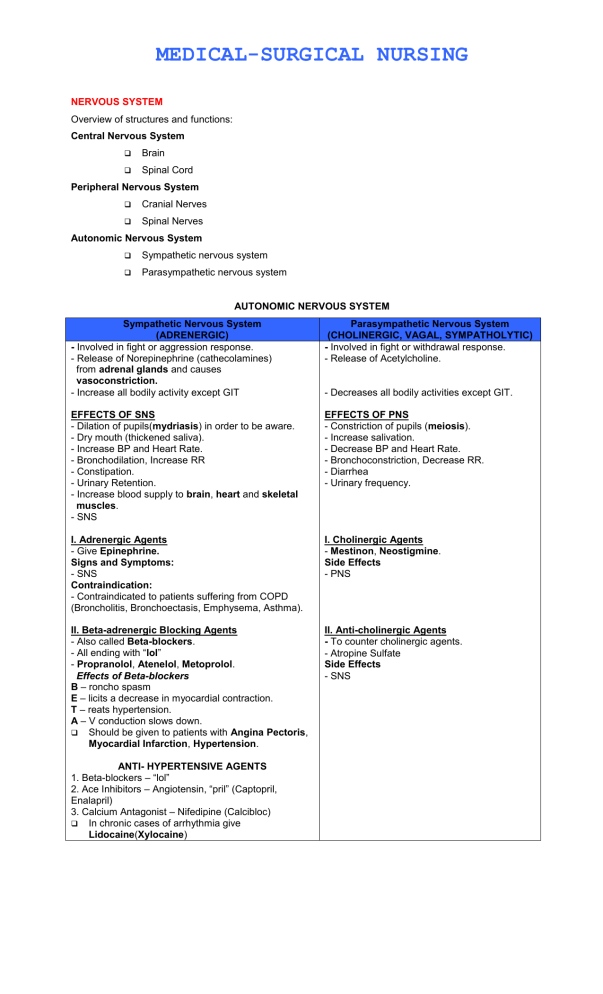
MEDICAL-SURGICAL NURSING NERVOUS SYSTEM Overview of structures and functions: Central Nervous System Brain Spinal Cord Peripheral Nervous System Cranial Nerves Spinal Nerves Autonomic Nervous System Sympathetic nervous system Parasympathetic nervous system AUTONOMIC NERVOUS SYSTEM Sympathetic Nervous System (ADRENERGIC) - Involved in fight or aggression response. - Release of Norepinephrine (cathecolamines) from adrenal glands and causes vasoconstriction. - Increase all bodily activity except GIT Parasympathetic Nervous System (CHOLINERGIC, VAGAL, SYMPATHOLYTIC) - Involved in fight or withdrawal response. - Release of Acetylcholine. EFFECTS OF SNS - Dilation of pupils(mydriasis) in order to be aware. - Dry mouth (thickened saliva). - Increase BP and Heart Rate. - Bronchodilation, Increase RR - Constipation. - Urinary Retention. - Increase blood supply to brain, heart and skeletal muscles. - SNS EFFECTS OF PNS - Constriction of pupils (meiosis). - Increase salivation. - Decrease BP and Heart Rate. - Bronchoconstriction, Decrease RR. - Diarrhea - Urinary frequency. I. Adrenergic Agents - Give Epinephrine. Signs and Symptoms: - SNS Contraindication: - Contraindicated to patients suffering from COPD (Broncholitis, Bronchoectasis, Emphysema, Asthma). I. Cholinergic Agents - Mestinon, Neostigmine. Side Effects - PNS II. Beta-adrenergic Blocking Agents - Also called Beta-blockers. - All ending with “lol” - Propranolol, Atenelol, Metoprolol. Effects of Beta-blockers B – roncho spasm E – licits a decrease in myocardial contraction. T – reats hypertension. A – V conduction slows down. Should be given to patients with Angina Pectoris, Myocardial Infarction, Hypertension. II. Anti-cholinergic Agents - To counter cholinergic agents. - Atropine Sulfate Side Effects - SNS ANTI- HYPERTENSIVE AGENTS 1. Beta-blockers – “lol” 2. Ace Inhibitors – Angiotensin, “pril” (Captopril, Enalapril) 3. Calcium Antagonist – Nifedipine (Calcibloc) In chronic cases of arrhythmia give Lidocaine(Xylocaine) - Decreases all bodily activities except GIT. CENTRAL NERVOUS SYSTEM Brain and Spinal Cord. I. CELLS A. NEURONS Basic cells for nerve impulse and conduction. PROPERTIES Excitability – ability of neuron to be affected by changes in external environment. Conductivity – ability of neuron to transmit a wave of excitation from one cell to another. Permanent Cell – once destroyed not capable of regeneration. TYPES OF CELLS BASED ON REGENERATIVE CAPACITY 1. Labile Capable of regeneration. Epidermal cells, GIT cells, GUT cells, cells of lungs. Capable of regeneration with limited time, survival period. Kidney cells, Liver cells, Salivary cells, pancreas. 2. Stable 3. Permanent Not capable of regeneration. Myocardial cells, Neurons, Bone cells, Osteocytes, Retinal Cells. B. NEUROGLIA Support and protection of neurons. TYPES 1. Astrocytes – maintains blood brain barrier semi-permeable. Majority of brain tumors (90%) arises from called astrocytoma. 2. Oligodendria 3. Microglia 4. Epindymal SUBSTANCES THAT CAN PASS THE BLOOD-BRAIN BARRIER 1. Ammonia Cerebral toxin Hepatic Encephalopathy (Liver Cirrhosis) Ascites Esophageal Varices Early Signs of Hepatic Encephalopathy asterixis (flapping hand tremors). Late Signs of Hepatic Encephalopathy Headache Dizziness Confusion Fetor hepaticus (ammonia like breath) Decrease LOC PATHOGNOMONIC SIGNS 1. PTB – low-grade afternoon fever. 2. PNEUMONIA – rusty sputum. 3. ASTHMA – wheezing on expiration. 4. EMPHYSEMA – barrel chest. 5. KAWASAKI SYNDROME – strawberry tongue. 6. PERNICIOUS ANEMIA – red beefy tongue. 7. DOWN SYNDROME – protruding tongue. 8. CHOLERA – rice watery stool. 9. MALARIA – stepladder like fever with chills. 10. TYPHOID – rose spots in abdomen. 11. DIPTHERIA – pseudo membrane formation 12. MEASLES – koplik’s spots. 13. SLE – butterfly rashes. 14. LIVER CIRRHOSIS – spider like varices. 15. LEPROSY – lioning face. 16. BULIMIA – chipmunk face. 17. APPENDICITIS – rebound tenderness. 18. DENGUE – petechiae or (+) Herman’s sign. 19. MENINGITIS – Kernig’s sign (leg pain), Brudzinski sign (neck pain). 20. TETANY – HYPOCALCEMIA (+) Trousseau’s sign/carpopedal spasm; Chvostek sign (facial spasm). 21. TETANUS – risus sardonicus. 22. PANCREATITIS – Cullen’s sign (ecchymosis of umbilicus); (+) Grey turners spots. 23. PYLORIC STENOSIS – olive like mass. 24. PDA – machine like murmur. 25. ADDISON’S DISEASE – bronze like skin pigmentation. 26. CUSHING’S SYNDROME – moon face appearance and buffalo hump. 27. HYPERTHYROIDISM/GRAVE’S DISEASE – exopthalmus. 28. INTUSSUSCEPTION – sausage shaped mass 2. Carbon Monoxide and Lead Poisoning Can lead to Parkinson’s Disease. Epilepsy Treat with ANTIDOTE: Calcium EDTA. 3. Type 1 DM (IDDM) Causes diabetic ketoacidosis. And increases breakdown of fats. And free fatty acids Resulting to cholesterol and (+) to Ketones (CNS depressant). Resulting to acetone breath odor/fruity odor. KUSSMAUL’S respiration, a rapid shallow respiration. Which may lead to diabetic coma. Signs of jaundice (icteric sclerae). Caused by bilirubin (yellow pigment) Increase bilirubin in brain (Kernicterus). Causing irreversible brain damage. 4. Hepatitis 5. Bilirubin Astrocites Maintains integrity of blood brain barrier. Oligodendria Produces myelin sheath in CNS Act as insulator and facilitates rapid nerve impulse transmission. DEMYELINATING DISORDERS 1. ALZHEIMER’S DISEASE Atrophy of brain tissues. Sign and Symptoms 4 A’s of Alzheimer a. Amnesia – loss of memory. b. Agnosia – no recognition of inanimate objects. c. Apraxia – no recognition of objects function. d. Aphasia – no speech (nodding). *Expressive aphasia “motor speech center” Broca’s Aphasia *Receptive aphasia inability to understand spoken words. Wernicke’s Aphasia General Knowing Gnostic Area or General Interpretative Area. DRUG OF CHOICE: ARICEPT (taken at bedtime) and COGNEX. 2. MULTIPLE SCLEROSIS Chronic intermittent disorder of CNS characterized by white patches of demyelination in brain and spinal cord. Characterized by remission and exacerbation. Women ages 15-35 are prone Unknown Cause Slow growing virus Autoimmune disorders Pernicious anemia Myasthenia gravis Lupus Hypothyroidism GBS Ig G – only antibody that pass placental circulation causing passive immunity. - short term protection. - Immediate action. Ig A – present in all bodily secretions (tears, saliva, colostrums). Ig M – acute in inflammation. Ig E – for allergic reaction. Ig D – for chronic inflammation. * Give palliative or supportive care. Signs and Symptoms 1. Visual disturbances blurring of vision (primary) diplopia (double vision) scotomas (blind spots) 2. Impaired sensation to touch, pain, pressure, heat and cold. tingling sensation paresthesia numbness 3. Mood swings euphoria (sense of well being) 4. Impaired motor function weakness spasticity paralysis 5. Impaired cerebral function scanning speech TRIAD SIGNS OF MS Ataxia (Unsteady gait, (+) Romberg’s test) CHARCOTS TRIAD IAN Intentional tremors Nystagmus 6. Urinary retention/incontinence 7. Constipation 8. Decrease sexual capacity DIAGNOSTIC PROCEDURE CSF analysis (increase in IgG and Protein). MRI (reveals site and extent of demyelination). (+) Lhermitte’s sign a continuous and increase contraction of spinal column. NURSING MANAGEMENT 1. Administer medications as ordered a. ACTH (Adreno Corticotropic Hormone)/ Steroids for acute exacerbation to reduce edema at site of demyelination to prevent paralysis. b. Baclofen (Dioresal)/ Dantrolene Sodium (Dantrene) – muscle relaxants. c. Interferons – alter immune response. d. Immunosupresants 2. Maintain side rails to prevent injury related to falls. 3. Institute stress management techniques. a. Deep breathing exercises b. Yoga 4. Increase fluid intake and increase fiber to prevent constipation. 5. Catheterization to prevent retention. a. Diuretics b. Bethanicol Chloride (Urecholine) Nursing Management Only given subcutaneous. Monitor side effects bronchospasm and wheezing. Monitor breath sounds 1 hour after subcutaneous administration. c. For Urinary Incontinence Anti spasmodic agent a. Prophantheline Bromide (Promanthene) Acid ash diet like cranberry juice, plums, prunes, pineapple, vitamin C and orange. To acidify urine and prevent bacterial multiplication. COMMON CAUSE OF UTI Female short urethra (3-5 cm, 1-1 ½ inches) poor perineal hygiene vaginal environment is moist Nursing Management avoid bubble bath (can alter Ph of vagina). avoid use of tissue papers avoid using talcum powder and perfume. Urethra (20 cm, 8 inches) urinate after intercourse Male MICROGLIA stationary cells that carry on phagocytosis (engulfing of bacteria or cellular debris, eating), pinocytosis (cell drinking). MACROPHAGE ORGAN Microglia Brain Monocytes Blood Kupffers cells Kidney Histiocytes Skin Alveolar Lung Macrophage EPINDYMAL CELLS Secretes a glue called chemo attractants that concentrate the bacteria. COMPOSITION OF BRAIN 80% brain mass 10% blood 10% CSF I. Brain Mass PARTS OF THE BRAIN 1. CEREBRUM largest part composed of the Right Cerebral Hemisphere and Left Cerebral Hemisphere enclosed in the Corpus Callosum. Functions of Cerebrum integrative sensory motor Lobes of Cerebrum 1. Frontal higher cortical thinking controls personality controls motor activity Broca’s Area (motor speech area) when damaged results to garbled speech. 2. Temporal hearing short term memory for appreciation discrimination of sensory impulses to pain, touch, pressure, heat, cold, numbness. 3. Parietal 4. Occipital for vision Insula (Island of Reil) visceral function activities of internal organ like gastric motility. Limbic System (Rhinencephalon) controls smell and if damaged results to Anosmia (absence of smell). controls libido controls long term memory 2. BASAL GAGLIA areas of grey matter located deep within each cerebral hemisphere. release dopamine (controls gross voluntary movement. NEURO TRANSMITTER DECREASE INCREASE Acethylcholine Myasthenia Gravis Bi-polar Disorder Dopamine Parkinson’s Disease Schizophrenia 3. MIDBRAIN/ MESENCEPHALON acts as relay station for sight and hearing. size of pupil is 2 – 3 mm. equal size of pupil is isocoria. unequal size of pupil is anisocoria. hearing acuity is 30 – 40 dB. positive PERRLA 4. INTERBRAIN/ DIENCEPHALON Parts of Diencephalon A. Thalamus acts as relay station for sensation. B. Hypothalamus controls temperature (thermoregulatory center). controls blood pressure controls thirst appetite/satiety sleep and wakefulness controls some emotional responses like fear, anxiety and excitement. controls pituitary functions androgenic hormones promotes secondary sex characteristics. early sign for males are testicular and penile enlargement late sign is deepening of voice. early sign for females telarche and late sign is menarche. 5. BRAIN STEM located at lowest part of brain Parts of Brain Stem 1. Pons pneumotaxic center controls the rate, rhythm and depth of respiration. 2. Medulla Oblongata controls respiration, heart rate, swallowing, vomiting, hiccup, vasomotor center (dilation and constriction of bronchioles). 3. Cerebellum smallest part of the brain. lesser brain. controls balance, equilibrium, posture and gait. INTRA CRANIAL PRESSURE Monroe Kellie Hypothesis Skull is a closed container Any alteration or increase in one of the intracranial components Increase intra-cranial pressure (normal ICP is 0 – 15 mmHg) Cervical 1 – also known as ATLAS. Cervical 2 – also known as AXIS. Foramen Magnum Medulla Oblongata Brain Herniation Increase intra cranial pressure * Alternate hot and cold compress to prevent HEMATOMA CSF cushions brain (shock absorber) Obstruction Early of flow of CSF will lead to enlargement of skull posteriorly called hydrocephalus. closure of posterior fontanels causes posterior enlargement of skull in hydrocephalus. NEUROLOGIC DISORDERS INCREASE INTRACRANIAL PRESSURE – increase in intra-cranial bulk brought about by an increase in one of the 3 major intra cranial components. Causes: head trauma/injury inflammatory condition (stroke) localized abscess hydrocephalus cerebral edema tumor (rarely) hemorrhage Signs and Symptoms (Early) decrease LOC lethargy/stupor restlessness/agitation coma irritability Signs and Symptoms (Late) changes in vital signs blood pressure (systolic blood pressure increases but diastolic remains the same). widening of pulse pressure is neurologic in nature (if narrow cardiac in nature). heart rate decrease respiratory rate decrease temperature increase directly proportional to blood pressure. projective vomiting headache papilledema (edema of optic disc) abnormal posturing decorticate posturing (damage to cortex and spinal cord). decerebrate posturing (damage to upper brain stem that includes pons, cerebellum and midbrain). unilateral dilation of pupils called uncal herniation bilateral dilation of pupils called tentorial herniation resulting to mild headache possible seizure activity Nursing Management 1. Maintain patent and adequate ventilation by: a. Prevention of hypoxia and hypercarbia Early signs of hypoxia restlessness agitation tachycardia Late signs of hypoxia Bradycardia Extreme restlessness Dyspnea Cyanosis HYPERCARBIA Increase CO2 (most powerful respiratory stimulant) retention. In chronic respiratory distress syndrome decrease O2 stimulates respiration. b. Before and after suctioning hyper oxygenate client 100% and done 10 – 15 seconds only. c. Assist in mechanical ventilation 2. Elevate bed of client 30 – 35o angle with neck in neutral position unless contraindicated to promote venous drainage. 3. Limit fluid intake to 1200 – 1500 ml/day (in force fluids 2000 – 3000 ml/day). 4. Monitor strictly input and output and neuro check 5. Prevent complications of 6. Prevent further increase ICP by: a. provide an comfortable and quite environment. b. avoid use of restraints. c. maintain side rails. d. instruct client to avoid forms of valsalva maneuver like: straining stool excessive vomiting (use anti emetics) excessive coughing (use anti tussive like dextromethorphan) avoid stooping/bending avoid lifting heavy objects e. avoid clustering of nursing activity together. 