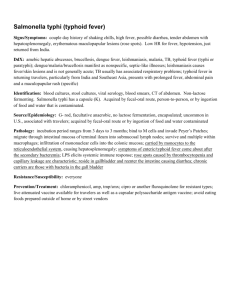
•У ЕРСИТЕТ НИВ НА Ц ЬКОВСКИЙ ХАР • Й • МЕД ЬНЫ ИЦ ИН С Й КИ Л НА О И Kharkiv National Medical University Department of Infectious Diseases Typhoid fever. Paratyphoid fevers TYPHOID FEVER Acute infectious disease caused by Salmonella enterica typhi and characterized with bacteriemia, severe intoxication, continuous fever and affection of lymphatic formations of small intestine with formation of ulcers. HISTORY 460-377 y. BC Beginning of ХІХ c. Hippocrates epoch Bretonio and Charle Loue Typhoid – all “feverish” diseases (by Greek smoke). Typhoid fever first described as separated disease 1868 S.P. Botkin 1874 Borovich, I. Sokoliv 1880 Ebert Extracted S. typhi from sections of spleen of patients, described pathogen 1884 Gaffki Extracted S. typhi in pure culture 1896 Geuber and Vidal ХХ c. different years I.S. Kildushevsky, N.I. Rogoza, J. Padalka, К.V. Bunin and other Made classical description of clinical symptoms and complications. Was discovered Salmonella typhi Implemented reaction of agglutination (Vidal test). Detailed description of clinical symptoms, methods of diagnostics, treatment and prophylaxis. Typhoid fever infects roughly 21.6 million people (incidence of 3.6 per 1,000 population) and kills an estimated 200,000 people every year ETIOLOGY • • • • • • • • • Pathogen – Salmonella enterica Typhi Family – Enterobacteriacae Genus – Salmonella, Sp. – enterica Gram-negative non-sporing, motile rods (2-4X0.5µm), do not have capsules. Antigenic structure: О – somatic, Н – flagellar, Vi – virulence antigen Serogroup D (classification by Kauffman-White). PATHOGENIC FACTORS Endotoxin (LPS) Gialuronidase, fibrinolsysin, hemolysin, catalase and other enzymes «pathogenic isles»: SPI-1, SPI-2, SPI-7 и др. ETIOLOGY • Resistance in an environment is rather high • Can survive several months away from the host (in water and soil). • Can survive refrigeration, freezing and dry conditions. • Can survive in the stuff-foods (milk, meat) from 1-2 till 25-30 days. • Boiling or chlorination of water immediately destroy the bacilli • The bacilli are killed at 55ºC in one hour or at 60ºc in 15 minutes. EPIDEMIOLOGY • Anthroponosis • Source of infection – sick person or carriers • Mechanism of transmission – fecal-oral • Routs of transmission – alimentary, watery, contact • Outbreaks – alimentary and watery routs • Sporadic cases – contact rout • Susceptibility is high • Season: summer, autumn • Immunity – strong, steady Environmental and behavioral risk factors that are independently associated with typhoid fever • eating food from street vendors, • living in the same household with someone who has new case of typhoid fever, • washing the hands inadequately, • sharing food from the same plate, • drinking unpurified water, • living in a household that does not have a toilet In 1906, Irish immigrant Mary Mallon worked as a cook in the home of New York banker Charles Henry Warren and his family. By the end of the summer, Mary Mallon six members of the household (wearing glasses) photographed had contracted typhoid fever. with The Warrens hired sanitary engineer, bacteriologist Emma Sherman on North Brother George Soper, to determine Island in 1931 or 1932, over 15 years after she the source of the disease. Soper had been there concluded that Mallon, while immune quarantined permanently. herself to the disease, was its carrier. For three years, she was isolated on North Brother Island, near Rikers Island, earning the nickname "Typhoid Mary." Instructed not to cook for others upon her release, she nevertheless changed her name and became a cook at a maternity hospital in Manhattan. At least 25 staff members contracted typhoid. "Typhoid Mary" returned to North Brother Island, where she lived alone for 23 years in quarantine, until her death of a stroke in 1938. PATHOGENESIS 1. 2. 3. 4. 5. 6. 7. 