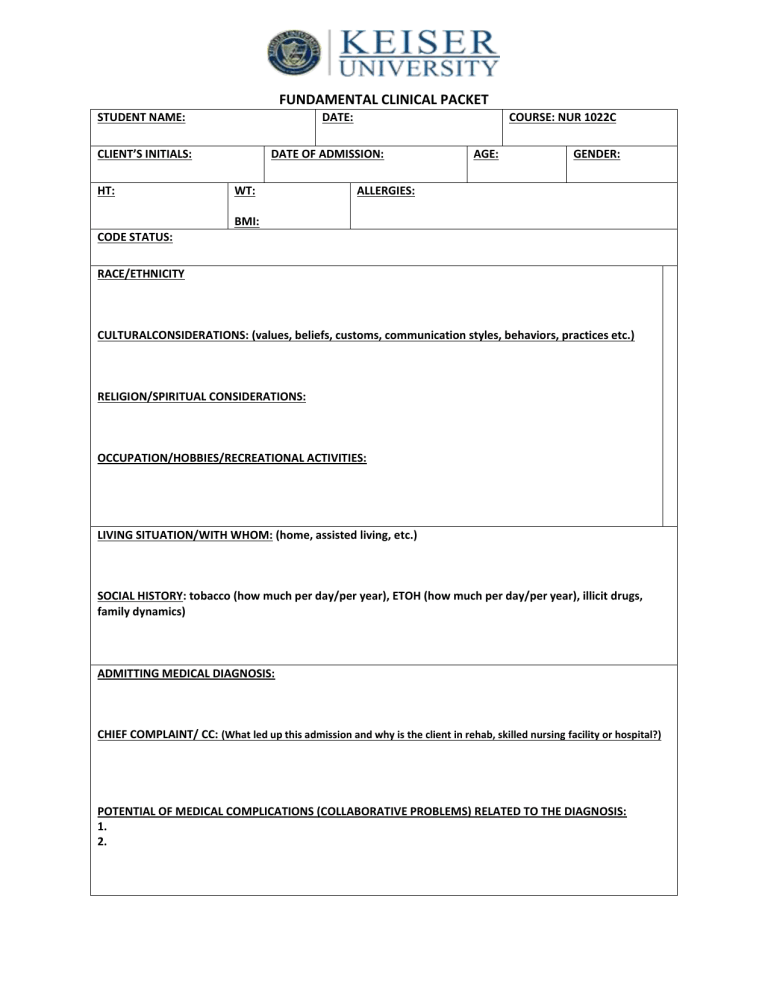
FUNDAMENTAL CLINICAL PACKET STUDENT NAME: DATE: CLIENT’S INITIALS: HT: COURSE: NUR 1022C DATE OF ADMISSION: WT: AGE: GENDER: ALLERGIES: BMI: CODE STATUS: RACE/ETHNICITY CULTURALCONSIDERATIONS: (values, beliefs, customs, communication styles, behaviors, practices etc.) RELIGION/SPIRITUAL CONSIDERATIONS: OCCUPATION/HOBBIES/RECREATIONAL ACTIVITIES: LIVING SITUATION/WITH WHOM: (home, assisted living, etc.) SOCIAL HISTORY: tobacco (how much per day/per year), ETOH (how much per day/per year), illicit drugs, family dynamics) ADMITTING MEDICAL DIAGNOSIS: CHIEF COMPLAINT/ CC: (What led up this admission and why is the client in rehab, skilled nursing facility or hospital?) POTENTIAL OF MEDICAL COMPLICATIONS (COLLABORATIVE PROBLEMS) RELATED TO THE DIAGNOSIS: 1. 2. SECONDARY MEDICAL DIAGNOSIS: (include pertinent preexisting diagnoses such as DM, COPD, etc.) PAST MEDICAL/SURGICAL HISTORY: (including tobacco, ETOH, illicit drugs) SURGERIES/MEDICAL PROCEDURES THIS ADMISSION: (include date performed and explanation) CONSULTS: (IF APPLICABLE: include date, discipline and reason for consult) PT: OT: RT: SPEECH: DIETARY: CARDIAC: OTHER: OTHER: DIAGNOSTIC TESTS: (CT, MRI, CXR, U/S, EKG, etc.; include date, reason for test, and results) CXR: CT: MRI: ECG OTHER: OTHER: OTHER: DVT PREVENTION: Anticoagulation Medications/TEDS/SCD’s/ROM/Ambulation Diagnostic Test Name Na+ Sodium K+ Potassium CLChloride Glucose BUN Creatinine WBC Normal Range Purpose of Test Patient Preparation Patient Findings / Results Reason why your patient’s exam is Abnormal Diagnostic Test Name HGB HCT Platelets Normal Range Purpose of Test Patient Preparation Patient Findings / Results Reason why your patient’s exam is Abnormal Medication (Brand/Generic name) Indications (Circle the reason why your client is taking the med.) Prescribed dose, Route, and Frequency Side Effects Contraindications What nursing assessment is needed prior to med administration / lab-value associated with med / specific things that you need to monitor/major side effect that nurse needs to teach client Medication (Brand/Generic name) Indications (Circle the reason why your client is taking the med.) Prescribed dose, Route, and Frequency Side Effects Contraindications What nursing assessment is needed prior to med administration / lab-value associated with med / specific things that you need to monitor/major side effect that nurse needs to teach client Report Quick Sheet (Please fill in all sections) Patient’s Initials: ___________ Neurological A & O/Confused: ______________ Room #: ___________ PAIN Management Pain Scales (0-10) Medication: ______________________ LOC: _______________________ HEENT Pupils: ________________________ Hearing: _______________________ Frequency: ______________________ Speech: _____________________ Vision: ________________________ Last Dose: ______________________ Commands: __________________ Daily Tasks □ Daily Weight (Y / N) IV’S #1: Location: _____________________ Accu-Checks (Y / N ) AC/HS or ______________________ □ Turn Q 2 Hr Type/Gauge: _____________________ Time Blood Sugar Units ________ ________ ____________ □ Patient Rounds Q1hr Start Date: ______________________ □ I & O Total UOP___________ #2: Location: _____________________ □ Bed/Bath/Room Tidy Type/Gauge: _____________________ □ Fresh Ice and Water Start Date: ______________________ ________ ________ ____________ ________ ________ ____________ ________ ________ ____________ Respiratory O2: ___________ O2 Sat: _________ Chest Tubes: ___________________ Cough (Y / N ) Sputum; _________ RUL: _________ LUL: ___________ IVF/Drips Vital Signs Temp – HR – BP – RR – O2 Fluid: ____________ Rate: _________ Fluid: ____________ Rate: _________ Temp – HR – BP – RR – O2 Fluid: ____________ Rate: _________ RLL: _________ LLL: ____________ Respiratory Treatments (Y / N ) ABG: __________________________ Cardiac/Circulatory Tele # _________ Rhythm ________ Musculoskeletal Activity: _________________________ Gastrointestinal Diet:___________________________ Heart Sounds ___________________ Assistive Devices: _________________ Tubes:_________________________ Chest Pain (Y / N ) PT Eval (Y / N ) Feedings: Rate:__________________ Pacemaker (Y / N ) RUE: ___________ LUE:___________ Bowel Sounds:__________________ Edema ________________________ RLE: ___________ LLE:___________ LBM:__________________________ Integumentary Wounds:_________________________ Notes Skin Temp _____________________ Genitourinary Urine Description :_________________ Voids: Foley Bedpan BSC Dressing:_________________________ Dialysis:________________________ HEAD TO TOE ASSESSMENT Each section needs to be filled out completely. VITAL SIGNS BP Da y 1 Pulse Radial Pedal Apical Rhythm B=bounding; S=strong; W=weak; A=absent; D=doppler Respiration: Rate and quality Temperature Oxygen Saturation if applicable Pain Assessment (scale 0-10) Note presence, onset, location, intensity Frequency, duration. Radiation Precipitating factors, facial appearance Guarding, inability to focus, change in VS EGO INTEGRITY: Erickson: _____________ Physical Appearance: Behavior and Thought processes: Appropriate to Situation: Memory intact: Affect appropriate: Memory Intact Tobacco: Alcohol: Recreational Drug / Substance use: Da y 2 HEAD TO TOE ASSESSMENT (continued) Describe Skin: Intact, temperature, moisture. Note and describe on chart ANY of the following: rashes, wounds, pressure ulcers, ecchymotic areas, scars, tattoos, IV site (anything applicable and visible). Number or label each area. Hygiene (participation in ADLs) (Assistance required) Color Turgor Peripheral edema sites Degree of edematous areas (Use Scale Below) Nail beds (color and angle) Capillary refill (seconds) Edema Scale: 1+ =barely detectable, 2mm 2+ =indentation of 4 mm 3+ =indentation of 5 to 7 mm 4+ =indentation 8mm or greater Pupil Size: Neurosensory: Mark “X” where applicable ORIENTED: PUPILS: PERRLA Pupil Size Prosthetic Devices Alert Person Equal Place R: Glasses Circulation: Mark “X” where applicable” Absent Edema Warm Perfusion Restless Lethargic Comatose Time Unequal Confused Reactive Sedated Sluggish L: Hearing Aids Dentures Other Present Dry Site Diaphoretic Pattern: Breath Sounds: Respiratory Even Uneven Shallow Dyspnea Clear where or if adventitious describe type and location Cough SOB @rest or exertion Sputum amount and color Hemoptysis Orthopnea O2 Therapy (type/amount) Secretions: Treatment: Peripheral and or central cyanosis Color of mucous membranes Use of accessory muscles Pain on Inspiration or Expiration Other treatments Activity/ Sleep: (list any assistive devices) Activity: ROM Activity Restriction Contractures: Joint Swelling Stiffness Ambulation: Steady Gait PT/OT Assessment Rest/Sleep: Quality & Quantity of Sleep STRENGTH: RIGHT ARM LEG LEFT STRENGTH Code: 4= normal strength, grip strong or good pressure resistance can move, lift and and hold extremity 3= grip weak and/or poor pressure resistance lifts and holds, can move, lift and hold extremity 2= weak grip or pressure resistance lifts and falls back, can move and lift extremity but cannot hold position 1= little or no grip or pressure resistance moves on bed, cannot lift or hold 0= no movement ELIMINATION: Note any of the following food intolerance or allergies, N or V, change of bowel habits, rectal bleeding or black tarry stools, use of laxative and type. Oral mucosa: Bowel sounds: Bowel movement: Ostomy ( type) Color/moist Other Active/hypoactive/ hyperactive/absent Last BM Frequency (Hx) Character/Color Note any abnormalities on the chart: areas of tenderness or pain, location of ostomy or none. RUQ LUQ RLQ LLQ URINARY Urine Last Voided: Retention Frequency Nocturia Polyuria Quantity sufficient: Anuria Hematuria Dysuria Incontinent Catheter Type: Color Critical Thinking Weekly Self - Evaluation 1. Identify 2 psychomotor skills you consider to be a: STRENGTH a. b. WEAKNESS*** a. b. ***Indicate how you will improve your weak skills 2. List 