7. Administer medications like: a. Osmotic diuretic (Mannitol) for cerebral diuresis Nursing Management monitor vital signs especially BP (hypotension). monitor strictly input and output every 1 hour notify physician if output is less 30 cc/hr. administered via side drip regulated fast drip to prevent crystal formation. b. Loop diuretic (Lasix, Furosemide) Drug of choice for CHF (pulmonary edema) Loop of Henle in kidneys. Nursing Management Monitor vital signs especially BP (hypotension). monitor strictly input and output every 1 hour notify physician if output is less 30 cc/hr. administered IV push or oral. given early morning immediate effect of 10 – 15 minutes. maximum effect of 6 hours. c. Corticosteroids Dexamethasone (Decadron) Hydrocortisone Prednisone (to reduce edema that may lead to increase ICP) Mild Analgesics (Codeine Sulfate for respiratory depression) Anti Convulsants (Dilantin, Phenytoin) *CONGESTIVE HEART FAILURE Signs and Symptoms dyspnea orthopnea paroxysmal nocturnal dyspnea productive cough frothy salivation cyanosis rales/crackles bronchial wheezing pulsus alternans anorexia and general body malaise PMI (point of maximum impulse/apical pulse rate) is displaced laterally S3 (ventricular gallop) Predisposing Factors/Mitral Valve RHD Aging TREATMENT Morphine Sulfate Aminophelline Digoxin Diuretics Oxygen Gases, blood monitor RIGHT CONGESTIVE HEART FAILURE (Venous congestion) Signs and Symptoms jugular vein distention (neck) ascites pitting edema weight gain hepatosplenomegaly jaundice pruritus esophageal varices anorexia and general body malaise Signs and Symptoms of Lasix in terms of electrolyte imbalances 1. Hypokalemia decrease potassium level normal value is 3.4 – 5.5 meq/L Sign and Symptoms weakness and fatigue constipation positive U wave on ECG tracing Nursing Management administer potassium supplements as ordered (Kalium Durule, Oral Potassium Chloride) increase intake of foods rich in potassium FRUITS VEGETABLES Apple Asparagus Banana Brocolli Cantalope Carrots Oranges Spinach 2. Hypocalcemia/ Tetany decrease calcium level normal value is 8.5 – 11 mg/100 ml Signs and Symptoms tingling sensation paresthesia numbness (+) Trousseau’s sign/ Carpopedal spasm (+) Chvostek’s sign Complications Arrhythmia Seizures Nursing Management Calcium Gluconate per IV slowly as ordered * Calcium Gluconate toxicity – results to SEIZURE Magnesium Sulfate Magnesium Sulfate toxicity S/S BP Urine output DECREASE Respiratory rate Patellar relfex absent 3. Hyponatremia decrease sodium level normal value is 135 – 145 meq/L Signs and Symptoms hypotension dehydration signs (Initial sign in adult is THIRST, in infant TACHYCARDIA) agitation dry mucous membrane poor skin turgor weakness and fatigue Nursing Management force fluids administer isotonic fluid solution as ordered 4. Hyperglycemia normal FBS is 80 – 100 mg/dl Signs and Symptoms polyuria polydypsia polyphagia Nursing Management monitor FBS 5. Hyperuricemia increase uric acid (purine metabolism) foods high in uric acid (sardines, organ meats and anchovies) *Increase in tophi deposit leads to Gouty arthritis. Signs and Symptoms joint pain (great toes) swelling Nursing Management force fluids administer medications as ordered a. Allopurinol (Zyloprim) Drug of choice for gout. Mechanism of action: inhibits synthesis of uric acid. b. Colchecine Acute gout Mechanism of action: promotes excretion of uric acid. * KIDNEY STONES Signs and Symptoms renal colic Cool moist skin Nursing Management force fluids administer medications as ordered a. Narcotic Analgesic Morphine Sulfate ANTIDOTE: Naloxone (Narcan) toxicity leads to tremors. b. Allopurinol (Zyloprim) Side Effects Respiratory depression (check for RR) PARKINSON’S DISEASE/ PARKINSONISM Chronic progressive disorder of CNS characterized by degeneration of dopamine producing cells in the SUBSTANCIA NIGRA of the midbrain and basal ganglia. Predisposing Factors 1. Poisoning (lead and carbon monoxide) 2. Arteriosclerosis 3. Hypoxia 4. Encephalitis 5. Increase dosage of the following drugs: a. Reserpine(Serpasil) b. Methyldopa(Aldomet) AntihypertensiveS c. Haloperidol(Haldol) d. Phenothiazine AntipsychoticS SIDE EFFECTS RESERPINE Major depression leading to suicide Aloneness Multiple loss causes suicide Loss of spouse Loss of Job direct approach towards the client close surveillance is a nursing priority time to commit suicide is on weekends early morning Signs and Symptoms for Parkinson’s pill rolling tremors of extremities especially the hands. bradykinesia (slowness of movement) rigidity (cogwheel type) stooped posture shuffling and propulsive gait over fatigue mask like facial expression with decrease blinking of the eyes. difficulty rising from sitting position. Monotone type speech mood lability (in state of depression) increase salivation (drooling type) autonomic changes a. increase sweating b. increase lacrimation c. seborrhea d. constipation e. decrease sexual capacity Nursing Management 1. Administer medications as ordered Anti Parkinsonian agents Levodopa (L-dopa) short acting Amantadine Hydrochloride (Symmetrel) Carbidopa (Sinemet) Mechanism of Action increase level of dopamine Side Effects GIT irritation (should be taken with meals orthostatic hypotension arrhythmia hallucinations Contraindications clients with narrow angle closure glaucoma clients taking MAOI’s (no foods with triptophan and thiamine) urine and stool may be darkened no Vitamin B6 (Pyridoxine) reverses the therapeutic effects of Levodopa * Increase Vitamin B when taking INH (Isoniazid), Isonicotinic Acid Hydrazide Anti Cholinergic Agents (ARTANE and COGENTIN) - to relieve tremors Mechanism of Action inhibits action of acethylcholine Side Effects SNS Anti Histamine (Dipenhydramine Hydrochloride) Side Effects Adult: drowsiness Children: CNS excitement (hyperactivity) because blood brain barrier is not yet fully developed. Dopamine Agonist - relieves tremor rigidity Bromocriptene Hydrochloride (Parlodel) Side Effects Respiratory depression 2. Maintain side rails to prevent injury 3. Prevent complications of immobility 4. Decrease protein in morning and increase protein in afternoon to induce sleep 5. Encourage increase fluid intake and fiber. 6. Assist/supervise in ambulation 7. Assist in Stereotaxic Thalamotomy MAGIC 2’s IN DRUG MONITORING DRUG NORMAL RANGE Digoxin/ Lanoxin (Increase force of cardiac output) Lithium/ Lithane (Decrease level of Ach/NE/Serotonin) Aminophylline (Dilates bronchial tree) Dilantin/ Phenytoin Acetaminophen/Tylenol .5 – 1.5 meq/L TOXICITY LEVEL 2 .6 – 1.2 meq/L INDICATION CLASSIFICATION CHF Cardiac Glycoside 2 Bipolar Anti-Manic Agents 10 – 19 mg/100 ml 20 COPD Bronchodilators 10 – 19 mg/100 ml 10 – 30 mg/100 ml 20 200 Seizures Osteo Arthritis Anti-Convulsant Non-narcotic Analgesic 1. Digitalis Toxicity Signs and Symptoms nausea and vomiting diarrhea confusion photophobia changes in color perception (yellowish spots) Antidote: Digibind 2. Lithium Toxicity Signs and Symptoms anorexia nausea and vomiting diarrhea dehydration causing fine tremors hypothyroidism Nursing Management force fluids increase sodium intake to 4 – 10 g% daily 3. Aminophylline Toxicity Signs and Symptoms tachycardia palpitations CNS excitement (tremors, irritability, agitation and restlessness) Nursing Management only mixed with plain NSS or 0.9 NaCl to prevent development of crystals or precipitate. administered sandwich method avoid taking alcohol because it can lead to severe CNS depression avoid caffeine 4. Dilantin Toxicity Signs and Symptoms gingival hyperplasia (swollen gums) hairy tongue ataxia nystagmus Nursing Management provide oral care massage gums 5. Acetaminophen Toxicity Signs and Symptoms hepatotoxicity (monitor for liver enzymes) SGPT/ALT (Serum Glutamic Pyruvate Transaminace) SGOT/AST (Serum Glutamic Oxalo-Acetil Transaminace) nephrotoxicity monitor BUN (10 – 20) and Creatinine (.8 – 1) hypoglycemia Tremors, tachycardia Irritability Restlessness Extreme fatigue Diaphoresis, depression Antidote: Acetylcisteine (mucomyst) prepare suction apparatus as bedside. MYASTHENIA GRAVIS neuromuscular disorder characterized by a disturbance in the transmission of impulses from nerve to muscle cells at the neuromuscular junction leading to descending muscle weakness. Incidence rate: women 20 – 40 years old Predisposing factors unknown autoimmune: it involves release of cholinesterase an enzyme that destroys Ach. Signs and Symptoms initial sign is ptosis a clinical parameter to determine ptosis is palpebral fissure. diplipia mask like facial expression dysphagia hoarseness of voice respiratory muscle weakness that may lead to respiratory arrest extreme muscle weakness especially during exertion and morning Diagnostic Procedure Tensilon test (Edrophonium Hydrochloride) provides temporary relief of signs and symptoms for about 5 – 10 minutes and a maximum of 15 minutes. if there is no effect there is damage to occipital lobe and midbrain and is negative for M.G. Nursing Management 1. airway 2. aspiration maintain patent airway and adequate ventilation 3. mmobility * assist in mechanical ventilation and monitor pulmonary function test * monitor strictly vital signs, input and output and neuro check * monitor strength or motor grading scale 4. maintain side rails to prevent injury related to falls 5. institute NGT feeding 6. administer medications as ordered a. Cholinergic (Mestinon) b. Anti Cholenisterase (Neostegmin) Mechanism of Action increase level of Ach Side Effects PNS Cortocosteroids suppress immune response monitor for 2 types of crisis: MYASTHENIC CRISIS Causes: - under medication - stress - infection Signs and Symptoms - The client is unable to see, swallow, speak, breathe Treatment - administer cholinergic agents as ordered CHOLINERGIC CRISIS Cause: - over medication Signs and Symptoms - PNS Treatment - Administer anti cholinergic agents (Atropine Sulfate) 7. Assist in surgical procedure known as thymectomy because it is believed that the thymus gland is responsible for M.G. 8. Assist in plasma paresis and removing auto immune anti bodies 9. Prevent complications INFLAMMATORY CONDITIONS OF THE BRAIN MENINGITIS Meninges 3 fold membrane that covers brain and spinal cord. for support and protection for nourishment blood supply LAYERS OF THE MENINGES 1. Dura matter – outer layer 2. Arachnoid – middle layer 3. Pia matter – inner layer subdural space between the dura and arachnoid subarachnoid space between the arachnoid and pia, CSF aspiration is done. A. Etiology 1. Meningococcus – most dangerous 2. Pneumococcus 3. Streptococcus - causes adult meningitis 4. Hemophilus Influenzae – causes pediatric meningitis B. Mode of transmission airborne transmission (droplet nuclei) C. Signs and Symptoms headache photophobia projectile vomiting fever, chills, anorexia, general body malaise and weight loss Possible increase in ICP and seizure activity Abnormal posturing (decorticate and decerebrate) Signs of meningeal irritation a. Nuchal rigidity or stiff neck b. Opisthotonus (arching of back) c. (+) Kernig’s sign (leg pain) d. (+) Brudzinski sign (neck pain) D. Diagnostic Procedures Lumbar puncture: a hollow spinal needle is inserted in the subarachnoid space between the L3 – L4 to L5. Nursing Management for LP Before Lumbar Puncture 1. Secure informed consent and explain procedure. 2. Empty bladder and bowel to promote comfort. 3. Encourage to arch back to clearly visualize L3-L4. Post Lumbar Puncture 1. Place flat on bed 12 – 24 o 2. Force fluids 3. Check punctured site for any discoloration, drainage and leakage to tissues. 4. Assess for movement and sensation of extremities. CSF analysis reveals 1. Increase CHON and WBC 2. Decrease glucose 3. Increase CSF opening pressure (normal pressure is 50 – 100 mmHg) 4. (+) cultured microorganism (confirms meningitis) CBC reveals 1. Increase wbc E. Nursing Management 1. Enforce complete bed rest 2. Administer medications as ordered a. Broad spectrum antibiotics (Penicillin, Tetracycline) b. Mild analgesics c. Anti pyretics 3. Institute strict respiratory isolation 24 hours after initiation of anti biotic therapy 4. Elevate head 30-45o 5. Monitor strictly V/S, input and output and neuro check 6. Institute measures to prevent increase ICP and seizure. 7. Provide a comfortable and darkened environment. 8. Maintain fluid and electrolyte balance. 9. Provide client health care and discharge planning concerning: a. Maintain good diet of increase CHO, CHON, calories with small frequent feedings. b. Prevent complications most feared is hydrocephalus hearing loss/nerve deafness is second complication consult audiologist c. Rehabilitation for neurological deficit mental retardation delayed psychomotor development CVA (STROKE/BRAIN ATTACK/ ADOPLEXY/ CEREBRAL THROMBOSIS) a partial or complete disruption in the brains blood supply. 2 most common cerebral artery affected by stroke a. Mid Cerebral Artery b. Internal Cerebral Artery – the 2 largest artery A. Incidence Rate men are 2-3 times high risk B. Predisposing Factors thrombus (attached) embolus (detached and most dangerous because it can go to the lungs and cause pulmonary embolism or the brain and cause cerebral embolism. Signs and Symptoms of Pulmonary Embolism Sudden sharp chest pain Unexplained dyspnea Tachycardia Palpitations Diaphoresis Mild restlessness Signs and Symptoms of Cerebral Embolism Headache and dizziness Confusion Restlessness Decrease LOC Fat embolism is the most feared complications after femur fracture. Yellow bone marrow are produced from the medullary cavity of the long bones and produces fat cells. If there is bone fracture there is hemorrhage and there would be escape of the fat cells in the circulation. Compartment syndrome (compression of arteries and nerves) C. Risk Factors 1. Hypertension, Diabetes Mellitus, Myocardial Infarction, Atherosclerosis, Valvular Heart Disease, Post Cardiac Surgery (mitral valve replacement) 2. Lifestyle (smoking), sedentary lifestyle 3. Obesity (increase 20% ideal body weight) 4. Hyperlipidemia more on genetics/genes that binds to cholesterol 5. Type A personality a. deadline driven b. can do multiple tasks c. usually fells guilty when not doing anything 6. Related to diet: increase intake of saturated fats like whole milk 7. Related stress physical and emotional 8. Prolong use of oral contraceptives promotes lypolysis (breakdown of lipids) leading to atherosclerosis that will lead to hypertension and eventually CVA. D. Signs and Symptoms dependent on stages of development Initial sign of stroke or warning sign 1. TIA Signs and Symptoms headache and dizziness tinnitus visual and speech disturbances paresis (plegia) possible increase ICP 2. Stroke in evolution progression of signs and symptoms of stroke 3. Complete stroke resolution phase characterized by: Signs and Symptoms headache and dizziness Cheyne Stokes Respiration anorexia, nausea and vomiting dysphagia (+) Kernig’s sign and Brudzinski sign which may lead to hemorrhagic stroke focal neurological deficits a. phlegia b. aphasia c. dysarthria (inability to articulate words) d. alexia (difficulty reading) e. agraphia (difficulty writing) f. homonymous hemianopsia (loss of half of visual field) E. Diagnostic Procedure 1. CT Scan – reveals brain lesions 2. Cerebral Arteriography reveals the site and extent of malocclusion uses dye for visualization most of dye are iodine based check for shellfish allergy after diagnostic exam force fluids to release dye because it is nephro toxic check for distal pulse (femoral) check for hematoma formation F. Nursing Management 1. Maintain patent airway and adequate ventilation by: a. assist in mechanical ventilation b. administrate O2 inhalation 2. Restrict fluids to prevent cerebral edema that might increase ICP 3. Elevate head 30 – 45o 4. Monitor strictly vitals signs, I & O and neuro check 5. Prevent complications of immobility by: a. turn client to side b. provide egg crate mattresses or water bed c. provide sand bag or food board. 