a common endocrine disorder, and an important cause of hypercalcemia
- The frequency of occurrence of the various parathyroid lesions underlying the hyperfunction is
as follows:
1. Adenoma—85% to 95%
2. Primary hyperplasia (diffuse or nodular)—5% to 10%
3. Parathyroid carcinoma—1%
- In more than 95% of cases, primary hyperparathyroidism is caused by a sporadic parathyroid
adenoma or sporadic hyperplasia
- The genetic defects identified in familial primary hyperparathyroidism include multiple endocrine
neoplasia syndromes, specifically MEN-1 and MEN-2A
- Familial hypocalciuric hypercalcemia is a rare cause of hyperparathyroidism, caused by
inactivating mutations in the calcium-sensing receptor gene on para- thyroid cells, leading to
constitutive PTH secretion
Morphology
- In 75% to 80% of cases, one of the parathyroids harbors a solitary adenoma, which, like the
normal parathyroids, may lie in close proximity to the thyroid gland or in an ectopic site (e.g., the
mediastinum)
- The typical parathyroid adenoma is a well- circumscribed, soft, tan nodule, invested by a
delicate capsule
- By definition, parathyroid adenomas are almost invariably confined to single glands
- Most parathyroid adenomas weigh between 0.5 and 5 g
- On microscopic examination, parathyroid adenomas are composed predominantly of chief cells
- In most cases, at least a few nests of larger oxyphil cells also are present
- A rim of compressed, non-neoplastic parathyroid tissue, generally separated by a fibrous
capsule, often is visible at the edge of the adenoma
- This finding constitutes a helpful internal control, since the chief cells of the adenoma are larger
and show greater nuclear size variability than that typical for the normal chief cells
- Cells with bizarre and pleomorphic nuclei are often seen within adenomas (so-called endocrine
atypia) and must not be taken as a sign of malignancy
- Mitotic figures are rare
- In contrast with the normal parathyroid parenchyma, adipose tissue is inconspicuous within
adenomas
Secondary Hyperparathyroidism
- caused by any condition associated with a chronic depression in the serum calcium level,
because low serum calcium leads to compensatory overactivity of the parathyroids
- Renal failure is by far the most common cause of secondary hyperparathyroidism
- The mechanisms by which chronic renal failure induces secondary hyperparathyroidism are
complex and not fully understood
- Chronic renal insufficiency is associated with decreased phosphate excretion, which in turn
results in hyperphosphatemia
- The elevated serum phosphate levels directly depress serum calcium levels and thereby stimulate parathyroid gland activity
Page 74 of 269
- In addition, loss of renal substances reduces the availability of α1-hydroxylase enzyme
necessary for the synthesis of the active form of vitamin D, which in turn reduces intestinal
absorption of calcium
Morphology
- The parathyroid glands in secondary hyperparathyroidism are hyperplastic
- As in the case of primary hyperplasia, the degree of glandular enlargement is not necessarily
symmetric
Parathyroid neoplasms
Parathyroid Hyperplasia
- typically a multiglandular process
- enlargement may be grossly apparent in only one or two glands, complicating the distinction
between hyperplasia and adenoma
- The combined weight of all glands rarely exceeds 1.0 g and often is less
- Microscopically, the most common pattern seen is that of chief cell hyperplasia, which may
involve the glands in a diffuse or multinodular pattern
- Less commonly, the constituent cells contain abundant clear cytoplasm as a consequence of
accumulation of glycogen
- => a condition designated “water- clear cell hyperplasia.”
- As in the case of adenomas, stromal fat is inconspicuous within foci of hyperplasia
Parathyroid carcinomas
- may be circumscribed lesions that are difficult to distinguish from adenomas, or they may be
clearly invasive neoplasms
- These tumors enlarge one parathyroid gland and consist of gray-white, irregular masses that
sometimes exceed 10 g in weight
- The cells usually are uniform and resemble normal parathyroid cells
- They are arrayed in nodular or trabecular patterns with a dense, fibrous capsule enclosing the
mass
- There is general agreement that a diagnosis of carcinoma based on cytologic detail is unreliable,
and invasion of surrounding tissues and metastasis are the only definitive criteria
- Local recurrence occurs in one third of cases, and more distant dissemination occurs in another
third
Treatment for Parathyroid tumors
1. Localized Parathyroid Cancer
- Surgery (en bloc resection)
- Surgery followed by radiation therapy.
- Radiation therapy
- Supportive care to treat hypercalcemia
2. Metastatic Parathyroid Cancer
- Surgery (metastasectomy) to remove cancer from the places where it has spread.
- Surgery followed by radiation therapy
- Radiation therapy
- Chemotherapy
- Supportive care to treat hypercalcemia
3. Recurrent Parathyroid cancer
- Surgery (metastasectomy) to remove cancer from the places where it has recurred.
- Surgery (tumor debulking)
- Surgery followed by radiation therapy.
- Radiation therapy
- Chemotherapy
- Supportive care to treat hypercalcemia
Page 75 of 269
23.) Benign tumors of the mammary gland: Precanceroses
Fibroadenomas
- common benign (non-cancerous) breast tumors made up of both glandular tissue and stromal
(connective) tissue
- most common in women in their 20s and 30s, but they can be found in women of any age.
- tend to shrink after a woman goes through menopause
- can often feel like a marble within the breast
- Some fibroadenomas are too small to be felt, but some are several inches across.
- tend to be round and have clear-cut borders
- You can move them under the skin and they’re usually firm or rubbery, but not tender
- Excised if suspicious
Phyllodes Tumors
- rare breast tumors that start in the connective (stromal) tissue of the breast
- Phyllodes tumors are most common in women in their 40s, but any age possible
- Women with Li-Fraumeni syndrome (a rare, inherited genetic condition) have an increased risk
for phyllodes tumors
- Most phyllodes tumors are benign, but about 1 out of 4 are malignant
Treatment
- Breast-conserving surgery (lumpectomy) is the main treatment
- Will recurr if not excised completely
- treated by taking out the tumor along with a margin of normal breast tissue around it
- Mastectomy may be needed if a cancer-free margin of normal breast tissue cannot be taken
out with the tumor
Intraductal Papillomas
- benign, wart-like tumors that grow within the milk ducts of the breast
- made up of gland tissue along with fibrovascular tissue
- Solitary papillomas (solitary intraductal papillomas) are single tumors that often grow in the
large milk ducts near the nipple
- They are a common cause of clear or bloody nipple discharge, especially when it comes from
only one breast
- may be felt as a small lump
- Papillomas may also be found in small ducts in areas of the breast farther from the nipple
- => In this case, there are often several growths (multiple papillomas)
- => less likely to cause nipple discharge
- In papillomatosis, there are very small areas of cell growth within the ducts, but they aren’t as
distinct as papillomas are.
- The usual treatment is surgery to remove the papilloma and the part of the duct it’s in
Granular cell tumors
- thought to start in early forms of nerve cells
- very rarely found in the breast
- Most granular cell tumors are found in the skin or the mouth, but they are uncommon even
in those places
- A granular cell tumor of the breast can most often be felt as a firm lump that you can move, but
some may be attached to the skin or chest wall
- They are most often are in the upper, inner part of the breast
- Granular cell tumors are usually removed along with a small margin (rim) of normal breast tissue
around them
24.) Breast cancer
Etiology and risk factors
- A large number of risk factors for breast cancer have been identified
Page 76 of 269
1. Age
- Risk steadily increases throughout life, especially after menopause, peaking at roughly 80 years
of age
- 75% of women with breast cancer are older than 50 years of age, and only 5% are younger than
40
2. Geographic Variations
- Surprising differences in the inci-dence and mortality rates of breast cancer have been reported
for various countries
- For example, the incidence and mortality rates are five times higher in the United States than in
Japan
- These differences seem to be environmental rather than genetic in origin, because migrants
from low-incidence to high-incidence areas tend to acquire the rates of their adoptive countries,
and vice versa
- Diet, reproductive patterns, and nursing habits are thought to be involved
3. Race/Ethnicity
- The highest rate of breast cancer is in non- Hispanic white women
- However, Hispanic and African American women tend to develop cancer at a younger age and
are more likely to develop aggressive tumors that present at an advanced stage
- Such disparities between ethnicities are an area of intense study and currently are thought to be
due to a combination of genetic differences and social factors, such as lifestyle choices and
access to health care.
4. Other Risk Factors
- Prolonged exposure to exogenous estrogens postmenopausally, as occurs with hormone
replace- ment therapy, has been proved to be useful for the prevention of osteoporosis
- relatively short-term use of combined estrogen plus progestin hormone therapy is associated
with an increased risk of breast cancer, diagnosis at a more advanced stage of breast cancer,
and higher incidence of abnormal mammogram
Pathogenesis
1. Genetic changes
- As with all cancers, mutations affecting proto-oncogenes and tumor suppressor genes in breast
epithelium underlie oncogenesis
- Among the best-characterized is overexpression of the HER2/NEU proto-oncogene
- Roughly one third of women with hereditary breast cancer have mutations in BRCA1 (at
chromosomal locus 17q21.3) or BRCA2 (located on chromosomal band 13q12-13)
2. Hormonal influences
- Many of the risk factors mentioned involve increased exposure to estrogen unopposed by progesterone
- Functioning ovarian tumors that elaborate estrogens are associated with breast cancer in
postmenopausal women
- Estrogens stimulate the production of growth factors, such as transforming growth factor-α,
platelet-derived growth factor, and fibroblast growth factor and others, which may promote tumor
development through paracrine and autocrine mechanisms
3. Environmental variables
- Environmental influences are suggested by the variable incidence of breast cancer in genetically
homogeneous groups and the geographic differences in prevalence, as discussed earlier
Page 77 of 269
Classification (WHO)
1. Epithelial tumors
- microinvasive carcinoma
2. Invasive breast carcinoma
- Invasive carcinoma of no special type (NST)
- Invasive lobular carcinoma
- Tubular carcinoma
- Cribiform carcinoma
- Mucinous carcinoma
- Metaplastic carcinoma of no special type
3. Papillary carcinomas
- Intraductal papillary carcinoma
- Encapsulated papillary carcinoma
- Solid papillary carcinoma
4. Mesenchymal tumors
- Myofibroblastoma
- Liposarcoma
- Angiosarcoma
- Rhabdomyosarcoma
- Osteosarcoma
- Leiomyoma
- Leiomyosarcoma
5. Malignant lymphomas
- Diffuse large B cell lymphoma
- Burkitt lymphoma
- T cell lymphoma
- Extranodal marginal-zone B cell lymphoma of MALT-type
- Follicular lymphoma
Diagnosis
- Breast cancer screening refers to testing otherwise-healthy women for breast cancer in an
attempt to achieve an earlier diagnosis under the assumption that early detection will improve
outcomes
- A number of screening tests have been employed including clinical and self breast exams,
mammography, genetic screening, ultrasound, and magnetic resonance imaging
1. Breast exam
- involves feeling the breast for lumps or other abnormalities
- Clinical breast exams are performed by health care providers, while self-breast exams are
performed by the person themselves
- Evidence does not support the effectiveness of either type of breast exam, as by the time
a lump is large enough to be found it is likely to have been growing for several years and
thus soon be large enough to be found without an exam
2. Mammography
- Mammographic screening for breast cancer uses X-rays to examine the breast for any
uncharacteristic masses or lumps
- During a screening, the breast is compressed and a technician takes photos from multiple
angles
- A general mammogram takes photos of the entire breast, while a diagnostic mammogram
focuses on a specific lump or area of concern
3. Genetic screening
4. Ultrasound
5. Magnetic resonance
Treatment
- depends on various factors, including the stage of the cancer and the age of the patient.
- Increasingly aggressive treatments are employed in accordance with the poorer the patient's
prognosis and the higher the risk of recurrence of the cancer following treatment
- usually treated with surgery, which may be followed by chemotherapy or radiation therapy, or
both
- A multidisciplinary approach is preferable
Page 78 of 269
- Hormone receptor-positive cancers are often treated with hormone-blocking therapy over
courses of several years
- Monoclonal antibodies, or other immune-modulating treatments, may be administered in
certain cases of metastatic and other advanced stages of breast cancer
Surgery
- Surgery involves the physical removal of the tumor, typically along with some of the surrounding
tissue
- One or more lymph nodes may be biopsied during the surgery
- increasingly the lymph node sampling is performed by a sentinel lymph node biopsy
1. Mastectomy (whole breast)
2. Quadrantectomy (one quarter of the breast)
3. Lumpectomy (smaller parts of the breast)
- Once the tumor has been removed, if the patient desires, breast reconstruction surgery, a type
of plastic surgery, may then be performed to improve the aesthetic appearance of the treated
site.
- Nipple prosthesis can be used at any time following the mastectomy
Staging of primary Tumor
T0
No evidence of primary tumor
TIS
Carcinoma in situ
T1
Tumor less than 2 cm
T1a
> 0,1 cm but < 0,5 cm
T1b
>0.5 cm but <1 cm
T1c
> 1 cm but < 2 cm
T2
> 2 cm but < 5 cm
T3
> 5 cm
T4
Extension to chest wall, inflammation,
satellite lesions, ulcerations
25.) Rare forms of mammary gland malignancies. Cancer of mammary gland in males.
Male breast cancer
- Breast cancer is about 1/150th as frequent in men as in women
- usually presents as a unilateral lump in the breast and is frequently not diagnosed promptly
- When male breast cancer is matched to female breast cancer by age and stage, its overall
prognosis is identical
- Although gynecomastia may initially be unilateral or asymmetric, any unilateral mass in a man
older than age 40 years should receive a careful workup including biopsy
- the risk of cancer is much greater in men with bilateral gynecomastia due to other causes
(endocrine, metabolic)
- in such men, gross asymmetry of the breasts should arouse suspicion of cancer
- Male breast cancer is best managed by mastectomy and axillary lymph node dissection or
SLNB
- Patients with locally advanced disease or positive nodes should also be treated with irradiation
- Approximately 90% of male breast cancers contain estrogen receptors, and approximately
60% of cases with metastatic disease respond to endocrine therapy
- The sites of relapse and spectrum of response to chemotherapeutic drugs are virtually identical
for breast cancers in either sex
Page 79 of 269
Inflammatory breast cancer
General
- rare disease, accounting for 1% to 5% of all invasive breast cancers
- a high grade aneuploid cancer, with mutations and overexpression of p53, high levels of Ecadherin and abnormal cadherin function
- the most aggressive form of breast cancer, with a five year survival rate of 40%
- Quick onset of symptoms is typical, the breast often looks swollen and red, or “inflamed”,
sometimes overnight, and are easy to misdiagnose as mastitis
Pathogenesis
- Invasion of the local lymphatic ducts impairs drainage and causes edematous swelling of the
breas
- Because the skin of the breast is tethered by the suspensory ligament of Cooper, the
accumulation of fluid may cause the skin of the breast to assume a dimpled appearance similar
to an orange peel (peau d'orange)
- A palpable tumor is frequently not obvious as in other forms of breast cancer
Symptoms
- Sudden swelling of the breast
- Skin changes on breast
- Reddened area with texture resembling the peel of an orange (peau d’orange)
- Nipple retraction (flattened look) or discharge
- Pain, itching in the breast
- Swelling of lymph nodes under the arm or in the neck
- Unusual warmth of the affected breast
- Breast is harder or firmer
Diagnosis
- The only reliable method of diagnosis is full-thickness skin biopsy
- Mammography, MRI or ultrasound often show suspicious signs; however in a significant
proportion of cases they would miss a diagnosis
- Clinical presentation is typical only in 50-75% of cases; and many other conditions such as
mastitis or even heart insufficiency can mimic the typical symptoms
Treatment
- The standard treatment for newly diagnosed inflammatory breast cancer is to receive systemic
therapy prior to surgery
- Achieving no disease in the surgical samples gives the best prognosis
- Surgery is modified radical mastectomy
- Lumpectomy, segmentectomy, or skin sparing mastectomy is not recommended. Immediate
reconstruction is not recommended
- Upfront surgery is contraindicated
- After surgery, all cases are recommended for radiation therapy unless it is contraindicated
Medullary breast cancer
- a rare subtype of invasive ductal carcinoma, accounting for about 3-5% of all cases of breast
cancer
- It is called “medullary” carcinoma because the tumor is a soft, fleshy mass that resembles a
part of the brain called the medulla
- It can occur at any age, but it usually affects women in their late 40s and early 50s
- Medullary carcinoma is more common in women who have a BRCA1 mutation
- Studies have shown that medullary carcinoma is also more common in Japan than in the
United States
- Medullary carcinoma cells are usually high-grade in their appearance and low-grade in their
behavior
- => they look like aggressive, highly abnormal cancer cells, but they don’t act like them
- Medullary carcinoma doesn’t grow quickly and usually doesn’t spread outside the breast to the
lymph nodes
- it’s typically easier to treat than other types of breast cancer
Page 80 of 269
Mucinous breast cancer
- a rare form of invasive ductal carcinoma
- the tumor is made up of abnormal cells that “float” in pools of mucin
- mucin becomes part of the tumor and surrounds the breast cancer cells.
- only about 2-3% of invasive breast cancers are “pure” mucinous carcinomas
- Although it can be diagnosed at any age, it tends to affect women after they’ve gone through
menopause
- Some studies have found that the average age at diagnosis is in the 60s or early 70s
- Even though mucinous carcinoma is an invasive breast cancer, it tends to be a less aggressive
type that responds well to treatment
- Mucinous carcinoma is less likely to spread to the lymph nodes than other types of breast
cancer
Tubular breast cancer
- Tubular carcinomas are usually small (about 1 cm or less) and made up of tube-shaped
structures called "tubules."
- These tumors tend to be low-grade, meaning that their cells look somewhat similar to normal,
healthy cells and tend to grow slowly
- At one time, tubular carcinomas accounted for about 1-4% of all breast cancers
- Now that screening mammography is widely used, however, tubular carcinomas are being
diagnosed more frequently
- studies suggest that tubular carcinomas may account for anywhere from just under 8% to 27%
of all breast cancers
- Studies also suggest that the average age of diagnosis for tubular carcinoma is the early 50s,
although women can be diagnosed with it at any age
- Even though tubular carcinoma is an invasive breast cancer, it tends to be a less aggressive
type that responds well to treatment
- It isn't likely to spread outside the breast and is considered to have a very good prognosis
Adenoid cystic carcinoma
- a rare special subtype of breast cancer characterized by the presence of a dual cell population
of luminal and basaloid cells arranged in specific growth patterns
- Most breast cancers with triple-negative, basal-like breast features (i.e., tumors that are devoid
of estrogen receptor, progesterone receptor, and human epidermal growth factor receptor 2
expression, and express basal cell markers) are generally high-grade tumors with an aggressive
clinical course
- Conversely, while ACCs also display a triple-negative, basal-like phenotype, they are usually
low-grade and exhibit an indolent clinical behavior
Metaplastic breast cancer
- a heterogeneous group of cancers that exhibit varied patterns of metaplasia and differentiation
along multiple cell lines
- This rare and aggressive form of breast cancer is characterized as being composed of a mixed
group of neoplasms containing both glandular and non-glandular patterns with epithelial and/or
mesenchymal components
- accounts for fewer than 1% of all breast cancer diagnoses
- It is most closely associated with invasive ductal carcinoma of no special type. (IDC), and
shares similar treatment approaches
- Relative to IDC, MCB generally has higher histological grade and larger tumor size at time of
diagnoses, but a lower incidence of axillary lymph node involvement
- MCB tumors are typically estrogen receptor (ER), progesterone receptor (PR), and human
epidermal growth factor-2 (HER-2) negative, meaning hormone therapy is generally not an
effective treatment option, which correlates to a relatively poor prognosis
- treatment options are standard with other breast cancers
- If the tumor is diagnosed early, breast-saving surgery could be an option, although this is
relatively uncommon
- In non-metastatic MCB, the most common treatment is mastectomy
- If the tumor is metastatic, surgery is no longer a viable option, and treatment generally defaults
to aggressive chemotherapy
Page 81 of 269
Lymphoma of the breast
- Lymphoma of the breast is uncommon whether it is primary or secondary
- Constitutes 0.04 - 0.05% of malignant breast neoplasms
- Most breast lymphomas are of B cell origin
- The most frequent mode of presentation is a painless breast mass
- Treatment can include surgery, chemotherapy, and radiation
Phyllodes tumors
- are typically large, fast-growing masses that form from the periductal stromal cells of the breast
- They account for less than 1% of all breast neoplasms
- predominantly a tumor of adult women, with very few examples reported in adolescents
- Patients typically present with a firm, palpable mass
- These tumors are very fast-growing, and can increase in size in just a few weeks
- Occurrence is most common between the ages of 40 and 50, prior to menopause
- The common treatment for phyllodes is wide local excision
- Other than surgery, there is no cure for phyllodes, as chemotherapy and radiation therapy are
not effective
- The risk of developing local recurrence or metastases is related to the histologic grade,
according to the above-named features
- Despite wide excision, a very high percentage of surgeries yielded incomplete excision margins
that required revision surgery
- Radiation treatment after breast-conserving surgery with negative margins may significantly
reduce the local recurrence rate for borderline and malignant tumors
26.) Chest injuries: types - diagnosis and treatment
General
- Chest injuries most often affect the ribs, upper part of the abdomen, lungs, blood vessels,
heart, muscles, soft tissues, and breastbone
- Sometimes the esophagus, collarbone, or shoulder blade is also injured.
- In the United States, chest injuries cause about 25% of deaths due to severe injury
- Many of the injuries that can cause death during the first minutes or hours after injury can be
treated or stabilized in the emergency department without the need for major surgery
Etiology
- The chest can be injured by blunt force (such as in motor vehicle crashes, falls, or sports
injuries) or by an object that penetrates it (such as a bullet or knife)
- Chest injuries are often serious or immediately life threatening because they interfere with
breathing or circulation
- Some injuries damage the ribs and chest wall severely enough to make it difficult for the lungs
to inflate normally
- Damage to the lungs themselves interferes with gas exchange
- Chest injuries can cause circulatory problems if they result in a lot of bleeding
- Bleeding is often inside the chest wall, which also interferes with breathing
- Also, injury to the heart can affect circulation by interfering with the heart's ability to pump
blood to the body
Most important
1. Blunt injury to the heart
- a blow to the chest that bruises the heart muscle, tears (ruptures) the heart's walls, or
damages a heart valve
2. Cardiac tamponade
- pressure on the heart by blood or fluid that accumulates in the two-layered sac around the
heart (pericardium)
3. Hemothorax
- an accumulation of blood between the lung and the chest wall
4. Pulmonary contusion
5. Rib fractures
6. Injury to the aorta
- can be partially or completely torn by severe blunt force to the chest
Page 82 of 269
7. Traumatic pneumothorax
- when air accumulates between the chest wall and the lung because of an injury
- causes the lung to collapse partially or completely
Diagnosis
1. Blunt injury to the heart
- an ECG is usually done to check for abnormal heart rhythms
- Sometimes doctors also check the blood for serum markers released by the damaged
heart
- Echocardiography may show abnormalities in the way the heart's walls move. It may also
show blood or fluid around the heart, or rupture of a heart wall, or damage to a heart valve
2. Cardiac tamponade
- Prompt diagnosis and treatment are essential because cardiac tamponade can be rapidly
fatal
- The diagnosis is based on symptoms, examination results, and usually echocardiography.
- => is usually done to confirm the diagnosis
3. Hemothorax
- If doctors suspect hemothorax, they take a chest x-ray
4. Pulmonary contusion
- a bruise of a lung, which causes bleeding and swelling
5. Rib fractures
- suspect rib fracture when one or more ribs are very tender in one particular spot
- Sometimes you can feel the broken ribs when they gently push the injured area
- do not always need to confirm rib fractures with an x-ray because the presence of rib
fractures does not change the way a chest injury is treated
- Nonetheless, doctors usually do a chest x-ray to detect serious problems that can
accompany rib fractures, such as a bruised or collapsed lung
- Not all rib fractures can be seen on a chest x-ray
6. Injury to the aorta
- A chest x-ray is required for anyone who has had a chest injury
- a tear in the aorta may not be seen on a chest x-ray, and overlooking this injury may have
serious consequences
- Thus, other imaging tests, such as computed tomography (CT) angiography,
echocardiography, ultrasonography, or aortography are often done when severe chest
injuries are caused by a high-speed motor vehicle crash or a fall from a height
7. Traumatic pneumothorax
- based on a chest x-ray
- Sometimes pneumothorax is diagnosed when CT or ultrasonography is done to diagnose
other chest or abdominal injuries
Treatment
1. Blunt injury to the heart
- People with an abnormal heart rhythm are kept in the hospital for monitoring because the
abnormal heart rhythm may suddenly become serious.
- If a blunt injury to the heart causes other problems (such as heart failure or a damaged
heart valve), people are admitted to the hospital, and the problem is treated.
- People who collapse after a blunt blow to the chest must be evaluated immediately to see
if they are in cardiac arrest
- If they are in cardiac arrest, cardiopulmonary resuscitation is started as soon as possible
and an automated external defibrillator (AED) is used if available
- About 35% of people who are treated with an AED survive.
- Several measures may help prevent commotio cordis
Page 83 of 269
- They include teaching players ways to protect themselves (certain defensive strategies),
using chest protectors and softer baseballs, and having AEDs and trained emergency
medical personnel at youth sporting events
2. Cardiac tamponade
- is a medical emergency
- Doctors treat it immediately by using a needle to remove the blood or fluid from around the
heart (pericardiocentesis)
- => relieves pressure on the heart and enables it to beat normally
- Sometimes pericardiocentesis fails to remove enough fluid.
- => make an incision into the chest wall (thoracotomy) and then the pericardium
(pericardiotomy) to drain the fluid
- You may also need to remove part of the pericardium (pericardiectomy)
3. Hemothorax
- give fluids intravenously to increase the amount of fluid in the bloodstream and thus
increase blood pressure
- If a large amount of blood has been lost, a blood transfusion is necessary.
- insert a chest tube (thoracostomy) into the chest to remove the blood and to allow the lung
to reinflate
- => The tube may need to remain in place for several days.
- If a lot of blood is present or if bleeding continues, surgery (thoracotomy) may be done to
stop the bleeding
4. Pulmonary contusion
- suspect a pulmonary contusion when people become short of breath after a chest injury,
especially if shortness of breath develops gradually.
- A chest x-ray is taken
- because a contusion may develop gradually, doctors may take more than one x-ray over a
period of many hours to detect a contusion
- also measure the amount of oxygen in the blood by attaching a device to a finger or toe
(pulse oximeter)
- => helps to determine how well the lungs are functioning
5. Rib fractures
- Patients with rib fractures are given pain relievers (analgesics)
- Those with severe pain are usually given opioid pain relievers such as oxycodone or
hydrocodone
- Sometimes hospitalized patients who have severe pain are treated by numbing the nerve
to the affected ribs or with injection of drugs around the spinal cord (epidural analgesia).
- Patients with a rib fracture are asked to cough or breathe deeply about once an hour while
they are awake to keep the air sacs in the lung open and prevent pneumonia
- Patients with flail chest often need to have their breathing supported with a ventilator until
the injuries heal
6. Injury to the aorta
- The first priority is to control the person's heart rate and blood pressure.
- If blood pressure and heart rate are high, a tear can become worse, sometimes causing
the aorta to burst
- Drugs, such as beta-blockers, can help control both
- Other measures that may help can include giving pain relievers, trying to keep the person
calm, and refraining from doing procedures that may cause gagging or vomiting
- After heart rate and blood pressure are controlled, surgery is done to repair the tear
- Sometimes doctors place a mesh tube (stent) into the aorta to cover the tear
7. Traumatic pneumothorax
- The goal of treatment is to remove the air from the pleural space and allow the lung to
reinflate.
- Usually, a tube (thoracostomy or chest tube) is inserted into the chest between two ribs
- The tube is attached to a suction device to remove the air and to allow the lung to reinflate
Page 84 of 269
- the procedure can be done using only a local anesthetic
27.) Bronchiectasis: Pulmonary abcess and pulmonary gangrene
General
- a disease in which there is permanent enlargement of parts of the airways of the lung
- Symptoms typically include a chronic cough productive of mucus
- Other symptoms include shortness of breath, coughing up blood, and chest pain
- Wheezing and nail clubbing may also occur
- may result from a number of infective and acquired causes, including pneumonia, tuberculosis,
immune system problems, and cystic fibrosis
- Cystic fibrosis eventually results in severe bronchiectasis in nearly all cases
- The mechanism of disease is breakdown of the airways due to an excessive inflammatory
response
- Involved airways (bronchi) become enlarged and thus less able to clear secretions
- These secretions increase the amount of bacteria in the lungs, result in airway blockage and
further breakdown of the airways
- It is classified as an obstructive lung disease, along with chronic obstructive pulmonary disease
and asthma
- The diagnosis is suspected based on a person's symptoms and confirmed using computed
tomography
Etiology
- can arise from infectious or noninfectious causes
- Clues to the underlying etiology are often provided by the pattern of lung involvement
- Focal bronchiectasis refers to bronchiectatic changes in a localized area of the lung and can be
a consequence of obstruction of the airway
- => either extrinsic (e.g. due to compression by adjacent lymphadenopathy or parenchymal
tumor mass) or intrinsic (e.g. due to an airway tumor or aspirated foreign body, a scarred/
stenotic airway or bronchial atresia from congenital underdevelopment of the airway)
- Diffuse bronchiectasis is characterized by widespread bronchiectatic changes throughout the
lung and often arises from an underlying systemic or infectious disease process
- More pronounced involvement of the upper lung fields is most common in cystic fibrosis (CF)
and is also observed in postradiation fibrosis corresponding to the lung region encompassed
by the radiation port
- Bronchiectasis with predominant involvement of the lower lung fields usually has its source in
chronic recurrent aspiration (e.g. due to esophageal motility disorders like those in
scleroderma), end stage fibrotic lung disease (e.g traction bronchiectasis from idiopathic
pulmonary fibrosis) or recurrent immunode ciency-associated infections (e.g.
hypogammaglobulinemia)
- In many cases the etiology of bronchiectasis is not determined.
- In case series as many as 25-50% of patients referred for bronchiectasis have idiopathic
disease
Pathogenesis
- "vicious cycle hypothesis”
- => susceptibility to infection and poor mucociliary clearance result in microbial colonization of
the bronchial tree
- Some organisms such as Pseudomonas aeruginosa exhibit a particular propensity for
colonizing damaged airways and evading host defense mechanisms
- Impaired mucociliary clearance can result from inherited conditions such as CF or dyskinetic
cilia syndrome and it has been proposed that a single severe infection (e.g. pneumonia caused
by Bordetella pertussis or Mycoplasma pneu moniae) can result in significant airway damage
and poor secretion clearance
- The presence of the microbes incites continued chronic inflammation with consequent damage
to the airway wall continued impairment of secretion and microbial clearance and ongoing
propagation of the infectious/inflammatory cycle
- Moreover it has been proposed that mediators released directly from bacteria can interfere with
mucociliary clearance
Page 85 of 269
Clinical Manifestation
- a persistent productive cough with ongoing production of thick tenacious sputum
- Physical findings often include crackles and wheezing on lung auscultation and some patients
with bronchiectasis exhibit clubbing of the digits
- Mild to moderate air flow obstruction is often detected on pulmonary function tests,
overlapping with that seen at presentation with other conditions such as chronic obstructive
pulmonary disease (COPD)
- Acute exacerbations of bronchiectasis are usually characterized by changes in the nature of
sputum production with increased volume and purulence
- typical signs and symptoms of lung infection such as fever and new infilltrates may not be
present
Diagnosis
- usually based on presentation with a persistent chronic cough and sputum production
accompanied by consistent radiographic features
- Although chest radiographs lack sensitivity, the presence of "tram tracks" indicating dilated
airways is consistent with bronchiectasis
- Chest computed tomography (CT) is more specific for bronchiectasis and is the imaging
modality of choice for confirming the diagnosis
- CT findings include airway dilation (detected as parallel "tram tracks" or as the “signet-ring
sign"-a cross-sectional area of the airway with a diameter at least 1.5 times that of the adjacent
vessel), lack of bronchial tapering,bronchial wall thickening in dilated airways or cysts
emanating from the bronchial wall
Treatment
Antibiotic treatment
- Antibiotics targeting the causative or presumptive pathogen (with Haemophilus influenzae and
P. aeruginosa isolated commonly) should be administered in acute exacerbation
- => usually for a mini mum of 7-10 days and perhaps for as long as 14 days
- Decisions about treatment of NTM infection can be difficult, given that these organisms can be
colonizers as well as pathogens and the prolonged treatment course often is not well tolerated.
- MAC strains are the most common NTM pathogens and the recommended regimen for HIVnegative patients includes a macrolide combined with rifampin and ethambutol
- Consensus guidelines also recommend macrolide susceptibility testing for clinically significant
MAC isolate
Bronchial Hygiene
- The numerous approaches used to enhance secretion clearance in bronchiectasis include
hydration and mucolytic administration, aerosolization of bronchodilators and hyperosmolar
agents (e.g. hypertonic saline) and chest physiotherapy (e.g. postural drainage, traditional
mechanical chest percussion via hand clapping to the chest or use of devices such as an
oscillatory positive expiratory pressure flutter valve or a high-frequency chest wall oscillation
vest)
- Pulmonary rehabilitation and a regular exercise program may assist with secretion clearance as
well as with other aspects of bronchiectasis, including improved exercise capacity and quality
of life. The mucolytic dornase (DNase) is recommended routinely in CF-related bronchiectasis
but not in non-CF bronchiectasis, given concerns about lack of efficacy and potential harm in
the non-CF population
Anti-inflammatory therapy
- control of the inflammatory response may be of benefit in bronchiectasis
- relatively small-scale trials have yielded evidence of alleviated dyspnea, decreased need for
inhaled ß-agonists and reduced sputum production with inhaled glucocorticoids
- However, no significant differences in lung function or bronchiectasis exacerbation rates have
been observed
- Risks of immunosuppression and adrenal suppression must be carefully considered with use of
anti-inflammatory therapy in infectious bronchiectasis
- administration of oral/systemic glucocorticoids may be important in treatment of
bronchiectasis due to certain etiologies, such as ABPA or of noninfectious bronchiectasis due
Page 86 of 269
to underlying conditions, especially that in which an autoimmune condition is believed to be
active (e.g. rheumatoid arthritis or Sjögren's syndrome)
- Patients with ABPA may also benefit from a prolonged course of treatment with the oral
antifungal agent itraconazole.
Pulmonary abscess
- a type of liquefactive necrosis of the lung tissue and formation of cavities (more than 2 cm)
containing necrotic debris or fluid caused by microbial infection
- This pus-filled cavity is often caused by aspiration, which may occur during anesthesia,
sedation, or unconsciousness from injury
- Alcoholism is the most common condition predisposing to lung abscesses
Symptoms
- Onset of symptoms is often gradual, but in necrotizing staphylococcal or gram-negative
bacillary pneumonias patients can be acutely ill
- =>Cough, fever with shivering, and night sweats are often present
- => Cough can produce foul smelling purulent mucus (≈70%) or less frequently blood I
- Affected individuals may also complain of chest pain, shortness of breath, lethargy and other
features of chronic illness
- Those with a lung abscess are generally cachectic at presentation
- Finger clubbing is present in one third of patients
- Dental decay is common especially in alcoholics and children
- On examination of the chest there will be features of consolidation such as localized dullness
on percussion and bronchial breath sounds
Diagnosis
1. Imaging
- often on one side and single involving posterior segments of the upper lobes and the
apical segments of the lower lobes as these areas are gravity dependent when lying down.
Presence of air-fluid levels implies rupture into the bronchial tree or rarely growth of gas
forming organism
- Fiber optic bronchoscopy is often performed to exclude obstructive lesion; it also helps in
bronchial drainage of pus
2. Lab studies
- Raised inflammatory markers (high ESR, CRP) are common but nonspecific
- Examination of the coughed up mucus is important in any lung infection and often reveals
mixed bacterial flora
- Transtracheal or transbronchial (via bronchoscopy) aspirates can also be cultured
Treatment
- Broadspectrum antibiotic to cover mixed flora is the mainstay of treatment
- Pulmonary physiotherapy and postural drainage are also important
- Surgical procedures are required in selective patients for drainage or pulmonary resection
Pulmonary gangrene
- A Putrefactive Necrosis of the Lung, either circumscribed or diffuse
Etiology
- Gangrene of the lung can only occur where the organ has previously been weakened, hence is
always a secondary affection
- Putrefactive bacteria thrive in the necrotic soil
- may follow lobar pneumonia, aspiration-pneumonia, broncho-pneumonia, fetid bronchitis,
thrombosis of the pulmonary artery, rupture of a bronchus, from an ulcerated or cancerous
esophagus, from pressure due to tumors or thoracic aneurism, and from sepsis due to
protracted adynamic fevers
Page 87 of 269
Symptoms
- In addition to the symptoms of the primary disease, the cough becomes more pronounced, and
is attenuated by profuse expectoration
- The respiration is slightly increased in frequency, and the breath is offensive
- Where erosion of the blood-vessels occurs, hemorrhages take place
- There is some fever present in all cases; the patient loses flesh and strength, becomes anemic,
chills and night-sweats follow, and the evidence of sepsis is pronounced
- There is dullness on percussion in the earlier stages, followed by the sign of cavity formation in
later stages
Diagnosis
- A complete cell count and biochemistry is mandatory
- Elevated white blood cells with shift- to-left usually indicates for systemic inflammation or
infection
- C-reactive protein, erythrocyte sedimentation rate and procalcitonin are also useful infection
indicators
- When systemic infection is severe and non-pulmonary origins can be reasonably excluded,
gangrenous changes, a form of the most severe lung infection and tissues decomposition,
should be kept in mind as one of the differential diagnosis
- Blood culture is obtained if bacteremia is likely and serology test will be useful in some
instances of infection
- Bronchoscopy is a useful tool to help evaluate the condition of trachea and bronchus
- Imaging: Chest radiograph, Angiography, CT, Nuclear imaging
Treatment
1. Medical
- The goals of medical treatment is to control both local and systemic infection, preventing
occurrence of SIRS and septic shock
- Administration of broad-spectrum of antibiotics, proper fluid replacement therapy, steroid
therapy
- Empiric antibiotics should be modified according to culture results
- When patient's response is poor despite aggressive medical treatment, consider surgical
evaluation
- after aggressive medical treatment for 48 hrs, surgical evaluation is to be expected to
prevent bilateral involvement of necrotizing pneumonia and unavoidable lethal outcome
- If patient's condition become stablized and the infected lung was only confined locally,
resection of the local infection can be either delayed or deemed unnecessary depending
on infection control
2. Surgery
- Adequate timing of surgical intervention isn't easy to determine because gangrenous
changes of lung are often accompanied by pleural infection including empyema thoracis
and chest wall infection
- Resection of lung, division of pulmonary vessels and bronchus in an infected pleural space
is risky for postoperative bleeding, prolonged air leaks due to bronchial rupture and
persistent pleural infection
- A two-stage approach had been proposed a reasonable strategy
- With concomitant pleural space infection, tube thoracostomy to allow drainage of purulent
pleural effusion or thoracoscopic deloculation and decortication to help cleaning of pleural
space and prepare for subsequent lung resection
- infection may be overwhelming in some situations and surgical intervention is emergent
- The most appropriate timing should be judged
- If tube thoracostomy failed to alleviate systemic infection, prompt surgical intervention
should be started
- If bronchial or vascular structure is fragile and necrotic, pleural or muscle flap may be
considered during operation
- Extent of resection is according to the involved lung tissues with normal lung spared
Page 88 of 269
28.) Pulmonary cysts
Bronchogenic cysts
- Bronchogenic cysts are small, solitary cysts or sinuses
- typically located in the region of the suprasternal notch or over the manubrium
Pathology
- formed in the 6th week of gestation from an abnormal budding of the tracheal diverticulum
- lined by respiratory type (ciliated) epithelium, which is characterized by cilia
- Histologically these are also composed of cartilage, smooth muscle, fibrous tissue and mucous
glands
- These cysts originate from the ventral foregut that forms the respiratory system
- located close to the trachea or main stem bronchi
- Rarely there is communication of the cyst with the tracheobronchial tree
Clinical features
- found most often in young adults and are rare in infancy
- The usual symptoms are the result of compression by the cyst, e.g., difficulty breathing or
swallowing, cough, and chest pain
- Malignant degeneration has been reported in these cysts on rare occasions
- Chest x-rays show a smooth density just in front of the trachea or main stem bronchi at the
carinal level
- When the cyst communicates with the tracheobronchial tree, the air-fluid level may be seen
within the cyst
- CT scanning is useful in localizing these cysts
Treatment
1. Excision (definitive diagnosis and cure)
2. Biopsy (definitive diagnosis with less surgical risk)
3. Observation
- minimal risk from the intervention, but carries some risk of bleeding or infection of the cyst
at a later time, making excision more difficult if it occurs
Lymphangioleiomyomatosis
- a rare, progressive and systemic disease
- typically results in cystic lung destruction
- predominantly affects women, especially during childbearing years
- The term sporadic LAM is used for patients with LAM not associated with tuberous sclerosis
complex (TSC), while TSC-LAM refers to LAM that is associated with TSC
- The average age of onset is the early to mid 30s
- Exertional dyspnea (shortness of breath) and spontaneous pneumothorax (lung collapse) have
been reported as the initial presentation of the disease in 49% and 46% of patients
- Diagnosis is typically delayed 5 to 6 years
- The condition is often misdiagnosed as asthma or chronic obstructive pulmonary disease
Other symptoms
- Fatigue
- Cough
- Hemoptysis (rarely massive)
- Chest pain
- Chylous complications arising from lymphatic obstruction, including
•
Chylothorax
•
Chylous ascites
•
Chylopericaridium
•
Chyloptysis
•
Chyluria
•
Chyle in vaginal discharge
•
Chyle in stool
Page 89 of 269
Etiology
- LAM occurs in two settings: in the disease tuberous sclerosis complex (TSC-LAM) and in a
sporadic form, in women who do not have TSC (sporadic LAM)
- In both settings, genetic evidence indicates that LAM is caused by inactivating or “loss of
function” mutations in the TSC1 or TSC2 genes
Pathophysiology
- A variable percentage of cells within the LAM lesion contain mutational inactivation of the
Tuberous Sclerosis Complex (TSC1 or TSC2) tumor suppressor genes
- TSC1 and TSC2 form a tumor suppressor complex that regulates mammalian target of
rapamycin (mTOR) signaling complex by directly controlling the activity of the small GTPase
Rheb via the GTPase activating protein (GAP) domain of TSC2
- Rheb binds to Raptor and controls the activity of mTOR complex 1 (mTORC1) that directly
phosphorylates p70 S6 kinase (S6K1) and 4E-BP1
- Loss of TSC1/TSC2 in LAM induces uncontrolled LAM cell growth and increases LAM cell
viability
- Upregulation of STAT1 and STAT3 and autophagy are known mediators of LAM cell viability and
survival
- LAM cells behave, in many ways, like metastatic tumor cells
- => appear to arise from an extrapulmonary source and migrate to the lung.
- => The cellular and molecular mechanisms of neoplastic transformation and lung parenchymal
destruction by LAM cells remain unknown
Diagnosis
- LAM can come to medical attention in several ways, most of which trigger a chest CT
- Thin-walled cystic change in the lungs may be found incidentally on CT scans of the heart,
chest or abdomen (on the cuts that include lung bases) obtained for other purposes
- HRCTs of TSC patients reveals that about 20% of women have cystic change by age 20 and
about 80% of women have cystic changes after age 40
- LAM is sometimes revealed by chest CT in patients who present with an apparent primary
spontaneous pneumothorax, but more often CT scanning is not ordered until recurrences occur
- Progressive dyspnea on exertion without the exacerbations and remissions that are
characteristic of asthma or COPD sometimes prompt a chest CT
Treatment
- An FDA-approved drug for treatment of LAM, sirolimus, is available for stabilization of lung
function decline
- Lung transplant remains the last resort for patients with advanced disease
29.) Pneumothorax (see also question 39)
General
- the presence of gas in the pleural space
- A spontaneous pneumothorax is one that occurs without antecedent trauma to the thorax
- A primary spontaneous pneumothorax occurs in the absence of underlying lung disease,
whereas a secondary pneumothorax occurs in its presence
- A traumatic pneumothorax results from penetrating or nonpenetrating chest injuries
- A tension pneumothorax is a pneumothorax in which the pressure in the pleural space is
positive throughout the respiratory cycle
Primary Spontaneous Pneumothorax
- are usually due to rupture of apical pleural blebs
- => small cystic spaces that lie within or immediately under the visceral pleura
- occur almost exclusively in smokers; this suggests that these patients have subclinical lung
disease
- Approximately one-half of patients with an initial primary spontaneous pneumothorax will have
a recurrence
Page 90 of 269
- The initial recommended treatment for primary spontaneous pneumothorax is simple aspiration.
If the lung does not expand with aspiration or if the patient has a recurrent pneumothorax,
thoracoscopy with stapling of blebs and pleural abrasion is indicated
- Thoracoscopy or thoracotomy with pleural abrasion is almost 100% success l in preventing
recurrences.
Secondary Pneumothorax
- Most are due to chronic obstructive pulmonary disease, but pneumothoraxes have been
reported with virtually every lung disease
- in patients with lung disease it is more life-threatening than it is in normal individuals because
of the lack of pulmonary reserve in these patients
- Nearly all patients with secondary pneumothorax should be treated with tube thoracostomy
- Most should also be treated with thoracos copy or thoracotomy with the stapling of blebs and
pleural abrasion
- If the patient is not a good operative candidate or refuses surgery, pleurodesis should be
attempted by the intrapleural injection of a sclerosing agent such as doxycycline
Traumatic pneumothorax
- can result from both penetrating and nonpenetrating chest trauma
- Traumatic pneumothoraxes should be treated with tube thoracostomy unless they are very
small
- If a hemopneumothorax is present, one chest tube should be placed in the superior part of the
hemithorax to evacuate the air and another should be placed in the inferior part of the
hemithorax to remove the blood
- Iatrogenic pneumothorax is a type of traumatic pneumothorax that is becoming more common
- The leading causes are transthoracic needle aspiration, thoracentesis and the insertion of
central intravenous catheters
- Most can be managed with supplemental oxygen or aspiration, but if these measures are
unsuccessful a tube thoracostomy should be performed
Tension Pneumothorax
- usually occurs during mechanical ventilation or resuscitative efforts
- The positive pleural pressure is life-threatening both because ventilation is severely
compromised and because the positive pressure is transmitted to the mediastinum resulting in
decreased venous return to the heart and reduced cardiac output.
- Difficulty in ventilation during resuscitation or high peak inspiratory pressures during
mechanical ventilation strongly suggest the diagnosis
- diagnosis is made by physical examination showing an enlarged hemithorax with no breath
sounds, hyperresonance to percussion and shift of the mediastinum to the contralateral side
- Tension pneumothorax must be treated as a medical emergency
- If the tension in the pleural space is not relieved the patient is likely to die from inadequate
cardiac output or marked hypoxemia
- A large-bore needle should be inserted into the pleural space through the second anterior
intercostal space
- If large amounts of gas escape from the needle after insertion the diagnosis is confirmed
- The needle should be left in place until a thoracostomy tube can be inserted
30.) Hydatid pulmonary cyst- echinococcosis
General
- Echinococcosis, also called hydatid disease, hydatidosis, or echinococcal disease
- a parasitic disease of tapeworms of the Echinococcus type
- The two main types of the disease are cystic echinococcosis and alveolar echinococcosis
- Less common forms include polycystic echinococcosis and unicystic echinococcosis
- The disease often starts without symptoms and this may last for years
Page 91 of 269
Classification
1. cystic echinococcosis (also known as unilocular echinococcosis)
- The most common form found in humans
- caused by Echinococcus granulosus sensu lato
2. alveolar echinococcosis
- The second most common form is alveolar echinococcosis
- also known as alveolar colloid of the liver, alveolar hydatid disease, alveolococcosis,
multilocular echinococcosis, "small fox tapeworm“
- caused by Echinococcus multilocularis
3. polycystic echinococcosis
- also known as human polycystic hydatid disease or neotropical echinococcosis
- caused by Echinococcus vogeli and very rarely, Echinococcus oligarthrus.
- alveolar and polycystic echinococcosis are rarely diagnosed in humans and are not as
widespread as cystic echinococcosis
- but polycystic echinococcosis is relatively new on the medical scene and is often left out
of conversations dealing with echinococcosis
- alveolar echinococcosis is a serious disease that has not only a significantly high fatality
rate, but the potential to become an emerging disease in many countries
Signs and Symptoms
- In the human manifestation of the disease, E. granulosus, E. multilocularis, E. oligarthrus and
E. vogeli are localized in the liver (in 75% of cases), the lungs (in 5–15% of cases) and other
organs in the body such as the spleen, brain, heart, and kidneys (in 10–20% of cases)
- Depending on the location of the cyst in the body, the patient could be asymptomatic even
though the cysts have grown to be very large, or be symptomatic even if the cysts are
absolutely tiny
- If the patient is symptomatic, the symptoms will depend largely on where the cysts are located
- => For instance, if the patient has cysts in the lungs and is symptomatic, they will have a
cough, shortness of breath and/or pain in the chest
- => if the patient has cysts in the liver and is symptomatic, they will suffer from abdominal pain,
abnormal abdominal tenderness, hepatomegaly with an abdominal mass, jaundice, fever and/
or anaphylactic reaction
- In addition, if the cysts were to rupture while in the body, whether during surgical extraction of
the cysts or by trauma to the body, the patient would most likely go into anaphylactic shock
and suffer from high fever, pruritus (itching), edema (swelling) of the lips and eyelids, dyspnea,
stridor and rhinorrhea
Imaging
Cystic
- For cystic echinococcosis diagnosis, imaging is the main method
- serology tests that use antigens specific for E. granulosus verify the imaging results
- The imaging technique of choice is ultrasonography, since it is not only able to visualize the
cysts in the body's organs, but it is also inexpensive, non-invasive and gives instant resultsIn
addition to ultrasonography, both MRI and CT scans can and are often used although an MRI is
often preferred to CT scans when diagnosing cystic echinococcosis since it gives better visual
Alveolar
- ultrasonography is the imaging technique of choice for alveolar echinococcosis
- usually complemented by CT scans since CT scans are able to detect the largest number of
lesions and calcifications that are characteristic of alveolar echinococcosis
- MRIs are also used in combination with ultrasonography though CT scans are preferred
- In addition to imaging and serology, identification of E. multilocularis infection via PCR or a
histological examination of a tissue biopsy from the patient is another way to diagnose alveolar
echinococcosis
Treatment
- based on considerations of the size, location, and manifestations of cysts and the overall health
of the patient
- ultrasound staging is recommended for E. granulosus infections
- Small CL, CE1, and CE3 lesions may respond to chemotherapy with albendazole
Page 92 of 269
- For CE1 lesions and uncomplicated CE3 lesions, PAIR (percutaneous aspiration, infusion of
scolicidal agents, and reaspiration) is now recommended instead of surgery
- PAIR is contraindicated for superficially located cysts (because of the risk of rupture), for cysts
with multiple thick internal septal divisions (honeycombing pattern), and for cysts
communicating with the biliary tree
- For prophylaxis of secondary peritoneal echinococcosis due to inadvertent spillage of fluid
during PAIR, the administration of albendazole (15 mg/kg daily in two divided doses) should be
initiated at least 2 days before the procedure and continued for at least 4 weeks afterward
- In experienced hands, some CE2 lesions can be treated by aspiration with a trocar
- Daughter cysts within the primary cyst may need to be punctured separately, and catheter
drainage may be required
Surgery
- remains the treatment of choice for complicated E. granulosus cysts (e.g., those
communicating with the biliary tract), for most thoracic and intracranial cysts, and for areas
where PAIR is not possible
- For E. granulosus of the liver, the preferred surgical approach is pericystectomy
- => the entire cyst and the surrounding fibrous tissue are removed
- The risks posed by leakage of fluid during surgery or PAIR include anaphylaxis and
dissemination of infectious protoscolices
- Albendazole, which is active against Echinococcus, should be administered adjunctively,
beginning several days before resection of the liver and continuing for several weeks for E.
granulosus
- Praziquantel (50 mg/kg daily for 2 weeks) may hasten the death of the protoscolices
- Surgical resection remains the treatment of choice for E. multilocularis infection
- Complete removal of the parasite continues to offer the best chance for cure
- Ongoing therapy with albendazole for at least 2 years after presumptively curative surgery is
recommended
- Most cases are diagnosed at a stage at which complete resection is not possible; in these
cases, albendazole treatment should be continued indefinitely, with careful monitoring
- In some cases, liver transplantation has been used because of the size of the necessary liver
resection
- However, continuous immunosuppression favors the proliferation of E. multilocularis larvae and
reinfection of the transplant
- => indefinite treatment with albendazole is required
Prevention
- In endemic areas, echinococcosis can be prevented by administering praziquantel to infected
dogs, by denying dogs access to infected animals, or by vaccinating sheep
- Limitation of the number of stray dogs is helpful in reducing the prevalence of infection among
humans
31.) Pleural empyema ( Pyothorax)
General
- a collection of pus in the pleural cavity caused by microorganisms, usually bacteria
- Often it happens in the context of a pneumonia, injury, or chest surgery
- It is one of various kinds of pleural effusion
- There are three stages:
1. exudative, when there is an increase in pleural fluid with or without the presence of pus
2. fibrinopurulent, when fibrous septa form localized pus pockets
3. organizing stage, when there is scarring of the pleura membranes with possible
inability of the lung to expand
- Simple pleural effusions occur in up to 40% of bacterial pneumonias
- They are usually small and resolve with appropriate antibiotic therapy
- If however an empyema develops additional intervention is required
Page 93 of 269
Clinical Manifestation
- depends upon several factors, including the causative micro-organism
- Most cases present themselves in the setting of a pneumonia, although up to one third of
patients do not have clinical signs of pneumonia and as many as 25% of cases are associated
with trauma (including surgery)
- Typical symptoms include cough, chest pain, shortness of breath and fever
Diagnosis
- The initial investigations for suspected empyema remains chest X-ray, although it cannot
differentiate an empyema from uninfected parapneumonic effusion
- Ultrasound must be used to confirm the presence of a pleural fluid collection and can be used
to estimate the size of the effusion, differentiate between free and loculated pleural fluid and
guide thoracocentesis if necessary
- Chest CT and MRI do not provide additional information in most cases and should therefore not
be performed routinely
- The most often used "golden" criteria for empyema are pleural effusion with macroscopic
presence of pus, a positive Gram stain or culture of pleural fluid, or a pleural fluid pH under 7.2
with normal peripheral blood pH
Treatment
1. Pleural fluid drainage
- Proven empyema is an indication for prompt chest tube drainage
- => has been shown to improve resolution of the infection and shorten hospital admission
- a pleural fluid pH of <7.2 is the most powerful indicator to predict the need for chest tube
drainage in patients with non-purulent, culture negative fluid
- Other indications for drainage include poor clinical progress during treatment with
antibiotics alone and patients with a loculated pleural collection
- Because of the viscous, lumpy nature of infected pleural fluid, in combination with possible
septation and loculation, it has been proposed that intrapleural fibrinolytic or mucolytic
therapy might improve drainage and therefore might have a positive effect on the clinical
outcome
- Intrapleural fibrinolysis with urokinase decreased the need for surgery but there is a trend
to increased serious side effects
- Approximately 15 to 40 percent of people require surgical drainage of the infected pleural
space because of inadequate drainage due to clogging of the chest tube or loculated
empyema
- Patients should thus be considered for surgery if they have ongoing signs of sepsis in
association with a persistent pleural collection despite drainage and antibiotics
- Video-assisted thoracoscopic surgery (VATS) is used as a first-line therapy in many
hospitals, although open thoracic drainage remains a frequently used alternative
technique.
2. Antibiotics
- Experts agree that all patients should be hospitalized and treated with antibiotics
intravenously
- The specific antimicrobial agent should be chosen based on Gram stain and culture, or on
local epidemiologic data when these are not available
- Anaerobic coverage must be included in all adults, and in children if aspiration is likely
- Good pleural fluid and empyema penetration has been reported in adults for penicillins,
ceftriaxone, metronidazole, clindamycin, vancomycin, gentamycin and ciprofloxacin
- Aminoglycosides should typically be avoided as they have poor penetration into the
pleural space
- There is no clear consensus on duration of intravenous and oral therapy
- Switching to oral antibiotics can be considered upon clinical and objective improvement
(adequate drainage and removal of chest tube, declining CRP, temperature normalization)
- Oral antibiotic treatment should then be continued for another 1–4 weeks, again based on
clinical, biochemical and radiological response
Page 94 of 269
32.) Benign tumors of the pleura and lungs
Pleura
Solitary fibromas
- also known as fibrous tumor of the pleura,
- a rare mesenchymal tumor originating in the pleura or at virtually any site in the soft tissue
including seminal vesicle
- Approximately 78% to 88% of SFT's are benign and 12% to 22% are malignant
Clinical manifestation
- About 80% of pleural SFTs originate in the visceral pleura, while 20% arise from parietal pleura.
- Although they are often very large tumors (up to 40 cm. in diameter), over half are
asymptomatic at diagnosis
- While some researchers have proposed that a SFT occupying at least 40% of the affected
hemithorax be considered a "giant solitary fibrous tumor", no such "giant" variant has yet been
recognized within the most widely used pleural tumor classification scheme
- Some SFTs are associated with the paraneoplastic Doege–Potter syndrome, which is caused
by tumor production of IGF-2
Treatment
- The treatment of choice for both benign and malignant SFT is complete en bloc surgical
resection
- Prognosis in benign SFTs is excellent. About 8% will recur after first resection, with the
recurrence usually cured after additional surgery
- The prognosis in malignant SFTs is much more guarded
- Approximately 63% of patients will have a recurrence of their tumor, of which more than half will
succumb to disease progression within 2 years
- Adjuvant chemotherapy and/or radiotherapy in malignant SFT remains controversial
Lungs
Hamartomas
- account for about 55% of all benign lung tumors, and 8% of all lung tumors
- 80% are found in the peripheral, or outer, portion of the lung's connective tissue. The remainder
are found inside the bronchial tubes (the airways leading to the lungs)
- => Deeper growths may be difficult to distinguish from cancerous nodules.
- made up of "normal" tissues such as cartilage, connective tissue, fat, and muscle but in
abnormal amounts.
- usually less than 4 centimeters in diameter.
- Stay within a limited area and are not likely to press against nearby tissue.
- Usually appear in chest X-rays as a coin-like round growth.
- May look like fluffy wool or popcorn in about 15% of cases.
- found more often in males than females, and between the ages of 50 and 70.
Papillomas
- grows in the bronchial tubes, sticking out from the surface area where it is attached
- not very common
- divided into three types
1. Squamous
- Occur in both children and adults
- May appear as just one nodule or many
- Result from infection by human papilloma virus (HPV)
2. Glandular
- No cause has been identified
- less common than squamous papillomas
- Develop in larger airways than squamous papillomas
- Can occur in all ages but mostly adults
- Almost always appear as one nodule, centrally located
3. Mixed
Page 95 of 269
- Contain a mix of squamous and glandular papilloma tissue
- Only a small number of cases have been reported
- Has the potential to eventually turn cancerous because the squamous cells can change over
time
Symptoms of benign lung tumors
- Often there are no symptoms that a benign lung tumor is present
- More than 90% are found by accident, when a patient receives a chest X-ray or CT (computed
tomography) scan for some other reason.
- If symptoms do appear, they may include the following:
•
Persistent coughing or wheezing
•
Shortness of breath or difficulty breathing
•
Coughing up blood
•
Rattling sounds in the lungs
•
Higher likelihood of pneumonia
•
Lung tissue collapse
Diagnosis
- CT, Xray
- a growth chart to analyse growth curve of tumor can be an indication mark for malignancy
- Biopsy
Treatment
- generally only monitoring
- If there is any reason to believe the tumor might become malignant, immediate excision is
recommended
33.) Lung cancer
Epidemiology
- the most common cause of cancer death
- The projected lifetime probability of developing lung cancer is estimated to be approximately
8% among males and approximately 6% among females
- The incidence of lung cancer varies by racial and ethnic group with the highest age-adjusted
incidence rates among African Ameriιans
- The excess in age-adjusted rates among African Americans occurs only among men, but
examinations of age-specific rates show that below age 50, mortality from lung cancer is more
than 25% higher among African American than Caucasian women
- Incidence and mortality rates among Hispanics and Native and Asian Americans are
approximately 40-50% those of whites
Risk factors
- Tobacco smoke
- Exposure to radon, asbestos, cancer causing-agents
- Arsenic in drinking water
- Air pollution
- Previous radiation therapy
- Family history of lung cancer
- Certain dietary supplements
Pathology
- The World Health Organization (WHO) defines lung cancer as tumors arising from the
respiratory epithelium (bronchi, bronchioles and alveoli)
- The WHO classification system divides epithelial lung cancers into four major cell types: smallcell lung cancer (SCLC), adenoιarcinoma, squamous cell carcinoma and large-cell carcinoma;
- the latter three types are collectively known as non-small-cell carcinomas (NSCLCs)
- Small-cell carcinomas consist of small cells with scant cytoplasm, ill-defined cell borders, finely
granular nuclear chromatin, absent or inconspicuous nucleoli and a high mitotic count
- SCLC may be distinguished from NSCLC by the presence of neuroendocrine markers including
CD56, neural cell adhesion molecule (NCAM), synaptophysin and chromogranin
Page 96 of 269
Types of Lung cancer
Type
Localisation
Histology
Freque
ncy
Central
Near to hilus
Mostly small cell and squamous cell
carcinoma
70 %
Peripheral
In the outer lung parts
Often large cell or adenocarcinoma
25 %
Diffuse growing
Diffusely localized (simulating
pneumonia)
Alveolar carcinoma
Pancoast tumor
In the apex of the lung
infiltrating the thoracic wall
3%
2%
Histologic types of lung cancer
Types
Annotation
Frequency
Small cell carcinoma (oat cell)
Worst prognosis, paraneoplastic
endocrinopathy
20-25%
Non-small cell lung cancer
- Squamous cell carcinoma
75-80%
-
(40%)
Adenocarcinoma (30%, most
common type in non-smokers)
Large cell carcinoma (10%)
Clinical Manifestation
- Over half of all patients diagnosed with lung cancer present with locally advanced or metastatic
disease at the time of diagnosis
- The majority of patients present with signs, symptoms or laboratory abnormalities that can be
attributed to the primary lesion, local tumor growth, invasion or obstruction of adjacent
structures, growth at distant metastatic sites or a paraneoplastic syndrome
- The prototypical lung cancer patient is a current or former smoker of either sex usually in the
seventh decade of life
- A history of chronic cough with or with out hemoptysis in a current or former smoker with
chronic obstructive pulmonary disease (COPD) age 40 years or older should prompt a thorough
investigation for lung cancer even in the face of a normal CXR
- A persistent pneumonia without constitutional symptoms and unresponsive to repeated
courses of antibiotics also should prompt an evaluation for the underlying cause
- Lung cancer arising in a life time never smoker is more common in women and East Asians
- Such patients also tend to be younger than their smoking counterparts at the time of diagnosis
- The clinical presentation of lung cancer in never smokers tends to mirror that of current and
former smokers
Presenting signs and symptoms
- Cough
- Weight loss
- Dyspnea
- Chest pain
- Hemoptysis
- Bone pain
- Clubbing
- Fever
- Weakness
- Superior vena cava onstruction
- Dysphagia
- Wheezing and stridor
Page 97 of 269
Diagnosis
- Tissue sampling is required to confirm a diagnosis in all patients with suspected lung cancer
- In patients with suspected metastatic disease, a biopsy of the most distant site of disease is
preferred for tissue confirmation
- Given the greater emphasis placed on molecular testing for NSCLC patients, a core biopsy is
preferred to ensure adequate tissue for analysis
- Tumor tissue may be obtained via minimally invasive techniques such as bronchial or
transbronchial biopsy during beroptic bronchoscopy, by fine needle aspiration or percutaneous
biopsy using image guidance or via endobronchial ultrasound (EBUS) guided biopsy
- Depending on the location, lymph node sampling may occur via transesophageal endoscopic
ultrasound-guided biopsy (EUS), EBUS or blind biopsy
- In patients with clinically palpable disease such as a lymph node or skin metastasis, a biopsy
may be obtained
- In patients with suspected metastatic disease, a diagnosis may be confirmed by percutaneous
biopsy of a so tissue mass, lytic bone lesion, bone marrow, pleural or liver lesion or an
adequate cell block obtained from a malignant pleural effusion
- In patients with a suspected malignant pleural effusion, if the initial thoracentesis is negative,
a repeat thoracentesis is warranted
- Although the majority of pleural effusions are due to malignant disease, particularly if they are
exudative or bloody, some may be parapneumonic
- In the absence of distant disease such patients should be considered for possible curative
treatment
Staging
- consists of two parts:
- determination of the location of the tumor and possible metastatic sites (anatomic staging)
- an assessment of a patient's ability to withstand various antitumor treatments (physiologic
staging )
- All patients with lung cancer should have a complete history and physical examination with
evaluation of all other medical problems, determination of performance status and history of
weight loss
- The most significant dividing line is between those patients who are candidates for surgical
resection and those who are inoperable but will benefit from chemotherapy, radiation therapy,
or both
- Staging with regard to a patient's potential for surgical resection is principally applicable to
NSCLC
T1
Tumor 3 cm or less in the greatest dimension, surrounded by lung or visceral pleura, without
bronchoscopic evidence of invasion mllre proximal than the lobar bronchus
T2
Any of the following features:
- More than 3 cm in widest dimension
- Involves main bronchus, 2 cm or more distal to the carina
- Invades the visceral pleura
- Associated with atelectasis or obstructive pneumonitis that extends to the hilar region but
does not involve the entire lung
T3
- Tumor of any size that directly invades any of the Chest wall, diaphragm, mediastinal pleura
or parietal pericardium
- Tumor in the main bronchus less than 2cm distal to the carina but without involvement of
the carina
- or associated atelectasis or obstructive pneumonitis of the entire lung
T4
Tumor of any size that invades any of the mediastinum, heart, great vessels, trachea,
esophagus, vertebral body or carina
Or a tumor with malignant pleural effusion
Page 98 of 269
Treatment
Small cell lung cancer
- limited disease:
- Tumor resection
- polychemotherapy (Cisplatin and Etopside)
- Radiation of the mediastinum and primary tumor (40gy)
- prophylactic radiation of the skull if complete remission
- Extensive disease
- Palliative chemotherapy (Carboplatin, Etopside and Vincristine)
- If needed radiation of skeletal and brain metastases+
Non-small cell lung cancer
- stage I,II or IIIa (T3)
- if locally limited and inoperable the alternative is radiation (60-70Gy)
- perhaps neoadjuvant, combined chemo-radiation before operation
- Stage IIIA or higher
- palliative radiation, chemotherapy (e.g. Cisplatin and Gemcitabin/Taxan/Pemetrexed/Vinorelbin
or Carboplatin, Paclitaxel and Bevacizumab),
- perhaps bronchoscopic stenting, lasertherapy and possibly chemoembolisation
- if bone metastases there are bisphosphonate infusions
- pain medication and other symptomatic therapies
34.) Metastatic lung tumors
General
- seen in 20-54% of extrathoracic malignancies
- Lungs are the second most frequent site of metastases from extrathoracic malignancies
- Twenty percent of metastatic disease is isolated to the lungs
- The development of pulmonary metastases in patients with known malignancies indicates
disseminated disease and places the patient in stage IV in TNM (tumor, node, metastasis)
staging systems
- => implies an adverse prognosis and alters the management plan
- Imaging plays an important role in the screening and detection of pulmonary metastases
- Imaging guidance is also used in histologic confirmation of metastatic disease
- In patients with poor cardiorespiratory function and comorbidities, imaging-guided thermal
ablation procedures are an effective alternative to surgical resection to improve survival
Pathophysiology
1. Hematogenous spread (pulmonary or bronchial artery)
- occurs in tumors that have direct venous drainage to the lungs.