8. Invasion. Penetration of the pathogen into GI tract Invasion of the pathogen into mesentherial lymph nodes (regional lymphogenic reaction) Bacteriemia Endotoxinemia Parenchymatous diffusion (bone marrow, liver, spleen, kidneys, other organs) Excretory allergic phase. Morphologic changes. Immunologic reactions Convalescence MORPHOLOGICAL CHANGES IN INTESTINE IN TYPHOID FEVER 1-week 2- week 3- week 4- week 5- week “cerebral-like swelling” of solitary follicules and Peyer's patches – proliferation of typhoid cells Massive secondary entrance of S. typhi on background of hyperreactivity leads to formation of local necrosis of follicles Seizure of necrotic masses and formation of ulcers. Perforation of intestinal wall or bleeding are possible. Full ablution of ulcers (“clear ulcers”). Perforation of intestinal wall or bleeding are possible. Healing of ulcers without formation of scars. CLINICAL CLASSIFICATION I. Typical forms - mild - moderate - severe - very severe II. Atypical forms - oblitereted - abortive - ambulatory III. Masked forms pneumotyphus, nephrotyphus, meningotyphus, encephalotyphus, colonotyphus IV. Bacteria carrying - acute (about 3 month) - chronic (long time, sometimes lifelong). - transitional (singular detection of the pathogen,without specific changes in immune system). Periods I. Incubation 9-14 days (3-60) II. Initial Stadium incrementi 1st week III. Climax Stadium fastigii 2-4th week IV. Decreasing of symptoms. Cjnvalescence Stadium decrementi 5th week . Initial period Stadium incrementi 1st week of the disease • • • • • • • • • Moderate increasing of temperature, Constant headache, Disorders of sleeping, insomnia (from the 5th day) Increasing weakness, loss of apetite Skin is pale. Abdominal distension. Constipation. Relative bradicardia, decreasing of BP. Presence of Padalka symptom. Hepatosplenomegaly (from the 5th day). TYPHOID FEVER. TYPES OF TEMPERATURE CURVES DAY OF DISEASE 1 3 5 7 9 11 13 15 17 19 21 23 25 27 29 31 33 35 37 39 41 43 45 47 49 51 1 53 41 42 40 41 4 7 10 13 16 19 22 25 28 31 34 37 40 43 46 49 52 55 58 61 64 67 70 73 40 39 39 38 38 37 37 36 36 35 35 Botkin, 1868 Wunderlich, 1856 1 3 5 7 9 11 13 15 17 19 21 23 25 27 29 31 33 35 37 39 41 43 45 47 49 51 53 55 42 1 3 5 7 9 11 13 15 17 19 21 23 25 27 29 31 33 35 37 39 38 41 40 37 39 38 36 37 36 35 35 Kildushevsky Irregular 41 43 45 47 49 51 53 55 57 59 Climax period (Stadium fastigii ) (2-4th week of the disease) • • • • • • • • • • • Fever is maximal and stable. Constant headache, insomnia. Patient is adynamic, apathetic. Skin is pale. Rose spots (from the 8-10 d of the disease). Relative bradycardia and dicrotic pulse (double beat, the second beat weaker than the first) Fuliginous “typhoid” tongue. Severe abdominal distension. Some patients experience foul, green-yellow, liquid diarrhea (pea soup diarrhea), some – constipations. Hepatosplenomegaly. Padalka sign. Philippovich sign. “Typhoid state” - prolonged apathy, lethargy, confusion, delirium, hallucinations, disorientation. Possibility of intestinal bleeding and perforation. . Characteristics of exanthema • • • • • Rose spots, Rash is monomorphic salmon-colored, blanching, truncal (abdomen and lower part of thorax), • usually 1-5 mm wide • not abundant (3-10 elem.); • generally resolve within 2-5 days Convalescence period (Stadium decrementi) 5th week of the disease. • Gradual decreasing of temperature and intoxication. • Decrease of headache. • Better sleep, appetite. The clinical course of typhoid fever may deviate from the description of classic disease. • The timing of the symptoms and host response may vary based on geographic region, race factors, and the infecting bacterial strain. • The stepladder fever pattern that was once the hallmark of typhoid fever now occurs in as few as 12% of cases. • In most contemporary presentations of typhoid fever, the fever has a steady insidious onset. • Young children, individuals with AIDS, and one third of immunocompetent adults who develop typhoid fever develop diarrhea rather than constipation. COMPLICATIONS OF TYPHOID FEVER Specific • • • • Intestinal bleeding; Intestinal perforation; Toxic shock; Status typhosus; Nonspecific • • • • • • pneumonia; parotitis; abscesses; otitis; pyelitis; trombophlebitis; • exacerbation; • relapse INTESTINAL BLEEDING (1-8%) Paleness of skin Dryness of mucous membranes Dizzines, tinnitus, severe weakness Decreasing of temperature Tachycardia “Cross” or “scissors” sign Hypotonia Meteorism and hyperperistalsis Detection of blood in feaces (blobs or “melena”) PERFORATION OF INTESTINE (0,3-8%) Abrupt pain in abdomen (nonsevere) Local muscular defense in right iliac region, Depression of peristaltic Abdomen does not take part in breathing Absence of hepatic dullness Peritonitis with increasing of