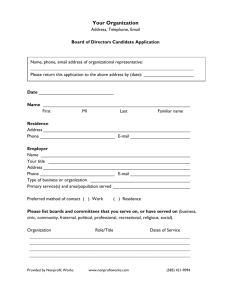
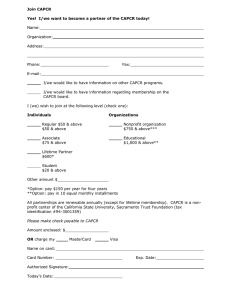
Health Services Organizations, Financing and Quality Improvement Health Care Systems • Complex organizations • Developed for the provision of care that include multiple players, such as hospitals, government, doctors, pharmaceutic companies, private practices, and public health departments. • The main mission of a given health care system is to keep the population healthy and to treat disease. • In the United States, outlays for medical care have steadily risen and are currently taking up close to 18% of the gross domestic product (GDP). Health Systems Management Exists to measure and improve how well our health care system meets its stated goals. Mission Improving an organization's performance requires understanding of its: Core functions Inputs and outputs Health Care Managers “Management's job is to create an environment where everybody may take joy in his work.” - W.E. Deming • Basic Functions • Planning • Organizing • Controlling • Leading • Must understand the environment in which they operate • Need to know how to • Manage change, • Supervise employees • Lead teams to improve quality of care. • Assess organizational performance • Finances “Operational • Clients or patients Skills” • Other stakeholders Organization and Structure: HEALTH CARE DELIVERY SYSTEMS • Hybrid of private and governmental health systems in US, in contrast to many other developed nations. • State governments establish policies and laws, which govern the conduct of health care providers and institutions. • Dichotomy of functions between the public health departments and health care institutions, such as hospitals. • Public health departments • Many do not engage in the direct provision of health care, although some function as provider of last resort to special populations. • Hospitals and private clinics • • Traditionally deal only with direct patient care and often expend little effort to engage in health promotion in the community. Laypersons usually think of the health care system consisting only of a hospital and affiliated practices where they usually get care. • Many other entities that are integral to the health system • • • • • Pharmacies Visiting nurses Nursing homes, Rehabilitation centers. The government has a direct role in financing of health care services through Medicare, Medicaid, and the Children's Health Insurance Program • Funded through taxpayer money • Great deal of interest in ensuring that health care consumers are getting the best health outcomes for their tax payments. Nonprofits are sometimes called tax-exempt organizations, or referred to by the section of the tax code that designates them (a code that should be remembered as it is part of the accepted parlance): A. 501(c)(3) B. 501(c)(4) C. 105(c)(3) D. 105(c)(4) E. 105(6)(4) A. The term 501 (c)(3) is often used as a synonym for nonprofit organization. Under the US tax code, organizations that qualify for tax-exempt status under section 501 (c)(3) include religious, educational, charitable, scientific, and literary organizations, and organizations that do testing for public safety, that foster national or international amateur sports competition, or that prevent cruelty to children or animals. For the other answer choices, (B) 501(c)(4) concerns civic leagues, social welfare organizations, and local associations of employees; (C) to (E) are nonsense distracters. Organization and Structure: MANAGEMENT OF HEALTH CARE ORGANIZATIONS • In the United States, most hospitals are designated as nonprofit under the IRS code 501(c)(3). • The majority of private practices are for-profit entities. • Nonprofit health organizations are exempt from paying income taxes. • Some believe that, if an organization is nonprofit, it cannot or need not make profit. • However, despite their name, even nonprofit organizations need to make a profit to be financially viable. • If they do not, they cannot invest in infrastructure, new technology, or personnel development; consequently, they will eventually close or become obsolete ("no (profit) margin, no mission"). • To qualify as a nonprofit, an organization's purpose must meet one of the exempt purposes in the federal tax code, which include charitable, religious, educational, and scientific endeavors. • Nonprofit hospitals, for instance, must demonstrate that they provide charity care to poor patients to remain exempt from income taxes. Organization and Structure: GOVERNANCE OF HEALTH CARE INSTITUTIONS • Nonprofit organizations are governed by a board of trustees; in for-profits, such an oversight committee is called the board of directors. • These boards are ultimately responsible for setting the organization's policies and strategies. • One of the board's most important jobs is to hire and fire the chief executive officer (CEO). • The board also approves budgets, oversees the organizational performance, and sets the overall mission of the organization. • The CEO is assisted by vice presidents