- includes cancers of the head and neck, thyroid, adrenals, kidneys, and testes, as well as
malignant melanoma, soft-tissue sarcomas, and osteosarcoma
- tumor cells embolize to the lungs through the pulmonary or bronchial arteries
- some tumor cells pass through the vascular wall and develop parenchymal metastasis in
the alveolar space or the interstitium
2. Lymphatic spread
- occurs to the lungs, pleura, or mediastinum
- Lymphatic spread occurs either in an antegrade fashion by lymphatic invasion through the
diaphragm and/or pleural surfaces or by retrograde lymphatic spread from hilar lymph
nodal metastasis
- Lymphangitic spread refers to tumor growth in lymphatic channels, which are seen in the
axial interstitium (peribronchovascular and centrilobular interstitium) and peripheral
interstitium (interlobular septa and subpleural)
3. Pleural space
- can occur by pleural invasion by a local tumor, such as lung cancer or thymoma
4. Endobronchial spread
- occurs with airway tumors
Page 99 of 269
- more common in primary pulmonary adenocarcinoma, less common in other types of lung
cancer, and even less common in tracheobronchial papillomatosis
5. Direct invasion
- occurs in tumors contiguous to the lung
- => thyroid, esophageal, mediastinal, airway, and cardiovascular structures
Symptoms
- a large number of patients with pulmonary metastases are asymptomatic at the time of
diagnosis
- some patients develop symptoms such as hemoptysis, cough, shortness of breath, chest pain,
weakness, and weight loss
- Patients with lymphangitic carcinomatosis present with respiratory dysfunction, including
severe dyspnea
Frequency
- Breast, colorectal, lung, kidney, head and neck, and uterus cancers are the most common
primary tumors with lung metastasis at autopsy
- Choriocarcinoma, osteosarcoma, testicular tumors, malignant melanoma, Ewing sarcoma, and
thyroid cancer frequently metastasize to lung, but the frequency of these tumors is low
Diagnosis
- CXR is the initial imaging modality used in the detection of suspected pulmonary metastasis
- Chest CT scanning without contrast is more sensitive
- For patients with bone or soft-tissue sarcoma, malignant melanoma, or head and neck
carcinoma, CT scanning of the chest should be performed as an initial evaluation
- In patients with primary renal or testicular cancer, chest CT scanning should be performed
based on the presence of metastatic disease elsewhere
- CT guidance is often required for obtaining samples from a suspected metastatic disease
- Several thermal ablation options are available for treatment of pulmonary metastases, which is
performed under CT guidance
Mortality and Morbidity
- The presence pulmonary metastasis usually indicates advanced disseminated disease
- The mortality depends on the primary tumor
- Early diagnosis is critical in planning effective therapy in patients who can be cured
- Depending on several factors, metastasis can be resected, with 5-year survival rates up to 30
to 40%
Treatment
Pulmonary metastasectomy
- The definitive treatment for pulmonary metastases from extrathoracic malignancies is surgical
resection
- Surgery is performed if the primary tumor is controlled, if no extrathoracic lesions are present, if
it is technically resectable, and if general and functional risks are tolerable
- Only 15 to 25% of patients have lesions confined to the lung and are appropriate candidates for
curative resection
- For this reason, staging for metastatic disease outside of the lung is performed before
pulmonary resection, by CT of the chest and abdomen, and, in selected cases, by PET scan
and brain imaging with either MRI or CT scan
Alternatives
- In patients who are not in adequate physical condition
- alternative options available include stereotactic radiosurgery and thermal ablation procedures
- Thermal ablation procedures induce coagulation necrosis of tumor cells and are typically
performed with CT guidance
- include radiofrequency ablation (RFA), microwave ablation, laser ablation, and cryoablation
- the primary goal is to eradicate all the malignant cells along with a margin of normal tissue, but
cause minimal damage to normal lung disease
- => adequate tumor control is achieved and survival is prolonged
Page 100 of 269
- The main advantage of thermal ablation procedures is selective and limited damage of lung
tissue to minimally impact pulmonary function
- ablation procedures can be performed regardless of previous therapy, even in patients who
have adhesions from previous surgeries or radiation-induced pneumonitic changes
- => often used as a salvage treatment for oligo-recurrence after surgery and radiation.
35.) Pulmonary Tuberculosis: diagnosis, clinical symptoms, treatmentt
Causative agent
- Mycobacterium tuberculosis causes 95% of human tuberculosis
- Mycobacterium bovis is responsible for the rest
- Mycobacteria are small, nonmotile, slightly curved acid-fast rods
Epidemiology
- Only 10% of individuals with normal immune status who are infected with Mycobacterium
tuberculosis develop active tuberculosis
- Factors that decrease host resistance include:
- Malnutrition, immunosuppression, malignancies, other major illnesses
- Age: Children 3 years of age have a more severe course; 3–12 year-olds almost always
have spontaneous healing. Later, resistance drops with increasing age
- Pulmonary silicosis: Increased risk for tuberculosis
- drug abusers, patients with HIV/AIDS, lymphoma, leukemia, and iatrogenic
immunosuppression are all at great risk for tuberculosis. In some situations, such as
prisoners in some parts of Eastern Europe, the problem is epidemic
- Immigration of patients from countries where tuberculosis is endemic is another factor in
the surge of cases in developed countries
- Mycobacterium bovis has become uncommon as cattle tuberculosis has almost been
eliminated in most developed countries
Resistance
- The number of strains resistant to single agents or to multiple drugs is continuing to increase
- Factors include inappropriate single drug therapy and inadequate duration of therapy
- Strict combination regimens, perhaps administered under direct observation, are considered
the only effective public health measure
- Patients with HIV/AIDS and multidrug resistant Mycobacterium tuberculosis are currently the
major sources of infection
Diagnosis
- Microscopic examination: Staining with Ziehl–Neelsen stain or auramine fluorescence staining
can be used to examine tissue sections or bodily fluids
- => Rapid, but only sensitive when large numbers of organisms are present (103 104/mL).
- Culture: Both species grow slowly on special media( Löwenstein–Jensen) under anaerobic
conditions
- Initial growth takes 3–10 weeks, followed by differentiation and determination of drug
sensitivity, lasting total of 2–3 months
- BACTEC method with radiometric measurement of metabolites takes 7–10 days
- Other possibilities: PCR for Mycobacterium tuberculosis DNA in skin biopsies; this technique
has become important because it is so difficult to culture the organisms in skin.
Pathogenesis
1. Primary infection
- usual site of infection is the lungs following droplet spread
- A nonspecific leukocyte-rich inflammatory response develops, known as a tubercle
- From there the bacteria move to regional lymph nodes (Ghon complex)
- Then the bloodstream is invaded, so that the mycobacteria can be spread throughout the
body
- After 2–4 weeks a specific cell-mediated immunity develops and the host is usually able to
bring the infection under control
- Healing occurs with fibrosis and calcification
Page 101 of 269
2. Endogenous reactivation
- Organisms that have been spread about the body during the primary infection can survive
in different organs for years
- If the host immune response diminishes, then the bacteria can once again cause active
disease
- If the resistance is modest, tIf the resistance is modest, the disease will remain localized
- with sharp diminution in resistance, disseminated disease occurs
3. Secondary infection
- uncommon with specific immunity and good resistance, but they can occur
Treatment
- Standard chemotherapy consists of six months of rifampicin and isoniazid (usually given as
combination tablets), initially supplemented by two months of pyrazinamide and ethambutol
- A reliable preparation containing rifampicin, isoniazid, and pyrazinamide in combination is
available, as is a combination tablet of all four of these first line drugs
- Fixed dose combinations of drugs in a single tablet have the great advantage of reducing the
possibility of emergence of drug resistance.
- Whenever possible, cure should be confirmed by smear and culture of sputum at the end of
treatment
- If the pleural cavities are involved, the chemotherapy regimen is the same, but pleural aspiration
may be needed to reduce breathlessness
- If the effusion recurs, glucocorticoids for three to six weeks help to prevent or reduce further
reaccumulation
36.) Tumors of the mediastinum (see also Nr. 38)
General
- The mediastinum is the region between the pleural sacs
- separated into three compartments
- The anterior mediastinum extends from the sternum anteriorly to the pericardium and brachiocephalic vessels posteriorly
- => contains the thymus gland, the anterior mediastinal lymph nodes and the internal
mammary arteries and veins
- The middle mediastinum lies between the anterior and posterior mediastina
- => contains the heart; the ascending and transverse arches of the aorta; the venae cavae;
the brachiocephalic arteries and veins; the phrenic nerves; the trachea, the main bronchi and
their contiguous Iymph nodes; and the pulmonary arteries and veins
- The posterior mediastinum is bounded by the pericardium and trachea anteriorly and the
vertebral column posteriorly
- => contains the descending thoracic aorta, the esophagus, the thoracic duct, the azygos and
hemiazygos veins and the posterior group of mediastinal lymph nodes
Mediastinal Masses
- The first step in evaluating a mediastinal mass is to place it in one of the three mediastinal
compartments, since each has different characteristic lesions
- The most common lesions in the anterior mediastinum are thymomas, lymphomas,
teratomatous neoplasms and thyroid masses
- The most common masses in the middle mediastinum are vascular masses, Iymphnode
enlargement from metastases or granulomatous disease and pleuropericardial and
bronchogenic cysts
- In the posterior mediastinum, neurogenic tumors, meningoceles, meningomyeleles,
gastroenteric cysts and esophageal diverticula are commonly found.
- Computed tomography (CT) scanning is the most valuable imaging technique for evaluating
mediastinal masses and is the only imaging technique that should be done in most instances
- Barium studies of the gastrointestinal tract are indicated, because hernias, diverticula and
achalasia are readily diagnosed in this manner
- An iodine 1 3 1 scan can efficiently establish the diagnosis of intrathoracic goiter.
- A definite diagnosis can be obtained with mediastinoscopy or anterior mediastinotomy in many
patients with masses in the anterior or middle mediastinal compartments
Page 102 of 269
- A diagnosis can be established without thoraιotomy via percutaneous fine needle aspiration
biopsy or endoscopic transesophageal or endobronchial ultrasound-guided biopsy of
mediastinal masses in most cases
- An alternative way to establish the diagnosis is video-assisted thoracoscopy
- In many cases the diagnosis can be established and the mediastinal mass removed with videoassisted thoracoscopy
Compart
ment
Borders
Normal structures
Masses
Anterior
Ant: sternum
Posterior: pericardium,
ascending aorta,
brachocephalic vessels
Lymph nodes
Connective tissue
Thymus (remnant in adults)
Thymoma, Germ cell
neoplasm, Lymphoma,
Thyroid enlargement
(intrathoracic goiter)
Middle
Anterior: anterior pericardium,
ascending aorta,
brachiocephalic vessels
Posterior: posterior pericardium
Pericardium
Heart
Vessels (ascending aorta, venae
cavae, main pulmonary arteries
Carcinoma, Lymohoma,
Pericardial cyst,
Bronchogenic cyst,
Benign lymph node
enlargement
Posterior
Anterior: posterior pericardium
Posterior: pos. chest wall
Descending aorta, Esophagus,
vertebral column, Nerves
(sympathetic chain, lower
vagus), lymph nodes,
Connective tissue
Neurogenic tumor,
Diaphragmatic hernia
37.) Mediastinits
Pathophysiology
- Infection from either bacterial pathogens or more atypical organisms can inflame any of the
mediastinal structures, causing physiologic compromise by compression, bleeding, systemic
sepsis, or a combination of these
- Most cases occur in the aftermath of cardiovascular surgery
Risk factors (in the setting of CV surgery)
- the use of pedicled bilateral internal thoracic (mammary) artery (BITA) grafts carries increased
risk for mediastinitis after coronary artery bypass grafting (CABG)
- => even higher among patients with diabetes, thus rendering many surgeons reluctant to use
BITA grafting in this subgroup
- Emergency surgery
- External cardiac compression
- Obesity (>20% of ideal body weight)
- Postoperative shock, especially when multiple blood transfusions are required
- Prolonged bypass and operating room time
- Reoperation
- Reexploration following initial surgery
- Sternal wound dehiscence
- Surgical technical factors (eg, excessive use of electrocautery, bone wax, paramedian
sternotomy)
Other Etiologies
- Esophageal perforation
- Trauma, especially blunt trauma to the chest or abdomen
- Tracheobronchial perforation, due to either penetrating or blunt trauma or instrumentation
during bronchoscopy
Page 103 of 269
-
Descending infection following surgery of the head and neck, great vessels, or vertebrae
Progressive odontogenic infection ( Ludwig angina)
Mediastinal extension of lung infection
Chronic fibrosing mediastinitis due to granulomatous infections
Ultrasound-guided transbronchial needle aspiration
Pathogens
- Most mediastinitis cases involve gram-positive cocci, with Staphylococcus aureus and
Staphylococcus epidermidis accounting for 70-80% of cases (see the image below)
- Mixed gram-positive and gram-negative infections account for approximately 40% of cases
- Isolated gram-negative infections are rare causes
Symptoms
- The typical postoperative patient presents with fever, high pulse, and report symptoms
suggestive of a sternal wound infection (eg, sternal instability)
- two thirds of patients present within 14 days following surgery
- Patients may report sternal pain that has increased since surgery, drainage from the wound
site, an audible click due to sternal nonunion, and progressive redness over a variable period
Physical examination
- tachycardia and fever
- In more advanced cases of sepsis, hypotension may be present, and the patient may require
large volumes of crystalloid or vasopressor medication for support
- The Hamman sign is a crunching sound heard with a stethoscope over the precordium during
systole
- Direct signs of sternal infection may be among the initial presenting signs or may be delayed
until after the diagnosis is already considered
- Sternal pain, instability, or click; local cellulitis; and drainage can all be observed
- Distinguishing between a superficial wound infection and a deeper chest infection associated
with mediastinitis can be challenging
- Systemic signs of sepsis strongly suggest mediastinal involvement
- Local wound exploration should be utilized as a mechanism to distinguish a superficial wound
infection from a deep sternal wound infection
Treatment
Medical
- Most patients have already received prophylactic antibiotics, usually a first-generation
cephalosporin
- Because as many as 20% of organisms cultured from infected sternotomy sites are methicillinresistant S aureus and because another 20% are gram-negative organisms, it is vital to institute
very broad and deep antibiotic coverage that includes Pseudomonas species
- Culture results should then guide antibiotic use
- Therapy is usually prolonged, ranging from weeks to months
- 4-6 weeks of therapy is adequate for most patients
- Enteral nutritional support should be instituted immediately, with a duodenal feeding tube, if
necessary
Surgery
1. After cardiac surgery
- Effective treatment for simple sternal dehiscence without infection is rewiring the sternum
- Cultures should be taken to exclude active infection in the cases of sternal dehiscence
- Failure to adequately debride and sterilize the mediastinum during the first reoperation is
the most common cause of repeat postoperative mediastinitis
- options are:
- Immediate closure after sternal debridement
- Delayed closure after sternal debridement
- Sternal irrigation after sternal debridement
- The optimal strategy for a given case depends on the duration of the infection, the
condition of the mediastinal structures, and the experience of the surgeon
Page 104 of 269
- leave the wound open or treat with vacuum-assisted closure for subsequent debridement
efforts after initial sternal reexploration
- In this case, the wound is packed daily until it appears clean with adequate granulation
tissue
- At this point, muscle flap closure is achieved (Usually, bilateral pectoralis flaps are used)
- Occasionally, the rectus abdominis that is opposite the internal mammary artery used for
bypass is employed for coverage
2. Chronic fibrosing Mediastinitis
- Surgery is seldom recommended for cases of chronic fibrosing mediastinitis unless
compression of major mediastinal structures has occurred
- Whether surgical debulking early in the process minimizes the development of superior
vena cava syndrome or cardiac compression has not been adequately studied.
3. Oropharyngeal descending infections
- some surgeons attempt to limit drainage and debridement to the cervical region
- In a more advanced infection, often the best plan to offer a maximal chance of cure is to
proceed with formal thoracic drainage and debridement
Complications
- Systemic sepsis is a major complication of mediastinitis and manifests with tachycardia,
hypotension, poor urine output, and other signs of poor systemic perfusion
- Pneumoperitoneum and pneumothorax can produce serious local problems and eventual
hemodynamic compromise.
- If pleural effusions become infected and develop into empyema, systemic sepsis may occur
- Severe and life-threatening bleeding from ruptured vessels or the heart itself can occur when
the chest is packed and left open to await definitive closure
- Superior vena cava syndrome and compression of critical mediastinal structures are sometimes
observed with chronic fibrosing mediastinitis
- Compression of the pulmonary vessels may give rise to pulmonary hypertension
Prognosis
- The development of mediastinitis dramatically increases mortality
- postoperatively, a patient's chance of dying is as high when mediastinitis develops
- Some studies have reported death rates as high as 47%
- Mediastinitis also raises the 2-year mortality from 2% to 8% following CABG
- substantially lengthens the hospital stay as well
- Patients with postoperative mediastinitis stay in the hospital six to seven times longer than
those without the condition
38.)Primary mediastinal tumors and cysts. Castelman’s disease
Mediastinal masses
- The most common lesions in the anterior mediastinum are thymomas, lymphomas,
teratomatous neoplasms, and thyroid masses
- The most common masses in the middle mediastinum are vascular masses, lymph node
enlargement from metastases or granulomatous disease, and pleuropericardial and
bronchogenic cysts
- In the posterior mediastinum, neurogenic tumors, meningoceles, meningomyeloceles,
gastroenteric cysts, and esophageal diverticula are commonly found
- Computed tomography (CT) scanning is the most valuable imaging technique for evaluating
mediastinal masses and is the only imaging technique that should be done in most instances
- Barium studies of the gastrointestinal tract are indicated in many patients with posterior
mediastinal lesions, because hernias, diverticula, and achalasia are readily diagnosed in this
manner
- An iodine-131 scan can efficiently establish the diagnosis of intrathoracic goiter.
- A definite diagnosis can be obtained with mediastinoscopy or anterior mediastinotomy in many
patients with masses in the anterior or middle mediastinal compartments
Page 105 of 269
Thymoma
- Most common primary anterior mediastinal tumor (20%) in adults but rarely seen in children
- Thymomas are most common in the fifth and sixth decades, are uncommon in children, and are
distributed evenly between men and women.
Symptoms
- About 40–50% of patients are asymptomatic
- masses are detected incidentally on routine chest radiographs
- When symptomatic, patients may have cough, chest pain, dyspnea, fever, wheezing, fatigue,
weight loss, night sweats, or anorexia
- Occasionally, thymomas may obstruct the superior vena cava
- Pericardial effusion may be present
- About 40% of patients with thymoma have another systemic autoimmune illness related to the
thymoma (30% of patients with thymoma have myasthenia gravis, 5–8% have pure red cell
aplasia, and ~5% have hypogammaglobulinemia)
Diagnosis
- An initial mediastinoscopy or limited thoracotomy can be undertaken to get sufficient tissue to
make an accurate diagnosis
- Fine-needle aspiration is poor at distinguishing between lymphomas and thymomas but is more
reliable in diagnosing germ cell tumors and metastatic carcinoma
- Thymomas and lymphomas require sufficient tissue to examine the tumor architecture to assure
an accurate diagnosis and obtain prognostic information
Staging
- Once a diagnosis of thymoma is defined, subsequent staging generally occurs at surgery.
- CT scans can assess local invasiveness
- Some 90% of thymomas are in the anterior mediastinum, but some may be in other mediastinal
sites or even the neck, based on aberrant migration of the developing thymic enlage
- The 5-year sur- vival of patients in the various stages is as follows: stage I, 96%; stage II, 86%;
stage III, 69%; and stage IV, 50%
I
II
III
IV
Macroscopically and microscopically completely encapsulated; no invasion through capsule
IIA
Microscopic invasion outside the capsule
IIB
Macroscopic invasion into surrounding fat or grossly adherent to pleura or pericardium
IIIA
Macroscopic invasion into neighbouring organs, pericardium or pleura, but not great vessels
IIIB
Macroscopic invasion into neighbouring organs including great vessels
IVA
Pleural or pericardial dissemination
IVB Lymphatic or hematogenous metastases
Treatment
- For patients with encapsulated tumors and stage I disease, complete resection is sufficient to
cure 96% of patients
- For patients with stage II disease, complete resection may be followed by 30–60 Gy of
postoperative radiation therapy to the site of the primary tumor
- For patients with stage III and IV disease, the use of neoadjuvant chemotherapy followed by
radical surgery, with or without additional radiation therapy, and additional consolidation
chemotherapy has been associated with excellent survival
- Chemotherapy regimens that are most effective generally include a platinum compound (either
cisplatin or carboplatin) and an anthracycline
- This multimodality approach appears to be superior to the use of surgery followed by radiation
therapy alone, which produces a 5-year survival of ≤50% in patients with advanced-stage
disease
Page 106 of 269
Mediastinal seminoma
- Germ cell tumors of the mediastinum are uncommon
- Fewer than 5-7% of germ cell tumors occur outside the gonads, but of the extragonadal sites,
the mediastinum is the most common location for these tumors
Pathophysiology
- The histology of mediastinal tumors is very similar to that of tumors in the gonadal tissues
- Of the germ cell tumors, benign teratomas (ie, dermoid cysts) are the most commonly
diagnosed mediastinal mass and are present in 50-70% of infants and children with germ cell
tumors
- Seminomas are the predominant malignant lesions, accounting for nearly 50% of mediastinal
lesions
- They are generally bulky tumors and tend to infiltrate into adjacent structures early in the
growth process
- The cells are large and contain variable amounts of glycogen
Etiology
- Experimental evidence suggests that the cells responsible for mediastinal tumors are derived
from germinal cells that transmigrate to the mediastinum from the urogenital ridge during
embryonic life
- their prevalence is known to be increased in men with Klinefelter syndrome
- => known to develop mediastinal germ cell tumors at least 10 years earlier than those without
the syndrome
Treatment
- Surgical results for mediastinal seminomas have ranged from poor to borderline
- All series in which a mediastinal mass has been completely resected have shown 5-year
survival rates lower than 50%, with a greater than 40% chance of recurrence
- Currently, treatment of pure seminomas is nonsurgical (radiation therapy and chemotherapy)
- only the small, resectable tumors in asymptomatic patients should be completely excised and
managed with postoperative radiation therapy using doses of 40-50 Gy.
Castleman’s disease
General
- a group of three immunological disorders
- occur in individuals of all ages
- share a similar microscopic lymph node appearance
- Approximately 6,600-7,700 patients are estimated to be diagnosed with CD every year in the
United States
- There is significant variability in clinical features, treatments, and survival across the three
subtypes
Subtypes
1. Unicentric
- involves a single region of enlarged lymph nodes that demonstrate CD-like features under
the microscope
- Patients may be asymptomatic or present with a variety of signs and symptoms
2. Human-Herpesvirus 8 (HHV-8) associated multicentric CD
- involves multiple regions of enlarged lymph nodes with CD-like features
- flulike symptoms, abnormal blood counts, and dysfunction of vital organs
- due to uncontrolled infection with HHV-8 and the following excessive production of
inflammatory cytokines
- often occurs in immunocompromised individuals, such as those with HIV infection
- Patients are at increased risk of developing Kaposi sarcoma, non-Hodgkin lymphoma, and
Hodgkin lymphoma
3. HHV-8-negative/ idiopathic multicentric CD (iMCD)
- multiple regions of enlarged lymph nodes with CD-like features
- flulike symptoms, abnormal blood counts, and dysfunction of vital organs
- due to an unknown cause
Page 107 of 269
- Cytokines, such as interleukin-6 (IL-6) are also elevated in iMCD
- iMCD patients are negative for HHV-8 and HIV
- These patients are at increased risk of developing non-Hodgkin lymphoma, Hodgkin
lymphoma, and POEMS syndrome
- The cause of iMCD is not known, but hypothesized etiologies include acquired mutations
in a clonal cell population, inherited mutations leading to autoimmunity or
autoinflammation, or a pathogen
Epidemiology
- rare (6500 to 7700 new cases each year in the United States)
- 1000 of those are HHV-8–associated multicentric Castleman disease (HHV-8–associated MCD)
and 1000 are HHV-8–negative MCD
- UCD, HHV-8–associated MCD, and HHV-8–negative MCD can affect individuals of all ages,
including children
- UCD is slightly more common in women and younger individuals
- HHV-8–associated MCD is more common in men and individuals with HIV infection
Unicentric CD
- pathophysiology is poorly understood
- The lymph node is characterized by abnormal features that include small or large germinal
centers, follicular dendritic cell (FDC) prominence, hypervascularity, polyclonal plasmacytosis,
and/or expansion of polyclonal B cells and T cells
- Etiology is unknown
Treatment
- surgical removal of the enlarged lymph node is usually curative and is considered the gold
standard for treatment
- Systemic symptoms and laboratory abnormalities, if present, tend to resolve with complete
resection of the enlarged lymph node or solitary region of lymph nodes
Prognosis
- Patients are usually cured after lymph node excision
- Development of lymphoma and/or paraneoplastic pemphigus are two rare co-morbidities that
can be deadly for UCD patients
HHV-8 associated MCD
- Immunocompromise due to HIV or other causes enables the uncontrolled infection and
replication of HHV-8 in lymph node plasmablasts and B cells
- => they signal for viral IL-6 and other proinflammatory cytokines
- Depletion of B cells with rituximab typically results in resolution of symptoms
- Etiology: HHV-8 virus
Treatment
- treatment with rituximab is highly effective
- For patients with concomitant HIV infection and a low CD4 count and/or higher HIV load,
antiretroviral therapy (ART) should be included with the rituximab
- Treatment with rituximab should be repeated upon relapse
- Rituximab may be administered or without steroids and/or chemotherapy
- However, rituximab therapy occasionally worsens Kaposi sarcoma, which must be carefully
considered in HIV-positive patients with a high viral load, low CD4 count, and active Kaposi
sarcoma
Prognosis
- have a good prognosis when treated with rituximab, with greater than 90% 5-year overall
survival
- In patients who do not respond to rituximab alone, chemotherapy agents may be added to
control the disease
iMCD
- Patients experience atypical, CD-like lymphoproliferation
- occurs along with systemic inflammatory symptoms (fevers, weight loss, fatigue, night sweats),
abnormal blood cell counts, and multiple organ system dysfunction
- The pathophysiology of the disease is caused by excess IL-6 in a portion of patients
Page 108 of 269
- Inhibition of IL-6 with siltuximab is effective in approximately 34-44% of patients
- The pathophysiology in the remaining patients who do not improve with IL-6 inhibition is not
known but is suspected to involve cytokines or mechanisms other than IL-6 excess
- Etiology unknown
Treatment
- Siltuximab (Sylvant) is the only drug approved by the FDA for HHV-8–negative MCD
- Siltuximab is a monoclonal antibody that binds interleukin-6 (IL-6)
Prognosis
- not as good as that for patients with HHV-8–associated MCD
- According to studies performed prior to the advent of anti–IL-6 therapy, approximately 65% of
patients survive for 5 years after diagnosis
- worse than lymphoma, breast cancer, and prostate cancer
Mediastinal Cysts
- Various cysts can originate in the mediastinum
- usually result from abnormal embryologic development
- Foregut cysts
- Gastroenteric (enterogenic) cysts
- Neurenteric cysts
- Mesothelial cysts
- Thoracic duct cysts
39.) Closed chest trauma. Spontaneous pneumothorax
Closed (Blunt) chest trauma
- Blunt injury to the chest can affect any one or all components of the chest wall and thoracic
cavity
- These components include the bony skeleton (ribs, clavicles, scapulae, and sternum), the lungs
and pleurae, the tracheobronchial tree, the esophagus, the heart, the great vessels of the chest,
and the diaphragm
Etiology
- the most important cause of significant blunt chest trauma is motor vehicle accidents (MVAs).
- MVAs account for 70-80% of such injuries
- Vehicles striking pedestrians, falls, and acts of violence are other causative mechanisms
- Blast injuries can also result in significant blunt thoracic trauma
Categories
- Chest-wall fractures, dislocations, and barotrauma (including diaphragmatic injuries)
- Blunt injuries of the pleurae, lungs, and aerodigestive tracts
- Blunt injuries of the heart, great arteries, veins, and lymphatic vessels
Indication for surgical intervention
1. Chest wall fractures, dislocations and barotrauma
- immediate indication:
- Traumatic disruption with loss of chest-wall integrity
- Blunt diaphragmatic injuries
- relatively immediate to long-term indication:
- Delayed recognition of blunt diaphragmatic injury
- Development of a traumatic diaphragmatic hernia
2. Blunt injury of pleurae, lungs and aerodigestive tract
- immediate indications:
- Massive air leak following chest-tube insertion
- Massive hemothorax or continued high rate of blood loss via the chest tube (ie, 1500
mL of blood upon chest-tube insertion or continued loss of 250 mL/hr for 3
consecutive hours)
- Radiographically or endoscopically confirmed tracheal, major bronchial, or
esophageal injury
- Recovery of gastrointestinal (GI) tract contents via the chest tube
- Relatively immediate to long-term indications:
Page 109 of 269
- Chronic clotted hemothorax or fibrothorax, especially when associated with a trapped
or nonexpanding lung
Empyema
Traumatic lung abscess
Delayed recognition of tracheobronchial or esophageal injury
Tracheoesophageal fistula
Persistent thoracic duct fistula/chylothorax
3. Blunt injuries to heart, great arteries, veins and lymphatic vessels
- immediate indications:
- Cardiac tamponade
- Radiographic confirmation of a great-vessel injury
- Embolism into the pulmonary artery or the heart
- Relatively immediate to long-term indications:
- late recognition of a great-vessel injury (eg, development of traumatic
pseudoaneurysm)
-
Surgical approach
- Patients with immediately life-threatening injuries that necessitate surgery cannot afford a
protracted workup
- the ABCs (airay, breathing, and circulation) must be established
- cervical spine radiography; CT of the head, chest, and abdomen; and focused assessment with
sonography for trauma [FAST]) are completed if time and the patient's condition permit
- Blood is drawn and sent for typing, crossmatching, and other tests (eg, complete blood count
and arterial blood gas analysis)
- An adequate, secured airway is necessary, as is intravenous access
- Monitoring devices (eg, a Foley urinary catheter, central venous pressure monitor, or pulmonary
artery catheter) should be considered on the basis of the severity of injury, the patient's
preoperative functional status, and the anticipated length of the operation
- Cardiopulmonary bypass or a centrifugal pump is used when necessary
- Patient positioning and choice of incision are very important
- A median sternotomy is used to access the heart, the intrapericardial portion of the pulmonary
vessels, the ascending aorta and aortic arch, the SVC and IVC, and the innominate artery
- Branches of the innominate artery are exposed by extending the median sternotomy into the
neck
- A posterolateral left thoracotomy in the fourth intercostal space is used to approach the
descending thoracic aorta.
- he right subclavian artery is exposed via a median sternotomy that is extended into the neck
- Proximal control for the left subclavian artery is achieved through an anterolateral left
thoracotomy in the third intercostal space. Distal control for this vessel is obtained through a
supraclavicular incision
- The distal esophagus can be approached via a left posterolateral thoracotomy; more proximal
injuries require a right thoracotomy
- The thoracic duct is approached through a right thoracotomy
- Injuries to the lung or more peripheral pulmonary vessels are accessed through a posterolateral
thoracotomy
- Injuries to the proximal two thirds of the trachea are best approached through a collar incision
and extension via a T-incision through the manubrium, which allows exposure to the middle and
distal trachea
- Injuries to the distal trachea, the carina, or the right mainstem bronchus are best approached
through a right fourth intercostal posterolateral thoracotomy
- Injuries to the left mainstem bronchus are best approached through a left posterolateral
thoracotomy.
Page 110 of 269
Prognosis
- For the great majority of patients with blunt chest trauma, outcome and prognosis are excellent
- Most (>80%) require either no invasive therapy or, at most, a tube thoracostomy
- The most important determinant of outcome is the presence or absence of significant
associated injuries of the central nervous system, abdomen, and pelvis
- Some injuries, such as cardiac chamber rupture, thoracic aortic rupture, injuries of the
intrathoracic IVC and SVC, and delayed recognition of esophageal rupture, are associated with
high morbidity and mortality
Primary spontaneous pneumothorax
General
- Commonly seen in young tall male smokers
- More common on the right side
- Less than 10% of cases are bilateral
- Usually caused by rupture of small subpleural blebs (collections of air <2cm) found at the apex
of the upper lobe or the apical segment of the lower lobe
- The rest of the lung parenchyma is normal
- May also be caused by rupture of bullae (large air-filled spaces)
Presentation
- Dyspnoea, chest pain, cough, tachypnoea
- Ipsilateral decreased chest wall movement, hyperresonant hemithorax to percussion, absent
breath sounds on auscultation, pleural rub, tachycardia
Diagnosis
- PA chest radiograph usually diagnostic
- CT scan gives an accurate estimate of size of pneumothorax and is
useful for assessment of remaining lung parenchyma and contralateral lung
Complications
- Tension pneumothorax.
- Pneumomediastinum.
- Haemopneumothorax
- Recurrent pneumothorax
Conservative Treatment
- Observation (small, <20% pneumothorax).
- Needle aspiration.
- Tube thoracostomy with/without chemical pleurodesis
Surgery
- indicated in:
- If first episode with prolonged air leak, tension pneumothorax, haemothorax,
bilateral pneumothoraces, residual collapse of lung despite non-surgical treatment, 100%
pneumothorax, occupational hazard, pneumothorax secondary to giant bulla or previous
contralateral pneumonectomy
- Recurrence of pneumothorax
- resect the blebs or bullae and obliterate the pleural space with adhesions, either using chemical
or abrasion pleurodesis or parietal pleurectomy (apical or full)
- may be performed through a mini-thoracotomy, axillary incision, or thoracoscopically
Recurrence rate
- Less than 2% following surgical pleurectomy via mini-thoracotomy
- Five per cent following thoracoscopic procedures
- Five to ten per cent following chemical pleurodesis
Page 111 of 269
Secondary spontaneous pneumothorax
Etiology
- Cystic fibrosis, chronic obstructive airways disease (COAD) and other bullous disease, asthma
- Interstitial lung disease
- Infections, including AIDS, mycobacterial, Pneumocystis carinii, bacterial, parasitic, mycotic
- Malignancy. Bronchogenic carcinoma, metastatic lung cancer (sarcoma
and lymphoma)
- Collagen diseases, catamenial, Ehlers–Danlos syndrome, histiocytosis X, scleroderma,
lymphangioleiomyomatosis, Marfan’s syndrome
- Rupture of the oesophagus
- Catamenial pneumothorax (occurring in conjunction with menstrual periods believed to be
caused primarily by endometriosis of the pleura)
Cystic fibrosis
- Pneumothorax found in 10% of patients
- Remember these patients are possible candidates for future lung transplantation when
considering management options
- Full parietal pleurectomy is a contraindication to lung transplantation
COAD
- most common cause of secondary pneumothorax
- Age usually >50y
- Patients often have very little pulmonary reserve
- They may not tolerate surgical management and single lung ventilation
- Treatment options are therefore tube thoracoscopy and chemical pleurodesis or long-term tube
thoracoscopy
AIDS
- Usually secondary to Pneumocystis carinii and pneumonia
- May be presenting feature of AIDS
- Most effective treatment is surgical
Catamenial
- Age 20–30y
- Incidence 3–6% of women
- Occurs 2–3 days following onset of menstruation
- Right side more commonly affected
- Usually small, presenting with dyspnoea and chest pain
Primary spontaneous pneumomediastinum
General
- Uncommon, Males affected more frequently than females
- Occurs following exertion or increased intra-abdominal pressure
- Commonly associated with cocaine, marijuana, and crack cocaine usage
- caused by rupture of alveolar sacs with air tracking along the peribronchial and perivascular
spaces into the neck
Presentation
- Sudden onset of chest pain, dyspnoea, dysphagia, cough
- Subcutaneous emphysema over neck and chest wall, Hamman’s sign
- Chest radiograph confirms diagnosis
Treatment
- Non-operative, treat expectantly
- Emergency surgical decompression very rare
Page 112 of 269
40.) Open chest trauma. Complications of thoracic trauma
Open (Penetrating) chest trauma
- Thoracic injuries account for 20-25% of deaths due to trauma and contribute to 25-50% of the
remaining death
- thoracic injuries are a contributing factor in as many as 75% of all trauma-related deaths
Etiology
1. Low velocity injuries
- impalement (eg, knife wounds)
- disrupts only the structures penetrated
2. Medium velocity injuries
- bullet wounds from most types of handguns and air-powered pellet guns
- characterized by much less primary tissue destruction than wounds caused by highvelocity forces
3. High velocity injuries
- bullet wounds caused by rifles and wounds resulting from military weapons
- The amount of tissue damage is directly related to the amount of energy exchange between the
penetrating object and the body part
- The density of the tissue involved and the frontal area of the penetrating object are the
important factors determining the rate of energy loss
Anamnesis and Physical Examination
- Evaluations of vital signs, consciousness, airway competency, vascular integrity, and pump
(cardiac) function are rapidly performed before devoting attention to the point of injury.
- If the patient is stable and no significant injury is found that requires immediate surgery, a full
diagnostic evaluation can be performed
- Any entry wound below the nipples (front) and the inferior scapular angles (dorsum) should be
considered an entry point for a course that may have carried the missile into the abdominal
cavity
- Missiles from gunshot wounds (GSWs) can penetrate all body regions regardless of the point of
entry
- Any patient with a gunshot entry wound for which a corresponding exit wound cannot be
identified should be considered to have a retained projectile, which could embolize to the
central or distal vasculature
- A patient with combined intrathoracic and intra-abdominal wounds has a markedly greater
chance of dying
Acute indications for Thoracotomy
- Cardiac tamponade
- Acute hemodynamic deterioration/cardiac arrest in the trauma center
- Penetrating truncal trauma (resuscitative thoracotomy)
- Vascular injury at the thoracic outlet
- Loss of chest wall substance (traumatic thoracotomy)
- Massive air leak
- Endoscopic or radiographic evidence of significant tracheal or bronchial injury
- Endoscopic or radiographic evidence of esophageal injury
- Radiographic evidence of great vessel injury
- Mediastinal passage of a penetrating object
- Significant missile embolism to the heart or pulmonary artery
- Transcardiac placement of an inferior vena caval shunt for hepatic vascular wounds
Thoracoscopy
- video-assisted thoracoscopic surgery (VATS) was Initially promoted for the management of
retained hemothoraces and the diagnosis of diaphragmatic injury
- Now also being used by trauma and thoracic surgeons for treatment of chest wall bleeding,
diagnosis of transmediastinal injuries, pericardial window, and persistent pneumothoraces
- The major contraindication for VATS is hemodynamic instability.
Page 113 of 269
TREATMENT
Primary survey
Tension pneumothorax
- A clinical diagnosis. There is no time for X-rays
- Patient has respiratory distress, is tachycardic and hypotensive
- Look for tracheal deviation, decreased movement, hyperresonant percussion note, and absent
breath sounds over affected hemithorax
- Treat with immediate decompression. Insert a 12G cannula into the second intercostal space in
the mid-clavicular line
- Follow this with insertion of an underwater seal chest drain into the fifth intercostal space
between the anterior and mid-axillary line
Open pneumothorax
- Occlude with a three-sided dressing
- Follow by immediate insertion of an intercostal drain through a separate incision
Flail chest
- Results in paradoxical motion of the chest wall
- Hypoxia is caused by restricted chest wall movement and underlying lung contusion
- If the segment is small and respiration is not compromised, nurse patient in HDU with adequate
analgesia
- Encourage early ambulation and vigorous physiotherapy
- Do regular blood gas analysis
- In more severe cases, endotracheal intubation with positive pressure ventilation is required
Massive haemothorax
- Accumulation of >1500mL of blood in pleural cavity
- Suspect when shock is associated with dull percussion note and absent breath sounds on one
side of chest
- Simultaneously restore blood volume and carry out decompression by inserting a wide bore
chest drain
- Consider need for urgent thoracotomy to control bleeding if there is continued brisk bleeding
and need for persistent blood transfusion
Cardiac tamponade
- Most commonly results from penetrating injuries, but blood can also accumulate in pericardial
sac after blunt trauma
- Recognize by haemodynamic instability
- => Hypotension, tachycardia, raised JVP, pulsus paradoxus, and faint heart sounds
- If critically ill with suspected tamponade, perform ‘blind’ pericardiocentesis and call
cardiothoracic or general surgeons to consider emergency thoracotomy
- If unwell, but responding to treatment, arrange urgent transthoracic echo or focused abdominal
ultrasound in A&E
Secondary Survey
- Perform a further in-depth examination
- In stab injuries, expose the patient fully and position them so that you can assess front, back,
and sides of the chest for any wounds missed in the primary survey
- An erect CXR looking for the following injuries:
Simple pneumo/haemothorax
- Treat with a chest drain if large or symptomatic or in any patient likely to undergo GA.
Pulmonary contusion
- Most common potentially lethal chest injury
- Risk of worsening associated consolidation and local pulmonary oedema
- Treat with analgesia, physiotherapy, and oxygenation
- Consider respiratory support for a patient with significant hypoxia
Page 114 of 269
Tracheobronchial rupture
- Suspect when there is persistent large air leak after chest drain insertion
- Seek immediate (cardiothoracic) surgical consultation
- Thoracic CT scan usually diagnostic
Blunt cardiac injury
- Suspect when there are significant abnormalities on ECG or echocardiography
- Seek cardiological/cardiothoracic surgical advice
Aortic disruption
- Patients survive immediate death because the haematoma is contained.
- Suspect when history of decelerating force and where there is widened mediastinum on CXR
- Thoracic CT scan is diagnostic
- Consider cardiothoracic surgical referral
Diaphragmatic rupture
- Usually secondary to blunt trauma in restrained car passengers (seat belt compression causes
‘burst’ injury commonly on the left side)
- Suspect in patient with a suitable history and a raised left hemidiaphragm on CXR.
- Penetrating trauma below the fifth intercostal space can produce a perforation
- Thoracoabdominal CT scan usually diagnostic
Complications of thoracic trauma
Retained pulmonary parenchymal foreign bodies
- The decision to remove a retained foreign body depends on its size, its location, and any
specific problems
- Objects larger than 1.5 cm in diameter, centrally located missiles, irregularly shaped objects,
and missiles associated with evidence of contamination may be prophylactically removed
- such removal is best performed 2-3 weeks following the acute injury
Chest wall hernia
- usually a complication of thoracotomy
- patient presents with pain and an obvious defect
- occasionally a lung may be entrapped and become necrotic
- Management includes resection of nonviable tissue and closure with tissue flaps or artificial
material
Post-traumatic lung cyst
- usually manifests as a well-circumscribed, rounded, central air cavity identified on chest
radiographs or CT scans
- Most do not require specific treatment and resolve spontaneously within a few weeks
- Patients with secondary infection present with a lung abscess
- => should be treated with standard therapy, including antibiotics and drainage.
Pulmonary hematoma
- Hematomas form in 4-11% of patients with pulmonary contusions
- Symptoms of fever and hemoptysis usually abate in 1 week, though chest radiograph findings
usually demonstrate resolution within 4 weeks
- associated with an increased prevalence of abscess formation.
Systemic air embolism
- usually described following central penetrating lung injury
- Air can enter the left side of the heart through bronchial and pulmonary venous fistulae and
embolize to the coronary and systemic circulations
- A precipitating factor is often the institution of PPV with resulting air being forced into the lowpressure pulmonary venules
- Embolism can also occur with any thoracic great vessel injury
Page 115 of 269
- Manifestations include seizures, arrhythmias, and cardiac arrest
- Resuscitation requires thoracotomy, clamping of the pulmonary hilum, and aspiration of air from
the left ventricle and ascending aorta
Bronchial stricture
- Missed tracheobronchial laceration may result in significant strictures
- Patients present with variable degrees of dyspnea
- Evaluation with bronchoscopy and CT
- treatment with open operative repair or stenting
Tracheoesophageal fistula
- Delayed tracheoesophageal fistula is rare, generally manifesting approximately 10 days
following injury
- possibly from delayed necrosis following a blast injury
- Usually, the airway at or just above the carina is involved
- The timing of surgery or intervention is unclear and depends on the degree of ventilatory leak
and the overall condition of the patient
Prognosis
- The outcomes of treating patients with PCT are directly related to the extents of patients'
injuries and the timeliness of initiation of treatments
- Patients arriving in a stable condition may expect full recovery, but patients presenting with
lesser levels of stability have diminishing probabilities of survival
- No attempt should be made to resuscitate, let alone definitively treat, patients presenting with
no vital signs or with obviously nonsurvivable injuries (eg, massive cardiac destruction)
41.) Diseases of the esophagus: diverticulosis, strictures, Berretts esophagus
Diverticula
- Esophageal diverticula are categorized by location with the most common being epiphrenic,
hypopharyngeal (Zenker’s), and midesophageal
- Epiphrenic and Zenker's diverticula are false diverticula involving herniation of the mucosa and
submucosa through the muscular layer of the esophagus
- => result from increased intraluminal pressure associated with distal obstruction
- In the case of Zenker, the obstruction is a stenotic cricopharyngeus muscle (upper esophageal
sphincter) and the hypopharyngeal herniation most commonly occurs in an area of natural
weakness proximal to the cricopharyngeus known as Killian's triangle
- Small Zenker's diverticula are usually asymptomatic, but when they enlarge sufficiently to retain
food and saliva they can be associated with dysphagia, halitosis and aspiration
- Treatment is by surgical diverticulectomy and criopharyngeal myotomy or a marsupialization
procedure in which an endoscopic stapling device is used to divide the cricopharyngeus.
- Epiphrenic diverticula are usually associated with achalasia or a distal esophageal stricture
- Midesophageal diverticula may be caused by traction from adjacent inflammation (classically
tuberculosis) in which case they are true diverticula involving all layers of the esophageal wall,
or by pulsion associated with esophageal motor disorders
- Midesophageal and epiphrenic diverticula are usually asymptomatic until they enlarge
sufficiently to retain food and cause dysphagia and regurgitation
- Symptoms attributable to the diverticula tend to correlate more with the underlying esophageal
disorder than the size of the diverticula
- Large diverticula can be removed surgically, usually in conjunction with a myotomy if the
underlying cause is achalasia
- Diffuse intramural esophageal diverticulosis is a rare entity that results from dilatation of the
excretory ducts of submucosal esophageal glands
- Esophageal candidiasis and proximal esophageal strictures are commonly found in association
with this disorder
Page 116 of 269
Strictures
- A benign esophageal stricture, or peptic stricture, is a narrowing or tightening of the esophagus
that causes swallowing difficulties
- can be caused by or associated with gastroesophageal reflux disease, esophagitis, a
dysfunctional lower esophageal sphincter, disordered motility, lye ingestion, or a hiatal hernia
- Strictures can form after esophageal surgery and other treatments such as laser therapy or
photodynamic therapy
- While the area heals, a scar forms, causing the tissue to pull and tighten, leading to difficulty in
swallowing
- can be diagnosed with an X-ray while the patient swallows barium (called a barium study of the
esophagus), by a computerized tomography scan, a biopsy,or by an endoscopy
- Symptoms of esophageal strictures include heartburn, bitter or acid taste in the mouth,
choking, coughing, shortness of breath, frequent burping or hiccups, pain or trouble
swallowing, throwing up blood, or weight loss
Barretts esophagus
- refers to an abnormal change in the cells of the lower portion of the esophagus
- characterized by the replacement of the normal stratified squamous epithelium lining of the
esophagus by simple columnar epithelium with goblet cells
- The medical significance of Barrett's esophagus is its strong association (0.1 per 1 cm Prague
C>M> total segment length per patient-year) with esophageal adenocarcinoma, a very often
deadly cancer, because of which it is considered to be a
- The main cause of Barrett's esophagus is thought to be an adaptation to chronic acid exposure
from reflux esophagitis
- The condition is found in 5–15% of patients who seek medical care for heartburn
(gastroesophageal reflux disease), although a large subgroup of patients with Barrett's
esophagus do not have symptoms
- Diagnosis requires endoscopy (more specifically, esophagogastroduodenoscopy, a procedure
in which a fibreoptic cable is inserted through the mouth to examine the esophagus, stomach,
and duodenum) and biopsy
- The cells of Barrett's esophagus, after biopsy, are classified into four general categories:
1. nondysplastic
2. low-grade dysplasia
3. high-grade dysplasia
4. carcinoma
- High-grade dysplasia and early stages of adenocarcinoma can be treated by endoscopic
resection and new endoscopic therapies such as radiofrequency ablation
- advanced stages (submucosal) are generally advised to undergo surgical treatment
- Nondysplastic and low-grade patients are generally advised to undergo annual observation
with endoscopy, with radiofrequency ablation as a therapeutic option
- In high-grade dysplasia, the risk of developing cancer might be at 10% per patient-year or
greater
- the value of endoscopic ablation of dysplastic lesions in an area of Barrett’s esophagus on
reducing subsequent mortality from esophageal carcinoma is uncertain
- Some experts have advocated fundoplica- tion surgery (i.e., the removal of the
gastroesophageal junction) as a means of cancer prevention in patients with Barrett’s
esophagus
42.) Achalasia: diagnosis, differential diagnosis, treatment
General
- a rare disease caused by loss of ganglion cells within the esophageal myenteric plexus with a
population incidence of about 1 : 1 00,000
- usually presents between age 25 and 60
- involves both excitatory (cholinergic) and inhibitory (nitric oxide) ganglionic neurons
- Functionally inhibitory neurons mediate deglutitive lower esophageal sphincter (LES) relaxation
and the sequential propagation of peristalsis
- Their absence leads to impaired deglutitive LES relax ation and absent peristalsis
Page 117 of 269
- Increasing evidence suggests that the ultimate cause of ganglion cell degeneration in achalasia
is an autoimmune process attributable to a latent infection with human herpes simplex virus 1
combined with genetic susceptibility
Clinical Manifestation
- Long-standing achalasia is characterized by progressive dilatation and sigmoid deformity of the
esophagus with hypertrophy of the LES
- Clinical manifestations may include dysphagia, regurgitation, chest pain and weight loss
- Most patients report solid and liquid food dysphagia
- Regurgitation occurs when food, fuid and secretions are retained in the dilated esophagus
- Patients with advanced achalasia are at risk for bronchitis, pneumonia or lung abscess from
chronic regurgitation and aspiration
- Chest pain is frequent early in the course of achalasia thought to result from esophageal spasm
- Patients describe a squeezing, pressure-like retrosternal pain sometimes radiating to the neck,
arms, jaw and back
- Paradoxically, some patients complain of heartburn that may be a chest pain equivalent
- Treatment of achalasia is less effective in relieving chest pain than it is in relieving dysphagia or
regurgltation
Diagnosis
- diagnosed by barium swallow x-ray and/or esophageal manometry
- endoscopy has a relatively minor role other than to exclude pseudoachalasia
- The barium swallow x-ray appearance is of a dilated esophagus with poor emptying, an air- uid
level and tapering at the LES giving it a beak-like appearance
- In long-standing achalasia the esophagus may assume a sigmoid configuration
- The diagnostic αiteria for achalasia with esophageal manometry are impaired LES relaxation
and absent peristalsis
- High-resolution manometry has somewhat advanced this diagnosis; three subtypes of
achalasia are differentiated based on the pattern of pressurization in the nonperistaltic
esophagus
- Because manometry identifies early disease before esophageal dilatation and food retention,
it is the most sensitive diagnostic test.
Treatment
- There is no known way of preventing or reversing achalasia
- Therapy is directed at reducing LES pressure so that gravity and esophageal pressurization
promote esophageal emptying
- Peristalsis rarely if ever recovers
- in many instances, remnants of peristalsis masked by esophageal pressurization and dilatation
prior to therapy are demonstrable following effective treatment
- LES pressure can be reduced by pharmacologic therapy, pneumatic balloon dilatation or
surgical myotomy
- No large, controlled trials of the therapeutic alternatives exist and the optimal approach is
debated
- Pharmacologic therapies are relatively ineffective but are often used as temporizing therapies
- Nitrates or calcium channel blockers are administered before eating advising caution because
of their effects on blood pressure
- Botulinum toxin, injected into the LES under endoscopic guidance, in acetocholine release
from nerve endings and improves dysphagia in about 66% of cases for at least 6 months
- Sildena l and alternative phosphodiesterase inhibitors effectively decrease LES pressure, but
practicalities limit their clinical use in achalasia
- The only durable therapies for achalasia are pneumatic dilatation and Heller myotomy
- Pneumatic dilatation with a reported efficacy ranging from 32-98% is an endoscopic technique
using a noncompliant, cylindrical balloon dilator positioned across the LES and inflated to a
diameter of 3-4 cm
- The major complication is perforation with a reported incidence of 0.5-5%
- The most common surgical procedure for achalasia is laparoscopic Heller myotomy usually
performed in conjunction with an antireflux procedure (partial fundoplication)
- => good to excellent results are reported in 62- 1 00% of cases
Page 118 of 269
- A European randomized controlled trial demonstrated an equivalent response rate of
-
approximately 90% for both pneumatic dilation and laparoscopic Heller myotomy at 2-year
follow-up
Occasionally patients with advanced disease fail to respond to pneumatic dilatation or Heller
myotomy
=> In such refractory cases esophageal resection with gastric pull-up or interposition of a
segment of transverse colon may be the only option other than gastrostomy feeding.
An endoscopic approach to LES myotomy has been introduced referred to as per oral
esophageal myotomy
=> involves the creation of a tunnel within the esophageal wall through which the circular
muscle of the LES and distal esophagus are transected with electrocautery
43.) Tumors of the esophagus
General
- Esophageal cancer is about 10 times less common than colorectal cancer but kills about onequarter as many patients
- These statistics emphasize both the rarity and lethality of esophageal cancer
- One notable trend is the shift of dominant esophageal cancer type from squamous cell to
adenocarcinoma, strongly linked to reflux disease and Barrett's metaplasia
- Other distinctions between cell types are the predilection for adenocarcinoma to affect the
distal esophagus in white males and squamous cell to affect the more proximal esophagus in
black males with the added risk factors of smoking, alcohol consumption, caustic injury and
human papilloma virus infection
Clinical Manifestation
- The typical presentation of esophageal cancer is of progressive solid food dysphagia and
weight loss
- Associated symptoms may include odynophagia, iron deficiency and with midesophageal
tumors, hoarseness from left recurrent laryngeal nerve injury
- Generally these are indications of locally invasive or even metastatic disease manifest by
tracheoesophageal stulas and vocal cord paralysis
- Even when detected as a small lesion esophageal cancer has poor survival because of the
abundant esophageal lymphatics leading to regional lymph node metastases
- Benign esophageal tumors are uncommon and usually discovered incidentally
- In decreasing frequency of occurrence, cell types include leiomyoma, fibrovascular polyps,
squamous papilloma, granular cell tumors, lipomas, neurofibromas and inflammatory fibroid
polyps
- => These generally become symptomatic only when they are associated with dysphagia and
merit removal only under the same circumstances
Types
- Esophageal cancers are typically carcinomas that arise from the epithelium of the esophagus
- Most esophageal cancers fall into one of two classes: esophageal squamous-cell carcinomas
(ESCC), which are similar to head and neck cancer in their appearance and association with
tobacco and alcohol consumption—and esophageal adenocarcinomas (EAC), which are often
associated with a history of GERD and Barrett's esophagus
- A rule of thumb is that a cancer in the upper two-thirds is likely to be ESCC and one in the
lower one-third EAC
- Rare histologic types of esophageal cancer include different variants of squamous-cell
carcinoma, and non-epithelial tumors, such as leiomyosarcoma, malignant melanoma,
rhabdomyosarcoma and lymphoma, among others
Squamous cell carcinoma
- The two major risk factors for esophageal squamous-cell carcinoma are tobacco (smoking or
chewing) and alcohol
- The combination of tobacco and alcohol has a strong synergistic effect
- Risks associated with alcohol appear to be linked to its aldehyde metabolite and to mutations
in certain related enzymes
Page 119 of 269
- Other relevant risk factors include regular consumption of very hot drinks (over 65 °C or 149 °F)
and ingestion of caustic substances
- Other associated factors include nutritional deficiencies, low socioeconomic status, and poor
oral hygiene
Adenocarcinoma
- Male predominance is particularly strong in this type of esophageal cancer, which occurs about
7 to 10 times more frequently in men
- This imbalance may be related to the characteristics and interactions of other known risk
factors, including acid reflux and obesity
- The long-term erosive effects of acid reflux (an extremely common condition, also known as
gastroesophageal reflux disease or GERD) have been strongly linked to this type of cancer
Diagnosis
- Although an occlusive tumor may be suspected on a barium swallow or barium meal, the
diagnosis is best made with an examination using an endoscope
(esophagogastroduodenoscopy)
- Biopsies taken of suspicious lesions are then examined histologically for signs of malignancy
- Additional testing is needed to assess how much the cancer has spread
- Computed tomography (CT) of the chest, abdomen and pelvis can evaluate whether the cancer
has spread to adjacent tissues or distant organs
Staging
- Staging is based on the TNM staging system, which classifies the amount of tumor invasion (T),
involvement of lymph nodes (N), and distant metastasis (M)
T1
Limited to mucosa and submucosa
T2
Extension into but not through muscularis propria
T3
Invasion of perirectal fat
T4
Invasion of adjacent structures
N0
No involved lymph nodes
N1
Fewer than 4 regional lymph nodes positive for tumor
N2
More than 4 regional lymph nodes positive for tumor
M0
No metastasis
DM1
Distant metastasis
Treatment
- Adequate nutrition must be assured, and appropriate dental care is essential
- Factors that influence treatment decisions include the stage and cellular type of cancer (EAC,
ESCC, and other types), along with the person's general condition and any other diseases that
are present
- In general, treatment with a curative intention is restricted to localized disease, without distant
metastasis: in such cases a combined approach that includes surgery may be considered.
- Disease that is widespread, metastatic or recurrent is managed palliatively
- => chemotherapy may be used to lengthen survival, while treatments such as radiotherapy or
stenting may be used to relieve symptoms and make it easier to swallow
Surgery (Esophagectomy)
- is the removal of a segment of the esophagus
- as this shortens the length of the remaining esophagus, some other segment of the digestive
tract is pulled up through the chest cavity and interposed
Page 120 of 269
- This is usually the stomach or part of the large intestine (colon) or jejunum
- Reconnection of the stomach to a shortened esophagus is called an esophagogastric
anastomosis
- Esophagectomy can be performed using several methods
- The choice of the surgical approach depends on the characteristics and location of the tumor,
and the preference of the surgeon
- Clear evidence from clinical trials for which approaches give the best outcomes in different
circumstances is lacking
- A first decision, regarding the point of entry, is between a transhiatial and a transthoracic
procedure
- The more recent transhiatial approach avoids the need to open the chest; instead the surgeon
enters the body through an incision in the lower abdomen and another in the neck
- The lower part of the esophagus is freed from the surrounding tissues and cut away as
necessary
- The stomach is then pushed through the esophageal hiatus (the hole where the esophagus
passes through the diaphragm) and is joined to the remaining upper part of the esophagus at
the neck
44.) Emergencies in cardiovascular surgery
Cardiopulmonary arrest
General
- a sudden and unexpected loss of perfusing pulsatile blood flow attributable to cessation of
cardiac mechanical activity
- occurs as a result of a multitude of cardiovascular, metabolic, infectious, neurologic,
inflammatory, and traumatic diseases
- These diseases can be generally classified into 5 H's and 5 T's (Hypovolemia, Hypoxemia,
Hydrogen ion (acidosis), Hypo- or Hyperkalemia, Hypothermia, Tension pneumothorax,
Tamponade, Toxins, and Thrombosis–both pulmonary and cardiac)
- The endpoint of these disorders is commonly pulseless ventricular tachycardia (VT) or
ventricular fibrillation (VF), pulseless electrical activity, or asystole
Pulseless VT of VF
1. Start chest compressions as early as cardiopulmonary arrest is identified. Place airway device
as soon as possible and confirm oxygenation and ventilation. Establish IV access, identify
rhythm, and administer drugs appropriate for rhythm and condition. Search for and treat
identified reversible causes (5 H's and 5 T's), with focus on basic CPR and early defibrillation
2. On arrival to an unwitnessed cardiac arrest or downtime longer than 4 minutes, five cycles (~2
min) of CPR (each cycle is 30 compressions at a rate of ~100 compressions per minute) are to
be initiated before evaluation of rhythm. If the cardiac arrest is witnessed or downtime is
shorter than 4 minutes, one shock may be administered immediately if the patient is in VF or
pulseless VT followed by five cycles of CPR.
3. If the patient is in VF or pulseless VT, shock the patient once using 200 J on biphasic (on
equivalent monophasic, 360 J).
4. Resume CPR immediately after attempted defibrillation, beginning with chest compressions.
Rescuers should not interrupt chest compression to check circulation (e.g., evaluate rhythm or
pulse) until five cycles or 2 minutes of CPR have been completed.