6. Assist in passive ROM exercise every 4 hours to promote proper bodily alignment and prevent contractures 7. Institute NGT feeding 8. Provide alternative means of communication a. non verbal cues b. magic slate 9. If positive to hemianopsia approach client on unaffected side 10. Administer medications as ordered a. Osmotic Diuretics (Mannitol) b. Loop Diuretics (Lasix, Furosemide) c. Cortecosteroids d. Mild Analgesics e. Thrombolytic/Fibrinolytic Agents – dissolves thrombus Streptokinase Side Effect: Allergic Reaction Urokinase Tissue Plasminogen Activating Factor Side Effect: Chest Pain f. Anti Coagulants Heparin (short acting) check for partial thromboplastin time if prolonged there is a risk for bleeding. give Protamine Sulfate Comadin/ Warfarin (long acting) give simultaneously because Coumadin will take effect after 3 days check for prothrombin time if prolonged there is a risk for bleeding give Vit. K (Aqua Mephyton) g. Anti Platelet PASA (Aspirin) Contraindicated for dengue, ulcer and unknown cause of headache because it may potentiate bleeding 11. Provide client health teachings and discharge planning concerning a. avoidance of modifiable risk factors (diet, exercise, smoking) b. prevent complication (subarachnoid hemorrhage is the most feared complication) c. dietary modification (decrease salt, saturated fats and caffeine) d. importance of follow up care GUILLAIN BARRE SYNDROME a disorder of the CNS characterized by bilateral symmetrical polyneuritis leading to ascending muscle paralysis. A. Predisposing Factors 1. Autoimmune 2. Antecedent viral infections such as LRT infections B. Signs and Symptoms 1. Clumsiness (initial sign) 2. Dysphagia 3. Ascending muscle weakness leading to paralysis 4. Decreased of diminished deep tendon reflex 5. Alternate hypotension to hypertension ** ARRYTHMIA (most feared complication) 6. Autonomic symptoms that includes a. increase salivation b. increase sweating c. constipation C. Diagnostic Procedures 1. CSF analysis reveals increase in IgG and protein D. Nursing Management 1. Maintain patent airway and adequate ventilation by: a. assist in mechanical ventilation b. monitor pulmonary function test 2. Monitor strictly the following a. vital signs b. intake and output c. neuro check d. ECG 3. Maintain side rails to prevent injury related to fall 4. Prevent complications of immobility by turning the client every 2 hours 5. Institute NGT feeding to prevent aspiration 6. Assist in passive ROM exercise 7. Administer medications as ordered a. Corticosteroids – suppress immune response b. Anti Cholinergic Agents – Atrophine Sulfate c. Anti Arrythmic Agents Lidocaine, Zylocaine Bretylium – blocks release of norepinephrine to prevent increase of BP 8. Assist in plasma pharesis (filtering of blood to remove autoimmune anti-bodies) 9. Prevent complications a. Arrythmia b. Paralysis or respiratory muscles/Respiratory arrest * Sengstaken Blakemore Tube for liver cirrhosis to decompress bleeding esophageal verices (prepare scissor to cut tube incase of difficulty in breathing to release air in the balloon for hemodialysis prepare bulldog clips to prevent air embolism. CONVULSIVE DISORDER/ CONVULSION disorder of CNS characterized by paroxysmal seizure with or without loss of consciousness abnormal motor activity alternation in sensation and perception and changes in behavior. Seizure – first convulsive attack Epilepsy – second or series of attacks Febrile seizure – normal in children age below 5 years A. Predisposing Factors 1. Head injury due to birth trauma 2. Genetics 3. Presence of brain tumor 4. Toxicity from a. lead b carbon monoxide 5. Nutritional and Metabolic deficiencies 6. Physical and emotional stress 7. Sudden withdrawal to anti convulsant drug is predisposing factor for status epilepticus (drug of choice is Diazepam, Valium) B. Signs and Symptoms Dependent on stages of development or types of seizure I. Generalized Seizure 1. Grand mal Seizure (tonic-clonic seizure) a. Signs or aura with auditory, olfactory, visual, tactile, sensory experience b. Epileptic cry – is characterized by fall and loss of consciousness for 3 – 5 minutes c. Tonic contractions - direct symmetrical extension of extremities Clonic contractions - contraction of extremities d. Post ictal sleep – unresponsive sleep 2. Petit mal Seizure – absence of seizure common among pediatric clients characterized by a. blank stare b. decrease blinking of eyes c. twitching of mouth d. loss of consciousness (5 – 10 seconds) II. Partial or Localized Seizure 1. Jacksonian Seizure (focal seizure) Characterized by tingling and jerky movement of index finger and thumb that spreads to the shoulder and other side of the body. 2. Psychomotor Seizure (focal motor seizure) a. automatism – stereotype repetitive and non propulsive behavior b. clouding of consciousness – not in contact with environment c. mild hallucinatory sensory experience III. Status Epilepticus A continuous uninterrupted seizure activity, if left untreated can lead to hyperpyrexia and lead to coma and eventually death. Drug of choice: Diazepam, Valium and Glucose C. Diagnostic Procedures 1. CT Scan – reveals brain lesions 2. EEG – reveals hyper activity of electrical brain waves D. Nursing Management 1. Maintain patent airway and promote safety before seizure activity a. clear the site of blunt or sharp objects b. loosen clothing of client c. maintain side rails d. avoid use of restrains e. turn clients head to side to prevent aspiration f. place mouth piece of tongue guard to prevent biting or tongue 2. Avoid precipitating stimulus such as bright/glaring lights and noise 3. Administer medications as ordered a. Anti convulsants (Dilantin, Phenytoin) b. Diazepam, Valium c. Carbamazepine (Tegretol) – Trigeminal neuralgia d. Phenobarbital, Luminal 4. Institute seizure and safety precaution post seizure attack a. administer O2 inhalation b. provide suction apparatus 5. Document and monitor the following a. onset and duration b. types of seizures c. duration of post ictal sleep may lead to status epilepticus d. assist in surgical procedure cortical resection COMPREHENSIVE NEURO EXAM GLASGOW COMA SCALE objective measurement of LOC sometimes called as the quick neuro check Components 1. Motor response 2. Verbal response 3. Eye opening Conscious 15 – 14 Lethargy 13 – 11 Stupor 10 – 8 Coma 7 Deep Coma 3 Survey of mental status and speech a. LOC b. Test of memory Levels of orientation Cranial nerve assessment Sensory nerve assessment Motor nerve assessment Deep tendon reflex Autonimics Cerebellar test a, Romberg’s test – 2 nurses, positive for ataxia b. Finger to nose test – positive result mean dimetria (inability of body to stop movement at desired point) c. Alternate supination and pronation – positive result mean dimetria I. LEVEL OF CONSCIOUSNESS 1. Conscious - awake 2. Lethargy – lethargic (drowsy, sleepy, obtunded) 3. Stupor stuporous (awakened by vigorous stimulation) generalized body weakness decrease body reflex comatose light coma (positive to all forms of painful stimulus) deep coma (negative to all forms of painful stimulus) 4. Coma DIFFERENT PAINFUL STIMULATION 1. Deep sternal stimulation/ deep sternal pressure 2. Orbital pressure 3. Pressure on great toes 4. Corneal or blinking reflex Conscious client use a wisp of cotton Unconscious client place 1 drop of saline solution II. TEST OF MEMORY 1. Short term memory ask most recent activity positive result mean anterograde amnesia and damage to temporal lobe 2. Long term memory ask for birthday and validate on profile sheet positive result mean retrograde amnesia and damage to limbic system consider educational background III. LEVELS OF ORIENTATION 1. Time – first asked 2. Person – second asked 3. Place – third asked CRANIAL NERVES CRANIAL NERVES FUNCTION I. OLFACTORY S II. OPTIC S III OCCULOMOTOR M IV. TROCHLEAR M (Smallest) V. TRIGEMINAL B (Largest) VI. ABDUCENSE M VII. FACIAL B VIII. ACOUSTIC S IX. GLOSSOPHARYNGEAL B X. VAGUS B (Longest) XI. SPINAL ACCESSORY M XII. HYPOGLOSSAL M CRANIAL NERVE I: OLFACTORY sensory function for smell Material Used don’t use alcohol, ammonia, perfume because it is irritating and highly diffusible. use coffee granules, vinegar, bar of soap, cigarette test each nostril by occluding each nostril Procedure Abnormal Findings 1. Hyposnia – decrease sensitivity to smell 2. Dysosmia – distorted sense of smell 3. Anosmia – absence of smell Indicative of 1. head injury damaging the cribriform plate of ethmoid bone where olfactory cells are located 2. may indicate inflammatory conditions (sinusitis) CRANIAL NERVE II: OPTIC sensory function for vision or sight Functions 1. Test visual acuity or central vision or distance use Snellen’s Chart Snellen’s Alphabet chart: for literate clients Snellen’s E chart: for illiterate clients Snellen’s Animal chart: for pediatric clients normal visual acuity 20/20 numerator is constant, it is the distance of person from the chart (6 – 7 m, 20 feet) denominator changes, indicates distance by which the person normally can see letter in the chart. - 20/200 indicates blindness 20/20 visual acuity if client is able to read letters above the red line. 2. Test of visual field or peripheral vision a. Superiorly b. Bitemporaly c. Nasally d. Inferiorly COMMON VISUAL DISORDERS 1. Glaucoma increase IOP normal IOP is 12 – 21 mmHg preventable but not curable A. Predisposing Factors Common among 40 years old and above Hereditary Hypertension Obesity B. Signs and Symptoms 1. Loss of peripheral vision pathognomonic sign is tunnel vision 2. Headache, nausea, vomiting, eye pain (halos around light) steamy cornea may lead to blindness C. Diagnostic Procedures 1. Tonometry 2. Perimetry 3. Gonioscopy D. Treatment 1. Miotics – constricts pupil a. Pilocarpine Sodium, Carbachol 2. Epinephrine eyedrops – decrease formation of aqueous humor 3. Carbonic Anhydrase Inhibitors a. Acetazolamide (Diamox) – promotes increase outflow of aqueous humor or drainage 4. Timoptics (Timolol Maleate) E. Surgical Procedures 1. TRABECULECTOMY (Peripheral Indectomy) – drain aqueous humor 2. Cataract Decrease opacity of lens A. Predisposing Factor 1. Aging 65 years and above 2. Related to congenital 3. Diabetes Mellitus 4. Prolonged exposure to UV rays B. Signs and Symptoms 1. Loss of central vision C. Pathognomonic Signs 1. Blurring or hazy vision 2. Milky white appearance at center of pupils 3. Decrease perception to colors Complication is blindness D. Diagnostic Procedure 1. Opthalmoscopic exam E. Treatment 1. Mydriatics (Mydriacyl) – constricts pupils 2. Cyclopegics (Cyclogyl) – paralyses cilliary muscle F. Surgical Procedure Extra Intra Capsular Capsular Cataract Cataract Lens Lens Extraction Extraction - Partial removal - Total removal of cataract with its surrounding capsules Most feared complication post op is RETINAL DETACHMENT 3. Retinal Detachment Separation of epithelial surface of retina A. Predisposing Factors 1. Post Lens Extraction 2. Myopia (near sightedness) B. Signs and Symptoms 1. Curtain veil like vision 2. Floaters C. Surgical Procedures 1. Scleral Buckling 2. Cryosurgery – cold application 3. Diathermy – heat application 4. Macular Degeneration Degeneration of the macula lutea (yellowish spot at the center of retina) A. Signs and Symptoms 1. Black Spots CRANIAL NERVE III, IV, VI: OCULOMOTOR, TROCHLEAR, ABDUCENS Controls or innervates the movement of extrinsic ocular muscle (EOM) 6 muscles Superior Rectus Superior Oblique Lateral Rectus Medial Rectus Inferior Oblique Inferior Rectus trochlear controls superior oblique abducens controls lateral rectus oculomotor controls the 4 remaining EOM Oculomotor controls the size and response of pupil normal pupil size is 2 – 3 mm equal size of pupil: Isocoria Unequal size of pupil: Anisocoria Normal response: positive PERRLA CRANIAL NERVE V: TRIGEMINAL largest cranial nerve consists of ophthalmic, maxillary, mandibular sensory: controls sensation of face, mucous membrane, teeth, soft palate and corneal reflex) motor: controls the muscle of mastication or chewing damage to CN V leads to trigeminal neuralgia/thickdolorum medication: Carbamezapine(Tegretol) CRANIAL NERVE VII: FACIAL Sensory: controls taste, anterior 2/3 of tongue pinch of sugar and cotton applicator placed on tip of tongue Motor: controls muscle of facial expression instruct client to smile, frown and if results are negative there is facial paralysis or Bell’s Palsy and the primary cause is forcep delivery. CRANIAL NERVE VIII: ACOUSTIC/VESTIBULOCOCHLEAR Controls balance particularly kinesthesia or position sense, refers to movement and orientation of the body in space. Parts of the Ear 1. Outer Ear Pinna Eardrum 2. Middle Ear Hammer Malleus Anvil Incus Stirrup Stapes 3. Inner Ear Vestibule: Meinere’s Disease Cochlea Mastoid Cells Endolymph and Perilymph COCHLEA: controls hearing, contains the Organ of Corti (the true organ of hearing) Let client repeat words uttered CRANIAL NERVE IX, X: GLOSOPHARYNGEAL, VAGUS NERVE Glosopharyngeal: controls taste, posterior 1/3 of tongue Vagus: controls gag reflex Uvula should be midline and if not indicative of damage to cerebral hemisphere Effects of vagal stimulation is PNS CRANIAL NERVE XI: SPINAL ACCESSORY Innervates with sternocleidomastoid (neck) and trapezius (shoulder) CRANIAL NERVE XII: HYPOGLOSSAL Controls the movement of tongue Let client protrude tongue and it should be midline and if unable to do indicative of damage to cerebral hemisphere and/or has short frenulum. ENDOCRINE SYSTEM Overview of the structures and functions 1. Pituitary Gland (Hypophysis Cerebri) o Located at base of brain particularly at sella turcica o Master gland