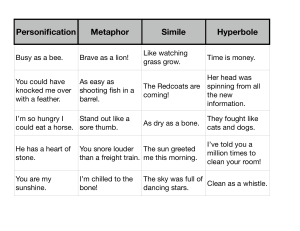
Bone Tissue Engineering Presented by Mariah Udeh What is Bone Tissue Engineering? • Bone tissue engineering (BTE) is an upcoming field with a goal to develop and help the fight with limitations of traditional treatments of bone disease • Bone is a vascularized tissue that must provide a firm structural support, withstand load bearing, and rapidly respond to metabolic demand (Amini et al., 2012). • A bone defect is defined as a loss of bone where it should normally appear. Possible causes of bone defects are the following trauma, tumor, or infection (osteomyelitis) • The standard treatment of bone defects are autografts which are in finite supply and most importantly donor site morbidity is a huge problem. Endochondral bone formation • Endochondral bone formation (Fig. 8.2) involves mesenchymal progenitor cells differentiating into chondrocytes. ( Elsevier) • Chondrocytes are responsible for depositing a cartilaginous template that is later mineralized and replaced by bone (Gilbert & Sunderland) • Requires: • Several growth factors— bone morphogenetic proteins (BMPs), vascular endothelial growth factor (VEGF), and fibroblast growth factors (FGFs) Tissue Engineering Made Easy. 2016. Elsevier. Current methods of Bone Tissue Engineering • Development of biocompatible and biodegradable scaffolds • Designing bioreactors to improve in vitro osteogenic priming • “ Identifying growth factors which can induce or promote endogenous bone and vascular formation.” (Baro et.al 2013) • Essential components for successful bone formation include the following appropriate cells, a biocompatible scaffold, growth factors, and vascularization to meet the growing tissue nutrient supply • Most recently Three-Dimensional (3D) printing of scaffolds Background of 3D printing: • 3D printing’s origin can be traced back to the 19th century, when photo sculpture and geomorphology technologies were developed. • 3D printing is an adaptable technique to fabricate an assortment of materials to include the following polymers, ceramics, metals and composites, with customized shapes and dense or macro/micro porous architecture • “Among numerous methods, 3D printing has been considered as an advantageous technique in fabricating tissue engineering scaffolds, as the 3D printed macro-micro structure could morphologically mimic the multi-scale structure of human body tissues.”(Wang et.al) • Different 3D printing techniques include fused deposition modeling (FDM), Selective Laser Sintering (SLS), stereolithography selective laser melting ink jet 3D printing, adhesive droplet and powder bed-based AM. Types of Scaffolds created via 3D printing techniques Table 1 Comparison of bone tissue engineering scaffolds made through different 3D printing techniques. (Wang et.al) Types of Scaffolds created via 3D printing techniques ( continued) Table 1 Comparison of bone tissue engineering scaffolds made through different 3D printing techniques. (Wang et.al) My Experiment • “Bone marrow–derived mesenchymal stem cells (BMSCs) are the most studied adult stem cells for skeletal tissue regeneration and have demonstrated broad potential.” Leong et.al • Objective: • To fabricate a composite Silk Fibroin (SF) / polysulfone Si(OH)4 scaffold via SLS 3D printing for regeneration of cartilage in-vitro • Fuse 1 Selective Laser Sintering (SLS) 3D printer • Manufactured by Formlabs in the United States • Price: $9,999.00 USD Materials • Growth factor of my experiment: • Bone Morphogenetic protein- 2 ( BMP-2) belongs to the TGFβ family and are most commonly known to affect bone formation. • BMP-2 can activate Mesenchymal stem cells (MSCs) to create osteoblasts and has an enormous effect on differentiation. • “Multiple BMPs, including BMP2, BMP6, BMP7 and BMP9, promote osteoblastic differentiation of MSCs both in vitro and in vivo” (Beederman et.al) • Bone Morphogenetic protein- 2 ( BMP-2) growth factor for bone osteocytes cells. Methods (biocompatibility) • Human bone marrow-derived mesenchymal stem cells(hBMSCs) were used to test for biocompatibility. Cell isolation was completed first and cells were then subcultured to obtain hBMSCs. • Silk from the Bombyx mori (silkworm) (natural biodegradable polymer) has excellent biocompatibility due to its mechanical execution, adjustable degradation, and easy accessibility to acquire from the sericulture industry • Polysulfone Bioceramic composite(biodegradable) • Gamma irradiation was used for sterilization of scaffold. • To sterilize biodegradable scaffolds radiation methods offer multiple benefits to include lower temperatures, cheaper cost, and shortness in processing time.