5. If there is persistent or recurrent VT or VF despite several shocks and cycles of CPR, perform
a secondary ABC survey with a focus on more advanced assessments and pharmacologic
therapy. Pharmacologic therapy should include epinephrine (1 mg IV push, repeated every 3-5
min) or vasopressin (a single dose of 40 U IV, one time only).
6. Consider using antiarrhythmics for persistent or recurrent pulseless VT or VF. These include
amiodarone, lidocaine, magnesium, and procainamide
7. Resume CPR and attempts to defibrillate
8. If spontaneous circulation returns, start immediate post-cardiac arrest care. This includes
optimization of oxygenation and ventilation with emphasis on avoiding hyperventilation,
treating hypotension by starting vasopressor infusion or inserting intra-aortic balloon pump,
assessing neurologic status and starting induced hypothermia if indicated and assessing need
for coronary reperfusion if high suspicion for acute coronary syndrome
Page 121 of 269
Asystole
1. Assess the patient and begin chest compressions immediately.
2. Administer epinephrine (1 mg IV push repeated every 3-5 min). Consider transcutaneous
pacing if asystole
3. Conduct a secondary ABC survey and consider reversible causes (5 H's and 5 T’s)
4. Resume immediate post-cardiac arrest care if there is a return of spontaneous circulation as
above
Bradycardia
1. Heart rate typically <50 beats per minute.
2. Identify and treat underlying cause if patient is stable (5 H's and 5 T’s).
3. Check for serious signs of low cardiac output due to bradycardia such as hypotension, altered
mental status, or acute heart failure.
4. If serious signs or symptoms are present, begin the following intervention sequence:
a
Atropine, 0.5 mg, up to a total of 3 mg IV
b
Transcutaneous pacing, if available
c
Dopamine, 5 to 20 µg/kg/min
d
Epinephrine, 2 to 10 µ/min
e
Isoproterenol, 2 to 10 µ/min
f
Consider glucagon for beta-blocker toxicity, calcium infusion for calcium channel
blocker toxicity
5. If no serious signs or symptoms are present, evaluate for a type II second-degree
atrioventricular block or third-degree atrioventricular block.
6. If neither of these types of heart block is present, observe.
7. If one of these types of heart block is present, prepare for transvenous pacing.
8. Resume immediate post-cardiac arrest care if there is a return of spontaneous circulation as
above
Hypertensive emergency
General
- an acute, severe elevation in blood pressure accompanied by end-organ compromise
- usually associated with a systolic blood pressure (SBP) equal to or higher than 180 mm Hg
and/or a diastolic blood pressure (DBP) equal to or higher than 120 mm Hg
- End-organ compromise includes acute renal failure due to nephrosclerosis, ocular involvement
with retinal exudates, hemorrhages, or papilledema, hypertensive encephalopathy, acute stroke
or intracranial hemorrhage, acute myocardial infarction, aortic dissection, and eclampsia
- Hypertensive encephalopathy signals the presence of cerebral edema and loss of vascular
integrity
- If left untreated, hypertensive encephalopathy may progress to seizure and coma
- Aortic dissection is associated with severe elevations in systemic blood pressure and wall
stress, requiring immediate lowering of the blood pressure and emergent surgery for type A
dissection to reduce morbidity and mortality
- Eclampsia, the second most common cause of maternal death, occurs from the second
trimester to the peripartum period
- It is characterized by the presence of seizures, coma, or both, in the setting of preeclampsia
- Delivery remains its only cure
Etiology
- result from an exacerbation of previously uncomplicated hypertension
- or have a secondary cause, including renal, vascular, pregnancy-related, pharmacologic,
endocrine, neurologic, and autoimmune etiologies
Evaluation
- The symptoms and signs of a hypertensive emergency vary widely
- symptoms of end-organ involvement include headache, blurred vision, confusion, chest pain,
shortness of breath, back pain (e.g., aortic dissection), seizures, and altered consciousness
- Physical examination should assess end-organ involvement, including detailed fundoscopic,
neurologic, and cardiovascular examinations, with emphasis on the presence of congestive
heart failure and bilateral upper extremity blood pressure measurements
Page 122 of 269
- Laboratory evaluation should include measurement of the complete blood count with
differential and smear evaluations, measurements of electrolyte, blood urea nitrogen, and
creatinine levels, and electrocardiography, chest radiography, and urinalysis
Treatment
1. Pharmacologic
- IV vasodilator therapy to achieve a decrease in mean arterial pressure (MAP) of 20% to
25% or a decrease in DBP to 100 to 110 mm Hg within the first 24 hours is recommended
- Decreasing the MAP and DBP further should be done more slowly, over a period of days,
because of the risk of decreasing perfusion of end organs
- Several drugs have proved beneficial in achieving this goal
- Example: Nitroglycerin 5- 200 µg/kg/min
2. Surgery
- In addition to reducing MAP and DBP with medications as described above, early surgical
intervention for type A dissection has been proven to reduce morbidity and mortality
- Reduction in shear stress is best achieved with IV beta blockade and SNP
Aortic dissection
General
- a tear of the aortic intima that allows the shear forces of blood flow to dissect the intima from
the media and, in some cases, penetrate the diseased media with resultant rupture and
hemorrhage
- Sixty-five percent of dissections originate in the ascending aorta, 20% in the descending aorta,
10% in the aortic arch, and the remainder in the abdominal aorta
- The most commonly used old classification system is the Stanford system; a dissection that
involves the ascending aorta is classified as type A, and one that does not, only affecting the
aorta distal to the left subclavian artery, is classified as type B
- Dissections are further classified by chronicity as acute (<2 weeks) or chronic (>2 weeks)
- mortality peaks at 80% after 2 weeks, and then levels off
Etiology
- Any disease that weakens the aortic media predisposes patients to dissection
- These include aging, hypertension, Marfan syndrome, Ehlers-Danlos syndrome, Loeys-Dietz
syndrome, bicuspid aortic valve (associated with medial degeneration), coarctation, and
Turner's syndrome
- Pregnancy poses a unique risk to women with any of these diseases because of increased
blood volume, cardiac output, and shear forces on the aorta
Clinical presentation
- Most patients present with acute chest pain that peaks in intensity at onset, and is often selfdescribed as "tearing" or "ripping" in nature
- Uncommonly, patients present with congestive heart failure from accompanying acute aortic
valve insufficiency, tamponade, or both
- Also seen are cerebrovascular accidents due to involvement of the carotid artery or
vertebrobasilar system, syncope from tamponade, or cardiac arrest
- On physical examination, hypertension is usually present, either as the primary cause of
dissection or secondary to renal artery involvement
- Acute aortic valve insufficiency with a resultant diastolic murmur may complicate ascending
dissections
- Loss of pulse, decrease in blood pressure, or both (often asymmetric) are also found in many
patients
- Dissection into the spinal arteries, although rare, may produce secondary paraplegia
Diagnosis
- The sensitivity of computed tomography angiography (CTA) for detecting aortic dissection is
approximately 83% to 100%, and its specificity ranges from 87% to 100%, depending on the
study.
Page 123 of 269
- In the current age of ECG-gated CTA, the sensitivity and specificity for detecting dissections
approaches 100%, and thus it is the diagnostic imaging modality of choice
Treatment
1. Surgery
- the best option for acute aortic dissection involving the ascending aorta
- Studies have shown that delaying surgical intervention, even to carry out left heart
catheterization, aortography, or both, results in worse outcomes
- Mortality increases by 1% per hour while waiting for surgery
- Surgical repair in patients with type B dissection is generally reserved for those with end-organ
compromise or those who do not respond to medical therapy.
2. Medical therapy
- should be initiated in all patients with acute dissection
- Reductions of shear force and blood pressure should be the primary goals
- Beta-blockers should be given intravenously and titrated to the desired effect
- In the US they typically start by using boluses of IV metoprolol to achieve a heart rate of 50 to
60 beats/min, which may require very high doses of 200 to 1,000 mg.
- => then add SNP if needed because of its rapid onset and ease of titration, aiming for a MAP of
65 to 75 mm Hg
Acute pulmonary edema
General
- an emergency that necessitates admission to the hospital
- has two major forms, cardiogenic and noncardiogenic
- focus on cardiogenic pulmonary edema, which generally is more reversible than the
noncardiogenic form
- Cardiogenic pulmonary edema results from an absolute increase in left atrial pressure, with
resultant increases in pulmonary capillary and venous pressures
- In the setting of normal capillary permeability, this increased pressure causes extravasation of
fluid into the alveoli and overwhelms the ability of the pulmonary lymphatics to drain the fluid,
thus impairing gas exchange in the lung
Pathophysiology
- Left ventricular systolic dysfunction, left ventricular diastolic dysfunction, and obstruction of the
left atrial outflow tract are the primary causes of increased left atrial pressure
- Left ventricular systolic dysfunction is the most common cause of cardiogenic pulmonary
edema
- => can be the result of coronary artery disease, hypertension, valvular heart disease,
cardiomyopathy, toxins, endocrinologic or metabolic causes, or infections
- Diastolic dysfunction results in impaired left ventricular filling and elevation in left ventricular
end-diastolic pressure. In addition to myocardial ischemia, left ventricular hypertrophy,
hypertrophic obstructive cardiomyopathy, and infiltrative or restrictive cardiomyopathy are all
causes of diastolic dysfunction
- Left atrial outflow obstruction is often a result of valvulopathy, such as mitral stenosis or mitral
regurgitation, but also can be caused by tumors (atrial myxoma), dysfunctional prosthetic
valves, thrombus, and cor triatriatum
- It is imperative to distinguish between mitral regurgitation and mitral stenosis, given their very
different treatments
Diagnosis
- Pulmonary edema is diagnosed by the presence of various signs and symptoms, including
tachypnea, tachycardia, crackles (reflecting alveolar edema), hypoxia (secondary to alveolar
edema), and the S3 or S4 heart sounds, individually or in combination
- Additionally, if hypertension is present, it may represent diastolic dysfunction, decreased left
ventricular compliance, decreased cardiac output, and increased systemic vascular resistance
- The presence of increased jugular venous pressure indicates increased right ventricular filling
pressure secondary to right ventricular or left ventricular dysfunction
- Finally, the presence of peripheral edema indicates a certain degree of chronicity to the
patient's condition
Page 124 of 269
Treatment
- Mainstays of immediate therapy include improving oxygen delivery to end organs, decreasing
myocardial oxygen consumption, increasing venous capacitance, decreasing preload and
afterload (with careful attention to MAP), and avoiding hemodynamic compromise
- All patients should receive supplemental oxygen to maximize hemoglobin oxygen saturation
- Administration of continuous positive airway pressure can increase gas exchange, and may
perhaps decrease preload via increased intrathoracic pressure
- The pharmacologic agents most commonly used in the treatment of acute pulmonary edema
are nitroglycerin, SNP, and diuretics
Page 125 of 269
51.) Congenital heart diseases: treatment
General
- CHD malformations are simple, intermediate or complex
- Simple defects generally are single lesions with a shunt or a valvular malformation
- Intermediate defects may have two or more simple defects
- Complex defects generally have components of an intermediate defect plus more complex
cardiac and vascular anatomy often with cyanosis and frequently with transposition complexes
- The goal of these tables is to suggest when cardiology consultation or advanced CHD specialty
care is needed
- Patients with complex CHD (which includes most "named" surgeries that usually involve
complex CHD) should virtually always be managed in conjunction with an experienced
specialty adult CHD center
- Patients with intermediate lesions should have an initial consultation and subsequent
occasional intermittent follow-up with an adult CHD specialist
- Patients with simple lesions often may be managed by a well-informed internist or general
cardiologist although consultation with a speci cally trained adult congenital cardiologist is
occasionally advisable
Simple adult congenital heart disease
1. Uncomplicated congenital aortic valve disease
2. Mild congenital mitral valve disease
3. Uncomplicated small atrial septal defect
4. Uncomplicated small ventricular septal defect
5. Mild pulmonic stenosis
Intermediate complexity congenital heart disease
1. Ostium primum or sinus venosus atrial septal defect
2. Anomalous pulmonary venous drainage, partial or total Atrioventricular canal defects (partial
or complete)
3. Ventricular septal defect complicated (e.g. absent or abnormal valves or with associated
obstructive Iesions, aortic regurgitation)
4. Coarctation of the aorta
5. Pulmonic valve stenosis (moderate to severe)
6. Infundibular right ventricular outflow obstruction of significance Pulmonary valve regurgitation
(moderate to severe)
7. Patent ductus arteriosus (nonclosed)-moderate to large
8. Sinus of Valsalva fistula/aneurysm
9. Subvalvular or supravalvular aortic stenosis
Complex adult congenital heart disease
1. Cyanotic congenital heart diseases (all forms)
2. Eisenmenger’s syndrome
3. Ebstein's anomaly
4. Tetralogy of Fallot or pulmonary atresia (all forms)
5. Transposition of the great arteries
6. Single ventricle; tricuspid or mitral atresia
7. Double-outlet ventricle
8. Truncus arteriosus
9. Fontan or Rastelli procedures
Atrial septal defect
- Atrial septal defect (ASD) is a common cardiac anomaly that may be first encountered in the
adult and occurs more frequently in females
- Sinus venosus ASD occurs high in the atrial septum near the entry of the superior vena cava
into the right atrium and is associated frequently with anomalous pulmonary venous connection
from the right lung to the superior vena cava or right atrium
- Ostium primum ASDs lie adjacent to the atrioventricular valves either of which may be
deformed and regurgitant
Page 126 of 269
- Ostium primum ASDs are common in Down's syndrome, often as part of complex
-
atrioventricular septal defects with a common atrioventricular valve and a posterior defect of
the basal portion of the interventriιular septum
The most common ostium secundum ASD involves the fossa ovalis and is mid ovale
Anatomic obliteration of the foramen ovale ordinarily follows its functional closure soon after
birth but residual "probe patency" is a common normal variant
ASD denotes a true deficiency of the atrial septum and implies functional and anatomic patency
The magnitude of the left-to-right shunt depends on the ASD size, ventricular diastolic
properties and the relative impedance in the pulmonary and systemic circulations
The left-to-right shunt causes diastolic overloading of the RV and increased pulmonary blood
flow
Patients with ASD are usually asymptomatic in early life although there may be some physical
underdevelopment and an increased tendency for respiratory infections
Beyond the fourth decade a significant number of patients develop atrial arrhythmias,
pulmonary arterial hypertension and right heart failure
Patients exposed to the chronic environmental hypoxemia of high altitude tend to develop
pulmonary hypertension at younger ages
In older patients left-to-right shunting across the ASD increases as progressive systemic
hypertension and/or coronary artery disease (CAD) result in reduced compliance of the LV
Treatment
- Operative repair, usually with a patch of pericardium or of prosthetic material or percutaneous
transcatheter device closure should be advised for all patients with uncomplicated secundum
- Excellent results may be anticipated at low risk even in patients >40 years in the absence of
severe pulmonary hypertension
- In ostium primum ASD cleft mitral valves may require repair in addition to patch closure of the
ASD
- Closure is not usually carried out in patients with small defects and trivial left-to-right shunts or
in those with severe pulmonary vascular disease without a significant left-to-right shunt.
- the use of pulmonary vasodilators with resultant reduction in pulmonary artery pressure and
resistance may allow closure of ASD in patients with pulmonary vascular disease.
- Patients with sinus venosus or ostium secundum ASDs rarely die before the fifth decade
- During the fifth and sixth decades, the incidence of progressive symptoms often leading to
severe dis ability, increases substantially
- Medical management should include prompt treatment of respiratory tract infections
- antiarrhythmic medications for atrial fibrillation or supraventricular tachycardia
- Plus the usual measures for hypertension, coronary disease or heart failure, if these
complications occur
- The risk of infective endocarditis is low and antibiotic prophylaxis is not recommended
Ventricular septal defect
- VSD is one of the most common of all cardiac birth defects either as an isolated defect or as a
component of a combination of anomalies
- The VSD is usually single and situated in the membranous or midmuscular portion of the
septum
- The functional disturbance depends on its size and on the status of the pulmonary vascular bed
- Only small- or moderate-size VSDs are seen initially in adulthood, as most patients with an
isolated large VSD come to medical or surgical attention early in life.
- the outcome ranges from spontaneous closure to congestive cardiac failure and death in
infancy
- Included within this spectrum is the possible development of pulmonary vascular obstruction,
RV out ow tract obstruction, aortic regurgitation, or infective endocarditis
- Spontaneous closure is more common in patients born with a small VSD which occurs in early
childhood in most
- The pulmonary vasιular bed is often a principal determinant of the clinical manifestations and
course of a given VSD and feasibilty of surgical repair
- Increased pulmonary arterial pressure results from increased pulmonary blood ow and/or
resistance, the latter usually the result of obstructive obliterative structural changes within the
pulmonary vascular bed
Page 127 of 269
- The term Eisenmenger's syndrome is applied to patients with a large communication between
the two circulations at the aortopulmonary, ventricular or atrial levels and bidirectional or
predominantly right-to-left shunts because of high resistance and obstructive pulmonary
hypertension
Treatment
- Closure is not recommended for patients with normal pulmonary arterial pressures with small
shunts (pulmonary-to-systemic flow ratios of <1.5:1)
- Operative correction or transcatheter closure is indicated when there is a moderate to large leftto-right shunt with a pulmonary-to-systemic flow ratio >1 .5:1 in the absence of prohibitively
high levels of pulmonary vascular resistance
Patent Ductus ateriosus
- The ductus arteriosus is a vessel leading from the bifurcation of the pulmonary artery to the
aorta just distal to the left subclavian artery
- Normally the vascular channel is open in the fetus but closes immediately after birth
- The flow across the ductus is determined by the pressure and resistance relationships between
the systemic and pulmonary circulations and by the cross-sectional area and length of the
ductus
- In most adults with this anomaly, pulmonary pressures are normal and a gradient and shunt
from aorta to pulmonary artery persist throughout the cardiac cycle => resulting in a
characteristic thrill and a continuous "machinery" murmur with late systolic accentuation at the
upper leftr sternal edge
- In adults who were born with a large left-to-right shunt through the ductus arteriosus,
pulmonary vascular obstruction (Eisenmenger's syndrome) with pulmonary hypertension,
right-to-Ieft shunting and cyanosis have usually developed
- Severe pulmonary vascular disease results in reversal of flow through the ductus
- => unoxygenated blood is shunted to the descending aorta; and the toes-but not the fingersbecome cyanotic and clubbed, a finding termed differential cyanosis
- The leading causes of death in adults with patent ductus arteriosus are cardiac failure and
infective endocarditis
- sometimes severe pulmonary vascular obstruction may cause aneurysmal dilatation,
calcification and rupture of the ductus
Treatment
- in the absence of severe pulmonary vascular disease and predominant left-to-right shunting of
blood, the patent ductus should be surgically ligated or divided
- Transcatheter closure has become common for appropriately shaped defects
- Operation should be deferred for several months in patients treated successfully for infective
endocarditis because the ductus may remain somewhat edematous and friable
Congenital aortic stenosis
- Malformations that cause obstruction to LV outflow include congenital valvular aortic stenosis,
discrete subaortic stenosis or supravalvular aortic stenosis
- Bicuspid aortic valves are more common in males than in females
- The congenital bicuspid aortic valve which may initially be functionally normal is one of the
most common congenital malformations of the heart and may go undetected in early life
- Because bicuspid valves may develop stenosis or regurgitation with time or be the site of
infective endocarditis, the lesion may be dificult to distinguish in older adults from acquired
rheumatic or degenerative calcific aortic valve disease
- The dynamics of blood flow associated with a congenitally deformed rigid aortic valve
commonly lead to thickening of the cusps and, in later life to calcifiation
- Hemodynamically significant obstruction causes concentric hypertrophy of the LV wall. The
ascending aorta is often dilated
- => this is due to histologic abnormalities of the aortic media and may result in aortic dissection
- Diagnosis is made by echocardiography which reveals the morphology of the aortic valve and
aortic root and quantitates severity of stenosis or regurgitation
Page 128 of 269
Treatment (Valvular aortic stenosis)
- In patients with diminished cardiac reserve medical management includes the administration of
digoxin and diuretics and sodium restriction while awaiting operation
- A dilated aortic root may require beta blockers, angiotensin receptor blockers or angio tensinconverting enzyme inhibitors
- Aortic valve replacement is indicated in adulzts with a critical obstruction i.e. with an aortic
valve area <0.45 cm2/m2 with symptoms secondary to LV dysfunction or myocardial ischemia
or with hemodynamic evidence of LV dysfunction
- In asymptomatic children or adolescents or young adults with critical aortic stenosis without
valvular calcification or these features, aortic balloon valvuloplasty is often useful
- If surgery is contraindicated in older patients because of a complicating medical problem such
as malignancy or renal or hepatic failure, balloon valvuloplasty may provide short-term
improvement
- This procedure may serve as a bridge to aortic valve replacement in patients with severe heart
failure
- Transcatheter aortic valve replace ment is a potential alternative to surgery
Coartctation of the aorta
- Narrowing or constriction of the lumen of the aorta may occur any where along its length but is
most common distal to the origin of the left subclavian artery near the insertion of the
ligamentum arteriosum
- Coarctation occurs in -7% of patients with CHD, is more common in males than females and is
particularly frequent in patients with gonadal dysgenesis (e.g. Turner's syndrome)
- Clinical manifestations depend on the site and extent of obstruction and the presence of
associated cardiac anomalies, most commonly a bicuspid aortic valve
- Circle of Willis aneurysms may occur in up to 10%
Treatment
- surgical or involves percutaneous catheter balloon dilatation with stent placement
- the use of transcatheter treatment techniques has increased dramatically and many previously
"surgical" cases are treated via percutaneous or hybrid techniques
- Late postoperative systemic hypertension in the absence of residual coarctation is related
partly to the duration of preoperative hyper tension
- Follow-up of rest and exercise blood pressures is important; many have systolic hypertension
only during exercise in part due to a diffuse vasculopathy and to noncompliance of the stented
or surgically reconstructed region
- AII operated or stented coarctation patients deserve a high-quality MRI or CT procedure in
follow-up
Pulmonary stenosis
- Obstruction to RV outflow may be localized to the supravalvular, valvular or subvalvular levels
or occur at a combination of these sites
- Multiple sites of narrowing of the peripheral pulmonary arteries are a feature of rubella
embryopathy and may occur with both the familial and sporadic forms of supravalvular aortic
stenosis
- Valvular pulmonic stenosis (PS) is the most common form of isolated RV obstruction
- The severity of the obstructing lesion rather than the site of narrowing is the most important
determinant ofthe clinical course
- In the presence of a normal cardiac output a peak systolic pressure gradient <30 mmHg
indicates mild PS and >50 mmHg indicates severe PS
- pressures between these limits are considered to indicate moderate stenosis
- Patients with mild PS are generally asymptomatic and demonstrate little or no progression in
the severity of obstruction with age
- In patients with more significant stenosis the severity may increase with time
- => Fatigue, dyspnea, RV failure and syncope may limit the activity of older patients in
whom moderate or severe obstruction may prevent an augmentation of cardiac output
with exercise.
- In patients with severe obstruction the systolic pressure in the RV may exceed that in the LV,
because the ventricular septum is intact
Page 129 of 269
- => RV ejection is prolonged with moderate or severe stenosis and the sound of pulmonary
valve closure is delayed and soft
- => RV hypertrophy reduces the compliance of that chamber and a force l contraction is
necessary to augment RV filling
- => A fourth heart sound; prominent a waves in the jugular venous pulse; and
ocιasionally, presystolic pulsations of the liver reflect vigorous atrial contraction
Tetralogy of Fallot
- The four components of the tetralogy of Fallot are malaligned VSD, obstruction to RV outflow,
aortic override of the VSD and RV hypertrophy due to the RVs response to aortic pressure via
the large VSD
- The severity of RV outflow obstruction determines the clinical presentation
- The severity of hypoplasia of the RV outflow tract varies from mild to complete (pulmonary
atresia)
- Pulmonary valve stenosis and supravalvular and peripheral pulmonary arterial obstruction may
coexist
- => rarely there is unilateral absence of a pulmonary artery (usually the left )
- A right-sided aortic arch and descending thoracic aorta occur in -25%.
Treatment
- Fora variety of reasons only a few adults with tetralogy of Fallot have not had some form of
previous surgical intervention
- Reoperation in adults is most commonly for severe pulmonary regurgitation or pulmonary
stenosis.
- Ventricular and atrial arrhythmias occur respectively in 15% and 25% of adults and may require
medical treatment, electrophysiologic study and ablation, defibrillator placement or
transcatheter or surgical intervention usually including pulmonary valve replacement
- Transcatheter pulmonary valve replacement is widely used in patients meeting anatomic criteria
- The aortic root has a medial tissue defect; it is commonly enlarged and associated with aortic
regurgitation
- Endocarditis remains a risk despite surgical repair
52.) Vascular trauma: complications. Pseudoaneurysm
Pseudoaneurysm
- also known as a false aneurysm
- a collection of blood that forms between the two outer layers of an artery, the muscularis
propria and the adventitia.
- usually caused by a penetrating injury to the vessel, which then bleeds, but forms a space
between the above two layers, rather than exiting the vessel+
- may be pulsatile and can resemble a true aneurysm
- A true aneurysm involves all three layers of the blood vessel
- A dissecting aneurysm is when blood from the vessel lumen tracks between the two inner
layers, the intima and the muscularis
- => can cause blockage of the flow
- A perivascular hematoma is a collection of blood that is external to the three vessel layers
- Due to being close to the vessel, it can also be pulsatile, and can be mistaken for a
pseudoaneurysm or aneurysm
- Femoral pseudoaneurysms may complicate up to 8% of vascular interventional procedures
- Small pseudoaneurysms can spontaneously clot, while others need definitive treatment
- A pseudoaneurysm may also occur in a chamber of the heart following myocardial damage due
to ischemia or trauma
- A pseudoaneurysm of the left ventricle is a potentially lethal complication from a myocardial
infarction
Page 130 of 269
Symptoms
- usually present as a painful, tender, pulsatile mass
- The overlying skin is sometimes erythematous (red)
- can sometimes be confused with abscesses
- The patient may describe a history of catheterization or trauma, and they may note that the
pulsatile mass is gradually expanding
Diagnosis
- should be suspected if the patient has a history of arterial trauma
- => can include arterial access for catheterization (i.e. the common femoral artery), blunt trauma
(i.e. to an extremity), or penetrating trauma (i.e. gunshot or blast injury)
- Blunt or penetrating trauma can cause a disruption in the arterial wall, leading to a
pseudoaneurysm
- A patient with such a history who presents with a painful, pulsatile, tender mass at the site of
catheterization or trauma should be suspected to have a pseudoaneurysm
- The diagnosis should be confirmed using Duplex ultrasonography, which will reveal arterial
blood flow into the pseudoaneurysm
- A CT angiogram or conventional angiogram can also diagnose a pseudoaneurysm
Treatment
1. Covered stent
- a covered stent may be placed endovascularly across this hole to "exclude it," or to prevent
it from receiving blood flow from the artery
- The covered stent is composed of metal and is covered with polytetrafluoroethylene (PTFE)
or another sterile fabric-like material.
- It remains in place permanently, and the pseudoaneurysm, without a continuous flow of
arterial blood, then thromboses
- Advantages of this technique are that it has a high success rate without the need for an open
surgery
- Complications include covered stent migration, persistent leakage of blood into the
pseudoaneurysm, fracturing (breaking) of the stent, and infection of the stent or of the arterial
insertion site
2. Ultrasound probe compression
- ultrasound probe compression of the neck of the pseudoaneurysm
- The "neck" of the pseudoaneurysm is the narrow path of blood flow between the artery,
through the arterial wall, and into the pseudoaneurysm cavity
- The artery, neck, and pseudoaneurysm are seen on ultrasound
- The ultrasound probe can be pushed firmly against the patient's skin to compress the
neck of the pseudoaneurysm for usually about 20 minutes
- During this time, the blood within the pseudoaneurysm clots; after the probe is then
removed, the pseudoaneurysm will hopefully remain clotted and will not continue to
expand
- The procedure may be stopped early due to patient discomfort
- is less successful if the patient is obese, since there is more fatty tissue between the skin
and the neck of the pseudoaneurysm
3. Ultrasound-guided thrombin injection
- In addition to covered stent placement, another popular, minimally-invasive technique
used today is ultrasound-guided thrombin injection
- Thrombin (factor IIa in the coagulation cascade)is a clotting factor that converts fibrinogen
into fibrin, which then polymerizes to form a blood clot
- Under ultrasound guidance, thrombin can be injected directly into a pseudoaneurysm,
causing it to clot
- Advantages are that the technique is relatively easy to perform, is successful, and is
minimally invasive
- One contraindication to this procedure is if there is an arteriovenous fistula
(communication between an artery and vein), in addition to the pseudoaneurysm
- This occurs with about 10% of pseudoaneurysms
- => If this is present, thrombin injected into the pseudoaneurysm could then enter the
venous circulation and possibly lead to distant thrombosis
Page 131 of 269
4. Surgical ligation
- Open surgery may also be performed to remove pseudoaneurysms or prevent them from
expanding
- If the artery is small and "expendable" - the tissues it supplies have adequate collateral
blood flow - then the artery supplying the pseudoaneurysm may be ligated both proximally
and distally to the pseudoaneurysm
- The pseudoaneurysm may or may not be removed
- If the tissues supplied by the artery do not have sufficient collateral flow (the artery is not
expendable), then a vein or synthetic graft would have to be anastomosed proximally and
distally to allow for continued blood flow around the pseudoaneurysm
- Advantages are that the technique has been successful for many years
- it is more invasive (a large skin incision is necessary), and there is more postoperative pain
and a risk for wound infection
- One of the less invasive options may be preferred in a patient with many comorbidities,
who is at high risk for surgery
53.) Arterial insufficiency of the extremities - acute and chronic
General
- Atherosclerosis is the most common cause of chronic arterial occlusive disease of the lower
extremities
- The arterial narrowing or obstruction that occurs as a result of the atherosclerotic process
reduces blood flow to the lower limb during exercise or at rest
- A spectrum of symptoms results, the severity of which depends on the extent of the
involvement and the available collateral circulation
- => symptoms may range from intermittent claudication to pain at rest. Intermittent claudication
denotes pain that develops in the affected limb with exercise and is relieved with rest
- => pain usually occurs distal to the arterial narrowing or obstruction
- Since the superficial femoral and popliteal arteries are the vessels most commonly affected by
the atherosclerotic process, the pain of intermittent claudication is most often localized to the
calf
- The distal aorta and its bifurcation into the two iliac arteries are the next most frequent sites of
involvement
- Narrowing of these arteries may produce pain in the buttocks or the thighs as well as the legs
Symptoms
- Painful cramping in hip, thigh or calf muscles after certain activities, such as walking or
climbing stairs (claudication)
- Leg numbness or weakness
- Coldness in the lower leg or foot, especially when compared with the other side
- Sores on toes, feet or legs that won't heal
- A change in the color of legs
- Hair loss or slower hair growth on feet and legs
- Slower growth of toenails
- Shiny skin on legs
- No pulse or a weak pulse in legs or feet
- Erectile dysfunction in men
Risk factors
- Smoking
- Diabetes
- Obesity (a body mass index over 30)
- High blood pressure
- High cholesterol
- Increasing age, especially after reaching 50 years of age
- A family history of peripheral artery disease, heart disease or stroke
- High levels of homocysteine, a protein component that helps build and maintain tissue
Page 132 of 269
Complications
1. Critical limb ischemia
- begins as open sores that don't heal, an injury, or an infection of feet or legs
- Critical limb ischemia occurs when such injuries or infections progress and can cause tissue
death (gangrene), sometimes requiring amputation of the affected limb
2. Stroke and heart attack
- atherosclerosis that causes the signs and symptoms of peripheral artery disease isn't limited to
the legs
- Fat deposits also build up in arteries supplying the heart and brain.
Diagnosis
1. Physical exam
- weak or absent pulse below a narrowed area of the artery
- whooshing sounds (bruits) over the arteries that can be heard with a stethoscope
- evidence of poor wound healing in the area where the blood flow is restricted
- decreased blood pressure in the affected limb
2. Ankle-brachial index (ABI)
- compares the blood pressure in the ankle with the blood pressure in the arm
3. Ultrasound
- Special ultrasound imaging techniques, such as Doppler ultrasound, can help evaluate
blood flow through your blood vessels and identify blocked or narrowed arteries
4. Angiography
- trace the flow of the contrast material using imaging techniques, such as X-ray imaging or
procedures called magnetic resonance angiography (MRA) or computerized tomography
angiography (CTA)
5. Blood tests
- measure cholesterol and triglycerides and check for diabetes
Surgery
1. Angioplasty
- a catheter is threaded through a blood vessel to the affected artery
- There, a small balloon on the tip of the catheter is inflated to reopen the artery and flatten
the blockage into the artery wall, while at the same time stretching the artery open to
increase blood flow
2. Bypass surgery
- create a graft bypass using a vessel from another part of the body or a blood vessel made
of synthetic fabric
- allows blood to flow around — or bypass — the blocked or narrowed artery
3. Thrombolytic therapy
- if there is clot formation, inject a clot-dissolving drug into the artery at the point of the clot
to break it up
55.) Arteriosclerosis and diabetic gangrene of the extremities
Arteriosclerosis
- a disease in which the inside of an artery narrows due to the build up of plaque
- Initially, there are no symptoms
- When severe, it can result in coronary artery disease, stroke, peripheral artery disease, or
kidney problems depending on the arteries which are affected
- Symptoms, if they occur, generally do not begin until middle age
- The exact cause is not known
- Risk factors include high blood pressure, diabetes, smoking, obesity, family history, and an
unhealthy diet
- The Plaque is made up of fat, cholesterol, calcium, and other substances found in the blood.
- The narrowing of arteries limits the flow of oxygen-rich blood to parts of the body.
- Diagnosis is based upon a physical exam, electrocardiogram, and exercise stress test among
others
- Prevention is generally by eating a healthy diet, exercise, not smoking, and maintaining a
normal weight
Page 133 of 269
Symptoms
- asymptomatic for decades because the arteries enlarge at all plaque locations, thus there is no
effect on blood flow
- Even most plaque ruptures do not produce symptoms until enough narrowing or closure of an
artery, due to clots, occurs
- Signs and symptoms only occur after severe narrowing or closure impedes blood flow to
different organs enough to induce symptoms
- Most of the time, patients realize that they have the disease only when they experience other
cardiovascular disorders such as stroke or heart attack
- Typically, atherosclerosis begins in childhood, as a thin layer of white-yellowish streaks with the
inner layers of the artery walls (an accumulation of white blood cells, mostly monocytes/
macrophages) and progresses from there
- Clinically, given enlargement of the arteries for decades, symptomatic atherosclerosis is
typically associated with men in their 40s and women in their 50s to 60s
- While coronary artery disease is more prevalent in men than women, atherosclerosis of the
cerebral arteries and strokes equally affect both sexes
Diagnosis
- Examples of anatomical detection methods include coronary calcium scoring by CT, carotid
IMT (intimal media thickness) measurement by ultrasound, and intravascular ultrasound (IVUS)
- Examples of physiologic measurement methods include lipoprotein subclass analysis, HbA1c,
hs-CRP, and homocysteine
- Both anatomic and physiologic methods allow early detection before symptoms show up,
disease staging and tracking of disease progression
- Anatomic methods are more expensive and some of them are invasive in nature, such as IVUS
- On the other hand, physiologic methods are often less expensive and safer, but they do not
quantify the current state of the disease or directly track progression
- In recent years, developments in nuclear imaging techniques such as PET and SPECT have
provided ways of estimating the severity of atherosclerotic plaques
Treatment
- treatments often focus on alleviating symptoms
- measures which focus on decreasing underlying atherosclerosis—as opposed to simply
treating symptoms—are more effective
- Non-pharmaceutical means are usually the first method of treatment, such as stopping
smoking and practicing regular exercise
- If these methods do not work, medicines are usually the next step in treating cardiovascular
diseases, and, with improvements, have increasingly become the most effective method over
the long term
1. Lifestyle changes
2. Statins
- widely prescribed for treating atherosclerosis
- have shown benefit in reducing cardiovascular disease and mortality in those with high
cholesterol with few side effects
- Monocyte counts, as well as cholesterol markers such as LDL:HDL ratio and apolipiprotein
B: apolipoprotein A-1 ratio can be used as markers to monitor the extent of atherosclerotic
regression which proves useful in guiding patient treatments
3. Surgery
- When atherosclerosis has become severe and caused irreversible ischemia, such as tissue
loss in the case of peripheral artery disease, surgery may be indicated
- Vascular bypass surgery can re-establish flow around the diseased segment of artery
- angioplasty with or without stenting can reopen narrowed arteries and improve bloodflow
- Coronary artery bypass grafting without manipulation of the ascending aorta has
demonstrated reduced rates of postoperative stroke and mortality compared to traditional
on-pump coronary revascularization
4. Other
- There is evidence that some anticoagulants, particularly warfarin, which inhibit clot
formation by interfering with Vitamin K metabolism, may actually promote arterial
calcification in the long term despite reducing clot formation in the short term
Page 134 of 269
Diabetic gangrene of the extremities
- Atherosclerotic lesions in the arteries of diabetic patients occur at sites similar to those of non
diabetic individuals (such as arterial bifurcations)
- advanced disease is more common in diabetic patients, affecting even collateral vessels
- The pathology of the affected arteries is similar in both those with and those without diabetes.
- Typical atherosclerotic lesions in diabetic patients with peripheral vascular disease include
diffuse multifocal stenosis and a predilection for the tibioperoneal arteries
- All tibial arteries may be occluded, with distal reconstitution of a dorsal pedal or common
plantar artery
- Diabetes has the greatest impact on the smaller vessels (diameter less than 5 mm) in the body
- The atherosclerotic procedure starts at a younger age and progresses more rapidly in those
who have diabetics than those who do not
- Although non - diabetic men are affected by peripheral vascular disease much more commonly
than non- diabetic women (a male- to- female ratio of 30 : 1), diabetic women are affected half
as often as diabetic men
- Gangrene is characterized by the presence of cyanotic, anesthetic tissue associated with or
progressing to necrosis
- it occurs when the arterial blood supply falls below minimal metabolic requirements
- Gangrene can be described as dry or wet, wet gangrene being dry gangrene complicated by
infection
- Amputation may often be required
56.) Primary varicosity of the extremities. Superficial thrombophlebitis
Varicose veins
- veins that have become enlarged and twisted
- commonly refers to the veins on the leg, although varicose veins can occur elsewhere
- Veins have pairs of leaflet valves to prevent blood from flowing backwards (retrograde flow or
venous reflux)
- => Leg muscles pump the veins to return blood to the heart (the skeletal-muscle pump),
against the effects of gravity
- => When veins become varicose, the leaflets of the valves no longer meet properly, and the
valves do not work (valvular incompetence)
- => allows blood to flow backwards and they enlarge even more. Varicose veins are most
common in the superficial veins of the legs, which are subject to high pressure when standing
- Besides being a cosmetic problem, varicose veins can be painful, especially when standing
- Severe long-standing varicose veins can lead to leg swelling, venous eczema, skin thickening
(lipodermatosclerosis) and ulceration
- Although life-threatening complications are uncommon, varicose veins may be confused with
deep vein thrombosis, which may be life-threatening
Complications
- generally benign, but may sometimes lead to major complications
- Pain, tenderness, heaviness, inability to walk or stand for long hours, thus hindering work
- Skin conditions / dermatitis which could predispose skin loss
- Skin ulcers especially near the ankle, usually referred to as venous ulcers.
- Development of carcinoma or sarcoma in longstanding venous ulcers. Over 100 reported cases
of malignant transformation have been reported at a rate reported as 0.4% to 1%.
- Severe bleeding from minor trauma, of particular concern in the elderly.
- Blood clotting within affected veins, termed superficial thrombophlebitis. These are frequently
isolated to the superficial veins, but can extend into deep veins, becoming a more serious
problem.
- Acute fat necrosis can occur, especially at the ankle of overweight people with varicose veins.
Females are more frequently affected than males
Diagnosis
- Trendelenburg test–to determine the site of venous reflux and the nature of the saphenofemoral
junction
- People with varicose veins now be investigated using lower limbs venous ultrasonography
Page 135 of 269
- The results from a randomised controlled trial on patients with and without routine ultrasound
have shown a significant difference in recurrence rate and reoperation rate at 2 and 7 years of
follow-up
Stages (CEAP classification)
C0
No visible or palpable signs of venous disease
C1
telangectasia or reticular veins
C2
Varicose veins
C3
Edema
C4a
Pigmentation of eczema
C4b
lipodermatosclerosis, atrophie blanche
C5
Healed venous ulcer
C6
Active venous ulcer
Etiology
- more common in women than in men, and are linked with heredity.
- Other related factors are pregnancy, obesity, menopause, aging, prolonged standing, leg injury
and abdominal straining
- Varicose veins are unlikely to be caused by crossing the legs or ankles
- Less commonly, but not exceptionally, varicose veins can be due to other causes, as post
phlebitic obstruction or incontinence, venous and arteriovenous malformations
- often caused by venous reflux
- More recent research has shown the importance of pelvic vein reflux (PVR) in the development
of varicose veins
Treatment
- can be either conservative or active
- Active treatments can be divided into surgical and non-surgical treatments
- Newer methods including endovenous laser treatment, radiofrequency ablation and foam
sclerotherapy appear to work as well as surgery for varices of the greater saphenous vein
1. Conventional
- Elevating the legs often provides temporary symptomatic relief.
- Advice about regular exercise sounds sensible but is not supported by any evidence
- The wearing of graduated compression stockings with variable pressure gradients (Class II
or III) has been shown to correct the swelling, nutritional exchange, and improve the
microcirculation in legs affected by varicose veins
- The wearing of intermittent pneumatic compression devices have been shown to reduce
swelling and increase circulation
- Diosmin/hesperidin and other flavonoids
2. Surgical
- stripping (Stripping consists of removal of all or part the saphenous vein (great/long or
lesser/short) main trunk)
- Chiva (There is tentative evidence that conservative hemodynamic correction of venous
insufficiency method (CHIVA) which works to save the veins, decreases varicose veins and
is safer than vein stripping in those with chronic venous insufficiency)
- Ambulatory phlebectomny
- Cryosurgery (cryoprobe is passed down the long saphenous vein following
saphenofemoral ligation. Then the probe is cooled with NO2 or CO2 to −85o F. The vein
freezes to the probe and can be retrogradely stripped after 5 seconds of freezing. It is a
variant of Stripping)
Page 136 of 269
Superficial thrombophlebitis
- common inflammatory-thrombotic disorder in which a thrombus develops in a vein located near
the surface of the skin
- Most superficial veins that develop thrombosis also have phlebitis, in contrast to deep venous
thrombosis (DVT), a sometimes asymptomatic condition in which phlebitis may be absent
- It is due to inflammation and/or thrombosis, and less commonly infection of the vein
- is generally a benign, self-limited disorder, however, it can be complicated by deep vein
thrombosis (DVT) and even pulmonary embolism (PE)
- Migratory superficial thrombophlebitis is known as Trousseau's syndrome
Signs and symptoms
- Findings of tenderness, induration, pain and/or erythema along the course of a superficial
veinusually establish a clinical diagnosis, especially in patients with known risk factors
- In addition, there is often a palpable, sometimes nodular cord, due to thrombus within the
affected vein
- Persistence of this cord when the extremity is raised suggests the presence of thrombus
Complications
1. Superficial vein thrombosis
- extension to the deep vein system and/or recurrence of SVT
2. Suppurative thrombophlebitis
- suspected when erythema extends significantly beyond the margin of the vein
- associated with significant fever
- if suspected, antibiotic treatment, surgical drainage and potentially vein excision are
indicated
3. Venous thromboembolism
- can occur with superficial vein thrombosis
- Estimates of the percentage of patients with SVT who also have DVT vary between 6%
and 53%, and symptomatic pulmonary embolism has been reported in 0% to 10% of
patients with SVT
Diagnosis
1. Clinical evaluation
- the primary diagnostic tool for thrombophlebitis
- Patients with thrombophlebitis complain of pain along the affected area
- Some report constitutional symptoms such as low grade fever and aches
- On physical examination, the skin over the affected vein exhibits erythema, warmth,
swelling, and tenderness
- Later in the disease, as induration subsides, erythema gives way to a ruddy or bruised
color.
2. Duplex ultrasound
- identifies the presence, location and extent of venous thrombosis
- can help identify other pathology that may be a source of the patient's complaints
- Ultrasound is indicated if superficial phlebitis involves or extends into the proximal onethird of the medial thigh, there is evidence for clinical extension of phlebitis
- lower extremity swelling is greater than would be expected from a superficial phlebitis
alone or diagnosis of superficial thrombophlebitis in question
Treatment
1. Compression stockings
- should be offered to patients with lower extremity superficial phlebitis, if not
contraindicated (e.g., peripheral artery disease)
- Patients may find them helpful for reducing swelling and pain once the acute inflammation
subsides
2. NSAIDS
- effective in relieving the pain associated with venous inflammation and were found in a
randomized trial to significantly decrease extension and/or recurrence of superficial vein
thrombosis
3. Anticoagulation
Page 137 of 269
- for patients with lower extremity superficial thrombophlebitis at increased risk for
thromboembolism
- (affected venous segment of ≥5 cm, in proximity to deep venous system, positive medical
risk factors)
4. Fondaparinux
- reduces the risk of subsequent venous thromboembolism
5. Surgery
- reserved for extension of the clot to within 1 cm of the saphenofemoral junction in patients
deemed unreliable for anticoagulation, failure of anticoagulation and patients with intense
pain
- Surgical therapy with ligation of saphenofemoral junction or stripping of thrombosed
superficial veins appears to be associated higher rates of venous thromboembolism
compared with treatment with anitcoagulants
57.) Deep vein thrombosis (DVT). Pulmonary embolism
General
- Venous thromboembolism (VTE) encompasses deep venous thrombosis (DVT) and pulmonary
embolism (PE) and causes cardiovascular death and disability
- PE is the most common preventable cause of death among hospitalized patients
- Survivors may succumb to the disabilities of chronic thromboembolic pulmonary hypertension
or postthrombotic sydrome
- Chronic thromboembolic pulmonary hypertension causes breathlessness, especially with
exertion
- Postthrombotic syndrome (also known as chronic venous insufficiency) damages the venous
valves of the leg and causes ankle or calf swelling and leg aching, especially after prolonged
standing
- In its most severe form, postthrombotic syndrome causes skin ulceration
Pathophysiology
Inflammation and platelet activation
- Virchow's triad of inflammation, hypercoagulability and endothelial injury leads to recruitment of
activated platelets which release microparticles
- These microparticles contain proin ammatory mediators that bind neutrophils, stimulating them
to release their nuclear material and form web-like extracellular networks called neutrophil
extracellular traps
- These prothrombotic networks contain histones that stimulate platelet aggregation and
promote platelet- dependent thrombin generation
- Venous thrombi form and flourish in an environment of stasis, low oxygen tension and
upregulation of proinflammatory genes
Prothrombotic states
- The two most common autosomal dominant genetic mutations are factor V Leiden, which
causes resistance to the endogenous anticoaguant, activated protein C (which inactivates clot
ting factors V and VIII) and the prothrombin gene mutation, which increases the plasma
prothrombin concentration
- Antithrombin, protein C and protein S are naturally occurring coagulation inhibitors
- Deficiencies of these inhibitors are associated with VTE but are rare
- Antiphospholipid antibody syndrome is the most common acquired cause of thrombophilia and
is associated with venous or arte rial thrombosis
- Other common predisposing factors include cancer, obesity, cigarette smoking, systemic
arterial hypertension, chronic obstructive pulmonary disease, chronic kidney disease, blood
transfusion, long-haul air travel, air pollution, oral contraceptives, pregnancy, postmenopausal
hormone replacement, surgery and trauma
Page 138 of 269
Embolization
- When deep venous thrombi detach from their site of formation, they embolize to the vena cava,
right atrium and right ventricle and lodge in the pulmonary arterial circulation, thereby causing
acute PE
- Paradoxically, these thrombi occasionally embolize to the arterial circulation through a patent
foramen ovale or atrial septal defect
- Many patients with PE have no evidence of DVT because the clot has already embolized to the
lungs
Pulmonary Hypertension, Right Ventricular Dysfunction and RV Microinfarction
- Pulmonary artery obstruction causes a rise in pulmonary artery pressure and in pulmonary
vascular resistance
- When RV wall tension rises, RV dilation and dysfunction ensue with release of the cardiac
biomarker, brain natriuretic peptide
- The interventricular septum bulges into and compresses an intrinsically normal left ven tricle
(LV)
- Diastolic LV dysfunction reduces LV distensibility and impairs LV lling
- Increased RV wall tension also compresses the right coronarγ artery, limits myocardial oxygen
supply and precipitates right coronary artery ischemia and RV microinfarction with release of
cardiac biomarkers such as troponin
- Underfilling of the LV may lead to a fall in LV cardiac output and systemic arterial pressure,
with consequent circulatory collapse and death
Classification
Pulmonary Embolism
1. Massive PE
- accounts for 5-10% of cases
- characterized by extensive thrombosis affecting at least half of the pulmonary vasculature
- Dyspnea, syncope, hypotension and cyanosis are hallmarks of massive PE
- Patients may present in cardiogenic shock and can die from multisystem organ failure
2. Submassive PE
- accounts for 20-25% of patients
- characterized by RV dysfunction despite normal systemic arterial pressure
- The combination of right heart failure and release of cardiac biomarkers indicates an
increased likelihood of clinical deterioration
- Low-risk PE constitutes about 70-75% of cases
- These patients have an excellent prognosls
Deep vein thrombosis
1. Lower extremity DVT
- usually begins in the calf
- propagates proximally to the popliteal vein, femoral vein and iliac veins
- Leg DVT is about 10 times more common than upper extremity DVT
2. Upper extremity DVT
- often precipitated by placement of pace makers, internal cardiac defibrillators or indwelling
central venous catheters
- The likelihood of upper extremity DVT increases as the catheter diameter and number of
lumens increase
3. Superficial venous thrombosis
- usually presents with erγthema, tenderness and a "palpable cord."
- Patients are at risk for extension of the thrombosis to the deep venous system
Manifestations
1. PE
- PE is known as "the Great Masquerader."
- Diagnosis is difficult because symptoms and signs are nonspecific
- The most common symptom is unexplained breathlessness
Page 139 of 269
- When occult PE occurs concomitantly with overt congestive heart failure or pneumonia,
clinical improvement often fails to occur despite standard medical treatment of the
concomitant ilIness
2. DVT
- the most common symptom is a cramp or "charley horse" in the lower calf that persists
and intensifies over several days
- Point score criteria help estimate the clinical likelihood of DVT and PE
- Patients with a low-to-moderate likelihood of DVT or PE should undergo initial diagnostic
evaluation with D-dimer testing alone without obligatory imaging tests
- patients with a high clinical likelihood of VTE should skip D-dimer testing and undergo
imaging as the next step in the diagnostic algorithm.
Diagnosis
Lab tests
1. D-dimer testing
2. Ischemia-modified albumin level
3. White blood cell count
4. Arterial blood gases
5. Serum troponin levels
6. Brain natriuretic peptide
Imaging studies
1. Computed tomography angiography (CTA): Multidetector-row CTA (MDCTA) is the criterion
standard for diagnosing pulmonary embolism
2. Pulmonary angiography: Criterion standard for diagnosing pulmonary embolism when MDCTA
is not available
3. Chest radiography: Abnormal in most cases of pulmonary embolism, but nonspecific
4. V/Q scanning: When CT scanning is not available or is contraindicated
5. ECG: Most common abnormalities are tachycardia and nonspecific ST-T wave abnormalities
6. MRI: Using standard or gated spin-echo techniques, pulmonary emboli demonstrate
increased signal intensity within the pulmonary artery
7. Echocardiography: Transesophageal echocardiography may identify central pulmonary
embolism
8. Venography: Criterion standard for diagnosing DVT
9. Duplex ultrasonography: Noninvasive diagnosis of pulmonary embolism by demonstrating the
presence of a DVT at any site
Treatment
Pulmonary Embolism
1. Risk stratification
- Thrombolytic therapy should be used in patients with acute PE associated with hypotension
(systolic BP<90 mm HG) who do not have a high bleeding risk.
- Do not delay thrombolysis in this population because irreversible cardiogenic shock can
develop
- Thrombolytic therapy is suggested in select patients with acute PE not associated with
hypotension and with a low bleeding risk whose initial clinical presentation or clinical course
after starting anticoagulation suggests a high risk of developing hypotension
- Assessment of pulmonary embolism severity, prognosis, and risk of bleeding dictate whether
thrombolytic therapy should be started
- Thrombolytic therapy is not recommended for most patients with acute PE not associated with
hypotension.
2. Anticoagulation
1. Unfractionated Heparin study
- The efficacy of heparin therapy depends on achieving a critical therapeutic level of heparin
within the first 24 hours of treatment
- The critical therapeutic level of heparin is 1.5 times the baseline control value or the upper
limit of normal range of the activated partial thromboplastin time (aPTT).
2. Low molecular weight heparin therapy
Page 140 of 269
- Current guidelines for patients with acute PE recommend LMWH over IV UFH (grade 2C)
and over SC UFH (grade 2B)
- In patients being treated with LMWH, once-daily regimens are preferred over twice-daily
regimens (grade 2C)
3. Direct thrombin inhibitors and factor Xa inhibitors
- Apixaban, dabigatran, rivaroxaban, and edoxaban are alternatives to warfarin for
prophylaxis and treatment of PE
- Apixaban, edoxaban, and rivaroxaban inhibit factor Xa, whereas dabigatran is a direct
thrombin inhibitor
4. Fondaparinux
- fondaparinux as initial treatment is favored over IV UFH and over SC UFH
- The choice between fondaparinux and LMWH should be based on local considerations to
include cost, availability, and familiarity of use
- Fondaparinux is a synthetic polysaccharide derived from the antithrombin binding region of
heparin
- it catalyzes factor Xa inactivation by antithrombin without inhibiting thrombin
5. Warfarin therapy
- A vitamin K antagonist such as warfarin should be started on the same day as anticoagulant
therapy in patients with acute PE
- Parenteral anticoagulation and warfarin should be continued together for a minimum of at least
five days and until the INR is 2.0.
Deep Vein Thrombosis
1. Primary therapy
- consists of clot dissolution with pharmacomechanical therapy that usually includes low-dose
catheter-directed thrombolysis
- => reserved for patients with extensive femoral, iliofemoral or upper extremity DVT
- The open vein hypothesis postulates that patients who receive primary therapy will sustain less
long-term damage to venous valves with consequent lower rates of postthrombotic syndrome
2. Secondary prevention
- Anticoagulation or placement of an inferior vena caval filter constitutes secondary prevention of
VTE
- To lessen the severity of post thrombotic syndrome of the legs, below-knee graduated
compression stockings may be prescribe
- => 30-40 mmHg for 2 years after the DVT episode
- => should be replaced every 3 months because they lose their elasticity
58.) Hernias. Definition, types, diagnosis, complications and treatment
Definition
- a protrusion of an organ or part (such as the intestine) through connective tissue or through a
wall of the cavity (as of the abdomen) in which it is normally enclosed
Types
1. Inguinal
- protrusion of abdominal-cavity contents through the inguinal canal
2. Femoral
- a type of groin herniation and comprise of a protrusion of a peritoneal sac through the
femoral ring into the femoral canal, posterior and inferior to the inguinal ligament
- The sac may contain preperitoneal fat, omentum, small bowel, or other structures
3. Umbilical
- a health condition where the abdominal wall behind the navel is damaged
- may cause the navel to bulge outwards (bulge consists of abdominal fat from the greater
omentum or occasionally parts of the small intestine)
4. Incisional
- caused by an incompletely-healed surgical wound
Page 141 of 269
- Since median incisions in the abdomen are frequent for abdominal exploratory surgery,
ventral incisional hernias are often also classified as ventral hernias due to their location
5. Epigastric
- Hernia of the epigastrium
6. Hiatal
- abdominal organs (typically the stomach) slip through the diaphragm into the middle
compartment of the chest
Etiology
1. Mechanical causes
- improper heavy weight lifting
- hard coughing bouts
- sharp blows to the abdomen
- incorrect posture
2. Pressure increasing conditions
- obesity
- straining during a bowel movement or urination (constipation, enlarged prostate)
- chronic lung disease
- fluid in the abdominal cavity (ascites)
3. Trauma
- Abdominal wall hernia may occur due to trauma
- If this type of hernia is due to blunt trauma it is an emergency condition and could be
associated with various solid organs and hollow viscus injuries
Complications of an untreated Hernia
- Inflammation
- Obstruction of any lumen, such as bowel obstruction in intestinal hernias
- Strangulation
- Hydrocele of the hernial sac
- Hemorrhage
- Irreducibility or Incarceration (In intestinal hernias, this substantially increases the risk of bowel
obstruction and strangulation)
Treatment of Hernias
- Surgery is recommended for some types of hernias to prevent complications like obstruction of
the bowel or strangulation of the tissue, although umbilical hernias and hiatus hernias may be
watched, or are treated with medication
- Most abdominal hernias can be surgically repaired
- Time needed for recovery after treatment is reduced if hernias are operated on laparoscopically.
- Uncomplicated hernias are principally repaired by pushing back, or "reducing", the herniated
tissue, and then mending the weakness in muscle tissue (herniorrhaphy)
- Muscle reinforcement techniques often involve synthetic materials (a mesh prosthesis)
- => The mesh is placed either over the defect (anterior repair) or under the defect (posterior
repair)
- =>At times staples are used to keep the mesh in place
Page 142 of 269
61.) Inguinal hernias. Types, anatomy, diagnosis. Complications and treatment
General
- a protrusion of abdominal-cavity contents through the inguinal canal
- Symptoms are present in about 66% of affected people
- may include pain or discomfort especially with coughing, exercise, or bowel movements
- Often gets worse throughout the day and improves when lying down
- A bulging area may occur that becomes larger when bearing down
- occur more often on the right than left side
- The main concern is strangulation, where the blood supply to part of the intestine is blocked.