or master clock o Controls all metabolic function of body PARTS OF THE PITUITARY GLAND 1. Anterior Pituitary Gland o called as adenohypophysis 2. Posterior Pituitary Gland o called as neurohypophysis o secretes hormones oxytocin -promotes uterine contractions preventing bleeding/ hemorrhage o administrate oxytocin immediately after delivery to prevent uterine atony. o initiates milk let down reflex with help of hormone prolactin 2. Antidiuretic Hormone o Pitressin (Vasopressin) o Function: prevents urination thereby conserving water o Diabetes Insipidus/ Syndrome of Inappropriate Anti Diuretic Hormone DIABETES INSIPIDUS o Decrease production of anti diuretic hormone A. Predisposing Factor o Related to pituitary surgery o Trauma o Inflammation o Presence of tumor B. Signs and Symptoms 1. Polyuria 2. Signs of dehydration a. Adult: thirst b. Agitation c. Poor Skin turgor d. Dry mucous membrane 3. Weakness and fatigue 4. Hypotension 5. Weight loss 6. If left untreated results to hypovolemic shock (sign is anuria) C. Diagnostic Procedures 1. Urine Specific Gravity o Normal value: 1.015 – 1.030 o Ph 4 – 8 2. Serum Sodium o Increase resulting to hypernatremia D. Nursing Management 1. Force fluids 2. Monitor strictly vital signs and intake and output 3. Administer medications as ordered a. Pitressin (Vasopresin Tannate) – administered IM Z-tract 4. Prevent complilcations – HYPOVOLEMIC SHOCK is the most feared complication SIADH o hypersecretion of anti diuretic hormone A. Predisposing Factors 1. Head injury 2. Related to presence of bronchogenic cancer o initial sign of lung cancer is non productive cough o non invasive procedure is chest x-ray 3. Related to hyperplasia (increase size of organ brought about by increase of number of cells) of pituitary gland. B. Signs and Symptoms 1. Fluid retention a. Hypertension b. Edema c. Weight gain 2. Water intoxication may lead to cerebral edema and lead to increase ICP – may lead to seizure activity C. Diagnostic Procedure 1. Urine specific gravity is increased 2. Serum Sodium is decreased D. Nursing Management 1. Restrict fluid 2. Administer medications as ordered a. Loop diuretics (Lasix) b. Osmotic diuretics (Mannitol) 3. Monitor strictly vital signs, intake and output and neuro check 4. Weigh patient daily and assess for pitting edema 5. Provide meticulous skin care 6. Prevent complications ANTERIOR PITUITARY GLAND o also called ADENOHYPOPHYSIS secretes 1. Growth hormones (somatotropic hormone) o Promotes elongation of long bones o Hyposecretion of GH among children results to Dwarfism o Hypersecretion of GH results to Gigantism o Hypersecretion of GH among adults results to Acromegaly (square face) o Drug of choice: Ocreotide (Sandostatin) 2. Melanocyte Stimulating hormone o for skin pigmentation o Hyposecretion of MSH results to Albinism o Most feared complications of albinism a. Lead to blindness due to severe photophobia b. Prone to skin cancer o Hypersecretion of MSH results to Vitiligo 3. Adrenochorticotropic hormone (ACTH) o promotes development of adrenal cortex 4. Lactogenic homone (Prolactin) o promotes development of mammary gland o with help of oxytocin it initiates milk let down reflex 5. Leutinizing hormone o secretes estrogen 6. Follicle stimulating hormone o secretes progesterone PINEAL GLAND o secretes melatonin o inhibits LH secretion o it controls/regulates circadian rhythm (body clock) THYROID GLAND o located anterior to the neck 3 Hormones secreted 1. T3 (Tri iodothyronine) - 3 molecules of iodine (more potent) 2. T4 (tetra iodothyronine, Thyroxine) o T3 and T4 are metabolic or calorigenic hormone o promotes cerebration (thinking) 3. Thyrocalcitonin – antagonizes the effects of parathormone to promote calcium resorption. HYPOTHYROIDISM o all are decrease except weight and menstruation o memory impairment Signs and Symptoms o there is loss of appetite but there is weight gain o menorrhagia o cold intolerance o constipation HYPERTHYROIDISM o all are increase except weight and menstruation Signs and Symptoms o increase appetite but there is weight loss o amenorrhea o exophthalmos THYROID DISORDERS SIMPLE GOITER o enlargement of thyroid gland due to iodine deficiency A. Predisposing Factors 1. Goiter belt area a. places far from sea b. Mountainous regions 2. Increase intake of goitrogenic foods o contains pro-goitrin an anti thyroid agent that has no iodine. o cabbage, turnips, radish, strawberry, carrots, sweet potato, broccoli, all nuts o soil erosion washes away iodine o goitrogenic drugs a. Anti Thyroid Agent – Prophylthiuracil (PTU) b. Lithium Carbonate c. PASA (Aspirin) d. Cobalt e. Phenylbutazones (NSAIDs) - if goiter is caused by B. Signs and Symptoms 1. Enlarged thyroid gland 2. Mild dysphagia 3. Mild restlessness C. Diagnostic Procedures 1. Serum T3 and T4 – reveals normal or below normal 2. Thyroid Scan – reveals enlarged thyroid gland. 3. Serum Thyroid Stimulating Hormone (TSH) – is increased (confirmatory diagnostic test) D. Nursing Management 1. Enforce complete bed rest 2. Administer medications as ordered a. Lugol’s Solution/SSKI ( Saturated Solution of Potassium Iodine) o color purple or violet and administered via straw to prevent staining of teeth. o 4 Medications to be taken via straw: Lugol’s, Iron, Tetracycline, Nitrofurantoin (drug of choice for pyelonephritis) b. Thyroid Hormones o Levothyroxine (Synthroid) o Liothyronine (Cytomel) o Thyroid Extracts Nursing Management when giving Thyroid Hormones 1. Instruct client to take in the morning to prevent insomnia 2. Monitor vital signs especially heart rate because drug causes tachycardia and palpitations 3. Monitor side effects o insomnia o tachycardia and palpitations o hypertension o heat intolerance 4. Increase dietary intake of foods rich in iodine o seaweeds o seafood’s like oyster, crabs, clams and lobster but not shrimps because it contains lesser amount of iodine. o iodized salt, best taken raw because it it is easily destroyed by heat 5. Assist in surgical procedure of subtotal thyroidectomy HYPOTHYROIDISM o hyposecretion of thyroid hormone o adults: MYXEDEMA non pitting edema o children: CRETINISM the only endocrine disorder that can lead to mental retardation A. Predisposing Factors 1. Iatrogenic Cause – disease caused by medical intervention such as surgery 2. Related to atrophy of thyroid gland due to trauma, presence of tumor, inflammation 3. Iodine deficiency 4. Autoimmune (Hashimotos Disease) B. Signs and Symptoms (Early Signs) 1. Weakness and fatigue 2. Loss of appetite but with weight gain which promotes lipolysis leading to atherosclerosis and MI 3. Dry skin 4. Cold intolerance 5. Constipation (Late Signs) 1. Brittleness of hair and nails 2. Non pitting edema (Myxedema) 3. Hoarseness of voice 4. Decrease libido 5. Decrease in all vital signs – hypotension, bradycardia, bradypnea, hypothermia 6. CNS changes o lethargy o memory impairment o psychosis o menorrhagia C. Diagnostic Procedures 1. Serum T3 and T4 is decreased 2. Serum Cholesterol is increased 3. RAIU (Radio Active Iodine Uptake) is decreased D. Nursing Management 1. Monitor strictly vital signs and intake and output to determine presence of o Myxedema coma is a complication of hypothyroidism and an emergency case o a severe form of hypothyroidism is characterized by severe hypotension, bradycardia, bradypnea, hypoventilation, hyponatremia, hypoglycemia, hypothermia leading to pregressive stupor and coma. Nursing Management for Myxedema Coma Assist in mechanical ventilation Administer thyroid hormones as ordered Force fluids 2. Force fluids 3. Administer isotonic fluid solution as ordered 4. Administer medications as ordered Thyroid Hormones a. Levothyroxine b. Leothyronine c. Thyroid Extracts 5. Provide dietary intake that is low in calories 6. Provide comfortable and warm environment 7. Provide meticulous skin care 8. Provide client health teaching and discharge planning concerning a. Avoid precipitating factors leading to myxedema coma o stress o infection o cold intolerance o use of anesthetics, narcotics, and sedatives o prevent complications (myxedema coma, hypovolemic shock o hormonal replacement therapy for lifetime o importance of follow up care HYPERTHYROIDISM o increase in T3 and T4 o Grave’s Disease or Thyrotoxicosis o developed by Robert Grave A. Predisposing Factors 1. Autoimmune – it involves release of long acting thyroid stimulator causing exopthalmus (protrusion of eyeballs) enopthalmus (late sign of dehydration among infants) 2. Excessive iodine intake 3. Related to hyperplasia (increase size) B. Signs and Symptoms 1. Increase appetite (hyperphagia) but there is weight loss 2. Moist skin 3. Heat intolerance 4. Diarrhea 5. All vital signs are increased 6. CNS involvement a. Irritability and agitation b. Restlessness c. Tremors d. Insomnia e. Hallucinations 7. Goiter 8. Exopthalmus 9. Amenorrhea C. Diagnostic Procedures 1. Serum T3 and T4 is increased 2. RAIU (Radio Active Iodine Uptake) is increased 3. Thyroid Scan- reveals an enlarged thyroid gland D. Nursing Management 1. Monitor strictly vital signs and intake and output 2. Administer medications as ordered Anti Thyroid Agent a. Prophythioracill (PTU) b. Methymazole (Tapazole) Side Effects of Agranulocytosis o increase lymphocytes and monocytes o fever and chills o sore throat (throat swab/culture) o leukocytosis (CBC) 3. Provide dietary intake that is increased in calories. 4. Provide meticulous skin care 5. Comfortable and cold environment 6. Maintain side rails 7. Provide bilateral eye patch to prevent drying of the eyes. 8. Assist in surgical procedures known as subtotal thyroidectomy ** Before thyroidectomy administer Lugol’s Solution (SSKI) to decrease vascularity of the thyroid gland to prevent bleeding and hemorrhage. POST OPERATIVELY, 1. Watch out for signs of thyroid storm/ thyrotoxicosis Agitation TRIAD SIGNS Hyperthermia o Tachycardia administer medications as ordered a. Anti Pyretics b. Beta-blockers o monitor strictly vital signs, input and output and neuro check. o maintain side rails o offer TSB 2. Watch out for accidental removal of parathyroid gland that may lead to Hypocalcemia (tetany) Signs and Symptoms o (+) trousseau’s sign o (+) chvostek sign o Watch out for arrhythmia, seizure give Calcium Gluconate IV slowly as ordered 3. Watch out for accidental Laryngeal damage which may lead to hoarseness of voice Nursing Management o encourage client to talk/speak immediately after operation and notify physician 4. Signs of bleeding (feeling of fullness at incisional site) Nursing Management o Check the soiled dressings at the back or nape area. 5. Hormonal replacement therapy for lifetime 6. Importance of follow up care PARATHYROID GLAND o A pair of small nodules behind the thyroid gland o Secretes parathormone o Promotes calcium reabsorption o Hypoparathyroidism o Hyperparathyroidism HYPOPARATHYROIDISM o Decrease secretion of parathormone leading to hypocalcemia o Resulting to hyperphospatemia A. Predisposing Factors 1. Following subtotal thyroidectomy 2. Atrophy of parathyroid gland due to: a. inflammation b. tumor c. trauma B. Signs and Symptoms 1. Acute tetany a. tingling sensation b. paresthesia c. numbness d. dysphagia e. positive trousseu’s sign/carpopedal spasm f. positive chvostek sign g. laryngospasm/broncospasm h. seizure feared complications i. arrhythmia 2. Chronic tetany a. photophobia and cataract formation b. loss of tooth enamel c. anorexia, nausea and vomiting d. agitation and memory impairment C. Diagnostic Procedures 1. Serum Calcium is decreased (normal value: 8.5 – 11 mg/100 ml) 2. Serum Phosphate is decreased (normal value: 2.5 – 4.5 mg/100 ml) 3. X-ray of long bones reveals a decrease in bone density 4. CT Scan – reveals degeneration of basal ganglia D. Nursing Management 1. Administer medications as ordered such as: a. Acute Tetany Calcium Gluconate IV slowly b. Chronic Tetany Oral Calcium supplements Calcium Gluconate Calcium Lactate Calcium Carbonate c. Vitamin D (Cholecalciferol) for absorption of calcium CHOLECALCIFEROL ARE DERIVED FROM Drug Diet (Calcidiol) Sunlight (Calcitriol) d. Phosphate binder Aluminum Hydroxide Gel (Ampogel) Side effect: constipation ANTACID A.A.C ▼ Aluminum Containing Antacids ▼ Aluminum Hydroxide Gel ▼ Side Effect: Constipation MAD ▼ Magnesium Containing Antacids ▼ Side Effect: Diarrhea 2. Avoid precipitating stimulus such as glaring lights and noise 3. Encourage increase intake of foods rich in calcium a. anchovies b. salmon c. green turnips 4. Institute seizure and safety precaution 5. Encourage client to breathe using paper bag to produce mild respiratory acidosis result. 