or chiefs of service, such as a chief financial officer (CFO) in charge of finances and the chief operational officer (COO), who oversees day-to-day operations. • Most organizations have additional chief officers, depending on their mission and size, such as chief nursing officer (CNO), chief medical officer (CMO), and chief information officer (CIO). • In other organizations, such positions might be called vice president (VP), such as VP of nursing or VP of medical affairs. • Organizations also have stakeholders. • A stakeholder is someone who has a vested interest in or is affected by the organization's operations. Stakeholders can include patients, community members, employees, local govern-ments, churches, charitable organizations, vendors, visiting nurses, and unions. Most organizations cannot reach major public health goals by themselves; they need to build coalitions with stakeholders to leverage resources and build political will. • Lastly, public health and health care delivery are moral pursuits. This requires that the management and conduct of a public health agency or health care organization be ethical, and that the organization's mission should be reflected in its management methods. The final responsibility in a nonprofit health organization rests with the: A. Chief executive officer (CEO) B. Chief financial officer (CFO) C. Chief medical officer (CMO) D. Board of directors E. Board of trustees E. The final responsible body in a nonprofit organization is the board of trustees; the board of directors (D) is the analogous body in a forprofit organization. The board of trustees hires and fires the CEO, who then hires the various officers representing the other answer choices. The board also approves the budget and oversees the overall organizational performance. The chief executive officer (A) is the highest ranking officer under the board, and similarly approves budgets and oversees overall organizational performance. Underneath the CEO is a vice presidential suite that usually includes the chief financial officer (B). Organizations engaged in direct patient care will also have a chief medical officer (C). In a nonprofit organization, any profits go to: A. The chief executive officer B. Stakeholders C. Shareholders D. The organization E. Nonprofit organizations do not make profits • D. Even nonprofit organizations need to have revenues exceed expenses. In other words, they hope to have profit (not E), although this profit is then reinvested into the organization. Profits go to infrastructure, new technology, or personnel development, as opposed to being distributed to shareholders (C), the case with for-profit organizations. Because the aim is to operate successfully without generating net losses (i.e., to generate profit), there has been a shift away from the term nonprofit to the term not for profit, which helps clarify that organizations definitely want to do more than break even, even though the ultimate goal is not to produce financial return for investors. The profits do not go directly to stakeholders (B) but may indirectly affect them through organizational improvements and enhanced service delivery. The chief executive officer The act of comparing actual performance to budgets is called: A. Variable costing B. Variance analysis C. Volume variance D. Quantity variance E. Price variance • B. The act of comparing actual performance to budgets is called variance analysis. In conducting variance analis. both fixed and variable costs need to be considered, but variable costing (A) is not a legitimate term. Types of variance that might be discovered in conducting a variance analysis are volume variance (C), quantity or use variance (D), and price (spending or rate) variance (E). Before purchasing new equipment or starting a new budgetary line to provide health-related services, what is the most important economic question that must be asked? A. What are the fixed costs of the equipment or service? B. What are the variable costs of the equipment or service? C. What is the expected volume of procedures or services to be provided with the new equipment or service line? D. What will be the expected lost revenue with the new equipment or service line? E. What is the expected net revenue compared with the alternatives of not moving forward or doing something else? E. While fixed (A) and variable (B) costs are important considerations, as well as expected utilization (C) and possible losses of revenue (D), from an economic petspective, the most fundamental question is, Will mov ing forward with new equipment or a new service line result in greater net revenue? In other words, will mating the change produce greater profit than the alterna. tives of making no change, or doing something else (e.g., purchasing different equipment, starting different service line). Economics is not the only consideration in plans for change, however, and the org.