=> usually produces severe pain and tenderness of the area
- Risk factors for the development of a hernia include: smoking, chronic obstructive pulmonary
disease, obesity, pregnancy, peritoneal dialysis, collagen vascular disease, and previous open
appendectomy
- Hernias are partly genetic and occur more often in certain families
- can often be diagnosed based on signs and symptoms
- Occasionally medical imaging is used to confirm the diagnosis or rule out other possible causes
- Most common hernias
Anatomy
- In men, indirect hernias follow the same route as the descending testes, which migrate from the
abdomen into the scrotum during the development of the urinary and reproductive organs
- The larger size of their inguinal canal, which transmitted the testicle and accommodates the
structures of the spermatic cord, might be one reason why men are 25 times more likely to
have an inguinal hernia than women
- several mechanisms such as strength of the posterior wall of the inguinal canal and shutter
mechanisms compensating for raised intra-abdominal pressure prevent hernia formation in
normal individuals
Types
1. Indirect inguinal hernia
- protrudes through the inguinal ring
- is the result of the failure of embryonic closure of the processus vaginalis after the testicle
passes through it
- Lateral to inferior epigastric vessels
- Covered by internal spermatic fascia
2. Direct inguinal hernia
- enters through a weak point in the fascia of the abdominal wall (Hesselbach triangle)
- Medial to inferior epigastric vessels
Diagnosis
- history and physical exam are usually sufficient
- Can also be seen on imaging (US, CT, MRI)
Complications
1. Pressure on surrounding tissues
- Most inguinal hernias enlarge over time if not repaired surgically
- In men, large hernias can extend into the scrotum, causing pain and swelling
2. Incarcerated hernia
- the contents of the hernia become trapped in the weak point in the abdominal wall
- => can obstruct the bowel, leading to severe pain, nausea, vomiting, and the inability to have a
bowel movement or pass gas
3. Strangulation
- An incarcerated hernia can cut off blood flow to part of the intestine
- => can lead to the death of the affected bowel tissue
- strangulated hernia is life-threatening and requires immediate surgery
Page 143 of 269
Treatment
1. Non-urgent repair
- Elective surgery is planned in order to help relieve symptoms, respect the person's preference,
and prevent future complications that may require emergency surgery
- Surgery is offered to the majority of people who: have symptoms that interfere with their normal
level of activity, have hernias that become increasingly difficult to reduce, are female as it is
often difficult to classify the subtype of hernia based on an exam alone
2. Urgent repair
- A hernia in which the small intestine has become incarcerated or strangulated constitutes a
surgical emergency
- Symptoms include: fever, nausea and vomiting, extreme pain in the area of the hernia, warm
hernia bulge with surrounding skin redness, inability to pass gas or stool
- Surgical repair within 6 hours of the above symptoms may be able to save the strangulated
portion of intestine
Open surgery
- All techniques involve an approximate 10-cm incision in the groin
- Once exposed, the hernia sac is returned to the abdominal cavity or excised and the abdominal
wall is very often reinforced with mesh
- There are many techniques that do not utilize mesh and have their own situations where they
are preferable
Laparoscopic surgery
- There are two main methods of laparoscopic repair: transabdominal preperitoneal (TAPP) and
totally extra-peritoneal (TEP) repair
- When performed by a surgeon experienced in hernia repair, laparoscopic repair causes fewer
complications, particularly less chronic pain
- many surgeons are moving to laparoscopic methodologies as they cause smaller incisions,
resulting in less bleeding, less infection, faster recovery, reduced hospitalization, and reduced
chronic pain
62.) Femoral hernias. Types, anatomy, diagnosis, complications and treatment
General
- occur just below the inguinal ligament, when abdominal contents pass through a naturally
occurring weakness in the abdominal wall called the femoral canal
- Femoral hernias are a relatively uncommon type, accounting for only 3% of all hernias
- While femoral hernias can occur in both males and females, almost all of them develop in
women due to the increased width of the female pelvis
- more common in adults than in children
- Seventy percent of pediatric cases of femoral hernias occur in infants under the age of one
Types
1. Retrovascular (Narath’s Hernia)
- hernial sac emerges from the abdomen within the femoral sheath but lies posteriorly to the
femoral vein and artery
- visible only if the hip is congenitally dislocated
2. Serafini’s hernia
- hernial sac emerges behind femoral vessels
3. Valpeau Hernia
- hernia sac lies in front of the femoral blood vessels in the groin
4. External femoral hernia of Hesselbach and Cloquet
- the neck of the sac lies lateral to the femoral vessels
5. Transpectineal femoral hernia of Laugier
- the hernial sac transverses the lacunar ligament or the pectineal ligament of cooper
6. De Garengeots hernia
- this is a vermiform appendix trapped within the hernial sac
Page 144 of 269
Diagnosis
- largely done by physical examination of the groin
- in obese patients, imaging in the form of ultrasound, CT or MRI may aid in the diagnosis
- For example, an abdominal x-ray showing small bowel obstruction in a female patient with a
painful groin lump needs no further investigation
Signs and symptoms
- typically present as a groin lump or bulge, which may differ in size during the day, based on
internal pressure variations of the intestine
- The bulge or lump is typically smaller or may disappear completely in the prone position
- may or may not be associated with pain
- cough impulse is often absent and is not relied on solely when making a diagnosis of femoral
hernia
- The lump is more globular than the pear-shaped lump of the inguinal hernia
- The bulk of a femoral hernia lies below an imaginary line drawn between the anterior superior
iliac spine and the pubic tubercle (which essentially represents the inguinal ligament) whereas
an inguinal hernia starts above this line
- Nonetheless, it is often impossible to distinguish the two pre-operatively
Complications
1. Incarcerated femoral hernia
- contents of the hernia are unable to return to their original cavity
2. Obstruction
- bowel lumen has become obstructed, leading to the symptoms of bowel obstruction
3. Strangulation
- compression of the hernia causing a compression of the blood siupply leading to ischemia
of the bowel
- A strangulated hernia will present as an irreducible ant tense lump with unproportional pain
- Surgical emergency
Treatment
- Repair is either performed by suturing the inguinal ligament to the pectineal ligament using
strong non-absorbable sutures
- or by placing a mesh plug in the femoral ring
- With either technique care should be taken to avoid any pressure on the femoral vein
Page 145 of 269
66.) Gastric and duodenal ulcers (Zollinger-Ellison syndrome)
See Gastric and duodenal ulcers at topic 37
General
- a disease in which tumors cause the stomach to produce too much acid, resulting in peptic
ulcers
- caused by a gastrinoma, a neuroendocrine tumor that secretes a hormone called gastrin
- The tumor causes excessive production of gastric acid, which leads to the growth of gastric
mucosa and proliferation of parietal and ECL cells
- ZES may occur on its own or as part of an autosomal dominant syndrome called multiple
endocrine neoplasia type 1 (MEN 1)
- The primary tumor is usually located in the pancreas, duodenum or abdominal lymph nodes,
but ectopic locations (e.g., heart, ovary, gallbladder, liver, and kidney) have also been described
Signs and symptoms
- the diagnosis is suspected in patients who have severe ulceration of the stomach and small
bowel, especially if they fail to respond to treatment
- Gastrinomas may occur as single tumors or as multiple small tumors. About one-half to twothirds of single gastrinomas are malignant tumors that most commonly spread to the liver and
to lymph nodes near the pancreas and small bowel
- Nearly 25 percent of patients with gastrinomas have multiple tumors as part of a condition
called multiple endocrine neoplasia type 1 (MEN 1)
- MEN I patients have tumors in their pituitary gland and parathyroid glands, in addition to tumors
of the pancreas
Symptoms
- Chronic diarrhea, including steatorrhea (fatty stools)
- Pain in the esophagus, especially between and after meals at night
- Nausea
- Wheezing
- Vomiting blood
- Malnourishment
Pathogenesis
- Gastrin works on the parietal cells of the gastric glands, causing them to secrete more
hydrogen ions into the stomach lumen
- also gastrin acts as a trophic factor for parietal cells, causing parietal cell hyperplasia
- => increase in the number of acid-secreting cells, and each of these cells produces acid at a
higher rate
- The increase in acidity contributes to the development of peptic ulcers in the stomach and
duodenum
Diagnosis
- may be suspected when the above symptoms prove resistant to treatment, when the
symptoms are especially suggestive of the syndrome, or when endoscopy is suggestive
- The diagnosis is made through several laboratory tests and imaging studies:
1. Secretin stimulation test (measures evoked gastrin levels)
2. Fasting gastrin levels on at least three separate occasions
3. Gastric acid secretion and pH (normal basal gastric acid secretion is less than 10 mEq/hour; in
Zollinger–Ellison patients, it is usually more than 15 mEq/hour)
4. An increased level of chromogranin A is a common marker of neuroendocrine tumors
5. In addition, the source of the increased gastrin production must be determined using MRI or
somatostatin receptor scintigraphy
Treatment
- Proton pump inhibitors (such as omeprazole and lansoprazole) and histamine H2-receptor
antagonists (such as famotidine and ranitidine) are used to slow acid secretion
- Once gastric acid is suppressed, symptoms normally improve
Page 146 of 269
67.) Gastric and duodenal ulcers
Essentials
•
H. pylori and NSAIDs are the most common causes of peptic ulceration
•
most duodenal ulcers are caused by H. pylori
•
most gastric ulcers in developed countries are caused by NSAIDs
•
smoking is an important co-factor particularly for H. pylori-induced ulcers
•
virulence factors (CagA, VacA and others) influence whether H. pylori colonization leads to
ulceration
•
NSAIDs inhibit the synthesis of gastroprotective prostaglandins
•
typical ulcer symptoms are loclized epigastric pain occuring overnight or pre-prandially and
relieved by milk or anatacids
•
many ulcers are now treated without formal diagnosis; where diagnosis is needed
endoscopy is the method of choice
•
biopsy of gastric ulcers is traditionally recommended
Introduction and definition
•
peptic ulcers are localized breaches of the gastric or duodenal mucosa with tissue
destruction at least to the depth of the muscularis mucosa
•
peptic ulcers include ulcers in the stomach, pylorus, duodenum, or a Meckel’s diverticulum,
as well as ulcers at sites of GI anastomosis (stomal ulcers) and at the gastroesophageal
junction
•
the commonest symptom is pain
•
the most serious complications are bleeding and perforation
Causes of peptic ulceration
•
most ulcers are directly caused by infection with H. pylori or by NSAIDs, incl. aspirin, which
inhibits prostaglandin synthesis and abrogates mucosal defence mechanisms
•
uncommon causes: Crohn’s disease, conditions causing acid hypersecretion (ZollingerEllison syndrome, multiple endocrine neoplasia,…) severe physical stress (e.g. being in
intensive care) and mucosal ischemia due to critical celiac axis vascular disease and
radiation
•
gastric ulceration may also indicate gastric adenocarcinoma or gastric lymphoma
Pathogenesis
•
mucosal integrity represents a balance between aggressive and protective factors
=> H. pylori infection and acid are the main aggressive factors; the main protective factors
are mucus and bicarbonate secretion, hydrophobicity of epithelial cells and mucosal blood
flow (mediated by prostaglandins)
•
H. pylori associated ulcers: only in about 15% of infected people develop peptic ulceration
in their lifetime; development is due to combination of bacterial virulence (CagA, VacA,…),
host genetic susceptibility (e.g. inadequate regulatory T cell responses) and environmental
co-factors (smoking)
•
Localization of H. pylori-associated ulcers:
•
Duodenal ulcers occur a against a background of H. pylori colonization with a
predominantly antral pattern of gastritis
•
Antral inflammation results in reduced somatostatin production by antral D cells and, as
somatostatin normally has a negative feedback on gastrin, this results in hypergastrinemia
•
gastrin stimulates the healthy gastric corpus to produce more acid => the increased acid
load in the duodenum contributes to the formation of gastric metaplasia in duodenum —>
H. pylori, which can only colonize gastric-type mucosa, can now colonize the duodenum
and cause inflammation, damage and ulceration
•
Gastric ulcers occur in H. pylori-colonized people with a corpus-predominant or
pangastritis — such persons also have hypergastrinemia, but acid production is unchanged
or reduced because of the inflamed and damaged gastric corpus => This leads to a cycle of
chronic damage with progressive atrophy of gastric glands and further hypochlorhydria
Page 147 of 269
•
NSAIDs inhibit the synthesis of gastroduodenal prostaglandins, which are centrally
importnat for mucosal protection via bicarbonate secretion and mucosal blood flow =>
abrogation of prostaglandin-dependent mechanisms is sufficient to cause local erosions,
which deepen to form ulcers in the presence of acid and pepsin
Clinical presentation of uncomplicated ulcers
Duodenal ulceration
•
classical symptom is epigastric pain, occuring before meals or overnight, relieved by
antacids, milk, food and acid-suppressing treatments
•
pain radiate to the back, particularly in patients with posterior duodenal ulcers
•
because ulcers naturally form and heal, pain is classically episodic, typically with clusters of
pain lasting for 1–3 months with asymptomatic spells in between
•
if present, the pointing sign, in which a patient points to a discrete epigastric site of pain, is
moderately predictive of duodenal ulceration
•
also may present with any combination of heartburn, anorexia, weight loss or vomiting
Gastric ulcers
•
less stereotypical presentation
•
an epigastric location is common, but pointing is less so
•
pain is more likely to occur soon after meals and less likely to be relieved by food
•
anorexia, nausea, vomiting, and weight loss are more common than in duodenal ulcers
Diagnostic approach
•
definite diagnosis can be made only after investigation, usually upper gastrointestinal
endoscopy
•
because dyspeptic symptoms are so common, most healthcare systems reserve
endoscopy for patients at higher risk of malignancy —> This includes dyspeptic patients
with “alarm” features such as overt GI bleeding, anemia due to GI blood loss, dysphagia,
weight loss, persistent vomiting, or an upper GI mass; It also usually includes patients with
new onset persistent dyspepsia above a specific age cut-off, typically 55 years
•
Diagnosis of the cause of an ulcer:
•
H. pylori: most conveniently established at the time of endoscopy by urease testing and/ or
histology of antral and corpus biopsies; other non-invasive testing, e.g. urea breath test or
stool antigen tst
•
NSAIDs: depends on accurate history
•
Zollinger-Ellison syndrome: fasting serum gastrin level; increased gastric acid output and a
fasting gastrin level of less than 1000pg/mL with an intragastric pH of 2.0
•
Duodenal Crohn’s disease: any patient not taking NSAIDs who is H. pylori negative should
have duodenal biopsies and the possibility of Crohn’s disease should be considered
•
Stress ulcer: ulcer bleeding occuring in the context of current or recent severe illness and/
or intensive care
Treatment and prevention
H. pylori associated ulcers - Eradication of H. pylori
•
check treatment at H. pylori infection
•
usually multi-drug regimes (triple or quadruple): e.g. PPI, clarithromycin 500mg,
metronidazole 400mg, all twice daily
•
two weeks treatment is slightly more effective than one
Management of patients taking NSAIDs
•
Ulcer healing — PPIs accelerate healing compared with standard doses of H2 antagonists
•
to reduce the risk of development, NSAIDs users should remove the cause of the ulcer, by
stopping the drug or switching to one that doesn’t damage the stomach or duodenum OR,
where needed, continue the NSAID at the lowest possible dose + concurrent antiulcer
prophylaxis with a PPI
Page 148 of 269
Aspirin
•
it is possible that H. pylori eradication may be sufficiently effective to protect low-dose
aspirin users
•
usually a prophylaxis with PPI is recommended, mainly in risk patients (age above 65 or
past ulcer history)
Complications and their management
Bleeding
•
peptic ulcer is the commonest cause of acute upper GI bleeding; accounting for nearly half
of all instances and occurring in approximately 2–5 per 1000 of people aged over 60 years
•
Clinical presentation: hematemesis and/or melena are usually obvious, especially when
accompanied by tachycardia or hypotension, usually leading to emergency hospital
admission
•
endoscopic therapy of bleeding ulcers reduces rebleeding and the need for surgery
•
the choices are injection therapy with epinephrine (adrenaline), light- or heat-based
coagulation of the vessel, clipping or a combination — using at least two modalities is better
than using one alone
Perforation
•
incidence: 7-10 per 100.000 population per annum
•
perforation is more common in men than in women, in those with duodenal versus gastric
ulcers, in cigarette smokers and in users of aspirin and NSAIDs
•
usually with an abrupt onset of severe upper abdominal pain, rapidly spreading through the
abdomen and the development of symptoms and signs of peritonitis, hypotension and
shock
•
diagnosis is largerly based on history, examination and plain radiography (air under the
diaphragm is seen on plain abdominal and erect chest radiographs)
•
endoscopy is avoided because of theoretical risks of increased peritoneal soiling
•
patients should be resuscitated with intravenous fluids and given broad-spectrum antibiotics
(e.g. cefuroxime and metronidazole)
•
laparotomy to close the perforation should be carried out as soon as possible after
resuscitation
Penetration
•
posterior perforation may result in digestive penetration into an adjacent organ rather than
free perforation
•
posterior duodenal ulcer perforation most commonly involves the pancreas, other organs
include left lobe of the liver, common bile duct (choledochoduodenal fistula), colon
(gastrocolic fistula), lung and pericardium
•
except where fistulae formed, treatment is by acid suppression with H. pylori eradication or
NSAID cessation
Stress ulcers
•
severe medical stresses, such as burns, head injuries, major trauma, sepsis, multisystem
organ failure, or ventilation on an intensive caure unit are associated with the development
of stress ulcers in the stomach or duodenum that may bleed and are associated with higher
mortality rate
•
Curling’s ulcers are those associated with burns, Cushing’s ulcers with head injury
•
pathogenesis varies according to etiology: reduced mucosal defence largely because of
poor bloodflow that allows increased acid back diffusion, predisposes to stress ulcers in
ventilated patients and after severe burns, despite an overall reduction in acid secretion
•
Cushing’s ulcers are associated with hypergastrinemia and hypersecretion of acid
•
prophylaxis: H2 receptor antagonists, proton pump inhibitors and sucralfate
Page 149 of 269
68. Upper gastrointestinal bleeding (UGI hemorrhage)
UGIB
- Incidence 100:100.000 adults per year; increasing with advancing age
- Mortality is 10% and usually results from complications of underlying disease rather than from
exsanguination
- Etiologies:
• PUD (55%)
• G astroesophageal varices, vascular ectasia, Mallory-Weiss tear, erosive gastritis/
esophagitis, Cameron’s ulcer
• Other: Dieulafoy’s lesion, aortoenteric fistula, hemobilia
Symptoms/Exam
- patients present with nausea, retching, hematemesis (bright red blood or „coffee ground“
emesis), dyspepsie, abdominal pain, melena or hematochezia and orthostasis
- exam may reveal melena or hematochezia, pallor, hypotension, and tachycardia
- stigmata of chronic liver disease (spider angioma, ascites, jaundice) or a history of alcohol use
are usually found among those with variceal hemorrhage
Diagnosis
- History: Assess NSAID use (peptic ulcer), retching prior to hematemesis (Mallory-Weiss tear),
alcohol abuse (esophagitis, Mallory-Weiss tear, varices), prior abdominal aortic graft
(aortoenteric fistula), chronic GERD (esophagitis), and weight loss/iron deficiency (malignancy)
- NG tube lavage: Useful if (red blood, coffee grounds); if (clear or bilious), does not exclude
UGIB — Ten percent of UGIB cases have a lavage
- EGD (upper gastroscopy): perform after stabilization and resuscitation; often done < 12 hours
from admission. Diagnostic, prognostic, and therapeutic
- H. pylori testing: perform on all patients with peptic ulcers
Risk Assessment in Patients with UGIB
Low
Moderate
High
History
Age < 60
Age < 60
Age > 60, comorbidities,
onset while in hospital
Exam
SBP > 100
HR < 100
SBP > 100
HR > 100
SBP < 100
HR > 100
EGD
Small, clean-based
ulcer; erosions; no
lesions found
Ulcer with pigmented
spot or adherent clot
Active bleeding varices,
ulcer > 2cm, visible
vessel
Rebleed risk
< 5%
10-30%
40-50%
Triage
Ward/Home
Ward
ICU
Treatment
- Stabilization:
• NPO; consider an NG tube and place two large-bore IVs
• If the patient is in shock, treat with aggressive IV fluids and cross- matched blood with a
hematocrit goal of 25–30%
• In the presence of active UGIB and platelets < 50,000/µL or if there is known impaired
function (uremia, aspirin), transfuse platelets or desmopressin
- Medical therapy:
• Give high-dose oral PPIs twice daily upon presentation
• Initiate an IV PPI drip if EGD suggests a high risk of rebleeding (i.e., active bleeding, visible
vessel, adherent clot) — Reduces the relative risk of bleeding by 50%
• IV octreotide for suspected variceal hemorrhage; continue for three days if verified by EGD
Page 150 of 269
- Endoscopy: of all patients with active UGIB at EGD, > 90% can be effectively treated with
banding, sclerosant, epinephrine, and/or electrocautery; Predictors of rebleeding include
significant comorbidities, size of lesion, and high-risk stigmata (visible vessel, adherent clot)
- Refractory or recurrent UGIB:
• Esophageal balloon tamponade (Minnesota or Sengstaken-Blakemore tubes) for varices
• Angiogram with intra-arterial embolization or surgery for refractory nonvariceal bleeding
- H. pylori eradication: for all peptic ulcers causing UGIB
Treatment for H. pylori
Treatment
Standard initial therapy
PPI (e.g. esomeprazole)
Amoxicillin
Clarithromycin
Penicillin allergic patients:
Subst. amoxicillin with metronidazole
20mg
1g
500mg
bid
bid
bid
500mg
bid
Bismuth-based therapy
Bismuth subsalicyclate/subcitrate
Tetracycline
Metronidazole
PPI
OR Ranitidine
120mg
500mg
250mg
20mg
150mg
qid
qid
qid
bid
bid
Sequential therapy
PPI (e.g. pantoprazol)
Amoxicillin
Clarithromycin
Tinidazole
40mg
1g
500mg
500mg
bid
bid
bid
bid
1g
500mg
bid
bid
bid
Salvage therapy
PPI
Amoxicillin
Quinolone (e.g. levofloxacin)
Duration
Cure rate
7-14 days
<80%
10-14 days
> 80%
89 %
87 %
10 days
69. Benign tumors of the stomach. Precanceroses.
Non-cancerous tumors of the stomach
- a benign growth is a tumor that does not spread (metastasize) to other parts of the body,
usually isn’t life-threathening and it is typically removed by surgery and does not recur
- many times of benign tumors but gastric polyps are the most common
Gastric polyps
- most common non-cancerous stomach tumors that develop in the lining of the stomach
- there are several types of gastric polyps:
• Fundic gland polyp – These polyps usually measure less than 1 cm and may occur by
chance or in people with polyposis syndromes
• Hyperplastic polyps – These typically measure less than 2 cm and are often found in people
with an inflamed stomach (gastritis)
• Inflammatory fibroid polyps – These polyps are hard, red and swollen (inflamed). They can
grow large enough to cause a blockage
• Xanthoma – This fatty, yellowish growth is usually very small (most are less than 3 mm)
• Hamartomatous polyps – These are surrounded by normal stomach lining and may occur by
chance or in people with polyposis syndromes
- polyposis syndromes are inherited conditions where large numbers of polyps develop in the GI
tract, usually the colon or small intestine => benign gastric polyps can occur in the following
Page 151 of 269
polyposis syndromes: Peutz-Jeghers syndrome, juvenile polyposis, Cowden syndrome,
Cronkhite-Canada syndrome, Gardner syndrome, familial adenomatous polyposis (FAP)
- FAP causes hundreds to thousands of adenomas to develop in the lining of the colon and
rectum and in some cases other parts of the GI tract including the stomach
Other non-cancerous gastric tumors
- gastrointestinal stromal tumor (GIST) - small GISTs may be non-cancerous but larger ones are
often cancerous
- lipoma – made up of fat, or adipose, cells
- leiomyoma – made up of smooth muscle cells
- tumours of the peripheral nerves – for example, schwannoma and neurofibroma
- ectopic pancreas, or pancreatic heterotopia – made up of pancreatic tissue cells
- hemangioma – made up of abnormal blood vessels
- lymphangioma – develops in lymph vessels
- glomus tumour, or perivascular tumour – develops around blood vessels
- fibroma, or fibromyoma – made up of fibrous tissue
- cystic tumour – develops when a mucus-releasing gland becomes blocked
Risk factors
- gastric polyps may develop because of an inherited condition or in areas of the stomach that
are inflamed or damaged
- fundic gland polyps may also develop in people who take drugs that lower the amount of acid
made in the stomach (such as proton-pump inhibitors)
Symptoms
- non-cancerous stomach tumors rarely cause signs and symptoms
- most tumors are found accidentally when an upper gastrointestinal endoscopy is done for other
reasons
- signs and symptoms may appear if the polyp grows very large and may include:
• upper abdominal pain
• bleeding
• anemia
• gastric outlet obstruction (blocked opening from the stomach to the small intestine)
• digestive problems such as nausea and vomiting or feeling full after a small meal (early
satiety)
• lump in the abdomen (if the tumor is large)
Diagnosis
- usually discovered when tests done for other reasons
- tests to diagnose or rule out tumors include:
• upper gastrointestinal endoscopy
• endoscopic ultrasound
• endoscopic biopsy
- also seen on CT or MRI
Treatments
- treatment is not necessary if the tumor is small (less than 1 cm) and isn’t causing any signs or
symptoms; but need regular checkups with endoscopy to see if it grows or starts to look
different
- the standard treatment for benign tumors is sugery — the type of surgery mostly depends on
the size of the tumor and includes the following:
• endoscopic biopsy — to remove single polyps that are less than 2cm
• gastrostomy — uses an incision, or a surgical cut, in the stomach wall to remove polyps
larger than 5 cm or many flat, or sessile, polyps
• gastric resection – to remove a small tumour along with a margin of healthy tissue
• removal of all or part of the stomach (gastrectomy) – may be used for many polyps
Page 152 of 269
Precanceroses - Precancerous conditions of the stomach
= changes to the stomach cells that make them more likely to develop into cancer
Gastric epithelial dysplasia
- occurs when the cells of the stomach lining (called the mucosa) change and become abnormal.
- These abnormal cells may eventually become adenocarcinoma, the most common type of
stomach cancer
- Gastric epithelial dysplasia can be divided into 2 types:
• low-grade dysplasia – The abnormal cells change and grow slowly; It has a low risk of
becoming cancer and may change back to normal (regress)
• high-grade dysplasia – The abnormal cells change and grow quickly; It has a high risk of
becoming cancer.
Risk factors
The following risk factors increase the chance of developing gastric epithelial dysplasia:
• H. pylori (Helicobacter pylori) infection
• chronic atrophic gastritis – the lining of the stomach becomes thin, or atrophies, due to longterm inflammation of the stomach, called gastritis
• intestinal metaplasia – the lining of the stomach is replaced by tissue that is normally found in
the lining of the small and large intestines
• pernicious anemia
=> Each of these conditions causes changes in the stomach lining that can lead to the
development of abnormal cells and dysplasia
Signs and symptoms
Gastric epithelial dysplasia does not cause any signs or symptoms
Diagnosis
- Gastric epithelial dysplasia is often found during stomach tests, such as an upper
gastrointestinal endoscopy, done for other health reasons
- tests used to diagnose gastric epithelial dysplasia may include:
• upper gastrointestinal endoscopy
• endoscopic biopsy
• chromoendoscopy (a special stain or pigment is used during an endoscopy to help identify
the area of gastric epithelial dysplasia)
• endoscopic ultrasound
Treatments
Treatment options for gastric epithelial dysplasia will depend on the grade of dysplasia:
Low-grade dysplasia
- Surgery is not usually needed
- The doctor will closely monitor the patient and do an upper gastrointestinal endoscopy and a
biopsy once a year
High-grade dysplasia
Treatment for high-grade dysplasia may include:
• endoscopic mucosal resection (removal of the area during an endoscopy)
• limited surgical resection (removal of the area along with a section of healthy tissue)
Gastric adenoma
- Gastric adenoma (adenomatous gastric polyp) is a type of polyp made up of abnormal (atypical)
glandular cells from the stomach lining
- They are found in areas of the stomach where the normal tissue has been changed by chronic
inflammation
- If left untreated, a gastric adenoma could develop into adenocarcinoma, the most common
type of stomach cancer
- Gastric adenoma is usually found in the antrum of the stomach
- It may grow as a slightly elevated area on the lining of the stomach (sessile) or outward from the
surface with a head and stalk (pedunculated)
Page 153 of 269
- A gastric adenoma usually measures less than 2 cm in size
- Gastric adenomas are more likely to become cancerous if they:
•
•
•
•
are larger than 2 cm
have high-grade dysplasia
grow with tiny, finger-like projections (villous)
are ulcerated (have the appearance of an open sore)
Risk factors
- familial adenomatous polyposis (FAP) – an inherited condition that causes hundreds to
thousands of polyps to develop on the lining of the colon and rectum as early as adolescence
- chronic atrophic gastritis – the lining of the stomach becomes thin, or atrophies, due to longterm inflammation of the stomach, called gastritis
- intestinal metaplasia
Signs and symptoms
- Small gastric adenomas do not cause any signs or symptoms
- Signs and symptoms may appear if the gastric adenoma grows larger and causes a blockage
(obstruction) in the stomach
- They may include:
• mild, vague upper abdominal discomfort
• digestive problems such as nausea, vomiting, feeling full after a small meal (early satiety) or
difficulty swallowing
• bleeding
• anemia
Diagnosis
Tests used to diagnose gastric adenoma may include:
• physical exam
• ultrasound
• upper gastrointestinal endoscopy
• endoscopic biopsy
Treatments
Treatment options for gastric adenoma include:
• endoscopic removal of the polyp (used for single polyps that are 2 cm or smaller)
• endoscopic mucosal resection
• gastrostomy (uses an incision, or a surgical cut, in the stomach wall to remove polyps larger
than 5 cm, many polyps or a sessile polyp)
• partial gastrectomy (removes part of the stomach in people who cannot have a gastrostomy)
70. Malignant tumors of the stomach.
Key revision points - anatomy and physiology of the stomach
- The fundus is predominantly a storage zone with few active cells
- The body contains mostly chief cells (secrete pepsinogen; stimulated by gastrin and local ACh
release) and oxyntic cells (secrete H+; stimulated by gastrin, histamine, and ACh; inhibited by
H+, secretin, and GIP)
- The antrum contains G cells (secrete gastrin; stimulated by ACh from vagus, stretch; inhibited
by VIP, secretin, H+)
- The pyloric sphincter is a functional sphincter of circular muscle
- Arterial supply is profuse (gastric ischaemia is rare) via coeliac axis—left gastric, splenic, and
common hepatic arteries
- Lymphatic drainage follows arteries and is profuse (significant lymph
node metastases are usually fatal)
Page 154 of 269
Essentials
Risk factors for adenocarcinoma (commonest, incidence > 50y)
- diet rich in nitrosamines (smoked or fresh fish, pickled fruit)
- chronic atrophic gastritis
- blood group A
- chronic gastric ulceration related to H. pylori
Pathogenesis
- environmental factors: nitrates/nitrites, excess salt, lack of fresh fruits, smoking
- gene polymorphism
- H. pylori infection
- chronic atrophic gastritis and intestinal metaplasia
Diagnosis
- Symptoms: nonspecific but epigastric pain, nausea and vomiting, dysphagia, weight loss are
found in advanced stages
- upper GI endoscopy: highly sensitive and specific for advanced cancer, chromoendoscopy and
magnifying endoscopy useful for early cancer
Treatment
- eradication of H. pylori probably reduces the risk of gastric cancer
- surgery: for resectable disease
- early cancer: can be treated by endoscopic mucosal resection (EMR) or endoscopic submocosal
dissection (ESD)
- chemotherapy (5-FU based) is the most common regime
Introduction and epidemiology
- may arise from the tissues of the mucosa (adenocarcinoma), connective tissue of the stomach
wall (previously known as leiomyoma or leiomyosarcoma, but part of the spectrum of disease
called gastrointestinal stromal tumours (GISTs)), the neuroendocrine tissue (carcinoid tumours),
or the lymphoid tissue (lymphomas)
- gastric adenocarcinoma is the most frequently observed malignant gastric disease (90-95% of
gastric neoplasms)
- mostly occurs at the age of 55 to 70 years and is the second cause of all cancer deaths
- great gender and ethnis variation: highest incidence in Japan, China, South America and
Eastern Europe, and the lowest incidence in North America, Western Europe, Australia and New
Zealand
- males are nearly 2 times more likely to have gastric adenocarcinomas than females
- gastric adenocarcinoma can be subdivided into intestinal and diffuse type
- the intestinal type is better differentiated, characterized by cohesive neoplastic cells that form
gland-like tubular structures
- the diffuse type is less differentiated, characterized by individual cells which infiltrate and thicken
the stomach wall —> results in loss of distensibility of the gastric wall and carries a poor
prognosis
Etiology and pathognesis
- definite etiology is unknown; multifactorial and multi-step process
- epidemiologic studies find high nitrate concentrations in soil and drinking water in areas with
high death rates from gastric cancer, and people in high- incidence areas prefer to ingest dried,
smoked and salted foods which have a high concentration of nitrates and salt
- these people also have high prevalance of H. pylori infection => the nitrates are converted to
carcinogenic nitrites by the bacteria (- this process is enhanced by deficiency of fresh fruit,
vegetables and vitamins A and C)
- genetic factors: studies have showns that gastric adenocarcinoma has familiar clustering and
higher prevalance rate in first degree relatives, especially in diffuse type
Page 155 of 269
- several genetic mechanisms may account for the pathogenesis of gastric carcinogenesis:
oncogene activation, tumor suppressor gene inactivation, DNA microsatellite instability and gene
polymorphism
- chronic atrophic gastritis and intestinal metaplasia are associated with an appr. 25-fold increase
in gastric cancer
Clinical presentation
- Early gastric cancer: limited only to the mucosa and/ or submucosa, no matter whether there is
lymph node involvement and distant metastasis or not
- patients with early gastric cancer are often asymptomatic or have nonspecific symptoms
- Advanced gastric adenocarcinoma: invaded beyond the submucosa
- in advanced cases epigastic pain is the most common symptom, it cannot be relieved by food or
antacids
- nausea and vomiting are found in patients with gastric outlet obstruction; dysphagia and early
satiety may be the major symptoms caused by diffused lesions originating in the cardia
- weekness, fatigue, melena, hematemesis and anemia occur when the tumor bleeds
- some special signs may appear as a result of regional invasion or distant metastasis:
• right upper quadrant pain, jaundice, and/ or fever can occur when gastric cancer
metastasizes to the liver
• lung metastases can cause cough, hiccups and hemoptysis
• pain radiating to the back may indicate that the tumor has penetrated to the pancreas
• intraabdominal (periumbilical node: Sister Mary Joseph’s node) and supraclavicular lymph
nodes (Virchow’s node) are frequently involved
- physical examination may reveal epigastric mass
- ascites, hepatomegaly and Virchow’s node may present when metastasis occurs
Differential Diagnosis
- Benign gastric ulcer: a benign ulcer is small and smooth with a regular base, whereas a
malignant ulcer is large with an everted and irregular margin
- Gastric leiomyoma: arises from smooth muscle; usually located in the corpus or antrum;
radiographic examination usually reveals a smooth intramural filling defect, with or without
ulceration
- Primary gastric lymphoma: difficult to distinguish because both present with similar clinal and
radiographic appearance; the diagnosis of gastric lymphoma requires endoscopic biopsy or
laparatomy; most gastric lymphoid tumors are non-Hodgkin’s lymphomas that origin from B cells
Diagnostic methods
- endoscopy and radiographic examination are two main methods to diagnose gastric
adenocarcinoma
- endoscopic ultrasonography, CT and laboratory studoes are also helpful
- cancer may be detected as mucosal ulceration, polypoid mass, infiltrating lesion, or large gastric
folds
- when ulcers are observed, at least sex biopsy specimens, from both the edge and the base of
the ulcer, need to be obtained
- CT and EUS are combined to evaluate staging of gastric cancer
- laboratory studies may detect iron deficiency anemia
Page 156 of 269
Staging of gastric adenocarcinoma
Stage
TNM
Characteristics
0
TisN0M0
node negative; limited to mucosa
IA
T1N0M0
node negative; invasion of lamina propria or submucosa
IB
T2N0M0
node negative; invasion of muscularis propria
II
T1N2M0 or
T2N1M0
T3N0M0
node positive; invasion beyond mucusa but within wall
IIIA
T2N2M0 or
T3N1-2M0
node positive; invasion of muscularis propria or through wall
IIIB
T4N0-1M0
node negative; adherence to surrounding tissue
IV
T4N2M0
T1-4N0-2M1
node positive; adherence to surrounding tissue
distant metastases
node negative; extension through wall
Treatment and prevention
- the only chance for cure of gastric cancer is surgical removal of the tumor and the adjacent
lymph nodes
- even when gastric cancer is not suitable for cure, palliative surgical resection is still effective to
relieve symptoms
- subtotal gastrectomy is often chosen for patients with distal cancers, but promixal tumors need
total gastrectomy
- therapeutic endoscopy can alse be applied to manage gastric adenocarcinoma: early gastric
cancer can be treated by endoscopic mucosal resection (EMR) or endoscopic submucosal
dissection (ESD)
- EMR is suitable for patients with intestinal type mucosal cancer less than 2 cm which has no
lymph node metastasis, ESD can remove larger lesions
- for advanced gastric cancer, therapeutic endoscopy can provide palliative procedures such as
stent placement and tumor ablation
- gastric adenocarcinoma is resistant to radiotherapy
- chemotherapy usually adopts postoperatively or preoperatively as an adjuvant therapy in
patients with advanced gastric cancer, because gastric carcinoma has a low survival rate and
high recurrence rates
- effect of a single chemotherapeutic agent is limited (20% response rate) => combination
regimes often applied (response rate 40%)
- prevention: screening program in high risk groups and in high-incidence areas
Complications
- Bleeding: GA often produces chronic, occulent bleeding which can result in anemia —
endoscopic therapy; angiographic therapy; drug therapy; sometimes palliative surgery is
necessary to stop bleeding
- Perforation: unusual to develop perforation; when it occurs, abrupt and severe abdominal pain,
abdominal muscular spasm, board-like rigidity of the abdomen, other manifestations of
peritoneal irritation and shock may take place; management: start with correcting hemodynamic
fluid, fluid and electrolyte imbalances, and emergency surgery is usually necessary
- Obstruction: often in patients with tumors originating from pylorus or cardia; early satiety, nausea
and vomiting, dysphagia and weight loss are the main signs; treatment: nasogastric suction,
endoscopic stenting and palliative surgical resection
Page 157 of 269
Prognosis
- about one third of patients who undergo a curative surgical resection are alive after 5 years
- survival of patients without treatment is about 1 year
- the overal 5-year survival rate is appr. 10%
- lymph node invovlement, regional extension, distant metastases and tumor cell DNA aneuploidy
often indicate poor prognosis
72.) Diseases of the small intestine. Benning and malignant tumors. Meckel’s diverticulum.
Benning and malignant tumors of the small intestine
General
-
Although the small bowel accounts for 75% of the gastrointestinal length and 90% of its absorptive
surface, neoplasms of this organ, both benign and malignant, are relatively rare
They represent less than 10% of all gastrointestinal tumors, 1%-3% of gastrointestinal malignancies
and 0.4% of all malignancies
In recent years, the incidence of two small bowel tumors, lymphomas, and gastrointestinal stromal
tumors (GIST), have increased substantially
In the case of primary small bowel lymphoma, the incidence in the United States has nearly doubled
in the last two decades, due to the increased numbers of immunocompromised patients and
immigrants from developing countries
Several predisposing conditions associated with small bowel malignancies have been identified: CD,
familial adenomatous polyposis, hereditary nonpolyposis colorectal cancer, blind loop syndrome,
Peutz–Jeghers syndrome, celiac sprue, neurofibromatosis, and IgA deficiency
The disproportion between the low incidence of malignant tumors of the small bowel and the size of
its surface area suggests a significant sparing from or resistance to the development of malignancy
o Carcinogens in the enteric content may be in contact with small bowel mucosa over a limited
time due to the relatively rapid transit time or may be in a diluted and less carcinogenic form
o Small bowel microscopic and chemical environment
The limited and metabolically inactive bacterial flora of the small bowel is likely unable to
transform procarcinogens into their active metabolites especially in an alkaline milieu
o In addition, the proximal small bowel secretes a number of enzymes that detoxify
carcinogens
Finally, the presence of a high concentration of B cells and lymphocytes and high amounts of
secretory IgA in the distal small bowel might constitute an effective local immunosurveillance
system that prevents carcinogenesis
o Immunocompromised patients have increased incidence of lymphoma of the distal small
bowel
Dietary risk factors, such as high caloric dietary intake in general and more specifically consumption
of red meat, fat, and salt-cured smoked foods have been shown to increase the incidence of small
bowel carcinoma in large population-based studies
o This similarity in risk factors explains the relatively high risk of synchronous or
metachronous colorectal cancer in patients with a known small bowel malignancy
o
-
-
Pathology
-
Approximately one-third of primary small bowel neoplasms are benign, and two-thirds are malignant
The most common benign tumors are leiomyomas and adenomas; less common lesions include
inflammatory polyps, hemangiomas, lipomas, hamartomas (Peutz–Jeghers syndrome), and fibromas
These tumors can occur throughout the small bowel but tend to increase in frequency from proximal
to distal, with the exception of adenomas, which occur with the highest frequency in the duodenum
Page 158 of 269
Benign Tumors
Adenomas
-
the most common benign tumors of the small intestine
The duodenum is the most common site of involvement, and the lesion most commonly noted is a
villous adenoma
These lesions tend to involve the region of the ampulla of Vater
They may present with obstructive jaundice and are easily diagnosed by upper endoscopy and biopsy
Up to 30 percent of these tumors may have malignant degeneration
The risk of malignant degeneration in a significant proportion of patients poses challenges to
treatment planning
Leiomyomas
-
arise from smooth muscle and can grow both intra- and extraluminally
They can often become very large before causing symptoms
On gross inspection, it is sometimes difficult to distinguish these lesions from their malignant
counterparts
This distinction is made histologically with standard criteria including nuclear pleomorphism,
increased mitosis and the presence of necrosis although, at times, even histological examination may
fail to distinguish between benign and malignant histology
Lipomas
-
are collections of fatty tissue within the wall of the intestine that, when viewed
endoscopically, have a mild yellowish appearance
These are completely benign tumors with no malignant potential
Lipomas do not need to be removed unless they become very large and cause obstructive
symptoms (or bleeding due to ulceration)
Hemangiomas
-
are collections of blood vessels that form a benign vascular tumor in the wall of
the stomach or intestine
-
They are benign and sometimes found in conjunction with other syndromes
-
can cause gastrointestinal bleeding and anemia
-
detected by endoscopy
-
They can be treated endoscopically with application of a heater probe to burn the vessels
-
Patients may need resection of areas of intestine heavily involved with hemangiomas if they
cause significant bleeding
Malignant Tumors
-
tend to increase in frequency from proximal to distal, with the exception of adenocarcinomas which
are most frequent in the duodenum
Adenocarcinoma is the most common histologic type (45%), followed by carcinoids (30%),
lymphomas (15%), sarcomas, and GISTs (10%)
Adenocarcinoma
-
solitary, sessile lesions, often appearing in association with adenomas
They are usually moderately to well differentiated and almost always positive for acid mucin
Most arise in the duodenum: within the duodenum, 15% of these tumors are located in the first
portion, 40% in the second portion, and 45% in the distal duodenum
Most of these tumors are sporadic with the exception of the ones originating in the context of
familial adenomatous polyposis
Page 159 of 269
-
Presenting symptoms include epigastric and abdominal pain or discomfort, and possibly jaundice
and gastric outlet obstruction, depending on the location of the tumor
These symptoms and the accessibility of the duodenum and proximal small bowel to endoscopic
modalities allow a relatively high rate of diagnosis and resectability
Carcinoid tumors
-
the most common endocrine tumors of the gastrointestinal system
In the small bowel itself, carcinoids are the most common distal small-bowel neoplasm
These neoplasms arise from enterochromaffin cells and are characterized by the ability to secrete
many biologically active substances, including serotonin, bradykinin, dopamine, histamine, and 5hydroxyindoleacetic acid (5-HIAA)
They tend to be small (< 2 cm) and submucosal in location, with a propensity for multicentricity
The most common classification for these tumors is based on embryologic derivation: foregut
(stomach and pancreas), midgut (small bowel 90% or more), and hindgut (colon and rectum)
Their presentation depends largely on the hormones elaborated and on the site of origin
Up to 40% of small bowel carcinoids are associated with a second gastrointestinal malignancy and
30% present as multiple synchronous lesions
Intestinal Lymphoma
-
The gastrointestinal tract is the most frequent site of extra nodal lymphoma
the stomach is the most common site followed by the small bowel and the colon
within the small bowel, lymphomas parallel the distribution of lymphoid follicles, resulting in the
ileum being the most common site of involvement
These tumors may be primary or secondary as a manifestation of generalized involvement of
systemic lymphoma
For the diagnosis of primary small bowel lymphomas there must be no peripheral or mediastinal
lymphadenopathy, with a normal white cell count and differential, and the tumor must be
predominantly in the gastrointestinal tract
When primary, they may be multifocal in as many as 15% of cases
Predisposing conditions include immunodeficiency conditions, CD, and celiac disease
Sarcomas
-
make up only 10% of small-bowel malignancies
Overall these tumors are located in the jejunum and ileum, are relatively slow growing, and are
locally invasive
Their growth pattern is most commonly extramural and therefore, they rarely result in obstruction,
but sometimes present with free intra-abdominal bleeding
Due to their insidious nature and growth pattern, greater than three-fourths of these tumors exceed 5
cm in diameter at the time diagnosis
The most common histologic subtypes are GISTs, leiomyosarcomas, fibrosarcomas, liposarcomas,
and malignant schwannomas and angiosarcomas
small-bowel sarcomas rarely metastasize to regional lymph nodes
Hematogenous dissemination tends to be the preferred route of distant spread, primarily to the liver,
lungs, and bone
Peritoneal sarcomatosis is noted in later stages of the disease
Malignant GIST
-
is now considered the most common sarcoma of the gastrointestinal tract and accounts for about 5%
of all small bowel malignancies
Clinical, histopathological, ultrastructural, and molecular-biological findings havemade clear that
GIST is a completely separate entity from leiomyoma and leiomyosarcoma
GISTs originate from stem cells that differentiate towards the interstitial cells of Cajal (ICCs)
ICCs arise from precursor mesenchymal cells and are the pacemaker cells of the gastrointestinal tract
Both ICCs and GISTs express KIT protein, have similar ultrastructural features, and express the
embryonic form of the heavy chain of smooth muscle myosin
KIT immunostaining has become the gold standard for the diagnosis of GIST and the term “GIST”
should apply only to tumors with KIT immunopositivity
Page 160 of 269
Clinical Features
Benign Neoplasms
- The vast majority of patients are asymptomatic
-
The most common presentation of benign tumors:
o intermittent episodes of acute crampy abdominal pain associated with intussusception
o followed by chronic bleeding with iron deficiency anemia in up to 50% of patients
Malignant Neoplasms
-
most of those with malignancies are symptomatic prior to diagnosis
Generally associated with weight loss
Vague, nonspecific symptoms
In general, most symptoms can be attributed to the location of the tumor, its rate of growth, and its
size
For example, tumors in the duodenum tend to be symptomatic at an earlier stage, presenting with
pain, gastric outlet obstruction, or obstructive jaundice
Those in the jejunum or ileum may present at a later stage with obstructive symptoms
Obstruction in this setting tends to be progressive, compared to benign lesions, whose obstructive
symptoms tend to be intermittent as they relate to episodes of intussusception
Bleeding and perforation (in up to 10%) may also occur, predominantly in lymphomatous lesions,
but this can also be a feature of any malignant tumor because of ulceration or necrosis
Carcinoid tumors produce symptoms secondary to hormone production: hot flashes, bronchospasms,
and arrhythmias
This constellation of symptoms, called carcinoid syndrome, occurs when the liver is not able to
metabolize the active substances produced by the carcinoid tumor
This is usually the case when tumors are either bulky or metastatic or their venous drainage bypasses
the liver
Laboratory Findings
-
A high index of suspicion is required due to the lack of specificity of these tumor’s signs and
symptoms
A correct preoperative diagnosis is made in up to only 50% of patients
Biochemical and hematologic studies are often not helpful
Iron deficiency anemia may be detected with chronic blood loss; elevated liver enzymes may be
noted with periampullary lesions or hepatic metastases
elevated 24-hour urinary 5-hydroxyindoleacetic acid can be detected in more than 50% of patients
with carcinoid tumors
Imaging Studies
-
Radiographic-contrast imaging modalities tend to be the most useful in the establishment of the
diagnosis
Plain films of the abdomen are generally not helpful- may demonstrate nonspecific signs of
obstruction or a mass
CT, US, MRI
Abdominal CT has a sensitivity of 50%-80% in detecting the primary small bowel tumors and
occasionally plays an important role in differentiating benign from malignant tumors
CT is valuable in staging malignant tumors
Fluorodeoxyglucose (labeled with fluorine-18) positron emission tomography (FDG-PET)
o has been shown to be highly sensitive to assess disease status in patients with GISTs
o FDG-PET is used for preoperative staging, but more importantly to assess response to
therapy
Page 161 of 269
Endoscopy
Staging Classification
Primary tumor (T)
-
TX: primary tumor cannot be assessed
-
T0: no evidence of primary tumor is present
-
Tis: carcinoma in situ is present
-
T1: tumor invades the lamina propria or submucosa
-
T2: tumor invades the muscularis propria
-
T3: tumor invades through the muscularis propria into subserosa or into nonperitonealized
perimuscular tissue (mesentery or retroperitoneum), with extension of less than 2 cm
-
T4: tumor penetrates the visceral peritoneum or directly invades other organs or structures
Regional lymph nodes (N)
-
NX: Regional lymph nodes cannot be assessed
-
N0: No regional lymph node metastasis is present
-
N1: Regional lymph node metastasis has occurred
Distant metastases (M)
-
MX: Presence of distant metastasis cannot be assessed
-
M0: No distant metastasis is present
-
M1: Distant metastasis has occurred
For small bowel lymphoma the most commonly used staging system is the Ann Arbor system based on
lymphatic and extralymphatic involvement on either side of the diaphragm
Treatment
Treatment of adenocarcinoma
-
For duodenal lesions the availability of endoscopic ultrasound has allowed better preoperative
staging and the availability of endoscopic resection techniques has offered additional therapeutic
options
Ultrasound proven benign duodenal or ampullary adenomas can be resected endoscopically with
excellent results
Invasive lesions of the first and second portion of the duodenum without major vessel involvement
and distant spread are best treated by a pancreaticoduodenectomy (Whipple procedure)
For tumors in the third or fourth portion of the duodenum segmental resection with regional
lymphadenectomy is indicated
Palliative options for unresectable or metastatic duodenal carcinoma include gastrojejunostomy and/
or biliary enteric bypass or endoscopic/interventional placement of stents to relieve the intestinal
and/or biliary obstruction
Adenocarcinoma of the jejunum and ileum is treated by wide excision, including areas of contiguous
spread and the associated mesentery, with negative surgical margins
Page 162 of 269
-
Palliation of chronic blood loss in patients with locally advanced unresectable duodenal carcinomas
radiotherapy may provide short-term benefit
Therapy for carcinoid tumors
-
The mainstay therapy is radical surgical excision
-
These lesions have the propensity to metastasize even when very small
Large lesions near the ampulla may require a pancreaticoduodenectomy for cure, while smaller
lesions may be treated with either local excision or endoscopic resection with close endoscopic
follow-up
Likewise lesions of the terminal ileum or carcinoid tumors of the appendix larger than 2 cm require a
formal right hemicolectomy for oncologic clearance of disease
-
Treatment for advanced locoregional and distant disease
-
includes both medical and surgical modalities
Surgery should be indicated in patients with resectable metastatic disease for potential cure or at
least meaningful palliation
Treatment of small bowel lymphoma
-
requires conservative resections with para-aortic and mesenteric lymph node sampling, liver biopsy
and bone marrow biopsy performed for staging
Low-grade localized lesions are treated with resection alone, while for intermediate and high-grade
lesions resection and chemotherapy is recommended
Radiation is used only for palliation in poor performance patients (bowel necrosis, bleeding,
perforation)
Treatment for small bowel sarcomas
-
Consists of an en block resection with tumor free margins
There is no role for extended lymphadenectomy in these tumors
Hematogenous dissemination is the preferred route of metastatic spread to the liver lungs and bones
In the presence of metastatic disease, local excision or palliative bypass procedure might be
indicated to prevent or ameliorate bleeding and obstruction
there is no clear benefit from chemoradiation therapy in the adjuvant setting, since radiation doses
are limited due to small bowel toxicity
Treatment of localized GISTs
-
is based on surgical resection: the tumor should be removed en block with its pseudocapsule and
margins of normal soft tissue or bowel
In the presence of large lesions involving other organs, where an en block resection may be
associated with significant morbidity, preoperative neoadjuvant use of imatinib mesylate may be
entertained
Prognosis
Adenocarcinoma
-
based on similar variables as for colorectal cancer, including stage, perineural and vascular invasion,
grade, resectability, and surgical margins
The majority of tumors have regional spread at time of diagnosis, and up to one-fourth of patients
have distant organ disease
Overall, the 5-year survival rate is 20%-30%
For resectable disease of the duodenum, the 5-year survival rate approaches 50%
Page 163 of 269
Carcinoid tumors
-
with localized disease is excellent with 5-years survival rates approaching 100% after resection
More than 90% of the symptomatic patients have metastatic disease at the time of surgical
exploration
For tumors less than 1 cm in size, the risk of lymph node metastases is on the order of 2%; for 1-2
cm lesions, there is an approximate 50% incidence of lymph node involvement; and 80% of tumors
greater than 2 cm have positive nodes
Survival rates of up to 68% at 5 years have been reported when all gross metastatic disease,
including hepatic metastases, is resected
The 5-years survival for unresectable disease is approximately 35%-40%
Small bowel lymphoma
-
include higher grade, greater depth of tumor penetration, lymph node involvement, peritoneal
disease and distant metastases
Overall 5-year survival rates range from 20% to 40% for all stages
Five-year survivals of up to 60% have been reported for patients with resected localized low-grade
tumors
Sarcomas
-
GIST
-
an insidious growth pattern and greater than three-fourths of these tumors are larger than 5 cm at the
time of diagnosis and up to 50% of them are not resectable for cure when the diagnosis is established
Five-year survival after curative resection ranges from 60% to 80% for low-grade tumors and is no
more than 20% for high-grade lesions
While almost all small (< 1 cm) GISTs are clinically benign and tumors larger than 5 cm in diameter
are generally malignant
The median disease-specific survival is about 5 years for primary disease, and 10-20 months in
recurrent or metastatic disease
Most recurrences take place within 5 years of the primary diagnosis, but in the slowly proliferating
subset of GISTs and especially after therapy with imatinib mesylate, metastases can appear more
than 10 years after the primary diagnosis
Meckel’s diverticulum
General
-
-
is a congenital outpouching or bulge in the lower part of the small intestine
The bulge is a leftover of the umbilical cord
is the most commonly encountered congenital anomaly of the small intestine, occurring in about
2%-3% of the population
is located on the antimesenteric border of the ileum 45 to 60 cm proximal to the ileocecal valve
results from incomplete closure of the omphalomesenteric, or vitelline, duct
may exist in different forms, ranging from a small bump that may be easily missed to a long
projection that communicates with the umbilicus by a persistent fibrous cord or, much less
commonly, a patent fistula
The usual manifestation is a relatively wide-mouthed diverticulum measuring about 5 cm in
length, with a diameter of up to 2 cm
Cells lining the vitelline duct are pluripotent; therefore, it is not uncommon to find heterotopic
tissue within the Meckel diverticulum
o the most common of which is gastric mucosa (present in 50% of all Meckel’s
diverticula)
▪ cells from stomach can secrete acid, which can cause ulcers and bleeding
o Pancreatic mucosa is encountered in about 5% of diverticula
o Less commonly, diverticula may harbor colonic mucosa
The condition is equally common among males and females, but males are two to three times
more likely to have complications
Page 164 of 269
Etiology
-
Meckel's diverticulum occurs in a fetus early in the pregnancy
Normally, the vitelline duct, which connects the growing fetus with the yolk sac, is absorbed into
the fetus by the seventh week of the pregnancy! When the vitelline duct is not fully absorbed, a
Meckel's diverticulum develops
Clinical Features
-
Gastrointestinal bleeding (which can be seen in the stool)- The most common clinical
presentation, occurs in 25% to 50% of patients who present with complications:
o Hemorrhage in children 2 years of age or younger
o This complication may present as acute massive hemorrhage, anemia secondary to
chronic bleeding, or a self-limiting recurrent episodic event
o The usual source of the bleeding is a chronic acid-induced ulcer in the ileum adjacent to
a Meckel’s diverticulum that contains gastric mucosa
-
Abdominal pain and cramping
Tenderness near the belly button
Obstruction of the bowels. This can cause pain, bloating, diarrhea, constipation, and vomiting
o
-
-
Diagnosis
Treatment
-
may occur as a result of a volvulus of the small bowel around a diverticulum associated
with a fibrotic band attached to the abdominal wall, intussusception or, rarely,
incarceration of the diverticulum in an inguinal hernia
Diverticulitis (swelling of the intestinal wall)
o
10%-20% of symptomatic complications
o
More common in adult patients
o
Clinically indistinguishable from appendicitis (should be consider in the DDx of a
patient with RLQ pain)
Rare complications include neoplasms
o with the most common benign tumors reported as leiomyomas, angiomas, and lipomas
o malignant neoplasms include adenocarcinomas, which generally originate from the
gastric mucosa, sarcoma, and carcinoid tumor
The diagnosis of Meckel’s diverticulum may be difficult
Plain abdominal radiography, CT, and ultrasonography are rarely helpful
In children the single most accurate diagnostic test is Technetium scan (99mTc)
The 99mTc-pertechnetate is preferentially taken up by the mucus-secreting cells of gastric
mucosa and ectopic gastric tissue in the diverticulum
The diagnostic sensitivity of 85%, specificity of 95% and an accuracy of 90% in the pediatric
age group
In adults, however, 99mTc-pertechnetate scanning is less accurate because of the reduced
prevalence of ectopic gastric mucosa within the diverticulum
Colonoscopy: In this test, a small, flexible tube with a camera on the end is inserted into the
rectum and colon to look for blockages and the cause of bleeding
Wireless capsule endoscopy: For this test, the patient swallows a small camera that can detect
sources of bleeding in the small intestine
May be asymptomatic, in this case usually does not require treatment
The treatment of a symptomatic Meckel’s diverticulum should be prompt surgical intervention
with resection of the diverticulum or resection of the segment of ileum bearing the diverticulum
Segmental intestinal resection is required for treatment of patients with bleeding because the
bleeding site is usually in the ileum adjacent to the diverticulum
Resection of the diverticulum for nonbleeding Meckel’s diverticula can be performed using a
hand-sewn technique or stapling across the base of the diverticulum in a diagonal or transverse
line to minimize the risk for subsequent stenosis
Reports have demonstrated the feasibility and safety of laparoscopic diverticulectomy
The long-term prognosis is excellent. Patients can expect a full recovery after treatment
Page 165 of 269
73. Cholecystitis: definition, types, causes, diagnosis, complications and treatment.
Cholelithiasis (gallstones)
Cholecystitis
Definition
= Inflammation of the gallbladder
Types
- acute calculous
- acute acalculous
- chronic
General
- acalculous cholecystitis develops in absence of gallstones as a result of ischemia and
gallbladder stasis (incidence 0.2-3% in critically ill patients or in patients with vascular disorders)
- in acute cholecystitis the gallbladder is usually distended and, besides bile, contains stones,
sludge and an inflammatory exudate; histologically comprises an inflammatory infiltrate of
polymorphous nuclear granulocytes with edema or, in advanced stages, necrosis
- in chronic cholecystitis, the inflammatory infiltrate is replaced by lymphocytes and plasma cells
eventually resulting in mucosal atrophy and fibrous thickening of the gallbladder wall
Causes
- Gallstones: most often, cholecystitis result of gallstones; they can block the cystic duct through
which bile flows when it leaves the gallbladder —> bile builds up, causing inflammation
- Tumor: a tumor may prevent bile from draining out of your gallbladder properly, causing bile
buildup that can lead to cholecystitis
- Bile duct blockage: kinking or scarring of bile ducts can cause blockages that lead to
cholecystitis
- Infection: AIDS and certain viral infections can trigger gallbladder inflammation
- Blood vessel problems: a very severe illness can damage blood vessels and decrease blood
flow to the gallbladder, leading to cholecystitis
- The greates risk facotr for cholecystitis is gallstones — Risk factors for gallstones include:
female sex, increasing age, pregnancy, oral contraceptives, obesity, diabetes mellitus, ethnicity
(Native North American), rapid weight loss
- Chronic cholecystitis occurs after repeated episodes of acute cholecystitis and is almost always
due to gallstones
Clinical presentation
- typically causes worsening pain lasting longer than 5 hours
- located in the right upper quadrant and accompanied by signs of inflammation such as fever,
chills, and in severe cases, signs of sepsis
- jaundice may be present in patients with sepsis or as a consequence of Mirizzi syndrome (a
stone impacted in the cystic duct may produce intermittent obstruction of the common bile duct)
- on examination, there is tenderness in the right hypochondrium with or without a palpable mass
- pain and an arrest in inspiration upon deep palpation underneath the right costal margin
(Murphy’s sign) may be present and has a sensitivity and speci city of 65% and 87%,
respectively
Diagnosis
- blood chemistry will show signs of inflammation and possibly of cholestasis; aerobe and
anaerobe blood cultures may become positive
- transabdominal ultrasaound is the single most useful diagnostic tool with a sensitivity of
specificity of >90% and >80%
- typical findings are thickening of the gallbladder wall, which, however, may also be present in
patients with ascites or hypoalbuminemia, a positive sonographic Murphy’s sign,
Page 166 of 269
emphysematous cholecystitis with gas bubbles in the gallbladder wall (so-called champagne
sign), or signs of perforation or abscess formation
- abdominal CT is useful, particularly if the initial diagnosis of abdominal pain is obscure
- Boas’s sign: pain in the are below the right scapula, can be a symptom of acute cholecystitis
Complications
- if not detected early or treated properly, signs of complications include:
- high fever, shock, jaundice
- gangrene; gallbladder rupture (Cholecystitis causes the gallbladder to become distended and
firm. Distension can lead to decreased blood flow to the gallbladder, causing tissue death and
eventually gangrene. Once tissue has died, the gallbladder is at greatly increased risk of rupture
(perforation); Rupture can also occur in cases of chronic cholecystitis)
- empyema (collection of pus surrounding the gallbladder)
- fistula formation and gallstone ileus (adhesions most commonly between the gallbladder and
other parts of GI tract)
- gallstone pancreatitis
- common bile duct stones
- inflammation of the common bile duct
Treatment
- emergency treatment consists of fasting, fluid resuscitation, spasmolytics, and analgesia,
preferably with NSAIDs
- in addition, intravenous antibiotic therapy covering Gram-negative enteric microorganisms (e.g.,
broad spectrum acyl-ureidopenicillins/third-generation cephalosporins/chinolones) should be
started
- most patients respond to initial conservative medical treatment; However, up to 20% develop
signs of advanced cholecystitis (fever >38°C, serum bilirubin >10 mg/dL or 170 μmol/L) and
need emergency surgery to avoid complications such as gangrene, perforation, peritonitis, or
sepsis
- laparascopic gallbladder removal, within 24 hours if possible (iwie sind da zwei verschiedene
ansätze — konservativ oder operativ)
Cholelithiasis
Essentials
- prevalence: 10-15% in Western societies
- 80% cholesterol stones; <20% pigment stones
- Gallbladder stones: appr. 30% become symptomatic (mostly biliary pain, less often from
complications)
- bile duct stones: at least 50% become symptomatic
- risk factors: genetic predisposition, older age, female gender, obesity, weight loss, pregnancy,
terminal ileal disease, parenteral nutrition, drugs
- lower than average incidence observed with increased physical activty, caffeine, statin use,
alcohol consumption
- prevention of gallstone formation to be considered during weight reduction using
ursodeoxycholic acid 600mg/day or during prolonged parenteral nutrition
- diagnosis is typically confirmed by ultrasound
- complications may be detected on blood tests
General
- mostly formed from cholesterol crystals in cholesterol-supersaturated gallbladder bile —>
crystals are then trapped in mucin, which overlays a dysfunctional gallbladder wall, and finally
become stones
- most frequent symptom caused by sludge or gallstones is biliary colic, characterized by pain in
the right upper quadrant and epigastrium; but mostly asymptomatic
- bile duct stones (choledocholithiasis) more often induce biliary pain, jaundice, acute biliary
pancreatitis and/or ascending cholangitis
Page 167 of 269
- inflammatory reaction of the gallbladder wall (cholecystitis) usually initiated when a stone or a
sludge becomes impacted by the gallbladder neck or cystic duct
- acalculous cholecystitis may occur as a consequence of an impaired microcirculation and/or
infection of the gallbladder wall
Causes and pathogenesis
Causes and risk factors
- pregnancy and childbirth are important risk factors
- other risks are age, obesity, rapid weight loss or weight fluctuations
- risk also increases with serum triglyceride levels and there is an inverse correlation to HDL
cholesterol in serum
- clinical conditions associated with gallstone formation are parenteral nutrition, diseases of the
terminal ileum (Crohn’s disease), pancreatic insufficiency and spinal cord injury
- black pigment stones are more frequently observed in chronic hemolysis and in up to 30% of
patients with liver cirrhosis
Gallstone formation
- gallstones are classified as cholesteral and pigment stones
- cholesterol stones consist of > 50% cholesterol monohydrate crystals, bound in a matrix of
glycoproteins often with a core of calcium bilirubinate (up to 80% in western world)
- three principal mechanisms contribute to their formation: secretion of bile supersaturated with
cholesterol, accelerated nucleation of cholesterol crystals and gallbladder hypomotility
- in bile, cholesterol is kept in aqueous solution by the detergent action of bile acids and
phospholipids —> An increase in cholesterol saturation results in the formation of unilamellar
and nally unstable multilamellar vesicles
- accelerated nucleation time may be due to an excess of pronucleating factors (e.g. mucin
glycoproteins) or a deficiency of antinucleating factors
- black pigment stones are mainly found with chronic hemolysis, liver cirrhosis, cystic fibrosis, or
diseases of the terminal ileum
- pigment stones are composed of calcium bilirubinate and develop as a consequence of bilirubin
supersaturation of bile along with biliary proetins and mucins
- brown pigment stones are mostly formed within the bile ducts as a consequence of bacterial
infection and hydrolysis of glucuronic acid from bilirubon by bacterial beta-glucuronidase —>
decreased solubility of deconjugated bilirubin
Treatment
- Asymptomatic cholelithiasis is not an indication for cholecystectomy (risk outweighs advantage),
exception are e.g. prevention of gallbladder cancer in male patients with stones >3cm; in
patients undergoing baratric surgery for morbid obesity
- in symptomatic cholelithiasis, emergency treatment of biliary colic is accomplished by
spasmolytics (e.g. butylscopolamine 40mg i.v.) and NSAIDs (e.g. metamizol 1g i.v., diclofenac
75mg i.m.)