6. Prepare trache set at bedside for presence of laryngo spasm 7. Prevent complications 8. Hormonal replacement therapy for lifetime 9. Importance of follow up care. HYPERTHYROIDISM o Decrease parathormone o Hypercalcemia: bone demineralization leading to bone fracture (calcium is stored 99% in bone and 1% blood) o Kidney stones A. Predisposing Factors 1. Hyperplasia of parathyroid gland 2. Over compensation of parathyroid gland due to vitamin D deficiency a. Children: Ricketts b. Adults: Osteomalacia B. Signs and Symptoms 1. Bone pain especially at back (bone fracture) 2. Kidney stones a. renal cholic b. cool moist skin 3. Anorexia, nausea and vomiting 4. Agitation and memory impairment C. Diagnostic Procedures 1. Serum Calcium is increased 2. Serum Phosphate is decreased 3. X-ray of long bones reveals bone demineralization D. Nursing Management 1. Force fluids to prevent kidney stones 2. Strain all the urine using gauze pad for stone analysis 3. Provide warm sitz bath 4. Administer medications as ordered a. Morphine Sulfate (Demerol) 5. Encourage increase intake of foods rich in phosphate but decrease in calcium 6. Provide acid ash in the diet to acidify urine and prevent bacterial growth 7. Assist/supervise in ambulation 8. Maintain side rails 9. Prevent complications (seizure and arrhythmia) 10. Assist in surgical procedure known as parathyroidectomy 11. Hormonal replacement therapy for lifetime 12. Importance of follow up care ADRENAL GLAND o Located atop of each kidney o 2 layers of adrenal gland a. Adrenal Cortex – outermost b. Adrenal Medulla – innermost (secretes catecholamines a power hormone) 2 Types of Catecholamines o Epinephrine and Norepinephrine (vasoconstrictor) o Pheochromocytoma (adrenal medulla) o Increase secretion of norepinephrine o Leading to hypertension which is resistant to pharmacological agents leading to CVA o Use beta-blockers ADRENAL CORTEX 3 Zones/Layers 1. Zona Fasciculata - secretes glucocortocoids (cortisol) - function: controls glucose metabolism - Sugar 2. Zona Reticularis - secretes traces of glucocorticoids and androgenic hormones - function: promotes secondary sex characteristics - Sex 3. Zona Glumerulosa - secretes mineralocorticoids (aldosterone) - function: promotes sodium and water reabsorption and excretion of potassium - Salt ADDISON’S DISEASE o Hyposecretion of adreno cortical hormone leading to a. metabolic disturbance – Sugar b. fluid and electrolyte imbalance – Salt c. deficiency of neuromuscular function – Salt/Sex A. Predisposing Factors 1. Related to atrophy of adrenal glands 2. Fungal infections B. Signs and Symptoms 1. Hypoglycemia – TIRED 2. Decrease tolerance to stress 3. Hyponatremia - hypotension - signs of dehydration - weight loss 4. Hyperkalemia - agitation - diarrhea - arrhythmia 5. Decrease libido 6. Loss of pubic and axillary hair 7. Bronze like skin pigmentation C. Diagnostic Procedures 1. FBS is decreased (normal value: 80 – 100 mg/dl) 2. Plasma Cortisol is decreased 3. Serum Sodium is decrease (normal value: 135 – 145 meq/L) 4. Serum Potassium is increased (normal value: 3.5 – 4.5 meq/L) D. Nursing Management 1. Monitor strictly vital signs, input and output to determine presence of Addisonian crisis (complication of addison’s disease) o Addisonian crisis results from acute exacerbation of addison’s disease characterized by a. severe hypotension b. hypovolemic shock c. hyponatremia leading to progressive stupor and coma Nursing Management for Addisonian Crisis 1. Assist in mechanical ventilation, - administer steroids as ordered - force fluids 2. Administer isotonic fluid solution as ordered 3. Force fluids 4. Administer medications as ordered Corticosteroids a. Dexamethasone (Decadrone) b. Prednisone c. Hydrocortisone (Cortison) Nursing Management when giving steroids 1. Instruct client to take 2/3 dose in the morning and 1/3 dose in the afternoon to mimic the normal diurnal rhythm 2. Taper dose (withdraw gradually from drug) 3. Monitor side effects a. hypertension b. edema c. hirsutism d. increase susceptibility to infection e. moon face appearance 4. Mineralocorticoids (Flourocortisone) 5. Provide dietary intake, increase calories, carbohydrates, protein but decrease in potassium 6. Provide meticulous skin care 7. Provide client health teaching and discharge planning a. avoid precipitating factor leading to addisonian crisis leading to - stress - infection - sudden withdrawal to steroids b. prevent complications - addisonian crisis - hypovolemic shock c. hormonal replacement for lifetime d. importance of follow up care CUSHING SYNDROME o Hypersecretion of adenocortical hormones A. Predisposing Factors 1 Related to hyperplasia of adrenal gland 2. Increase susceptibility to infections 3. Hypernatremia a. hypertension b. edema c. weight gain d. moon face appearance and buffalo hump e. obese trunk f. pendulous abdomen g. thin extremities 4. Hypokalemia a. weakness and fatigue b. constipation c. U wave upon ECG (T wave hyperkalemia) 5. Hirsutism 6. Acne and striae 7. Easy bruising 8. Increase masculinity among females B. Diagnostic Procedures 1. FBS is increased 2. Plasma Cortisol is increased 3. Serum Sodium is increased 4. Serum Potassium is decreased C. Nursing Management 1. Monitor strictly vital signs and intake and output 2. Weigh patient daily and assess for pitting edema 3. Measure abdominal girth daily and notify physician 4. Restrict sodium intake 5. Provide meticulous skin care 6. Administer medications as ordered a. Spinarolactone – potassium sparring diuretics 7. Prevent complications (DM) 8. Assist in surgical procedure (bilateral adrenoraphy) 9. Hormonal replacement for lifetime 10. Importance of follow up care PANCREAS - Located behind the stomach - Mixed gland (exocrine and endocrine) - Consist of acinar cells which secretes pancreatic juices that aids in digestion thus it is an exocrine gland - Consist of islets of langerhans - Has alpha cells that secretes glucagons (function: hyperglycemia) - Beta cells secretes insulin (function: hypoglycemia) - Delta cells secretes somatostatin (function: antagonizes the effects of growth hormones) 3 Main Disorders of Pancreas 1. Pancreatic Tumor/Cancer 2. Diabetes Mellitus 3. Pancreatitis DIABETES MELLITUS - metabolic disorder characterized by non utilization of carbohydrates, protein and fat metabolism CLASSIFICATION OF DM Type 1 (IDDM) Type 2 (NIDDM) - Juvenile onset type - Adult onset - Brittle disease - Maturity onset type - Obese over 40 years old A. Incidence Rate A. Incidence Rate - 10% general population has type 1 DM - 90% of general population has type 2 DM B. Predisposing Factors B. Predisposing Factors 1. Hereditary (total destruction of pancreatic cells) 1. Obesity – because obese persons lack insulin 2. Related to viruses receptor binding sites 3. Drugs a. Lasix b. Steroids 4. Related to carbon tetrachloride toxicity C. Signs and Symptoms C. Signs and Symptoms 1. Polyuria 1. Usually asymptomatic 2. Polydypsia 2. Polyuria 3. Polyphagia 3. Polydypsia 4. Glucosuria 4. Polyphagia 5. Weight loss 5. Glucosuria 6. Anorexia, nausea and vomiting 6. Weight gain 7. Blurring of vision 8. Increase susceptibility to infection 9. Delayed/poor wound healing D. Treatment D. Treatment 1. Insulin therapy 1. Oral Hypoglycemic agents 2. Diet 2. Diet 3. Exercise 3. Exercise E. Complication E. Complications 1. Diabetic Ketoacidosis 1. Hyper 2. Osmolar 3. Non 4. Ketotic 5. Coma MAIN ANABOLISM CATABOLISM 1. Carbohydrates Glucose Glycogen 2. Protein Amino Acids Nitrogen 3. Fats Fatty Acids Free Fatty Acids FOODSTUFF - Cholesterol - Ketones HYPERGLYCEMIA Increase osmotic diuresis Glycosuria Polyuria Cellular starvation – weight loss Cellular dehydration Stimulates the appetite/satiety center Stimulates the thirst center (Hypothalamus) (Hypothalamus) Polyphagia Polydypsia * Liver has glycogen that undergo glycogenesis/ glycogenolysis GLUCONEOGENESIS Formation of glucose from non-CHO sources Increase protein formation ▼ Negative Nitrogen balance ▼ Tissue wasting (Cachexia) ▼ INCREASE FAT CATABOLISM ▼ Free fatty acids Cholesterol Ketones ▼ Atherosclerosis ▼ Hypertension ▼ Diabetic Keto Acidosis Acetone Breath odor MI Kussmaul’s Respiration CVA Death Diabetic Coma DIABETIC KETOACIDOSIS - Acute complication of type 1 DM due to severe hyperglycemia leading to severe CNS depression A. Predisposing Factors 1. Hyperglycemia 2. Stress – number one precipitating factor 3. Infection B. Signs and Symptoms 1. Polyuria 2. Polydypsia 3. Polyphagia 4. Glucosuria 5. Weight loss 6. Anorexia, nausea and vomiting 7. Blurring of vision 8. Acetone breath odor 9. Kussmaul’s Respiration (rapid shallow breathing) 10 CNS depression leading to coma C. Diagnostic Procedures 1. FBS is increased 2. BUN (normal value: 10 – 20) 3. Creatinine (normal value: .8 – 1) 4. Hct (normal value: female 36 – 42, male 42 – 48) due to severe dehydration D. Nursing Management 1. Assist in mechanical ventilation 2. Administer 0.9 NaCl followed by .45 NaCl (hypotonic solutions) to counteract dehydration and shock 3. Monitor strictly vital signs, intake and output and blood sugar levels 4. Administer medications as ordered a. Insulin therapy (regular acting insulin/rapid acting insulin peak action of 2 – 4 hours) b. Sodium Bicarbonate to counteract acidosis c. Antibiotics to prevent infection HYPER OSMOLAR NON KETOTIC COMA - Hyperosmolar: increase osmolarity (severe dehydration) - Non ketotic: absence of lypolysis (no ketones) A. Signs and Symptoms 1. Headache and dizziness 2. Restlessness 3. Seizure activity 4. Decrease LOC – diabetic coma B. Nursing Management 1. Assist in mechanical ventilation 2. Administer 0.9 NaCl followed by .45 NaCl (hypotonic solutions) to counteract dehydration and shock 3. Monitor strictly vital signs, intake and output and blood sugar levels 4. Administer medications as ordered a. Insulin therapy (regular acting insulin peak action of 2 – 4 hours) - for DKA use rapid acting insulin b. Antibiotics to prevent infection INSULIN THERAPY A. Sources of Insulin 1. Animal sources - Rarely used because it can cause severe allergic reaction - Derived from beef and pork 2. Human Sources - Frequently used type because it has less antigenicity property thus less allergic reaction 3. Artificially Compound Insulin B. Types of Insulin 1. Rapid Acting Insulin (clear) - Regular acting insulin (IV only) - Peak action is 2 – 4 hours 2. Intermediate Acting Insulin (cloudy) - Non Protamine Hagedorn Insulin (NPH) - Peak action is 8 – 16 hours 3. Long Acting Insulin (cloudy) - Ultra Lente - Peak action is 16 – 24 hours C. Nursing Management for Insulin Injections 1. Administer at room temperature to prevent development of lipodystrophy (atrophy, hypertrophy of subcutaneous tissues) 2. Place in refrigerator once opened 3. Avoid shaking insulin vial vigorously instead gently roll vial between palm to prevent formation of bubbles 4. Use gauge 25 – 26 needle 5. Administer insulin either 45o – 90o depending on amount of clients tissue deposit 6. No need to aspirate upon injection 7. Rotate insulin injection sites to prevent development of lipodystrophy 8. Most accessible route is abdomen 9. When mixing 2 types of insulin aspirate first the clear insulin before cloudy to prevent contaminating the clear insulin and promote proper calibration. 10. Monitor for signs of local complications such as a. Allergic reactions b. Lipodystrophy c. Somogyis Phenomenon – rebound effect of insulin characterized by hypoglycemia to hyperglycemia ORAL HYPOGLYCEMIC AGENTS - Stimulates the pancreas to secrete insulin A. Classsification 1. First Generation Sulfonylureas a. Chlorpropamide (Diabenase) b. Tolbutamide (Orinase) c. Tolamazide (Tolinase) 2. Second Generation Sulfonylureas a. Glipzide (Glucotrol) b. Diabeta (Micronase) Nursing Management when giving OHA 1. Instruct the client to take it with meals to lessen GIT irritation and prevent hypoglycemia 2. Instruct the client to avoid taking alcohol because it can lead to severe hypoglycemia reaction or Disulfiram (Antabuse) toxicity symptoms B. Diagnostic Procedures 1. FBS is increased (3 consecutive times with signs or polyuria, polydypsia, polyphagia and glucosuria confirmatory for DM) 2. Random Blood Sugar is increased 3. Oral glucose tolerance test is increased – most sensitive test 4. Alpha Glycosylated Hemoglobin is increased C. Nursing Management 1. Monitor for peak action of insulin and OHA and notify physician 2. Administer insulin and OHA therapy as ordered 3. Monitor strictly vital signs, intake and output and blood sugar levels 4. Monitor for signs of hypoglycemia and hyperglycemia - administer simple sugars - for hypoglycemia (cold and clammy skin) give simple sugars - for hyperglycemia (dry and warm skin) 5. Provide nutritional intake of diabetic diet that includes: carbohydrates 50%, protein 30% and fats 20% or offer alternative food substitutes 6. Instruct client to exercise best after meals when blood glucose is rising 7. Monitor signs for complications a. Atherosclerosis (HPN, MI, CVA) b. Microangiopathy (affects small minute blood vessels of eyes and kidneys) EYES KIDNEY -PREMATURE CATARACT -RECURRENT PYELONEPHRITIS - Blindness - Renal failure c. HPN and DM major cause of renal failure d. Gangrene formation e. Shock due to dehydration - peripheral neuropathy - diarrhea/constipation - sexual impotence 8. Institute foot care management a. instruct client to avoid walking barefooted b. instruct client to cut toenails straight c. instruct client to avoid wearing constrictive garments d. encourage client to apply lanolin lotion to prevent skin breakdown e. assist in surgical wound debriment (give analgesics 15 – 30 mins prior) 9. Instruct client to have an annual eye and kidney exam 10. Monitor for signs of DKA and HONKC 11. Assist in surgical procedure HEMATOLOGICAL SYSTEM I. Blood 55% Plasma Serum 45% Formed II. Blood Vessels III. Blood Forming Organs 1. Arteries 2. Veins 1. Liver 3. Spleen 4. Lymphoid Organ 5. Lymph Nodes 6. Bone Marrow Plasma CHON (formed in liver) 1. Albumin 2. Globulins 3. Prothrombin and Fibrinogen ALBUMIN - Largest and numerous plasma CHON - Maintains osmotic pressure preventing edema GLOBULINS - Alpha globulins - transport steroids, bilirubin and hormones - Beta globulins – iron and copper - Gamma globulins a. anti-bodies and immunoglobulins b. prothrombin and fibrinogen clotting factors FORMED ELEMENTS 1. RBC (ERYTHROCYTES) - normal value: 4 – 6 million/mm3 - only unnucleated cell - biconcave discs - consist of molecules of hgb (red pigment) bilirubin (yellow pigment) biliverdin (green pigment) hemosiderin (golden brown pigment) - transports and carries oxygen to tissues - hemoglobin: normal value female 12 – 14 gms% male 14 – 16 gms% - hematocrit red cell percentage in wholeblood - normal value: female 36 – 42% male 42 – 48% - substances needed for maturation of RBC a. folic acid b. iron c. vitamin c d. vitamin b12 (cyanocobalamin) e. vitamin b6 (pyridoxine) f. intrinsic factor - Normal life span of RBC is 80 – 120 days and is killed in red pulp of spleen 2. WBC (LEUKOCYTES) - normal value: 5000 – 10000/mm3 A. Granulocytes 1. Polymorpho Neutrophils - 60 – 70% of WBC - involved in short term phagocytosis for acute inflammation 2. Polymorphonuclear Basophils - for parasite infections - responsible for the release of chemical mediation for inflammation 3. Polymorphonuclear Eosinophils - for allergic reaction B. Non Granulocytes 1. Monocytes - macrophage in blood - largest WBC - involved in long term phagocytosis for chronic inflammation 2. Lymphocytes B-cell T-cell - bone marrow - thymus for immunity Natural killer cell - anti viral and anti tumor property HIV - 6 months – 5 years incubation period - 6 months window period - western blot opportunistic - ELISA - drug of choice AZT (Zidon Retrovir) 2 Common fungal opportunistic infection in AIDS 1. Kaposi’s Sarcoma 2. Pneumocystis Carinii Pneumonia 3. Platelets (THROMBOCYTES) - Normal value: 150,000 – 450,000/mm3 - Promotes hemostasis (prevention of blood loss) - Consist of immature or baby platelets or megakaryocytes which is the target of dengue virus - Normal life span of platelet is 9 – 12 days Signs of Platelet Dysfunction 1. Petechiae 2. Echhymosis 3. Oozing of blood from venipunctured site BLOOD DISORDERS Iron Deficiency Anemia - A chronic microcytic anemia resulting from inadequate absorption of iron leading to hypoxemic tissue injury A. Incidence Rate 1. Common among developed countries 2. Common among tropical zones 3. Common among women 15 – 35 years old 4. Related to poor nutrition