(Dai et.al) Methods • Fabrication of SF / Si(OH)4 scaffolds by 3D printing • The domesticated silkworm (Bombyx mori)’s cocoon was used for extraction of silk fibroin. Silk fibroin was boiled in Sodium bicarbonate solution (0.6 %) for the degumming process. Wei et.al Methods continued • 40 wt % SF solution and Si(OH)4 powders were combined together to create a paste in order begin 3D Selective Laser Sintering (SLS) printing of the scaffold. • 3D printer ink is hydroxyapatite (HA) which is a ceramic powder. • Finally after printing the composite scaffold SF/ Si(OH)4 will be immersed in ethanol to cross link. • Finally hBMSC cells and BMP-2 were seeded on 3D printed Silk Fibroin (SF)/ Polysulfone(Si(OH)4 composite scaffolds (1 x 105 cells each scaffold) with culture medium then cells were cultured at 37 degrees Celsius for 7 days Conclusion & Results • What does the differentiation of MSCs in vitro depend on? • According to Mackay et.al Culture conditions must include MSCs plus growth factors (e.g., transforming growth factor-ß (TGF-ß) familychondrogenic differentiation) • In my experiment the culture conditions are hBMSCs plus BMP2 growth factor Park et.al • Results: After 28 days, chondrocytes were formed in vitro and was shown by performing Scanning Electron Microscopy (SEM) analysis. • Study shows that cartilage can be regenerated, however further studies are required to test in-vivo of scaffold in animal models which could be used to test if scaffold can be a replacement in long bone including proper strength and mechanical stability. “Chondrocytes : Chondrocytes produce all of the structural components of cartilage, including collagen, proteoglycans and glycosaminoglycans” Yale.edu/histology connective tissue lab Chondrocytes distribution on the designed 3D-printed scaffolds. (A-D) SEM images showing the adhesion of chondrocytes after (A) 1, (B) 3, (C) 5, and (D) 7 h (Biomedicine & Pharmacotherapy) References • “Bone Defects.” 2017. Paley Orthopedic & Spine Institute. https://paleyinstitute.org/blog/conditions/bone-defects/ (May 1, 2020). • Tissue Engineering Made Easy. 2016. Elsevier. https://linkinghub.elsevier.com/retrieve/pii/C20150043581 (May 1, 2020). • Bao, Chao Le Meng et al. 2013. “Advances in Bone Tissue Engineering.” Regenerative Medicine and Tissue Engineering. https://www.intechopen.com/books/regenerative-medicine-and-tissue-engineering/advances-in-bone-tissueengineering (May 4, 2020). • Wang, Chong et al. 2020. “3D Printing of Bone Tissue Engineering Scaffolds.” Bioactive Materials 5(1): 82–91. • Park, In-Kyu, and Chong Cho. 2010. “Stem Cell-Assisted Approaches for Cartilage Tissue Engineering.” International journal of stem cells 3: 96–102. • “3D Printing of Silk Fibroin-Based Hybrid Scaffold Treated with Platelet Rich Plasma for Bone Tissue Engineering | Elsevier Enhanced Reader • https://www.aniwaa.com/buyers-guide/3d-printers/best-professional-desktop-sls-3d-printers/ • https://www.aniwaa.com/product/3d-printers/formlabs-fuse-1/ • Beederman, Maureen et al. 2013. “BMP Signaling in Mesenchymal Stem Cell Differentiation and Bone Formation.” Journal of biomedical science and engineering 6(8A): 32–52. • Cao, Yang, and Bochu Wang. 2009. “Biodegradation of Silk Biomaterials.” International Journal of Molecular Sciences 10(4): 1514–24. • Bone Marrow Derived Mesenchymal Stem Cells Augmented Mesh Scaffold for Wound Healing in Guinea Pig.” Biomedicine & Pharmacotherapy 121: 109573. • http://medcell.med.yale.edu/histology/connective_tissue_lab/chondrocytes.php Questions?