- cholecystectomy by laparoscopic approach should be performed to avoid the 50-70% rate of
recurrence as well as the 1-2% risk of complications from gallstone disease
- in selected patients who do not wish to undergo an operation and have solitary, non-calci ed
stones with a diameter of less than 20 mm and a well-contracting gallbladder, an attempt of
extracorporeal shock wave lithotripsy (ESWL) and oral litholysis with UDCA (ursodeoxycholic
acid 10–15mg/kg body weight/day) for 6–12 months is justified
- patients with tiny floating stones may profit from prolonged UDCA treatment alone
Page 168 of 269
74.) Choledocholithiasis
General
-
Choledocholithiasis, or common bile duct stones, are classified by their point of origin
Primary common duct stones arising de novo in the bile duct
Secondary common duct stones passing from the gallbladder into the bile duct
o Usually cholesterol stones (yellow-green stones)
o Most common found in developed countries
Primary choledocholithiasis is generally from brown pigment stones, which are a combination of
precipitated bile pigments and cholesterol
Brown stones are more common in Asian populations and are associated with a bacterial
infection of the bile duct
The bacteria secrete an enzyme that hydrolyzes bilirubin glucuronides to form free bilirubin,
which then precipitates
Most common duct stones found in the United States are secondary, and are termed retained
common duct stones when found within 2 years following cholecystectomy
Clinical Features
Clinically silent
-
Many common duct stones are clinically silent and may be identified only during
cholangiography, if performed routinely during cholecystectomy
Without pain or an abnormal liver function panel, a setting in which selective cholangiography is
not performed, 1% to 2% of patients following cholecystectomy will present with a retained
stone
When performed routinely, intraoperative cholangiography identifies choledocholithiasis in
approximately 10% of asymptomatic patients, suggesting that most choledocholithiasis remains
clinically silent
Presents with symptoms
Diagnosis
-
-
Symptoms ranging from biliary colic to the clinical manifestations of obstructive jaundice, such
as darkening of the urine, scleral icterus, and lightening of the stools
Jaundice with choledocholithiasis is more likely to be painful because the onset of obstruction is
acute, causing rapid distention of the bile duct and activation of pain fibers
Fever, a common symptom, can be associated with right upper quadrant pain and jaundice, a
constellation known as Charcot’s triad
This triad suggests ascending cholangitis and, if untreated, may progress to septic shock
The addition of hypotension and mental status changes, both evidence of shock, to Charcot’s
triad is known as Reynolds pentad
Murphy's sign is commonly negative on physical examination in choledocholithiasis, helping to
distinguish it from cholecystitis
In the setting of choledocholithiasis, abnormalities of the hepatic function panel are common but
neither sensitive nor specific and, with superinfection, leukocytosis may also be present
Ultrasound may show choledocholithiasis or only biliary ductal dilation
In patients with biliary pain, gallstones and jaundice, a dilated bile duct (>8 mm) is highly
suggestive of choledocholithiasis, even if common duct stones are not documented
ultrasonographically
Even without symptoms of biliary colic, a dilated bile duct in the presence of gallstones suggests
choledocholithiasis
Ultrasound should be used routinely for evaluation of the gallbladder and biliary tree, but the
remaining studies should be chosen selectively based on the likelihood of finding common duct
stones
Patients with highest risk, such as those with cholangitis or a dilated biliary tree, should undergo
ERCP
Those with lower risk can undergo laparoscopic cholecystectomy with cholangiography, and
possible laparoscopic common duct exploration, or MRCP, depending on the surgeon’s expertise
Page 169 of 269
-
Generally, choledocholithiasis identified but not removed during cholecystectomy mandates an
ERCP for stone extraction
ERCP (endoscopic retrograde cholangiopancreatography)
-
ERCP is highly sensitive and specific for choledocholithiasis
can usually be therapeutic by clearing the duct of all stones in approximately 75% of patients
during the first procedure and approximately 90% with repeat ERCP
During the endoscopic procedure, a sphincterotomy is performed with a balloon sweep and
extraction of the stone, all of which have a complication rate of 5% to 8%
Indications for preoperative ERCP prior to cholecystectomy include cholangitis, biliary
pancreatitis, limited surgeon experience with common duct exploration, and patients with
multiple comorbidities
MRCP (magnetic resonance cholangiopancreatography)
-
is highly sensitive (>90%) with an almost 100% specificity for the diagnosis of common duct
stones
As a noninvasive test, MRCP provides accurate imaging of the biliary tree but, in the setting of
choledocholithiasis, does not provide a therapeutic solution
A clear cholangiogram by MRCP eliminates the need for ERCP
However, choledocholithiasis identified by MRCP requires intervention by some other method
PTC (percutaneous transhepatic cholangiography)
-
can also be used to diagnose and treat choledocholithiasis
is an invasive test with a complication rate similar to ERCP
Although requiring less skill, and at a lower cost, PTC is as effective in patients with a dilated
biliary ductal system but less effective in the setting of a nondilated biliary tree
Treatment
ERCP
-
Endoscopic sphincterotomy with stone extraction is effective for the treatment of
choledocholithiasis
It can avoid an open procedure
Common reasons for endoscopic failure include large stones, intrahepatic stones, multiple
stones, altered gastric or duodenal anatomy, impacted stones, and duodenal diverticula
Sphincterotomy with stone extraction does not eliminate the risk of recurrent biliary stone
disease
Almost 50% of all patients have recurrent symptoms of biliary tract disease if not also treated by
cholecystectomy
More than one third of these patients eventually require cholecystectomy, suggesting that
cholecystectomy should be offered to patients who present with choledocholithiasis
Interestingly, older patients (>70 years), have only a 15% rate of symptom recurrence, so
cholecystectomy can be offered selectively to this patient population
Laparoscopic Common Bile Duct Exploration
-
At the time of cholecystectomy, an intraoperative cholangiogram will help identify
choledocholithiasis
A laparoscopic common duct exploration can then be performed in an attempt to manage all
calculous biliary tract disease in one setting, without the need for an additional anesthetic or
procedure
Access to the common duct with a small-caliber cholangioscope is provided via the cystic duct
or through a separate incision in the common duct itself
In the transcystic approach, the cystic duct is dilated and a flexible cholangioscope is passed
down into the common bile duct
For the transcystic approach in the setting of a narrow cystic duct, the duct can be dilated with a
flexible dilator passed over a wire, using a Seldinger technique
Page 170 of 269
o
-
stones in the common hepatic duct above the cystic duct insertion are not accessible
through the transcystic route
Other contraindications for the transcystic approach include a small, friable cystic duct,
numerous (more than eight) stones in the common bile duct, and large stones (>1 cm), which
would be difficult or impossible to extract through the cystic duct orifice
In any of these settings, a separate incision can be made in the common bile duct, with the only
contraindication being that of a small common duct that may become strictured on closure
Open Common Bile Duct Exploration
-
The frequency of open procedure has decreased because of the great use of endoscopic and
laparoscopic methods
Open exploration is used when endoscopy and laparoscopy are not feasible or when concomitant
biliary drainage is required
Open exploration carries a low morbidity (8% to 15%) and mortality (1% to 2%), with a low rate
of retained stones (5%)
Impacted stones at the ampulla present a difficult problem for ERCP and common duct
exploration
With unsuccessful attempts to remove an impacted stone in the setting of a nondilated biliary
tree, a transduodenal sphincteroplasty can provide drainage
In a similar setting, but with a dilated biliary tree, drainage of the biliary tree through a separate
choledochoenterostomy can be successful
The two options for drainage are that of a choledochoduodenostomy and Roux-en-Y
choledochojejunostomy
Anastomosis to the duodenum can be performed rapidly with a single anastomosis
This anatomic arrangement continues to allow endoscopic access to the entire biliary tree
The downside of this approach is that the bile duct distal to the anastomosis (side-to-side
choledochoduodenostomy) does not drain well and may collect debris that obstructs the
anastomosis or the pancreatic duct, a process known as sump syndrome
Anastomosis to the jejunum in a Roux-en-Y arrangement provides excellent drainage of the
biliary tree without a risk of sump syndrome, but does not allow future endoscopic evaluation of
the biliary tree
Intrahepatic stones, which are almost uniformly brown pigment stones, represent a different
management challenge than secondary bile duct stones (uncommon in Western populations)
These stones tend to occur specifically in patients with stasis of the biliary tree, such as those
with strictures, parasites, choledochal cysts, or sclerosing cholangitis
Because these stones collect at sites above obstructions, the transhepatic approach to
cholangiography is generally more successful
Percutaneous drainage catheters are left in place and upsized to perform percutaneous stone
extraction
Long-term management of intrahepatic stones must be carefully tailored to the disease but
frequently requires hepaticojejunostomy for better biliary drainage
Liberal use of choledochoscopy at the time of drainage procedure ensures removal of all current
stones
This approach allows a stone clearance rate of more than 90%
75.Cholangitis
Definition = an infection of the bile duct (cholangitis), usually caused by bacteria ascending from
its junction with the duodenum
Clinical presentation
- ascending cholangitis is usually due to bile duct obstruction with subsequent infection by gramnegative enteric bacteria (e.g. Klebsiella) or enterococci (in absence of obstruction even heavy
bacterial contamination of the ducts fails to produce symptoms or pathologic changes)
- the obstruction may be partial, or less commonly, complete
- the principal causes are choledocholithiasis, biliary stricture, and neoplasm. Less common
causes are chronic pancreatitis, ampullary stenosis, pancreatic pseudocyst, duodenal
diverticulum, congenital cyst, and parasitic invasion
Page 171 of 269
- it is a potential life-threatening complication presenting with fever, chills, and often posthepatic
jaundice => necessitates emergency treatment
- the symptoms of the Charcot’s triad (cholangitis) are biliary colic, jaundice and chills and fever
- longterm complications can be stricture formation, recurrent cholangitis with intrahepatic stone
formation, and secondary biliary cirrhosis
=> fever, chills and/ or persistent pain localized in the right upper quadrant lasting longer than 12
hours are suggestive of cholecystitis and/ or cholangitis
Diagnostic methods
- routine blood tests show features of acute inflammation (raised WBC count and elevated Creactive protein level) and usually abnormal liver function tests (LFTs)
- in most cases the LFTs will be consistent with obstruction: raised bilirubin, alkaline phosphatase
and y-glutamyl transpeptidase
- blood cultures are often performed in people with fever and evidence of acute infection; most
common bacteria are E. coli, Klebsiella and enterobacter or the gram-postive enterococcus
- medical imaging to identify the site and nature of obstruction
- ultrasound — may show dilation of bile duct and identifies 38% of bile duct stones; helps to
differentiatie between cholangitis and cholecystitis
- magnetic resonance cholangiopancreatography (MCRP)
- gold standard test for biliary obstruction is endoscopic retrograde cholangiopancreatography
(ERCP) — involves the use of endoscopy to pass a small cannula into the bile duct;
radiocontrast is injected to opacify the duct and x-rays are taken
Treatment
- i.v. fluids are administered, especially if BP is low; and antibiotics are commenced
- empirical treatment with broad-spectrum antibiotics is usually necessary until it is known for
certain which pathogen is causing the infection (combinations of penicillins and
aminoglycosides/ or ciprofloxacin are widely used; metronidazole is often added to specifically
treat the anaerobic pathogens; antibiotics are continues for 7-10 days)
- the definitive treatment is relief of the underlying biliary obstruction; usually done 24-48 hours
after admission, when patient is stable
- for patients with severe cholangitis or unremitting cholangitis despite antibiotic therapy, the bile
duct must be promptly decompressed — Most cases of severe acute cholangitis are associated
with choledocholithiasis, for which the best treatment consists of emergency endoscopic
sphincterotomy
- ERCP is the most common approach to unblock the bile duct
- obstructing stones that are too large to be removed or broken mechanically by ERCP may be
managed by extracorporeal shock wave lithotripsy
Primary sclerosing cholangitis (weiß nicht ob das auch dazu gehört)
- it is a chronic cholestatic liver disease with a male predominance that usually presents during
the fourth decade of life
- it is characterized by slowly progressive inflammation and fibrosis of the intra- and extrahepatic
biliary trees, culminating with the development of biliary cirrhosis
- the pathogenesis is multifactorial; it has a strong association with inflammatory bowel disease
(IBD), especially ulcerative colitis
- risk for PSC is significantly decreased among current and former smokers
- currently no effective medical therapy is available —> liver transplantation is the only treatment
to improve the survival of patients with PSC
Page 172 of 269
Pathogenesis
- pathogenesis is multifactorial and further studies are required
- a genetic predisposition resulting in dysregulation of the immune system is evident
—> high prevalance (nearly 100 times higher) of PSC in first-degree relatives
- the role of an immune-related process and other mechanisms such as toxic and infectious
injuries related to intestinal transmigration of bacteria in patients with IBD has been considered
Liver pathology
- common liver histological findings include periductal fibrosis and inflammation, portal edema and
fibrosis, focal proliferation of bile ducts and ductules, focal bile duct obliteration, loss of bile
ducts, and cholestasis
- for histological staging, the commonly used criteria of Ludwig are as follows:
• stage I, cholangitis or portal hepatitis
• stage II, periportal fibrosis or periportal hepatitis
• stage III, septal fibrosis, bridging necrosis, or both
• stage IV, biliary cirrhosis
- but liver biopsy is not necessary used for diagnosis
Clinical presentation
- typical symptoms are pruritus and fatigue, although some patients (21%) are asymptomatic
when investigated for liver test abnormalities in IBD
- the course is a slowly progressive liver disease with inflammatory destruction of both
intrahepatic and extrahepatic bile ducts
- three quaters of patients with PSC in the US have IBD involving the colon, usually ulcerative
colitis —> the average time from onset of IBD to PSC is 9 years
- patients commonly have a high serum alkaline phosphatase (ALP) level of 3-5 times the upper
limit of normal; the serum transaminase levels elevated to a mild degree
- if hyperbilirubinemia develops, prompt investigation should be performed for identification of
complicating stricture
- endoscopic retrograde cholangiopancreatography is still considered the gold standard for PSC
diagnosis and to detect complications including biliary strictures, biliary stones, or CCA
- the key diagnostic features for PSC are composed of 1) the cholangiographic findings by ERCP
or magnetic resonance cholangiography (MRCP) showing diffuse multifocal biliary strictures or a
beading pattern of intra- or extrahepatic bile ducts with 2) compatible cholestatic liver enzyme
abnormalities with elevations in serum ALP and 3) exclusion of secondary causes, which can
cause biliary stricture (e.g. ischemia, cryptosporidosis, trauma)
Treatment
- Ursodeoxycholic acid (UDCA), a hydrophilic bile acid, is the most widely evaluated treatment of
PSC; dose of 8-30mg/kg/day —> improves liver tests
- Minocycline — 100mg orally twice daily for 1 year; significantly improves serum alkaline
phosphatase (ALP) and Mayo risk score
- Endoscopic therapy is currently used for patients with high-grade focal strictures of the bile
ducts, which are associated with poor outcome —> dominant biliary strictures are managed by
repeated angioplasty-type balloon dilation or biliary stent placement
- Liver transplantation is the best treatment in end stage PSC; it improves survival
Complications
- the complications of PSC include metabolic bone disease, chronic cholestasis, and malignancy,
and malignancy, especially CCA, which is the most lethal complication of PSC
- steatorrhea and vitamin deficiency (mainly vit. A/D or E) secondary to fat malabsorption, may
occur during the late stages of disease
- osteopenia occurs in appr. 9% of patients with PSC; older patients with longer duration of IBD
and more advanced liver disease are a high-risk group
- cholangiocarcinoma (CCA) — lifetime risk is up to 14-20% in PSC patients
- other cancers possible: gallbladder carcinoma, hepatocellular carcinoma, colorectal cancer
- colorectal cancer in PSC patients is 9%, 31% and 50% after 10, 20, and 25 years of disease
duration
Page 173 of 269
76. Mechanical jaundice (icterus mechanicus)
Key facts — physiology of bile
- Unconjugated bilirubin formed mainly in spleen by the breakdown of haemoglobin
- It is insoluble and is transported in the plasma bound to albumin
- Taken up by the liver by active transport, it is converted in the hepatocytes into conjugated
bilirubin (water-soluble)
- It is excreted into the bile canaliculi and via the main bile ducts into the duodenum
- Ten per cent of the unconjugated bilirubin is reduced to urobilinogen by small intestinal
bacteria, reabsorbed in the terminal ileum, and then excreted in the urine (enterohepatic
circulation)
- Ninety per cent is converted by colonic bacteria to stercobilinogen which is excreted in faeces
Jaundice is clinically apparent at serum bilirubin levels above 40mmol!!
General
- jaundice is a yellowish or greenish pigmentation of the skin and whites of the eyes due to high
bilirubin levels
- it is commonly associated with itchiness
- the feces may be pale and the urine dark
- jaundice in babies occurs in over half in the first week following birth and in most is not a
problem —> If bilirubin levels in babies are very high for too long, a type of brain damage,
known as kernicterus, may occur
- levels of bilirubin in blood are normally below 1.0 mg/dL (17 µmol/L) and levels over 2–3 mg/dL
(34-51 µmol/L) typically results in jaundice
- high bilirubin is divided into two types: unconjugated (indirect) and conjugated (direct)
- conjugated bilirubin can be confirmed by finding bilirubin in the urine
- other conditions that can cause yellowish skin but are not jaundice include carotenemia from
eating large amounts of certain foods and medications like rifampin
- blockage of the bile duct may occur due to gallstones, cancer, or pancreatitis
- Mechanical jaundice = post-hepatic jaundice (the pathology is located after the conjugation of
bilirubin in the liver caused due to obstruction of biliary passage
- Medical imaging such as ultrasound is useful for detecting bile duct blockage
- Treatment of jaundice is typically determined by the underlying cause —> If a bile duct
blockage is present, surgery is typically required; otherwise, management is medical (e.g.
treating infectious diseases)
Causes of Jaundice
Pre-hepatic jaundice (haemolytic)
- congenital abnormalities of red cell structure or content (e.g. hereditary spherocytosis, sickle
cell disease)
- autoimmune haemolytic anemia
- transfusion reactions
- drug toxicity
Hepatic jaundice (hepatocellular)
- Hepatic unconjugated hyperbilirubinaemia
• Gilbert’s syndrome: Deficiency or abnormalities of unconjucated biliruin uptake
• Crigler-Najjar syndrome: Abnormality of conjugation process enzymes
- Hepatic conjugated hyperbilirubinaemia
• Infection: viral (e.g. hepatitis A, B, C, EBV, CMV), bacterial (e.g. liver abscess), parasitic (e.g.
amoebic)
• Drugs, e.g. paracetamol overdose, antipsychotics, antibiotics
• Non-infective hepatitis, e.g. chronic active hepatitis, alcohol-related
Post-hepatic jaundice (obstructive/mechanical)
- Intraluminal abnormalities of bile ducts
• gallstones
Page 174 of 269
• blood clot
• parasites (e.g. flukes)
- Mural abnormalities of bile ducts
• cholangiocarcinoma
• congenital atresia
• sclerosing cholangitis
• biliary cirrhosis (primary (autoimmune) or secondary to sepsis)
• traumatic/post-surgical stricture
- Extrinsic compression of bile ducts
• pancreatitis
• tumors, e.g. head of pancreas, ampulla of Vater
• lymphadenopathy of porta hepatis nodes
Diagnostic tests
Function Test
Prehepatic jaundice
Hepatic jaundice
Posthepatic jaundice
Total Bilirubin
normal/increased
increased
increased
Conjugated bilirubin
normal
increased
increased
Unconjugated bilirubin
normal/increased
increased
normal
Urobilinogen
normal/increased
decreased
decreased/negative
Urine color
normal
dark
(urobilinogen+conjugate
d bilirubin)
dark (conjugated
bilirubin)
Stool color
normal
normal/pale
pale
Alkaline phosphatase
levels
normal
increased
increased
Alanine transferase
and aspartate
transferase levels
normal
increased
increased
Conjugated bilirubin in
the urine
not present
present
present
Splenomegaly
present
present
absent
Advanced tests
- Ultrasound scan (liver, gall bladder, bile duct and pancreas) — exclude the presence of
extrahepatic obstruction (dilated common bile duct); May locate cause and site of obstruction
- Magnetic resonance cholangiopancreatograpy (MRCP) for suspected extrahepatic obstruction
with no cause seen on ultrasound
- Liver biopsy for suspected hepatitis
Post-heaptic jaundice
- caused by interruption to drainage of bile containing bilirubin in the biliary system
- the most common causes are gallstones in the common bile duct, and pancreatic cancer in the
head of the pancreas
- in complete obstruction of the bile duct, no urobilinogen is found in the urine, since bilirubin has
no access to the intestine and it is in the intestine that bilirubin gets converted to urobilinogen
by microorganisms, with the urobilinogen later being partially reabsorbed from the intestine into
the general circulation, and then excreted into the urine
=> in this case, presence of bilirubin (conjugated) in the urine without urine-urobilinogen
suggests obstructive jaundice, either intra-hepatic or post-hepatic
Page 175 of 269
- the presence of pale stools and dark urine suggests an obstructive or post-hepatic cause as
normal feces get their color from bile pigments
- patients also can present with elevated serum cholesterol, and often complain of severe itching
or "pruritus" because of the direct and indirect effects of pruritogens in bile such as bile salts
Complications of jaundice
- Renal failure (hepatorenal syndrome): Caused by a combination of infection, dehydration, and
a direct effect of high levels of bilirubin and other toxic products of metabolism on the kidney;
mortality is highest when the patient is over 65 with an elevated blood urea
- Biliary infection (cholangitis): Commonest in obstructive jaundice or with previously damaged
biliary tree; commonly due to Gram –ve bacteria (e.g. Escherichia coli, Pseudomonas)
- Deranged coagulation: Due to decreased synthesis of vitamin K dependent clotting factors
(III, VII, IX, X) and impaired platelet function
- Relative immunosuppression: Predisposes to systemic infections (e.g. chest infection) and
reduces wound healing due to combinations of jaundice, infection, and reduced
proteosynthesis
Treatment
- General treatment includes fluid balance
- Correct dehydration — give up to 1000mL IV crystalloid if there is no pre-existing liver disease
- Monitor hourly urine ouptut — urethral catheter
- Treat infection
Specific treatments
- Endoscopic procedures (ERCP)
• Sphincterotomy: Used for common bile duct stone extraction, treatment of ampullary
strictures due to tumours or inflammation
• Stent insertion (plastic or expanding metal): Used for bile duct stones that cannot be
removed easily, post-operative or benign strictures, malignant strictures, external
compression of bile duct
• Percutaneous transhepatic cholangiogram (PTC): Used for stent insertion (often in
combination with ERCP), temporary external drainage of obstructed biliary system
• Surgical drainage (e.g. choledochoduodenostomy): Very rarely used
if other interventions failed due to very high morbidity and mortality
Elective treatment for obstructive jaundice
- ERCP and PTC may be used as above for stones, strictures, compression
- Surgical drainage (e.g. choledochoduodenostomy or cholecystojejunostomy) used for failed
interventional treatments
- Surgical resection, e.g. Whipple’s pancreaticoduodenectomy. Used for very selected cases
where pancreatic or distal bile duct tumours are benign or malignant, but potentially curable on
staging; staging of potentially suitable patients may include endoscopic ultrasound, CT scan,
ERCP or MRCP, visceral arteriography, laparoscopy.
77. Gallbladder mucocele (hydrops). Gallbladder empyema. Biliary peritonitis (bile
peritonitis).
Gallbladder mucocele
= distention of the gallbladder by an inappropriate accumulation of mucus or clear watery fluid
- the gallbladder is larger in size than normal due to overdistention caused by fluid within
- when left untreated, the gallbladder may become infected, press on the stomach thereby
blocking it and gallbladder rupture is also possible
- most cases of gallbladder mucocele arise as a complication of gallstones disease
Gallbladder anatomy and function
- the gallbladder is a hollow sac that stores bile containing wastes and fats among other
substances that need to be evacuated from the body
- normally this bile is secreted when a person eats food and digestion is occurring in the
duodenum, the first part of the small intestine
Page 176 of 269
- since bile has an emulsifying property, it is useful for breaking down the oils and fats in a fatty
meal —> by doing so, other digestive enzymes can act on the fats to break it down further and
allow for the body to absorb it from the gut
- the gallbladder can store as much as 1.5 liters of bile by drawing water out of the bile in the
gallbladder —>his concentrates the bile but also helps to reduce the space occupied in the
gallbladder
- the gallbladder has a fairly thick wall which can stretch to a very large degree thereby allowing
for a large quantity of bile to be stored if necessary
Blockage in the gallbladder
- bile empties out of the gallbladder through the narrow duct that joins the common bile duct
which leads to the duodenum
- when the neck of the gallbladder and its duct (cystic duct) is blocked, bile cannot flow out
- over a prolonged period of time, the bile and its salts are gradually resorbed through the
gallbladder wall
- mucus and water are secreted from the wall and accumulates within the gallbladder => this is a
mucocele
- usually the fluid within the gallbladder is sterile meaning that there are no microbes like bacteria
and there is also no pus
- over time the gallbladder expands and distends often close to its maximum capacity, and
sometimes even beyond where it may then rupture
Effect on gallbladder
- in long term cases of overdistention, the walls of the bladder become thinner and even slightly
transparent
- the enlarged gallbladder may press against the duodenum and hamper stomach emptying
—> causes gastric outlet obstruction
- blood supply to the gallbladder is affected and an infection can set in eventually leading to
gangrene of the organ
- the thinner and overdistended gallbladder is weak and can rupture with serious implications
- the gallbladder contents that empty into the abdominal cavity may lead to peritonititis
Gallbladder mucocele causes
- a wide range of causes; most of them blocking the gallbladder outlet; some arise when a
person is not eating which does not stimulate the release of bile
- common causes:
• gallstones
• tumors, including polyps and cancer
• narrow cystic duct from birth (congenital)
• parasites in the gallbladder or bile ducts
Page 177 of 269
• external compressions of the gallbladder neck or cystic duct by swollen lymph nodes, or
tumors and enlarged organs around the gallbladder
• prolonged total parenteral nutrition (TPN)
• long term use of ceftriaxone (antibiotics)
- Rare causes in babies and children:
• Familial Mediterranean fever
• Fibrocystic disease
• Hepatitis
• Kawasaki sndrome
• Leptospirosis
• Mesenteric adenitis
• Nephrotic syndrome
• Streptococcal pharyngitis
• Typhoid
- other, less likely causes:
• hepatomegaly, bile duct cyst (choledochal cyst), kidney mass, adrenal mass, mass on
ascending colon, parasitic cysts, pancreatic pseudocyst
Symptoms
- non-specific and many other types of gallbladder disease and conditions of related organs may
present in a similar way:
• abdominal discomfort or pain on the upper right side (RUQ) or epigastric region
• nausea and vomiting
• palpable abdominal mass with some tenderness
• symptoms may worsen with eating, particularly fatty meals
- Symptoms of complications:
• fever and chills — infcted gallbladder and empyema
• pain persisting for more than 6 hours — acute cholecystitis
• jaundice — bilde duct obstruction
Diagnosis
- the symptoms alone may not be indicative
- the presence of a large palpable mass extending sometimes as low as the pelvis along with a
history of gallbladder disease and absence of fever and chills may raise the suspicion of a
mucocele
- further testing includes:
• Abdominal x-ray
• Ultrasound of the abdomen
• CT scan
• Magnetic resonance cholangiopancreatography (MRCP=
• diagnostic findings during surgery, such as clear fluid in the gallbladder and a blocked duct,
confirms the diagnosis
Treatment
- no medical treatment
- gallbladder obstruction, with or without mucocele or empyema, requirs surgical removal
(Cholecystectomy)
- removal can be either with open or laparoscopic approach
- open surgery — large incision is made in the right upper portion of the abdomen and the
gallbladder is then removed
- laparoscopic surgery
Gallbladder empyema
= abscess in the gallbladder/ distention of the gallbladder by pus
- it may be a complication of acute cholecystitis or the result of infection of a mucocele
- the gallbladder is distended with pus and may be palpable
- there is an increased incidence in those with diabtes and/or advanced atherosclerotic disease
- Clinical presentation: while patients with a gallbladder empyema may experience symptoms
similar to those with acute uncomplicated cholecystitis (fever, chills, rigors, and right upper
quadrant pain), signs of sepsis may not always be present
Page 178 of 269
- Pathology: the gallbladder neck is usually obstructed by a calculus (or rarely from a malignant
-
-
mass such as an underlying cholangiocarcinoma) which prevents pus from draining through
cystic duct
part of the gallbladder wall may become necrotic causing perforation — often walled off by the
omentum, forming a localized abscess
sometimes a perforation from the gallbladder may lead to the formation of a subphrenic
abscess or a generalised peritonitis
however, necrosis is rare because of the rich blood supply to the gallbladder from both the
cystic artery and the hepatic bed
Radiographic features:
• Ultrasound: may show the usual sonographic features of cholecystitis with added echogenic
content within the gallbladder lumen
• CT: may show general imaging features of cholecystitis with added high-attenuating material
(representing pus) within the distended gallbladder lumen
• MRI: may be helpful in distinguishing pus from sludge by using heavily T2 weighted
sequences, which may show fluid-fluid levels with dependent layering of purulent bile
the empyema must be drained at once — usualy achieved by ultrasonic or radiographic CTguided placement of a big tail catheter (if not possible, drained surgically)
also cholecystectomy can be an option
Biliary peritonitis
= peritonitis caused due to the presence of bile in the peritoneum or choleperitoneum
- bile peritonitis is a type of inflammation of the peritoneum which is caused due to the escape of
bile in to the free peritoneal cavity
- perforation of gall bladder, biliary trauma (thoracoabdominal trauma or Iatrogenic trauma), and
extra-hepatic bile ducts or peptic ulcers' spontaneous perforation may cause the leakage of
bile in to the peritoneal cavity and generate the symptoms in Bile Peritonitis
- there are various conditions which may cause perforations in gallbladder or the common bile
duct carrying the bile in to the small intestine whenever essential for digestion
—> mostly such perforations are caused during per-cutaneous needle biopsy of the liver and
also rarely erosion from biliary calculi may also cause the perforation leading to leakage of bile
from the gall bladder or the common bile duct
- there are serious conditions in Bile peritonitis where it may be fatal unless operation is carried
out to repair bile peritonitis
Symptoms
- abdominal pain is the most common symptom
- loss of appetite
- energy loss
- vomiting
- loss of weight
- diarrhea
- skin turns yellow; yellowish eyes
- swollen abdomen; comperatively larger in size than normal
- in case of of an infectious bile peritonitis, there can be symptoms of fever in the patient
Causes
- usually caused by inflammation of the gallbladder or common bile duct which may be due to
perforations or ruptures caused during percutaneous needle biopsy
- inflammation in gallbladder leading to bile peritonitis may also be due to infection or a blockage
of the gallbladder ducts because of the diseased conditions like gallstones, cancer,
stenosis, pancreatitis etc.
Diagnosis
- in case of the onset of peritonitis, the peritoneum gets dull within 2-4 hours
- there may be scarce serous or light turbid fluid in the peritoneum in case of peritonitis and may
later on the exudates get creamy
- symptoms shown or experienced in bile peritonitis form the basis of diagnosis
Page 179 of 269
- the diagnostic procedures include: blood sample to determine WBC count, abdominal x-ray, CT
of abdomen, whole abdomen ultrasound, laparoscopic or peritoneal lavage may also be
performed
Treatment
- treatment depends on the source or underlying cause of peritonitis
- in serious cases, an emergency laparotomy is usually performed where any damaged, ruptured
or perforated organ is repaired
- also treated by giving antibiotics via i.v. together with essential fluids to prevent dehydration
- antibiotics may also be directly infused in to the peritoneum —> e.g. Cefoxitine, Cephalosporin,
Ampicillin, …
Prognosis
- untreated unfavorable outcome, often leading to the patients’ death
- with reatment the prognosis may vary based on the symptoms, level and conditions in the
individual suffering from the bile peritonitis
78. Cancer of the gallbladder and biliary ducts.
Cancer of the gallbladder
- Uncommon neoplasm, occuring in elderly patients (twice as common in women; due to
gallstone epidemiology)
- It is associated with gallstones in 70% of cases, and the risk of malignant degeneration
correlates with the length of time gallstones have been present
- Most primary tumors of the gallbladder are adenocarcinomas that appear histologically to be
scirrhous (60%), papillary (25%), or mucoid (15%)
- Dissemination of the tumor occurs early by direct invasion of the liver and hilar structures and
by metastases to the common duct lymph nodes, liver, and lungs
- In an occasional case, where carcinoma is an incidental finding after cholecystectomy for
gallstone disease, the tumor is confined to the gallbladder as a carcinoma in situ or an early
invasive lesion
- Most invasive carcinomas, however, have spread by the time of surgery, and spread is virtually
certain if the tumor has progressed to the point where it causes symptoms.
Signs and Symptoms
- most common complaint is right upper quadrant pain similar to previous episodes of biliary
colic but more persistent
- obstruction of the cystic duct by tumor sometimes initiates an attack of acute cholecystitis
- other cases present with obstructive jaundice and, occasionally, cholangitis due to secondary
involvement of the common duct
- if cholangitis is the prin- cipal symptom, a palpable gallbladder would be an unusual finding
with choledocholithiasis alone and should suggest gallbladder carcinoma
Imaging Studies
- CT and ultrasound scans may demonstrate the extent of disease, but more often they show
only gallstones
- The correct diagnosis is made preoperatively in only 10% of cases
Complications
- obstruction of the common duct may produce multiple intrahepatic abscesses
- abscesses in or next to the tumor laden gallbladder are frequent
Treatment
- if a localized carcinoma of the gallbladder is recognized at laparotomy, cholecystectomy should
be performed along with en bloc wedge resection of an adjacent 3-5 cm of normal liver and
dissection of the lymph nodes in the hepatoduodenal ligament
- If a small invasive carcinoma overlooked during cholecystectomy for gallstone disease is later
discovered by the pathologist, reoperation is indicated to perform a wedge resection of the liver
bed plus regional lymphadenectomy
Page 180 of 269
- In the few cases when cancer has not penetrated the muscularis mucosae, cholecystectomy
alone should suffice
- Lesions that invade the bile duct and produce jaundice should be resected if possible; When
not, a stent should be inserted endoscopically or percutaneously
- There is little that surgery can offer in cases with hepatic metastases or more distant spread.
Prognosis
- Radiotherapy and chemotherapy are not effective palliative measures
- About 85% of patients are dead within a year after diagnosis
- The 10% of patients who presently survive more than 5 years consist of those whose
carcinoma was an incidental finding during cholecystectomy for symptomatic gallstone disease
and those in whom an aggressive resection has removed all gross tumor
Malignant tumors of the bile duct
Essentials of diagnosis
- intense cholestatic jaundice and pruritus
- anorexia and dull right upper quadrant pain
- dilated intrahepatic bile ducts on ultrasound or
CT scan
- focal stricture on transhepatic or retrograde
endoscopic cholangiogram
General Considerations
- Primary bile duct tumors are not more common in patients with cholelithiasis, and men and
women are affected with equal frequency
- Tumors appear at an average age of 60 years but may appear at any time between 20 and 80
years of age
- More young people have been seen with this disease in recent years
- Ulcerative colitis is a common associated condition, and in occasional cases bile duct cancer
develops in a patient with ulcerative colitis who has been known to have sclerosing cholangitis
for several years
- Chronic parasitic infestation of the bile ducts in the Orient may be responsible for the greater
incidence of bile duct tumors in that area
- Most malignant biliary tumors are adenocarcinomas located in the hepatic or common bile duct
- The histologic pattern varies from typical adenocarcinoma to tumors composed principally of
fibrous stroma and few cells
- About 10% are bulky papillary tumors, which tend to be less invasive and less apt to
metastasize
- At presentation, metastases are uncommon, but the tumor has often grown into the portal vein
or hepatic artery
Signs and Symptoms
- Presents with gradual onset of jaundice or pruritus
- Chills, fever, and biliary colic are usually absent, and except for a deep discomfort in the right
upper quadrant the patient feels well
- Bilirubinuria is present from the start, and light-colored stools are usual
- Anorexia and weight loss develop insidiously with time
- Icterus is the most obvious physical finding
- If the tumor is located in the common duct, the gallbladder may distend and become palpable
in the right upper quadrant (The tumor itself is never palpable)
- Patients with tumors of the hepatic duct do not develop palpable gallbladders
- Hepatomegaly is common
- If obstruction is unrelieved, the liver may eventually become cirrhotic, and splenomegaly,
ascites, or bleeding varices become secondary manifestations
Page 181 of 269
Laboratory findings
- Since the duct is often completely obstructed, the serum bilirubin is usually over 15 mg/dL
- Serum alkaline phosphatase is also increased
Imaging studies
- Ultrasound or CT scans usually detect dilated intrahepatic bile ducts
- THC or ERCP clearly depicts the lesion, and both are indicated in most cases
- With tumors involving the bifurcation of the common hepatic duct (Klatskin tumors), it is
important to determine the proximal extent of the lesion (ie, whether the first branches of the
lobar ducts are also involved)
- ERCP is of value with proximal tumors because if it shows concomitant obstruction of the
cystic duct, the diagnosis will most often prove to be gallbladder cancer invading the common
duct (not a primary common duct neoplasm)
- The typical pattern with distal bile duct cancers consists of stenosis of the bile duct with
sparing of the pancreatic duct
- Adjacent stenoses of both ducts (the double-duct sign) indicate primary cancer of the pancreas
—> MR cholangiopancreatography may be useful if high-quality studies are available
Differential Diagnosis
- must consider other causes of extrahepatic or intrahepatic cholestatic jaundice
- choledocholithiasis is characterized by episodes of partial obstruction, pain and cholangitis,
which contrast with the unremitting jaundice of malignant obstruction
- bilirubin concentrations rarely surpass 15 mg/dL and are usually below 10 mg/dL in gallstone
obstruction, whereas bilirubin levels almost always exceed 10 mg/dL and are usually above 15
mg/dL in neoplastic obstruction
- a rapid rise of the bilirubin level to above 15 mg/dL in a patient with sclerosing cholangitis
should suggest superimposed neoplasm
- Dilatation of the gallbladder may occur with tumors of the distal common duct but is rare with
calculous obstruction
- the combination of an enlarged gallbladder with obstruc- tive jaundice is usually recognized as
being due to tumor
Treatment
- patients without evidence of metastases or other signs of advanced cancer (eg, ascites) are
candidates for laparotomy
- the 30% of patients who do not qualify may be treated by insertion of a tube stent into the bile
duct transhepatically under radiologic control or from the duodenum under endoscopic control
- the tube is positioned so that holes above and below the tumor reestablish flow of bile into the
duodenum
- if both lobar ducts are blocked by a tumor at the bifurcation of the common hepatic duct, it is
usually necessary to place a transhepatic tube into only one lobar duct
- If the lesion blocks the takeoff of the segmental ducts, stents are rarely beneficial
- Laparotomy is indicated in most cases, however, with the objective of removing the tumor
- Tumors of the distal common duct should be treated by radical pancreaticoduodenectomy
(Whipple procedure) if it appears that all tumor would be removed
- Secondary involvement of the portal vein is the usual reason for unresectability of tumors in this
location
- Mid-common duct or low-hepatic duct tumors should also be removed if possible —> If the
tumor cannot be excised, bile flow should be reestablished into the intestine by a
cholecystojejunostomy or Roux-en-Y choledochojejunostomy
- Tumors at the hilum of the liver should be resected if possible and a Roux-en-Y
hepaticojejunostomy performed
- A curative operation nearly always requires resection of either the right or the left lobe of the
liver and, in all cases, the caudate lobe
- Extension into the lobar and segmental ducts and secondary involvement of the hepatic artery
and portal vein are the most common reasons for inability to resect the tumor
- Subtotal resections offer little in the way of palliation
- Postoperative radiotherapy is commonly recommended
Page 182 of 269
Prognosis
- the average patient with adenocarcinoma of the bile duct survives less than a year
- the overall 5-year survival rate is 15%
- Following a thorough radical operation, 5-year survival is about 40%
- Biliary cirrhosis, intrahepatic infection, and general debility with terminal pneumonitis are the
usual causes of death
- Palliative resections and stents may improve the length and quality of survival in this disease
even though surgical cure is uncommon
79. Hydatid cyst (echinococcosis) of the liver.
Hydatid disease
Key facts
Occurs in sheep- and cattle-raising areas of the world, e.g. rural Wales, New Zealand, and not just
the tropics
Clinicopathological features
Pathological features
- Caused by the larval forms of the cestode worms, Echinococcus granulosus and
Echinococcus multinodularis
- Dogs are usually the primary host, eating infected sheep or cow offal, and the echinococcus
parasite, about 1cm long, develops in the dog’s intestine
- It consists of a head and three segments, the last of which contains hundreds of ova; These
are passed on to grass, for example, by defecation
- Sheep and cattle ingest the ova to complete the normal life cycle; Humans are an incidental
‘dead end’ host, but the ova penetrate the small intestine and enter the portal circulation
- Eighty per cent of the ova thrive in the liver with the development of hydatid cysts
- They may also enter the general circulation, forming cysts elsewhere (e.g. kidneys, lungs,
brain)
Clinical features/complications
- Infection is usually contracted in childhood, but produces symptoms and signs in adult life
- Commonest presentation is of a liver cyst (either found as a palpable mass, incidentally on
CT scanning, or during abdominal surgery)
- Compression of the intrahepatic bile ducts may produce jaundice
- Rupture of a cyst into the peritoneal cavity causes peritonitis and shock; Cyst fluid also
causes a severe allergic reaction with urticaria and eosinophilia if it enters the circulation
(either by spontaneous rupture or surgical intervention)
- The prognosis is poor
Diagnosis
- Casoni’s test (serum antigen) is positive in 80%, but gives many false positives
- Indirect haemagglutination tests are most accurate
- Ultrasound and CT scanning may be used to localize cysts
- ERCP may demonstrate connections with or compression of the bile ducts
Treatment
- Medical —Mebendazole 400mg tds for 30 days
- Intraperitoneal rupture
• Treat shock
• Carry out peritoneal toilet
• Give hydrocortisone before, during, and after surgery
- Surgical
• excision or aspiration of the cyst(s)
• extreme caution must be taken to prevent peritoneal contamination; Black packs soaked
in hypochlorite are placed around the liver to show up any daughter cysts or solices
• the cyst is partially aspirated and partially refilled with hypertonic saline which is scolicidal;
it is then carefully separated from the liver and the cavity closed or drained
• give mebendazole post-operatively
Page 183 of 269
80. Abscesses of the liver.
General/Etiology
- hepatic abscesses may be bacterial, parasitic, or fungal in origin (pyogenic most common,
followed by amebic)
- even distribution between single and multiple abscesses (90% of right love abscesses are
solitary, 10% of left lobe abscesses are solitary)
- in most cases, the development of a hepatic abscess follows a suppurative process elsewhere
in the body —> Many abscesses are due to direct spread from biliary infections such as
empyema of the gallbladder or protracted cholangitis; Abdominal infections such as
appendicitis or diverticulitis may spread through the portal vein to involve the liver with abscess
formation
- about 40% of patients have an underlying malignancy; other cases develop after generalized
sepsis from bacterial endocarditis, renal infection, or pneumonitis
- In 25% of cases, no antecedent infection can be documented (cryptogenic abscesses)
- Rare causes include secondary bacterial infection of an amebic abscess, hydatid cyst, or
congenital hepatic cyst
- in most common cases, the organism is of enteric origin: E. coli, Klebsiella pneumoniae,
bacteroides, enterococci, anaerobic streptococci are most common
- clinical suspicion is based on the presence of malaise, fever, anorexia, right upper quadrant
pain, and leukocytosis
- CT confirms the diagnosis by demonstrating one or more cystic lesions with internal bubbles and
ill-defined margins (also ultrasound and MRI)
- Differential diagnosis: amebiasis, echinococcal cyst, liver neoplasm, pyogenic abscess:
cholangitis, appendicitis, diverticulitis, gallbladder bacteremia
Symptoms and Signs
- when liver abscess develops in the course of another intraabdominal infection such as
diverticulitis, it is accompanied by increasing toxicity, higher fever, jaundice, and a generally
deteriorating clinical picture; Right upper quadrant pain and chills may appear
- in other cases, the diagnosis is much less obvious (illness develops insidiously) —> first
symptoms are usually malaise and fatigue, followed after several weeks by fever; epigastric or
right upper quadrant pain is present in half of cases (pain may be aggrevated by motion)
- the course of fever is often erratic, and spikes to 40-41°C are common
- Chills are present in about 25% of cases
- the liver is usually enlarged and may be tender to palpation
- Jaundice is unusal in solitary abscess, but often present in patients with multiple abscesses
and primary disease in the biliary tree and in general is a bad prognostic sign
Laboratory findings
- leukocytosis is present in most cases and is usually over 15,000/μL
- anemia is present in most; the average hematocrit is 33%
- serum bilirubin is usually normal except in patients with multiple abscesses or biliary
obstruction or when hepatic failure has supervened
- Alkaline phosphatase is often elevated even in the presence of a normal bilirubin
Treatment
- treatment includes antibiotics and percutaneous or surgical drainage
• when a pyogenic liver abscess is suspected, the first-line treatment is antibiotic therapy
• The most frequent bacteria are E. coli, Bacteroides, and streptococci
• The antibiotics should provide a broad Gram-negative and anaerobic coverage for 6 weeks
• If many small abscesses (<2cm) are encountered, it has been recommended that one fluid
collection be aspirated for culture and sensitivity
• If the abscess is large, percutaneous drainage should be attempted
• The complication rate is about 20% and complications include catheter dislodgement,
empyema, bacteremia, and hepaticobronchial fistula
• If no clinical improvement is observed after 72 hours of antibiotic treatment and percutaneous
drainage, surgical unroofing should be considered
Page 184 of 269
• The mortality rate for a treated hepatic abscess is 12–17%, depending on the patient
population
• Septic shock, jaundice, hypoalbuminemia, adult respiratory distress syndrome, and diabetes
are predictors of poor outcome
Complications
- the main complication of pyogenic liver abscess is sepsis — causes severe systemic
inflammation; can lead to a dangerous drop in BP; if not treated promptly with antibiotics and
intravenous fluid, sepsis can be fatal
- bacteria released and spread throughout the body can cause septic pulmonary embolism
(bacterium stimulates a clot), brain abscess and endophthalmitis
81. Benign tumors of the liver.
Hepatic hemangioma
- = disorganized collections of small blood vessels in the liver
- most frequent liver tumor, with a prevalence of 0.4-7.4%
- usually solitary and small, but can reach 20cm in diameter
- most patients are asymptomatic, their course is benign and diagnosis is incidental
- symptoms are uncommon but may include chronic abdominal pain and problems with eating,
especially with large lesions; rarely cause blood disorders (including platelet problems)
- bleeding is extremely infrequent
- giant hemangiomas may become symptomatic in the event of infarction or thrombosis
- US shows a well defined hyperechogenic lesion that after contrast administration displays an
initial peripheral globular-nodular enhancement and is followed by a centripedal fill in
- usually show up incidentally on an x-ray
- MRI is the best diagnostic method
- Treatment: can be removed by laparoscopic or open surgery
Focal nodular hyperplasia
- FNH is the second most common benign liver tumor
- in most cases it is solitary and smaller than 5cm, but it may be larger and multiple in 20% of
cases
- it is considered a regenerative cell response to an aberrant dystrophic artery
- the presence of a central fibrotic scar containing the feeding artery is a characteristic finding and
is used to establish the diagnosis
- in contrast to hepatic adenomas, it does not cause bleeding or have a risk of cancer
- Treatment: usually no treatment needed; if you have pain or other symptoms, sugery may be
performed to remove the tumor
Hepatocellular adenoma
- very uncommon, more frequently in young women; associated with oral contraceptive or
anabolic treatment and with glycogen storage disease type Ia
- mostly solitary, but in up to 10-20% more than one can be detected
- pain (right upper quadrant) is most common symptom, but not always present
- most frequent complication is necrosis and bleeding
- Recommended treatment:
• since many patients with adenomas are taking birth control pills, stopping these drugs is the
first line of therapy —> Tumors in some patients will shrink after withdrawal of birth control
pills
• adenomas larger than 4 cm should be surgically removed as there is a risk of rupture and a
small risk of cancer
• clotting the blood supply with embolization is a first line therapy for a bleeding adenoma
• radiofrequency ablation may help patients with many adenomas
Page 185 of 269
82. Liver cancer.
Hepatocellular carcinoma
- usually develops in the setting of chronic liver disease, and cirrhosis represents its strongest
predisposing factor (HBV)
- peak incidence between 50-60 years of age; most common malignancy in Asia and parts of
Africa (here hepatitis B infection is the predominant risk factor)
- other risk factors include: Aflatoxine (mainly Aflatoxin B1, Aspergillus flavus), Nitrosamine, and
nicotine and alcohol abuse, genetic metabolic diseases
- extremely poor prognosis
Symptoms
- pressure in the upper right abdomen possible
- weight loss, decrease in performance
- evtl. fever
- icterus
- complications: decompensation of a preexisting liver cirrhosis
Diagnosis
- α1-Fetoprotein (AFP) >20 μg/l (ca. 2/3 of cases)
- abdominal ultrasound shows a solitary/ multicentric/ diffuse infiltrating tumor
- biopsy for histologic confirmation
- CT-abdomen (with contrast), MRI, x-ray of the chest
Differential diagnosis
- malignant: embryonic hepatoblastoma, angiosarcoma, liver metastases, cholangiosarcoma,
cholangiocellular carcinoma
- benign: liver hemangioma, focal nodular hyperplasia (hamartoma), hepatocellular adenoma,
intrahepatic ductal cystic adenoma,
Page 186 of 269
Staging
Treatment
- partial liver resection (early stages) or even liver transplantation (when it fits the „Milan“ criteria
— one nodule up to 5cm, three nodules up to 3cm each)
- locally ablative therapy, e.g. percutaneous ablation, radiofrequency ablation, laser-induced
thermotherapy, intravasal injection with radioactive microspheres, transarterial
chemoembolisation (TACE)
- palliative systemic therapy with multi-kinase-inhibitor Sorafenib (Nexavar) (chemotherapy)
- in case of liver metastases, chemotherapy could be beneficial
Page 187 of 269
Angiosarcoma
- most common mesenchymal malignant tumor of the liver
- the tumor cells infiltrate the sinusoids, hepatic and portal veins and finally substitutes the hepatic
parenchyma
- morphology: spongy haemorrhagic nodules throughout the liver
- more common in males than in females
- etiologic agents include thorium dioxide, vinyl chloride, arsenic, copper sulphate, anabolic and
other steroids
- spread to regional lymph nodes, spleen, lungs, bone, adrenals, brain
- symptoms may mimic those of chronic liver disease, but in 15% of patients angiosarcoma is
diagnosed because of acute hemoperitoneum due to tumor rupture
- exttremely poor prognosis
Hepatic metastasis
- most malignant liver tumors are metastases from cancers that orginate in other organs, the most
frequent being lung, colon, stomach, pancreas, gallbladder, breast and ovaries
- metastatic involvement of the liver implies a poor prognosis, except in patients with colorectal or
neuroendocrine metastases that can be treated surgically
- fine-needle aspiration biopsy has an 85% diagnostic sensitivity with more than 95% specificty
- CT: metastases are hypovascular lesions
Hepatoblastoma
- most common malignant liver tumor in yound children
Intrahepatic Cholangiocarcinoma (to liver cancer)
- cholangiocarcinoma (bile duct cancer) makes up a small fraction of primary liver cancers
- unlike hepatocellular carcinoma, intrahepatic cholangiocarcinoma is less frequently associated
with cirrhosis
- primary sclerosing cholangitis is a predisposing condition in a small minority of patients
- widespread infection with liver flukes (Clonorchis sinensis) is at least partly responsible for the
higher incidence of these tumors in some parts of Asia
- emerging evidence has implicated chronic hepatitis C infection, obesity, diabetes mellitus,
chronic liver disease, and cigarette smoking as risk factors for intrahepatic cholangiocarcinoma
- it generally presents as a large mass within the liver and is therefore clinically distinct from
cholangiocarcinoma arising from the extrahepatic biliary tree
- Histologically, these tumors are most often invasive adenocarcinomas (a cancer that forms
glands or secretes significant amounts of mucin)
- Intrahepatic or extrahepatic spread of disease is not uncommon by the time the tumor is
detected —> These tumors infrequently cause symptoms at early stages and therefore often
grow to a large size before they become apparent, frequently because of pain
- Infrequently, these tumors may contain cells of both cholangiocellular and hepatocellular origin
Page 188 of 269
83. Cirrhosis of the liver: definition, stages, causes, symptoms, diagnosis, and treatment.
Definition
- Cirrhosis is a „diffuse process characterized by fibrosis and conversion of normal liver
architecture into structurally abnormal regenerative nodules“
- it represents the end-stage of chronic liver damage resulting from several different causes and
leading to altered hepatic function and portal hypertension
Essential facts about pathogenesis
- most common cause is hepatitis C virus infection, followed by alcohol abuse
- other factors: hepatitis B virus infection, non-alcoholic steatohepatitis, autoimmune, metabolic,
biliary and genetic disorders
- key pathogenic processes: hepatocyte damage and death; ECM deposition due to proliferation
and activation of hepatic stellate cells; ductular proliferation and vascular reorganization
Causes
- Hepatitis C virus
- Alcohol
- Hepatitis B or B/D virus
- Autoimmune hepatitis
- Metabolic disorders: hemochromatosis, Wilson disease, α1-Antitrypsin deficiency, non-alcoholic
steatohepatitis, diabetes, glygogen storage diseases, porphyria
- Biliary diseases: primary biliary cirrhosis, primary sclerosing cholangitis
- Venous outflow obstruction: veno-occlusive disease, cardiac failure
Staging of cirrhosis
1) Inflammation
2) Fibrosis
3) Cirrhosis
4) Failure
Pathogenesis
- characterized by progressive accumulation of collagen types I and III in the liver parenchyma
- results in alteration of both the exchange between hepatocytes and plasma, and the regulation
of intrahepatic resistance to blood flow
- active fibrogenesis has been related to the increased expression of transforming growth factor-ß
(TGF-ß) and platelet-derived growth factor (PDGF), which stimulate the activation and
proliferation of hepatic stellate cells, the main source of extracellular matrix in fibrotic liver
- another important event in development of cirrhosis is the disruption of vascular architecture,
with obstruction of veins and/or sinusoids leading to hypoxia and ischemic changes
characterized by parenchymal extinction
- hypoxia-inducible transcription factors in turn stimulate the secretion of vascular endothelial
growth factor (VERGF) that induces angiogenesis and increases the permeability and promotes
the development of portal hypertension
Pathology
- histologically, cirrhosis is characterized by nodular regeneration, scarring with formation of
diffuse fibrous septa, and a variable degree of parenchymal necrosis
- morphologic classification is based on the size of nodules, identifies three types of cirrhosis:
• Micronodular — characterized by nodules mostly <3mm, surrounded by fibrous tissue and
generally lacking terminal veins and portal tracts; found mostly in alcoholic cirrhosis,
hemochromatosis and bile duct obstruction
• Macronodular — characterized by nodules of variable size, from >3mm to a few centimeters;
nodules contain both portal tracts and terminal veins; common in chronic viral hepatitis and
autoimmune hepatitis
• Mixed
Page 189 of 269
Clinical presentation / Symptoms
- clinically cirrhosis can be divided into compensated and decompensated stages
- compensated cirrhosis may be totally asymptomatic, diagnosed on routine biochemical testing
or ultrasonography
- non-specific asthenia, malaise, right upper quadrant abdominal discomfort or sleep disturbances
may be the only complaints
- on physical examination, spider angiomas may be found, mostly on the trunk, face and upper
limbs — their number and size correlate with disease severity
- palmar erythema, white nails (leukonychia), common in male patients is hair loss on the chest
and abdomen; also gynecomastia and loss of libido may occur
- petechiae and ecchymoses may be present as a result of thrombocytopenia and/or prolonged
prothrombin time
- Dupuytren’s contracture, involving the palmar fascia, particularly common in alcoholic patients
- hepatomegaly is very common
- signs of decompensation — ascites, variceal hemorrhage, jaundice and/or portosystemic
encephalopathy
- on physical examination patients with advanced cirrhosis often present with malnutrition and
muscle wasting, particularly in alcoholic cirrhosis
- also flapping tremor, mental state alterations (coma), GI hemorrhage (hematemesis, melena)
Diagnostic methods
- liver biopsy is the gold standard
- detection of signs of decompensation, such as ascites, variceal bleeidng and encephalopathy, in
patients with virological, serological, and biochemical markers of liver disease rules in the
diagnosis of cirrhosis
- Laboratory findings:
• AST:ALT ratio >1
• Low platelet count (< 140 × 109/L)
• Hypoalbuminemia
• Hypergammaglobulinemia
• Prolonged prothrombin time
• Hyperbilirubinemia
- Ultrasonographic findings:
• liver nodular surface
• reduced portal flow velocity
• portal vein diameter > 13mm
- Endoscopic findings:
• esophageal varices
• gastric varices
• congestive gastropathy
Treatment and prevention
- no specific antifibrotic therapy accepted
- treatment of underlying liver diease is the most effective way to reduce or eliminate hepatic
fibrosis
- no treatment effective in pereventing development of esophageal varices or ascites
- treatment mainly aimed at reversing disease complications (ascites, GI bleeding and
encephalopathy)
- liver transplantation in advanced disease
Page 190 of 269
Child-Pugh class — Stages
Parameter
A
B
C
Serum bilirubin in mmol/l
< 35
35-50
> 50
Serum albumin (g/L)
> 35
28-35
< 28
Prothrombin time (sec)
<4
4-6
>6
Ascites
none
controlled, not tense
tense, refractory
Encephalopathy
none
1-2
3-4
MELD score
MELD = 3.78×ln[serum bilirubin (mg/dL)] + 11.2×ln[INR] + 9.57×ln[serum creatinine (mg/dL)] +
6.43
- with a score of more than 40, there is a 71,3% 3 month mortality rate
- best outcomes with score less than
84.) Liver transplantation
General
-
Dr Thomas Starzl performed the first successful human liver transplantation in 1967
Today, more than 5000 liver transplants are performed annually in the United States, and 1-year
patient survival rates are more than 85%
The most common indication for liver transplantation is currently cirrhosis due to chronic
hepatitis C infection
Other diseases for which liver transplant is indicated include cirrhosis due to hepatitis B,
alcoholic cirrhosis, primary biliary cirrhosis, sclerosing cholangitis, autoimmune hepatitis, and
cirrhosis secondary to nonalcoholic fatty liver disease
In children, the most common indication is biliary atresia
o Other common diagnoses include α1-antitrypsin deficiency, tyrosinemia, and other
inborn errors of metabolism
Alcoholic cirrhosis
- was once a subject of considerable controversy because of the self-induced nature of the disease
- The world community rejected the notion that lifesaving therapy should be withheld from
patients who could benefit from it merely because their disease is self-induced
- It is now recognized that alcoholic cirrhosis is an accepted indication for liver transplant if the
patient has demonstrated the ability to abstain from alcohol and is clearly committed to
continued abstinence
Chronic active hepatitis B
- was formerly considered to be a controversial indication for liver transplantation because
recurrence was quite frequent and tended to result in rapid graft failure
- This changed when effective strategies to prevent recurrence of hepatitis B using high-dose
hepatitis B hyperimmune globulin infusions posttransplant were reported
- Now hepatitis B is considered to be a standard indication, and results are equal to those obtained
for other diagnoses
- In contrast, the outcome for patients transplanted for hepatitis C was once considered to be equal
to that of other diagnoses
- Recent data, however, suggest that recurrence of hepatitis C in the new liver graft is virtually
universal following transplantation, and 25% of patients will have developed cirrhosis in the
graft within 5 years
- It is not surprising that longer-term data are now appearing showing that the 10-year survival for
patients transplanted for hepatitis C is significantly worse than for other diagnoses
Hepatocellular carcinoma
- Patients with cirrhosis are at risk for development of primary hepatocellular cancer
Page 191 of 269
-
Since these patients usually die of liver failure, it was reasoned that transplantation would be a
curative therapy
Unfortunately, the initial results with transplantation for hepatoma were disappointing due to a
high rate of tumor recurrence
These poor results prompted many programs to stop doing transplants for hepatoma
The group from Barcelona, Spain, then reported that survival rates are good if the tumor is small
(<5 cm in diameter) but poor if the tumor is large or shows evidence of large vessel invasion
Liver transplantation is considered to be a standard treatment for patients with small hepatomas
Results for liver transplantation for other malignancies remain poor, with the exception of
several encouraging reports of reasonable survival rates for highly selected patients with
cholangiocarcinoma who receive adjuvant radiation and chemotherapy
Contraindications
- are few and are primarily related to evidence of cardiopulmonary disease that prohibits safe liver
transplantation
- Examples are, uncorrected coronary artery disease; pulmonary hypertension with pulmonary
artery systolic pressures greater than 70 mm Hg; and FEV1 of less than 1 L on pulmonary
function testing
- Active substance abuse is also an absolute contraindication to transplantation
- Diabetes increases the risks associated with transplantation and the incidence of posttransplant
complications, but it is not an absolute contraindication to liver transplantation
- Even infection with HIV, long considered a contraindication to transplantation, is no longer an
absolute contraindication at some centers that are reporting good results in small numbers of
carefully selected HIV-positive patients
- Portal vein thrombosis, which at one time was a contraindication to transplant, is now managed
by performing thrombectomy on the portal vein, by using vein grafts to bypass thrombosed
vessels, or by using the intrahepatic cava for portal inflow
Donor Selection
-
The ideal liver donor (young and otherwise completely healthy) is increasingly rare, because the
cause of death for most donors has shifted from trauma to cerebrovascular accidents
Most transplant centers want you to be between 18 and 60 years old, although the exact age range
varies. The reason is that older donors tend to have more complications than younger ones
It is important that the liver is a rough size match for the donor
Blood-type compatibility is preferred but not an absolute requirement
Matching of tissue antigens does not appear to be relevant for liver transplantation
The technique of preserving the liver grafts after removal from the donor is based on decreasing
metabolic requirements by keeping the graft cold
Blood is flushed from the organ to prevent vascular occlusion; preservation solution is infused;
and the organ is kept on ice at 4°C
Multiple preservative solutions are in common use worldwide. Most contain inert highmolecular-weight molecules that do not diffuse into the cell to prevent cellular swelling
Also, free oxygen radical scavengers, which are thought to prevent injury upon reperfusion of
the graft, are frequently included
The introduction of Viaspan solution in the late 1980s revolutionized liver transplantation by
extending the period of safe in vitro liver preservation from 10 hours to more than 24 hours
Despite this advance, it is clear that prolonged cold ischemia is bad for the liver graft,
particularly if the graft contains a large amount of intracellular fat or is from an older donor
Transplant programs therefore continue to try to minimize the cold ischemic time to whatever
degree is feasible
Operative technique
-
Liver transplantation is an orthotopic procedure
The host liver is removed, and the donor organ placed in an orthotopic position
The liver has several key connections that must be re-established for the new organ to receive
blood flow and to drain bile from the liver
The structures that must be reconnected are the inferior vena cava, the portal vein, the hepatic
artery, and the bile duct
The operation is performed in three phases:
Page 192 of 269
-
-
Dissection phase: during which the attachments of the diseased liver are dissected and the
vascular structures are prepared for resection
Anhepatic phase: which extends from the time the host liver is removed until the time the donor
liver is revascularized
Reperfusion phase: during which blood is circulating through the new organ and the biliary tree
is reconstructed
The sequence of events in the operating room is as follows:
o Incision
o Evaluation of the abdomen for abnormalities that would preclude liver transplantation
(for example: undiagnosed infection or malignancy)
o Mobilization of the native liver (dissection of the liver attachments to the abdominal
cavity)
o Isolation of important structures (the inferior vena cava above, behind, and below the
liver; the portal vein; the common bile duct; the hepatic artery)
o Transection of the above mentioned structures and removal of the native, diseased liver
o Sewing in the new liver: First, venous blood flow is re-established by connecting the
donor's and the recipient's inferior vena cava and portal veins. Next, arterial flow is reestablished by sewing the donor's and recipient's hepatic arteries. Finally, biliary
drainage is achieved by sewing the donor's and recipient's common bile ducts.