B. Predisposing Factors 1. Chronic blood loss due to trauma a. Heavy menstruation b. Related to GIT bleeding resulting to hematemesis and melena (sign for upper GIT bleeding) c. fresh blood per rectum is called hematochezia 2. Inadequate intake of iron due to a. Chronic diarrhea b. Related to malabsorption syndrome c. High cereal intake with low animal protein digestion d. Subtotal gastrectomy 4. Related to improper cooking of foods C. Signs and Symptoms 1. Usually asymptomatic 2. Weakness and fatigue (initial signs) 3. Headache and dizziness 4. Pallor and cold sensitivity 5. Dyspnea 6. Palpitations 7. Brittleness of hair and spoon shape nails (koilonychias) 8. Atropic Glossitis (inflammation of tongue) - Stomatitis PLUMBER VINSON’S SYNDROME - Dysphagia 9. PICA (abnormal appetite or craving for non edible foods D. Diagnostic Procedures 1. RBC is decreased 2. Hgb is decreased 3. Hct is deceased 4. Iron is decreased 5. Reticulocyte is decreased 6. Ferritin is decreased E. Nursing Management 1. Monitor for signs of bleeding of all hema test including urinw, stool and GIT 2. Enforce CBR so as not to over tire client 3. Instruct client to take foods rich in iron a. Organ meat b. Egg (yolk) c. Raisin d. Sweet potatoes e. Dried fruits f. Legumes g. Nuts 4. Instruct the client to avoid taking tea and coffee because it contains tannates which impairs iron absorption 5. Administer medications as ordered Oral Iron Preparations a. Ferrous Sulfate b. Ferrous Fumarate c. Ferrous Gluconate - 300 mg/day Nursing Management when taking oral iron preparations 1. Instruct client to take with meals to lessen GIT irritation 2. When diluting it in liquid iron preparations administer with straw to prevent staining of teeth Medications administered via straw - Lugol’s solution - Iron - Tetracycline - Nitrofurantoin (Macrodentin) 3. Administer with Vitamin C or orange juice for absorption 4. Monitor and inform client of side effects a. Anorexia b. Nausea and vomiting c. Abdominal pain d. Diarrhea/constipation e. Melena 5. If client cant tolerate/no compliance administer parenteral iron preparation a. Iron Dextran (IM, IV) b. Sorbitex (IM) Nursing Management when giving parenteral iron preparations 1. Administer Z tract technique to prevent discomfort, discoloration and leakage to tissues 2. Avoid massaging the injection site instead encourage to ambulate to facilitate absorption 3. Monitor side effects a. Pain at injection site b. Localized abscess c. Lymphadenopathy d. Fever and chills e. Skin rashes f. Pruritus/orticaria g. Hypotension (anaphylactic shock) PERNICIOUS ANEMIA - Chronic anemia characterized by a deficiency of intrinsic factor leading to hypochlorhydria (decrease hydrochloric acid secretion) A. Predisposing Factors 1. Subtotal gastrectomy 2. Hereditary factors 3. Inflammatory disorders of the ileum 4. Autoimmune 5. Strictly vegetarian diet STOMACH ▼ Pareital cells/ Argentaffin or Oxyntic cells Produces intrinsic factors Secretes hydrochloric acid ▼ Promotes reabsorption of Vit B12 ▼ Aids in digestion ▼ Promotes maturation of RBC B. Signs and Symptoms 1. Weakness and fatigue 2. Headache and dizziness 3. Pallor and cold sensitivity 4. Dyspnea and palpitations as part of compensation 5. GIT changes that includes a. mouth sore b. red beefy tongue c. indigestion/dyspepsia d. weight loss e. jaundice 6. CNS changes a. tingling sensation b. numbness c. paresthesia d. positive to Romberg’s test – damage to cerebellum resulting to ataxia e. result to psychosis C. Diagnostic Procedure Schilling’s Test – reveals inadequate/decrease absorption of Vitamin B12 D. Nursing Management 1. Enforce CBR 2. Administer Vitamin B12 injections at monthly intervals for lifetime as ordered - Never given orally because there is possibility of developing tolerance - Site of injection for Vitamin B12 is dorsogluteal and ventrogluteal - No side effects 3. Provide a dietary intake that is high in carbohydrates, protein, vitamin c and iron 4. Instruct client to avoid irritating mouth washes instead use soft bristled toothbrush 5. Avoid heat application to prevent burns APLASTIC ANEMIA - Stem cell disorder leading to bone marrow depression leading to pancytopenia PANCYTOPENIA Decrease RBC (anemia) Decrease WBC (leucopenia) Decrease Platelet (thrombocytopenia) A. Predisposing Factors 1. Chemicals (Benzine and its derivatives) 2. Related to irradiation/exposure to x-ray 3. Immunologic injury 4. Drugs Broad Spectrum Antibiotics a. Chloramphenicol (Sulfonamides) Chemotherapeutic Agents a. Methotrexate (Alkylating Agent) b. Vincristine (Plant Alkaloid) c. Nitrogen Mustard (Antimetabolite) Phenylbutazones (NSAIDS) B. Signs and Symptoms 1. Anemia a. Weakness and fatigue b. Headache and dizziness c. Pallor and cold sensitivity d. Dyspnea and palpitations 2. Leukopenia a. Increase susceptibility to infection 3. Thrombocytopenia a. Petechiae (multiple petechiae is called purpura) b. Ecchymosis c. Oozing of blood from venipunctured sites C. Diagnostic Procedures 1. CBC reveals pancytopenia 2. Bone marrow biopsy/aspiration (site is the posterior iliac crest) – reveals fat necrosis in bone marrow D. Nursing Management 1. Removal of underlying cause 2. Institute BT as ordered 3. Administer oxygen inhalation 4. Enforce CBR 5. Institute reverse isolation 6. Monitor for signs of infection a. fever b. cough 7. Avoid IM, subcutaneous, venipunctured sites 8 Instead provide heparin lock 9. Instruct client to use electric razor when shaving 10. Administer medications as ordered a. Corticosteroids – caused by immunologic injury b. Immunosuppressants Anti Lymphocyte Globulin ▼ Given via central venous catheter ▼ Given 6 days to 3 weeks to achieve Maximum therapeutic effect of drug DISSEMINATED INTRAVASCULAR COAGULATION Acute hemorrhagic syndrome characterized by wide spread bleeding and thrombosis due to a deficiency of prothrombin and fibrinogen A. Predisposing Factors 1. Related to rapid blood transfusion 2. Massive burns 3. Massive trauma 4. Anaphylaxis 5. Septecemia 6. Neoplasia (new growth of tissue) 7. Pregnancy B. Signs and Symptoms 1. Petechiae (widespread and systemic) eye, lungs and lower extremities 2. Ecchymosis 3. Oozing of blood from punctured sites 4. Hemoptysis 6. Oliguria (late sign) C. Diagnostic Procedures 1. CBC reveals decreased platelets 2. Stool occult blood positive 3. ABG analysis reveals metabolic acidosis 4. Opthamoscopic exam reveals sub retinal hemorrhages D. Nursing Management 1. Monitor for signs of bleeding of all hema test including stool and GIT 2. Administer isotonic fluid solution as ordered 3. Administer oxygen inhalation 4. Force fluids 5. Administer medications as ordered a. Vitamin K b. Pitressin/ Vasopresin to conserve fluids c. Heparin/Coumadin is ineffective 6. Provide heparin lock 7. Institute NGT decompression by performing gastric lavage by using ice or cold saline solution of 500 – 1000 ml 8. Monitor NGT output 9. Prevent complication a. Hypovolemic shock b. Anuria – late sign BLOOD TRANSFUSION Goals/Objectives 1. Replace circulating blood volume 2. Increase the oxygen carrying capacity of blood 3. Prevent infection in there is a decrease in WBC 4. Prevent bleeding if there is platelet deficiency Principles of blood transfusion 1. Proper refrigeration - Expiration of packed RBC is 3 – 6 days - Expiration of platelet is 3 – 5 days 2. Proper typing and cross matching a. Type O – universal donor b. Type AB – universal recipient c. 85% of population is RH positive 3. Aseptically assemble all materials needed for BT a. Filter set b. Gauge 18 – 19 needle c. Isotonic solution (0.9 NaCl/plain NSS) to prevent hemolysis 4. Instruct another RN to re check the following a. Client name b. Blood typing and cross matching c. Expiration date d. Serial number 5. Check the blood unit for bubbles cloudiness, sediments and darkness in color because it indicates bacterial contamination - Never warm blood as it may destroy vital factors in blood. - Warming is only done during emergency situation and if you have the warming device - Emergency rapid BT is given after 30 minutes and let natural room temperature warm the blood. 6. BT should be completed less than 4 hours because blood that is exposed at room temperature more than 2 hours causes blood deterioration that can lead to BACTERIAL CONTAMINATION 7. Avoid mixing or administering drugs at BT line to prevent HEMOLYSIS 8. Regulate BT 10 – 15 gtts/min or KVO rate or equivalent to 100 cc/hr to prevent circulatory overload 9. Monitor strictly vital signs before, during and after BT especially every 15 minutes for first hour because majority of transfusion reaction occurs during this period a. Hemolytic reaction b. Allergic reaction c. Pyrogenic reaction d. Circulatory overload e. Air embolism f. Thrombocytopenia g. Cytrate intoxication h. Hyperkalemia (caused by expired blood) Signs and Symptoms of Hemolytic reaction 1. Headache and dizziness 2. Dyspnea 3. Diarrhea/Constipation 4. Hypotension 5. Flushed skin 6. Lumbasternal/ Flank pain 7. Urine is color red/ portwine urine Nursing Management 1. Stop BT 2. Notify physician 3. Flush with plain NSS 4. Administer isotonic fluid solution to prevent shock and acute tubular necrosis 5. Send the blood unit to blood bank for re examination 6. Obtain urine and blood sample and send to laboratory for re examination 7. Monitor vital signs and intake and output SIGNS AND SYMPTOMS OF ALLERGIC REACTION 1. Fever 2. Dyspnea 3. Broncial wheezing 4. Skin rashes 5. Urticaria 6. Laryngospasm and Broncospasm Nursing Management 1. Stop BT 2. Notify physician 3. Flush with plain NSS 4. Administer medications as ordered a. Anti Histamine (Benadryl) - if positive to hypotension, anaphylactic shock treat with Epinephrine 5. Send the blood unit to blood bank for re examination 6. Obtain urine and blood sample and send to laboratory for re examination 7. Monitor vital signs and intake and output SIGNS AND SYMPTOMS PYROGENIC REACTIONS 1. Fever and chills 2. Headache 3. Tachycardia 4. Palpitations 5. Diaphoresis 6. Dyspnea Nursing Management 1. Stop BT 2. Notify physician 3. Flush with plain NSS 4. Administer medications as ordered a. Antipyretic b. Antibiotic 5. Send the blood unit to blood bank for re examination 6. Obtain urine and blood sample and send to laboratory for re examination 7. Monitor vital signs and intake and output 8. Render TSB SIGNS AND SYMPTOMS OF CIRCULATORY REACTION 1. Orthopnea 2. Dyspnea 3. Rales/Crackles upon auscultation 4. Exertional discomfort Nursing Management 1. Stop BT 2. Notify physician 3. Administer medications as ordered a. Loop diuretic (Lasix) CARDIOVASCULAR SYSTEM OVERVIEW OF THE STRUCTURE AND FUNCTIONS OF THE HEART HEART - Muscular pumping organ of the body. - Located on the left mediastinum - Resemble like a close fist - Weighs approximately 300 – 400 grams - Covered by a serous membrane called the pericardium 2 layers of pericardium a. Parietal – outer layer b. Visceral – inner layer - In between is the pericardial fluid which is 10 – 20 cc - Prevent pericardial friction rub - Common among MI, pericarditis, Cardiac tamponade A. Layers of Heart 1. Epicardium – outer layer 2. Myocardium – middle layer 3. Endocardium – inner layer - Myocarditis can lead to cardiogenic shock and rheumatic heart disease B. Chambers of the Heart 1. Upper Chamber (connecting or receiving) a. Atria 2. Lower Chamber (contracting or pumping) a. Ventricles - Left ventricle has increased pressure which is 120 – 180 mmHg - In order to propel blood to the systemic circulation - Right atrium has decreased pressure which is 60 – 80 mmHg C. Valves - To promote unidimensional flow or prevent backflow 1. Atrioventricular Valves – guards opening between a. tricuspid valve b. mitral valve - Closure of AV valves give rise to first heart sound (S1 “lub”) 2. Semi – lunar Valves a. pulmonic b. aortic - Closure of SV valve give rise to second heart sound (S2 “dub”) Extra Heart Sounds 1. S3 – ventricular gallop usually seen in Left Congestive Heart Failure 2. S4 – atrial gallop usually seen in Myocardial Infarction and Hypertension D. Coronary Arteries - Arises from base of the aorta Types of Coronary Arteries 1. Right Main Coronary Artery 2. Left Main Coronary Artery - Supplies the myocardium E. Cardiac Conduction System 1. Sino – Atrial Node (SA or Keith Flack Node) - Located at the junction of superior vena cava and right atrium - Acts as primary pacemaker of the heart - Initiates electrical impulse of 60 – 100 bpm 2. Atrio – Ventricular Node (AV or Tawara Node) - Located at the inter atrial septum - Delay of electrical impulse for about .08 milliseconds to allow ventricular filling 3. Bundle of His - Right Main Bundle of His - Left Main Bundle of His - Located at the interventricular septum 4. Purkinje Fibers - Located at the walls of the ventricles for ventricular contraction SA NODE AV NODE BUNDLE OF HIS JLJLJLJJLJLJL PURKINJE FIBERS - P WAVE (atrial depolarization) contraction - QRS WAVE (ventricular depolarization) - T WAVE (ventricular repolarization) Insert pacemaker if there is complete heart block Most common pacemaker is the metal pacemaker and lasts up to 2 – 5 years ABNORMAL ECG TRACING 1. Positive U wave - Hypokalemia 2. Peak T wave – Hyperkalemia 3. ST segment depression – Angina Pectoris 4. ST segment elevation – Myocardial Infarction 5. T wave inversion – Myocardial Infarction 6. Widening of QRS complexes – Arrythmia CARDIAC DISORDERS Coronary Arterial Disease/ Ischemic Heart Disease Stages of Development of Coronary Artery Disease 1. Myocardial Injury - Atherosclerosis 2. Myocardial Ischemia – Angina Pectoris 3. Myocardial Necrosis – Myocardial Infarction ATHEROSCLEROSIS ATHEROSCLEROSIS ARTERIOSCLEROSIS - narrowing of artery - hardening of artery - lipid or fat deposits - calcium and protein deposits - tunica intima - tunica media A. Predisposing Factors 1. Sex – male 2. Race – black 3. Smoking 4. Obesity 5. Hyperlipidemia 6. sedentary lifestyle 7. Diabetes Mellitus 8. Hypothyroidism 9. Diet – increased saturated fats 10. Type A personality B. Signs and Symptoms 1. Chest pain 2. Dyspnea 3. Tachycardia 4. Palpitations 5. Duaphoresis C. Treatment Percutaneous Transluminal Coronary Angioplasty Objectives of PTCA 1. Revascularize myocardium 2. To prevent angina 3. Increase survival rate - Done to single occluded vessels - If there is 2 or more occluded blood vessels CABG is done Coronary Arterial Bypass And Graft Surgery 3 Complications of CABG 1. Pneumonia – encourage to perform deep breathing, coughing exercise and use of incentive spirometer 2. Shock 3. Thrombophlebitis ANGINA PECTORIS (SYNDROME) Clinical