3 goals (psychomotor or cognitive behaviors) you would like to strive for the next week a. b. c. This self-evaluation will help your instructor in evaluating your clinical experiences Date: Nurses Progress Note NUR1022C – Fundamentals of Nursing Patient Initials: __________________________________________________________________ __________________________________________________________________ __________________________________________________________________ __________________________________________________________________ __________________________________________________________________ __________________________________________________________________ __________________________________________________________________ __________________________________________________________________ __________________________________________________________________ __________________________________________________________________ __________________________________________________________________ __________________________________________________________________ __________________________________________________________________ __________________________________________________________________ __________________________________________________________________ __________________________________________________________________ __________________________________________________________________ __________________________________________________________________ __________________________________________________________________ __________________________________________________________________ __________________________________________________________________ __________________________________________________________________ __________________________________________________________________ Nursing Diagnosis Statement: Maslow’s/Developmental Theory: Nursing Assessment Date (includes at least 3 subjective data and / or objective data that leads to the nursing diagnosis) Subjective 1. Outcome/Goal – 1 long term goal & 2 short term goals (Follow SMARTspecific, measurable, achievable, realistic, timely criteria, dated and timed) STG 1: Nursing Interventions: ((3) interventions for each the STG and (2) interventions for the LTG) include a frequency on each intervention. Rationales: (Provide reason why intervention is indicated with citations and page numbers) Implementation: (Documentation) What you did /the response from the patient or family: include date, Action, Response from the patient Evaluation: State each goal as met, not met, partially met “AEB”. If not metrevise it, state goal discontinued and list why modifications needed, date and time. Care Plan status: continue, revise, discontinue STG 1 1. 1. 1. 1. 2. 2. 2. 3. 3. 3. 2. 3. Objective 1. 2. 3. LTG 1: LTG 1 1. 1. 1. 2. 2. 2. 1. PATHOPHYSIOLOGY CARD CONDITION/DISEASE: DEFINITION: A brief definition in your own words and include: the pathological process(es); organ(s) involved; nature of the organ’s change; and physiological functions involved. ETIOLOGY: Include when applicable: -Causative factor(s) -Incidence -Genetic factors -Predisposing and contributing factors PROGNOSIS AND COURSE OF CONDITION/DISEASE: This should be a generalized prognosis, which can be sued to compare with to your patient. Do not write the specific prognosis of your assigned patient; you may take care of patients with the same condition but different prognosis. CLINICAL MANIFESTATIONS: -Subjective signs: What does the patient or family tell you? -Objective signs: This can include the physical exam and the laboratory findings TREATMENT: -Dietary: -Medication: -Surgical: -Psychosocial Considerations: -Other: ***Once again, this is a generalized card; what you write is under this section should be able to apply to MOST patients with this condition or disease. COMPLICATIONS: What signs and/or symptoms do you need to be aware of to prevent any complications? PREVENTIVE MEASURES: What generalized nursing measures could you institute?