o Ensuring adequate control of bleeding
o Closure of the incision
Although the liver can function normally with only portal venous flow, the bile duct is dependent
on hepatic arterial flow
For this reason, the hepatic arterial anastomosis is crucial to postoperative graft survival
The arterial supply of the liver is quite variable, with nearly half of the patients having some
form of aberrant circulation
The most common aberrancies are replacement of the right hepatic artery to the superior
mesenteric artery and the presence of an accessory left hepatic artery that derives from the left
gastric artery
When aberrant arterial vessels are identified on a deceased donor, it is important that they are
carefully preserved so that reconstruction can occur when the liver has been perfused and cooled
and is sitting in sterile ice slush
Multiple methods of reconstruction of aberrant vessels are available and, if necessary, a conduit
of donor iliac artery may be used in the reconstruction
Immunosuppressive Therapy
-
-
The mainstay of immunosuppression for liver transplant recipients is a calcineurin inhibitor
(cyclosporine, tacrolimus)
o This class of drugs blocks the function of calcineurin, a molecule critical to a very
important lymphocyte signaling pathway that triggers the production of multiple
cytokines
An antimetabolite or corticosteroids, or both, may also be included but are not absolutely
necessary
Induction therapy with antilymphocyte preparations was once considered standard but has now
been abandoned by many liver transplant programs because it appears unnecessary
Despite being one of the largest organs transplanted in terms of mass, the liver seems to require
less immunosuppression for maintenance therapy compared to other organs
Corticosteroids can frequently be safely discontinued
Typically, monotherapy with a low dose of a calcineurin inhibitor is all that is required to
suppress rejection long term
Spontaneous tolerance with normal graft function despite complete discontinuation of all
immunosuppressants occurs in approximately 10%-20% of liver transplant recipients
The liver is unique in this regard, since rejection is almost universal if immunosuppression is
discontinued in recipients of renal, cardiac, pulmonary, and pancreatic grafts
Complications
-
Complications following liver transplantation are common, but most can be treated effectively
Coagulopathy is routinely present during liver transplant procedures, particularly during the
anhepatic phase
For this reason, bleeding is common following the procedure, and 5%-10% of liver transplant
recipients will require reoperation because of continued bleeding following the procedure
Page 193 of 269
Primary nonfunction of the liver
- is a condition in which the new liver does not function and death results unless a second
transplant is performed
- Patients with primary nonfunction typically have profoundly elevated serum transaminases
together with severe coagulopathy and acidosis
- Incidence is between 5%-10%
- The cause of primary nonfunction is poorly understood, but multiple donor factors are known to
be associated
- Risk factors: Long cold ischemic times, poor perfusion of the graft with preservative solution,
severe hepatic steatosis, and elevation of the donor serum sodium level above 165 mEq/L
Vascular complications
- Occur in 5%-10% of transplant recipients
- The hepatic artery is particularly prone to thrombosis, especially in children
- If this is detected early, it is frequently possible to perform thrombectomy and restore hepatic
arterial flow
- If flow cannot be reestablished, necrosis of the intrahepatic and extrahepatic biliary tree usually
occurs, resulting in death from sepsis if retransplantation is not performed
Bile duct
Rejection
Infections
-
It has been called the Achilles heel of the liver transplant because it is so prone to anastomotic
leakage or stricture
As many as 20% of liver transplant recipients will experience a bile duct complication
Uncommon to be lethal
Leaks tend to occur early and can often be managed by placing a biliary stent using ERCP
If a large collection of bile develops because of a bile leak, it is usually necessary to drain the
area either operatively or by placing a percutaneous suction drain
Biliary stenosis can occur early or late
The transplanted liver will not always develop intrahepatic biliary dilatation when the bile duct
is obstructed (necessary to have high index of suspicion)
Patients with elevated bilirubin or elevated serum alkaline phosphatase levels (or both) should be
evaluated with either ERCP or magnetic resonance cholangiography
Strictures can often be managed noninvasively with biliary stents and balloon cholangioplasty,
but in some cases, operative correction is required
Patients who develop multiple intrahepatic strictures usually require retransplantation
Frequent complication, it occurs in 20%-50%
It should be suspected whenever serum transaminases or bilirubin levels, or both, worsen or fail
to gradually normalize following a liver transplant
The diagnosis of rejection is made histologically by the finding of a mixed portal cellular
infiltrate together with injury to bile duct epithelium and inflammation of the central vein
endothelium (endotheliitis)
The treatment for rejection depends on its severity
Mild rejection is treated either with corticosteroid pulse therapy or by increasing the dosage of
maintenance immunosuppressive therapy
Rejection that does not respond to these measures may require treatment with an antilymphocyte
preparation
Prior to the availability of prophylaxis against this virus, as many as half of liver transplant
recipients developed clinical CMV infection
Symptoms typically include fever, leukopenia, and malaise, but a more serious clinical syndrome
with pneumonitis or hepatitis is possible
Patients at greatest risk for severe CMV disease are those without previous CMV exposure who
receive a liver from a CMV-positive donor, but reactivation of CMV infection is possible in any
patient with prior exposure to the virus
Page 194 of 269
-
In order to prevent CMV infection, most liver transplant programs prescribe either ganciclovir or
valganciclovir for a period of months following liver transplantation to all patients at risk for
CMV infection
EBV is another common viral pathogen in these patients
EBV infection is usually mild, it may be associated with development of a lymphoproliferative
disorder known as posttransplant lymphoma
This disorder can progress to frank malignancy, and the mortality rate is high
If the lymphoproliferative tissue expresses CD20, treatment with the monoclonal antibody
rituximab may be helpful
Immunosuppression
- predisposes to fungal infections, especially esophageal Candida albicans (“thrush”)
- The incidence of this infection is reduced by the use of prophylactic nystatin to decrease
gastrointestinal fungal colonization
Living Donor Liver Transplantation and Split Liver Transplantation
-
The shortage of organs for small children in the late 1980s prompted the development of
techniques to reduce the size of an adult liver graft by performing an anatomic resection of one
or more lobes and transplanting the reduced graft
Standard method of obtaining grafts for small children (but also for adults)
The major advantage of living donor liver transplantation appears to be the ability to allow
transplant to occur prior to the deterioration of the recipient’s condition into a poor state of
health
Living donor liver transplants have become a standard option when timely deceased donor liver
transplantation is not possible
By applying the living donor technique to deceased donors, two transplants can be obtained from
a single adult liver from a deceased donor (split liver transplant)
Typically, the lateral segment of the left lobe is used for a child or very small adult, while the
remainder of the liver consisting of the right lobe plus the medial segment of the left lobe is used
for an adult
Less commonly, the liver from an adult deceased donor can also be split into a right lobe graft
and a left lobe graft and used for two adults
85. Portal hypertension.
= the elevation of hepatic venous pressure gradient to >5mmHg
- portal hypertension is caused by two simultaneously occurring hemodynamic processes:
• increased intrahepatic resistance to the passage of blood flow through the liver due to
cirrhosis and regenerative nodules
• Increased splanchnic blood flow secondary to vasodilation within the splanchnic vascular bed
- Portal hypertension is directly responsible for the three major complications of cirrhosis: varices
within esophagus, stomach, rectum or umbilical area; variceal hemorrhage and ascites
- Variceal hemorrhage is an immediate life-threatening problem with 20-30% mortality rate
associated with each episode of bleeding (marked by black, tarry stools or blood in the stools;
hematemesis)
- the portal venous system normally drains blood from the stomach, intestines, spleen, pancreas,
and gallbladder, and the portal vein is formed by the confluence of the superior mesenteric and
splenic veins
- the cause of portal hypertension are usually subcategorized as prehepatic, intrahepatic, and
posthepatic
• Prehepatic causes include portal vein thrombosis and splenic vein thrombosis
• Posthepatic causes encompass those affecting the hepatic veins and venous drainage to the
heart; they include BCS, venoocclusive disease, and chronic right-sided cardiac congestion
• Intrahepatic causes account for 95% of cases and are represented by the major forms of
cirrhosis
Page 195 of 269
-
• Intrahepatic causes can be further subdivided into presinusoidal (congenital hepatic fibrosis
and schistosomiasis), sinusoidal (related to cirrhosis from various causes) and postsinusoidal
(venoocclusive disease)
Cirrhosis is the most common cause of portal hypertension; present in >60% of patients with
cirrhosis
portal vein obstruction may be idiopathic or can occur in association with cirrhosis or with
infection, pancreatitis or abdominal trauma
Diagnosis usually based on the presence of ascites or of dilated veins or varices as seen during
physical exam of the abdomen or the anus; various lab tests; x-ray tests, and endoscopic exams
most cases of portal hyypertension cannot be treatet
Treatment includes:
• Endoscopic therapy: usually first line treatment for variceal bleeding and consits of either
banding (rubber bands to block off the blood vessel) or sclerotherapy (blood-clotting solution
injected into bleeding varices)
• Medications: nonselective beta-blockers (nadolol or propanolol)
86. Acute pancreatitis.
Acute pancreatitis
- inflammation of the pancreas with dysfunctional exocrine and possibly endocrine function
- frequent causes:
• mostly acute biliary pancreatitis (45%)
• alcoholic pancreatitis (35%)
• idiopathic pancreatitis (15%)
- risk increased in alcoholics, the obese and patients with gallstones
- rare causes:
• drug-induced toxic pancreatitis (e.g. due to glucocorticoids, thiazide, tetracyclines,
carbamazepin, ciclosporin A, azathioprin)
• viral pancreatitis
• due to juxtacapillary duodenaldiverticle
• due to massive hypertriglycerinemia
• primary hyperparathyreoidism
• after pancreatic transplantation (postischemic, due to rejection or CMV infection)
• hereditary pancreatitis (Genetic predisposition: mutations in cationic trypsinogen (PRSS1),
cystic brosis transmembrane conductance regulator (CFTR), and serine protease inhibitor
Kazal type 1 (SPINK1) for recurrent acute pancreatitis are most common genetic factors)
- the magnitude of the acute in ammatory response determines the severity of the disease and
related complications —> there is a light pancreatitis (edematous) or the necrotizing pancreatitis
with high martality rate (ca. 20%)
- pathogenesis: any injury that leads to trypsinogen activation or the activation of the immune
system
Symptoms
- strong epigastric pain (sudden, epigastric, knife-like) radiating to the back (often belt-like), often
8-12 hours after alimentary or alcohol excess
- nausea, vomiting, meteorismus
- fever
- icterus
- periumbilical bluish spots (Cullen-sign) or in the flank area (Grey-Turner-sign) when severe
pancreatitis with necrosis
- complications: intestinal paresis (paralytic ileus), bacterial superinfection of the necrosis,
formation of abscesses, pseudocysts, splenic vein thrombosis, sepsis, shock, acute kidney
failure,…
Page 196 of 269
Diagnosis
- acute pancreatitis requires 2 of 3 diagnostic signs:
• amylase or lipase 3x upper limit of normal values
• characteristic sudden onset abdominal pain
• characteristic changes on abdominal images
- palpable elastic abdominal wall tension
- auscultatory and percussive pleural effusion
- in the laboratory: signs of inflammation (increased CRP, leukocytosis), lipase, sometimes also
elastase 1 and amylase in the serum increased, increased conjugated bilirubin,…
- sonography: hypodense organ structure, evidence of abscesses, pseudocysts, possibly
evidence of a gallstone and an extrahepatic cholestasis
- imaging: CT with or without contrast, MRI with or without contrast, transcutaneous ultrasound
- ERCP (endoscopic retrograde cholangiopankreaticography) with papillotomy if acute biliary
pancreatitis
Differential diagnosis
- sudden onset of abdominal pain similar to AP include myocardial infarction, dissecting aortic
aneurism, mesenteric thrombosis, ischemia or infarction, vovlulus, intussusception, penetrating
gastric or duodenal ulcers, biliary colic, and acute cholecystitis
Treatment
- aggressive fluid resuscitation (to prevent systemic inflammation, vascular leak syndrome, or
multiple organ failure due to hypovolemia) should be initiated upon the diagnosis of acute
pancreatitis and continued until signs of resuscitation are met, whether or not the clinical course
is predicted to be severe
- pain control: parenteral narcotics, such as meperidine, morphine, fentanyl, and hydromorphone,
are usually administered to relieve the pain
- early ERCP with biliary sphincterotomy should be considered in selected patients to prevent
bacterial cholangitis
- enteral nutrition is the preferred route of nutrition in severe acute pancreatitis and should be
started within 48 hours of admission
- prophylactic antibiotics (ciprofloxacin, metronidazol, imipenem) are not recommended, but may
be present considred in the presence of > 30% pancreatic necrosis
- electrolyte substitution
- prevent stress ulcers by PPI
- the etiology of an episode of acute pancreatitis should be systematically investigated, and the
source of pancreatic injury treated before discharge, if possible
87. Chronic pancreatitis. Pseudocysts of the pancreas. Pancreatic fistulas
- chronic, mostly progressive changes of the pancreas parenchyma (focal necrosis, segmental or
diffuse fibrosis, calcification)
- alcohol is the main cause in the western world (70%) — the association between alcohol and
pancreatitis complex is only partly dose dependent
- other risk factors are genetic predisposition, smoking and nutrition
- rarely it is hereditary, drug induced toxic, due hyperparathyreoidism, hyperlipoproteinemia, cystic
fibrosis
- special form: obstructive chronic pancreatitis (obstruction of the ducts (Gangsysteme)with
atrophy)
- mean age of onset is 40-60 years
Pathogenesis
- remains controversial
- alcohol and other insults trigger multifactorial cascades in the pancreas, which lead to chronic
inflammation, progressive fibrosis, pain, and loss of exocrine and endocrine function
- three main concepts:
Page 197 of 269
• Increased viscosity of pancreatic juice and formation of protein plugs, subsequently
obstructing pancreatic ducts
• Direct toxic effect of alcohol and its metabolites on pancreatic acinar and ductal cells
• Free radical injury of the pancreatic parenchyma as a result of reduced hepatic detoxification
- new distinct mechanisms that might explain the morphological, functional and clinical picture of
chronic pancreatitis:
• Growth factors — many growth factors are overexpressed in chronic pancreatitis; e.g. TGF-ß
or TGF-a, that develop severe pancreatic fibrosis
• Stellate cells — evidence suggests that pancreatic fibrosis requires the differentiation and
stimulation of specific cells called pancreatic stellate cells. It is thought that recurrent acinar
cell injury, caused by oxidative stress (e.g., alcohol, ischemia), and other factors result in
cytokine and chemokine release from acinar cells and the activation of resident macrophages.
These macrophages, in turn, sup press acute inflammation by releasing TGF-β and other
cytokines, which stimulate stellate cells to produce collagen, and thereby promote fibrosis
• Immune functions - data suggests that decreased regulatory CD4 T cells and uncontrolled
activation of CD8 T lymphocytes result in T-cell-mediated cytotoxicity
- Malabsorption is due to deficiency of pancreatic enzymes
- in chronic pancreatitis the pancreas usually has firm appearance with signs of calcification; duct
obstruction by protein plugs or small calculi are occasionally seen
Symptoms
- recurring episodic or continuous pain in the upper abdomen, which may radiate to the back
- nausea, vomiting
- ggf. recurring icterus
- evtl. thrombophlebitis
- evtl. latent diabetes mellitus as a sign of endocrine pancreas insufficiency
- maldigestion and impaired absorption of food (especially of fats) due to exocrine insufficiency
• weight loss
• diarrhea, steatorrhea (bulky, smelly stools due to too much fat), meteorism
• rarely night blindness, coagulation disorder, osteomalacia
- complications: pseudocysts, abscesses, splenic or pylethrombosis (of the portal vein), stenosis
of the pancreatic ducts and the ductus choledochus, pancreatic carcinoma
Diagnosis
- endosonography detects earliest parenchymal changes (like caclification or pseudocysts)
- ductal changes can be detected eary through endoscopic retrograde cholangiopancreatography
(ERCP)
- CT scanning is widely available and shows complications
- Magnetic resonance cholangiopancreatography (MRCP) has the potential to be the „all-in-one“
diagnostic investigation (including standard scan, MRCP, angiography)
- the pancreatic enzymes can be increased
- in the secretin-pancreozymin-test there is direct evidence of exocrine insufficiency (rarely
indicated because expensive)
- decreased chymotrypsin- and elastase-1 concentration in stool
Treatment
Conservative treatment
- pain control (NSAIDs, opiods for severe pain)
- avoidance of exacerbating factors (abstinence from alcohol and nicotine consumption and
avoidance of fatty foods)
- pancreatic enzymes to treat maldigestion, management of diabetes mellitus
- stenting of the bile and pancreatic duct once only — then consider surgery
Page 198 of 269
Surgical treatment
- indication should be considered when complications occur or conservative treatment fails
- operations are:
• longitudinal pancreaticojejunostomy (Pusteow and Partington–Rochelle procedures);
• pancreaticoduodenectomy (Whipple operation, classic and pylorus preserving);
• duodenum- preserving pancreatic head resection (Beger operation);
• longitudinal pancreaticojejunostomy and local pancreatic head excision (Frey operation);
• central pancreatic head resection (Büchler– Farkas operation)
Pancreatic fistula
- = an abnormal communication between the pancreas and other organs due to leakage of
pancreatic secretions from damaged pancreatic ducts
- an external pancreatic fistula is one that communicates with the skin, and is also known as a
pancreaticocutaneous fistula
- an internal pancreatic fistula communicates with other internal organs and or soaces
- causes include pancreatic disease, trauma or surgery
- signs and symptoms: marked recent weight loss is a major manifestation; unresponsiveness of
the ascites to diuretics is an additional diagnostic clue
Pathogenesis
- internal pancreatic fistuals are most commonly caused by disruption of the pancreatuc duct
due to chronic pancreatitis
- the hronic pancreatitis is usually alcoholic in origin in adults, and traumatic in origin in children
- may also be caused by leakage from a pancreatic pseudocyst
- anterior disruption of a pseudocyst or a pancreatic duct leads to leakage of pancreatic
secretions into the free peritoneal cavity, leading to pancreatic ascites
- if the duct is disrupted posteriorly, the secretions leak through the retroperitoneum into the
mediastinum via the aortic or esophageal hiatus
- once in the mediastinum, the secretions can either be contained in a mediastinal pseudocyst,
lead to enzymatic mediastinitis, or, more commonly, leak through the pleura to enter the chest
and form a chronic pancreatic pleural effusion
Diagnosis
- pleural or ascitic fluid should be sent for analysis
- an elevated amylase level, usually > 1,000 IU/L, with protein levels over 3.0 g/dL is diagnostic
- Serum amylase is often elevated as well, due to enzyme diffusion across the peritoneal or
pleural surface
- Contrast-enhanced computed tomography and endoscopic retrograde
cholangiopancreatography (ERCP) may also assist in diagnosis, with the latter an essential
component of treatment
Treatment
- the production of pancreatic enzymes is suppressed by restricting the patient's oral intake of
food patient in conjunction with the use of long-acting somatostatin analogues
- The patient's nutrition is maintained by total parenteral nutrition —> This treatment is continued
for 2–3 weeks, and the patient is observed for improvement
- If no improvement is seen, the patient may receive endoscopic or surgical treatment
- If surgical treatment is followed, an ERCP is needed to identify the site of the leak
- Fistulectomy is done in which the involved part of the pancreas is also removed
Page 199 of 269
88. Cancer of the pancreas.
-
highly malignant, mostly starting as a ductal adenocarcinoma
ductal carcinoma vs. acinar carcinoma 10:1
localization in 80% in the head of the pancreas
major risk factors: age, smoking, chronic pancreatitis, late-onset diabetes mellitus
inherited risk: hereditary pancreatitis, cancer family syndromes, familial pancreatic cancer
there is an activation of the K-ras oncogene and the inactivation of the tumor suppressor gene
p53, p16 and DPC4
- peak incidence between the age 60-80, majority of patients present with advanced disease
(85%)
- 5-year survival rate in total <1%
- Sites of metastasis: liver, peritoneum, lung, adrenal, bone, rarely CNS
Symptoms
- no early symptoms
- unspecific epigastric pain
- nausea, vomiting, loss of appetite, abdominal bloating, weight loss
- back pain (occurs in 25% of patients and is associated with worse prognosis)
- thrombophlebitis migrans and thrombosis
- painless obstructive jaundice
- 75% of patients with carcinoma of the head of the pancreas present with weight loss, obstructive
jaundive and deep-seated abdominal pain
- metastastic subumbilical („Sister Mary Joseph node“) and peritoneal („Blumer’s shelf“) deposits
and left supraclavicular lymphadenopathy („Virchow’s node“)
- malignant ascites caused by peritoneal carcinomatosis may also be present
Histology
- ductal carcinoma 82% — long term survival rare
- anaplastic 5% — worse prognosis than ductal
- mucinous cystadenocarcinoma 3% and acinar cell 2% — variable
- adenosquamous 2% — poor prognosis
- small cell 1% — extremely poor prognosis
Histological grading of ductal adenocarcinoma
Grade 1 — well differentiated duct-like glands — mucin production is intensive
Grade 2 — moderately differentiated duct-like and tubular — mucin production is irregular
Grade 3 — poorly differentiated glands, mucoepidermoid and pleomorphic structures — abortive
mucin production
TNM classification
T1 - tumor limited to the pancreas, 2 cm or less in the greatest diameter
T2 - tumor limited to the pancreas, more than 2 cm in greatest diameter
T3 - tumor extends directly into any of the following duodenum, bile duct, peripancreatic tissues
T4 - tumor extends directly into any of the following stomach, spleen, colon, adjacent large vessels
N0 - no regional lymph node metastasis
N1 - regional lymph node metastasis (N1a - single, N1b - multiple)
M1 - distant metastasis
Page 200 of 269
Differential diagnosis
- depends on the clinical presentation of the patient:
- in presence of jaundice, intrahepatic causes, cholangiocarcinoma, and benign causes such as
gallstone disease or Mirizzi syndrome may be considered; Ultrasound scan and CT will
differentiate these causes
- epigastric pain will need to be differentiated from benign gastric disease such as peptic ulcer
disease, gastritis, or malignant gastric tumors; Endoscopic examination may be required
- back pain will need to be differentiated from musculoskeleta cause of back pain
- an abdominal mass in the epigastrium needs to be differentiated from a hepatic, gastric, colonic
or omental mass
- the main diagnostic differentation is between pancreatic cancer and chronic pancreatitis, both of
which may present with very similar symptoms and may coexist
Diagnosis
- initial investigation include blood tests for anemia, clotting profile, liver function test and serum
CA19-9 in jaundiced patients
- tumor markers CA19-9 and CA 50 are taken for further follow-up
- transabdominal ultrasound is usually the initial investigation because most patients will present
with jaundice; Tumors larger than 2 cm in size, dilatation of the biliary and main pancreatic
ducts, and possible extrapancreatic spread, notably liver metastases may be detected, but a
normal ultrasound scan does not rule out pancreatic cancer
- multidetector computed tomography (MDCT) — diagnostic rates of 97% for pancreatic cancer
- MRI is an alternative to MDCT and is useful for patients who cannot receive intravenous contrast
- Endoscopic cholangiopancreatography (ERCP) visualizes the biliary tree and pancreatic duct
and is used therapeutically to place stents in jaundice
- percutaneous biopsy only for patients not undergoing resection
Treatment
Unresectable
- endoscopic biliary stent
- endoscopic duodenal stent
- percutaneous biliary stent
- palliative bypass surgery
- pancreatic enzyme supplements
- analgesia
- celiac plexus block
- thoracoscopic splanchnicectomy
- pancreas enzyme supplements
- systemic chemotherapy: gemcitabine plus capectabine
Resectable
- Preoperative short covered metal stent preferred
- Kausch-Whipple pancreatoduodenectomy (KW-PPD) (standard for tumors of the head)
- Pylorus-preserving pancreatoduodenectomy (PP-PPD)
- Total pancreatectomy
- Left pancreatectomy
- Adjuvant chemotherapy — avoid chemoradiation
Factors contraindicating resection
- liver, peritoneal, or other metastasis
- uncertain wheter distant lymph node metastasis influence prognosis
- major venous encasement (>2cm in length, >50% circumference involvement)
- superior mesenteric, celiac, or hepatic artery encasement
- severe co-morbid illness
- cirrhosis with portal hypertension
Page 201 of 269
Factors that do not contraindicate resection
- continuous invasion of duodenum, stomach or colon
- lymph node metastasis within operative field
- venous impairment or minimal invasion of superior mesentric and hepatic portal vein
- gastroduodenal artery encasement
- age of patient
Pancreatic pseudocyst
= a circumscribed collection of fluid rich in pancreatic enzymes, blood and necrotic tissue (without
epithelial lining; the wall is vascular and fibrotic)
- typically located in the lesser sac of the abdomen
- usually complications of pancreatitis
- in children frequently occur following abdominal trauma
- account for 75% of all pancreatic masses
- signs and symptoms include abdominal discomfort and indigestion
- complications of pancreatic pseudocysts include infection, hemorrhage, obstruction and rupture
Diagnosis
- can be based on cyst fluid analysis:
• Carcinoembryonic antigen (CEA) and CEA-125 (low in pseudocysts and elevated in tumors)
• Fluid viscosity (low in pseudocysts and elevated in tumors)
• Amylase (usually high in pseudocysts and low in tumors)
- the most useful imaging tools:
• Ultrasonography
• CT
• MRCP (magnetic resonance cholangiopancreatography)
Treatment
- if no signs of infection are present, initial treatment can include conservative measures such as
bowel rest (NPO), parenteral nutrition (TPN), and observation
- if symptoms do not improve by 6 weeks, surgical intervention may be appropriate:
• Cystogastrostomy: In this surgical procedure a connection is created between the back wall
of the stomach and the cyst such that the cyst drains into the stomach
• Cystjejunostomy: a connection is created between the cyst and the small intestine so that the
cyst fluid directly into the small intestine
• Cystdudodenostomy: a connection is created between the duodenum (the first part of the
intestine) and the cyst to allow drainage of the cyst content into duodenum (when cyst in the
head of pancreas)
• => type of procedure depends on the location of cyst
89.) Endocrine tumors of the pancreas
Pancreatic Islet Cells Tumors
General
-
Islet cell tumors may be functioning (ie, hormone-producing) or nonfunctioning, malignant or
nonmalignant
More than half are functioning; less than half are malignant
Insulinoma, the most common functioning islet cell neoplasm, arises from beta cells and
produces insulin and symptoms of hypoglycemia
Tumors of the {d} or {a}1 cells produce gastrin and the Zollinger–Ellison syndrome
Alpha2 cell neoplasms may produce excess glucagon and hyperglycemia
Non-beta islet cell tumors may secrete serotonin, ACTH, MSH, and kinins (and evoke the
carcinoid syndrome)
Some produce pancreatic cholera, a severe diarrheal illness
Page 202 of 269
Nonfunctioning Islet Cell Tumors
-
Most of these lesions are malignant tumors of the head of the gland
Present with abdominal and back pain, weight loss, and, in many cases, a palpable abdominal
mass
Jaundice is encountered occasionally
CT scans reveal a pancreatic mass, and angiography typically shows it to be hypervascular
The histologic pattern on biopsy specimens is diagnostic of islet cell tumor, but whether or not
the lesion is malignant rests on evidence of invasiveness or metastases, not the appearance of the
cells
Immunohistochemical staining of the tissue is positive for chromogranin and neuron- specific
enolase (markers of APUD tumors)
Metastases are present at the time of diagnosis in 80% of patients
Resection of all gross tumor (eg, by a Whipple procedure), the preferred treatment, is possible in
less than half of patients because of local extension or distant metastases
A combination of streptozocin and doxorubicin is the most effective chemotherapeutic regimen
The 5-year disease-free survival rate is about 15%
Insulinoma
-
They have been reported in all age groups
About 75% are solitary and benign
About 10% are malignant, and metastases are usually evident at the time of diagnosis
The remaining 15% are manifestations of multifocal pancreatic disease—either adenomatosis,
nesidioblastosis, or islet cell hyperplasia
The symptoms (related to cerebral glucose deprivation) are bizarre behavior, memory lapse, or
unconsciousness
Patients may be mistakenly treated for psychiatric illness
There may be profuse sympathetic discharge, with palpitations, sweating, and tremulousness
Hypoglycemic episodes are usually precipitated by fasting and are relieved by food, so weight
gain is common
The classic diagnostic criteria (Whipple triad) are present in most cases:
o (1) hypoglycemic symptoms produced by fasting
o (2) blood glucose below 2.8 mmol/l during symptomatic episodes
o (3) relief of symptoms by intravenous administration of glucose
The most useful diagnostic test and the only one indicated in all but a few patients is
demonstration of fasting hypoglycemia in the presence of inappropriately high levels of insulin
The patient is fasted, and blood samples are obtained every 6 hours for glucose and insulin
measurements
The fast is continued until hypoglycemia or symptoms appear or for a maximum of 72 hours
(some investigators truncate the test at 48 hours)
Although insulin levels are not always elevated in patients with insulinoma, they will be high
relative to the blood glucose concentration
A ratio of plasma insulin to serum glucose greater than 0.3 is diagnostic. Ratios should be
calculated before and during the fast
Proinsulin, which constitutes more than 25% of total insulin (the upper limit of normal) in about
85% of patients with insulinomas, should also be measured
Proinsulin levels greater than 40% suggest a malignant islet cell tumor
Localization of the tumor is important but may be difficult
In about 10% of cases, the tumor is so small or located so deeply that it is difficult or impossible
to find at laparotomy
High-resolution CT and MR scans are successful in demonstrating about 40% of tumors
Endoscopic ultrasound of the pancreas may be helpful
The most important examination is intraoperative ultrasound, which can identify a pancreatic
tumor in nearly all cases
Transhepatic portal venous sampling has proved an accurate preoperative localizing method,
demonstrating the position in the pancreas in about 95% of lesions
Entering the portal vein with a catheter passed percutaneously through the liver and testing blood
at various sites within the portal, superior mesenteric, and splenic veins for insulin levels
The point where insulin concentrations rise sharply indicates the site of the tumor
Page 203 of 269
Treatment- Insulinoma
Medical Treatment
- Diazoxide is administered to suppress insulin release
- For incurable islet cell carcinomas, streptozocin is the best chemotherapeutic agent
Surgical Treatment
- Surgery should be done promptly, because with repeated hypoglycemic attacks, permanent
cerebral damage occurs and the patient becomes progressively more obese
- Moreover, the tumor may be malignant
- At operation, the entire pancreas must be palpated carefully because the tumors are usually small
and difficult to find
- The gland should also be examined intraoperatively with ultrasound, which may be able to
locate a tumor that cannot be felt, or to demonstrate signs of invasion (ie, irregular borders) that
indicate malignancy
- When the tumor is found, it may be enucleated if it is superficial or resected as part of a partial
pancreatectomy if it is deep-seated or invasive
- Insulinomas in the head of the gland can nearly always be enucleated
Pancreatic Cholera (WDHA Syndrome: Watery Diarrhea, Hypokalemia, Achlorhydria)
-
Most cases of pancreatic cholera are caused by a non-beta islet cell tumor of the pancreas that
secretes VIP and peptide histidine isoleucine
The syndrome is characterized by profuse watery diarrhea, massive fecal loss of potassium, low
serum potassium, and extreme weakness
Severe metabolic acidosis frequently results from loss of bicarbonate in the stool
Many patients are hypercalcemic, possibly from secretion by the tumor of a parathyroid
hormone-like substance
Abnormal glucose tolerance may result from hypokalemia and altered sensitivity to insulin
Patients who complain of severe diarrhea must be studied carefully for other causes before the
diagnosis of WDHA syndrome is entertained seriously
CT scan is the best initial imaging test; somatostatin receptor scintigraphy is also very useful for
localization
Approximately 80% of the tumors are solitary, located in the body or tail, and can be removed
easily
About half of the lesions are malignant, and three-fourths of those have metastasized by the time
of exploration
Even if all of the tumor cannot be removed, resection of most of it alleviates symptoms in about
40% of patients even though the average survival is only 1 year
Treatment with long-acting somatostatin analogues decreases VIP levels, controls diarrhea, and
may even reduce tumor size
Glucagonoma
-
Glucagonoma syndrome is characterized by migratory necrolytic dermatitis (usually involving
the legs and perineum), weight loss, stomatitis, hypoaminoacidemia, anemia, and mild to
moderate diabetes mellitus
Scotomas and changes in visual acuity have been reported in some cases
The age range is 20-70 years, and the condition is more common in women
The diagnosis may be suspected from the distinctive skin lesion; in fact, the presence of a
prominent rash in a patient with diabetes mellitus should be enough to raise suspicions
It should also be suspected in any patient with new onset of diabetes after the age of 60
Confirmation of the diagnosis depends on measuring elevated serum glucagon levels
CT scans demonstrate the tumor and sites of spread
Glucagonomas arise from {a}2 cells in the pancreatic islets
Most are large at the time of diagnosis
About 25% are benign and confined to the pancreas
The remainder has metastasized by the time of diagnosis, most often to the liver, lymph nodes,
adrenal gland, or vertebrae
Severe malnutrition should be corrected preoperatively with a period of total parenteral nutrition
and treatment with somatostatin analogues
Page 204 of 269
-
Surgical removal of the primary lesion and resectable secondaries is indicated if technically
feasible
If the tumor is confined to the pancreas, cure is possible
Low-dose heparin therapy should be administered pre- and postoperatively because of a high
risk of deep venous thrombosis and pulmonary embolism
Streptozocin and dacarbazine are the most effective chemotherapeutic agents for unresectable
lesions
Somatostatin therapy normalizes serum glucagon and amino acid levels, clears the rash, and
promotes weight gain
Somatostatinoma
-
Somatostatinomas are characterized by diabetes mellitus (usually mild), diarrhea and
malabsorption, and dilation of the gallbladder (usually with cholelithiasis)
Serum calcitonin and IgM concentrations may be elevated
The syndrome results from secretion of somatostatin by an islet cell tumor of the pancreas
Half of the cases are malignant and accompanied by hepatic metastases
The lesion is usually large and readily demonstrated by CT scan
The diagnosis may be made by recognizing the clinical syndrome and measuring increased
concentrations of somatostatin in the serum
When the disease is localized, resection is able to cure about 50% of cases
Enucleation is inappropriate for these tumors
Chemotherapy with streptozocin, dacarbazine, or doxorubicin is the best treatment for
unresectable tumors
Small somatostatin-rich tumors of the duodenum or ampulla of Vater have also been reported,
but none of these lesions have been associated with high serum levels of somatostatin or the
clinical syndrome
Gastrinoma
-
-
A tumor that forms in cells that make gastrin
Both gastrin and stomach acid are increased by gastrinomas
When increased stomach acid, stomach ulcers, and diarrhea are caused by a tumor that makes
gastrin, it is called Zollinger-Ellison syndrome
A gastrinoma usually forms in the head of the pancreas and sometimes forms in the small
intestine
Most gastrinomas are malignant
Symptoms:
o Stomach ulcers
o Pain in the abdomen, which may spread to the back. The pain may come and go, and it
may go away after taking an antacid
o Gastroesophageal reflux
o Diarrhea
Diagnosis:
o Physical examination and history
o CT scan
o Fasting serum gastrin test: A test in which a blood sample is checked to measure the
amount of gastrin in the blood. This test is done after the patient has had nothing to eat
or drink for at least 8 hours
o Basal acid output test: A test to measure the amount of acid made by the stomach. The
patient is fasting for at least 8 hours. A tube is inserted through the nose or throat, into
the stomach. The stomach contents are removed and four samples of gastric acid are
removed through the tube
o Secretin stimulation test : The tube is moved into the small intestine and samples are
taken from the small intestine after a drug called secretin is injected. Secretin causes the
small intestine to make acid
o Somatostatin receptor scintigraphy: A type of radionuclide scan that may be used to
find small pancreatic NETs
Page 205 of 269
90. Spleen: surgical diseases and injuries. Blood disorders and diseases of surgical
importance.
Anatomy
- the pleen is a dark purplish, highly vascular, coffee bean-shaped organ of mesodermal origin
situated in the left upper quadrant of the abdomen at the level of the eighth to eleventh ribs
between the fundus of the stomach, the diaphragm, the splenic flexure of the colon, and the left
kidney
- the spleen measures about 12 × 7 × 4 cm, and usually cannot be palpated
- the splenic capsule consists of peritoneum overlying a 1- to 2-mm fibroelastic layer that
contains a few smooth muscle cells —> The fibroelastic layer sends into the pulp numerous
fibrous bands (trabeculae) that form the framework of the spleen
- the splenic artery enters the hilum of the spleen, branches into the trabecular arteries, and then
branches into the central arteries that course through the surrounding white pulp and send
radial branches to the peripheral marginal zone and the more distant red pulp
- the white pulp consists of lymphatic tissue including T cells adjacent to the central artery
(periarteriolar lymphoid sheets [PALS]), with a surrounding area containing lymphoid follicles
rich in B cells interspersed with dendritic and reticular cells important in antigen presentation
- the red pulp vascular structures have a noncontiguous basement membrane that filters cells
such as senescent erythrocytes into the macrophage-lined sinuses
- accessory spleens are seen in 10-15% of the normal population and are located primarily in the
gastrosplenic, gastrocolic, and lienorenal ligaments
- ectopic spleen (wandering spleen) is an unusual condition in which a long splenic pedicle
allows the spleen to move within the peritoneum; It often resides in the lower abdomen or
pelvis, where even a normal-sized spleen can be felt as a mass
Physiology
- the spleen has a dual function as a secondary lymphoid organ important in host immunity, and
as a large filter for blood removing senescent erythrocytes and recycling iron
- immune activity in the white pulp and the hematologic function in the red pulp
- the spleen receives 5% of the total cardiac output
- normal blood cells pass rapidly through the spleen, while abnormal and senescent cells are
slowed and entrapped — As they travel through the hypoxic, acidotic, glucose-deprived splenic
cords and sinuses of the red pulp, senescent erythrocytes pass into the vascular spaces and
are phagocytosed by macrophages in a process called “culling“
- in the presence of splenomegaly and other disease states, the flow patterns of the spleen
become more circuitous as the red pulp volume expands, so that even normal cells may be
trapped
- the spleen represents the largest single collection of lymphoid tissue in the body
- the white pulp of the spleen contains the various cellular components needed to generate an
immune response, with structural and functional relationships similar to those of lymph nodes
- lymphocytes and circulating antigen-presenting cells enter the white pulp via the marginal zone
capillaries and traverse the T cell-rich PALS before passing through bridging channels into the
red pulp
- primary follicles or germinal centers with secondary follicles at the periphery of the white pulp
are sites of B cell expansion and immunoglobulin production
- tissue macrophages in the spleen are key components of generating an immune response
particularly in encapsulated organs
- normally , about 30% of the total platelet pool is sequestered in the spleen
- splenomegaly typically involves expansion of the red pulp, which increases this sequestration
to between 80% and 95% of the platelet cell mass
- storage of erythrocytes and granulocytes in the spleen is limited in humans, but newly formed
reticulocytes released from the bone marrow concentrate in the spleen to undergo a
maturational process
Page 206 of 269
Operative indications for splenectomy
1. Hypersplenism
• characterized by diffuse enlargement of the spleen by neoplastic disorders, hematopoietic
disorders of the bone marrow, and metabolic or storage disorders
• these various disease processes result in diffuse enlargement of the spleen and amplify
the normal function of elimination of circulating blood cells resulting in general
pancytopenia
• erythrocytes and platelets are most commonly affected
• hypersplenism also may cause symptoms of early satiety due to the splenic size
2. Autoimmune/erythrocyte disorders
• specific cytopenias are related either to antibodies targeting platelets, erythrocytes, or
neutrophils
• a second category of diseases relates to intrinsic structural changes within the erythrocyte
that lead to a shortened red blood cell half- life with accelerated splenic clearance
• there is nothing intrinsically wrong with the spleen, and splenic size is typically normal
3. Trauma or injury to the spleen
4. Vascular diseases
• splenic vein thrombosis
• splenic artery aneurysm may require splenectomy for treatment
5. Cysts, abscesses and primary splenic tumors
• = mass lesions of the spleen
• includes treatment of simple cysts, echinococcal cysts, splenic abscess, and various
benign neoplasms including hamartomas, hemangiomas, lymphangiomas and rare
malignant lesions
6. Diagnostic procedures
• spleen is removed primarily to make a clinical diagnosis when none is available
• a subcategory would be staging laparotomy for Hodgkin disease
7. Iatrogenic splenectomy
• splenectomy that is performed due to an incidental injury to the spleen during surgery
within the general abdominal cavity or specifically, the left upper quadrant
8. Incidental splenectomy
• the spleen may be removed as part of a standard operation to remove the distal pancreas
most commonly, and also for gastric cancers, left-sided renal cell carcinomas, adrenal
cancers, and retroperitoneal sarcomas in the left upper quadrant
• the spleen is removed in these instances due to direct tumor extension, vascular
involvement, or the need for excision of splenic hilum lymph nodes
Splenectomy is always indicated in:
- primary splenic tumor (rare)
- hereditary spherocytosis (congenital hemolytic anemia)
Splenectomy is usually indicated in:
- primary hypersplenism
- chronic immune thrombocytopenic purpura
- splenic vein thrombosis causing gastric varices
- splenic abscess (rare)
Splenectomy is sometimes indicated:
- splenic injuriy
- autoimmune hemolytic disease
- Hodgkin disease (for staging)
- thrombotic thrombocytopenic purpura
- splenic artery aneurysm
- Gaucher disease
- …
Page 207 of 269
Splenectomy is rarely indicated in:
- chronic leukemia
- splenic lymphoma
- macroglobulinemia
- thalassemia major
- sickle cell anemia
- congestive splenomegaly and hypersplenism due to portal hypertenison
- sarcoidosis
Splenectomy is not indicated in:
- asymptomatic hypersplenism
- splenomegaly with infection
- splenomegaly associated with elevated IgM
- acute leukemia
Hypersplenism
- in the past, the term hypersplenism or increased splenic function has been used to denote the
syndrome characterized by splenic enlargement, deficiency of one or more blood cell lines,
normal or hyperplastic cellularity of deficient cell lines in the marrow, and increased turnover of
affected cells
- increased understanding of pathophysiology has shown that hypersplenism is not synonymous
with splenomegaly
- the defects in hypersplenism are exaggerations of normal splenic functions primarily associated
with the red pulp
- the principal cause of cytopenias in hypersplenism is increased sequestration and destruction
of blood cells in the spleen, which is hypertrophied or increased in volume in a variety of
diseases
- Etiologic factors include: (1) neoplastic infiltration, (2) disease of the bone marrow in which the
spleen becomes a site of extramedullary hematopoiesis, or (3) metabolic/ genetic disorders
such as Gaucher disease
- the hyperplastic spleen is not selective in its hyperfunction in most of these disorders
- the splenomegaly can lead to an increased turn- over in erythrocytes and platelets, with a
lesser effect on leukocytes
Disorders associated with secondary hypersplenism
- congestive splenomegaly (cirrhosis, portal or splenic vein obstruction)
- neoplasms (leukemia, metastatic carcinoma)
- inflammatory disease (sarcoid, lupus erythematosus, Felty syndrome)
- acute infections with splenomegaly
- chronic infection (tuberculosis, brucellosis, malaria)
- storage diseases (Gaucher disease, amyloidosis)
- chronic hemolytic diseases (spherocytosis, thalassemia, glucose -6- phosphate dehydrogenase
deficiency,…)
- myeloproliferative disorders
Clinical findings
- depend largely on underlying disorder or are secondary to the depletion of circulating blood
elements caused by the hypersplenism
- manifestation susually develop gradually, and the diagnosis often follows a routine physical or
laboratory examination
- some patients experience left upper quadrant fullness, discomfort, or early satiety
- other have hematemesis due to gastroesophageal varices
- purpura, bruising, and diffuse mucous membrane bleeding are unusual symptoms despite the
presence of thrombocytopenia
- Anemia may produce significant fatigue that may be the chief complaint in this patient
population
- Recurrent infections may be seen in patients with severe leukopenia
Page 208 of 269
Laboratory findings
- patients with primary hypersplenism usually exhibit pancytopenia of moderate degree and
generalized marrow hyperplasia
- anemia is most prominent, reflecting the destruction of erythrocytes in the hypertrophied red
pulp of the spleen
- thrombocytopenia occurs due to sequestration of platelets but also possibly due to increased
turnover
- in most cases more immature cell types such as reticulocytes are present, reflecting the
overactivity of the bone marrow to compensate for the pancytopenias
Treatment and Prognosis
- splenectomy may decrease transfusion requirements, decrease the incidence and number of
infections, prevent hemorrhage, and reduce pain
- the course of congestive splenomegaly due to portal hypertension depends upon the degree of
venous obstruction and liver damage
- the hypersplenism is rarely a major problem and is almost always overshadowed by variceal
bleeding or liver dysfunction
Metabolic disorders
- metabolic disorders amenable to splenectomy are rare inherited diseases that include as a
component splenic enlargement due to the pathologic deposition of material within the spleen
- in Gaucher disease, excess sphingolipid is deposited in the spleen
- in sarcoidosis, the spleen becomes involved with non-caseating granulomas as can be seen in
lymph nodes
Gaucher Disease
- = an autosomal recessive disorder characterized by a deficiency in beta-glucosidase, a
lysosomal enzyme that degrades the sphingolipid glucocerebroside
- pathologically the disease results in lipid accumulation within the white pulp of the spleen, the
liver, or the bone marrow
- predominant symptoms relate to massive splenomegaly from either the direct effects of the size
of the spleen or secondary to cytopenias from hypersplenism
- Treatment by total splenectomy alleviates the symptoms but results in accelerated hepatic and
bone disease as well as a significant increased risk of postsplenectomy infections
- removing most of the spleen corrects the symptoms of splenomegaly, but leaving a splenic
remnant provides a site for further deposition of lipid that protects the liver and bone
Wiskott-Aldrich Syndrome
- = an X-linked disease characterized by thrombocytopenia, combined B and T cell
immunodeficiency, eczema, and a propensity to develop malignancies
- thrombocytopenia is the major feature of this rare disorder, with most patients presenting with
bloody diarrhea, epistaxis, and petechiae at a young age
- platelet counts typically range between 20,000/mL and 40,000/mL, and the platelets that are
present are between one-fourth and one-half of normal size
- the spleen sequesters and destroys platelets in this disease, releasing “microplatelets” back
into the circulation
- splenectomy normalizes platelet shape, size, and numbers, but the postoperative course was
characterized by severe and fatal infections due to the underlying immune defect of this
disorder combined with loss of the immune function of the spleen (=> prophylactic antibitoics
after splenectomy have significantly increased survival rates)
- the optimal treatment of Wiskott- Aldrich syndrome is an HLA-matched sibling bone marrow
transplantation
- however, splenectomy with antibiotics results in better survival than an unmatched bone
marrow transplantation
Page 209 of 269
Chédiak-Higashi Syndrome
- = a rare autosomal recessive disease characterized by immunodeficiency that increases the
susceptibility to bacterial and viral infections and is manifested by recurrent fever, nystagmus,
and photophobia
- standard treatment includes chemotherapy, steroids, and ascorbic acid, but these patients
have a poor prognosis
- splenectomy has been used in the accelerated phase with beneficial results
Sarcoidosis
- = a granulomatous disease of unknown origin
- patients have significant cytopenias related to hypersplenism as well as the constitutional
symptoms and hypercalcemia of sarcoidosis
Erythrocyte disorders
- in this category of diseases there is generally no intrinsic abnormality of the spleen, as opposed
to hypersplenism, in which the spleen is primarily infiltrated by neoplasia or storage products
and causes cytopenias due to increased volume of splenic tissue
- in the autoimmune disorders, there is a humoral antibody response against proteins on
circulating blood cells, resulting in depletion primarily within the spleen
- erythrocyte disorders are genetic defects in structural components or hemoglobin that increase
the clearance of red cells in the spleen, causing a significant decrease in erythrocyte half-life
Hereditary Spherocytosis
- the most common conegnital hemolytic anemia
- autosomal dominant trait
- the genetic defects result in decreased cellular plasticity with membrane loss
- the normal shape of the erythrocyte is changed from a biconcave disk into a sphere, and the
decreased membrane-to-cell volume ratio causes a lack of deformability that delays passage
through the channels of the splenic red pulp
- significant cell destruction occurs only in the presence of the spleen
- hemolysis is largely relieved by splenectomy
- the principal manifestations are splenomegaly, mild to moderate anemia, and jaundice
- splenectomy is the sole treatment for hereditary spherocytosis and is indicated even when
anemia is fully compensated and the patient is asymptomatic
- the longer the hemolytic process persists, the greater the potential risk of complications such
as hypoplastic crises and cholelithiasis
Thalassemia Major
- in the most common form of this autosomal dominant disorder, a structural defect in the βglobin chain causes excess α chains to precipitate on the inner surface of the membrane of the
erythrocyte and produces abnormal red cells (eg, target cells)
- heterozygotes usually have mild anemia (thalassemia minor)
- however, starting early in infancy, homozygotes have severe chronic anemia accompanied by
jaundice, hepatosplenomegaly (often massive), retarded body growth, and enlargement of the
head
- since the anemia of thalassemia is due to both increased destruction of red cells and
decreased hemoglobin production, splenectomy does not cure the anemia, as in spherocytosis,
but it may reduce transfusion requirements by removing an enlarged, uncomfortable spleen
- Treatment is by iron chelation and transfusion.
Page 210 of 269
Autoimmune disorders
- the production of IgG autoantibodies specific for cell membrane proteins on erythrocytes
causes autoimmune hemolytic anemia; on platelets, it causes ITP and may cause neutropenia
in Felty syndrome
- macrophages express Fc receptors for IgG, and antibody-coated cells that pass through the
splenic sinuses of the red pulp come into contact with these phagocytic cells
- production of autoantibodies in the white pulp germinal centers may also enhance cellular
destruction, particularly in ITP
- Understanding this pathophysiologic mechanism is important, since autoimmune hemolytic
anemia caused by IgM autoantibodies (ie, cold agglutinin hemolytic anemia) does not respond
to splenectomy because macrophages do not have Fc receptors for IgM
=> this mechanism also explains why treatment with high-dose intravenous immune globulin is
beneficial in these diseases because it blocks the macrophage Fc receptor
- main presenting symptoms and signs in acquired hemolytic anemia are fatigue, pallor, jaundice,
splenomegaly, persistent anemia and reticulocystosis
- main symptoms of Immune Thrombocytopenic Purpura (ITP) are petechiae, ecchymoses,
epistaxis, and easy bruising, decreased platelet count, prolonged bleeding time, poor clot
retraction, normal coagulation time; no splenomegaly
Iatrogenic splenectomy
- procedures in which mobilization of the left upper quadrant is done (such as reflection of the
spleen and pancreas medially to expose retroperitoneal tissue, left adrenalectomy, and left
nephrectomy) put the spleen at risk for injury during the dissection
- simple mobilization of the splenic flexure of the colon can lead to bleeding from the inferior pole
of the spleen that may be difficult to control
- the ligaments that go directly from the omentum to the capsule of the spleen may be the most
common cause of iatrogenic splenic trauma, as it is a common practice to aggressively retract
the omentum as needed for exposure
91.) Abscess of the spleen. Echinococcosis of the spleen.
Abscess of the spleen
General
Etiology
-
Splenic abscess is an unusual but potentially life-threatening illness
The mortality rate for splenic abscess ranges from 15% to 20% in previously healthy patients,
with single unilocular lesions, to 80% for multiple abscesses in immunocompromised patients
Illnesses and other factors that predispose to splenic abscess include malignancies, polycythemia
vera, endocarditis, prior trauma, hemoglobinopathies, urinary tract infections, IV drug use, and
AIDS
Approximately 70% of splenic abscesses result from hematogenous spread of the infective
organism from another location, as in endocarditis
Spread may also occur in a contiguous fashion from local infections of the colon, kidney, or
pancreas
Gram-positive cocci (commonly Staphylococcus, Streptococcus, or Enterococcus spp.) and
gram-negative enteric organisms are typically involved
Mycobacterium tuberculosis, Mycobacterium avium, and Actinomyces spp. have also been found
Fungal abscesses (e.g., Candida spp.) also occur, typically in immunosuppressed patients
May be caused by splenic trauma resulting in a secondarily infected splenic hematoma
Splenic abscess is a complication of intravenous drug abuse
Clinical Features- Diagnosis
-
Splenic abscesses present with nonspecific symptoms— vague abdominal pain, fever, peritonitis,
and pleuritic chest pain
Splenomegaly is not typical
Page 211 of 269
Treatment
-
The spleen may not be palpable, because of left upper quadrant tenderness and guarding
The finding of gas in the spleen on plain abdominal x-ray is pathognomonic of splenic abscess
CT is the preferred method for diagnosis
However, the diagnosis can also be made with ultrasound
Depends on whether the abscess is unilocular or multilocular
In one third of adult patients, the abscess is multilocular
In one third of children, the abscess is unilocular
Unilocular abscesses are often amenable to percutaneous drainage, along with antibiotics, with
success rates reported at 75% to 90% for unilocular lesions
Multilocular lesions, however, are usually treated with splenectomy, drainage of the left upper
quadrant, and antibiotics
Laparoscopic splenectomy for abscess has been reported
Percutaneous drainage of large, solitary juxtacapsular abscesses may occasionally be feasible but
is associated with an extremely high mortality rate and should be reserved for patients unable to
withstand an operation
Echinococcosis of the spleen
General
Etiology
-
Hydatid disease (echinococcosis), a zoonosis, occurs worldwide but its prevalence is high in
those countries where sheep and cattle raising constitute an important industry due to close
association between man, sheep and dog
Most common sites of involvement by hydatid disease are liver followed by lung
Splenic involvement by hydatid disease is very rare accounting for only 0.9% to 8.0% of all
cases
Hydatid disease (Echinococcosis) is a zoonotic infection caused by the larval form of parasites
of tapeworm, Echinococcus granulosus
Definitive hosts are dogs- pass eggs in their feces
Humans, sheep, cattle, goats, horses are the accidental intermediate host in the development
cycle of hydatid disease
Four species of Echinococcus cause infection in humans
o Echinococcus granulosus and Echinococcus multilocularis are the most common,
causing cystic Echinococcosis and alveolar Echinococcosis respectively
o E. vogeli and E. oligarthrus cause polycystic echinococcosis and are less frequently
associated with human infection
Clinical Manifestations
Diagnosis
-
In endemic areas, 50-80% of splenic cysts are echinococcal
Splenic echinococcal cysts may be primary or secondary to ruptured liver cysts
Possible routes of primary hydatid of spleen include arterial route after passing through liver
(first filter) and lung (second filter)
Another route is the venous route through portal circulation bypassing liver and lung
Secondary hydatid spleen usually follows systemic dissemination or intraperitoneal spread
following ruptured hepatic hydatid cyst
Hydatid cysts are usually slow growing
They can reach an enormous size and be asymptomatic
Symptoms:
o Splenic cysts present with local or referred pain (often postural) or signs and symptoms
relating to splenomegaly, abdominal distension and compression of nearby structures
However, secondary infection, cyst rupture and anaphylactic shock may develop
At present sonography and CT, are the most valuable imaging techniques for the diagnosis
Serological tests are highly sensitive and specific for Echinococcosis (ELISA)
Page 212 of 269
-
Treatment
-
More recently, immune-electrophoresis has improved diagnostic accuracy in up to 95% of cases
Histopathological examination, the hydatid cyst consists of three layers. The outermost
adventitia (pseudo cyst) is formed of compressed splenic tissue, a middle layer laminated
membrane of friable ectocyst and an innermost germinal layer, endocyst
Total splenectomy, partial splenectomy, cyst enucleation and unroofing with omentoplasty are
the various preferred surgical techniques to treat splenic hydatid disease
However, during surgical treatment extreme caution must be taken to avoid life threatening
complications like anaphylactic shock due to rupture of the cyst
Laparoscopic approach has also been advocated for uncomplicated hydatid cyst of the spleen
Albendazole is an effective adjuvant therapy in the treatment of hydatid cyst
There are less chances of recurrence in patient who received albendazole therapy
Following treatment, hydatid cysts are best followed sonographically
Cysts 5-10cm or >10cm! surgery / Cysts 2-5cm! albendazole
92. Acute appendicitis and Meckel’s diverticulum.
Acute Appendicitis
General
- appr. 7% of people in Western countries have appendicitis at some point during their lives
- obstruction of the proximal lumen by fibrous bands, lymphoid hyperplasia, fecaliths, calculi, or
parasites has long been considered to be the major cause of acute appendicitis
- a fecalith or calculus is found in only 10% of acutely inflamed appendices
- as appendicitis progresses, the blood supply is impaired by bacterial infection in the wall and
distention of the lumen; gangrene and perforation occur at about 24 hours
- Pathophysiology:
• acute appendicitis seems to be the end result of a primary obstruction of the appendix
• once this obstruction occurs, the appendix becomes filled with mucus and swells
• the continued production of mucus leads to increased pressures within the lumen and the
walls of the appendix
• the increased pressure results in thrombosis and occlusion of the small vessels, and stasis
of lymphatic flow
• at this point spontaneous recovery rarely occurs
• as the occlusion of blood vessels progresses, the appendix becomes ischemic and then
necrotic
• as bacteria begin to leak out through the dying walls, pus forms within and around the
appendix (suppuration)
• the end result is appendiceal rupture (a 'burst appendix') causing peritonitis, which may lead
to sepsis and eventually death
- gangrene implies microscopic perforation, bacterial contamination of the peritoneum, and
peritonitis
Signs and Symptoms
- typically begins with vague midabdominal or periumbilical discomfort followed by nausea,
anorexia, and indigestion
- the pain is continuous but not severe, with occasional mild cramping
- the patient may feel constipated or may vomit
- importantly, within several hours of the onset of symptoms the pain shifts to the right-lower
quadrant, becoming localized and causing discomfort on moving, walking, or coughing
- physical examination shows localized tenderness to palpation and perhaps slight muscular
guarding temperature is only slightly elevated in the absence of perforation
Page 213 of 269
Laboratory Findings
- the average leukocyte count is 15,000/μL, and 90% of patients have counts over 10,000/μL
- one in ten patients has normal leukocyte count
- urinalysis is typically normal, but a few leukocytes and erythrocytes and occasionally even
gross hematuria may be noted, particularly in retrocecal or pelvic appendicitis
Imaging Studies
- on plain radiographs localized air-fluid levels, localized ileus, or increased soft tissue density in
the right-lower quadrant is present in 50% of patients with early acute appendicitis
- less common findings are a calculus, an altered right psoas shadow, an abnormal right flank
stripe, or free peritoneal air (from perforated appendicitis)
- in general, the findings on plaim films rarely aid in diagnosis
- CT: enlarged appendix with wall thickening, enhancement, or periappendiceal fat stranding is
the most useful CT findings of acute appendicitis
Diagnosis and Differential Diagnosis
- the clinical diagnosis of appendicitis rests on a combination of localized pain and tenderness
accompanied by signs of inflammation, such as fever, leukocytosis, and elevated C-reactive
protein level
- migration of pain from the periumbilical area to the right-lower quadrant is also diagnostically
significant
- in unclear cases CT and observe the patient for a period of 6 hours or more —> during this
time, patients with appendicitis experience increasing pain and signs of inflammation, while
those without appendicitis generally improve
- diagnosis may be difficult in patients at the extremities of age, and it is in these groups that
diagnosis is most often delayed:
• Infants display only lethargy, irritability, and anorexia in the early stages, but may develop
vomiting, fever, and pain as the disease progresses
• the elderly may not display any classic symptoms, even though the course of appendicitis is
more virulent in this age group
- The highest incidence of false-positive diagnosis (20%) is in women between ages 20 and 40
and is attributable to gynecologic conditions such as pelvic inflammatory disease (here pain is
more often associated with bilateral lower quadrant tender- ness, left adnexal tenderness,
onset of illness within 5 days of the last menstrual period, and a history that does not include
nausea and vomiting)
Clinical signs:
- Dunphy’s sign: increased pain in right lower quadrant with coughing
- Kocher’s sign: From the person's medical history, the start of pain in the umbilical region with a
subsequent shift to the right iliac region
Complications
- include perforation, peritonitis, abscess and pylephlebitis
- Perforation:
• most likely appears because of delay in seeking treatment
• Perforation is accompanied by more severe pain and higher fever (average, 38.3°C) than in
simple appendicitis
• It is unusual for the acutely inflamed appendix to perforate within the first 12 hours
• Appendicitis has progressed to perforation by the time of appendectomy in about 50% of
patients under age 10 or over age 50
- Peritonitis:
• Localized peritonitis results from microscopic perforation of a gangrenous appendix, while
spreading or generalized peritonitis usually implies gross perforation into the free peritoneal
cavity
• Increasing tenderness and rigidity, abdominal distention, and adynamic ileus are obvious in
these patients. High fever and severe toxicity mark progression of this catastrophic illness
- Appendiceal Abscess:
• clinical presentation consists of the usual findings in appendicitis, and may include a rightlower quadrant mass
Page 214 of 269
• ultrasound or CT should be performed; if an abscess is found, it is best treated by
percutaneous imaging-guided aspiration
- Pylephlebitis:
• = suppurative thrombophlebitis of the portal venous system
• chills, high fever, low-grade haundice and later hepatic abscesses are the hallmarks of this
grave but rare condition
• prompt surgery and antibiotic therapy is indicated
Treatment
- with few exceptions, the treatment of appendicitis is surgical (appendectomy)
- operation can be done open or laparoscopically
- prophylactic antibiotics are indicated preoperatively with a single-drug regimen (usually
cephalosporin)
Meckel’s diverticulum
= an outpouching from the small intestine, due to failure of obliteration of the yolk stalk (remnant
of the connection from the yolk sac to the small intestine present during embryonic development)
- most common malformation of the gastrointestinal tract and is present in appr. 2% of the
population
Signs and symptoms
- the majority of people with a Meckel’s diverticulum are asymptomatic (silent)
- if symptoms occur, they typically appear before the age of two years
- the most common presenting symptom is painless rectal bleeding such as melaena-like black
offensive stools, followed by intestinal obstruction, volvulus and intussusception
- occasionally, Meckel's diverticulitis may present with all the features of acute appendicitis
- at times, the symptoms are so painful that they may cause sleepless nights with acute pain felt
in the foregut region, specifically in the epigastric and umbilical regions
Pathophysiology
- the omphalomesenteric duct (vitelline duct or yolk stalk) normally connects the embryonic
midgut to the yolk sac ventrally, providing nutrients to the midgut during embryonic
development
- the vitelline duct narrows progressively and disappears between the 5th and 8th weeks
gestation
- in Meckel's diverticulum, the proximal part of vitelline duct fails to regress and involute, which
remains as a remnant of variable length and location
- having its own blood supply, Meckel's diverticulum is susceptible to obstruction or infection (a
terminal branch of superior mesenteric artery which develops from right vitelline artery)
- the Meckel's diverticulum is located in the distal ileum, usually within 60–100 cm of the
ileocecal valve
- this blind segment or small pouch is about 3–6 cm long and may have a greater lumen diameter
than that of the ileum
- it is a true diverticulum consisting of all 3 layers of the bowel wall (mucosa, submucosa and
muscularis propria)
- heterotopic rests of gastric mucosa and pancreatic tissue are seen in 60% and 6% of cases
respectively
Diagnosis
- a technetium-99m (99mTc) pertechnetate scan (Meckel scan) is the investigation of choice to
diagnose diverticula in children
- angiography might identify brisk bleeding in patients with Meckel’s diverticulum
- ultrasonography could demonstrate omphaloenteric duct remnants or cysts
- CT migh be useful to demonstrate a blind ended and inflamed structure in the mid-abdominal
cavity
- in asymptomatic patients, Meckel’s diverticulum is often diagnosed as an incidental finding
during laparoscopy or laparotomy
Page 215 of 269
Treatment
- treatment is surgical, potentially with a laparoscopic resection
- in patients with bleeding, strangulation of bowel, bowel perforation or bowel obstruction,
treatment involves surgical resection of both the Meckel's diverticulum itself along with the
adjacent bowel segment, and this procedure is called a "small bowel resection“
- in patients without any complications, only resection of the diverticulum (diverticulectomy)
- with asymptomatic Meckel’s diverticulum, some recommend that a search for Meckel's
diverticulum should be conducted in every case of appendectomy/laparotomy done for acute
abdomen, and if found, Meckel's diverticulectomy or resection should be performed to avoid
secondary complications arising from it
Complications
- bleeding — most common in young children; symptoms may include bright red blood stools,
weakness, abdominal tenderness or pain
- diverticulitis — can mimic symptoms of appendicitis
- intestinal obstruction — vominitin, abdominal pain and severe or complete constipation
93. Infectious bowel disease.
???