syndrome characterized by paroxysmal chest pain that is usually relieved by rest or nitroglycerine due to temporary myocardial ischemia A. Predisposing Factors 1. Sex – male 2. Race – black 3. Smoking 4. Obesity 5. Hyperlipidemia 6. sedentary lifestyle 7. Diabetes Mellitus 8. Hypothyroidism 9. Diet – increased saturated fats 10. Type A personality B. Precipitating Factors 4 E’s of Angina Pectoris 1. Excessive physical exertion – heavy exercises 2. Exposure to cold environment 3. Extreme emotional response – fear, anxiety, excitement 4. Excessive intake of foods rich in saturated fats – skimmed milk C. Signs and Symptoms 1. Levine’s Sign – initial sign that shows the hand clutching the chest 2. Chest pain characterized by sharp stabbing pain located at sub sterna usually radiates from back, shoulder, arms, axilla and jaw muscles, usually relieved by rest or taking nitroglycerine 3. Dyspnea 4. Tachycardia 5. Palpitations 6. Diaphoresis D. Diagnostic Procedure 1. History taking and physical exam 2. ECG tracing reveals ST segment depression 3. Stress test – treadmill test, reveal abnormal ECG 4. Serum cholesterol and uric acid is increased E. Nursing Management 1. Enforce complete bed rest 2. Administer medications as ordered a. Nitroglycerine (NTG) – when given in small doses will act as venodilator, but in large doses will act as vasodilator - Give first dose of NTG (sublingual) 3 – 5 minutes - Give second dose of NTG if pain persist after giving first dose with interval of 3 - 5 minutes - Give third and last dose of NTG if pain still persist at 3 – 5 minutes interval Nursing Management when giving NTG - Keep the drug in a dry place, avoid moisture and exposure to sunlight as it may inactivate the drug - Monitor side effects o Orthostatic hypotension o Transient headache and dizziness - Instruct the client to rise slowly from sitting position - Assist or supervise in ambulation - When giving nitrol or transdermal patch o Avoid placing near hairy areas as it may decrease drug absorption o Avoid rotating transdermal patches as it may decrease drug absorption o Avoid placing near microwave ovens or duting defibrillation as it may lead to burns (most important thing to remember) b. Beta-blockers - Propanolol - side effects PNS - Not given to COPD cases because it causes bronchospasm c. ACE Inhibitors - Enalapril d. Calcium Antagonist - NIfedipine 3. Administer oxygen inhalation 4. Place client on semi fowlers position 5. Monitor strictly vital signs, intake and output and ECG tracing 6. Provide decrease saturated fats sodium and caffeine 7. Provide client health teachings and discharge planning a. Avoidance of 4 E’s b. Prevent complication (myocardial infarction) c. Instruct client to take medication before indulging into physical exertion to achieve the maximum therapeutic effect of drug d. The importance of follow up care MYOCARDIAL INFARCTION Heart attack Terminal stage of coronary artery disease characterized by malocclusion, necrosis and scarring. A. Types 1. Transmural Myocardial Infarction – most dangerous type characterized by occlusion of both right and left coronary artery 2. Subendocardial Myocardial Infarction – characterized by occlusion of either right or left coronary artery B. The Most Critical Period Following Diagnosis of Myocardial Infarction ** 6 – 8 hours because majority of death occurs due to arrhythmia leading to PVC’s C. Predisposing Factors 1. Sex – male 2. Race – black 3. Smoking 4. Obesity 5. Hyperlipidemia 6. sedentary lifestyle 7. Diabetes Mellitus 8. Hypothyroidism 9. Diet – increased saturated fats 10. Type A personality D. Signs and Symptoms 1. Chest pain - Excruciating visceral, viselike pain located at substernal and rarely in precordial - Usually radiates from back, shoulder, arms, axilla, jaw and abdominal muscles (abdominal ischemia) - Not usually relieved by rest or by nitroglycerine 2. Dyspnea 3. Increase in blood pressure (initial sign) 4. Hyperthermia 5. Ashen skin 6. Mild restlessness and apprehension 7. Occasional findings a. Pericardial friction rub b. Split S1 and S2 c. Rales/Crackles upon auscultation d. S4 or atrial gallop E. Diagnostic Procedure 1. Cardiac Enzymes a. CPK – MB - Creatinine phosphokinase is increased - Heart only, 12 – 24 hours b. LDH – Lactic acid dehydroginase is increased c. SGPT – Serum glutamic pyruvate transaminase is increased d. SGOT – Serum glutamic oxal-acetic transaminase is increased 2. Troponin Test – is increased 3. ECG tracing reveals a. ST segment elevation b. T wave inversion c. Widening of QRS complexes indicates that there is arrhythmia in MI 4. Serum Cholesterol and uric acid are both increased 5. CBC – increased WBC F. Nursing Management Goal: Decrease myocardial oxygen demand 1. Decrease myocardial workload (rest heart) - Administer narcotic analgesic/morphine sulfate - Side Effects: respiratory depression - Antidote: Narcan/Naloxone - Side Effects of Naloxone Toxicity is tremors 2. Administer oxygen low inflow to prevent respiratory arrest at 2 – 3 L/min 3. Enforce CBR without bathroom privileges a. Using bedside commode 4. Instruct client to avoid forms of valsalva maneuver 5. Place client on semi fowlers position 6. Monitor strictly vital signs, intake and output and ECG tracing 7. Provide a general liquid to soft diet that is low in saturated fats, sodium and caffeine 8. Encourage client to take 20 – 30 cc/week of wine, whisky and brandy to induce vasodilation 9. Administer medication as ordered a. Vasodilators - Nitroglycerine - ISD (Isosorbide Dinitrate, Isodil) sublingual b. Anti Arrythmic Agents - Lidocaine (Xylocane - Side Effects: confusion and dizziness - Brutylium c. Beta-blockers d. ACE Inhibitors e. Calcium Antagonist f. Thrombolytics/ Fibrinolytic Agents - Streptokinase - Side Effects: allergic reaction, pruritus - Urokinase - TIPAF (tissue plasminogen activating factor) - Side Effects: chest pain - Monitor for bleeding time g. Anti Coagulant - Heparin (check for partial thrombin time) - Antidote: protamine sulfate - Coumadin/ Warfarin Sodium (check for prothrombin time) - Antidote: Vitamin K h. Anti Platelet - PASA (Aspirin) - Anti thrombotic effect - Side Effects of Aspirin Tinnitus Heartburn Indigestion/Dyspepsia - Contraindication Dengue Peptic Ulcer Disease Unknown cause of headache 10. Provide client health teaching and discharge planning concerning a. Avoidance of modifiable risk factors - arrhythmia (caused by premature ventricular contraction) b. Cardiogenic shock - late sign is oliguria c. Left Congestive Heart Failure d. Thrombophlebitis - homan’s sign e. Stroke/CVA f. Post MI Syndrome/Dressler’s Syndrome - client is resistant to pharmacological agents, administer 150,000 – 450,000 units of streptokinase as ordered g. Resumption of ADL particularly sexual intercourse is 4 – 6 weeks post cardiac rehab, post CABG and instruct to - make sex as an appetizer rather than dessert - instruct client to assume a non weight bearing position - client can resume sexual intercourse if can climb staircase - dietary modification h. Strict compliance to mediation and importance of follow up care CONGESTIVE HEART FAILURE Inability of the heart to pump blood towards systemic circulation Types of Heart Failure 1. LEFT SIDED HEART FAILURE A. Predisposing Factors 1. 90% is mitral valve stenosis due to a. RHD – inflammation of mitral valve due to invasion of Grp. A beta-hemolytic streptococcus - Formation of aschoff bodies in the mitral valve - Common among children - ASO Titer (Anti streptolysin O titer) - Penicillin - Aspirin b. Aging 2. Myocardial Infarction 3. Ischemic heart disease 4. Hypertension 5. Aortic valve stenosis B. Signs and Symptoms 1. Dyspnea 2. Paroxysmal nocturnal dyspnea – client is awakened at night due to difficulty of breathing 3. Orthopnea – use 2 – 3 pillows when sleeping or place in high fowlers 4. Productive cough with blood tinged sputum 5. Frothy salivation 6. Cyanosis 7. Rales/Crackles 8. Bronchial wheezing 9. Pulsus Alternans – weak pulse followed by strong bounding pulse 10. PMI is displaced laterally due to cardiomegaly 11. There is anorexia and generalized body malaise 12. S3 – ventricular gallop C. Diagnostic Procedure 1. Chest x-ray – reveals cardiomegaly 2. PAP (pulmonary arterial pressure) – measures pressure in right ventricle or cardiac status PCWP (pulmonary capillary wedge pressure) – measures end systolic and dyastolic pressure - both are increased - done by cardiac catheterization (insertion of swan ganz catheter) 3. Ecocardiography – enlarged heart chamber (cardiomyopathy), dependent on extent of heart failure 4. ABG – reveals PO2 is decreased (hypoxemia), PCO 2 is increased (respiratory acidosis) 2. RIGHT SIDED HEART FAILURE A. Predisposing Factors 1. Tricuspid valve stenosis 2. Pulmonary embolism 3. Related to COPD 4. Pulmonic valve stenosis 5. Left sided heart failure B. Signs and Symptoms (venous congestion) 1. Neck/jugular vein distension 2. Pitting edema 3. Ascites 4. Weight gain 5. Hepatosplenomegaly 6. Jaundice 7. Pruritus 8. Anorexia 9. Esophageal varices C. Diagnostic Procedures 1. Chest x-ray – reveals cardiomegaly 2. Central venous pressure (CVP) - Measure pressure in right atrium (4 – 10 cm of water) - CVP fluid status measure - If CVP is less than 4 cm of water hypovolemic shock - Do the fluid challenge (increase IV flow rate) - If CVP is more than 10 cm of water hypervolemic shock - Administer loop diuretics as ordered - When reading CVP patient should be flat on bed - Upon insertion place client in trendelendberg position to promote ventricular filling and prevent pulmonary embolism 3. Ecocardiography – reveals enlarged heart chambers (cardiomyopathy 4. Liver enzymes – SGPT and SGOT is increased D. Nursing Management Goal: increase cardiac contractility thereby increasing cardiac output (3 – 6 L/min) 1. Enforce CBR 2. Administer medications as ordered a. Cardiac glycosides - Digoxin (Lanoxin) - Increase force of cardiac contraction - If heart rate is decreased do not give b. Loop Diuretics - Lasix (Furosemide) c. Bronchodilators d. Narcotic analgesics - Morphine Sulfate e. Vasodilators - Nitroglycerine f. Anti Arrhythmic - Lidocaine (Xylocane) 3. Administer oxygen inhalation with high inflow, 3 – 4 L/min, delivered via nasal cannula 4. High fowlers position 5. Monitor strictly vital signs, intake and output and ECG tracing 6. Measure abdominal girth daily and notify physician 7. Provide a dietary intake of low sodium, cholesterol and caffeine 8. Provide meticulous skin care 9. Assist in bloodless phlebotomy – rotating tourniquet, rotated clockwise every 15 minutes to promote decrease venous return 10. Provide client health teaching and discharge planning a. Prevent complications - Arrythmia - Shock - Right ventricular hypertrophy - MI - Thrombophlebitis b. Dietary modification c. Strict compliance to medications PERIPHERAL VASCULAR DISORDER Arterial Ulcer I. Thrombo Angitis Obliterans Burger’s Disease Reynaud’s Disease Venous Ulcer 1. Varicose Veins 2. Thrombophlebitis (deep vein thrombosis) THROMBOANGITIS OBLITERANS Acute inflammatory disorder usually affecting the small medium sized arteries and veins of the lower extremities A. Predisposing Factors 1. High risk groups – men 30 years old and above 2. Smoking B. Signs and Symptoms 1. Intermittent claudication – leg pain upon walking 2. Cold sensitivity and changes in skin color (pallor, cyanosis then rubor) 3. Decreased peripheral pulses 4. Trophic changes 5. Ulceration 6. Gangrene formation C. Diagnostic Procedures 1. Oscillometry – decrease in peripheral pulses 2. Doppler UTZ – decrease blood flow to the affected extremity 3. Angiography – reveals site and extent of malocclusion D. Nursing Management 1. Encourage a slow progressive physical activity a. walking 3 – 4 times a day b. out of bed 3 – 4 times a day 2. Administer medications as ordered a. Analgesics b. Vasodilators c. Anti coagulants 3. Institute foot care management 4. Instruct client to avoid smoking and exposure to cold environment 5. Assist in surgical procedure – bellow knee amputation REYNAUD’S DISEASE Disorder characterized by acute episodes of arterial spasm involving the fingers or digits of the hands A. Predisposing Factors 1. High risk group – female 40 years old and above 2. Smoking 3. Collagen diseases a. SLE (butterfly rash) b. Rheumatoid Arthritis 4. Direct hand trauma a. Piano playing b. Excessive typing c. Operating chainsaw B. Signs and Symptoms 1. Intermittent claudication – leg pain upon walking 2. Cold sensitivity and changes in skin color (pallor, cyanosis then rubor) 3. Trophic changes 4. Ulceration 5. Gangrene formation C. Diagnostic Procedures 1. Doppler UTZ – decrease blood flow to the affected extremity 2. Angiography – reveals site and extent of malocclusion D. Nursing Management 1. Administer medications as ordered a. Analgesics b. Vasodilators 2. Encourage to wear gloves 3. Instruct client on importance of cessation of smoking and exposure to cold environment VARICOSITIES Abnormal dilation of veins of lower extremities and trunks due to Incompetent valve resulting to Increased venous pooling resulting to Venous stasis causing Decrease venous return A. Predisposing Factors 1. Hereditary 2. Congenital weakness of veins 3. Thrombophlebitis 4. Cardiac disorder 5. Pregnancy 6. Obesity 7. Prolonged standing or sitting B. Signs and Symptoms 1. Pain after prolonged standing 2. Dilated tortuous skin veins 3. Warm to touch 4. Heaviness in legs C. Diagnostic Procedure 1. Venography 2. Trendelenburg’s Test - veins distends quickly in less than 35 seconds D. Nursing Management 1. Elevate legs above heart level to promote increased venous return by placing 2 – 3 pillows under the legs 2. Measure the circumference of leg muscle to determine if swollen 3. Wear anti embolic stockings 4. Administer medications as ordered a. Analgesics 5. Assist in surgical procedure a. Vein stripping and ligation (most effective) b. Sclerotherapy – can recur and only done in spider web varicosities and danger of thrombosis (2 – 3 years for embolism) THROMBOPHLEBITIS Deep vein thrombosis Inflammation of the veins with thrombus formation A. Predisposing Factors 1. Obesity 2. Smoking 3. Related to pregnancy 4. Chronic anemia 5. Prolong use of oral contraceptives – promotes lipolysis 6. Diabetes mellitus 7. Congestive heart failure 8. Myocardial infarction 9. Post op complication 10. Post cannulation – insertion of various cardiac catheter 11. Increase in saturated fats in the diet. B. Signs and Symptoms 1. Pain at affected extremity 2. Warm to touch 3. Dilated tortuous skin veins 4. Positive