intoxication, enteroparesis, dryness of a tongue, tachycardia meteorism without wind peritoneal signs Leucocytosis in blood test PERFORATION OF INTESTINE (0,3-8%) Relapse • 5-20% of typhoid fever cases that have apparently been treated successfully. • A relapse is heralded by the return of fever soon after the completion of antibiotic treatment. • The clinical manifestation is frequently milder than the initial illness. • Cultures should be obtained and standard treatment should be administered. MOST FREAQUENT REASONS AND SIGNS OF RELAPSES • Reasons: • – genetic peculiarities; • – immunodeficiency; • – faults of treatment (insensibility of antibiotics or low dosage, early cancellation). • Signs: • – prolonged subfebrile temperature; • – prolonged hepatosplenomegaly; • – stable meteorism (wind); • – Low titers of serum antibodies; • – aneosinophilia. Differential diagnosis of typhoid fever Paratyphoid А and В, generalized Influenza, ARVI, pneumonia. Sepsis. Louse – borne typhus. Brucellosis. Viral Hepatitis Malaria Tuberculosis. salmonellosis. DIFFERENTIAL DIAGNOSIS OF PARATYPHOID A AND B PARATYPHOID А - anthroponosis (sick persons or carriers) - incubation period - 8-10 days - acute onset (50%); - fever is remittent, sometimes – hectic; - affection of respiratory system from the beginning of disease (cough, sore throat, dysphonia); - dyspepsia; - hyperemia of skin and sclera, signs of pharyngitis; - chills and sweating are possible; - rash appears on 5-7 day, polymorphic, plentiful, on trunk, upper extremities; - status typhosus is rare - in blood – normal WBC or leucocytosis; - relapses more frequent, perforation or bleeding are rare; - rather mild, moderate course. PARATYPHOID В -Zooanthroponosis (sick persons, livestock, poultry) ; -- incubation period is shorter (5-8 days); - acute onset, -- fever is subfebrile or remittent, continue during 1-5 days - Gastrointestinal syndrome – nausea, vomiting, diarrhea -hyperemia of skin and sclera -Chills, sweating - Rash appears on 4-5 day, polymorphic, plentiful, sometimes on skin of face; - status typhosus is rare in blood leucocytosis, ESR increasing; - Clinical course can be severe, accompanied with meningitis, sepsis. - rather mild, subclinical course (1-3 days) CLINICAL CLASSIFICATION OF PARATYPHOID FEVER • Typhoid form Paratyphoid А – 50 – 60% Paratyphoid В – 10 – 12% • Catarrhal form Paratyphoid А – 20 – 25% Paratyphoid В – 10 – 12% • Gastrointestinal form Paratyphoid В – 60 – 65% • Mixed forms Diagnostics • CBC: Initial period – moderate leucocytosis or normocytosis , shift to the left, an elevated ESR • Climax period – leucopenia, aneosinophilia, lymphomonocytosis, thrombocytopenia, an elevated ESR. • Urine test – no specific changes. • Additional methods • • • • X-ray of lungs X-ray of abdomen ECG USI Specific diagnostics • Culture: blood, urine, bile, faeces, bone marrow, rose spots. • Hemoculture is positive during all feverish period. Most frequent positive hemoculture on a first week. • Coproculture and urinoculture are positive from the second week. • Bone marrow culture is 90% sensitive until at least 5 days after commencement of antibiotics. However, this technique is extremely painful, which may outweigh its benefit • Bile culture – is obligatory component of diagnostics of convalescents. Duodenal intubation must be performed not earlier then 5th week of the disease (threat of perforation or bleeding). Wilson and Blair bismuth sulphite medium jet black colony with a metallic sheen Serologic tests • Widal test – was the traditional method for decades. Diagnostic titer - 1:200. It is not specific, due to O – antigen can be positive for other Salmonella groups. • Indirect hemagglutination is more specific. • Latex agglutination or coagglutination tests for antibody to the Vi antigen (sensitivity to 95%). • Indirect enzyme-linked immunosorbent assay (ELISA) for immunoglobulin M (IgM) and IgG antibodies to S typhi polysaccharide • Reaction of immune fluorescence - 100 times more specific then Widal test. • Polymerase chain reaction (PCR) PRINCIPLES OF TREATMENT OF TYPHOID FEVER • Strict bed rest up to 5-10th day of normal temperature; • Diet N 2 up to 5th week of disease; • Antibacterial treatment up to 10th day of normal temperature; • Pathogenic treatment: • Desintoxication (40 ml/kg per day) PO, IV; • Vitamins