Inflammatory bowel disease
- Inflammatory bowel disease (IBD) is a chronic condition resulting from inappropriate mucosal
immune activation
- encompasses two major entities: Crohn disease and ulcerative colitis (distinction between
disease based to a large part to affected sites and morphologic expression)
- ulcerative colitis is limited to the colon and rectum and extends only into the mucosa and
submucosa
- Crohn disease may involve any area of the GI tract and frequently is transmural
Epidemiology
- both are more common in women, frequently present in adolescence or in young adults
- most prevalent in North America, northern Europe and Australia
- episode of acute gastroenteritis increases the risk of developing IBD
Etiology
1. genetic predisposition
2. an altered, dysregulated immune response
3. altered respond to gut microorganisms
Pathogenesis
- the causes of IBD remain uncertain -> mostly believed that IBD results from a combination of
errant host interactions with intestinal microbiota, intestinal epithelial dysfunction, and aberrant
mucosal immune responses
- Genetics:
• risk increases if there is an affected family member
• in Crohn disease the concordance rate for monozygotic twins is appr. 50% in ulcerative
colitis 16%
• NOD2 is a susceptible gene in Crohn disease
- Mucosal immune responses:
• polarization of helper T cells to T H I type is well recognized in Crohn’s disease, Th17 T
cells also contribute to pathogenesis
• pathogenic immune respone in ulcerative colitis includes T H2 component
• it is likely that some combination of derangements that activate mucosal immunity and
suppress immunoregulation contribute to both ulcerative colitis and Crohn’s disease
Page 216 of 269
- Epithelial defects
• a variety of epithelial defects have been described in Crohn disease. ulcerative colitis or
both
• e.g. defects in intestinal epithelial tight junction barrier function are present in patients with
Crohn disease
• Paneth cell granules (contain antimicrobial peptides that can affect composition of luminal
microbiota) are abnormal in patients with Crohn disease carrying ATGI6LI mutations
- Microbiota which amounts for about 10^12 organisms/mL of fecal material in the colon (50%)
Pathophysiology
- common end pathway of ulcerative colitis is inflammation of the mucosa of the intestinal tract,
causing ulceration, edema, bleeding, and fluid and electrolyte loss
- geneteic factors appeared to influence risk of IBD by causing disruption of epithelial barrier
integrity, deficits in autophagy, deficiencies in innate pattern recognition receptors, and problems
with lymphocyte differentiation, especially in Crohn disease
- inflammatory mediators have been identified in IBD:
• cytokines released by macrophages in response to various antigenic stimuli, bind to
different receptors and produce autocrine, paracrine, and endocrine effects
• cytokines differentiate lymphocytes into different types of T cells
• helper T cells type 1 (Th-1) in Crohn disease, Th-2 in ulcerative colitis
• the immune response dirupts the intestinal mucosa and leads to a chronic inflammatory
process
Pathophysiology of ulcerative colitis
- inflammation begins in rectum and extends proximally in an uninterrupted fashion to the
proximal colon and could eventually involve the entire length of the large intestine
- rectum always involved
- unlike Crohn disease, it is continuous with no ‚skip areas‘ (normal areas interspersed with
diseased areas)
- as ulcerative colitis becomes chronic, the colon becomes a rigid foreshortened tube that lacks its
usual haustral markings, leading to lead-pipe appearance observed in barium enema
Pathophysiology of Crohn disease
- can affect any portion of the GI tract, from mouth to anus
- causes 3 patterns of involvement: inflammatory disease, structures and fistulas
- most important pathologic feature is, that it is transmural -> involving all layers of the bowel, not
just the mucosa and submucosa
- it is discontinuous with skip areas
- late in disease, the mucosa deveops a cobblestone appearance, which results from deep,
longitudinal ulcerations interlaced with intervening normal mucosa
- in 35% Crohn disease occurs in ileum and colon, 32%, solely in colon, 28% in the small bowel,
and 5% in gastroduodenal region
Symptoms
- Diarrhea, cramping, and abdominal pain are common symptoms of Crohn disease in all of the
above locations, except for the gastroduodenal region, in which anorexia, nausea, and vomiting
are more common
- In spite of Crohn's and UC being very different diseases, both may present with any of the
following symptoms: abdominal pain, vomiting, diarrhea, rectal bleeding, severe internal cramps/
muscle spasms in the region of the pelvis and weight loss
Page 217 of 269
- Anemia is the most prevalent extraintestinal complication of inflammatory bowel disease
- Associated complaints or diseases include arthritis, pyoderma gangrenosum, primary sclerosing
cholangitis, and non-thyroidal illness syndrome (NTIS)
Treatment
ULCERATIVE COLITIS
Acute
CROHN’S DISEASE
Maintenance
Acute
Maintenance
Aminosalicyclates
+
+
+
-
Corticosteroids
+
-
+
-
Purine analogues
-
+
-
+
Methotrexate
-
-
+
+
Cyclosporine
+
-
-
-
Anti-TNF(infliximab)
+
+
+
+
A. Ulcerative colitis
= a chronic relapsing and remitting inflammatory disease of the colorectal mucosa; confined to the
mucosa and restricted to the large bowel
Pathogenesis
- Etiology: a convergence of genetic susceptibility, environmental modifiers and immune-mediated
tissue injury
- Pathogenesis — major theories:
1. An organ-specific autoimmune disease with immune reactivity against colonic mucosa;
the bacterial flora are required but play a permissive role priming the development of the
mucosal immune respone
2. An abnormal immune reactivity against components of the colonic flora in which the
mucosa is subject to innocent bystander injury
3. A heterogenous syndrome or group of conditions with different causes but with a final
common pathway of tissue damage
Disease modifiers/ Risk factors
- Industrialized society: a complex array of lifestyle (e.g. increased antibiotic usage, refrigeration,
delayed or altered pattern of exposure to childhood mucosal infections) and environmental
factors (e.g. exposure to environmental microbes, particularly in early life)
- Smoking: impact differs from that in Crohn’s disease; smoking is less common in colitis than in
general population; a history of recent cessation of smoking is common prior to onset or relpase
- Appendectomy: apparently protective against risk of developing colitis
- Stress: unproven adverse effect in humans but persuasive evidence in animal models
- Drugs: relapses have been linked with usage of antibiotics and NSAIDs and other barrier
breakers
Disease associations
- extraintestinal disease associations and manifestations may occur in up to 5–10% of patients
- some are true disease associations, whereas other conditions are complications or
manifestations secondary to the inflammatory activity or are side effects of treatment
- those involving the joints (peripheral arthritis and spondyloarthropathy), skin (erythema
nodosum, pyoderma gangrenosum), eye (uveitis, episcleritis) and liver (sclerosing cholangitis)
are the most common
Page 218 of 269
Pathophysiology of symptoms
- diarrhea in ulcerative colitis is multifactorial — inflammation may inhibit fluid absorption and/or
increase in secretion
- mechanisms of reduced absorption include:
• decreased colonic surface area with epithelial denudation in severe cases
• neural and hormonal inhibition of salt absorption
• increased motor activity and transit in some cases
• increased osmolar load from nutrient malabsorption such as impaired colonic salvage of
carbohydrate
- increased secretion is due to inflammation-derived secretagogues including arachidonic acid
metabolites, leakage of plasma from denuded mucosa and loss of barrier function
- bowel frequency and urgency in colitis are due not only to increased stool volume (diarrhea) but
may also arise because of irritability and reduced compliance of the inflamed rectum
- despite increased stool frequency, proximal colonic transit may be reduced (proximal
constipation) particularly in patients with proctitis or left-sided colitis
- bleeding is secondary to the adverse effects of inflammation on the mucosal microvasculature
—> Mucosal capillaries become engorged, leaky and occasionally thrombosed; Bleeding is
almost always present when ulcerative colitis is severe enough to cause diarrhea, and if absent,
another diagnosis should be suspected
Clinical presentation
- onset of symptoms is frequently gradual and intermittent, becoming progressively more severe
and persistent over a period of weeks or months
- bloody diarrhea or the passage of blood and mucus are the cardinal symptoms
- nocturnal diarrhea is common
- depending on severity of inflammation, there may be urgency and tenesmus
- cramping and abdominal pain are usually mild or absent, if pain is particularly severe or
persistent, an alternative diagnosis or a complication such as microperforation should be
considered
- when inflammation is confined to the rectum (proctitis), patients often complain of passing fresh
blood and mucus and may have constipation; It is common for such patients to have an empty
distal colon and rectum combined with fecal loading of the proximal colon
- with increasing severity of disease, anemia, fever, tachycardia and fluid become apparent
- laboratory markers of the presence of severe in ammation include a raised erythrocyte
sedimentation rate (ESR) or C-reactive protein, leukocytosis and thrombocytosis and anemia
- it is a relapsing disorder characterized by attacks of bloody diarrhea with expulsion of stringy,
mucoid material and lower abdominal pain and cramps, temporarily relieved by defecation
- colectomy cures intestinal disease, but extraintestinal manifestations may persist
Diagnosis
- colonoscopy
- clinical picture, biopsy
- plain abdominal radiology of the abdomen provides useful information regarding the extent of
colonic involvement and the presence of right-sided fecal loading in patients with proctitis
- immunological disturbances in patients with IBD include various serum antibody markers such
as pANCA (ulcerative colitis) and ASCA (Crohn’s)
Differential diagnosis
- Crohn’s disease
- Behcet disease
- Infectious colitides (e.g. campylobcter, salmonella, shigella, C. difficile)
- Sexually transmitted proctitides (cytomegalovirus, herpes simplex, chlamydia,..)
- Colorectal cancer
- Ischemic colitis
Page 219 of 269
Treatment
- Antiinflammatory drugs
• 5- aminosalicylates e.g. sulfasalazine, mesalamine, balsalazide and olsalazine (orally,
enema, suppository)
• Corticosteroids e.g. prednisone and hydrocortisone; used for moderate to severe UC that
doesn’t respond to other treatments; when given also calcium supplements prescribed
- Immune supressors
• Azothioprine (Imuran) and mercaptopurine (Purixan) — most widely used
immunosuppressants for IBD; regular check ups to look for side effects, including effects on
liver and pancreas
• Cyclosporin — reserved for patients that haven’t responded well to other medications;
potential for serious side effects, not for longtime use
• Infliximab, adalimumab, golimumab — tumor necrosis factor(TNF) inhibitors; for severe UC
• Vedolizumab — works by blocking inflammatory cells from getting to the site of inflammation
- Surgery
• can often eliminate UC, but that usually means removing the entire colon and rectum
(proctocolectomy)
• involves ileal pouch anal anastomosis — pouch is formed from the end of the small intestine
and then directly attached to the anus
- Cancer surveillance
Patients with mild-to-moderate disease
- aminosalicylstes remain cornerstone for treatment of active disease and for maintenance of
remission
- efficiacy is dose-dependent —> patients should receive maximum tolerated doses before
resorting to the use of systemic steroids
- for patients with distal or left-sided disease, topical aminosalicylate enemas alone or in
combination with oral aminosalicylates are at least as good, or in most studies better, than
steroid enemas
Moderately severe
- corticosteroid treatment — goal of treatment is to prevent progression to severe or fulminant
disease and to achieve reduced inflammatory activity and remission
- corticosteroids should be prescribed at high dosage (e.g., 40mg/d prednisolone) to bring the
condition under control and tapered as the clinical course permits
- The tapering regimen should be individualized but typically is not linear and will be by weekly
decrements of 5 mg/d while tapering from 40 mg/d to 20mg/d, and thereafter by 2.5mg/d
decrements weekly
Acute severe or fulminant ulcerative colitis
- require admission to hospital for treatment and observation
- surgical consultation should be obtained
- the four components of management are intravenous uid and electrolyte replacement, broad
spectrum antibiotic coverage, intravenous corticosteroids and discontinuation of all opiate or
anticholinergic, antispasmodic or anti-diarrheal drugs because they are risk factors for toxic
megacolon
- for severe disease, intravenous cyclosporine is an effective option either alone or in conjunction with steroids; initial reports used a relatively high dose (4mg/kg per day) of cyclosporine, but
it is clear that lower doses (2 mg/kg per day) are safer and equally effective
- advantage of cyclosporine is its rapid action, however, because of its potential toxicity, the drug
cannot be recommended as a routine oral therapy over the long term
- in the transition to long-term therapy, consideration should be given to switching to azathioprine/
6-mercaptopurine in those patients who respond to steroids and/or cyclosporine in the acute
phase
Page 220 of 269
- infliximab (anti-TNF; 5 mg/kg ivi) will be a preferable option to cyclosporine; it has been shown to
be an effective rescue therapy for induction of remission, appears to be safer and less
complicated than cyclosporine but more expensive
B. Crohn’s disease
Pathogenesis
- Crohn’s disease has a multifactorial etiology
- mucosal inflammation originates from an abnormal activation of the mucosal immune system in
the gut (to normal luminal flora), due to loss of tolerance against bacterial antigens in a
genetically predisposed individual
- Crohn’s disease is characterized by a T-helper 1 and 17 cytokine response
- Advances in IBD genetics have identified more than 50 Crohn’s disease genes, of which the
NOD2/CARD15 gene has been most studied
- the best environmental factor that predisposes to Crohn’s disease is cigarette smoking
- a general dysbiosis has been described in Crohn’s disease and the most replicated findings
have been the association of adherent-invasive E. coli and a reduction in the number of
Faecalibacterium prausnitzii
Diagnosis
- referral from primary to secondary care is often delayed by a failure to distinguish Crohn’s
disease from irritable bowel syndrome
- Laboratory findings that raise the suspicion of Crohn’s disease include a raised platelet count,
sedimentation rate or C-reactive protein, anemia or hypoalbuminemia
- Colonoscopy is used to obtain histological confirmation of terminal ileum or large bowel
involvement
- Discontinuous inflammation and non-caseating granulomata are highly suggestive of Crohn’s
disease
- Increasingly, magnetic resonance imaging is preferred to barium studies for small bowel imaging
because of the hazards of cumulative eradication
- Capsule endoscopy allows visualization of a small bowel mucosa
Symptoms
- regional enteritis, in any area of GI tract; discontinuous and transmural, with a preference for the
terminal ileum and right colon
- develops mostly in young people between the ages of 15 and 25 years
- clinical manifestations are variable, in most patients the disease begins with intermittent attacks
of relatively mild diarrhea, fever and abdominal pain
- 20% of patients are present acutely with right lower quadrant pain, fever, and bloody diarrhea
that may mimic acute appendicitis or bowel perforation
- weight loss: may be variously due to inflammatory cachexia, malabsorption and anorexia
- periods of active disease are usually interrupted by asymptomatic intervals that last for weeks to
many months
- disease reactivation may be associated with external triggers, like physical or emotional stress,
specific dietary items and cigarette smoking
- iron deficiency anemia may develop
- extensive small bowel disease may result in serum protein loss and hypoalbunemia, generalized
nutrient malabsorption, or malabsorption of vit. B12 and bile salts
- fibrosing structures (particularly of terminal ileum) require surgical resection
- extraintestinal manifestations include uveitis, migratory polyarthritis, sacroiliitis, aknylosing
spondylitis, erythema nodosum, clubbing of the fingertips
- pericholangitis and primary sclerosing cholangitis also occur
Page 221 of 269
Symptoms by site
Mouth: oral Crohn disease is characterized by aphthous ulceration, often on a background of
mucosal edema greater than that seen with simple mouth ulcers
Esophagus: rare, but may cause dysphagia or pain
Stomach and duodenum: asymptomatic gastric involvement is not uncommon; Duodenal
involvement may result in typical ulcer symptoms; Stricturing may result in symptoms of gastric
outlet obstruction
Small bowel: diffuse extensive mucosa involvement can lead to malalbsorption, protein-losing
enteropathy, diarrhea and sometimes steatorrhea; Segmental thickening or stricturing results in
painful obstructive symptoms and may lead to bacterial overgrowth
Ileocecal involvement: symptoms of obstruction due to inflammatory swelling or stricturing are
common, with post-prandial bloating, pain, and borborygmi, particularly after consumption of
fibrous vegetables or fruit; Transmural inflammation and local sepsis result in matting of local loops
of bowel and a palpable inflammatory mass
Colon: typically, colonic involvement results in diarrhea that, in contrast to that seen in ulcerative
colitis, is seldom bloody and more often associated with abdominal pain
Perianal disease: anal involvement with abscesses, fistulae or fissures
Treatment
- Salicylates are of limited efficiacy
- Corticosteroids, including budesonide, methotrexate, and anti-TNF agents, are all superior to
placebo and aminosalicylates for induction of remission
- Corticosteroids inhibit T-cell activation and proinflammatory cytokine production, however man
get dependent and it has a multitude of side effects, both short term (gastrointestinal intolerance
and dyspepsia, moon facies, acne, hypertension, hyperglycemia, depression, and psychosis)
and long term (osteoporosis, cataract, growth failure)
- Budesonide, a synthetic glucocorticosteroid, provides the efficacy of a corticosteroid without its
toxicity — budenoside 9 mg/day was as effective as prednisone 40 mg/day in inducing remission
- Immunosuppressive drugs (azathioprine, 6-mercaptapurine or methotrexate) and anti-TNF
agents are effective for consolidation and maintenance of remission
- Azathioprine is associated with a number of side effects, incl. bone marrow toxicity, pancreatitis
and hepatotoxicity
- Methotrexate: in active disease 25mg once weekly and in maintenance 15mg i.m. once weekly
- Combining an anti-TNF and immunosuppressive agent is superior to either treatment alone
- Choice of traditional treatment escalation (bottom up) versus initial intensive (top down)
treatment varies from country to country
- Antibiotics: Metronidazole and ciprofloxacin (quinolone) are valuable, particularly as adjunctive
treatment in perianal disease
- Anti-TNF-alpha antibodies (infliximab): prescribed for treatment of active therapy-resistant
and active fistulizing Crohn’s disease; response rates of 75–80% are reached after a single
infusion of in iximab 5 mg/ kg, with up to 50% of patients entering clinical remission; most
patients relapse 8-12 weeks after initial inusion —> retreatment every 8 weeks
- other more humanized anti-TNF are Adalinumab (Humira) and certolizumab
- surgery should be reserved for patients in whom medical treatment fails to control inflammation
or for complications such as strictures, abscesses or fistulae
94.) Megacolon
Definition
-
Loss of intestinal peristalsis and subsequent dilation of the colon in the abscence of a mechanical
obstruction
Classification
-
Acute megacolon
Chronic megacolon
Toxic megacolon
Page 222 of 269
Acute megacolon (or Ogilvie’s syndrome)
Definition
Etiology
-
Acute dilation of the colon in the absence of a mechanical obstruction, characteristically seen in
severely ill or postoperative patients
Occurs in seriously ill patients or those who have undergone a major surgical procedure
Idiopathic; possible factors include:
o Electrolyte imbalance
o
Trauma; major surgery
o
Hypothyroidism
o
Drugs (e.g., anticholinergic drugs, opioid analgesics, antipsychotics, calcium channel
blockers)
Pathophysiology
-
Etiological factors → impairment/destruction of the autonomic nervous system → imbalance
between sympathetic and parasympathetic control of intestinal motility → accumulation of
feces, air, and intestinal secretions in the intestine → colonic dilation
Clinical Features
-
Gradual abdominal distention
Abdominal pain; constipation/diarrhea
Tympanitic abdominal percussion; decreased frequency of bowel sounds
Signs of colonic ischemia or impending perforation: Fever, tachycardia and peritoneal signs
(guarding, rigidity, rebound tenderness)
Diagnosis
-
Laboratory values: may show signs of underlying disease; hypokalemia as a potential cause
-
Abdominal x-ray: dilation of the cecum and right colon (occasionally up to the rectum) with/
without multiple air-fluid levels; haustrae are preserved (The cecum, ascending, and transverse
colon are the first to dilate, followed by the splenic flexure, descending, and sigmoid colon)
-
Contrast enhanced CT scan (oral and IV contrast)
o
Confirms x-ray findings
o
Rules out mechanical obstruction (e.g., tumor/stricture)
o
Can diagnose complications (ischemic bowel segments or perforation peritonitis)
o
Colonoscopy and endoscopy: indicated in hemodynamically stable patients when CECT
(contrast enhanced CT) cannot be performed; rules out a mechanical obstruction
Treatment
- Conservative management (regular abdominal examinations)
- Supportive measures
o Indications: patients with mild symptoms and cecal dilation <12 cm
Page 223 of 269
o Treat the inciting factor
o IV fluids and bowel rest
o Bowel decompression
▪ Nasogastric tube to decompress the stomach
▪ Rectal tube to decompress the rectum and distal colon
- Pharmacologic management: neostigmine
o Indications:
▪ No improvement > 12-48h of bowel rest and decompression
▪ Cecal dilation >12 cm and no signs of colonic ischemia/ perforation or
peritonitis
- Colonoscopic bowel decompression: if neostigmine is contraindicated or unsuccessful
-
Surgery
o
Signs of impending or actual colonic ischemia/perforation or peritonitis
o
Failure of conservative therapy
o
Cecostomy (Cecostomy is a decompression procedure in which a tube is placed into
the cecum, and brought out through the skin, to deflate the cecum. It can be performed
percutaneously, under image-guidance or via laparotomy)
o
Colectomy with/without colostomy (The necrosed bowel is resected. The cut-ends, if
healthy are anastomosed. If not, a temporary colostomy is created, and reversed at a later
date)
Chronic megacolon
Definition
-
Permanent dilation of the colon caused by congenital/acquired colonic dysmotility in the absence
of a mechanical obstruction
Etiology
-
-
Congenital (e.g., Hirschsprung disease)
Acquired
o
Neuropathies (e.g., diabetic neuropathy, spinal cord injury, Parkinson's disease)
o
Myopathies (e.g., Duchenne's muscular dystrophy, myotonic muscular dystrophy)
o
Connective tissue disorders (e.g., scleroderma, systemic lupus
erythematosus, dermatomyositis)
o
Chronic Chagas disease
Idiopathic - reason unknown
Pathophysiology
-
Etiological factors cause a neural and/or motor dysfunction of the bowel → bowel
dysmotility → progressive colonic dilation
Page 224 of 269
Clinical Features
-
-
Recurrent episodes of:
o
Constipation
o
Abdominal pain and distention (bloating)
o
Anorexia, early satiety, and nausea
Examination findings: Abdominal distention; mild abdominal tenderness
Signs and symptoms of the underlying disorder
Diagnosis
-
Laboratory values: may show signs of underlying disease
-
Contrast-enhanced CT scan (CECT; oral and IV contrast)
Abdominal x-ray: dilation of the cecum and right colon (occasionally up to the rectum) with/
without multiple air-fluid levels; haustrae are preserved
o
Confirms x-ray findings
o
Rules out mechanical obstruction (e.g., tumor/stricture)
o
Can diagnose complications (ischemic bowel segments or perforation peritonitis)
-
Colonoscopy and endoscopy: indicated in hemodynamically stable patients when CECTcannot
be performed; rules out a mechanical obstruction
-
Assessment of colonic motility
-
o
Colon transit scintigraphy: Investigation of choice to diagnose and determine the extent
of delayed colonic transit
o
Colon transit test using radio-opaque markers
Manometry
Colonic biopsy
Treatment
-
-
Conservative management
o
Dietary modifications
o
Osmotic laxatives and enemas to empty the colon and prevent fecal impaction
o
Prokinetic drugs: Erythromycin, metoclopramide, neostigmine
o
Treatment of the underlying disorder
Surgery: indicated in patients who do not improve/worsen on conservative therapy
o
Total abdominal colectomy with ileorectal anastomosis
o
"Surgical treatment" of Hirschsprung's disease
Toxic megacolon
Definition
-
A life-threatening, acute dilation of the colon associated with systemic toxicity
Page 225 of 269
Etiology
-
-
Infectious colitis
o
Bacterial: C. difficile (pseudomembranous
colitis), Salmonella, Shigella, Campylobacter infections
o
Parasitic: Trypanosoma cruzi (Chagas disease), E. histolytica (amebic dysentery)
infections
Inflammatory colitis: Ulcerative colitis, Crohn's disease
Pathophysiology: Colitis
-
→ colonic accumulation of inflammatory mediators and bacteria → nitric oxide synthesis
→ colonic dilation
-
→ edema and inflammation of the colonic smooth muscle → colonic dysmotility → colonic
dilation
Clinical Findings
-
(Bloody) diarrhea and vomiting
Abdominal distention and pain
Signs of sepsis (fever, tachycardia, hypotension) and dehydration
Signs of underlying disease (Ulcerative colitis, Crohn's disease)
Diagnosis
-
-
-
Laboratory findings: neutrophilic leukocytosis, anemia, ↑ ESR/CRP, hypokalemia
Abdominal x-ray findings
o
Dilation of the colon (transverse colon diameter > 6 cm)
o
Loss of haustration
o
Multiple air-fluid levels
Contrast enhanced CT scan (oral and IV contrast)
o
Confirms x-ray findings
o
Rules out mechanical obstruction (e.g., tumor/stricture)
o
Can diagnose complications (ischemic bowel segments or perforation peritonitis)
Stool tests for C. difficile toxin: in patients with preceding diarrhea
Colonoscopy and endoscopy: contraindicated in suspected toxic megacolon due to high risk of
perforating the colon
Diagnostic Criteria
-
Radiographic evidence of colonic dilatation
-
One of the following: dehydration, hypotension, altered mental status, or electrolyte disturbance
Three of the following: fever (> 38,6C), tachycardia (> 120 beats/min), leukocytosis(> 10,500/
µL), or anemia
Page 226 of 269
Complications
-
Colonic ischemia → colonic perforation→ peritonitis
Sepsis and multiorgan dysfunction
Treatment
-
-
Conservative treatment
o
Complete bowel rest: NPO, nasogastric tube insertion, IV fluids, correction of fluid and
electrolyte imbalances
o
Antibiotics: oral metronidazole for C. difficile colitis
o
Inflammatory bowel disease: IV steroids (hydrocortisone, dexamethasone)
Surgery
o
Indications: no response to medical management within 24–72 hours; development of
complications
o
Procedure: subtotal colectomy and end ileostomy
▪
Anastomosing the cut ends of the bowel is contraindicated in patients with toxic
megacolon since the bowel wall is inflamed and friable, which increases the
chance of postoperative anastomotic leaks. Once the patient is stable, can
tolerate an enteral diet, and the inflammation has subsided, bowel continuity can
be restored by performing an ileorectal anastomosis
95.) Diverticulosis of the colon
Definition
-
Diverticulum: is an abnormal sac or pouch protruding from the wall of a hollow organ
Diverticulosis: is a term used to indicate the presence of colonic diverticula
General considerations:
-
-
Diverticula are more common in the colon than in any other portion of the GIT
Most colonic diverticula are false diverticula
o They consist of mucosa and submucosa that have herniated through the muscular layer
of the colon wall
True diverticula
o Contain all the layers of the bowel wall
o Rare in the colon
Most common location for diverticula is the sigmoid colon
Diverticula form as a result of increased intraluminal pressure acting at areas of relative
weakness on the bowel wall caused by the blood supply (Pulsion diverticula) (push from inside)
o The vasa recta extend onto the colon wall, then penetrate the muscular layer between the
taenia to supply the mucosa
o Diverticula are most commonly located in the area between the mesenteric taenia and
the antimesenteric taenia with a skip area on the antimesenteric border
Traction diverticula: extrinsic inflammation retracts or pulls the bowel wall outwards (pull from
outside), uncommon
Epidemiology
-
More common in Western nations: 30%-60% develop diverticula
In Asian countries: right-sided diverticula
Prevalence increases with age
10% of patients are affected by the age of 40
65% by the age of 80
Page 227 of 269
Risk factors
-
Contribution of a low fiber diet rich in red meat (increases colonic pressure)
Poor physical activity
Constipation
Increasing age
Smoking
Obesity
Alcohol
NSAID use
Patients with Ehlers-Danlos and Marfan syndrome are at increased risk because both of which
involve abnormal connective tissue
Symptoms and Signs
-
Remains asymptomatic in up to 80% of people
Constipation
Abdominal cramping
Bloating
Diarrhea
Complications
-
20% of patients with diverticulosis develop complications
Rectal bleeding (bright red blood per rectum)
Diverticulitis
Stricture
Fistula
Physical Examination
-
Abdominal examination: mild tenderness in the LLQ
Left colon is sometimes palpable as a firm tubular structure
-
Barium enema
CT scan
Colonoscopy
Diagnosis
Treatment
Prognosis
-
Asymptomatic patients- high fiber diet
Weight loss
Smoking cessation
Diet low in red meat
Surgery is not indicated for uncomplicated diverticulosis
About 75% of patients who have presented with complications of diverticular disease report no
prior colonic symptoms
Diverticulitis
-
Acute diverticulitis is the result of micro- or macroscopic perforation of a diverticulum resulting
in an inflammatory response
The severity of disease can range from mild inflammation localized to a segment of the bowel
wall (microperforation) to feculent peritonitis (macroperforation)
The majority of patients (75%) present with simple, uncomplicated, diverticulitis
Complicated diverticulitis occurs in 25% of patients and refers to macro- or gross perforation
with abscess or peritonitis, as well as those who develop complications including stricture or
fistula
Patients with acute diverticulitis classically present with abdominal pain and fullness localized to
the left-lower quadrant
The severity of abdominal pain ranges from mild to severe, often described as steady aching or
cramping
Changes in bowel habits, including constipation, diarrhea, or both are common
Page 228 of 269
-
-
Dysuria is indicative of inflammation adjacent to the bladder
Nausea and vomiting may be present depending on the location and severity of the inflammation
Physical findings characteristically include low-grade fever, mild abdominal distention, and leftlower quadrant tenderness
There may be a palpable mass
Leukocytosis is common
CT scan of the abdomen and pelvis with intravenous contrast is the preferred initial imaging
study
Hinchey classification- stages:
o (0) mild clinical diverticulitis
o (1a) pericolic inflammation or phlegmon
o (1b) pericolic or mesocolic abscess
o (2) pelvic, intra-abdominal, or retroperitoneal abscess resulting from an extension of a
pericolic abscess
o (3) purulent peritonitis
o (4) feculent peritonitis
In case of surgery: resection of the diseased segment with temporary colostomy and several
months later reconnection
96. Benign diseases of the colon: diverticulosis, polyps and polyposis syndromes.
Diverticulosis
- results from weakening of the colonic wall
- in industrialized nations, has a 30–50% prevalence in patients > 50 years of age
- Rates ↑ with low dietary fiber and advancing age
- In the United States, the predominant location is the left colon
Symptoms
- appr. 70% remain asymptomatic, 20% will develop diverticulitis and 10% will develop
diverticular bleeding
- in asymptomatic patients, the disorder is associated with excessive flatulence and pellet-like
stools
Exam
- exam may be normal, or patients may present with mild abdominal distention and pellet-like
stools
Differential diagnosis
- colorectal cancer
- Irritable bowel syndrome
Diagnosis
- No diagnosis is needed in patients who are asymptomatic
- Barium enema: accurate for diverticulosis, but insufficient to rule out colorectal cancer
- Colonoscopy: recommended for routine colorectal cancer screening in patients >50 years of
age
Treatment
- Dietary fiber 20-30g/d
- Coarse bran or supplements (psyllium) to ↑ stool bulk and ↓ colonic pressure
Complications
- Diverticular bleeding affects 10-20% of patients
• presents with painless rectal bleeding, usually from a single diverticulum (more frequently in
the right colon)
• spontaneous cessation is common (80%), but apparently one third of patients have recurrent
bleeding
• treat with colonoscopy and angiography with embolization; consider elective colonic
resection after the second recurrence
Page 229 of 269
- Diverticulitis
• microperforation of the diverticula with associated inflammation
• occurs in 10-25% of those with diverticulosis and commonly affects sigmoid colon; frequency
increases with advancing age
• Symptoms: LLQ pain (93–100%); fever, nausea, vomiting, constipation, diarrhea, urinary
frequency (“sympathetic cystitis”)
• Exam may reveal LLQ tenderness, localized involuntary guarding, percussion tenderness, and
tender LLQ fullness or mass
• Treat with IV fluids, bowel rest, and NG suction for ileus or obstruction; Broad spectrum
antibiotics; surgery for perforation, abscess, fistula, obstruction or recurrent diverticulitis (>2
episodes)
Colorectal polyps
- colorectal cancer usually begins as a „polyp“ (= a growth on the inner surface of the colon)
- the two most common types of polyps found in the colon and rectum include:
• Hyperplastic and inflammatory polyps: these polyps usually don’t carry a risk of developing
into cancer; however large hyperplastic polyps, especially on the right side of the colon, are of
concern and should be removed
• Adenomas or adenomatous polyps: pre-cancerous
- with the growing size of adenoma the risk to become cancerous grows (>2cm up to 40%)
- with increasing age the frequency of polyps increases (appr. 30% > 60yrs.)
- Intestinal polyposis syndromes:
• Familial adenomatous polyposis (FAP)
- starts > 15 years of age
- mutation in the APC-tumor suppressor gene with autosomal-dominant inheritance in
75% of cases
- risk of carcinoma is 100%, also duodenal carcinomas
- Gardner-syndrome: Adenomatosis coli, Osteomas and epidermoid cysts
- Turcot-syndrome: Adenomatosis coli and Glio-/Medulloblastomas
• Cronkhite-Canada-Syndrome
- starts > 50 years of age
- generalized gastrointestinal polyposis (only low risk of malignancy) and diarrhea with
protein and electrolyte loss, hyperpigmentation of the skin, alopezia (baldness) and nail
dystrophy
• Familial juvenile polyposis
- hamartomatous polyps with increased risk of malignancy
- increased familial incidence in 30% of cases
• Peutz-Jeghers-Syndrome
- starts between the 30.-40. year of age
- hamartomatous polyps of the small intestine, more rare gastric or colon polyps
- autosomal-dominant inheritance and new mutations occur in a 1:1 ratio
- perioral hyperpigmentation
- increased incidence of pancreas, mamma-, ovarial or testicular carcinoma
Symptoms
- mostly without symptoms, rarely diarrhea
- complications: perianal bleeding, formation of stenoses and malignancy
Diagnosis
- recto-digital examination
- rectoscopy and ileocoloscopy including polypectomy and histologic examination
- to exclude polyps in the small intestine: Hydro-MRT
Page 230 of 269
Treatment
- endoscopic ablation
- with very big and wide polyps, resection of the rectal segment
- with familial adenomatous polyposis prophylactic proctocolectomy with ileoanal pouch operation
before the age of 20
- regular endoscopic check ups if adenomas are present: the first control after one year,
afterwards every 3 years if no polyps present and every 2 years with multiple adenomas
97. Colon cancer.
Risk factors
- high fat and protein consumption, low fiber content of the nutrition and adipositas
- longtime nicotine and alcohol consumption
- colorectal adenomas
- chronic-inflammatory diseases of the colon
- genetic factors: positive familial anamnesis for colorectal carcinoma, familial syndrome
• familial polyposis syndrome, e.g. adenomatous polyposis
• hereditary, non-polyposis colorectal carcinoma (HNPCC, Lynch-syndrome): mutation of the
DNA repair genes with autosomal-dominant inheritance; manifestation around 45 years of
age; often adenocarcinomas of other organs, e.g. endometrial-, ovarial-, gastric- and
urothelcarcinomas
- more than 2/3 of all colorectal carcinomas are found in the rectosigmoid
- 95% of all carcinomas develop from adenomas (in classic adenomas (70-80%) due to activation
of oncogenes, e.g. K-ras and the inactivation of tumor suppressor genes, e.g. APC-gene
(adenomatous polyposis coli), DCC-gene (deleted in colorectal carcinoma), p53-gene)
- 90% of cases appear after the age of 50
- 5-year survival rate depends on the stage of the tumor: 90-95% in stage I, 60-90% in stage II,
30-60% in stage III, <10% in stage IV
Symptoms
- initially often asymptomatic
- visible/occult blood in feces
- changes in normal stool habits, e.g. „fake friend“ (Flatus mit Stuhlabgang, fart with defecation),
paradox diarrhea
- abdominal pain
- weakness in performance, pallor (anemia), weight loss, fever
- complications: obstruction (ileus) mainly in left-sided colon cancer
Diagnosis
- eventually abdominal palpable resistance (mainly with right-sided colon cancer)
- during recto-digital examination appr. 10% of colorectal cancers are found
- in blood tests an anemia may be present
- coloscopy including biopsy
- histologically there are „low-grade“ carcinomas (G1 and G2), „high-grade“ carcinomas (G3 and
G4 undifferentiated)
- also possible are 3D-MRT (virtual coloscopy) or colon-contrast-enema
- for staging: CT of the abdomen and pelvis, eventual angio-CT of the liver, abdominal
sonography, x-ray of the thorax
- eventual transrectal ultrasound to estimate the depth of the rectal carcinoma
- before starting the therapy detect the tumor marker CEA (carcino-embryonal antigen) and CA
19-9 for check ups
- for recurrence diagnosis FDG (fluor-desoxyglucose)-PET or radioimmunoscintigraphy with
99mTc- marked CEA antibodies
- primary hematogenous metastases in the liver and lung (25% of patients already have hepatic
metastases when cancer is initially found)
Page 231 of 269
- lymph node metastases depend on the localisation ot the rectal carcinoma
- staging according to the TNM-system (tumor, lymph nodes, metastases)
Staging
T1 - tumor infiltrating submucosa
T2 - tumor infiltrating muscularis propria
T3 - tumor infiltrating subserosa or non-peritoneal pericolic/perirectal tissue
T4 - tumor perforates the visceral peritoneum or infiltrates neighbouring organs, e.g. vagina,
prostate, bladder, ureter, kidneys
N1 - 1-3 pericolic/perirectal infested lymph nodes
N2 - more than 4 lymph nodes are infested
M1 - metastases
M1a - metastases only in one organ (liver, lung, ovar, non-regional lymph nodes)
M1b - metastases in several organs or in the peritoneum
Treatment
Surgery for early-stage colon cancer
- Removing polyps during colonoscopy: If your cancer is small, localized and completely
contained within a polyp and in a very early stage, your doctor may be able to remove it
completely during a colonoscopy
- Endoscopic mucosal resection: Removing larger polyps may require also taking a small
amount of the lining of the colon or rectum in a procedure called an endoscopic mucosal
resection
- Minimal invasive surgery: Polyps that can't be removed during a colonoscopy may be
removed using laparoscopic surgery. In this procedure, the surgeon performs the operation
through several small incisions in your abdominal wall, inserting instruments with attached
cameras that display the colon on a video monitor. The surgeon may also take samples from
lymph nodes in the area where the cancer is located.
Surgery for invasive colon cancer
- Partial colectomy: During this procedure, the surgeon removes the part of the colon that
contains the cancer, along with a margin of normal tissue on either side of the cancer. The
surgeon is often able to reconnect the healthy portions of your colon or rectum. This procedure
can commonly be done by a minimally invasive approach (laparoscopy)
- Ostomy: when the healthy portions of the colon or rectum are not possible to reconnect, an
artifical opening in the wall of the abdomen is needed to allow the elimination of stool
(sometimes only temporary)
- Lymph mode removal to check for metastatic invasion
- „En-bloc“ resection including the mesentrium and removal of the regional lymph drainage area
with a „no-touch“ technique (hemicolectomy, transversumresection or radical sigmaresection)
- evtl. resection of solitary liver- and lung metastases
- in stage II postoperative adjuvant fluoropyrimidin-monotheraphy (e.g. Capecitabin, oral 5-FU
prodrug)
- in stage III adjuvant chemotherapy with 5-FU (5-Fluorouracil), folinic acid and Oxaliplatin
- in stage IV palliative chemotherapy with 5-FU, folinic acid and Oxaliplatin or Irinotecan, evtl.
additional Anti-VEGF-antibodies (e.g. Bevacizumab (Avastin)) or Anti-EGF-antibodies
(Cetuximab)
- possibly palliative local treatments, e.g. cryo-, laser-, radiofrequence therapy
Page 232 of 269
98. Injuries of the abdomen. Types.
- doctors often classify abdomen injuries by the type of structure that is damaged and how the
injury occured
- the types of structures include:
• abdominal wall
• solid organs (ie, the liver, spleen, pancreas or kidney)
• hollow organs (ie, the stomach, small intestine, colon, ureters or bladder)
- abdominal injuries may also be classified by wheter the injury is:
• blunt
• penetrating
Blunt Trauma
- may involve a direct blow (e.g. a kick), impact with an object (e.g., a fall onto bicycle
handlebars), or a sudden decrease in speed (e.g., a fall from a height or a motor vehicle crash)
- the spleen and liver are the two most commonly injured organs
- hollow organs are less likely to be injured
Penetrating Injuries
- occur when an object breaks the skin (e.g., as a result of a gunshot or a stabbing)
- some penetrating injuries involve only the fat and muscles under the skin —> These penetrating
injuries are much less concerning than those that enter the abdominal cavity
- gunshots that enter the abdominal cavity almost always cause significant damage
- stab wounds that enter the abdominal cavity do not always damage organs or blood vessels
- sometimes, a penetrating injury involves both the chest and the upper part of the abdomen
—> For example a downward stab wound to the lower chest may go through the diaphragm
into the stomach, spleen, or liver
- blunt or penetrating injuries may cut or rupture abdominal organs and/or blood vessels
- blunt injury may cause blood to collect inside the structure of a solid organ or in the wall of a
hollow organ (such as the small intestine) —> such collections of blood are called hematomas
- uncontained bleeding into the abdominal cavity, in the space surrounding the organs, is called
hemoperitoneun
cuts and tears begin bleeding immediately
bleeding may be minimal and cause few problems
more serious injuries may cause massive bleeding with shock and sometimes death
bleeding from abdominal injury is mostly internal (within the abdominal cavity); when there is a
penetrating injury, a small amount of external bleeding may occur through the wound
- when a hollow organ is injured, the contents of the organ (for example, stomach acid, stool, or
urine) may enter the abdominal cavity and cause irritation and inflammation (peritonitis).
-
Symptoms
- people usually have abdominal pain or tenderness
- pain can be mild, and the person may not notice or complain about it because of other more
painful injuries (such as fractures) or because the person is not fully conscious (for example,
because of a head injury, substance abuse, or shock)
- pain from a spleen injury sometimes radiates to the left shoulder
- pain from a small intestinal tear is minimal at first but worsens steadily
- people with a kidney or bladder injury may have blood in the urine
- in people with severe bleeding the abdomen may be swollen because of the excess blood
- people who have lost a large amount of blood may have:
•
•
•
•
•
a rapid heart rate
rapid breathing
sweating
cold, clammy, pale or bluish skin
confusion or low level of alertness
Page 233 of 269
Complications
- in addition to the immediate damage, abdominal injuries may also cause problems later on
- these delayed problems include:
• hematoma rupture
• intra-abdominal collection of pus (abscess)
• intestine blockage (obstruction)
• abdominal compartment syndrome
Hematoma rupture
- the body is usually able to reabsorb collections of blood (hematomas), although it may take
several days to weeks
- sometimes a hematoma ruptures rather than being resorbed
- rupture can occur within the first few days after injury, but sometimes rupture occurs later,
occasionally even months later
- Rupture of a hematoma of the spleen or liver can cause life-threatening bleeding into the
abdominal cavity
- Rupture of a hematoma of the wall of the intestine can allow intestinal contents to leak into the
abdomen and cause peritonitis
- Intestinal wall hematomas sometimes form a scar when they heal —> This scarring can cause
narrowing of the intestine at that spot that leads to intestinal obstruction, typically years later
Intra-abdominal abscess
- may occur if injury to a hollow organ is not detected
- abscesses may also form after surgery to repair serious abdominal injury
Intestinal obstruction
- sometimes scar tissue forms after an injury heals or after surgery on the abdomen
- that scar tissue forms fibrous bands (adhesions) between loops of intestine
- usually, these adhesions cause no symptoms, but sometimes another loop of intestine gets
twisted under an adhesion —> this twisting can block the intestine and cause abdominal pain
and vomiting
Abdominal compartment syndrome
- just as a sprained ankle, abdominal organs swell after injury
- although there is usually enough room in the abdomen for such swelling, unchecked swelling
ultimately increases pressure in the abdomen
- the increased pressure squeezes the organs and restricts their blood supply, which causes pain
and then organ damage
- such pressure-related damage is called abdominal compartment syndrome
- increased abdominal pressure may eventually also increase pressure in other body tissues,
such as the lungs, kidneys, heart, blood vessels, and central nervous system
- abdominal compartment syndrome tends to develop in people with severe injuries or injuries
that require surgery
- abdominal compartment syndrome is extremely serious and increases the risk of death
Diagnosis
- Imaging tests (CT, ultrasound)
- Urinalysis
- Sometimes, exploratory surgery
- in some people, abdominal injury is obviously severe (such as many gunshot wounds)
—> Doctors take such people directly to the operating room for exploratory surgeryand do not
do tests to identify the specific injuries
Treatment
- manage or reverse blood loss
- sometimes surgery
- i.v. fluids as needed to replace blood loss; with significant blood loss give blood transfusions
- surgery may be needed to repair damaged organs and stop bleeding
Page 234 of 269
99. Obstruction syndrome — Ileus: definition, causes, diagnosis, classification,
complications and treatment. Paralytic and spastic ileus.
Ileus = Failure of appropriate forward movement of bowel contents — may be secondary to
either mechanical obstruction of the bowel (mechanical ileus) or a disturbance in neural
stimulation (adynamic/paralytic ileus)
Small Bowel Obstruction (SBO)
General
- SBO is one of the most common disorders affecting the small bowel
- Characterized by impairment in the normal flow of intraluminal contents and can be divided into
mechanical obstruction and paralytic ileus (classification)
- Mechanical obstruction implies an extrinsic or intrinsic obstacle that prevents the aboral
progression of intestinal contents and it may be complete or partial
- Simple obstruction occludes the lumen only; obstruction with strangulation impairs the blood
supply also and leads to necrosis of the intestinal wall
- Paralytic (or adynamic) ileus is due to a neurogenic failure of peristalsis to propel intestinal
contents with no mechanical obstruction
Etiology
- Causes causes of mechanical obstruction can be divided into three groups according to the
relationship to the intestinal wall:
• intraluminal by abnormal materials (obturation): bezoars, gallstone, worms, or foreign body
(usually obstructs at the ileocecal valve)
• intramural: encroaching on the lumen (inflammatory bowel disease [5%]), fibrous stricture
secondary to trauma, ischemia, or radiation, intussusception)
• extrinsic compression: adhesions (60%), malignancy (20%), hernias (10%), volvulus and
others (5%)
- The most common etiologies are intra-abdominal adhesions (e.g. after abdominal sugery),
hernias (most common in patients without previous abdominal operation), and neoplasms
- Other causes inlcude Crohn disease, intussception (most often seen in children without an
organic lesion), volvulus (consequence of intestinal malrotation in children, or adhesions in
adults), foreign bodies, gallstones through a cholecysto-duodenal fistula
- Also common after surgery because people are often prescribed medication that can slow
intestinal movement (type of paralytic ileus) — examples of medicines causing paralytic ileus:
• hydromorphon, morphine, oxycodon, trcyclic antidepressant
Pathophysiology
- with the onset of obstruction, gas and fluid accumulate and distend the intestinal loops
proximal to the site of obstruction => intraluminal and intramural pressures rise until
microvascular perfusion to the intestine is impaired, leading to intestinal wall ischemia, and
ultimately necrosis
- activity of the smooth muscle of the small bowel is increased in an attempt to propel its
contents past the obstruction consuming all energy sources => intestine becomes atonic and
enlarges further
- emesis could be feculent due to bacterial overgrowth —particularly with distal obstruction—as
the intestinal dilation progresses proximally
- when full thickness necrosis of the intestinal wall occurs, luminal content with an elevated
bacterial load enters the peritoneal cavity, is absorbed by the peritoneum causing septic shock
- progression of pathophysiologic events when the bowel is strangulated occurs more rapidly
than with simple obstruction and is characterized by an acute impairment of venous return
initially followed by arterial flow with subsequent ischemia, necrosis, and perforation of the
intestinal wall
Clinical findings
- patients usually present with nausea, vomiting, colicky abdominal pain, and obstipation,
although residual gas and stool distal to the obstruction may be expelled
Page 235 of 269
- with proximal SBO, emesis is usually profuse, containing undigested food in close temporal
association with oral intake; abdominal pain is more often described as upper abdominal
discomfort associated with epigastric distension
- Distal SBO is characterized by diffuse and poorly localized crampy abdominal pain
- Feculent vomiting present in cases of longstanding distal SBO is the consequence of bacterial
overgrowth and is pathognomonic for a complete mechanical obstruction
- In the presence of strangulation, fever often develops, and previously crampy abdominal pain
becomes peritonitis
SBO - variable manifestations of obstruction depend on the level of blockage of the small bowel
High
Middle
- frequent vomiting
- moderate vomiting
- no distention
- moderate distention
- intermittent pain but not classic - intermittent oain (crescendo,
crescendo type
colicky) with free intervals
Low
- vomiting late, feculent
- marked distention
- variable pain; may not be
classic crescendo type
Laboratory findings
- intravascular volume depletion and dehydration
- elevated hematocrit is indicative of hemoconcentration
- leukocytosis is often the result of dehydration and an acute stress response rather than an
underlying infection
- features of strangulated obstruction or perforation include marked leukocytosis and metabolic
acidosis
Imaging Studies
- plain x-rays of the abdomen with the patient in supine and upright position can confirm the
clinical diagnosis of SBO
• They reveal dilated small bowel loops with air-fluid levels in a ladder-like appearance, and a
paucity of air in the colon
• These features may be minimal or absent in early or high grade obstructions
- CT scan of abdomen and pelvis with both intravenous and oral contrast is widely used
• CT scan can visualize the specific location of the obstruction, showing a discrepancy in the
caliber between distended proximal bowel loops and collapsed distal intestine
• CT can also reveal the etiology of SBO and demonstrate signs of strangulation including
thickening of the bowel wall, air in the bowel wall or portal venous system and poor uptake
of contrast by the affected bowel wall
• Ascites between dilated bowel loops and in the pelvis is often reported in both simple and
strangulated obstruction
• Intraperitoneal free air indicates perforation
Differential Diagnosis
- pain in patients with paralytic ileus is usually not severe but is constant and diffuse, and the
abdomen is often distended and mildly tender
- if ileus has resulted from an acute intraperitoneal inflammatory process, there should be
symptoms and signs of the primary disease as well as the ileus; Abdominal x-rays show the
presence of gas in both the colon and in the small bowel
- a postoperative ileus may be caused by several factors, including drugs used for anesthesia
and analgesia, and intraoperative manipulation of intestinal loops and the mesentery — usually
temporary
- colonic obstruction is usually diagnosed by abdominal x-rays that show colonic dilation
proximal to the obstructing lesion
- acute gastroenteritis, acute appendicitis, and acute pancreatitis can mimic simple intestinal
obstruction, while acute mesenteric ischemia (AMI) must be considered in the differential of
small bowel strangulation
Page 236 of 269
Other classification - types of SBO, based on bowel viability
1) Simple obstruction: Nothing passes the point of obstruction, but the vascular supply is not
compromised. It may be partial and resolve with nonoperative management.
2) Strangulated obstruction: The mesentery is twisted or there is so much dilation of the bowel
that arterial or venous flow is cut off and the bowel becomes ischemic. Urgent surgery is
mandatory.
3) Closed loop obstruction: The bowel is obstructed proximally and distally, usually for a short
segment, and that segment becomes massively dilated and susceptible to strangulation and
perforation. Urgent surgery is mandatory.
=> Classic signs of strangulation: continuous pain (not colicky), fever, tachycardia, peritoneal
signs (localized guarding or tenderness, rebound tenderness), leukocytosis
Treatment
- SBO is associated with a marked depletion of liquids caused by decreased oral intake,
vomiting, and sequestration of fluid in the bowel lumen => Therefore, vigorous fluid
resuscitation and correction of electrolyte disorders (hypochloremic, hypokalemic metabolic
alkalosis) is mandatory
- A urinary catheter should be placed to monitor urinary output
- Gastrointestinal decompression with a nasogastric tube provides relief of symptoms, prevents
further gas and fluid accumulation proximally, and decreases the risk of aspiration
- Obstruction that occurs in the early postoperative period is usually partial and only rarely
associated with strangulation => prolonged period of total parenteral nutrition and hydration
- Treatment for a paralytic ileus starts by identifying the underlying cause
- As soon as resuscitation is complete, prompt surgical intervention is mandatory for complete
obstruction and for anyone with symptoms and signs of strangulation
What operative interventions may be needed for treatment of SBO?
- Open or laparoscopic lysis of adhesions at the point of obstruction
- Reduction and repair of hernia
- Resection of obstructing lesions with primary anastomosis
- Resection of strangulated segment with primary anastomosis
- Bypass of obstructing lesions (used mostly for carcinomatosis)
- Placement of long tube down through the duodenum and into the small bowel (a Baker tube is
the most commonly used)
Complications associated with surgery for SBO
- enterotomy
- prolonged ileus
- wound infection
- abscess
- recurrent obstruction
Products that decrease adhesion formation:
- Oxidized cellulose
- Sodium hyaluronate and carboxymethylcellulose
- Icodextrin
Complications
- Two of the most severe complications are necrosis and peritonitis
- Necrosis can happen when an obstruction cuts off blood supply to the intestine —> dead
tissue weakens the intestinal wall —> easier to tear and leak —> bowel perforation
- bowel perforation can cause peritonitis (e.g. by E. coli spilled from gut)
Page 237 of 269
Paralytic Ileus
- Caused by a failure of intestinal peristalsis, there is no evidence of mechanical obstruction
- common after abdominal surgery, especially when anticholinergic drugs are given
preoperatively and/or narcotics ae used postoperatively
- usually lasts 2 to 3 days
- paralytic ileus may also be caused by peritonitis;ischemia or surgical manipulation of the bowel;
retroperitonealhemorrhage; spinal fracture; systemic sepsis;shock; hypokalemia; uremia;
pharmacologic agents (eg,vincristine, loperamide, and calcium channel blockers);diabetic
ketoacidosis; and myxedema
Presentation
- typically presents with abdominal distention and minimal pain, which intensifies with increasing
distention
- Bowel sounds are generally minimal or absent <—> In contrast, mechanical obstructions are
associated with hyperactive bowel sounds
Diagnosis
- plain abdominal radiographs in patients with paralytic ileus demonstrate uniform distribution of
gas throughout the bowel, including the colon and rectum
- In contrast, mechanicalobstructions cause progressive bowel distention,with distended
proximal and collapsed distal segments
Treatment
- includes nasogastric suction
- i.v. fluid administration
- correction of electrolyte imbalance
Spastic ileus
- rare occurence
- spasm of the constrictor muscles of the small and/or large bowel in one (usually) or many
places
- common location is the lower portion of ileum
- several approaches to define the etiology:
• some contribute to local causes — irritation of the peritoneal or mucous surfaces, contusion
of external abdomen (Trendelenburg), or even severe muscular strain
• others prefer to assume that the sympathetic system or the vagus are the source of difficulty
• also some blame the CNS alone (hysteria, neurasthenia, tabes dorsalis, etc.)
• also seen in lead-poisoning and hernia
100. Acute abdomen.
-
Acute abdomen refers to a sudden, severe, abdominal pain
it is in many cases a medical emergency, requiring urgent and specific diagnosis
several causes need surgical treatment
acute abdominal pain is the commonest emergency presentation to hospitals in the UK
it is often a daunting challenge to the admitting team because of the huge differential diagnosis
possible
- for establishing diagnosis and treatment follow simple rules:
• take a proper history and examination
• resuscitate the patient properly and give adequate analgesia - often helps to clarify the
diagnosis
• try to clarify if you think the patient has signs of peritonitis (localized or generalized); this will
narrow the differential and may require surgery as part of the diagnostic work-up
- initial assessment should attempt to determine if the patient has an acute surgical
problem that requires immediate and prompt surgical intervention, or urgent medical therapy
- presentations requiring urgent surgery are bleeding, perforated viscus and ischaemic bowel
Page 238 of 269
Bleeding
- most serious cause of intra-abdominal bleeding is a ruptured aortic aneurysm
- other common causes usually involve a slower rate of bleeding, but with urgent surgery still
required, include ruptured ectopic pregnancy, bleeding gastric ulcer, and trauma
- These patients will typically go into hypovolemic shock
- Clinical features include tachycardia and hypotension, pale and clammy on inspection, and cool
to touch with a thread pulse
Perforated Viscus
- peritonitis is the inflammation of the peritoneum and a generalised peritonitis is most commonly
caused by perforation of an abnormal abdominla viscus
- the causes of perforation are broad but include peptic ulceration, small or large bowel
obstruction, diverticular disease and inflammatory bowel disease
- patients with a generalised peritonitis present with some characteristic features:
• patients often lay completely still, not to move their abdomen (important when compared to
a renal colic, whereby patients are constantly moving and cannot get comfortable)
• tachycardia and potential hypotension
• a completely rigid ‘washboard’ abdomen with percussion tenderness
• involuntary guarding — the patient involuntarily tenses their abdominal muscles when you
touch the abdomen
• reduced or absent bowel sounds — suggesting the presence of paralytic ileus
Ischaemic Bowel
- any patient who has severe pain out of proportion to the clinical signs has ischaemic bowel
until proven otherwise
- patient will often complain of a diffuse and constant pain, however the examination can often
otherwise be unremarkable
- definitive diagnosis is via a CT scan with IV contrast, with early surgical involvement
Causes
According to the abdominal region
Right hypochondriac
- right lower lobe pneumonia/
embolism
- cholecystitis
- biliary colic
- hepatitis
Epigastric
- pancreatitis
- gastritis
- peptic ulcer
- myocardial infarction
Left hypochondriac
- left lower lobe pneumonia/
embolism
- large bowel obstruction
Right lumber
- renal colic
- appendicitis
Umbilical
- intestinal obstruction
- intestinal ischaemia
- aortic aneurysm
- gastroenteritis
- Crohn’s disease
Left lumbar
- renal colic
- large bowel obstruction
Right iliac
- appendictis
- Crohn’s disease
- right tubo-overian pathology
Hypogastric
- cystitis
- urinary retention
- dysmenorhoea
- endometriosis
Left iliac
- sigmoid diverticulitis
- left tubo-overian pathology
Signs and symptoms
- constant pain, gradual in onset, but progressive worsening suggests an underlying
inflammatory cause
- Intermittent pain that is poorly localized suggests colic arising from a visceral structure
- Central and lower abdominal pain in children (under the age of 12) is self-limiting (non-specific)
in 70%, from benign gynaecological causes in 25% (girls), and only pathological in 10–20%
- Severe pain out of proportion to the clinical signs suggests ischaemic bowel until proven
otherwise
- Pain in the loin or back arises from (at least partially) retroperitoneal structures; consider the
pancreas, renal tract, and abdominal aorta
Page 239 of 269
Emergency management
Resuscitation
- Establish IV access
- Catheterize and place on a fluid balance chart only if hypotensive
- Give adequate analgesia; If renal pathology is suspected, diclofenac
(Voltarol®) 100mg pr is very effective (avoid in asthma and renal disease); If intra-abdominal
pathology is suspected, 5–10mg morphine iv is reasonable — Morphine IV never hides
established clinical signs; it often helps to clarify the diagnosis by its anxiolytic effect on
patients
- Send blood for FBC (Hb, WCC), U&E (Na, K), amylase, LFTs, CRP, group and save
Establish a diagnosis
- The time frame for the diagnosis of acute abdominal pain varies according to the presentation
- It is not uncommon for 12–24h of ‘masterful inactivity’ to be used to allow the diagnosis to be
clarified — Young patients with central and mild RIF pain are typical of this sort of management
- Some causes of acute abdominal pain require diagnosis and management immediately upon
admission or within 6–8h or less
- Blood investigations are very rarely diagnostic
- Serum amylase more than 3x normal maximum is very highly suggestive of acute pancreatitis
- Plain abdominal radiographs are very rarely diagnostic
- Always request a plain erect chest radiograph; it is the first-line test of choice for free
abdominal air
- Upper abdominal ultrasound is an excellent investigation for suspected hepatobiliary pathology
- Pelvic ultrasound (transabdominal or transvaginal) is a good test for suspected tubo-ovarian
disease
- CT scanning may well be indicated and is a good ‘general survey ‘ of the abdomen, but
exposes the patient to significant radiation and should not be routinely requested.
Early treatment
- IV antibiotics are inappropriate without a clear diagnosis; they will suppress, but may not
adequately treat, developing infection
- Until a definitive management plan is established, concentrate on fluid balance, analgesia, and
monitoring vital signs.
101. Mesenteric ischemia (acute mesenteric arterial occlusion; mesentric venous occlusion)
- = a medical condition in which injury of the small intestine occurs due to not enough blood
supply
- can start suddenly, known as acute mesenteric ischemia, or gradually, known as chronic
mesenteric ischemia
- acute disease often presents with sudden severe pain
- signs and symptoms of chronic disease include abdominal pain after eating, unintentional
weight loss, vomiting and being afraid of eating
- risk factors include: atrial fibrillation, heart failure, chronic renal failure, being prone to form
blood clots and previous MI; chronic diseases is a risk factor for acute disease
- there are four mechanisms by which poor blood flow occurs:
-
• a blood clot from elsewhere getting lodged in an artery
• a new blood clot forming in an artery
• a blood clot forming in the superior mesenteric vein
• insufficient blood flow due to low blood pressure or spasms of arteries
best method of diagnosis is angiography, or CT
treatment of acute ischaemia may include stenting or medications (e.g. heparin and warfarin) to
break down the clot at the site of obstruction
open surgery may also be used to remove or bypass the obstruction and may be required to
remove any intestines that may have died
if not rapidly treated, outcomes are often poor — even with treatment the risk of death is
70-90%
Page 240 of 269
Acute mesenteric ischemia
- AMI is a life-threatening clinical condition if not diagnosed promptly and treated adequately
(despite it, mortality remains high)
- results from four main processes:
1. arterial embolism (50%) most commonly in patients with previous myocardial infarction
of atrial fibrillation
2. acute arterial thrombosis (25%) in patients with diffuse atherosclerosis or less
frequently with connective tissue disorders
3. nonocclusive mesenteric ischemia (20%)
4. venous thrombosis (5%), associated with portal hypertension, abdominal sepsis,
hypercoagulable states or trauma
- the clinical consequences of acute arterial or venous mesenteric ischemia depend on several
factors, including the vessel involved, the level of occlusion, the development of collaterals, and
reperfusion
- Tissue injury caused by the ischemic event compromises the immune and barrier functions of
the small bowel, allowing bacterial translocation, cellular degradation, reactive oxygen species
formation in case of reperfusion and intravascular thrombosis
- The release of these products into the portal system and the systemic circulation initiates a
cascade of events leading to damage of targets organs such as the lungs and kidneys
Signs and symptoms
- nonspecific clinical presentation
- patients with arterial embolism initially present with sudden-onset diffuse abdominal pain that is
out of proportion to the clinical examination and often unresponsive to narcotics
- the lack of well-developed collaterals causes ischemia which eventually becomes transmural
- As ischemia worsens, patients develop nausea and vomiting, bloody diarrhea, and eventually
peritonitis
- Patients with acute thrombotic mesenteric occlusion also present with severe abdominal pain,
but it is usually chronic postprandial abdominal pain (intestinal angina) accompanied by weight
loss
- With cardiogenic or hypovolemic shock, blood is shunted away from the mesenteric circulation
and this process is exacerbated by the following local vasoconstriction
- Pain in patients with nonocclusive mesenteric ischemia is usually not as sudden as that with
embolic or thrombotic occlusion
- Patients with venous thrombosis commonly complain of nausea, vomiting, diarrhea, and nonlocalized abdominal pain
Laborartoy findings
- no lab tests diagnostic
- in most cases WBCC is elevated, as are lactic acid, amylase (50% of patients) and creatine
kinase levels (BB isoenzyme) correlate with intestinal infarction
- significant metabolic acidosis is usually present
Imaging studies
- abdominal radiographs are not diagnostic, but can reveal late signs consistent with bowel
ischemia, such as gas in the bowel wall or the portal venous system, and free air in the
peritoneum
- angiography is considered the gold standard for diagnosis for acute embolic and acute
thrombotic arterial mesenteric ischemia
- Angiography should include both AP and lateral views of the celiac artery, the SMA and the
inferior mesenteric artery; By selective injection of contrast into the SMA, emboli and thrombi
can be identified, whereas patients with nonocclusive mesenteric ischemia typically exhibit
evidence of SMA vasospasm
- CT or MRA (magnetic resonance angiography)
Page 241 of 269
Differential diagnosis
- acute pancreatitis
- intestinal obstruction
- aortic dissection
- cholecystitis
Treatment
- once diagnosis is made, fluid resuscitation, antibiotics, and anticoagulants or drugs that inhibit
platelet aggregation should be started
- the treatment consists of nonsurgical and surgical options depending on the underlying cause
- the goals of surgery are to restore blood flow when feasible and resect the segments of bowel
that are no longer viable
- because the appearance of ischemic bowel may improve dramatically after restoring blood
flow, the small bowel should be observed for at least 30 minutes after reperfusion before any
decision for resection is undertaken
- for acute SMA embolism, the standard treatment is a laparotomy and embolectomy, with a
catheter passed under direct vision into the arterial segment in order to dislodge and retrieve
the embolus
- surgical treatment of acute thrombotic mesenteric occlusion consists of an antegrade or
retrograde bypass because a simple thrombectomy usually leads to reocclusion,
Revascularization with saphenous vein or prosthetic graft (in the absence of peritonitis) is the
most common procedure
- in case of nonocclusive mesenteric ischemia, the treatment requires reversal of the underlying
causes of the hypoperfusion; local infusion of vasodilators using selective catheterization of the
SMA may also play a role
- treatment of mesenteric venous thrombosis is nonsurgical and relies on anticoagulation to
reverse the hypercoagulable state; Full anticoagulation with heparin is needed with careful
monitoring for gastrointestinal bleeding — Long-term oral or subcutaneous anticoagulation
therapy is then begun
- finally, econd-look laparotomy within 24-48 hours is a key point in the management of patients
with AMI who require extensive bowel resection during the first operation or have areas of
marginally viable bowel after revascularization
Prognosis
- prognosis of AMI is poor because diagnosis and treatment are often delayed, infarction is
extensive, and arterial reconstruction is difficult
- Perioperative mortality rates range from 32% to 69%, and 5-year survival ranges from 18% to
50%
- Mortality varies substantially according to the cause of AMI, being lower in cases of venous
thrombosis than in cases of arterial origin
- The only way to reduce the morbidity and mortality associated with this disease is early
diagnosis and treatment, before bowel necrosis develops
Page 242 of 269
102. Peritonitis: definition, causes, classification, symptoms, diagnosis and treatment.
Acute peritonitis = Acute inflammation in the peritoneal cavity
Causes
May be primary (rare) or secondary (common) (=classification)
- Primary peritonitis: Typically streptococcal with probable portal of entry via bloodstream
rather than intra-abdominal organs
- Commonest causes of secondary peritonitis are:
• Acute perforated appendicitis—commonest cause of peritonitis especially in under 45s)
• Acute perforated diverticular disease—commonest cause in elderly
• Upper GI perforation
• Perforated tumours (colonic or gastric)
• Perforated ischaemic bowel, e.g. due to adhesions
• Acute pancreatitis (usually inflammatory rather than infective)
• Peritoneal dialysis-related—often atypical or cutaneous organisms gaining entry via
contaminated dialysate bags or catheter
• Post-surgical intervention, e.g. anastomotic leak, enteric injury
Classification - more specific
1) According to the clinical course: acute and chronic
2) According to the route of penetration of bacteria into the peritoneal cavity
a. Primary peritonitis when the infection spreads by hematogenic or lymphogenic route or via
the fallopian tubes
b. Secondary peritonitis when the infection penetrates due to the acute surgical conditions or
the injury of the peritoneal organs
I. Infectious and inflammatory peritonitis results from the following:
• acute appendicitis
• acute cholecystitis
• acute ileus
• acute pancreatitis
• thromboembolia of the mesenterial blood vessels
• diverticulitis
• intestinal tumors
• gynecological conditions
II. Perforative peritonitis results from the perforation due to:
• duodenal and gastric ulcers
• intestinal, ulcerations associated with typhus, dysentry, tuberculosis, cancer,
stress etc.