-nization might be willing to accept less of a profit margin if a change will result in greater care delivery or improved client services. As long as the organization will confidently break even and maintain some revenue over cost for safety, a relative decrease in proft might be acceptable given humanitarian, service, or other concerns related to the organization's mission. The Joint Commission (TIC, formerly JCAHO) is an independent, nonprofit organization that evaluates the quality and safety of most US health care institutions. In TIC assessment, how institutions screen and treat patients for tobacco use is an example of what type of measure? A. Structure B. Process C. Outcome D. Small area E. HEDIS B. Assessing the procedures in place to identify and treat smoking patients would be an example of a process measure. Process measures are not as common as ouf-come measures; current quality improvement efforts focus increasingly on outcomes (C). With smoking pa-tients, the number counseled to quit would be a related outcome measure, an example of a HEDIS (E) measure. A related measure pertaining to structure (A) might be whether a health care facility has an established smoking cessation program or substance abuse counselors available. Small area (D) is a term referring to a typed geographic analysis, looking at variation in quality measures by different geographic regions. Which of the following is a governmental organization involved in defining and fostering high-quality health care? A. ICAHO B. IHI C. AHRQ D. NCQA E. NOF C. The Agency for Healthcare Research and Quality is the lead federal agency to improve the quality, efficiency, safety, and effectiveness of US health care. The Joint Commission, formerly known as JCAHO (A), the Institute for Healthcare Improvement (B), the National Committee for Quality Assurance (D), and the National Quality Forum (E) are independent, non-profit, nongovernmental groups involved in defining and fostering quality health care. Two hospitals have comparable facilities, staff, polices, and procedures. However, when an independent group measured quality based on outcomes only, Hospital A performed much better than Hospital B. In response, leadership at Hospital B put procedures in place to stop accepting the sickest patients, knowing that these most severe cases were driving the institution's poor quality score. The next year, Hospital B performed just as well as Hospital A, receiving an excellent quality score. In this ironic case, measuring quality likely led to poorer quality for the patients most in need; the sickest patients were effectively abandoned. The moral fabric of Hospital B's leadership aside, this unfortunate result might have been avoided if Hospitals A and B were compared using: A. Failure mode and effects analysis (FMEA) B. Root cause analysis (RCA) C. Six Sigma D. Case-mix adjustment E. Rapid cycle improvement D. Case-mix adjustment describes the process of adjusting quality analyses for the severity of illness. Unless outcomes are adjusted for the severity of patient it nesses, organizations treating the sickest patients (e.g., Hospital B) would be at an unfair disadvantage The case in the question demonstrates one means of dealing with this unfair disadvantage and illustrates is limitations of relying on outcome measures only at quality assessment. Outcome assessments inherent create incentives to "cherry pick" or (to use terminology of the insurance industry) to avoid "adverse selection," such that only the healthiest people remain patients, and outcomes naturally improve as a result. Although scores are better and quality improves for the organization, quality actually can worsen for a community, or at least its most vulnerable segments. What you may achieve with nonadjusted outcome scoring is institutions gaming the system rather than actually improving care. Failure mode and effects analysis (A), root cause analysis (B), and Six Sigma (C) are different quality improvement methodologies, and rapid cycle improvement (E) is about making system improvements in small, incremental steps. In general, regarding health care at present, the largest and most expedient improvements in quality might come from: A. Studying novel health care delivery approaches B. Proposing innovative community programs C. Developing new service delivery systems D. Finding fresh solutions to quality problems E. Implementing existing interventions E. Although there are many established, effective inter-ventions, substantial energy goes into finding still more new solutions. If just a fraction of energy pursuing new ideas were instead focused on implementing established, effective care consistently (giving every patient the right interventions the right way at the right time), the gains in mortality and morbidity would be great. Quests to develop new, novel, fresh, and innovative approaches (AD) might ultimately be helpful, but also might be completely fruitless. Regardless, they would not be as expedient as implementing existing interventions now. improvement (E) is about making system improvements in small, incremental steps.