Hpman’s Signs – pain at the calf or leg muscle upon dorsi flexion of the foot C. Diagnostic Procedure 1. Venography 2. Angiography D. Nursing Management 1. Elevate legs above heart level to promote increase venous return 2. Apply warm moist pack – to reduce lymphatic congestion 3. Measure circumference of leg muscle to determine if swollen 4. Encourage to wear anti embolic stockings or knee elastic stockings 5. Administer medications as ordered a. Analgesics b. Anti Coagulant - Heparin 6. Monitor for signs of complications Embolism a. Pulmonary - Sudden sharp chest pain - Unexplained dyspnea - Tachycardia - Palpitations - Diaphoresis - Restlessness b. Cerebral - Headache - Dizziness - Decrease LOC MURPHY’S SIGN is seen in clients with cholelithiasis, cholecystitis characterized by pain at the right upper quadrant with tenderness RESPIRATORY SYSTEM OVERVIEW OF THE STRUCTURES AND FUCNTIONS OF THE RESPIRATORY SYSTEM I. Upper Respiratory System 1. Filtering of air 2. Warming and moistening of air 3. Humidification A. Nose - Cartillage - Right nostril - Left nostril - Separated by septum - Consist of anastomosis of capillaries known as Keissel Rach Plexus (the site of nose bleeding) B. Pharynx/Throat - Serves as a muscular passageway for both food and air C. Larynx - For phonation (voice production) - For cough reflex Glottis - Opening of larynx - Opens to allow passage of air - Closes to allow passage of food going to the esophagus - The initial sign of complete airway obstruction is the inability to cough II. Lower Respiratory System - For gas exchange A. Trachea/Windpipe - Consist of cartilaginous rings - Serves as passageway of air going to the lungs - Site of tracheostomy B. Bronchus - Right main bronchus - Left main bronchus C. Lungs - Right lung (consist of 3 lobes, 10 segments) - Left lung (consist of 2 lobes, 8 segments) - Serous membranes Pleural Cavity a. Pareital b. Pleural fluid c. Visceral With Pleuritic Friction Rub a. Pneumonia b. Pleural effusion c. Hydrothorax (air and blood in pleural space Alveoli - Site of gas exchange (CO2 and O2) - Diffusion (Dalton’s law of partial pressure of gases) Respiratory Distress Syndrome - Decrease oxygen stimulates breathing - Increase carbon dioxide is a powerful stimulant for breathing Type II Cells of Alveoli - Secretes surfactant - Decrease surface tension - Prevent collapse of alveoli - Composed of lecithin and spingomyelin - L/S ratio to determine lung maturity - Normal L/S ratio is 2:1 - In premature infants 1:2 - Give oxygen of less 40% in premature to prevent atelectasis and retrolental fibroplasias - retinopathy/blindness in prematurity Disorders of Respiratory System 1. PTB/Pulmonary Tuberculosis (Koch’s Disease) - Infection of lung tissue caused by invasion of mycobacterium tuberculosis or tubercle bacilli - An acid fast, gram negative, aerobic and easily destroyed by heat or sunlight A. Precipitating Factors 1. Malnutrition 2. Overcrowded places 3. Alcoholism 4. Over fatigue 5. Ingestion of an infected cattle with mycobacterium bovis 6. Virulence (degree of pathogenecity) of microorganism B. Mode of Transmission 1. Airborne transmission via droplet nuclei C. Signs and Symptoms 1. Low grade afternoon fever, night sweats 2. Productive cough (yellowish sputum) 3. Anorexia, generalized body malaise 4. Weight loss 5. Dyspnea 6. Chest pain 7. Hemoptysis (chronic) D. Diagnostic Procedure 1. Mantoux Test (skin test) - Purified protein derivative - DOH 8 – 10 mm induration, 48 – 72 hours - WHO 10 – 14 mm induration, 48 – 72 hours - Positive Mantoux test (previous exposure to tubercle bacilli but without active TB) 2. Sputum Acid Fast Bacillus - Positive to cultured microorganism 3. Chest X-ray - Reveals pulmonary infiltrates 4. CBC - Reveals increase WBC E. Nursing Management 1. Enforce CBR 2. Institute strict respiratory isolation 3. Administer oxygen inhalation 4. Force fluids to liquefy secretions 5. Place client on semi fowlers position to promote expansion of lungs 6. Encourage deep breathing and coughing exercise 7. Nebulize and suction when needed 8. Comfortable and humid environment 9. Institute short course chemotherapy a. Intensive phase - INH (Isonicotinic Acid Hydrazide) - Rifampicin (Rifampin) - PZA (Pyrazinamide) - Given everyday simultaneously to prevent resistance - INH and Rifampicin is given for 4 months, taken before meals to facilitate absorption - PZA is given for 2 months, taken after meals to facilitate absorption - Side Effect INH: peripheral neuritis/neuropathy (increase intake of Vitamin B6/Pyridoxine) - Side Effect Rifampicin: all bodily secretions turn to red orange color - Side Effect PZA: allergic reaction, hepatotoxicity, nephrotoxicity - PZA can be replaced by Ethambutol - Side Effect Ethambutol: optic neuritis b. Standard phase - Injection of streptomycin (aminoglycoside) - Kanamycin - Amikacin - Neomycin - Gentamycin - Side Effect: - Ototoxicity damage to the 8th cranial nerve resulting to tinnitus leading to hearing loss - Nephrotoxicity check for BUN and Creatinine - Give aspirin if there is fever - Side Effect: tinnitus, dyspepsia, heartburn 10. Provide increase carbohydrates, protein, vitamin C and calories 11. Provide client health teaching and discharge planning a. Avoidance of precipitating factors b. Prevent complications (atelectasis, military tuberculosis) PTB - Bones (potts) - Meninges - Eyes - Skin - Adrenal gland c. Strict compliance to medications d. Importance of follow up care PNEUMONIA Inflammation of the lung parenchyma leading to pulmonary consolidation as the alveoli is filled with exudates A. Etiologic Agents 1. Streptococcus Pneumonae – causing pneumococal pneumonia 2. Hemophylus Influenzae – causing broncho pneumonia 3. Diplococcus Pneumoniae 4. Klebsella Pneumoniae 5. Escherichia Pneumoniae 6. Pseudomonas B. High Risk Groups 1. Children below 5 years old 2. Elderly C. Predisposing Factors 1. Smoking 2. Air pollution 3. Immuno compromised a. AIDS - Pneumocystic carini pneumonia - Drug of choice is Retrovir b. Bronchogenic Cancer - Initial sign is non productive cough - Chest x-ray confirms lung cancer 4. Related to prolonged immobility (CVA clients), causing hypostatic pneumonia 5. Aspiration of food causing aspiration pneumonia D. Signs and Symptoms 1. Productive cough with greenish to rusty sputum 2. Dyspnea with prolong expiratory grunt 3. Fever, chills, anorexia and general body malaise 4. Weight loss 5. Rales/crackles 6. Bronchial wheezing 7. Cyanosis 8. Pleuritic friction rub 9. Chest pain 10. Abdominal distention leading to paralytic ileus (absence of peristalsis) E. Diagnostic Procedure 1. Sputum Gram Staining and Culture Sensitivity – positive to cultured microorganisms 2. Chest x-ray – reveals pulmonary consolidation 3. ABG analysis – reveals decrease PO2 4. CBC – reveals increase WBC, erythrocyte sedimentation rate is increased F. Nursing Management 1. Enforce CBR 2. Administer oxygen inhalation low inflow 3. Administer medications as ordered Broad Spectrum Antibiotic a. Penicillin b. Tetracycline c. Microlides (Zethromax) - Azethromycin (Side Effect: Ototoxicity) - Antipyretics - Mucolytics/Expectorants - Analgesics 4. Force fluid 5. Place on semi fowlers position 6. Institute pulmonary toilet (tends to promote expectoration) - Deep breathing exercises - Coughing exercises - Chest physiotherapy - Turning and reposition 7. Nebulize and suction as needed 8. Assist in postural drainage - Drain uppermost area of lungs - Placed on various position Nursing Management for Postural Drainage a. Best done before meals or 2 – 3 hours to prevent gastro esophageal reflux b. Monitor vital signs c. Encourage client deep breathing exercises d. Administer bronchodilators 15 – 30 minutes before procedure e. Stop if client cannot tolerate procedure f. Provide oral care after procedure g. Contraindicated with - Unstable vital signs - Hemoptysis - Clients with increase intra ocular pressure (Normal IOP 12 – 21 mmHg) - Increase ICP 9. Provide increase carbohydrates, calories, protein and vitamin C 10. Health teaching and discharge planning a. Avoid smoking b. Prevent complications - Atelectasis - Meningitis (nerve deafness, hydrocephalus) c. Regular adherence to medications d. Importance of follow up care HISTOPLASMOSIS Acute fungal infection caused by inhalation of contaminated dust or particles with histoplasma capsulatum derived from birds manure A. Signs and Symptoms PTB or Pneumonia like 1. Productive cough 2. Dyspnea 3. Fever, chills, anorexia, general body malaise 4. Cyanosis 5. Hemoptysis 6. Chest and joint pains B. Diagnostic Procedures 1. Histoplasmin Skin Test – positive 2. ABG analysis PO2 decrease C. Nursing Management 1. Enforce CBR 2. Administer oxygen inhalation 3. Administer medications as ordered a. Antifungal - Amphotericin B - Fungizone (Nephrotoxicity, check for BUN and Creatinine, Hypokalemia) b. Steroids c. Mucolytics d. Antipyretics 4. Force fluids to liquefy secretions 5. Nebulize and suction as needed 6. Prevent complications – bronchiectasis 7. Prevent the spread of infection by spraying of breeding places COPD (Chronic Obstructive Pulmonary/Lung Disease) Chronic Bronchitis Inflammation of bronchus resulting to hypertrophy or hyperplasia of goblet mucous producing cells leading to narrowing of smaller airways A. Predisposing Factors 1. Smoking 2. Air pollution B. Signs and Symptoms 1. Productive cough (consistent to all COPD) 2. Dyspnea on exertion 3. Prolonged expiratory grunt 4. Anorexia and generalized body malaise 5. Scattered rales/ronchi 6. Cyanosis 7. Pulmonary hypertension a. Peripheral edema b. Cor Pulmonale (right ventricular hypertrophy) C. Diagnostic Procedure ABG analysis – reveals PO2 decrease (hypoxemia), PCO2 increase, pH decrease Bronchial Asthma Reversible inflammatory lung condition due to hypersensitivity to allergens leading to narrowing of smaller airways A. Predisposing Factors (Depending on Types) 1. Extrinsic Asthma ( Atopic/ Allergic ) Causes a. Pollen b. Dust c. Fumes d. Smoke e. Gases f. Danders g. Furs h. Lints 2. Intrinsic Asthma (Non atopic/Non allergic) Causes a. Hereditary b. Drugs (aspirin, penicillin, beta blocker) c. Foods (seafoods, eggs, milk, chocolates, chicken d. Food additives (nitrates) e. Sudden change in temperature, air pressure and humidity f. Physical and emotional stress 3. Mixed Type 90 – 95% B. Signs and Symptoms 1. Cough that is non productive 2. Dyspnea 3. Wheezing on expiration 4. Cyanosis 5. Mild Stress/apprehension 6. Tachycardia, palpitations 7. Diaphoresis C. Diagnostic Procedure 1. Pulmonary Function Test - Incentive spirometer reveals decrease vital lung capacity 2. ABG analysis – PO2 decrease - Before ABG test for positive Allens Test, apply direct pressure to ulnar and radial artery to determine presence of collateral circulation D. Nursing Management 1. Enforce CBR 2. Oxygen inhalation, with low inflow of 2 – 3 L/min 3. Administer medications as ordered a. Bronchodilators – given via inhalation or metered dose inhalaer or MDI for 5 minutes b. Steroids – decrease inflammation c. Mucomysts (acetylceisteine) d. Mucolytics/expectorants e. Anti histamine 4. Force fluids 5. Semi fowlers position 6. Nebulize and suction when needed 7. Provide client health teachings and discharge planning concerning a. Avoidance of precipitating factor b. Prevent complications - Emphysema - Status Asthmaticus (give drug of choice) - Epinephrine - Steroids - Bronchodilators c. Regular adherence to medications to prevent development of status asthmaticus d. Importance of follow up care BRONCHIECTASIS Abnormal permanent dilation of bronchus leading to destruction of muscular and elastic tissues of alveoli A. Predisposing Factors 1. Recurrent lower respiratory tract infections 2. Chest trauma 3. Congenital defects 4. Related to presence of tumor B. Signs and Symptoms 1. Productive cough 2. Dyspnea 3. Cyanosis 4. Anorexia and generalized body malaise 5. Hemoptysis (only COPD with sign) C. Diagnostic Procedure 1. ABG – PO2 decrease 2. Bronchoscopy – direct visualization of bronchus using fiberscope Nursing Management PRE Bronchoscopy 1. Secure inform consent and explain procedure to client 2. Maintain NPO 6 – 8 hours prior to procedure 3. Monitor vital signs and breath sound POST Bronchoscopy 1. Feeding initiated upon return of gag reflex 2. Avoid talking, coughing and smoking, may cause irritation 3. Monitor for signs of gross 4. Monitor for signs of laryngeal spasm – prepare tracheostomy set D. Treatment 1. Surgery (pneumonectomy , 1 lung is removed and position on affected side) 2. Segmental Wedge Lobectomy (promote re expansion of lungs) - Unaffected lobectomy facilitate drainage EMPHYSEMA Irreversible terminal stage of COPD characterized by a. Inelasticity of alveoli b. Air trapping c. Maldistribution of gases d. Over distention of thoracic cavity (barrel chest) A. Predisposing Factors 1. Smoking 2. Air pollution 3. Allergy 4. High risk: elderly 5. Hereditary – it involves deficiency of ALPHA-1 ANTI TRYPSIN (needed to form Elastase, for recoil of alveoli) B. Signs and Symptoms 1. Productive cough 2. Dyspnea at rest 3. Prolong expiratory grunt 4. Anorexia and generalized body malaise 5. Resonance to hyperresonance 6. Decrease tactile fremitus 7. Decrease or diminished breath sounds 8. Rales or ronchi 9. Bronchial wheezing 10. Barrel chest 11. Flaring of alai nares 12. Purse lip breathing to eliminates excess CO2 (compensatory mechanism) C. Diagnostic Procedure 1. Pulmonary Function Test – reveals decrease vital lung capacity 2. ABG analysis reveals a. Panlobular/ centrilobular - Decrease PO2 (hypoxemia leading to chronic bronchitis, “Blue Bloaters”) - Decrease ph - Increase PCO2 - Respiratory acidosis b. Panacinar/ centriacinar - Increase PO2 (hyperaxemia, “Pink Puffers”) - Decrease PCO2 - Increase ph - Respiratory alkalosis D. Nursing Management 1. Enforce CBR 2. Administer oxygen inhalation via low inflow 3. Administer medications as ordered a. Bronchodilators b. Steroids c. Antibiotics d. Mucolytics/expectorants 4. High fowlers position 5. Force fluids 6. Institute pulmonary toilet 7. Nebulize and suction when needed 8. Institute PEEP (positive end expiratory pressure) in mechanical ventilation promotes maximum alveolar lung expansion 9. Provide comfortable and humid environment 10. Provide high carbohydrates, protein, calories, vitamins and minerals 11. Health teachings and discharge planning concerning a. Avoid smoking b. Prevent complications - Atelectasis - Cor Pulmonale - CO2 narcosis may lead to coma - Pneumothorax c. Strict compliance to medication d. Importance of follow up care