B, C; • Desensibilisation; • Glucocorticoids (shock, delirium). Antibacterial treatment • Chloramphenicol was used universally to treat typhoid fever from 1948 until the 1970s, when widespread resistance occurred. • Ampicillin and trimethoprim-sulfamethoxazole (TMP-SMZ) then became treatments of choice. However, in the late 1980s, some S typhi and S paratyphi strains developed simultaneous plasmid-mediated resistance to all three of these agents. Antibacterial treatment • Fluoroquinolones (ciprofloxacin, ofloxacin, levofloxacin, gatifloxacin) are now recommended by most authorities for the treatment of typhoid fever. • Unfortunately, resistance to first-generation fluoroquinolones is widespread in many parts of Asia. Antibacterial treatment • Therefore, for strains that originate outside of south or Southeast Asia, the WHO recommendations are: • uncomplicated disease should be treated empirically with oral ciprofloxacin and • complicated typhoid fever from these regions should be treated with intravenous ciprofloxacin Guideline for the treatment of typhoid fever in south Asia (Indian Association of Pediatrics) • For empiric treatment of uncomplicated typhoid fever, the IAP recommends cefixime and, as a second-line agent, azithromycin. • For complicated typhoid fever, they recommend ceftriaxone. Aztreonam and imipenem are second-line agents for complicated cases. There is opinion, if the origin of the infection is unknown, the combination of a first-generation fluoroquinolone and a third-generation cephalosporin should be used. the combination of azithromycin and fluoroquinolones is not recommended because it may cause QT prolongation and is relatively contraindicated. PRINCIPLES OF TRATMENT OF TYPHOID FEVER Drug Dosage Duration Course Levomycetin (Chloramfenicol) Ampicillin, amoxicillin Co-trimoxazol (Biseptol) Azitromicin 50-75 mg/kg 4 td 14-21 Uncomplicated 75-100 mg/kg 3 td 14 Uncomplicated 8 mg/kg 2 td 14 Uncomplicated 10 mg/kg 1 td 7 Uncomplicated Ceftriaxon 60 mg/kg 1 td 10-14 Cefotoxim 80 mg/kg 2-3 td 10-14 Cyprofloxacin 20 mg/kg 2 td 10-14 severe, complicated severe, complicated severe, complicated Treatment of GI complication • Patients with intestinal haemorrhage need intensive care, monitoring and blood transfusion. Surgical intervention is not needed unless there is significant blood loss. • Strict bed rest • Cold compress on a stomach • Fasting on 10 – 12 hours • Further begin feeding by broths, jelly, mousse, kissel • For stoppage of bleeding – dicinonum, calcium chloride, vicasolum, aminocapronic acid, plasma • In the absence of effect – surgical intervention – an intestinal resection • Surgical consultation for suspected intestinal perforation is indicated. • If perforation is confirmed, surgical repair should not be delayed longer than six hours. Prevention For travelers Buy bottled drinking water or bring it to a rolling boil for one minute before drinking it. Ask for drinks without ice, unless the ice is made from bottled or boiled water. Avoid Popsicles and flavored ices. Eat food that have been thoroughly cooked and that are still hot and steaming. Avoid raw vegetables and food that cannot be peeled like lettuce. When eat raw fruit and vegetables that can be peeled, peel yourself. Don’t eat the peelings. Avoid foods and beverages from street vendors. Be vaccinated against typhoid while traveling to a country where typhoid is common. Need to complete your vaccination at least one week before travel. Typhoid vaccines lose their effectiveness after several years so check with your doctor to see if it is time for a booster vaccination. Indications for Vaccination 1.Travelers going to endemic areas who will be staying for a prolonged period of time, 2. Persons with intimate exposure to a documented S. typhi carrier 3. Microbiology laboratory technologists who work frequently with S. typhi 4. Military personnel Travelers should be vaccinated at least one week prior to departing for an endemic area. Typhoid fever vaccines • injected Vi capsular polysaccharide (ViCPS; Typhim Vi, Pasteur Merieux) antigen, • enteric Ty21a (Vivotif Berna, Swiss Serum and Vaccine Institute) live-attenuated vaccine, • an acetone-inactivated parenteral vaccine (used only in members of the armed forces). The efficacy of both vaccines available to the general public approaches 50%.