• decubitus ulcer in the obturation ileus
• strangulation groove in strangulated intestinal obstruction in the foreign bodies of
GI tract
• intestinal necrosis in the strangulated hernia or thromboembolia of the mesentrial
blood vessels
III. Traumatic peritonitis develops in the open and closed abdominal traumas both with
accompanying damage of the abdominal organs and without such damage
IV. Postoperative peritonitis results from:
• the failure of the sutures of anastomosis after the abdominal surgery
• the infection of the peritoneal cavity in the course of surgery
• the defects of the ligatures applied to the large areas of the omentum and the
mesentry followed by the necrosis of the tissues distal to the ligature
3) According to the microbiological features (bacterial, aseptical - due to exposure to toxic and
enzymatic agents of non-infectious origin (blood, bile, gastric juice,…), carcinomatous,
parasitic, rheumatoid, granulomatous)
4) According to the character o the peritoneal exudate (serous, fibrinous, purulent, hemorrhagic)
5) According to the character of the lesions of the peritoneal surface
6) According to the phases of the development
Page 243 of 269
Clinical features - signs and symptoms
- There are features common to all causes
- Additional features suggestive of an underlying cause should also be sought, particularly in the
history
Symptoms
• Anorexia and fever
• Severe generalized abdominal pain radiating to shoulders and back
• Abdominal pain worse with movement, coughing, sneezing
Signs
• Fever, tachycardia
• Generalized abdominal tenderness with guarding and rigidity
• Differential maximal tenderness may indicate the possible underlying cause
• Gentle palpation may allow identification of an underlying mass
Diagnosis
- blood investigations may show neutrophilia, and increased CRP
- raised amylase may suggest pancreatitis
- abdominal CT scanning is the investigation of choice for diagnosis (it should reliably exclude
acute pancreatitis and often locate the probable source of the pathology)
Treatment
Preoperative Care
- the presentation of patients with peritoneal inflammation following bacterial contamination can
range from mild to life threatening
- it is necessary to approach each patient with the same goals of diagnosis and prompt
treatment in mind
- initial management consists of assessing the patient’s resuscitative needs and determining the
underlying pathology
- once resuscitation is begun, antibiotics administration and other supportive care measures
should be pursued followed by imaging and treatment considerations
- most causes of acute peritonitis require surgery to correct them, but surgery is contraindicated
in most cases of acute pancreatitis
Resuscitation
- establish large calibre IV access
- catheterize and place on a fluid balance chart
- send blood for FBC (Hb, WCC), Na, K, CRP, amylase
- ABGs if shocked or ischaemic bowel/pancreatitis suspected
Antibiotics
- should be administrated once diagnosis is made
- i.v. antibiotics are first line to ensure therapeutic serum levels in early course of treatment
- e.g. metronidazole 500mg IV tds + cefuroxime 750mg IV tds
Peritoneal lavage
- in diffuse peritoneal contamination, irrigation with copious amounts of warm isotonic crystalloid
solution removes gross particulate matter as well as blood and fibrin clots
- the addition of antiseptics or antibiotics to the irrigating solution is generally useless or even
harmful because of induced adhesions (eg, tetracycline, povidone-iodine)
- all fluid in the peritoneal cavity should be aspirated because it may hamper local defense
mechanisms by diluting opsonins and removing surfaces upon which phagocytes destroy
bacteria
Definitive management
- solve the underlying cause
Page 244 of 269
103. Hematogenic peritonitis.
Primary peritonitis??
General
- primary (spontaneous) peritonitis occuring in the absence of gastrointestinal perforation is
caused mainly by hematogenous spread but occassionally by transluminal or direct bacterial
invasion of the peritoneal cavity
- impairment of the hepatic reticuloendothelial system and compromised peripheral destruction
of bacteria by neutrophils promotes bacteremia, which readily infects ascitic fluid that has
reduced bacterium-killing capacity
- Primary peritonitis is most closely associated with cirrhosis and advanced liver disease with a
low ascitic fluid protein concentration
- It is also seen in patients with the nephrotic syndrome or systemic lupus erythematosus, or
after splenectomy during childhood
- Recurrence is common in cirrhosis and often proves fatal
Clinical Findings
- clinical presentation simulates secondary peritonitis with abrupt onset of fever, abdominal pain,
distention and rebound tenderness
- however one fourth of patients have minimal or no perineal symptoms
- most have clinical and biochemical manifestations of advanced cirrhosis or nephrosis
- Leukocytosis, hypoalbuminemia, and a prolonged prothrombin time are characteristic finding
- The diagnosis hinges upon examination of the ascitic fluid, which reveals a white blood cell
count greater than 500/μL and more than 25% polymorphonuclear leukocytes
- A blood-ascitic fluid albumin gradient greater than 1.1 g/dL, a raised serum lactic acid level, or
a reduced ascitic fluid pH (< 7.31) supports the diagnosis
- Bacteria are seen on Gram-stained smears in only 25% of cases
- Culture of ascitic fluid inoculated immediately into blood culture media at the bedside usually
reveals a single enteric organism, most commonly Escherichia coli, Klebsiella, or streptococci,
but Listeria monocytogenes has been reported in immunocompromised hosts
Treatment
- antibiotic prophylaxis is of no proven value
- systemic antibiotics with third-generation cephalosporins (eg, cefotaxime) or a β-lactamclavulanic acid combination along with supportive treatment are begun once the diagnosis has
been established
104. Congenital diseases of the colon. Hirschsprung’s disease.
Hirschsprung disease
- due to a failure in the cephalocaudal migration of the parasympathetic myenteric nerve cells
into the distal bowel => the abscence of ganglion cells always begins at the anus and extends
a varying distance proximally
- the aganglionic bowel produces functional obstruction because the bowel fails to relax in
response to distention
- Short-segment aganglionosis involving only the terminal rectum occurs in about 10% of cases;
the disease extends to the sigmoid colon in 75%; more proximal colon in 10%; and the entire
colon with small bowel involvement in 5%
- Extensive involvement of the small bowel is rare
- Males are affected four times more frequently than females when the disease is limited to the
rectosigmoid
Clinical findings
- There is failure to pass meconium within 24–48h, abdominal distension, and bile vomiting
- It may be associated with Down’s syndrome
- It may present late with poor weight gain, offensive diarrhoea, or enterocolitis
Page 245 of 269
Diagnosis and investigations
- Radiograph shows dilated colon to level of ‘transition zone’ to aganglionic bowel
- Contrast enema shows less distensible rectum and may indicate transition zone
- Suction rectal biopsy confirms diagnosis; thickened nerve fibres and aganglionisis (i AChE)
- Anorectal manometry (in older children) shows failure of anal relaxation on rectal balloon
distension (loss of recto-anal inhibitory reflex)
Treatment
- Resuscitation and analgesia
- Decompression of the colon with regular saline rectal wash-outs
- If decompression is not achieved or there is total colonic involvement, a defunctioning stoma is
necessary
- Definitive surgery is to remove the aganglionic bowel and bring normally innervated bowel to
the anus (pull-through technique— Soave, Swenson, or Duhamel types)
- It is usually performed as a one-stage procedure without a covering stoma
- The pull-through can be performed transanally or abdominally
- Laparoscopy assists in establishing a level and mobilizing the colon/rectum
Complications
- Constipation
- Enterocolitis can affect 20–50% of children pre- and post-operatively (uncommon >5y of age
unless an obstructive component exists)
Prognosis
- the mortality for untreated aganglionic megacolon in infancy may be as high as 80%
- nonbacterial, nonviral entercolitis is the principle cause of death
105. Congenital diseases of the rectum and anus.
Anorectal Anomalies — Imperforate anus
General
- the normal continence mechanism for bowel control consists of an internal sphincter
composed of smooth muscle and the striated muscle complex from the levator ani and external
sphincter
- the striated muscles assume a funnel shape, originating from the pubis, pelvic rim, and sacrum
=> These muscles converge at the perineum while interdigitating with the internal and external
sphincters
- Most of the striated muscle complex consists of horizontal muscles that contract against the
wall of the rectum and anus while longitudinal muscle fibers run in a cephalocaudal direction
and elevate the anus
- Anomalies of the anus result from abnormal growth and fusion of the embryonic anal hillocks;
The rectum is normally developed, and the sphincter mechanism is usually intact
=> With proper surgical treatment, the sphincter will function normally
- Anomalies of the rectum develop as a result of faulty division of the cloaca into the urogenital
sinus and rectum by the urorectal septum —> In these anomalies, the internal sphincter and
striated muscle complex are hypoplastic
=> surgical repair results in varying degrees of continence
Classification
- physical examination of the perineum and imaging studies determine the extent of
malformation of the anus or rectum
- When an orifice is evident at the perineum or distal introitus, the anomaly is referred to as a low
imperforate anus
- the absence of an obvious orifice at the perineal level suggests a high imperforate anus
- In most instances, with high imperforate anus, there is a communication (fistula) of the rectum
with the urethra or bladder in the male or with the upper vagina in the female
- Distinguishing between a high and low anomaly may be possible radiologically by determining
the position of the rectum in relation to the levator ani or pubococcygeal line
Page 246 of 269
Low Anomalies
- the anus may be ectopically placed anterior to its normal position or it may be in the normal
position with a narrow outlet due to stenosis or an anal membrane
- a small fistula usually extends from the anus anteriorly to open in the raphe of the perineum,
scrotum, or penis in the male or the vulva in the female
- These babies often have well-developed perineal and gluteal musculature and rarely have
sacral vertebral anomalies
High Anomalies
- the rectum may end blindly (10%), but more commonly there is a fistula to the urethra or
bladder in the male or the upper vagina in the female
- Patients with high imperforate anus often have deficient pelvic and gluteal innervation and
musculature, a high incidence of sacral anomalies (caudal regression), and a poor prognosis for
continence after surgical repair
- the most severe of the high deformities is a cloacal anomaly in which there is a common
channel between the poorly developed pelvic structures (urogenital sinus and rectum) with a
single perineal opening
Clinical Findings/Diagnosis
- best means of establishing the type of anorectal anomaly is by physical examination:
• in low anomalies, an ectopic opening from the rectum can be detected in the perineal raphe
in males or in the lower vagina, vestibule, or fourchette in females
• A high anomaly exists when no orifice or fistula can be seen upon examination of the
perineum or when meconium is found at the urethral meatus, in the urine, or in the upper
vagina
• Absence of external sphincter contraction with cutaneous stimulation of the anus may also
help differentiate between high and low lesions
- lower abdominal and perineal ultrasound, CT, and MRI have been used to define the pelvic
anatomy and location in relation to the rectal musculature
- Anomalies of the vertebrae and the urinary tract occur in two-thirds of all patients with high
anomalies and in one-third of male patients with low anomalies
Complications
- Delay of diagnosis of imperforate anus may result in excessively large bowel distention and
perforation
- The presence of a rectourinary fistula allows reflux of urine into the rectum and colon, and
absorption of ammonium chloride may cause acidosis
- Colon contents will reflux into the urethra, bladder, and upper tracts, producing recurrent
pyelonephritis
Treatment
- three main goals of treatment are (1) to allow passage of stool (ie, relieve obstruction), (2) to
place the rectal pouch on the perineum in good position, and (3) to close the fistula
- Low anomalies:
• usually repaired from the perineal approach in the newborn period using a muscle stimulator
to precisely determine the location of the sphincter complex
• The anteriorly placed anal opening is completely mobilized and transferred to the normal
position
• After healing, the anal opening must be dilated daily for 3-5 months to prevent stricture
formation and to allow for growth
- High anomalies:
• Traditionally, a high deformity was treated by a three-stage repair consisting of colostomy
and mucous fistula formation, a posterior sagittal anorectoplasty 4-6 weeks later, and
closure of the colostomy several months after that
• Recently, the staged approach has been challenged and a one-stage repair has been
performed by both posterior sagittal and laparoscopic approaches
• Because the anal sphincters are poorly developed—especially the internal sphincter—
continence is most dependent upon a functioning striated muscle complex, which requires
conscious voluntary contraction
• the surgically created anus must be dilated for several months to prevent circumferential
cicatrix formation
Page 247 of 269
Prognosis
- surgical complications include damage to the nervi erigentes, resulting in poor bladder and
bowel control and failure of erection
- division of a rectourethral fistula some distance from the urethra produces a blind pouch
prone to recurrent infection and stone formation, while cutting the fistula too short may
result in urethral stricture
- patients with imperforate anus tend to have varying degrees of constipation as an inherent
part of the defect, believed to be due to poor inherent motility of the rectosigmoid
- Patients with low anomalies usually have good sphincter function
- Children with high anomalies do not have an internal sphincter that provides continuous,
unconscious, and unfatiguing control against soiling
- in the absence of a lower spine anomaly, perception of rectal fullness, ability to distinguish
between flatus and stool, and conscious voluntary control of rectal discharge by
contraction of the striated muscle complex can be achieved
- when the stools become liquid, sphincter control is usually impaired in patients with high
anomalies
106.) Rectal hemorrhage
Causes of rectal bleeding
- Hemorrhoids (most common cause)
- Anal fissure
- Proctitis
- Anal fistula
- Cancer
- Ulceration/ infection
- Rectal prolapse/ rectal ulcer
- Inflammatory bowel disease
- Constipation or passing hard stools
- Polyps (they can bleed after passing stool)
General- Diagnosis
-
Bleeding is the most common presenting symptom in patients with anorectal disorders
While a careful history may suggest the etiology of bleeding, patients can tolerate and require a
thorough physical examination as well as anoscopy and lower endoscopy
Even if anorectal pathology is identified on physical examination or anoscopy, endoscopic
evaluation is always necessary in order to rule out proximal pathology such as polyps or cancer
In patients with anorectal bleeding, the history can help identify the source of the bleeding by
fully characterizing the amount, timing and location of the bleeding
Blood seen just on the toilet paper suggests anal canal pathology whereas blood seen mixed with
the stool suggests a more proximal bleeding source
Inspection of the anus may reveal prolapsing hemorrhoids, an anal fissure, an anal fistula, or anal
ulcer
Anoscopy is necessary to evaluate for possible internal hemorrhoids and distal proctitis
Flexible sigmoidoscopy is typically recommended for younger patients (< 40 years old) who do
not have a family history of colon cancer
Colonoscopy is recommended for patients over age 40 with anorectal bleeding or patients under
age 40 who have a family history of colon cancer
While these general guidelines are appropriate for most patients, the choice between flexible
sigmoidoscopy and colonoscopy is individualized to each patient’s clinical scenario
May also ask for CBC to determine if the patient has lost a significant amount of blood
Signs of rectal bleeding
-
Bright red blood indicates bleeding somewhere in the lower gastrointestinal tract, such as the
colon or rectum
Dark red or wine-colored blood may indicate bleeding in the small intestine or early portion of
the colon
Page 248 of 269
-
Black, tarry stools may indicate bleeding from the stomach or the upper part of the small
intestine
Additional symptoms associated with rectal bleeding include:
-
Confusion
Fainting
Feeling dizzy
Rectal pain
Abdominal pain or cramping
Management
-
-
Rectal bleeding treatments depend upon the cause and severity
Hemorrhoids
o You may relieve the pain and discomfort of hemorrhoids by taking warm baths
o Applying over-the-counter or prescription creams can also reduce irritation
o More invasive treatments if your hemorrhoid pain is severe or the hemorrhoids are very
large
o These include rubber band ligation, laser treatments, or surgical removal of the
hemorrhoid
Like hemorrhoids, anal fissures may resolve on their own
o Using stool softeners can address issues with constipation and help anal fissures to heal
Infections can require antibiotic therapy
Colon cancers may require more invasive and long-term treatments, such as surgery,
chemotherapy, and radiation to remove the cancer and reduce the risk of recurrence
Treatments to prevent constipation can reduce the risk of rectal bleeding. These include:
o eating high-fiber foods
o exercising regularly to prevent constipation
o keeping the rectal area clean
o staying well hydrated
107. Rectal cancer.
General
- Rectal cancer is the growth of abnormal cancerous cells in the lower part of the colon that
connects the anus to the large intestine
- Rectal cancer develops usually over years; its actual cause is not known, but risk factors
include increasing age (over 50), smoking, family history, high-fat diet, or a history of polyps or
colorectal cancer or inflammatory bowel disease
- Chemoprevention: beta-carotenes, antioxidants, Vit. C, Vit. E, calcium, NSAIDs, Aspirin
(120-140mg)
- The major symptom of rectal cancer is bleeding from the rectum; other symptoms include
anemia, fatigue, shortness of breath, dizziness and/or a fast heartbeat, bowel obstruction, small
diameter stools, and weight loss
- For diagnosis, exams and tests may include fecal occult blood testing, endoscopy, digital rectal
examination, sigmoidoscopy, CT/MRI imaging studies, along with routine blood tests and
detection of carcinoembryonic antigen (CEA)
- Medical treatment depends on the stage of rectal cancer (stages I-IV), with IV being the most
severe stage; multiple chemotherapy medications are available and are chosen by the specialist
(oncologist) to fit the individual's stage of rectal cancer; other specialists may need to be
consulted
- Surgery is used to both treat and reduce symptoms and, in some individuals, may result in a
remission of the cancer
- Radiation therapy is also used to kill or shrink rectal cancers
- Prevention involves detection and removal of precancerous growths
Etiology of rectum Ca
A. Obligate precancerous
• adematous polys
• villous tumor
• diffuse polyposis (FAP) and other polypous syndromes
Page 249 of 269
• chronic ulcerative colitis & Crohn disease
• non-epitheloid benign lesions
• carcinoids
B. Non-obligate precancerous
• colitis
• actinomycosis
• ulcerations
• paraproctitis, etc.
=> the frequency of malignant transformation of adenoma is different depending on 3 factors:
size, type of growth, degree of epithelial dysplasia
Forms of Rectal cancer
1. Hereditary
• familial anamnesis
• young age
• other tumors and defects
2. Sporadic
• older age (>60-80y.)
• one tumor
3. LYNCH syndrome
• genetic changes
• progression of benign polyps to invasive carcinoma
Pathoanatomy
Exofitous
- the cancer grows into the lumen of the intestine
- most commonly seen in the right half of the column
- there are three varieties: polypous (looks like polyp), papillomatous (looks like a cauliflower),
nodular (solid with uneven, ulcerating surface)
Endofitous
- cancer grows in the intestinal wall and narrows the lumen
- ulcerative: most common form; it represents an ulcer with raised edges like a shaft with rough
bottom
- diffuse-infiltrative (scirous): cancerous process infiltrate the intestinal wall, in the early stages
the mucosa may look normal
WHO classification of RC
1) Adenocarcinoma (97-98%)
• highly differentiated G1
• moderately differentiated G2
• low differentiation G3
• non-differentiated G4
2) Mucoepidermoid and coloid adenoCa
3) Annular-cell carcinoma
4) Non-differentiated (Ca. simpley, medullar, trabecullar)
Staging
T1 - tumor infiltrating submucosa
T2 - tumor infiltrating muscularis propria
T3 - tumor infiltrating subserosa or non-peritoneal pericolic/perirectal tissue
T4 - tumor perforates the visceral peritoneum or infiltrates neighbouring organs, e.g. vagina,
prostate, bladder, ureter, kidneys
N1 - 1-3 pericolic/perirectal infested lymph nodes
N2 - more than 4 lymph nodes are infested
Page 250 of 269
M1 - metastases
M1a - metastases only in one organ (liver, lung, ovar, non-regional lymph nodes)
M1b - metastases in several organs or in the peritoneum
Prognosis
- overall 5-y-rate is 50%
- fourth place in cancer deaths
Clinical signs and symptoms
- long time asymptomatic course
- later leading to functional disturbances: constiaption — diarrhea — change C/D
- pathological fecal ingredients: blood, mucus, pus
- tenesmus (feeling of unpropper empyting)
- rarely obturation ileus
- pelvic pain: in the late stages of disease in locally advanced process with infiltration of the pelvic
nerve’s branches or inflammation
Diagnosis
- Digital rectal examination (2/3 ae distal tumors)
- Proctoscopy
- Barium enema
- Colonoscopy
- CT/MRI
- Tumor markers: CEA, CA19-9, CA 125
Differential diagnosis
- ulcerative colitis/ Morbus Crohn
- Diverticulosis/Diverticulitis
- chronic anal fissure
- prolapsed rectum
- hemorrhoids
- polyps
Treatment
- the main treatment for cancer of the rectum is surgery
- adjuvant therapy assisting surgery includes chemotherapy, radiotherapy, immunotherapy
- if the tumor is in the upper or medial third: sphincter-/continence maintaining anterior rectal
resection
- if the tumor is in the lower third, we perform a abdominoperineal rectum extirpation with creating
a colostoma (Hartmann-operation)
- transanal local excision if cancer is detected early
- in advanced stages (II-III) neoadjuvant radio-/chemotherapy with the aim of possible operability
108. Prolapse of the rectum and anus.
Abnormal rectal fixation
- it is a general term for a group of diseases in which the attachment of the rectum to its
surrounding structures has developed more laxity, allowing the rectum to, completely or
incompletely, protrude through the anal canal
- exact pathophysiology is unknown but, in large part, this is related to chronic straining with
defecation
- common anatomic variations may include a patulous anus, redundant sigmoid colon, diastasis
of the levator ani muscles, and a deep cul-de-sac
- rectal prolapse is characterized by an intussusception of the rectum
Page 251 of 269
- there are three general categories that ultimately influence symptoms and overall management:
(1) internal prolapse (intussusception), which does not extend beyond the anal canal,
(2) mucosal prolapse, and (3) complete prolapse, which involves full-thickness protrusion of the
rectum through the anus
- In adults, older women are six times more likely to develop rectal prolapse, accounting for 80%
to 90% of the patient populations
- The peak incidence is after the fifth decade
Partial prolapse
- also called mucosal prolapse
- the lining (mucous membrane) of the rectum slides out of place and usually sticks out of the
anus
- this can happen when you strain to have a bowel movement
- partial prolapse is most common in children younger than 2 years
Complete prolapse
- the entire wall of the rectum slides out of place and usually sticks out of the anus
- at first, this may occur only during bowel movements
- eventually it may occur while standing or walking
- in some cases, the prolapsed tissue may remain outside at all time
Internal prolapse
- = intussusception
- one part of the wall of the colon or rectum may slide into or over another part, like foldin parts
of a telescope
- the rectum does not stick out of the anus
- most common in children, rarely affects adults
- in children the cause is usually not known
- in adults usually related to another intestinal problem, such as a growth of tissue in the wall of
the intestines (e.g. polyp or tumor)
Symptoms and Signs
- symptoms can vary with the degree of rectal prolapse, but typical complaints include a perianal
mass that protrudes with straining, mucoid or bloody discharge, incomplete evacuation,
incontinence, pain if the rectum becomes incarcerated
- digital rectal may reveal diminished or absent tone with complete prolapse but may suggest a
mass with straining for internal intussusception
- the diagnosis is most easily made with the patient straining in the seated position, which should
reproduce the rectal prolapse, identified by the concentric folds of mucosa
- in patients who also present with complaints of longstanding constipation, anorectal manometry, and colon transit studies are also crucial
- prior to any surgical intervention, these patients should also undergo colonoscopy.
Differential Diagnosis
- complete rectal prolapse is often confused with prolapsing internal hemorrhoids; however, the
two can easily be separated by close examination of the mucosa
- prolapsing internal hemorrhoids produce radials folds in the visible rectal mucosa, which
contrasts with the concentric folds seen with rectal prolapse
Complications
- the most dreaded complication for rectal prolapse is incarceration, which may lead to tissue
ischemia and necrosis
- chronic reducible rectal prolapse may also impair fecal continence due to the repeated
stretching of the sphincter muscles
Treatment
Medical Treatment
- a trial of fiber supplementation and diet modification may prove to be beneficial for mild cases
of internal intussusception
Page 252 of 269
Surgical Treatment
- indicated in patients with full-thickness rectal prolapse
- surgical treatment is broadly divided into abdominal and perineal approaches, which are
dictated by the patient’s age and comorbidities as well as surgeon preference and experience
- perineal approaches generally results in reduced length of hospital stay and less perioperative
morbidity and pain; however, they are plagued by higher recurrence rates
- rectopexy, resection rectopexy, and mesh rectopexy are the three abdominal procedures that
are most widely practiced
- the principle component of each of these procedures is the posterior mobilization of the rectum
down to the level of the levator muscles —> the rectum is elevated from the deep pelvis and
sutured to the presacral fascia at the level of the sacral promontory
- the lateral ligaments are preserved, as this has been shown to decrease postoperative
constipation
- Complications include bowel obstruction, erosion of the mesh, and fistulas
109. Acute and chronical paraproctitis. Dermoid cyst (pilonidal cyst).
Paraproctitis
Definition = purulent-inflammatory processes of adipose tissue around the rectum
- most frequent cause is penetration of bacterial flora from the rectum into the surrounding
cellular tissues, which may occur through an anal fissure
- the inflammation is sometimes limited to the formation of an abscess, and in some cases it
spreads for a considerable distance and may be complicated by sepsis
- the symptoms are acute pain in the rectal region, tenderness during defecation, elevated body
temperature and the appearance of an infiltrate in the anal region or on the buttocks
- an unlanced abscess may burst and a fistula form
- the disease becomes chronic after recurrences
- treatment includes administration of antibiotics and anti-inflammatory agents; and in the
suppurative stage surgical lancing of the abscess
Classification
1. According to the type of agent:
• specific - lues, tuberculosis, actinomycosis
• non-specific - general bacteria (gram +/-, anaerobic)
2. According to the course:
• acute paraproctitis - in the first stage
• chronic paraproctitis - perianal fistule
Nonspecific paraproctitis
- pelvio-rectal abscess — abvove diaphragma pelvis
- ischio-rectal abscess — below diaphragma pelvis
- perianal abscess — inflammation around the anus and rectum and covered by subcutaneous or
submucosal tissue
Superficial perianal abscesses — 60%
- subcutaneous — from infected hemorrhoidal nodes
• Clinic: fever around 38°C, chills, severe pain during bowel movements, swelling around the
edge of the anus, painful pulsating character
• Subcutaneous can pass in the submucous => subcutaneous - mucous abscess: absent
external events, high body temperature, tightening of m. sphinter ani externi —> pulling the
anal edge inside
• Treatment: operation under general anesthesia - anal dilatation with subsequent skin; mucosal
incision, antibiotics
Extrasphincter perianal abscesses
- an ischio-rectal abscess infection passes from subcutaneous and/or submucosal tissue to
cavum ischiorectal through lymphatic way
Page 253 of 269
- Clinic: acute onset of fever to 39-40°C with chills, pain and deterioration of general condition of
-
the patient, difficulty in urinating
objectively — swelling in the anal half; hyperemia of the overlying skin
when the abscess passes to the opposite site — „horseshoe“ abscess
in a spontaneous perforation — extrasphincteric complete fistula
in a breakthrough towards the lumen — incomplete internal fistula
Treatment: arch-shape incision, lavage, wide drainage, antibiotics
Pelvio-rectal abscesses
- the infection goes through the lymph path of proctitis, fissures or rectal ulceration
- Clinic: general symptoms prevail over local
- acute onset with chills and temperature up to 40°C, severe pain
- septic general condition
- Diagnosis: digital examination shows painful infiltrate, CT, MRI
- in case of perforation to:
• rectum - incomplete internal fistula
• peritoneum - peritonitis
Chronic paraproctitis - anorectal fistula
- Definition: abnormal connection between the anal canal or rectum with the outer skin or internal
organs
- 1-5% of all surgical patients; more common in men
Etiology of paraproctitis - with acute abscess
- Crohn’s disease
- Ulcerative colitis
- TBC
- Carcinoma
- HIV
Pathologic classification of fistulas
1. Superficial and deep
2. Regarding the sphintcer
• intersphincteric (consequence of ano-rectal subcutaneous and submucosal abscesses;
channel is simple or V or Y-shape)
• transsphincteric (low and high)
• extrasphincteric (inner hole of the external fistula lies always above the sphincters; external
opening more than 2cm away from anus)
3. Regarding the fistula canal
• full - with two holes (skin and intraluminal)
• incomplete - one hole (blind fistula)
4. In respect to the clinic
• simple
• complex (in the shape of a „horseshoe“; several skin holes and passages)
• complicated
5. Regarding the etiology
• acquired
• congenital
• traumatic
• symptomatic
Clinical features of fistulas
- „wetting“
- perianal itching
- excretion of gas and feces through outher hole (for complex fistulas)
Diagnosis
- determining the location of the fistula tract towards the external anal sphincter
- detecting and determining the nature of the openings of the fistula
- establishing the nature of fistulas — simple, complex and complicated
Page 254 of 269
-
fistulography, methylene blue
rectoscopy
MRI
ultrasound
Treatment - surgical
- excision
- ligature method of Hippocrates
- laser scalpel
- anal fistula plug
- mucosal advancement flap
- LIFT (ligation of intersphincteric fistula tract)
Dermoid cysts/ pilonidal sinus
- Def.: cystic formations covered with different epithelia (flat, multilayer, cuboidal)
- contents: dirt, fat, hair and connective tissue
- located in pre-sacral area/retrosacral area
- Diagnosis: fistulography
- Treatment: exiscion and extirpation of teh cyst and fistula opening
Pilonidal sinus = a small hole or tunnel in the skin
- it may be filled with fluid or pus, causing the formation of a cyst or abscess
- it occurs in the cleft at the top of the buttocks
- usually contain hair, dirt and debris
- it can cause severe pain and often become infected
- if it becomes infected, it may ooze pus and blood and have a foul odor
Dermoid cyst = an abnormal saclike growth (teratoma) containing epidermis, hair follicles and
sebaceous glands, derived from residual embryonic cells; present at birth
110. Perianal fistulas.
Anatomy
- defined as a communication of an abscess cavity with an identifiable internal opening within the
anal canal
- most commonly located at the dentate line where the anal glands enter the anal canal
- Patients experiencing continuous drainage following the treatment of a perianal abscess likely
have a fistula in ano
- fistulas are classified by their relationship to the anal sphincter muscles:
1. Intersphincteric (70%)
2. Transsphincteric (23%)
3. Suprasphincteric (5%)
4. Extrasphincteric (2%)
Incidence
- parallels the incidence of anorectal absces
- estimated to be 1 in 10000 individuals
- Some 30-40% of abscesses will give rise to fistula in ano
- Although the majority of the fistulas are cryptoglandular in origin, 10% are associated with IBD,
tuberculosis, malignancy, and radiation
Symptoms
- constant drainage from the perianal region associated with a firm mass
- => may increase with defecation
- Perianal hygiene is difficult to maintain
Diagnosis
- Examination under anesthesia is the best way to evaluate a fistula
- At the time of the examination, anoscopy is performed to look for an internal opening
- Diluted hydrogen peroxide will aid in identifying such an opening
- An MRI with an endoanal coil will also identify thits in 80% of the cases
Page 255 of 269
- After drainage of an abscess with insertion of a Mallenkot catheter, a fistulagram through the
catheter can be obtained in search of an occult fistula tract
- Goodsall's rule states that a posterior external stula will enter the anal canal in the posterior
midline, whereas an anterior fistula will enter at the nearest crypt
- A fistula exiting >3 cm from the anal verge may have a complicated upward extension and may
not obey Goodsall's rule
Treatment
- A newly diagnosed draining fistula is best managed with placement of a seton, a vessel loop or
silk tie placed through the fistula tract
- => maintains the tract open and quiets down the surrounding inflammation that occurs from
repeated blockage of the tract
- Once the inflammation is subdued, the exact relationship of the fistula tract to the anal
sphincters can be ascertained
- A simple fistulotomy can be performed for intersphincteric and low (less than one-third of the
muscle) transsphincteric fistulas without compromising continence
- For a higher transsphincteric fistula, an anorectal advancement flap in combination with a
drainage catheter or fibrin glue may be used
- Very long (>2 cm) and narrow tracts respond better to fibrin glue than shorter tracts.
- simple ligation of the internal fistula tract (LlFT procedure) has also been used in the
management of simple fistula with good success
- Patients should be maintained on stool-bulking agents, nonnarcotic pain medication and sitz
baths following surgery for a fistula
Complications
- Early complications from these procedures include urinary retention and bleeding
- Later complications are rare (<1 0%) and include tem porary and permanent incontinence.
- Recurrence is 0-1 8% following fistulotomy and 20-30% following anorectal advancement flap
and the LlFT procedure
111. Hemorrhoids.
Definition = varicose changes in the haemorrhoidal plexus in the ano-rectal area
Anatomy
- Hemorrhoidal cushions are a normal part of the anal canal
- The vascular structures in these cushions aid in continence by preventing damage to the
sphincter muscle
- The three main hemorrhoidal complexes traverse the anal canal (left lateral, right anterior, right
posterior)
- Engorgement and straining lead to prolapse of the tissue into the anal canal
- Over time, the anatomical support of the hemorrhoidal complex weakens => exposing the
tissue outside the anal canal
- The standard classification of hemorrhoidal disease is based on the progression of the disease
from their normal internal location to the prolapsing external position
1. External hemorrhoids
- originate below the dentate line
- covered with squamous epithelium
- associated with an internal component
- painful when thrombosed
2. Internal hemorrhoids
- originate above the dentate line
- covered with mucosa and transitional zone epithelium
- represent the majority of hemorrholids
Page 256 of 269
General
- abnormal swelling of vascular cushions (hyperplasia) due to prolapse of upper anal / lower
rectal tissue within/out of anal canal
- similar in both genders, peak 45-65 years of age
- Risk factors: chronic straining, constipation, low-fiber, high fat diet
- Pathogenesis: weakening of the supporting tissues with slippage of cushions
- there are two types: primary (idiopathic) and secondary (symptomatic)
- Symptoms of hemorrhoids: bleeding, discomfort, itching, prolapse, swelling, pain, secretion
- (Etiology: hereditary, anatomical features, meal, profession, sedentary lifestyle, climate,
physiological problems (senility, endochrine changes), medicaments, infections, pregnancy,
exercise (exertion, cough, vomiting), tight clothes, constipation)
- Essentials of treatment:
• all grades: high fiber diet, increased water intake
• Grades I-III: rubber band ligation, sclerotherapy, and infrared coagulation
• Grades II-IV: stapled hemorrhoidopexy or hemorrhoidectomy
Classification
- Grade I hemorrhoids - the veins in the anal canal are increased in size and number and may
bleed during defecation; hemorrhoidal nodes are not prolapsed
- Grade II hemorrhoids - prolapsed internal hemorrhoids during defecation but sponatneously
fold back
- Grade III hemorrhoids - internal hemorrhoids during bowel movements and physical effort are
prolapsed and remain constantly outside; the manual reposition is ineffective
Classification according to WHO
- I - bleed but not prolapsed and palpated
- II - prolapse and reposition - spontaneously with/without bleeding
- III - prolapsed which require the reposition by the patient
- IV - permanent prolapse with frequent complications
Stages according to clinical course
- acute stage
- chronic stage
- stage of hemorrhoidal nodes
Pathogenesis
- anatomical studies revealed that maintenance and supporative tissue degenerates with age,
especially after the third decade (venous distension, erosion, bleeding and thrombosis)
- there are several theories of pathogenesis:
• abnormal dilatation of the internal hemorrhoidal venous plexus
• abnormal dilatation of the arteriovenous anastomoses
• prolapse of the „anal cushions“
• destruction of the connective tissue supportive system
• reverse venous blood flow in a transient increase of the abdominal pressure
• vascular congestion is the result of a defect in the venous drainage
Clinical features
- pain after defecation
- bleeding (alcohol - wine-tannin) - scarlet red blood (bright red is suggestive for hemorrhoids!)
=> may lead to secondary anemia
- prolapse of hemorrhoidal nodes
- general phenomena - headache, insomnia, poor general condition
Complication - necrotizing
- severe pain
- acute intoxication
- high temperature - up to 38°C
- chills
- headache
- general weakness
Page 257 of 269
Local complications
- anal fissures
- haemorrhages
- anal pruritus
- proctitis
- anorectal abscess
- ano-rectal fistula
- insufficiency of the anal sphincter - incontinence
Diagnosis
- history
- inspection
- palpation
- digital examination
- anoscopy
- sigmoidoscopy
Differential diagnosis
- cancer of the anus or rectum
- benign tumors of the anus and rectum
- dermal papillae
- rectal prolapse
- hypertrophy of the anal papillae
- chronic fissure
- condylomata acuminata
- condylomata lata
- specific infections - tuberculosis, syphilis, actinomycosis
- veneral diseases
Treatment
Conservative
- diet
- hygiene regime
- regulation of defecation - avoid constipation (stool softeners)
- sit baths
Medical
- lioton 1000 gel
- Detralex
- sclerotherapy
- ligation with a rubber ring (Blaisdel and Barron - Rubber Band Ligation)
- Additional therapy for bleeding hemorrhoids includes the on ice procedures of banding and
sclerotherapy
- Bands are placed around the engorged tissue, causing ischemia and fibrosis
- Aids in fixing the tissue proximally in the anal canal
- Patients may complain of a dull ache for 24 hours following band application
- During sclerotherapy, 1-2 ml of a scleroserant is injected using a 25-gauge needle into
the submuscosa of the hemorrhoidal complex
- Do not inject into the anal canal circumferentially or stenosis may occur
Surgical - Indications
- refractory to conservative treatment
- third degree haemorrhoids
- hemorrhages leading to anemic syndrome
- prolapse of hemorrhodial nodes
- thrombosis hemorrhoidal nodes
- hemorrhoids are often inflamed with edema and pain syndrome
- abundant secretion of mucus and anal pruritus
Page 258 of 269
Contraindications to surgical treatment
- pregnancy
- cirrhosis
- ascites
- tumors in the pelvis
Surgery techniques
- Surgery is the definitive treatment and can be done by standard hemorrhoidectomy or by
stapled hemorrhoidopexy
- both techniques can be used for second- and third-degree hemorrhoids
- Hemorrhoidectomy is a better option for grade IV hemorrhoids, when there is an external
component or other condition that requires surgery such as fissure or fistula
112.) Plastic surgery
General
-
Plastic surgery is used to repair and reconstruct missing or damaged tissue and skin
The main aim of plastic surgery is to restore the function of tissues and skin to as close to normal
as possible
Improving the appearance of body parts is an important, but secondary, aim
Plastic surgery is different from cosmetic surgery, which is surgery carried out solely to change a
healthy person's appearance to achieve what they feel is a more desirable look
Plastic surgery can often help improve a person's self-esteem, confidence and overall quality of
life
Plastic surgery can be used to repair:
-
abnormalities that have existed from birth, such as a cleft lip and palate, webbed
fingers, and birthmarks
areas damaged by the removal of cancerous tissue, such as from the face or breast
extensive burns or other serious injuries
Plastic surgery techniques:
-
skin grafts – where healthy skin from an unaffected area of the body is removed and used to
replace lost or damaged skin
skin flap surgery – where a piece of tissue from one part of the body is transferred to another,
along with the blood vessels that keep it alive; it's called flap surgery because the healthy tissue
usually remains partially attached to the body while it's repositioned
tissue expansion – where surrounding tissue is stretched to enable the body to "grow" extra
skin, which can then be used to help reconstruct the nearby area
As well as these techniques, plastic surgeons also use many other methods, such as:
-
fat transfer or grafting – where fat is removed from one area and inserted in another area,
usually to correct unevenness
vacuum closure – where suction is applied to a wound through a sterile piece of foam to draw
out fluid and encourage healing
prosthetic devices, such as artificial limbs
Risk of plastic surgery
-
The degree of risk depends on the size of the affected area, the surgeon's level of experience, and
the overall health of the person having the procedure
Some procedures carry specific risks, but general risks include:
o pain and discomfort
o bleeding
o infection
o scarring
Page 259 of 269
Skin grafts
-
-
-
They can be used for bone fractures that break the skin (open fractures), large wounds, or where
an area of the skin is surgically removed – for example, due to cancer or burns
Partial or split thickness skin graft
o This is where a thin layer of skin (as thin as tissue paper) is shaved from an area that
usually heals well, such as the thigh, buttocks or calf
o The donor area usually takes 2 to 3 weeks to heal and is pink for a few months before
fading to leave a faint (hardly noticeable) scar
Full thickness skin graft
o This is where the full thickness of skin (the top layer and layers underneath) are
removed and the area is directly closed
o Sites often used include the neck, behind the ear, the upper arm and groin
o Because this type of skin graft is thicker, picking up a new blood supply can be more
difficult, so any dressing will be left in place for 5 to 7 days before being removed by the
surgical team
At first, the grafted area will appear reddish-purple, but it should fade over time. It can take a
year or two for the appearance of the skin to settle down completely
The final colour may be slightly different from the surrounding skin, and the area may be
slightly indented
Tissue expansion
-
Tissue expansion is a procedure that encourages the body to "grow" extra skin by stretching
surrounding tissue. This extra skin can then be used to help reconstruct the nearby area
Examples of when tissue expansion may be used include breast reconstruction and
repairing large wounds
Under general anaesthetic, a balloon-like device called an expander is inserted under the skin
near the area to be repaired
This is gradually filled with salt water, causing the skin to stretch and grow
The time it takes for the tissue to be expanded can vary, depending on the size of the area to be
repaired
If a large area of skin is affected, it can take as long as 3 or 4 months for the skin to grow
enough. During this time, the expander will create a bulge in the skin
Once the skin has expanded sufficiently, a second operation is needed to remove the expander
and reposition the new tissue
This technique ensures that the repaired area of skin has a similar colour and texture to the
surrounding area
There's also a lower chance of the repair failing because the blood supply to the skin remains
connected
Flap surgery
-
Flap surgery involves the transfer of a living piece of tissue from one part of the body to another,
along with the blood vessels that keep it alive
It may be used for a variety of reasons, including breast reconstruction, open fractures, large
wounds, and, in rare cases, for improving a cleft lip and palate
In most cases, the skin remains partially attached to the body, creating a "flap". The flap is then
repositioned and stitched over the damaged area
For more complex reconstruction, a technique called a free flap is used
This is where a piece of skin, and the blood vessels supplying it, are entirely disconnected from
the original blood supply and then reconnected at a new site
A technique called microsurgery (surgery using a microscope) is used to connect the tiny blood
vessels at the new site
A free flap is often used when large areas of specific tissue types are needed for reconstruction
Depending on the location and size of the flap, the operation can be carried out under general or
local anaesthetic
As flap surgery allows the blood supply to the repaired area to be maintained, there's a lower risk
of the repair failing compared with a skin graft
Page 260 of 269
113. The basics of laparoscopic and minimally invasive surgery.
Non-robotic minimally invasive surgery (endoscopic)
- includes terms like laparoscopic, thoracoscopic or „keyhole“ surgery
- these are minimally invasive procedures that utilize an endoscope to reach internal organs
through very small incisions
- during endoscopic surgery the surgeon inserts a thin, flexible tube with a video camera through
a small incision or a natural orifice like the mouth or nostrils
- the tube has a channel to utilize tiny surgical instruments, which the surgeon uses while viewing
the organs on a computer monitor
- this technique allows the surgeon to see inside the patient’s body and operate through a much
smaller incision than would otherwise be required of traditional open surgery
Benefits
- Small incisions, few incisions, or no incision
- Less pain
- Low risk of infection
- Short hospital stay
- Quick recovery time
- Less scarring
- Reduced blood loss
Examples for conditions treated by non-robotic minimally invasive surgery
- General — Pancreatic cancer, benign pancreatic lesions, hernias, severe gastroesophageal
reflux disease (GERD), liver tumors (benign and malignant), gallbladder cancer, obesity (gastric
bypass, bariatric surgery, gastric banding), gastrointestinal/rectal conditions, hernias
(paraesophageal, ventral, hiatal or incisional)
- Lung – Some lung tumors, esophageal cancer and diseases
- Gynecologic – Gynecologic cancer, benign tumors, endometriosis, uterine fibroids, ovarian
cysts, benign cervical disorders, conditions requiring hysterectomy, removal of ovaries and
staging of lymph nodes
- Head and neck – Skull base brain tumors, anterior cranial fossa (front skull base) tumors,
posterior cranial fossa (back of the skull base) tumors
- Heart – Atrial septal defects, aortic regurgitation, aortic insufficiency, aortic stenosis, mitral
valve repair
- Neurosurgery/Spine – Spine conditions, cervical disc hernias, lumbar disc hernias,
degenerative disc disease, spinal trauma: skull base brain tumors, anterior cranial fossa (front
skull base) tumors, posterior cranial fossa (back of the skull base) tumors
- Vascular – varicose veins, venous insufficiency, peripheral vascular disease
- Urological – Kidney disorders, kidney cysts, kidney stones, kidney blockage, kidney donation,
prostate cancer, incontinence, vaginal prolapse
Robotic surgery
- advanced robotic systems give doctors greater control and vision during surgery, allowing them
to perform safe, less invasive, and precise surgical procedures
- during robotic-assisted surgery, surgeons operate from a console equipped with two master
controllers that maneuver four robotic arms
- By viewing a high-definition 3-D image on the console, the surgeon is able to see the surgical
procedure better than ever before
- Computer software takes the place of actual hand movements and can make movements very
precise
How is minimally invasive surgery performed?
- several different techniques with the goal to decrease pain and speed recovery by eliminating
the need for a large abdominal incision
- All minimally invasive surgeries are performed with the patient asleep under a general
anesthetic
Page 261 of 269
- Laparoscopic surgery refers to a technique where the surgeon makes several small incisions
about ½” in size, instead of a single large incision
- For most colon and rectal operations, 3-5 incisions are needed
- Small tubes, called “trocars,” are placed through these incisions and into the abdomen
- Carbon dioxide gas is used to inflate the abdomen in order to give the surgeon room to work
—> This allows the surgeon to use a camera attached to a thin metal telescope (called a
laparoscope) to watch a magnified view of the inside the abdomen on operating room monitors
- Special instruments have been developed for the surgeon to pass through the trocars to take
the place of the surgeon’s hands and traditional surgical instruments
- Surgical stapling devices to divide and reconnect intestine as well as energy devices to cut and
cauterize tissues and blood vessels have also been adapted for laparoscopic use
- For most operations, one slightly larger incision (about 2-4 inches in length) must be made in
order to remove tissue (sometimes called a “specimen”) from the abdomen
- “Laparoscopic-assisted surgery” is used to describe a procedure that is performed largely
laparoscopically and then completed through a small abdominal incision
- Strictly speaking, many “laparoscopic” procedures are actually laparoscopic-assisted because
some part of the operation may be performed through the specimen-removal incision
- “Hand-assisted laparoscopic surgery” refers to another variation of laparoscopic surgery in
-
which a device is placed in a small (2-3 inch) incision that allows the surgeon to pass a hand
into the abdomen to assist in performing the operation
The surgeon still uses the laparoscope to view the operation on monitors and uses the same
instruments, staplers and energy devices as in traditional laparoscopic surgery
The specimen is removed through the device used by the surgeon to place a hand in the
abdomen
The main advantage of this procedure is that the ability to use the surgeon’s hand may be very
helpful in performing the operation
The disadvantage is that the incision required might be slightly larger than would otherwise be
necessary
- “Single incision surgery” or “single site surgery” is another minimally invasive option
- With this technique, both the laparoscopic camera and the operating instruments are passed
through a single, small incision (about 2 inches in length) that can also be used to remove the
specimen
- The primary advantage of this technique is less visible scarring since no additional small trocar
incisions are necessary
- The disadvantage is that most surgeons find this technique more difficult than traditional
laparoscopic surgery because the instruments are placed so closely together
- “Robotic surgery” or “robotic-assisted surgery” is a newer variation on minimally invasive
colon and rectal surgery
- The technique is very similar to standard laparoscopic surgery in that instruments are passed
into the abdomen through trocars
- Rather than manipulate the instruments manually, the surgeon sits at a console, or special
computer desk, and manipulates small controllers while observing the inside of the abdomen
with a 3-D monitor
- A sophisticated computer system translates the movements of the surgeon’s hands to the
robot, which then moves the surgical instruments
- Because the robot is only capable of working in a relatively small part of the abdomen at a time
and is difficult to reposition, it is often used for only a portion of an operation
- The remainder of the operation is usually performed laparoscopically
Page 262 of 269
114. The basics and principles of surgical oncology.
- Surgery is used to diagnose, stage and treat cancer, and certain cancer-related symptoms
- Surgery is the oldest form of cancer treatment, and for most patients, part of the curative plan
includes surgery
- whether a patient is a candidate for surgery depends on factors such as the type, size, location,
-
grade and stage of the tumor, as well as general health factors such as age, physical fitness
and other medical comorbidities
For many patients, surgery will be combined with other cancer treatments such as
chemotherapy, radiation therapy or hormone therapy => These may be administered before
surgery (neoadjuvant) or after surgery (adjuvant) to help prevent cancer growth, spread or
recurrence
the goals of the surgical oncologist are to remove the cancer and an area of healthy tissue
surrounding it, also known as a clear margin or clear excision, in order to prevent the cancer
from recurring in that area (local recurrence)
Sometimes it is not possible to remove the whole tumor, and a surgery known as "debulking"
may be done to remove as much of the tumor as possible and to relieve symptoms such as
pain, airway obstruction, or bleeding
Excision of lymph nodes in the area of the tumor may be done at the time of surgery,
depending on the type of cancer —> The information regarding lymph node status (i.e. do they
contain cancer cells or not?) can help determine prognosis as well as further treatment options
Sometimes, after removal of the tumor, there is a defect left behind that could be physically
devastating or impact on function —> To remedy this, reconstructive techniques are
increasingly being used for certain cancers and are important because of the impact on the
patient's quality of life
Reconstruction can take place at the same time that the cancer is removed, ("immediate
reconstruction"), or weeks to months later, "delayed reconstruction"
115.) Non-surgical postoperative complications. Compartment syndrome
Compartment syndrome
Etiology
-
is caused by increased pressure in a closed fascial space that initially leads to compromised
perfusion followed by severe tissue damage
Nerves and muscles in the affected area can be significantly compromised in a matter of hours
Severe ischemia for 6-8 hours leads to muscle and nerve death leading to chronic debilitating
dysfunction of the affected extremity
As a result, compartment syndrome is an orthopedic emergency requiring immediate evaluation
and treatment
Compartment syndrome can occur after fracture, limb compression or crush, vigorous exercise,
or burns
Clinical Features
-
-
It most commonly occurs in the forearm and leg, it can occur in the foot, thigh, and arm
Typically presents as a painful, swollen, tense extremity
Pain with passive range of motion of the digits and pain out of proportion are considered to be
the most reliable early indicators of compartment syndrome
Clinical signs include the 5 P:
o pain,
o poikilothermia,
o pallor,
o paresthesias
o Pulselessness
A change in pulses is a very late sign occurring after significant damage has already occurred
Of note, compartment syndrome can occur at intracompartmental pressures well below arterial
pressure. Therefore, compartment syndrome can occur in a pink limb with normal pulses
Page 263 of 269
Diagnosis
Treatment
-
Many authors advocate that if compartment syndrome is suspected immediate fasciotomy should
be carried out
In scenarios where patients are obtunded, intubated, or otherwise unable to express having pain,
compartment pressure can be evaluated using a commercially available self-contained pressure
monitor
If a commercial pressure monitor is not available, large bore catheter can be inserted in the
compartment under sterile technique
The catheter is connected to a pressure monitor via intravenous tubing filled with sterile saline
solution
Absolute pressure more than 30 mm Hg in any compartment, or a pressure within 30 mm Hg of
the diastolic blood pressure in hypotensive patients are indications for surgical compartment
release
Fasciotomy should be carried out with complete release of the skin and fascia of the involved
compartments
Adjacent compartments in the same limb are typically released as well
Compartment pressures are rechecked after release to ensure adequate decompression
The wounds are left open and covered with sterile dressings or a vacuum-assisted closure (VAC),
and are subsequently treated with delayed primary closure or skin grafting days later
Abdominal Compartment Syndrome
-
Aggressive resuscitation of patients, particularly those involved in trauma or requiring an
emergent celiotomy, may result in increased abdominal pressure
Intra-abdominal hypertension, as measured by bladder pressure, is generally self-limiting;
however, it can become dangerous when pressures exceed 30 mm Hg
In this scenario venous outflow from the bowel and kidney may become compromised
Furthermore, respiratory complications may ensue as the pressure exerted upon the diaphragm
may decrease tidal volume and result in respiratory acidosis
In this situation, the abdominal compartment must be rapidly decompressed, usually by opening
the abdomen, in order to reestablish flow from the viscera
Unlike the extremities, patients with abdominal compartment syndrome do not exhibit the five P
However, a high index of suspicion, rapid diagnosis, and expeditious treatment result in
restoration of flow and prevention of morbidity in both scenarios
116.) Surgical postoperative complications. Emergency laparotomy
General
-
Postoperative complications are problems that can happen after you have had surgery, but which
were not intended
-
Doctors are aware of the risk of complications and take steps before, during and after surgery to
reduce this risk
-
However, some complications are common and occur frequently despite precautions
The most common postoperative complications include fever, small lung blockages,
infection, pulmonary embolism (PE) and deep vein thrombosis (DVT)
Occurrence of postoperative complications
-
Postoperative complications include immediate complications (up to three days after the
surgery), early complications (most likely in the few weeks after your surgery) and late
complications (up to years afterwards)
Immediate
-
Bleeding (from the wound or internally)
Lung blockage or collapse
Shock
Heart problems
Page 264 of 269
Early
Late
-
Pulmonary embolism (PE)
Severe infection (septicaemia)
Acute kidney injury
-
Pain
Bruising
Confusion
Nausea and vomiting
Fever
Bleeding
Wound breakdown
Deep vein thrombosis (DVT)
Acute urinary retention - inability to pass urine
Infections: pneumonia, wound infection, urinary tract infection
Constipation
Bowel problems
-
Bowel blockage due to scarring inside the abdomen
Incisional hernia
Persistent sinus
Thickening or tightening of scar
The original problem coming back
General Complications
Pain
Confusion
-
Pain should be well controlled
Painkillers taken by mouth or IV (paracetamol, codeine)
Anti-inflammatory painkillers have traditionally been widely avoided as they were thought to
slightly increase the risk of bleeding, but in many types of surgery these are safe
Medicines which are anaesthetic and are infused around the nerves in the spine, or into the
wound, to add numbness temporarily
is quite common after surgery, particularly in elderly patients
It can be caused by the anaesthetic or by other medicines which may have been given, including
painkillers
Confusion can occur for several other reasons, including pain, disturbed sleep, infection,
constipation and abnormalities of fluid balance (ie you are lacking in fluid in the body
(dehydrated) or you have been given too much fluid
Nausea and vomiting
-
common reaction to an anaesthetic
can also occur because of infection, or as a side-effect of medication, particularly painkillers
These symptoms are more likely in the bowel surgery
Temperature
Septicemia
-
Fever may occur after surgery and may be caused by infection in the surgical wound, infection in
lungs, cystitis, deep vein thrombosis (DVT), after blood transfusion, and as a reaction to
medication
is an uncommon complication of surgery
It usually results from the spread of infection from somewhere more localised, like the wound,
the lungs (pneumonia) or the bladder
Septicaemia is more likely after surgery which carried a higher infection risk, particularly
abdominal surgery involving cutting the bowel, surgery after trauma where wounds may be
contaminated, and severe burns
Page 265 of 269
-
It is more likely if your immune system is suppressed, if you have diabetes, or if you are very
young or very elderly
Bleeding, wound and skin complications
Light bleeding
-
Bleeding which hasn't stopped since surgery or starts straight afterwards usually means that tiny
blood vessels around the area of surgery are leaking very slightly
Heavy bleeding
-
If heavy bleeding does occur this may mean stitches have burst, or that your blood is not clotting
well as an effect of the surgery
This is an emergency, as losing blood may lead to shock and collapse
you may need a blood transfusion
is mainly seen after more major operations, when large blood vessels may have been cut or
damaged
This is more likely to happen after surgery to large blood vessels, large joint replacements,
surgery after you have experienced serious trauma (such as a road accident), and surgery
associated with cancer, when there may be abnormal blood vessels present
Hematoma formation
Bruising
-
A haematoma is a trapped pocket of blood in the body which has leaked from a wound or blood
vessel
It may be just under the skin, where it may form a bluish lump, close to the wound (where it may
leak but won't completely empty, as it will have partially clotted), or inside the body where it
can't be seen
They can leave a small lump even after healing has occurred, as the trapped blood may leave
behind a bit of fibrous tissue as it is reabsorbed
They can be also a site of infection
Bruising is the leakage of blood from cut or damaged blood vessels into the subcutaneous tissues
Surgical infection
-
can happen after any surgery but is particularly a problem after abdominal surgery which
involves opening the bowel
-
To try to prevent this, you may be given antibiotics before your operation; however, drugresistant bugs (pathogens) are an increasing problem
-
A wide range of organisms are involved in these infections, but what is very concerning is the
increasing prevalence of antibiotic-resistant bacteria, such as methicillin-resistant
Staphylococcus aureus (MRSA) and vancomycin-resistant Enterococcus (VRE)
Postoperative diarrhea due to C difficile is a common nosocomial infection in surgical patients
The most common type of infection is surface (superficial) wound infection occurring within the
first week
-
o
-
Deeper infections are most likely after bowel-related surgery. They can occur any time from
immediately after surgery to up to three weeks later
o
-
It causes soreness and localized pain, redness and, sometimes, a slight sticky discharge
They cause a high temperature, sometimes with confusion, nausea and feeling unwell
Abscess is a collection of pus inside the body, where infection has collected
o
Abscesses cause swinging fever - a temperature that goes up and down
o
Confusion and nausea are common
Page 266 of 269
o
-
Abscesses need to be drained
Wound sinus is a late infection from a deep but undetected abscess that finds a way of
discharging through the skin
o
Mild temperature
o
there will be a sticky discharge, often through the surgical scar, hinting at the infection
hidden inside
Wound dehiscence
-
is partial or total disruption of any or all layers of the operative wound
Rupture of all layers of the abdominal wall and extrusion of abdominal viscera is evisceration
Wound dehiscence occurs in 1%-3% of abdominal surgical procedures
Systemic and local factors contribute to the development of this complication
Systemic risk factors
o It is more common in patients with diabetes mellitus, uremia, immunosuppression,
jaundice, sepsis, hypoalbuminemia, cancer, obesity, and in those receiving
corticosteroids
Local risk factors
o inadequate closure, increased intra-abdominal pressure, and deficient wound healing
o The type of incision (transverse, midline, etc) does not influence the incidence of
dehiscence
Incisional hernia
-
Incisional hernia develops as a late complication of about 1 in 10 abdominal operations
Usually, the hernia is a bulge in the abdominal wall near the surgical scar
Risk factors
o obesity, weak abdominal muscles, wound infection and repeated re-operations through
the same site
Nerve damage
-
If nerves are damaged these can take a particularly long time to heal and they may never
completely recover
Pressure ulcers
-
is an ulcerated area of skin caused by irritation and continuous pressure on part of your body
more common over places where your bones are close to your skin (bony prominences), such as
your heels, the lower part of your back and your bottom, and your risk of developing a pressure
ulcer is increased if you are spending long periods lying in bed or sitting in a chair
Breathing and lung complications
Lung atelectasis
- This is very common and involves a blockage and then a collapse (atelectasis) of a part of one of
your lungs, usually at the bottom, so that it no longer fills with air when you inhale
- Lung collapse occurs when the finer airways get blocked with trapped mucus
- Once air can't get in or out, the air that is already behind the blockage is absorbed by the body
and the fine tubes collapse
- These collapsed sections of lung easily become infected due to trapping of bacteria
- Symptoms are breathless and painful cough
Pneumonia
-
You may have a cough or abdominal pain and you are likely to have fever, and shortness of
breath
Pneumonia often follows atelectasis and is treated with antibiotics
Additional oxygen may be needed
Page 267 of 269
Deep vein thrombosis and pulmonary embolism
-
There is an increased risk of PE and DVT any time from surgery until you are fully mobilised
again
the risk is highest in the first two to three days after the operation
The risk of clotting is increased by long periods of being immobile, by being on hormones, if
you are overweight, by certain medicines (including hormone replacement therapy (HRT) and
the combined oral contraceptive (COC) pill), by pregnancy and, particularly, by being a smoker
DVT is not always detected but it causes painful swelling of the leg (particularly the calf)
Smaller pulmonary emboli cause sudden breathlessness, chest pain and confusion, while large
ones cause collapse and may be fatal
If you are particularly at risk you will be given blood-thinning medicines for the period of your
surgery
Aspiration pneumonitis
-
It is a chemical inflammation of the lungs which occurs because acidic stomach contents are
inhaled, usually due to vomiting or regurgitation followed by inhalation whilst you are under
anaesthetic
Acute respiratory distress syndrome (ARDS)
-
This rare condition comes on 24-48 hours after surgery, usually after multiple trauma
It causes severe breathlessness and confusion due to low oxygen levels
It is more common in sepsis, after serious head injury and serious burns
-
They include heart attacks, abnormal heart rhythms, angina and heart failure
They can sometimes go undetected, which mask pain and discomfort, or you are still sleepy or
confused
Heart complications
Kidney and bladder complications
Urinary retention
-
It is sometimes necessary to pass a catheter to allow the bladder to drain
Cystitis
Acute kidney injury
Complications of bowel surgery
Constipation
-
Inability to pass a stool is very common in the days and weeks after surgery
Anesthetic can trigger constipation
Constipation can sometimes be due to paralytic ileus and bowel obstruction
Paralytic ileus
-
The bowel stops its usual rhythmic contracting, so food is not pushed through it and you stop
opening your bowels or passing air
Often happens after abdominal surgery
Painkillers (particularly opiate medicine) make it more likely and it is more likely to occur in
older people, in people with an underactive thyroid gland, in people with Parkinson's disease and
in people with diabetes
Symptoms: nausea, vomiting, bloating, abdominal discomfort
IV fluids
Nasogastric tube to keep the stomach empty
Bowel obstruction
-
After bowel or abdominal surgery the bowel can become twisted, which causes a sudden
blockage
Page 268 of 269
-
It can also be blocked by strings of scar tissue called adhesions, which can form inside the
abdomen
Symptoms: colicky abdominal pain, constipation, nausea and vomiting
IV fluids
Bowel leakage
-
If the bowel has been cut and then stitched closed (for example, in appendicectomy) or if a
section of bowel has been removed, the 'join' (anastomosis) in the bowel can leak or come apart
Small leaks are common and cause small abscesses in the abdomen, sometimes several weeks
after surgery
Larger leaks are rare but cause severe abdominal pain and widespread infection (peritonitis)
Hemoperitoneum
-
Bleeding is the most common cause of shock in the first 24 hours after abdominal surgery
Postoperative hemoperitoneum— a rapidly evolving, life-threatening complication— is usually
the result of a technical problem with hemostasis, but coagulation disorders may play a role
Hemoperitoneum usually becomes apparent within 24 hours after the operation
It manifests as intravascular hypovolemia: tachycardia, hypotension, decreased urine output, and
peripheral vasoconstriction
The differential diagnosis of immediate postoperative circulatory collapse also includes
pulmonary embolism, cardiac dysrhythmias, pneumothorax, myocardial infarction, and sever
allergic reactions
If hypotension or other signs of hypovolemia persist, one usually must reoperate promptly.
At operation, bleeding should be stopped, clots evacuated, and the peritoneal cavity rinsed with
saline solution
Emergency laparotomy
-
An emergency laparotomy is a surgical operation that is used for people with severe abdominal
pain to find the cause of the problem and in many cases to treat it
You will have a general anaesthetic and the surgeon will make an incision (cut) to open the
abdomen (stomach area)
Often the damaged part of an organ is removed and the abdomen washed out to limit any
infection
An emergency laparotomy might be carried out for several reasons including bowel obstruction
(blockage), bowel perforation (burst) and bleeding in the abdominal cavity (internal bleeding)
These are conditions which if left untreated could be life-threatening
An emergency laparotomy is used either to save life or to limit illness, and in many cases it
might be the only option available in order for the patient to get better
Page 269 of 269